19 October 2023: Clinical Research
Impact of Mental State on the Severity of Psoriasis Symptoms: A Study on Patient’s Emotional Well-Being
Milena WojciechowskaDOI: 10.12659/MSM.941636
Med Sci Monit 2023; 29:e941636
Abstract
BACKGROUND: Psoriasis is a chronic systemic skin disease affecting approximately 2% of the global population. In addition to the characteristic inflammatory changes on the skin, patients with psoriasis often experience comorbidities, including depressive symptoms and anxiety. This study aimed to investigate the relationship between the course of psoriasis and the mental state of patients.
MATERIAL AND METHODS: The study was conducted among 70 patients with psoriasis. An interview was conducted to assess the course of psoriasis. The Beck Depression Inventory (BDI) and Hospital Anxiety and Depression Scale (HADS) were used. CRP concentration as well as VAS, NRS, and PASI scales were measured. The results were subjected to statistical analysis.
RESULTS: Psoriasis was severe in 50% of the patients. Most (52.8%) of patients had moderate pruritis (VAS) and 58.5% had moderate pain (NRS). Moderate depressive symptoms (BDI) were present in 60% of patients, 18.6% had pathological anxiety (HADS-A), and 18.6% had pathological depression (HADS-D). CRP levels were significantly associated with PASI, VAS, and NRS.
CONCLUSIONS: The mental state of the patient plays an essential role in the course of psoriasis, and negative emotions affect the severity of skin symptoms. Emotional stress to patients with psoriasis should be limited, which will undoubtedly contribute to overall improvement of health.
Keywords: Anxiety, Depression, Psoriasis, Humans, Emotions, Anxiety Disorders, Severity of Illness Index
Background
Psoriasis is an incurable, non-infectious skin disease. It is characterized by a chronic and relapsing course with periods of exacerbation and remission. It is estimated that approximately 1.5% of children in Europe have psoriasis, and patients with psoriasis make up 4% of dermatological patients under the age of 16 years. In the general world population, the proportion of adults with psoriasis is approximately 2% [1]. The etiopathogenesis of psoriasis is complex and still not fully understood. Genetic factors play an undeniable role, with approximately 30% of psoriasis cases having a familial pattern. The morphological picture of the disease is characterized by great diversity and varying degrees of severity. The primary lesion is a small papule that increases in size, resulting in the formation of confluent inflammatory foci. The pathomechanism involves many pro-inflammatory cytokines (IL-1, IL-6, IL-8, IL-12, IL-17, IL-18, IL-22, IL-23, TNF, INF, TGF) released by lymphocytes, keratinocytes, mast cells, endothelial cells, and fibroblasts. The essence of the disease process is excessive proliferation of the epidermis, with an 8-fold reduction in the duration of the cell cycle, from 28 to 3-4 days [2].
One of the key dimensions of the human mental condition is the importance of external appearance and attitude towards one’s own body. Physicality, including the appearance of the skin, is associated with well-being, self-esteem, building self-esteem, and maintaining satisfying interpersonal relationships. Psychodermatology is a sub-branch of medicine that explains the relationship between the nervous system and the skin and its appendages. Up to 60% of patients with psoriasis have depression [3]. Studies explaining the comorbidity of psoriasis with depression are ongoing, and suggest a bidirectional relationship in which psoriasis can cause depression and depression can lead to psoriasis, through an immune-mediated inflammatory process [4]. Psoriasis, like many other dermatoses, has a negative impact on the patient’s physical appearance, which can lead to depressed mood, loss of self-esteem, stigmatization, and social withdrawal, which can lead to anxiety and depressive disorders, social phobias, or other adaptation problems [2]. In addition, patients with psoriasis often also have systemic diseases, including cardiovascular diseases, which can reduce functional abilities and quality of life, which also contributes to depression [5].
The research results obtained so far emphasize the similarities in some elements of the pathomechanism of psoriasis and depression. Pro-inflammatory cytokines involved in the pathogenesis of psoriasis can cause excessive activation of the hypothalamic-pituitary-adrenal axis, which causes a decrease in serotonin levels and, consequently, the development of depression. Decreased melatonin levels demonstrated in both psoriasis and depression correlate with increased release of pro-inflammatory cytokines such as IL-6, IL-8, and TNF-α. Other common aspects of the pathomechanism include increased activity of CD4+/CD8+ cells, and release of cytokines IL-17, IL-13, IL-23, IL-10, IL-1β, IL-2, and INF-γ through processes mediated by Th1 and Th17 lymphocytes [4]. Treating patients with psoriasis with TNF-α or IL-12/IL-23 antagonists reduces depressive symptoms, while treating depressed patients with antidepressants reduces the need for anti-psoriatic drugs. Higher levels of IL-6 in patients with psoriasis correlate with increased severity of depressive symptoms in these patients. However, the results of many studies do not support the assumption that all patients with psoriasis are depressed and vice versa. It is therefore necessary to carry out further work on this topic [6]. Elevated levels of the C-reactive protein (CRP) have been shown in both depression and psoriasis. It was found that the severity of symptoms such as fatigue, anxiety, sleep disorders, psychomotor impairment, and difficulty concentrating are correlated with an increase in CRP concentration [7]. In patients with psoriasis, higher CRP levels were correlated with greater severity of the disease, and the CRP level can be used as a predictor of cardiovascular risk in these patients [8].
Although the association between psoriasis and the mental health of patients has been the subject of previous scientific research, our study enriches the understanding of the psychosomatic dimensions of psoriasis. We focused on the psychological implications of psoriasis and the necessity of a holistic approach to psoriasis treatment. The aim of our study was to analyze the relationship between the course of psoriasis and the mental state of patients.
Material and Methods
PARTICIPANTS:
The study sample consisted of 70 respondents, including 33 women and 37 men, average age 44.5 years, selected from among inpatients at the Dermatology and Venerology Department of the University Hospital of Nicolaus Copernicus University in Toruń, Ludwik Rydygier Collegium Medicum in Bydgoszcz, Poland.
The sampling followed strict inclusion criteria: 1) clinical diagnosis of psoriasis confirmed by a dermatologist, 2) no general psoriasis treatment in the least 3 months preceding the study, 3) no mental and neurological diseases, 4) age over 18 years.
PSYCHOLOGICAL ASSESSMENT:
Depression was screened by using both the Beck Depression Inventory (BDI) and the Hospital Anxiety and Depression Scale (HADS). Anxiety was screened using the Hospital Anxiety and Depression Scale. The respondents were not subjected to a formal psychiatric diagnosis.
CRP CONCENTRATION:
We collected 10 ml of blood from the ulnar vein from all patients. Blood samples were collected in tubes containing a clot activator. After clotting at room temperature, the blood was centrifuged (centrifugation parameters: 4500 rpm/10 min) to isolate the serum, which was stored at −80°C until further use. CRP concentration was measured by our local hospital laboratory according to routine protocols and following the manufacturers’ instructions.
CLINICAL ASSESSMENT:
We conducted an analysis of respondent data, including selected clinical parameters (age, gender, disease course), and results of the VAS, NRS, PASI, HADS, and BDI questionnaires, which are reported below.
The Visual Assessment Scale (VAS) is a scale consisting of a 10-cm-long line and a single question. It is mostly used in clinical trials for measuring itch intensity and has high reliability and concurrent validity. The left end-point represents “no itch” and the right end-point represents the “worst imaginable itch” [9].
It can be interpreted as follows:
The Numeric Pain Rating Scale (NRS) is a unidimensional measure of pain intensity in adults. The 11-point numeric scale ranges from ‘0’ representing one pain extreme (eg, “no pain”) to ‘10’ representing the other pain extreme (ie, “pain as bad as you can imagine” or “worst pain imaginable”) [10].
The Psoriasis Area and Severity Index (PASI) is a widely used instrument in psoriasis trials that assesses and grades the severity of psoriatic lesions and the patient’s response to treatment. It produces a numeric score ranging from 0 to 72. In general, a PASI score of 5 to 10 is considered moderate disease, and a score over 10 is considered severe. In calculating the PASI, severity is determined by dividing the body into 4 regions: head (h), upper extremities (u), trunk (t), and lower extremities (l), that account for 10%, 20%, 30%, and 40% of the total body surface area, respectively. Each of these areas is assessed separately for erythema, induration, and scaling, which is rated on a scale of 0 (none) to 4 (very severe). The extent of psoriatic involvement is graded as follows [11]:
BDI is a 21-item, self-report rating inventory that measures characteristic attitudes and symptoms of depression, addressing the severity of cognitive and somatic aspects of depression. Although the BDI was originally developed as a measure of the intensity of depression, it has also been used as a screening instrument in clinical settings [12].
HADS is a widely used short 14-item scale for the measurement of anxiety and depression. It was initially designed as a tool for hospital staff to use for assessment of the level of psychological distress of patients. The authors originally proposed a 2-factor solution with 7 items measuring anxiety and 7 items measuring depression, each with a 4-point Likert response format. For both scales, results between 0 and 7 points indicate no symptoms, between 8 and 10 points indicate borderline states, while results between 11 and 21 points suggest pathologies [13].
STATISTICAL ANALYSES:
Python 3.8.10. was used for all analyses. Python modules used: pandas (1.4.3) used to work on and process data, matplotlib (3.6.2) and seaborn (0.11.2) for data visualization, pingouin (0.5.2) to perform statistical tests, and SciPy (1.9.0) as background for pingouin library tests. Graphs and basic information were created for all variables. For continuous variables, histograms with kernel density estimation and boxplots were created and 95% confidence intervals were calculated. For category variables, bar charts with a frequency occurrence count of a given category were created. Normally distributed data are presented as mean±standard deviation and were analyzed using the independent-samples
For the purpose of analysis, we deleted/merged categories. We removed
Correlations were assessed using the Spearman rank correlation test for nonparametric distribution. Not-normally distributed data (NRS, VAS, and BDI results) are presented as median with 1 and 3 quartiles and were analysed using the Mann-Whitney
Results
Most patients had moderate (52.8%), severe (21.4%), or very severe (17.1%) pruritus. Only 5 patients described their itch as mild, and 1 respondent declared no itching (Table 1).
Most patients (58.5%) had moderate pain, 18.5% of them declared severe pain, with only 2 patients declared no pain (Table 2).
Psoriasis was severe for 50% of patients, with the other half having moderate disease (Table 3) (mean PASI result of 20.3).
In the BDI questionnaire, most patients (60%) had moderate depressive symptoms, 34.2% of them declared high depression, and only 4 patients declared low depression (Table 4). In the HADS-A questionnaire, most patients (68.6%) had no anxiety, 18.6% had pathological anxiety, and 12.8% had borderline states (Table 5). In the HADS-D questionnaire, most patients (54%) showed no depressive symptoms, with 27% of respondents indicating borderline states, and 18.6% had pathological depression (Table 6).
We found statistically significant positive correlations (
Among those in the moderate VAS variable group, lower values of BDI trait were observed compared to the severe group (Figure 1). Those in the moderate group of NRS variable had higher average values of BDI variable than those in the severe group (Figure 2).
We demonstrated a lack of statistically significant positive correlations between patient gender and psoriasis severity indices (PASI, VAS, NRS) as well as emotional state (HADS-A, HADS-D, BDI) (Figures 3A, 3B; 4A, 4B).
Discussion
Psoriasis is a chronic dermatosis whose complex symptomatology also includes subjective symptoms such as itching and pain. Itching is a bothersome experience for 60–90% of patients with psoriasis [14]. Nearly 100% of the respondents in our sample experienced itching, with nearly 40% of them experiencing severe or very severe itching. This symptom significantly impairs everyday functioning, and scratching the skin leads to breaking its continuity or the Auspitz symptom. It is estimated that about 40% of patients with psoriasis also have cutaneous pain, defined by patients as pain, burning, stinging, tenderness, and tingling [15]. The NRS scale showed that 97% of the respondents felt pain, and 27% had severe or very severe pain. Cutaneous pain is caused by neurogenic inflammation and aggravated by stress and psychological factors. The pathomechanism of pain in psoriasis has not been fully explained and further work is needed on this topic. It is known, however, that psoriasis has underlying neurogenic inflammation that generates a form of nociceptive pain with both an immunologic and neurologic basis [15]. Itching and pain in psoriasis both increase with disease severity (PASI), as confirmed in our study.
In addition to genetic conditions or immunological disorders, the course of psoriasis can be modified by stress, emotional conflict, or a tendency to suppress feelings. A special role is attributed to stress and the accompanying negative emotions. The interrelationships of the mind and body are analyzed by psychosomatic medicine based on a holistic approach to the human being, paying attention to biological, psychological, and social aspects. Numerous studies confirm a strong relationship between the state of the central nervous system and the course of psoriasis. Increased stress often exacerbates psoriasis, which in turn causes even more stress for the patient. The results of the previous studies indicate a large range in relation to the estimates of the coexistence of psoriasis with depression, and the percentage of such patients is in the range of 6–62% [16]. In our study, using the BDI scale, moderate symptoms of depression were confirmed in 60% of patients with psoriasis, and in 34% of them these symptoms were severe. The HADS-D questionnaire showed symptoms of depression in 45.6% of patients with psoriasis, of which 18.6% had pathology symptoms. Anxiety (HADS-A) was present in 31.4% of the respondents, of which in the majority (18.6%) of patients was pathological anxiety. Among the Asian population, a higher prevalence of depression was found in patients with psoriasis than in the general population: 11.5% vs 7.7%. In addition, it was estimated that comorbidities with psoriasis (eg, cerebrovascular disease, hypertension, diabetes, obesity, liver cirrhosis, kidney disease) are more common in patients with psoriasis and depression than in patients without depression [17]. In a German study, 40% of 722 patients with psoriasis were depressed [18]. Most of these patients assessed themselves as less happy and less satisfied with their lives, which was significantly correlated with the severity of psoriasis. A Danish meta-analysis by Wu et al [16] showed that mental health disorders were observed in 3.1% of patients with psoriasis compared to 2.2% of patients in the control group. A similar proportion was confirmed for the percentage of respondents taking antidepressants, antipsychotics, or anxiolytics – these preparations were more often prescribed to patients with psoriasis than to the control group without psoriasis. In our study, HADS values were significantly higher in correlation (
CRP is one of the most sensitive acute-phase parameters in tissue damage or inflammation. It is a cyclic pentamer, a glycoprotein synthesized mainly in hepatocytes of the liver. The CRP molecule is made up of 206 amino acids, with a molecular weight of 118 kilodaltons (kD). Its synthesis and secretion increase many times during the first hours of inflammation, reaching its apogee after 24–48 h, and CRP returns to baseline values within 7–12 days (after the pathogenic factor subsides). CRP is considered a biomarker of many diseases, such as rheumatoid arthritis, tuberculosis, cancer and psoriasis. As an acute-phase protein, CRP recognizes antigens, forms complexes with them and, after activation of the complement system, participates in their elimination. CRP also supports the process of phagocytosis by affecting monocytes, macrophages, and neutrophils, as well as by chemotactic and opsonizing actions. CRP induces monocytes/macrophages to synthesize pro-inflammatory cytokines such as IL-6, which in hepatocytes is the main inducer of CRP synthesis [20]. Studies evaluating correlations of CRP levels with the course (severity) of psoriasis provide conflicting data. In our study, we demonstrated statistical significance for the positive correlation (
Psoriasis is a chronic immune-mediated disease with a systemic nature. As psoriasis develops and persists, there is a generalized increase in pro-inflammatory markers, including TNF-α, IFN-γ, IL-6, IL-8, IL-12, IL-17, and IL-18, which have significant clinical implications in the development of other diseases. In patients with psoriasis, there is an increased risk compared to the control group for developing conditions such as hypertension, coronary heart disease, and diabetes [24]. Moreover, moderate and severe forms of psoriasis are associated with numerous comorbidities, such as myocardial infarction, coronary artery disease, diabetes complications, atherosclerosis, inflammatory bowel diseases (eg, Crohn’s disease, ulcerative colitis), rheumatic diseases, kidney diseases, peptic ulcer disease, obesity, and venous thromboembolism [25]. Environmental factors, mainly lifestyle factors (eg, diet, physical activity, exposure to stress, and substance use), play an important role in the etiology of each of these diseases. Around 15–20% of patients with psoriasis are have obesity, which is associated with a poorer prognosis for the course of the disease. As BMI increases, the risk of developing psoriatic arthritis also rises, but weight reduction can alleviate the course of this disease. Indeed, a reduction in skin lesions was observed in over half of the obese patients with psoriasis who underwent bariatric surgery, which undoubtedly indicates a link between psoriasis and obesity [24,26]. Given this, in the treatment of psoriasis in patients who are overweight or obese, it is essential to introduce recommendations to reduce calorie intake, which can result in a reduction of PASI index by up to 75% [27]. Severe forms of psoriasis significantly increase the risk of cardiovascular diseases. “Psoriatic march” is a term explaining the causal relationship between psoriasis and cardiovascular diseases, which suggests that the systemic inflammatory state accompanying psoriasis, exacerbated by pro-inflammatory cytokines and adipokines from adipose tissue, enhances insulin resistance and endothelial dysfunction. This predisposes individuals to atherosclerosis and coronary events [28]. An important marker for the development of cardiovascular events is CRP, considered a proatherogenic factor. CRP is involved in the formation of atherosclerotic plaques, contributes to endothelial dysfunction, enhances prothrombotic tendencies, and activates the complement system. Synthesis of CRP occurring in the liver is regulated by cytokines involved in the pathogenesis of psoriasis (eg, TNF-α, IFN-γ, and IL-6) [29]. In our study, we found a statistically significant correlation between CRP and PASI index. The clinical implication of this relationship could be the potential occurrence of cardiovascular disorders in the future among patients with moderate and severe psoriasis. Therefore, CRP levels could serve as a good predictor of future cardiovascular events in patients with psoriasis. These results emphasize the necessity of treating psoriasis as a multi-system disease. In addition to the standard treatment of skin lesions, diet therapy should be considered, which, besides achieving potentially necessary weight reduction, can also lower the serum levels of cytokines and pro-inflammatory markers.
The relationship between psoriasis and the emotional state of patients highlights the need for psychological intervention as one of the ways to treat psoriasis effectively. Clearly, psychological interventions, especially cognitive-behavioral therapy, along with supportive methods like music therapy, relaxation training, and interest-based therapy, can be beneficial in managing psoriasis [30]. The results of our study show the multi-faceted issues of psoriasis. We would like these findings to serve as guidance for specialists from various fields on how to plan treatment of patients with psoriasis. We found significant correlations between psoriasis and symptoms of anxiety and depression. Therefore, clinical practitioners must pay attention to the emotions of patients with psoriasis, as the patient’s psychological state can significantly impact treatment outcomes. Establishing a collaboration between a physician and a psychologist/psychotherapist would be beneficial. The outcomes of such cooperation are likely to be highly effective, both in terms of reducing skin lesions and improving the patient’s psychological well-being. An essential direction for future research is assessment of the effectiveness of psychotherapy in the treatment of psoriasis.
Conclusions
In addition to recurrent skin lesions, psoriasis also includes severe itching and pain sensations. The patient’s mental state plays an important role in the course of psoriasis and affects the severity of skin symptoms. Chronic inflammation makes psoriasis a systemic disease with serious health consequences. Emotional stress to patients with psoriasis should be limited, which will undoubtedly contribute to the overall improvement of health.
Figures
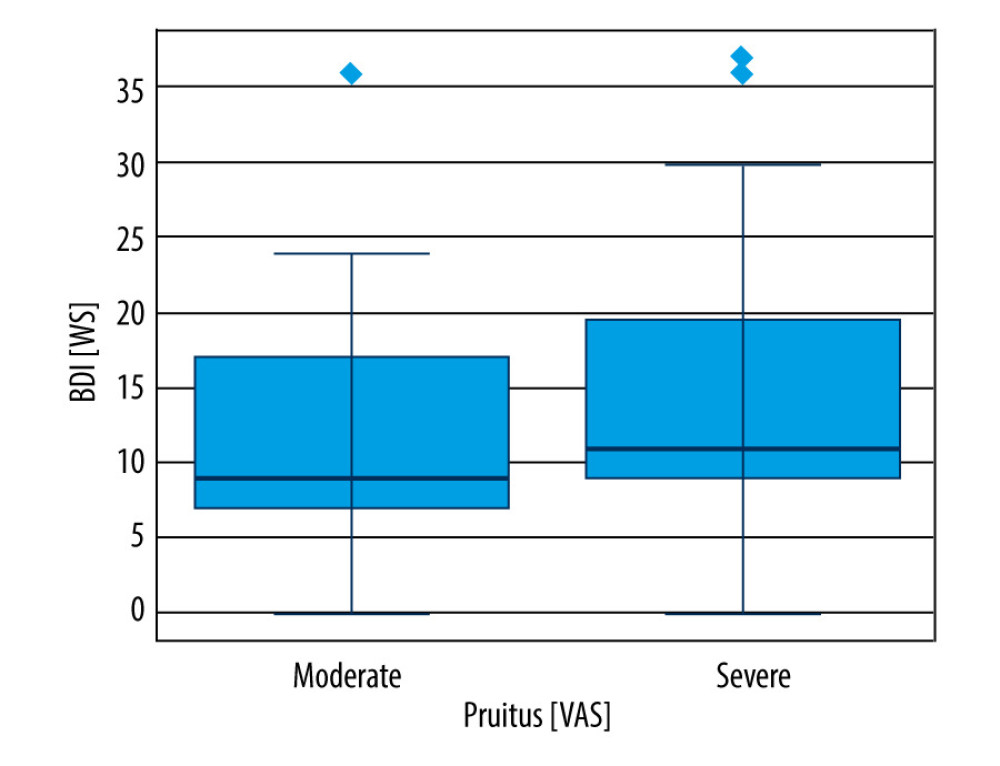 Figure 1. BDI and pruritus severity. Among those in the “moderate” group of VAS variable, lower values of the BDI trait were observed compared to the “severe” group. All quartiles of the “moderate” group of the BDI variable are lower than the corresponding quartiles of the “severe” group.
Figure 1. BDI and pruritus severity. Among those in the “moderate” group of VAS variable, lower values of the BDI trait were observed compared to the “severe” group. All quartiles of the “moderate” group of the BDI variable are lower than the corresponding quartiles of the “severe” group. 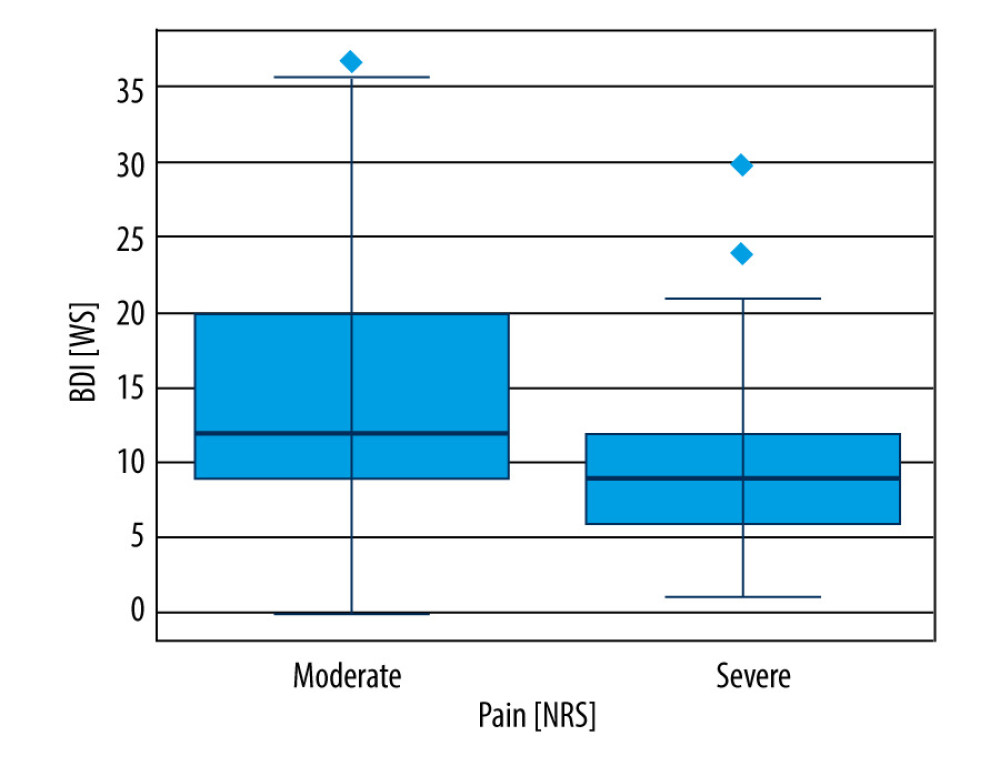 Figure 2. BDI and pain severity. Those in the “moderate” group of NRS variable have higher average values of the BDI variable than those in the “severe” group. In addition, a larger interquartile range was observed in the “moderate” group, and the extreme outliers in the “severe” group are lower than the third quartile in the “moderate” group.
Figure 2. BDI and pain severity. Those in the “moderate” group of NRS variable have higher average values of the BDI variable than those in the “severe” group. In addition, a larger interquartile range was observed in the “moderate” group, and the extreme outliers in the “severe” group are lower than the third quartile in the “moderate” group. 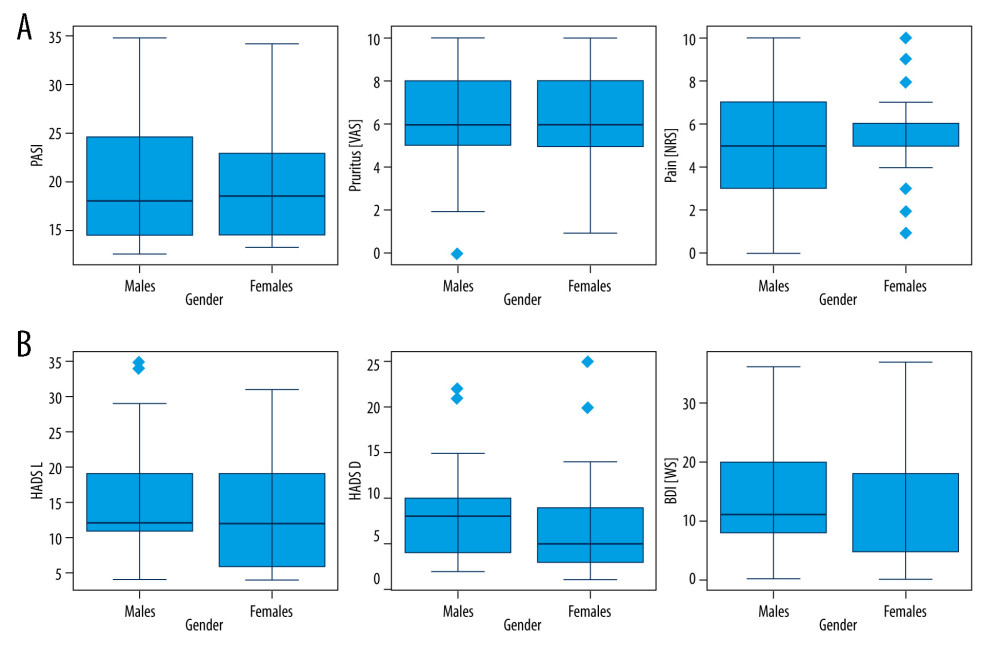 Figure 3. Gender and the course of psoriasis (A) and the emotional state of patients (B). The t test for independent samples. Due to the sample sizes being larger than 30 in the studied subgroups, the t test for paired samples was applied (without the Welch correction, as the Levene’s test did not show significant differences in variances). The t test did not reveal any significant differences between the groups defined by the gender variable.
Figure 3. Gender and the course of psoriasis (A) and the emotional state of patients (B). The t test for independent samples. Due to the sample sizes being larger than 30 in the studied subgroups, the t test for paired samples was applied (without the Welch correction, as the Levene’s test did not show significant differences in variances). The t test did not reveal any significant differences between the groups defined by the gender variable. 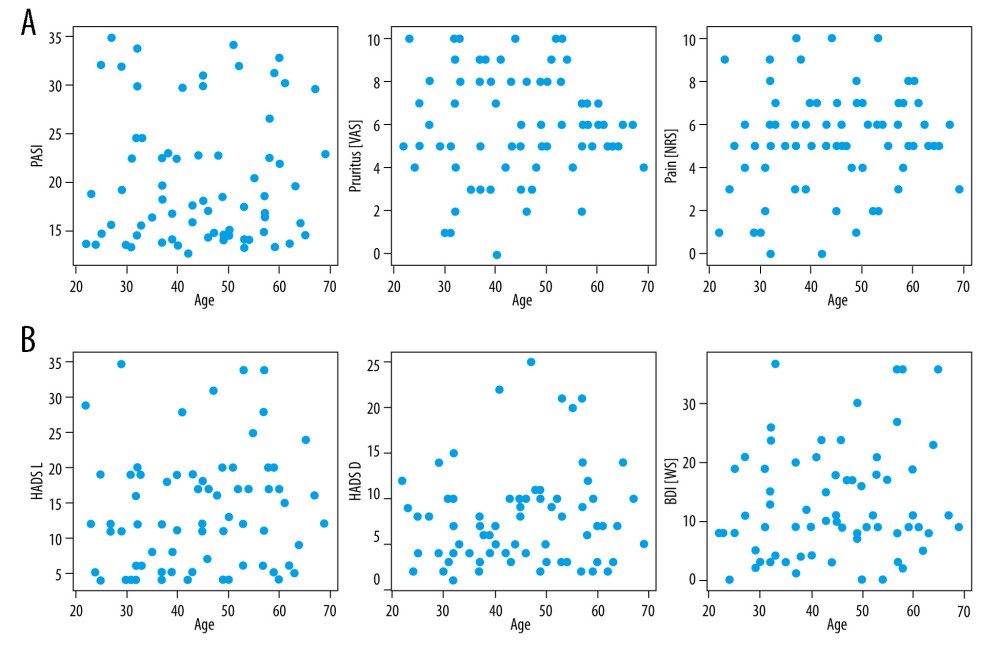 Figure 4. Age and the course of psoriasis (A) and the emotional state of patients (B). The Spearman correlation tests did not show any significant relationships between the studied variables.
Figure 4. Age and the course of psoriasis (A) and the emotional state of patients (B). The Spearman correlation tests did not show any significant relationships between the studied variables. Tables
Table 1. Visual Assessment Scale (VAS) results of the study sample.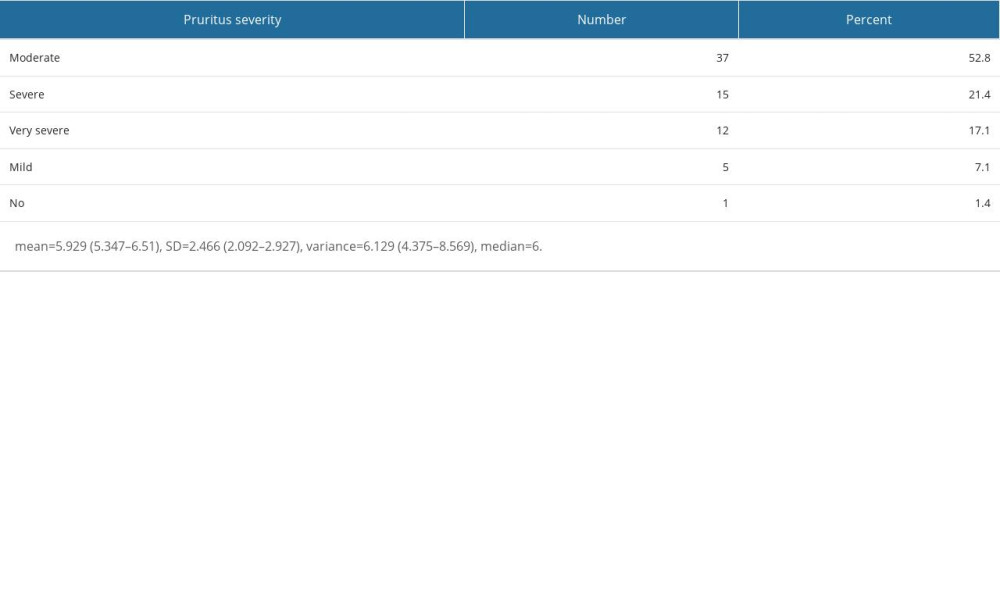 Table 2. Numeric Pain Rating Scale (NRS) results of the study sample.
Table 2. Numeric Pain Rating Scale (NRS) results of the study sample.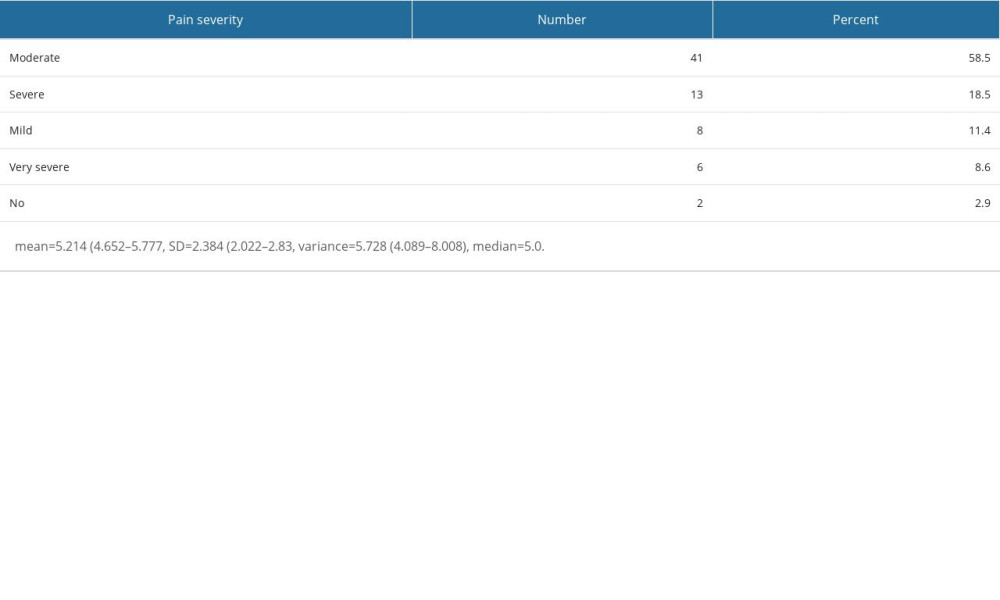 Table 3. Psoriasis Area and Severity Index (PASI) results of the study sample.
Table 3. Psoriasis Area and Severity Index (PASI) results of the study sample.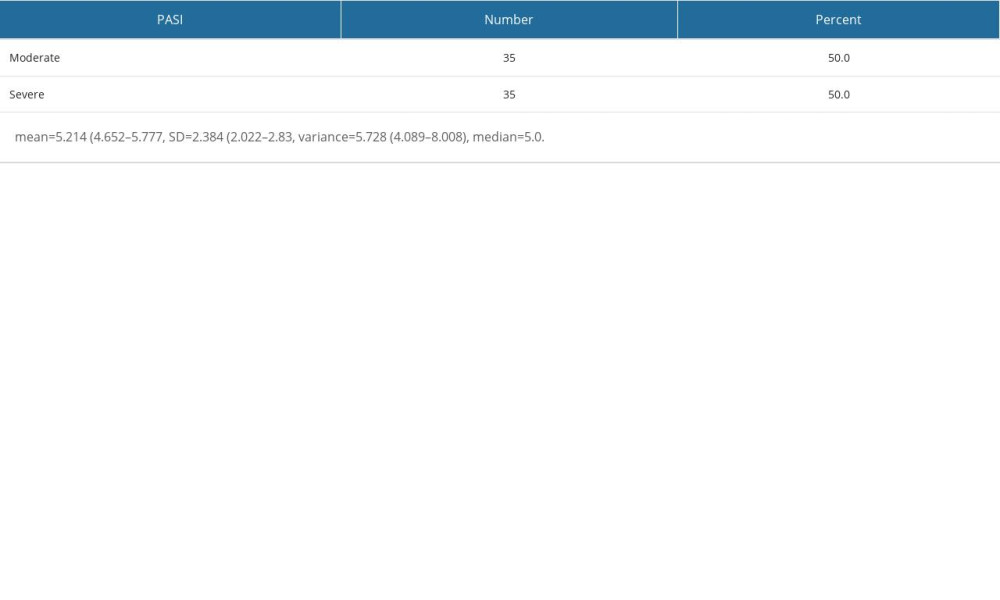 Table 4. Beck Depression Inventory (BDI) results of the study sample.
Table 4. Beck Depression Inventory (BDI) results of the study sample.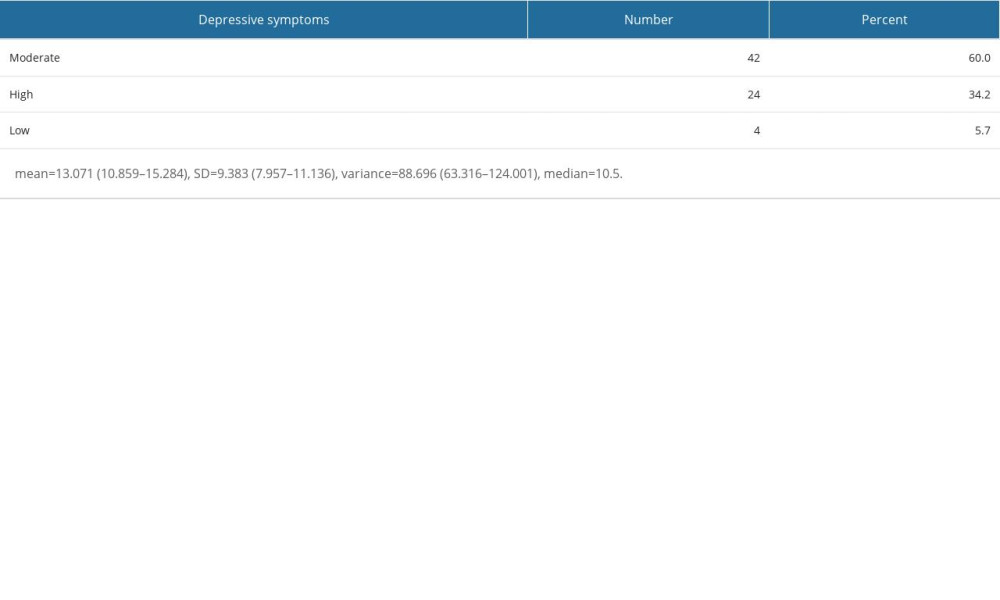 Table 5. Hospital Anxiety and Depression Scale – Anxiety (HADS-A) results of the study sample.
Table 5. Hospital Anxiety and Depression Scale – Anxiety (HADS-A) results of the study sample.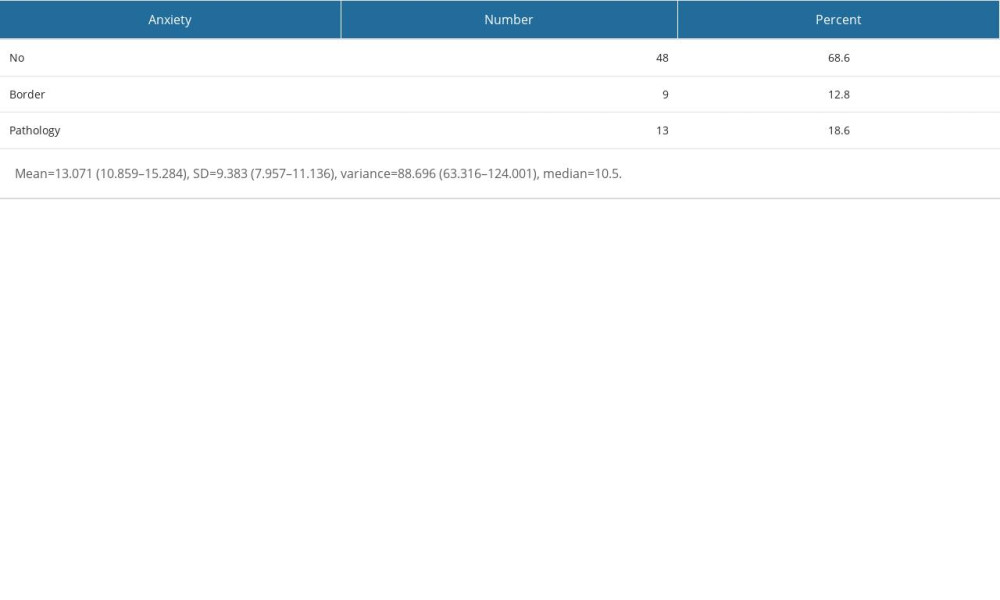 Table 6. Hospital Anxiety and Depression Scale – Anxiety (HADS-D) results of the study.
Table 6. Hospital Anxiety and Depression Scale – Anxiety (HADS-D) results of the study.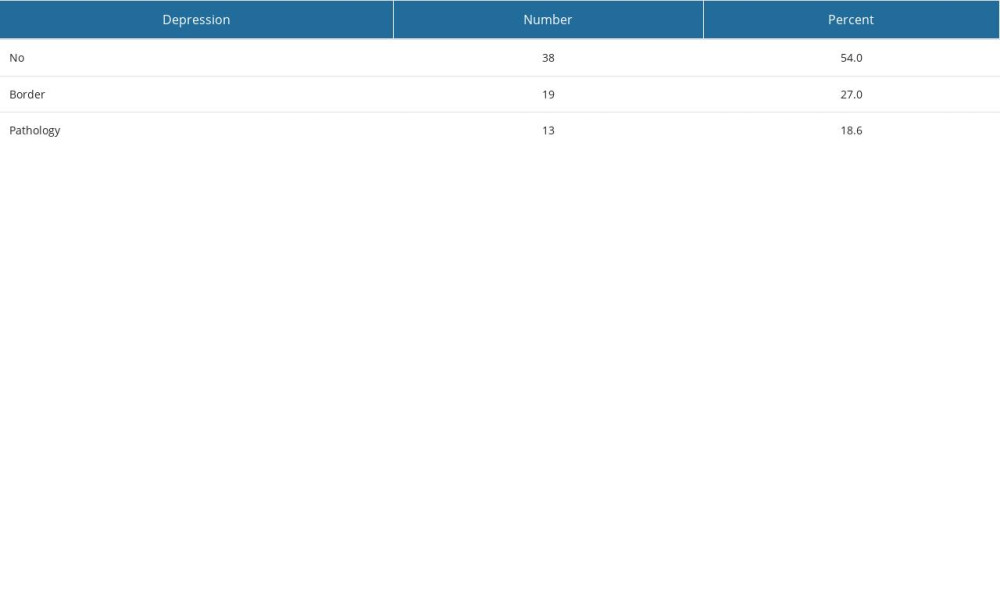 Table 7. Spearman rank correlations.
Table 7. Spearman rank correlations.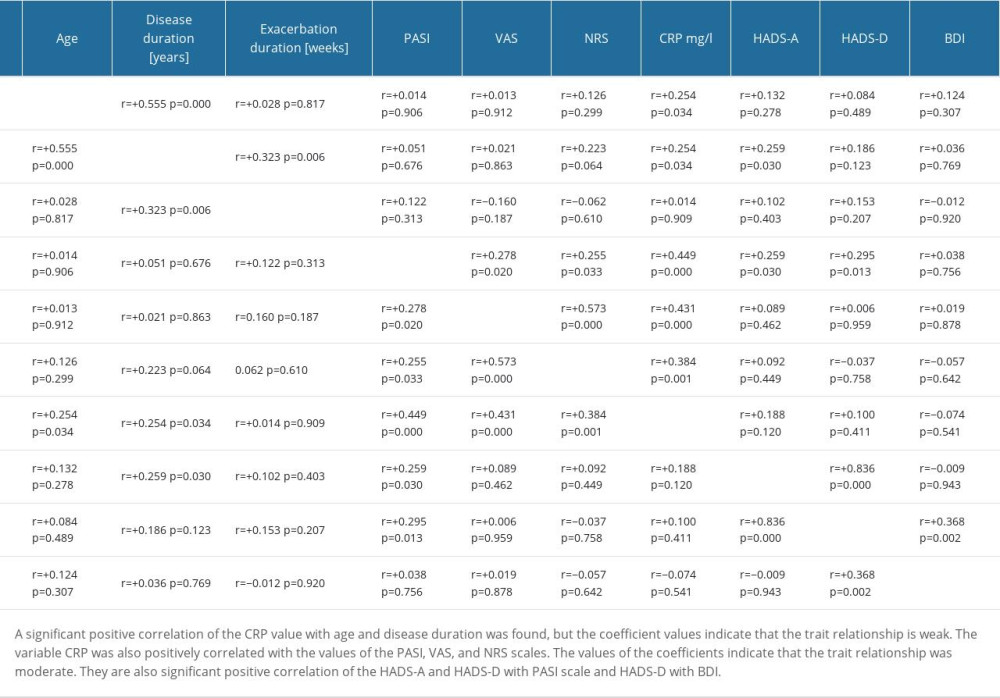
References
1. Chu-Sung S, Gwo-Shing Ch, Hung-Pin T, Epidemiology of depression in patients with psoriasis: A nationwide population-based cross-sectional study: Acta Derm Venereol, 2019; 99; 530-38
2. Maqbool S, Ihtesham A, Langove MN, Neuro-dermatological association between psoriasis and depression: An immune-mediated inflammatory process validating skin-brain axis theory: Aims Neurosci, 2021; 8(3); 340-54
3. Esposito M, Giunta A, Nanni RC, Depressive symptoms and insecure attachment predict disability and quality of life in psoriasis independently from disease severity: Arch Deramtol Res, 2021; 313; 431-37
4. Strain JJ, Globalization of psychosomatic medicine: Gen Hosp Psychiatry, 2017; 48; 62-64
5. Wojtyna E, Lakuta P, Marcinkiewicz K, Gender, body image and social support: Biopsychosocial determinants of depression among patients with psoriasis: Acta Derm Venereol, 2017; 97; 91-97
6. Marek-Józefowicz L, Jaracz M, Borkowska A, Affective temperament, depressive symptoms and interleukins in patients with psoriasis: Adv Dermatol Allergol, 2021; 38(1); 137-43
7. Orsolini L, Pompili S, Valenta ST, C-reactive protein as a biomarker for major depressive disorder?: Int J Mol Sci, 2022; 23; 2-39
8. Balta I, Balta S, The relation between C-reactive protein-albumin ratio and carotid intima-media thickness in psoriasis: Angiology, 2022; 73(8); 772-80
9. Klimek L, Bergmann KC, Biedermann T, Visual analogue scales (VAS): Measuring instruments for the documentation of symptoms and therapy monitoring in cases of allergic rhinitis in everyday health care: Allerg J Int, 2017; 26(1); 16-24
10. Childs JD, Piva SR, Fritz JM, Responsiveness of the numeric pain rating scale in patients with low back pain: Spine, 2005; 30; 1331-34
11. Fredriksson T, Pettersson U, Oral treatment of pustulosis palmo-plantaris with a new retinoid, Ro 10-9359: Dermatologica, 1979; 158; 60-66
12. Beck AT, Ward CH, Mendelson M, An inventory for measuring depression: Arch General Psychiatr, 1961; 4; 561-71
13. Zigmond AS, Snaith RP, The hospital anxiety and depression scale: Acta Psychiatr Scand, 1983; 67(6); 361-70
14. Komiya E, Tominaga M, Kamata Y, Molecular and cellular mechanisms of itch in psoriasis: Int J Mol Sci, 2020; 21; 1-25
15. Pithadiaa DJ, Reynoldsb KA, Leec EB, Psoriasis-associated cutaneous pain: Etiology, assessment, impact, and management: J Dermatol Treat, 2019; 30(5); 435-40
16. Wu JJ, Feldman SR, Koo J, Epidemiology of mental health comorbidity in psoriasis: J Dermatol Treat, 2018; 29(5); 487-95
17. Kleyn CE, Talbot PS, Mehta NN, Psoriasis and mental health workshop report: Exploring the links between psychosocial factors, psoriasis, neuroinflammation and cardiovascular disease risk: Acta Derm Venerol, 2020; 100(10); 1-8
18. Schuster B, Peifer C, Ziehfreund S, Happiness and depression in psoriasis: A cross sectional study in Germany: Qual Life Res, 2022; 31; 1761-73
19. Talamonti M, Malara G, Natalini Y, Secukinumab improves patient perception of anxiety and depression in patients with moderate to severe psoriasis: A post hoc analysis of the SUPREME Study: Acta Derm Venerol, 2021; 101(3); 1-9
20. Mishra S, Kadnur M, Jartarkar S, Correlation between serum uric acid, C-reactive protein, and neutrophil-to-lymphocyte ratio in patients with psoriasis: A case-control study: Turk Arch Dermatol Venerol, 2022; 56; 28-33
21. Gupta S, Garg P, Gupta N, High sensitivity C-reactive protein, a predictor of cardiovascular mortality and morbidity, and psoriasis: A case control study: Int J Res Dermatol, 2019; 5(2); 338-41
22. Solak B, Dikicier BS, Erdem T, Impact of elevated serum uric acid levels on systemic inflammation in patients with psoriasis: Angiology, 2017; 68; 266-70
23. Garshick MS, Ward NL, Krueger JG, Cardiovascular risk in patients with psoriasis: JACC review topic of the week: J Am Coll Cardiol, 2021; 13; 1670-80
24. Andújar I, Esplugues J, García-Martínez P, Looking beyond the skin: Pathophysiology of cardiovascular comorbidity in psoriasis and the protective role of biologics: Pharmaceuticals, 2022; 15; 1101
25. Fatás-Lalana B, Cantón-Sandoval J, Rodríguez-Ruiz L, Impact of comorbidities of patients with psoriasis on phototherapy responses: Int J Mol Sci, 2022; 23; 9508
26. Cicekliyurt M, Öguretmen Z, Clinical features and comorbidities in psoriasis. A retrospective study: Dermatol Rev, 2022; 9; 263-71
27. Ko SH, Chi CC, Yeh ML, Lifestyle changes for treating psoriasis: Syst Rev, 2019; 7; CD011972
28. Wierzbowska-Drabik K, Lesiak A, Skibińska M, Psoriasis and atherosclerosis – skin, joints, and cardiovascular story of two plaques in relation to the treatment with biologics: Int J Mol Sci, 2021; 22; 10402
29. Bafei S, Zhao X, Changying C, Interactive effect of increased high sensitive C-reactive protein and dyslipidemia on cardiovascular diseases: A 12-year prospective cohort study: Lipids Health Dis, 2023; 22; 95-111
30. Dewi D, Wijayanti F, Chen S, Cognitive behavioral therapy as an adjunctive treatment for anxiety and depression in psoriasis patients: J Res Comm Serv, 2023; 4(6); 1234-41
Figures
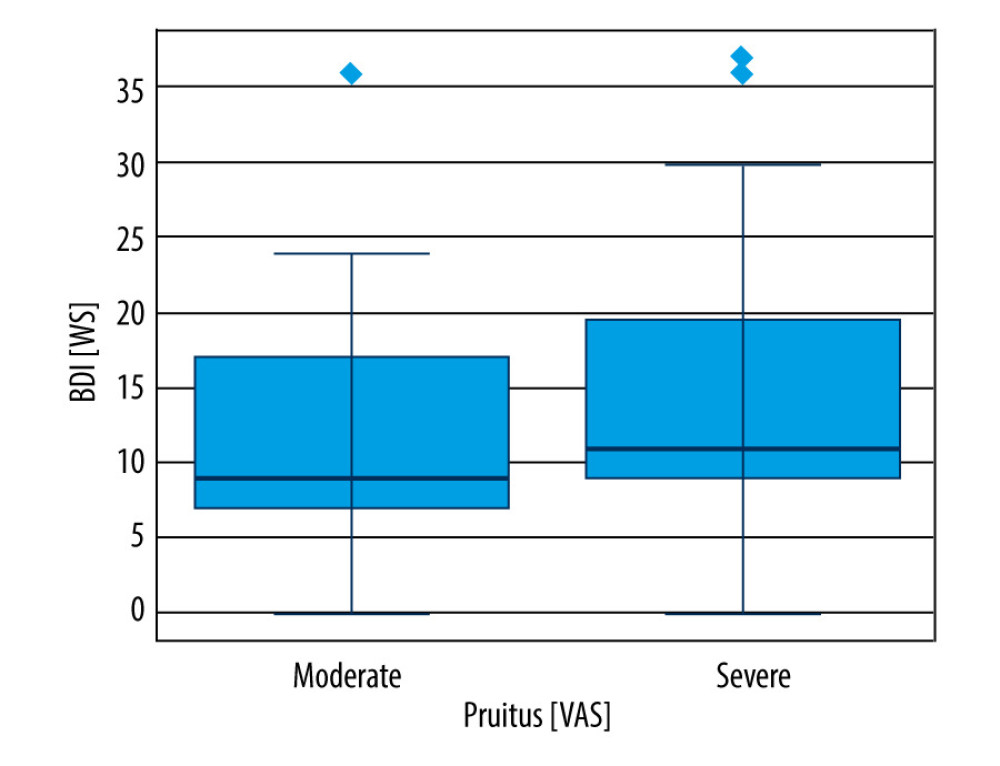 Figure 1. BDI and pruritus severity. Among those in the “moderate” group of VAS variable, lower values of the BDI trait were observed compared to the “severe” group. All quartiles of the “moderate” group of the BDI variable are lower than the corresponding quartiles of the “severe” group.
Figure 1. BDI and pruritus severity. Among those in the “moderate” group of VAS variable, lower values of the BDI trait were observed compared to the “severe” group. All quartiles of the “moderate” group of the BDI variable are lower than the corresponding quartiles of the “severe” group.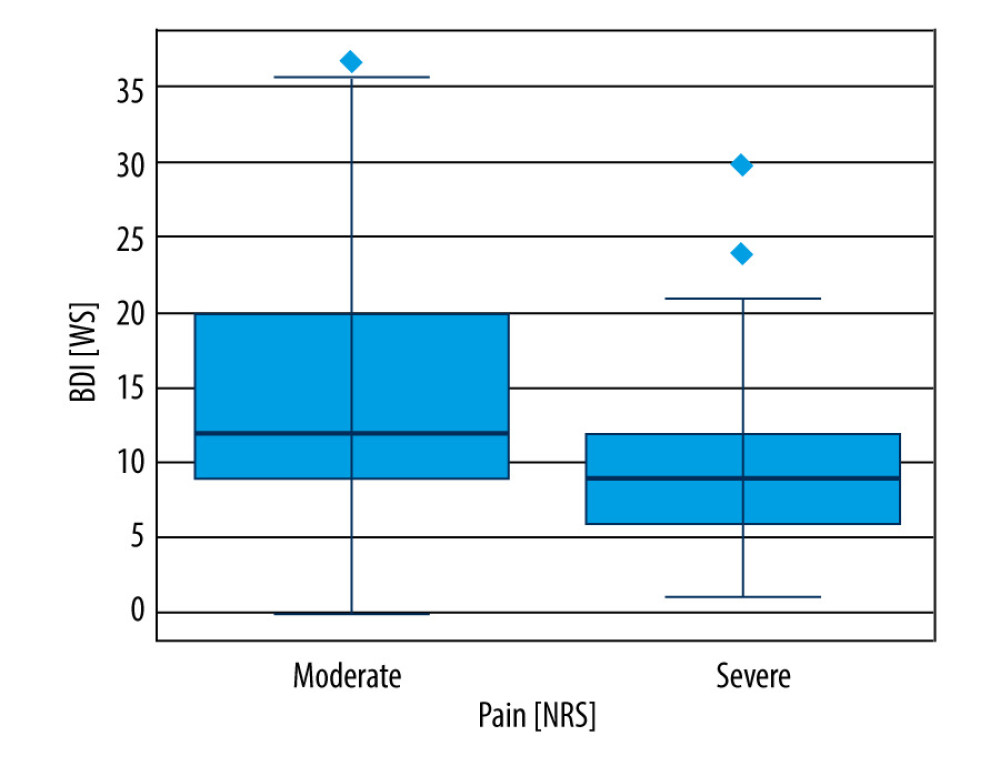 Figure 2. BDI and pain severity. Those in the “moderate” group of NRS variable have higher average values of the BDI variable than those in the “severe” group. In addition, a larger interquartile range was observed in the “moderate” group, and the extreme outliers in the “severe” group are lower than the third quartile in the “moderate” group.
Figure 2. BDI and pain severity. Those in the “moderate” group of NRS variable have higher average values of the BDI variable than those in the “severe” group. In addition, a larger interquartile range was observed in the “moderate” group, and the extreme outliers in the “severe” group are lower than the third quartile in the “moderate” group.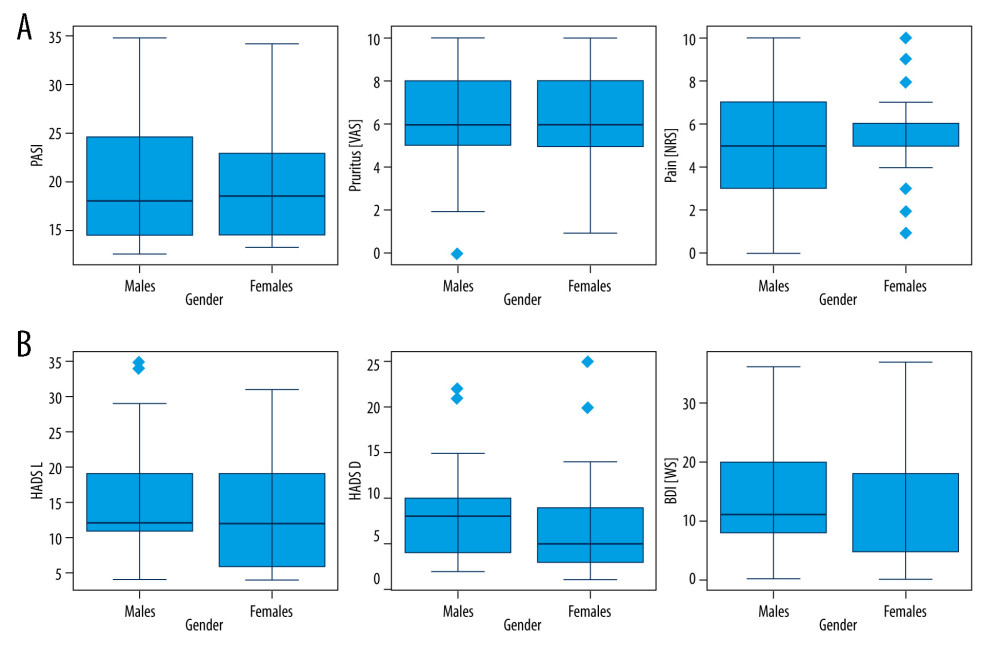 Figure 3. Gender and the course of psoriasis (A) and the emotional state of patients (B). The t test for independent samples. Due to the sample sizes being larger than 30 in the studied subgroups, the t test for paired samples was applied (without the Welch correction, as the Levene’s test did not show significant differences in variances). The t test did not reveal any significant differences between the groups defined by the gender variable.
Figure 3. Gender and the course of psoriasis (A) and the emotional state of patients (B). The t test for independent samples. Due to the sample sizes being larger than 30 in the studied subgroups, the t test for paired samples was applied (without the Welch correction, as the Levene’s test did not show significant differences in variances). The t test did not reveal any significant differences between the groups defined by the gender variable.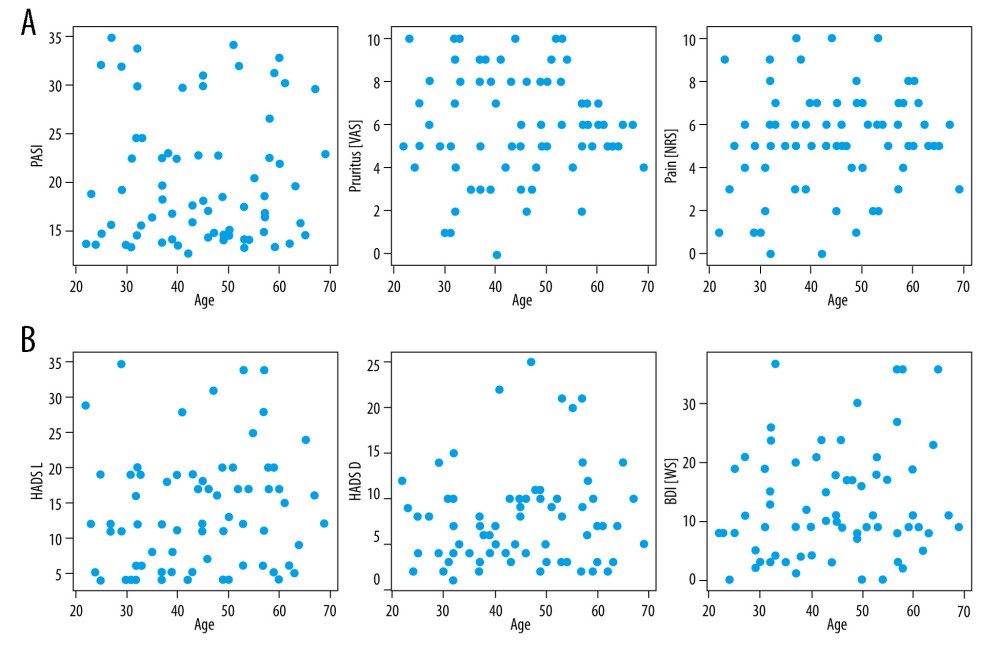 Figure 4. Age and the course of psoriasis (A) and the emotional state of patients (B). The Spearman correlation tests did not show any significant relationships between the studied variables.
Figure 4. Age and the course of psoriasis (A) and the emotional state of patients (B). The Spearman correlation tests did not show any significant relationships between the studied variables. Tables
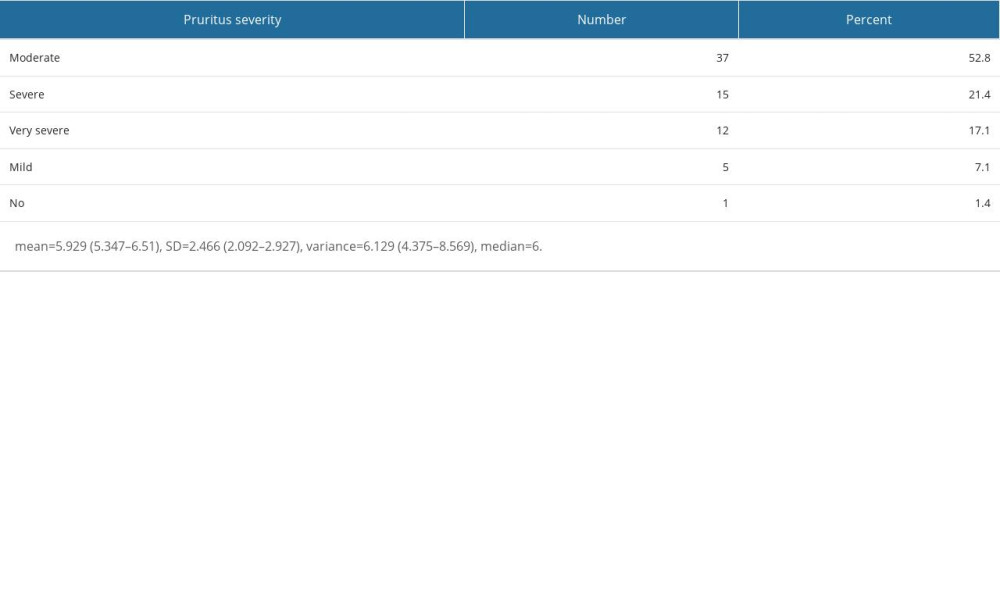 Table 1. Visual Assessment Scale (VAS) results of the study sample.
Table 1. Visual Assessment Scale (VAS) results of the study sample.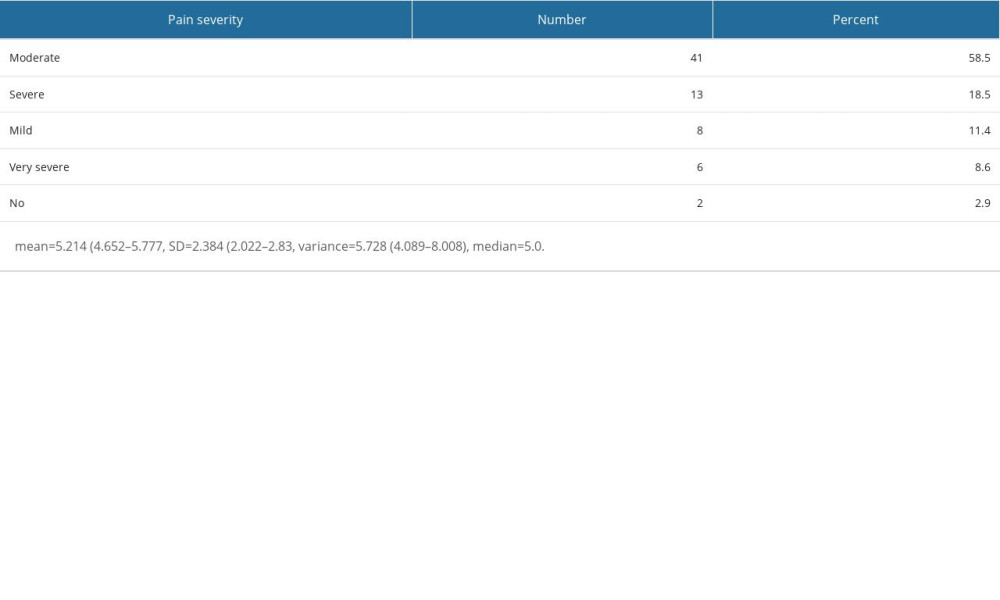 Table 2. Numeric Pain Rating Scale (NRS) results of the study sample.
Table 2. Numeric Pain Rating Scale (NRS) results of the study sample.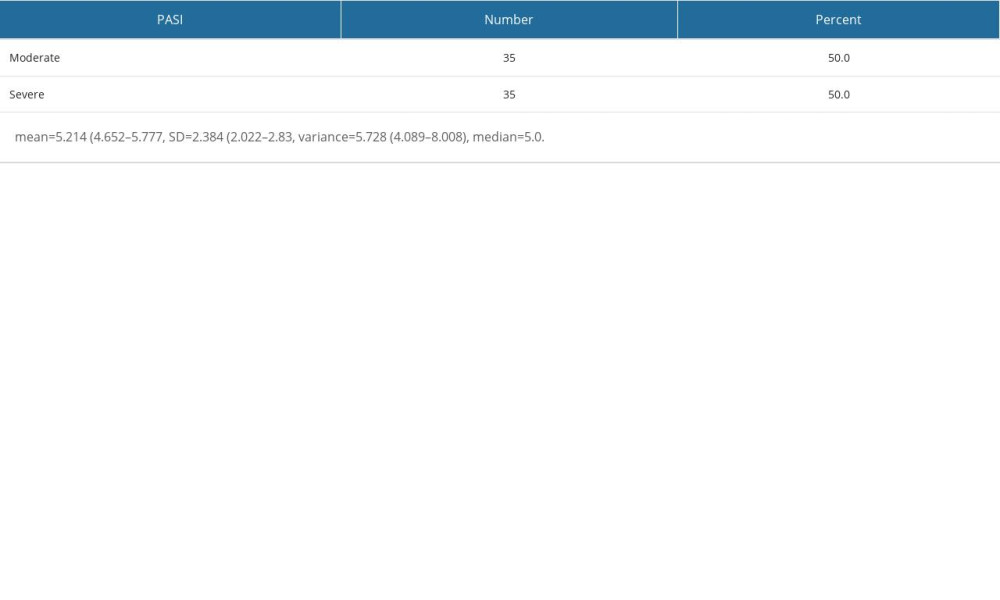 Table 3. Psoriasis Area and Severity Index (PASI) results of the study sample.
Table 3. Psoriasis Area and Severity Index (PASI) results of the study sample.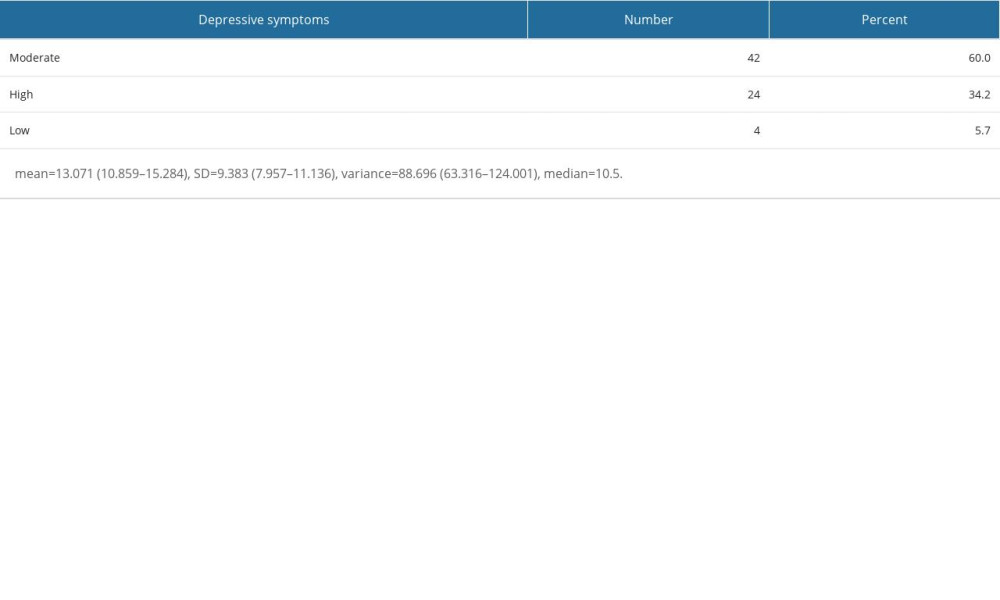 Table 4. Beck Depression Inventory (BDI) results of the study sample.
Table 4. Beck Depression Inventory (BDI) results of the study sample.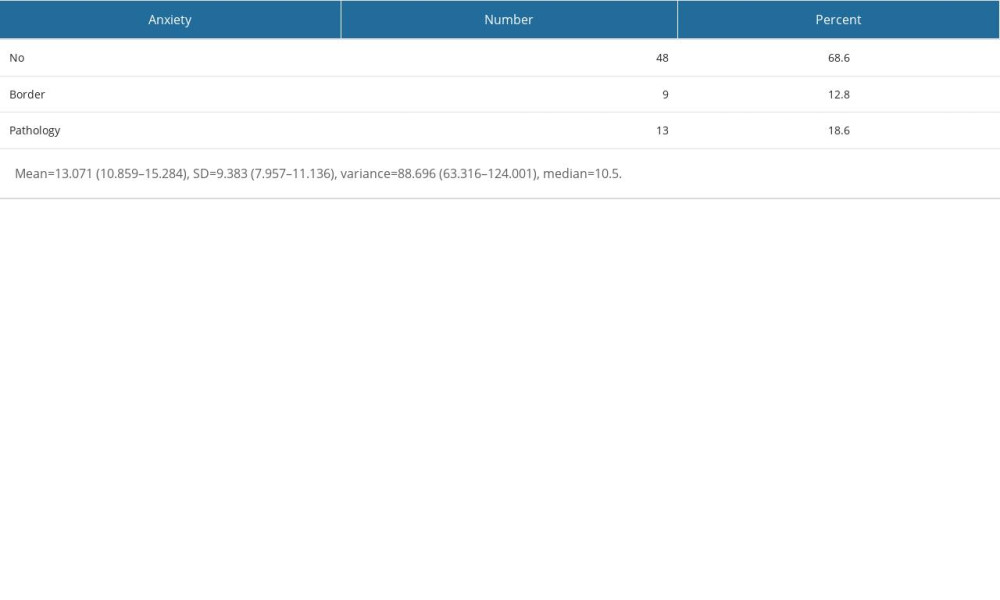 Table 5. Hospital Anxiety and Depression Scale – Anxiety (HADS-A) results of the study sample.
Table 5. Hospital Anxiety and Depression Scale – Anxiety (HADS-A) results of the study sample.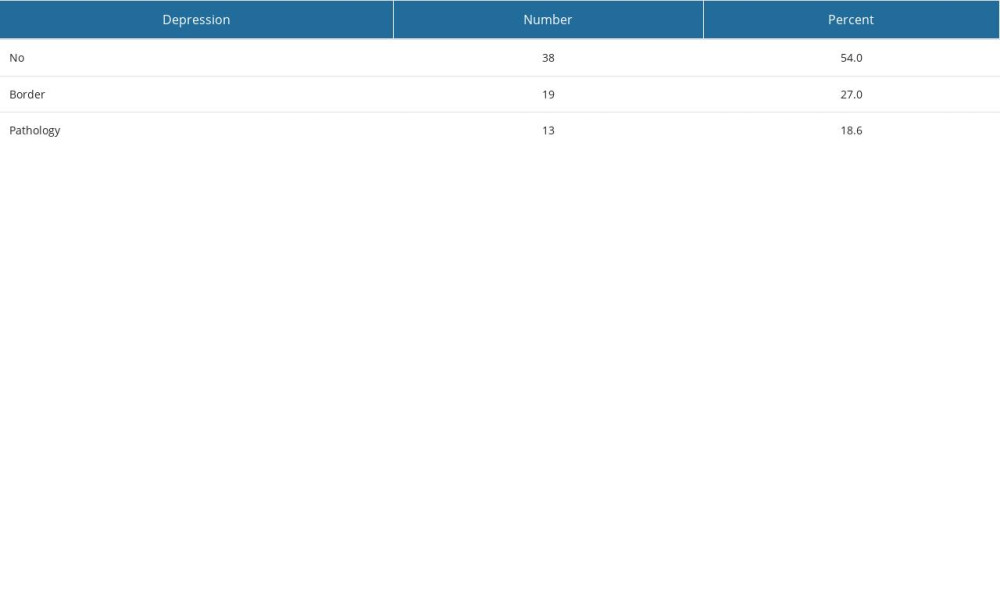 Table 6. Hospital Anxiety and Depression Scale – Anxiety (HADS-D) results of the study.
Table 6. Hospital Anxiety and Depression Scale – Anxiety (HADS-D) results of the study.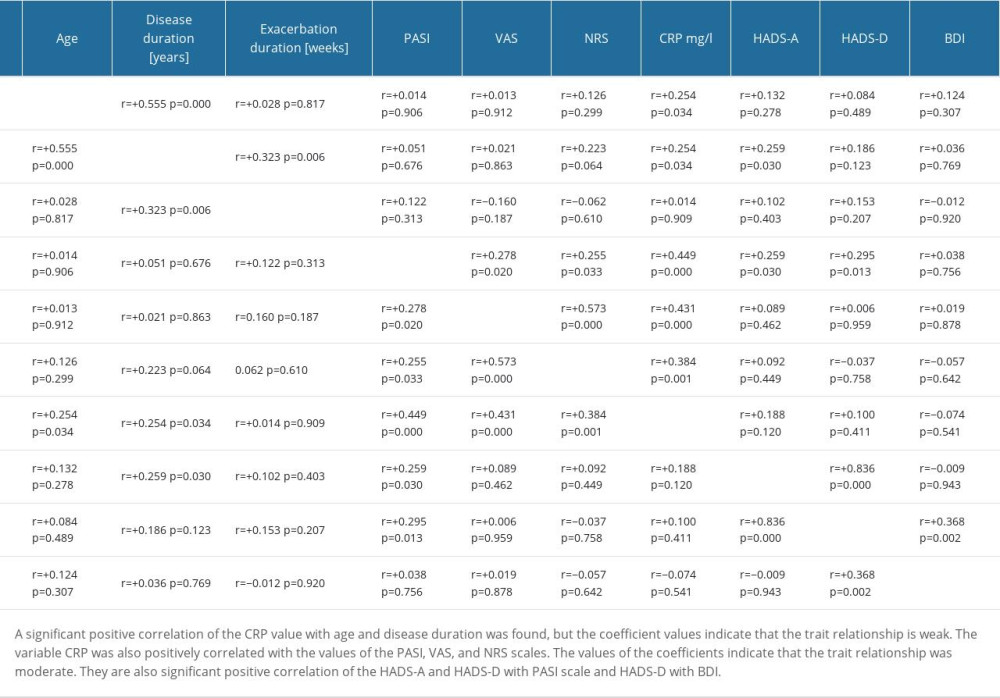 Table 7. Spearman rank correlations.
Table 7. Spearman rank correlations.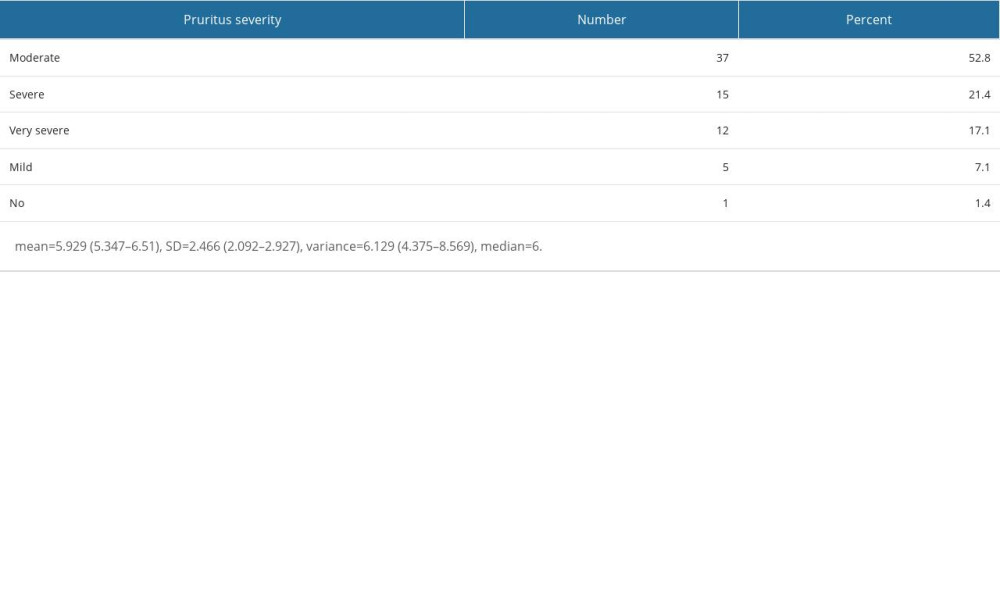 Table 1. Visual Assessment Scale (VAS) results of the study sample.
Table 1. Visual Assessment Scale (VAS) results of the study sample.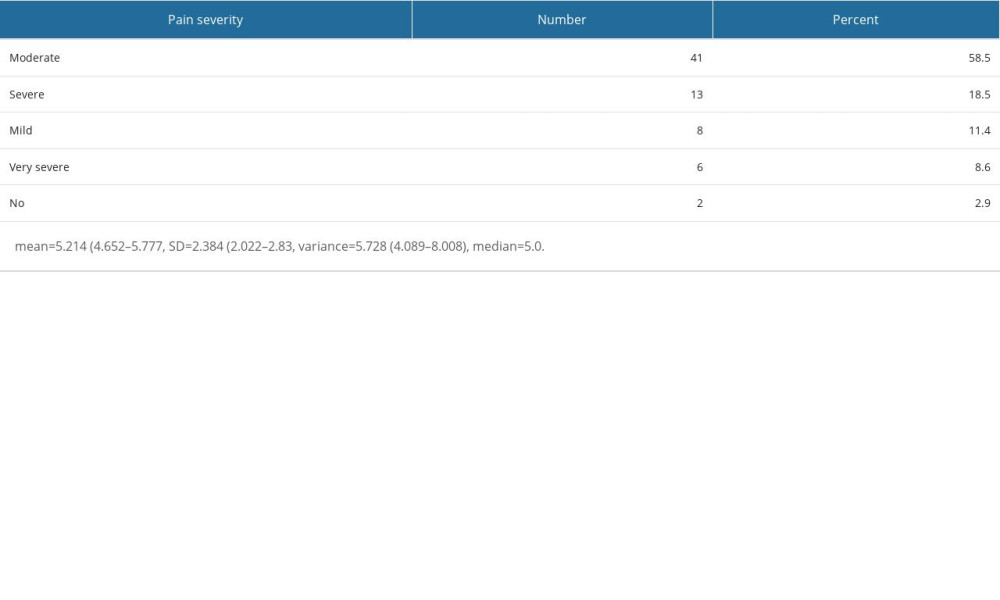 Table 2. Numeric Pain Rating Scale (NRS) results of the study sample.
Table 2. Numeric Pain Rating Scale (NRS) results of the study sample.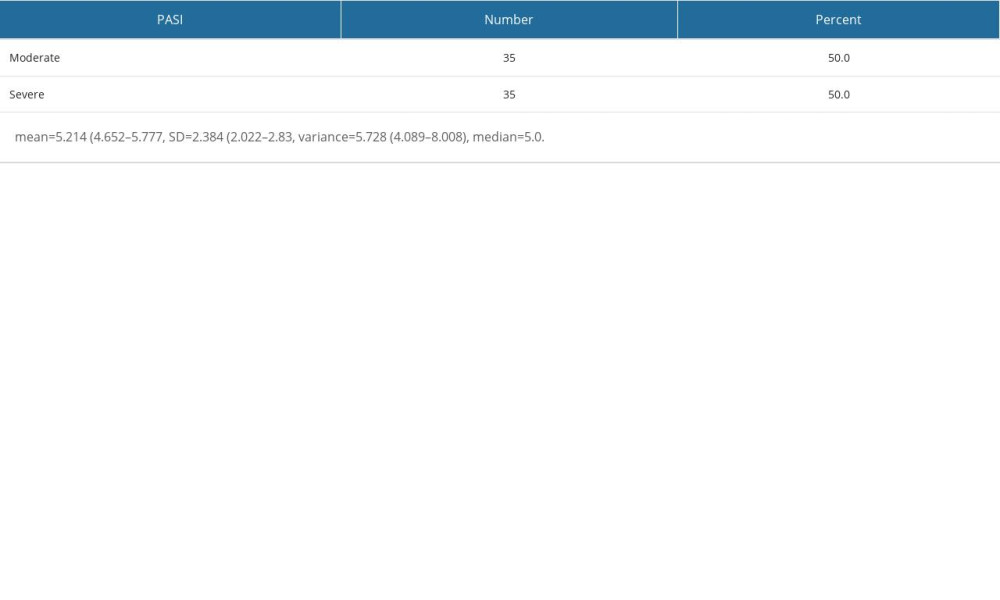 Table 3. Psoriasis Area and Severity Index (PASI) results of the study sample.
Table 3. Psoriasis Area and Severity Index (PASI) results of the study sample.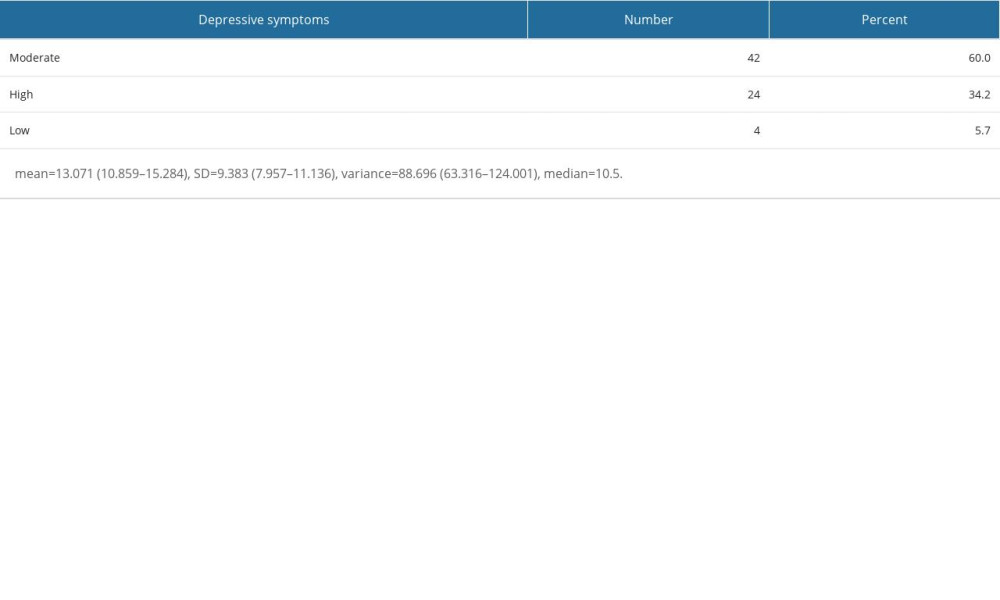 Table 4. Beck Depression Inventory (BDI) results of the study sample.
Table 4. Beck Depression Inventory (BDI) results of the study sample.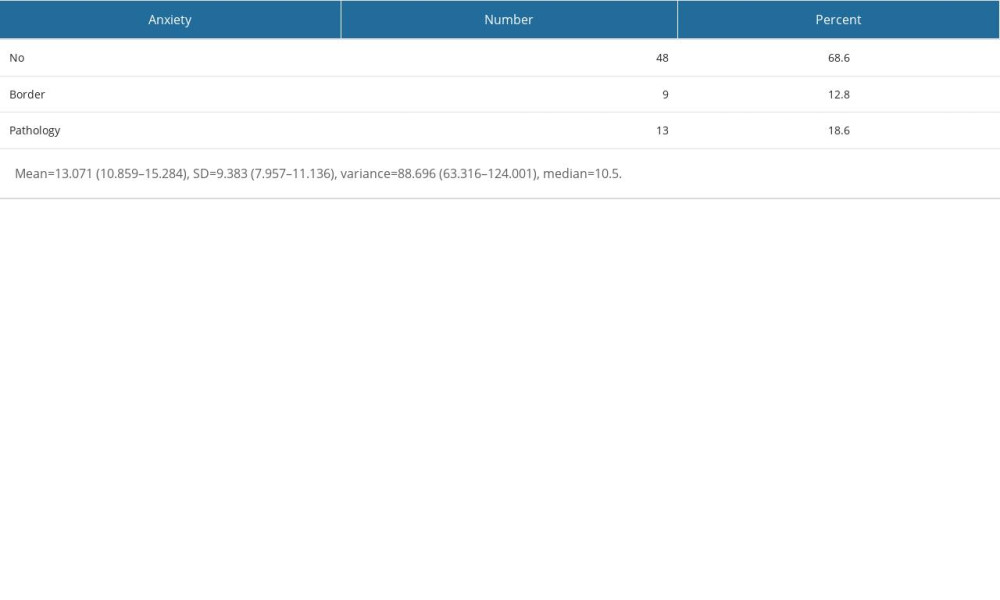 Table 5. Hospital Anxiety and Depression Scale – Anxiety (HADS-A) results of the study sample.
Table 5. Hospital Anxiety and Depression Scale – Anxiety (HADS-A) results of the study sample.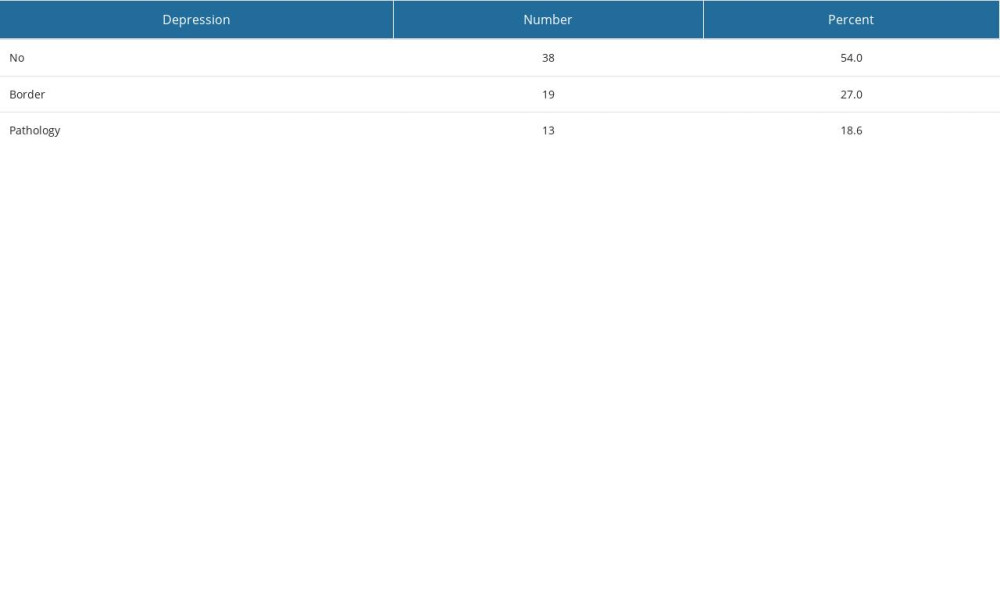 Table 6. Hospital Anxiety and Depression Scale – Anxiety (HADS-D) results of the study.
Table 6. Hospital Anxiety and Depression Scale – Anxiety (HADS-D) results of the study.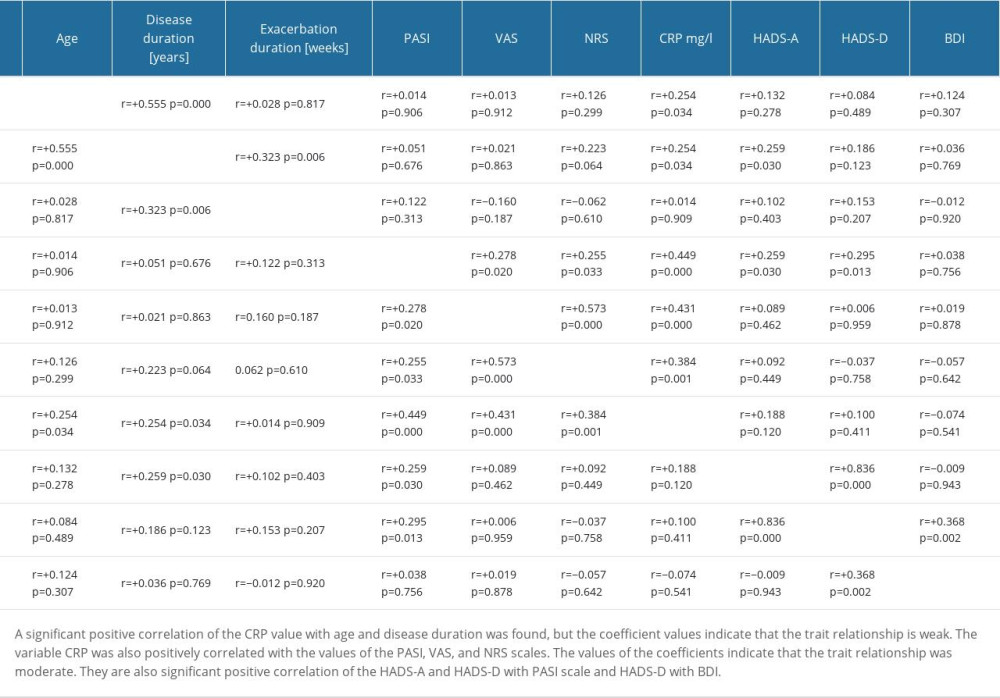 Table 7. Spearman rank correlations.
Table 7. Spearman rank correlations. In Press
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








