25 January 2024: Clinical Research
Enhanced Pain Relief and Muscle Growth in Individuals with Low Back Instability: The Impact of Blood Flow Restriction Exercise during Sit to Stand Movements
Keun-Hyo LeeDOI: 10.12659/MSM.942508
Med Sci Monit 2024; 30:e942508
Abstract
BACKGROUND: Blood flow restriction exercise (BFRE) improves muscle strength at a relatively low intensity by temporarily restricting blood flow. This study compared pain and quadriceps muscle mass (QMM) in 40 patients with lower back pain (LBP) undertaking sit-to-stand (STS) exercise with and without blood flow restriction.
MATERIAL AND METHODS: Forty adults were divided into 2 groups, and the experimental group (n=20) performed an STS exercise with BFRE, and the control group (n=20) performed an STS exercise without BFRE. Blood pressure, including systolic blood pressure (SBP) and diastolic blood pressure (DBP), was measured using a portable blood pressure monitor. Saturation of percutaneous oxygen (SpO2) was measured using oxygen saturation. Pain was measured using the visual analog scale (VAS) and the Oswestry disability index (ODI). QMM was assessed using ultrasonography.
RESULTS: Data were analyzed using paired and independent t tests. SBP (P=.000), DBP (P=.004), and SpO2 (P=.001) were significantly different in the experimental group, both before and during the intervention. The VAS scores showed a statistically significant difference in the post-test (P=.003) and rate of change (P=.009) between the groups. The ODI scores showed statistically significant differences in the post-test (P=.000) and rate of change (P=.001) comparison between the groups. The rate of change in QMM, including the rectus femoris (P=.000), vastus intermedius (P=.004), vastus medialis (P=.001), and vastus lateralis (P=.014), increased significantly in the experimental group compared to that in the control group.
CONCLUSIONS: This study demonstrates that the additive effect of BFRE on pain relief and QMM increase, thus contributing to existing knowledge about therapeutic exercise for the effective management of LBP.
Keywords: Blood Flow Restriction Therapy, Low Back Pain, Muscle Development, Quadriceps Muscle
Background
Lower back pain (LBP) is common and the leading cause of musculoskeletal disorder that frequently occurs because of muscle and ligament damage caused by excessive lower back movement and incorrect posture [1]. Back pain causes muscle weakness in the lower back, limits the range of motion of the joints [2], and leads to back instability due to asymmetrical spinal movements [3]. In LBP, the main aim of physical therapy and rehabilitation is to reduce pain and enhance motor function in the back area through various intervention methods, such as muscle strengthening, aerobic exercise, coordination exercise, corrective exercise, and trunk-centered exercise [4].
Strengthening exercises are applied in various ways according to the functional exercise ability of the individual, up to the point at which pain is bearable [5]. Several strengthening exercises have been widely used, including core stability, resistance bands, plyometric, and pilates [6]. Blood flow restriction exercise (BFRE) is a rehabilitation method that uses a compression cuff to block arterial inflow and delay venous outflow during exercise such as resistance training [7]. Recently, BFRE, which involves temporary restriction of blood flow in patients with LBP, has been used to control pain, motor function, and prevent the recurrence of musculoskeletal injuries [8].
Specifically, BFRE is a method of performing low-intensity strength training by partially restricting arterial and venous blood flow through compression using a tool such as a cuff to an arm or leg [9]. Tanimoto et al [10] reported that BFRE temporarily blocks muscle oxygen supply, thereby activating growth hormone through a local hypoxic state and helping improve muscle strength. Karabulut et al [11] suggested that low-intensity exercise through BFRE can elicit increased muscle strength, similar to that of resistance exercise. Thus, it may be effectively used in women, and in elderly individuals with muscle weakness. Park et al [12] reported that lumbar stabilization exercises with blood flow restriction on the lower extremities improved gait, trunk flexion strength, and muscular endurance in patients with LBP.
The sit-to-stand (STS) motion equally develops the lower body of patients with LBP [13]. STS can be used to enhance functional weight-bearing capacity [14]. Shum et al [15] reported that back pain can be controlled by changing the movement of the hip joint and lower back using the STS motion. McGregor and Hukins [16] reported that patients with back instability are characterized by lower-extremity muscle weakness and limited hip joint movement. Mayer et al [17] reported that strengthening exercises for the extensor muscles of the lower limbs reduced pain and improved gait in patients with back instability.
To quantitatively investigate the effect of BFRE on pain and associated quadriceps muscle mass (QMM) of the lower extremities, we studied patients with LBP using the real-time US imaging technique. Our basic premise was that our BFRE would significantly reduce the pain and increase muscle mass of the patients with LBP, thereby improving blood flow and saturation of percutaneous oxygen (SpO2).
Material and Methods
ETHICS:
All participants fully understood the purpose and methods of the study and provided informed consent. This study was approved by the university’s ethics and institutional review boards (IRB approval no. KYU 2022-03-010-002).
PARTICIPANTS:
All participants were recruited from the Konyang Medical University community in Dae-jeon Metropolitan City. Participants were adults who had experienced an episode of LBP. Their ages ranged from 20 to 27 years, with an average of 23.6 years (Table 1). An orthopedist diagnosed LBP according to clinical assessment criteria [18]. The clinical assessment criteria employed consisted of a passive lumbar extension test, and if severe pain in the lumbar region occurred during the process of lifting both legs, it was judged to be a lumbar region instability.
The inclusion criteria were: (1) visual analog scale pain intensity ≥4, (2) no pain control drug use, and (3) the ability to walk independently and perform daily activities without assistive devices. The exclusion criteria were: (1) a history of recent illness, (2) thrombophlebitis or familial thrombosis disease, (3) hypertension, (4) cardiac failure, (5) arrhythmia, (6) surgical history of the lumbar region, and (7) inflammatory spine disease.
Randomization was performed using sealed envelopes. Sealed letters for the experimental (BFRE with STS) and control groups (STS) were arranged by the investigator. The investigator prepared the group allocation on a sheet of paper and provided it to participants in a blinded manner. The participants were allocated before the initial assessment and all of them participated in the measurements. The physiotherapist who performed the assessment was also blinded to the group allocation (Table 2).
To ensure the validity and appropriate interpretation of the study, the overall bias of the research method was assessed using 10 items. If the answer was ‘yes,’ 1 point was awarded; if the answer was ‘no’, zero points were awarded. A total score of 6 or less indicated low quality, 7 points indicated medium quality, and 8 points or more indicated high quality [19].
INTERVENTION:
A blood flow restriction device (Kaatsu Nano, Kaatsu Global, Huntington, USA) was used as the intervention tool. For the BFRE, elastic cuffs with a width of 50 mm were worn 25 cm above the center of the patella in both lower extremities. During both exercise and rest, the pressure was set to 40 mmHg so that the cuff would not slip down the leg, and the veins on the skin surface were compressed. During BFRE, the cuff pressure was set to the premeasured systolic blood pressure (SBP) level for low intensity. If the patient had pain due to increased cuff pressure, the pressure was reduced. In addition, when the intervention was applied, it was set so that the skin color would not change for more than 3 s.
For the application of low-intensity BFRE, an exercise intensity of 20–30% of 1 repetition maximum (1RM) was applied. The participants were asked to perform STS while sitting on a chair without armrests and without moving their feet [20]. Audiovisual feedback was provided using a mirror to ensure correct posture during STS, and the flexion angle of the knee joint was lowered from 45° to 70°, depending on the participant’s condition. STS was performed 20 times in the first set and 10 times in the second to fourth sets, with a 30-s break between sets, and applied for a total of 10 min [21]. A metronome was provided to ensure the correct rhythm of the STS, at a rate of 1 s down and 1 s up using the metronome [22]. The cuff was removed immediately at the end of the exercise [23].
BODY COMPOSITION: Body composition was assessed using a bioelectrical impedance analysis system (In Body 4; Biospace, Seoul, Korea). The body mass index test-retest reliability of the measurement tool was r=.851 [24]. The participants entered their data into the device, including sex, age, height, and weight. Metal materials such as necklaces, earrings, and watches were removed. After wiping the participants’ palms and soles with an electrolyte tissue, they stood with the soles of their feet against the electrode and held the hand electrode. This was measured in a static, standing anatomical position.
BLOOD PRESSURE: Blood pressure was measured using the Omron HBP-1300 professional portable blood pressure monitor (HBP-1300, Omron Corp, Kyoto, Japan). The reliability of the measurement tool was ICC=.94 in SBP and ICC=.92 in diastolic blood pressure (DBP) [25]. Measurements were taken after the participants arrived at the laboratory, sat, and rested for at least 5 min. The cuff was leveled with the heart, then tightly wrapped around the upper arm 2 cm above the elbow, and placed over the brachial artery.
SATURATION OF PERCUTANEOUS OXYGEN: A portable pulse oximeter (Model CMS-50E, Contec Corp, Qinhuangdao, China) was used to analyze SpO2. The pulse oximeter used in this study measures the amount of oxygen in the blood noninvasively without blood sampling. The clip tube worn on the finger has an infrared receiver; therefore, the pulse oximeter is automatically measured when the finger is inserted. Oxygen levels in people with healthy lungs show ranges between 95% and 100%. The reliability of the measurement tool was ICC=.97 [26]. Before the measurement, the participant’s fingernail was washed with an alcohol swab to remove any foreign substances, and the measurement was performed with the right index finger.
VISUAL ANALOG SCALE: The pain was evaluated using the visual analog scale (VAS). The measurement tool has a test-retest reliability and inter-rater reliability of r=1.00 and r=.99, respectively [27]. The participants were instructed to assume ‘0 cm’ as no pain experienced, whereas 10 cm represented the most pain experienced. The participants were then instructed to visually indicate the degree of pain they experienced on the VAS, with a perpendicular line representing their pain scores [28].
OSWESTRY DISABILITY INDEX: The Oswestry disability index (ODI) questionnaire was used to identify functional disabilities caused by back pain in the study participants. According to Mousavi et al [29], the ODI has excellent test-retest reliability (ICC=.91). The ODI is used to measure LBP related functional impairment and consists of 10 inquiries; each item is worth 5 points, with the total score expressed as a percentage [30]. The higher the score, the more severe the limitation in functional performance due to back pain.
ULTRASOUND IMAGING: QMM was measured using an ultrasonographic imaging device (My-sono U6; Medison, Seoul, Korea). The ultrasonic transducers used for ultrasonic imaging measurement were 7.5 MHz linear transducers, and the frequency modulation range was set to 6~8.5 MHz. According to Menon et al [31], the intra-rater reliability of ultrasound measurements of the QMM is.98 in ICC. Additionally, the inter-rater reliability of the QMM is.95 in the ICC.
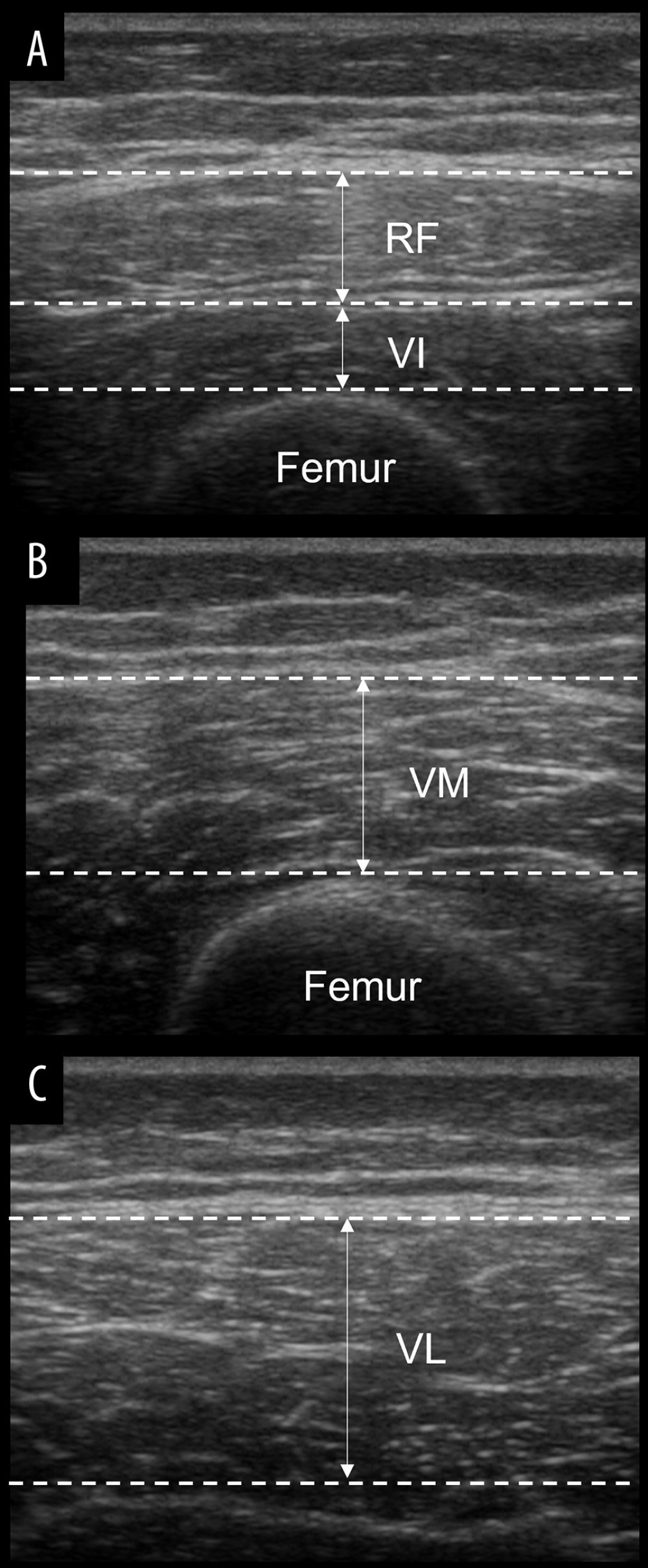
Measurements were taken with the patient in the supine position with their knees completely extended. Ultrasound gel was applied to minimize the distortion generated by the underlying tissues. Shaving was not needed. The location of the rectus femoris (RF) and vastus intermedius (VI) was measured by marking the midpoint of an imaginary line connecting the base of the patella run to the anterior superior iliac spine (ASIS). The vastus medialis (VM) was measured at 12.5% of the medial part of the muscle circumference after finding a 20% point between the patella and the ASIS. The vastus lateralis (VL) was measured as 10% of the lateral part of the muscle circumference from the RF and VI locations.
Specifically, the mass of the RF muscle was determined by measuring the distance between the interface of the superficial adipose and deep muscle layers (Figure 1A). The mass of the VI muscle was determined by measuring the distance between the interface of the superficial muscle and the femur [32] (Figure 1A). The mass of the VM muscle was determined by measuring the distance between the interface of the superficial adipose tissue and muscle, as well as the interface of the muscle and bone (Figure 1B). The mass of the VL muscle was measured by assessing the distance between the deep edge of the superficial aponeurosis and the superficial edge of the deep aponeurosis (Figure 1C). The change rate of the muscle mass (%) was calculated using the formula = ((post-test – pre-test) / pre-test) ×100.
STATISTICAL ANALYSIS:
G-Power 3.1.9.4 software (University of Dusseldorf, Dusseldorf, Germany) was used to perform the sample size calculation. The power (1-β) and alpha levels (α) were set to.80 (80%) and.05, respectively. Additionally, the effect size was set to.95. According to a preliminary analysis, a sample size of 21 participants was required for each group, so 42 participants were selected in this study, although there were 2 dropouts. The Kolmogorov-Smirnov test was performed as a normality test for all measured variables.
The general characteristics of the participants are expressed as means and standard deviations using descriptive statistics to compare the groups. Independent
Results
GENERAL CHARACTERISTICS OF PARTICIPANTS:
The general characteristics of the participants are summarized in Table 1. The experimental and control groups were comparable with respect to sex, age, height, weight, and body mass index.
BLOOD PRESSURE AND SATURATION OF PERCUTANEOUS OXYGEN:
A result of the pre and during the intervention showed significant differences in SBP (P=.000), DBP (P=.004), and SpO2 (P=.001) in the experimental group, suggesting stronger BFRE during the intervention state (latter) than during the pre-intervention state (former) (Table 3).
PAIN:
The experimental (P=.000) and control groups (P=.000) showed statistically significant differences in the pre- and post-VAS scores, respectively. There was a statistically significant difference in the post-test comparison between the groups (P=.003). A statistically significant difference was noted in the rate of change between the groups (P=.009) (Table 4).
The experimental (P=.000) and control groups (P=.000) showed statistically significant differences in pre- and post-ODI scores, respectively. There was a statistically significant difference in the post-test comparison between the groups (P=.000). There was a statistically significant difference in the rate of change between the groups (P=.001) (Table 4).
QUADRICEPS MUSCLE MASS:
In the experimental group, all muscles, including the RF (P=.000), VI (P=.000), VM (P=.000), and VL (P=.000), showed statistically significant differences in the pre and post comparisons. In the control group, all muscles, including the RF (P=.000), VI (P=.001), VM (P=.002), and VL (P=.030) showed statistically significant differences in pre and post comparisons. Comparisons between groups showed statistically significant differences in the rate of change of all muscles, including the RF (P=.000), VI (P=.004), VM (P=.001), and VL (P=.014) (Table 5).
Discussion
This study showed immediate effects of the BFRE on pain relief and reduction of the altered muscle mass of the quadriceps muscle in patients with LBP. As anticipated, muscle mass (or muscle thickness) was significantly increased as a function of the intervention. Intervention-related changes in altered muscle mass were successfully quantified by ultrasound imaging. This morphological improvement in muscle mass was paralleled with increased blood flow and decreased SpO2 during the BFRE, showing that our BFRE intervention may be more helpful than the other strengthening interventions administered reported elsewhere. Methodologically, significant differences were observed in SBP and DBP measured before and during the experiment, confirming the validity of the BFRE.
Moderate- and high-intensity exercises between 60% and 80% of 1RM are recommended to improve muscle strength, although BFRE involves low-intensity loads of 20–30% of 1RM [33]. Ladlow et al [34] reported that BFRE exercise at approximately 30% of 1RM significantly improved muscle strength and motor function during rehabilitation after lower-extremity musculoskeletal injury. Therefore, in this study, BFRE was performed at a low intensity (30%). Thus, BFRE offers an advantage for children, the elderly, and individuals with weak bodies, who can expect to experience muscle strength improvements with low-intensity loads. In addition, STS is a great way to strengthen your lower back and stabilizer muscles [12], hence its selection as the intervention exercise for this study.
If cuff pressure is excessive, BFRE can cause discomfort and even muscle damage. According to Aniceto and da Silva [35], higher SBP has been reported when using narrower cuffs in comparison with wider cuff. Therefore, the cuff pressure used in this study was the previously measured SBP [36]. The direct 1RM method carries a risk of injury. Therefore, in this study, 1RM was calculated using the indirect measurement proposed by Baechle et al [37], considering the safety of patients with LBP. In other words, indirect 1RM manual can be used safely in a potentially at-risk population.
Neurophysiologically, BFRE increases muscle protein synthesis due to muscle hypoxia and the accumulation of anerobic metabolites, and increased muscle fiber recruitment, ultimately resulting in improved strength [38,39]. It has also been reported that endocrine system function is improved through neuromuscular activity [40]. Low-intensity (20–30% of 1RM or less than 150 mmHg) BFRE was found to be more efficient for intramuscular metabolite accumulation than high-intensity blood flow compression (80% of 1RM or more than 200 mmHg), and that excessive compression causes blood vessel damage [36].
To confirm the accurate application of BFRE, blood pressure and saturation of percutaneous oxygen were compared before and during the intervention, respectively. Consequently, the SBP was 116 mmHg in the pre-intervention state and 125 mmHg in during the intervention state, and the DBP was 75 mmHg pre-intervention and 79 mmHg during the intervention increased by approximately 8% and 5%, respectively. In addition, the SpO2 decreased by 2% from pre-intervention (96%) to during the intervention (94%). These scores indicate the validity of the low-intensity BFRE related to this study. Especially, this study shows that BFRE increases blood pressure [41] and decreases oxygen saturation [42] in the experimental intervention.
Substantially, pain relief was observed to a greater extent in the experimental group after STS with BFRE. The pain findings show that VAS score (3.5→1.4 point) and ODI score (28.3→13.1 point) decreased by approximately 58% and 53%, respectively, after intervention. In addition, the rate of change in pain scale findings show that VAS score and ODI score during the STS with BFRE decreased by approximately 26% and 22%, respectively, compared with that of the STS alone. Importantly, BFRE was effective in reducing pain in patients with knee injury [43]. In 48 patients with knee arthritis, BFRE was applied as a low-intensity resistance exercise for 12 weeks, and the pain was reduced by approximately 50% [44]. It has been reported that low-intensity BFRE is an effective method for pain management [45]. These previous studies showed that BFRE was effective in controlling pain in patients with various musculoskeletal disorders, including LBP.
The rates of change in QMM were as follows: RF (experimental group, 10%; control group, 5%), VI (experimental group, 6%; control group, 2%), VM (experimental group, 6%; control group, 2%), and VL (experimental group, 6%; control group, 2%); and all were significantly increased. Yasuda et al [46] reported that the cross-sectional area of the quadriceps muscles was increased by 8% by applying BFRE for 12 weeks in 21 elderly people, and Hughes et al [33] and Li et al [43] reported that BFRE is effective in improving muscle strength in patients with various musculoskeletal symptoms. Young et al [47] reported an increase in muscle mass and hypertrophy within 3 h after BFRE application. Consequently, BFRE is thought to result in muscle morphological changes through the rapid recruitment of muscle fibers.
There are some limitations to this study. First, it is difficult to generalize the study results because the number of participants was small. Second, because the participants were relatively young, it is difficult to generalize our findings to people of various ages. Third, assessment was performed after application of a short-term intervention with insufficient intervention time. Fourth, description of the STS exercise was somewhat lacking in the Methods section because we were conducting practical research within a clinic environment. Therefore, to address these limitations, it is necessary to conduct research on long-term application of BFRE in a larger group of LBP patients.
Conclusions
This study provides empirical evidence to show that the BFRE combined with STS is useful in enhancing QMM and associated pain relief in patients with LBP. Our results offer clinical insights into the additive effect of BFRE in selectively stimulating the quadriceps muscle, and suggests that it may be used as an alternative strengthening technique for the management of patients with LBP.
References
1. Nadler SF, Malanga GA, Bartoli LA, Hip muscle imbalance and low back pain in athletes: influence of core strengthening: Med Sci Sports Exerc, 2002; 34(1); 9-16
2. Kim WD, Shin D, Effects of pelvic-tilt imbalance on disability, muscle performance, and range of motion in office workers with non-specific low-back pain: Healthcare (Basel), 2023; 11(6); 893
3. Kim WD, Shin D, Correlations between hip extension range of motion, hip extension asymmetry, and compensatory lumbar movement in patients with nonspecific chronic low back pain: Med Sci Monit, 2020; 26; e925080
4. Hayden JA, Ellis J, Ogilvie R, Exercise therapy for chronic low back pain: Cochrane Database Syst Rev, 2021; 9(9); CD009790
5. Dejonghe LAL, Rudolf K, Becker J, Health coaching for promoting physical activity in low back pain patients: A secondary analysis on the usage and acceptance: BMC Sports Sci Med Rehabil, 2020; 12; 2
6. Martuscello JM, Nuzzo JL, Ashley CD, Systematic review of core muscle activity during physical fitness exercises: J Strength Cond Res, 2013; 27(6); 1684-98
7. Cognetti DJ, Sheean AJ, Owens JG, Blood flow restriction therapy and its use for rehabilitation and return to sport: Physiology, application, and guidelines for implementation: Arthrosc Sports Med Rehabil, 2022; 4(1); e71-e76
8. Amano S, Ludin AF, Clift R, Effectiveness of blood flow restricted exercise compared with standard exercise in patients with recurrent low back pain: Study protocol for a randomized controlled trial: Trials, 2016; 17; 81
9. Kumagai K, Kurobe K, Zhong H, Cardiovascular drift during low intensity exercise with leg blood flow restriction: Acta Physiol Hung, 2012; 99(4); 392-99
10. Tanimoto M, Madarame H, Ishii N, Muscle oxygenation and plasma growth hormone concentration during and after resistance exercise: Comparison between “KAATSU” and other types of regimen: Int J Kaatsu Train Res, 2005; 1(2); 51-56
11. Karabulut M, Abe T, Sato Y, Bemben MG, The effects of low-intensity resistance training with vascular restriction on leg muscle strength in older men: Eur J Appl Physiol, 2010; 108(1); 147-55
12. Park JC, Mun DJ, Lee SH, Effect of lumbar stabilization exercise using blood flow restriction on muscle strength, muscular endurance, and gait in patients with chronic back pain: J Korean Soc Neur Ther, 2021; 25(3); 71-76
13. Cho M, The effects of modified wall squat exercises on average adults’ deep abdominal muscle thickness and lumbar stability: J Phys Ther Sci, 2013; 25(6); 689-92
14. Zawadka M, Smołka J, Skublewska-Paszkowska M, Altered squat movement pattern in patients with chronic low back pain: Ann Agric Environ Med, 2021; 28(1); 158-62
15. Shum GL, Crosbie J, Lee RY, Effect of low back pain on the kinematics and joint coordination of the lumbar spine and hip during sit-to-stand and stand-to-sit: Spine (Phila Pa 1976), 2005; 30(17); 1998-2004
16. McGregor AH, Hukins DW, Lower limb involvement in spinal function and low back pain: J Back Musculoskelet Rehabil, 2009; 22(4); 219-22
17. Mayer J, Mooney V, Dagenais S, Evidence-informed management of chronic low back pain with lumbar extensor strengthening exercises: Spine J, 2008; 8(1); 96-113
18. Kasai Y, Morishita K, Kawakita E, A new evaluation method for lumbar spinal instability: Passive lumbar extension test: Phys Ther, 2006; 86(12); 1661-67
19. Gelaw AY, Janakiraman B, Teshome A, Ravichandran H, Effectiveness of treadmill assisted gait training in stroke survivors: A systematic review and meta-analysis: Glob Epidemiol, 2019; 1; 100012
20. Sedrez JA, Mesquita PV, Gelain GM, Candotti CT, Kinematic characteristics of sit-to-Stand movements in patients with low back pain: A systematic review: J Manipulative Physiol Ther, 2019; 42(7); 532-40
21. Loenneke JP, Wilson JM, Marín PJ, Low intensity blood flow restriction training: A meta-analysis: Eur J Appl Physiol, 2012; 112(5); 1849-59
22. Hazell TJ, Kenno KA, Jakobi JM, Evaluation of muscle activity for loaded and unloaded dynamic squats during vertical whole-body vibration: J Strength Cond Res, 2010; 24(7); 1860-65
23. Karabulut M, Bemben DA, Sherk VD, Effects of high-intensity resistance training and low-intensity resistance training with vascular restriction on bone markers in older men: Eur J Appl Physiol, 2011; 111(8); 1659-67
24. Kim HC, Park KJ, Analysis of body composition according to short distance and middle & long distance of youth national athletic athletes: J Korean Soc Phys Med, 2021; 16(1); 33-39
25. Cao X, Song C, Guo L, Quality control and validation of oscillometric blood pressure measurements taken during an epidemiological investigation: Medicine (Baltimore), 2015; 94(37); e1475
26. Cheatham SW, Kolber MJ, Ernst MP, Concurrent validity of resting pulse-rate measurements: A comparison of 2 smartphone applications, the polar H7 belt monitor, and a pulse oximeter with bluetooth: J Sport Rehabil, 2015; 24(2); 171-78
27. Wagner DR, Tatsugawa K, Parker D, Young TA, Reliability and utility of a visual analog scale for the assessment of acute mountain sickness: High Alt Med Biol, 2007; 8(1); 27-31
28. Lutfi M, Dalleck LC, Drummond C, A single session of a digital health tool-delivered exercise intervention may provide immediate relief from pelvic pain in women with endometriosis: A pilot randomized controlled study: Int J Environ Res Public Health, 2023; 20(3); 1665
29. Mousavi SJ, Parnianpour M, Mehdian H, The Oswestry disability index, the Roland-Morris disability questionnaire, and the Quebec back pain disability scale: Translation and validation studies of the Iranian versions: Spine (Phila Pa 1976), 2006; 31(14); E454-59
30. Kim TH, Park SK, Cho IY, Substantiating the therapeutic effects of simultaneous heat massage combined with conventional physical therapy for treatment of lower back pain: A randomized controlled feasibility trial: Healthcare (Basel), 2023; 11(7); 991
31. Menon MK, Houchen L, Harrison S, Ultrasound assessment of lower limb muscle mass in response to resistance training in COPD: Respir Res, 2012; 13(1); 119
32. Akazawa N, Harada K, Okawa N, Relationships between muscle mass, intramuscular adipose and fibrous tissues of the quadriceps, and gait independence in chronic stroke survivors: A cross-sectional study: Physiotherapy, 2018; 104(4); 438-45
33. Hughes L, Paton B, Rosenblatt B, Blood flow restriction training in clinical musculoskeletal rehabilitation: A systematic review and meta-analysis: Br J Sports Med, 2017; 51(13); 1003-11
34. Ladlow P, Coppack RJ, Dharm-Datta S, Low-load resistance training with blood flow restriction improves clinical outcomes in musculoskeletal rehabilitation: A single-blind randomized controlled trial: Front Physiol, 2018; 9; 1269
35. Aniceto RR, da Silva Leandro L, Practical blood flow restriction training: New methodological directions for practice and research: Sports Med Open, 2022; 8(1); 87
36. Karabulut M, Abe T, Sato Y, Bemben M, Overview of neuromuscular adaptations of skeletal muscle to KAATSU Training: Int J Kaatsu Train Res, 2007; 3(1); 1-9
37. Baechle TR, Earle RW, Wathen D: Resistance training Essentials of strength training and conditioning, 2000, Champaign (IL), Human Kinetics
38. Fujita S, Abe T, Drummond MJ, Blood flow restriction during low-intensity resistance exercise increases S6K1 phosphorylation and muscle protein synthesis: J Appl Physiol (1985), 2007; 103(3); 903-10
39. Rossi FE, de Freitas MC, Zanchi NE, The role of inflammation and immune cells in blood flow restriction training adaptation: A review: Front Physiol, 2018; 9; 1376
40. Abe T, Kearns CF, Sato Y, Muscle size and strength are increased following walk training with restricted venous blood flow from the leg muscle, Kaatsu-walk training: J Appl Physiol (1985), 2006; 100(5); 1460-66
41. Iida H, Kurano M, Takano H, Hemodynamic and neurohumoral responses to the restriction of femoral blood flow by KAATSU in healthy subjects: Eur J Appl Physiol, 2007; 100(3); 275-85
42. Neto GR, Sousa MS, Costa e Silva GV, Acute resistance exercise with blood flow restriction effects on heart rate, double product, oxygen saturation and perceived exertion: Clin Physiol Funct Imaging, 2016; 36(1); 53-59
43. Li S, Shaharudin S, Abdul Kadir MR, Effects of blood flow restriction training on muscle strength and pain in patients with knee injuries: A meta-analysis: Am J Phys Med Rehabil, 2021; 100(4); 337-44
44. Rodrigues R, Ferraz RB, Kurimori CO, Low-load resistance training with blood-flow restriction in relation to muscle function, mass, and functionality in women with rheumatoid arthritis: Arthritis Care Res (Hoboken), 2020; 72(6); 787-97
45. Song JS, Spitz RW, Yamada Y, Exercise-induced hypoalgesia and pain reduction following blood flow restriction: A brief review: Phys Ther Sport, 2021; 50; 89-96
46. Yasuda T, Fukumura K, Fukuda T, Muscle size and arterial stiffness after blood flow-restricted low-intensity resistance training in older adults: Scand J Med Sci Sports, 2014; 24(5); 799-806
47. Young TR, Duncan BT, Cook SB, Evaluation of muscle thickness of the vastus lateralis by ultrasound imaging following blood flow restricted resistance exercise: Clin Physiol Funct Imaging, 2021; 41(4); 376-84
Tables
 Table 1. General characteristics of participants.
Table 1. General characteristics of participants.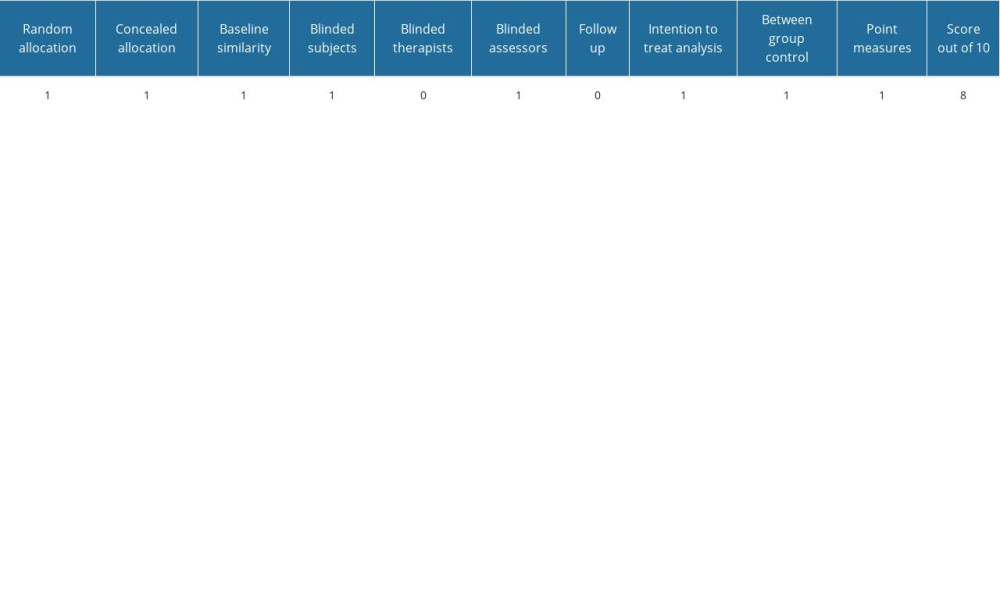 Table 2. Risk of bias.
Table 2. Risk of bias.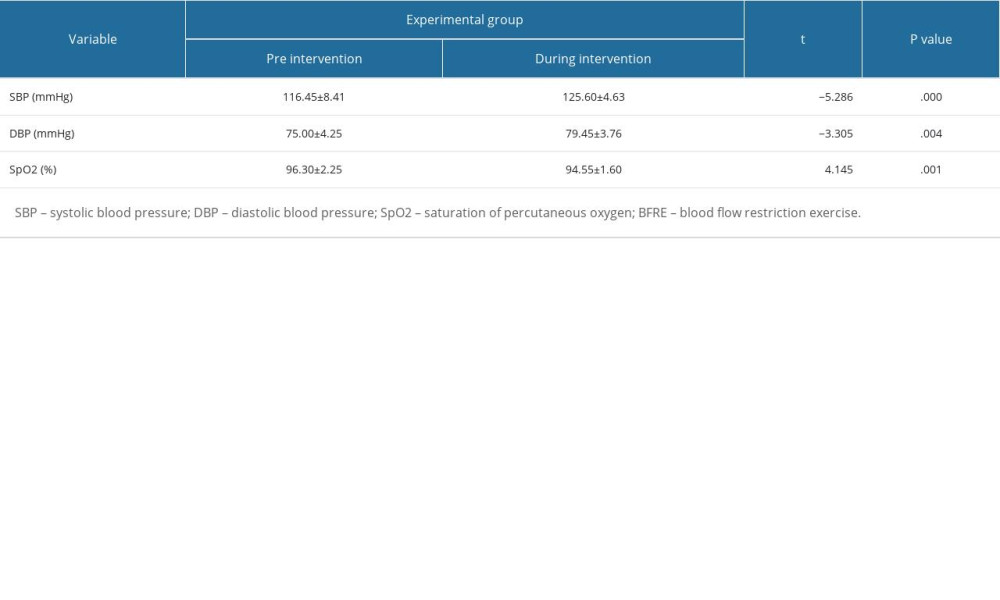 Table 3. Changes in SBP, DBP, and SpO2 according to BFRE in the experimental group.
Table 3. Changes in SBP, DBP, and SpO2 according to BFRE in the experimental group.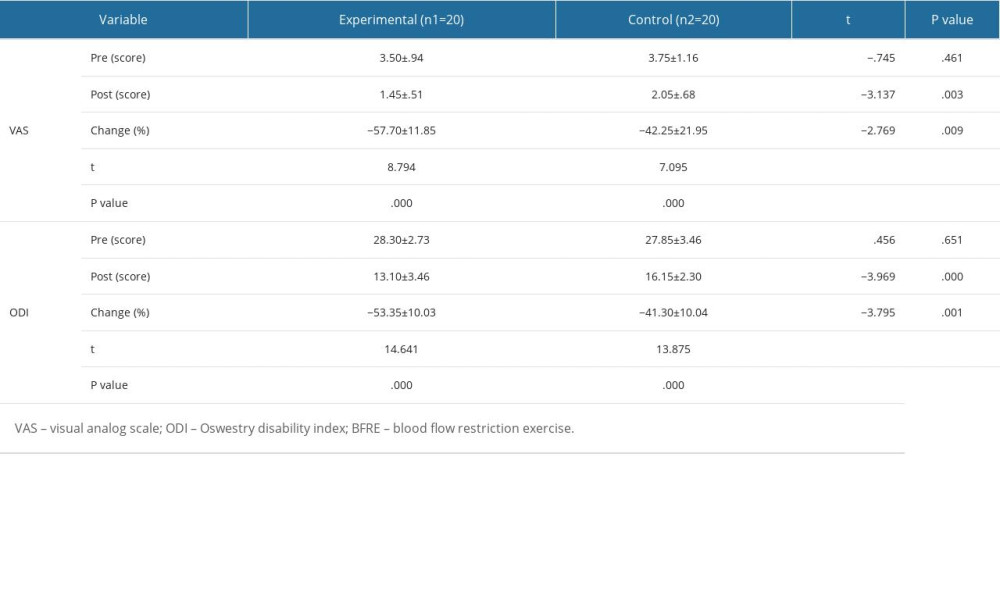 Table 4. Changes in VAS and ODI according to the BFRE.
Table 4. Changes in VAS and ODI according to the BFRE.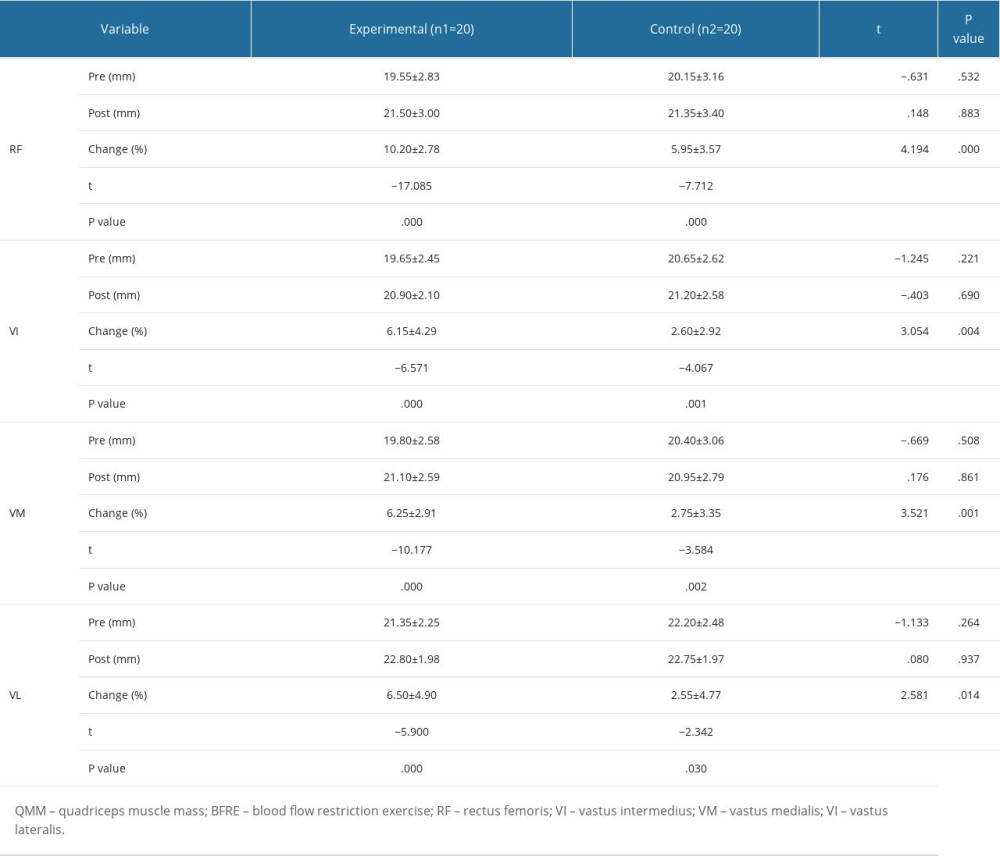 Table 5. Changes of QMM according to the BFRE.
Table 5. Changes of QMM according to the BFRE. Table 1. General characteristics of participants.
Table 1. General characteristics of participants.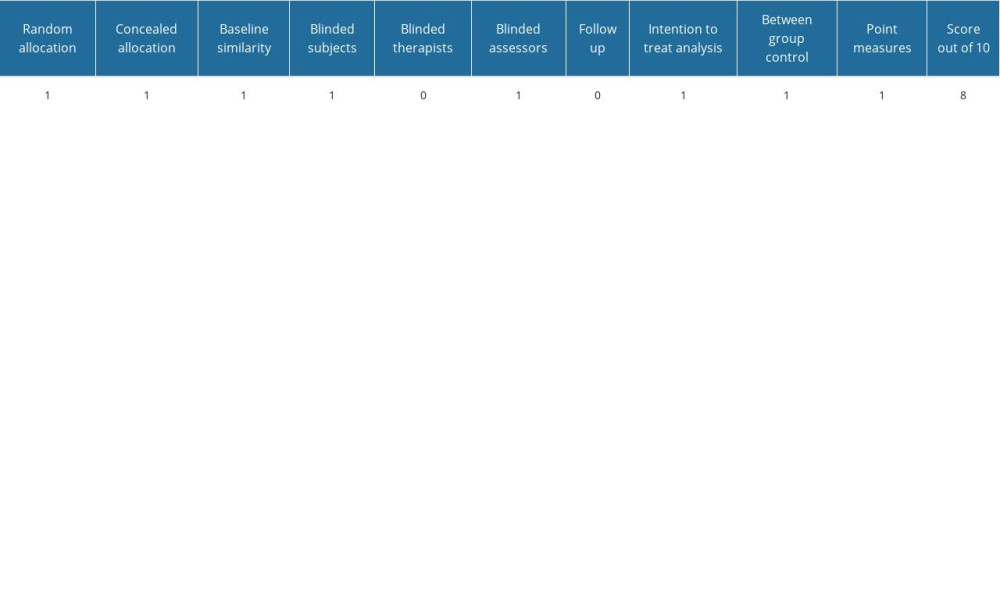 Table 2. Risk of bias.
Table 2. Risk of bias.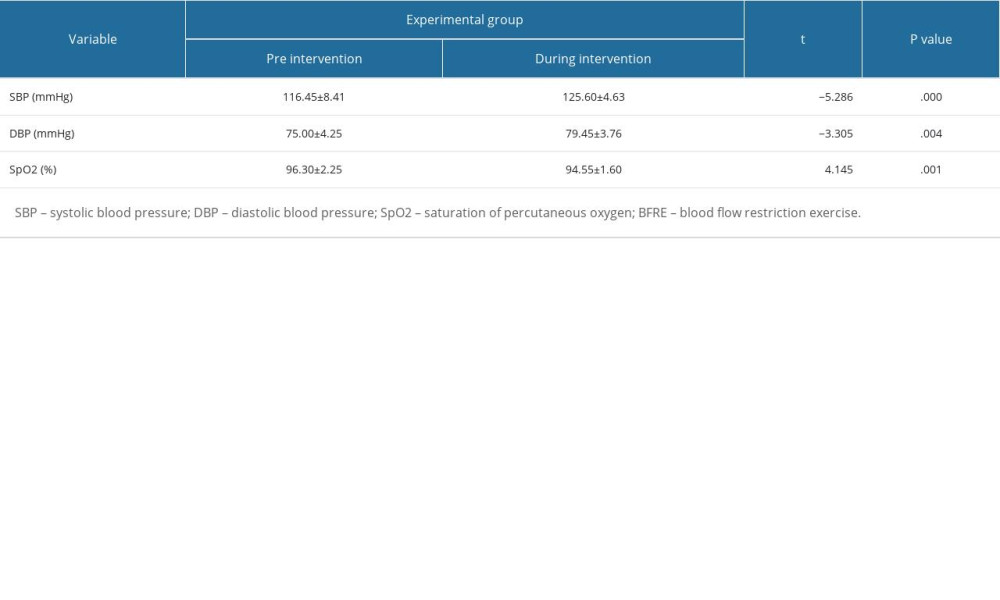 Table 3. Changes in SBP, DBP, and SpO2 according to BFRE in the experimental group.
Table 3. Changes in SBP, DBP, and SpO2 according to BFRE in the experimental group.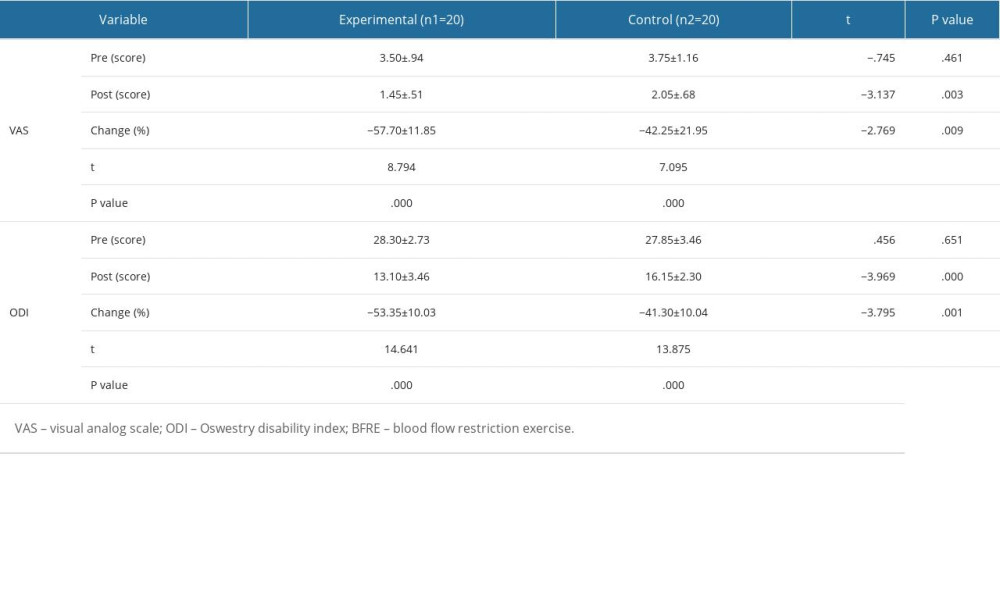 Table 4. Changes in VAS and ODI according to the BFRE.
Table 4. Changes in VAS and ODI according to the BFRE.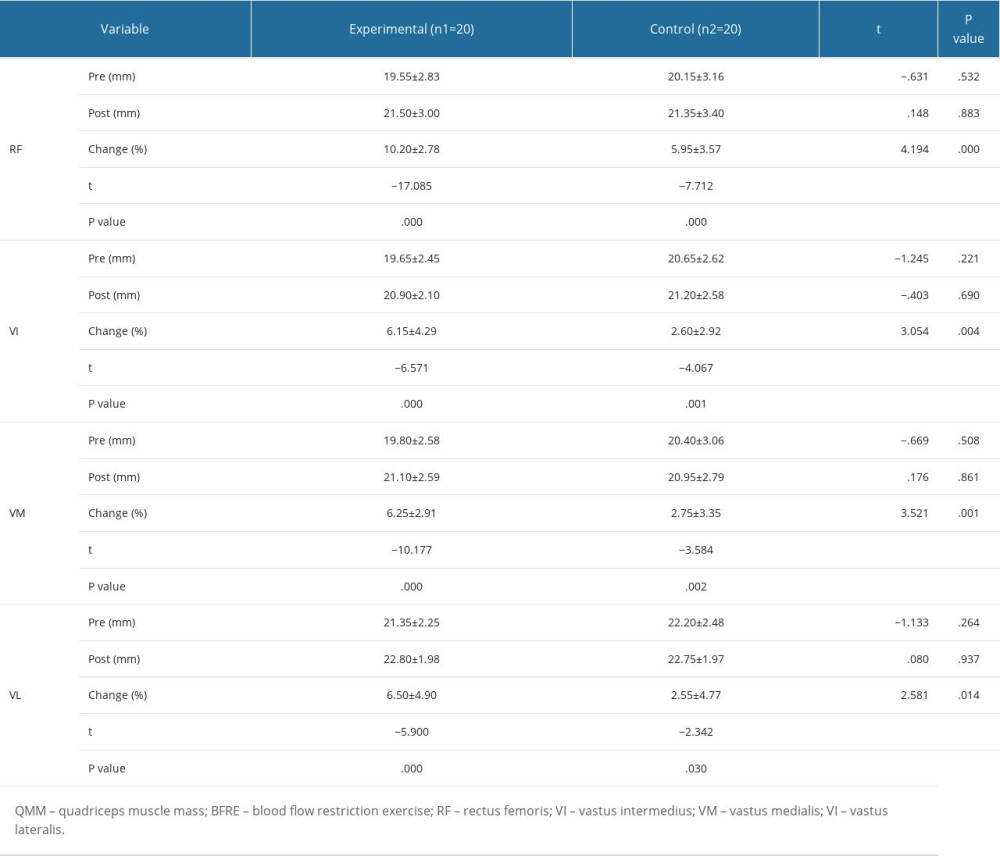 Table 5. Changes of QMM according to the BFRE.
Table 5. Changes of QMM according to the BFRE. In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952