22 February 2024: Clinical Research
Effectiveness of Glutamine Oral Care in Reducing Oral Mucositis and Improving Oral Health After Neurosurgery: A Randomized Controlled Trial with Microbiome Analysis
Yan Gao1DE, Hong Yang1B, Xiaohong Zhang1C, Ying Ma1DF, Ling Wang1AE*DOI: 10.12659/MSM.942585
Med Sci Monit 2024; 30:e942585
Abstract
BACKGROUND: Hospital-acquired infections negatively impact the health of inpatients and are highly costly to treat. Oral care reduces the microorganism number in the mouth and lungs and is essential in preventing postoperative oral inflammation, lung infection, and other complications. This study was designed to determine the effects of oral care with glutamine on oral health, oral flora, and incidence of pneumonia in patients after neurosurgery.
MATERIAL AND METHODS: This was a parallel, double-blind, randomized trial. Patients admitted to the Neurosurgery Department of the hospital from July to October 2021 were selected. Three hundred patients who met the inclusion criteria were randomized into 3 groups. The control group (n=100) received oral care with routine oral nursing methods with saline, whereas the experimental group (n=100) received oral care with 5% glutamine. A compound chlorhexidine group (n=100) was set as a positive control. All patients, care providers, and investigators were blinded to the group assignment. The incidence of local debris, oral mucositis, halitosis, dryness, oral mucositis disorders, and oral flora types were collected and analyzed in all groups.
RESULTS: The incidence of local debris, oral mucositis, halitosis, dryness, and other oral mucositis disorders in the glutamine oral care group was significantly decreased, compared with that of the control group. Oral flora types in the glutamine and chlorhexidine groups were significantly reduced.
CONCLUSIONS: Oral care with 5% glutamine after neurosurgery is associated with a lower incidence of oral disorders and pneumonia, and a significant reduction in oral flora.
Keywords: Glutamine, Inflammation, Neurosurgery, Nursing Research
Background
It has been well acknowledged that hospital-acquired infections significantly negatively impact the health of inpatients, are highly costly to treat, and result in clinical deterioration, escalation of preventable hospital admissions, increased mortality, and greater cost of care, particularly for older people in residential care; however, hospital-acquired infections are preventable [1]. Oral care effectively reduces the number of microorganisms in the mouth and lungs and is essential in preventing postoperative oral inflammation, lung infection, and other complications [2,3].
Patients undergoing neurosurgery are frail and mostly stay in bed with conditions such as hemiplegia or coma after surgery, with sputum drainage disorder [4]. Neurosurgical patients mostly require mechanical ventilation in order to sustain postoperative respiratory needs. Under such a circumstance, they are often placed on bedrest and are not able to participate in mobility exercises, until extubated. Moreover, invasive operations, such as endotracheal intubation and general anesthesia, are commonly used in neurosurgery patients for treatment, which increases the risk of pulmonary infection [5,6]. It is reported that patients with brain injury are particularly susceptible to ventilator-associated pneumonia (VAP), with the incidence ranging from 22% to 71% [7]. For long-bedridden patients, especially comatose patients, their saliva secretion and oral self-cleaning ability are significantly reduced [8]. Theiroral cavity hygiene worsens, with the number of bacteria excessively increasing, leading to bacterial colonization, including
Many studies focus on the inadequate oral care that causes microbial accumulation; the standard oral care includes brushing the teeth with a toothpaste once a day and mouth washing with rinse solution [3,12]. Solutions for oral care vary among studies. As a dental plaque inhibitor, chlorhexidine is used for the treatment of gingivitis. There is a large body of literature suggesting that oral care is effective in the prevention of VAP. In patients undergoing cardiac surgery, oral rinsing with chlorhexidine was reported to reduce the incidence of VAP by a factor of 0.56, compared with no rinsing [13]. A study of 12 randomized controlled trials by Labeau et al showed a similar reduction in the incidence of VAP, of 0.72-fold [14]. Mouth rinses containing chlorhexidine are helpful in improving oral hygiene care because chlorhexidine has been found to be effective in decreasing the amount of dental plaque and in reducing certain aerobic and anaerobic species [15]. Özçaka et al found VAP to be less frequent in chlorhexidine-treated patients than in patients receiving saline solution oral care [16]. In the study by Berry et al, the incidence of VAP in patients using saline solution and chlorhexidine was 1% and 0.2%, respectively [17]. Another study on mechanically ventilated patients found that the Clinical Pulmonary Infection Score (CPIS) was higher in patients who had their teeth brushed than in patients who used chlorhexidine [18]. The adverse reactions of current oral care include mainly oral mucosal injury, foreign body swallowing, allergies, painless superficial desquamation damage, tooth discoloration, and taste disorders. Hydrogen peroxide and sodium bicarbonate are effective for removing debris but if not appropriately diluted, lead to superficial burns. Glutamine is an essential amino acid for protein synthesis and regulation of nitrogen transport [19]. As a substrate for glutathione synthesis, glutamine can offer raw material for mucous membrane healing. Immune cells, such as macrophages, are critical in mucosal barrier defenses and mucosal repair of oral injuries due to mechanical and inflammatory factors. Owing to its role in fueling leukocytes, oral glutamine may be helpful in mucosal healing not only by its direct effect on the mucosal epithelial cells but also by the improvements in mucosal immune function and the ability to resist various microbial invasions. Studies have shown that moderate and severe oral mucositis can be reduced by 20% in patients receiving gastric tumor chemotherapy after the local application of glutamine [20]. After reviewing 8 studies, including 6 randomized controlled trials, Sharron et al recommend glutamine oral care to mitigate oral mucositis [21]. On reviewing various studies, we have determined that there is a need for evidence-based studies on cost-effective and practical oral solutions with fewer adverse effects. Studies on glutamine oral cleaning are limited, and randomized control trials with large samples are rare, especially in neurosurgery patients with a high risk of oral and lung infections. There is a need for high-quality studies with large sample sizes to reduce heterogeneity and examination of the cost-effectiveness of glutamine oral care. Therefore, we designed this study to evaluate the effects of glutamine in oral care on preventing oral inflammation and lung infection in patients after neurosurgery. We also provided guidance and references for clinical nurses to select targeted oral care methods.
Material and Methods
STUDY AIMS:
We aimed to determine the effects of oral care with glutamine on oral health, oral flora, and incidence of pneumonia in patients who have undergone neurosurgery. Oral health complications, such as local debris, oral mucositis, and halitosis rates, were analyzed to estimate oral health conditions. Oral microbiomes play an important role in the human microbial community, and oral health and accumulated evidence links poor oral health status with an increased risk of pneumonia, which can be caused by bacterial pathogens in the mouth [22]; therefore, we also included oral flora and pneumonia incidence into the analysis.
GENERAL INFORMATION:
A total of 324 patients, aged 35 to 55 years, who were hospitalized for more than 48 h after surgery in the Neurosurgery Department of the hospital from July to October 2020 and who met the inclusion criteria were included as study participants. The study was approved by the hospital ethics board. A total of 300 patients met the inclusion/exclusion criteria and were divided into 3 groups: the control group (100 patients), glutamine group (100 patients), and the chlorhexidine group (100 patients), using an encoded program system provided by a third party. Inclusion criteria were the following: (1) patients with a diagnosis of neurosurgical disease confirmed by computed tomography or magnetic resonance imaging and who were scheduled for surgery; (2) no pneumonia or oral infection was found before the surgery (before inclusion in the study, all patients underwent a chest X-ray and oral examination to find any signs of infection. Patients with fever, cough, and sputum or suspected cases were also excluded); and (3) patients agreed to sign the informed consent before the surgery and volunteered to participate in the project. Exclusion criteria were the following: (1) diagnosis of pneumonia on admission; (2) patients undergoing chemotherapy or patients with immune deficiency; (3) patients with severe coma and inability to gargle autonomously; (4) patients who died before discharge; (5) patients allergic to chlorhexidine; and (6) patients who declined to participate in the study. The general demographic data of the groups were analyzed using one-way ANOVA, showing no significant differences in variables including age, length of hospital stay, sex, diagnosis, and smoking status (
STUDY DESIGN:
All patients received oral care from senior and skilled nurses who had been working in the Neurosurgery Department ward for more than 5 years.
Patients in the control group received traditional oral care twice daily (morning and night), including oral rinse, swab, and topical decontamination with 0.9% saline, according to the instructions. The oral care steps were as follows. (1) Patients were asked to sit fully upright or in an elevated side-lying position to prevent aspiration during mouth cleaning. (2) Any existing dentures were removed. The treatment towel was spread under the jaw, and the mouth was wet. (3) The teeth and mouth were rinsed with saline 0.9% solution for 150 to 180 s, and the condition of the oral cavity was checked. (4) The teeth were brushed with a suction toothbrush (or soft toothbrush) with toothpaste for 180 s, ensuring all 4 quadrants were cleaned. (5) A swab was dipped into a standard 0.9% saline oral rinse. (6) The mouth was cleaned with the swab for 150 to 180 s. (7) The hard palate, tongue, and the bottom of the tongue were cleaned with a swab for 150 to 180 s. (8) The mouth and lips were wiped for 20 to 30 s. Finally, (9) patients were asked about their feelings about the whole care process, and the oral condition was checked (for example, whether it was clean, any residues left, bleeding, or ulcer) with a flashlight.
In the glutamine group, saline 0.9% solution was replaced by a diluted mouthwash solution with 5 mL glutamine injection (Kelun Pharmaceutical, National drug approval H20043702) and 95 mL normal saline (normal temperature) to rinse and swab the mouth of the patients each time. The nursing method and sequence were the same as with the traditional oral care with saline, as described above.
In the chlorhexidine group, oral care was conducted by rinsing the mouth with 0.2% chlorhexidine twice daily after the teeth were brushed [23]. A description of the study is shown in Figure 1.
RANDOMIZATION AND BLINDING:
Because smoking is a risk factor of oral disorders, the patients were stratified based on their smoking status and then randomized by a member of the research team who was not involved in patient follow-up to the control group (100 patients), glutamine group (100 patients), and chlorhexidine group (100 patients). Stratified randomization was used for grouping. The patient was first allocated to the strata according to the diagnosis, then the group was determined through simple randomization applied to the strata. For simple randomization, each patient received a random sequence number enclosed in a sealed envelope from the researcher. The numbers were allocated to each group using an encoded program system provided by a third party (https://www.random.org). To improve adherence to the oral care regimen, an evidence-based practice education program was implemented, and a checklist of all procedures was used to document adherence to oral care (Table 1). All nurses must have completed every step in the table to maintain uniformity across the study. The design of the study was a barrier to blinding the patients; therefore, to reduce bias, all patients were educated and told all oral care methods were proven effective to a certain extent. The workers in charge of data analysis and outcome evaluation were kept blinded to the groups to which the patients were allocated.
OUTCOME EVALUATION:
Several team members measured the outcome indicators to evaluate the effects of the different treatments. The primary outcome indicators were the incidence of oral inflammation and pneumonia.
Oral health: The oral condition, including of the mouth and the teeth, was checked. Lips, teeth, gums, inside cheeks, tongue, and mucosa of the floor of mouth and palate were checked to note if there was any food, coating, bleeding, dryness, edema, redness, or other debris. The nurses also checked whether there was oral thrush accumulating on the lining of the mouth; bad breath and dry mouth; pain or discomfort in oral care; and any wound or ulcer in the mouth. A questionnaire was also used to evaluate the patients’ oral condition (Table 2).
Oral flora: The existence of bacteria at different sites of the mouth was determined using a previously reported method [24]. Oral cavity culture samples were collected by rolling a sterile, flocked swab in the mouth for 5 s, avoiding contact with facial hair. The swab was brought into contact with all areas of the oral cavity (tooth surfaces, dorsal and lateral tongue surfaces, buccal epithelium, and hard palate). After the sampling procedure, the oral cavity was thoroughly examined. Baseline specimens were collected 4 h before surgery. Oral flora specimens were then obtained in the same manner 24 h after oral care. All specimens were sent daily to the microbial laboratory to identify the types and colonization of flora. The isolated bacteria after oral care were compared with those isolated before surgery, from the saliva of the same patients.
Pneumonia: The diagnosis of pneumonia was made by reviewing patients’ medical history, physical examination, and tests, and was determined by evaluating the patients’ conditions with the CPIS, to confirm the condition based on the criteria of hospital-acquired pneumonia and ventilator-associated pneumonia [25] as follows: (1) new cases that developed 24 h after surgery; (2) clinical symptoms and signs such as cough, fever, and/or lung turbidity and dullness; X-ray showed infiltrating shadows in the lungs; and (3) at least 1 of the following: pathogenic bacteria detected in an exhalation of tracheae, such as expectoration of pus or sputum, blood culture, or bronchial brush specimen; positive serum antibody; and pneumonia detection based on histopathology. Briefly, the detection criteria included temperature, volume of respiratory secretions, white blood cells, infiltration in the chest radiograph, and secretion culture results. The radiography results were interpreted by a respiratory physician blinded to the procedure. The CPIS was 0 to 10, and a score of 6 or higher indicated the incidence of pneumonia, as confirmed in different studies [18]. The scores of all groups were evaluated by a respiratory physician blinded to the study procedure.
ETHICAL CONSIDERATIONS:
The ethics committee of the hospital approved this study (No. XJODCT2020001). Written consent was also obtained from all patients who had agreed to participate. All staff who participated in the study had appropriate practices to ensure data security. Training was essential, since it had a beneficial relationship with the opinions, views, and actions of staff. Thus, planning continuous training on policies and regulations about data safety and privacy may have assisted in improving healthcare setting practices, safeguarding participant confidentiality and data security. The trial was conducted in compliance with the institutional review board regulations in accordance with the Helsinki Declaration of 1975 as revised in 1983 and was registered as NCT03867214 at
STATISTICAL ANALYSIS:
SPSS19.0 software was used for data processing. Data were described using means and standard deviations for quantitative variables and percentages for qualitative variables. In the descriptive analysis, we calculated frequencies and percentages for qualitative variables, and measures of central tendency and 95% confidence intervals for quantitative variables. In demographic characteristics analysis, one-way ANOVA test was used to assess homogeneity between the groups for measurement data (age, length of hospital stay, and body mass index), while the chi-square test and Fisher’s exact test were used for enumeration data (sex, diagnosis, smoke, hypertension, and alcohol use). All data were tested to ensure they met the assumptions for the inferential statistical analyses. To determine the efficacy of oral care on each objective, we performed the following analysis: (1) oral disorders: the chi-square test and Fisher’s exact test were used; (2) bacterial colonization: one-way ANOVA was used; (3) incidence of pneumonia: one-way ANOVA was used for CPIS analysis, while the chi-square test and Fisher’s exact test were used for incidence comparison. Tukey post hoc analysis or Bonferroni post hoc analysis were used to evaluate differences between groups.
Results
DEMOGRAPHIC CHARACTERISTICS:
A total of 324 patients were selected, of which 7 patients did not give consent to initiate or continue the study. A further 17 patients were excluded for not meeting the inclusion criteria. Hence data were analyzed from the remaining 300 eligible patients: 100 patients in the control group, 100 in the glutamine group, and 100 in the chlorhexidine group (Figure 1). The demographic variables of the study sample are summarized in Table 3. Apart from the 7 patients who declined to participate, 4 patients had a diagnosis of pneumonia on admission, and 2 patients were undergoing chemotherapy. One patient died before discharge and 3 patients were allergic to chlorhexidine. These conditions might have affected the results of the study, and therefore the patients were excluded. Among excluded patients, 11 were women and 13 were men. Ten were diagnosed with cerebral hemorrhage, 6 with brain tumor, and 8 with brain trauma. Thirteen were smokers and 14 had hypertension. Nine were alcohol users. The average body mass index of the excluded patients was 24.6.
COMPARISON OF ORAL DISORDERS:
No significant differences were observed between the 3 groups in demographic and clinical conditions, as shown in Table 2. The 3 groups were treated with different oral cleaning solutions as indicated, while the procedure, frequency, and duration of each step remained the same, which reduced bias brought by other factors. Oral care with rinsing and swab cleaning reduced local debris and eliminated possible triggers of oral disorders. The data showed that both the glutamine group and chlorhexidine group were superior to the control group in terms of local debris (38 in the control group, 14 in the glutamine group, and 12 in the chlorhexidine group), oral mucositis (52 in the control group, 23 in the glutamine group, and 22 in the chlorhexidine group), and halitosis (46 in the control group, 23 in the glutamine group, and 21 in the chlorhexidine group). Oral health improved in the glutamine and chlorhexidine groups (P<0.001). The incidence of dryness had no significant difference among groups, as shown in Table 4 (P=0.528). Questionnaire score analysis showed that the scores of the control group were lower than the scores of the other 2 groups (Figure 2).
COMPARISON OF ORAL BACTERIAL COLONIZATION:
More than 20 taxonomic types of flora were identified, including staphylococci, streptococcus, Pseudomonas aeruginosa, and Veillonella. Almost all specimens tested positive for flora. Bacteria isolated from the mouth of the patients after oral care was significantly reduced, compared with that before the surgery. All flora types in the 3 groups were then compared across different time points (data after oral care/data before the surgery). The mean of flora types was 0.91 in the control group, 0.83 in the glutamine group, and 0.81 in the chlorhexidine group at baseline. Compared with the control group, flora types of the glutamine and chlorhexidine groups were significantly reduced (Figure 3). Oral flora was concentrated in dental plaque. In patients undergoing neurosurgery, the potential pathogens from the oral cavity were also found. Microorganisms in the mouth also translocated to the lung and resulted in ventilator-associated pneumonia. Oral care, especially on the teeth, reduced oral microbial flora via oral care in these patients, in mechanical or pharmacological approaches. Since all groups were subjected to the same oral care procedures, including frequency and duration of each step, the differences in bacterial colonization were the results of differentiated oral care solutions.
COMPARISON OF THE INCIDENCE OF PNEUMONIA BETWEEN THE 2 GROUPS:
Microorganisms in the mouth translocate to the lung and result in ventilator-associated pneumonia in various ways in patients undergoing neurosurgery. Thus, the incidence of pneumonia is closely related with oral health. Therefore, we detected the incidence of pneumonia in these patients. After all the patients were treated with different oral cleaning methods, 24 patients in the control group developed acute respiratory tract infections, and no patients died. In the glutamine group, 8 patients had a respiratory infection, and no patients died. Six patients in the chlorhexidine group developed respiratory infections, and none had dangerous conditions. The numbers of patients with a new lung infection in the glutamine and chlorhexidine groups were significantly lower than that in the control group. The scores of all the groups were also analyzed, as shown in Table 5. These results were consistent with the results of oral microbial flora analysis. As previously stated, the reduced incidence of pneumonia was most likely related to the reduced flora in the mouth. Oral care with glutamine and chlorhexidine rinsing and swab cleaning significantly reduced incidence of pneumonia.
Discussion
LIMITATIONS:
The limitations of this study include its small size and lack of exploration of underlying mechanisms, which is planned to be further discussed and practiced in future studies. The variations in methodologies, including heterogeneity in patient populations, outcomes, and assessment methods, which can bring potential biases, limited our discussion and can affect the generalizability of the study. Another limitation was the intervention time, which was limited to 3 days, and the follow-up data collection was also limited. Thus, in the next study, we will conduct a prolonged intervention to explore further long-term clinical outcomes, such as length of hospital stay and a larger, more diverse sample size, covering the major proportion of neurosurgery patients. Moreover, future studies should also use more specific outcome evaluations, such as oral mucous membrane integrity, mucosal score, and plaque score index, as well as the oral health-related quality of life scale to detect the oral condition in various aspects.
Conclusions
In conclusion, this study demonstrated that 5% glutamine used in oral care was effective in reducing the incidence of pneumonia in patients after neurosurgery, highlighting its potential as a valuable addition to perioperative care. However, the findings also indicated that glutamine’s effectiveness was comparable to that of compound chlorhexidine oral care, without showing superior results in terms of oral disorders, CPIS, and pneumonia incidence. This suggests that while glutamine is a viable alternative, especially considering its lower adverse effect profile, it does not necessarily offer enhanced benefits over existing chlorhexidine treatments in the context of preventing pneumonia.
Given these findings, future research with larger sample sizes and more diverse patient populations is recommended to further elucidate the comparative effectiveness of glutamine and chlorhexidine in oral care. Additionally, considering that current studies have focused on the effects of glutamine on radiation-induced oral mucositis or Intensive Care Unit patients, exploring the long-term effects of glutamine on oral health, its potential benefits in different types of surgical patients, and a deeper investigation into its mechanisms of action would contribute significantly to the field of postoperative care and patient recovery. Recent studies have reported the role of the oral flora in neuropsychiatric disorders, and the result of our flora analysis is also a hint that glutamine may mitigate neuropsychiatric disorders by affecting oral flora. In conclusion, this study lays the groundwork for further investigations and underscores the importance of continuous exploration in the realm of oral care interventions in clinical settings.
Figures
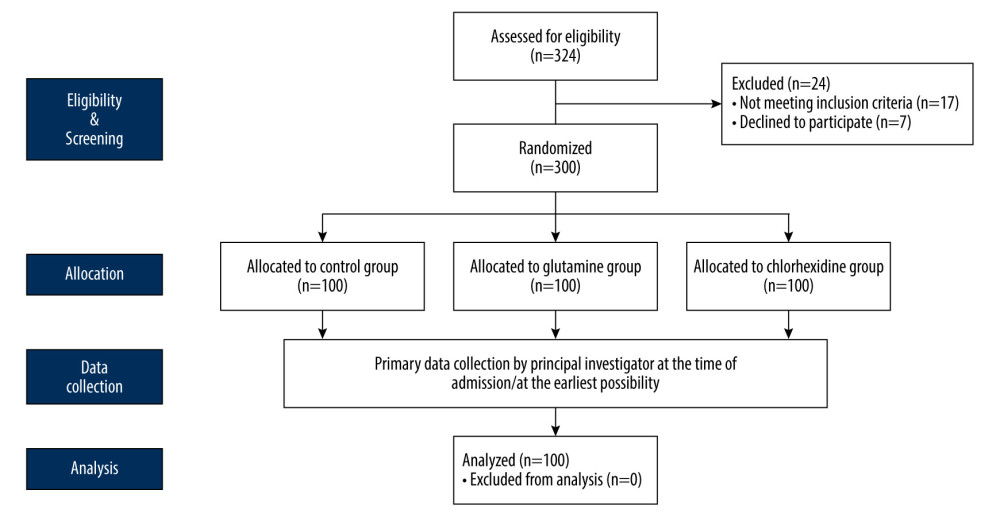 Figure 1. Diagrammatic algorithm of participant flow. (Drawn with Adobe Illustrator, 2020, 24.2.1.).
Figure 1. Diagrammatic algorithm of participant flow. (Drawn with Adobe Illustrator, 2020, 24.2.1.). 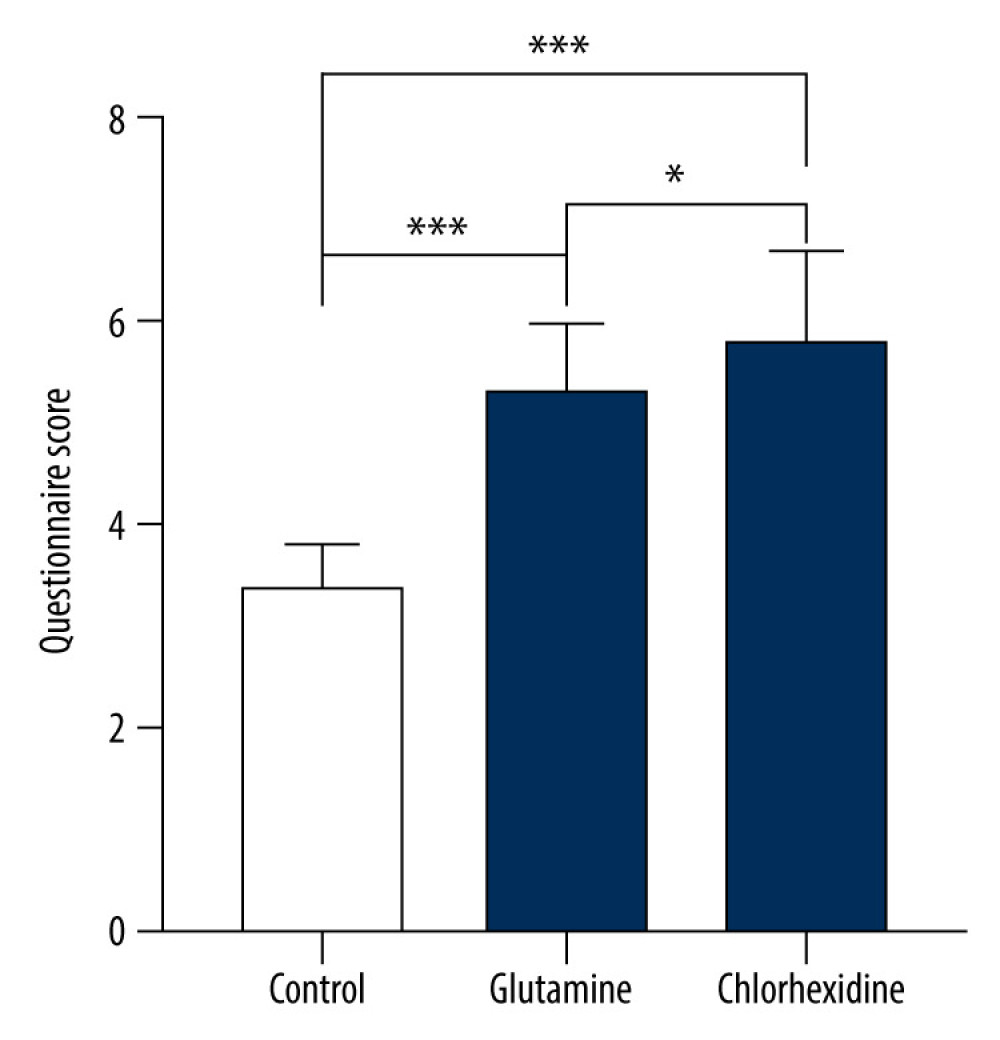 Figure 2. Comparison of questionnaire scores. (Drawn with GraphPad Prism 9, version 9.5.1.).
Figure 2. Comparison of questionnaire scores. (Drawn with GraphPad Prism 9, version 9.5.1.). 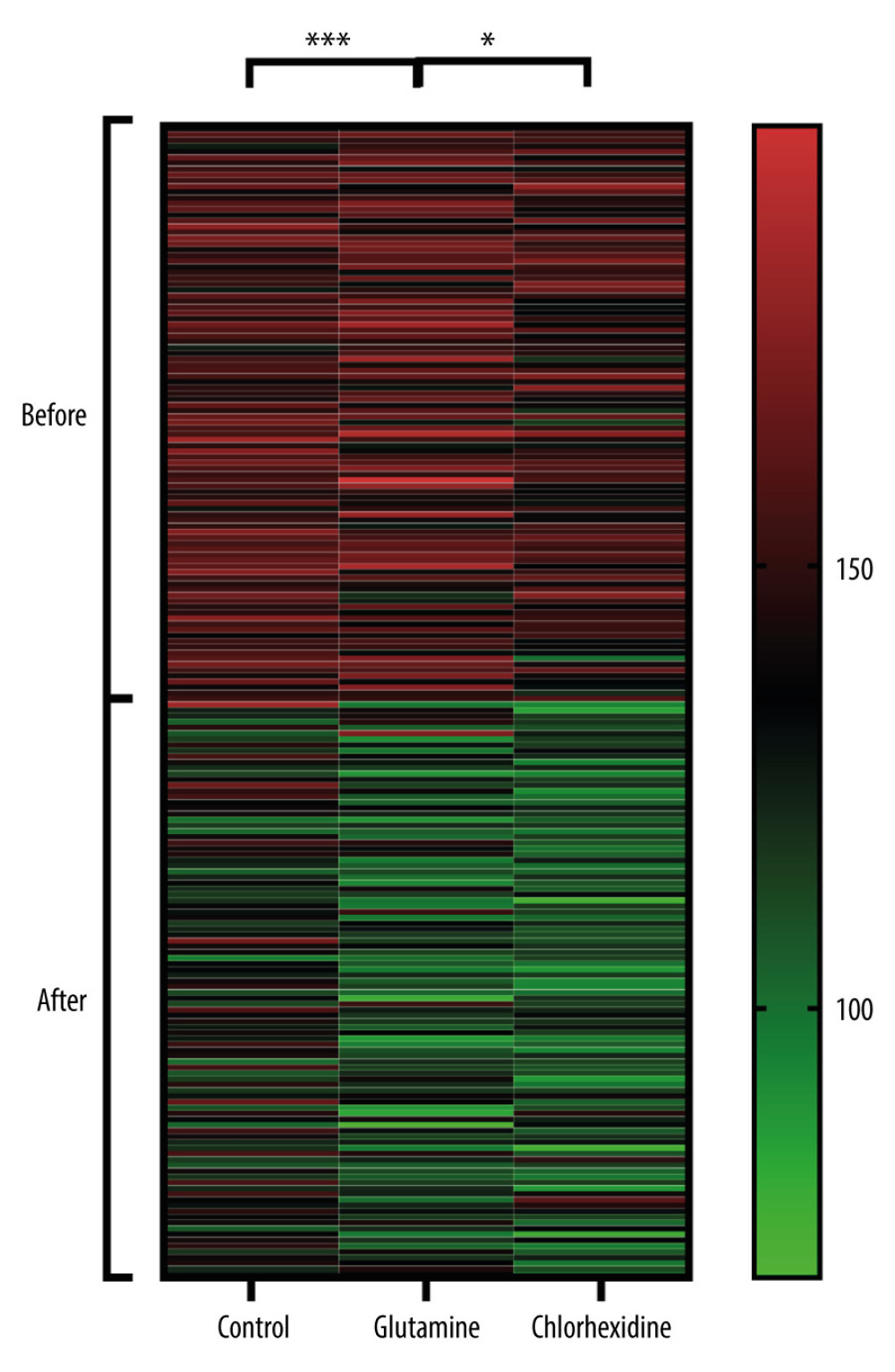 Figure 3. Bacterial comparison. All specimens were sent to the microbial laboratory to identify the types and colonization of flora. Bacteria isolated from the mouth of the patients before and after oral care in all groups were analyzed. All flora types in the 3 groups were compared across different time points: data after oral care/data before surgery. (Drawn with GraphPad Prism 9, version 9.5.1.).
Figure 3. Bacterial comparison. All specimens were sent to the microbial laboratory to identify the types and colonization of flora. Bacteria isolated from the mouth of the patients before and after oral care in all groups were analyzed. All flora types in the 3 groups were compared across different time points: data after oral care/data before surgery. (Drawn with GraphPad Prism 9, version 9.5.1.). References
1. Manchal N, Mohamed MRS, Ting M, Hospital acquired viral respiratory tract infections: An underrecognized nosocomial infection: Infect Dis Health, 2020; 25(3); 175-80
2. Warren C, Medei MK, Wood B, Schutte D, A nurse-driven oral care protocol to reduce hospital-acquired pneumonia: Am J Nurs, 2019; 119(2); 44-51
3. Haghighi A, Shafipour V, Bagheri-Nesami M, The impact of oral care on oral health status and prevention of ventilator-associated pneumonia in critically ill patients: Aust Crit Care, 2017; 30(2); 69-73
4. Sarwal A, Neurologic complications in the postoperative neurosurgery patient: Continuum (Minneap Minn), 2021; 27(5); 1382-404
5. Driver BE, Klein LR, Schick AL, The occurrence of aspiration pneumonia after emergency endotracheal intubation: Am J Emerg Med, 2018; 36(2); 193-96
6. Inai Y, Nomura Y, Takarada T, Hanada N, Wada N, Risk factors for postoperative pneumonia according to examination findings before surgery under general anesthesia: Clin Oral Investig, 2020; 24(10); 3577-85
7. Dahyot-Fizelier C, Frasca D, Lasocki SPROPHY-VAP Study group, ATLANREA group, Prevention of early ventilation-acquired pneumonia (VAP) in comatose brain-injured patients by a single dose of ceftriaxone: PROPHY-VAP study protocol, a multicentre, randomised, double-blind, placebo-controlled trial: BMJ Open, 2018; 8(10); e021488
8. Cecon F, Ferreira LE, Rosa RT, Gursky LC, Time-related increase of staphylococci, Enterobacteriaceae and yeasts in the oral cavities of comatose patients: J Microbiol Immunol Infect, 2010; 43(6); 457-63
9. Zuanazzi D, Souto R, Mattos MB, Prevalence of potential bacterial respiratory pathogens in the oral cavity of hospitalised individuals: Arch Oral Biol, 2010; 55(1); 21-28
10. Mandell LA, Niederman MS, Aspiration pneumonia: N Engl J Med, 2019; 380(7); 651-63
11. Giuliano KK, Penoyer D, Middleton A, Baker D, Original research: Oral care as prevention for nonventilator hospital-acquired pneumonia: A four-unit cluster randomized study: Am J Nurs, 2021; 121(6); 24-33
12. Browne JA, Evans D, Christmas LA, Rodriguez M, Pursuing excellence: development of an oral hygiene protocol for mechanically ventilated patients: Crit Care Nurs Q, 2011; 34(1); 25-30
13. Klompas M, Speck K, Howell MD, Reappraisal of routine oral care with chlorhexidine gluconate for patients receiving mechanical ventilation: systematic review and meta-analysis: JAMA Intern Med, 2014; 174(5); 751-61
14. Labeau SO, Van de Vyver K, Brusselaers N, Prevention of ventilator-associated pneumonia with oral antiseptics: A systematic review and meta-analysis: Lancet Infect Dis, 2011; 11(11); 845-54
15. Hollaar VRY, van der Putten GJ, van der Maarel-Wierink CDThe effect of a daily application of a 0, 05% chlorhexidine oral rinse solution on the incidence of aspiration pneumonia in nursing home residents: a multicenter study: BMC Geriatr, 2017; 17; 128
16. Özçaka Ö, Başoğlu OK, Buduneli N, Chlorhexidine decreases the risk of ventilator-associated pneumonia in Intensive Care Unit patients: A randomized clinical trial: J Periodontal Res, 2012; 47(5); 584-92
17. Berry AM, Davidson PM, Masters J, Effects of three approaches to standardized oral hygiene to reduce bacterial colonization and ventilator associated pneumonia in mechanically ventilated patients: A randomised control trial: Int J Nurs Stud, 2011; 48(6); 681-88
18. Munro CL, Grap MJ, Jones DJ, Chlorhexidine, toothbrushing, and preventing ventilator-associated pneumonia in critically ill adults: Am J Crit Care, 2009; 18(5); 428-37 quiz 438
19. Noé JE, L-glutamine use in the treatment and prevention of mucositis and cachexia: A naturopathic perspective: Integr Cancer Ther, 2009; 8(4); 409-15
20. Mahendran VJ, Stringer AM, Semple SJ, Advances in the use of anti-inflammatory agents to manage chemotherapy-induced oral and gastrointestinal mucositis: Curr Pharm Des, 2018; 24(14); 1518-32
21. Davy C, Heathcote S, A systematic review of interventions to mitigate radiotherapy-induced oral mucositis in head and neck cancer patients: Support Care Cancer, 2021; 29(4); 2187-202
22. Scannapieco FA, Giuliano KK, Baker D, Oral health status and the etiology and prevention of nonventilator hospital-associated pneumonia: Periodontol 2000, 2022; 89(1); 51-58
23. Jackson L, Owens M, Does oral care with chlorhexidine reduce ventilator-associated pneumonia in mechanically ventilated adults?: Br J Nurs, 2019; 28(11); 682-89
24. Ahn Y, Jun Y, Kim N, Sohn M, Flora colonization and oral care in high-risk newborns: J Spec Pediatr Nurs, 2019; 24(1); e12233
25. Martin-Loeches I, Rodriguez AH, Torres A, New guidelines for hospital-acquired pneumonia/ventilator-associated pneumonia: USA vs. Europe: Curr Opin Crit Care, 2018; 24(5); 347-52
26. Chughtai M, Gwam CU, Khlopas A, The incidence of postoperative pneumonia in various surgical subspecialties: A dual database analysis: Surg Technol Int, 2017; 30; 45-51
27. Tuon FF, Gavrilko O, Almeida S, Prospective, randomised, controlled study evaluating early modification of oral microbiota following admission to the Intensive Care Unit and oral hygiene with chlorhexidine: J Glob Antimicrob Resist, 2017; 8; 159-63
28. Takeyasu Y, Yamane GY, Tonogi M, Ventilator-associated pneumonia risk decreased by use of oral moisture gel in oral health care: Bull Tokyo Dent Coll, 2014; 55(2); 95-102
29. Brookes ZLS, Bescos R, Belfield LA, Current uses of chlorhexidine for management of oral disease: A narrative review: J Dent, 2020; 103; 103497
30. Hashimoto K, Emerging role of the host microbiome in neuropsychiatric disorders: Overview and future directions: Mol Psychiatry, 2023; 28(9); 3625-37
31. Raison MH, Corcoran R, Burnside G, Harris R, Oral hygiene behaviour automaticity: Are toothbrushing and interdental cleaning habitual behaviours?: J Dent, 2020; 102; 103470
32. Morand M, Hatami A, Multiple superficial oral mucoceles after Mycoplasma-induced mucositis: Pediatr Dermatol, 2018; 35(4); e210-e11
33. Hua F, Xie H, Worthington HV, Oral hygiene care for critically ill patients to prevent ventilator-associated pneumonia: Cochrane Database Syst Rev, 2016; 10(10); CD008367 Update in: Cochrane Database Syst Rev. 2020;12(12):CD008367
34. Ustrell-Borràs M, Traboulsi-Garet B, Gay-Escoda C, Alcohol-based mouthwash as a risk factor of oral cancer: A systematic review: Med Oral Patol Oral Cir Bucal, 2020; 25(1); e1-e12
35. Madan PD, Sequeira PS, Shenoy K, Shetty J, The effect of three mouthwashes on radiation-induced oral mucositis in patients with head and neck malignancies: A randomized control trial: J Cancer Res Ther, 2008; 4(1); 3-8
36. Breslin PA, Tharp CD, Reduction of saltiness and bitterness after a chlorhexidine rinse: Chem Senses, 2001; 26(2); 105-16 Erratum in: Chem Senses 2001;26(4):447
37. Flötra L, Gjermo P, Rölla G, Waerhaug J, Side effects of chlorhexidine mouth washes: Scand J Dent Res, 1971; 79(2); 119-25
38. Yates R, Jenkins S, Newcombe R, A 6-month home usage trial of a 1% chlorhexidine toothpaste (1). Effects on plaque, gingivitis, calculus and toothstaining: J Clin Periodontol, 1993; 20(2); 130-38
39. Khan MW, Layden BT, Chakrabarti P, Inhibition of mTOR complexes protects cancer cells from glutamine starvation induced cell death by restoring Akt stability: Biochim Biophys Acta Mol Basis Dis, 2018; 1864(6 Pt A); 2040-52
40. McGuire DB, Fulton JS, Park JMucositis Study Group of the Multinational Association of Supportive Care in Cancer/International Society of Oral Oncology (MASCC/ISOO), Systematic review of basic oral care for the management of oral mucositis in cancer patients: Support Care Cancer, 2013; 21(11); 3165-77
41. Yildirim ZK, Bidev D, Buyukavci M, Parenteral glutamine supplementation has no effect on chemotherapy-induced toxicity in children with non-Hodgkin lymphoma: J Pediatr Hematol Oncol, 2013; 35; 371-76
42. Klimberg VS, Salloum RM, Kasper M, Oral glutamine accelerates healing of the small intestine and improves outcome after whole abdominal radiation: Arch Surg, 1990; 125(8); 1040-45
Figures
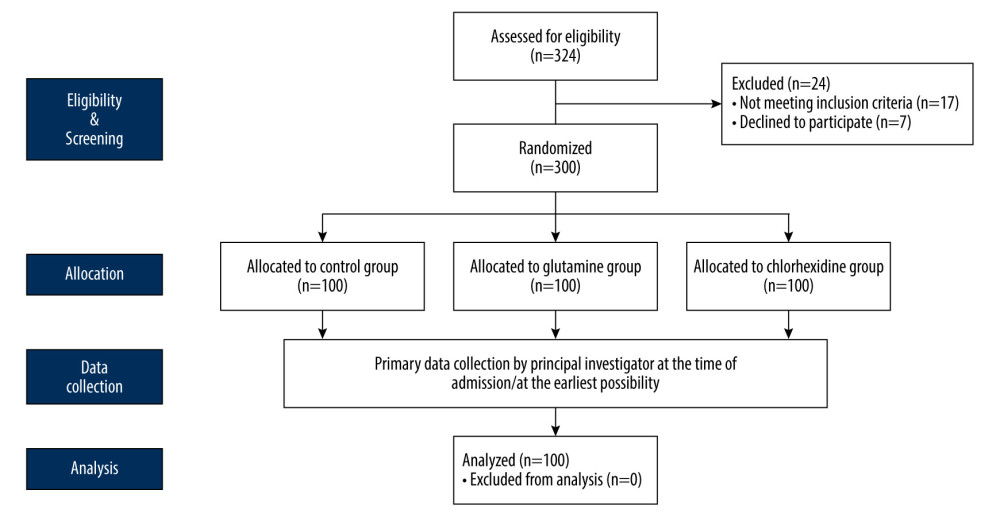 Figure 1. Diagrammatic algorithm of participant flow. (Drawn with Adobe Illustrator, 2020, 24.2.1.).
Figure 1. Diagrammatic algorithm of participant flow. (Drawn with Adobe Illustrator, 2020, 24.2.1.).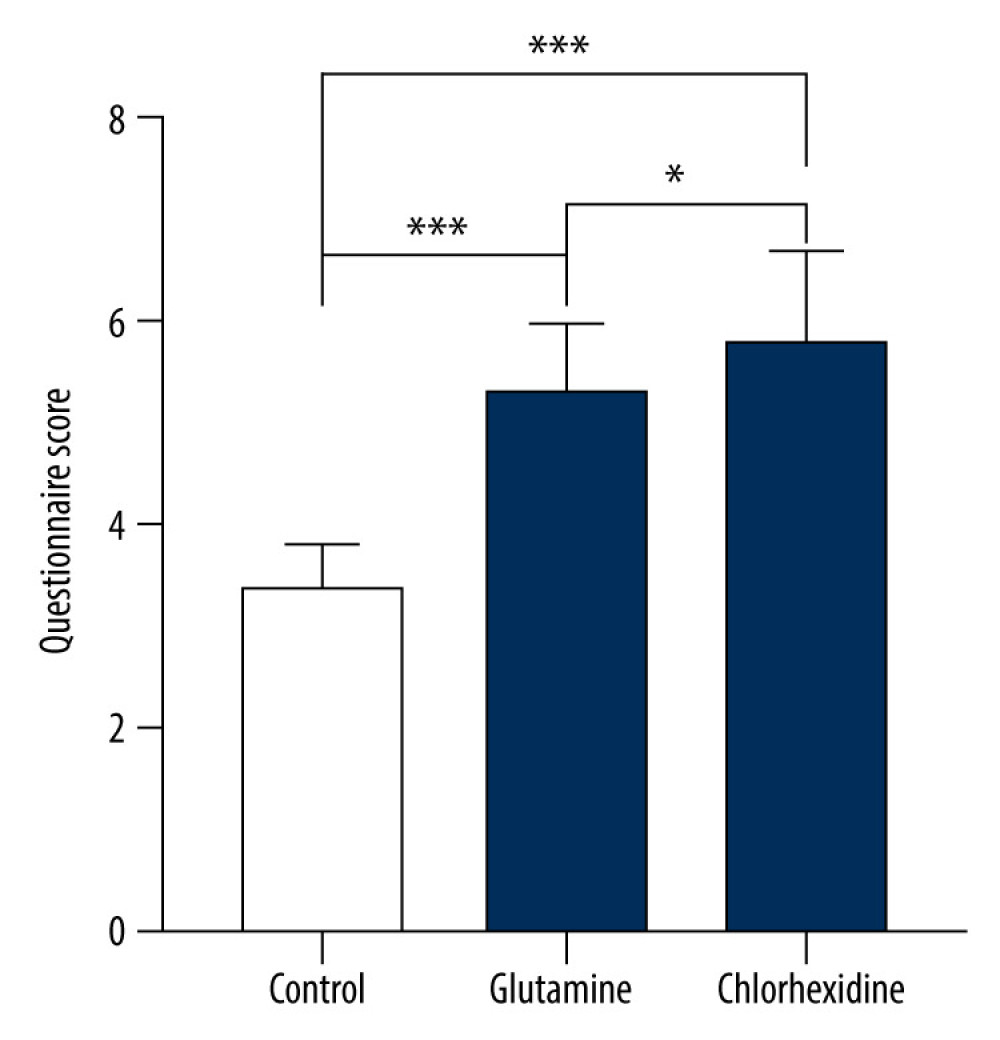 Figure 2. Comparison of questionnaire scores. (Drawn with GraphPad Prism 9, version 9.5.1.).
Figure 2. Comparison of questionnaire scores. (Drawn with GraphPad Prism 9, version 9.5.1.).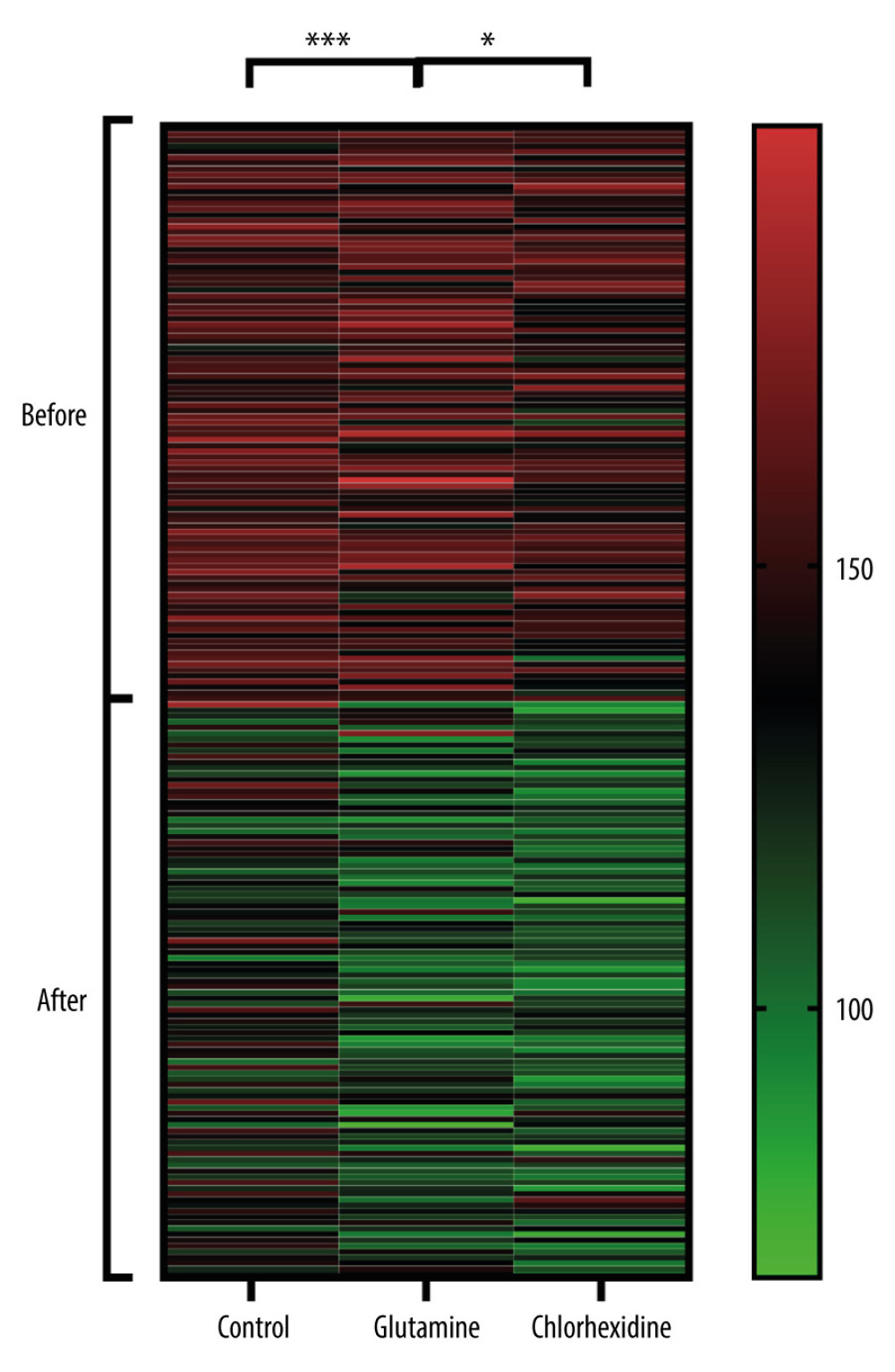 Figure 3. Bacterial comparison. All specimens were sent to the microbial laboratory to identify the types and colonization of flora. Bacteria isolated from the mouth of the patients before and after oral care in all groups were analyzed. All flora types in the 3 groups were compared across different time points: data after oral care/data before surgery. (Drawn with GraphPad Prism 9, version 9.5.1.).
Figure 3. Bacterial comparison. All specimens were sent to the microbial laboratory to identify the types and colonization of flora. Bacteria isolated from the mouth of the patients before and after oral care in all groups were analyzed. All flora types in the 3 groups were compared across different time points: data after oral care/data before surgery. (Drawn with GraphPad Prism 9, version 9.5.1.). Tables
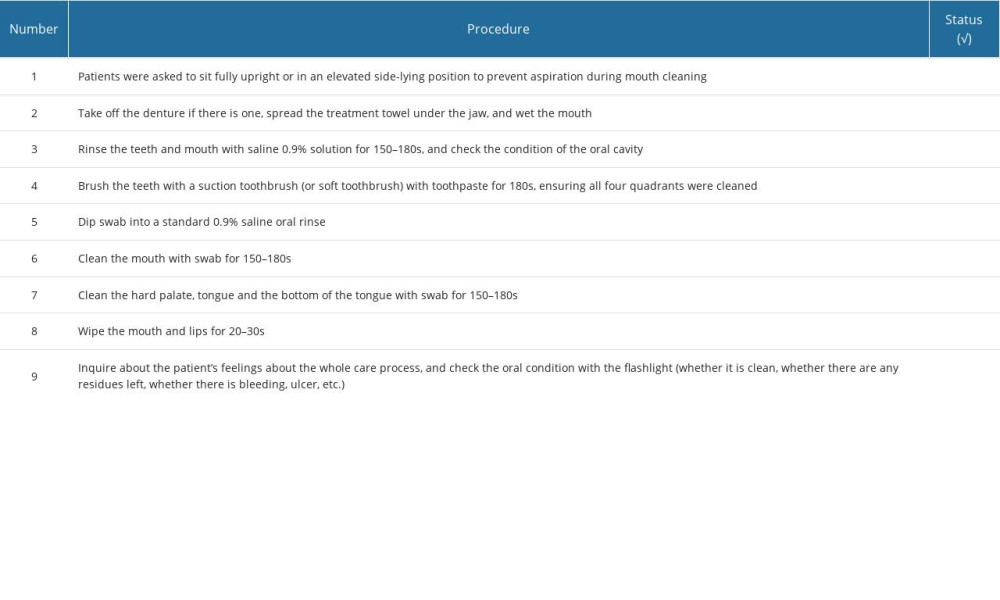 Table 1. Checklist of oral care procedures.
Table 1. Checklist of oral care procedures.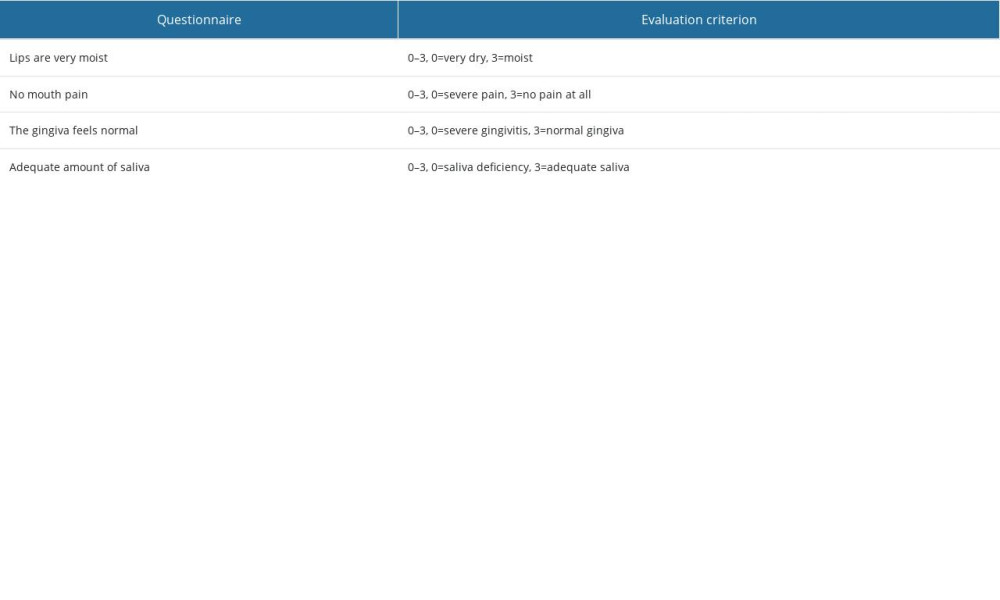 Table 2. Questionnaire used to evaluate the patients’ oral condition.
Table 2. Questionnaire used to evaluate the patients’ oral condition.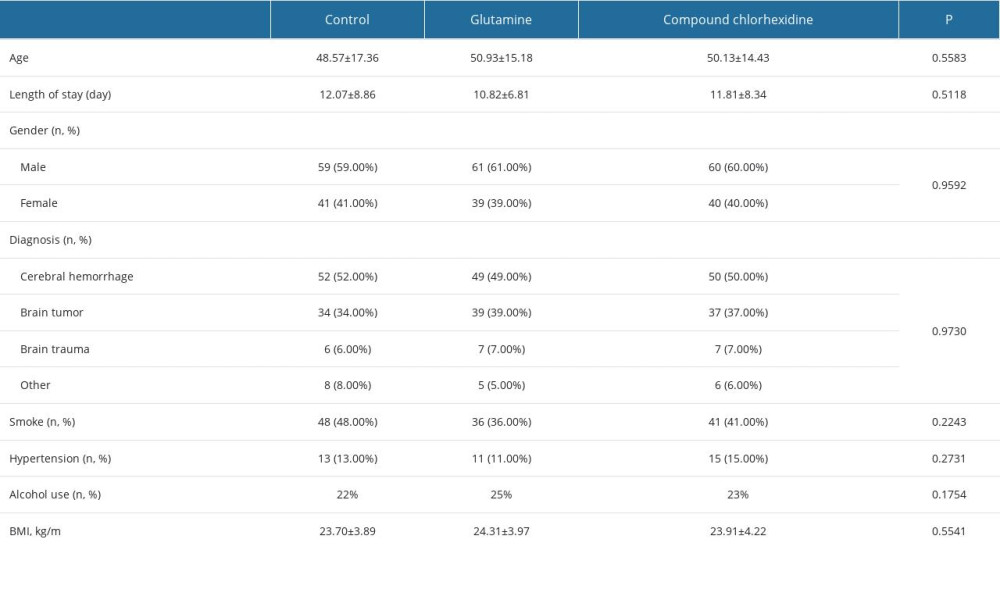 Table 3. General information.
Table 3. General information.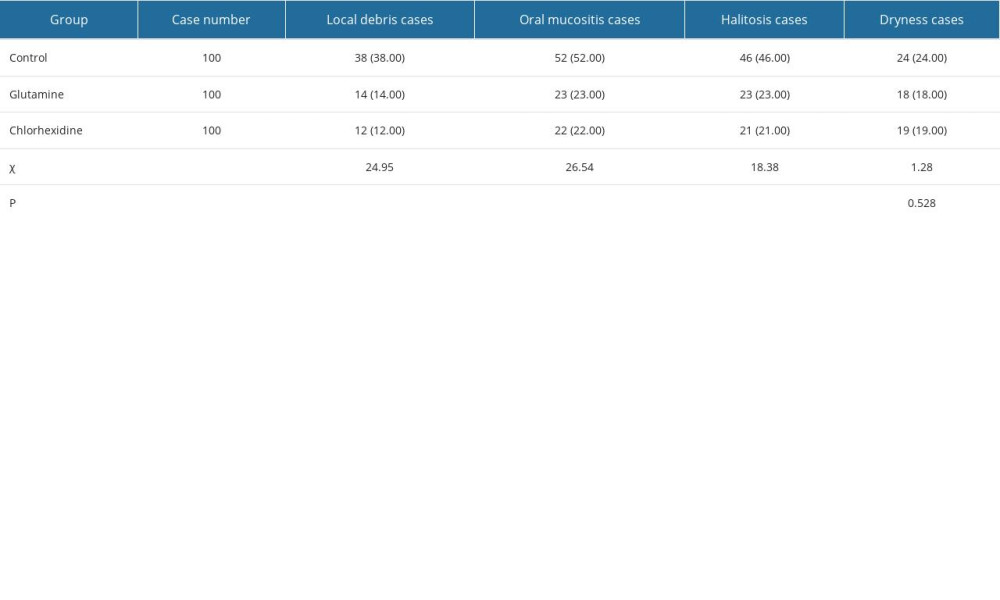 Table 4. Comparison of oral disorders.
Table 4. Comparison of oral disorders.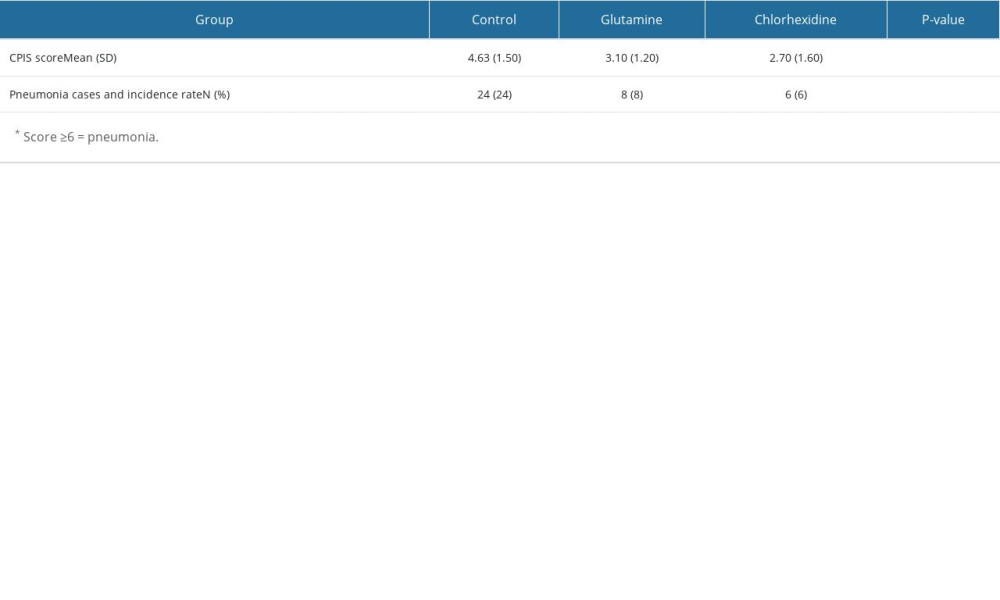 Table 5. Clinical Pulmonary Infection Score and pneumonia incidence rate*.
Table 5. Clinical Pulmonary Infection Score and pneumonia incidence rate*.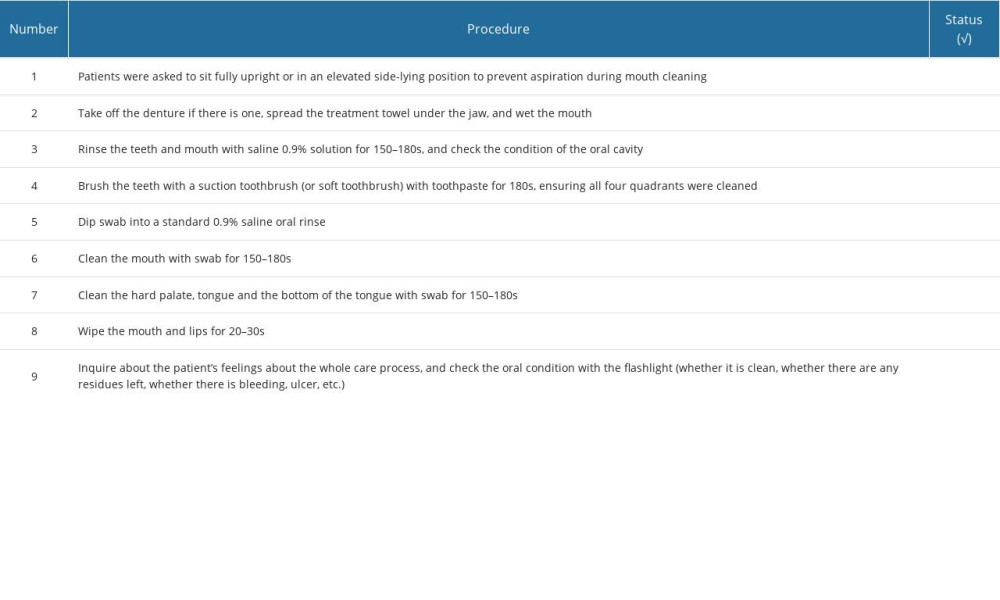 Table 1. Checklist of oral care procedures.
Table 1. Checklist of oral care procedures.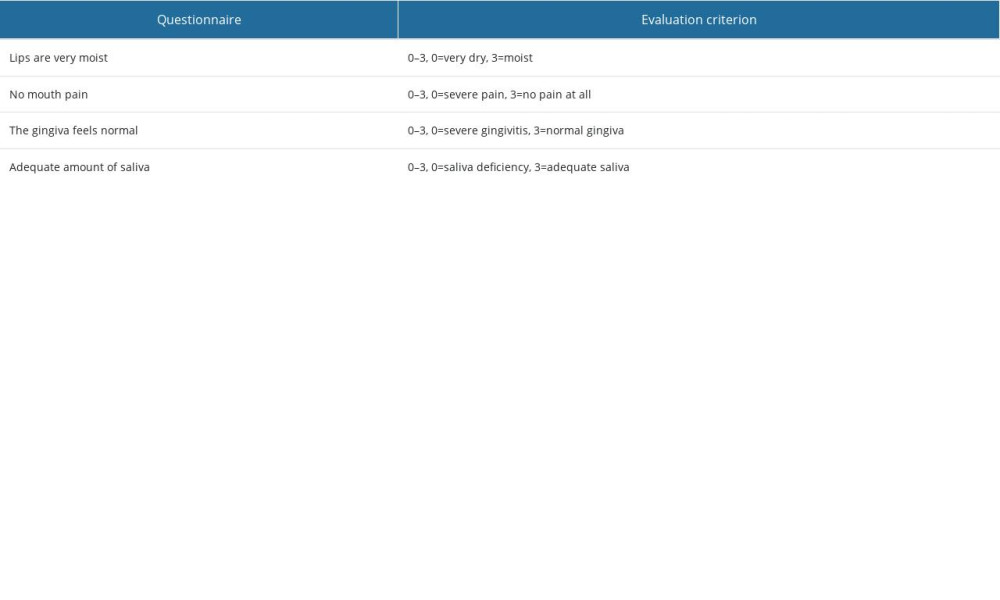 Table 2. Questionnaire used to evaluate the patients’ oral condition.
Table 2. Questionnaire used to evaluate the patients’ oral condition.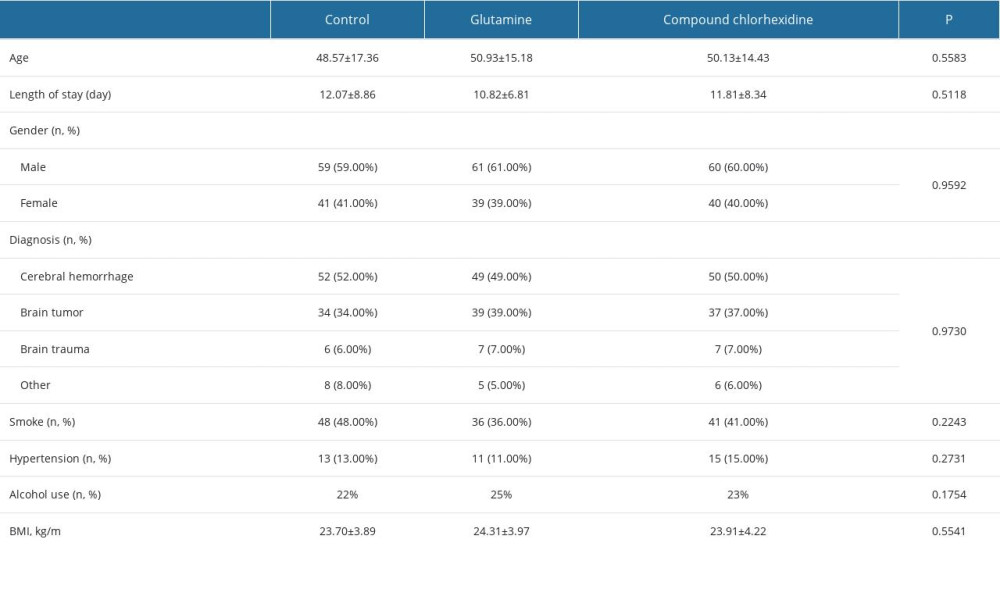 Table 3. General information.
Table 3. General information.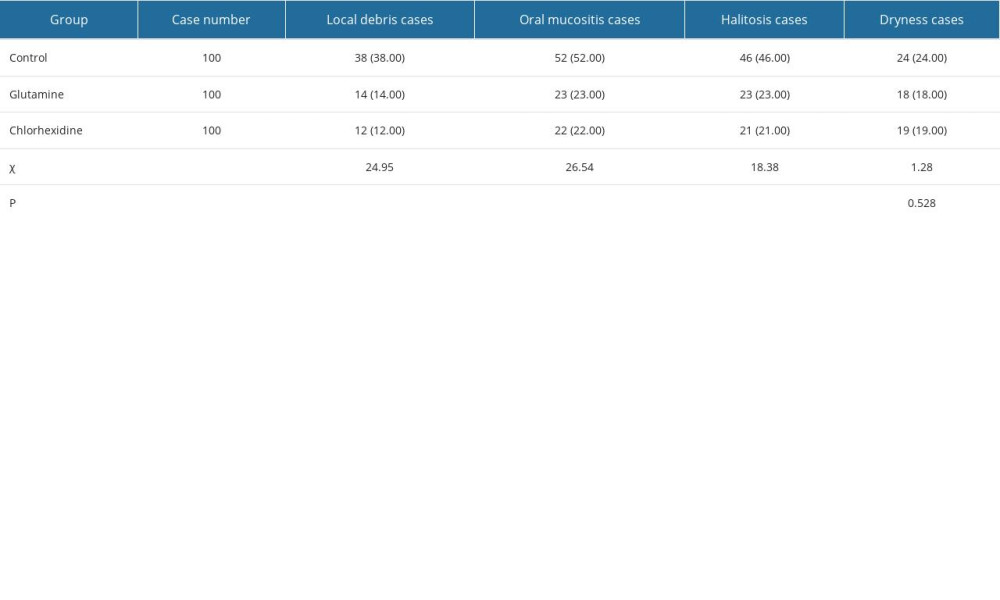 Table 4. Comparison of oral disorders.
Table 4. Comparison of oral disorders.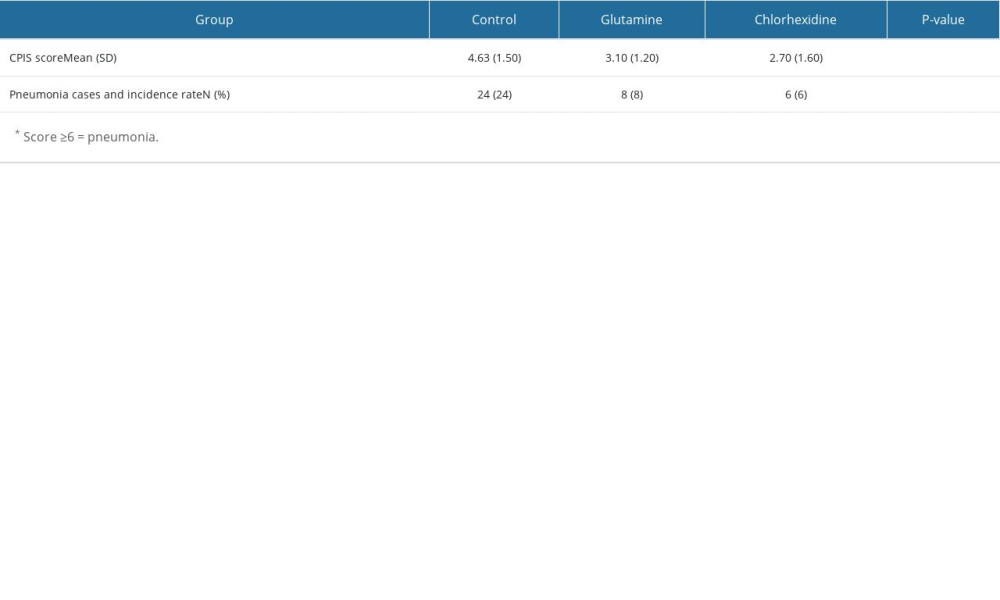 Table 5. Clinical Pulmonary Infection Score and pneumonia incidence rate*.
Table 5. Clinical Pulmonary Infection Score and pneumonia incidence rate*. In Press
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








