22 November 2023: Clinical Research
Prevalence and Risk Factors for Modic Changes in Symptomatic Cervical Ossification of the Posterior Longitudinal Ligament: A Retrospective Study of 203 Patients
Binbin LiuDOI: 10.12659/MSM.941674
Med Sci Monit 2023; 29:e941674
Abstract
BACKGROUND: Modic changes (MC) are abnormal bone signals under the vertebral endplates on magnetic resonance imaging (MRI) of the spine. Three types of MC may be seen on MRI as abnormal bone signals of the vertebral endplate and adjacent bone marrow. This retrospective study of 203 patients with symptomatic cervical ossification of the posterior longitudinal ligament (OPLL) aimed to evaluate factors associated with MC on cervical spine MRI.
MATERIAL AND METHODS: We included 203 patients with symptomatic cervical ossification of the OPLL. All patients underwent MRI with T1 and T2 sequences to assess the presence and type of MC. Univariate and multivariate logistic regression analyses were used to identify the risk factors for MC.
RESULTS: The prevalence of MC in patients with symptomatic cervical OPLL was 21.18%. Type 2 MC accounted for 88.64% of the cases. Local type and MC share the same segment (100.00%), followed by segmental type (77.27%), mixed type (75.00%), and continuous type (75.00%). Age (OR=1.05, 95% CI: 1.01-1.09, P=0.013) and neck pain (OR=2.67, 95% CI: 1.04-6.83, P=0.041) were significantly correlated with MC. Further receiver operating characteristic (ROC) analysis displayed an area under the curve (AUC) of 0.657 (P=0.002) for age, and the optimal cutoff was 60.50 years (sensitivity 0.67, specificity 0.68).
CONCLUSIONS: The results of this study found that older age and neck pain were significantly associated with development of cervical spine MC. Patients ≥60.5 years with symptomatic cervical OPLL had a higher probability of developing MC.
Keywords: Neck Pain, Ossification of the Posterior Longitudinal Ligament of the Spine, Risk Factors
Background
Modic changes (MC) are abnormal bone signals under the vertebral endplates on magnetic resonance imaging (MRI) of the spine, classified by Modic in 1988, suggesting vertebral endplates and bone marrow lesions near the vertebral body [1]. The magnetic resonance imaging T1 sequence and T2 sequence showed different signal changes in the 3 types of MC [2]. The 3 types of MCs are: Type 1, which shows a hypointense signal seen on T1 sequences and a hyperintense signal seen on T2 sequences; Type 2, which shows a hyperintense signal seen on T1 sequences and a hyperintense or isointense signal seen on T2 sequences; and Type 3, which shows a hypointense signal seen on T1 and T2 sequences [3]. Type 1 MC represents vascularized bone marrow and edema; Type 2 MC includes fatty change of the bone marrow; and Type 3 MC, which is rare, represents subchondral sclerosis. Types 1, 2, and 3 MC evolve and have been previously shown to be associated with advancing cervical vertebral degeneration [4]. Peterson et al first found that cervical spine MRI MCs were also present in 2007; 19 cases (16%) had MCs, and cervical spine MCs gradually became a focus of clinical research [5]. Yang et al analyzed 223 cases of single-segment nerve root neck type treated by surgery, and the imaging data of patients with spondylosis showed that 18% of patients had cervical spine MCs [6]. Kong et al found that in patients with cervical degenerative diseases, the incidence of cervical spine MCs was 12.34% [7]. Leboeuf-Yde et al proposed that heavy physical labor increased stress on the intervertebral disc, which eventually led to the occurrence and development of MC [8]. Mok et al reported that disc herniation can cause MC. Symptomatic cervical ossification of the posterior longitudinal ligament (OPLL) is attributed to heterotopic ossification of the cervical posterior longitudinal ligament, which results in spinal cord compression and neurological deterioration. Ossification of the posterior longitudinal ligament of the cervical spine directly compresses the nerve root or spinal cord, resulting in spinal cord involvement [9]. Cervical OPLL consists 4 types of cervical OPLL: continuous, segmental, mixed, and local. The age of onset of OPLL was 50–60 years old, and there was a significant sex difference, with a male-to-female ratio of approximately 2–3: 1 [10]. There have been few studies on whether ossification of the cervical posterior longitudinal ligament is associated with MC. Therefore, this retrospective study of 203 patients with ossification of the posterior longitudinal ligament aimed to evaluate factors associated with MC on cervical spine MRI.
Material and Methods
ETHICS STATEMENT:
This study was approved by the Ethics Committee of the Third Hospital of Hebei Medical University. Since this study was retrospective, the ethics committee agreed to sign a waiver of informed consent, and the ethics committee requires that the entire research process be kept strictly confidential and the collection of personal information such as the patient’s name and address is strictly prohibited.
INCLUSION AND EXCLUSION CRITERIA FOR STUDY PARTICIPANTS:
Patients presenting from July 2014 to April 2022 for symptomatic cervical ossification of the posterior longitudinal ligament, such as myelopathy, were included in our study. All patients were scanned using computed tomography (CT) and were divided into 4 types according to their scan results. The exclusion criteria were as follows: (1) patients with cervical OPLL without spinal symptoms; (2) cervical spine fractures; (3) cervical tumor; (4) previous cervical spine surgeries; (5) ankylosing spondylitis and immune disorders associated with OPLL, and (6) incomplete patient information and blank selection [11–13]. From this database, a total of 203 patients with symptomatic cervical ossification of the posterior longitudinal ligament were collected, and 43 patients were identified as having MC from July 2014 to April 2022 and were assessed for prevalence and risk factors.
CLASSIFICATION OF MC ON MRI:
All patients were examined using a 3.0-imager (Siemens Magnetic Symphony; Siemens, Berlin, Germany) to assess for the presence of MC. The magnetic resonance imaging T1 sequence and T2 sequence showed different signal changes in the 3 types of MC. According to the classification criteria specified by Modic et al, type 1 represents vascularized bone marrow and/or edema, with hypointensity on MRI T1 images and hyperintensity on MRI T2 images; type 2 represents proliferation of fatty tissue, and hyperintensity on MRI T1 image, MRI T2 images are hypointense or isointense; type 3 represents subchondral bone sclerosis, and both T1 and T2 MRI images are hypointense. Figure 1 shows an example of segmental OPLL with type 2 MC at the C5–6 levels on cervical MRI. The classification of MC on MRI was performed by 2 independent reviewers who obtained images without screening patient information, and disagreements between the 2 reviewers were finally decided by a third reviewer [14–17].
DATA COLLECTION PROCESS AND COLLECTION METHODS:
The demographic and clinical characteristics of patients with symptomatic cervical ossification of the posterior longitudinal ligament were divided into: age (years), sex (female and male), weight (<65 and ≥65 kg), body mass index (BMI; <25 and ≥25 kg/m2), neck pain (without neck pain and with neck pain), physical workload category (no heavy and heavy), smoking history (yes or no), drinking history (yes or no), combined diabetes (yes or no), combined hypertension (yes or no), and combined coronary heart disease (yes or no). The patient’s occupation was divided into sedentary, light physical labor, moderate physical labor, and heavy and very heavy physical labor. Patients with the first 3 workloads were defined as “non-heavy,” and patients with the last 2 workloads were defined as “heavy” [18].
The laboratory tests of patients with symptomatic cervical ossification of the posterior longitudinal ligament were divided into: white blood cell (WBC), neutrophil percentage (NEUT%), high-density lipoprotein (HDL), low-density lipoprotein (LDL), and triglyceride (TRIG); C2–7 Cobb angle (<20° and ≥20°); cervical alignment and range of motion/ROM (<40° and ≥40°); type of cervical ossification of the posterior longitudinal ligament (mixed, local, segmental, and continuous); k line [(+) and (−)]; and the relationship between MC and OPLL on sagittal CT images (same segment, adjacent segment, and different segment). The cervical spine was measured using SL radiography. C2–7 Cobb angle was defined as the angle formed by a straight line parallel to the lower endplate of the C2 vertebral body and a straight line parallel to the lower endplate of the C7 vertebral body. C2–7 range of motion (ROM) was determined by measuring the Cobb angle of cervical hyperextension and hyperflexion, in which hyperextension is α, hyperflexion is β (negative value when cervical kyphosis), and ROM=α+β. On the CT sagittal plane, OPLL was divided into 4 types: continuous, segmental, mixed and local. The K line is a virtual line connecting the midpoint of the anterior and posterior diameter of the spinal canal from C2 to C7. Ossification of OPLL beyond the K line is called the K line (−) or the K line (+). On the CT sagittal plane, MC and OPLL location were divided into the same segment, adjacent segment, and different segment [19,20]. We converted some continuous variables into binary variables (body weight ≥65 kg, body weight <65 kg; BMI ≥25 kg/m2, <25 kg/m2; C2–7 Cobb angle ≥20°, <20°; C2–7 ROM ≥40°, <40°) based on the research of Bai et al [21].
STATISTICAL ANALYSIS:
Statistical analyses were performed using SPSS version 25.0 (IBM, Armonk, NY, USA). Differences in the prevalence of MC were analyzed using Pearson’s chi-squared test or rank-sum test. The risk factors for MC were first determined using univariate logistic regression (
Results
DEMOGRAPHIC CHARACTERISTICS OF MC:
In total, 203 patients with symptomatic cervical OPLL were included in our study. Among them, 43 (21.18%) patients had MC and 160 (78.82%) had no MC. The prevalence of MC in males and females was 18.88% and 15.38%, respectively, and there was no statistically significant difference between the groups with and without MC in terms of sex (χ2=0.063a, P=0.802). The prevalence of MC in patients weighing <65 and ≥65 kg was 9.52% and 22.53%, respectively, and there was no significant difference in weight between patients with and without MC (χ2=1.907a, P=0.167). The prevalence of MC <25 kg/m2 and ≥25 kg/m2 was 27.78% and 19.76%, respectively, and there was no significant difference in the BMI between patients with and without MC (χ2=1.140a, P=0.286). There was no significant difference in the prevalence of WBC, NEUT%, HDL, LDL, or TRIG between the 2 groups with or without MC. This study showed that there were significant differences in the distribution of MC patients according to neck pain (χ2=5.005a, P=0.025). The laboratory test results and other clinical data are presented in Table 1.
IMAGING FEATURES OF THE MC:
The number of vertebral segments with MC was 50, and the numbers of type 1, type 2, and type 3 MC were 3 (6.00%), 45 (90.00%), and 2 (4.00%), respectively. The most common site of MC was C5–6 (40.00%), followed by C2–3 (20.00%), C6–7 (14.00%), C3–4 (14.00%), C4–5 (12.00%), and C1–2 (0.00%) (Figure 2). There were 136 vertebral segments with OPLL, and the number of mixed, local, segmental, and continuous were 54 (39.71%), 5 (3.68%), 64 (47.06%) and 13 (9.56%), respectively. The OPLL was most frequent at C5–6 (25.00%), followed by C4–5 (23.53%), C3–4 (20.59%), C6–7 (15.44%), C2–3 (11.03%), and C1–2 (4.41%) (Figure 3). The relationship between the vertebral body segment with MC and the vertebral body segment with OPLL was defined as same segment, adjacent segment, and non-adjacent segment, and the number of same segment, adjacent segment, and non-adjacent segment were 34 (79.07%), 6 (13.95%), and 3 (6.98%), respectively. Local type and MC share the same segment (100.00%), followed by segmental type (77.27%), mixed type (75.00%), and continuous type (75.00%) (Figure 4). OPLL and MC share the same segment in type 3 MC, with a ratio of 100.00%, followed by type 2 MC (79.49%), and type 1 MC (66.67%) (Figure 5).
RISK FACTORS FOR DEVELOPING THE MC:
According to univariate logistic analysis, multiple characteristics were significantly related to MC. These factors included age (OR=1.05, 95% CI: 1.01–1.09, P=0.011), and neck pain (OR=2.76, 95% CI: 1.10–6.91, P=0.030). Multivariate logistic analysis showed that OPLL type was significantly associated with MC. These items were: age (OR=1.05, 95% CI: 1.01–1.09, P=0.013), and neck pain (OR=2.67, 95% CI: 1.04–6.83, P=0.041) (Table 2).
We selected MCs as the state variable and age as the test variable. The area under ROC curve between MC and age was shown in Figure 6 (AUC=0.657, P=0.002). Based on the ROC curve, the age corresponding to the optimal Youden index (0.349) was 60.50 (sensitivity: 0.67, specificity: 0.68). It could be assumed that 60.5 years was the critical age for MC, with a higher probability of MC for ≥60.5 years and a lower probability of MC for <60.5 years.
Discussion
OPLL was first reported by Key in 1838. It is generally believed that OPLL is mainly found in East Asians, especially the Japanese, but now it has been found in Europe and the United States [22,23]. European and American scholars believe that OPLL is a subtype of diffuse idiopathic skeletal hyperosteosis (DISH) [24–26]; but there have been few studies on cervical posterior longitudinal ligament ossification and MC.
MC is a common imaging manifestation on MRI, suggesting lesions of the vertebral endplate and bone marrow. In our study, we found that the most common type of MC in patients with cervical posterior longitudinal ligament ossification was type 2 MC. Peterson et al reported that type 1 MC was the most common type in patients with symptomatic cervical spondylosis [5], while Mann et al and Hayashi et al found that type 2 MC was the most common [27,28]. The conclusions of this study are similar to those of Hayashi et al. Li et al found that patients in the total disc replacement group had more significant improvement in neck pain, perhaps because more inflammatory disc tissue was removed, which is related to the effect of inflammation on cervical MCs [29]. This study found that inflammatory factors were not the influencing factors of MC in patients with cervical posterior longitudinal ligament ossification. Kong et al found that in patients with cervical spine degeneration, cervical MCs were associated with chronic neck pain, and the neck pain score of patients with type 1 MCs was significantly higher than that of patients with type 2 MCs [30]. This study found that neck pain is an influencing factor of MC in patients with cervical posterior longitudinal ligament ossification, and it was not possible to compare the differences in neck pain between the different MCs types due to the small number of type 1 MCs and type 3 MCs medical records. An et al found that for patients with cervical kyphosis associated with MCs, the range of motion between single cervical spine segments was significantly reduced [31]. Hayashi et al found that MC can lead to cervical stiffness, loss of mobility, and severe instability [32], and that cervical ROM was not an influencing factor of MC in patients with ossification of the posterior longitudinal ligament. Li et al found that the onset of MC in either the cervical or lumbar spine was age-related, and that MC increased with age, and also found that older age (≥60.5 years) was significantly associated with the occurrence of MC in cervical OPLL [33].
Our study had several limitations. First, it did not assess whether the severity and duration of neurological symptoms in the selected population affected MC. Second, it did not determine whether the selected population had cervical disc herniation and whether it affected MC. Finally, further research is needed to validate our results.
Conclusions
We found that older age and neck pain were significantly associated with development of cervical spine MC. Clinicians should pay attention to the possible occurrence of MC in patients aged ≥60.5 years with symptomatic cervical OPLL.
Figures
 Figure 1. A segmental OPLL with type 2 MC at the C5–6 level. From left to right: X-ray, CT sagittal, T1 sequence, and T2 sequence of MRIs. This figure was created using GraphPad Prism (version 9, USA). OPLL – ossification of the posterior longitudinal ligament; MC – Modic change; MRI – magnetic resonance imaging.
Figure 1. A segmental OPLL with type 2 MC at the C5–6 level. From left to right: X-ray, CT sagittal, T1 sequence, and T2 sequence of MRIs. This figure was created using GraphPad Prism (version 9, USA). OPLL – ossification of the posterior longitudinal ligament; MC – Modic change; MRI – magnetic resonance imaging. 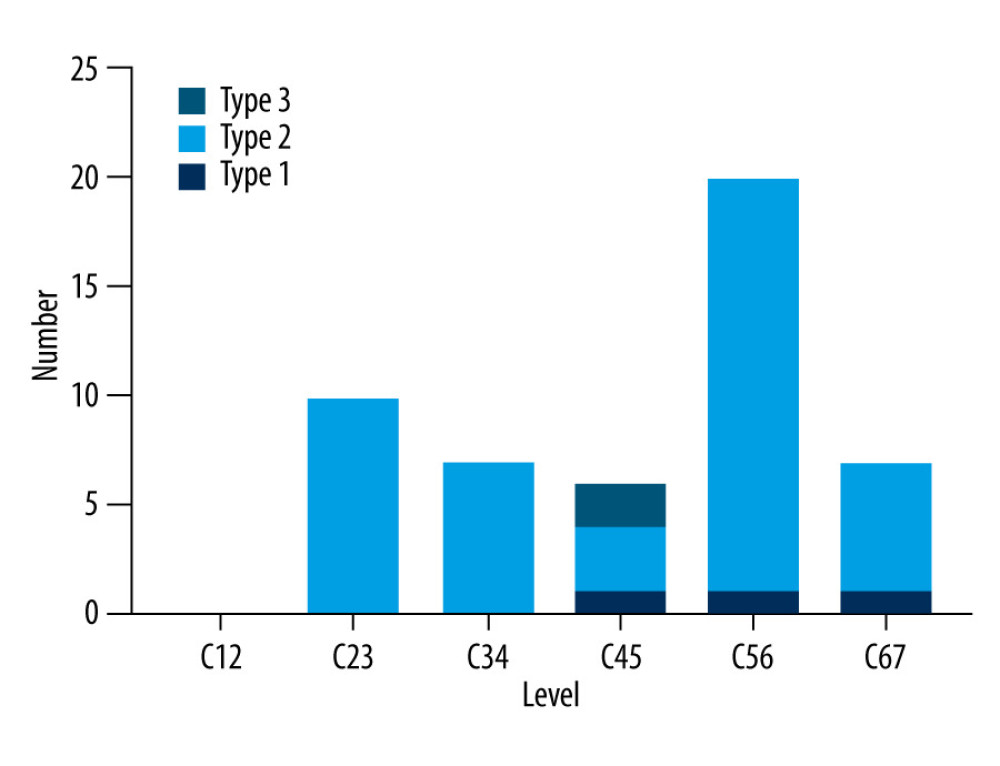 Figure 2. The distribution of MC according to cervical disc level. This figure was created using GraphPad Prism (version 9, USA). MC – Modic change.
Figure 2. The distribution of MC according to cervical disc level. This figure was created using GraphPad Prism (version 9, USA). MC – Modic change. 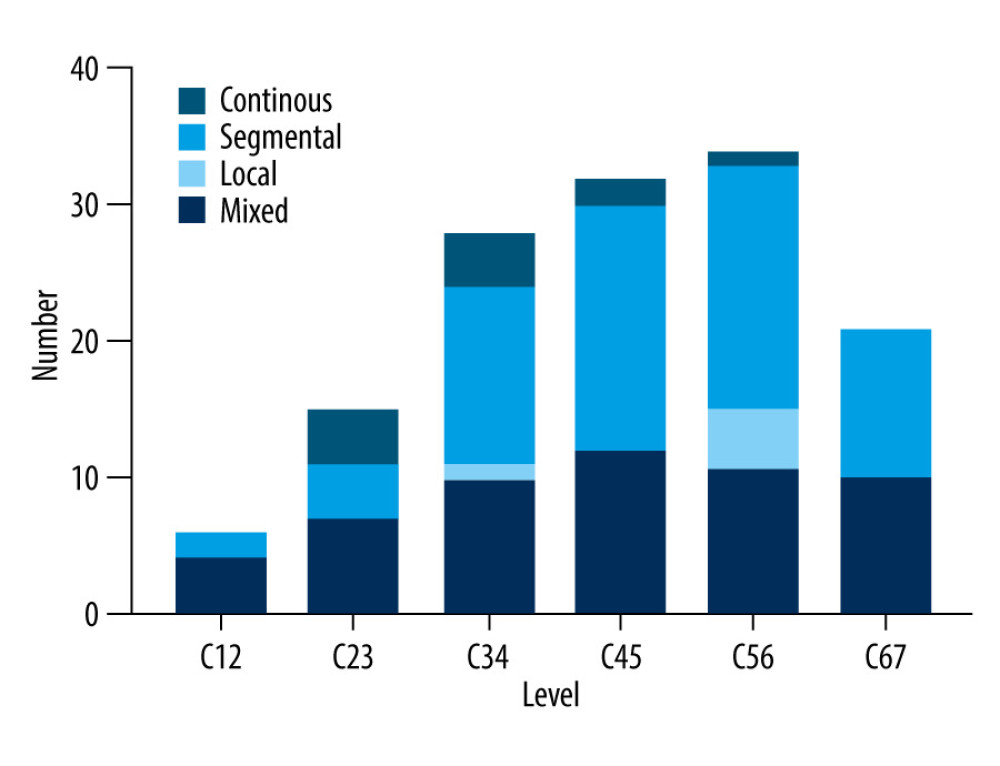 Figure 3. The distribution of OPLL typing according to cervical disc level. This figure was created using GraphPad Prism (version 9, USA). OPLL – ossification of the posterior longitudinal ligament.
Figure 3. The distribution of OPLL typing according to cervical disc level. This figure was created using GraphPad Prism (version 9, USA). OPLL – ossification of the posterior longitudinal ligament. 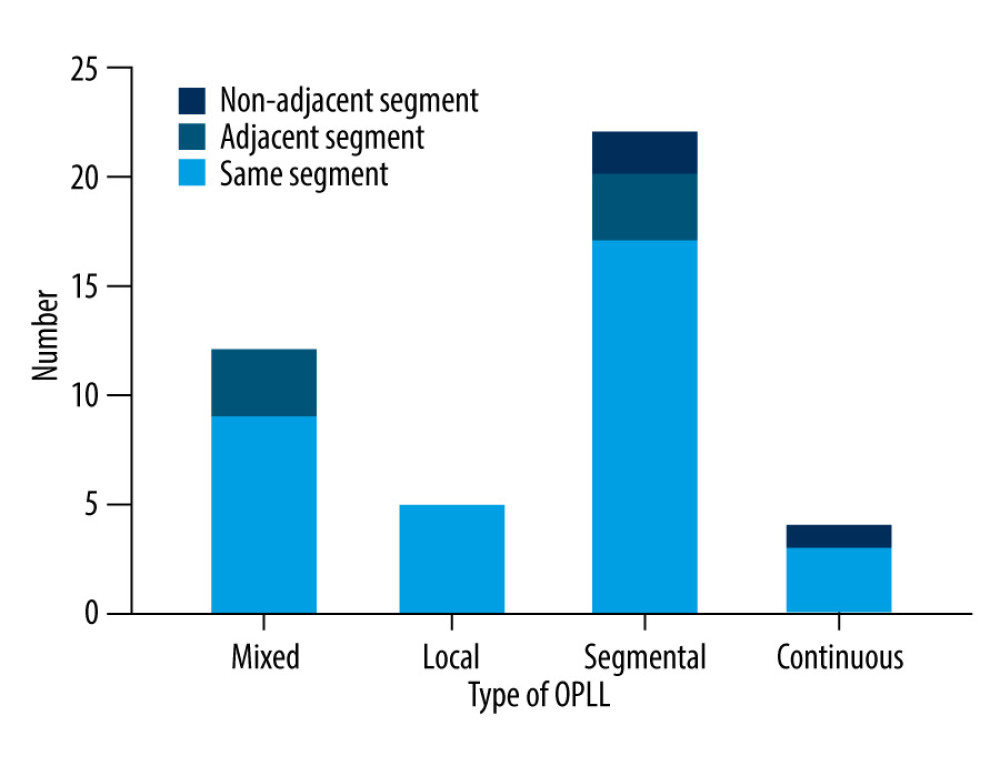 Figure 4. The relationship between cervical segments corresponding to different OPLL types and cervical MC segments. This figure was created using GraphPad Prism (version 9, USA). MC – Modic change; OPLL – ossification of the posterior longitudinal ligament.
Figure 4. The relationship between cervical segments corresponding to different OPLL types and cervical MC segments. This figure was created using GraphPad Prism (version 9, USA). MC – Modic change; OPLL – ossification of the posterior longitudinal ligament. 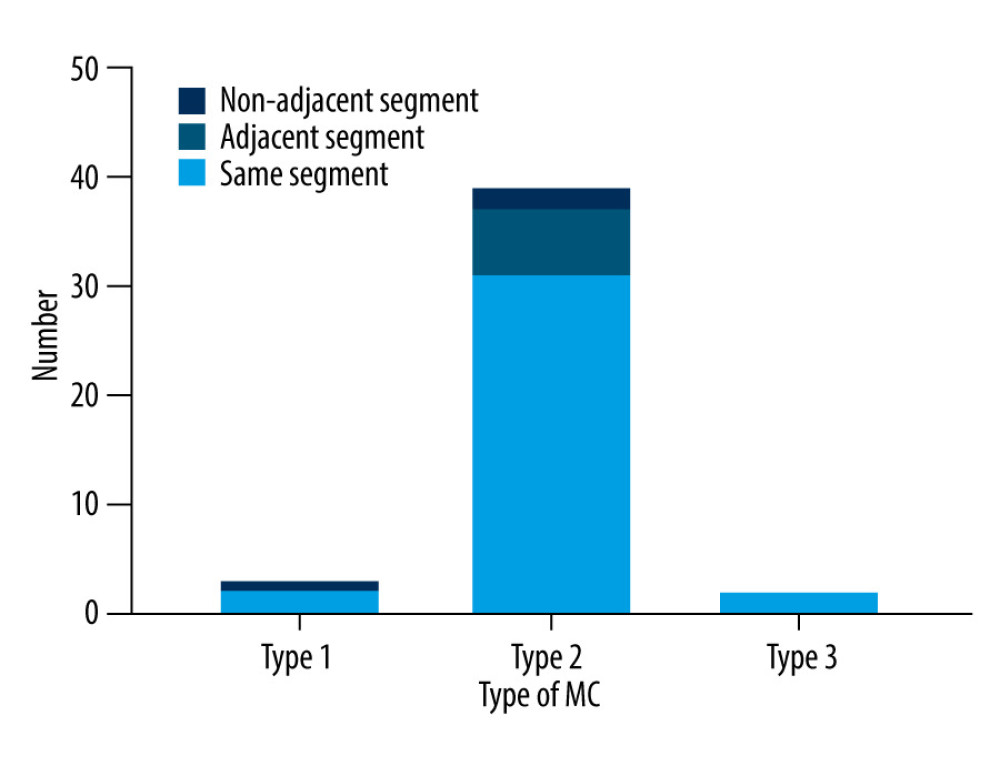 Figure 5. The relationship between cervical segments corresponding to different MC types and cervical OPLL segments. This figure was created using GraphPad Prism (version 9, USA). MC – Modic change; OPLL – ossification of the posterior longitudinal ligament.
Figure 5. The relationship between cervical segments corresponding to different MC types and cervical OPLL segments. This figure was created using GraphPad Prism (version 9, USA). MC – Modic change; OPLL – ossification of the posterior longitudinal ligament. 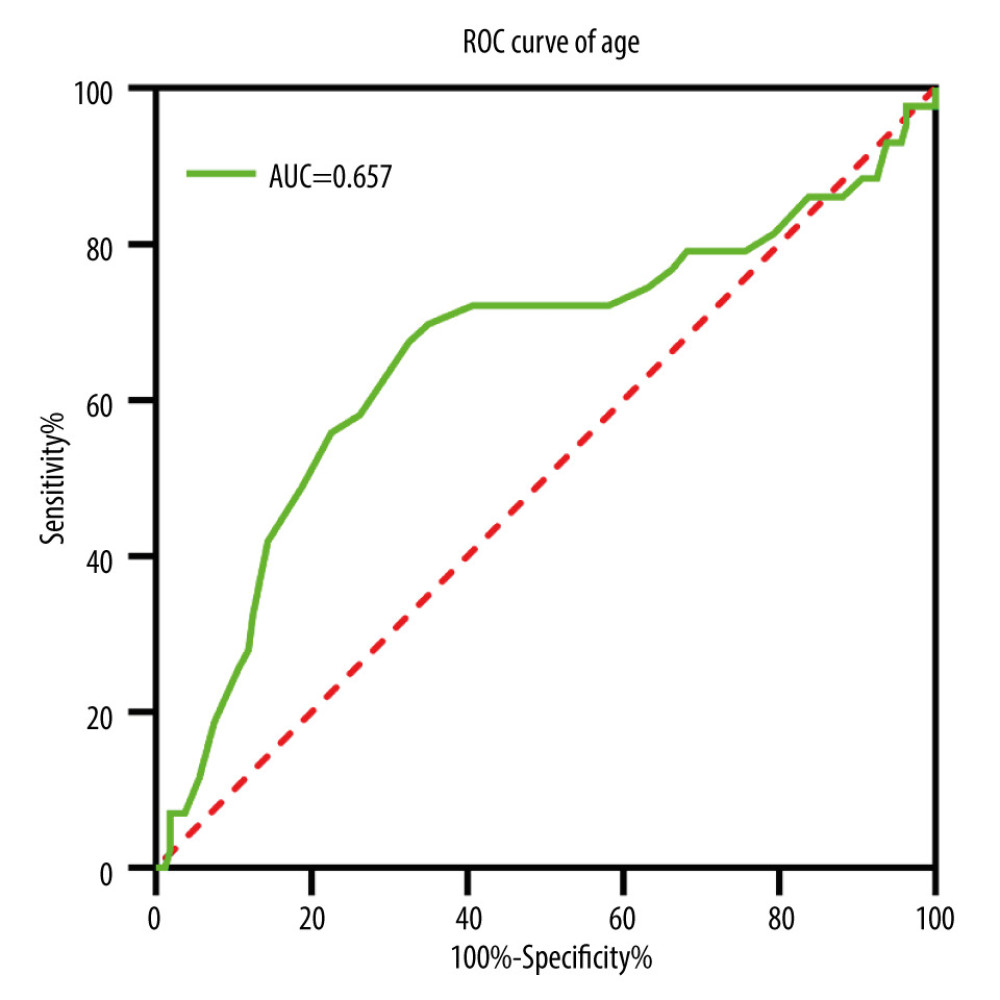 Figure 6. Receiver operating characteristics (ROC) curve of age in patients with symptomatic cervical ossification of the posterior longitudinal ligament for Modic changes. This figure was created using GraphPad Prism (version 9, USA).
Figure 6. Receiver operating characteristics (ROC) curve of age in patients with symptomatic cervical ossification of the posterior longitudinal ligament for Modic changes. This figure was created using GraphPad Prism (version 9, USA). Tables
Table 1. Univariate logistic regression analysis of characteristics of patients with symptomatic cervical ossification of the posterior longitudinal ligament (diagnosed between 2014 and 2022).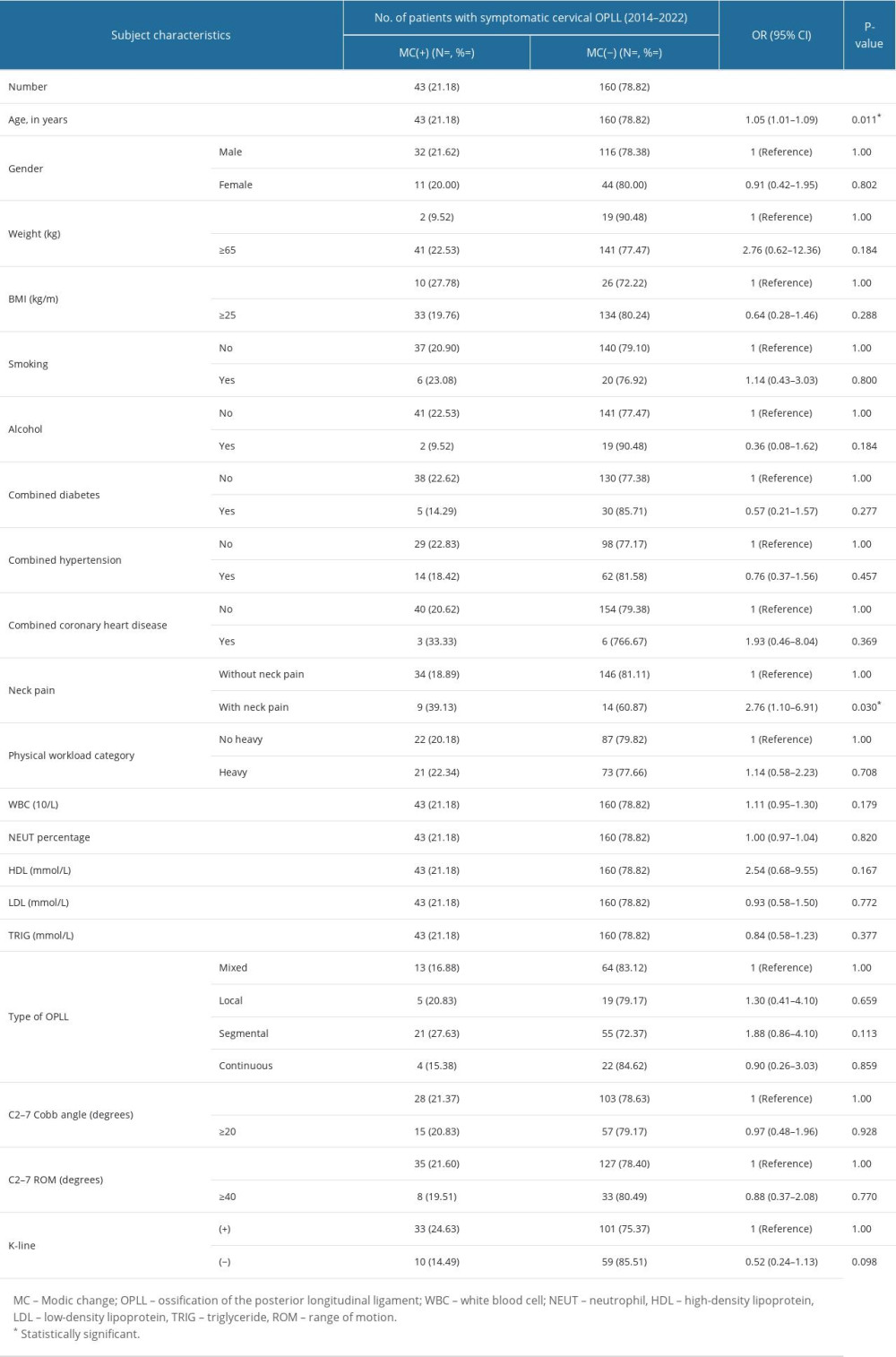 Table 2. Univariate and multivariate logistic regression analyses associated with MC in patients with symptomatic cervical ossification of the posterior longitudinal ligament (diagnosed between 2014 and 2022).
Table 2. Univariate and multivariate logistic regression analyses associated with MC in patients with symptomatic cervical ossification of the posterior longitudinal ligament (diagnosed between 2014 and 2022).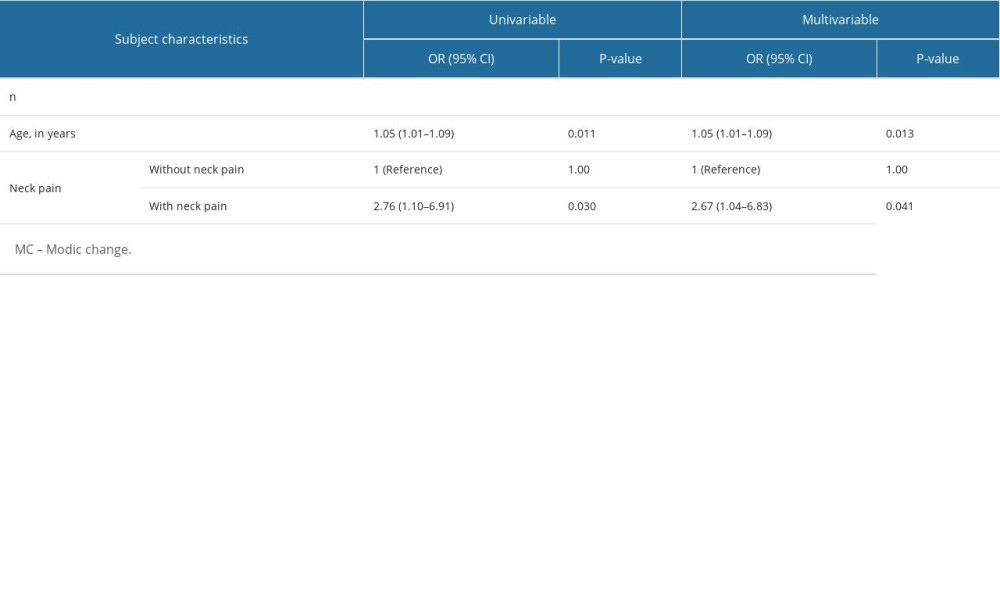
References
1. Modic MT, Steinberg PM, Ross JS, Degenerative disk disease: Assessment of changes in vertebral body marrow with MR imaging: Radiology, 1988; 166; 193-99
2. Dudli S, Fields AJ, Samartzis D, Pathobiology of Modic changes: Eur Spine J, 2016; 25(11); 3723-34
3. Chung CB, Berg BC, Tavernier T, End plate marrow changes in the asymptomatic lumbosacral spine: Frequency, distribution and correlation with age and degenerative changes: Skeletal Radiol, 2004; 33; 399-404
4. Modic MT, Masaryk TJ, Ross JS, Imaging of degenerative disk disease: Radiology, 1988; 168; 177-86
5. Peterson CK, Humphreys BK, Pringle TC, Prevalence of modic degenerative marrow changes in the cervical spine: J Manipulative Physiol Ther, 2007; 30; 5-10
6. Yang X, Donk R, Arts MP, Are Modic vertebral end-plate signal changes associated with degeneration or clinical outcomes in the cervical spine: World Neurosurg, 2019; 129; e881-e89
7. Kang KT, Son DW, Kwon O, Effect of Modic changes in cervical degenerative disease: Korean J Spine, 2017; 14; 41-43
8. Leboeuf-Yde C, Kjaer P, Bendix T, Manniche C, Self-reported hard physical work combined with heavy smoking or overweight may result in so-called Modic changes: BMC Musculoskelet Disord, 2008; 9; 5
9. Mok FP, Samartzis D, Karppinen J, Modic changes of the lumbar spine: Prevalence, risk factors, and association with disc degeneration and low back pain in a large-scale population-based cohort: Spine J, 2016; 16; 32-41
10. Hirai T, Yoshii T, Egawa S, Increased height of fused segments contributes to early-phase strut dislodgement after anterior cervical corpectomy with fusion for multilevel ossification of the posterior longitudinal ligament: Spine Surg Relat Res, 2020; 4; 294-99
11. Matsunaga S, Sakou T, Ossification of the posterior longitudinal ligament of the cervical spine: Etiology and natural history: Spine (Phila Pa 1976), 2012; 5; E309-14
12. Baker JD, Harada GK, Tao Y, The impact of Modic changes on preoperative symptoms and clinical outcomes in anterior cervical discectomy and fusion patients: Neurospine, 2020; 17; 190-203
13. Kitis S, Cevik S, Kaplan A, Relationship between degeneration or sagittal balance with Modic changes in the cervical spine: Cureus, 2021; 13; e12949
14. Gjefsen E, Braten LCH, Goll GL, The effect of infliximab in patients with chronic low back pain and Modic changes (the BackToBasic study): study protocol of a randomized, double blind, placebo-controlled, multicenter trial: BMC Musculoskelet Disord, 2020; 21; 698
15. Xiong Z, Ding J, Zhou J, Correlation between the HIF-1alpha/Notch signaling pathway and Modic changes in nucleus pulposus cells isolated from patients with low back pain: BMC Musculoskelet Disord, 2020; 21; 500
16. Bivona LJ, Camacho JE, Usmani F, The prevalence of bacterial infection in patients undergoing elective ACDF for degenerative cervical spine conditions: A prospective cohort study with contaminant control: Global Spine J, 2021; 11; 13-20
17. Sun Y, Yan C, Shen Y, Relation between neck pain and Modic changes in cervical spondylotic myelopathy: Med Sci Monit, 2020; 26; e923908
18. Ulrich NH, Burgstaller JM, Gravestock I, The influence of endplate (Modic) changes on clinical outcomes in lumbar spinal stenosis surgery: A Swiss prospective multicenter cohort study: Eur Spine J, 2020; 29; 2205-14
19. Huang K, Hong Y, Liu H, Is the bone fusion affected by Modic-2 changes in single-level anterior cervical discectomy and fusion: Medicine (Baltimore), 2020; 99; e18597
20. Nouri A, Cheng JS, Davies B, Degenerative cervical myelopathy: A brief review of past perspectives, present developments, and future directions: J Clin Med, 2020; 9; 535
21. Bai J, Yu K, Sun Y, Prevalence of and risk factors for Modic change in patients with symptomatic cervical spondylosis: an observational study: J Pain Res, 2018; 11; 355-60
22. Park JY, Chin DK, Kim KS, Thoracic ligament ossification in patients with cervical ossification of the posterior longitudinal ligaments: Tandem ossification in the cervical and thoracic spine: Spine (Phila Pa 1976), 2008; 33; E407-10
23. Hirai T, Yoshii T, Egawa S, Increased height of fused segments contributes to early-phase strut dislodgement after anterior cervical corpectomy with fusion for multilevel ossification of the posterior longitudinal ligament: Spine Surg Relat Res, 2020; 4; 294-99
24. Tsuyama N, Ossification of the posterior longitudinal ligament of the spine: Clin Orthop Relat Res, 1984; 184; 71-84
25. Hong M-W, Kim J-K, Park M-J, A case report on ossification of posterior longitudinal ligament treated by Korean medicine: Focusing on chunatherapy: J Korea CHUNA Manual Med Spine Nerves, 2020; 15; 135-45
26. Lee JK, Ham CH, Kwon W-K, Classification for cervical ossification of the posterior longitudinal ligament based on the coexistence of segmental disc degeneration: J Korean Neurosurg Soc, 2021; 64; 69
27. Mann E, Peterson CK, Hodler J, Degenerative marrow (modic) changes on cervical spine magnetic resonance imaging scans: Prevalence, Intel and intra-examiner reliability and the link to disc herniation: The Spine (Phila Pa 1976), 2011; 36; 1081-85
28. Hayashi T, Daubs MD, Suzuki A, Effect of Modic changes on spinal canal stenosis and segmental motion in cervical spine: Eur Spine J, 2014; 23; 1737-42
29. Li J, Zhang D, Ding W, Comparison of clinical outcomes after anterior cervical discectomy and fusion versus cervical total disk replacement in patients with Modic 2 changes on MRI: Clin Spine Surg, 2017; 30; E1088-E92
30. Kong L, Tian W, Cao P, Predictive factors associated with neck pain in patients with cervical disc degeneration: A cross-sectional study focusing on Modic changes: Medicine (Baltimore), 2017; 96; e8447
31. An Y, Li J, Li Y, Characteristics of Modic changes in cervical kyphosis and their association with axial neck pain: J Pain Res, 2017; 10; 1657-61
32. Nicholson KJ, Millhouse PW, Pflug E, Cervical sagittal range of motion as a predictor of symptom severity in cervical spondylotic myelopathy: Spine (Phila Pa 1976), 2018; 43; 883-89
33. Li SY, Letu S, Chen J, Comparison of modic changes in the lumbar and cervical spine, in 3167 patients with and without spinal pain: PLoS One, 2014; 9; e114993
Figures
 Figure 1. A segmental OPLL with type 2 MC at the C5–6 level. From left to right: X-ray, CT sagittal, T1 sequence, and T2 sequence of MRIs. This figure was created using GraphPad Prism (version 9, USA). OPLL – ossification of the posterior longitudinal ligament; MC – Modic change; MRI – magnetic resonance imaging.
Figure 1. A segmental OPLL with type 2 MC at the C5–6 level. From left to right: X-ray, CT sagittal, T1 sequence, and T2 sequence of MRIs. This figure was created using GraphPad Prism (version 9, USA). OPLL – ossification of the posterior longitudinal ligament; MC – Modic change; MRI – magnetic resonance imaging.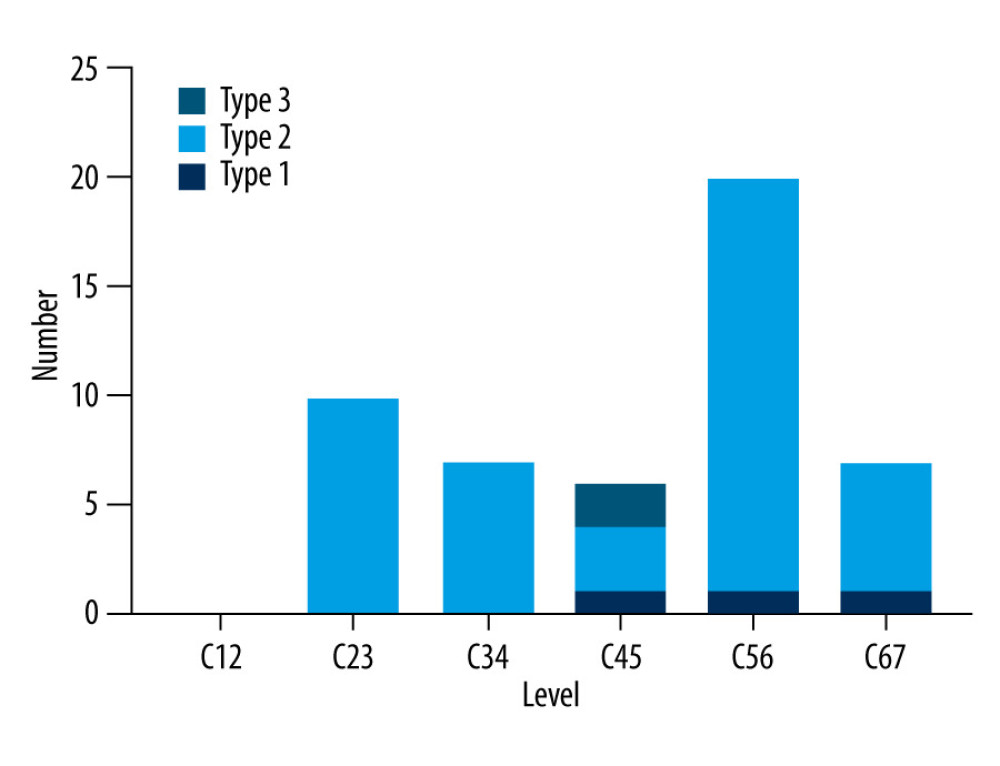 Figure 2. The distribution of MC according to cervical disc level. This figure was created using GraphPad Prism (version 9, USA). MC – Modic change.
Figure 2. The distribution of MC according to cervical disc level. This figure was created using GraphPad Prism (version 9, USA). MC – Modic change.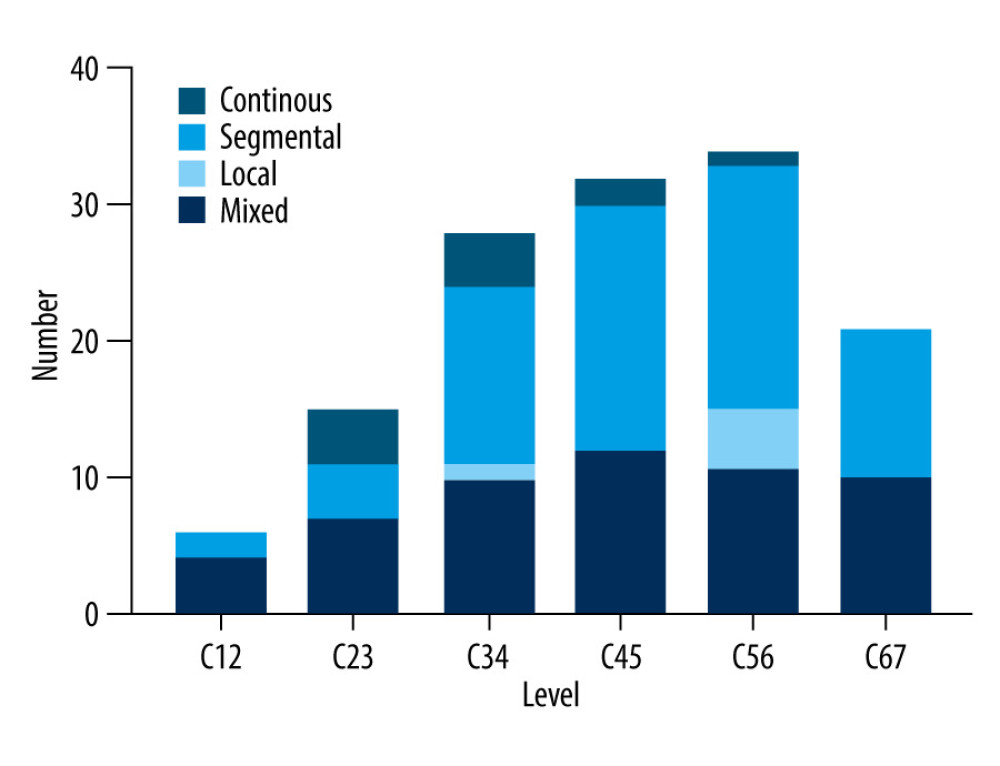 Figure 3. The distribution of OPLL typing according to cervical disc level. This figure was created using GraphPad Prism (version 9, USA). OPLL – ossification of the posterior longitudinal ligament.
Figure 3. The distribution of OPLL typing according to cervical disc level. This figure was created using GraphPad Prism (version 9, USA). OPLL – ossification of the posterior longitudinal ligament.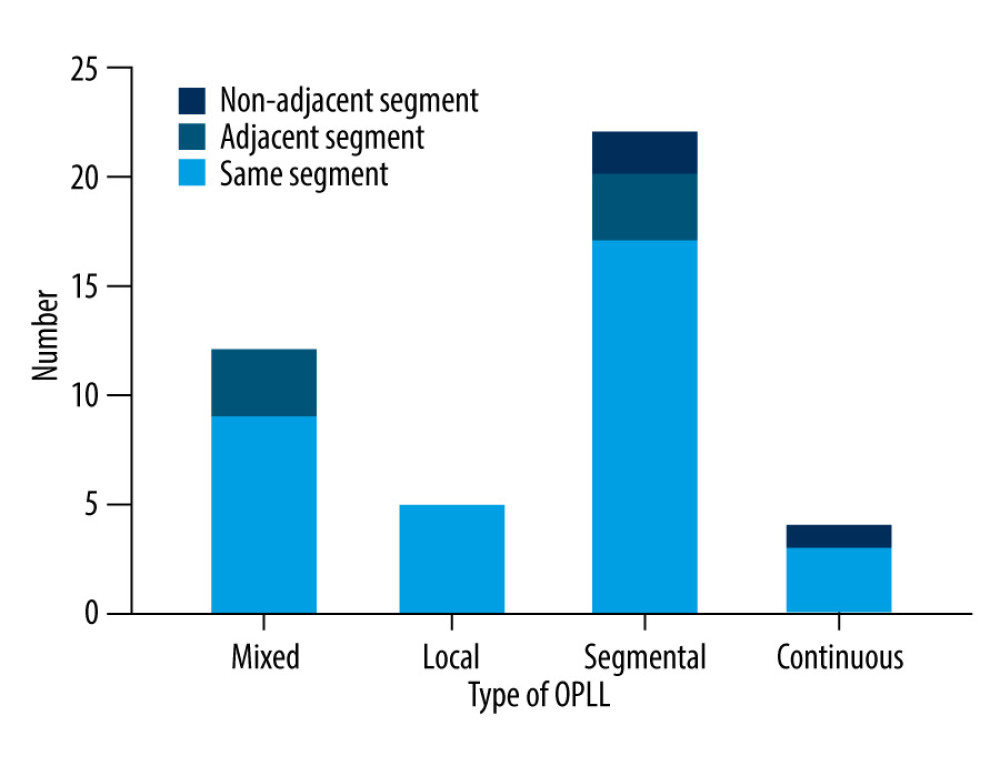 Figure 4. The relationship between cervical segments corresponding to different OPLL types and cervical MC segments. This figure was created using GraphPad Prism (version 9, USA). MC – Modic change; OPLL – ossification of the posterior longitudinal ligament.
Figure 4. The relationship between cervical segments corresponding to different OPLL types and cervical MC segments. This figure was created using GraphPad Prism (version 9, USA). MC – Modic change; OPLL – ossification of the posterior longitudinal ligament.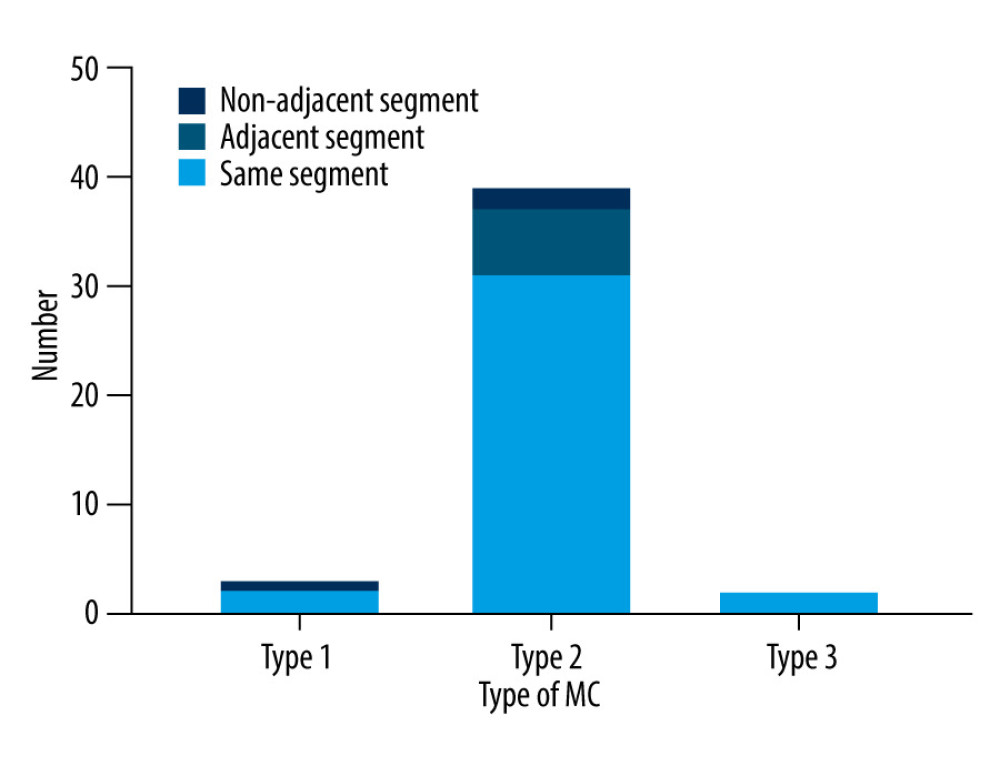 Figure 5. The relationship between cervical segments corresponding to different MC types and cervical OPLL segments. This figure was created using GraphPad Prism (version 9, USA). MC – Modic change; OPLL – ossification of the posterior longitudinal ligament.
Figure 5. The relationship between cervical segments corresponding to different MC types and cervical OPLL segments. This figure was created using GraphPad Prism (version 9, USA). MC – Modic change; OPLL – ossification of the posterior longitudinal ligament.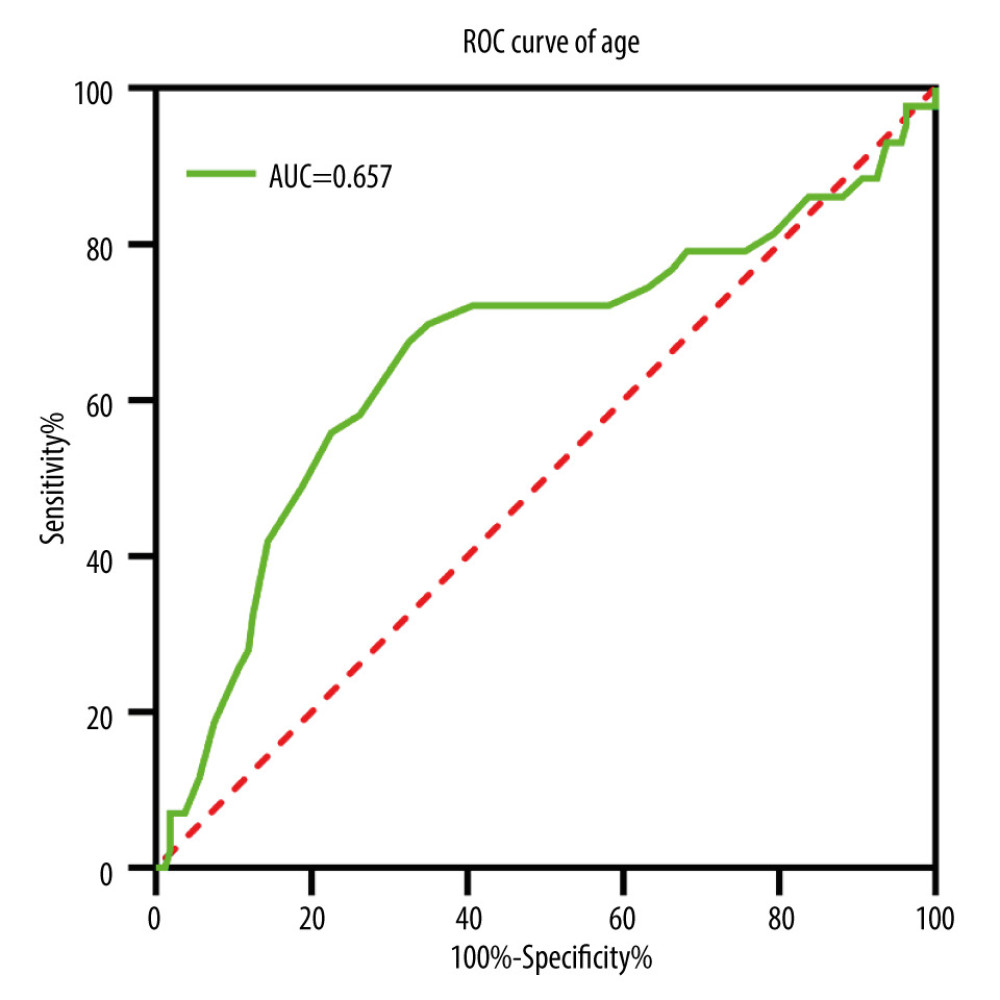 Figure 6. Receiver operating characteristics (ROC) curve of age in patients with symptomatic cervical ossification of the posterior longitudinal ligament for Modic changes. This figure was created using GraphPad Prism (version 9, USA).
Figure 6. Receiver operating characteristics (ROC) curve of age in patients with symptomatic cervical ossification of the posterior longitudinal ligament for Modic changes. This figure was created using GraphPad Prism (version 9, USA). Tables
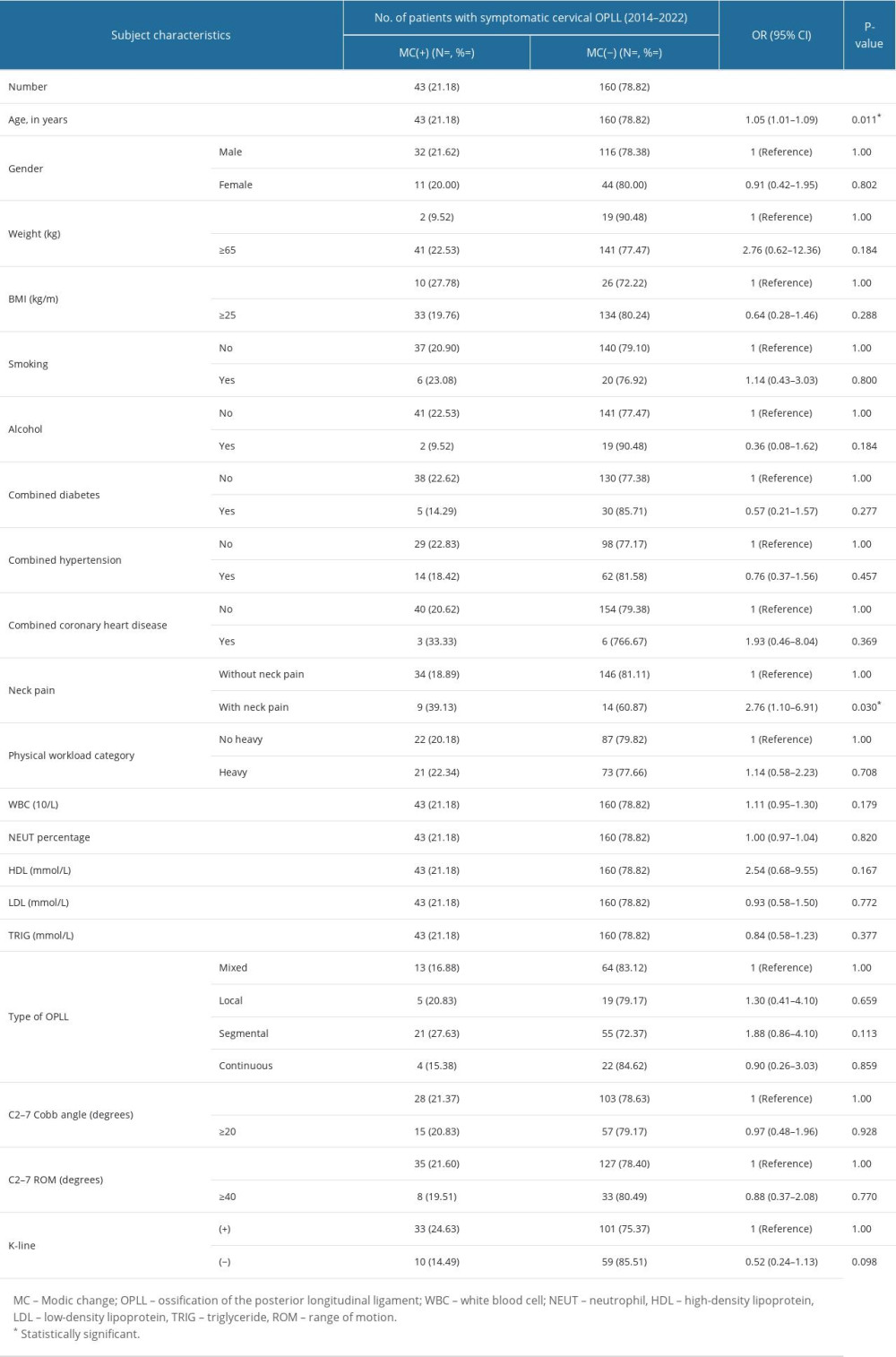 Table 1. Univariate logistic regression analysis of characteristics of patients with symptomatic cervical ossification of the posterior longitudinal ligament (diagnosed between 2014 and 2022).
Table 1. Univariate logistic regression analysis of characteristics of patients with symptomatic cervical ossification of the posterior longitudinal ligament (diagnosed between 2014 and 2022).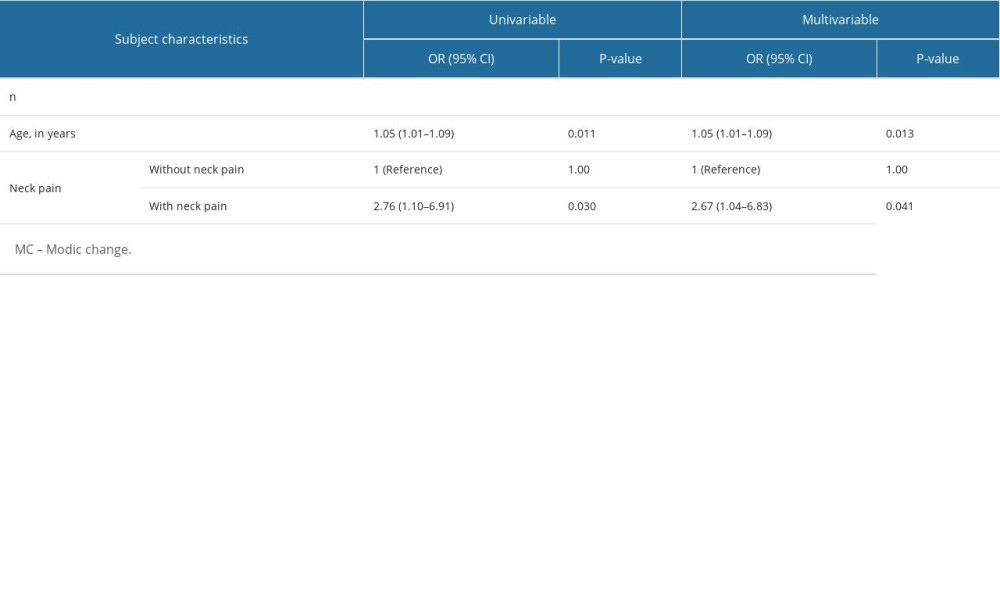 Table 2. Univariate and multivariate logistic regression analyses associated with MC in patients with symptomatic cervical ossification of the posterior longitudinal ligament (diagnosed between 2014 and 2022).
Table 2. Univariate and multivariate logistic regression analyses associated with MC in patients with symptomatic cervical ossification of the posterior longitudinal ligament (diagnosed between 2014 and 2022).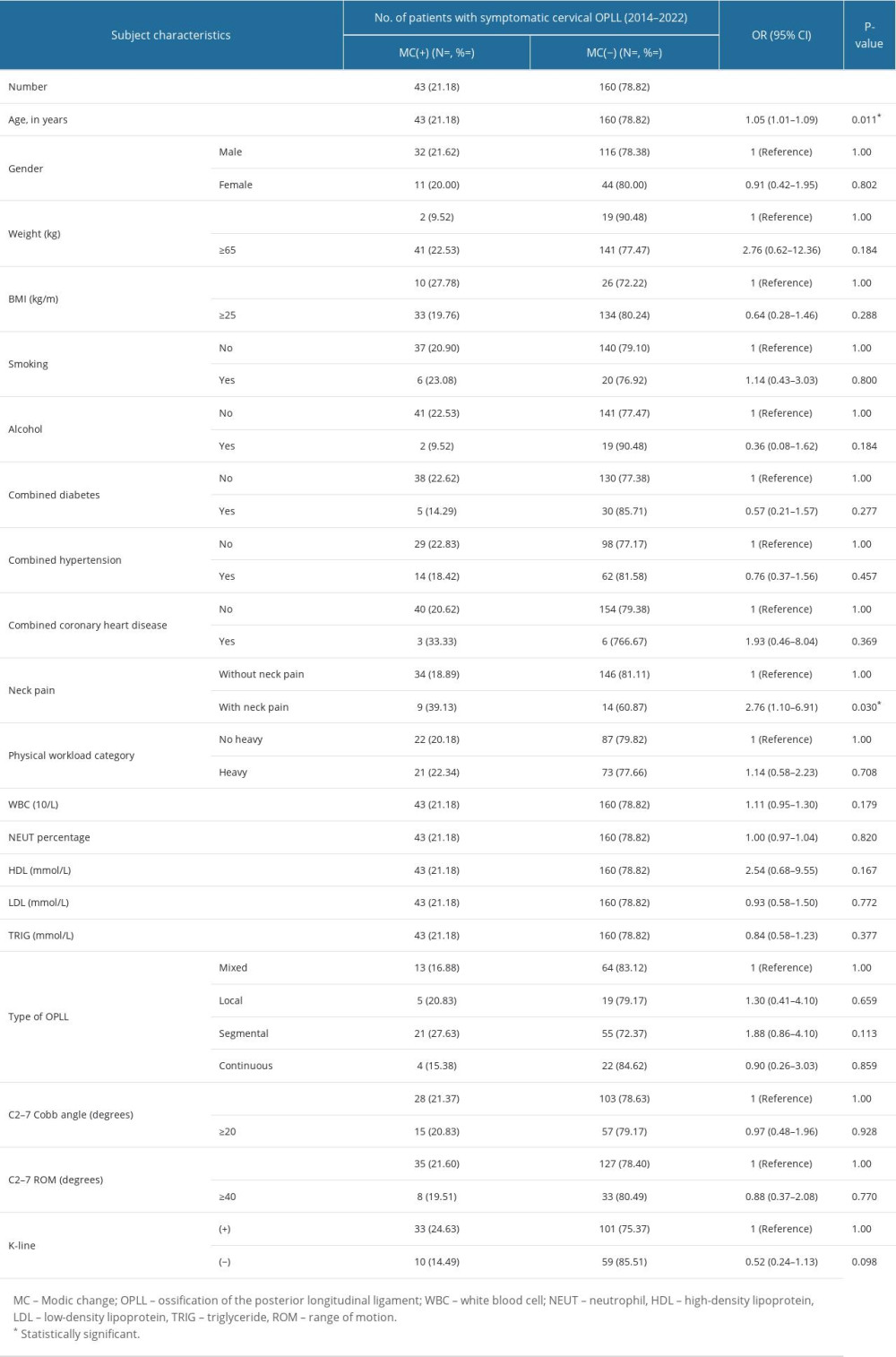 Table 1. Univariate logistic regression analysis of characteristics of patients with symptomatic cervical ossification of the posterior longitudinal ligament (diagnosed between 2014 and 2022).
Table 1. Univariate logistic regression analysis of characteristics of patients with symptomatic cervical ossification of the posterior longitudinal ligament (diagnosed between 2014 and 2022).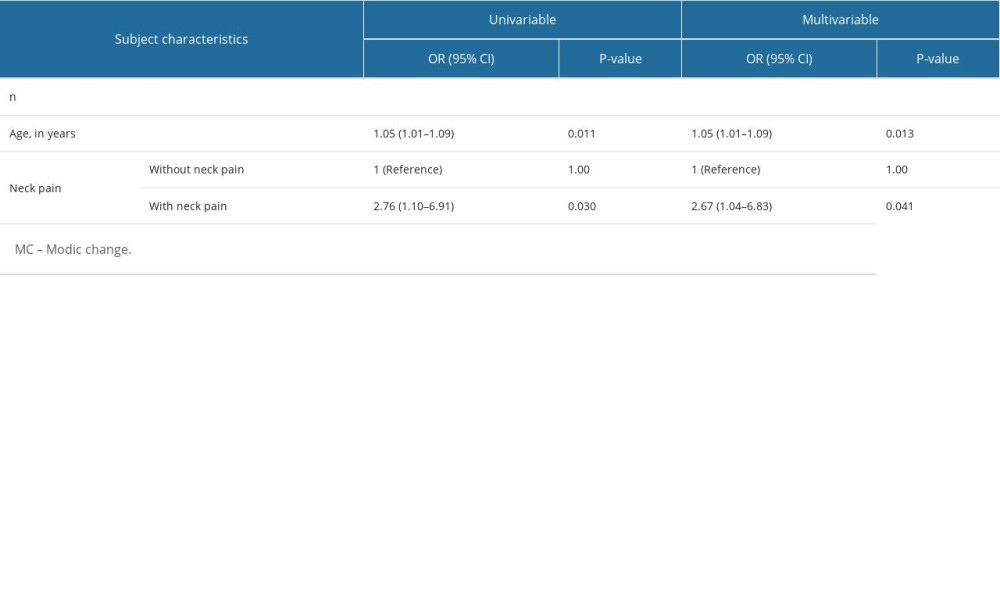 Table 2. Univariate and multivariate logistic regression analyses associated with MC in patients with symptomatic cervical ossification of the posterior longitudinal ligament (diagnosed between 2014 and 2022).
Table 2. Univariate and multivariate logistic regression analyses associated with MC in patients with symptomatic cervical ossification of the posterior longitudinal ligament (diagnosed between 2014 and 2022). In Press
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
12 Mar 2024 : Clinical Research
Tissue Inhibitors of Metalloproteinase 1 (TIMP-1) and 3 (TIMP-3) as New Markers of Acute Kidney Injury Afte...Med Sci Monit In Press; DOI: 10.12659/MSM.943500
12 Mar 2024 : Review article
Optimizing Behçet Uveitis Management: A Review of Personalized Immunosuppressive StrategiesMed Sci Monit In Press; DOI: 10.12659/MSM.943240
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








