30 December 2023: Clinical Research
Factors Influencing Recurrence Rates and Surgical Outcomes in Lumbar Microdiscectomy: A Retrospective Study of 130 Patients in Turkey
Serdal AlbayrakDOI: 10.12659/MSM.942012
Med Sci Monit 2023; 29:e942012
Abstract
BACKGROUND: Lumbar disc herniation surgery, specifically lumbar microdiscectomy, shows recurrence in 3-24% of patients, necessitating potential re-operations. This study focuses on the outcomes and recurrence causes in 130 cases of lumbar disc herniations. These cases were managed by a single surgeon at a single center, offering a unique perspective on a common issue in neurosurgery.
MATERIAL AND METHODS: The study involved 130 patients treated for lumbar disc herniations. Analysis considered various factors: age, sex, symptoms, surgical level, complications, pre- and postoperative pain levels, and quality of life indices.
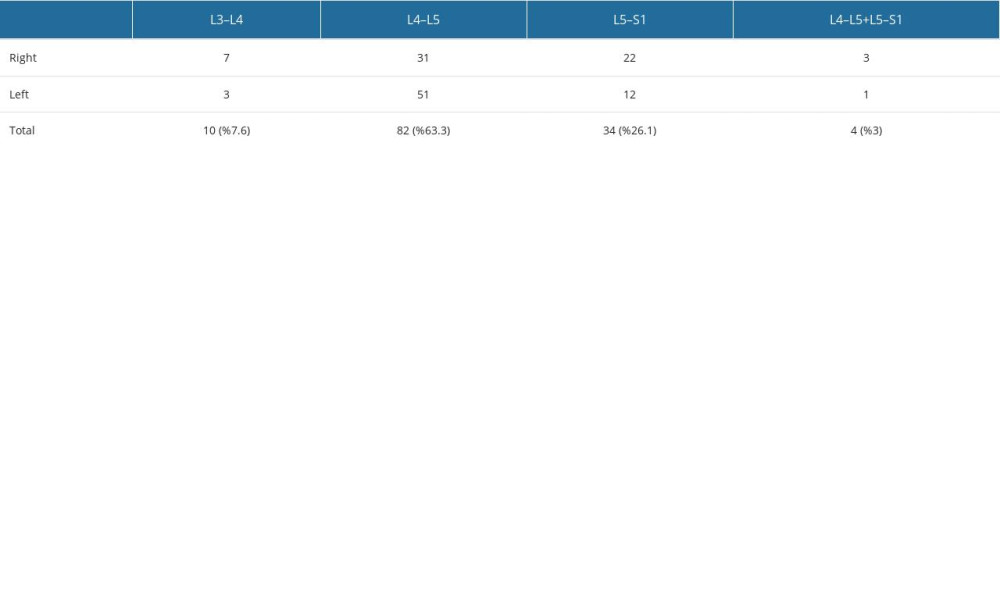
RESULTS: Of the 130 cases analyzed, all underwent initial surgery by the same surgeon or sought treatment from this surgeon after recurrence. Inclusion criteria were based on radiologic and clinical indications for re-operation. The demographic split was 76 males (56.4%) and 54 females (43.6%). A notable finding was a higher recurrence rate in males and patients under 45 years, although the sex difference was not statistically significant. The average age was 47.5 years. Significant changes were noted in the Oswestry Disability Index (ODI) levels during follow-ups (P<0.001).
CONCLUSIONS: This study underscores the effectiveness of lumbar microsurgery in treating recurrent lumbar disc herniations. Techniques such as medial facet utilization and laminectomy border expansion show promise. However, determining instability rates requires long-term patient follow-up. Our findings contribute valuable insights into surgical approaches and patient outcomes in recurrent lumbar disc herniation cases.
Keywords: Spinal Cord, Lumbar Vertebrae, acute pain, Low Back Pain
Background
Lower back pain is a common problem of our society and causes workforce losses. Its lifetime prevalence reaches 80% and annual hospital admission rates are 15% in the adult population [1]. Studies have shown that the source of lower back pain is related to intervertebral disc pathologies in up to 39% of cases [2]. Most lumbar disc herniations can be treated with medications and conservative methods. However, in cases with severe pain that develops neurological deficit due to root and/or canal compression, surgical treatment is an option. There are 3 options for surgery. Open discectomy is now rarely used by very few surgeons with the introduction of the microscope, which is nowdays called microsurgery and endoscopic discectomy. There is a recurrence rate of 3–24% after the operation and re-operation may be required [3]. Microsurgery is a surgical option with a proven efficacy and reliablitiy in lumbar disc surgery.
Studies of lumbar disc herniation surgery have found some factors that may increase the recurrence rate. Allowing a weakened defect continues to increase the intradiscal pressure changes and thus does not seal completely the annular ring, and this is the major cause of recurrent disc herniations. The risk increases especially in young and middle-aged actively working men. A positive correlation has been found in the literature between lumbar disc herniation and having a job performing varied physical work [4]. However, in some studies, this correlation was not detected in subjects who had done repetitive heavy lifting (no significant relationship was found). Smoking, diabetes, high body mass index, weakness of the annular structure, prolonged exposure to vibration, the degree of the tear in the annulus fibrosus, the type of herniation, and its location are the common risk factors [5]. Reports of male sex as a risk factor are conflicting [6].
Recurrent disc herniation is a common complication in neurosurgery practice and a nightmare for neurosurgeons who have performed lumbar disc herniation surgery. It affects patient and physician satisfaction. It is important to know the risk factors before the operation and share them with the patient beforehand. In cases requiring surgery, complications increase and success rates decrease, especially as the number of relapses increases. This is why our series of 130 cases operated on by a single surgeon in a single center is important.
In our study, the surgical results of 130 lumbar disc herniations, operated on by a single surgeon in a single center and followed up for a long time, were discussed together with the reasons for the recurrence, and an attempt was made to clarify a current issue that is frequently seen in neurosurgery practice.
Material and Methods
STATICAL ANALYSIS:
Statistical analysis was performed with the Friedman test in the evaluation of Oswestry scores before and after the operation. In cases where the same parameter is measured under different conditions on the same subject, the Friedman test is preferred compared to other non-parametric tests. The Siegel Castellan test was used in the analysis of binary non-parametric values. A
Results
SURGICAL TECHNIQUE:
All surgeries were performed under general anesthesia by the same surgeon. Cases that were evaluated with dynamic radiographs, lumbar CT, and lumbar MRI before the operation and had instability and thus required fusion surgery were excluded from the study.
An incision was made with the old incision in the prone position, and then the fascia was opened. Paravertebral muscles were seen with a sharp and blunt dissection. The facets were opened with cauterization. The upper limit of the laminectomy defect was determined. With the help of curette and dissector, a window was opened from the facet side and the lamina side. The old defect was enlarged and progressed. Adhesion areas and normal dura were seen superiorly. Laterally, the articular surface was slightly enlarged. Effort was made to stay away from the granulation area. Discectomy was performed after foraminotomy.
Discussion
Recurrent lumbar disc herniation is defined as a relapsed lumbar disc herniation at least 6 months after the problems improve, at the same level and on the same side. However, it is generally accepted in the literature that the recurrent lumbar disc herniation definition includes ipsilateral or contralateral recurrence at the surgical level with symptomatic and radiological findings, and its occurrence does not depend on a specific time period.
Recurrent lumbar disc herniations continue to be a very frequent and crucial drawback in spinal surgery. Symptoms that do not go away after lumbar discectomy or treatment for lower back pain is defined as “Repeat Surgery-Recovered Lower Back Syndrome” and recurrent disc herniations are one of the main causes [8].
Most patients’ symptoms regress with medical and physical therapy applications [4]. However, a small number of patients with neurological deficits whose symptoms do not regress can be operated on. The operation can be performed as microdiscectomy, open surgery, or endoscopic. Recurrence of the lumbar disc herniation is what the surgeons most fear after the operation. The rate may increase depending on instability, sex, obesity, smoking, location of the disc, disc height before the operation, and age [9]. Although disc recurrence was more common in males in our study, the difference was not statistically significant, and the rate of disc recurrence was higher in the 25–55 age range. When BMI was evaluated, it was 30.0–34.9 kg/m2 in 7 patients.
Studies have reported that male sex and age under 40 years are associated with higher recurrence rates [10]. In addition, high disc height increases the size of the annular tear and the recurrence rate. If there is instability, the recurrence rate increases with disc degeneration [11]. Recurrent lumbar disc surgery is currently performed through microsurgery, endoscopic disc surgery, or fusion surgery after lumbar discectomy. There are many studies in the literature about these 3 surgical techniques. Surgical options include repeat discectomy either via a conventional or minimally invasive technique, with or without instrumented spinal fusion.
When determining the optimal approach, factors including surgeon preference, presenting symptoms, presence of axial low back pain, radiographic evidence of instability or deformity, and number of prior herniations must be considered. A 2017 study found of 1900 patients who underwent endoscopic surgery found that within 5 years 209 of these patients (11%) had relapsed and thus underwent endoscopic surgery [12].The endoscope is not available in all centers today and the learning pathway is lengthy. Although it is easier to recognize anatomical formations in the first operation, identifying the anatomy and intervention in endoscopic interventions may become difficult and complication rates may increase. For this reason, as the microsurgical technique is used more widely and most surgeons are accustomed to using the microscope, surgery can be more comfortable with a low complication rate. Fusion surgery can be considered in cases of instability and where the axial lower back pain is at the forefront.
In some studies, MRI was performed on the patients after surgery, and in 25% of the cases the disc was observed radiologically in the operated area [13]. Most of these patients are asymptomatic. The incidence of recurrence in the literature is 3–24% [14,15]. In a surgical series reported by Parker et al [13], the recurrence rate was 5.3% and the re-operation rate was 4.4%, but Kim et al [15] found that the rate of re-operation due to recurrence was 13.4% for the first 5 years in their series analysis.
In our study, 130 underwent microsurgery, in which a safe area was created from the facet side and then the foramen was enlarged. The literature shows that instability can develop in recurrent lumbar disc herniations and fusion surgery should be performed during the operation. If there was no preoperative instability in our cases, fusion was not performed. Studies have shown that microsurgery can be as effective as the first operation for the second operation, whereas stabilization surgery has not been found to be superior to microsurgery in pain control.
A previous publication reviewed the literature on recurrent lumbar disc herniation surgery and examined 74 articles between 2003 and 2011, presenting the effectiveness of microsurgery in revision disc surgery [15].
Several limitations should be considered when interpreting the results of the present study in which 130 cases of recurrence lumbar disc surgery were analyzed. The shortcomings of the study are the small number of cases, the extended follow-up period, and the lack of comparison of patients who were operated on with different surgeries, such as fusion surgery or endoscopic discectomy. However, following the patients with dynamic radiographs in the postoperative period and adding post-microsurgical instability rates in recurrent disc surgery may increase the power of future studies.
Conclusions
Lumbar microsurgery performed by taking the medial facet and creating a corridor in lumbar recurrent disc herniations, and widening the laminectomy border to the outside of the granulation is very effective. Instability rates will be determined by long-term follow-up of the patients.
References
1. Ropper AH, Zafonte RD, Sciatica: New Engl J Med, 2015; 372; 1240-48
2. Weinstein JN, Lurie JD, Tosteson TD, Surgical vs nonoperative treatment for lumbar disk herniation: The Spine Patient Outcomes Research Trial (SPORT) observational cohort: JAMA, 2006; 296; 2451-59
3. Yin SF, Du H, Yang W, Prevalence of recurrent herniation following percutaneous endoscopic lumbar discectomy: A meta-analysis: Pain Physician, 2018; 21; 337-50
4. An HS, Silveri CP, Simpson JM, Comparison of smoking habits between patients with surgically confirmed herniated lumbar and cervical disc disease and controls: J Spinal Disord, 1984; 7; 369-73
5. Shimia M, Babaei-Ghazani A, Sadat BE, Risk factors of recurrent lumbar disk herniation: Asian J Neurosurg, 2013; 8; 93-96
6. Kim KT, Lee DH, Cho DC, Preoperative risk factors for recurrent lumbar disc herniation in L5–S1: J Spinal Disord Tech, 2014; 28; E571-E77
7. Fairbank JC, Pynsent PB, The Oswestry Disability Index: Spine, 2000; 25; 2940-52
8. Dai LY, Zhou Q, Yao WF, Shen L, Recurrent lumbar disc herniation after discectomy: Outcome of repeat discectomy: Surgical Neurol, 2005; 64; 226-33
9. Ajiboye RM, Drysch A, Mosich GM, Surgical treatment of recurrent lumbar disk herniation: A systematic review and meta-analysis: Orthopedics, 2018; 41; e457-69
10. Aizawa T, Ozawa H, Kusakabe T, Re-operation for recurrent lumbar disc herniation: A study over a 20-year period in a Japanese population: J Orthop Sci, 2012; 17; 107-13
11. Meredith DS, Huang RC, Nguyen J, Obesity increases the risk of recurrent herniated nucleus pulposus after lumbar microdiscectomy: Spine J, 2010; 10; 575-80
12. Park CH, Park ED, Lee SH, Risk factors for early recurrence after transforaminal endoscopic lumbar disc decompression: Pain Physician, 2019; 22; E133-E38
13. Parker SL, Mendenhall SK, Godil SS, Incidence of low back pain after lumbar discectomy for herniated disc and ıts effect on patient-reported outcomes: Clin Orthop Relat Res, 2015; 473(6); 1988-99
14. Daneyemez M, Sali A, Kahraman S, Outcome analyses in 1072 surgically treated lumbar disc herniations: Minim Invasive Neurosurg, 1999; 42(2); 63-68
15. Kim CH, Chung CK, Park CS, Re-operation rate after surgery for lumbar herniated intervertebral disc disease: Nationwide cohort study: Spine (Phila Pa 1976), 2013; 38(7); 581-90
In Press
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
12 Mar 2024 : Clinical Research
Tissue Inhibitors of Metalloproteinase 1 (TIMP-1) and 3 (TIMP-3) as New Markers of Acute Kidney Injury Afte...Med Sci Monit In Press; DOI: 10.12659/MSM.943500
12 Mar 2024 : Review article
Optimizing Behçet Uveitis Management: A Review of Personalized Immunosuppressive StrategiesMed Sci Monit In Press; DOI: 10.12659/MSM.943240
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952