05 April 2024: Clinical Research
A Retrospective Study to Compare Patient Outcomes from Standard Total Knee Arthroplasty (TKA) versus Navigation-Guided Arthroplasty Using the Brainlab Software-Guided Surgical System at a Center in Hebei Province January 2021 to July 2023
Hao Pan1A, Meng Yang1B, Wen Hui Ji1C, Rui Zhi Cui1D, Guo Qiang Liu1D*DOI: 10.12659/MSM.942888
Med Sci Monit 2024; 30:e942888
Abstract
BACKGROUND: This retrospective study aimed to compare patient outcomes from standard total knee arthroplasty (TKA) vs navigation-guided arthroplasty using the Brainlab software-guided surgical system at Cangzhou Hospital of Integrated TCM-WM, Hebei, Hebei Province, China from January 2021 to July 2023.
MATERIAL AND METHODS: A total of 239 patients who underwent total knee arthroplasty in Cangzhou Hospital of Integrated TCM-WM, Hebei from January 2021 to July 2023 were retrospectively analyzed. According to the inclusion criteria, 212 eligible patients were selected for analysis and divided into a Navigation Group (NG) (n=105) and a Traditional Group (TG) (n=107) according to surgical method used. Outcomes measured included duration of disease, operative time, intraoperative blood loss volume, postoperative length of hospital stay, and pain measured by the hospital for special surgery knee score (HSS), Western Ontario and McMaster University Osteoarthritis Index (WOMAC), and forgotten joint score (FJS).
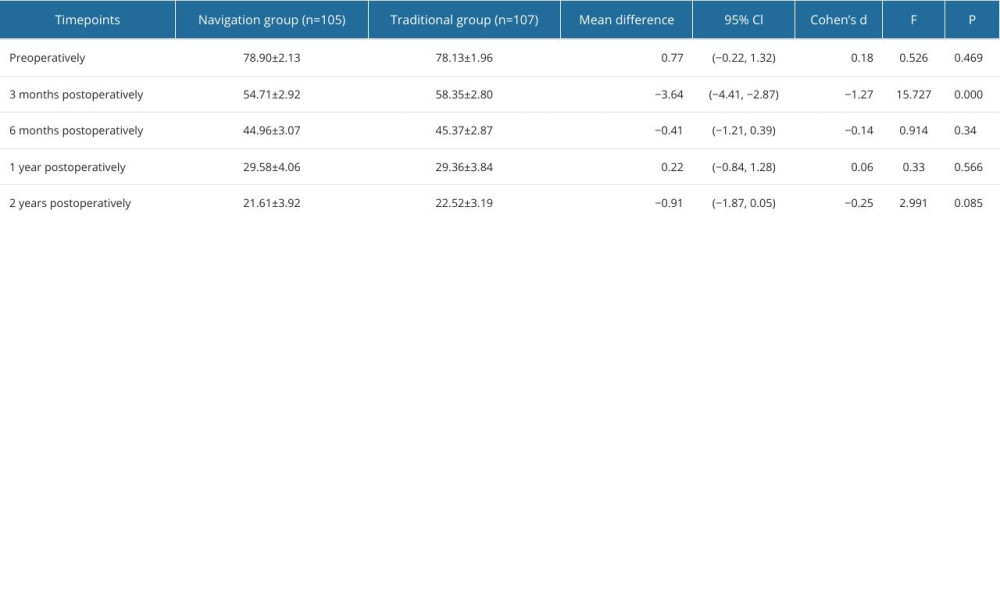
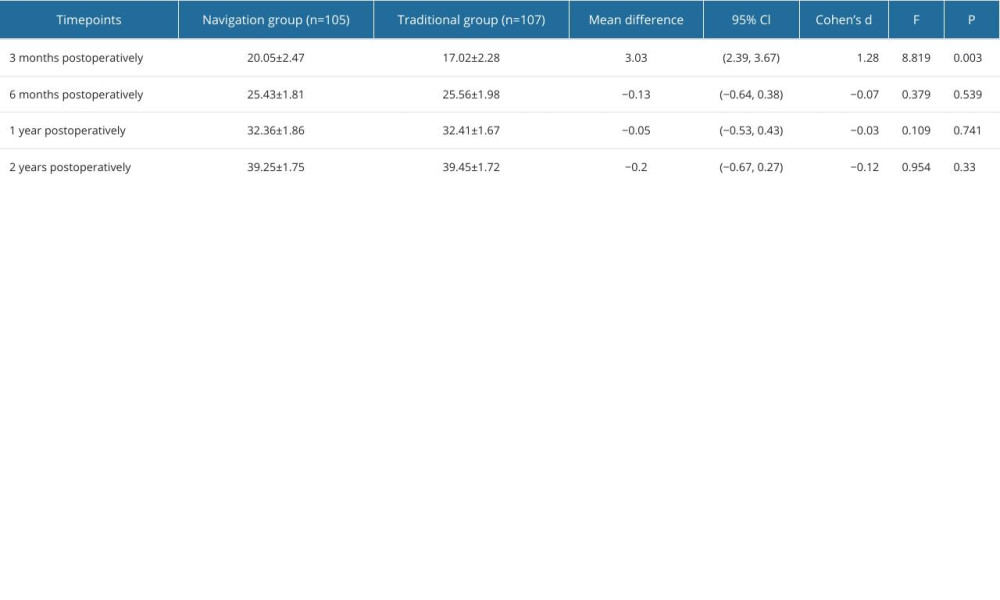
RESULTS: The comparison of perioperative results between the 2 groups showed that the incision length in the NG was significantly longer than that in the TG (P<0.001, 95% Cl 2.59-3.35). At 3 months after surgery, the HSS score of the NG was statistically higher than that of the TG (P=0.002, 95% Cl 3.42-4.46); the WOMAC score of the NG was lower than that of the TG (P<0.001, 95% Cl -4.41-2.87); and the FJS score of the NG was significantly higher than that of the TG (P=0.003, 95% Cl 2.39-3.67).
CONCLUSIONS: Compared with conventional TKA, use of the Brainlab navigation system is associated with a longer incision, more accurate implantation position of the prosthesis, faster recovery of knee joint function, and helps patients to “forget” about their knee prosthesis in the short term.
Keywords: Arthroplasty, Replacement, Knee, Surgical Navigation Systems
Introduction
Total knee arthroplasty (TKA) is a mature surgical technique that can effectively treat knee diseases such as end-stage knee osteoarthritis, rheumatoid knee arthritis, and traumatic knee arthritis, and can improve patient quality of life [1]. Hsu [2] reported that it is a good treatment option for patients with failed conservative treatment of knee osteoarthritis, and the design of prostheses has been continuously developing, focusing on restoring the anatomy and normal function of the knee joint. In addition, there have been advances in fixation techniques and wear characteristics of bearing surfaces, which have a positive impact on the service life of knee arthroplasty. Leitner [3] found that the number of primary TKAs performed varies widely among countries, with increasing annual number of knee replacements, decreasing relative number of revisions, and decreasing use of bone cement over the last decade. Nevertheless, the dissatisfaction rate of patients after conventional TKA approaches 20% [4]. Bae [5] concluded that postoperative patient dissatisfaction is mostly due to the need for femoral intramedullary localization in traditional TKA surgery, increasing the risk of surgical trauma, blood loss, fat embolism, thromboembolism, and insufficient localization accuracy, and differences in surgeon experience, which can cause surgical deviations, resulting in poor postoperative prosthesis position, alignment, and soft tissue imbalance, thus affecting functional recovery and prosthesis life.
Navigation-assisted TKA has been reported to prolong the service life of the prosthesis by achieving more accurate prosthesis position, more accurate alignment control at 1 degree error, and no need for femoral intramedullary localization during surgery, with less intraoperative bleeding and bone destruction due to an accurate positioning system [6]. Navigation systems are currently divided into accelerometer-based navigation (ABN) systems, conventional instrumentation (CONI) systems, and computer navigation (CN) systems. Among them, the ABN method has shorter operation time and lower cost. The ABN system also significantly improved the accuracy of component alignment compared to the CONI method, despite longer operative times [7]. Conteduca [8] showed that although there are cutting blocks to fix the osteotomy angle and extent of osteotomy in traditional TKA, the accuracy is still deficient, multiple repeated osteotomies are sometimes required, and the flattening of the osteotomy surface needs to be visually verified. Navigation-assisted TKA can accurately cut and the verifier is used to verify the extent of osteotomy and angle change after osteotomy. The application of a TKA navigation system not only reduces the number of osteotomies, but also accurately determines the alignment, which is a more appropriate position for the prosthesis placement. Pan [9] found that the Brainlab Knee3 navigation aid system can fine-tune the femur and tibia cut angles based on soft tissue conditions to reduce soft tissue loosening and is a more accurate position of the prosthesis. However, there are also some reports [10,11] that navigation-assisted TKA and conventional TKA showed similar clinical results on knee score, functional recovery outcome, and radiographic evaluation. Most reports on the results after navigation-assisted TKA focused on the perioperative period or knee joint function recovery, and did not evaluate the postoperative efficacy in combination with imaging results and “forgotten” joint score.
Therefore, the present retrospective study aimed to compare patient outcomes from standard total knee arthroplasty (TKA) vs navigation-guided arthroplasty using the Brainlab software-guided surgical system at a center in Hebei Province between January 2021 to July 2023.
Material and Methods
Participants and surgical methods
INCLUSION AND EXCLUSION CRITERIA:
The study was approved by the Ethics Committee of Cangzhou Hospital of Integrated TCM-WM, Hebei (approval number: 2021-KY-085.1). This was a retrospective study with anonymized data, and the requirement for informed consent was waived.
Inclusion criteria: (1) Patients with knee osteoarthritis (OA, M17) of Kellgren-Lawrence grade III or IV on X-ray; (2) Patients who were initially treated with TKA; (3) The follow-up time was 1 year or more; (4) Voluntarily received treatment using the navigation system treatment plan.
Exclusion criteria: (1) Severe knee joint deformity with preoperative flexion range of motion <90°, valgus deformity >15° or varus deformity >30°, severe joint bone defect that could affect prosthesis selection; (2) Bone or joint infections; (3) Autoimmune diseases; (4) Patients with incomplete medical records or radiological images; (5) Patients with surgical contraindications who cannot tolerate surgery; (6) Knee stability is poor and hinge prostheses must be used.
SAMPLE SIZE CALCULATION: The sample size needed to achieve sufficient statistical power was calculated using repeated measures analysis. The design involved measurements at 5 time points for both groups, with the goal of ensuring at least 90% power at an alpha level of 0.05. PASS 15.0 software calculation results showed that to detect the effect between groups, 98 subjects per group were required, with 196 in total. This power calculation was based on an effect size of 0.233, the standard deviation between means was 0.14 with a standard deviation of 0.60. After accounting for an anticipated 20% subject attrition rate, the total sample size was adjusted to 246 to ensure adequate power for analysis [12–14].
PARTICIPANTS:
This study retrospectively analyzed 239 patients who underwent total knee arthroplasty in our hospital from January 2020 to July 2023. According to the inclusion criteria, 212 eligible patients were selected for analysis and divided into the Navigation Group (n=105) and Traditional Group (n=107) according to the surgical method used. The data extraction process was designed to ensure the accuracy, consistency, and completeness of the study data.
Eligible patient records were screened through the hospital ‘s electronic medical record system according to the inclusion and exclusion criteria for the study. Advanced search functions were used to filter by keywords such as date of surgery and type of surgery. We designed a dedicated data extraction form that covered the patient’s basic information, perioperative data, radiographic data, and postoperative scores (HSS score, WOMAC score, and FJS score). Two trained researchers independently performed data extraction to reduce bias and entered the data into a pre-specified electronic database. To ensure the accuracy of the data, the extracted data were double-checked. After completion of data entry, some data were rechecked by random sampling to verify completeness and accuracy of data. Any discrepancies or questions encountered were collectively discussed and resolved by the study team. All data were de-identified to ensure patient privacy was protected. Missing data were handled using appropriate statistical methods to reduce their impact on study results.
Treatment compliance was achieved in 98% of patients undergoing total knee arthroplasty (TKA) with the Brainlab navigation system (the NG). In comparison, patients who underwent conventional TKA (the TG) had a treatment compliance rate of 96%. This high degree of treatment compliance reflects the patient ‘s good acceptance of both surgical approaches and their willingness to follow a postoperative recovery plan. During the study period, the NG had a dropout rate of 2%, mainly due to postoperative adverse reactions and personal selection. The TG had a slightly higher withdrawal rate of 4%; the reasons for withdrawal included postoperative complications and personal reasons. All patients who withdrew from the study were appropriately documented and subsequently managed to ensure patient safety. Reported adverse effects in the NG included postoperative infection (1%), prosthesis loosening (0.5%), and thrombosis (1%). Adverse effects in the TG included postoperative infection (2%), prosthesis loosening (1%), and thrombosis (1.5%). No cases of nerve injury were reported in either group. All patients who had adverse effects received prompt and appropriate treatment to minimize potential health risks.
In summary, TKA performed with the Brainlab navigation system showed lower dropout rates and adverse effects rates compared to conventional surgical methods, while maintaining high treatment compliance. This result further supports the potential of navigated surgery to improve the safety and efficacy of knee arthroplasty.
SURGICAL METHODS:
All procedures were performed by experienced chief surgeons, with Smith & Nephew (Smith & Nephew, London, UK) selected for prostheses, and preoperative templating was routinely performed in all patients.
In the NG, we used the medial parapatellar approach through an anterior midline incision of the knee. A tracer ball was placed on the medial side of the distal femur and the medial side of the middle and upper tibia, each reference point of the hip, knee and ankle joints was registered successively, and the tension of the medial and lateral ligaments was assessed to complete the modeling and develop a surgical plan. The Brainlab Knee3 navigation system (Brainlab, Munich, Germany) places osteotomy guides under the femoral and tibial osteotomy to verify the osteotomy effect, release soft tissue according to the gap curve, balance flexion, and extension gaps, and install the prosthesis.
In the TG, we used a medial parapatellar approach through anterior midline knee incision, extramedullary tibial localization, intramedullary femoral localization osteotomy followed by compression tamponade of the femoral medullary bone graft, patellar trimming, denervation, release of soft tissue balance flexion and extension gaps, and installation of prostheses.
POSTOPERATIVE MANAGEMENT:
Antibiotics were routinely administered postoperatively. Low-molecular-weight heparin sodium was administered until discharge and oral rivaroxaban was administered until 35 days after surgery. Postoperative rehabilitation instructions were given by a professional nurse and rehabilitator. On the first day after surgery, the patient was instructed to sit up in bed and perform an ankle pump exercise while performing quadriceps contraction exercise, and active or passive exercise methods could be selected according to the patient’s recovery. On the third day after the operation, patients without thrombosis were instructed to perform a bed support exercise after color Doppler ultrasound of the lower extremity, and were asked to sit at the edge of the bed and hook the affected leg with the unaffected leg for knee flexion and extension activities; at the same time, the patient was instructed to maintain hip flexion of 40° and relax after 15 s to enhance the muscle strength of the quadriceps femoris and hamstring muscles. In addition, the patient could get out of bed and walk with the help of nursing staff, walking aids, and other devices, and gradually increase the walking distance according to physical condition. Ice compress was given according to swelling of the surgical limb.
OUTCOME MEASURES:
The basic information and general condition of the patient were recorded, including age, sex, height, body mass index (BMI), alcohol consumption, and smoking. The duration of surgery, intraoperative bleeding, length of incision, and length of hospital stay were also recorded.
All patients were followed up clinically and radiologically at 3, 6, and 12 months after surgery, and then annually. HSS knee score, McMaster Universities Osteoarthritis Index score (WOMAC), and FJS were assessed at each follow-up visit to determine knee function after TKA.
IMAGING:
According to the weight-bearing ability, full-length radiographs of the lower limbs were taken 1 month after surgery, and the proximal medial angle (mMPTA) of the tibia was measured, including the medial angle between the mechanical axis of the tibia and the tangent of the tibial prosthesis, with a target value of 90°, <90° for varus, >90° for valgus, and varus and valgus more than 3° defined as the position deviation of the tibial prosthesis. To assess the lateral mechanical distal femur angle (mLDFA), we determined the lateral angle between the mechanical axis of the femur and the tangent line between the distal end of the femoral prosthesis, with a target value of 90°, >90°for varus, <90°for valgus, and varus more than 3° defined as femoral prosthesis position deviation. Hip-knee-ankle angle (HKA): the lateral angle of the midpoint line of the hip, knee, and ankle joints, and the target of the HKA angle is 180°, >180° is varus, and <180° is valgus; the HKA angle deviation angle is calculated, and varus and valgus more than 3°is defined as lower limb alignment deviation. We obtained each angle deviation value by comparing it with the set value. Angular measurements were performed by 2 senior orthopedic surgeons and the final results were averaged. If the difference between the 2 was too large (≥0.5°), it was measured by a third senior orthopedic surgeon, and the final result was the average of the 2 measured values that are most similar among the 3.
STATISTICAL ANALYSIS:
IBM SPSS 22.0 (IBM Corp. Armonk, NY, USA) statistical software was used for data analysis. The chi-square test was used to compare categorical variables such as gender and side of surgery. The independent sample
Results
BASELINE PATIENT PROFILES:
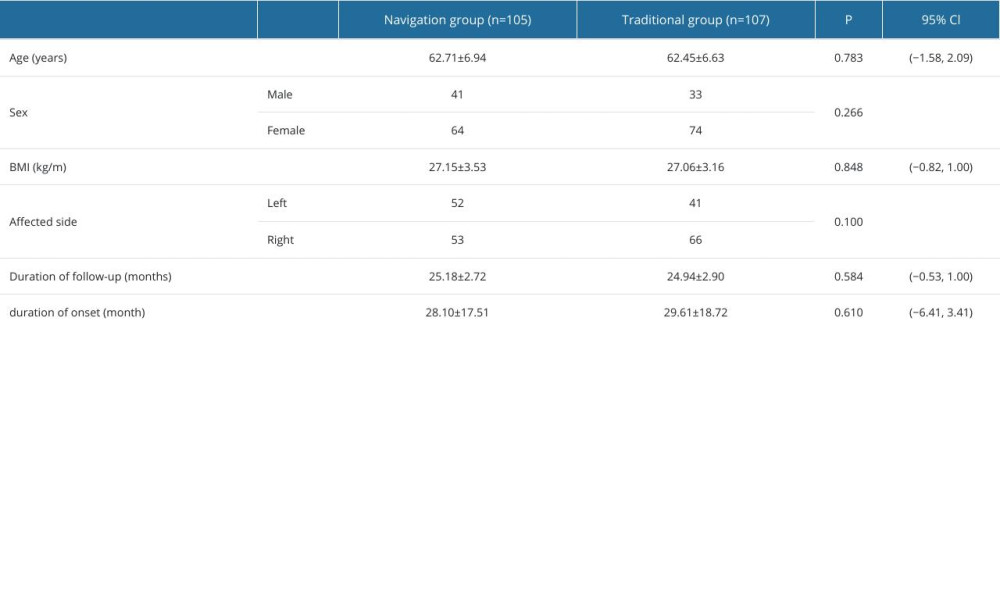
The general data of patients in the NG were not significantly different from those in the TG, including age, sex ratio, BMI, side, follow-up year and month, and time from onset (P>0.05) (Table 1).
PERIOPERATIVE RESULTS:
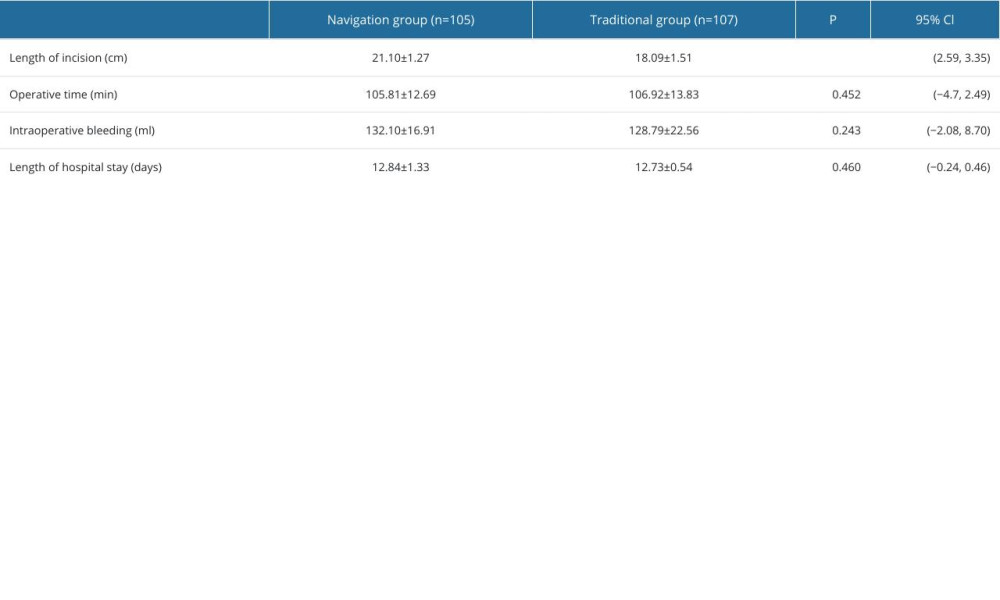
There were no statistically significant differences between groups in operation time, hospital stay, and intraoperative blood loss (P>0.05). Operative time was significantly longer in the NG than in the TG (P<0.001, 95% Cl 2.59–3.35) (Table 2).
COMPARISON OF FUNCTIONAL SCORES BETWEEN THE 2 GROUPS:
To assess the effect of surgical intervention, hospital-specific surgical scores (HSS) were compared between 2 independent groups at 5 different time points (preoperatively, 3 months postoperatively, 6 months postoperatively, 1 year postoperatively, and 2 years postoperatively) using repeated measures analysis of variance (repeated measures ANOVA). This analysis considered incision length (cm), operative time (min), intraoperative blood loss (ml), and length of hospital stay (days) as covariates to control for possible effects of these variables on HSS scores.
We investigated the effect of different surgical modalities (navigated versus traditional) on HSS scores over time by repeated measures analysis of variance. The differences between groups in the Motchley’s sphericity test (W=.702, chi-square=73.813, df=9,
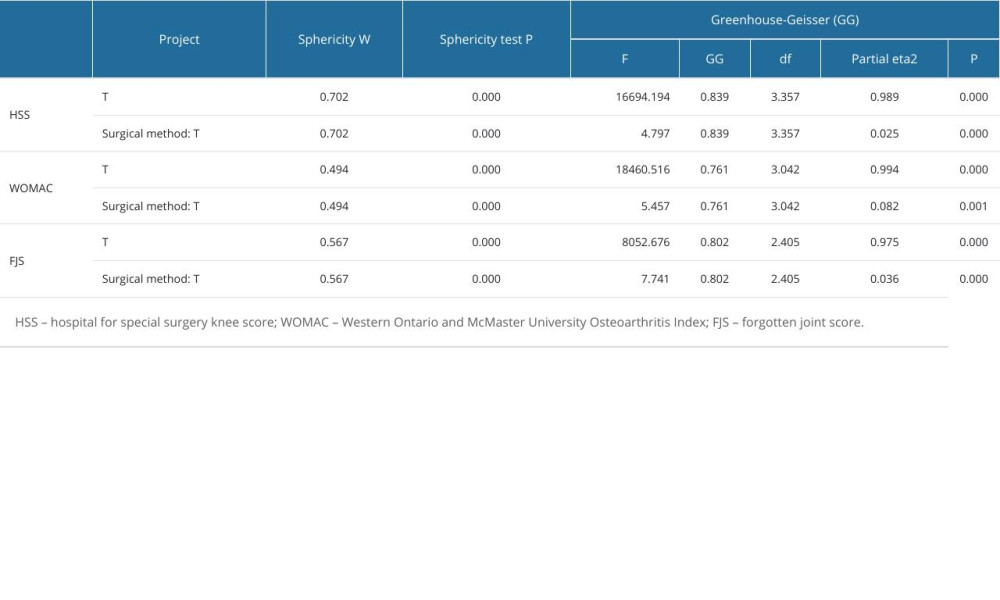
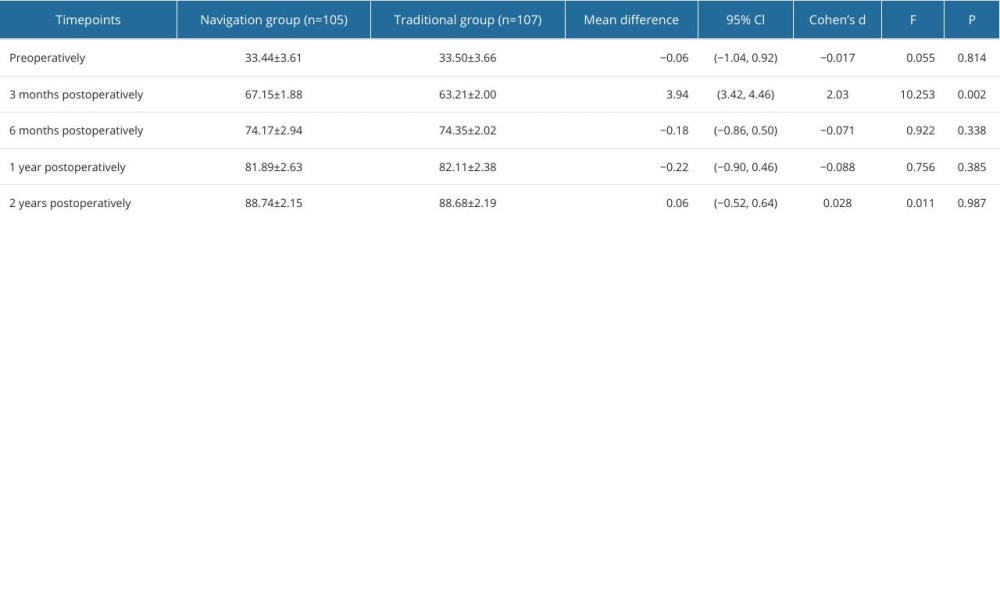
We investigated the effect of surgical approach on HSS score, WOMAC score, and FJS score in depth by repeated measures analysis of variance, with special attention to the time effect and its interaction with surgical approach. The analysis showed that the time effect had a significant effect on HSS score (F=16694.194, P<0.000, partial eta2=0.989), WOMAC score (F=18460.516, P<0.000, partial eta2=0.994), and FJS score (F=8052.676, P<0.000, partial eta2=0.975), indicating that these scores changed significantly over time, further emphasizing the important role of time in the postoperative recovery process. In addition, the interaction between surgical approach and time was significantly different in HSS score (F=4.797, P<0.000, partial eta2=0.025), WOMAC score (F=5.457, P=0.001, partial eta2=0.082), and FJS score (F=7.741, P<0.000, partial eta2=0.036), revealing that different surgical approaches have significantly different effects on the quality of postoperative recovery. To investigate the postoperative recovery effect of the 2 different surgical methods, the simple effect was further examined. HSS knee scores at 3 months after surgery were significantly higher in the TG (P=0.002, 95% Cl 3.42–4.46). WOMAC scores 3 months after surgery were significantly lower in the NG (P<0.001, 95% Cl −4.41–2.87). The scores at 6 months, 1 year, and 2 years after surgery were similar. The reference Cohen ‘s criterion was used, where 0.2 was considered a small effect, 0.5 was a medium effect, and above 0.8 was a large effect (Tables 3–6).
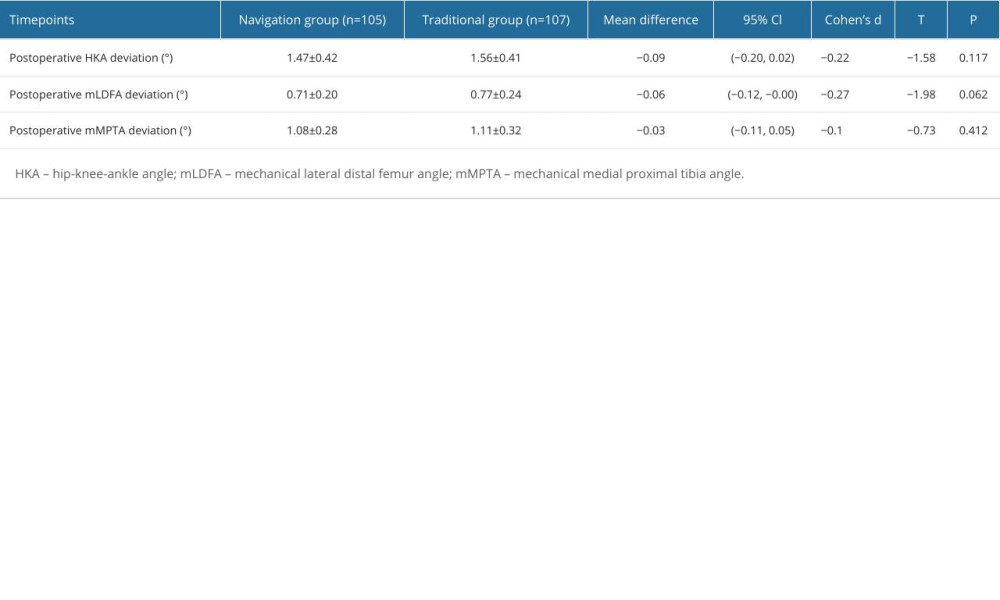
COMPARISON OF IMAGING INDICATORS BETWEEN THE 2 GROUPS:
The deviation of hip-knee-ankle angle group, lateral angle of distal femur, and medial angle of proximal tibia in NG was less than in the TG, but the difference was not significantly different (P>0.05) (Table 7).
Discussion
Although there are many reports on the efficacy of TKA in patients with knee osteoarthritis, most of them have focused on the efficacy of traditional TKA, and there are few reports on use of navigation system TKA. Whether navigated or conventional TKA, the aim of surgery is to reconstruct lower limb alignment and soft tissue balance and restore knee function [15]. Shah [16] showed that navigation system TKA has the advantages of accurate intraoperative osteotomy, avoiding multiple repeated osteotomies, and causing less soft tissue damage, as well as having shorter intraoperative operation time and less intraoperative blood loss than traditional TKA. Hickey [17] found that although accurate osteotomy was performed, there was no significant difference in operation time or intraoperative blood loss between navigated TKA and conventional TKA, possibly because the surgeon could skillfully master the surgical steps, and reported there was a significant difference in operation time, intraoperative blood loss, and hospital stay. The intraoperative incision length with the navigation system was significantly longer than in traditional TKA. Because the navigation system TKA needs to locate the femur and tibia, the intraoperative proximal incision length is longer [18].
The present study showed that the HSS knee score and WOMAC score of conventional system TKA were higher than those of the traditional TKA group in the first 3 months after the operation because the navigation system TKA improves the accuracy of osteotomy and quantifies the flexion and extension gap values, which can guide the surgeon to perform minimally invasive and accurate soft tissue release after osteotomy, obtain good gap balance and soft tissue tension, and restore the natural knee kinematic characteristics [19]. With soft tissue recovery, knee function showed similar functional outcomes in both groups from 6 months until last follow-up.
This study demonstrated that the navigation system performed significantly better than traditional TKA in patients undergoing TKA for knee OA after the first year. Patients in both groups tended to feel less discomfort over time after knee arthroplasty, indicating that there is a significant time dependence. In the short term, navigation system TKA patients tended to be able to “forget” about the knee prosthesis earlier and faster.
As a high-precision surgical aid, the Brainlab navigation system impacts surgical results by improving prosthesis positioning accuracy through the following mechanisms. (1)
This study has some limitations, including the short follow-up time and small sample size, and did not perform long-term knee function evaluation after surgery. Studies with larger sample sizes and longer follow-up periods are needed. By comparing the surgical reports and postoperative review of imaging data, we found that not all navigated TKA patients had postoperative imaging consistent with the surgical plan, which may be due to unclear anatomical landmarks and joint degeneration that seriously interfered with the accuracy of registration. In the future, follow-up should be continued, study cases should be supplemented, and clinical indicators such as test results and complications should be added for multifaceted analysis.
Conclusions
We compared outcomes of patients with knee osteoarthritis who underwent TKA with 2 different methods. Compared with the Traditional Group, the Navigation Group had longer incision, more accurate prosthesis implantation, faster recovery of joint function in the early stage, and easier to “forget” self-implanted knee prosthesis after surgery. Use of navigation is recommended for total knee arthroplasty.
References
1. Dong ZY, Li Y, Tian H, Research progress in application of patient-reported outcome measures in total knee arthroplasty: Zhongguo Yi Xue Ke Xue Yuan Xue Bao, 2023; 45(2); 327-33
2. Hsu H, Siwiec RMStatPearls: Knee arthroplasty, 2023, Treasure Island (FL), StatPearls Publishing Copyright© 2023, StatPearls Publishing LLC
3. Leitner L, Hauer G, Rasic L, Development of application and surgical technique of total knee arthroplasties: A systematic comparative analysis using worldwide registers: Arch Orthop Trauma Surg, 2023; 12(4); 125-29
4. Karasavvidis T, Pagan Moldenhauer CA, Haddad FS, Current concepts in alignment in total knee arthroplasty: J Arthroplasty, 2023; 38(7); S29-S37
5. Bae DK, Song SJ, Heo DB, Does the severity of preoperative varus deformity influence postoperative alignment in both conventional and computer-assisted total knee arthroplasty?: Knee Surg Sports Traumatol Arthrosc, 2013; 21(10); 2248-54
6. Zabat MA, Oakley CT, Marwin SE, The learning curve associated with imageless navigation in total knee arthroplasty: Arch Orthop Trauma Surg, 2023; 143(2); 1013-19
7. Luan Y, Wang H, Zhang M, Comparison of navigation systems for total knee arthroplasty: A systematic review and meta-analysis: Front Surg, 2023; 10(1); 101-7
8. Conteduca F, Massai F, Iorio R, Blood loss in computer-assisted mobile bearing total knee arthroplasty. A comparison of computer-assisted surgery with a conventional technique: Int Orthop, 2009; 33(6); 1609-13
9. Pan Y, Jiang B, Li Y, Alignment analysis of Brainlab knee 3 navigation-guided total knee arthroplasty using the adjusted mechanical method: Front Surg, 2022; 9; 21-26
10. Marques CJ, Daniel S, Sufi-Siavach A, No differences in clinical outcomes between fixed- and mobile-bearing computer-assisted total knee arthroplasties and no correlations between navigation data and clinical scores: Knee Surg Sports Traumatol Arthrosc, 2015; 23(6); 1660-68
11. Hantouly AT, Ahmed AF, Alzobi O, Mobile-bearing versus fixed-bearing total knee arthroplasty: A meta-analysis of randomized controlled trials: Eur J Orthop Surg Traumatol, 2022; 32(3); 481-95
12. Muller KE, Lavange LM, Ramey SL, Power calculations for general linear multivariate models including repeated measures applications: J Am Stat Assoc, 1992; 87(420); 1209-26
13. Muller KE, Edwards LJ, Simpson SL, Statistical tests with accurate size and power for balanced linear mixed models: Stat Med, 2007; 26(19); 3639-60
14. Simpson SL, Edwards LJ, Muller KE, A linear exponent AR(1) family of correlation structures: Stat Med, 2010; 29(17); 1825-38
15. Dai FL, Zhang P, Tian DWCase-control study on midterm follow-up effects of the extended release of posterior clearance in total knee arthroplasty: Zhongguo Gu Shang, 2015; 28(10); 888-92 [in Chinese]
16. Shah SM, After 25 years of computer-navigated total knee arthroplasty, where do we stand today?: Arthroplasty, 2021; 3(1); 41-45
17. Hickey MD, Anglin C, Masri B, Reply to the letter to the Editor: How large a study is needed to detect TKA revision rate reductions attributable to robotic or navigated technologies? A simulation-based power analysis: Clin Orthop Relat Res, 2022; 480(4); 838-41
18. Antonios JK, Kang HP, Robertson D, Population-based survivorship of computer-navigated versus conventional total knee arthroplasty: J Am Acad Orthop Surg, 2020; 28(20); 857-64
19. Aletto C, Zara A, Notarfrancesco D, Computer assisted total knee arthroplasty: 2.5 years follow-up of 200 cases: Surgeon, 2021; 19(6); e394-e401
20. Liu HX, Shang P, Ying XZ, Shorter survival rate in varus-aligned knees after total knee arthroplasty: Knee Surg Sports Traumatol Arthrosc, 2016; 24(8); 2663-71
21. Oh SM, Bin SI, Kim JY, Does the preoperative varus deformity influence the survival of postoperative neutral-aligned TKAs? An analysis with a minimum 5-year follow-up: J Arthroplasty, 2018; 33(10); 3181-85
22. Anderl W, Pauzenberger L, Kölblinger R, Patient-specific instrumentation improved mechanical alignment, while early clinical outcome was comparable to conventional instrumentation in TKA: Knee Surg Sports Traumatol Arthrosc, 2016; 24(1); 102-11
In Press
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952