16 October 2023: Clinical Research
Comparative Study of Minimally Invasive Plate Osteosynthesis (MIPO) and Intramedullary Nailing (IMN) for Treating Extraarticular Distal Tibial Fractures: Clinical and Radiological Outcomes
Oğuz KayaDOI: 10.12659/MSM.942154
Med Sci Monit 2023; 29:e942154
Abstract
BACKGROUND: Treatment of extra-articular distal tibial fractures is problematic owing to limited soft tissue cover, poor vascularity of the location, and adjacency to the ankle, and thus continues to be controversial. This study aimed to compare clinical and radiological outcomes in 69 patients with extra-articular distal tibia fractures treated with minimally invasive plate osteosynthesis (MIPO) and an interlocking intramedullary nail (IMN).
MATERIAL AND METHODS: Sixty-nine patients, with mean of age 39.8±18.3 years, were retrospectively evaluated. Thirty-five patients were treated with IMN, and 34 patients were treated with MIPO. Clinical and radiological outcomes were evaluated.
RESULTS: The average follow-up was 13.3±6 months and union time was 16.2±5.4 weeks. Nonunion was observed in only 4.3% of patients treated with MIPO (P=0.114). Non-acceptable malalignment of extremity was observed in 4.3% of patients with IMN and 7.2% of patients with MIPO. There were no significant differences in union time, nonunion, surgical timing, operating time, malalignment, and complications between groups (P>0.05). The mean American Orthopaedic Foot and Ankle Society (AOFAS) surgery score was 95.8±5 in IMN and 91.9±14.3 in MIPO. AOFAS, Tenny-Wiss radiological, and Ovadia-Beals clinical scores were better in IMN than MIPO (P=0.019, P=0.03, P=0.02, respectively). Mean time of full weight-bearing and of return to daily life with IMN was significantly shorter than with MIPO (P<0.001).
CONCLUSIONS: IMN and MIPO methods are reliable and effective methods with similar good results in the surgical treatment of extra-articular distal tibia fractures. However, IMN may be preferred for early full weight-bearing and early return to daily life (P<0.001).
Keywords: Fracture Fixation, Intramedullary, Minimally Invasive Surgical Procedures, Tibial Fractures, intra-articular fractures, Fractures, Bone, Humans, young adult, Adult, Middle Aged, Tibia, Retrospective Studies, Treatment Outcome, Fracture Healing, Fracture Fixation, Internal, Bone Plates, Lower Extremity, Ankle Joint
Background
Extra-articular distal tibial fractures are frequently observed after high-energy injuries, but can also be observed after ankle sprains, falls, and other low-energy injuries [1]. Surgical treatment has become preferred because it allows weight-bearing and rehabilitation in the early period. The treatment of these fractures is quite problematic owing to poor blood supply, decreased anterior muscle cover, subcutaneous location, and severe soft tissue damage. Many complications such as malunion, nonunion, delayed union, and wound site problems have been reported after surgical treatment [2–5].
The choice of an appropriate surgical option in the treatment of these fractures remains controversial [5–7]. An angulation of less than 5° in anterior-posterior imaging, less than 10° of sagittal angulation, less than 1 cm of shortening and more than 50% cortical apposition are acceptable criteria for closed reduction and non-operative treatment. In the surgical treatment, external fixation (the type that includes damage-controlled orthopedics and significant soft tissue trauma), interlocking intramedullary nailing (IMN), minimally invasive plate osteosynthesis (MIPO), and amputation (can be avoided with a mangled extremity severity score of 7 or more) can be considered [1–5].
The MIPO method aims to subcutaneously advance the plate from the distal to the proximal fracture site after indirect reduction without touching the tissues in the fracture area, aiming at osteosynthesis with screws from the proximal and distal fracture, thus protecting the periosteum and blood supply [8,9].
The IMN method in intraarticular distal tibia fractures uses the percutaneous patellar tendon incision approach. IMN has become a preferred method since the tissues in the fracture area are not touched and the fracture combined with the hematoma exposed during carving increases the union [10]. However, IMN and MIPO are both effective and reliable methods.
Although the IMN and MIPO techniques are successful in maintaining reduction and promoting stable union, careful planning should be done by considering the advantages and disadvantages of both techniques [2,4,11,12]. In addition, fractures observed in the distal fibula, which is a part of the ankle mortis, should be handled with care. Any malunion or nonunion that disrupts the alignment of the ankle mortis can lead to instability and joint arthritis by disrupting the normal biomechanics of the ankle and foot [3].
Therefore, this retrospective study aimed to compare the effectiveness of MIPO and IMN in 69 patients with extraarticular distal tibial fractures.
Material and Methods
ETHICS:
Approval for the study was given by the local ethics committee of our university (2018/8–18). Data collection and evaluation was done in accordance with the Declaration of Helsinki. All patients were informed about the treatment, and their written consent was obtained.
GENERAL PATIENT DATA:
A total of 69 patients aged between 18 and 71 years who underwent surgery for extra-articular distal tibia fracture between 2014 and 2020 were retrospectively analyzed. All imaging and medical records were extracted from electronic patient records (picture archiving and communication system software) in our hospital.
The patients were divided into 2 groups according to the surgical treatment, resulting in 35 patients in the IMN group and 34 patients in the MIPO group (Figures 1, 2).
All patients underwent standard radiological evaluation including lateral and anteroposterior views at presentation and at follow-up appointments. The fractures were classified according to AO/OTA classification [13], and open fractures were classified according to the Gustilo-Anderson system [14].
INCLUSION AND EXCLUSION CRITERIA:
Skeletally mature patients with fractures lined between 4 and 12 cm from the ankle joint and type I–II open fractures were included in the study. Patients with pathologic fractures, intraarticular or type III open fractures, immunodeficiency states, and vascular injury requiring repair were excluded from the study.
SURGICAL TECHNIQUE:
All operations were performed under spinal anesthesia and using a tourniquet to control bleeding. The timing of surgery was according to the condition of the soft tissue. In some patients, the distal fibula was stabilized to improve alignment and reduction of the tibia and to provide increased stability of the lateral column of the ankle. Tibia plating was performed with a distal tibia medial anatomical locking compression plate using a less invasive stabilization system following closed reduction under C-arm fluoroscopy. Static locking intramedullary nailing was performed with the same closed reduction technique after reaming, using the percutaneous patella tendon incision approach. At least 2 screws were used distally and proximally for locking the nail. Poller screws were used for improving reduction in some fractures using IMN.
POSTOPERATIVE REHABILITATION:
No patients had a cast and splint applied after surgery. Range of motion exercises for the ankle were started with all patients and encouraged after surgery. Partial weight-bearing was usually allowed at 1 week after surgery for IMN and at 4 to 6 weeks for MIPO, according to the stability of the fixation. The decision concerning full weight-bearing was made on an individual patient basis, depending on the condition of union and pain.
FUNCTIONAL AND RADIOLOGICAL ASSESSMENT:
All patients were evaluated clinically and radiologically at postoperative week 2, months 1, 2, 3, and 6, and at the last follow-up. Bone union was defined as the lack of tenderness at fracture location, painless weight-bearing, and callus of 3 of the 4 cortices on radiographs. Failure of bone union at 6 months was defined as delayed union, and the lack of bone union at 9 months was defined as nonunion. Malalignment was defined as varus/valgus deformity more than 5° in the coronal plane, anterior/posterior angulation (recurvatum or procurvatum) greater than 10° in the sagittal plane, a rotational deformity greater than 10°, and shortening >10 mm on postoperative antero-posterior and lateral X-rays [2,15,16]. The radiological assesment used the Tenny-Wiss score. The American Orthopaedic Foot and Ankle Society (AOFAS) surgery score and Ovadia-Beals clinical scoring system (objective and subjective evaluation) were used to evaluate the function of the ankle at the last follow-up [17,18]. Furthermore, the operating time, surgical timing, union time, time to hospital stay, full weight-bearing, return to daily life, malalignment, nonunion, wound problems, and other complications were evaluated at follow-up.
STATISTICAL ANALYSIS:
All statistical analyses were performed with SPSS version 16.0 (IBM Corp, Armonk, NY, USA). According to Kolmogorov-Smirnov, Shapiro-Wilk, and Levene Statistic tests applied to analyze the homogeneity and normal distribution of the findings of the study, all study findings were homogeneous and had a normal distribution in the groups (
Results
This study included 69 patients (range, 18–89 years) with a mean age of 39.8±18.26 years. There was no statistically significant difference in terms of age, extremity side, and sex between the IMN and NIPO groups (
The mean period of follow-up was 13.3±6.0 (range, 6–36) months. The mean time from injury to surgery was 2.86±3.5 (range, 1–21) days. There was no statistically significant difference in terms of surgical timing, operating time, follow-up period, and union time between the 2 groups (
The mean time to union was 16.2 (range, 10–28) weeks. The mean times of full weight-bearing and return to daily life in the IMN group were significantly shorter than that of the MIPO group (30.8 vs 55.0 and 61.28 vs 91.32 days, respectively;
There was no significant difference in the effect of fracture type and injury mechanism on clinical and radiological outcomes (
Non-acceptable malalignment of extremity was present in 3 patients in the IMN group and in 5 patients in the MIPO group, but there was no significant difference (
Nonunion was observed in 3 patients who underwent MIPO, and these patients had recurvatum and valgus deformity due to poor reduction, and distal fibula fixation was performed in 2 of them. Revision with open reduction and plate osteosynthesis was performed in 2 patients, while revision with IMN was performed in 1 patient, and all of them achieved bone union.
In 2 of our patients, iatrogenic fracture in the posterior cortex of the proximal tibia was observed while inserting the nail intramedullary. Additional fixation was made with an external fixator in only 1 patient and the other patient was stable. Skin necrosis was observed in 2 patients with distal fibula fixation, which was likely due to swelling and circulatory disturbance. There was no statistically significant difference in complications between the groups (Table 2).
Distal fibular fracture was observed in 34 (49.3%) patients. Distal fibula fractures were fixed in 7 of the patients treated with IMN and 21 of the patients treated with MIPO. The effect of fixation of the fibula on the union of the distal tibia fracture was not statistically significant between the groups (
Gustilo type 1 or 2 open fractures were observed in 11 patients, and there was no statistically significant difference between the IMN and MIPO groups (
The mean AOFAS score was 95.82±5.02 in the IMN group and 91.88±14.34 in the MIPO group. There was a statistically significant difference between the 2 groups (
Discussion
In our study, we evaluated surgical timing, operation time, follow-up time, effect of fibula fixation on distal tibial fracture union, time of fracture union, fracture type and injury mechanism in the treatment of distal tibial fractures and compared clinical and radiological results between IMN and MIPO groups. There was no statistically significant difference between the groups in terms of incidence rate, Ovadia-Beals Pain scores, and all complications. Mean AOFAS score, Tenny-Wiss radiological scores, and Ovadia-Beals Clinical scores were better in the IMN group than in the MIPO, and a statistically significant difference was found.
There continues to be controversy in choosing the best option of surgical treatment between the MIPO and IMN techniques for the treatment of extra-articular distal tibial fractures [4,12]. Treatment of these fractures is problematic owing to limited soft tissue cover, poor vascularity of the location, and adjacency to the ankle [4,11,19]. The main purpose of surgical treatment is to restore the anatomical alignment of the tibia by providing sufficient stability to allow early mobilization, minimize the soft tissue and bony devascularization, and reduce complications [4,11,19,20].
In many comparative studies, IMN and MIPO techniques are well-accepted, reliable, and effective biological fixation methods in the treatment of distal tibial fractures. However, these studies indicate different advantages over the treatment options [2,11,12,21–23]. Daolagupu et al [11] reported a short operating time, early weight bearing, rapid union, low incidence of infection, and less implant irritation and failure in the IMN group than in the plate group. Kumbaracı et al [22] stated that MIPO had less union delay and angular deformity than did IMN, but the MIPO group had wound problems and worse functional outcomes. Kariya ve et al [2] reported that IMN can be preferred in terms of early mobilization because it is stronger than the plate in terms of axial loading. Likewise, in the study of Hu et al, IMN was found to be superior in terms of functional improvement of the ankle and reduction of postoperative wound superficial infection; they also found no difference in delayed union and that IMN was worse in terms of malunion [24].
In the study of Kho et al, the AOFAS score was higher in the IMN group, that is, better recovery was observed, and postoperative complications were significantly lower after 12 months [25].
Kang et al [23] reported IMN could be preferred because of less soft tissue dissection, better healing rate, and early return to daily life. In our study, we found functionally and radiologically similar results between both groups (Table 2). However, Tenny-Wiss radiological scores and Ovadia-Beals Clinical scores were better in the IMN group than in the MIPO group. The mean time of full weight-bearing and of return to daily life in the IMN group was significantly shorter than in the MIPO group.
Many meta-analyses have indicated that the 2 treatment options have similar results and are suitable for the treatment of extraarticular distal tibia fracture [26–28]. However, He et al [26] reported that low-quality evidence comparing these 2 treatment options shows that, compared with IMN, the MIPO technique is associated with a shorter fracture recovery time, reduced rate of delayed union, and lower pain level. Yu et al [27] stated that IMN may be advantageous in the treatment of tibial distal fractures owing to its low incidence of superficial infection, compared with that of MIPO; however, IMN is associated with a high risk of malunion. In their review study, Li et al [29], reported that IMN should be given priority for extra-articular tibial fractures with serious soft tissue injuries.
The time between injury and surgery is slightly longer in patients treated with MIPO because surgeons tend to delay surgery with plating to avoid catastrophic complications, such as compartment syndrome and serious wound problems [2]. Beytemur et al [21] reported 7 (19.4%) superficial infections and 1 deep infection (2.8%) in the MIPO group and 3 superficial infections (8.1%) in the IMN group. In our study, the surgical timing was slightly shorter in the IMN group than in the MIPO group, but there was no statistically significant difference. Surgical timing depends on concomitant fractures as well as on the condition of the soft tissue. Although no skin problems were observed in the IMN group, cutaneous necrosis was observed in 2 patients in the MIPO group. We think that surgical intervention should be postponed in patients with serious soft tissue problems to avoid compartment syndrome, cutaneous necrosis, and soft tissue infection.
Kariya et al [2] found a higher duration of surgery and radiation exposure in the MIPO group than in the IMN group. They stated that this was due to the increased use of C-arms to achieve indirect reduction in the MIPO group. In the present study, although the operating time was slightly shorter in the IMN than in the MIPO, there was no statistically significant difference. Unfortunately, radiation exposure is one of the limitis of our study.
Kc et al [4] reported the rate of nonunion was 2% for MIPO and 6% for IMN. In our study, nonunion was observed in only 3 (4.3%) patients who underwent MIPO. We think the cause of nonunion is inadequate reduction and non-compliance with surgical principles rather than the MIPO technical option.
There is no consensus on the detection of distal fibula fractures accompanying distal tibial fractures. Fibular fixation aids reduction by correcting rotational aligment and increases the chance of union, but it also prevents cyclic loading of the tibia, which is essential for union [2,11,30]. Kariya et al [2] reported that fixation of the fibula has no impact on the functional outcome of distal tibia fractures. Fixation of the fibula should not be applied routinely but should be preferred for only specific fracture patterns, such as spiral oblique and segmented tibia fractures. In a randomized prospective study, Vallier et al [30] reported that fixation of the distal fibula facilitated the anatomical reduction of the tibia, but they observed a tendency for tibial nonunion. In our study, nonunion was observed in 3 (4.3%) patients, and distal fibula fixation had performed in 2 of them. Therefore, we think the effect of fixation of the distal fibula on fracture union and aligment should be investigated in a randomized controlled study with a large sample size.
The alignment of malunion was not emphasized in the studies. Beytemur et al [21] found more valgus alignment with IMN and more recurvatum with MIPO. They indicated that the increased valgus malalignment may be caused by the absence of fibula fixation, and the recurvatum deformity may be caused by pressing calcaneus to the operating table during surgery. Giacomo et al [15] reported that malalignment is more common in patients with fractures of the tibia and fibula at the same level. They observed that the fixation of the fibula fracture accompanying to distal tibial fractures treated with IMN increased the rate of nonunion despite the correction of the aligment. Yaligod et al [3] stated that nailing should be advanced to the subchondral bone after good reduction and the nail should be fixed by placing multiple distal locking screws, which was performed to avoid the malunion and reduce complications observed in IMN. In the present study, non-acceptable malalignment of extremity was present in 3 patients in the IMN group and in 5 patients in the MIPO group, but there was no significant difference between groups. All patients with nonunion had recurvatum and valgus deformity due to poor reduction, and distal fibula fixation was performed in 2 of them. We think that the most important factor to prevent the malalignment is anatomic fracture reduction rather than fixation of the distal fibula. In particular, in patients treated with IMN, due to the wide distal part, auxiliary procedures, such as the weber reduction clamp and poler blocking screw, should be applied to facilitate reduction, and the distal part should be well stabilized.
Prolonged hospital stays cause increased healthcare costs. Li et al [31] reported that the length of hospital stay was significantly shorter in the IMN group than in the plating group, and stated that this caused a decrease in hospital costs. We think that IMN is more advantageous in terms of cost effectiveness, because of shorter hospital stays.
The limitations of our study were the retrospective design, the small number of patients, and the fact that fibula fixation was not performed on every patient. Prospective, randomized conttolled studies with larger sample size are needed to confirm the results of this study.
Conclusions
The controversy continues regarding the best surgical technique to be used in the treatment of extra-articular distal tibial fractures. Although there are similar results between percutaneous plating and nailing, in this study, IMN seemed more advantageous than MIPO in terms of early weight bearing and early return to work.
Figures
 Figure 1. (A) Preoperative and (B) postoperative plain radiographic views of an extraarticular distal tibial fracture treated with interlocking intramedullary nailing (IMN).
Figure 1. (A) Preoperative and (B) postoperative plain radiographic views of an extraarticular distal tibial fracture treated with interlocking intramedullary nailing (IMN).  Figure 2. (A) Preoperative and (B) postoperative plain radiographic views of a extraarticular distal tibial fracture treated with minimally invasive plate osteosynthesis (MIPO).
Figure 2. (A) Preoperative and (B) postoperative plain radiographic views of a extraarticular distal tibial fracture treated with minimally invasive plate osteosynthesis (MIPO). Tables
Table 1. Demographic characteristics of the interlocking intramedullary nailing (IMN) and minimally invasive plate osteosynthesis (MIPO) groups.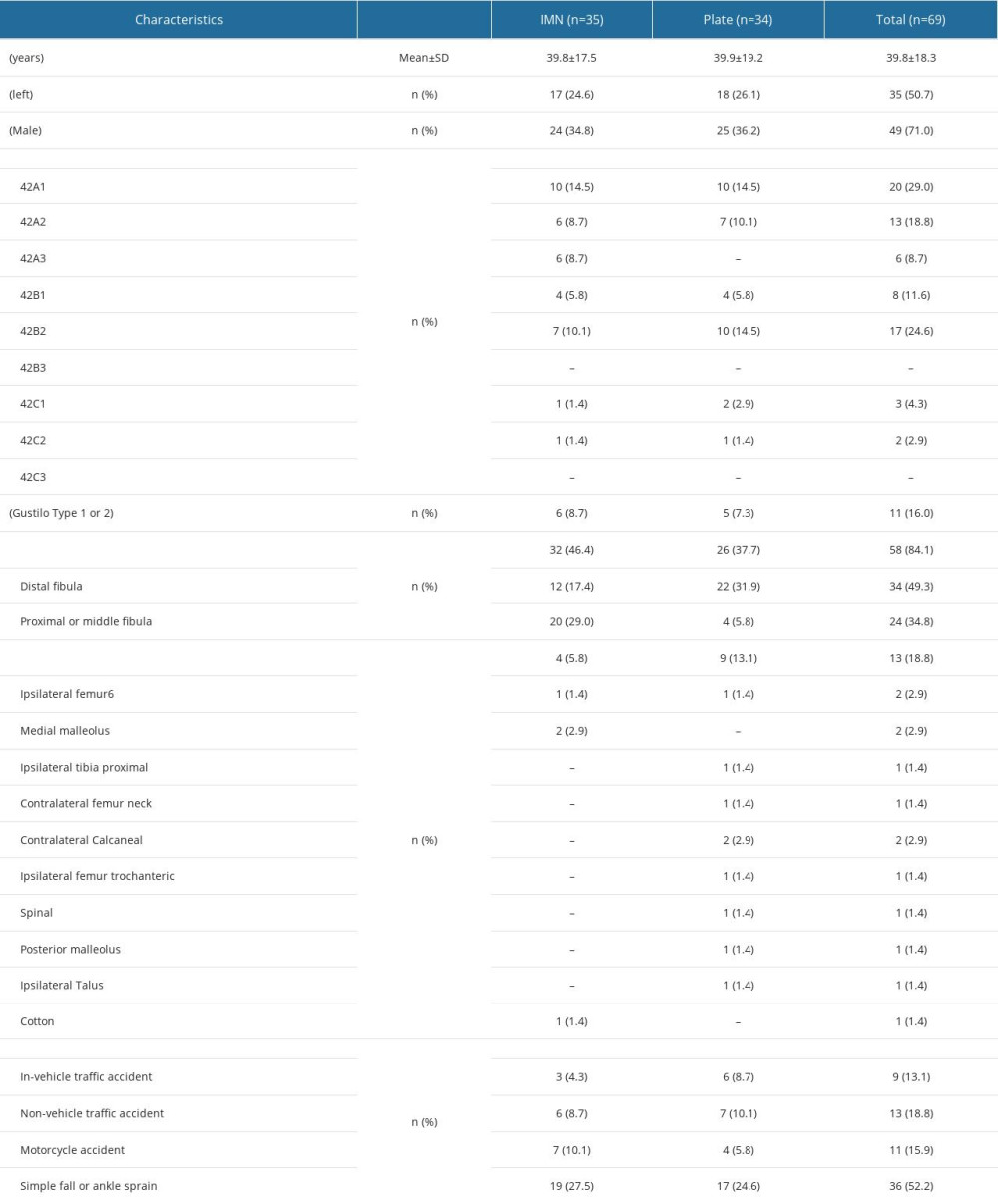 Table 2. Comparison of the results of the interlocking intramedullary nailing (IMN) and minimally invasive plate osteosynthesis (MIPO) treatment methods.
Table 2. Comparison of the results of the interlocking intramedullary nailing (IMN) and minimally invasive plate osteosynthesis (MIPO) treatment methods.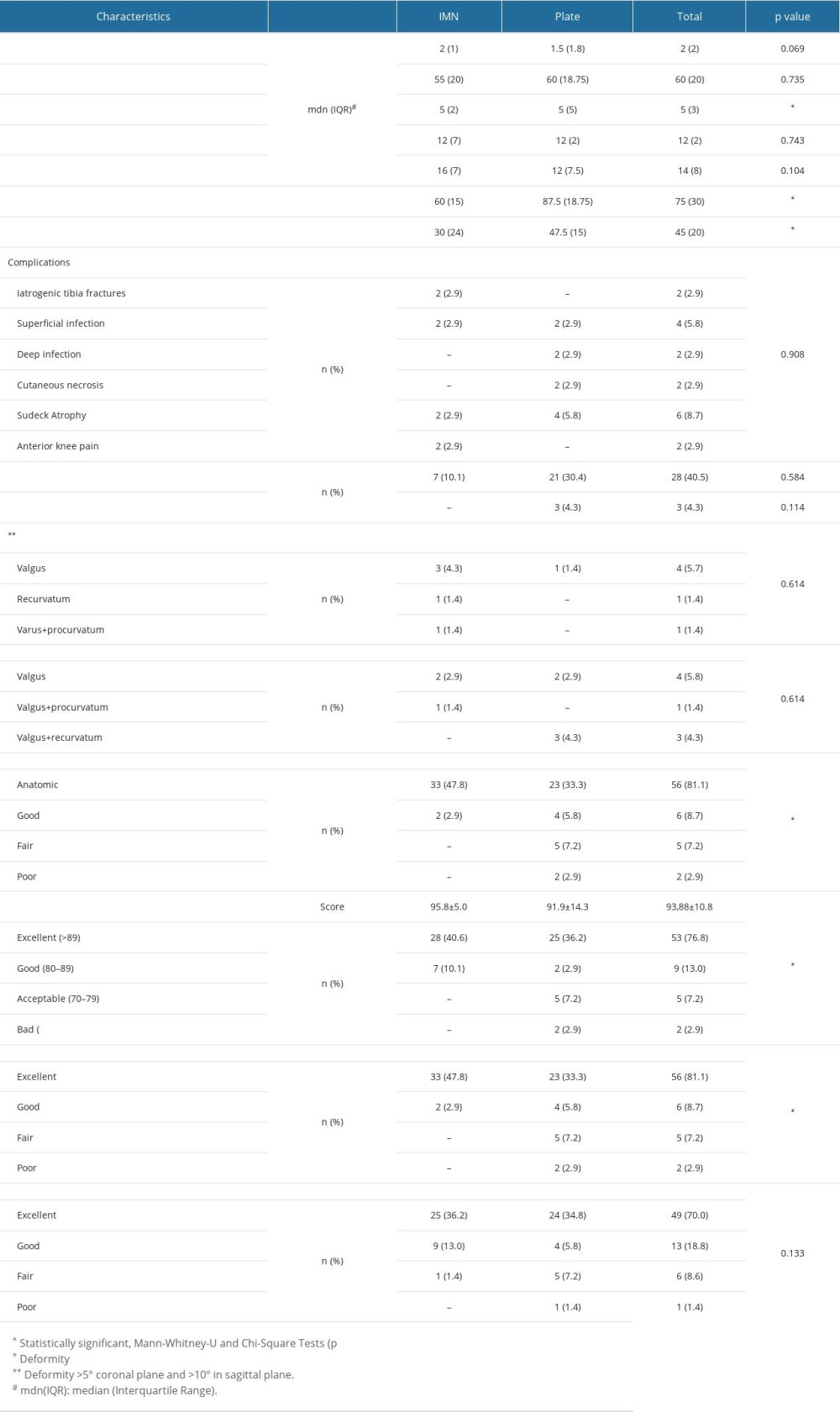
References
1. Thompson JH, Koutsogiannis P, Jahangir A, Tibia fractures overview. [Updated 2023 Jul 31]: StatPearls [Internet], 2023, Treasure Island (FL), StatPearls Publishing Available from: https://www.ncbi.nlm.nih.gov/books/NBK513267/
2. Kariya A, Jain P, Patond K, Mundra A, Outcome and complications of distal tibia fractures treated with intramedullary nails versus minimally invasive plate osteosynthesis and the role of fibula fixation: Eur J Orthop Surg Traumatol, 2020; 30(8); 1487-98
3. Yaligod V, Rudrappa GH, Nagendra S, Shivanna UM, Minimizing the complications of intramedullary nailing for distal third tibial shaft and metaphyseal fractures: J Orthop, 2013; 11(1); 10-18
4. Kc KM, Pangeni BR, Marahatta SB, Sigdel A, Kc A, Comparative study between intramedullary interlocking nailing and minimally invasive percutaneous plate osteosynthesis for distal tibia extra-articular fractures: Chin J Traumatol, 2022; 25(2); 90-94
5. Casstevens C, Le T, Archdeacon MT, Wyrick JD, Management of extra-articular fractures of the distal tibia: Intramedullary nailing versus plate fixation: J Am Acad Orthop Surg, 2012; 20(11); 675-83
6. Vallier HA, Current evidence: Plate versus ıntramedullary nail for fixation of distal tibia fractures in 2016: J Orthop Trauma, 2016; 30(Suppl 4); S2-S6
7. Mahmood A, Kumar G, Review of the treatment of distal tibia metaphyseal fractures; plating versus intramedullary nailing: A systematic review of recent evidence: Foot Ankle Surg, 2014; 20(2); 151
8. Krackhardt T, Dilger J, Flesch I, Fractures of the distal tibia treated with closed reduction and minimally invasive plating: Arch Orthop Trauma Surg, 2005; 125(2); 87-94
9. Sourougeon Y, Barzilai Y, Haba Y, Outcomes following minimally invasive plate osteosynthesis (MIPO) application in tibial pilon fractures – a systematic review: Foot Ankle Surg, 2023 [Online ahead of print]
10. Wong Wei Kang N, Tan WPJ, Phua YMC, Intramedullary nail: the past, present and the future – a review exploring where the future may lead us: Orthop Rev (Pavia), 2021; 13(2); 25546
11. Daolagupu AK, Mudgal A, Agarwala V, Dutta KK, A comparative study of intramedullary interlocking nailing and minimally invasive plate osteosynthesis in extra articular distal tibial fractures: Indian J Orthop, 2017; 51(3); 292-98
12. Wang B, Zhao Y, Wang Q, Minimally invasive percutaneous plate osteosynthesis versus intramedullary nail fixation for distal tibial fractures: A systematic review and meta-analysis: J Orthop Surg Res, 2019; 14(1); 456
13. Meinberg EG, Agel J, Roberts CS, Fracture and dislocation classification compendium – 2018: J Orthop Trauma, 2018; 32(Suppl 1); S1-S170
14. Marsh JL, Slongo TF, Agel J, Fracture and dislocation classification compendium – 2007: Orthopaedic Trauma Association classification, database and outcomes committee: J Orthop Trauma, 2007; 21(10 Suppl); S1-S133
15. De Giacomo AF, Tornetta P, Alignment after ıntramedullary nailing of distal tibia fractures without fibula fixation: J Orthop Trauma, 2016; 30(10); 561-67
16. Liu XK, Xu WN, Xue QY, Liang QW, Intramedullary nailing versus minimally ınvasive plate osteosynthesis for distal tibial fractures: A systematic review and meta-analysis: Orthop Surg, 2019; 11(6); 954-65
17. Kumar N, Thakur M, Kashyap S, Evaluation of functional outcome of distal tibial fractures stabilized with distal tibial locking plate: Int J Res Orthop, 2021; 7; 39-43
18. Ashok Kumar P, Palla A, Shah HM, Radiological and functional assessment of the tibial pilon fractures treated by Ilizarov external fixation: Int J Orthop Sci, 2017; 3(4); 427-31
19. Mushtaq A, Shahid R, Asif M, Maqsood M, Distal tibial fracture fixation with locking compression plate (LCP) using the minimally ınvasive percutaneous osteosynthesis (MIPO) technique: Eur J Trauma Emerg Surg, 2009; 35(2); 159-64
20. Barcak E, Collinge CA, Metaphyseal distal tibia fractures: A cohort, single-surgeon study comparing outcomes of patients treated with minimally ınvasive plating versus ıntramedullary nailing: J Orthop Trauma, 2016; 30(5); e169-e74
21. Beytemür O, Barış A, Albay C, Comparison of intramedullary nailing and minimal invasive plate osteosynthesis in the treatment of simple intra-articular fractures of the distal tibia (AO-OTA type 43 C1–C2): Acta Orthop Traumatol Turc, 2017; 51(1); 12-16
22. Kumbaracı M, Savran A, Comparison of minimally invasive plate osteosynthesis and intramedullary nailing in the treatment of distal extraarticular tibial fractures: Ege Tıp Dergisi, 2021; 60(3); 288-95
23. Kang H, Rho JY, Song JK, Comparison between intramedullary nailing and minimally invasive plate osteosynthesis for tibial shaft fractures: Injury, 2021; 52(4); 1011-16
24. Hu L, Xiong Y, Mi B, Comparison of intramedullary nailing and plate fixation in distal tibial fractures with metaphyseal damage: A meta-analysis of randomized controlled trials: J Orthop Surg Res, 2019; 14(1); 30
25. Kho DW, Kim HJ, Kim BJ, Choi SM, Intramedullary nailing as an alternative to plate fixation in patients with distal fibular fracture: Orthop Traumatol Surg Res, 2020; 106(1); 149-54
26. He GC, Wang HS, Wang QF, Effect of minimally invasive percutaneous plates versus interlocking intramedullary nailing in tibial shaft treatment for fractures in adults: A meta-analysis: Clinics (Sao Paulo), 2014; 69(4); 234-40
27. Yu J, Li L, Wang T, Intramedullary nail versus plate treatments for distal tibial fractures: A meta-analysis: Int J Surg, 2015; 16(Pt A); 60-68
28. Lin ZQ, Zhang HZ, Luo GG, Comparison of 3 treatment methods for distal tibial fractures: a network meta-analysis: Med Sci Monit, 2019; 25; 7480-87
29. Li B, Yang Y, Jiang LS, Plate fixation versus intramedullary nailing for displaced extra-articular distal tibia fractures: A system review: Eur J Orthop Surg Traumatol, 2015; 25(1); 53-63
30. Vallier HA, Cureton BA, Patterson BM, Randomized, prospective comparison of plate versus intramedullary nail fixation for distal tibia shaft fractures: J Orthop Trauma, 2011; 25(12); 736-41
31. Li Y, Liu L, Tang X, Comparison of low, multidirectional locked nailing and plating in the treatment of distal tibial metadiaphyseal fractures: Int Orthop, 2012; 36(7); 1457-62
Figures
 Figure 1. (A) Preoperative and (B) postoperative plain radiographic views of an extraarticular distal tibial fracture treated with interlocking intramedullary nailing (IMN).
Figure 1. (A) Preoperative and (B) postoperative plain radiographic views of an extraarticular distal tibial fracture treated with interlocking intramedullary nailing (IMN). Figure 2. (A) Preoperative and (B) postoperative plain radiographic views of a extraarticular distal tibial fracture treated with minimally invasive plate osteosynthesis (MIPO).
Figure 2. (A) Preoperative and (B) postoperative plain radiographic views of a extraarticular distal tibial fracture treated with minimally invasive plate osteosynthesis (MIPO). Tables
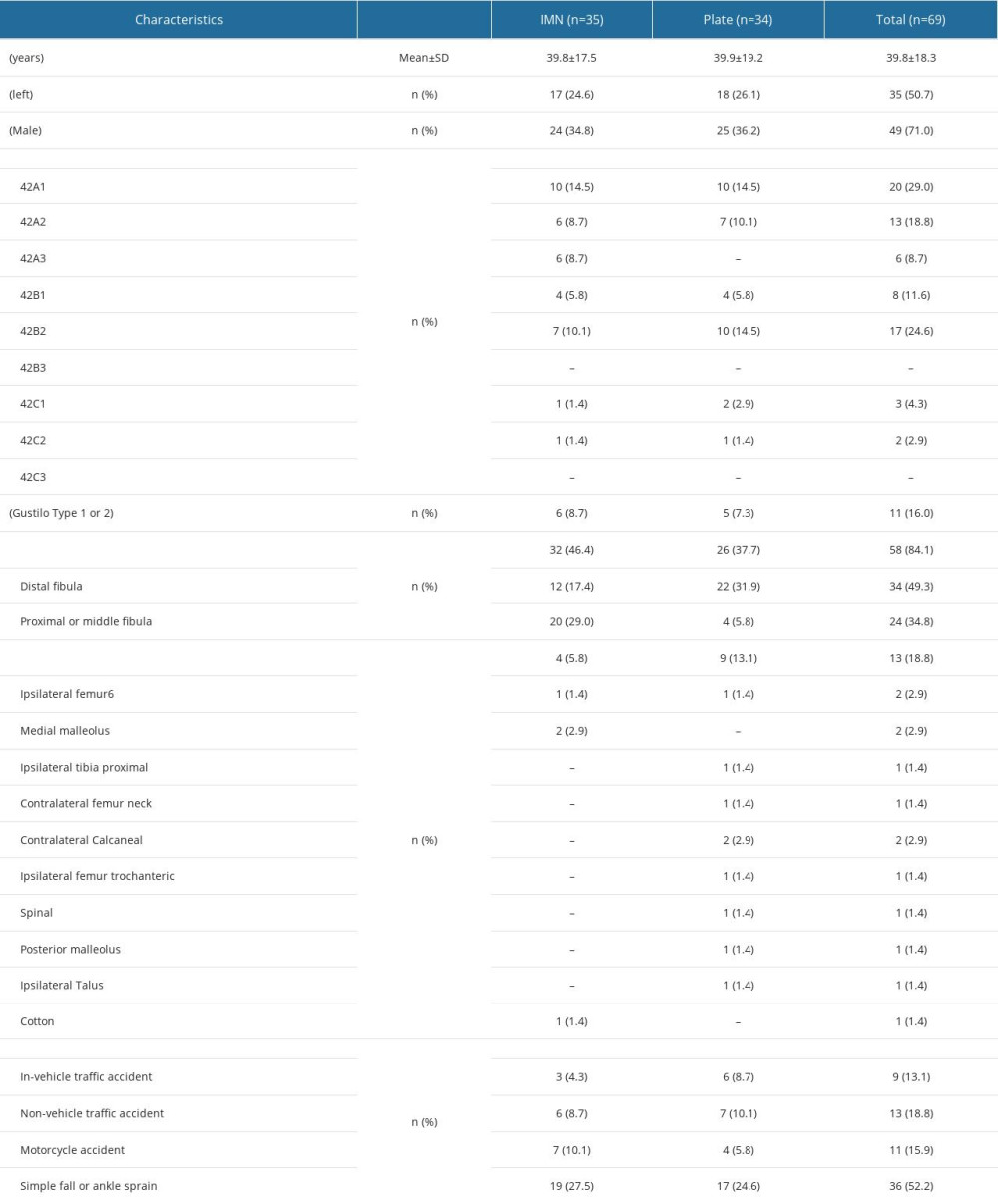 Table 1. Demographic characteristics of the interlocking intramedullary nailing (IMN) and minimally invasive plate osteosynthesis (MIPO) groups.
Table 1. Demographic characteristics of the interlocking intramedullary nailing (IMN) and minimally invasive plate osteosynthesis (MIPO) groups.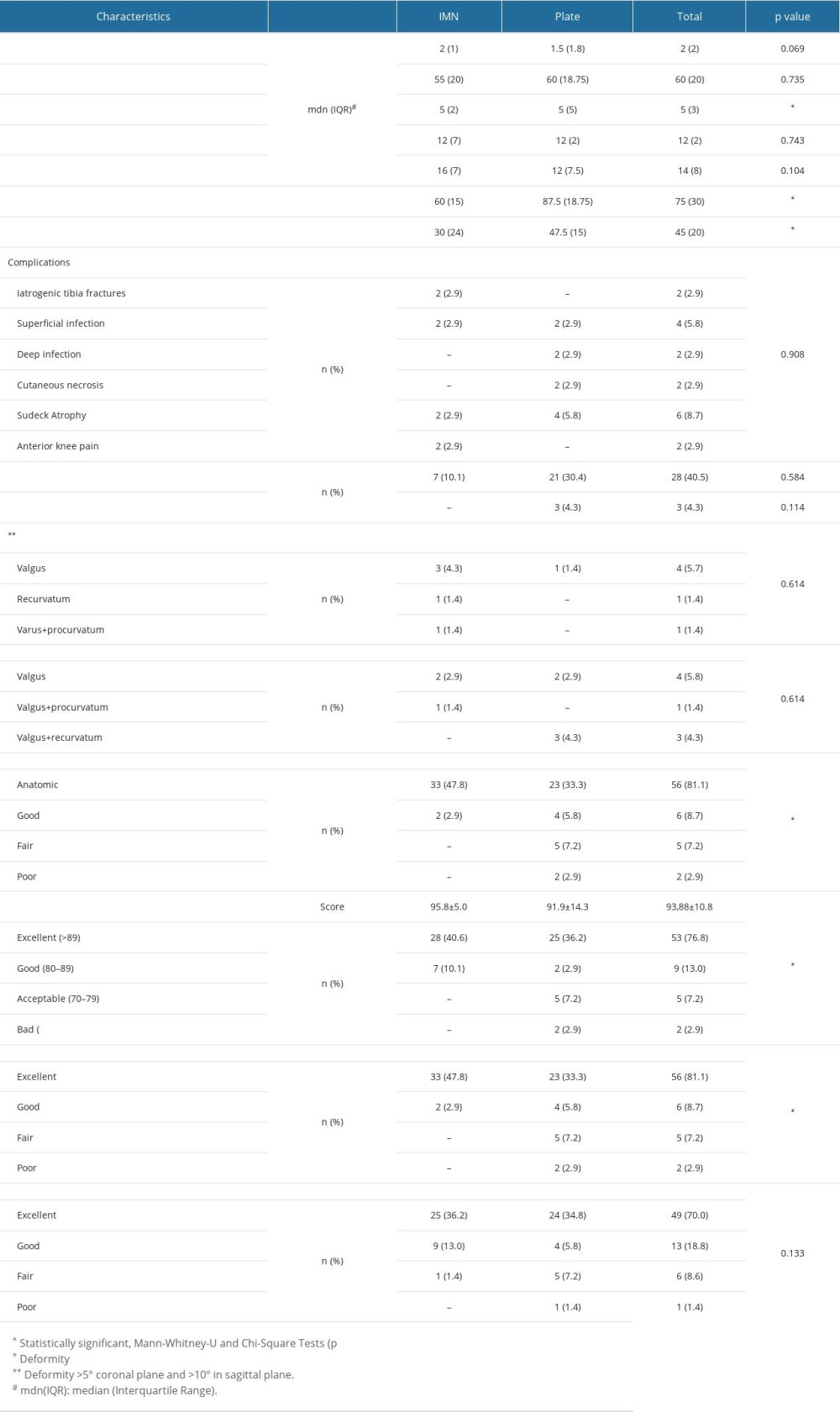 Table 2. Comparison of the results of the interlocking intramedullary nailing (IMN) and minimally invasive plate osteosynthesis (MIPO) treatment methods.
Table 2. Comparison of the results of the interlocking intramedullary nailing (IMN) and minimally invasive plate osteosynthesis (MIPO) treatment methods.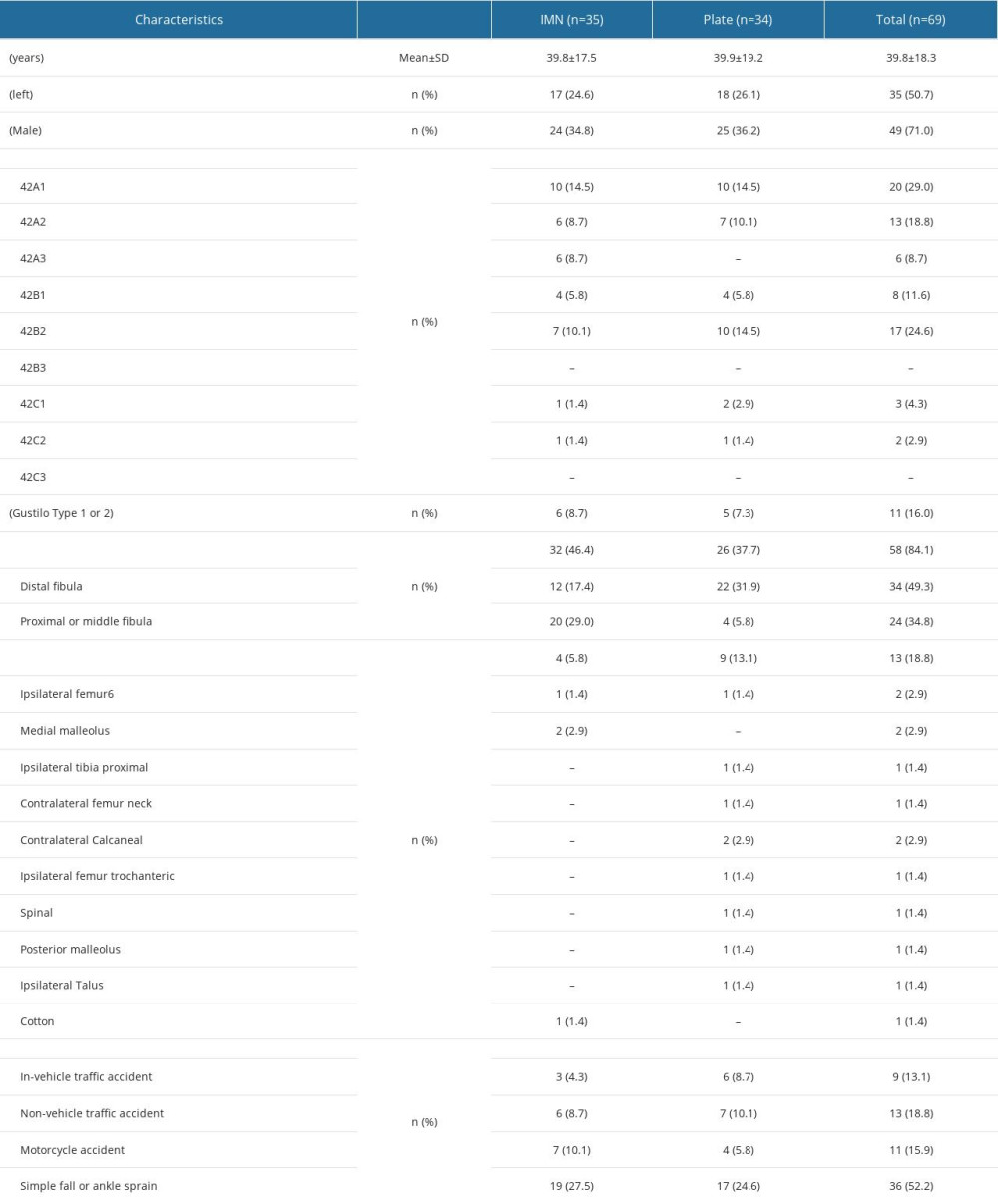 Table 1. Demographic characteristics of the interlocking intramedullary nailing (IMN) and minimally invasive plate osteosynthesis (MIPO) groups.
Table 1. Demographic characteristics of the interlocking intramedullary nailing (IMN) and minimally invasive plate osteosynthesis (MIPO) groups.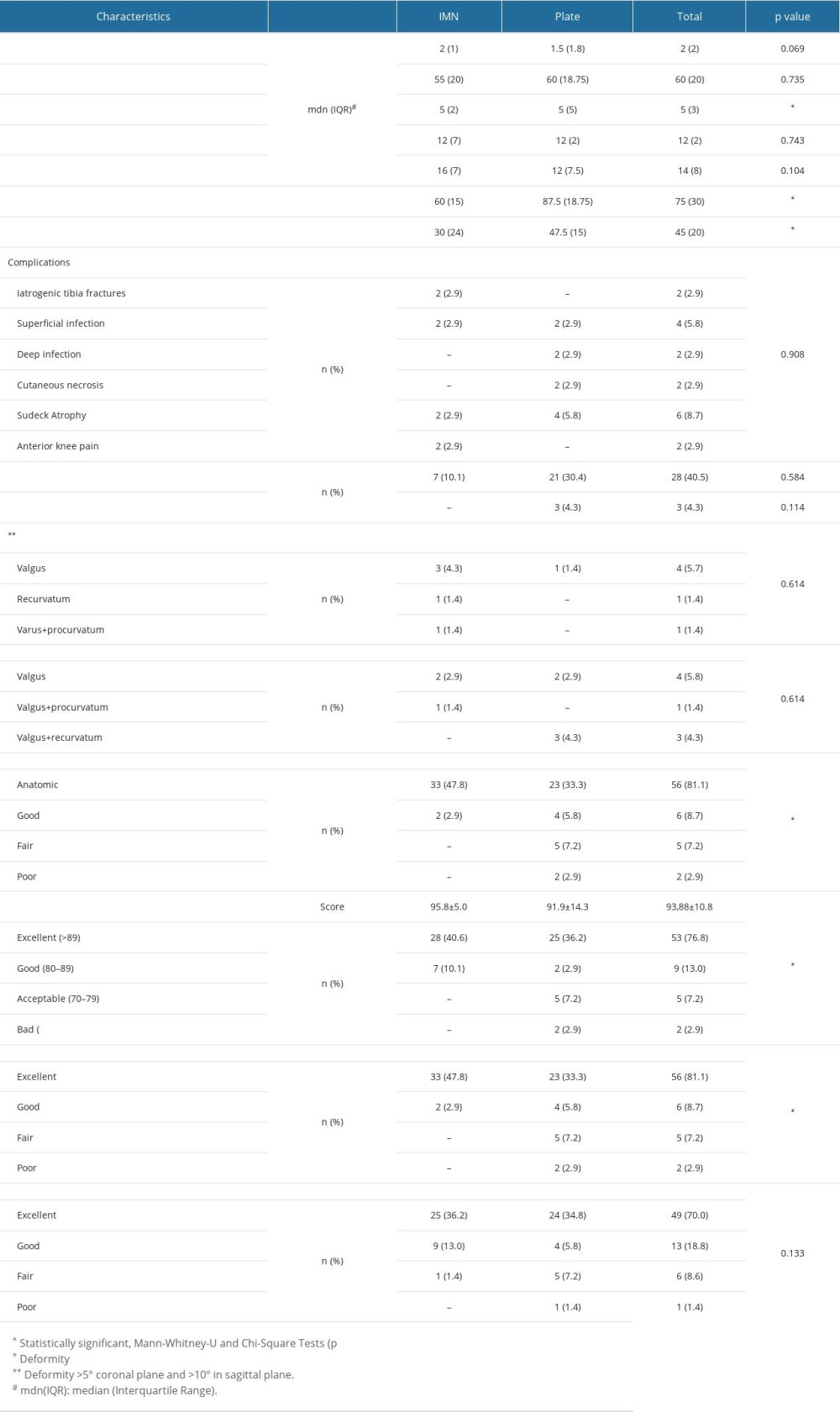 Table 2. Comparison of the results of the interlocking intramedullary nailing (IMN) and minimally invasive plate osteosynthesis (MIPO) treatment methods.
Table 2. Comparison of the results of the interlocking intramedullary nailing (IMN) and minimally invasive plate osteosynthesis (MIPO) treatment methods. In Press
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
12 Mar 2024 : Clinical Research
Tissue Inhibitors of Metalloproteinase 1 (TIMP-1) and 3 (TIMP-3) as New Markers of Acute Kidney Injury Afte...Med Sci Monit In Press; DOI: 10.12659/MSM.943500
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








