28 February 2024: Clinical Research
Patterns and Outcomes of Traumatic Suicides: A Retrospective Study of 132 Patients Admitted to a Turkish Medical Center
Meltem GürüDOI: 10.12659/MSM.943505
Med Sci Monit 2024; 30:e943505
Abstract
BACKGROUND: Patients who have attempted suicide by traumatic mechanisms and who present to the Emergency Department (ED) are important due to their severity and high mortality. This retrospective study aimed to evaluate the presentation 132 cases of attempted suicide admitted to a hospital ED in Ankara, Turkey, between September 2022 and August 2023.
MATERIAL AND METHODS: This retrospective study assessed data on 132 adult patients who presented at the ED of Ankara City Hospital due to attempted suicide by traumatic method during a 1-year study period. The descriptive characteristics of the cases, their chronic psychiatric diseases, and the characteristics of their injuries were analyzed based on the duration of stay in the ED and hospital as outcome measures.
RESULTS: Among our study population, 67% were men and 33% were women, and 52% had a previous psychiatric diagnosis. Incision was the predominant trauma mechanism (n=102, 77.3%). Patients with upper-extremity injuries had shorter stays in the ED (P=0.013), while those injured in with motor vehicle-related injuries and those falling from height stayed in the hospital longer (P=0.018).
CONCLUSIONS: In the traumatic suicides discussed, upper-extremity injuries with incision predominated. Upper-extremity injuries had shorter ED treatment times. Those injured by falling from heights or by motor vehicles required longer clinical care in the hospital.
Keywords: Mental Health, Preventive Medicine, Preventive Psychiatry, Suicide, Attempted, Trauma Centers
Background
Suicide refers to a range of self-harm behaviors that begin with thoughts and continue with a suicidal attempt possibly ending with death [1]. It is a complex behavioral pattern in which many biological, psychological, sociological, cultural, existential, historical, religious, philosophical, and economic factors are intertwined. It occurs in a wide range of society, from normal people who react to stressful living conditions to patients with severe mental disorders [1]. On the other hand, it is an important cause of death and disability [2]. The WHO (World Health Organization) recognizes suicide as a global public health problem and reports that 700 000 people die from suicide each year [3]. In 1981–2021 US (United States) data, suicides gradually increased and ranked second among all causes of death. In the same data, the most common cause of death was unintentional injuries [4]. When various reports are examined chronologically, it becomes clear that the number of suicides is increasing worldwide, which reveals that suicides are one of the public health problems that our society urgently needs to solve [4]. Various studies have emphasized that younger people are at higher risk [1, 5] and although this is generally accepted, it would also be valuable to obtain demographic data such as age only in cases of traumatic mechanisms.
Caring for emergency department (ED) patients with possible or attempted suicide also poses some difficulties. Whether the patients will attempt suicide again or not is a serious challenge for ED clinicians to make discharge decisions in terms of mortality. In addition, in cases where psychiatric beds are full for patients requiring hospitalization, monitoring the patient with a possible suicide waiting in the emergency room also causes problems for the EDs [6]. Patients who are treated in the ED for attempted suicide with a traumatic mechanism are also important [7,8]. In the US, firearms are the leading method used in suicide attempts with traumatic mechanism [9]. It is known that patients who recover from severe trauma have a lower risk of recurrence of suicide attempts in later life [7,8]. According to US data, the leading mechanism in completed suicide attempts is firearm wounds [9]. Among ED patients, those who attempted suicide using traumatic mechanisms are of particular importance due to their severity and high mortality [7], showing that it is necessary to focus on traumatic suicide attempts. Our study focused on the demographic characteristics, clinical course, treatment duration, mortality, previous chronic diseases, and especially psychiatric diagnoses of cases. The possible effects of these factors on traumatic suicide attempts and their completion were investigated in a very high-capacity Turkish medical center. This center has various emergency and surgical intervention possibilities and is also a regional referral center that accepts traumatic cases from other centers via ground and air ambulances [10]. Factors affecting the choice of mechanism and the patients’ clinical course were examined a high-capacity ED. The risk of suicide in individuals with a psychiatric pathology is higher than in the normal population [11]. Sometimes it is thought that a suicide attempt is caused by a new undiagnosed psychiatric disease [12]. Examining the mechanisms-related processes of suicide may also be important in terms of psychiatric diagnosis and treatment [11].
A good understanding of attempted suicide cases is as critical as the care of suicide cases in the ED. Detecting such cases before suicide occurs, or if there is no mortality, recognizing the risks of re-suicide and following up these individuals with preventive health services, is life-saving. For this reason, the terms suicidal ideation and parasuicide are also used, and patients who fit this definition must be carefully assessed by both emergency medicine clinicians and psychiatrists. Thoughts and wishes about death and suicide in the human mind are called suicidal ideation [2,13], which is a very broad term and the lack of a precise and consistent definition is a handicap that prevents data from different studies from being compared with each other [14]. Another imprecise term that is difficult to define clearly is parasuicide, which includes attempted suicide and personal self-harm behaviors that do not result in death [15,16]; it is a predictor of successful suicidal behavior and therefore should be taken into consideration clinically [16]. This retrospective study aimed to evaluate the presentation 132 cases of attempted suicide admitted to a hospital ED in Ankara, Turkey, between September 2022 and August 2023.
Material and Methods
ETHICS APPROVAL AND STUDY DESIGN:
This study was approved by the Ankara Bilkent City Hospital’s Ethics Committee-2 on October 25, 2023, with approval number E2-23-5320. Following ethics approval, the study was conducted in the ED of Ankara Bilkent City Hospital, a single large-capacity center. This hospital is a center where many emergency and surgical procedures can be performed, patients can apply on their own, and cases are referred from the surrounding area via ground and air ambulances. Within the scope of the study, adult cases aged 18 and over who were admitted to the ED during the 1-year period between September 01, 2022 and August 31, 2023, and who were brought to the emergency room due to attempted suicide with a traumatic method were included. Patients who simultaneously used another suicide method along with trauma and patients with irreparable deficiencies in the data set were excluded from the study. Patients under the age of 18 years were not included. Of course, this may cause some differences when obtaining demographic results and may constitute a limitation of the study.
DATA COLLECTION:
Data on patients’ age, gender, marital status, recurrent suicide attempt, how they attempted suicide, serious injury, superficial injury, previous psychiatric diagnosis, comorbidities, mortality, length of stay in the emergency room, length of hospital stay, and injured body zones were recorded. The dataset was obtained by scanning hospital electronic records. Although data about diagnoses were obtained, the retrospective design created limitations in accessing data from psychiatric examinations.
OUTCOME MEASURES:
Descriptive characteristics of the cases such as age, gender, marital status, chronic psychiatric and non-psychiatric diseases, and duration of stay in the ED and hospital were evaluated as outcome measures. Trauma-related data such as injury types and body zones injuries were also examined by comparing them with the duration of stay in the ED and hospital.
STATISTICAL ANALYSIS:
SPSS (IBM Corp., Armonk, NY, USA) version 25 was used for analysis. Demographic descriptive data of the patients are expressed as (n) and (%). The suitability of the data for normal distribution was checked with the Shapiro-Wilk test, and since it was seen that it did not fit, nonparametric tests were used. The chi-square test and Fisher exact test were used for analysis of categorical variables. The Mann-Whitney U test was used for analysis of 2 independent groups. For analysis of multiple independent groups, the Kruskal-Wallis test was used and post hoc analysis was performed with the Mann-Whitney U test. Spearman correlation analysis was used for numerical variables. The alpha error of the study was accepted as 0.05.
Results
DEMOGRAPHIC CHARACTERISTICS OF PATIENTS:
We included 132 patients in the study; 89 (67%) were male and 43 (33%) were female. Most of the patients were single (n=94, 71.2%). The mean age of the patients was 31.83 years (min: 18, max: 92). When age mean values were examined separately according to marriage status, the average age of singles was 28 and the median value was 26 (min: 18, max: 91). The average age of the married group was 38 years and the median was 34 years (min: 23–max: 62), while the average age of the divorced group was 40 years and the median was 33 years (min: 22, max: 92). Approximately half had a diagnosed psychiatric disorder (n=68, 52%). Most of them did not have any other non-psychiatric chronic diseases (n=126, 95%). The most commonly diagnosed psychiatric disease – depression – had a prevalence rate of 20%. Following closely in the second position was alcohol and substance addiction, with a prevalence rate of 17%; 13% were women and 87% were men (Table 1).
TRAUMA MECHANISMS AND FINDINGS:
Most patients (n=102, 77.3%) attempted suicide by incision; the most commonly injured body area was the upper extremities (n=46, 34.8%). Most of them had no serious injuries (n=108, 81.8%), and superficial injuries predominated (n=99, 75%) (Table 1).
CLINICAL OUTCOMES:
The mean value of length of stay of the cases in the ED was 9 h and the mean length of stay in the hospital was 3 days. The mechanism of trauma, such as motor vehicle injuries and falls from height, affected the length of hospital stay. Those with motor vehicle injuries and those who fell from height stayed in the hospital for a significantly longer time (P=0.004). There was no correlation between current psychiatric diagnoses and length of hospital stay (P=0.076). The hospital stay of those with head and neck injuries was significantly shorter than those with injuries to other body parts (P=0.018). Only 1 patient’s suicide attempt was completed and resulted in death; this female patient, at 91 years old, was the oldest case. Her trauma mechanism was falling from height. Data regarding the length of stay of patients in the ED are presented in Table 2. Age, gender, known diseases, type of trauma, whether the injury was serious or superficial were not significantly associated with length of stay of the patients in the ED, but married patients stayed in the ED longer than others (P=0.079; Z=−1.757). When the length of stay in the ED was compared with body zone injuries, a significant difference was found, and patients with thorax-abdomen injuries (p=0.46; Z=−1.994) and multi-trauma patients (P=0.003; Z=−2.935) stayed in the ED longer. No correlation was found between the mechanism of trauma and the length of stay in the ED. A correlation was found between length of hospital stay and trauma mechanisms. This difference was observed in patients who fell from a height (P=0.001; Z=−3253) and patients who attempted suicide by motor vehicle injury (P=0.004; Z=−2.874), who stayed in the hospital longer. A significant difference was found in the length of hospital stay depending on the body area injured. Patients with head and neck trauma (P=0.046; Z=−1.999) and patients with multi-trauma (P=0.017; Z=−2.389) stayed in the hospital longer (Tables 2, 3).
Discussion
In this study, most of the patients who attempted suicide and were treated in the ED were younger people and males. The most affected body zone was the upper extremities. Incisions were the most common trauma mechanism. We found that the length of hospital stay varied significantly depending on the mechanism and the injured body zone. According to current CDC (Centers for Disease Control and Prevention) data, most people who attempt suicide are male, and the same report showed a slightly higher incidence in the 16–44 year age range [9]. As in this study, Hadjizacharia et al, in their report dealing with suicides attempted only by the trauma mechanism, found the average age to be 35 years old and 83% were males [7]. Usul et al in Ankara, the same city where the present study was conducted, examined the cases of completed or attempted suicide, and found most were young and male. Even though non-traumatic suicides and attempts were also included in the study by Usul et al, our age and gender results were similar to theirs [1]. While Sahu et al reported the demographics of suicide cases in all age groups, they reported that young age and male gender predominated [12]. Compared to these data, the age and gender findings of our study are similar to the literature. Al-Khatri et al, in the report they presented with the data they collected on suicides committed by all traumatic and non-traumatic mechanisms in Oman, similarly found that most were young people, but there were more women, suggesting geographic differences. Compilations or meta-analyses that combine data from all over the world on gender and age may provide more accurate results on risk groups [5]. Hadjizacharia et al associated the young age of the cases with the weak awareness that suicide is irreversible in adolescence [7]. Accordingly to them and results of this report, it can be predicted that suicidal ideation decreases somewhat as age increases. The fact that our completed suicide case was the oldest patient, even though it was only 1 case, is compatible with the high mortality rate in elderly suicide cases in the literature, but more comprehensive studies are needed to clarify this. Suicides in the elderly group have been examined in other studies; for example, O’Connel et al stated that the rate of suicide completion increases after the age of 65 and that the number of successful suicide attempts increases proportionally compared to the unsuccessful suicide attempts [17]. Akbari et al reported more successful suicides among males [18]. The present study included 132 patients, but since the there was only 1 successful suicide attempt, we cannot make a comparison with the literature in these contexts. Subsequent reports can be written in the future in which this comparison can be made with other data on successful suicides. However, in terms of age and gender, similar to the literature, the predominance of males and younger people stands out and should be considered by psychiatrists and public health specialists. The majority of the traumatic suicide cases in our study were single. Akbari et al conducted a 5-year study assessing the relationship between marriage status and suicide attempts, finding that most of their subjects were single and that most successful suicides were married people [18]. Since there was only 1 successful suicide in our study, we cannot make a comparison in this sense. However, the very high rate of single individuals in our study is noteworthy. This inference is also guiding information for clinicians. Akbari et al found that marital status is not a factor that reduces suicidal ideation, and that the frequency of suicide is lower in married people because they tend to be older [18], which agrees with the present findings. However, many believe that being married reduces the risk of suicide. To resolve this difference in opinion, further research with different methodologies and data are needed.
Mental disorders are the most common suicide risk factors, and the presence of psychiatric disorders among people attempting suicide is 10 times higher than in the general population [19,20]. It is well-established in the literature that depressive symptoms and alcohol-substance misuse, among clinical factors, are recognized risk factors for suicide. Additionally, most patients with alcohol and substance addiction are male [19]. Therefore, the findings of our study align with the existing literature.
Trauma is the leading suicide mechanism both in Turkey and globally [20,21]. In CDC data, which considers all traumatic and non-traumatic suicides, it is seen that suicide with a firearm is the leading mechanism [9]. Hadjizacharia et al evaluated only the suicides committed with trauma mechanisms and found that the highest number of suicides were committed by firearms [7]. In our study, there were more superficial incisions than firearm injuries, and there were far fewer successful suicides than in the literature. We believe that choosing the mechanism of incision instead of a firearm reduces mortality. This situation can be explained by both the determination of the idea of suicide and the more limited access to firearms. However, more precise data on suicide mechanisms and intervention outcomes are needed in this context.
This study has some limitations, such as its retrospective design. In addition, data on trauma and psychiatric examinations are limited to hospital records. It would be possible to obtain more detailed data in studies examining the same subject prospectively. Almost all patients attempted suicide without resulting in death, suggesting that we did not include many patients with a strong determination to die by suicide. This consideration is important when interpreting the results of this study in future research.
Conclusions
Men and young people are at highest risk for attempting suicide by trauma. The most common trauma mechanism for suicide is incision. The upper extremities are the most frequently injured body zone. Cases who fall from heights and have multiple traumas have longer hospital stays. Those who attempted suicide through trauma mostly did not have a previous psychiatric diagnosis. This study underscores the imperative of recognizing and addressing trauma-induced suicides in psychiatry. By integrating trauma-focused perspectives into assessments and interventions, mental health professionals can enhance the quality of care, ultimately fostering improved outcomes for individuals grappling with the complex interplay of trauma and suicidal tendencies.
Tables
Table 1. Demographic characteristics, injury patterns, and clinical outcomes of patients who attempted suicide with traumatic mechanisms and evaluated in an emergency department.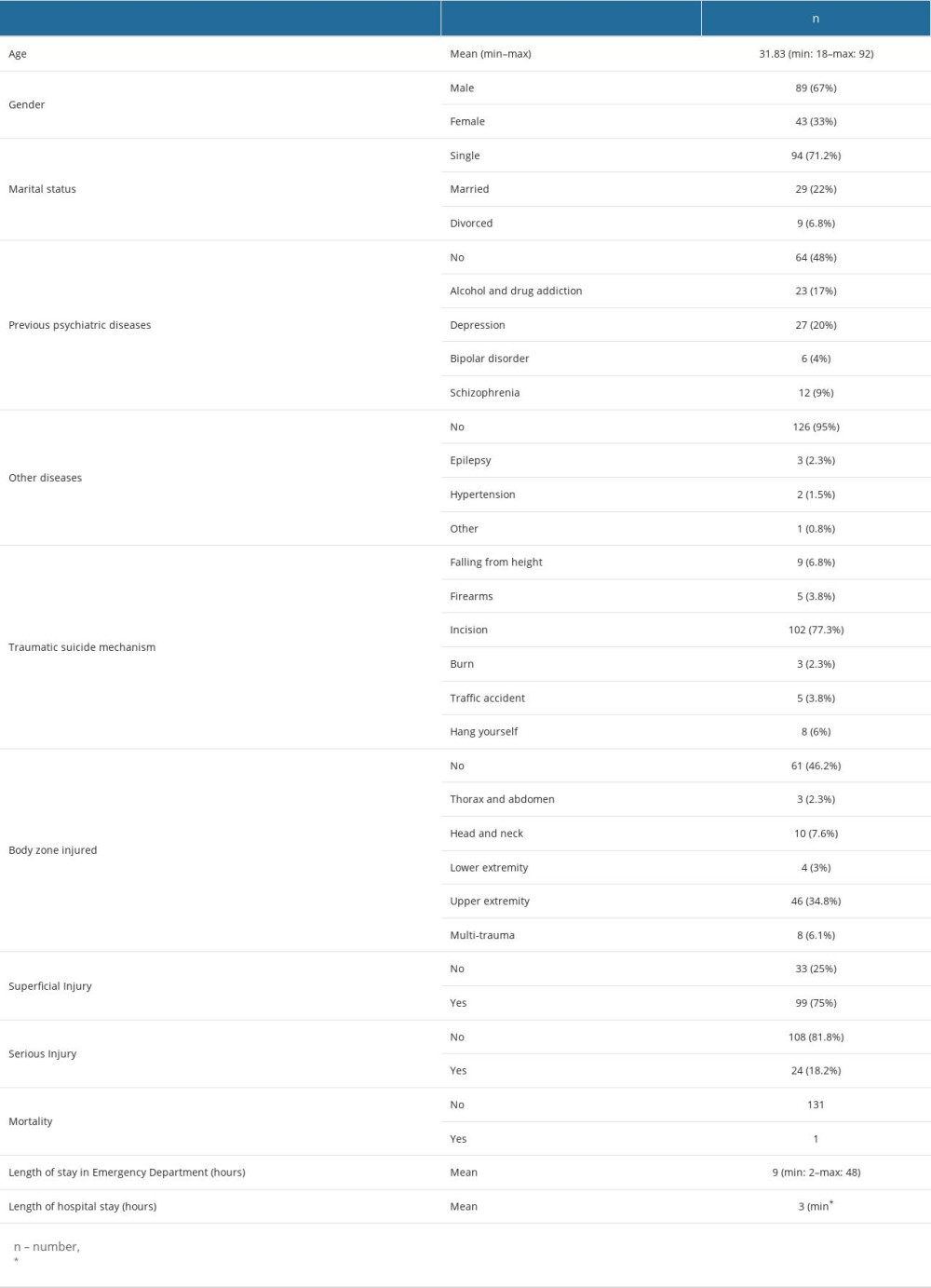 Table 2. Comparisons of demographic characteristics, injury patterns, and clinical outcomes of patients who attempted suicide with traumatic mechanisms and evaluated in emergency department, with length of stay in emergency department.
Table 2. Comparisons of demographic characteristics, injury patterns, and clinical outcomes of patients who attempted suicide with traumatic mechanisms and evaluated in emergency department, with length of stay in emergency department. Table 3. Comparisons of demographic characteristics, injury patterns, and clinical outcomes of patients who attempted suicide with traumatic mechanisms and evaluated in emergency department, with length of hospital stay.
Table 3. Comparisons of demographic characteristics, injury patterns, and clinical outcomes of patients who attempted suicide with traumatic mechanisms and evaluated in emergency department, with length of hospital stay.
References
1. Usul E, Şan İ, Korkut S, Analysis of suicide cases from Ankara Province: A 3-year emergency medical services experience: Acta Biomed, 2022; 93(2); e2022083
2. Klonsky ED, May AM, Saffer BY, Suicide, suicide attempts, and suicidal ideation: Annu Rev Clin Psychol, 2016; 12; 307-30
3. World Health Organization (WHO): Factsheet. Suicide August 28, 2023 Available from: https://www.who.int/news-room/fact-sheets/detail/suicide
4. Centers for Disease Control and Prevention (CDC), National Center for Injury Prevention and Control October 25, 2023 Available from:https://www.cdc.gov/injury/wisqars/animated-leading-causes.html
5. Al Khatri M, Al Huseini S, Almaqbali M, Sociodemographic characteristics and clinical profile of suicide attempters attending the Emergency Department at a Tertiary Care Hospital in Oman: A retrospective study: J Psychiatr Pract, 2023; 29(5); 390-402
6. Betz ME, Boudreaux ED, Managing suicidal patients in the Emergency Department: Ann Emerg Med, 2016; 67(2); 276-82
7. Hadjizacharia P, Brown CVR, Teixeira PGR, Traumatic suicide attempts at a Level I Trauma Center: J Emerg Med, 2010; 39(4); 411-18
8. Wirbel RJ, Olinger A, Karst M, Treatment of severe injuries caused by attempted suicide: Pattern of injury and influence of the psychiatric disorder on the postoperative course: Eur J Surg, 1998; 164(2); 109-13
9. Centers for Disease Control and Prevention (CDC), National Center for Injury Prevention and Control October 25, 2023 Available from:https://www.cdc.gov/injury/wisqars/animated-leading-causes.html
10. Özensoy HS, Gürü S, Helicopter ambulance transport to the Emergency Department: Demographic and clinical factors impacting outcomes in a Turkish Medical Center: Med Sci Monit, 2023; 29; e941464
11. Wasserman D, Carli V, Iosue M, Suicide prevention in psychiatric patients: Asia Pac Psychiatry, 2021; 13(3); e12450
12. Sahu S, Sahu RN, Agarwal J, Soni R, Sociodemographic, clinical profile, and psychiatric morbidities among patients with attempted suicide in a tertiary care center: A study from Central India: Ind Psychiatry J, 2021; 30(Suppl 1); S115-S19
13. Harmer B, Lee S, Duong TVH, Suicidal ideation: StatPearls, 2023, Treasure Island (FL), StatPearls Publishing Copyright © 2023, StatPearls Publishing LLC
14. Goodfellow B, Kõlves K, de Leo D, Contemporary nomenclatures of suicidal behaviors: A systematic literature review: Suicide Life Threat Behav, 2018; 48(3); 353-66
15. Bagley CR, Greer S, Kreitman N, Parasuicide: Br J Psychiatry, 1969; 115(523); 746-47
16. Comtois Katherine Anne, A review of interventions to reduce the prevalence of parasuicide: Psychiatr Ser, 2002; 53(9); 1138-44
17. O’Connell H, Chin A-V, Cunningham C, Recent developments: Suicide in older people: BMJ, 2004; 329(7471); 895-99
18. Akbarizadeh F, Hajivandi A, Hajivandi M, Marriage related suicide fatality rates: Iran J Psychiatry, 2019; 14(1); 54-59
19. Aiartzaguena M, Morentin B, Risk factors for completed suicide in young people and middle-aged adults: Population forensic study: Spanish Journal of Legal Medicine, 2022; 48(2); 53-59
20. Bachmann S, Epidemiology of suicide and the psychiatric perspective: Int J Environ Res Public Health, 2018; 15(7); 425
21. Yildirim E, Öztürk M, 2009–2018 arasinda Türkiye’de intihar hIzI ve ilişkili özellikler Dokuz Eylül Üniversitesi Tip Fakültesi Dergisi, 2021; 35(1); 23-32 [in Turkish]
Tables
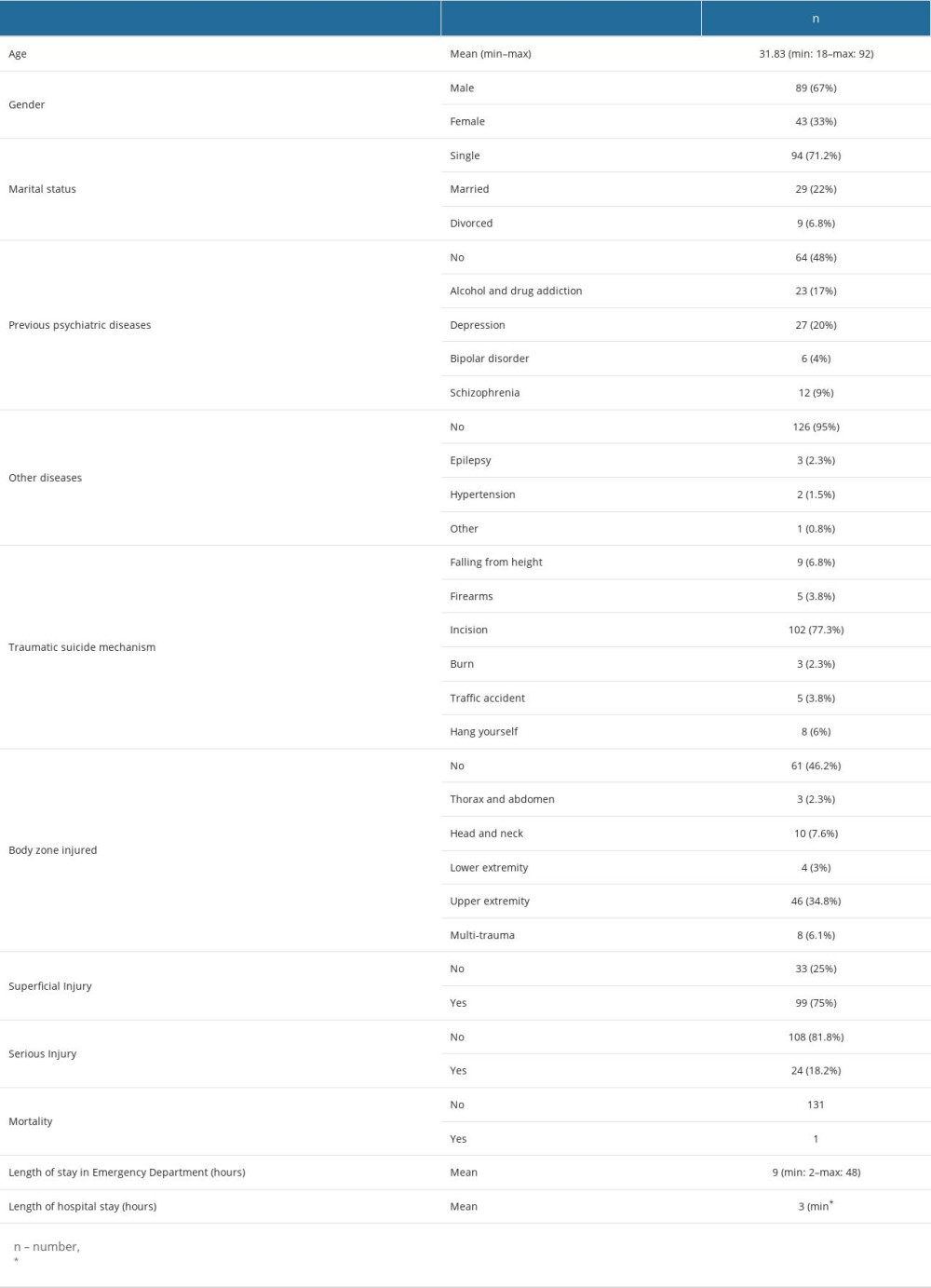 Table 1. Demographic characteristics, injury patterns, and clinical outcomes of patients who attempted suicide with traumatic mechanisms and evaluated in an emergency department.
Table 1. Demographic characteristics, injury patterns, and clinical outcomes of patients who attempted suicide with traumatic mechanisms and evaluated in an emergency department. Table 2. Comparisons of demographic characteristics, injury patterns, and clinical outcomes of patients who attempted suicide with traumatic mechanisms and evaluated in emergency department, with length of stay in emergency department.
Table 2. Comparisons of demographic characteristics, injury patterns, and clinical outcomes of patients who attempted suicide with traumatic mechanisms and evaluated in emergency department, with length of stay in emergency department. Table 3. Comparisons of demographic characteristics, injury patterns, and clinical outcomes of patients who attempted suicide with traumatic mechanisms and evaluated in emergency department, with length of hospital stay.
Table 3. Comparisons of demographic characteristics, injury patterns, and clinical outcomes of patients who attempted suicide with traumatic mechanisms and evaluated in emergency department, with length of hospital stay. In Press
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








