30 November 2023: Clinical Research
The Impact of Head Elevation on Prevalence and Severity of Emergence Cough in Male Patients during Endotracheal Extubation
Gang Mee Lim1B, Soo Jung Park2DE, Sung Young Park2CD, Ji Ho Kim3C, Ji Eun KimDOI: 10.12659/MSM.942597
Med Sci Monit 2023; 29:e942597
Abstract
BACKGROUND: Emergence cough during endotracheal extubation can lead to complications. This cough is triggered by the deviation of the endotracheal tube from the airway anatomy, causing pressure on the airway mucosal wall. Head elevation has the potential to align the airway passage with the tube's configuration. In this study, we aimed to investigate the impact of head elevation using a pillow on the prevalence and severity of emergence cough in male patients.
MATERIAL AND METHODS: A total of 71 male patients undergoing laparoscopic cholecystectomy were randomly assigned to either the head elevation group (n=35) or the control group (n=36). The head elevation group maintained a position with a neck flexion angle of 35º using a pillow, while the control group remained in a neutral position after anesthetic induction. The severity of cough was assessed before, during, and after extubation using a 4-point scale, with grades 2 and 3 indicating cough and grade 3 indicating severe cough.
RESULTS: The characteristics and intraoperative data of the patients were similar between the two groups. There was no significant difference in the incidence of cough and severe cough between the groups. However, the severity of cough was significantly lower in the head elevation group compared to the control group before extubation (cough scale: 0/5/8/23 vs 1/2/17/15 in the control group vs the head elevation group, P=0.039). The time to extubation, respiratory complications, nausea, pain, and the number of patients receiving fentanyl were comparable between the groups.
CONCLUSIONS: Head elevation using a pillow effectively reduced the severity of cough before endotracheal extubation during anesthesia emergence in male patients. However, it did not significantly reduce the incidence of cough. These findings highlight the potential benefits of head elevation in minimizing the discomfort associated with emergence cough.
Keywords: Airway Extubation, Anesthesia, Cough, Patient Positioning
Background
Extubation is the process of removing an endotracheal (ET) tube, which liberates a patient from the mechanical ventilators [1]. According to the American Thoracic Society and the American College of Chest Physicians Clinical Practice Guidelines, tracheal extubation is recommended to be managed with a ventilator liberation protocol, including weaning parameter assessment (eg, frequency-tidal volume ratio) or spontaneous breathing trial [2,3]. However, despite these preparations, adverse events associated with extubation can occur, such as patient distress, hemodynamic perturbations, compromised ventilation, and airway irritation or injury [4].
Emergence cough from general anesthesia occurs frequently, with an incidence of up to 76% [5]. Uncontrolled cough at perioperative extubation can increase thoracic and intracranial pressure, bleeding at the surgical site, and wound dehiscence, and can cause hemodynamic instability [6]. Thus, strategies for reducing cough have been proposed, such as smooth emergence techniques (deep extubation and no-touch extubation) or pharmacologic interventions (topical and intravenous [IV] lidocaine, IV opioid, and dexmedetomidine) [7–9]. However, there is limited evidence to support the efficacy of these techniques, and there are potential adverse effects (eg, local anesthetic toxicity, opioid abuse, vomiting, and delayed emergence), and they can be expensive [4]. Despite several studies on adjuvants for improving emergence, there are no adjuvant maneuvers to reduce the emergence cough to date [4].
The cough reflex is mediated by dual sensory neurons (nociceptor and mechanoreceptor) throughout the larynx, trachea, carina, and large intrapulmonary bronchi [10]. The curvature of the ET tube is deviated from the airway anatomy with a slight S-shaped curve, and thus can directly apply pressure to these structures [11,12]. This pressure activates mechanoreceptor, which is considered a main contributing factor provoking cough [10,13]. Mucosal pressure exerted by the ET tube contributes to grade 1 or 2 ulcers, laryngeal incompetence, and even airway structure deformation [14–16].
The 3-axis alignment theory remains a common airway concept for direct laryngoscopy despite a debate about the degree of elevation and extension of head alignment needed [17,18]. Neck flexion by head elevation causes the glottic aperture to move posteriorly, resulting in better alignment of the 3-axis [19]. In addition, head elevation, a commonly used maneuver to maintain airway patency in anesthesia, is possibly associated with better oxygen reserve [20]. Therefore, we hypothesized that head elevation lowers the pressure between the ET tube and the airway wall because the curved ET tube has a propensity to unbend. To the best of our knowledge, this is the first study to adjust the airway passage to the ET tube’s configuration by changing the head position to prevent emergence cough.
This study aimed to evaluate the effects of head position on the prevention of cough during extubation in 71 male patients requiring general anesthesia during cholecystectomy.
Material and Methods
ETHICS STATEMENT:
This study was approved by the Ethics committee of the Ajou’s Institutional Review Board (reference number AJIRB-MED-OBS-20-055, May 19, 2020) and registered at
The participants consisted of male patients aged 19–85 years undergoing elective laparoscopic cholecystectomy from June 2020 to November 2022. The exclusion criteria were individuals with an American Society of Anesthesiologists classification of 4 or higher, a body mass index (BMI) of ≥30 g/m2, a history of upper respiratory tract infection within the past 2 weeks, a diagnosis of asthma or chronic obstructive pulmonary disease, anticipated difficult intubation, uncontrolled hypertension or diabetes, and severe cardiovascular disease.
PATIENT ALLOCATION:
The participants were randomly assigned to 1 of the following 2 groups using R 3.4.0 (Vienna, Austria;
ANESTHESIA:
None of the patients were pre-medicated. In the operating room, patients received standard monitoring, including pulse oximetry for oxygen saturation, electrocardiography, non-invasive blood pressure measurements, and bispectral index. After a pillow (8–10 cm thick) was placed under the head of the patient, anesthesia induction was conducted with propofol of 2 mg/kg and remifentanil (Ultian, Hanlim Pharm. Co., Ltd., Korea) using target-controlled infusion based on Minto’s pharmacokinetics at a concentration of 1–5 ng/mL. Once loss of consciousness was achieved, IV rocuronium was administered at a dose of 1 mg/kg to facilitate adequate muscle relaxation. After ensuring sufficient muscle relaxation, intubation was performed using a 7.5 mm ET tube with the assistance of a video laryngoscope. Cuff pressure was adjusted to 20–25 mmHg using a hand pressure gauge. After anesthesia induction, the pillow was removed or kept according to the assigned group during surgery. Sevoflurane and remifentanil were adjusted to maintain bispectral index levels between 40 and 60. Mean arterial pressure (MAP) and heart rate (HR) were maintained within 20% of the baseline values by adjusting the anesthetic agents. Rocuronium was continuously infused to maintain a train-of-four count of 1–2.
All patients received IV acetaminophen of 20 mg/kg and ramosetron of 0.3 mg at the start of skin closure. At the completion of surgery, sevoflurane was stopped, and fresh gas flow was increased to 5 L/min with 100% oxygen. Remifentanil was maintained at a concentration of 1.0 ng/mL. Sugammadex 2 mg/kg was given to achieve a train-of-four ratio >0.9. Extubation was carried out by a single anesthesiologist after eye-opening upon verbal command and confirming adequate spontaneous ventilation. Remifentanil was immediately discontinued. After vital signs were monitored for 3 min, the patient was transferred to the Post-Anesthesia Care Unit (PACU).
DEFINITIONS AND MEASUREMENTS:
The primary outcome was the incidence and severity of cough around ET extubation. The secondary outcome included respiratory complications, time to extubation, and throat and overall pain score. Emergence cough was assessed at 3 time points: before extubation, at extubation, and after extubation, using a 4-point scale (cough grade: 0=no cough, 1 =a single cough, 2=more than 1 episode of non-sustained cough, and 3=sustained and repetitive cough). Cough was defined as having clinical meaning for grades 2 and 3. Severe cough was defined as only grade 3.
Preoperative data (age, weight, height, BMI, smoking history, and past medical history) were collected through electronic medical records and interviews. The number of intubation attempts, the end-tidal concentration of sevoflurane at the time of eye-opening upon verbal command without stimulation, operation time, and anesthesia time were also collected. Time to extubation was defined as the time from sevoflurane stop to extubation. HR and MAP were recorded at 5 time points: baseline (before anesthesia induction, T0), at the end of surgery (T1), immediately (T2), 3 min (T3) after extubation, and at the PACU (T4). Respiratory complications such as bradypnea (respiratory rate <8 times/min), laryngospasm, and desaturation (SpO2 <95% despite oxygen supplementation) were assessed. Immediately on arrival in the PACU, sedation levels were assessed using the Ramsay Sedation Scale (6 levels: 1=anxious and agitated or restless or both; 6=no response to a light glabellar tap or auditory stimulus). Nausea, vomiting, and overall and throat pain using the numeric rating scale (0=no pain, 10=worst pain) were evaluated. A fentanyl dose of 0.5 mcg/kg was administered in the event of pain score ≥5.
STATISTICAL ANALYSIS:
The sample size was calculated based on the incidence of emergence cough as the primary outcome. By referring to the findings of a previous study [21], the incidence of cough was 63% when extubation was achieved at remifentanil infusion of concentration 1.0 ng/mL after general anesthesia using sevoflurane and remifentanil. We considered a difference in the incidence of cough >50% as clinically relevant. Based on a significance level of 5% and statistical power of 80%, each group required 36 subjects to compensate for dropouts. Finally, a total of 72 patients was enrolled.
All statistical analyses were performed using SPSS (version 25.0, IBM Corporation, Armonk, NY, USA). Statistical significance was defined as
Results
COUGH PROFILES:
Around the ET extubation, the incidences of cough were up to approximately 90% despite the exclusion of grade 1 cough, and the incidences of severe cough also were over 50% in both groups (Table 2). Consequently, the incidences of cough and severe cough were not different between the 2 groups. However, the severity of cough was significantly lower in the head elevation group compared to the control group before extubation (cough scale 0/5/8/23 in the control group vs 1/2/17/15 in the head elevation group, P=0.039), although it was similar at extubation and after extubation.
EMERGENCE AND RECOVERY PROFILES:
During anesthesia emergence, time to extubation did not differ between the 2 groups (Table 3). Of the complications, desaturation after extubation was observed in 1 patient in the control group but resolved with encouragement. In the recovery room, sedation status upon arrival was observed within the range of awake levels (sedation scores 1, 2, and 3) except for 2 patients in the head elevation group (sedation scores 4). Nausea and vomiting, overall pain, throat pain, and the number of patients receiving fentanyl as rescue were similar between groups.
HEMODYNAMICS:
HR and MAP were comparable between the 2 groups during the perioperative period (Pgroup*time=0.621 and Pgroup*time=0.901 for HR and MAP, respectively) (Figure 2).
Discussion
In this prospective, randomized controlled study, we found that head elevation using a pillow (neck flexion angle of 35°) significantly reduced the severity of cough just before ET extubation during emergence from general anesthesia, as compared with neutral position. However, it did not reduce the incidences of cough or severe cough.
Although the underlying mechanism of cough remains uncertain, it is widely recognized that various signals transmitted through accepting receptors (nociceptor and mechanoreceptor) around the airway mucosa are relayed by vagal afferent nerves to the brainstem of the central nervous system, where the cough reflex is generated and regulated [10,22]. Anesthetic agents and opioids depress the cough evocation at the brainstem, whereas peripherally acting agents (eg, local anesthetics) block nociceptor and mechanoreceptor activation to reduce the cough [10]. Importantly, mechanoreceptors positioned beneath the epithelium proximally in the large airways are relatively insensitive to most chemical mediators (except local anesthetics) but are exquisitely sensitive to stimuli delivered to the mucosal surface [10]. In the intubated condition, cough can be triggered by several factors, such as airway secretion, inhalation agents, and an ET tube. Regarding mechanoreceptors, the ET tube exerts direct pressure and mechanical stimulation on the airway but provokes cough when the cough-inhibitory effects of anesthesia disappear at the brainstem during emergence.
The ET tube is an essential device for safety in mechanically ventilated patients in acute care or undergoing general anesthesia. The standard ET tube has a curvature called “the Magill curve”, with an approximate 140±20 mm radius [13]. This standard tube does not correspond to normal anatomy, in which the passage from the laryngeal inlet to the upper trachea forms a slight S-shaped curve [23,24]. The natural curve of the ET tube intends to align vertically with respect to the patient. Therefore, ET tubes deviating from airway anatomy can exert an elastic load on the pharynx and posterior larynx due to the lack of compliance [11,12].
Medical devices including an ET tube impose pressure on the surrounding tissue, and the subsequent mucocutaneous injuries generally mimic the device shape and size [25]. An ET tube is the most common device causing medical device-related pressure injuries, accounting for an estimated 7.5% in all care settings and up to 28% in ICU settings [26]. Although the intensity of pressure injury is less than the ET tube fixation, the ET tube itself can press against mucosal tissue, with intensity reported as grade 1 and 2 for 4-point device-related pressure ulcer grading [14]. In addition, the presence of an ET tube can cause pressure at all sites with tissue-endotracheal interaction (eg, the oral cavity, oropharynx, larynx, and trachea). Of these, the most frequently reported sites associated with ET tube-related pressure injury were the lips and tongue [25]. Many studies have focused on ET tube-related pressure injury affecting the skin and external soft tissue because internal airway injury lacks pressure measurement for grading [27,28]. However, internal airway pressure is also important, considering that subglottic and trachea endoluminal pressure consequently leads to tracheal stenosis [15]. Therefore, changes in head and neck position for fitting the airway passage to the ET tube’s configuration as much as possible might be essential to minimize the airway wall pressure as an extrinsic factor triggering a cough.
Since Magill first described the “sniffing position” as an elevation of the occiput and extension of the head, Bannister et al reformed the laryngoscopy positioning by suggesting the need to align the oral, pharyngeal, and laryngeal axes, called the “3-axis alignment theory” [17]. Horton et al further progressed this concept by establishing the ideal angles as 15º for upper cervical flexion and 35° for lower cervical extension [29]. Based on this theory, head elevation improves the alignment of the 3 axes compared to a neutral position. This was confirmed in magnetic resonance imaging (MRI) studies of the head and neck region [12,30]. Greenland et al acquired MRI sagittal slices from 10 awake adult volunteers and found that the nasopharynx was below the glottis in the neutral position but above the glottis in the sniffing position [30]. Later, they employed a “2-curve theory” to explain airway configuration, in which tangent was assessed at the point where the primary and secondary curves meet in the S-shaped airway [12]. As a result, head elevation caused an anticlockwise rotation of the tangent, meaning that a curved ET tube was more likely to pass from the airway into the trachea with less impact on the airway wall in the head-elevated position than in the neutral position [12]. Thus, the head elevation position seemed to cause less pressure on the airway wall than a neutral position in the intubated state. It might be helpful that crucial radiological imaging of the patients in the 2 head positions was achieved in the surgical room.
We chose head elevation, not the sniffing position, to compare with the neutral position in our study. After the formation and acceptance of the 3-axis alignment theory, its correctness has been under debate. It has been argued that the sniffing position does not bring the 3 axes into alignment [18,31]. In 2015, Orbany et al evaluated the laryngeal view in head extension without head elevation, 6 cm head-elevated, and 10 cm head-elevated sniffing positions [32]. Sniffing positions improved the laryngoscopic view, but a more head-elevated sniffing position further improved the view. The mechanism is assumed to be that head elevation (neck flexion) moves the glottis posteriorly, thus compensating for anterior displacement of the glottis during head extension and possibly resulting in better alignment of the 3-axis [19]. Therefore, if the same pillow height is applied to each position in our study, the head-elevated position might be more in accord with the ET tube configuration than the sniffing position and consequently lower the direct pressure between the ET tube and the airway wall. Further studies assessing the effect of the sniffing position on emergence cough are needed.
Another possible explanation underlying the reduction in emergence cough associated with head elevation could be related to tracheal accordion. In our study, all patients in both groups were intubated in a head-elevated position on a pillow, and insertion of the ET tube was stopped as soon as the vocal cord indicator passed the laryngoscope vocal cords. While the head elevation group was maintained in this position, the control group was changed to the neutral position by removing the pillow. It is well documented that neck flexion or extension can either decrease or increase the tracheal length [33]; therefore, the change in head position in the control group might lead to neck extension and trachea lengthening, displacing the endotracheal tube cuff cephalad towards the vocal cords in our study. Given that the most sensitive regions of the airways for mechanically triggering cough are the larynx and the tracheal and bronchial bifurcation, stimuli in the mechanosensitive receptors located more proximally to the larynx in the control group seem to act in provoking cough to some degree [10,34].
Our findings are particularly important with respect to presenting the clinical implication that a simple manipulation of the head position to align the physiological structures of the larynx and pharynx with the ET tube’s configuration, not pharmacologic interventions (eg, opioids), could reduce emergence cough in intubated patients. Another strength of this study lies in the single-sex (male) enrollment, single surgery with short operation time, and the additional effect of lowering airway edema because pressure forces are associated with local edema [25].
There were a few limitations to the methods in our study. First, blinding of the extubator was not practically possible. Second, tracheal diameter was associated with height in men’s anatomic studies [35]. ET tube size was best determined by each patient’s height, instead of using a uniform size of 7.5 mm. Third, the validity of the sniffing position on 3-axis alignment was significant in obese but not in non-obese patients [18]. Thus, the effect of head elevation on emergence cough should be evaluated in obese patients. Finally, target-controlled infusion of remifentanil was maintained at a concentration of 1.0 ng/mL during anesthesia emergence. Because the remifentanil concentration used to suppress emergence cough in a prior study enrolling male patients was approximately 2.5 ng/mL, it might have led to the high incidences of coughing, at up to approximately 90%, and consequently failed to reduce the incidence [36].
Conclusions
Head elevation using a pillow significantly reduced the severity of cough before ET extubation during anesthesia emergence in male patients.
Figures
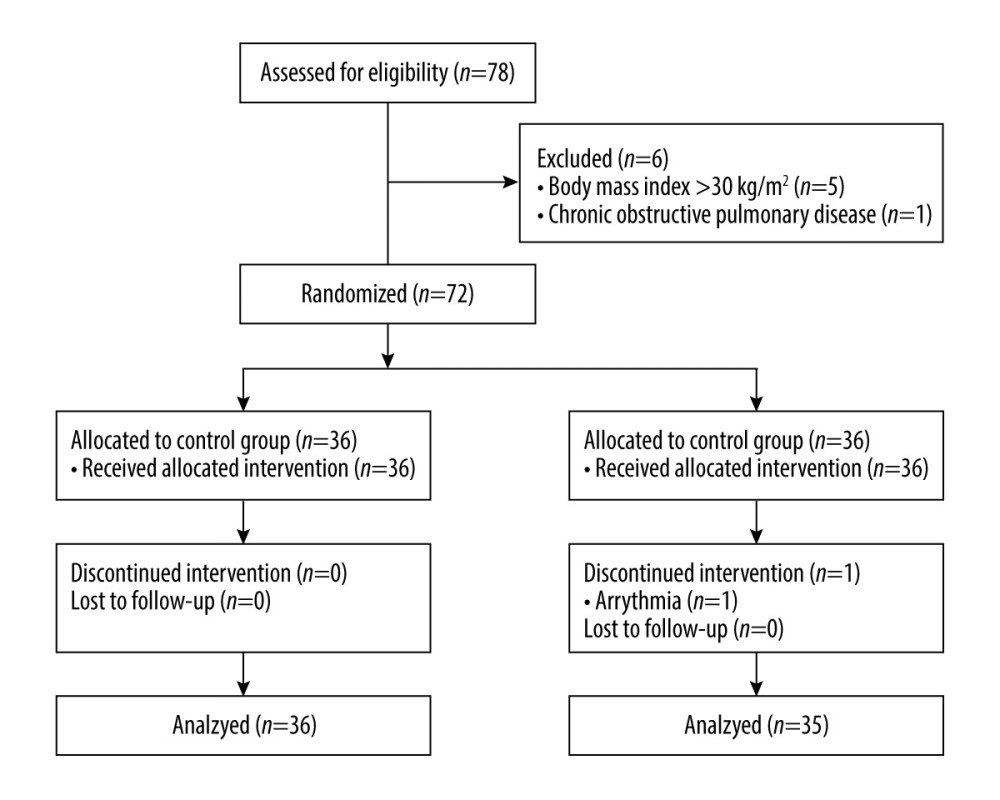 Figure 1. Flow diagram for patient enrollment. The control group was maintained in a neutral position without a pillow until endotracheal extubation. The head elevation group was maintained in a head-elevated position on a pillow until endotracheal extubation.
Figure 1. Flow diagram for patient enrollment. The control group was maintained in a neutral position without a pillow until endotracheal extubation. The head elevation group was maintained in a head-elevated position on a pillow until endotracheal extubation. 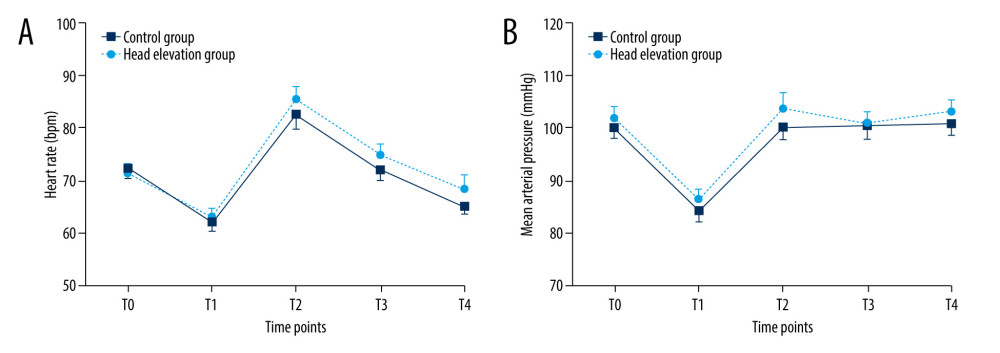 Figure 2. The (A) heart rate and (B) mean arterial pressure during perioperative period. Data are expressed as the mean±standard error. T0 – baseline (before anesthesia induction); T1 – at the end of surgery; T2 – immediately after extubation; T3 – 3 minutes after extubation; T4 – in the Post-Anesthesia Care Unit. The control group was maintained in a neutral position without pillow until the endotracheal extubation. The head elevation group was maintained in a head-elevated position on a pillow until the endotracheal extubation. There were no significant differences between the 2 groups in (A) and (B).
Figure 2. The (A) heart rate and (B) mean arterial pressure during perioperative period. Data are expressed as the mean±standard error. T0 – baseline (before anesthesia induction); T1 – at the end of surgery; T2 – immediately after extubation; T3 – 3 minutes after extubation; T4 – in the Post-Anesthesia Care Unit. The control group was maintained in a neutral position without pillow until the endotracheal extubation. The head elevation group was maintained in a head-elevated position on a pillow until the endotracheal extubation. There were no significant differences between the 2 groups in (A) and (B). References
1. Saeed F, Lasrado S, Extubation. [Updated 2023 Feb 9]: StatPearls [Internet], 2023, Treasure Island (FL), StatPearls Publishing Available from:https://www.ncbi.nlm.nih.gov/books/NBK539804/
2. Girard TD, Alhazzani W, Kress JP, An Official American Thoracic Society/American College of Chest Physicians Clinical Practice Guideline: Liberation from mechanical ventilation in critically ill adults. rehabilitation protocols, ventilator liberation protocols, and cuff leak tests: Am J Respir Crit Care Med, 2017; 195(1); 120-33
3. Tanios MA, Nevins ML, Hendra KP, A randomized, controlled trial of the role of weaning predictors in clinical decision making: Crit Care Med, 2006; 34(10); 2530-35
4. Wong TH, Weber G, Abramowicz AE, Smooth extubation and smooth emergence techniques: A narrative review: Anesthesiol Res Pract, 2021; 2021; 8883257
5. Kim ES, Bishop MJ, Cough during emergence from isoflurane anesthesia: Anesth Analg, 1998; 87(5); 1170-74
6. Irwin RS, Complications of cough: ACCP evidence-based clinical practice guidelines: Chest, 2006; 129(1 Suppl); 54s-58s
7. Tung A, Fergusson NA, Ng N, Hu V, Pharmacological methods for reducing coughing on emergence from elective surgery after general anesthesia with endotracheal intubation: Protocol for a systematic review of common medications and network meta-analysis: Syst Rev, 2019; 8(1); 32
8. Wasinwong W, Thongkhachok S, Kitsiripant C, Comparison of 40 and 100 mg of laryngotracheal lidocaine instillation to prevent cough during emergence from general anesthesia: A randomized controlled trial: Trends in Anaesthesia and Critical Care, 2023; 2023; 101235
9. Tung A, Fergusson NA, Ng N, Hu V, Medications to reduce emergence coughing after general anaesthesia with tracheal intubation: A systematic review and network meta-analysis: Br J Anaesth, 2020 [Online ahead of print]
10. Canning BJ, Chang AB, Bolser DC, Anatomy and neurophysiology of cough: CHEST Guideline and Expert Panel report: Chest, 2014; 146(6); 1633-48
11. Alexopoulos C, Larsson SG, Lindholm CE, The anatomical shape of the airway during endotracheal intubation: Acta Anaesthesiol Scand, 1983; 27(4); 331-34
12. Greenland KB, Edwards MJ, Hutton NJ, Changes in airway configuration with different head and neck positions using magnetic resonance imaging of normal airways: A new concept with possible clinical applications: Br J Anaesth, 2010; 105(5); 683-90
13. Haas CF, Eakin RM, Konkle MA, Blank R, Endotracheal tubes: old and new: Respir Care, 2014; 59(6); 933-52 discussion 952–55
14. Ham WH, Schoonhoven L, Schuurmans MJ, Leenen LP, Pressure ulcers in trauma patients with suspected spine injury: A prospective cohort study with emphasis on device-related pressure ulcers: Int Wound J, 2017; 14(1); 104-11
15. Li M, Yiu Y, Merrill T, Yildiz V, Risk factors for posttracheostomy tracheal stenosis: Otolaryngol Head Neck Surg, 2018; 159(4); 698-704
16. Burgess GE, Cooper JR, Marino RJ, Laryngeal competence after tracheal extubation: Anesthesiology, 1979; 51(1); 73-77
17. Bannister F, Macbeth R, Direct laryngoscopy and tracheal intubation: Lancet, 1944; 244; 651-54
18. Adnet F, Baillard C, Borron SW, Randomized study comparing the “sniffing position” with simple head extension for laryngoscopic view in elective surgery patients: Anesthesiology, 2001; 95(4); 836-41
19. Mohta M, Head elevation beyond sniffing position – an aid to airway management: J Anaesthesiol Clin Pharmacol, 2018; 34(2); 247-48
20. Khandelwal N, Khorsand S, Mitchell SH, Joffe AM, Head-elevated patient positioning decreases complications of emergent tracheal intubation in the Ward and Intensive Care Unit: Anesth Analg, 2016; 122(4); 1101-7
21. Jun N, Lee J, Song J, Optimal effect-site concentration of remifentanil for preventing cough during emergence from sevoflurane-remifentanil anaesthesia: Anaesthesia, 2010; 65(9); 930-35
22. Kondo T, Hayama N, Cough reflex is additively potentiated by inputs from the laryngeal and tracheobonchial receptors and enhanced by stimulation of the central respiratory neurons: J Physiol Sci, 2009; 59; 347-53
23. Eckerbom B, Lindholm CE, Alexopoulos C, Airway lesions caused by prolonged intubation with standard and with anatomically shaped tracheal tubes. A post-mortem study: Acta Anaesthesiol Scand, 1986; 30(5); 366-73
24. Nordang L, Lindholm CE, Larsson J, Linder A, Early laryngeal outcome of prolonged intubation using an anatomical tube: A double blind, randomised study: Eur Arch Otorhinolaryngol, 2016; 273(3); 703-8
25. Black J, Alves P, Brindle CT, Use of wound dressings to enhance prevention of pressure ulcers caused by medical devices: Int Wound J, 2015; 12(3); 322-27
26. Kayser SA, VanGilder CA, Ayello EA, Lachenbruch C, Prevalence and analysis of medical device-related pressure injuries: results from the international pressure ulcer prevalence survey: Adv Skin Wound Care, 2018; 31(6); 276-85
27. Moser CH, Peeler A, Long R, Prevention of endotracheal tube-related pressure injury: A systematic review and meta-analysis: Am J Crit Care, 2022; 31(5); 416-24
28. Jackson D, Sarki AM, Betteridge R, Brooke J, Medical device-related pressure ulcers: A systematic review and meta-analysis: Int J Nurs Stud, 2019; 92; 109-20
29. Horton WA, Fahy L, Charters P, Defining a standard intubating position using “angle finder”: Br J Anaesth, 1989; 62(1); 6-12
30. Greenland KB, Edwards MJ, Hutton NJ, External auditory meatus-sternal notch relationship in adults in the sniffing position: A magnetic resonance imaging study: Br J Anaesth, 2010; 104(2); 268-69
31. Adnet F, Borron SW, Lapostolle F, Lapandry C, The three axis alignment theory and the “sniffing position”: Perpetuation of an anatomic myth?: Anesthesiology, 1999; 91(6); 1964-65
32. El-Orbany MI, Getachew YB, Head elevation improves laryngeal exposure with direct laryngoscopy: J Clin Anesth, 2015; 27(2); 153-58
33. Herway ST, Benumof JL, The tracheal accordion and the position of the endotracheal tube: Anaesth Intensive Care, 2017; 45(2); 177-88
34. Nishino T, Kochi T, Ishii M, Differences in respiratory reflex responses from the larynx, trachea, and bronchi in anesthetized female subjects: Anesthesiology, 1996; 84(1); 70-74
35. Schiff BA, The relationship between body mass, tracheal diameter, endotracheal tube size, and tracheal stenosis: Int Anesthesiol Clin, 2017; 55(1); 42-51
36. Kim HY, Lee SY, Kang S, Effects of age on effect-site concentration of remifentanil for suppressing anesthetic emergence cough in male patients undergoing laparoscopic cholecystectomy: Clin Interv Aging, 2018; 13; 1053-60
Figures
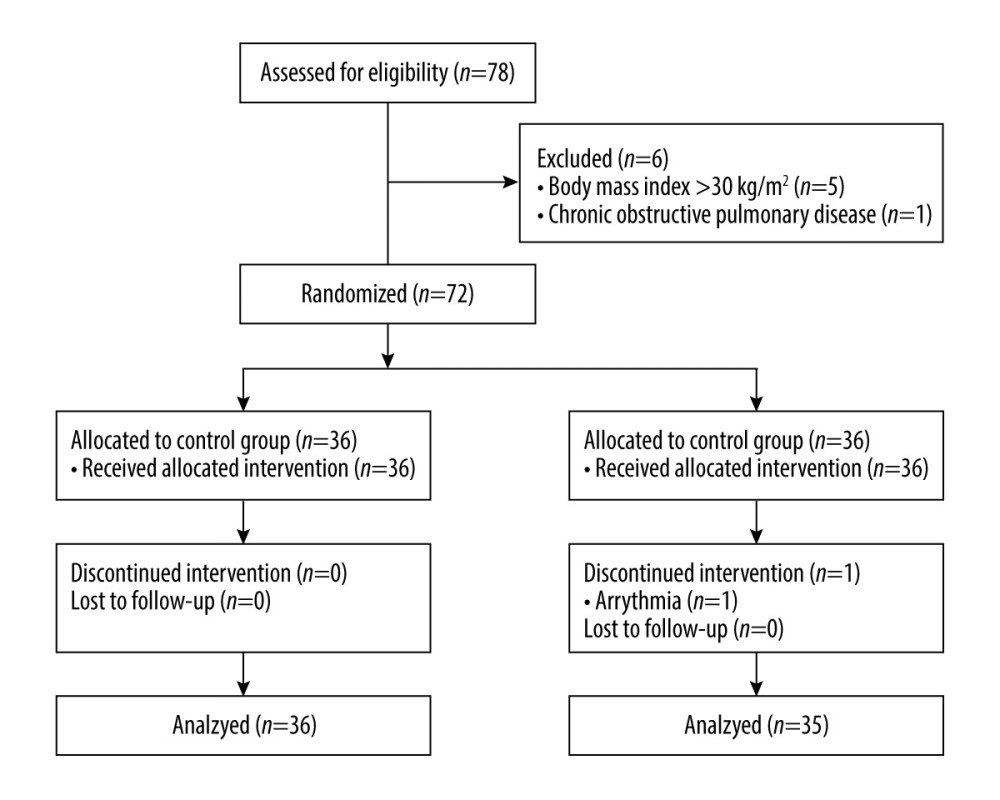 Figure 1. Flow diagram for patient enrollment. The control group was maintained in a neutral position without a pillow until endotracheal extubation. The head elevation group was maintained in a head-elevated position on a pillow until endotracheal extubation.
Figure 1. Flow diagram for patient enrollment. The control group was maintained in a neutral position without a pillow until endotracheal extubation. The head elevation group was maintained in a head-elevated position on a pillow until endotracheal extubation.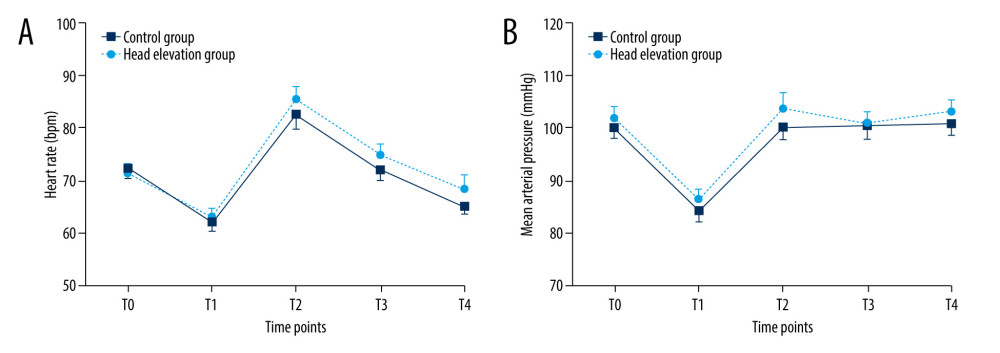 Figure 2. The (A) heart rate and (B) mean arterial pressure during perioperative period. Data are expressed as the mean±standard error. T0 – baseline (before anesthesia induction); T1 – at the end of surgery; T2 – immediately after extubation; T3 – 3 minutes after extubation; T4 – in the Post-Anesthesia Care Unit. The control group was maintained in a neutral position without pillow until the endotracheal extubation. The head elevation group was maintained in a head-elevated position on a pillow until the endotracheal extubation. There were no significant differences between the 2 groups in (A) and (B).
Figure 2. The (A) heart rate and (B) mean arterial pressure during perioperative period. Data are expressed as the mean±standard error. T0 – baseline (before anesthesia induction); T1 – at the end of surgery; T2 – immediately after extubation; T3 – 3 minutes after extubation; T4 – in the Post-Anesthesia Care Unit. The control group was maintained in a neutral position without pillow until the endotracheal extubation. The head elevation group was maintained in a head-elevated position on a pillow until the endotracheal extubation. There were no significant differences between the 2 groups in (A) and (B). Tables
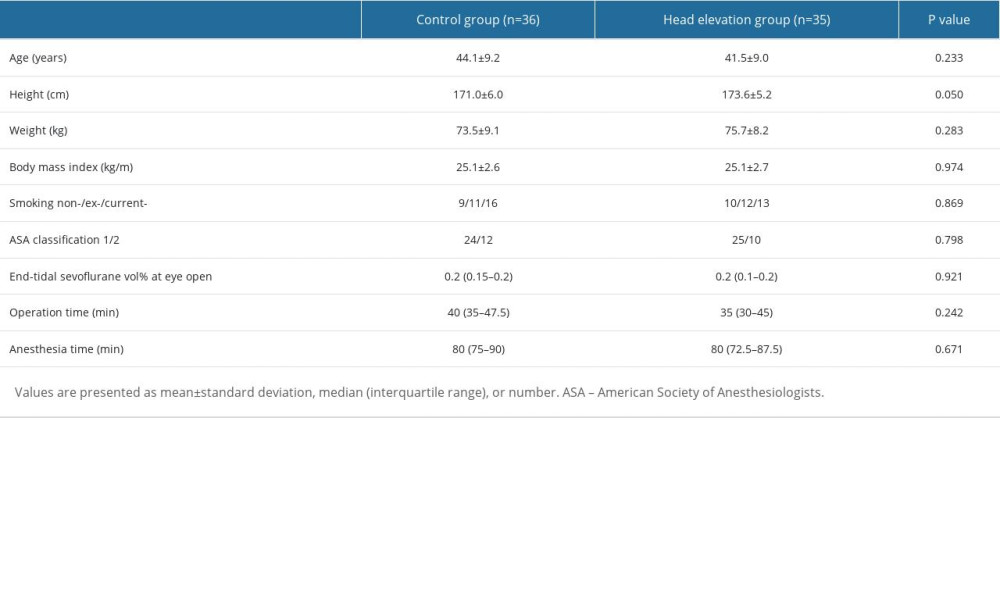 Table 1. Characteristics and intraoperative data of male patients.
Table 1. Characteristics and intraoperative data of male patients.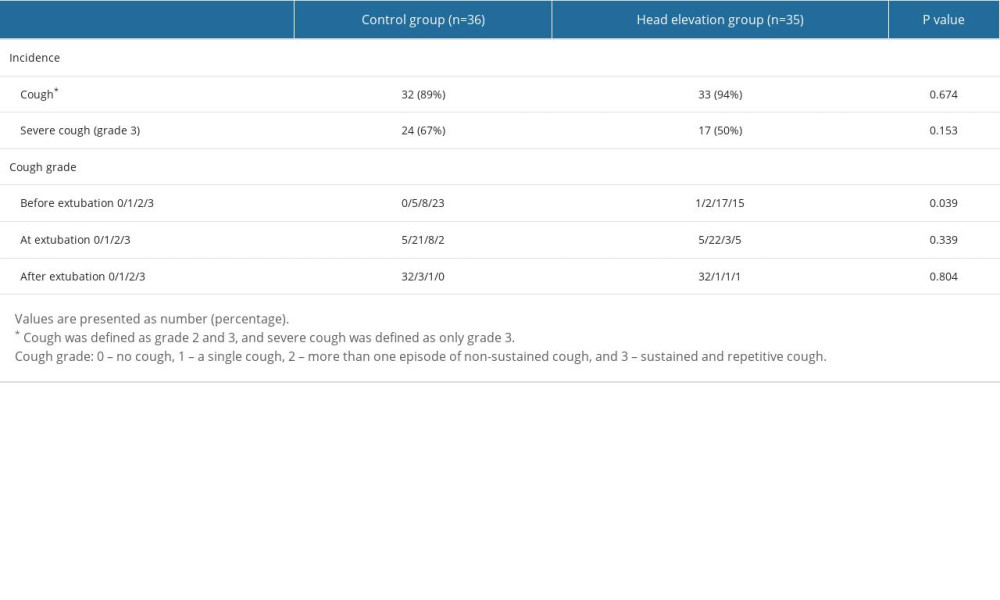 Table 2. Incidence and severity of cough.
Table 2. Incidence and severity of cough.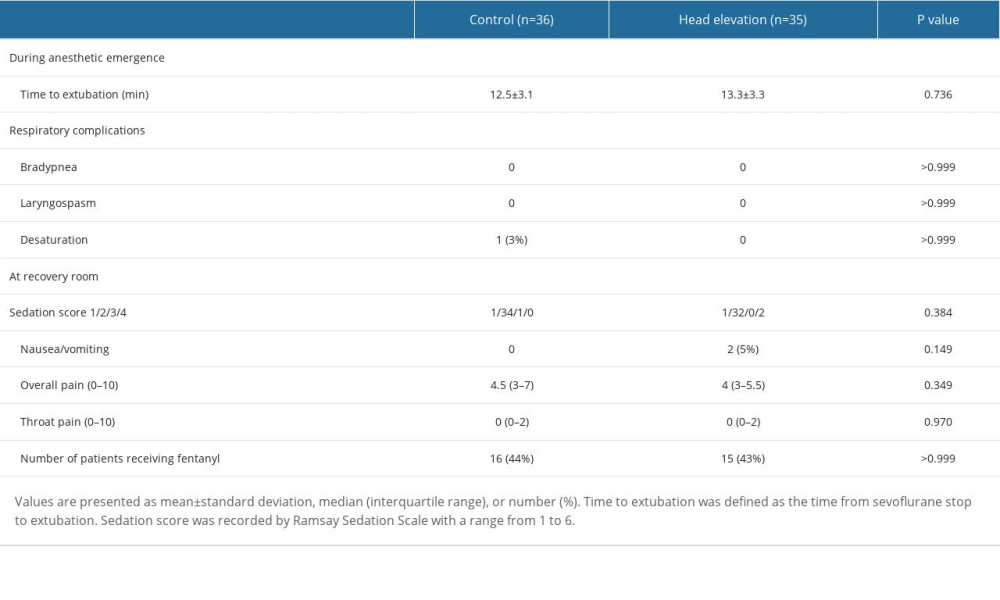 Table 3. Anesthetic emergence and recovery outcomes.
Table 3. Anesthetic emergence and recovery outcomes.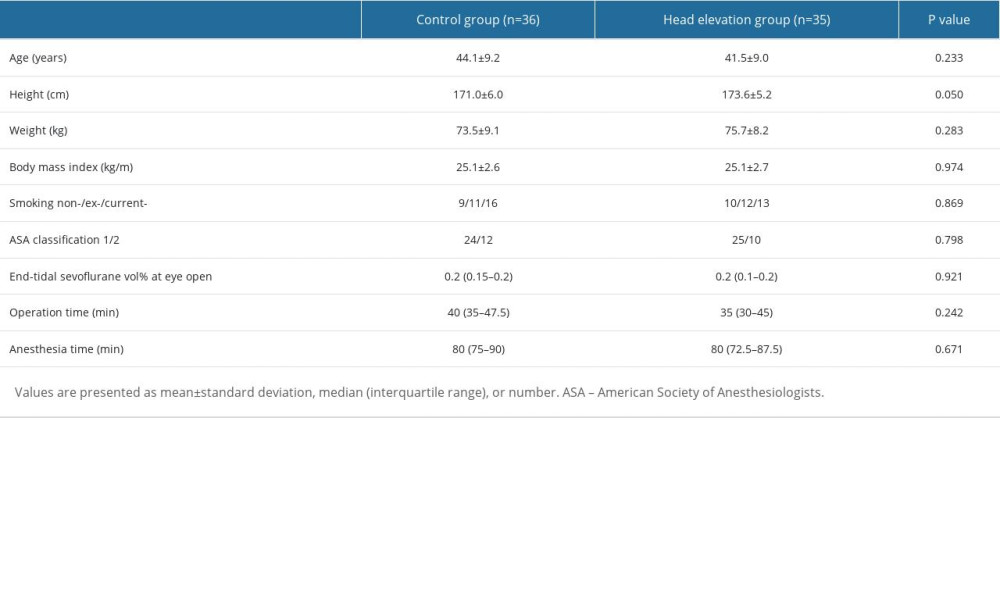 Table 1. Characteristics and intraoperative data of male patients.
Table 1. Characteristics and intraoperative data of male patients.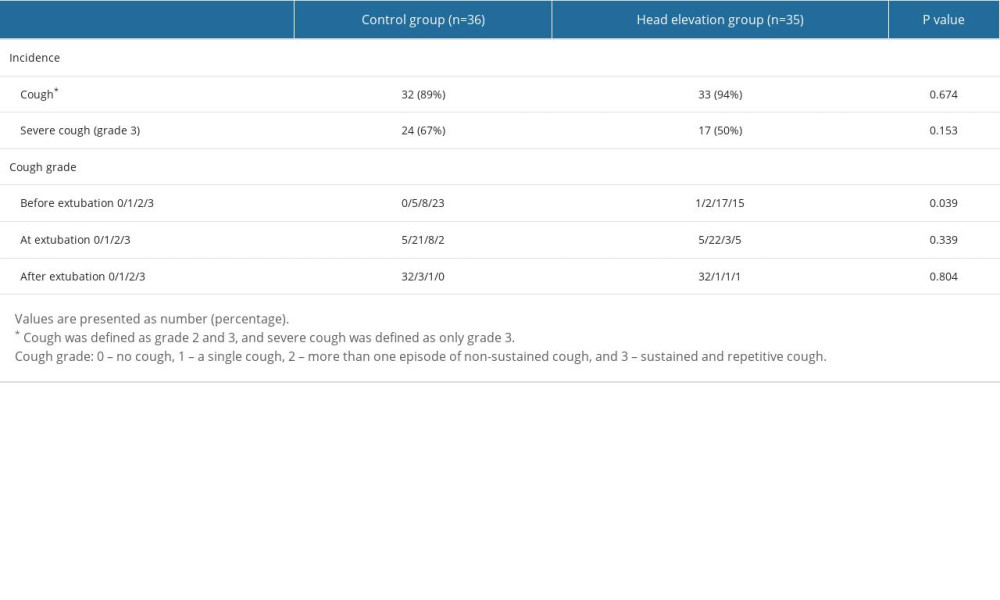 Table 2. Incidence and severity of cough.
Table 2. Incidence and severity of cough.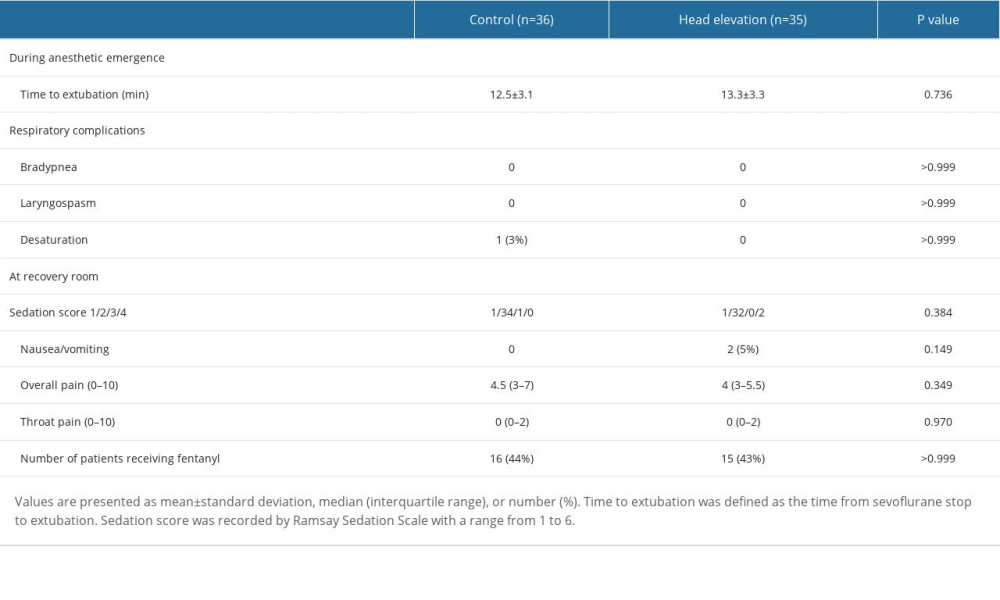 Table 3. Anesthetic emergence and recovery outcomes.
Table 3. Anesthetic emergence and recovery outcomes. In Press
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








