11 March 2024: Clinical Research
The Impact of Home Cardiac Rehabilitation on Quality of Life and Psychological Well-Being in Patients with Coronary Heart Disease: A Randomized Controlled Study
Yan Zheng1ABCDEF, Li-fang Zhou2BCDF, Shu-wen Qin3BCD, Jing Guo4BDF, Bi-yong Qin5ACDEG*DOI: 10.12659/MSM.942803
Med Sci Monit 2024; 30:e942803
Abstract
BACKGROUND: Percutaneous coronary intervention (PCI), a therapeutic approach to coronary heart disease, significantly alleviates symptoms of coronary heart disease (CHD) and substantially improves quality of life. This study aimed to investigate the effect of home cardiac rehabilitation (HCR) on patients after PCI.
MATERIAL AND METHODS: We randomly divided 106 patients after PCI into an Intervention group (n=52) and a Control group (n=53). Left ventricular ejection fraction (LVEF), blood pressure, blood glucose, and low-density lipoprotein were measured in both groups before hospital discharge and after 3 months of engaging in the intervention. Patients were assessed using the short-form health survey (SF-12) scale and Hospital Anxiety and Depression Scale (HADS) scale.
RESULTS: After 3 months of HCR intervention, SF-12 scores of patients in the Intervention group were significantly higher compared to patients in the Control group (physical component summary (PCS): 47.46±9.86 vs 43.28±8.21; and Mental Component Summary (MCS): 50.68±9.82 vs 48.26±9.69) (P<0.05). Three months after HCR intervention, HADS scores of patients in the Intervention group were remarkably decreased compared to patients in the Control group (HADS-A: 7.24±1.32 vs 9.26±1.89; HADS-D: 7.79±0.81 vs 9.68±1.29) (P<0.05). Risk factors control and compliance rates of patients in the Intervention group were significantly higher compared to patients in the Control group (blood pressure: 92.45% vs 67.92%; fasting blood glucose: 88.68% vs 66.04%; low-density lipoprotein: 86.79% vs 56.60%) (all P<0.05). There was no significant difference in LVEF value between the Intervention group and the Control group after intervention (P>0.05).
CONCLUSIONS: Home cardiac rehabilitation can improve quality of life and psychology state and can help to control risk factors of coronary heart disease.
Keywords: cardiac rehabilitation, Conditioning, Psychological, Coronary Artery Disease, Heart Function Tests, Quality of Life
Background
The incidence and mortality rates of coronary heart disease (CHD) have increased significantly year by year due to the increasing prevalence of susceptibility factors, along with improvement in living standards [1]. A report showed that the current number of cardiovascular diseases patients in China has exceeded 290 million, of which 11 million have CHD [2]. Percutaneous coronary intervention (PCI), the main therapeutic approach to coronary heart disease, significantly alleviates the symptoms of CHD and substantially improves quality of life. However, it cannot reverse or delay the biological process of atherosclerosis and rule out the possibility of restenosis or thrombus [3]. A study showed that the incidence of in-stent restenosis was 10–20% at 6 months following PCI, which had long-term effects [4]. Cardiac rehabilitation (CR) after PCI is the key to prevent recurrence of CHD and improve patient quality of life [5]. Although the benefits of CR after PCI have been verified, patients showed low adherence to hospital-based cardiac rehabilitation due to the time limitation, transportation conditions, medical insurance policies and other causes [4]. Compared with hospital-based cardiac rehabilitation, home-based cardiac rehabilitation (HCR) can be more convenient and acceptable, but it has not been widely adopted in China, and its effect still requires further validation. Hospital cardiac rehabilitation requires patients to use the hospital as a rehabilitation training venue. Patients must go to the hospital, and the cost of hospitalization or outpatient services is high, which consumes more time for patients. Therefore, the compliance and application rate of cardiac rehabilitation patients in hospitals are low.
Based on family-based cardiac rehabilitation, the home is used as the main venue for cardiac rehabilitation training. Patients can receive rehabilitation training at home, and physicians can use telephone follow-up for guidance. Therefore, family-based cardiac rehabilitation improves patient compliance and application efficiency. Therefore, this study aimed to investigate the effects of home-based cardiac rehabilitation on patients’ quality of life, mental state, cardiac function, and control of risk factors.
Material and Methods
STUDY DESIGN:
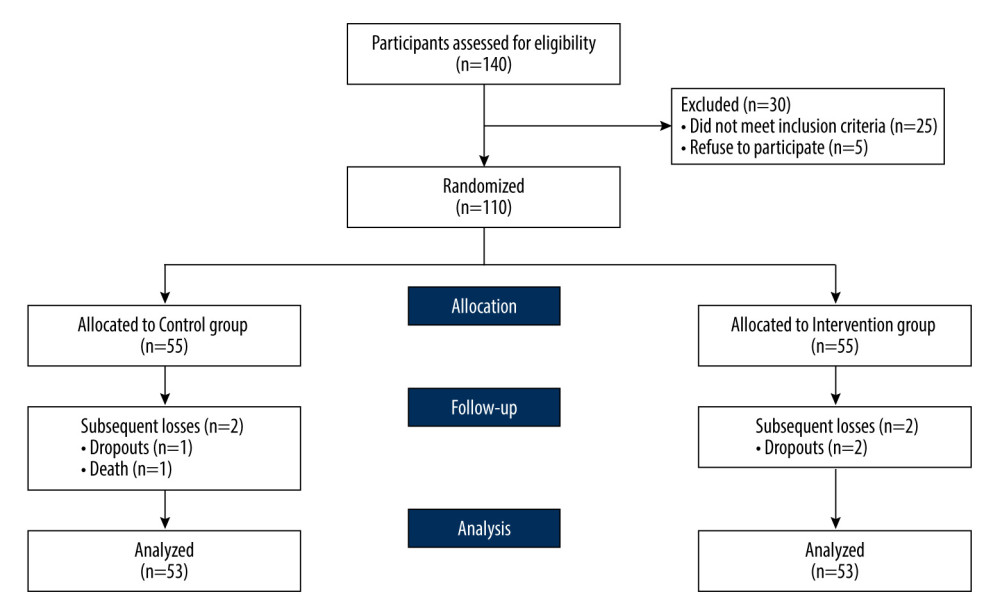
This study was a prospective, randomized, controlled trial. According to Schulz et al [6], the CONSORT statement was used to prepare the design and reporting of this study. This study was a registered clinical trial (registration number: ChiCTR2100050467). A total of 110 patients were recruited from December 2020 to September 2021 in the heart center of our hospital. Potential participants were identified by cardiac nurses based on medical interviews and medical records.
ETHICS APPROVAL:
This study was approved by Ethics Committee of the Sixth Hospital of Wuhan, Affiliated Hospital of Jianghan University (approval no. 2020031). All procedures of this study were carried out according to the Declaration of Helsinki. Informed consent was obtained from all subjects involved in the study.
RANDOMIZATION:
The 110 patients were sequentially numbered 001 to 110 according to order of hospital discharge, and then the random numbers were sequentially recorded from the random number table in any row. Patients with randomly assigned even numbers were assigned to the Intervention group (HCT group, 55 cases), and patients with odd numbers were assigned to the Control group (receiving usual care only, 55 cases).
INCLUSION AND EXCLUSION CRITERIA:
Patients with CHD after PCI who had been discharged from the hospital were recruited. Inclusion criteria for patients were as follows: 1) Conformed to the diagnostic criteria of coronary heart disease [7]. 2) PCI via radial artery was performed for the first time and the risk stratification of cardiac rehabilitation was middle-low risk [8]. 3) Age <75 years and NYHA cardiac function grading was below grade IV. The exclusion criteria were as follows: 1) Patients with middle or high risk, such as large area of myocardial infarction cardiac shock, and so on, as these patients were critically ill and could not safely perform cardiac exercise training at home without professional assistance. 2) Patients with peripheral vascular disease, renal insufficiency, malignancy, etc. 3) Patients with bone and joint diseases that affect movement or cognitive dysfunction.
TREATMENT IN CONTROL GROUP AND INTERVENTION GROUP:
Control group: On the day of their hospital discharge, patients received a routine discharge guidance and a health guide handbook, which included the risk factors of CHD, precautions after PCI, dietary guidance, and so on. Before discharge, the responsible nurse distributed the heart health guidance manual to the control group patients, which introduced the risk factors of coronary heart disease patients, postoperative precautions after PCI surgery, as well as precautions for exercise, diet, and medication. In addition, the attending physicians conducted a 10–15 min telephone follow-up of the patient every week to assess the patients’ medication compliance and disease recovery, answered the patients’ questions in time, and recorded them. The follow-up period was 3 months.
Intervention group: The Intervention group consisted of participants who participated in a 3-month HCR program. This intervention was delivered by 11 members of inter-professional cardiac rehabilitation team, which included a chief cardiac rehabilitation physician as the leader, to answer questions about rehabilitation training, 2 rehabilitation therapists to provide exercise prescription, 2 attending cardiovascular department physicians to adjust the medication plan according to results of the telephone follow-up and family visits, and 6 nurses to conduct health education and record patients’ data after exercise.
The intervention included 3 main parts: psychological intervention, remote rehabilitation exercise training, and health management. The remote rehabilitation exercise training and health management exercise prescriptions were based on home cardiac rehabilitation programs. 1) Psychological intervention: the researchers helped to solve any problems participants might have, such as complications after PCI, economic burden, and limited social function, providing positive psychological cues to patients and helping to establish an effective social support system. 2) Remote rehabilitation exercise training: Before discharge, a rehabilitation therapist made personalized exercise prescriptions for patients according to the cardiopulmonary exercise test results. The general prescription for exercise included: each session consisted of 5–10 min of warm-up exercises, 30–45 min of strengthening exercises, and 10 min of cool-down exercises. The intervention was conducted 3–5 times per week for 3 months. Patients conducted home-based rehabilitation according to the prescriptions. They were asked to wear an intelligent sports bracelet during training, which collected exercise data and physiological parameters such as heart rate. An intelligent sports bracelet app was used to quickly transfer patients’ data into background software. Patients in the Experimental group all wore the same brand and model of intelligent sports bracelets (Model: 100048760478, Xiaomi Corp., Beijing, China). The researchers adjusted the exercise prescriptions in a timely manner according to changes in heart rate and physical condition. Exercise intensity depends on the target heart rate and Borg’s rating of perceived exertion. The target training frequency was 3–5 days a week for 3 months. The target heart rate calculation formula was: individuals aged 60 and above [(220-Age)×(60–80%)], individuals aged [45–59 (220-Age)×0.7], individuals below 45 years old [(220-Age)×0.8. Borg scale for perceived exertion (self-perceived exertion levels): very, very light (6–8 points) very light (9–10 points), light (11–12 points), somewhat hard (13–14 points), hard (15–16 points), very hard (17–18 points), and extremely hard (19–20 points). 3) Health management: Telephone follow-up: The attending physician conducted telephone follow-up for 10–15 min every week to ensure implementation of the medication, diet, and exercise program of patients and answer questions about the disease. Home visiting: Rehabilitation therapists and nurses conducted 30–40 min home visits every week to evaluate the patients’ recovery from the disease and assist with guidance about diet, medicine, exercise, and psychology support.
The remote home-based cardiac rehabilitation system involves patients wearing activity trackers, inputting their basic information, and collecting data such as step count, heart rate, and exercise duration during physical activities. These data were then transmitted to the cloud via a dedicated mobile application (APP) and were shared with members of the cardiac rehabilitation team through their smartphones. The team members used this information to promptly adjust and guide the patient’s exercise plan based on changes in heart rate during exercise and the patient’s overall physical condition.
HCR COMPONENTS AND INTERVENTION VALIDATION:
Home-based cardiac rehabilitation mainly included the following steps: Prescription of rehabilitation exercises before discharge: 1) The rehabilitation therapist formulated a rehabilitation exercise prescription based on the individual condition of the patient before discharge. 2) In-hospital rehabilitation training: Patients completed 3 rehabilitation exercise sessions in the hospital before discharge. Members of the rehabilitation quality control team guided patients in mastering the rehabilitation training methods. 3) Guidance on wearing activity trackers: Before discharge, patients were instructed on correct use of activity trackers and were required to link them with their personal information. This enabled the collection of exercise data when patients engaged in home-based rehabilitation exercises. 4) Home-based rehabilitation exercises: Patients carried out rehabilitation exercises at home according to the prescribed rehabilitation exercise plan. During the implementation, rehabilitation team members collected patient exercise data through activity trackers and provided guidance based on the patient’s progress. 5) Post-discharge health management: After discharge, the rehabilitation team conducted a 3-month health management program for patients, which included bi-weekly telephone follow-ups and home visits.
To assess the intervention effects, the Control group received routine discharge instructions and telephone follow-ups, while the Experimental group underwent home-based cardiac rehabilitation treatment. After 3 months of engaging in the intervention, the survival, quality of life, left ventricular ejection fraction, anxiety and depression scores, blood pressure, blood glucose, and blood lipid control rates of the 2 groups were recorded to assess the intervention’s effectiveness.
DATA COLLECTION:
Patients’ clinical data and baseline data were collected before randomization. We analyzed data on age, sex, education, employment, income, marital status, residence, number of brackets, and blood biochemical indexes. Prior to discharge and 3 months after discharge, patients were required to complete the quality-of-life questionnaires and anxiety-depression in one-on-one interviews. Participants’ LVEF was determined before hospital discharge and 3 months after hospital discharge.
ANXIETY AND DEPRESSION:
Anxiety and depression were measured using the Hospital Anxiety and Depression Scale (HADS), which was conducted as described by Zigmond et al [9]. It comprised 2 subscales, with 14 items: 7 on anxiety and 7 on depression. The Likert 4-grade scoring method was used for each item. Higher scores indicated more unmet needs. A summary score of 0–7 was interpreted as no symptoms, 8–10 as suspected anxiety or depression, and 11–21 as strong anxiety or depression. The Cronbach’s alpha coefficient was 0.86.
CARDIAC FUNCTION:
Cardiac function was assessed by measuring left ventricular ejection fraction (LVEF). The LVEF values were detected with a conventional Simpson technique using 2-dimensional (2D) echocardiography.
CONTROL RISK FACTORS OF DISEASE:
According to the American Heart Association guideline revised in 2007 for PCI secondary prevention [10], the target levels of risk factors for CHD control are as high as the standard: blood pressure (BP) <140/90 mmHg (if patients live with diabetes, blood pressure <130/80 mmHg), low-density lipoprotein (LDL) <2.6 mmol/L, and fasting blood glucose (FBG) <6.1 mmol/L.
QUALITY OF LIFE:
The quality of life of the participants was evaluated using the 12-item Medical Outcomes Study Short-Form Health Survey (SF-12), which is a 12-item questionnaire used to evaluate patient quality of life [11]. SF-12 consists of 2 HRQoL measures: the Physical Component Summary (PCS) and the Mental Component Summary (MCS). The Cronbach α for the total scale was 0.775.
FOLLOW-UP:
The family cardiac rehabilitation team consisted of 11 members, who worked together during the implementation cycle of cardiac rehabilitation. The Control group of 55 patients received routine rehabilitation guidance before discharge, and within 3 months after discharge, telephone follow-up was only required in the 1st, 3rd, 8th, and 12th weeks after discharge, without home visits. A total of 55 patients in the Experimental group required home visits (weekly follow-up) during the 3-month intervention. Among the 11 team members, each member was responsible for an average of 5 patients. Each member visited twice a week, visiting all 5 patients for each home visit. Therefore, the workload of each group member’s visits was 120 times (12 weeks×5 times×2 patients=120), with 11 group members visiting a total of 1320 times (11 members×120 times=1320 times).
DATA ANALYSIS:
SPSS statistical package (version: 19.0, IBM SPSS, Inc., Chicago, IL, USA) was applied to carried out the statistical analyses. The descriptive analyses were applied to measure the demographic variables and the clinical variables of patients. The baseline demographic data and clinical data among groups were assessed with the chi-square test for nominal data, while the
Results
THE DEMOGRAPHICS DATA AND CLINICAL CHARACTERISTICS OF PATIENTS:
Among all 110 patients, 106 patients completed the whole process of the 3-month research (including 53 patients in the Intervention group (65.6% female) and 53 patients in the Control group (76.7% female)). We excluded 4 patients during the 3-month follow-up period because of death (1 patient in the Control group) and failure to follow up (1 patient in the Control group and 2 patients in the Intervention group). The selection process and the evaluations for the patients are shown in Figure 1.
Table 1 demonstrates the baseline characteristics of patients. There were no significant differences in demographic variables or clinical variables of patients between the Intervention group and the Control group (Table 1, P>0.05).
HCR INTERVENTION ENHANCED THE SF-12 SCORES OF PATIENTS:
SF-12 scores between groups were similar before discharge (Table 2, P>0.05). Three months after the HCR intervention, the Study Short-Form Health Survey (SF-12) scores of patients in the Intervention group were significantly higher compared to those of patients in the Control group (PCS: 47.46±9.86 vs 43.28±8.21; MCS: 50.68±9.82 vs 48.26±9.69) (III, all P<0.05). Therefore, HCR intervention obviously enhanced the SF-12 scores of the patients.
HCR INTERVENTION DECREASED THE HADS SCORES OF PATIENTS:
HADS scores between groups were similar before discharge (Table 2, P>0.05). After 3 months of HCR intervention, Hospital Anxiety and Depression Scale (HADS) scores of patients in the Intervention group were remarkably decreased compared to those of patients in the Control group (HADS-A: 7.24±1.32 vs 9.26±1.89; HADS-D: 7.79±0.81 vs 9.68±1.29) (Table 3, all P<0.05). These results clearly show the HCR intervention decreased the HADS scores of patients.
HCR INTERVENTION SLIGHTLY INCREASED LEVF VALUES:
LEVF values between groups were similar before discharge (Table 2, P>0.05). Although the LVEF values after the 3-month HCR intervention had increased to some extent, the differences between groups were not statistically significant (Table 3, P>0.05).
HCR INTERVENTION PROMOTED THE RISK FACTORS CONTROL COMPLIANCE RATES:
There were no significant differences between the 2 groups in risk factors control compliance rates, blood pressure, blood glucose, and low-density lipoprotein (Table 4, all P>0.05). The risk factors control compliance rates of patients in the Intervention group were significantly higher than in the Control group (blood pressure: 92.45% vs 67.92%; fasting blood glucose: 88.68% vs 66.04%; low-density lipoprotein: 86.79% vs 56.60%) (Table 4, all P<0.05). Therefore, the HCR intervention improved the risk factors control compliance rates of patients.
Discussion
This study indicated that HCR can improve quality of life after PCI of CHD patients. The scores of PCS and MCS domains showed significant improvement after the 3-month intervention compared with the usual care. These results were consistent with Chen’s [11] study, showing HCR had a better effect in improving quality of life compared with the usual care. With the development of medicine, we should not only pursue the relief and cure of patient’ clinical symptoms, but also pay more attention to improvement of patients’ quality of life. Hospital-based cardiac rehabilitation has been proven to be effective in improving quality of life [12,13]. However, a study [14] showed that 20% to 50% of patients were unable to comply with the hospital-based cardiac rehabilitation plan in the first 3–6 months after discharge, which increased readmission and in-stent restenosis rates and seriously decreased quality of life. In our study, HCR was used for patients’ rehabilitation treatment after PCI, the researchers regularly performed telephone follow-up and home visits, supervised the implementation of the exercise prescription, and provided physiological-psychological-social function multidimensional care. This remote rehabilitation model achieved the expansion of hospital function and outward extension, and integrated hospital-style treatment and nursing into family life, and it significantly improved the disease outcome of patients. HCR had little influence on the daily life of patients, which may be why the quality of life in the Intervention group was better than in the Control group after the 3-month intervention for patients after PCI. In addition, all participants included in this study resided in rural areas, urban settings, and townships, all within a radius of 15 kilometers from the hospital. Patients residing beyond this 15-kilometer radius were not included in the study. Therefore, all the patients could be followed up and visited by the rehabilitation team members.
HCR can improve the psychological state of patients with coronary heart disease after PCI. This study showed that after intervention, the anxiety and depression scores of the Intervention group were lower than those of the Control group, which means HCR can help improve the psychological state of patients. Patients after PCI worry about possible recurrence, the uncertain prognosis, and high medical costs, which causes a huge psychological burden. The incidence of depression in CHD patients was 77.23%, which can disturb the hypothalamic-pituitary axis, affect endothelial cell function, lead to increased myocardial oxygen consumption, and aggravate angina pectoris and other cardiovascular adverse events [15]. A previous study [16] reported that people with depression are twice as likely to have a heart attack than people without depression. Therefore, follow-up after discharge can quickly identify patients’ negative emotions such as anxiety and depression and assess the risk of disease. A systematic review also showed that psychological therapy can relieve patients’ negative emotions and improve their quality of life [17].
Here, we assessed the effect of home-based cardiac rehabilitation on cardiac function of patients, showing no significant changes in the levels of LVEF in the Intervention group compared with the Control group, which was different from another study [18]. Previous studies indicated that exercise could increase coronary blood flow and myocardial oxygen supply, and then improved coronary flow reserve capacity and cardiac function [19]. Smart et al [20] found that exercise training had no obvious effect on improving patients’ cardiac function in the short term. In our research, there was no significant change in LVEF before and after the intervention, which meant short-term home-based cardiac rehabilitation has no significant effect on improving cardiac function. Further long-term studies are required to verify the effects of exercise on cardiac function.
HCR can control the risk factors of CHD. Previous studies have shown that hypertension, obesity, abnormal lipid metabolism, diabetes, smoking, and other diseases are closely related to the occurrence and development of cardiovascular diseases, and there are overlapping effects [21]. Studies have shown that exercise can reduce the inflammatory state and cardiovascular risk factors in patients with coronary heart disease and protects against cardiovascular disease [22]. A meta-analysis [23] also found that HCR could effectively reduce plasma LDL and uric acid levels. In our study, the family was regarded as the main place for cardiac rehabilitation of patients; through regular telephone follow-up and door-to-door visits, nurses can clearly assess the implementation of rehabilitation training of patients and give professional answers to problems of patients. To avoid accidents or complications, we performed timely adjustment of treatment and follow-up plan according to the patients’ situation, which to some extent controlled the disease risk factors.
The safety of cardiac rehabilitation exercise intervention is a comprehensive issue, and previous research has confirmed the safety of appropriate unsupervised exercise [24]. In this study, patients underwent heart rehabilitation (HCR) under the guidance of medical professionals. Through meticulous assessment, monitoring, and personalized planning, the safety level of exercise was maximized to ensure that they could engage in rehabilitation activities safely and effectively.
HCR not only helps improve physical activity levels but also contributes to reducing patient anxiety and depression, enhancing the quality of life [25]. At the same time, by providing remote support in the home environment, HCR can detect and address patients’ health issues earlier, reducing the need for emergency medical services [26,27]. The decrease in use of hospital and emergency medical services can lower medical costs, enabling more effective utilization of healthcare resources. Therefore, we focused on the HCR training in patients after PCI. Overall, home cardiac rehabilitation has a positive impact on cardiovascular health, quality of life, and cost-effectiveness. Through personalized rehabilitation plans, remote monitoring, and patient education, it assists patients in better managing heart diseases and improving their quality of life, while alleviating the burden on the healthcare system.
The difference between home cardiac rehabilitation (HCR) and traditional intervention measures (CR) is: 1) Content of discharge guidance: The Control group (traditional intervention measures) received routine discharge guidance, and during the expected 3 months of intervention, patients were only followed up at home via telephone, and guidance was provided based on the patient’s chief concern, while the home-based cardiac rehabilitation group emphasized the home as the primary location for patient recovery, providing more personalized rehabilitation guidance. 2) Intervention methods during home study: In the Intervention group (family cardiac rehabilitation group), the family was the main venue for patient cardiac rehabilitation. Through the development of personalized rehabilitation exercise prescriptions, psychological intervention, remote rehabilitation training guidance, telephone follow-up, on-site visits, and other measures, the staff directly or indirectly communicated with patients to understand the implementation of rehabilitation training. 3) Comprehensive rehabilitation measures: Patients in the Intervention group actively engaged in the recovery process through comprehensive rehabilitation measures, including remote rehabilitation training guidance, psychological interventions, and home visits. Simultaneously, the staff provided professional and patient guidance on diet, medication usage, and lifestyle, aiming for a more holistic approach to addressing the patient’s health issues.
Furthermore, implementation of home-based cardiac rehabilitation has several impacts on patients after coronary heart disease percutaneous coronary intervention. 1) Implementing home-based cardiac rehabilitation can enhance the quality of life for patients after coronary heart disease PCI. 2) The implementation of home-based cardiac rehabilitation has a positive effect on improving the psychological well-being of patients after coronary heart disease PCI. 3) After the implementation of home-based cardiac rehabilitation, there is an improvement in cardiac function of patients. 4) Home-based cardiac rehabilitation has a positive effect on controlling coronary heart disease risk factors in patients after PCI. Our findings are consistent with previous studies showing long-term improvement in depression and quality of life [28,29].
This study has a few limitations. First, considering the small sample size and the recruitment of patients from a single center, the intervention effects in this research should be carefully considered. It is recommended to use a larger sample size and multiple centers for further research. Second, this study was phased research, which cannot fully observe the benefits of home-based cardiac rehabilitation in improving the cardiac function of patients after PCI. In the future, we will continue to carry out long-term research to further verify its effect. Coronary heart disease patients undergoing home-based cardiac rehabilitation for more than 12 months after PCI are expected to experience improved quality of life, psychological well-being, and cardiac function, and have better control over risk factors. This is anticipated to be superior to the traditional rehabilitation group, and the compliance rate in home-based cardiac rehabilitation is also expected to increase further. Third, this study did not measure the exercise endurance (such as six-minute walk test, AT and VO2max) for patients in the 2 groups, all of which are essential to evaluate the exercise. Fourth, we did not record and compare the physical performance of patients in the 2 groups.
Conclusions
Our study showed HCR can improve the quality of life and psychology state and can help control the risk factors of CHD. HCR is a feasible and effective method for cardiac rehabilitation. The home-based platform is more suitable for China, which has limited medical resources. In the future, it will be necessary for China to conduct long-term research to verify the effectiveness of HCR.
Tables
Table 1. Comparisons of the demographic characteristics and the clinical characteristics for participants between groups (mean±SD, n, %).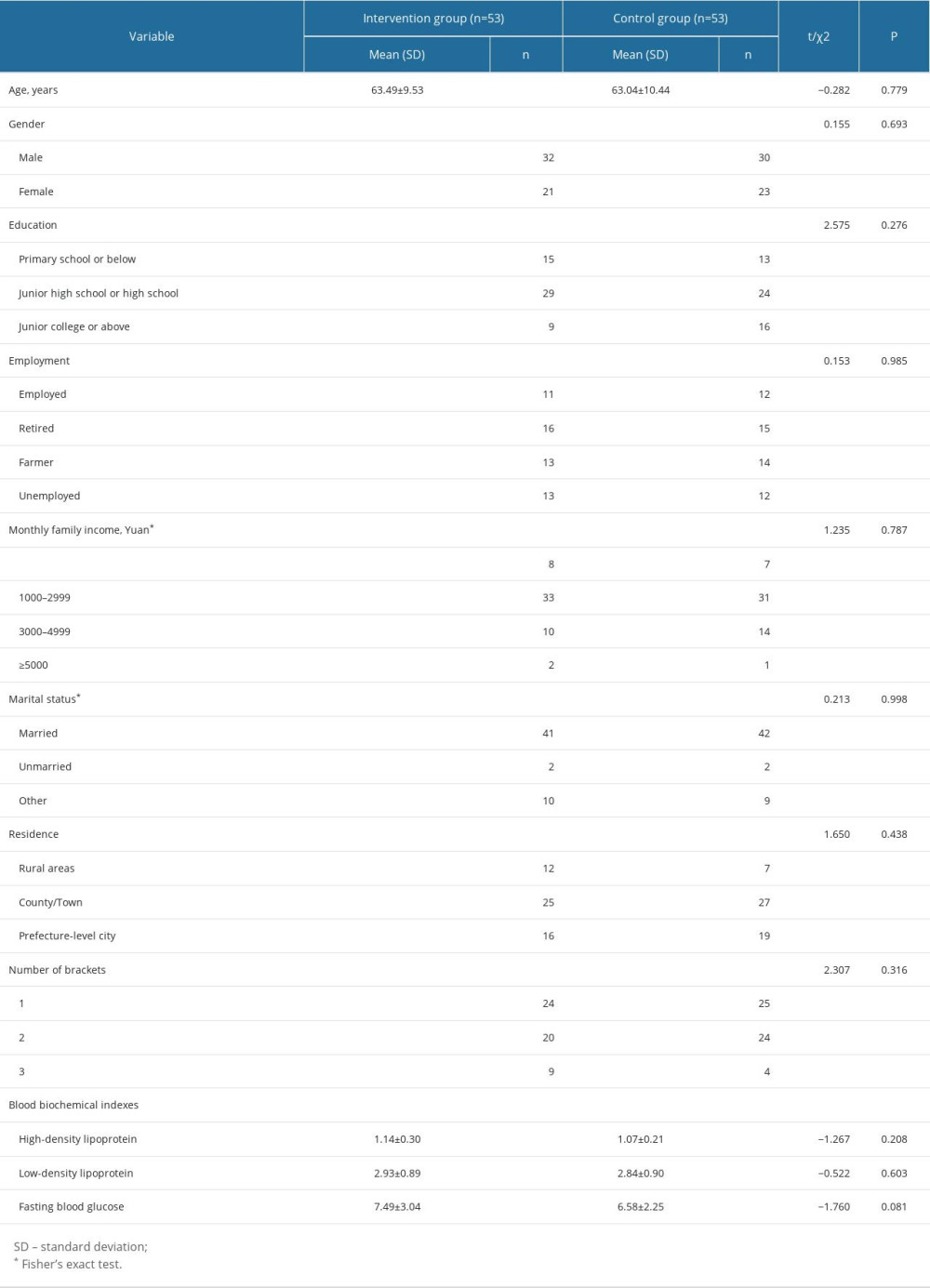 Table 2. SF-12 scores, HADS scores, and LVEF (%) for the Intervention and Control groups (baseline) (mean±SD).
Table 2. SF-12 scores, HADS scores, and LVEF (%) for the Intervention and Control groups (baseline) (mean±SD).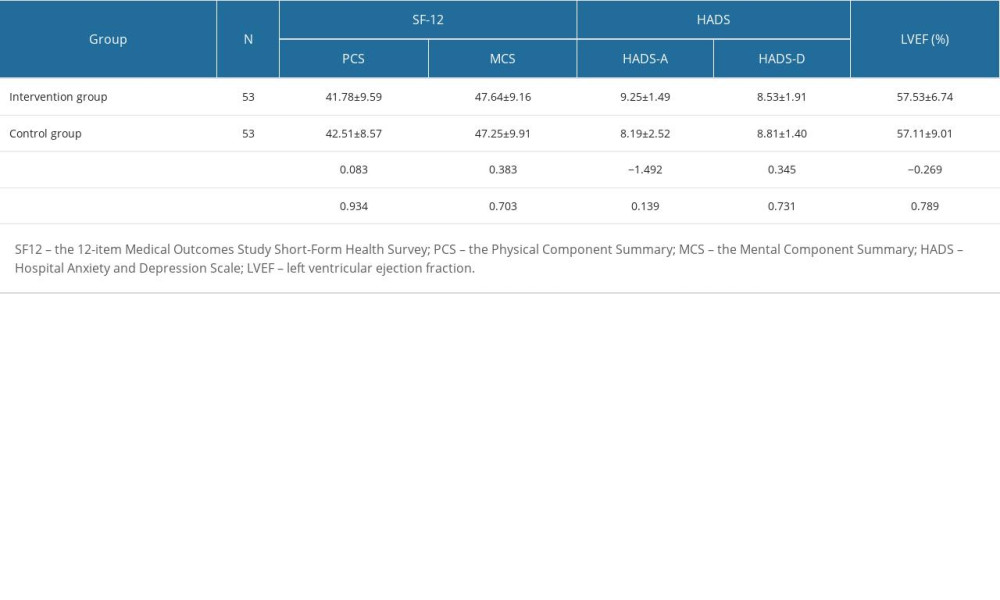 Table 3. SF-12 scores, HADS scores, and LVEF for the Intervention and Control groups (3 months after hospital discharge) (mean±SD).
Table 3. SF-12 scores, HADS scores, and LVEF for the Intervention and Control groups (3 months after hospital discharge) (mean±SD).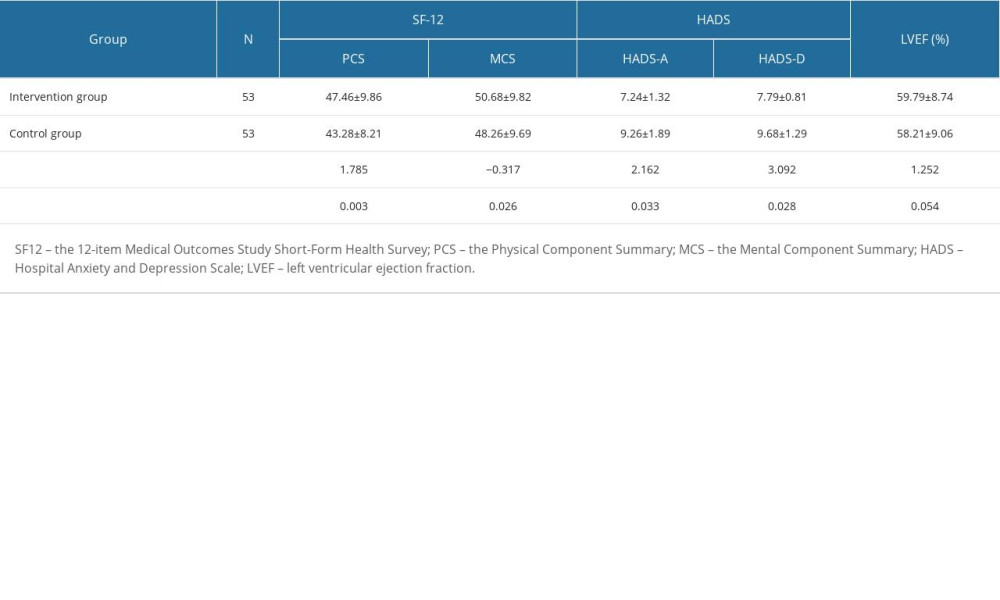 Table 4. Risk factors control compliance rate determined by BP, FBG, and AT between groups 3 months after hospital discharge and as percentage of baseline (n, %).
Table 4. Risk factors control compliance rate determined by BP, FBG, and AT between groups 3 months after hospital discharge and as percentage of baseline (n, %).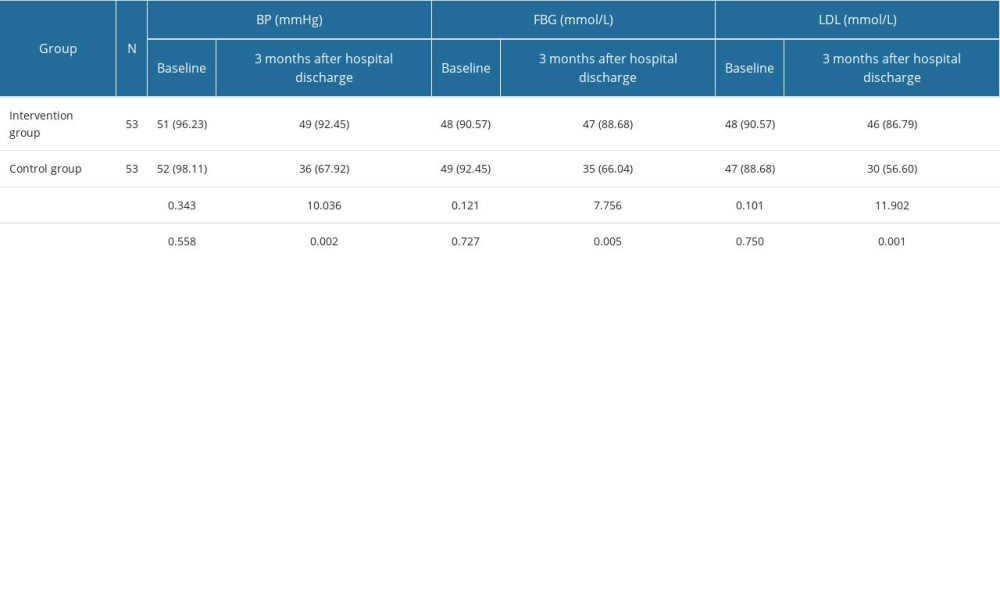
References
1. Yang L, Ruan L, Zhao Y, Association between thromboelastography and coronary heart disease: Med Sci Monit, 2022; 28; e935340
2. Zhao D, Liu J, Wang M, Epidemiology of cardiovascular disease in China: Current features and implications: Nat Rev Cardiol, 2019; 16; 203-12
3. Li S, Luo C, Chen H, Risk factors of in-stent restenosis in patients with diabetes mellitus after percutaneous coronary intervention: A protocol for systematic review and meta-analysis: Medicine, 2021; 100; e25484
4. Jiménez-Navarro MF, Lopez-Jimenez F, Pérez-Belmonte LM, Benefits of cardiac rehabilitation on cardiovascular outcomes in patients with diabetes mellitus after percutaneous coronary intervention: J Am Heart Assoc, 2017; 6; e006404
5. Winnige P, Vysoky R, Dosbaba F, Cardiac rehabilitation and its essential role in the secondary prevention of cardiovascular diseases: World J Clin Cases, 2021; 9; 1761-84
6. Schulz KF, Altman DG, Moher D, CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials: Trails, 2010; 11; 1-8
7. Siontis GC, Mavridis D, Greenwood JP, Outcomes of non-invasive diagnostic modalities for the detection of coronary artery disease: Network meta-analysis of diagnostic randomised controlled trials: BMJ, 2018; 360; k504
8. Antoniades C, Polkinghorne MD, Novel biomarkers for risk stratification in NSTE-ACS: Is there a place for Cathepsin S?: J Am Coll Cardiol, 2022; 80; 1011-13
9. Zigmond AS, Snaith RP, The hospital anxiety and depression scale: Acta Psychiatr Scand, 1983; 67; 361-70
10. Anderson HV, Shaw RE, Brindis RG, Risk-adjusted mortality analysis of percutaneous coronary interventions by American College of Cardiology/American Heart Association guidelines recommendations: Am J Cardiol, 2007; 99; 189-96
11. Chen YW, Wang CY, Lai YH, Home-based cardiac rehabilitation improves quality of life, aerobic capacity, and readmission rates in patients with chronic heart failure: Medicine, 2018; 97; e9629
12. Elsakr C, Wright L, Jagadish PS, Action plan for improving cardiac rehabilitation-related outcomes in a university hospital based on a review of previous interventions: Ann Transl Med, 2019; 7; 415
13. Xie X, Chen Q, Liu H, Barriers to hospital-based phase 2 cardiac rehabilitation among patients with coronary heart disease in China: A mixed-methods study: BMC Nurs, 2022; 21; 333
14. McDonagh ST, Dalal H, Moore S, Home-based versus centre-based cardiac rehabilitation: Cochrane Database Syst Rev, 2023; 10; CD007130
15. Richards SH, Anderson L, Jenkinson CE, Psychological interventions for coronary heart disease: Cochrane systematic review and meta-analysis: Eur J Prev Cardiol, 2018; 25; 247-59
16. Henao Pérez M, López Medina DC, Lemos Hoyos M, Depression and the risk of adverse outcomes at 5 years in patients with coronary heart disease: Heliyon, 2020; 6; e05425
17. Fuentes-Abolafio IJ, Stubbs B, Pérez-Belmonte LM, Physical functional performance and prognosis in patients with heart failure: A systematic review and meta-analysis: BMC Cardiovasc Disord, 2020; 20; 512
18. Bouchard K, Coutinho T, Reed J, Recovering from spontaneous coronary artery dissection: Patient-reported challenges and rehabilitative intervention needs: Health Psychol, 2021; 40; 472
19. Zanini M, Nery RM, de Lima JB, Effects of different rehabilitation protocols in inpatient cardiac rehabilitation after coronary artery bypass graft surgery: A Randomized Clinical Trial: J Cardiopulm Rehabil Prev, 2019; 39; E19-25
20. Smart NA, Taylor R, Walker S, Exercise training for chronic heart failure (ExTraMATCH II): Why all data are not equal: Eur J Prev Cardiol, 2019; 26; 1229-31
21. Lechner K, von Schacky C, McKenzie AL, Lifestyle factors and high-risk atherosclerosis: Pathways and mechanisms beyond traditional risk factors: Eur J Prev Cardiol, 2020; 27; 394-406
22. Long L, Mordi IR, Bridges C, Exercise-based cardiac rehabilitation for adults with heart failure: Cochrane Database Syst Rev, 2019; 1; CD003331
23. Meyer M, Brudy L, García-Cuenllas L, Current state of home-based exercise interventions in patients with congenital heart disease: A systematic review: Heart, 2020; 106; 333-41
24. Stefanakis M, Batalik L, Antoniou V, Safety of home-based cardiac rehabilitation: A systematic review: Heart Lung, 2022; 55; 117-26
25. Antoniou V, Davos CH, Kapreli E, Effectiveness of home-based cardiac rehabilitation, using wearable sensors, as a multicomponent, cutting-edge intervention: A systematic review and meta-analysis: J Clin Med, 2022; 11; 3772
26. McDonagh ST, Dalal H, Moore S, Home-based versus centre-based cardiac rehabilitation: Cochrane Database Syst Rev, 2017; 6; CD007130
27. Batalik L, Filakova K, Sladeckova M, The cost-effectiveness of exercise-based cardiac telerehabilitation intervention: A systematic review: Eur J Phys Rehabil Med, 2023; 59; 248-58
28. Jamalian M, Ansari-Moghaddam A, Roohafza H, The effect of home-based cardiac rehabilitation on depression score in patients with ischemic heart disease: A longitudinal clinical trial study: ARYA Atheroscler, 2022; 18; 1-7
29. Batalik L, Dosbaba F, Hartman M, Long-term exercise effects after cardiac telerehabilitation in patients with coronary artery disease: 1-year follow-up results of the randomized study: Eur J Phys Rehabil Med, 2021; 57; 807-14
Tables
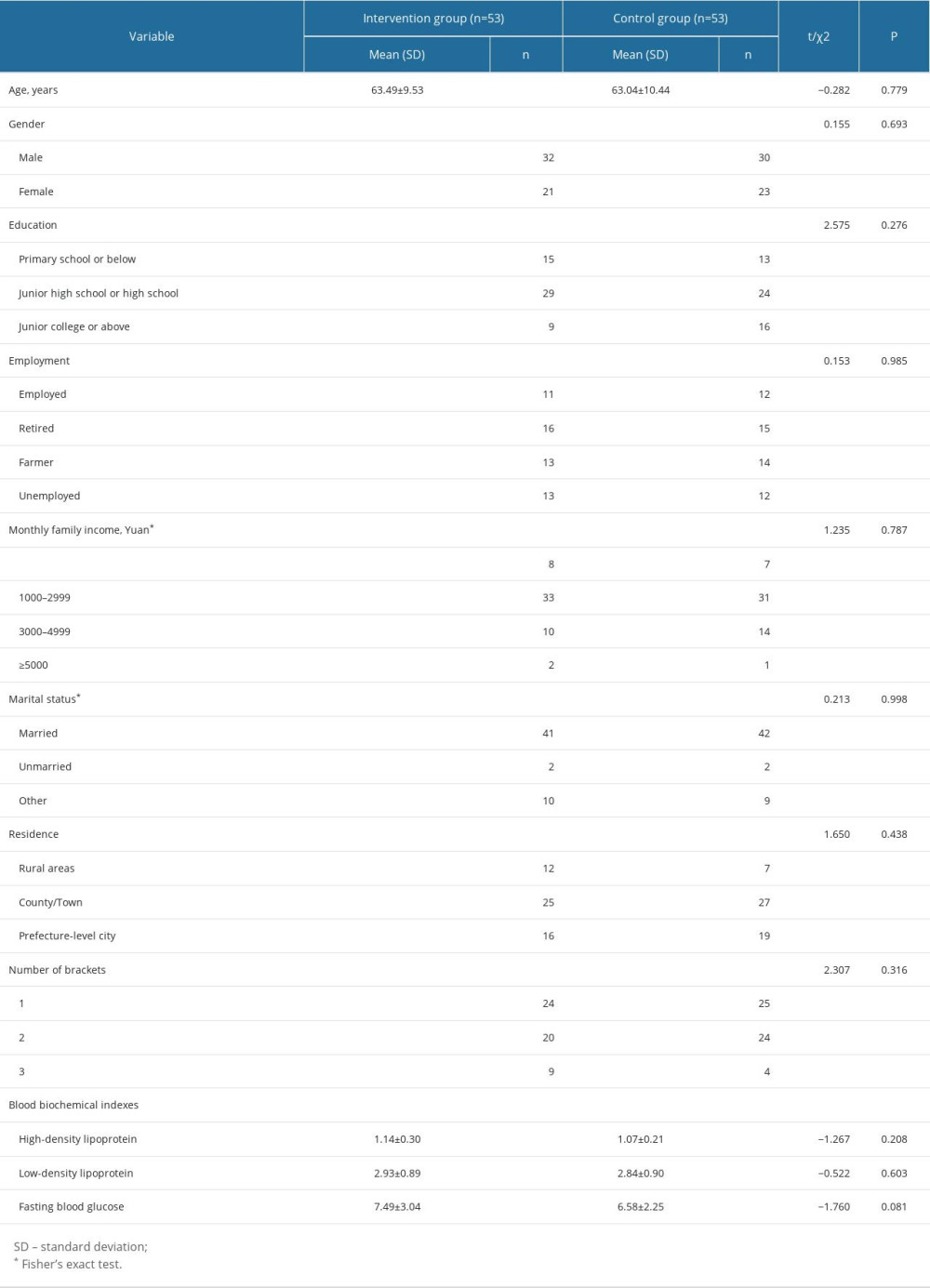 Table 1. Comparisons of the demographic characteristics and the clinical characteristics for participants between groups (mean±SD, n, %).
Table 1. Comparisons of the demographic characteristics and the clinical characteristics for participants between groups (mean±SD, n, %).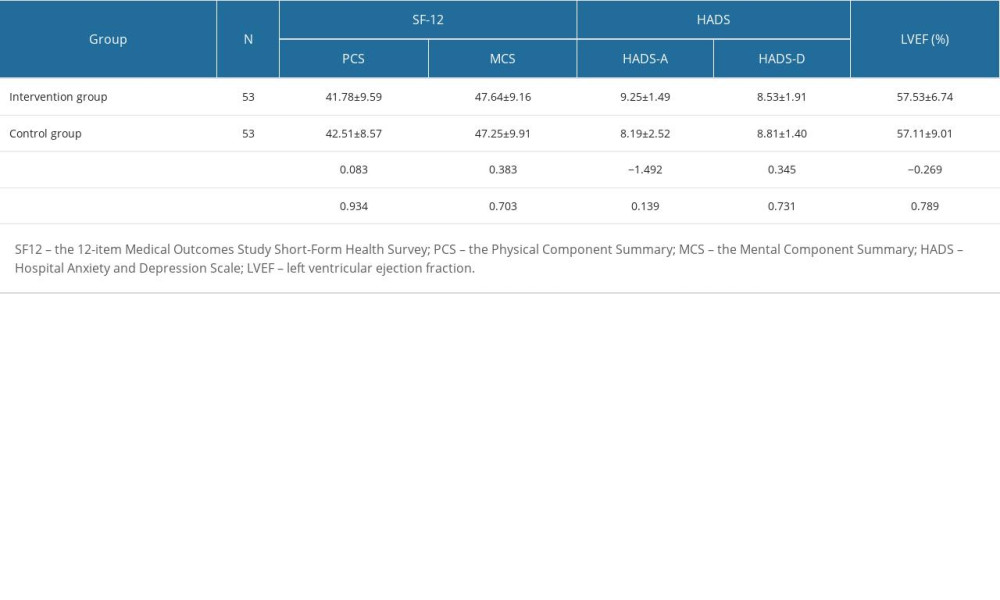 Table 2. SF-12 scores, HADS scores, and LVEF (%) for the Intervention and Control groups (baseline) (mean±SD).
Table 2. SF-12 scores, HADS scores, and LVEF (%) for the Intervention and Control groups (baseline) (mean±SD).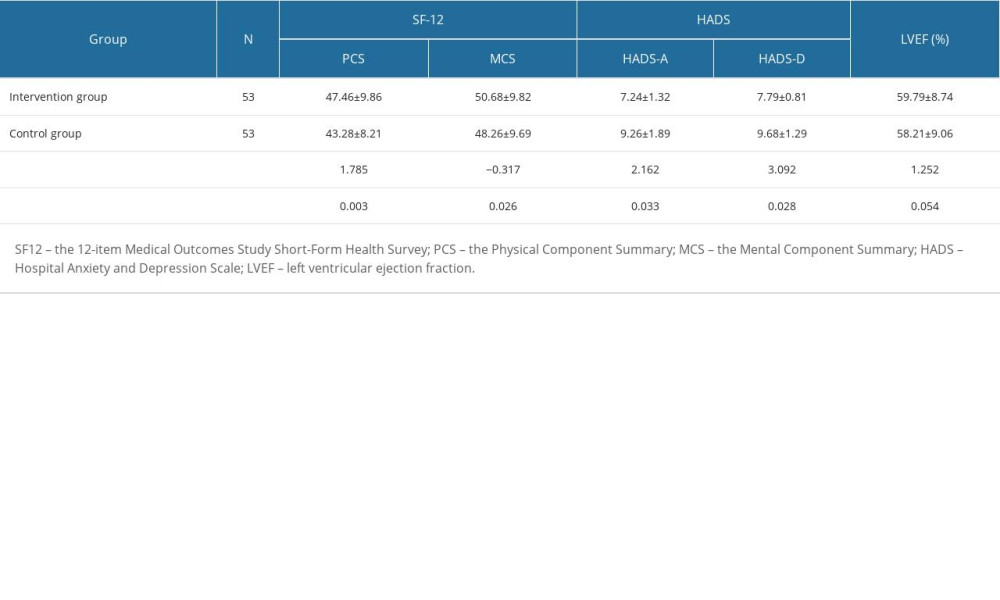 Table 3. SF-12 scores, HADS scores, and LVEF for the Intervention and Control groups (3 months after hospital discharge) (mean±SD).
Table 3. SF-12 scores, HADS scores, and LVEF for the Intervention and Control groups (3 months after hospital discharge) (mean±SD).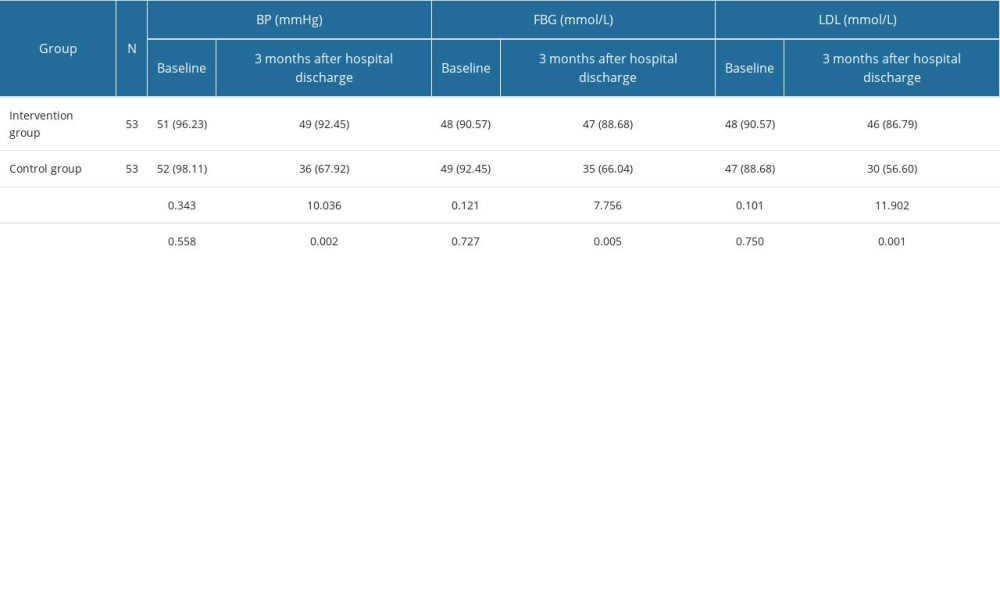 Table 4. Risk factors control compliance rate determined by BP, FBG, and AT between groups 3 months after hospital discharge and as percentage of baseline (n, %).
Table 4. Risk factors control compliance rate determined by BP, FBG, and AT between groups 3 months after hospital discharge and as percentage of baseline (n, %).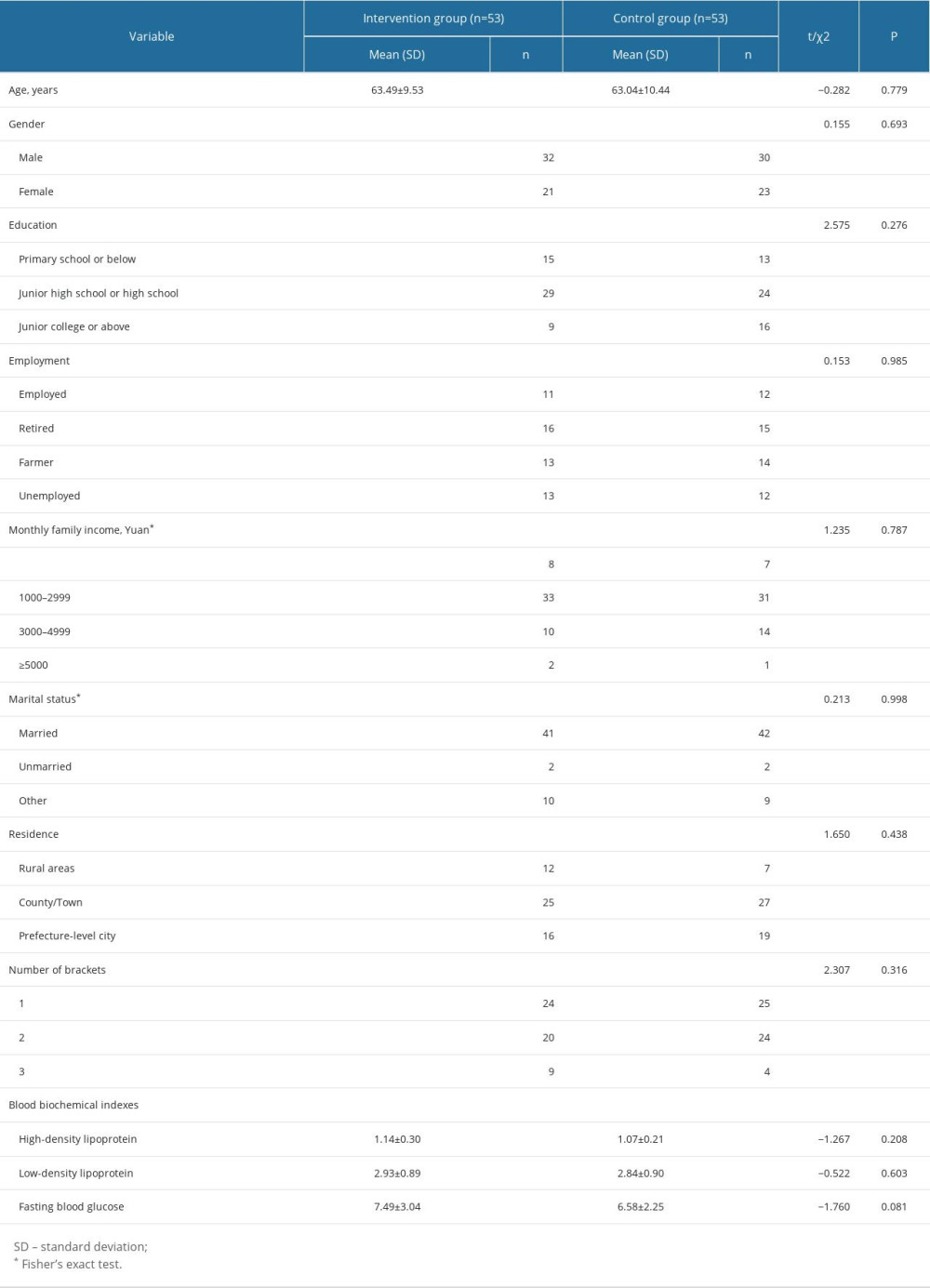 Table 1. Comparisons of the demographic characteristics and the clinical characteristics for participants between groups (mean±SD, n, %).
Table 1. Comparisons of the demographic characteristics and the clinical characteristics for participants between groups (mean±SD, n, %).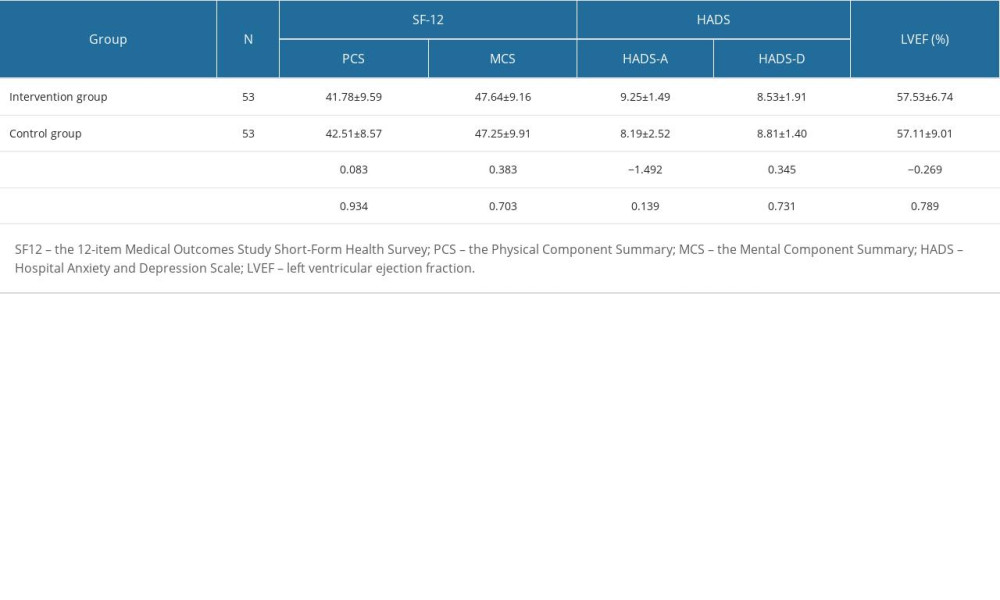 Table 2. SF-12 scores, HADS scores, and LVEF (%) for the Intervention and Control groups (baseline) (mean±SD).
Table 2. SF-12 scores, HADS scores, and LVEF (%) for the Intervention and Control groups (baseline) (mean±SD).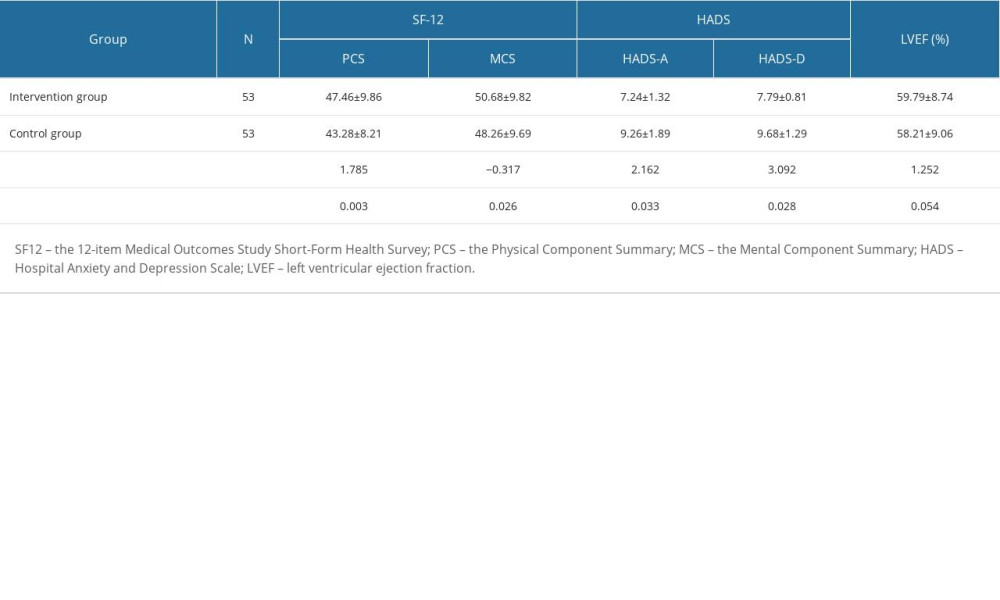 Table 3. SF-12 scores, HADS scores, and LVEF for the Intervention and Control groups (3 months after hospital discharge) (mean±SD).
Table 3. SF-12 scores, HADS scores, and LVEF for the Intervention and Control groups (3 months after hospital discharge) (mean±SD).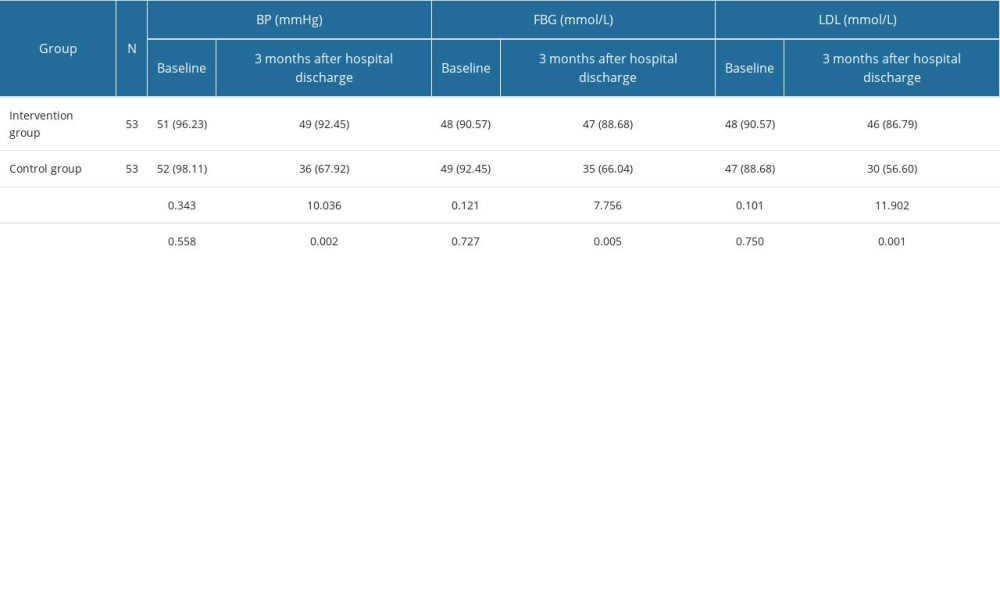 Table 4. Risk factors control compliance rate determined by BP, FBG, and AT between groups 3 months after hospital discharge and as percentage of baseline (n, %).
Table 4. Risk factors control compliance rate determined by BP, FBG, and AT between groups 3 months after hospital discharge and as percentage of baseline (n, %). In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952