08 April 2024: Clinical Research
Factors Influencing Time to First Medical Contact in Patients with Acute ST-Segment Elevation Myocardial Infarction: A Retrospective Analysis
Yong Sun1ACDE*, Qinnan Yang1BEF, Hongjin Liu1AEF, Binshi Li1BDE, Puqing Lin1ACDG, Yanrong Chen1CEF, Xuehua Wan1EFG, Qingxuan Yu1ABC, Chunxia Qi1BDF, Changjiang Hong1BCDOI: 10.12659/MSM.942080
Med Sci Monit 2024; 30:e942080
Abstract
BACKGROUND: Exploring the factors that impact the time from symptom onset to first medical contact (S2FMC) is crucial for improving outcomes in elderly patients diagnosed with acute ST-segment elevation myocardial infarction (STEMI). This study conducted a retrospective analysis on 282 patients who underwent emergency percutaneous coronary intervention (PCI) or percutaneous transluminal coronary angioplasty (PTCA) in Guangzhou City District to identify significant factors affecting S2FMC.
MATERIAL AND METHODS: A retrospective analysis was conducted on 282 patients with STEMI who underwent emergency percutaneous coronary intervention (PCI). Descriptive statistics, univariate and multivariate Cox regression analyses were used to identify significant factors affecting S2FMC. Additionally, interactions between risk factors were examined using multivariate logistic regression and the structural equation model (SEM).
RESULTS: Age (HR=0.984, 95% CI: 0.975-0.993), nature of chest pain (HR=2.561, 95% CI: 1.900-3.458), admission mode (HR=1.805, 95% CI: 1.358-2.400), and vascular characteristics (HR=1.246, 95% CI: 1.069-1.451) were independent influencing factors for S2FMC. Persistent chest tightness/pain, EMS admission, and vascular characteristics (RCADL or LCADL) played a protective role in S2FMC. Among the influencing factors, vascular characteristics (OR=1.072, 95% CI: 1.008-1.141) had an independent effect on the nature of chest pain. Meanwhile, the nature of chest pain (OR=1.148, 95% CI: 1.015-1.298) was an independent influencing factor in the admission mode.
CONCLUSIONS: Patients with persistent chest tightness/pain, EMS admission, and vascular characteristics (RCADL or LCADL) experienced shorter S2FMC and higher compliance rate (S2FMC ≤180 min). At the same time, age and other vascular features played an inverse role. This study proposes enhancing follow-up and monitoring measures, and shows the consequences of intermittent chest pain should not be disregarded.
Keywords: ST elevation myocardial infarction, percutaneous coronary intervention, Time-to-Treatment
Introduction
Acute ST-segment elevation myocardial infarction (STEMI) has the highest fatality rate among patients experiencing acute chest pain due to acute onset, rapid progression, and many complications. Focusing on the current treatment consensus, shortening the total ischemic time (TIT), and performing early reperfusion, the medical system has carried out a series of promotions of concepts such as green channels for chest pain and regional transport. However, compared to the higher response rate in the emergency department, the mortality rate of STEMI patients remains stable [1]. Two links in the process from symptom onset to reperfusion delay were analyzed: one was patient delay, which refers to the time of symptom onset to first medical contact (S2FMC), and the other was system delay, which refers to the time from the first medical contact to the guide wire (F2W). After many years of efforts, especially promotion of the concept of chest pain centers, F2W is gradually shortening, while in STEMI treatment registry data from 1987 to 2021 in the United States and France, it was found that S2FMC time had improved little [2–5]. According to data from the Global Registry of Acute Coronary Events study, the median S2FMC time for patients with STEMI was shortest in Australia/New Zealand (2.2 h) and longest in Argentina and Brazil (4.0 h) [6]. In China, a prospective study [7] found that the median S2FMC time for AMI patients was 4 h, highlighting the urgent need for further investigation into S2FMC in China.
Time is myocardium. In China, an extended S2FMC time is significantly associated with adverse in-hospital outcomes in patients with STEMI. To shorten the time of myocardial ischemia and improve the efficiency of STEMI treatment while gradually improving the system delay, many studies on the influencing factors of S2FMC have been carried out in China and abroad, including sociological studies involving sex [8–10], age [10,11], family income [12], and education [12], including the study of medical treatment process, involving urban/rural areas [13], medical treatment methods [13], onset time [10, 11], and use of emergency medical system; there are also medical information studies involving smoking, hypertension, hyperlipidemia, diabetes, cardiogenic shock, and old myocardial infarction. Many influencing factors of S2FMC have been found, but they differ for different regions and ages. The reported results of various studies vary or are contradictory. Currently, there is a lack of research reports on the current situation in China. Therefore, the influencing factors of S2FMC in China still need to be clarified.
China’s vast geographical spread and significant urban-rural disparities necessitate targeted research for specific regions, which bears more practical significance. As a first-tier city in China, Guangzhou represents the situation of major cities in the country. In this study, we aim to retrospectively analyze a single center in Guangzhou to evaluate the factors influencing S2FMC time and explore the underlying reasons. This study will provide evidential support for optimizing the construction of chest pain centers in China’s major cities and formulating clinical guidance.
Material and Methods
STUDY SUBJECTS:
Based on the comprehensive quality control score in 2020, Clifford Hospital’s Chest Pain Center topped the list in China. Located in the urban region of Guangzhou, the center serves a high-density population within a less than 10 km radius, as demarcated by the chest pain map area. From January 2018 to December 2020, this study included STEMI patients whose initial 18-lead ECG exhibited an ST-segment elevation of 1 mm or more in 2 or more contiguous leads [14], and who underwent emergency PCI intervention to open the infarct-related artery (IRA), excluding those who received thrombolytic therapy. Patients who developed STEMI during hospitalization or had missing clinical data were excluded. This study received approval from the Ethics Committee of Guangdong Clifford Hospital (Approval No.: 2/2021-65), with the informed consent form being waived after approval.
Patients’ S2FMC time and the Admission mode were collected through the National Chest Pain Center Data Reporting Platform (
After anonymizing personally identifiable information, we extracted data from the electronic medical record system, encompassing aspects such as age, sex, the nature of chest pain, the time of onset, the length of hospital stay, hospitalization costs, and medical insurance coverage. Chest pain was bifurcated into 2 categories: intermittent chest tightness/pain and persistent chest tightness/pain. The latter signifies an unrelieved continuation of symptoms from the time of symptom onset to their first medical encounter, with a duration equivalent to S2FMC. The time of onset was divided into 2 periods: daytime (from 8 am to 8 pm) and nighttime (from 8 pm to 8 am the following day). Based on the proportion of coverage, medical reimbursement was classified as high, medium, or low. The key parameters measured in the patient’s initial laboratory-assisted examination after admission included glycosylated hemoglobin, total cholesterol, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, and triglycerides. At discharge, diagnostic information was collated, and an assessment was made regarding the coexistence of diseases such as diabetes, hypertension, hyperlipidemia, hyperuricemia, heart failure, and arrhythmia.
The results of the emergency coronary angiography were collected. Only vessels with a diameter ≥1.5 mm were evaluated. Coronary arteries were diseased if they exhibited left main artery stenosis ≥30%, coronary artery stenosis ≥50%, or previous revascularization therapy. The dominant coronary artery type was categorized as left dominant, right dominant, or balanced. The infarct-related artery (IRA) was classified into the left anterior descending branch (including the left main), right coronary artery, and left circumflex branch. The degree of coronary artery stenosis was categorized as subtotal occlusion or total occlusion. The vascular characteristics were classified into 3 groups based on the dominance type of the coronary artery and the status of lesion branches: left coronary artery dominance with lesions (LCADL) refers to an acute occlusion of a dominant left anterior descending (LAD) artery, right coronary artery dominance with lesions (RCADL) refers to acute occlusion of a dominant right coronary artery (RCA), and other groups.
Study group: According to the Quality Control Report of the China Chest Pain Center, the statistical threshold for S2FMC is 180, to calculate the compliance rate for S2FMC ≤180 min or the non-compliance rate for S2FMC >180 min. In this study, patients were categorized into 2 groups according to their S2FMC time: the target group (S2FMC ≤180 min) and the delayed group (S2FMC >180 min).
DATA ANALYSIS:
The statistical analysis was performed using R software version 4.2.0 (
Results
BASELINE CHARACTERISTICS COMPARISON:
A total of 290 participants were included, with 8 individuals excluded due to incomplete data, resulting in 282 participants comprising 243 males and 39 females, with a mean age of 56.67±13.15 years. Comparisons among the groups revealed significant differences in age, nature of chest pain, admission mode, glycosylated hemoglobin levels, total cholesterol levels, low-density lipoprotein levels, length of hospital stay, and vascular characteristics across different S2FMC time groups (P<0.05). No significant differences were found in the onset period, F2W time, coronary dominance, infarct-related coronary artery, lesion vessel number, sex, high-density lipoprotein levels, triglyceride levels, inpatient costs, availability of medical insurance support, or presence of comorbid diseases (Table 1).
SCREENING OF S2FMC INFLUENCING FACTORS BASED ON UNIVARIATE AND MULTIVARIATE COX REGRESSION ANALYSIS:
The dependent variable was whether S2FMC exceeded the standard value of 180 min, with the delayed group coded as 1 and the target group coded as 0. The independent variables included factors that showed group differences and factors identified in previous literature as potential contributors to delay time. We performed a univariate Cox regression analysis to evaluate the impact of various factors on S2FMC in patients. Age (HR=0.989, 95% CI: 0.980–0.998, P=0.0120), nature of chest pain (HR=2.818, 95% CI: 2.100–3.781, P=0.000), admission mode (HR=1.865, 95% CI: 1.422–2.447, P=0.000), vascular characteristics (HR=1.295, 95% CI: 1.112–1.507, P=0.001), total cholesterol (HR=1.124, 95% CI: 1.018–1.241, P=0.021), and low-density lipoprotein level (HR=1.153, 95% CI: 1.035–1.284, P=0.010) were identified as risk factors contributing to S2FMC. For more details, please refer to Table 2. Next, we integrated these identified risk factors into a multivariate Cox regression analysis. This revealed that age (HR=0.984, 95% CI: 0.975–0.993, P=0.001), nature of chest pain (HR=2.561, 95% CI: 1.897–3.458, P=0.000), admission mode (HR=1.805, 95% CI: 1.358–2.400, P=0.000), and vascular characteristics (HR=1.246, 95% CI: 1.069–1.451, P=0.005) were independent risk factors for S2FMC in STEMI patients.
More specifically, older age was associated with a higher risk of prolonged S2FMC. Persistent chest tightness/pain and EMS admission, on the other hand, were linked to a reduced risk of prolonged S2FMC. Likewise, RCADL and LCADL were associated with a lower risk of delayed S2FMC compared to other types. This trend aligns with the results from our logistic regression analysis. More details can be found in Table 3.
KAPLAN-MEIER SURVIVAL ANALYSIS:
Using the surv_cutpoint function, the optimal cutoff value of age was determined to be 69 years. Participants were then classified into 2 groups: advanced age and younger age. The results revealed a higher compliance rate of S2FMC (≤180 min) in the younger age group compared to the older group (P=0.023) (Figure 1A).
When participants were grouped based on the nature of their chest pain, a statistically significant difference in the compliance rate of S2FMC was observed between the group experiencing intermittent chest tightness/pain and the group experiencing persistent chest tightness/pain. The group with persistent chest tightness/pain exhibited a higher compliance rate (P<0.001) (Figure 1B).
Furthermore, when participants were divided based on their admission mode, a statistically significant difference in the compliance rate of S2FMC was observed between the self-admission group and the EMS group. The EMS group demonstrated a higher compliance rate (P<0.001) (Figure 1C).
Lastly, a statistically significant difference in the compliance rate of S2FMC was observed among various combinations based on vascular characteristics. The group with acute occlusion of the RCADL exhibited the highest compliance rate of S2FMC, followed by the LCADL, with the other groups having the lowest compliance rate (P=0.003) (Figure 1D).
MULTIVARIATE LOGISTIC REGRESSION ANALYSIS BETWEEN S2FMC INFLUENCING FACTORS:
Multivariate logistic regression was used with the nature of chest pain as the dependent variable (intermittent chest tightness/pain=0, persistent chest tightness/pain =1), age (<69 years=0, ≥69 years=1), admission mode (self-admission=0, EMS=1), and vascular characteristics (others=0, LCADL=1, RCADL=2) as independent variables. The results showed that admission mode (OR=1.132, 95% CI: 1.013–1.264, P=0.029) and vascular characteristics (RCADL and LCADL) (OR=1.072, 95% CI: 1.008–1.141, P=0.027) had an independent effect on the nature of chest pain. Further details are provided in Table 4.
Considering the admission mode as the outcome variable (self-admission=0, EMS admission=1), the nature of chest pain (intermittent chest tightness/pain=0, persistent chest tightness/pain=1), age (<69 years=0, 1 ≥69 years=1), and vascular characteristics (others=0, LCADL=1, RCADL=2) were included as predictor variables. Multivariate logistic regression was employed. The analysis revealed that the nature of chest pain (OR=1.148, 95% CI: 1.015–1.298, P=0.029) was a significant independent factor influencing admission mode. Further details are provided in Table 5.
STRUCTURAL EQUATION MODELING OF S2FMC BASED ON SIGNIFICANTLY INFLUENCING FACTORS:
The significant, influential factors mentioned above were treated as observed variables, with S2FMC as the outcome variable to examine the interrelationships among factors. In the structural equation model, each variable directly or indirectly impacted S2FMC. Among them, the nature of chest pain had the greatest influence on S2FMC, with a direct effect coefficient of −0.46. The mediating effect through the admission mode was calculated as 0.03×−0.19=−0.0057. The vascular characteristics directly impacted −0.07 on S2FMC, with an indirect effect mediated by the nature of chest pain as 0.04×−0.46=−0.0184.
Additionally, S2FMC was also influenced by other factors. Age indirectly affected S2FMC through vascular characteristics as −0.21×−0.07=0.0147 and through the nature of chest pain as −0.42×−0.46=0.1932. The mediating effect of hospital admission mode on S2FMC was calculated as 0.58×−0.19=−0.1102, resulting in a total effect of 0.0977. Among the influential factors, age had a significant direct impact on hospital admission mode (0.58), a direct impact of −0.21 on vascular characteristics, and a direct impact of −0.42 on the nature of chest pain (Figure 2).
Discussion
Previous studies have suggested that for STEMI patients, a prolonged S2FMC (≥2 h) is associated with in-hospital mortality (OR=1.36, 95% CI: 1.09–1.69, P=0.006), whereas no significant correlation has been observed between an extended S2FMC (≥2 h) and in-hospital outcomes for NSTEMI patients [15]. This conclusion emphasizes the importance of controlling S2FMC in STEMI patients. However, the S2FMC of STEMI patients in China is significantly higher than in Western countries and other Asian countries like South Korea [6,16]. Some studies point out that S2FMC may be related to direct costs for doctors and the distance from patients to hospitals [17], which may vary between urban and rural areas. These studies did not specifically address the situation in China. Moreover, there is a correlation among the influencing factors. Therefore, this study focused on Guangzhou, a representative of large cities in China, to repeatedly verify the importance of factors affecting S2FMC and analyze the correlation among these factors, aiming to construct a systemic regulatory network for S2FMC.
Firstly, we classified patients into the ‘delayed’ group and the ‘target’ group based on whether S2FMC exceeded the threshold. We initially screened influential factors, including age, nature of chest pain, admission mode, glycosylated hemoglobin, total cholesterol, low-density lipoprotein, length of hospital stay, and vascular characteristics, through univariate Cox regression. Interestingly, in the multivariate Cox regression, only age, nature of chest pain, admission mode, and vascular characteristics were independent factors for exceeding S2FMC after adjusting for confounding factors. Mainly, persistent chest tightness/pain, EMS admission, and vascular characteristics (RCADL or LCADL) were found to have a protective effect on S2FMC, leading to a higher compliance rate. In contrast, age was an independent risk factor for S2FMC, with older age being associated with prolonged S2FMC. The primary manifestation of STEMI is chest tightness/pain, typically characterized by precordial crushing pain, with a feeling of suffocation and dyspnea. It may also radiate to the left arm, shoulder, or back [18]. However, some patients with ST-segment elevation myocardial infarction present with non-precordial squeezing pain in clinical practice. Elderly patients are more likely to ignore their symptoms [19]. Research shows that compared to patients without pain, not only thrombolytic treatment, patients with pre-infarction angina (PIA) have better in-hospital outcomes after PCI treatment [20]. Our study suggests that persistent chest tightness/pain is a protective factor of S2FMC, as continuous discomfort can attract patients’ attention and thereby shorten the S2FMC. However, as chest pain is a subjective sensation, individual tolerance greatly varies from perception. Patients may ignore or tolerate intermittent or mild chest pain symptoms, resulting in delayed medical attention. In other words, many patients may not have chest pain of sufficient concern, regardless of the nature or level of chest pain, even if they have severe acute coronary artery disease [21]. Our results suggest that patients with coronary heart disease lack proper management and education. Patients should manage the disease through regular follow-ups and screenings and should not limit the reason for seeking medical attention to the pain level. This proactive approach can identify disease progression and promote timely treatment.
In addition, the nature of chest pain in STEMI is correlated with the characteristic of diseased blood vessels [22], which is consistent with the findings of this study. The study showed that STEMI patients with RCADL experienced shorter relative delay times. The results of this study indicate that vascular characteristics can influence S2FMC through different types of chest pain. The intensity of chest pain is determined by the activation of free nerve endings resulting from myocardial ischemia [23]. Due to the greater blood supply in the dominant coronary artery, the resulting area of myocardial ischemia is larger, causing more severe chest pain and faster patient response to seeking medical treatment. Conversely, individuals with non-dominant coronary lesions are more likely to experience silent myocardial ischemia, which can lead to undetectable symptoms. Enhancing regular examinations for patients with coronary heart disease and implementing sufficient medical monitoring and early warning systems for individuals with plaque or narrowing in non-dominant coronary arteries can improve the speed of response and treatment rates during STEMI occurrences.
In the selection of hospital visits, only 26.2% of the patients participating in this study opted for EMS admission. Data from studies in New Zealand, Germany, Italy, and Hungary showed that 77%, 55.9% [21], 52.1% [24], and 51.4% [25] of patients experiencing chest pain chose EMS transport in their respective regions. However, in a study conducted in Henan Province, China, only 15.09% of patients chose EMS transport [11], which indicates a need for more understanding of the benefits of EMS use among Chinese people. Selecting EMS offers several benefits for patients with chest pain, including pre-hospital ECG transmission, early diagnosis, and prompt catheterization initiation, effectively reducing system delays [26]. Compared with metropolitan Italian data, EMS bypassing the emergency department and early triage based on electrocardiogram can significantly reduce system delays. When EMS bypasses the high proportion of emergency visits, reducing decision time alone can lead to further reduced system delays [27]. With the publicity and popularization of acute myocardial infarction-related knowledge, at this stage, with citizens having a greater understanding of the discriminatory symptoms of acute myocardial infarction, the focus should be on promoting awareness of the EMS treatment process and its benefits and on reducing total myocardial ischemia time, and improve the prognosis for patients with acute myocardial infarction.
According to the existing literature, young patients with STEMI tend to have typical chest pain symptoms, such as squeezing, burning, or stabbing sensations. However, with increasing age, the perception of pain may change. Older adults may experience different symptoms, such as chest tightness, discomfort, or no obvious symptoms. This may be due to age-related physiological changes, such as decreased pain perception or misunderstanding of heart disease. A trend of relatively lower compliance was observed in the older group in the KM survival analysis. Previous studies also support this view, showing a positive correlation between age and S2FMC delay [2,10,19], with a 4.9% increase in the probability of delayed seeking medical help for every 1-year increase [11]. This may be related to the insensitivity of elderly patients to chest pain symptoms and delayed seeking of help. These findings suggest that strategies for early identification and management of STEMI need to consider the influence of age. For older patients, further education may be needed to improve their awareness of heart disease symptoms and encourage them to use ambulances to reach the hospital.
While some studies have suggested that a medical history of conditions such as hypertension and diabetes may influence the S2FMC of STEMI patients, this trend was not found in the present study. Moreover, Hu et al [15] found that age ≥65 was a risk factor for S2FMC (OR=1.26, 95% CI: 1.19–1.35) but did not evaluate the optimal age cutoff. In our study, we found that the traditional cutoff of 65 years old could not be used as the optimal cutoff, which should be 69 years old. On the one hand, we believe this is due to the higher level of urban medical care and preventive measures, such as regular physical examinations, which slow down physical degradation. On the other hand, it may be related to the limited sample size of our study. Therefore, this controversy warrants further research and verification.
Although age, nature of chest pain, admission mode, and vascular characteristics are closely related to S2FMC, we also noticed that these 4 factors interact with each other. In the multivariate logistics regression model with the nature of chest pain as the outcome indicator, vascular features are independent influencing factors, and the nature of chest pain is also an independent influencing factor for admission mode. Therefore, this study explored the interaction between influencing factors based on the structural equation model. Although age does not directly affect S2FMC, it does so through factors such as vascular characteristics. Nevertheless, age affects the nature of chest pain, admission mode, and vascular characteristics, affecting S2FMC. Therefore, this study advocates strengthening follow-up and monitoring, paying attention to LCADL and RCADL, not ignoring the consequences of intermittent chest pain, and choosing EMS as much as possible, especially for older patients.
Conclusions
This study reveals the factors influencing delay of S2FMC in patients with STEMI in urban areas of China. It is necessary to further shorten the S2FMC time and focus on STEMI education for the elderly. When chest tightness/pain occurs, choosing EMS admission can significantly shorten the pre-hospital delay time.
This study has several limitations, including a small sample size, the use of single-center data, and the retrospective analysis. Furthermore, there was no follow-up to verify the prognosis of the patients, which necessitates further refinement in future studies. We expect to validate and expand the results of this study in a multi-center, large-sample study.
Figures
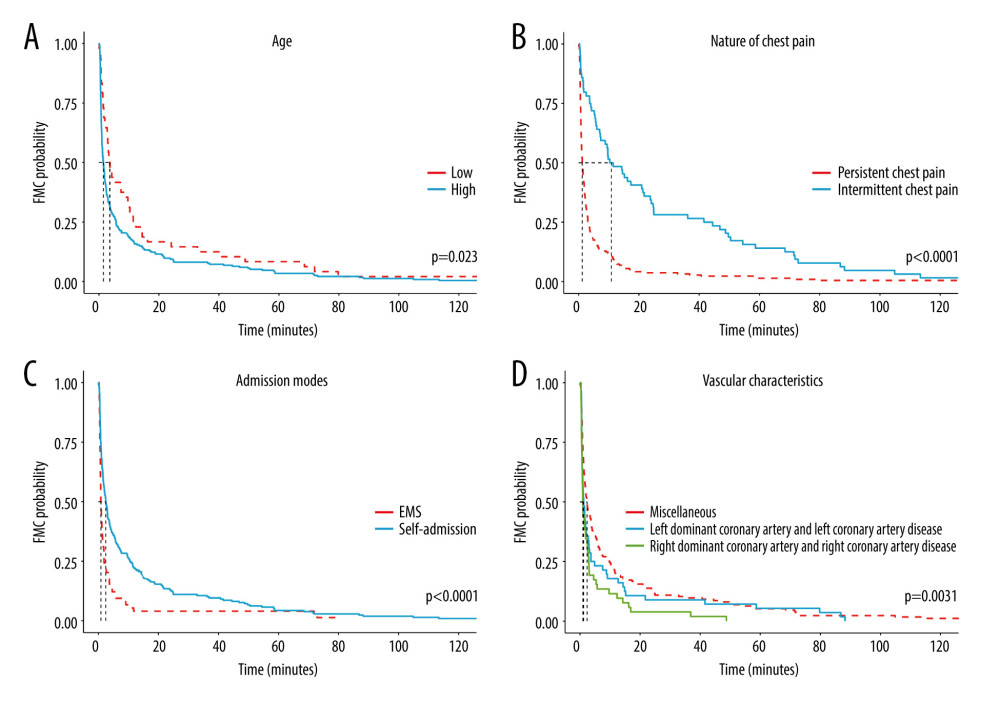 Figure 1. (A) KM curves of patients in different age groups. (B) KM curve of patients with different nature of chest pain. (C) KM curve of patients with different admission modes. (D) KM curve of patients with different vascular characteristics.
Figure 1. (A) KM curves of patients in different age groups. (B) KM curve of patients with different nature of chest pain. (C) KM curve of patients with different admission modes. (D) KM curve of patients with different vascular characteristics. 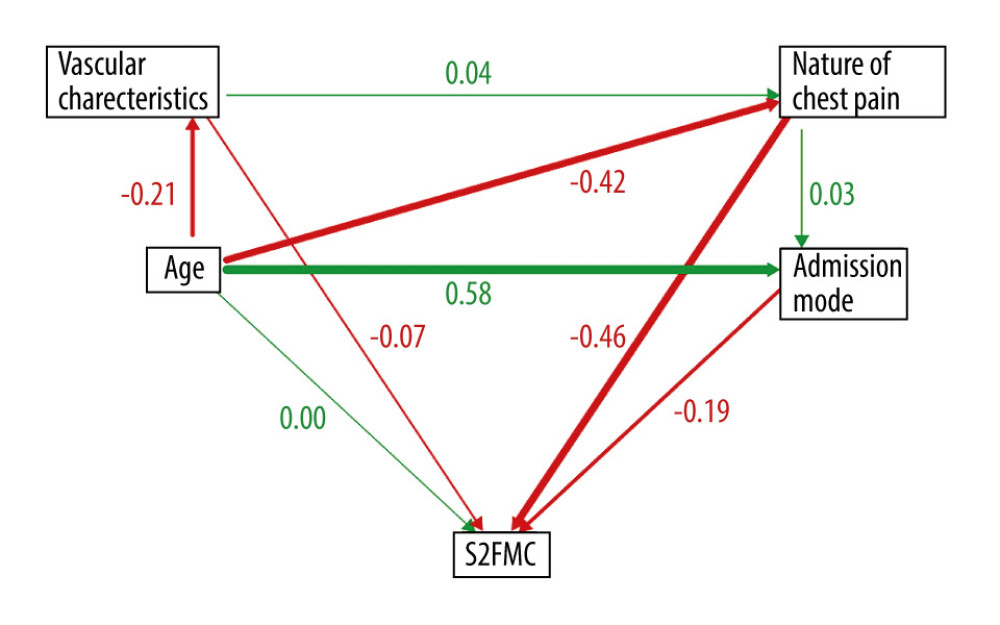 Figure 2. Results of the structural equation model.
Figure 2. Results of the structural equation model. Tables
Table 1. General characteristics table.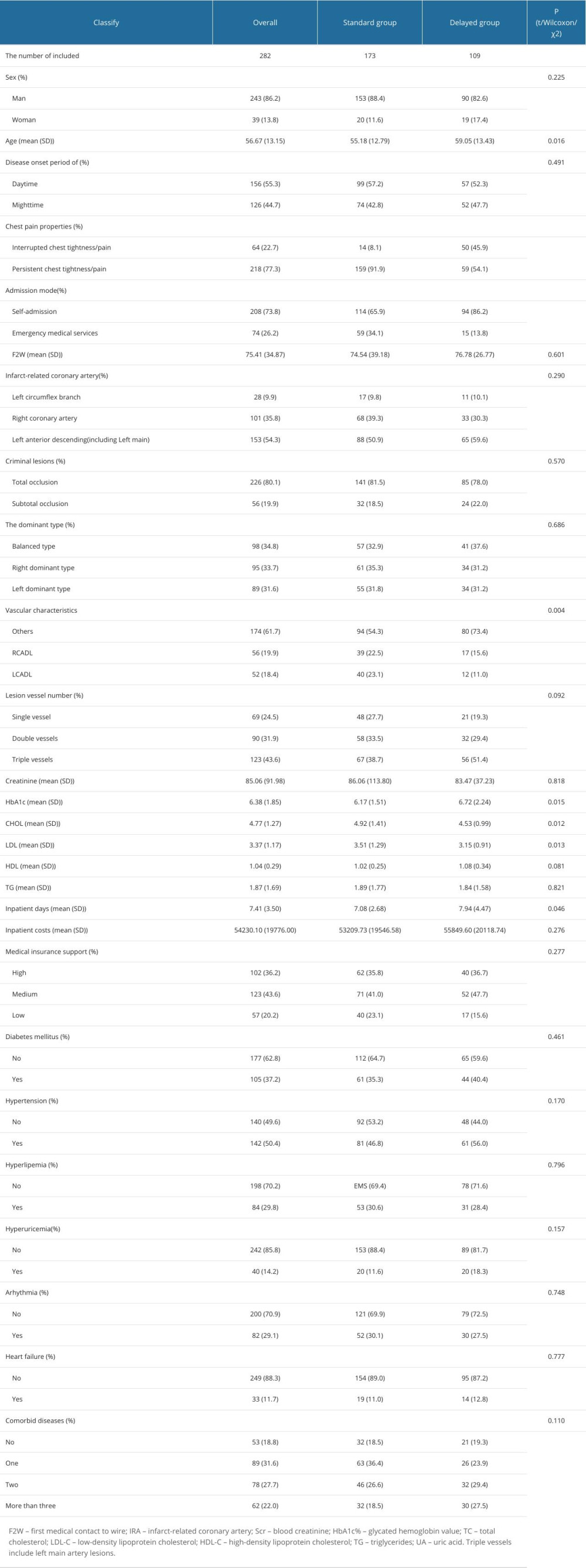 Table 2. Univariate Cox regression screening of S2FMC influencing factors.
Table 2. Univariate Cox regression screening of S2FMC influencing factors.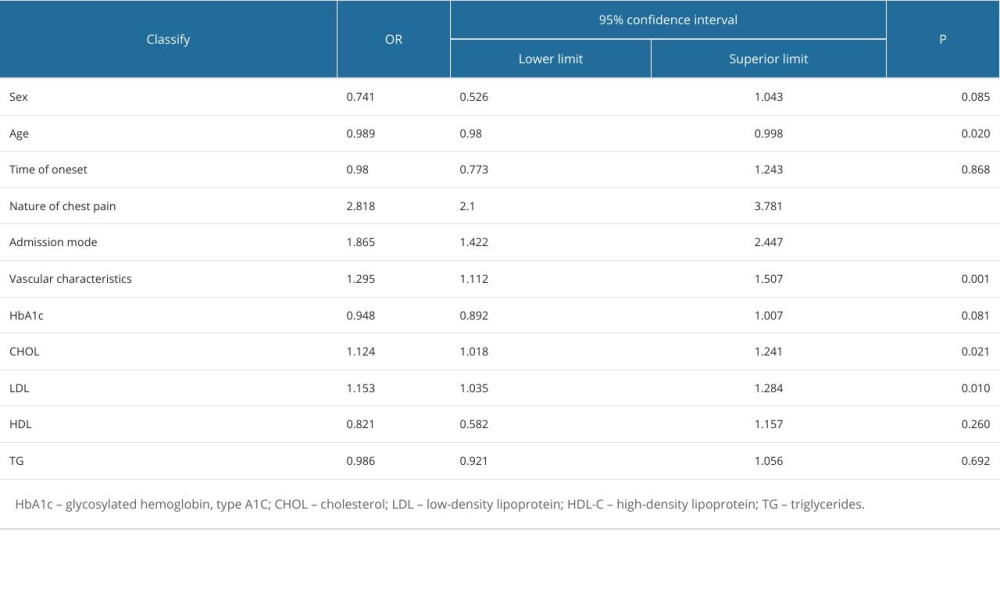 Table 3. Multivariate Cox regression screening of S2FMC influencing factors.
Table 3. Multivariate Cox regression screening of S2FMC influencing factors. Table 4. Multivariate logistics regression screening of chest pain influencing factors.
Table 4. Multivariate logistics regression screening of chest pain influencing factors.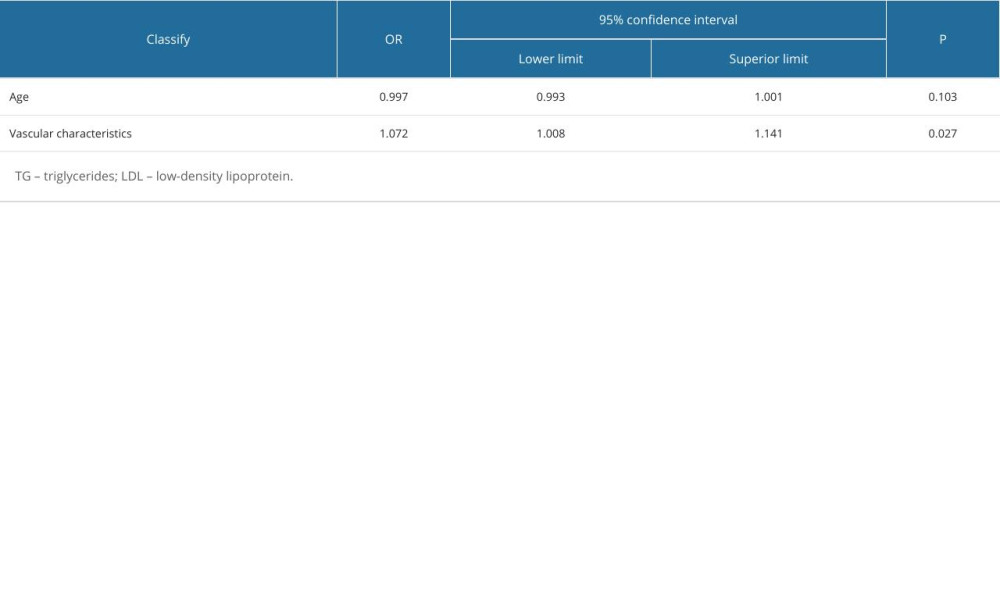 Table 5. Multivariate logistics regression screening of chest pain influencing factors.
Table 5. Multivariate logistics regression screening of chest pain influencing factors.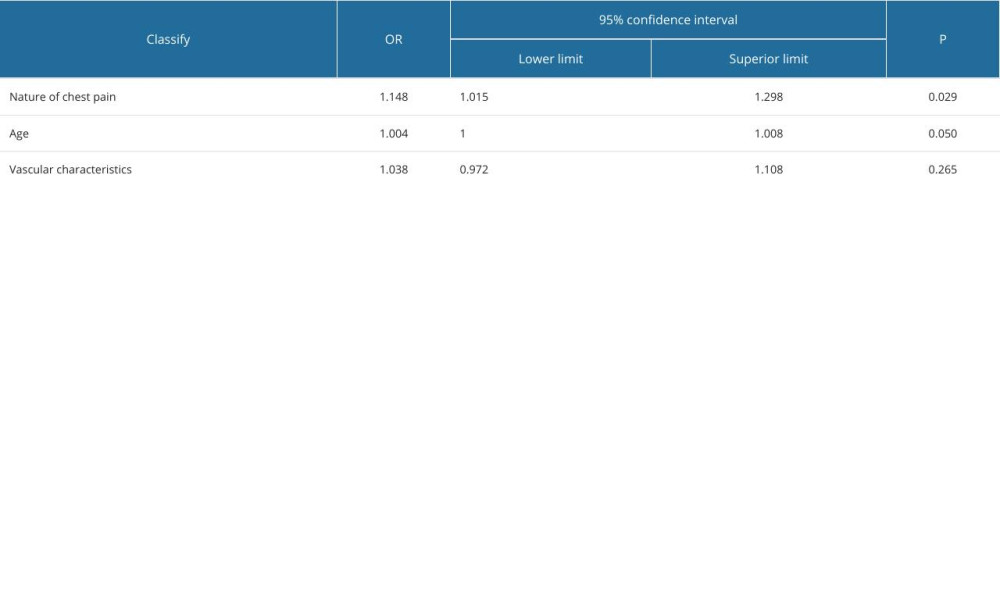
References
1. The Writing Committee Of The Report On Cardiovascular Health And Diseases In China (WCOTROCHADIC), Report on Cardiovascular Health and Diseases in China 2022: An updated summary: Biomed Environ Sci, 2023; 36(8); 669-701
2. McGinn AP, Rosamond WD, Goff DJ, Trends in prehospital delay time and use of emergency medical services for acute myocardial infarction: experience in 4 US communities from 1987–2000: Am Heart J, 2005; 150(3); 392-400
3. Granger CB, Bates ER, Jollis JG, Improving care of STEMI in the United States 2008 to 2012: J Am Heart Assoc, 2019; 8(1); e008096
4. El KC, Bochaton T, Flocard E, Five-year evolution of reperfusion strategies and early mortality in patients with ST-segment elevation myocardial infarction in France: Eur Heart J Acute Cardiovasc Care, 2017; 6(7); 573-82
5. Jollis JG, Granger CB, Zegre-Hemsey JK, Treatment time and in-hospital mortality among patients with ST-segment elevation myocardial infarction, 2018–2021: JAMA, 2022; 328(20); 2033-40
6. Goldberg RJ, Spencer FA, Fox KA, Prehospital delay in patients with acute coronary syndromes (from the Global Registry of Acute Coronary Events [GRACE]): Am J Cardiol, 2009; 103(5); 598-603
7. Guan W, Venkatesh AK, Bai X, Time to hospital arrival among patients with acute myocardial infarction in China: A report from China PEACE prospective study: Eur Heart J Qual Care Clin Outcomes, 2019; 5(1); 63-71
8. Stehli J, Dinh D, Dagan M, Sex differences in prehospital delays in patients with ST-segment-elevation myocardial infarction undergoing percutaneous coronary intervention: J Am Heart Assoc, 2021; 10(13); e019938
9. Sederholm LS, Isaksson RM, Ericsson M, Gender disparities in first medical contact and delay in ST-elevation myocardial infarction: A prospective multicentre Swedish survey study: BMJ Open, 2018; 8(5); e020211
10. Pereira H, Cale R, Pinto FJ, Factors influencing patient delay before primary percutaneous coronary intervention in ST-segment elevation myocardial infarction: The Stent for life initiative in Portugal: Rev Port Cardiol (Engl Ed), 2018; 37(5); 409-21
11. Sun X, Yao B, Shi K, The impact of chest pain center on treatment delay of STEMI patients: A time series study: BMC Emerg Med, 2021; 21(1); 129
12. Mochari-Greenberger H, Miller KL, Mosca L, Racial/ethnic and age differences in women’s awareness of heart disease: J Womens Health (Larchmt), 2012; 21(5); 476-80
13. Panda P, Singh NV, Kaur N, Delay in seeking medical treatment among patients with acute coronary syndrome: Cureus, 2021; 13(8); e17369
14. Vogel B, Claessen BE, Arnold SV, ST-segment elevation myocardial infarction: Nat Rev Dis Primers, 2019; 5(1); 39
15. Hu D, Hao Y, Liu J, Pre-hospital delay in patients with acute myocardial infarction in China: Findings from the Improving Care for Cardiovascular Disease in China-Acute Coronary Syndrome (CCC-ACS) project: J Geriatr Cardiol, 2022; 19(4); 276-83
16. Kim RB, Hwang JY, Park HW, Contemporary status of acute myocardial infarction in Korean patients: Korean registry of acute myocardial infarction for regional cardiocerebrovascular centers: J Clin Med, 2021; 10(3); 498
17. WilliaGontina S, Nurwahyuni A, Determinants of inpatient cost for patients with ST-elevation myocardial infarct at Mayapada Hospital, Tangerang: Childhood Stunting, Wasting, and Obesity, as the Critical Global Health Issues: Forging Cross-Sectoral Solutions, 2020
18. Legare CA, Dunn E, Arner K, History, ECG, risk factors (HER) scoring for cardiac risk stratification in patients <45 years of age presenting with chest pain: Cureus, 2023; 15(6); e40458
19. Berga CG, Martinez MM, Valverde BJ, Association of sex and age and delay predictors on the time of primary angioplasty activation for myocardial infarction patients in an Emergency Department: Heart Lung, 2023; 58; 6-12
20. Ahmed TAN, Abdel-Nazeer AA, Hassan AKM, Electrocardiographic measures of ventricular repolarization dispersion and arrhythmic outcomes among ST elevation myocardial infarction patients with pre-infarction angina undergoing primary percutaneous coronary intervention: Ann Noninvasive Electrocardiol, 2019; 24(4); e12637
21. Aitavaara-Anttila MK, Pernu HH, Rumpunen TK, Factors associated with time delay to angiography in acute ST-elevation myocardial infarction – a retrospective cohort study in Northern Finland: Australas Emerg Care, 2022; 25(3); 213-18
22. Kontos MC, de Lemos JA, Deitelzweig SB, 2022 ACC expert consensus decision pathway on the evaluation and disposition of acute chest pain in the Emergency Department: A report of the American College of Cardiology Solution Set Oversight Committee: J Am Coll Cardiol, 2022; 80(20); 1925-60
23. Longhurst JC, Tjen-A-Looi SC, Fu LW, Cardiac sympathetic afferent activation provoked by myocardial ischemia and reperfusion. Mechanisms and reflexes: Ann NY Acad Sci, 2001; 940; 74-95
24. Scorcu G, Meloni L, Pilleri AThe network for acute coronary syndromes in the metropolitan area of Cagliari (Italy): Management of ST-elevation myocardial infarction, reperfusion time, and adherence to guidelines: G Ital Cardiol (Rome), 2013; 14(1); 66-75 [in Italian]
25. Jánosi A, Ofner P, Al-Maktari F, A szívinfarktus miatt kezelt betegek ellátása Magyarországon. A Nemzeti Szívinfarktus Regiszter 2015. évi adatainak elemzése: Orv Hetil, 2017; 158(3); 90-93 [in Hungarian]
26. Hutchison AW, Malaiapan Y, Jarvie I, Prehospital 12-lead ECG to triage ST-elevation myocardial infarction and Emergency Department activation of the infarct team significantly improves door-to-balloon times: Ambulance Victoria and MonashHEART Acute Myocardial Infarction (MonAMI) 12-lead ECG project: Circ Cardiovasc Interv, 2009; 2(6); 528-34
27. Todt T, Thylen I, Alfredsson J, Strategies TO reduce time delays in patients with AcuTe coronary heart disease treated with primary PCI--the STOP WATCH study: A multistage action research project: BMJ Open, 2013; 3(9); e003493
Figures
Tables
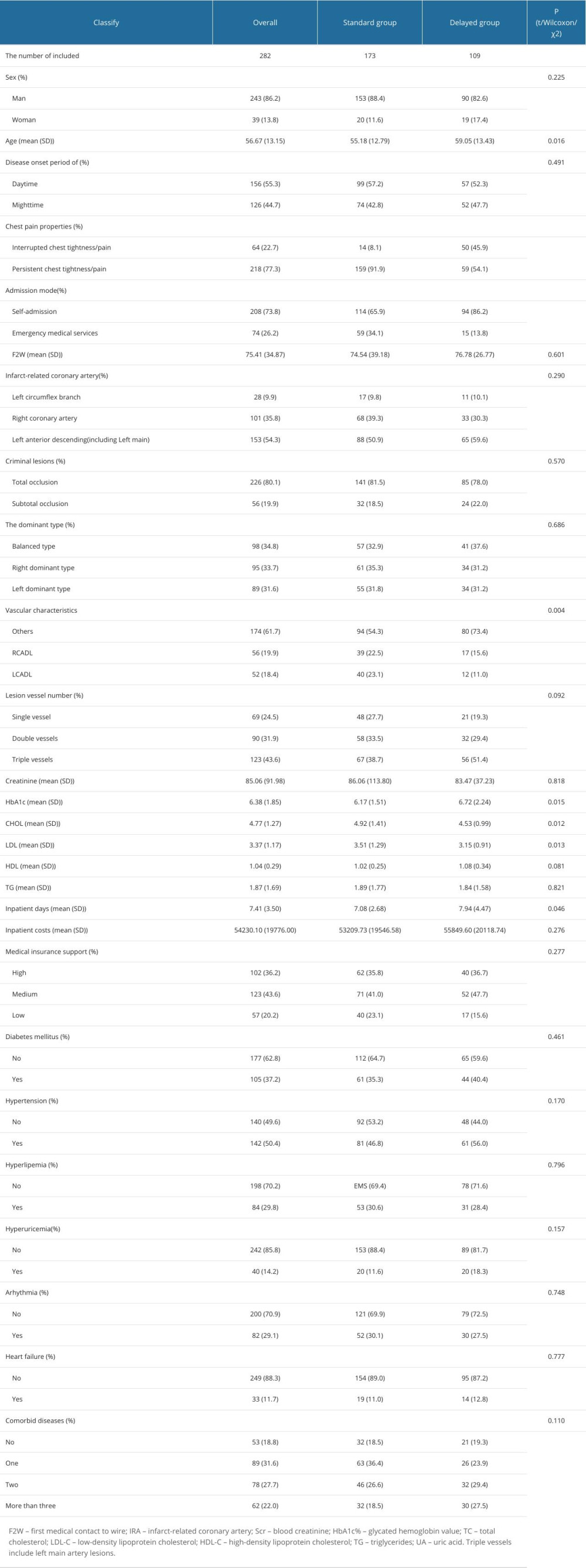 Table 1. General characteristics table.
Table 1. General characteristics table.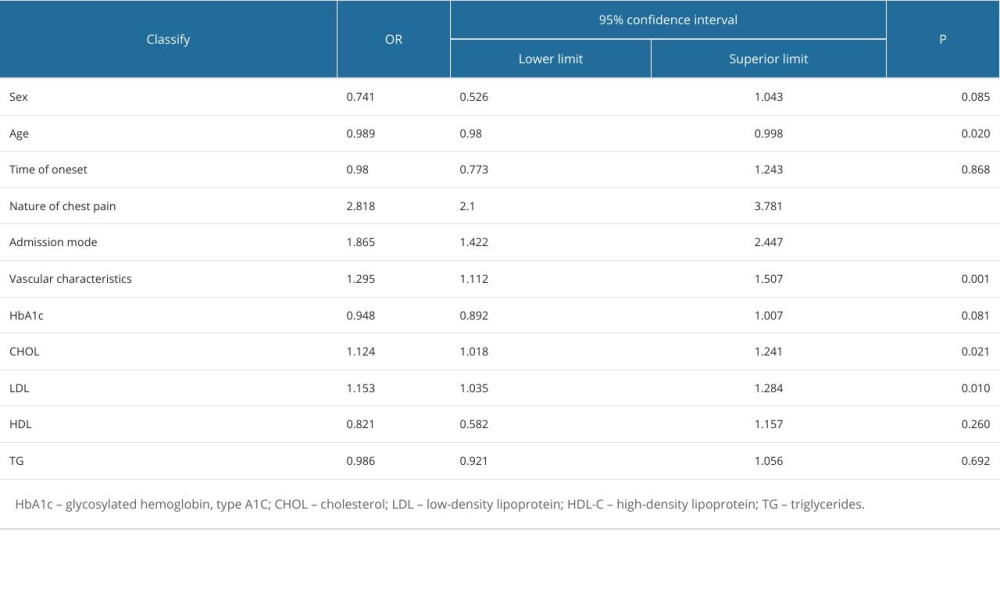 Table 2. Univariate Cox regression screening of S2FMC influencing factors.
Table 2. Univariate Cox regression screening of S2FMC influencing factors. Table 3. Multivariate Cox regression screening of S2FMC influencing factors.
Table 3. Multivariate Cox regression screening of S2FMC influencing factors.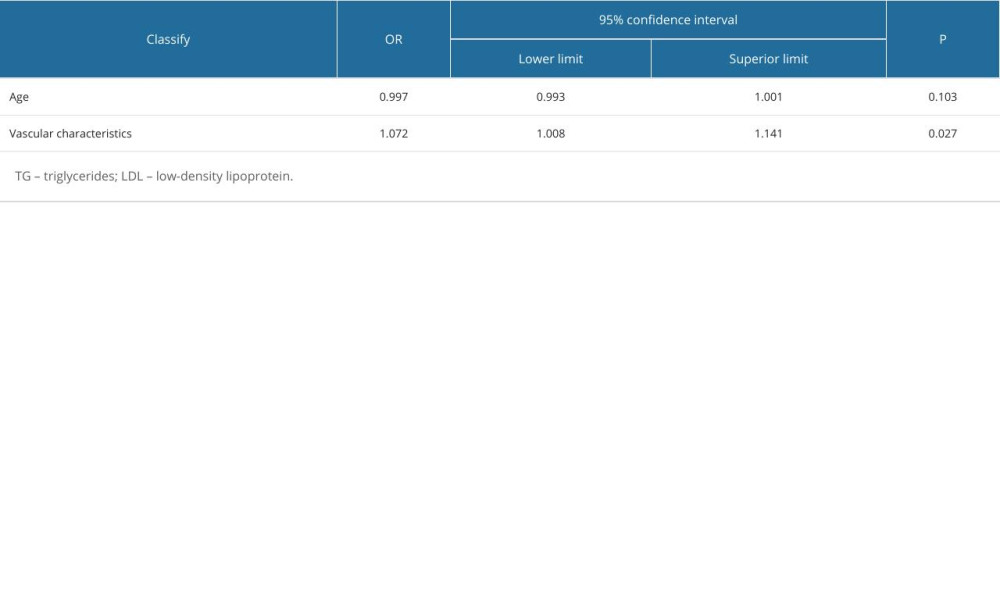 Table 4. Multivariate logistics regression screening of chest pain influencing factors.
Table 4. Multivariate logistics regression screening of chest pain influencing factors.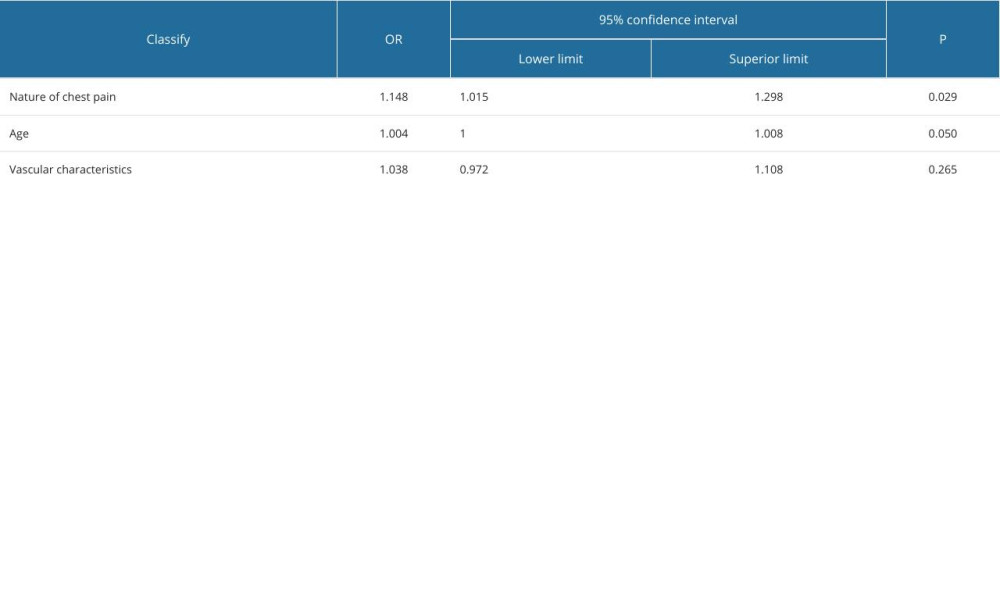 Table 5. Multivariate logistics regression screening of chest pain influencing factors.
Table 5. Multivariate logistics regression screening of chest pain influencing factors.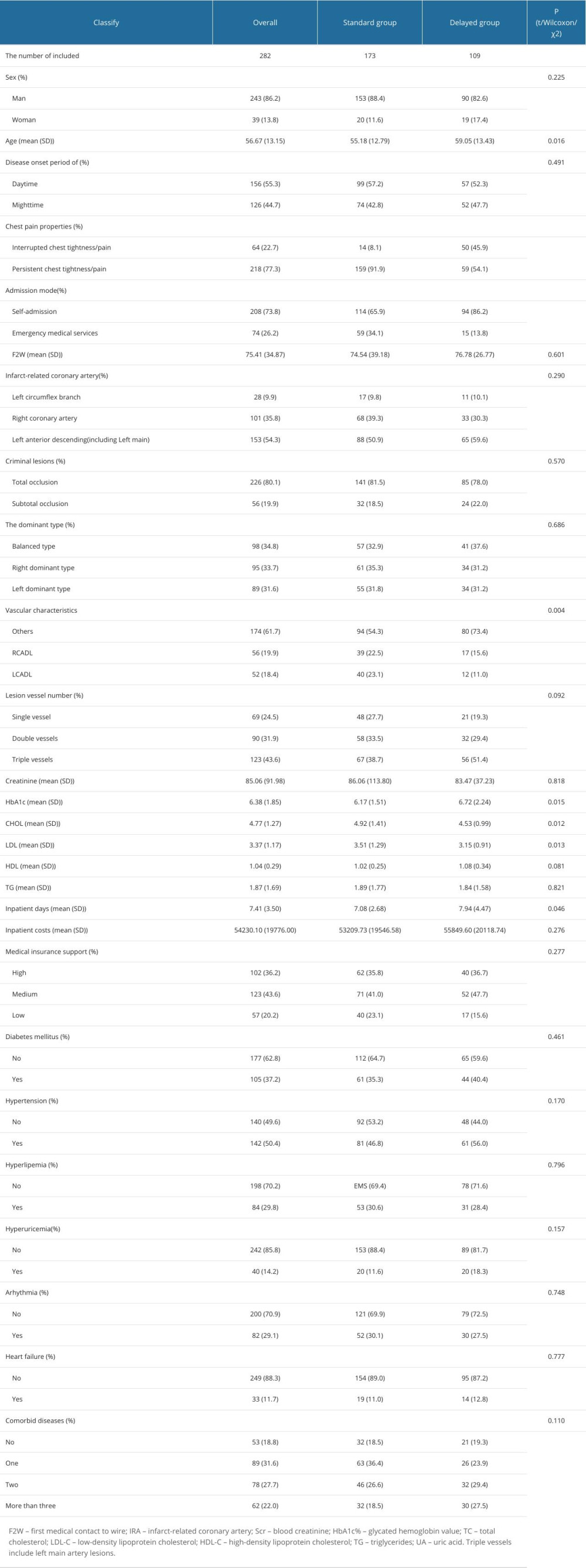 Table 1. General characteristics table.
Table 1. General characteristics table.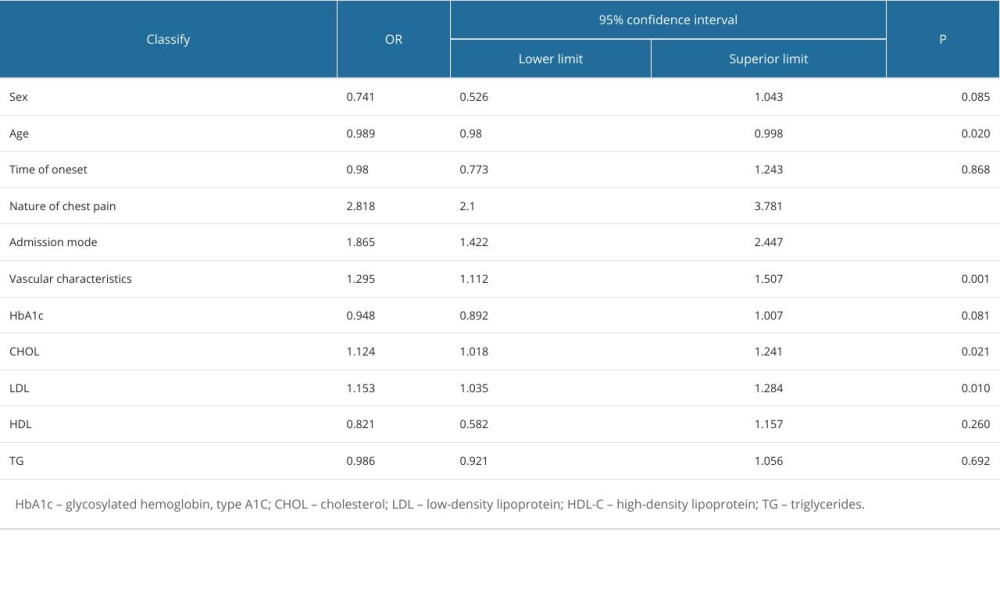 Table 2. Univariate Cox regression screening of S2FMC influencing factors.
Table 2. Univariate Cox regression screening of S2FMC influencing factors. Table 3. Multivariate Cox regression screening of S2FMC influencing factors.
Table 3. Multivariate Cox regression screening of S2FMC influencing factors.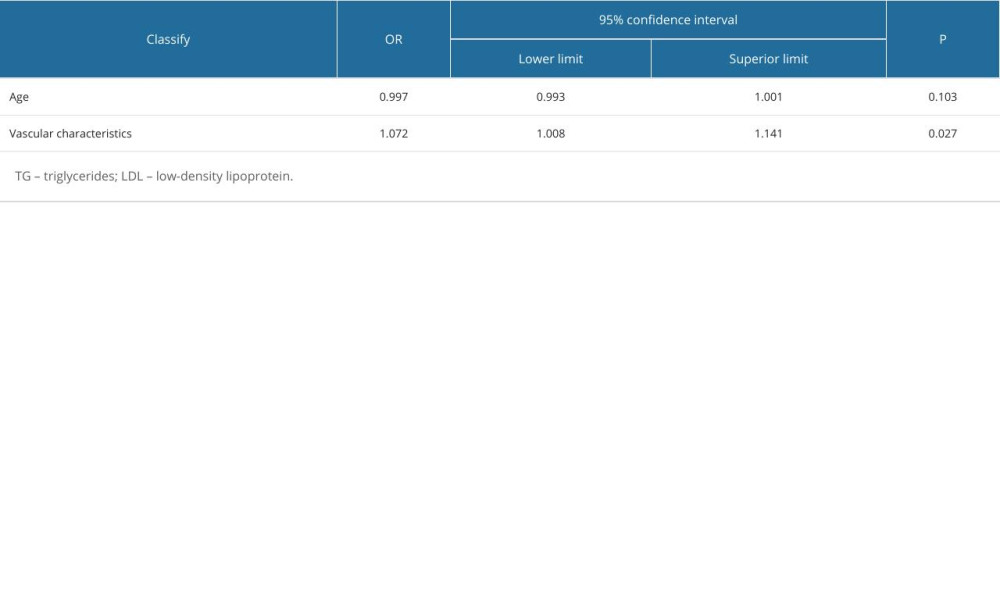 Table 4. Multivariate logistics regression screening of chest pain influencing factors.
Table 4. Multivariate logistics regression screening of chest pain influencing factors.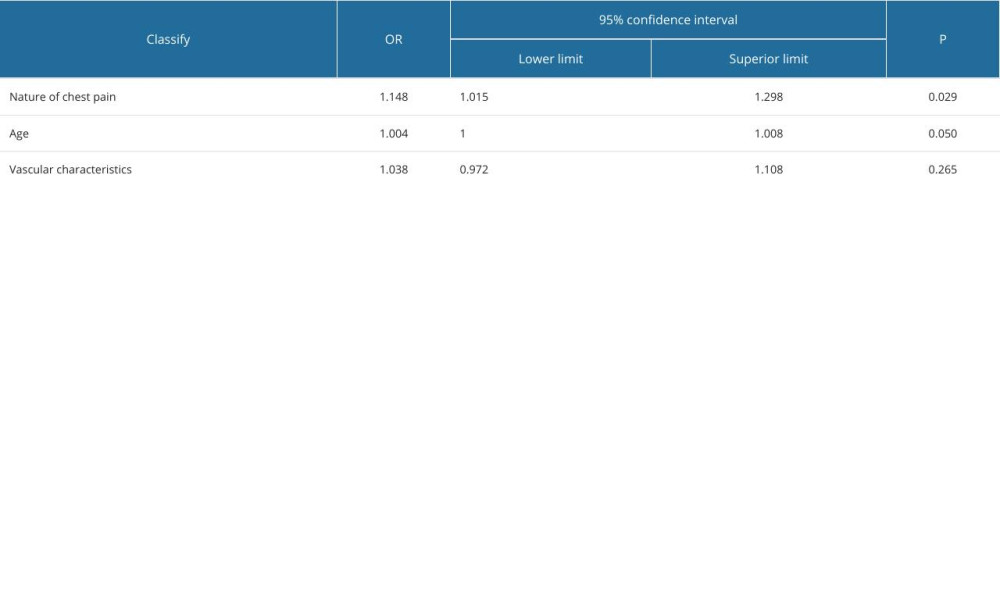 Table 5. Multivariate logistics regression screening of chest pain influencing factors.
Table 5. Multivariate logistics regression screening of chest pain influencing factors. In Press
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








