21 August 2023: Database Analysis
Impact of Preoperative Video-Based Education on Anxiety Levels in Patients with Renal Stones Scheduled for Flexible Ureteroscopic Lithotripsy: A Comparative Study Using APAIS and STAI
Mustafa Karalar1ABDEF*, Arif Demirbas1ABF, Osman Gercek1BC, Kutay Topal1BDF, Ibrahim Keles1ACEDOI: 10.12659/MSM.941351
Med Sci Monit 2023; 29:e941351
Abstract
BACKGROUND: Anxiety prior to surgery can impact patient outcomes and satisfaction. In light of this, our study aimed to examine the effects of preoperative video-based information versus verbal information on anxiety levels among 60 patients with renal stones slated for flexible ureteroscopic lithotripsy. Anxiety was measured using the Amsterdam Pre-Operative Anxiety and Information Scale (APAIS) and the State-Trait Anxiety Inventory (STAI).
MATERIAL AND METHODS: We enrolled 60 patients with renal stones who were scheduled for flexible ureteroscopic lithotripsy. These patients were divided randomly into two groups: Group 1 (30 patients) received preoperative video-based information and Group 2 (30 patients) received only verbal information. Anxiety levels were assessed preoperatively using both the APAIS and STAI. On the first postoperative day, each patient indicated their pain using a visual analogue scale and filled out a questionnaire about their willingness to undergo the procedure again.
RESULTS: Group 1 exhibited lower anxiety levels as reflected by the APAIS scores for anesthesia (P=0.02), surgery (P<0.001), overall (P<0.001), and information needs (P<0.001). While there was no significant difference in the STAI-trait anxiety scores between the groups (P=0.15), Group 2 demonstrated notably higher anxiety levels concerning the surgical procedure, as measured by the STAI-state scores (P<0.001). The average pain score was 4.23±2.17 for Group 1 and 5.37±2.83 for Group 2 (P=0.08). Patients in Group 1 showed a greater willingness to undergo the surgery again (P=0.02).
CONCLUSIONS: Delivering preoperative information through videos significantly diminishes anxiety levels in patients about to undergo retrograde intrarenal surgery compared to traditional verbal communication.
Keywords: Anxiety, Instructional Film and Video, Ureteroscopy, Humans, Kidney Calculi, Lithotripsy, Pain
Background
The prevalence rate of renal stone disease, known since the time of Hippocrates, has increased, especially over the last 3 decades [1]. The recurrence rate is high, ranging from 50% to 75% [2]. The high prevalence and recurrence rates render urolithiasis a serious social, economic, and health issue [1]. New technological developments have led to high success rates for kidney stone treatments. Stones were previously removed via with surgery, but shock wave lithotripsy, retrograde intrarenal surgery (RIRS) and percutaneous nephrolithotomy are now the most commonly used modalities [1,3].
Stone size, composition, and location, renal anomalies, and any previous treatments determine the surgical method [3]. The current guidelines recommend RIRS as the first-line treatment for kidney stones <2 cm or <1 cm for lower-pole stones [4,5]. In this surgical method, kidney stones are treated endourologically with a transureteral approach using flexible ureterenoscopes. Although RIRS is minimally invasive, some complications can develop related to surgery or anesthesia [6,7]. Renal colic, pyelonephritis, hematuria, and acute urinary retention can occur as early complications. There is even a risk of death due to anesthesia or sepsis [8]. These complication risks can cause anxiety in patients scheduled for RIRS.
Most patients experience varying degrees of anxiety before surgery. Fear of death, anesthesia, failure to recover, and organ injury can cause anxiety [9]. Fear of the unknown is another important factor causing high levels of anxiety [10]. Before surgery, every patient is informed about the procedure. Various methods can be used to impart such information [11–13]. Clinicians usually deliver information verbally, but the patient may not clearly understand, thus increasing stress and anxiety. A visual explanation is easier to understand and may reduce anxiety. There are several studies in the literature about decreased anxiety with preoperative video-based information before different types of procedures, such as percutaneous nephrolithotomy, transrectal prostate biopsy, and inguinal hernioplasty [11–13].
In this study, we aimed to compare a preoperative video-based information delivery with verbal information and anxiety levels in 60 patients with renal stones scheduled for flexible ureteroscopic lithotripsy evaluated using the Amsterdam Pre-Operative Anxiety and Information Scale (APAIS) and the State-Trait Anxiety Inventory (STAI).
Material and Methods
ETHICS STATEMENT:
This study was approved by the local ethics committee (AFSU 2011-KAEK-2/2021/374) and was conducted in accordance with the ethical standards of the Declaration of Helsinki. Informed consent was obtained from all patients included in the study.
PATIENTS AND STUDY DESIGN:
Sixty patients with renal stones scheduled for flexible ureteroscopic lithotripsy in our clinic between July 2021 and June 2022 were enrolled. Patients with urinary tract infections, a history of previous RIRS treatment, stones that could not be reached because of ureteral stenosis or kinking, patients with ureteral stents or renal colic were excluded, as were those for whom access sheathes could not be inserted into the ureter. All patients were older than 18 years; those with a history of alcohol or drug abuse or visual or hearing impairment, were excluded. A detailed anamnesis was obtained from all patients, and physical examinations were performed. X-ray of the kidneys, ureters, and bladder and ultrasound or computed tomography was used for urinary system imaging. Patient demographic characteristics (age, sex, educational level, and marital status), radiological parameters (stone side, size, and location), and surgical parameters (operation time and stone-free status) were recorded.
Patients were randomized to 2 groups, one by one. Preoperative video-based information was provided to the 30 patients in group 1, but only verbal information was provided to the 30 patients in group 2. The European Association of Urology (EAU) patient information video was translated into Turkish and dubbed again by us. [14]. The animated video was used with permission of the EAU. The video contains detailed information on all steps of ureteroscopy. The video was presented by the same clinician to all group 1 patients, who were encouraged to ask questions of the clinician when watching the video. All preoperative verbal patient information was provided to group 2 by the same clinician.
ANXIETY EVALUATION:
The APAIS and STAI were completed by all patients before surgery.
APAIS: The APAIS was developed by Moerman et al to evaluate preoperative anxiety [15]. In this test, anxiety is divided into anxiety about surgery, anesthesia, or a lack of knowledge. There are 6 questions, and the answers are transformed into numerical scores on a 5-point Likert scale. High scores indicate more anxiety and a greater desire for information.
STAI: The STAI is a Likert-type scale with 20 questions that measure state and trait anxiety levels. The STAI-state scale determines how a patient feels “right now”, while the STAI-trait scale measures how a patient “generally feels”. Lower scores indicate less anxiety [16].
SURGICAL TECHNIQUE:
All surgeries were performed under general anesthesia. Routine cystoscopy (19-Fr; Karl Storz, Tuttlingen, Germany) was performed on all patients, and a safety guidewire was inserted in the kidney under the guidance of fluoroscopy. A semi-rigid ureteroscope (8-Fr, Karl Storz, Germany) was used for ureteroscopy, and a second guidewire was inserted after cystoscopy. After placement of the ureteral access sheath under fluoroscopy, flexible ureteroscopy (Flex-X2; Karl Storz) proceeded, and lithotripsy was performed using a Holmium-YAG laser (Sphinx Holmium Laser 30w; LISA Laser Products, Katlenburg-Lindau, Germany). All surgeries were completed by placing JJ ureteric stents.
PAIN AND WILLINGNESS EVALUATION:
Each patient used the VAS and completed the willingness questionnaire on postoperative day 1.
STATISTICAL ANALYSIS:
We used IBM SPSS Statistics (version 21.0; IBM Corp, Armonk, NY, USA) for MS Windows. The Kolmogorov-Smirnov test was used to determine whether variables were normally distributed. The normally distributed data (age, operation time, STAI-state, STAI-trait) were compared using the independent-samples
Results
PATIENT CHARACTERISTICS:
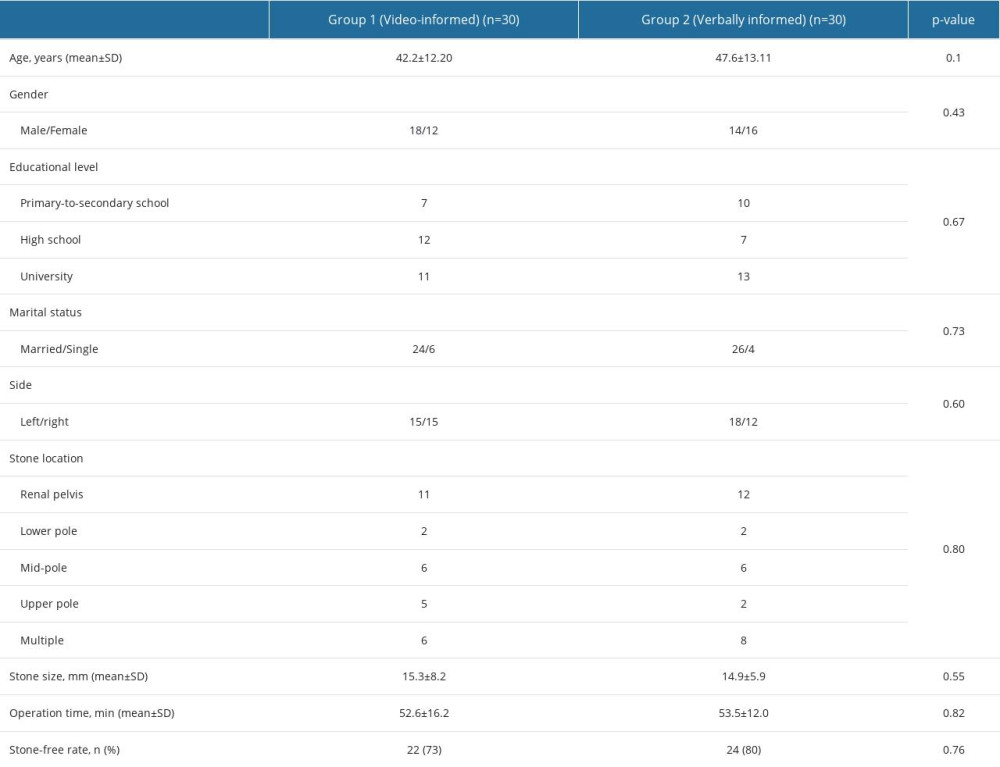
The demographic characteristics and radiological and surgical parameters are shown in Table 1. There were no differences in age, sex, marital status, operation time, stone side, location, or size, and the stone-free rate between the 2 groups.
ANXIETY-RELATED PARAMETERS:
The preoperative anxiety scores and postoperative mean pain and willingness scores are shown in Table 2. The APAIS anesthesia (P=0.02), surgery (P<0.001), total (P<0.001), and need for information (P<0.001) scores revealed lower anxiety levels in group 1. There were no significant group differences in STAI-trait anxiety scores (P=0.15), but STAI-state scores indicated high anxiety levels regarding the surgical procedure in group 2 (P<0.001).
PAIN AND WILLINGNESS:
The mean pain scores of patients were 4.23±2.17 in group 1 and 5.37±2.83 in group 2 (
Discussion
In this study, we evaluated the effect of video education on preoperative anxiety levels and found that patients who received RIRS video education had lower anxiety levels than did verbally informed patients. RIRS has become an essential component of stone management, and given the developments in endoscopic instruments and laser technology, the stone-free rates are high. Although RIRS is minimally invasive, it can nonetheless cause anxiety. Abate et al, in a systematic review and meta-analysis, found that the prevalence of preoperative anxiety was 48% [17]. Prolonged high levels of anxiety affect neuroendocrine function and increase the need for anesthesia and analgesics and the postoperative pain severity and recovery time from anesthesia [18]. Lin et al showed that inadequate preoperative information can cause anxiety [19]. Patients should be well informed before surgery, but preoperative verbal or written information can be insufficient [11–13].
In our study, we found that preoperative video-based information significantly reduced patient anxiety before RIRS. The APAIS anxiety scores were statistically lower in the video-informed group.
When the APAIS subgroups were examined, we observed that the APAIS anesthesia scores were also lower in video-informed group. The operation process should be evaluated as a whole, starting from the patient’s entry into the operating room and continuing to the patient’s awakening and removal from the room. We think that a decrease in anxiety level occurring in one or more of the components within this holistic approach can also affect other components. In this context, a decrease in APAIS surgery score may have led to a decrease in APAIS anesthesia score, although there is no detailed information about anesthesia in the information video.
In terms of the STAI scores, the general anxiety (STAI-trait) scores were similar in both groups, but the situational anxiety (STAI-state) scores were lower in the video-informed group. To the best of our knowledge, this is the first study on patients undergoing RIRS [11–13,20].
Patients can be educated verbally or using written materials before various procedures to reduce anxiety, but standardization of such methods is difficult [21]. Doctor-patient communication must be very good if verbal information is to be given. Ineffectiveness of this communication leads to patient dissatisfaction and complaints. A good doctor-patient relationship can increase patients’ self-confidence, motivation, and positive view of their health status, which can influence their health outcomes. But patients’ anxiety and fear and doctors’ burden of work can negatively affect this communication [22]. The physician must explain the procedure in a way that the patient fully understands. Patient reading and comprehension skills must be considered, and therefore, written information must be simple and comprehensible. Video-based education is easy to provide. Bozkurt et al reported that video education before percutaneous nephrolithotomy to remove kidney stones reduced anxiety more than verbal and written information [13]. In a study by Esen et al, it was shown that video-based information before stereotactic radiosurgery and stereotactic body radiation therapy significantly reduced anxiety levels in patients [21]. Tarhan et al showed that video-based education before transrectal prostate biopsy significantly reduced STAI-state scores [11]. Erdogan et al reported similar results in patients undergoing skin biopsy [23]. Tan et al reported lower anxiety levels in video-informed patients undergoing surgery for breast cancer [24]. In a study by Yang et al, it was shown that during flexible ureteroscopic lithotripsy, doctor-patient communication combined with real-time video significantly reduced patient anxiety and depression [25]. Similarly, we found that pre-procedural video education significantly reduced anxiety.
We also explored whether patients were willing to undergo repeat treatment if necessary and found that video-informed patients were more willing. The mean postoperative pain scores were lower in video-informed patients, but not significantly. Ketelaars et al reported similar results [20]. In another study, Padilla et al showed that self-visualization of cystoscopy did not impact pain perception in male patients [26].
We used an animated, 3-min EAU information video with colorful visuals, available on the EAU website. It is easy to understand, and patients can ask questions of the physician when watching the video.
The present study has several limitations. First, there is no information about anesthesia in the patient information video. Second, we excluded patients with a history of renal stone surgery, and patients who had a history of anesthesia for other reasons were not recorded. Anesthesia-related anxiety may be lower in patients with a previous history of anesthesia. The lack of patient comprehension and knowledge assessment can be another limitation of our study.
Conclusions
As is true of all surgeries, RIRS can cause patients stress, anxiety, and fear. Informing the patient preoperatively can reduce anxiety, but verbal information alone may not be sufficient. Preoperative video-based information delivery significantly reduces patient anxiety before RIRS, compared with verbal information. Video-based delivery can be widely used to inform patients preoperatively.
References
1. Raheem OA, Khandwala YS, Sur RL, Burden of urolithiasis: Trends in Prevalence, treatments, and costs: Eur Urol Focus, 2017; 3(1); 18-26
2. Moe OW, Kidney stones: Pathophysiology and medical management: Lancet, 2006; 367(9507); 333-44
3. Desai M, Sun Y, Buchholz N, Treatment selection for urolithiasis: Percutaneous nephrolithomy, ureteroscopy, shock wave lithotripsy, and active monitoring: World J Urol, 2017; 35(9); 1395-99
4. Assimos D, Krambeck A, Miller NL, Surgical Management of Stones: American Urological Association/Endourological Society Guideline, Part II: J Urol, 2016; 196(4); 1161-69
5. Türk C, Petřík A, Sarica K, EAU guidelines on diagnosis and conservative management of urolithiasis: Eur Urol, 2016; 69(3); 468-74
6. Dogan C, Yazici CM, Akgul HM, The predictive factors for readmission and rehospitalization after retrograde intrarenal surgery: The results of RIRSearch Study Group: J Endourol, 2022; 36(1); 56-64
7. Duan M, Chen Y, Sun L, Outcomes of retrograde intrarenal surgery performed under neuraxial vs. general anesthesia: An updated systematic review and meta-analysis: Front Surg, 2022; 9; 853875
8. Gayarre Abril P, Beltrán BB, Gascón DH, Does time and size matter in retrograde intrarenal surgery? Results analysis using a low-pressure technique: Arch Esp Urol, 2023; 76(2); 107-13
9. Perks A, Chakravarti S, Manninen P, Preoperative anxiety in neurosurgical patients: J Neurosurg Anesthesiol, 2009; 21(2); 127-30
10. Gürsoy A, Candaş B, Güner Ş, Yılmaz S, Preoperative stress: An operating room nurse intervention assessment: J Perianesth Nurs, 2016; 31(6); 495-503
11. Tarhan H, Cakmak O, Unal E, The effect of video-based education on patient anxiety in men undergoing transrectal prostate biopsy: Can Urol Assoc J, 2014; 8(11–12); E894-E900
12. Lunger F, Frank F, Peros G, Potential benefit in information providing and influence on patient anxiety and satisfaction by means of preoperative explanatory videos in total extraperitoneal inguinal hernioplasty: Study protocol of a multicentre, double-blinded, randomised parallel-group controlled trial: BMJ Open, 2021; 11(1); e043702
13. Bozkurt M, Erkoc M, Can O, The effect of an information video on preoperative anxiety level before percutaneous nephrolithotomy procedure: A prospective, randomized trial: Can Urol Assoc J, 2023; 17(3); E86-E89
14. https://patients.uroweb.org/videos/ureteroscopy-urs-video/
15. Moerman N, van Dam FS, Muller MJ, Oosting H, The Amsterdam Preoperative Anxiety and Information Scale (APAIS): Anesth Analg, 1996; 82(3); 445-51
16. Gürler H, Yılmaz M, Türk KE, Preoperative anxiety levels in surgical patients: A comparison of three different scale scores: J Perianesth Nurs, 2022; 37(1); 69-74
17. Abate SM, Chekole YA, Minaye SY, Basu B, Global prevalence and reasons for case cancellation on the intended day of surgery: A systematic review and meta-analysis: Int J Surg Open, 2020; 26; 55-63
18. Ali A, Altun D, Oguz BH, The effect of preoperative anxiety on postoperative analgesia and anesthesia recovery in patients undergoing laparascopic cholecystectomy: J Anesth, 2014; 28(2); 222-27
19. Lin SY, Huang HA, Lin SC, The effect of an anaesthetic patient information video on perioperative anxiety: A randomised study: Eur J Anaesthesiol, 2016; 33(2); 134-39
20. Ketelaars PJW, Buskes MHM, Bosgraaf RP, The effect of video information on anxiety levels in women attending colposcopy: A randomized controlled trial: Acta Oncol, 2017; 56(12); 1728-33
21. Esen CSB, Yazici G, Hurmuz P, The effect of video-based education on anxiety of patients receiving stereotactic radiosurgery and stereotactic body radiation therapy: J Cancer Educ, 2023; 38(2); 426-30
22. Ha JF, Longnecker N, Doctor-patient communication: A review: Ochsner J, 2010; 10(1); 38-43
23. Savaş Erdoğan S, Falay Gür T, Doğan B, Effect of video-based patient information on patients’ anxiety and pain levels before skin biopsy: A randomized controlled study: Postgrad Med, 2021; 133(8); 988-93
24. Tan ML, Lee KH, Yong WS, Rodgers C, The effects of a video-based education in women with newly diagnosed breast cancer in Singapore: Support Care Cancer, 2018; 26(11); 3891-97
25. Yang B, Liu S, Mi Y, The impact of watching real-time videos of flexible ureteroscopic lithotripsy on anxiety and depression in patients: Int Urol Nephrol, 2022; 54(5); 1009-15
26. González-Padilla DA, González-Díaz A, García-Gómez B, Cystoscopy real-time self-visualization and its impact in patient’s pain perception: J Endourol, 2019; 33(4); 309-13
In Press
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952