09 June 2024: Clinical Research
Determining the Optimal Dosage of Dexmedetomidine for Smooth Emergence in Older Patients Undergoing Spinal Surgery: A Study of 44 Cases
Hyoeun Ahn1CDEF, Yun Jeong Chae1DEF, Gyu Bin Choi1BF, Min Gyu Lee1BF, Ji Young Yoo1ABCF*DOI: 10.12659/MSM.944427
Med Sci Monit 2024; 30:e944427
Abstract
BACKGROUND: Emergence agitation, or delirium, occurs during early recovery from general anesthesia and involves disorientation, excitation, and uncontrolled physical movements. Dexmedetomidine is an alpha agonist that has sedative, anxiolytic, analgesic, and sympatholytic activities and is used as a continuous infusion to prevent emergence agitation. This study aimed to evaluate patients aged 65 years and older undergoing general anesthesia to determine the 90% effective dose (ED90) of dexmedetomidine continuous intraoperative infusion to prevent emergence agitation.
MATERIAL AND METHODS: We enrolled 44 patients aged 65 years and older undergoing spinal surgery under general anesthesia. Dexmedetomidine administration commenced 30 minutes before surgery completion, with a predetermined infusion dose (μg/kg/h), without a loading dose. The initial dose was 0.2 μg/kg/h, and subsequent step size was ±0.05 μg/kg/h. We tried to find ED90 of dexmedetomidine using the biased-coin design. Vital signs, extubation quality scores, extubation-related complications, and postoperative outcomes were monitored.
RESULTS: Dexmedetomidine ED₉₀ for smooth emergence in older patients was 0.34 μg/kg/h. Peri-extubation vital signs remained within 20% of baseline values, without requiring pharmacological intervention. No hypoxia, hypoventilation, or post-extubation agitation occurred. In the recovery room, 1 patient briefly exhibited excitement but quickly calmed. Nine patients initially unresponsive in the recovery room fully awoke and were promptly discharged.
CONCLUSIONS: For older patients who are vulnerable to adverse effects of anesthetics and opioids, dexmedetomidine enables gentle awakening without adverse vital sign changes, respiratory depression, excessive sedation, or emergence agitation (ED₉₀=0.34 μg/kg/h). Further studies should involve a larger patient cohort, considering diverse medical conditions in older individuals.
Keywords: Dexmedetomidine, Anesthesia, General, Aged, Emergence Delirium, Respiratory Insufficiency
Introduction
During emergence from anesthesia, patients often exhibit an airway reflex response, such as coughing, apnea, and laryngospasm, in response to laryngeal stimulation, primarily due to the presence of an endotracheal tube [1]. This response tends to be more severe and prolonged compared with that in the awake state [1]. Furthermore, it is frequently accompanied by hypertension and tachycardia [2] and can lead to increased intracranial and intra-abdominal pressures [2–4]. This heightened physiological response is especially concerning in older patients with multiple medical comorbidities, resulting in a high incidence of perioperative complications [5,6]. Therefore, the need to achieve a smooth emergence to mitigate this stress response in older patients becomes apparent.
Age ≥65 years was revealed to the risk factor for emergence agitation [7]. Emergence agitation involves restlessness, disorientation, and non-purposeful movement during early recovery from general anesthesia, and the incidence of emergence agitation varies with age from approximately 0.25% to 90.5% in previous studies [8]. Dexmedetomidine has been shown to have a decreased risk of delirium in mechanically ventilated patients, and prevents emergence agitation in children and adults [9,10].
Among the medications studied for achieving a smooth emergence, dexmedetomidine stands out due to its favorable properties, including arousable sedation without respiratory depression, cough suppression, or sympatholytic effects [11]. Therefore, dexmedetomidine may be useful for the smooth emergence of older patients. However, the dose of dexmedetomidine required for smooth emergence in older patients has not been clearly established due to differences in study designs [12]. Continuous infusion of dexmedetomidine without a loading dose has been used to reduce sudden hemodynamic changes caused by a loading dose [13]. Therefore, it can be easily applied during surgery and is particularly safe for older patients with stable hemodynamics. Consequently, this study evaluated 44 patients aged 65 years and older undergoing general anesthesia for spinal surgery to determine the 90% effective dose (ED90) of dexmedetomidine continuously without a loading dose to prevent emergence agitation and to reduce unfavorable respiratory complications.
Material and Methods
ETHICS STATEMENT:
This study was based on anonymous data obtained from the Department of Anesthesiology and Pain Medicine at Ajou University School of Medicine. This study protocol was reviewed and approved by the Institutional Review Board of Ajou University Hospital, approval number AJIRB-MED-OBS-18-331. Written informed consent was obtained from all patients.
STUDY DESIGN:
This study included older individuals aged ≥65 years with an American Society of Anesthesiologists physical status classification system of I to II, who were expected to undergo spine surgery under general anesthesia. The exclusion criteria were: patient rejection, difficult airway to intubate, gastroesophageal reflux disease, severe obesity with a body mass index >35 kg/m2, upper respiratory tract infection within 2 weeks, moderate-to-severe asthma or chronic obstructive pulmonary disease, drug treatment with cognitive impairment such as dementia or Parkinson’s disease, history of cerebrovascular disease, and risk of aspiration.
ANESTHESIA PROTOCOL AND CLINICAL MEASUREMENT:
Upon entering the operating room, patients were monitored using electrocardiography, blood pressure measurement, pulse oximetry, and bispectral index (BIS) (BIS™, Covidien LLC, USA). For anesthesia induction, thiopental (4 mg/kg) and fentanyl (1 mcg/kg) were administered intravenously, and when the patient lost consciousness, rocuronium 0.6 mg/kg was administered. After loss of consciousness, the patient was supplied with 3–5 vol% sevoflurane until endotracheal intubation. Following intubation, sevoflurane was adjusted to maintain a BIS of 40–60 at 1.5–2.5 vol%. Blood pressure (BP) and heart rate (HR) were maintained within 20% of baseline values, and mechanical ventilation was controlled to maintain end-tidal carbon dioxide values at 35–40 mmHg. Blood pressure measurements, pulse oximetry, and BIS were checked and recorded 7 times in the operating room (before anesthesia, dexmedetomidine starting point, dexmedetomidine stopping point, sevoflurane stopping point, just before extubation, 1 minute after extubation, and 5 minutes after extubation) and 3 times in the recovery room (arrival in the recovery room, 10 minutes after arrival, and 20 minutes after arrival).
The administration of dexmedetomidine was initiated at a predetermined infusion rate (μg/kg/h) 30 minutes before the end of the operation and was stopped 5 minutes before the end of the operation (at the start of skin closure). The predetermined dose was determined based on the response of the previous patient. However, the first patient received a fixed dose of 0.2 μg/kg/h as per the biased-coin design. After the operation, sevoflurane was discontinued, and 0.004 mg/kg glycopyrrolate and 0.02 mg/kg neostigmine were administered. Extubation was performed when muscle relaxation returned to normal, and tidal volume and respiratory rate were restored. The emergence time was defined as the time from the end of sevoflurane administration to extubation. Vital signs (BP, HR, oxygen saturation), BIS, emergence agitation, and post-extubation airway complications were observed while supplying the patient with 100% oxygen with a mask. After confirming stability, the patient was transferred to the post-anesthesia care unit (PACU). Five minutes after arriving in the PACU, postoperative nausea and vomiting (PONV), sore throat, hoarseness, and pain index using the numeric rating scale (NRS) were measured. If the pain index was ≥5, rescue fentanyl (1 μg/kg) was administered intravenously to the patient. The consciousness level was evaluated using the Ramsay sedation scale (RSS), which was measured 5 minutes after arrival and just before leaving the PACU. The RSS scores were: 1 – patient anxious and agitated, restless, or both; 2 – patient co-operative, oriented, and tranquil; 3 – patient responds to commands only; 4 – a brisk response to a light glabellar tap or loud auditory stimulus; 5 – a sluggish response; and 6 – no response [14].
The primary endpoint in this study was the presence or absence of smooth emergence, and the secondary endpoints were emergence time; the presence or absence of hypoxia, hypoventilation, or emergence agitation; and occurrence of hypotension or hypertension.
BIASED-COIN DESIGN:
In this study, we aimed to determine the ED90 (effective dose for 90% of patients) of dexmedetomidine in older patients using a biased-coin design [15,16] designed to establish an effective drug dose in >90% of patients. The biased-coin design was a modification of up-and-down methods, and it has been used for determination of the concentration or dose of anesthetic agents along the dose-response curve. In the biased-coin design, the response of the first patient determines the dose level for the second patient [16].
The initial starting dose of dexmedetomidine was 0.2 μg/kg/h, and the subsequent dose was determined based on the effectiveness of the dose (success) or ineffectiveness (failure) as assessed by the extubation quality score. The step size for dose adjustment was 0.05 μg/kg/h. If the dose was found to be ineffective and considered a failure, the dose for the next patient was increased by +0.05 μg/kg/h. Conversely, if the dose was effective and categorized as a success, the next subject received the same dose with a 90% probability, or a dose of −0.05 μg/kg/h was chosen with a 10% probability.
The criteria for smooth emergence, which determined success or failure, were based on the extubation quality score. An extubation quality score of 1 or 2 was considered successful, whereas 3 to 5 indicated failure. The extubation quality score is as follows: (1) no cough and easy breathing; (2) mild cough (defined as a cough mild enough that it did not cause patient’s head to lift from the bed, with an increase in blood pressure and heart rate during coughing of <20%) and easy breathing; (3) moderate cough (1 to 3 of loud coughs that were forceful enough to lift patient head in bed); (4) severe cough (4 or more consecutive loud coughs that caused the patient’s head to lift in bed) and difficulty breathing; and (5) laryngospasm and difficulty breathing [17,18].
STATISTICAL ANALYSIS:
According to a statistical reference [15], the up-and-down method was applied until 6 intersections were reached, typically requiring 35–40 subjects.
Statistical analyses were performed using R version 4.1.0. (The R Project for Statistical Computing;
Results
BASIC PATIENTS CHARACTERISTICS AND ANESTHESIA PROFILES DATA:
We enrolled 44 patients aged ≥65 years who underwent spinal surgery under general anesthesia. The mean age of the patients was 72.8 years. Among the 44 patients, 23 (52.27%) were female and 21 (47.73%) were male. The mean operation time was 140.2 minutes, and the mean anesthesia time was 200.2 minutes. The time from the completion of surgery to extubation, known as the mean emergence time, was 9.36 minutes (shown in Table 1). No significant differences in patient characteristics or basic operative data were observed between patients in whom smooth emergence succeeded and those in whom it failed. No instances of hypoxia, hypoventilation, or emergent agitation were observed following extubation.
CLINICAL RESULTS FOR EFFECTIVE DOSE OF DEXMEDETOMIDINE:
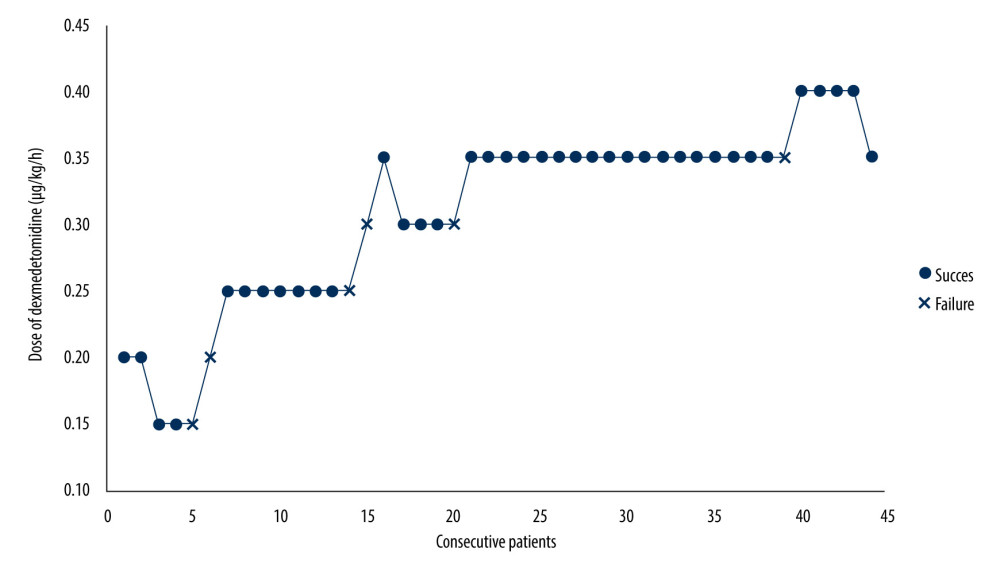
The success and failure responses of each patient at the assigned dose of dexmedetomidine were expressed graphically, with the patient sequence on the x-axis and each assigned dose on the y-axis (shown in Figure 1). In this study, the ED90 of dexmedetomidine, calculated using isotonic regression, was determined to be 0.34 μg/kg/h (95% CI, 0.26–0.38) for older patients undergoing general anesthesia to achieve smooth emergence. The frequency of trials for smooth emergence at each specific dexmedetomidine dose and the observed and PAVA-adjusted response rates for the subjects are presented in Table 2.
THE HEMODYNAMIC AND RESPIRATORY VARIABLES:
Significant changes in vital signs measured from the start of dexmedetomidine administration to 5 minutes after extubation are shown in Table 3. The vital signs were analyzed by dividing them into 2 time points centered around extubation: T1 and T2 (T1: dexmedetomidine starting point, dexmedetomidine stopping point, and sevoflurane stopping point; T2: immediately before extubation, 1 minute after extubation, and 5 minutes after extubation). The definition for these terms at these times were as follows: hypertension, systolic BP (SBP) >20% of baseline value or 150 mmHg, whichever was higher; hypotension, SBP <90 mmHg or mean arterial pressure (MAP) <60 mmHg, whichever was lower; tachycardia, HR >100 bpm; and bradycardia, HR <60 bpm. At T1, hypotension occurred in 22.7% of patients and remained relatively stable, with values close to SBP of 90 mmHg, requiring no use of vasopressors. At T2, hypertension occurred in 47.7% of patients, but was >20% of the baseline value in only 1 patient, and even in this case, the blood pressure decreased to <20% of the baseline value within 1 minute. Tachycardia was reported in only 1 case, with HR remaining <120 bpm, and patients with bradycardia did not require pharmacological treatment. No significant difference in the incidence of hypertension, hypotension, tachycardia, or bradycardia was observed between the patients who achieved smooth emergence and those who did not.
PATIENTS RECORDS IN PACU:
The postoperative data in the recovery room are presented in Table 4. The incidence of PONV was 4.5%, whereas that of sore throat and hoarseness was 22.7% and 20.5%, respectively. The mean NRS score was 4.09±1.82, and 11 patients (25.0%) required rescue fentanyl during their recovery. According to RSS records taken immediately after arrival at the PACU, most patients had an RSS score of 2 (34 patients, 77.2%). One patient (2.2%) had an RSS score of 1, and 9 patients (20.5%) had an RSS score of 3. These agitated or sedative patients recovered to an RSS score of 2 within 5 minutes and were promptly discharged from the ward.
Discussion
This study determined that when a continuous infusion of dexmedetomidine without a loading dose was administered 30 minutes before the end of the operation, the ED90 of dexmedetomidine required to achieve smooth emergence from general anesthesia was 0.34 μg/kg/h in older patients (95% CI, 0.26–0.38). The infusion dose of dexmedetomidine used in this study ranged from 0.15 to 0.4 μg/kg/h, and no adverse effects were reported.
Dexmedetomidine is a selective α2-receptor agonist with sympatholytic, sedative, anxiolytic, and analgesic properties [19]. Furthermore, it is among the most effective agents for alleviating cough during anesthesia emergence to obtain a smooth emergence [20]. However, owing to variations in target groups and regimens in small-series studies, the administration method and appropriate dosage have not been clearly determined, especially in older patients. In several clinical studies [21,22], the sedative and hemodynamic effects of dexmedetomidine were more pronounced in older patients, necessitating a reduction in the loading and maintenance dose [23]. Furthermore, omitting the loading dose is reportedly useful for lessening hemodynamic adverse effects [19,24], and a prolonged infusion time of 15–30 minutes is also sufficient for the clinical effect of dexmedetomidine, such as sedation [25]. In the present study targeting older patients aged ≥65 years, we adopted an infusion method without a loading dose that commenced 30 minutes before the conclusion of the operation and ceased 5 minutes before the end of the operation. This method is easily applicable and allows for a gradual onset of dexmedetomidine with minimal hemodynamic effects, even when combined with various anesthetic drugs during general anesthesia. The choice of a dexmedetomidine starting dose of 0.2 μg/kg/h in this study was based on a previous study that demonstrated an absence of cardiovascular adverse effects when dexmedetomidine infusion without loading dose was administered to patients with an average age of 60 years [13]. The infusion dosage range used in this study spanned from 0.15 to 0.4 μg/kg/h, and no significant hemodynamic changes, such as hypertension, hypotension, tachycardia, or bradycardia, were observed in relation to dexmedetomidine infusion within this range. In terms of clinical utility for achieving smooth emergence, infusing dexmedetomidine within the range of 0.15 to 0.4 μg/kg/h proved effective in mitigating cough during anesthesia emergence in older patients.
The biased-coin design, a modification of the up-and-down method, can directly target a high-quantile effective dose rather than a high-quantile effective dose estimated from ED50; therefore, the biased-coin design is reported to be more suitable if the dose we want to know is ED90 [16]. In this study, using a biased-coin design, the estimated ED90 of dexmedetomidine to achieve smooth emergence from general anesthesia was determined to be 0.34 μg/kg/h in older patients. In children, the estimated ED90 for preventing emergence agitation was 0.74 μg/kg/h [26]. Previous studies on adult patients aged <65 years have reported that administering 0.5 or 0.7 μg/kg for 5 or 10 minutes before the end of surgery [27,28], or continuously infusing at a rate of 0.4 or 0.6 μg/kg/h from anesthesia induction [24,29], was effective in achieving smooth emergence. Similar to our study, a previous study that administered an infusion 30 minutes prior to surgery without a loading dose reported that smooth emergence was achievable in 85% of patients using infusion rates of 0.4 or 0.6 μg/kg/h in patients with an average age of 56–58 years [12]. The infusion dosage measured in this study seems to be lower than those reported in previous studies and even lower than the dosage reported by Wan [12], which used a similar method. This difference may be attributed to 2 factors. Firstly, the infusion method without a loading dose, which allows for a slower onset of the effect, can reduce the amount of dexmedetomidine required, as observed in other studies [22,25]. Secondly, this study specifically targeted older patients with an average age of 71 years, who may require lower dosages because of age-related differences [21].
Tracheal extubation is associated with increased hemodynamic changes, such as hypertension and tachycardia, in both younger and older patients [30]. In this study, based on the occurrence of at least 1 of the first 3 points (dexmedetomidine starting point, dexmedetomidine stopping point, sevoflurane stopping point), hypertension was observed in 7 (15.9%), hypotension in 10 (22.7%), and bradycardia in 24 (54.5%), whereas tachycardia was observed in only 1 patient (2.3%). Considering the time points during extubation (just before extubation, 1 minute after extubation, and 5 minutes after extubation), hypertension was found in 21 (47.7%) patients with no hypotension, whereas bradycardia was observed in 8 patients (18.2%), and tachycardia in only 1 patient (2.3%). In other words, bradycardia was common during anesthesia with dexmedetomidine infusion. However, during extubation, blood pressure increased, and bradycardia decreased. Compared with a previous study [30], the use of dexmedetomidine in this study may have played a role in reducing the occurrence of tachycardia and lessening exaggerated hypertension associated with extubation.
The extubation time in our study was 9.36 minutes, which showed no delay compared with a previous study that used 0.4 μg/kg/h dexmedetomidine infusion in older patients (control group: 10.0 min, dexmedetomidine group: 11.7 min) [31]. This time was significantly shorter than in other studies that used remifentanil for achieving smooth emergence in older patients [32]. In this study, the extubation time was 17.2±4.1 minutes in older patients and 14.0±3.0 minutes in adult patients. Therefore, dexmedetomidine not only avoids delayed emergence but also offers stable recovery.
The mean BIS at 5 minutes after extubation was 88.2. At the time of admission to the PACU, patient levels of sedation based on RSS were as follows: 1 patient was rated as anxious, agitated, or restless; 34 patients were co-operative, oriented, and tranquil; 9 patients responded to commands only; and no patients were rated as having a deeper level of sedation. Only 1 patient exhibited signs of excitement, but quickly returned to a tranquil state. Nine patients who only responded to commands upon admission to the PACU became fully awake and were promptly discharged from the ward. The mean NRS was 4.09, and 11 patients (25%) required rescue fentanyl for pain relief. Additionally, 10 patients reported experiencing sore throat, 9 reported hoarseness, and 2 reported PONV; however, they generally recovered quietly in the recovery room. Based on previous studies that examined the effectiveness of dexmedetomidine on emergence agitation [24,31], the quiet and stable recovery observed in most patients in this study may be attributed to the use of dexmedetomidine. Even taking into account the previously available study indicating that spine surgery is a high-risk factor for emergence agitation [8], the ED90 value in this study would hold significance for patients who underwent surgery with a relatively lower risk of emergence agitation. This is considered a strength of the present study.
This study had several limitations. First, although it derived the ED90 for a specific age group, it could not distinguish differences based on other variables that might have influenced the results. Emergence agitation in adults can be influenced by factors such as sex, type and duration of surgery or anesthesia, and postoperative pain [8]. For instance, emergence agitation tends to occur more frequently in males, as observed in our study where 5 out of 6 patients with failed smooth emergence were male. If we had classified patients by sex, we believe the ED90 value might vary accordingly. Furthermore, this study exclusively focused on patients undergoing spinal surgery. Previous research has shown that the degree of postoperative pain can vary depending on the surgical site [33], and adequate perioperative pain control affects the onset of emergence agitation [8]. Therefore, if the surgical sites differ, there may be a difference in the value of ED90. Second, a drawback of this study is the lack of information about whether the older patients who participated were taking medications that could have affected their smooth emergence. Older patients often take medications for various underlying conditions, but we did not collect data on their pre-surgery information. Finally, due to the absence of a universally agreed-upon definition for smooth emergence, the determination of ED90 in older patients might differ from our study findings. We considered patients with no or mild cough as successful in achieving smooth emergence; however, if only the absence of cough was deemed as the success criterion, the ED90 value would probably be higher.
Conclusions
Dexmedetomidine provides a gentle awakening for older patients who are susceptible to anesthetics and opioids, with an ED90 of 0.34 μg/kg/h, without causing adverse vital sign changes, respiratory depression, excessive sedation, or emergence agitation. Further research targeting a larger patient cohort is necessary to establish optimal dosing regimens for dexmedetomidine in older patients, accounting for various medical conditions, and considering factors such as sex and surgical site.
References
1. Nishino T, Tagaito Y, Isono S, Cough and other reflexes on irritation of airway mucosa in man: Pulm Pharmacol, 1996; 9(5–6); 285-92
2. Venkatesan T, Korula G, A comparative study between the effects of 4% endotracheal tube cuff lignocaine and 1.5 mg/kg intravenous lignocaine on coughing and hemodynamics during extubation in neurosurgical patients: A randomized controlled double-blind trial: J Neurosurg Anesthesiol, 2006; 18(4); 230-34
3. Leech P, Barker J, Fitch W, Proceedings: Changes in intracranial pressure and systemic arterial pressure during the termination of anaesthesia: Br J Anaesth, 1974; 46(4); 315-16
4. Norisue Y, Kataoka J, Homma Y, Increase in intra-abdominal pressure during airway suctioning-induced cough after a successful spontaneous breathing trial is associated with extubation outcome: Ann Intensive Care, 2018; 8(1); 61
5. Kim J-Y, Park IS, Kang D-H, Prediction of risk factors after spine surgery in patients aged >75 years using the modified frailty index: J Korean Neurosurg Soc, 2020; 63(6); 827-33
6. Jain A, Hassanzadeh H, Puvanesarajah V, Incidence of perioperative medical complications and mortality among elderly patients undergoing surgery for spinal deformity: Analysis of 3519 patients: J Neurosurg Spine, 2017; 27(5); 534-39
7. Janjua MS, Spurling BC, Arthur ME, Postoperative delirium: StatPearls, 2024, StatPearls Publishing Copyright© 2024, StatPearls Publishing LLC.
8. Lee SJ, Sung TY, Emergence agitation: Current knowledge and unresolved questions: Korean J Anesthesiol, 2020; 73(6); 471-85
9. McLaughlin M, Marik PE, Dexmedetomidine and delirium in the ICU: Ann Transl Med, 2016; 4(11); 224
10. Reel B, Maani CV, Dexmedetomidine: StatPearls, 2024, StatPearls Publishing Copyright© 2024, StatPearls Publishing LLC.
11. Liu X, Li Y, Kang L, Wang Q, Recent advances in the clinical value and potential of dexmedetomidine: J Inflamm Res, 2021; 14; 7507-27
12. Wang Y, Chen L, Wu BDifferent doses of dexmedetomidine for quiet extubation during anesthesia recovery in hypertensive patients: Zhonghua Yi Xue Za Zhi, 2015; 95(38); 3129-32 [in Chinese]
13. Ickeringill M, Shehabi Y, Adamson H, Ruettimann U, Dexmedetomidine infusion without loading dose in surgical patients requiring mechanical ventilation: Haemodynamic effects and efficacy: Anaesth Intensive Care, 2004; 32(6); 741-45
14. Ramsay MA, Savege TM, Simpson BR, Goodwin R, Controlled sedation with alphaxalone-alphadolone: Br Med J, 1974; 2(5920); 656-59
15. Stylianou M, Flournoy N, Dose finding using the biased coin up-and-down design and isotonic regression: Biometrics, 2002; 58(1); 171-77
16. Pace NL, Stylianou MP, Advances in and limitations of up-and-down methodology: A précis of clinical use, study design, and dose estimation in anesthesia research: Anesthesiology, 2007; 107(1); 144-52
17. Bindu B, Pasupuleti S, Gowd UP, A double blind, randomized, controlled trial to study the effect of dexmedetomidine on hemodynamic and recovery responses during tracheal extubation: J Anaesthesiol Clin Pharmacol, 2013; 29(2); 162-67
18. Turan G, Ozgultekin A, Turan C, Advantageous effects of dexmedetomidine on haemodynamic and recovery responses during extubation for intracranial surgery: Eur J Anaesthesiol, 2008; 25(10); 816-20
19. Wang W, Huo P, Wang E, Dexmedetomidine infusion for emergence coughing prevention in patients undergoing an endovascular interventional procedure: A randomized dose-finding trial: Eur J Pharm Sci, 2022; 177; 106230
20. Saidie S, Modir H, Yazdi B, The effect of dexmedetomidine on decrease of cough, hemodynamic parameters and Ramsay score versus lidocaine during general anesthesia: A randomized clinical trial: Med Gas Res, 2021; 11(1); 1-5
21. Kim J, Kim WO, Kim HB, Kil HK, Adequate sedation with single-dose dexmedetomidine in patients undergoing transurethral resection of the prostate with spinal anaesthesia: A dose-response study by age group: BMC Anesthesiol, 2015; 15; 17
22. Ko KH, Jun IJ, Lee S, Effective dose of dexmedetomidine to induce adequate sedation in elderly patients under spinal anesthesia: Korean J Anesthesiol, 2015; 68(6); 575-80
23. Weerink MAS, Struys M, Hannivoort LN, Clinical pharmacokinetics and pharmacodynamics of dexmedetomidine: Clin Pharmacokinet, 2017; 56(8); 893-913
24. Kim SH, Kim YS, Kim S, Jung KT, Dexmedetomidine decreased the post-thyroidectomy bleeding by reducing cough and emergence agitation – a randomized, double-blind, controlled study: BMC Anesthesiol, 2021; 21(1); 113
25. Kung HC, Cheng CC, Kang DH, The effects of loading dose administration rate of dexmedetomidine on sedation and dexmedetomidine requirement in elderly patients undergoing spinal anesthesia: Anesth Pain Med, 2018; 13(3); 264-70
26. Zhou D, Yang XD, Wu HY: Anesth Analg, 2023 [Online ahead of print]
27. Fan Q, Hu C, Ye M, Shen X, Dexmedetomidine for tracheal extubation in deeply anesthetized adult patients after otologic surgery: A comparison with remifentanil: BMC Anesthesiol, 2015; 15; 106
28. Kim H, Min KT, Lee JR, Comparison of dexmedetomidine and remifentanil on airway reflex and hemodynamic changes during recovery after craniotomy: Yonsei Med J, 2016; 57(4); 980-86
29. Polat R, Peker K, Baran I, Comparison between dexmedetomidine and remifentanil infusion in emergence agitation during recovery after nasal surgery: A randomized double-blind trial: Anaesthesist, 2015; 64(10); 740-46
30. Waheed A, Hameed A, Bhat S, ProSeal laryngeal mask airway and endotracheal tube in elderly hypertensive patients undergoing routine surgical procedures: A comparison of hemodynamic parameters: Journal of Clinical Gerontology and Geriatrics, 2013; 4(3); 80-83
31. Kim DJ, Kim SH, So KY, Jung KT, Effects of dexmedetomidine on smooth emergence from anaesthesia in elderly patients undergoing orthopaedic surgery: BMC Anesthesiol, 2015; 15; 139
32. Yoo JY, Kim JY, Kwak HJ, Effect-site concentration of remifentanil for preventing cough during emergence in elderly patients undergoing nasal surgery: A comparison with adult patients: Clin Interv Aging, 2016; 11; 1247-52
33. Sommer M, de Rijke JM, van Kleef M, The prevalence of postoperative pain in a sample of 1490 surgical inpatients: Eur J Anaesthesiol, 2008; 25(4); 267-74
Tables
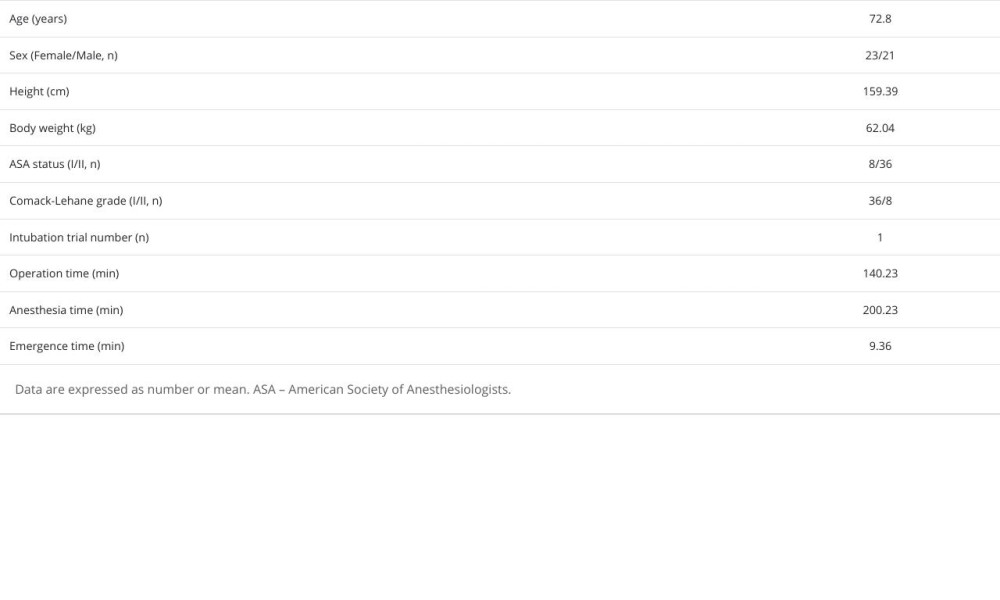 Table 1. Patient characteristics and basic operative data.
Table 1. Patient characteristics and basic operative data.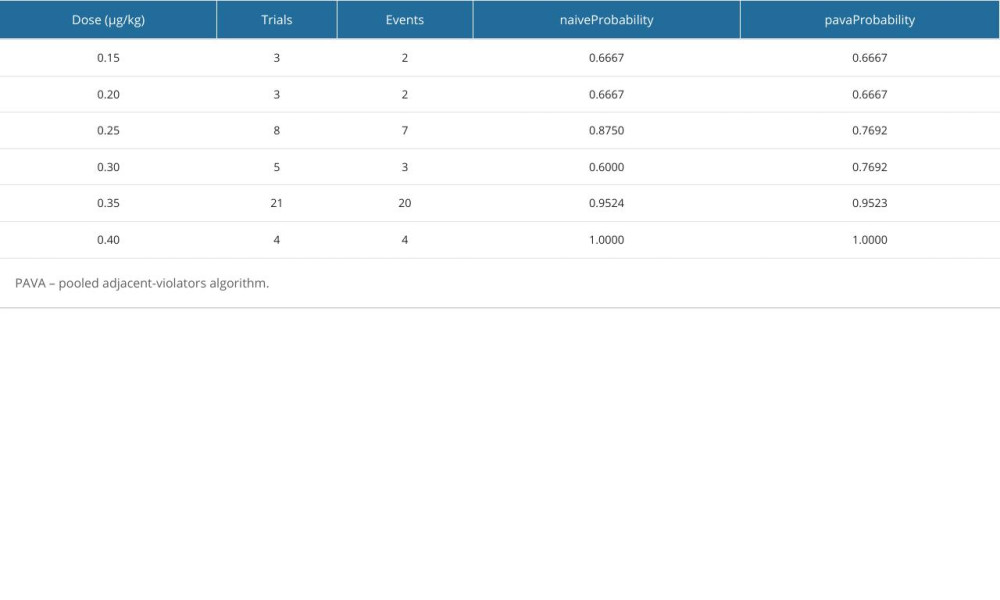 Table 2. Response rates observed and adjusted by PAVA approach.
Table 2. Response rates observed and adjusted by PAVA approach.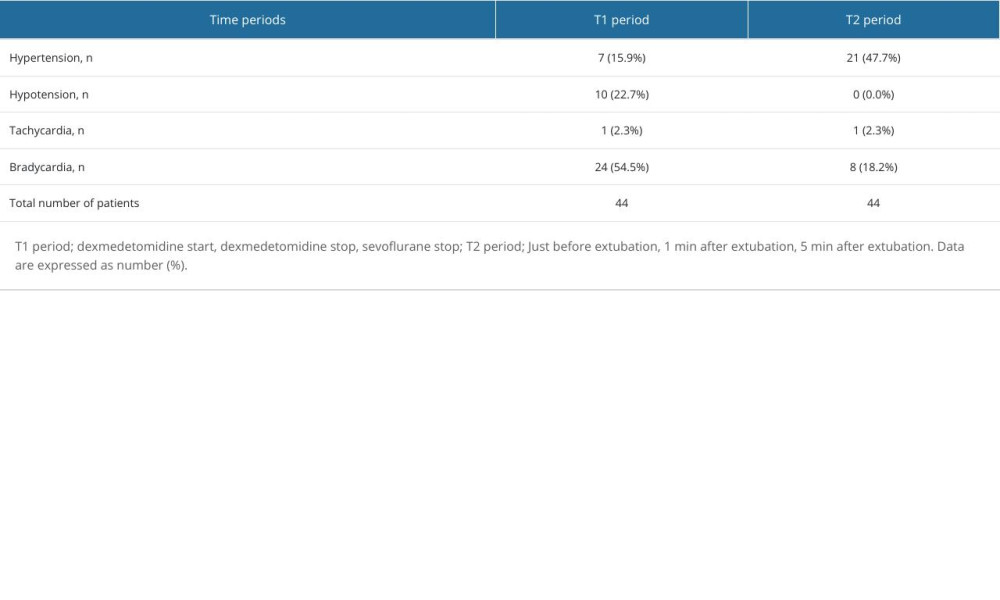 Table 3. Hemodynamic data from dexmedetomidine starting point to 5 min after extubation.
Table 3. Hemodynamic data from dexmedetomidine starting point to 5 min after extubation.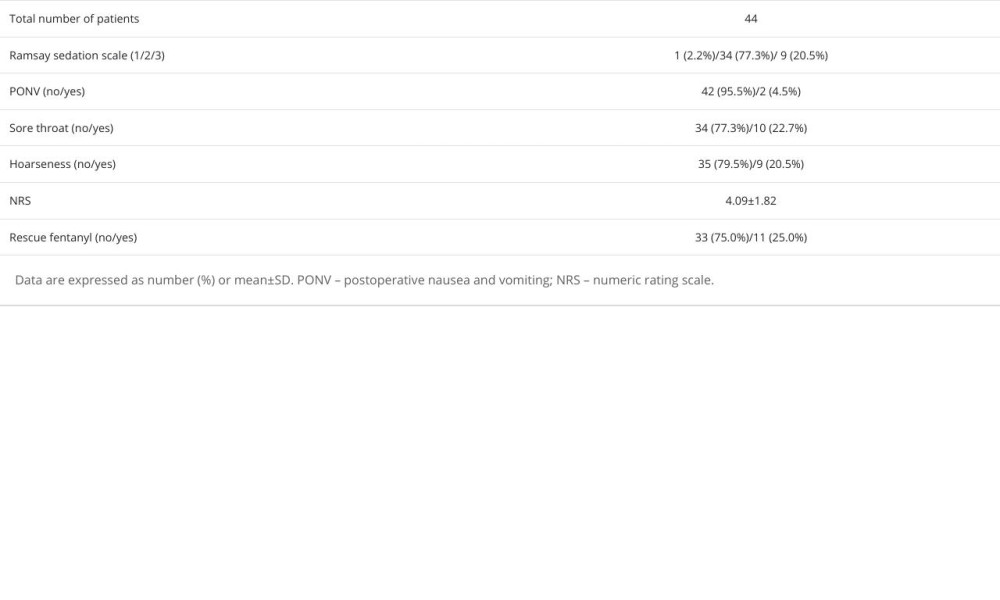 Table 4. Postoperative data in the recovery room.
Table 4. Postoperative data in the recovery room.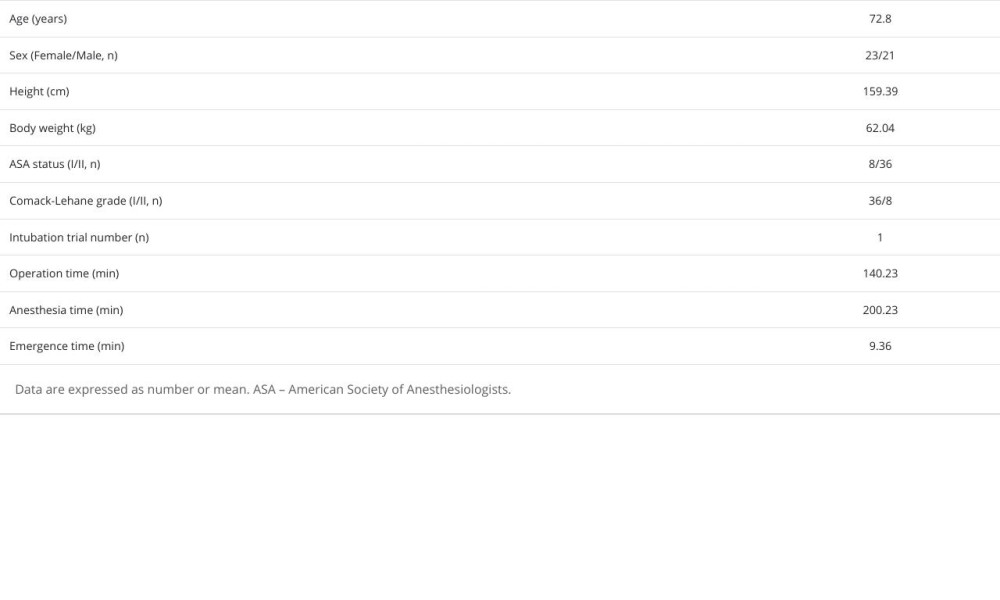 Table 1. Patient characteristics and basic operative data.
Table 1. Patient characteristics and basic operative data.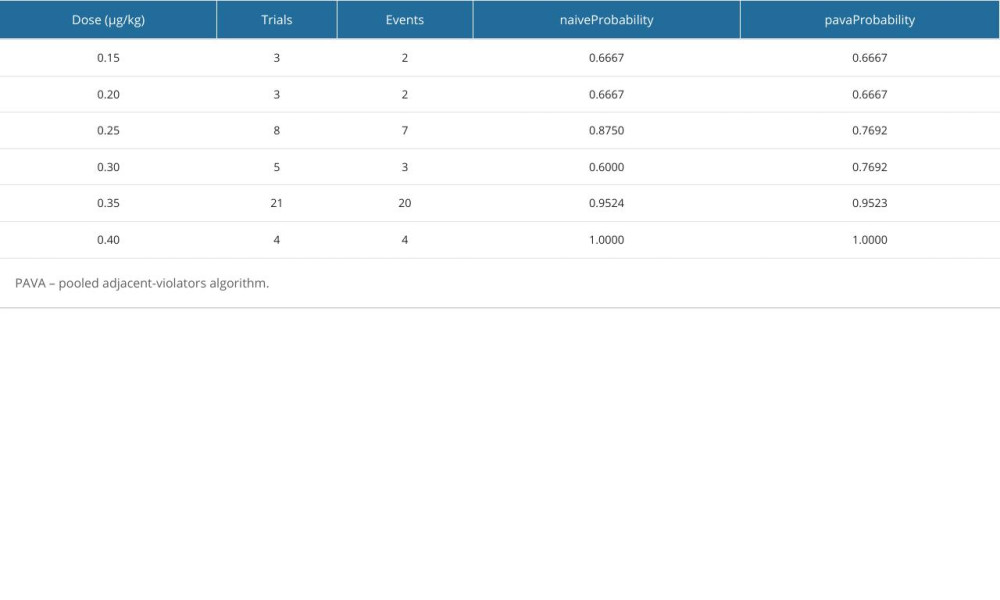 Table 2. Response rates observed and adjusted by PAVA approach.
Table 2. Response rates observed and adjusted by PAVA approach.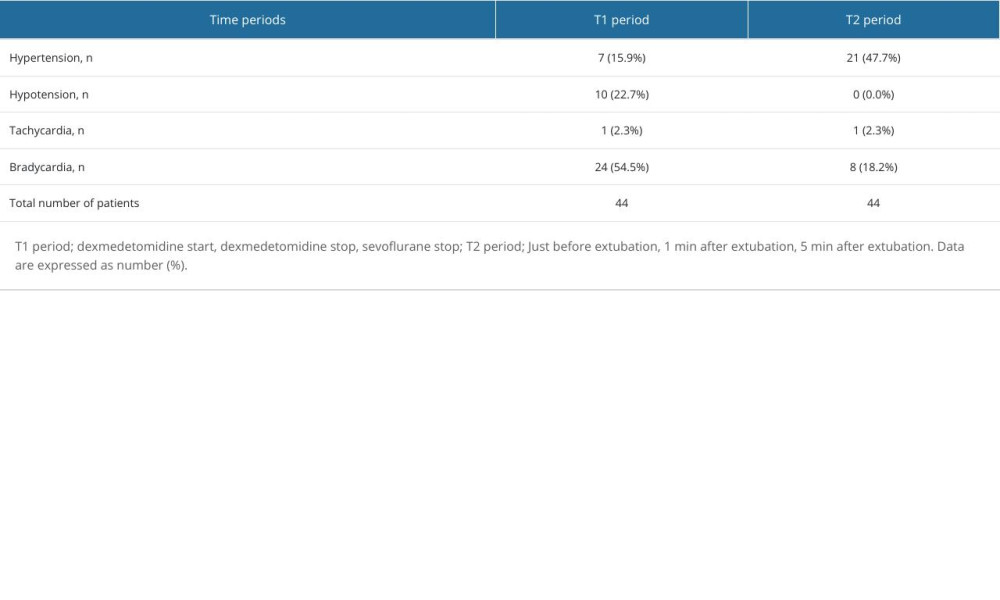 Table 3. Hemodynamic data from dexmedetomidine starting point to 5 min after extubation.
Table 3. Hemodynamic data from dexmedetomidine starting point to 5 min after extubation.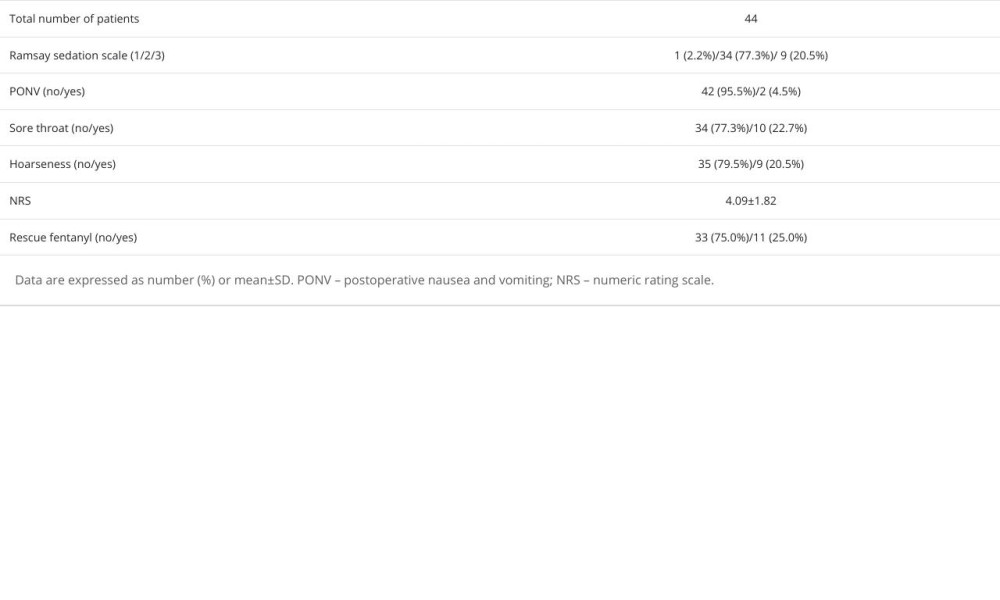 Table 4. Postoperative data in the recovery room.
Table 4. Postoperative data in the recovery room. In Press
Review article
Impact of Workplace Bullying on Nursing Care Quality: A Comprehensive ReviewMed Sci Monit In Press; DOI: 10.12659/MSM.944815
Clinical Research
Anterior Plate-Supported Cannulated Screw Surgery for Ankle Arthrodesis: Clinical and Radiologic Results in...Med Sci Monit In Press; DOI: 10.12659/MSM.944452
Clinical Research
Elevated Plasma Levels of Growth Arrest Specific 6 (Gas6) Protein in Severe Obesity: Implications for Adipo...Med Sci Monit In Press; DOI: 10.12659/MSM.944462
Database Analysis
Systemic Immune-Inflammation Index (SII) as a Predictor of Short-Term Mortality Risk in Sepsis-Associated A...Med Sci Monit In Press; DOI: 10.12659/MSM.943414
Most Viewed Current Articles
17 Jan 2024 : Review article 2,048,648
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research 1,553,068
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research 690,454
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial 50,367
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952