10 November 2023: Clinical Research
Changes in Upper Airway Anatomy Following Orthodontic Treatment for Malocclusion: A Comparative Retrospective Study in 96 Patients
Betul Yuzbasioglu Ertugrul12ABCDEFG*DOI: 10.12659/MSM.941749
Med Sci Monit 2023; 29:e941749
Abstract
BACKGROUND: This retrospective study aimed to compare pharyngeal anatomical changes measured in cephalometric images before and after treatment for malocclusion Class I, II, and III in 96 patients undergoing orthodontic treatment.
MATERIAL AND METHODS: A total of 96 patients who underwent fixed orthodontic treatment were included in the study. The patients were divided into 3 groups according to the malocclusion (32 people in each group). The upper airway data in the lateral cephalometric images of the patients were retrospectively analyzed before starting fixed orthodontic treatment and the upper airway data taken after the end of the fixed orthodontic treatment.
RESULTS: According to the findings, all the upper airway data in individuals in Class I (Skeletal Class I malocclusion) group and most of the upper airway data in Class II (Skeletal Class II malocclusion) groups increased after orthodontic treatment compared to before treatment (P<0.05). Most of the upper airway data in Class III (Skeletal Class III malocclusion) group individuals decreased after orthodontic treatment compared to before treatment (P<0.05).
CONCLUSIONS: Orthodontic treatment should be chosen considering that an increase may be observed in individuals with Class I and Class II malocclusion. Similarly, in individuals with Class III malocclusion, orthodontic treatment can be chosen considering that there will be a decrease in the upper airways. By determining the effects of fixed orthodontic treatment on the airways, airway problems experienced at an early age can be prevented.
Keywords: Orthodontic Appliances, Fixed, Dentistry, Radiology, Orthodontics, airway management
Background
Orthodontic treatment leads to improved occlusion, chewing function, and a more aesthetically pleasing appearance. However, these treatments can affect various anatomical structures, including those in the upper respiratory system. Among the most affected structures are the pharynx area, hyoid bone, and tongue [1]. In some cases, individuals may experience mouth breathing due to obstructions in the nasal and pharyngeal airway, leading to sleep-disordered breathing during sleep. This can result in pathological changes in the respiratory pattern, increasing morbidity and mortality, and potentially causing adverse effects on dental tissues [2]. To better understand the effects of orthodontic treatments on the upper respiratory tract, it is essential to examine the upper respiratory structures in patients with different growth patterns. Researchers have studied the impact of impaired nasal breathing on craniofacial development and dentition for many years. It is widely believed that abnormal growth is influenced by both genetic and environmental factors [3]. Notably, mouth breathing during childhood can disrupt muscle balance and contribute to facial deformities. Conversely, tracheotomy, a surgical procedure that creates an airway through the anterior tracheal wall, has been investigated. Patients who underwent tracheotomy had a 2.78% lower S-N-Gn value compared to those with nasal breathing and a 4.75% lower value compared to those with mouth breathing [4]. The size of the soft palate and its dynamic interactions with the pharyngeal air space play a crucial role in essential bodily functions such as chewing, respiration, and phonation [5]. The velopharyngeal closure mechanism is influenced by nasal airflow, and any disorders in this process can lead to phonation difficulties. Moreover, there is a clear connection between the dimensions of the pharynx and craniofacial anomalies [6]. Research indicates that a more anterior condyle position in 8-year-old children results in a wider lower pharyngeal airway. This widened airway may be a significant factor contributing to prognathism. Therefore, it is essential to thoroughly examine the lower pharyngeal airway, tongue positioning, and the presence of enlarged tonsils in prognathic children before initiating treatment [7]. Different orthodontic approaches are required for the treatment of different malocclusions. The upper airway can be affected in different orthodontic treatments. Movable and fixed orthodontic treatment methods are used in the treatment of malocclusions [8,9]. The effects of movable orthodontic treatment on the upper respiratory tract have been presented many times in the literature [10]. The effect of fixed orthodontic treatment in different malocclusions on anatomical structures affecting the upper airways has not been studied sufficiently.
Therefore, this retrospective study aimed to compare pharyngeal anatomical changes measured in cephalometric images before and after treatment for malocclusion Class I, II, and III in 96 patients undergoing orthodontic treatment.
Material and Methods
PARTICIPANTS:
This retrospective study enrolled patients with various malocclusions who needed fixed orthodontic treatment. All participants had both pre- and post-treatment radiographic films available. The study included a total of 96 patients who underwent fixed orthodontic treatment. To be eligible for the study, participants had to meet certain criteria: they should have had a lateral cephalometric film taken at the beginning of their treatment, no presence of any pathology affecting the region examined in the lateral cephalometric image, and no congenital or acquired anomalies like cleft lip, cleft palate, or trauma. Additionally, none of the participants should have a history of prior fixed orthodontic treatment.
Study tools and methods were approved by IKCU Non-Pharmacological Clinical Research Ethics Committee with committee resolution no: IKCU.16112020.1084.
GROUPS:
Chronological ages of all individuals were calculated according to the date the lateral cephalometric film was taken. The individuals included in the study were grouped according to their malocclusion types:
Angle Class I molar classification (also known as neutroclusion) is determined by the mesiobuccal cusp of the maxillary first molar occluding with the buccal groove of the mandibular first molar. Class II molar classification (mesoclusion) is determined by the mesiobuccal cusp of the maxillary first molar, occluding mesial to the buccal groove of the mandibular first molar. Lastly, a Class III molar classification is determined by the mesiobuccal cusp of the maxillary first molar occluding distal to the buccal groove of the mandibular first molar (distoclusion) [11].
UPPER AIRWAY MEASUREMENTS:
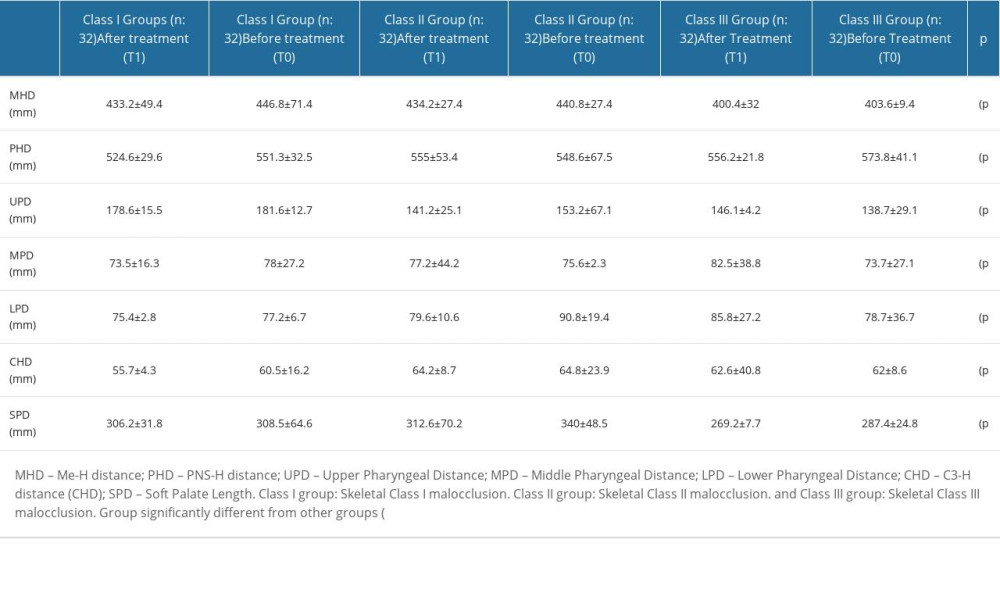
The lateral cephalometric images of patients before orthodontic treatment (T0) were compared with images taken after the completion of orthodontic treatment (T1) to analyze upper airway data across all groups. Various measurements were utilized to evaluate the upper airway, including the Me-H distance (MHD), PNS-H distance (PHD), upper pharyngeal distance (UPD) (measuring the width of the airway behind the soft palate along a line parallel to the Go-B plane), middle pharyngeal distance (MPD) (measuring the width of the airway at the uvula point along a line parallel to the Go-B plane), lower pharyngeal distance (LPD), C3-H distance (CHD), and the soft palate length (SPD) (measured as the PNS-U distance). Refer to Figure 1 for a visual representation.
ORTHODONTIC TREATMENT:
For individuals with skeletal Class I malocclusion, their ANB values fell within the range of 0° to 4°. In the case of Class II malocclusion, individuals exhibited a Class II molar-canine relationship, a convex profile, and an ANB angle greater than 4°, indicating a normodivergent growth pattern. When assembling the Class III malocclusion group, individuals were selected based on having a Class III molar-canine relationship, a concave or flat profile, an ANB angle less than 0°, and a normodivergent growth pattern. To ensure normodivergence, the SN/GoGn angle was considered, aiming to maintain it within the range of 26° to 38°. The participants in this study, consisting of individuals with Class I, Class II, and Class III malocclusion, underwent fixed orthodontic treatment using conventional brackets with a.018-inch slot. The teeth were aligned and leveled using nickel-titanium archwires with diameters of.012,.014, and.016, respectively. When necessary, maxillary and mandibular elastics were employed. The finishing phase involved the application of.016X.016 stainless steel and.016X.022 stainless steel archwires. Additionally, vertical elastics were used on the anterior and posterior teeth if deemed necessary.
LATERAL CEPHALOMETRIC FILMS:
For the analysis, lateral cephalometric films taken with the same X-ray device were used, including images captured at the beginning of orthodontic treatment and after treatment. Only images of sufficient quality, without issues such as magnification, low contrast, or blurriness, and those taken in or close to the natural head position were selected for examination. These lateral cephalometric images were calibrated and accurately measured at a 1: 1 scale to ensure precise dimensions in the study [12].
Cases were excluded from the study if they met any of the following criteria: the cephalogram exhibited significant asymmetry or improper patient positioning, as indicated by ear rod markers; the landmarks on the cephalograms could not be accurately identified due to motion artifacts, low resolution, or insufficient contrast; the cephalogram revealed craniofacial deformities or excessive soft tissues that could hinder the accurate location of anatomical points; or the bilateral anatomical structures did not exhibit satisfactory superimposition around the mid-sagittal plane [12].
STATISTICAL METHOD:
The statistical analysis was conducted using the SPSS 20.0 software package (Statistical Package for the Social Sciences, version 20.0, SPSS, Inc, Chicago IL, USA). The required sample size for the study was determined using G * Power analysis (G * Power Ver. 3.0.10, Kiel, Germany) with a significance level of 0.05 and a power of 90%. The normality of the data was assessed using the Kolmogorov-Smirnov test. Descriptive statistics are presented as X (mean) ± SD (standard deviation). Analysis of variance (ANOVA) was performed to examine the upper airway measurements among patients grouped based on malocclusion and the interactions between the groups. A significance level of
Results
UPPER AIRWAY MEASUREMENTS:
Upon analyzing the airway measurements, significant differences were observed in the MHD (T1: 433.2±49.4 and T0: 446.8±71.4), PHD (T1: 524.6±29.6 and T0: 551.3±32.5), UPD (T1: 178.6±15.5 and T0: 181.6±12.7), MPD (T1: 73.5±16.3 and T0: 78±27.2), LPD (T1: 75.4±2.8 and T0: 77.2±6.7), CHD (T1: 55.7±4.3 and T0: 60.5±16.2), and SPD (T1: 306.2±31.8 and T1: 308.5±64.6) data in the Class I group; MHD (T1: 434.2±27.4 and T0: 440.8±27.4), PHD (T1: 555±53.4 and T0: 548.6±67.5), UPD (T1: 141.2±25.1 and T0: 153.2±67.1), MPD (T1: 77.2±44.2 and T0: 75.6±2.3), LPD (T1: 79.6±10.6 and T0: 90.8±19.4), CHD (T1: 64.2±8.7 and T0: 64.8±23.9), and SPD (T1: 312.6±70.2 and T0: 340±48.5) data in the Class II group; and MHD (T1: 400.4±32 and T0: 403.6±9.4), PHD (T1: 556.2±21.8 and T0: 573.8±41.1), UPD (T1: 146.1±4.2 and T0: 138.7±29.1), MPD (T1: 82.5±38.8 and T0: 73.7±27.1), LPD (T1: 85.8±27.2 and T0: 78.7±36.7), CHD (T1: 62.6±40.8 and T0: 62±8.6), and SPD (T1: 269.2±7.7 and T0: 287.4±24.8) data in the Class III group (P<0.05) (Figures 2, 3).
UPPER AIRWAY MEASUREMENTS IN THE CLASS I GROUP:
Specifically, in the Class I group, there was a statistically significant increase in MHD, PHD, UPD, MPD, LPD, CHD, and SPD data (P<0.05) (Figures 2, 3).
UPPER AIRWAY MEASUREMENTS IN THE CLASS II GROUP:
In the Class II group, there was a statistically significant decrease in PHD and MPD data, along with a statistically significant increase in MHD, UPD, LPD, CHD, and SPD data (P<0.05) (Figures 2, 3).
UPPER AIRWAY MEASUREMENTS IN THE CLASS III GROUP:
For the Class III group, there was a statistically significant increase in MHD, PHD, and SPD data, while a statistically significant decrease in UPD, MPD, LPD, and CHD data was observed (P<0.05) (Figures 2, 3).
Comparing the 3 groups, the changes in MHD, PHD, UPD, MPD, LPD, CHD, and SPD data exhibited statistical significance (P<0.05) (Table 1). Notably, the Class I group showed greater changes in upper airway data compared to the Class II group but less compared to the Class III group. Additionally, the Class II group demonstrated smaller changes in upper airway data than the Class III group.
Discussion
Fixed orthodontic treatment enables various tooth movements, which can lead to alterations in airway dimensions. This study aimed to assess the impact of fixed orthodontic treatment on the upper airway of patients with Class I, Class II, and Class III malocclusions. The analysis revealed that, following orthodontic treatment (T1), most of the upper airway measurements exhibited an increase compared to the pre-treatment period (T0) in the Class I and Class II groups. Conversely, in the Class III group, these measurements generally decreased after orthodontic treatment. Fixed orthodontic treatments applied in different malocclusions affect the upper airways differently. According to our study results, orthodontic treatment should be chosen considering that an increase may be observed in individuals with Class I and Class II malocclusion. Similarly, in individuals with Class III malocclusion, orthodontic treatment can be chosen considering that there will be a decrease in the upper airways. When the relationship between fixed orthodontic treatment and malocclusions and upper respiratory tract anatomical structures was examined in the literature, some authors reported that fixed orthodontic treatment [13] decreased pharyngeal airway dimensions. In contrast, others [14] stated that it reduced pharyngeal airway volume, and the results of another study [15] reported that there was no difference in airways before and after orthodontic treatment in individuals with different malocclusions. Both treatments resulted in a general increase in several pharyngeal airway dimensions. However, it was challenging to differentiate the treatment-induced changes from the natural growth-related changes [16]. Stefanovic et al [17] and Valiathan et al [18] reported that fixed orthodontic treatment with or without premolar extraction did not affect pharyngeal airway dimensions in patients. However, Al-Jewair et al [19] determined that patients with skeletal Class II profile showed a decrease in pharyngeal airway volume. In the studies conducted by Akçam et al [6] on individuals with different types of mandibular rotation, soft palate length and height increased significantly in Class II individuals with posterior rotation. The ratio between the soft palate and the upper pharyngeal space did not differ significantly between patients with normal, anterior, and posterior growth patterns, and this indicates that this ratio is maintained throughout the active growth period. In the study of Crouse et al [5], the change in airway size with age was evaluated, determining that it caused an increase in nasal airway size from 9 to 13 years of age, reflecting the prepubertal hypertrophy of lymphoid and erectile tissues in the upper airway. Hong et al [20] found that pharyngeal airway volume was higher in patients with long faces. In patients with skeletal Class III malocclusion, the cross-sectional areas of the lower pharyngeal airway in the axial plane are considerably increased. The volume of the upper pharyngeal airway is increased compared to Class I patients. El and Palomo [8] found that the volume of the oropharyngeal airway in Class II patients was smaller than in Class III and Class I patients, and the position of the mandible relative to the cranial base affected the oropharyngeal airway volume. The only significant difference in nasopharynx volume was between Class 1 and Class 2 patients – it is smaller in Class 2 patients. Martin et al [9] found that the nasopharyngeal soft tissue features of Class III individuals were different in males and females – adenoidal tissue and upper airway length are higher in men, and upper airway width is greater in patients with ideal occlusion than in Class III patients. Jena et al [21] found that the sagittal mandibular development had significant effects on pharyngeal airway dimensions. Oropharynx depth was higher in Class III patients. Soft palate length is shorter among patients with mandibular prognathism than patients with normal mandible and mandibular retrognathia, but soft palate thickness was found to be higher. In the study of Valiathan et al [22], despite the expected changes in incisor angulation and position, there was no statistically significant change in oropharyngeal airway volume between the treatments with and without extraction. Skeletal Class III patients are characterized by maxillary insufficiency, maxillary retrusion, increased mandibular growth, and mandibular protrusion.
Clinically, the middle faces of these patients are retrusive, while the lower faces are protrusive and have concave profiles. The upper dental arch is usually small, with reduced or negative overjet. Chinrest treatment is related to lower jaw prognathism and is frequently used in treating Class III patients in the growth-developmental period. Tuncer et al [23] observed a significant increase in the forward position of the maxilla, maxillary, and effective mandibular length and vertical face height measurements. A significant increase was found in the nasopharyngeal area compared to the control group. Orthodontists widely use the application of a protracting force over the maxilla and the maxillary dental arch. Oktay and Ulukaya [24] found that maxillary protraction increases upper airway dimensions in patients with maxillary retrusion. Lee et al [10] observed that in patients with Class III malocclusion in the growth period, moving the maxilla forward with maxillary protraction therapy improves respiratory function by increasing the upper airway space.
Conclusions
The main cause of upper respiratory tract disorders is obstruction. Obstructive sleep apnea and upper airway resistance syndrome are common upper respiratory tract problems encountered by orthodontists. Orthodontic treatments may be decisive for treating upper respiratory tract disorders of these patients. Likewise, a disorder in the upper respiratory tract may be involved in the etiology of orthodontic problems. Therefore, the orthodontics-respiratory tract relationship should be defined. The effects of different orthodontic treatments on the airways should be determined. This study had several limitations, including the use of 2D images instead of 3D images. Additionally, the participant sample size could have been larger to enhance the study’s statistical power. Moreover, clinical examination of the patients’ upper respiratory tract data could have provided valuable insights.
Figures
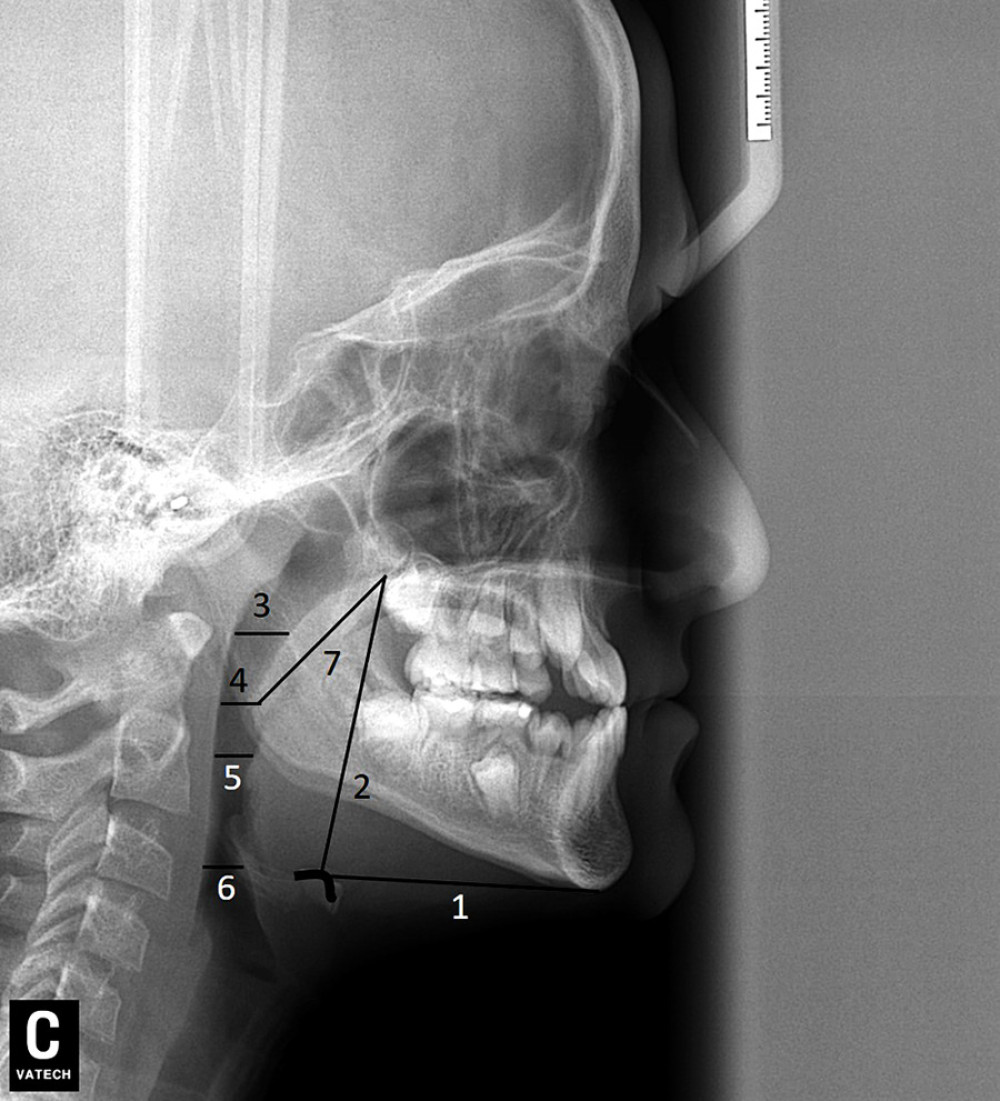 Figure 1. Airway size measured on cephalometric films*. MHD (Me-H Distance), PHD (PNS-H Distance), UPS (Upper Pharyngeal Distance), MPD (Middle Pharyngeal Distance), LPD (Lower Pharyngeal Distance), CHD (C3-H Distance), and SPD (Soft Palate Length)sizes measured on cephalometric films in patient groups (Class I, Class II, and Class III). 1. Me-H distance (MHD); 2. PNS-H distance (PHD); 3. Upper Pharyngeal Distance (UPD); 4. Middle Pharyngeal Distance (MPD); 5. Lower Pharyngeal Distance (LPD); 6. C3-H distance (CHD); 7. Soft Palate Length (SPD). * (Patient 1 cephalometric film).
Figure 1. Airway size measured on cephalometric films*. MHD (Me-H Distance), PHD (PNS-H Distance), UPS (Upper Pharyngeal Distance), MPD (Middle Pharyngeal Distance), LPD (Lower Pharyngeal Distance), CHD (C3-H Distance), and SPD (Soft Palate Length)sizes measured on cephalometric films in patient groups (Class I, Class II, and Class III). 1. Me-H distance (MHD); 2. PNS-H distance (PHD); 3. Upper Pharyngeal Distance (UPD); 4. Middle Pharyngeal Distance (MPD); 5. Lower Pharyngeal Distance (LPD); 6. C3-H distance (CHD); 7. Soft Palate Length (SPD). * (Patient 1 cephalometric film). 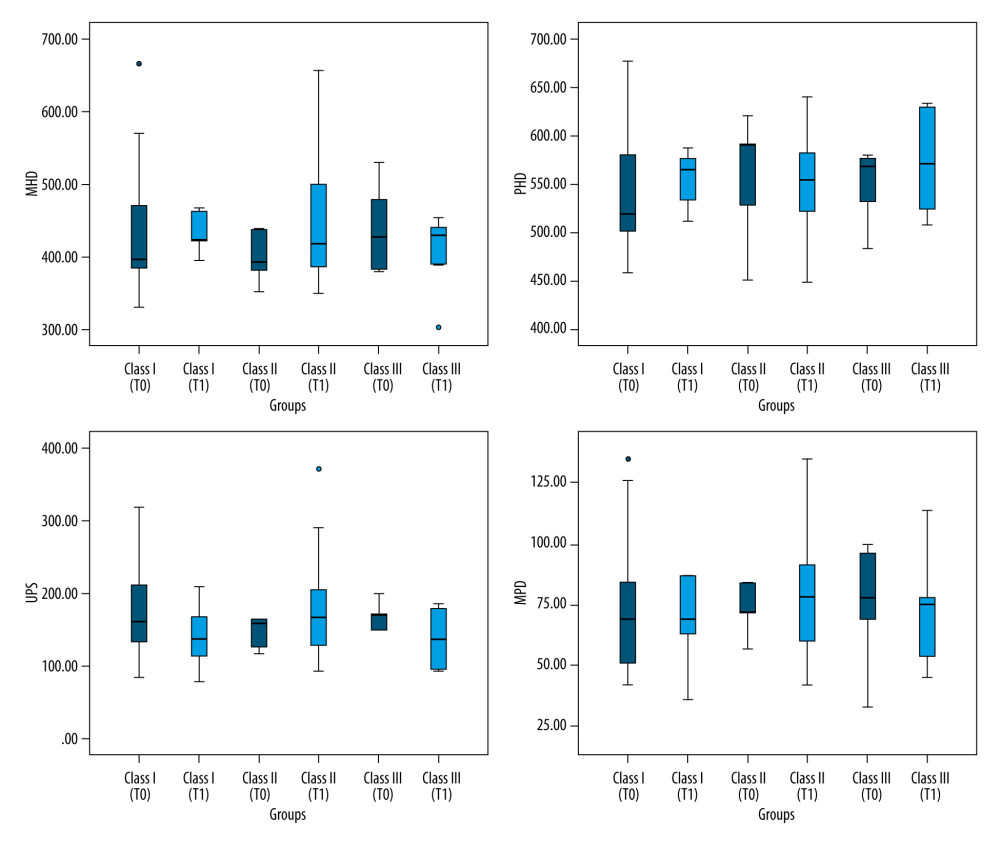 Figure 2. Airway size measured on cephalometric films. MHD (Me-H Distance), PHD (PNS-H Distance), UPS (Upper Pharyngeal Distance), and MPD (Middle Pharyngeal Distance) sizes measured on cephalometric films in patient groups (Class I, Class II, and Class III).
Figure 2. Airway size measured on cephalometric films. MHD (Me-H Distance), PHD (PNS-H Distance), UPS (Upper Pharyngeal Distance), and MPD (Middle Pharyngeal Distance) sizes measured on cephalometric films in patient groups (Class I, Class II, and Class III). 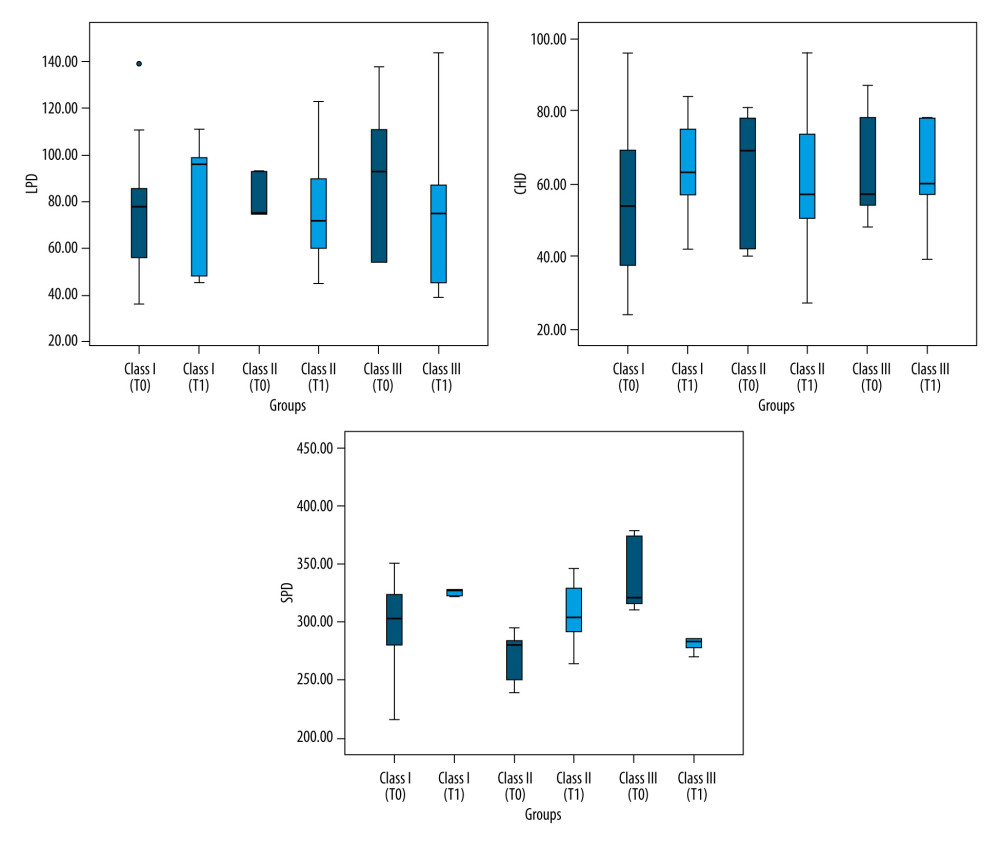 Figure 3. Airway size measured on cephalometric films. LPD (Lower Pharyngeal Distance), CHD (C3-H Distance), and SPD (Soft Palate Length) sizes measured on cephalometric films in patient groups (Class I, Class II, and Class III).
Figure 3. Airway size measured on cephalometric films. LPD (Lower Pharyngeal Distance), CHD (C3-H Distance), and SPD (Soft Palate Length) sizes measured on cephalometric films in patient groups (Class I, Class II, and Class III). Rererences
1. Kyung HS, Park YC, Pae EK, Obstructive sleep apnea patients with the oral appliance experience pharyngeal size and shape changes in three dimensions: Angle Orthod, 2004; 75(1); 15-22
2. Ingman T, Nieminen T, Hurmerinta K, Cephalometric comparison of pharyngeal changes in subjects with upper airway resistance syndrome or obstructive sleep apnoea in upright and supine positions: Eur J Orthod, 2004; 26(3); 321-26
3. Sheng CM, Lin LH, Su Y, Tsai HH, Developmental changes in pharyngeal airway depth and hyoid bone position from childhood to young adulthood: Angle Orthod, 2009; 79(3); 484-90
4. Bakor SF, Enlow DH, Pontes P, Craniofacial growth variations in nasal-breathing, oral-breathing, and tracheotomized children: Am J Orthod Dentofacial Orthop, 2011; 140(4); 486-92
5. Crouse U, Laine-Alava MT, Warren DW, A longitudinal study of nasal airway size from age 9 to age 13: Angle Orthod, 1999; 69(5); 413-18
6. Akçam MO, Toygar TU, Wada T, Longitudinal ınvestigation of soft palate and nasopharyngeal airway relations in different rotation types: Angle Orthod, 2002; 72(6); 521-26
7. Takemoto Y, Saitoh I, Iwasaki T, Pharyngeal airway in children with prognathism and normal occlusion: Angle Orthod, 2011; 81(1); 75-80
8. El H, Palomo JM, Airway volume for different dentofacial skeletal patterns: Am J Orthod Dentofacial Orthop, 2011; 139(6); 511-21
9. Martin O, Muelas L, Vinas MJ, Comparative study of nasopharyngeal soft-tissue characteristics in patients with Class III malocclusion: Am J Orthod Dentofacial Orthop, 2011; 139(2); 242-51
10. Lee JW, Park KH, Kim SH, Correlation between skeletal changes by maxillary protraction and upper airway dimensions: Angle Orthod, 2011; 81(3); 426-32
11. Hershfeld JJ, Edward H, Angle and the malocclusion of the teeth: Bull Hist Dent, 1979; 27(2); 79-84
12. Albarakati SF, Kula KS, Ghoneima AA, The reliability and reproducibility of cephalometric measurements: A comparison of conventional and digital methods: Dentomaxillofac Radiol, 2012; 41(1); 11-17
13. Sun FC, Yang WZ, Ma YKEffect of incisor retraction on three-dimensional morphology of upper airway and fluid dynamicsin adult class patients with bimaxillary protrusion: Zhonghua Kou Qiang Yi Xue Za Zhi, 2018; 53(6); 398-403 [in Chinese]
14. Oliveira PM, Cheib-Vilefort PL, de Parsia Gontijo H, Three-dimensional changes of the upper airway in patients with Class II malocclusion treated with the Herbst appliance: A cone-beamcomputed tomography study: Am J Orthod Dentofac Orthop, 2020; 157(2); 205-11
15. AlKawari HM, AlBalbeesi HO, Alhendi AA, Pharyngeal airway dimensionalchanges after premolar extraction in skeletal class II and class III orthodontic patients: J Orthod Sci, 2018; 7; 10
16. Thereza-Bussolaro C, Oh HS, Lagravère M, Flores-Mir C: Int Orthod, 2019; 17(4); 667-77
17. Stefanovic N, El H, Chenin DL, Glisic B, Three-dimensional pharyngeal airway changes in orthodontic patients treated with and without extractions: Orthod Craniofac Res, 2013; 16(2); 87-96
18. Valiathan M, El H, Hans MG, Palomo MJ, Effects of extraction versus non-extraction treatment on oropharyngeal airwayvolume: Angle Orthod, 2010; 80(6); 1068-74
19. Obelenis Ryan DP, Bianchi J, Ignácio J, Cone-beam computed tomography airway measure-ments: Can we trust them?: Am J Orthod Dentofac Orthop, 2019; 156(1); 53-60
20. Hong J, Oh K, Kim B, Three-dimensional analysis of pharyngeal airway volume in adults with anterior position of the mandible: Am J Orthod Dentofacial Orthop, 2011; 140(4); 161-69
21. Jena AK, Singh SP, Utreja AK, Sagittal mandibular development effects on the dimensions of the awake pharyngeal airway passage: Angle Orthod, 2010; 80(6); 1061-67
22. Valiathan M, El H, Hans MG, Effects of extraction versus non-extraction treatment on oropharyngeal airway volume: Angle Orthod, 2010; 80(6); 1068-74
23. Tuncer BB, Kaygisiz E, Tuncer C, Pharyngeal airway dimensions after chin cup treatment in Class III malocclusion subjects: J Oral Rehabil, 2009; 36(2); 110-17
24. Oktay H, Ulukaya E, Maxillary protraction appliance effect on the size of the upper airway passage: Angle Orthod, 2008; 78(2); 209-14
Figures
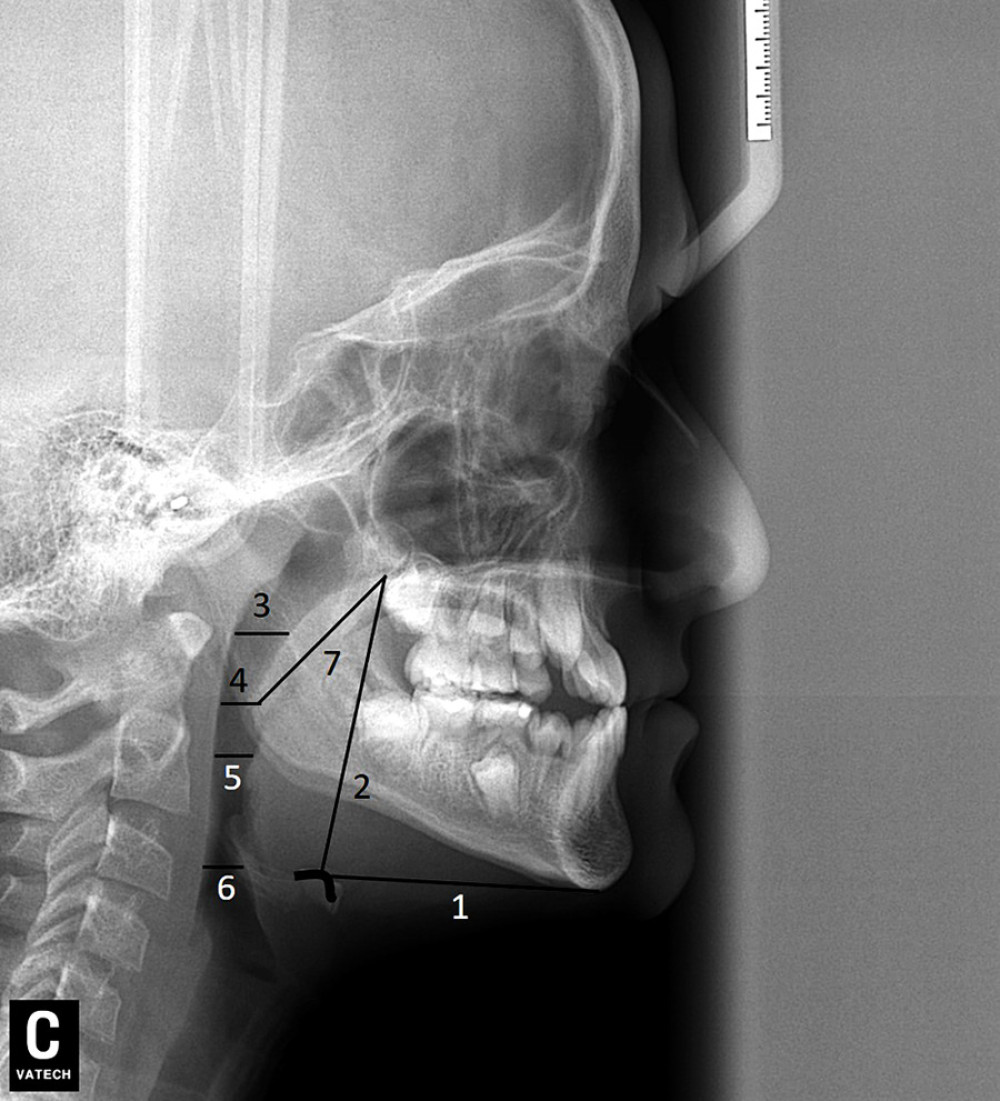 Figure 1. Airway size measured on cephalometric films*. MHD (Me-H Distance), PHD (PNS-H Distance), UPS (Upper Pharyngeal Distance), MPD (Middle Pharyngeal Distance), LPD (Lower Pharyngeal Distance), CHD (C3-H Distance), and SPD (Soft Palate Length)sizes measured on cephalometric films in patient groups (Class I, Class II, and Class III). 1. Me-H distance (MHD); 2. PNS-H distance (PHD); 3. Upper Pharyngeal Distance (UPD); 4. Middle Pharyngeal Distance (MPD); 5. Lower Pharyngeal Distance (LPD); 6. C3-H distance (CHD); 7. Soft Palate Length (SPD). * (Patient 1 cephalometric film).
Figure 1. Airway size measured on cephalometric films*. MHD (Me-H Distance), PHD (PNS-H Distance), UPS (Upper Pharyngeal Distance), MPD (Middle Pharyngeal Distance), LPD (Lower Pharyngeal Distance), CHD (C3-H Distance), and SPD (Soft Palate Length)sizes measured on cephalometric films in patient groups (Class I, Class II, and Class III). 1. Me-H distance (MHD); 2. PNS-H distance (PHD); 3. Upper Pharyngeal Distance (UPD); 4. Middle Pharyngeal Distance (MPD); 5. Lower Pharyngeal Distance (LPD); 6. C3-H distance (CHD); 7. Soft Palate Length (SPD). * (Patient 1 cephalometric film).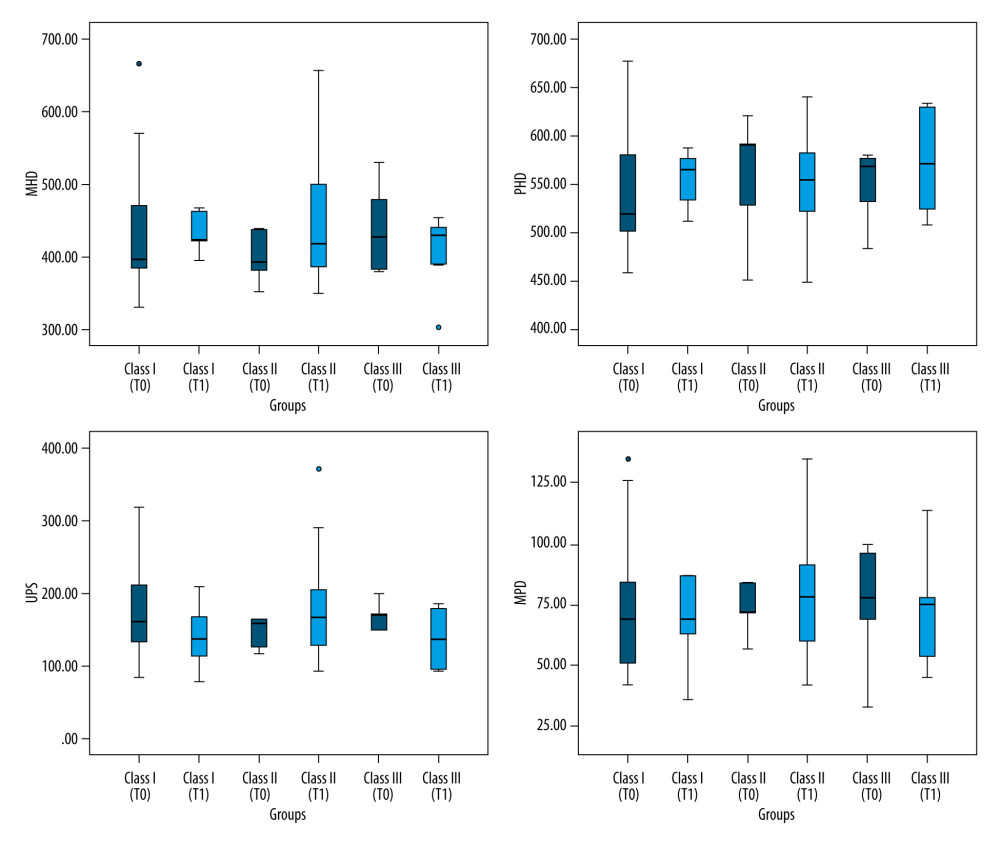 Figure 2. Airway size measured on cephalometric films. MHD (Me-H Distance), PHD (PNS-H Distance), UPS (Upper Pharyngeal Distance), and MPD (Middle Pharyngeal Distance) sizes measured on cephalometric films in patient groups (Class I, Class II, and Class III).
Figure 2. Airway size measured on cephalometric films. MHD (Me-H Distance), PHD (PNS-H Distance), UPS (Upper Pharyngeal Distance), and MPD (Middle Pharyngeal Distance) sizes measured on cephalometric films in patient groups (Class I, Class II, and Class III).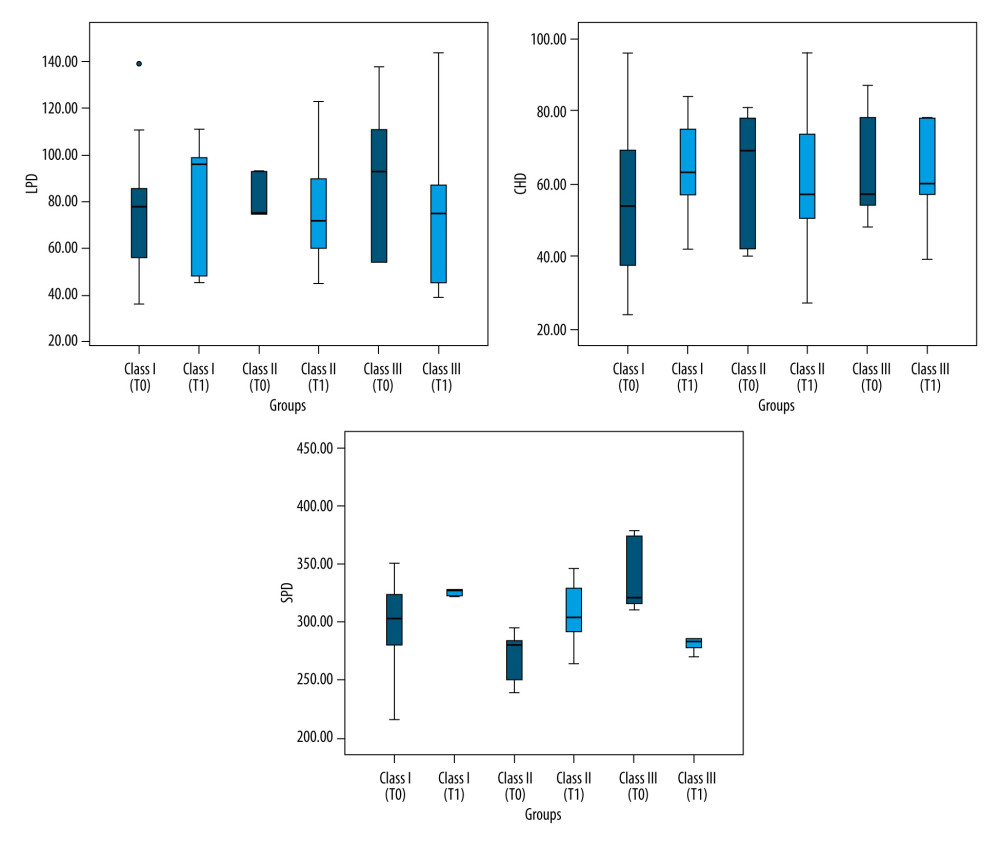 Figure 3. Airway size measured on cephalometric films. LPD (Lower Pharyngeal Distance), CHD (C3-H Distance), and SPD (Soft Palate Length) sizes measured on cephalometric films in patient groups (Class I, Class II, and Class III).
Figure 3. Airway size measured on cephalometric films. LPD (Lower Pharyngeal Distance), CHD (C3-H Distance), and SPD (Soft Palate Length) sizes measured on cephalometric films in patient groups (Class I, Class II, and Class III). In Press
12 Mar 2024 : Clinical Research
Tissue Inhibitors of Metalloproteinase 1 (TIMP-1) and 3 (TIMP-3) as New Markers of Acute Kidney Injury Afte...Med Sci Monit In Press; DOI: 10.12659/MSM.943500
12 Mar 2024 : Review article
Optimizing Behçet Uveitis Management: A Review of Personalized Immunosuppressive StrategiesMed Sci Monit In Press; DOI: 10.12659/MSM.943240
12 Mar 2024 : Clinical Research
Metabolomic Alterations in Methotrexate Treatment of Moderate-to-Severe PsoriasisMed Sci Monit In Press; DOI: 10.12659/MSM.943360
14 Mar 2024 : Clinical Research
Renal Dysfunction Increases Risk of Adverse Cardiovascular Events in 5-Year Follow-Up Study of Intermediate...Med Sci Monit In Press; DOI: 10.12659/MSM.943956
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952