12 February 2024: Lab/In Vitro Research
Evaluation of the Milled and Three-Dimensional Digital Manufacturing, 10-Degree and 20-Degree Preparation Taper, Groove and Box Auxiliary Retentive Features, and Conventional and Resin-Based Provisional Cement Type on the Adhesive Failure Stress of 3 mm Short Provisional Crowns
Mohammed SayedDOI: 10.12659/MSM.943237
Med Sci Monit 2024; 30:e943237
Abstract
BACKGROUND: This study evaluated the effects of milling (CADCAM), 3D printing, preparation taper angles (10-degree and 20-degree), auxiliary retentive features (groove and box), and provisional cement types (conventional and resin-based) on the adhesive failure stress of 3-mm short provisional crowns (PC). The research was motivated by the need to understand how digital dentistry technologies impact the retention and durability of provisional crowns.
MATERIAL AND METHODS: A total of 160 working models (3D-printed) and PCs [80 milled (CopraTemp)/80 printed (Asiga)] were fabricated from two 10- and 20-degree typodont master models and two 20-degree 3D-printed master models (groove and box), simulating a 3 mm high all-ceramic short PC. After provisional cementation with conventional (Kerr TempBond) and resin-based (ProviTemp) cements, 16 subgroups (n=10 each) underwent thermocycling (10 000 cycles; 5-55°C) and pull-off tests on a universal testing machine. Statistical analysis was performed using one-way ANOVA and post hoc Tukey test.
RESULTS: Conventional cement failed at lower stress for milled (47.68 to 73.54) and printed (48.40 to 77.91) as compared to resin cement for milled (104.2 to 137.27) and printed (184.85 to 328.84), respectively, with significant differences. Increased taper and groove decreased failure load except for the printed PC/resin cement combination. Use of proximal box preparation increased retention significantly. Except for 20-degree taper cemented with conventional cement, the differences in auxiliary retentive features for milled and printed provisional crowns were statistically significant at P≤0.05.
CONCLUSIONS: 3D-printed PC, resin-based cement, 10-degree taper, and proximal box preparation were associated with higher retention than milled, conventional cements, 20-degree taper, and vertical groove.
Keywords: Computer-Aided Design, Crowns, Dental Restoration Failure, Denture, Partial, Temporary, Printing, Three-Dimensional
Background
Despite implant restorations conservative transformation of natural teeth to support and retain a missing tooth, the conventional fixed dental prosthesis (FDP) continues to be one of the most common restorative dental practices [1]. Both restorative decisions require a fully functional and clinically successful provisional restoration (PR) in either the form of a single provisional crown (PC) or multi-unit provisional fixed dental prosthesis (PFDP), for either short- or long-time durations that are based on treatment objectives. Likewise, very often in clinical practice, clinicians find it difficult to remove a PC/PFDP, yet many patients report to clinicians that their PR came out, causing them severe discomfort and pain. PR defines and verifies therapeutic treatment benefits for the clinician, be it either during treatment preparation like crown lengthening [2], total occlusal rehabilitation [3], altering vertical occlusal dimensions [4], and progressive implant loading [5], or fulfilling and predicting the patient’s treatment expectations from definitive prosthesis [3,4]. Depending upon the treatment objective in different fixed prosthodontic treatment scenarios, a PC/PFDP may be required to serve the functional purpose for 6–12 months without retentive failure. Interdisciplinary conservative orthodontic treatments may also require a provisional crown for long-term function. In FDP treatments, the PR is cemented on the final prepared tooth that can no longer be altered further since it is destined to hold the definitive restoration. The wearing of the PR by a particular patient helps clinician to predict the most likely treatment outcome in terms of restoring functions and esthetics. Thus, principles that will define the outcome of the definitive prosthesis also apply to PR. However, while there has been ample research on definitive prosthesis failures, little research has been directed towards the failures of PR. Hyde et al observed a failure rate of 18.75% (n=189) and median failure time just 12 days, with retentive failure being most frequent [6]. Correspondingly, high failure rates (69.5%) in definitive cast restorations have been found to be mechanical in nature [7], thus emphasizing the significance of preparation designs [8] and degree of cement bond strength [9]. Short clinical crowns when defined by restorative criteria implies less than 2–3 mm of sound tooth structure remaining after necessary tooth preparations (axial and occlusal reduction) [10]. They are frequently encountered in clinical practice, with varied causes such as genetic variations, trauma, disease, eruption disharmony, and iatrogenic dentistry [11]. Besides hampering routine preparation designing, such a discrepancy alters the crown root ratio, which in turn influences final treatment outcomes, especially incorporating appropriate biological width and stress distribution to underlying structures [12]. Interdisciplinary compensation methods (orthodontic eruption, surgical crown lengthening) have biological and treatment time limitations for patients and clinicians. Primary (preparation taper) and auxiliary retentive features (groove, box) incorporated in preparation designs enhance inter-related retention and resistance forms [9], and are essential for restorative clinicians in restoring short clinical crowns. Whereas the resistance form enhances restoring stability along an axis other than the placement path, the retention form enhances restoration ability along the axis of placement.
The primary preparation feature is the total occlusal convergence (TOC) angle or the taper of the prepared abutment tooth [13], which is the fundamental single contributor to restoration retention and resistance forms. Preparation taper affects both resistance and retention forms, chiefly by altering mechanics (surface area, rotation axis, displacement forces) [1,9]. Maximum retention can be obtained at a clinically unrealistic 1 degree of TOC, as achieving such a taper is influenced by clinical factors like visibility, accessibility, and tooth location [14]. Since retention and resistance share a linear relationship, the ideal taper for achieving either one varies. Wilson et al discovered maximal tensile retention between 6- and 12-degrees TOC [15], while Goodacre et al recommended 10- and 12-degrees TOC for 4 mm (molars) and 3 mm (other teeth), respectively [16]. Supplementary research concluded a TOC of 16 degrees to be optimal for both retention and resistance form in abutment preparations [17]. Higher TOC reduces resistance forms, while decreased convergence does not significantly increase the retention form [9,17]. Adequate resistance requires a minimal abutment height of 3 mm (incisors and premolars) provided the taper is kept to acceptable limits (6 to 10 degrees) [18]. Observational clinical studies have reported greater TOC in the posterior than anterior, mandibular than maxillary, molar than other teeth, facio-lingual surface than mesiodistal, and FDP abutments than single crowns [16,17]. The non-viability of incorporating an ideal degree of taper clinically mandates augmenting tooth preparations with supplementary, secondary, or auxiliary preparation features in the form of pins, grooves, and a box, the placement of which depends on which parameter of tooth preparation needs to be enhanced (retention or resistance). A vertical groove placed axially enhances resistance form [14,16], while the same groove when placed horizontally along the circumference of the preparation enhances retention [19]. However, each auxiliary feature may enhance both through other mechanisms (increasing surface area, interlocking cement, changing dynamics mechanically). Increased resistance form using grooves proximally as well as the buccal or lingual location has been proposed with different specific objectives [9,20]. Advanced groove designs as proposed by Tjan et al (setting grooves) [21], and AlShaarani et al (frustum) [9] have shown significant influences on definitive restoration retention values, although both have been thought to make fitting restoration difficult, in addition to subjecting the tooth to hydraulic cement pressure. Auxiliary retentive features have been reported to achieve a 60% increased retention (circumferential groove) in implant abutment using zinc phosphate cement [22]. A positive influence of auxiliary preparation feature on retention and resistance is applicable when the TOC is within acceptable limits (less than 20 degrees) [16,22]. It is noteworthy to mention that irrespective of the type of restoration (provisional or definitive), these principles apply equally to both restoration types, although they have been found to be more effective in definitive restoration than PR. Generally, however, achieving adequate retention in short abutments has caused practitioners great concern throughout different eras [23].
In addition to preparation features, other significantly influential factors on retention and resistance of PR either directly or indirectly include the surface roughness of provisional material [24], internal fit [25], type of provisional material, and cement used [26]. PR retrieval may be either desired by the clinician (soft-tissue modelling around the implant) and/or may not be desired (due to risk of de-cementing in crown and bridge) [27]. Specific provisional cements have been developed in recent times, while earlier conventional definitive cements were used for cementing provisional restorations with the addition of weakening agents to ease removal by lowering adhesive failure stress [28]. Use of petroleum jelly in resin-based temporary cement has been shown to reduce de-cementing failure stresses from 131.6 Newtons (N) to 31.6 N [29]. Progressive cementation initially using weak luting agent, which progresses to strong cements later during future treatment has also been recommended in specific situations [27,29]. Such recommendations emphasize that a clinician should have a wide range of materials and cements available in various combinations to effectively cement PR whenever desired, without worrying about the ability to remove the cemented PR. The ability of cement to retain a PR is also dependent on preparation features, and under all circumstances the cement film thickness between 20 to 40 μm (ISO [International Organization for Standardization] standard less than 25 μm) should be maintained [27]. PR material in the form of polymethyl methacrylate (PMMA) has traditionally stood the test of time and continues to remain the same even with the advent of digital manufacturing and processing. The US Food and Drug Administration (FDA) has approved 4 different basic materials for making PR: polyethyl methacrylate (PEMA), bisacryl resin, light cure composite resin, and PMMA. [30]. PMMA is a frequently used PR materials that has undergone processing changes (traditional heat/self cure to milled/printed) to overcome its inherent disadvantages like exothermic polymerization, which has improved its accuracy (marginal, internal fit) and stability (degrading resin matrix) [31]. Additive and subtractive digital technologies (eg, computer-assisted diagnosis, computer-assisted machining/milling [CADCAM], and 3D printing) with the introduction of newer provisional restorative materials have decreased drawbacks of traditional techniques of fabricating provisional restorations. 3D printing allows clinicians to fabricate provisional restorations at chairside, avoiding laboratory-associated errors and delays. Both technologies have been reported to have improved physical, mechanical, and optical properties, in addition to accuracy and processing speed at reduced cost [32].
Despite these advances, there is disagreement on the ideal PR utilizing the most effective techniques and cemented with the most appropriate cement to increase retention in short abutment. Considering these multifaceted challenges, the present study performed an in-depth investigation of the influence of various independent variables (10- and 20-degree taper, groove, box, milled, 3D-printed, resin-based, and non-resin-based provisional cement) on the retention dynamics (retentive failure stress [dependent variable]) of 3-mm short provisional crowns. The primary aim of the study was to identify the different clinical combinations for different functional purposes of PR. We also sought to interpret the intricate relationship between these experimental variables that interact together with the success of PR. The study hypothesizes that differences in retentive failure stresses exist between milled and 3D-printed resins, that resin cement has higher failure stresses than conventional cements, that increased taper causes a provisional crown to fail at lower stress while auxiliary retentive features (box, groove) will increase resistance to retentive failure stresses, with box preparation failing at higher stress than a groove when higher taper is incorporated in the preparation. Alternately, the null hypothesis states that no differences exist between milled and 3D-printed PR, conventional, and resin cement, and preparation features (both primary and auxiliary).
Material and Methods
ETHICS:
This experimental laboratory research was appropriately supervised by the college/university ethical review committee at College of Dentistry, Jazan University (CODJU) (Reference number: CODJU-2220I dated 15 November, 2022). All materials used categorically are regulated and approved by national (Saudi food and drug authority) and international authorities (Food and Drug Authority).
STUDY DESIGN:
A progressive and comparative experimental study was designed that had 3 independent variables: (1) Preparation feature [primary (taper), auxiliary (groove, box)]; (2) Material/technique [CADCAM (milled) and 3D printed PMMA]; (3) Provisional non-eugenol cement (conventional and resin-based cement), the influence of which was determined based on the dependent variable (adhesive failure load). The experimental standardization included completing the study in 2 stages (specimen fabrication and testing) during the fourth quarter of 2022 and the first quarter of 2023.
OPERATIONAL DEFINITIONS:
In the context of the research and this paper, the following terms were operationally defined prior to conducting the study. The term “resistance form” was defined as that feature of tooth preparation that enhanced stability of the restoration (crown, bridge) and resisted its dislodgement, specifically along all axes other than its path of placement or removal [13,33]. The term “retentive form” was defined as a tooth preparation feature that resists crown dislodgment in the vertical direction or along the path of placement. The term “failure load” was defined as the bond failure at an interface between 2 materials because of tensile force. Higher failure load contextually indicates specimens failed at higher tensile load, while lower failure load indicates a specimen failing at lower tensile load. This term was specifically denoted as adhesion failure and has been used interchangeably during the manuscript. The term “taper” and “total occlusal convergence” was defined as a measure (in degrees) that was viewed in a plane that was formed between the external wall and placement path of tooth preparation or machined surface on material prepared for fixed prostheses [13,33]. ‘Working model’ was defined as a facsimile replica of the prepared tooth whose coronal surface was replicated exactly as per the anatomy of the prepared tooth (master model), while the base was geometric in shape (square) and was self-stabilized for ease of testing.
SAMPLE SIZE ESTIMATION: Estimation of the total sample and sample group size was determined using G Power, version 3.1.9.7 software (Heinrich Heine University Düsseldorf, Düsseldorf, Germany), effect size 91.23, alpha 5%, and power 80%. In total, 160 specimens divided into 16 subgroups (n=10) were used for testing with an extra 2 specimens for each subgroup kept as standby (Figure 1). Each specimen consisted of a working model and a milled or printed PC.
SAMPLE SPECIMEN FABRICATION: Materials used with respective manufacturer specifications, composition, and features, along with study coding, are presented in Table 1.
MASTER MODELS:
Two physically similar typodont models (Practicon, Greenville, NC, USA) with a full complement of typodont teeth were used to prepare 2 different master models (10- and 20-degree taper). The mandibular left first molar tooth (tooth number 36) was chosen for single all-ceramic crown preparation with tooth preparation guidelines outlined by recommended textbooks [17,34]. Initial depth orientation grooves were prepared by using a pre-tapered (10 and 20 degree) flat-end diamond bur (6856 314 016, Komet, Germany), using a high-speed air rotor hand piece (KaVo do Brazil Ind. Com. Ltd., Joinville, SC, Brazil) firmly attached to a dental cast surveyor (A3005 Surveyor Type A; Dental farm). Final tooth preparation included occlusal (remaining height of 3 mm to represent short clinical crown), axial (1.2 mm), and shoulder margin (1 mm circumferential) preparation clinically representing an all-ceramic tooth preparation. All reduction depths on both master models (10° and 20° taper) were verified using a multi-sectional putty index (Affinis, Coltène/Whaledent) and a graduated periodontal probe (Hu-Friedy, Chicago, IL, USA) for assessing depth. The preparation taper or the TOC was verified with the help of a stereomicroscope-connected Universal Serial Bus (USB) charge-coupled device (CCD) camera (Amscope, Irvine, CA, USA), which in turn was attached to a personal computer using compatible measurement software (version No. 3.7.12924) (Figure 2A, 2B). Both prepared modified short crowns were prepared in recommended axial planes, anatomical occlusal preparation, and rounded line and point angles.
MASTER MODELS WITH AUXILIARY PREPARATION FEATURES (GROOVE, BOX): The typodont master model with 20-degree taper at this stage was used to generate two 3D-printed replica working models to ensure that the taper and the amount of tooth reduction was standardized and the same for all test groups. Two 3D-printed models were manufactured by scanning using a bench-top scanner (3Shape A/S Holmens Kanal 7 1060 Copenhagen/Denmark) to generate data that were later transferred by software (Roland DG; VPanel) on a 3D printer (Asiga Pty Ltd. Alexandria, Australia) using polyetherimide resin liquid (Asiga Dentamodel Alexandria, Australia). The surface area of the 2 printed models was measured and compared with the typodont master model, and the percentage error was calculated statistically, which was later adjusted during data interpretation. These printed master models were also verified for desired taper with the same method as used for the typodont master models. One of the 20-degree taper printed models was modified to receive a 1-mm mid-buccal groove (vertical) with a 1-mm diameter cylindrical diamond bur (Figure 3A). Depth was verified by duplicating the groove in impression materials and measuring the deepest portion up to the cavo-surface of the prepared tooth. The other 20-degree taper printed model was modified to receive a mesial retentive box (width 4 mm, height 2 mm, depth 2 mm) (Figure 3A, 3B). These 2 modified 3D-printed models now served as master models to generate the remaining 80 working models [40 milled (20 models with groove, 20 models with box) and 40 3D printed (20 models with groove and 20 models with box)]. Thus, to generate samples 4 master models (2 typodont with 10- and 20-degree taper and 2 20-degree 3D-printed models, one with groove and one with box) were used for the study.
3D-PRINTED WORKING MODELS AND PROVISIONAL CROWNS: A digital light-processing 3D printer (Asiga Pty Ltd [limited], Alexandria, Australia) using 2 different 3D-printing resin liquids (Asiga Pty Ltd., Asiga Dentatooth and Dentamodel Alexandria, Australia) was used to fabricate provisional crowns and working models, respectively. The working models on which the PR would be placed for testing were fabricated for all test samples in all groups (n=160). Scanning and Standard Triangle Language or Standard Tessellation Language (STL) file data were obtained as described above. The printer was optimized for various parameters according to recommendations previously published [35]. These parameters include accuracy and precision, build volume (X, Y, Z=119×67×76 mm, 4.68×2.63×3 inches), surface finish and resolution (62-μm pixel size). Printing accuracy was determined by comparing the printed sample dimensions (length, thickness, and width) against the manufacturer’s test sample (a rectangular block) using a calibrated digital calliper. Light intensity (wavelength 385 nm) for resin liquid polymerization was determined using a power meter (Molectron Coherent, Santa Clara, CA) placed inside the printing chamber. Printing of provisional crowns was performed by setting the printing layer thickness to 100 μm, using the resin parameter ‘white’ on the machine. Curing was accomplished in a post-curing lightbox (NK Optik Otoflash G171) using 2000 flashes twice. Each crown sample was washed in clean water kept at room temperature for 60 min. Finishing/polishing was performed using routine dental procedures as recommended. All working 3D-printed models were fabricated according to manufacturer’s recommendations.
CADCAM (MILLED) PROVISIONAL CROWNS: All master models (10° and 20°) were first sprayed with powder (scan spray) (VITA CEREC; Bad Sackingen, Germany) using a propellant that limits the powder layer to an even thickness. The prepared tooth was then scanned using a bench-top scanner (3 Shape, Copenhagen, Denmark, Model No. 4), and the design software retrieved the scanned data. The respective size and shape for the milled provisional crown were then designed in accordance with the 3D-printed crowns’ files using design software (Roland DG; VPanel) for standardization of the crowns’ dimensions in both fabrication techniques. PMMA resin disks (CopraTemp White Peaks Dental Solutions GmbH, Wesel, Germany) of standard size (98/14), shade A2, were used for fabrication of milled specimens (n=20 each for 10° and 20°). New high-speed tools (HSS) with standard size (1 mm/2 mm wide, 5° edge rake angle/2° clearance angle) were loaded into the milling machine (DGSHAPE, Roland DGA, Irvine, CA, USA) under wet conditions as per the manufacturer’s recommendations [26]. Any crowns that showed cracks or defects were discarded. Finishing of specimens was performed using a kit (K0330 PMMA: Adjusting, Finishing & Polishing, KP, Brasseler USA), followed by polishing (automatic) (Spectrum System 1000 – SS1000; LECO Corp, St. Joseph, MI) in a wet environment (pumice and water) (90 s). This was followed by fine polishing (Fabulustre; Grobet USA) [36]. The crown thickness was standardized by standardized by keeping the thickness even (4±0.5 mm) using digital callipers. The final stage was to clean all samples in an ultrasonic cleaner (Eltrosonic Ultra Cleaner 07–08; Eltrosonic GmbH) for 10 min before open-air drying.
SUBGROUPING BASED ON THE PROVISIONAL CEMENT USED:
Before the cementation of the PC on their respective working models, each crown was observed for cracks, defects, and fit. Discarding a particular specimen was followed by refabrication to replace the discarded one. Each PC was allotted a group name and number along with a same corresponding number of the working model. Two provisional non-eugenol cements, 1 zinc oxide-containing conventional (Kerr Tempbond, Kerr, Romulus, MI, USA, Lot 8205180) and 1 resin-based (ProviTemp, Itena, France) cement formed the final subgroups for the study. In total, 16 subgroups (n=10) were formed with each group, designated by a letter or a number according to the independent variable [M=milled, P=printed; 1=10 degree, 2=20 degree; C=conventional cement, R=resin-based cement; G=groove, B=box]. Milled provisional crowns cemented with conventional provisional cement had 4 subgroups [Gp MC1, Gp MC 2, Gp MC 2G, Gp MC 2B], and there were 4 subgroups with resin-reinforced cement [Gp MR1, Gp MR2, Gp MR2G, Gp MR2B] (N=10 each). There were 4 subgroups of 3D-printed provisional crowns cemented with conventional provisional cement [Gp PC1, Gp PC2, Gp PC2G, Gp PC2B], and 4 subgroups with resin-reinforced cement [Gp PR1, Gp PR2, Gp PR2G, Gp PR2B] (n=10 each) (Figure 1). Each provisional crown was designed with a loop on the occlusal surface that was oriented mesiodistally, with a 4-mm external diameter and 2-mm internal diameter to facilitate retention testing. Each provisional crown was designed to provide a cement space of 50 μm. Subgroups with 10-degree taper for both milled and printed PCs served as control groups for 20-degree taper groups, and subgroups with 20-degree taper for both milled and printed PCs served as control groups for those with grooves and proximal box.
CEMENTATION AND THERMOCYCLING:
The PCs in each subgroup were cemented on their corresponding working models with the cement of the group to which they belonged. The cements were mixed in automix syringes and dispensed according to manufacturer’s recommendations. The PCs were held in position on the models under 2.5 kg force for 5 min until they set [37]. Excess set cement was eliminated using a sharp instrument around the margins of the PC with the underlying working model. All cemented PC on their respective models were then thermocycled for 10 000 cycles in alternating hot and cold baths, the temperature of which ranged between 5°C and 55°C in a thermocycling machine (Model 1100, SD Mechatronik, Bayern, Germany) [38]. The dwell time of 30 s and a transfer time of 5 s were standardized for all subgroups. This equalled the simulation of a clinical scenario and represented 6 months of use in the oral environment.
MEASURES, DATA COLLECTION, EVALUATION, AND ANALYSIS:
Subsequently, at the end of thermocycling, each sample was subjected to pull-off testing using a universal testing machine (Instron System ID 5967L1040; Model No 5967 Norwood, MA, USA) with a crosshead speed of 1.0 and 5.0 mm/min (Figure 4). The measurement of retentive failure was denoted when the provisional crown was separated from the prepared surface of the working model. The tensile force was denoted in newtons (N) and similar testing criteria were applied for each group.
STATISTICAL ANALYSIS:
The force measured in newtons for each sample in each subgroup was recorded and entered manually in a Microsoft excel spreadsheet. All data were then refined and coded and entered into SPSS software version 25.0 (SPSS, Inc., Chicago, IL, USA. Mean values and standard deviation were calculated for each group among 10 samples. Data distribution for normality within each individual subgroup and the comparative subgroup was assessed by Kolmogorov-Smirnov test. Differences between the subgroups were determined using a one-way analysis of variance (ANOVA) (independent measures). Differences between pairs of group means were followed up using a post hoc Tukey honest significant difference (HSD) test. The differences between primary and auxiliary retentive features (taper, groove, and box) were determined using the
Results
RETENTION OF MILLED AND 3D-PRINTED PC:
The mean failure (adhesive) stress values of various groups (milled and 3D-printed) and their respective subgroups based on the provisional cement and preparation features are presented in Table 2. Among all subgroups, the specimen in Gp PR2B (m=328.84) failed at highest stress while those in Gp MC2G (m=47.68) showed retentive failure at lowest stress. Both milled and printed PC subgroups when cemented with conventional provisional cement showed adhesive failure at lower load (47.68 to 77.91) as compared to the milled and printed PCs cemented with resin cement (104.2 to 328.84). Allotted subgroups based on preparation features (primary and auxiliary) made of milled provisional PMMA and cemented with conventional cement showed least failure load values among all investigated subgroups (mean 47.68 to 73.54). Highest loads to adhesive failure were obtained in subgroups of 3D-printed PMMA resin cemented with resin cements (mean 184.85 to 328.84). One-way ANOVA for independent measures showed that the differences between various subgroups of milled and 3D-printed resin cemented with provisional cements (conventional and resin-based) differed significantly (P<0.05), thereby indicating the influence of these independent variables on the retentive adhesive failure (Table 2). While interpreting these results, one may observe that milled PC showed adhesive failure at lower loads for both cements when compared to 3D-printed PCs. Within each subgroup, the differences were determined by the post hoc Tukey HSD, the results of which are presented in Table 3. In total, within 16 subgroups, the maximum number of subgroups that were not significantly different were those of milled PC groups cemented with conventional cement. For 3D-printed PCs, no differences were observed between subgroup MR2B with its control subgroup MR2 (mean difference 7.33). These results when interpreted show that the adhesive failure in milled PC is less influenced by primary and auxiliary retentive features (taper, box groove) when cemented with conventional cement.
:
The mean adhesive failure values observed for primary (taper) and auxiliary (groove, box) retentive features among various subgroups are presented Table 4 and graphical comparison with respective controls in Figure 5. For conventional cement, increasing the taper from 10 to 20 degrees reduced the provisional crown retention in all subgroups except GP PR, which showed an increase from PR1 (184.85) to PR2 (201.17) (difference 16.32N). Higher mean values were also observed in both milled (137.26) and 3D printed (184.85) provisional crowns prepared at 10-degree taper when cemented with resin cement. A statistically significant difference for 20-degree taper was observed only between GP MC2 and PC2 (P<.442) (Table 4). These results when interpreted show that an increase in taper reduces retention irrespective of the provisional material and cement used except when 3D-printed provisional is cemented with resin cement. For auxiliary retentive feature groove, retention decreased in GP MC2G (baseline 48.05), GP PC2G (baseline 48.4), GP MR2G (baseline 116.51), while it only increased in GP PR2G (baseline 201.17). For auxiliary feature box, retention was observed to increase in all 20-degree taper groups, with the highest increase from baseline observed in GP PR2B (baseline 201.17).
Discussion
INFLUENCE OF CEMENT AND PREPARATION FEATURES (PRIMARY AND AUXILIARY):
The 20-degree taper was investigated in this study because it represents the average TOC that most preparations have with molar teeth [64]. Two provisional cements were used in this study – the conventional (TempBond) and a resin-based (ProviTemp). Both cements, being non-eugenol, have different chemical constituents. Higher failure stresses were observed in groups cemented with resin-based cement, irrespective of the material used and the preparation feature incorporated with differences between resin and conventional provisional cement being significant except between GP MR2 and MR2B, thereby rejecting the null hypothesis that no differences exist between resin-based and conventional provisional cement. Results indicate that except when resin-based cement was used in 3D printed provisional at the 20-degree taper, an increase of taper from 10 to 20 degrees reduces failure stresses, thereby accepting the primary hypothesis that the increased taper will lower failure stresses. These results agree with the general scientific opinion [1,6,17,26] about the influence of taper in various types of definitive restorations made from different restorative materials like zirconia crown [65], resin-bonded fixed partial denture [8], cast gold [17], implant-supported restorations [20], and full-veneer crowns [21]. Our results of increased retention in 3D-printed PC cemented with resin cements at increased taper have been also observed by Zidan et al, for definitive restorations (high noble alloys) on extracted teeth using adhesive resin cements (C&B Metabond and Panavia) [66]. Although they used 24-degree taper, they observed a 20% increase in retention values from 6 to 24 degrees. Higher resistance of resin-based cements has been attributed to the cement being subjected to higher intra-coronal hydraulic pressures, resulting in higher resisting forces during cementation [67]. Wiskott et al also demonstrated that the axis of rotational resistance, rather than being at the crown margin, is actually at the cement interface, and concluded that the compressive strength of cements determines the amount of resistance of the preparation design [40]. Cement in a state of compression has also been reported to improve retention [68]. The optimum internal fit of PC produces uniform cement space which does not compromise retention and resistance form [69], which also explains the results obtained in this study for 3D-printed PR. Modifying the internal surface of milled PC (VitaCAD-Temp, VITA) has been reported to improve retention strength with definitive resin-based cements (PanaviaV5 and RelyX Ultimate), but has not been found beneficial for 3D-printed PC [70]. Decreased retention has been also attributed to thermal cycling, as was done in this study [71].
The results also show that addition of grooves improved retention in 3D-printed crowns, while all others subgroups showed little or no effect. Addition of boxes substantially increased retention in 3D-printed crowns cemented with resin cement, while improving retention in milled when cemented with conventional crowns. Our results for 3D-printed PCs with auxiliary features of a groove and the box preparation showed higher failure stresses. These can be explained by surface characteristics of 3D-printing and the resin cement. Resin cement showed increase while most groups using conventional cement showed decrease. The results cannot be compared, since there are no reports of the effect of the groove on PR. The effect of a vertical groove on retention has been found to be minimal and statistically insignificant in definitive restorations [72] due to a lower degree of adaptation found along grooves. However, grooves clearly improve the resistance of the crown, and improved resistance directly influences the overall retentive form of the crown. Mansour et al evaluated the effect of single groove on flat preparation and found a very low tensile load required to de-cement the crown using a weak cement (3.28 kg) [73]. The 3D-printed provisional crown has been investigated for surface roughness and studies have reported higher surface roughness after processing of the 3D-printed resin. The rough characteristics of 3D-printed resin are attributed to the differences in the pixel size used to cure at the center and at the edge [35]. While the rough surface of the provisional crown from the outer side needs to be corrected through sanding for esthetic finish and color reproduction, the inner fitting rough surface is left as is, which improves macro-mechanical retention for all cements. This also explains that why surface modifications like sand blasting in 3D-printed provisional did not improve micro-tensile bond strength in the study by Soto-Montero [70]. Sand blasting removes roughness and smooths the surface. On the contrary, our results of high retention in 3D-printed vs milled can be further explained on the inner surface characteristics. Milling produces smooth surfaces while 3D-printing produces rough surfaces, which alters macro-mechanical characteristics of the luting surface. Rough surfaces are not desirable on the outer surface of the PCs, as such surfaces are prone to deposit dental plaque, which needs to be mechanically removed from restoration surfaces irrespective of whether the restoration is provisional or definitive [74].
CLINICAL SIGNIFICANCE:
A short root canal-treated abutment tooth, when prepared with an acceptable taper, can be provisionally restored with either milled/printed provisional crowns or cemented with conventional cement if the provisional is desired for short term (a few weeks). For vital teeth with similar clinical requirements, a milled/printed cemented with conventional cement for short term or a milled/3D-printed for long term (6 months or more) should be considered as an alternative. Whenever a short-abutment tooth is prepared with increased taper, a milled/printed provisional crown cemented with resin cement may be indicated for short-term use, while for long-term use, a proximal box should be incorporated if clinically required. When a provisional crown is desired after crown lengthening or implant placement for enhancing the soft-tissue profile, a milled provisional crown cemented with resin cement may be placed if provisional restorations are desired to remain in place for 3 months or lower. For longer durations, the 3D-printed PR cemented with resin cement should be the ideal choice if all clinical variables are taken into consideration. For cantilever FDP, the best choice of PC will be 3D-printed cemented with resin cement.
STRENGTH AND LIMITATIONS OF THE STUDY:
We generated hypotheses followed by testing among different independent variables. Our study is limited because we only tested 2 technologies (milled and 3D-printed), 2 cements (conventional and resin-based), and only 2 primary preparation features (taper) and diverse auxiliary retentive features (groove and box). However, we included multiple independent variables, with wide combinations of provisional crowns, which may help clinicians in choosing a particular combination of material, technology, preparation feature, and cement for a specific clinical purpose. Limitations of methods include that all product ranges of PC and provisional cements were not included. The in vitro method does not present a complete picture and conditions in the oral cavity.
Conclusions
We found that resin cement failed at higher loads than conventional cements, irrespective of material used for PR and retentive features used. Between milled and 3D-printed PCs, the 3D-printed PCs failed at higher loads when cemented with conventional or resin cement. The combination of resin cement with 3D-printed crown had the highest retentive strengths. For the primary retentive feature taper, we found that increase in taper from 10 to 20 degrees was associated with decreased retention for both cements and milled PC, while increased retention was observed for 3D-printed cemented with resin cement. Addition of a groove as an auxiliary retentive feature was associated with decreased retention in milled PCs but increased retention for 3D-printed PCs. The box preparation improved retention 3D-printed crowns for both cements but only when milled PC was cemented with resin cement.
Figures
![Flowchart showing study sampling and group distribution. Figure created using MS PowerPoint, version 20H2 (OS [operating system] build 19042,1466), windows 11 Pro, Microsoft [MS] Corporation).](https://jours.isi-science.com/imageXml.php?i=medscimonit-30-e943237-g001.jpg&idArt=943237&w=1000) Figure 1. Flowchart showing study sampling and group distribution. Figure created using MS PowerPoint, version 20H2 (OS [operating system] build 19042,1466), windows 11 Pro, Microsoft [MS] Corporation).
Figure 1. Flowchart showing study sampling and group distribution. Figure created using MS PowerPoint, version 20H2 (OS [operating system] build 19042,1466), windows 11 Pro, Microsoft [MS] Corporation). ![Working models (A) 10-degree preparation taper and (B) 20-degree preparation taper verification of master models. Figure created using Microsoft Snip and Sketch 10.2008.30001.0 followed by compilation on MS PowerPoint, version 20H2 (OS [operating system] build 19042,1466), Windows 11 Pro, Microsoft [MS] Corporation).](https://jours.isi-science.com/imageXml.php?i=medscimonit-30-e943237-g002.jpg&idArt=943237&w=1000) Figure 2. Working models (A) 10-degree preparation taper and (B) 20-degree preparation taper verification of master models. Figure created using Microsoft Snip and Sketch 10.2008.30001.0 followed by compilation on MS PowerPoint, version 20H2 (OS [operating system] build 19042,1466), Windows 11 Pro, Microsoft [MS] Corporation).
Figure 2. Working models (A) 10-degree preparation taper and (B) 20-degree preparation taper verification of master models. Figure created using Microsoft Snip and Sketch 10.2008.30001.0 followed by compilation on MS PowerPoint, version 20H2 (OS [operating system] build 19042,1466), Windows 11 Pro, Microsoft [MS] Corporation). ![(A) 20-degree taper 3D-printed models on which auxiliary retentive groove (buccal) and box (proximal) were prepared. (B) Inset showing proximal view of the box preparation. Photograph taken using a digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash followed by compilation on MS PowerPoint, version 20H2 (OS [operating system] build 19042,1466), Windows 11 Pro, Microsoft [MS] Corporation.](https://jours.isi-science.com/imageXml.php?i=medscimonit-30-e943237-g003.jpg&idArt=943237&w=1000) Figure 3. (A) 20-degree taper 3D-printed models on which auxiliary retentive groove (buccal) and box (proximal) were prepared. (B) Inset showing proximal view of the box preparation. Photograph taken using a digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash followed by compilation on MS PowerPoint, version 20H2 (OS [operating system] build 19042,1466), Windows 11 Pro, Microsoft [MS] Corporation.
Figure 3. (A) 20-degree taper 3D-printed models on which auxiliary retentive groove (buccal) and box (proximal) were prepared. (B) Inset showing proximal view of the box preparation. Photograph taken using a digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash followed by compilation on MS PowerPoint, version 20H2 (OS [operating system] build 19042,1466), Windows 11 Pro, Microsoft [MS] Corporation. 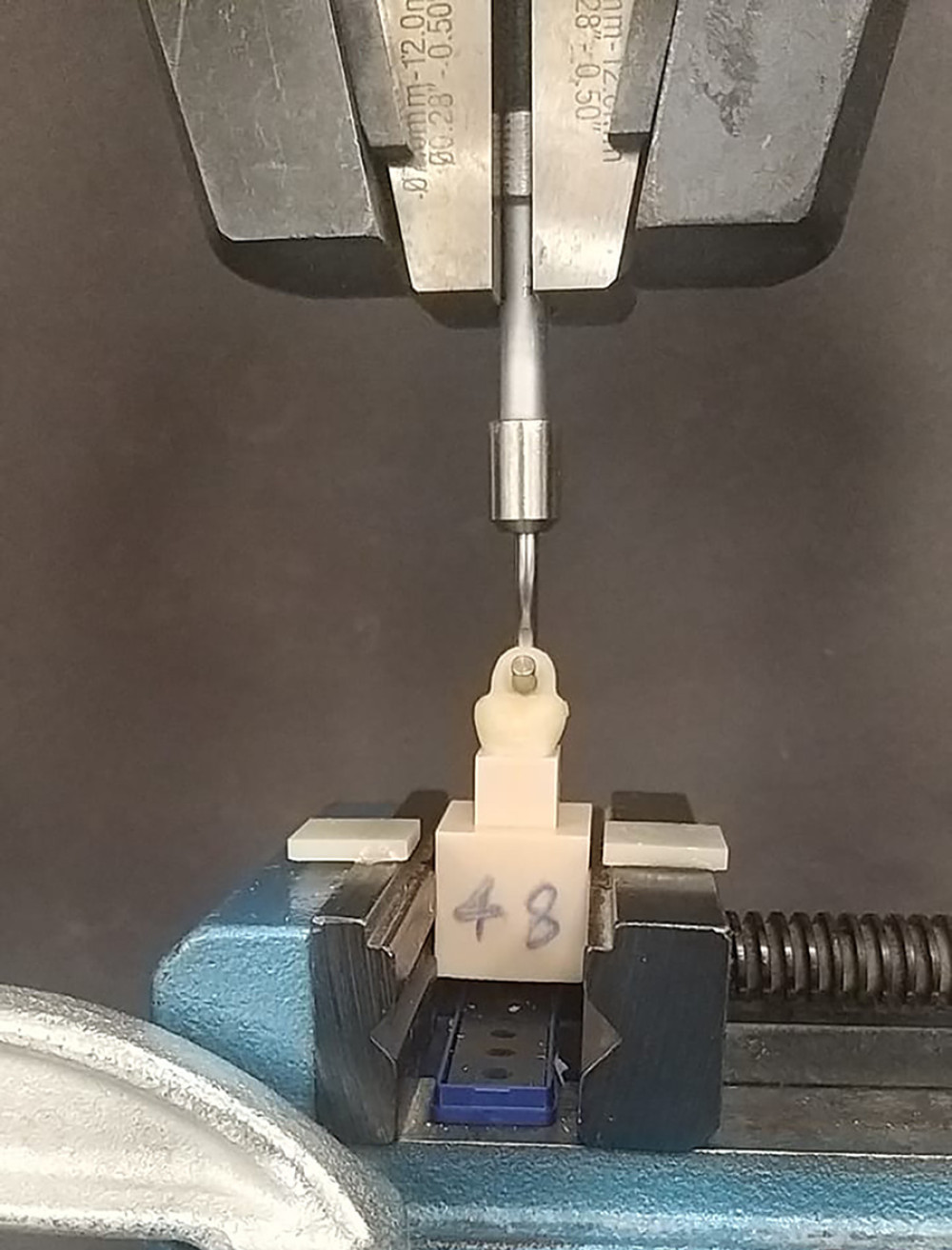 Figure 4. Universal testing machine showing engagement of the test samples for the pull-off test with handles of the provisional crowns aligned to engage the sample handle perpendicular to the line of direction of pulling force. Photograph taken using a digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash.
Figure 4. Universal testing machine showing engagement of the test samples for the pull-off test with handles of the provisional crowns aligned to engage the sample handle perpendicular to the line of direction of pulling force. Photograph taken using a digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash. ![Influence of supplementary retentive features (taper, groove, box) on the mean tensile forces for 2 different provisional crown materials (milled vs 3D-printed) cemented with 2 different provisional cements (conventional vs resin-modified). Figure created using ms excel sheet, version 20h2 (os [operating system] build 19042,1466), windows 11 pro, Microsoft [ms] Corporation).](https://jours.isi-science.com/imageXml.php?i=medscimonit-30-e943237-g005.jpg&idArt=943237&w=1000) Figure 5. Influence of supplementary retentive features (taper, groove, box) on the mean tensile forces for 2 different provisional crown materials (milled vs 3D-printed) cemented with 2 different provisional cements (conventional vs resin-modified). Figure created using ms excel sheet, version 20h2 (os [operating system] build 19042,1466), windows 11 pro, Microsoft [ms] Corporation).
Figure 5. Influence of supplementary retentive features (taper, groove, box) on the mean tensile forces for 2 different provisional crown materials (milled vs 3D-printed) cemented with 2 different provisional cements (conventional vs resin-modified). Figure created using ms excel sheet, version 20h2 (os [operating system] build 19042,1466), windows 11 pro, Microsoft [ms] Corporation). Tables
Table 1. List of materials, instrumentation, and manufacturer.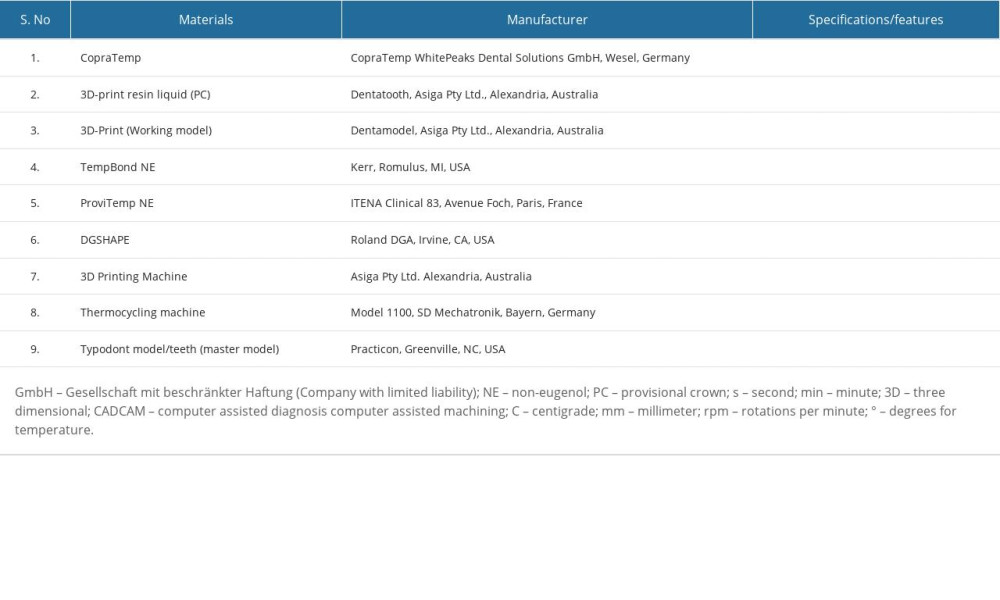 Table 2. One-Way ANOVA test results for comparison of tensile forces between 2 provisional crown materials (milled vs 3D-printed) cemented with 2 different provisional cements (conventional vs resin-modified) using different retentive features (taper, groove, box).
Table 2. One-Way ANOVA test results for comparison of tensile forces between 2 provisional crown materials (milled vs 3D-printed) cemented with 2 different provisional cements (conventional vs resin-modified) using different retentive features (taper, groove, box).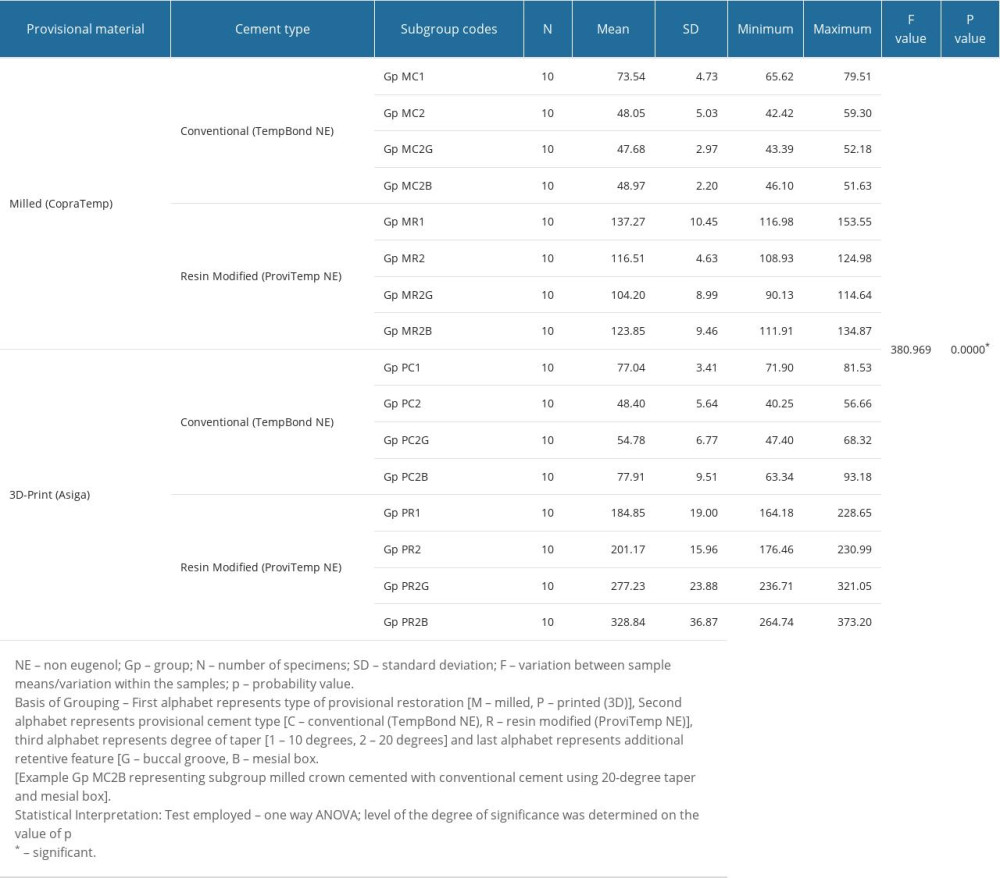 Table 3. Post hoc (Tukey HSD) test results for multiple group comparison showing differences in means and level of significance of these differences between 2 provisional crown materials (milled vs 3D-printed) cemented with 2 different provisional cements (conventional vs resin-modified) using different retentive features (taper, groove, box).
Table 3. Post hoc (Tukey HSD) test results for multiple group comparison showing differences in means and level of significance of these differences between 2 provisional crown materials (milled vs 3D-printed) cemented with 2 different provisional cements (conventional vs resin-modified) using different retentive features (taper, groove, box). Table 4. Comparative differences in mean values showing the effect of various retentive features (taper, supplementary groove, and box) when used in 2 different provisional crown materials (milled/3D-printed) after cementing with 2 different provisional cements (conventional vs resin-modified non-eugenol).
Table 4. Comparative differences in mean values showing the effect of various retentive features (taper, supplementary groove, and box) when used in 2 different provisional crown materials (milled/3D-printed) after cementing with 2 different provisional cements (conventional vs resin-modified non-eugenol).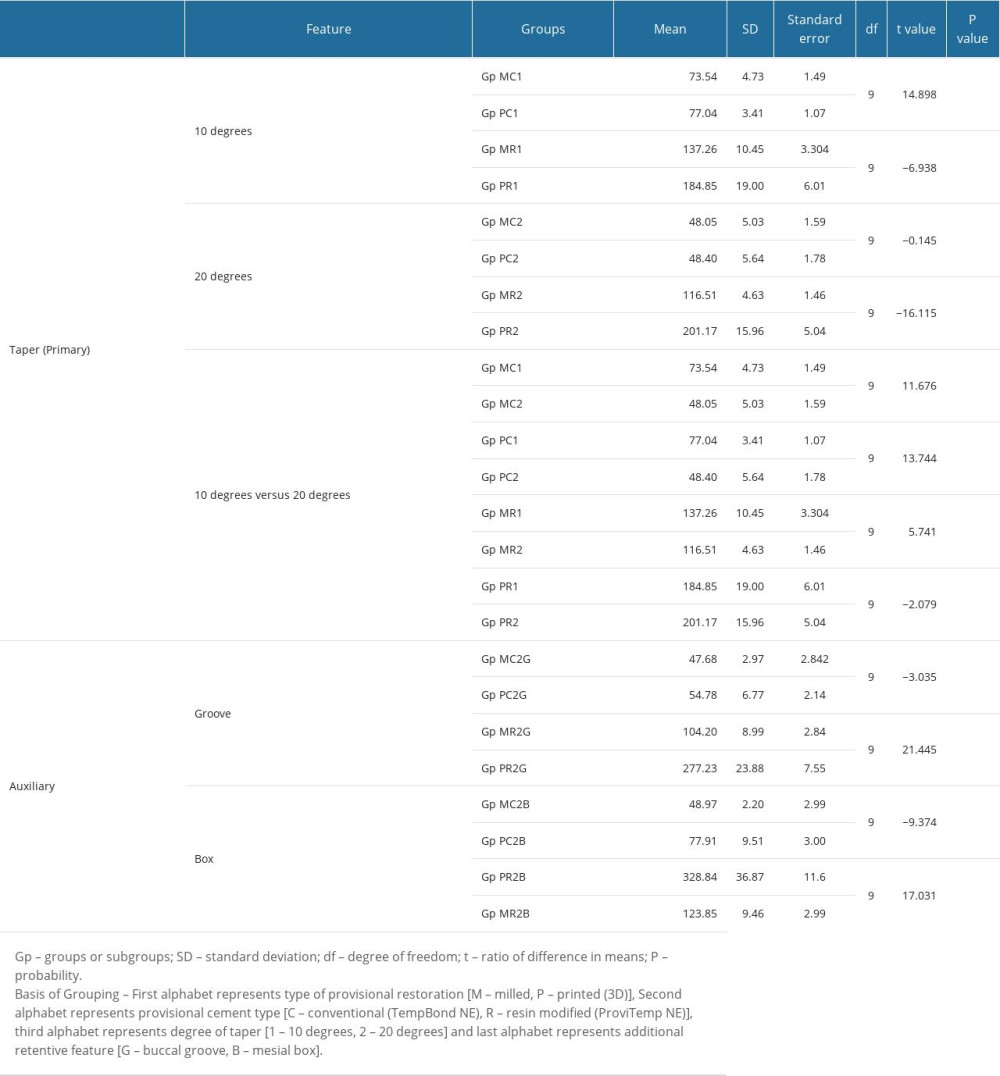
References
1. Vinaya K, Rakshith H, Prasad KD, To evaluate and compare retention of complete cast crown in natural teeth using different auxiliary retentive features with two different crown heights an in vitro study: Int J Biomed Sci, 2015; 11; 99-106
2. Tatakis DN, Silva CO, Contemporary treatment techniques for excessive gingival display caused by altered passive eruption or lip hypermobility: J Dent, 2023; 18; 104711
3. Mattoo KA, Kumar L, Sarvar S, Full mouth rehabilitation in an occupationally stressed bureaucrat: JMSCR, 2019; 7(10); 536-40
4. Brar A, Mattoo KA, Singh Y, Clinical reliability of different facial measurements in determining vertical dimension of occlusion in dentulous and edentulous subjects: Int J Prosthodont Restor Dent, 2014; 4(3); 68-77
5. Thompson J, Schoenbaum TR, Pannu D, Knoernschild K, Survival analysis of zirconia implant-supported, fixed complete dentures: A 5-year retrospective cohort study: J Prosthet Dent, 2023 [Online ahead of print]
6. Hyde JD, Bader JA, Shugars DA, Provisional crown failures in dental school predoctoral clinics: J Dent Educ, 2007; 71(11); 1414-19
7. Sayed ME, Lunkad H, Mattoo K, Evaluation of the effects of digital manufacturing, preparation taper, cement type, and aging on the color stability of anterior provisional crowns using colorimetry: Med Sci Monit, 2023; 29; e941919
8. Kale E, İzgi AD, Niğiz R, Bond strength evaluation of inlay-retained resin-bonded fixed partial dentures with two different cavity designs and two different adhesive systems: In vitro study: Balk J Dent Med, 2020; 24(1); 21-28
9. AlShaarani F, Alaisami RM, Aljerf L, An auxiliary factor for increasing the retention of short abutments: Heliyon, 2019; 5(10); e02674
10. Seol HW, Koak JY, Kim SK, Heo SJ, Full mouth rehabilitation of partially and fully edentulous patient with crown lengthening procedure: A case report: J Adv Prosthodont, 2010; 2; 50-53
11. Xenoudi P, Karydis A, Crown lengthening procedures for functional and esthetic purposes: Curr Oral Health Rep, 2019; 6; 230-36
12. Sindi AS, Al Sanabani F, Al-Makramani BM, A Radiographic study of the root-to-crown ratio of natural permanent teeth in 81 Saudi adults: Med Sci Monit, 2022; 28; e936085
13. , The glossary of prosthodontic terms: J Prosthet Dent, 2005; 94; 10-92
14. Naidoo N, Moipolai PD, Motloba PD, A Comparison of convergence angles of crown preparations in an undergraduate programme at a Tertiary Institution: S Afr Dent J, 2021; 76(10); 602-6
15. Wilson AH, Chan DC, The relationship between preparation convergence and retention of extracoronal retainers: J Prosthodont, 1994; 3; 74-78
16. Goodacre CJ, Campagni WV, Aquilino SA, Tooth preparations for complete crowns: An art form based on scientific principles: J Prosthet Dent, 2001; 85; 363-76
17. Shillingburg HT, Hobo S, Whitsett LD, Fundamentals of fixed prosthodontics: Preparations for cast gold restorations, 2012; 143-85, Chicago, Quintessence Publishing
18. Cano-Batalla J, Soliva-Garriga J, Campillo-Funollet M, Influence of abutment height and surface roughness on in vitro retention of three luting agents: Int J Oral Maxillofac Implants, 2012; 27(1); 36-41
19. Amarnath GS, Pandey A, Prasad HA, Hilal M, Comparative evaluation of enhancing retention of dislodged crowns using preparation modifications and luting cements: An in-vitro study: J Int Oral Health, 2015; 7; 47-51
20. Proussaefs P, Crowns cemented on crown preparations lacking geometric resistance form. Part II: Effect of cement: J Prosthodont, 2004; 13(1); 36-41
21. Tjan AH, Sarkissian R, Miller GD, Effect of multiple axial grooves on the marginal adaptation of full cast-gold crowns: J Prosthet Dent, 1981; 46(4); 399-403
22. Lewinstein I, Block L, Lehr Z, An in vitro assessment of circumferential grooves on the retention of cement-retained implant-supported crowns: J Prosthet Dent, 2011; 106(6); 367-72
23. Dhanraj M, Jain AR, Management of short abutments receiving complete veneer crowns – a cross sectional survey. Biomed. Pharmacol: J, 2017; 10(3); 1569-76
24. Song MY, An H, Park EJ, The effect of temporary cement cleaning methods on the retention of crowns: J Prosthod, 2019; 28(1); e210-15
25. Park YD, Kang W, Comparative evaluation of the fitness of anterior and posterior interim crowns fabricated by additive manufacturing: J Tech Dent, 2021; 43(4); 153-59
26. Mugri MH, Dewan H, Sayed ME, The effect of a digital manufacturing technique, preparation taper, and finish line design on the marginal fit of temporary molar crowns: An in-vitro study: Biomedicines, 2023; 11(2); 570
27. Akça K, Iplikçioğlu H, Cehreli MC, Comparison of uniaxial resistance forces of cements used with implant-supported crowns: Int J Oral Maxillofac Implants, 2002; 17(4); 536-42
28. Sheets JL, Wilcox C, Wilwerding T, Cement selection for cement-retained crown technique with dental implants: J Prosthodont, 2008; 17(2); 92-96
29. Jain S, Mattoo K, Khalid I, A Study of 42 partially edentulous patients with single-crown restorations and implants to compare bone loss between crestal and subcrestal endosseous implant placement: Med Sci Monit, 2023; 29; e939225
30. Balkenhol M, Köhler H, Orbach K, Wöstmann B, Fracture toughness of cross-linked and non-cross-linked temporary crown and fixed partial denture materials: Dent Mater, 2009; 25(7); 917-28
31. Karaman T, Eser B, Altintas E, Atala MH, Evaluation of the effects of finish line type and width on the fracture strength of provisional crowns: Odontology, 2021; 109; 76-81
32. Rezaie F, Farshbaf M, Dahri M, 3D printing of dental prostheses: current and emerging applications: J Compos Sci, 2023; 7(2); 80
33. Ferro KJ, Morgano SM, Driscoll CF, The glossary of prosthodontic terms: Journal of Prosthetic Dentistry, 2017; 117(5S); e1-e105
34. Rosenstiel SF, Land MF, Fujimoto J, Principles of tooth preparation: Contemporary fixed prosthodontics, 1995; 2; 135-67, St. Louis, Mosby-Year Book, Inc
35. Tahayeri A, Morgan M, Fugolin AP, 3D printed versus conventionally cured provisional crown and bridge dental materials: Dent Mater, 2018; 34(2); 192-200
36. Alp G, Johnston WM, Yilmaz B, Optical properties and surface roughness of prepolymerized poly (methyl methacrylate) denture base materials: J Prosthet Dent, 2019; 121; 347-52
37. Lepe X, Bales DJ, Johnson GH, Retention of provisional crowns fabricated from two materials with the use of four temporary cements: J Prosthet Dent, 1999; 81(4); 469-75
38. Mittal N, Khosla A, Jain S, Effect of storage media on the flexural strength of heat and self-cure denture base acrylic resins – an invitro study: Ann.Romanian Soc Cell Biol, 2021; 25(4); 11743-50
39. Edelhoff D, Özcan M, To what extent does the longevity of fixed dental prostheses depend on the function of the cement? Working Group 4 materials: Cementation: Clin Oral Implants Res, 2007; 18; 193-204
40. Wiskott HWA, Nicholls JI, Belser UC, The relationship between abutment taper and resistance of cemented crowns to dynamic loading: Int J Prosthodont, 1996; 9; 117-39
41. Dodge WW, Weed RM, Baez RJ, Buchanan RN, The effect of convergence angle on retention and resistance form: Quintessence Int, 1985; 16; 191-94
42. El-Mubarak N, Abu-Bakr N, Omer O, Ibrahim Y, Assessment of undergraduate students’ tooth preparation for full veneer cast restorations. Open J: Stomatol, 2014; 4(2); 43-48
43. Leloup G, D’Hoore W, Bouter D, Meta-analytical review of factors involved in dentin adherence: J Dent Res, 2001; 80; 1605-14
44. Heintze SD, Crown pull-off test (crown retention test) to evaluate the bonding effectiveness of luting agents: Dent Mater, 2010; 26(3); 193-206
45. Brar A, Mattoo K, Jain P, Designing cantilever prosthesis: A case study: RRJoD, 2014; 5(3); 5-9
46. Hidayat AS, Masulili C, Indrasari M, Resistance of full veneer metal crowns with different forms of axial grooves: In J Phys: Conference Series, 2017; 884(1); 012019
47. Parai P, Ojah P, Jain S, A comparative evaluation of the efficacy of two gingival retraction systems: An in vivo study: Eur J Mol Clin Med, 2020; 7(8); 4870-80
48. Alzahrani AH, Mechanical properties of selected CAD/CAM and conventional interim fixed restorative materials: Doctoral dissertation, 2018, New York, Faculty of the Graduate School of The University at Buffalo, State University
49. Tammam RA, Comparison in vitro between three-dimensionally printed, milled CAD-CAM and manually fabricated interim crown materials: Al-Azhar Assiut Dental Journal, 2021; 4(2); 141-50
50. Ayman AD, The residual monomer content and mechanical properties of CAD\CAM resins used in the fabrication of complete dentures as compared to heat cured resins: Electron Physician, 2017; 9(7); 4766
51. Lee WS, Lee DH, Lee KB, Evaluation of internal fit of interim crown fabricated with CAD/CAM milling and 3D printing system: J Adv Prosthodont, 2017; 9(4); 265-70
52. Al Wadei MH, Sayed ME, Jain S, Marginal adaptation and internal fit of 3D-printed provisional crowns and fixed dental prosthesis resins compared to CAD/CAM-milled and conventional provisional resins: A systematic review and meta-analysis: Coatings, 2022; 12(11); 1777
53. Abduo J, Lyons K, Bennamoun M, Trends in computer-aided manufacturing in prosthodontics: A review of the available streams: Int J Dent, 2014; 2014; 783948
54. Abdullah AO, Tsitrou EA, Pollington S, Comparative in vitro evaluation of CAD/CAM vs conventional provisional crowns: J Appl Oral Sci, 2016; 24; 258-63
55. Dede DÖ, Armaganci A, Ceylan G, Influence of abutment material and luting cements color on the final color of all ceramics: Acta Odontol Scand, 2013; 71; 1570-78
56. Peng CC, Chung KH, Yau HT, Assessment of the internal fit and marginal integrity of interim crowns made by different manufacturing methods: J Prosthet Dent, 2020; 123(3); 514-22
57. Mai HN, Lee KB, Lee DH, Fit of interim crowns fabricated using photopolymer-jetting 3D printing: J Prosthet Dent, 2017; 118(2); 208-15
58. Park JY, Lee JJ, Bae SY, In vitro assessment of the marginal and internal fits of interim implant restorations fabricated with different methods: J Prosthet Dent, 2016; 116(4); 536-42
59. Earar K, Iliescu AA, Popa G, Additive vs. subtractive CAD/CAM procedures in manufacturing of the PMMA interim dental crowns. A comparative in vitro study of internal fit: Rev Chim, 2020; 71; 405-10
60. Jeong YG, Lee WS, Lee KB, Accuracy evaluation of dental models manufactured by CAD/CAM milling method and 3D printing method: J Adv Prosthodont, 2018; 10(3); 245-51
61. Stansbury JW, Idacavage MJ, 3D printing with polymers: Challenges among expanding options and opportunities: Dent Mater, 2016; 32; 54-64
62. Dizon JR, Gache CC, Cascolan HM, Post-processing of 3D-printed polymers: Technol, 2021; 9(3); 61
63. Mârţu I, Murariu A, Baciu ER, An interdisciplinary study regarding the characteristics of dental resins used for temporary bridges: Medicina, 2022; 58(6); 811
64. Nordlander J, Weir D, Stoffer W, The taper of clinical preparations for fixed prosthodontics: J Prosth Dent, 1988; 60; 148-51
65. Jing L, Chen JW, Roggenkamp C, Suprono MS, Effect of crown preparation height on retention of a prefabricated primary posterior zirconia crown: Pediat Dent, 2019; 41(3); 229-33
66. Zidan O, Ferguson GC, The retention of complete crowns prepared with three different tapers and luted with four different cements: J Prosthet Dent, 2003; 89(6); 565-71
67. Shim JS, Lee JS, Lee JY, Effect of software version and parameter settings on the marginal and internal adaptation of crowns fabricated with the CAD/CAM system: J Appl Oral Sci, 2015; 23; 515-22
68. O’Kray H, Marshall TS, Braun TM, Supplementing retention through crown/preparation modification: An in vitro study: J Prosthet Dent, 2012; 107(3); 186-90
69. Martins LM, Lorenzoni FC, Melo AO, Internal fit of two all-ceramic systems and metal-ceramic crowns: J Appl Oral Sci, 2012; 20; 235-40
70. Soto-Montero J, de Cassia Romano B, dos Santos Noronha M, Microtensile bond strength of resin cements to 3-D printed and milled temporary restorative resins: Odovtos-Int J Dent Sc, 2023; 114-30
71. Michalakis K, Pissiotis AL, Kang K, The effect of thermal cycling and air abrasion on cement failure loads of 4 provisional luting agents used for the cementation of implant-supported fixed partial dentures: Int J Oral Maxillofac Implants, 2007; 22(4); 569-74
72. Rajkumar K, Bhat AM, Krishna PD, Effect of axial groove and resin luting cements on the retention of complete cast metal crowns: Dent Res J, 2009; 6(1); 39
73. Mansour A, Ercoli C, Graser G, Tallents R, Moss M, Comparative evaluation of casting retention using the ITI solid abutment with six cements: Clin Oral Implants Res, 2002; 13(4); 343-48
74. Abullais SS, Patel SI, Asiri EA, Comparative evaluation of 3 commercial mouthwash formulations on clinical parameters of chronic gingivitis: Med Sci Monit, 2022; 28; e937111
Figures
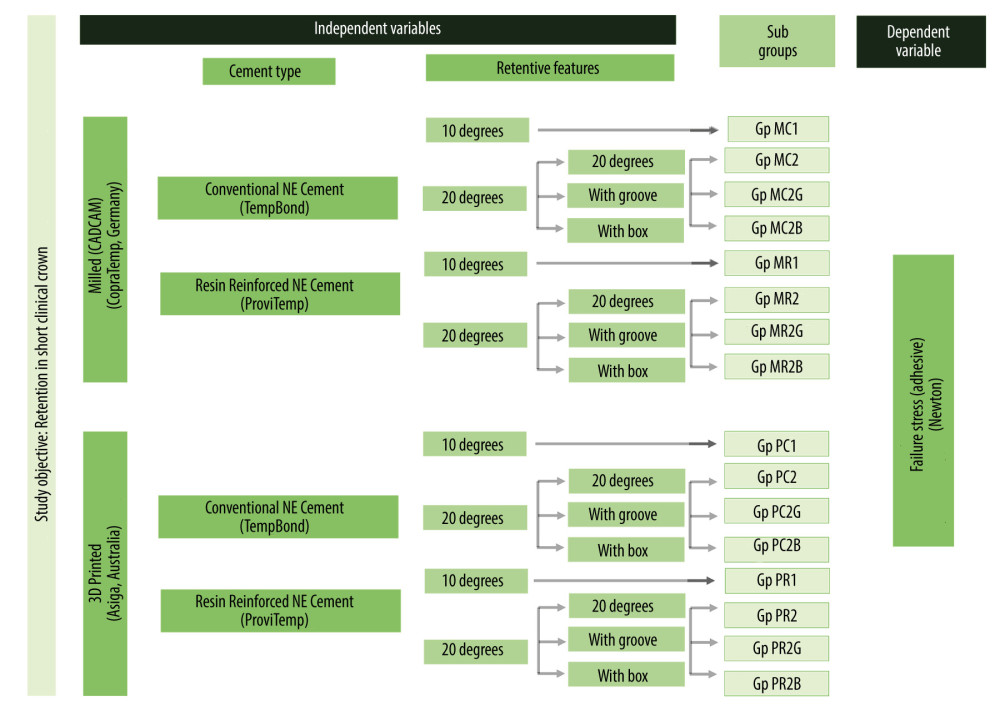 Figure 1. Flowchart showing study sampling and group distribution. Figure created using MS PowerPoint, version 20H2 (OS [operating system] build 19042,1466), windows 11 Pro, Microsoft [MS] Corporation).
Figure 1. Flowchart showing study sampling and group distribution. Figure created using MS PowerPoint, version 20H2 (OS [operating system] build 19042,1466), windows 11 Pro, Microsoft [MS] Corporation).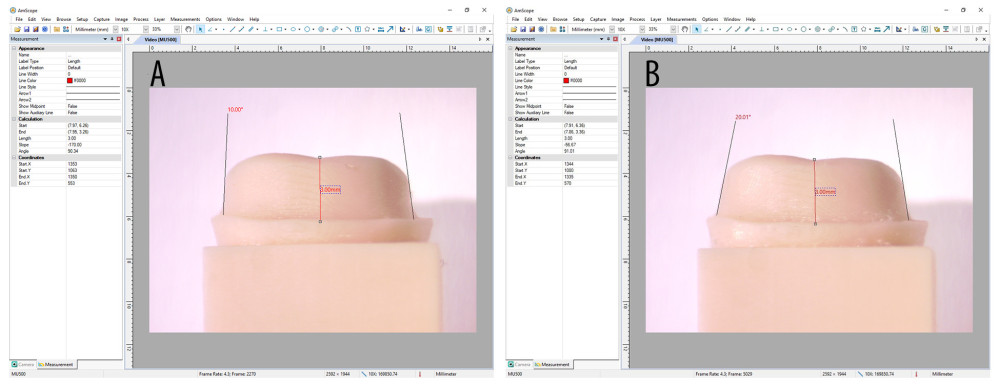 Figure 2. Working models (A) 10-degree preparation taper and (B) 20-degree preparation taper verification of master models. Figure created using Microsoft Snip and Sketch 10.2008.30001.0 followed by compilation on MS PowerPoint, version 20H2 (OS [operating system] build 19042,1466), Windows 11 Pro, Microsoft [MS] Corporation).
Figure 2. Working models (A) 10-degree preparation taper and (B) 20-degree preparation taper verification of master models. Figure created using Microsoft Snip and Sketch 10.2008.30001.0 followed by compilation on MS PowerPoint, version 20H2 (OS [operating system] build 19042,1466), Windows 11 Pro, Microsoft [MS] Corporation).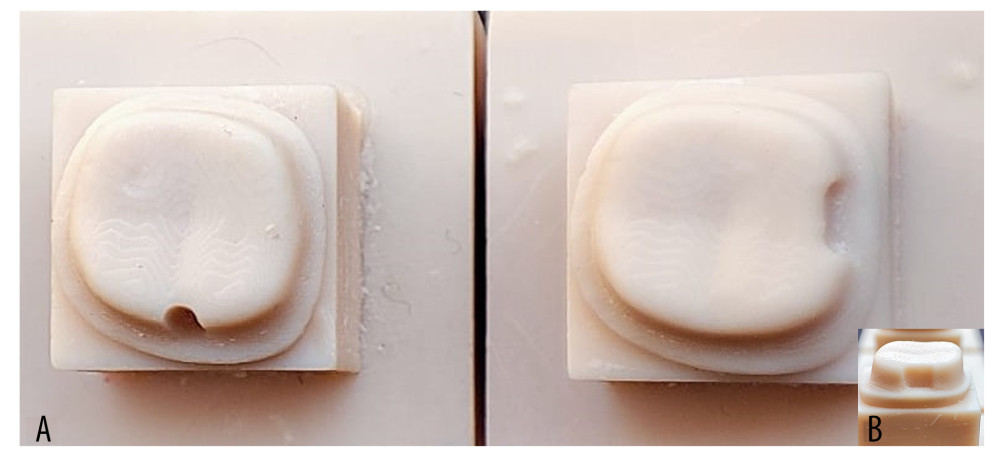 Figure 3. (A) 20-degree taper 3D-printed models on which auxiliary retentive groove (buccal) and box (proximal) were prepared. (B) Inset showing proximal view of the box preparation. Photograph taken using a digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash followed by compilation on MS PowerPoint, version 20H2 (OS [operating system] build 19042,1466), Windows 11 Pro, Microsoft [MS] Corporation.
Figure 3. (A) 20-degree taper 3D-printed models on which auxiliary retentive groove (buccal) and box (proximal) were prepared. (B) Inset showing proximal view of the box preparation. Photograph taken using a digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash followed by compilation on MS PowerPoint, version 20H2 (OS [operating system] build 19042,1466), Windows 11 Pro, Microsoft [MS] Corporation.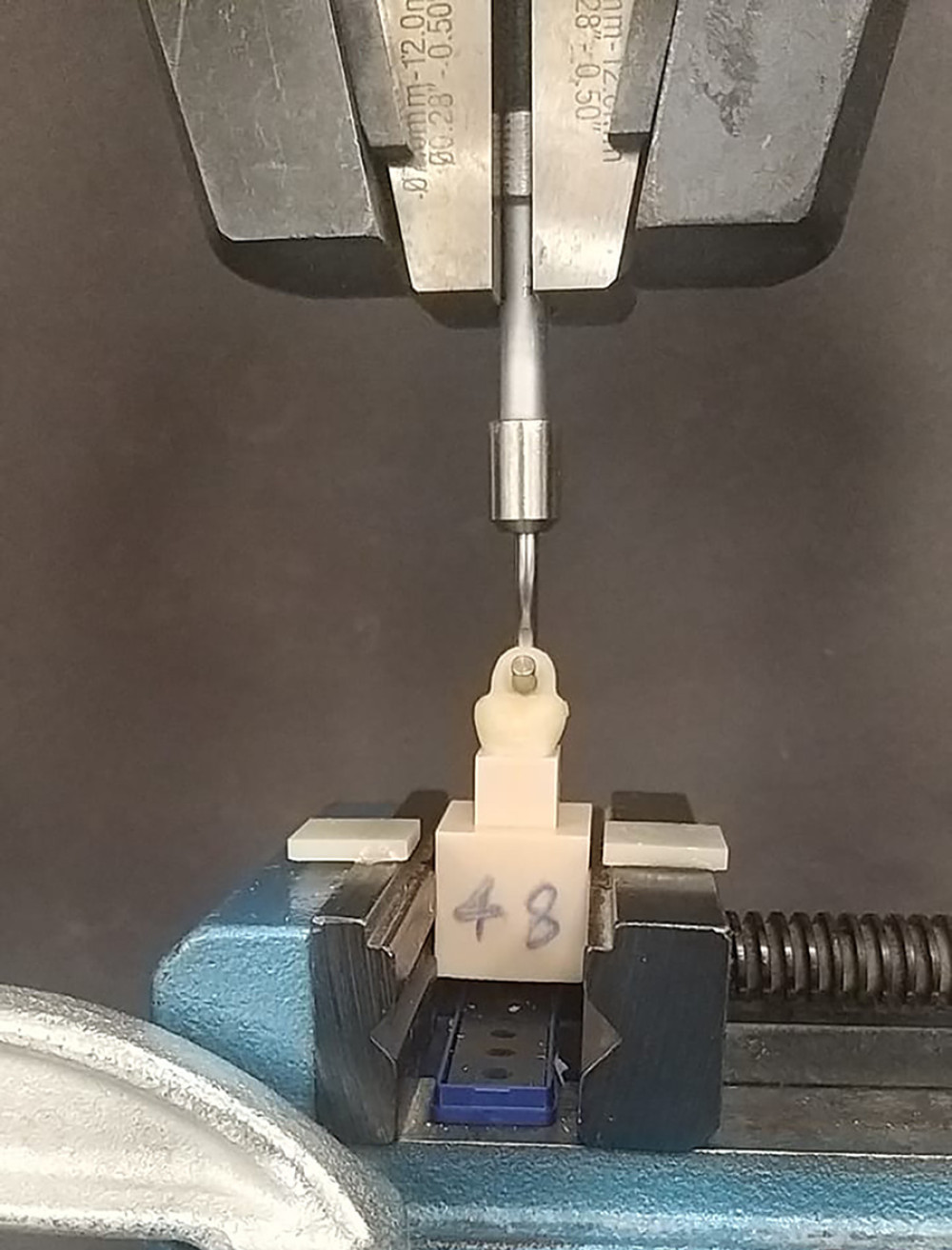 Figure 4. Universal testing machine showing engagement of the test samples for the pull-off test with handles of the provisional crowns aligned to engage the sample handle perpendicular to the line of direction of pulling force. Photograph taken using a digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash.
Figure 4. Universal testing machine showing engagement of the test samples for the pull-off test with handles of the provisional crowns aligned to engage the sample handle perpendicular to the line of direction of pulling force. Photograph taken using a digital single-lens reflex (DSLR) camera (Canon EOS 700D) with 100 mm macro lens) with/without ring flash.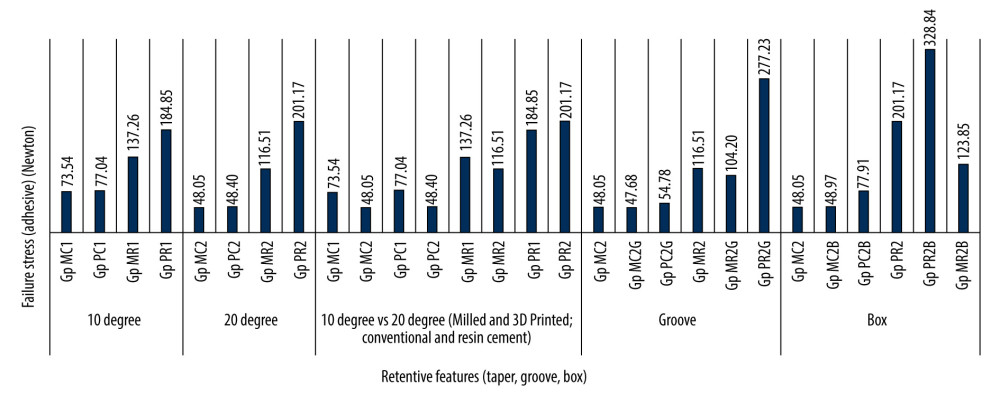 Figure 5. Influence of supplementary retentive features (taper, groove, box) on the mean tensile forces for 2 different provisional crown materials (milled vs 3D-printed) cemented with 2 different provisional cements (conventional vs resin-modified). Figure created using ms excel sheet, version 20h2 (os [operating system] build 19042,1466), windows 11 pro, Microsoft [ms] Corporation).
Figure 5. Influence of supplementary retentive features (taper, groove, box) on the mean tensile forces for 2 different provisional crown materials (milled vs 3D-printed) cemented with 2 different provisional cements (conventional vs resin-modified). Figure created using ms excel sheet, version 20h2 (os [operating system] build 19042,1466), windows 11 pro, Microsoft [ms] Corporation). Tables
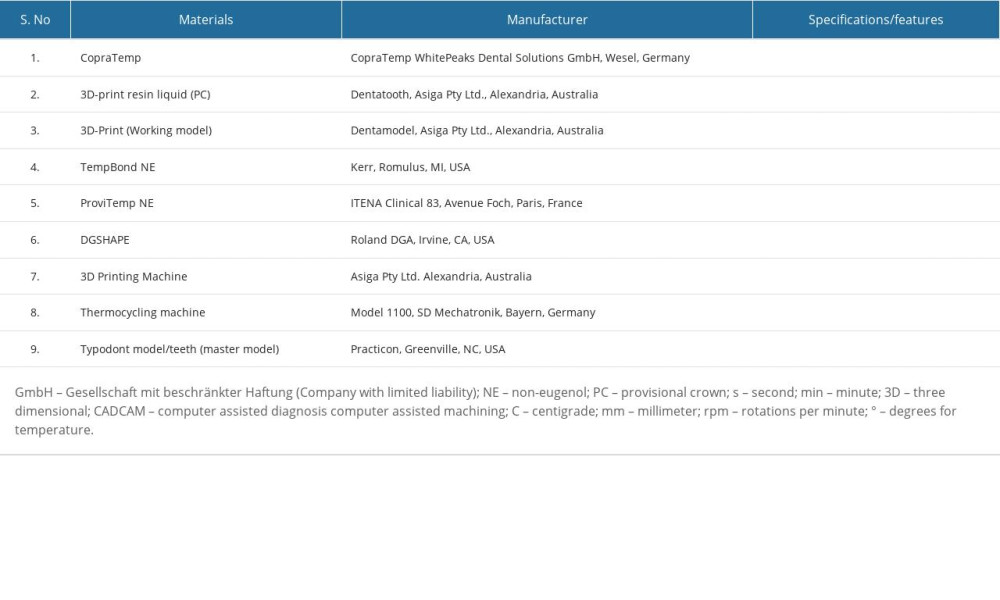 Table 1. List of materials, instrumentation, and manufacturer.
Table 1. List of materials, instrumentation, and manufacturer.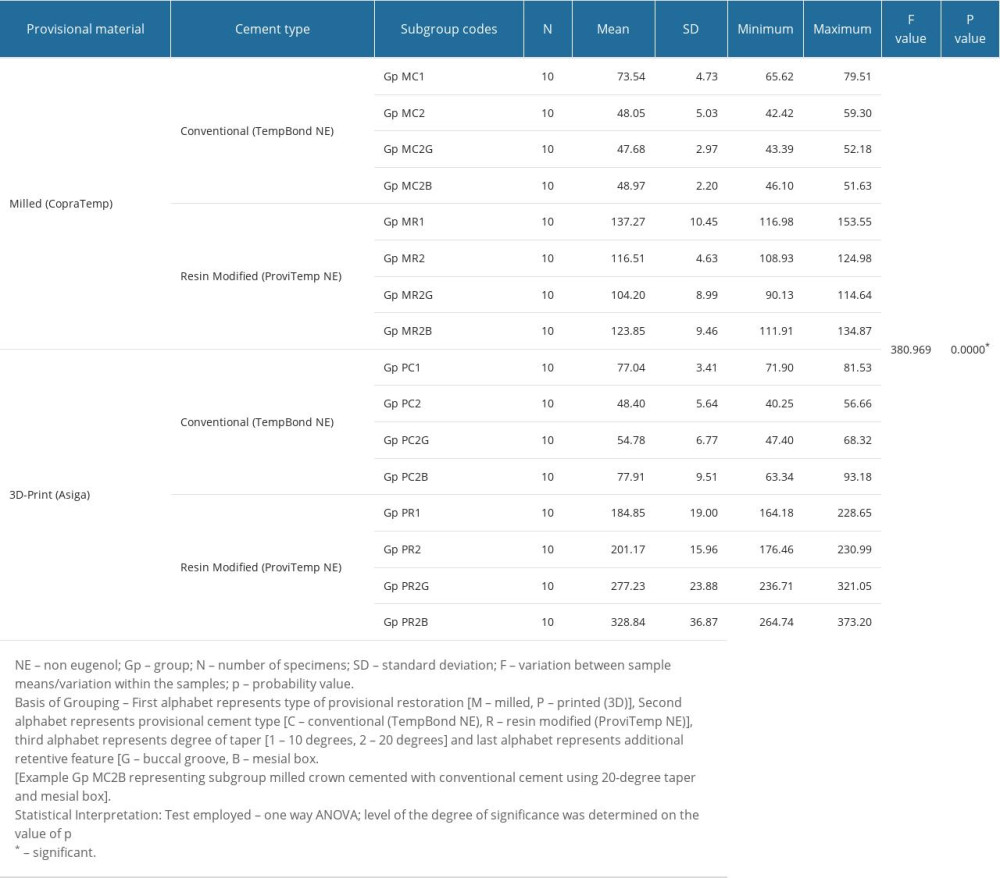 Table 2. One-Way ANOVA test results for comparison of tensile forces between 2 provisional crown materials (milled vs 3D-printed) cemented with 2 different provisional cements (conventional vs resin-modified) using different retentive features (taper, groove, box).
Table 2. One-Way ANOVA test results for comparison of tensile forces between 2 provisional crown materials (milled vs 3D-printed) cemented with 2 different provisional cements (conventional vs resin-modified) using different retentive features (taper, groove, box). Table 3. Post hoc (Tukey HSD) test results for multiple group comparison showing differences in means and level of significance of these differences between 2 provisional crown materials (milled vs 3D-printed) cemented with 2 different provisional cements (conventional vs resin-modified) using different retentive features (taper, groove, box).
Table 3. Post hoc (Tukey HSD) test results for multiple group comparison showing differences in means and level of significance of these differences between 2 provisional crown materials (milled vs 3D-printed) cemented with 2 different provisional cements (conventional vs resin-modified) using different retentive features (taper, groove, box).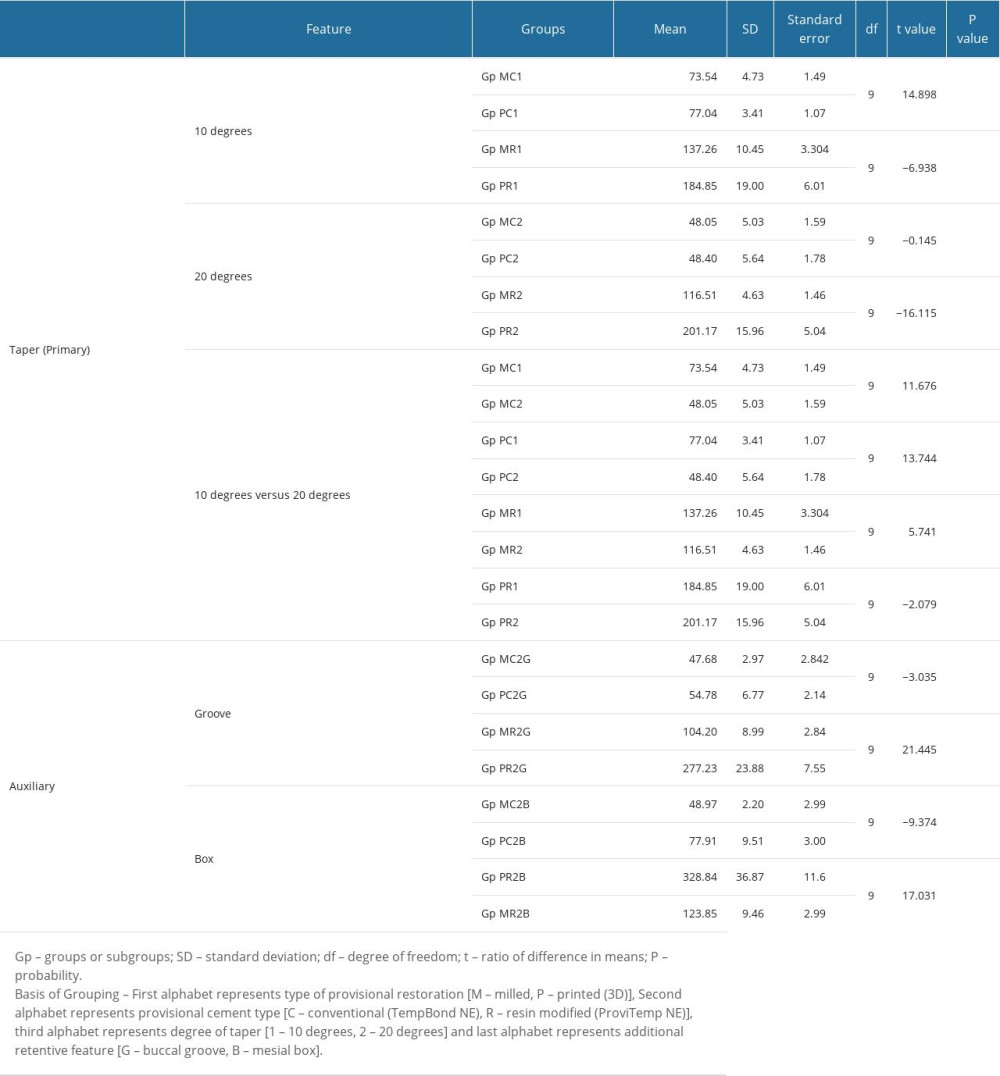 Table 4. Comparative differences in mean values showing the effect of various retentive features (taper, supplementary groove, and box) when used in 2 different provisional crown materials (milled/3D-printed) after cementing with 2 different provisional cements (conventional vs resin-modified non-eugenol).
Table 4. Comparative differences in mean values showing the effect of various retentive features (taper, supplementary groove, and box) when used in 2 different provisional crown materials (milled/3D-printed) after cementing with 2 different provisional cements (conventional vs resin-modified non-eugenol).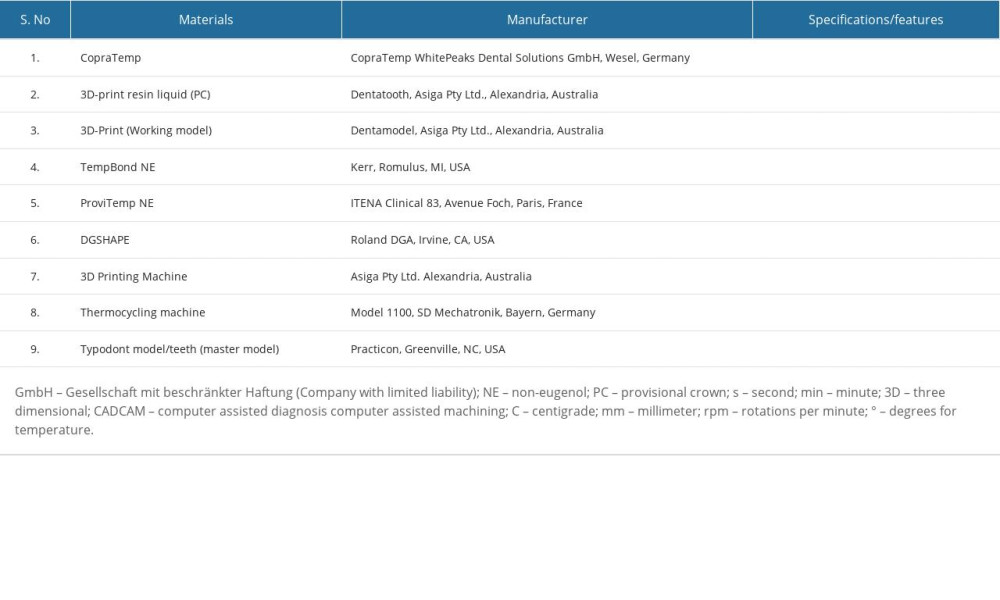 Table 1. List of materials, instrumentation, and manufacturer.
Table 1. List of materials, instrumentation, and manufacturer.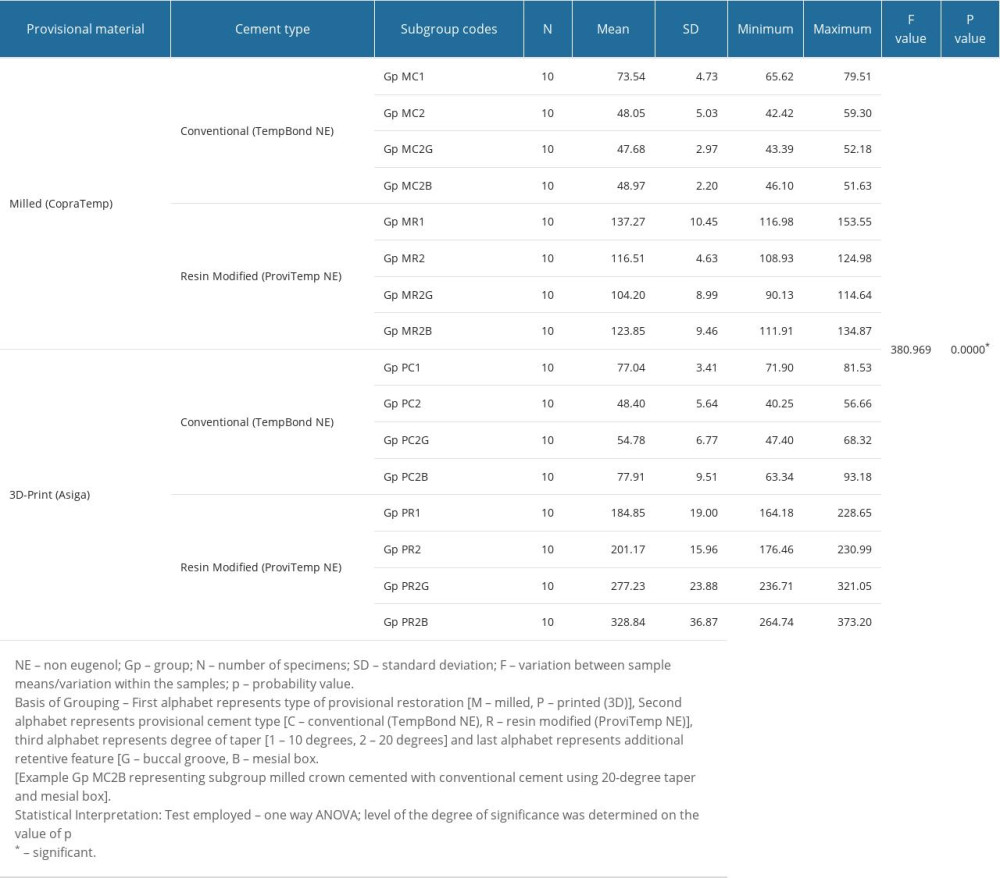 Table 2. One-Way ANOVA test results for comparison of tensile forces between 2 provisional crown materials (milled vs 3D-printed) cemented with 2 different provisional cements (conventional vs resin-modified) using different retentive features (taper, groove, box).
Table 2. One-Way ANOVA test results for comparison of tensile forces between 2 provisional crown materials (milled vs 3D-printed) cemented with 2 different provisional cements (conventional vs resin-modified) using different retentive features (taper, groove, box). Table 3. Post hoc (Tukey HSD) test results for multiple group comparison showing differences in means and level of significance of these differences between 2 provisional crown materials (milled vs 3D-printed) cemented with 2 different provisional cements (conventional vs resin-modified) using different retentive features (taper, groove, box).
Table 3. Post hoc (Tukey HSD) test results for multiple group comparison showing differences in means and level of significance of these differences between 2 provisional crown materials (milled vs 3D-printed) cemented with 2 different provisional cements (conventional vs resin-modified) using different retentive features (taper, groove, box).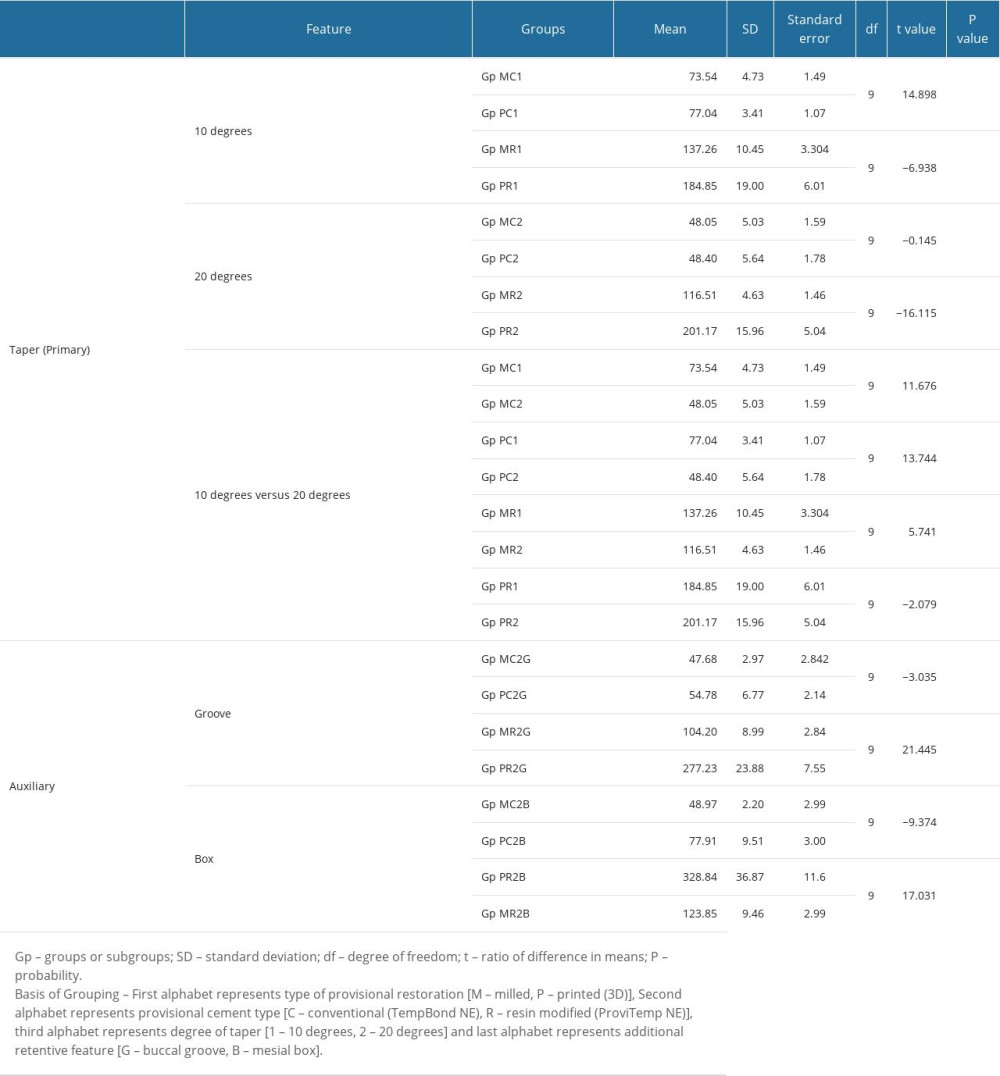 Table 4. Comparative differences in mean values showing the effect of various retentive features (taper, supplementary groove, and box) when used in 2 different provisional crown materials (milled/3D-printed) after cementing with 2 different provisional cements (conventional vs resin-modified non-eugenol).
Table 4. Comparative differences in mean values showing the effect of various retentive features (taper, supplementary groove, and box) when used in 2 different provisional crown materials (milled/3D-printed) after cementing with 2 different provisional cements (conventional vs resin-modified non-eugenol). In Press
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
12 Mar 2024 : Clinical Research
Tissue Inhibitors of Metalloproteinase 1 (TIMP-1) and 3 (TIMP-3) as New Markers of Acute Kidney Injury Afte...Med Sci Monit In Press; DOI: 10.12659/MSM.943500
12 Mar 2024 : Review article
Optimizing Behçet Uveitis Management: A Review of Personalized Immunosuppressive StrategiesMed Sci Monit In Press; DOI: 10.12659/MSM.943240
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








