02 February 2024: Clinical Research
Comparative Analysis of Intramedullary Nail versus Plate Fixation for Fibula Fracture in Supination External Rotation Type IV Ankle Injury
Hongfeng Chen1BE, Zhen Li1CF, Xiaoqi Li1DF, Jiongjiong Lu1BC, Beibei Chen1BC, Qiongchao Wang1DF, Pengke Cao2AG*DOI: 10.12659/MSM.941909
Med Sci Monit 2024; 30:e941909
Abstract
BACKGROUND: Lateral malleolus fractures, typically from trauma, sports, or accidents, are common, with supination external rotation (SER) injuries being most prevalent. SER injuries involve complex joint mechanics and often necessitate surgical intervention for instability. This study compares intramedullary nail and plate fixation for fibula fractures in SER type IV ankle injuries, considering their biomechanical properties and influence on fracture healing.
MATERIAL AND METHODS: A prospective, randomized study was conducted between January 2021 and December 2021. A total of 81 patients with SER injuries were included in the study. Surgical procedures were performed using either intramedullary nails or plates. The following parameters were recorded and analyzed: postoperative complications, operation times, bone healing times, American Orthopaedic Foot & Ankle Society (AOFAS) scores, visual analog scale (VAS) scores for pain, and ankle range of motion.
RESULTS: Out of the 81 cases, 42 were treated with intramedullary nails, while 39 received plate fixation. Statistical analysis revealed a significantly lower rate of postoperative complications in the intramedullary nail group than in the the plate fixation group (9.52% vs 30.77%, P<0.0164). However, there were no significant differences between the 2 groups in terms of operation time, bone healing time, AOFAS scores, VAS scores, and functional evaluations (P>0.05).
CONCLUSIONS: Plate fixation and intramedullary nail fixation are effective techniques for treating fibula fractures in SER type IV injuries. However, intramedullary nail fixation demonstrates a lower rate of complications. Therefore, intramedullary nails may be preferable to plate fixation for the management of fibula fractures in SER type IV ankle injuries.
Keywords: Fracture Fixation, Intramedullary, Fracture Fixation, Internal, ankle fractures, ankle fractures
Background
Lateral malleolus fractures represent a frequently encountered lower leg injury resulting from various etiologies, such as traumatic events, sports-related incidents, or accidental occurrences. Among ankle fractures, the supination external rotation (SER) injury pattern is highly prevalent, accounting for approximately 85% of all cases [1]. The SER injury occurs when a supinated foot experiences axial loading. The subtalar joint, characterized by its complex axis of movement [2], functions as an angulated hinge, leading to external rotation of the talus in response to calcaneus inversion [3]. This injury pattern is analogous to Weber B fractures. SER type IV ankle fractures are considered particularly unstable and necessitate surgical intervention, which typically involves addressing both lateral malleolus fractures and concurrent medial malleolus fractures or deltoid ligament injuries. The influence of minor clinical characteristics, such as chronic diseases and skeletal disorders, like osteoporosis, on fracture healing is a crucial aspect of orthopedic research. These factors can significantly affect the treatment outcomes and recovery process, warranting thorough consideration in the assessment of fracture management strategies. Understanding their effects on fracture healing is essential for optimizing patient care and treatment decisions in orthopedic practice.
The primary objectives in managing ankle joint fractures are to restore proper alignment of the lateral malleolus and preserve the integrity of the weight-bearing joint surface, thereby ensuring stability and mobility of the ankle joint [4]. In the context of treating fibula fractures associated with SER type IV injuries, 2 commonly used techniques are intramedullary nail fixation and plate fixation. Each method has distinct advantages and considerations. Traditionally, lateral or posterolateral plate fixation was widely favored for the management of spiral fibular fractures associated with SER type IV injuries. However, owing to their inherent biomechanical advantages, such as excellent stability, facilitation of anatomical reduction, and less soft tissue disruption, intramedullary nails have gained increasing popularity among certain surgeons.
In the present study, we aimed to compare the 2 fixation approaches to help enable patients and healthcare professionals to make well-informed decisions regarding the most suitable method for addressing fibula fractures in the context of SER type IV injuries.
Material and Methods
A prospective and randomized study was conducted to assess the efficacy of locking intramedullary nail fixation vs locking plate fixation for fibula fractures in SER injuries. In this study, patients were randomly assigned to either the intramedullary nail fixation group or the locking plate fixation group using a randomization sequence executed by an independent statistician uninvolved in subsequent study phases. Patients and surgeons were blinded to group assignments, receiving identical-looking interventions to prevent bias. Data collectors responsible for outcome assessments were also blinded, ensuring unbiased data collection and analysis. Blinding procedures were consistently maintained, and any unblinding events were promptly documented and addressed, upholding the study’s scientific integrity. Randomization was achieved using a random table of numbers to allocate patients to either the nail or plate group. A total of 81 patients with SER injuries were included in the study, all of whom were treated at our department between January 2021 and December 2021.
Inclusion criteria for participation in the study included closed fractures, SER IV injuries with medial malleolus fractures, Haraguchi type III posterior maleolus fractures, and an age range from 18 years to 65 years. Exclusion criteria were bilateral injuries, open fractures, associated injuries in other anatomical sites, osteoporosis, pathological fractures, and basic chronic diseases and some skeletal disorders.
Under general anesthesia, all patients underwent reduction and fixation of lateral and posterior malleolus fractures while positioned in the lateral recumbent position. Subsequently, patients were placed in the supine position for open reduction and internal fixation of medial malleolus fractures. Following surgery, a progressive weight-bearing protocol was initiated, and rehabilitation commenced 6 weeks after surgery. No postoperative plaster casts were applied.
To evaluate the outcomes of the 2 groups (nail group and plate group), various parameters were recorded, including complications, operation times, bone healing times, American Orthopaedic Foot & Ankle Society (AOFAS) scores, visual analog scale (VAS) scores for pain assessment, ankle range of motion, and radiographic parameters of medial clear space, tibiomedial malleolar angle, fibular length, talocrural angle, and tibiofibular clear space. Statistical analysis was performed using SPSS software (version 15.0.1, SPSS Inc., Chicago, IL, USA). The Wilcoxon rank-sum test was used for non-parametric data analysis, while the chi-square test was used for comparing rates. A significance level of
Results
In this study involving 81 patients with SER injuries, in which each patient represented a single injury case, the treatment outcomes between the 2 groups were rigorously assessed. Among these patients, 42 underwent intramedullary nail treatment (nail group, Figure 1), while 39 received plate fixation (plate group, Figure 2) (Table 1). All patients received at least 1 year of follow-up. The fracture healing time in the nail group was an average of 9.34±1.97 weeks, and 9.12±1.55 weeks in the plate group; no significant difference was found (
Discussion
The selection of internal fixation methods for fibula fractures remains a topic of debate within the medical community. Two commonly employed techniques are intramedullary nail fixation and plate fixation. While some comparative studies have been conducted to compare these methods [5–8], there is a relative lack of studies specifically focusing on fibula fractures in the context of SER type IV injuries.
The plate fixation technique offers excellent stability and enables precise control over alignment during surgery [9,10]. It is particularly favored for complex or comminuted fractures involving multiple bone fragments [5,11]. Plate fixation allows for superior control over the alignment of bone fragments, facilitating precise anatomical reduction and stable fixation. This feature is especially beneficial for complex fractures that necessitate structural alignment [12]. Furthermore, the presence of a metal plate provides immediate stability to the fractured bone, enabling early weight-bearing and promoting accelerated healing. It facilitates early mobilization and reduces the risk of malalignment [12]. Moreover, plate fixation permits customized contouring of the plate to match the specific shape of the fibula, ensuring an optimal fit and enhanced stability [13].
However, plate fixation also has certain considerations. Of note, the procedure of plate fixation involves a larger incision, which can result in greater soft tissue disruption. This can lead to increased postoperative pain, swelling, and a longer recovery period [14]. More importantly, the presence of metal plates and screws can occasionally cause irritation or discomfort. In some cases, the hardware may need to be removed following bone healing [15].
Therefore, as another common technique for fibula fractures, intramedullary nail fixation is widely used in SER injury. Compared with plate fixation, intramedullary nail fixation is a minimally invasive procedure. It requires a smaller incision, resulting in reduced soft tissue damage, decreased pain, and faster recovery [16]. Notably, the intramedullary nail bears a significant portion of the body’s weight, providing load-sharing capabilities. This promotes stability, enhances healing, and allows for early weight-bearing [8]. In addition, since the nail is inserted within the medullary canal, it causes less disruption to the surrounding soft tissues, including blood vessels and muscles [17].
Similar to plate fixation, there are also considerations for intramedullary nail fixation. Compared with plate fixation, intramedullary nail fixation offers less control over precise alignment. It may not be suitable for fractures requiring intricate anatomical reduction [18]. Furthermore, improper insertion or inadequate rotational control during intramedullary nail fixation can result in malrotation of bone fragments, potentially leading to functional issues or cosmetic deformities [19]. In the present study, we found that the incidence of postoperative complications was lower in the intramedullary nail group than in the plate fixation group. However, there were no significant differences between the 2 groups regarding operation time, bone healing time, AOFAS score, VAS score, and functional evaluations. Based on these results, it is preferable to use the intramedullary nail technique for managing fibula fractures in the context of SER type IV injuries.
Nevertheless, this study had limitations. First, the number of included cases was limited, and, second, it was not a long-term study. Further, the success of the intramedullary nail technique was highly dependent on the skill and experience of the surgeon, as there is a learning curve associated with this procedure. An experienced surgeon can have shorter operation times and use additional surgical techniques, which could potentially impact the complication rate and functional outcomes.
Conclusions
Plate and intramedullary nail fixation are effective for fibula fractures, and the choice of technique depends on factors such as fracture type and patient characteristics. Plates excel in precise alignment control, making them suitable for complex fractures. In contrast, intramedullary nails offer advantages including fewer complications, minimally invasive surgery, load sharing, and soft tissue preservation, as supported by our study findings that indicated lower complication rates with this method. In cases of SER type IV injuries, intramedullary nails may be a preferred option, but the decision should be individualized. Preoperative evaluation plays a crucial role in guiding the choice to optimize healing and patient recovery.
Figures
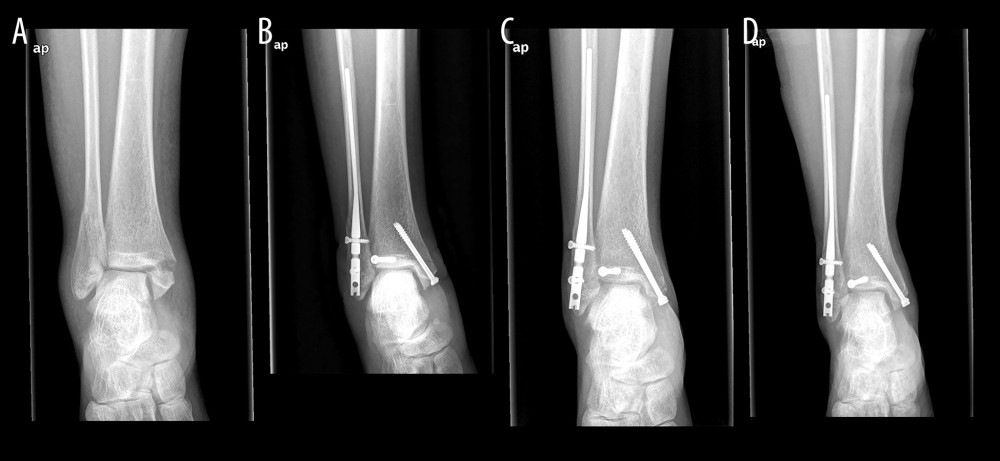 Figure 1. Typical case from the nail fixation group(A) Supination external rotation type IV injury. X-ray image showed displaced fractures of medial and lateral malleoli. (B) Immediately postoperative image showed intramedullary nail was used. (C) The nail position was good at 3 months after surgery. (D) The fracture completely healed at 1 year after surgery.
Figure 1. Typical case from the nail fixation group(A) Supination external rotation type IV injury. X-ray image showed displaced fractures of medial and lateral malleoli. (B) Immediately postoperative image showed intramedullary nail was used. (C) The nail position was good at 3 months after surgery. (D) The fracture completely healed at 1 year after surgery.  Figure 2. Typical case from the plate group(A) Supination external rotation type IV injury: X-ray image showed displaced fractures of medial and lateral malleoli. (B) Immediately postoperative image showed plate was used. (C) The fixation position was good at 3 months after surgery. (D) The fracture completely healed at 1 year after surgery.
Figure 2. Typical case from the plate group(A) Supination external rotation type IV injury: X-ray image showed displaced fractures of medial and lateral malleoli. (B) Immediately postoperative image showed plate was used. (C) The fixation position was good at 3 months after surgery. (D) The fracture completely healed at 1 year after surgery. References
1. Kosuge DD, Mahadevan D, Chandrasenan J, Pugh H, Managing type II and type IV Lauge-Hansen supination external rotation ankle fractures: current orthopaedic practice: Ann R Coll Surg Engl, 2010; 92(8); 689-92
2. Lundberg A, Goldie I, Kalin B, Selvik G, Kinematics of the ankle/foot complex: Plantarflexion and dorsiflexion: Foot Ankle, 1989; 9(4); 194-200
3. Gougoulias N, Khanna A, Sakellariou A, Maffulli N, Supination-external rotation ankle fractures: Stability a key issue: Clin Orthop Relat Res, 2010; 468(1); 243-51
4. Zhao HZ, Fan TS, Wang SL, Closed reduction for the treatment of grade IV supination-external rotation fracture of the ankle joint: A retrospective analysis: Orthop Surg, 2021; 13(7); 2163-69
5. Asloum Y, Bedin B, Roger T, Internal fixation of the fibula in ankle fractures: A prospective, randomized and comparative study: Plating versus nailing: Orthop Traumatol Surg Res, 2014; 100(4 Suppl); S255-59
6. Bäcker HC, Vosseller JT, Fibula fracture: Plate versus nail fixation: Clin Orthop Surg, 2020; 12(4); 529-34
7. Kohler FC, Schenk P, Nies T, Fibula nail versus locking plate fixation – a biomechanical study: J Clin Med, 2023; 12(2); 698
8. Switaj PJ, Fuchs D, Alshouli M, A biomechanical comparison study of a modern fibular nail and distal fibular locking plate in AO/OTA 44C2 ankle fractures: J Orthop Surg Res, 2016; 11(1); 100
9. Zawam SH, Mabrouk MG, El-Desouky MA, Lateral malleolar fractures Weber Type A and B: Does percutaneous intramedullary screw confer a solid alternative to the traditional neutralization plate?: Int Orthop, 2022; 46(9); 2127-34
10. Hasami NA, Smeeing DPJ, Pull Ter Gunne AF, Operative fixation of lateral malleolus fractures with locking plates vs nonlocking plates: A systematic review and meta-analysis: Foot Ankle Int, 2022; 43(2); 280-90
11. Bilgetekin YG, Çatma MF, Öztürk A, Comparison of different locking plate fixation methods in lateral malleolus fractures: Foot Ankle Surg, 2019; 25(3); 366-70
12. Canton G, Sborgia A, Maritan G, Fibula fractures management: World J Orthop, 2021; 12(5); 254-69
13. Zahn RK, Frey S, Jakubietz RG, A contoured locking plate for distal fibular fractures in osteoporotic bone: A biomechanical cadaver study: Injury, 2012; 43(6); 718-25
14. Hess F, Sommer C, Minimally invasive plate osteosynthesis of the distal fibula with the locking compression plate: First experience of 20 cases: J Orthop Trauma, 2011; 25(2); 110-15
15. Bäcker HC, Greisberg JK, Vosseller JT, Fibular plate fixation and correlated short-term complications: Foot Ankle Spec, 2020; 13(5); 378-82
16. Giordano V, Giannoudis PV, Boni G, Intramedullary nailing of lateral malleolus in ankle fractures – surgical technique and literature review: Rev Col Bras Cir, 2020; 47; e20202508
17. Boni G, Sanchez GT, Arliani G, Safety and efficacy of surgical fixation of fibula fractures using an intramedullary nail: A retrospective observational cohort study in 30 patients: Patient Saf Surg, 2019; 13; 31
18. Wang Q, Xu HG, Zhang YC, Dong LJ, Elastic nails for fibular fracture in adult tibiofibular fractures: Int J Clin Exp Med, 2015; 8(6); 10086-90
19. Sullivan M, Bonilla K, Donegan D, Malrotation of long bones: Orthop Clin North Am, 2021; 52(3); 215-29
Figures
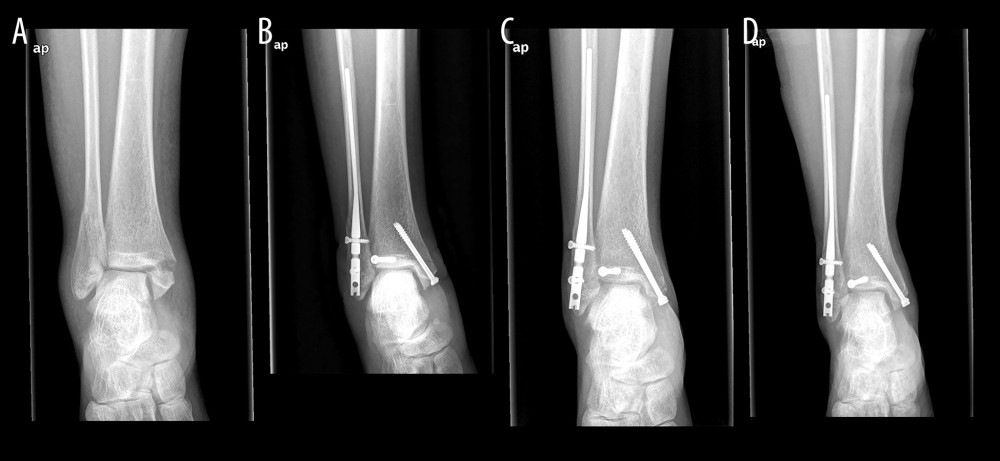 Figure 1. Typical case from the nail fixation group(A) Supination external rotation type IV injury. X-ray image showed displaced fractures of medial and lateral malleoli. (B) Immediately postoperative image showed intramedullary nail was used. (C) The nail position was good at 3 months after surgery. (D) The fracture completely healed at 1 year after surgery.
Figure 1. Typical case from the nail fixation group(A) Supination external rotation type IV injury. X-ray image showed displaced fractures of medial and lateral malleoli. (B) Immediately postoperative image showed intramedullary nail was used. (C) The nail position was good at 3 months after surgery. (D) The fracture completely healed at 1 year after surgery. Figure 2. Typical case from the plate group(A) Supination external rotation type IV injury: X-ray image showed displaced fractures of medial and lateral malleoli. (B) Immediately postoperative image showed plate was used. (C) The fixation position was good at 3 months after surgery. (D) The fracture completely healed at 1 year after surgery.
Figure 2. Typical case from the plate group(A) Supination external rotation type IV injury: X-ray image showed displaced fractures of medial and lateral malleoli. (B) Immediately postoperative image showed plate was used. (C) The fixation position was good at 3 months after surgery. (D) The fracture completely healed at 1 year after surgery. Tables
 Table 1. Characteristics of the patients from the 2 groups.
Table 1. Characteristics of the patients from the 2 groups. Table 2. Complications of the 2 groups.
Table 2. Complications of the 2 groups. Table 3. Radiographic results of the 2 groups.
Table 3. Radiographic results of the 2 groups.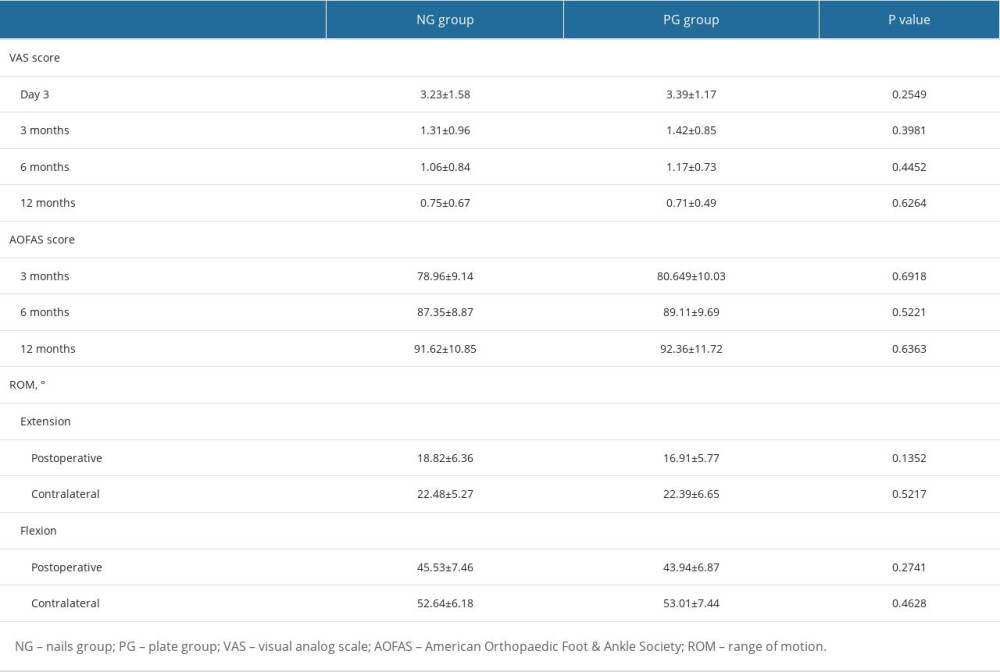 Table 4. Functional results of the 2 groups.
Table 4. Functional results of the 2 groups. Table 1. Characteristics of the patients from the 2 groups.
Table 1. Characteristics of the patients from the 2 groups. Table 2. Complications of the 2 groups.
Table 2. Complications of the 2 groups. Table 3. Radiographic results of the 2 groups.
Table 3. Radiographic results of the 2 groups.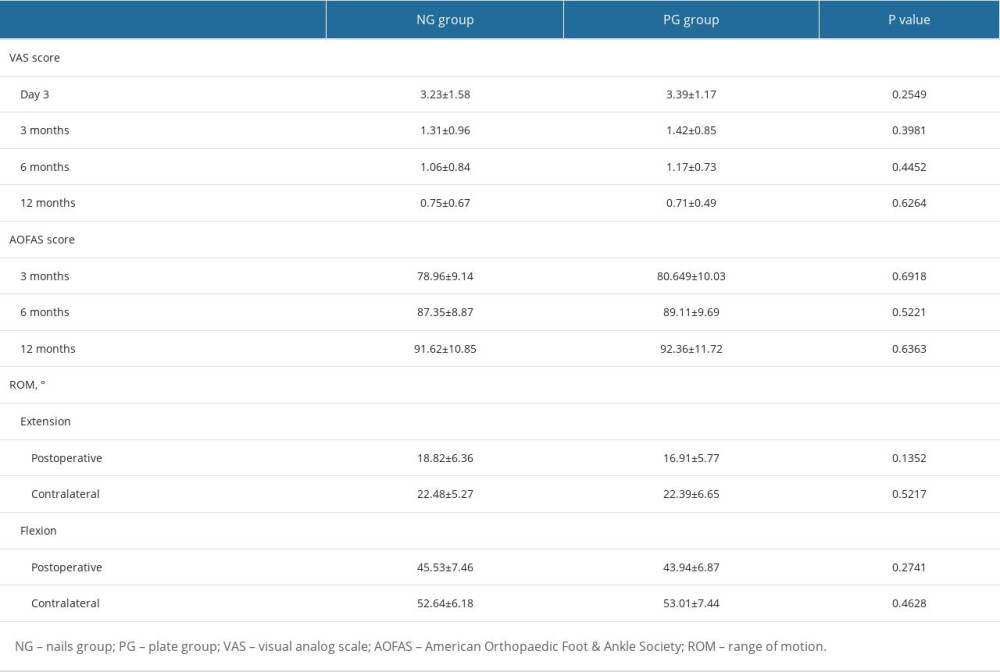 Table 4. Functional results of the 2 groups.
Table 4. Functional results of the 2 groups. In Press
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
12 Mar 2024 : Clinical Research
Tissue Inhibitors of Metalloproteinase 1 (TIMP-1) and 3 (TIMP-3) as New Markers of Acute Kidney Injury Afte...Med Sci Monit In Press; DOI: 10.12659/MSM.943500
12 Mar 2024 : Review article
Optimizing Behçet Uveitis Management: A Review of Personalized Immunosuppressive StrategiesMed Sci Monit In Press; DOI: 10.12659/MSM.943240
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








