11 March 2024: Database Analysis
Nanoparticle Augmentation of Adhesive Systems: Impact on Tensile Strength in Fiberglass Post Placement within Root Dentin
Abdulrahman H. AlzahraniDOI: 10.12659/MSM.943502
Med Sci Monit 2024; 30:e943502
Abstract
BACKGROUND: Modification of the glass fiber post (GFP) with titanium dioxide or silver particles can improve the durability and reliability of dental treatments for ensuring long-term success. This research assessed the tensile bond strength (TBS) of an adhesive system used for cementing GFPs into root dentin following the incorporation of nanoparticles of titanium dioxide (NTiO2) and silver (NAg).
MATERIAL AND METHODS: Sixty human maxillary canines were prepared to create a 10-mm intra-radicular space for post placement from the cementoenamel junction. The specimens were randomly allocated into 2 groups (a non-thermocycling group and a thermocycling group). Each group was divided into 3 subgroups (10 samples each) according to the adhesive system used (adhesive system devoid of any addition, adhesive system including 1% NAg, and adhesive system infused with 1% NTiO2). TBS tests were conducted and recorded in MPa using a Universal Testing Machine, with an axial load applied at a rate of 0.5 mm/min until failure. The TBS for both groups (non-thermocycling and thermocycling) was measured in megapascals (MPa), and the failure type was recorded. The data were statistically analyzed using one-way analysis of variance (ANOVA) and Tukey’s test with P<0.05 value as a significant difference.
RESULTS: The adhesive systems containing nanoparticles of titanium dioxide and NAg exhibited considerably higher values of TBS than adhesive systems without additives. Significant differences were recorded with P values of 0.001. In addition, thermocycling decreases the TBS.
CONCLUSIONS: Addition of nanoparticles to adhesive systems significantly increases their tensile bond strength. Such improvements hold promise for enhancing the durability and reliability of dental restorations, benefiting the patients and clinicians.
Keywords: Nanoparticles, Post and Core Technique, Root Canal Preparation, Tensile Strength
Background
Caries, early restorations, fractures, and the creation of an endodontic access are common culprits contributing to tooth structure loss in root canal-treated teeth. The practice of employing endodontic posts in teeth with insufficient coronal tooth structure is universally established [1]. While post systems were originally designed to be mechanically retentive within root canals, they often led to significant tooth structural loss [2]. The utilization of cast metal posts has been a long-standing approach, with an impressive 10-year survival rate, especially in terms of intra-radicular retention [3].
The development of posts made of glass fiber (GFP) emerged as an alternative to metal posts. Metal posts were perceived to have higher elastic moduli than dentin, posing a higher risk of root fractures and catastrophic failures [4]. However, GFPs exhibited mechanical properties akin to dentin, thereby reducing the risk of catastrophic failure, with most failures associated with post debonding [5]. The evolution of adhesive and resin cement systems marked a shift toward conservative repair of endodontically treated teeth [6,7]. Nevertheless, achieving adequate root canal adhesion remains challenging given the unfavorable shape of root canals and limitations of physical–chemical characteristics of adhesive materials [8].
The process of removing gutta percha and preparing for the placement of intra-radicular posts in completely filled root canals is crucial. Mechanical removal of sealer-impregnated dentin from the canal walls is recommended prior to cementing the posts. Neglecting this step results in the absence of a fresh surface for resin cement penetration and attachment, compromising retention [9].
When dentin is removed, the smear layer becomes prominent, necessitating its removal or effective permeation by the adhesive system. Chemical irrigants, such as EDTA and sodium hypochlorite, have been proposed for smear layer removal, but these compounds may also interfere with resin cement adhesion to radicular dentin [10].
One major impediment to achieving reliable adhesion is polymerization shrinkage, which frequently surpasses the adhesives’ dentin bond strength, causing gaps to form along surfaces with the weakest bonding [11,12].
Titanium dioxide (TiO2) possesses several advantageous features, including nontoxicity and chemical stability, as well as a highly efficient photocatalytic effect [13]. Nanoparticles of titanium dioxide (NTiO2) are particularly intriguing because of their demonstrated antibacterial properties in various biomaterials [14,15]. In addition, TiO2 offers a white color, exceptional stability, cost-effectiveness, and low toxicity [16]. Silver ions (Ag ion) are also incorporated into dental resins owing to their antibacterial properties, inhibiting bacteria on the resin surface and in the surrounding culture [17–19]. A unique property of nanoparticles of silver (NAg), characterized by tiny particle size and extensive surface area that release Ag ions with lower filler content, is the decreased concentration of (Ag) particles required for efficacy [20].
Alkahtany et al conducted a comparable study on the TBS of GFPs to radicular dentine at different root levels. The recorded values ranged between 4 and 11 MPS, especially at the medial and apical thirds, revealing significant differences among the tested groups [21]. Similar TBS values were recorded by Başaran et al at the coronal portion of root dentin, but they showed significantly higher bond strength values at other areas. However, no significant differences were found between the coronal-middle or middle-apical portions [22]. Raafat et al recorded a higher bond strength at different areas between GFP surfaces and root with an overall bond of 12.47±2.17 and 15.09±3.81 for a group of conventional with silane and other groups treated with Er: YAG laser, respectively, followed by silane application [23]. Contrary to all bond forces mentioned above, Zhu et al recorded much higher values (5–20 MPa) of bond strength [24].
This study aimed to examine the effect of the addition of nanoparticles of titanium dioxide (NTiO2) and nanoparticles of silver (NAg) at a concentration of 1% to adhesive systems for cementing GFPs to dentin in root canals. The study specifically assessed the effect of thermocycling on tensile bond strength and the potential to enhance the overall performance of the adhesive system.
Material and Methods
SAMPLE PREPARATION:
This cross-sectional study was approved by the Research Committee, College of Dentistry, Jazan University (REC-44/07/501on 30 January 2023). At the time of collection of teeth, informed consent was obtained from all participants. Sixty human maxillary canines, all of which were fully developed apices, and displayed no cavities, cracks, or prior endodontic treatment, were included in the research. Canines were selected due to similarity in the dimensions and sufficient thickness of dentine and cementum. The canine teeth were extracted due to periodontal disease with severe mobility. The teeth were preserved in a 0.1% thymol solution to maintain their integrity. Subsequently, any soft-tissue precipitate was meticulously removed using a hand scaler. To facilitate further experimentation, a low-speed handpiece equipped with a diamond double-faced disk was used to carefully remove the coronal portion of each tooth, ensuring constant cooling with air/water spray. To provide a consistent and stable base for testing, roots were introduced in acrylic resin chemical-cure (Acrostone Dental Factory, Egypt) within plastic cylinders.
SAMPLE SIZE ESTIMATION:
Sample size was calculated using G*Power software (version 3.1; University of Dusseldorf). The effect size (d) was 0.5, α was 0.05, and 1-β (power) was 0.65. The proper specimen size of 60 samples were calculated according to the tensile bond strength of the conventional GFPs from previous studies.
ENDODONTIC PROCEDURES:
After 1 week of collection of teeth and storage in an incubator, the endodontic instrumentation involved using a master apical file size #35 with a working length of 0.5 mm from the apex (Figure 1A) were carried out. Stainless steel K files (Dentsply Maillefer, Ballaigues, Switzerland) were used in a step-back approach to shape the root canals. Then, gutta percha, joined with epoxy resin sealer (Sealer 26; Dentsply Maillefer), was used in a lateral condensation technique to fill the canals (Figure 1B).
PREFABRICATED POST PLACEMENT:
A 10-mm-deep post-gap was created to accommodate a prefabricated GFP characterized by parallel sides and a tapered tip (Reforpost No. 2; Angelus Dental Products, Londrina, Brazil). After removing gutta percha with a heated tool, the root walls’ interior geometry was standardized using #4 and #5 intracanal largo drills (Reforpost drills #4 and #5; Angelus Dental Products) in a low-speed handpiece (Figure 1C). All canals were disinfected and kept for 48 h to be ready for post placement and cementation.
GROUPING AND APPLICATION OF ADHESIVE SYSTEMS:
According to the bonding type agent used, samples indiscriminately divided into 2 equal groups of 30 samples each, at 10 samples of each type: adhesive system devoid of any addition, adhesive system containing 1% titanium dioxide nanoparticles (NTiO2), and adhesive system including 1% silver nanoparticles (NAg). The samples were further subdivided into 2 groups, with and without thermocycling.
ADHESIVE APPLICATION:
The intra-radicular preparations were treated using Clearfil SE Bond (Kuraray America, Inc, NY, USA), a self-etching 2-step adhesive method. Clearfil SE primer was applied to the canal space using a micro-brush and dispersed for 20 s. Clearfil SE bond was applied with and without the addition of NTiO2 and NAg, with extra material being eliminated with a paper point. Light-emitting diode (LEDs) (Bluephase N, Ivoclar Vivadent, India) was used to light-cure specimens for 20 s.
CEMENTATION AND THERMOCYCLING:
Following the manufacturer’s instructions, RelyX ARC resin cement (3M Espe, St. Paul, MN, USA) was applied, and the cement was placed with a Lentulo spiral drill #60 (Dentsply/Maillefer, Ballaigues, USA) in a low-speed handpiece. After placement, the posts were light-cured for 40 s, excess cement was removed, and further light-curing was performed (Figure 1D). Prior to testing, the samples were stored in humidified medium for 24 hours at 37°C, then half of the specimens were subjected to 5000 thermocycles by a special machine (Thermocycler, SD Mechatronik, Feldkirchen-Westerham, Germany) in cold (5°C) and hot water (55°C) successively. The dwell time was 30 s, and TBS test was performed [25,26].
TENSILE BOND STRENGTH TEST:
After that, the samples were storage for 48 h in an incubator before the mechanical test and failure mode assessment. Acrylic resin cylinders with metallic loops were fabricated over the coronal region of the posts to test the tensile strength (Figure 2). A 0.5 mm/min axial tensile stress was applied to samples tested on Universal Testing Machine (Conten Industries, Inc, USA) until fracture occurred [22,24,26].
FAILURE TYPE ASSESSMENT:
The slices were evaluated using a Leica M165C stereomicroscope (Leica Microsystems, USA) at 25× magnification and LAS v4.4 software to analyze the failure type (Leica Microsystems). The failures were determined in percentages and classified as follows: type I) dentin adhesive, where the intracanal material was displaced from the dentin; type II) adhesive to resin cement, where the GFP was displaced from the resin cement; type III) mixed, where the GFP was displaced from the dentin and resin cement; type IV) dentin cohesive, where a fracture was found in the dentin; type V) GFP cohesive, where a fracture exists in the GFP [27,28].
STATISTICAL ANALYSIS:
Microsoft Excel worksheets were used to enter the data and analyzed using Stata 18 (StataCorp LLC, Texas, USA). The normality of the data was checked, and parametric tests were performed for analysis. The intergroup comparison was conducting using one-way analysis of variance (ANOVA) to determine the loads at failure. Tukey’s test was used to assess pairwise significant differences among the means of examined materials. The thermocycling and non-thermocycling groups were compared, with
Results
TENSILE BOND FORCES VALUES:
The mean of the tensile bond strength (MPa) of various adhesive systems was evaluated, including those devoid of additives, and those containing NTiO2 and NAg at a 1% concentration. The highest mean value for the TBS in the non-thermocycling group was observed in samples treated with Clearfile SE bond with NAg (9.42±0.19), followed by 7.32±0.74 for samples treated with Clearfile SE bond with NTiO2. Similarly, in thermocycling groups, the highest mean TBS value was found in samples of Clearfile SE bond with NAg (8.53±0.23), followed by 6.42±0.52 in samples of Clearfile SE bond with NTiO2, as shown in Figure 3. Significant differences were recorded within the 2 groups with P values of 0.001 (Tables 1, 2). In the comparisons between the thermocycling and non-thermocycling groups, the recorded P value of 0.049 was considered a marginally insignificant value.
FAILURE TYPE PERCENTAGES:
Table 3 and Figure 4 present the percentage with numbers in relation to failure types. For the thermocycling group, failure type III (mixed: when the GFP was displaced from the dentin and resin cement) obtained the highest value and recorded 60%, 40%, and 40% for Clearfile SE bond alone, Clearfile SE bond with NTiO2, and Clearfile SE bond with NAg, respectively. The failure type IV (dentin cohesive: when there was a fracture in the dentin) recorded 50%, 40%, and 20% for Clearfile SE bond with NTiO2, Clearfile SE bond with NAg, and Clearfile SE bond alone, respectively. For the non-thermocycling group, failure type III was the highest and recorded 50% and 50% for Clearfile SE bond alone and Clearfile SE bond with NTiO2, respectively, whereas type IV recorded 60% and 50% for Clearfile SE bond with NAg and Clearfile SE bond with NTiO2, respectively. No samples were classified as type I, which denotes dentin adhesive failure (intracanal displacement from the dentin), in the thermocycling or non-thermocycling samples.
Discussion
In modern dental rehabilitation techniques, GFPs have become more popular due to their elastic moduli, which are comparable to those of human radicular dentin [29,30]. When nanofillers were incorporated into the adhesive solution, tensile strengths significantly increased compared with the control group. This study examined the effect of NTiO2 and NAg addition at a concentration of 1% on an adhesive system for cementing GFPs to dentin in root canals, considering the influence of thermocycling. The study specifically assessed the effect of thermocycling on tensile strength and the potential to enhance the overall performance of these adhesive systems. The results revealed that an adhesive system containing 1% NTiO2 and NAg exhibited significantly higher tensile bond strength than an adhesive system without additives.
Overall, the TBS of GFPs recorded in the current study was between 9.42±0.19 and 4.76±0.37 MPa for the non-thermocycling and thermocycling samples. This finding is similar to the results documented by Alkahtany et al, who examined the bond strength of GFPs to radicular dentine at different root levels, especially at the medial and apical thirds, with significant differences between groups [21]. By contrast, the bond strength values recorded by Zhu et al were much higher than those obtained by the present study. This finding could be attributed to the approach of measuring the bond strength with different cement types [24]. Marginally equal fracture force values were recorded by Başaran et al at the coronal portion of the root dentin with significantly higher bond strength values. However, no significant differences were observed between the coronal-middle or middle-apical portions [22].
In addition, relatively higher fracture forces were recorded by Alves et al [26], and by Zhu et al between 5 to 20 MPa [24]. The durability and efficacy of restorations are influenced by post retention [31]. Debates have been triggered by the necessity of adhesive luting of GFPs [32]. The suggestion of dragging the post along the canal walls, contrary to relying solely on adhesive bonding, plays an important role in their attachment [29]. Raafat et al recorded a higher bond strength at different areas between GFP surfaces and root with an overall bond of 12.47±2.17 and 15.09±3.81 for a group of conventional with silane and other groups treated with Er: YAG laser, respectively, followed by silane application [23].
Compared with other cement types, the use of resin cements enhances GFP retention, thereby reinforcing bonded structures [33]. Adhesive cementation has also been linked to improved marginal adaptation, optimizing coronal sealing, reducing post length [33], enhancing retention, and optimizing patterns of fracture in the event of failures [34]. Although encouraging outcomes have been reported for GFP usage, issues related to bond integrity, cementation, and interface stability have been addressed. The optimal approach for establishing a robust and enduring adhesive that bonds between dentin root and reinforced GFPs [35] remains to be determined. An ideal interface between dentin and the post must be devoid of gaps, creating a symmetric unit (monobloc), which was once assumed but is now considered a theoretical concept [36]. However, the apical region of adhesive contact between the post and dentin has shown superior integrity to the rest of the interface [35,36]. This finding is evident during examination of the failure pattern.
Chemically stable, biocompatible, and antimicrobial TiO2 holds significant promise as an inorganic additive. Nanoparticles have been proposed as dental resin and epoxy reinforcing fillers [37]. NTiO2, characterized by large surface area and high biocompatibility, have found diverse applications in dentistry, enhancing fracture resistance in endodontically treated teeth, promoting dental implant osseointegration, bolstering antibacterial properties, and improving adhesion to human teeth in dental adhesives. Recent research has indicated that the inclusion of TiO2 nanoparticles in dental adhesives resulted in comparable water sorption, solubility, and biocompatibility compared with unaltered adhesives [38,39]. Self-adhesive resin cements with TiO2 exhibited a superior degree of conversion (DC) to their unaltered counterparts. Despite concerns about potential cytotoxicity at high concentrations within the human body, the typical TiO2 content in dentin adhesives (5–10 wt.%) minimizes this risk. As a result, the advantages of TiO2 inclusion outweigh the challenges [39,40].
The bonding agent with NAg content has demonstrated antibacterial properties on and off its surface. This observation suggests that NAg-containing resin can exert its antibacterial effects over a considerable distance, most likely attributed to the release of Ag ions [41]. The incorporation of NAg into a bonding agent can enhance the thermal and mechanical properties, biological stability, and antibacterial properties when present at low concentrations [42], thereby reducing or eliminating stress concentration at the adhesive bonding resin complex [43].
The addition of NTiO2 and NAg has improved strength, which can be attributed to the intrinsic properties of these nano titanium and nano silver particles. The strong ionic interatomic bonding in these nanoparticles contributes to their attractive material properties, including tensile strength [44].
The clinical significance of incorporating NTiO2 and NAg into adhesive bonding lies in their potential to enhance the long-term performance of dental restorations. These nanoparticles can contribute to the durability and stability of GFPs when bonded to root dentin by significantly increasing bond strength. This improvement can lead to better outcomes in terms of restoration longevity and reduced risk of post debonding or failure, ultimately increasing the overall success of dental rehabilitation techniques. Reinforcement of the experimental dentin adhesive with TiO2 increased the push-out bond strength of the GFP to root dentin [45]. Also, TiO2 nanofibers in 2.5% of weight inserted in dental adhesive reduced the nano-leakage but did not expand the μTBS to root dentin [46]. Moreover, dentin pre-treatment with the nanoparticles after applying the conditioner enhanced the TBS of the GIC to dentin related with the control group [47].
A recent review found insufficient evidence to conclude which is the best final rinse irrigator. Further research is warranted, emphasizing test standardization and well-documented randomized clinical studies, considering occlusal forces and tooth position in the arch [48]. The collected information suggested that the conditioning agent, such as laser, showed better results for dentin conditioning, increasing the bond strength of the GFP to the root canal [49], although such materials can be used during daily practice of post and core restorations. However, further clinical trials and studies with addition of those and other important adhesive materials systems in different proportions and concentration for GFPs are essential to confirm these laboratory findings and establish their practical applications in real-world dental practice.
A failure test is usually caried out after applying forces in bond strength test to estimate the value of forces that the materials can withstand prior to fracture. Regardless of the type of adhesive system used, the values of the TBS of all samples slightly decreased after thermocycling, and there is no published study that investigated this adhesive system type added to the GFPs.
Silva et al and Sheikh et al found marginally similar percentages and failure types, especially in the mixed type or type III (when the GFP was displaced from the dentin and resin cement) and dentin cohesive or type IV (when a fracture exists in the dentin) [50,51]. However, the findings did not agree with those of other failure types recorded in samples prepared by Alves Dos Santos et al and Bertolini et al, perhaps due to the methods of sample preparation and the use of different types of bonding and cementing structures [27,28].
This study has certain limitations. It was ore over conducted in vitro; thus, it cannot fully replicate oral conditions. Furthermore, the results are restricted to a single-load test; hence, future research must include heat, cyclic loading, and storage in water or artificial saliva to further stress the adhesive mediator.
Lastly, luting cements and adhesives techniques for bonding between the dentin root and GFPs should undergo additional assessments through long-term clinical performance and clinical trials.
Conclusions
The addition of 1% NTiO2 and NAg nanoparticles to adhesive bonds significantly increased TBS, whereas thermocycling reduced the values of the tensile fracture forces. Failure type III (mixed: when the GFP was displaced from the dentin and resin cement) and type IV (dentin cohesive: when the dentin is fractured) were the most predominant types among all samples. Further research is warranted to explore these additives’ effects on other mechanical and physical properties at various concentrations.
Figures
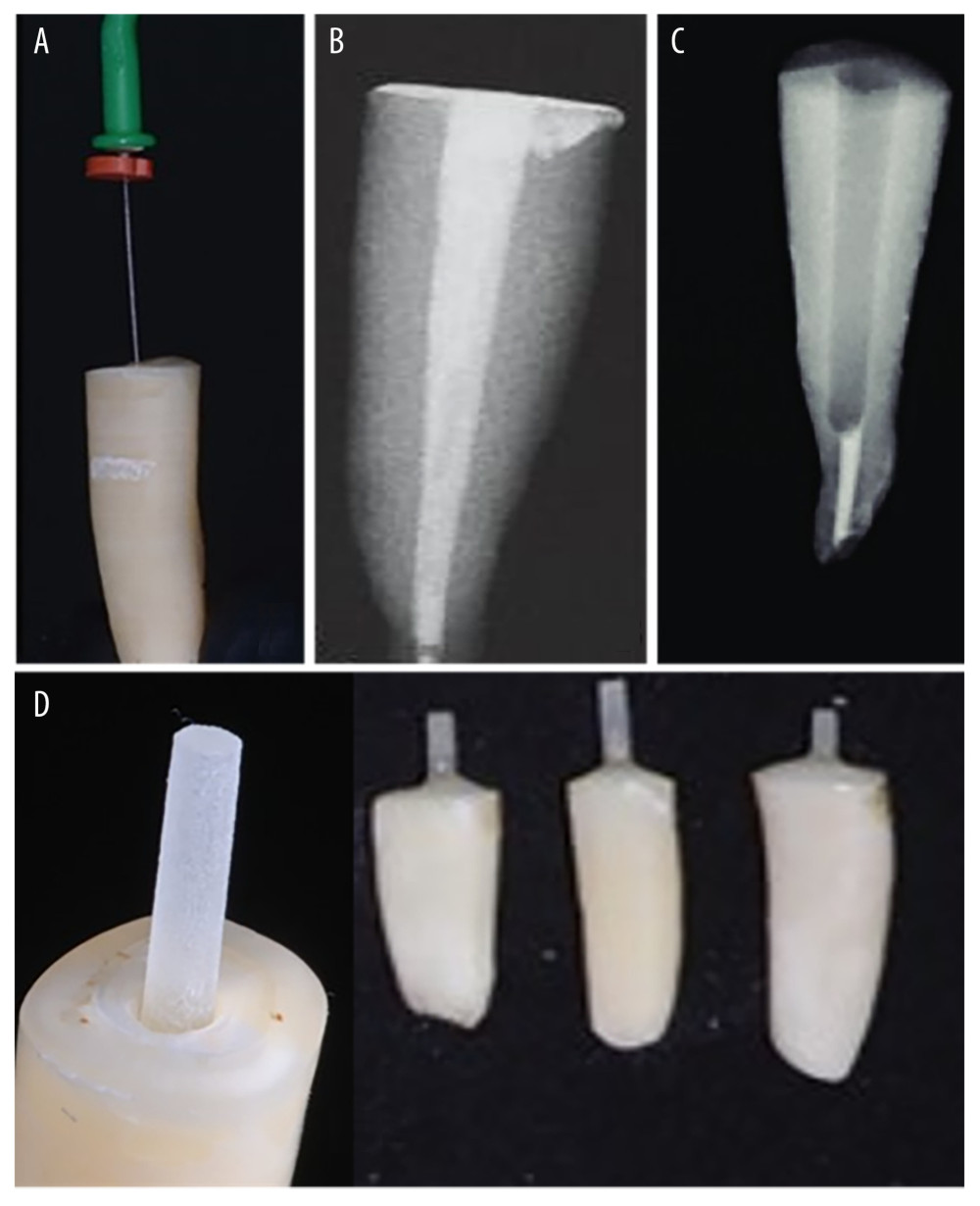 Figure 1. During endodontic treatment, (A) working length, (B) filling the canal with gutta percha, (C) post space preparation, and (D) after cementation of posts.
Figure 1. During endodontic treatment, (A) working length, (B) filling the canal with gutta percha, (C) post space preparation, and (D) after cementation of posts. 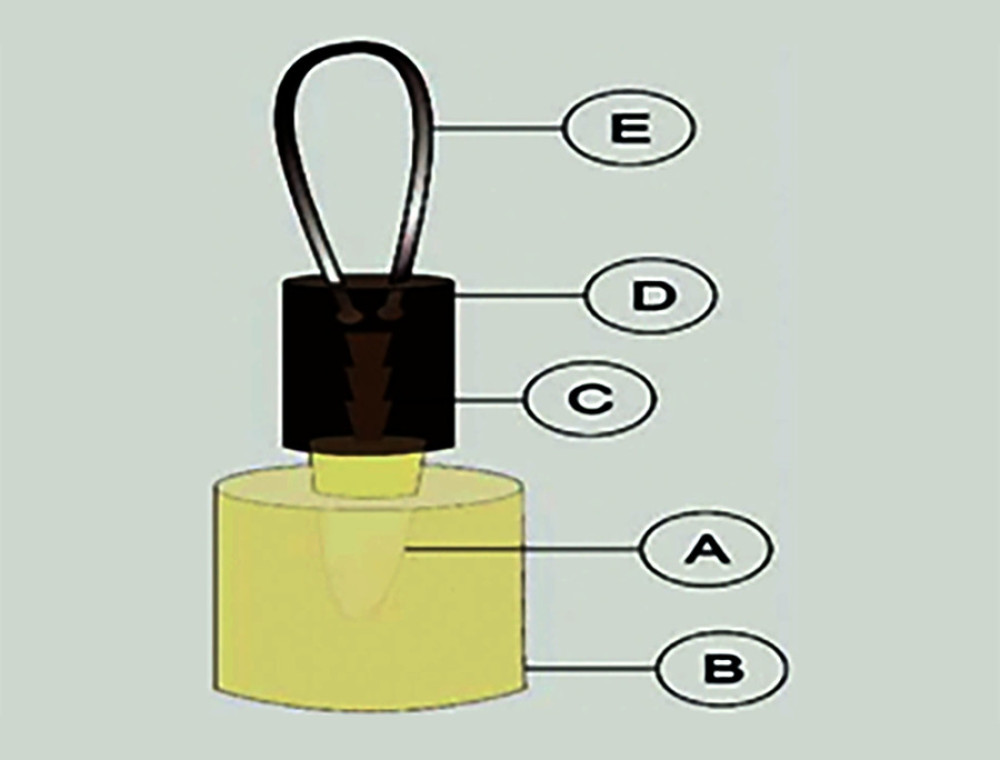 Figure 2. Sample ready for tensile bond strength test, A) human root; B) acrylic resin; C) glass fiber post; D) acrylic resin cylinder; E) metallic loop.
Figure 2. Sample ready for tensile bond strength test, A) human root; B) acrylic resin; C) glass fiber post; D) acrylic resin cylinder; E) metallic loop. 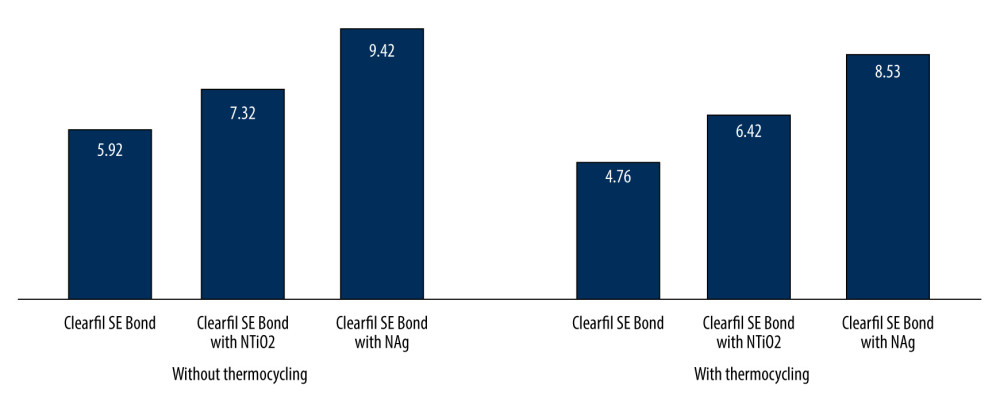 Figure 3. Bar chart of mean tensile bond strength in (MPa) of the tested bond adhesive system groups with and without thermocycling.
Figure 3. Bar chart of mean tensile bond strength in (MPa) of the tested bond adhesive system groups with and without thermocycling. 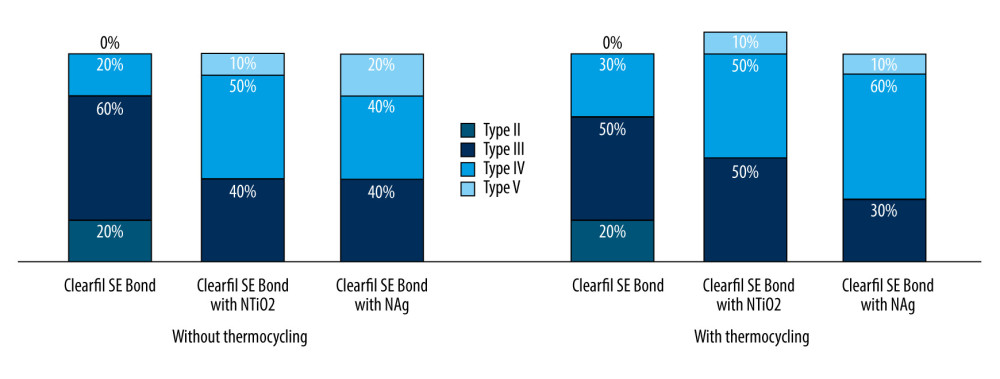 Figure 4. Percentage of the failure pattern of the tested bond adhesive system groups with and without thermocycling.
Figure 4. Percentage of the failure pattern of the tested bond adhesive system groups with and without thermocycling. Tables
Table 1. Comparison of the mean tensile strengths for non-thermocycling samples of tested adhesive systems in MPa.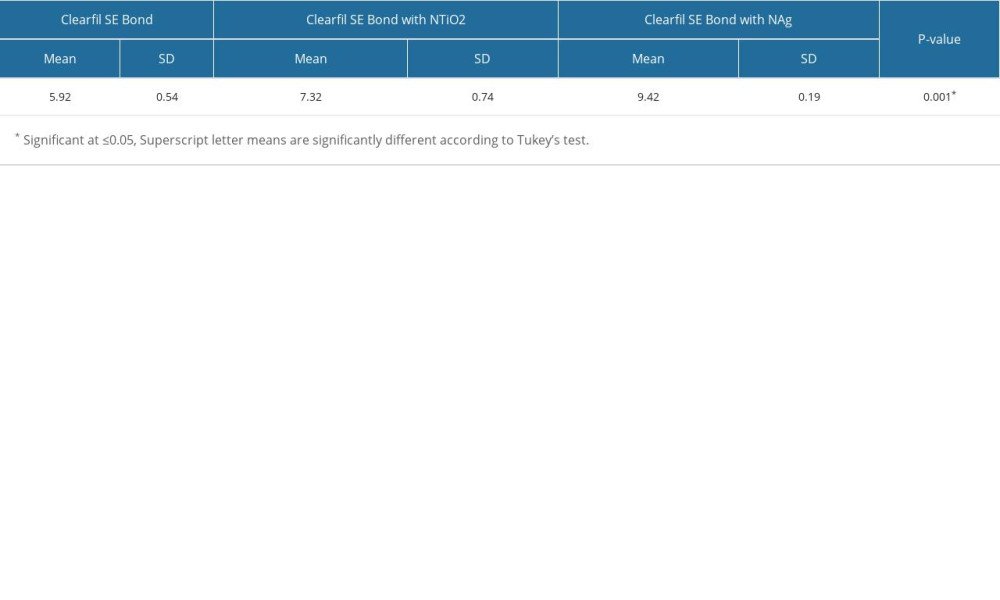 Table 2. Comparison of the mean tensile strengths for samples underwent for thermocycling of tested adhesive systems in MPa.
Table 2. Comparison of the mean tensile strengths for samples underwent for thermocycling of tested adhesive systems in MPa.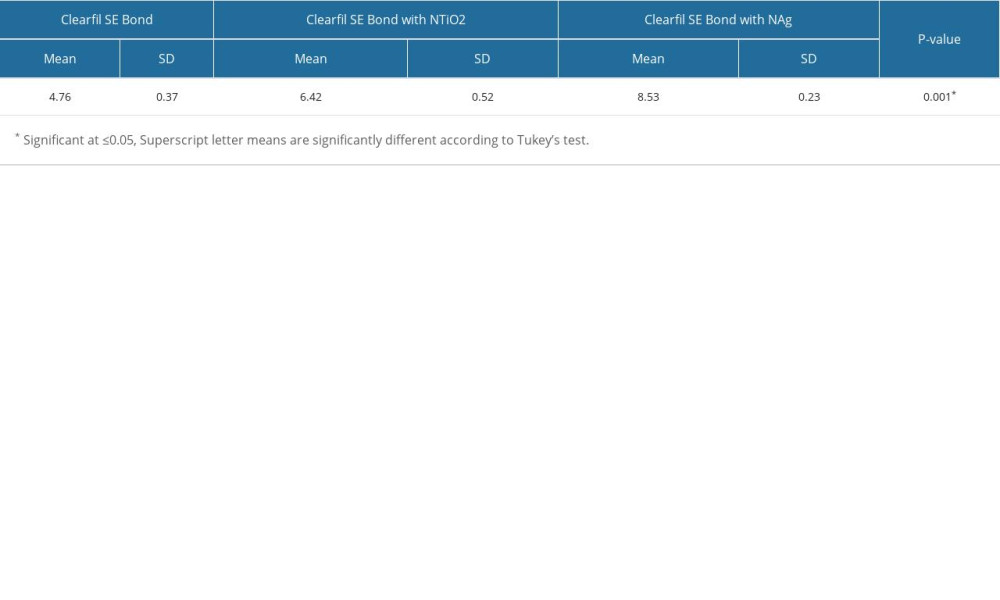 Table 3. Descriptive of the failure types of all tested samples.
Table 3. Descriptive of the failure types of all tested samples.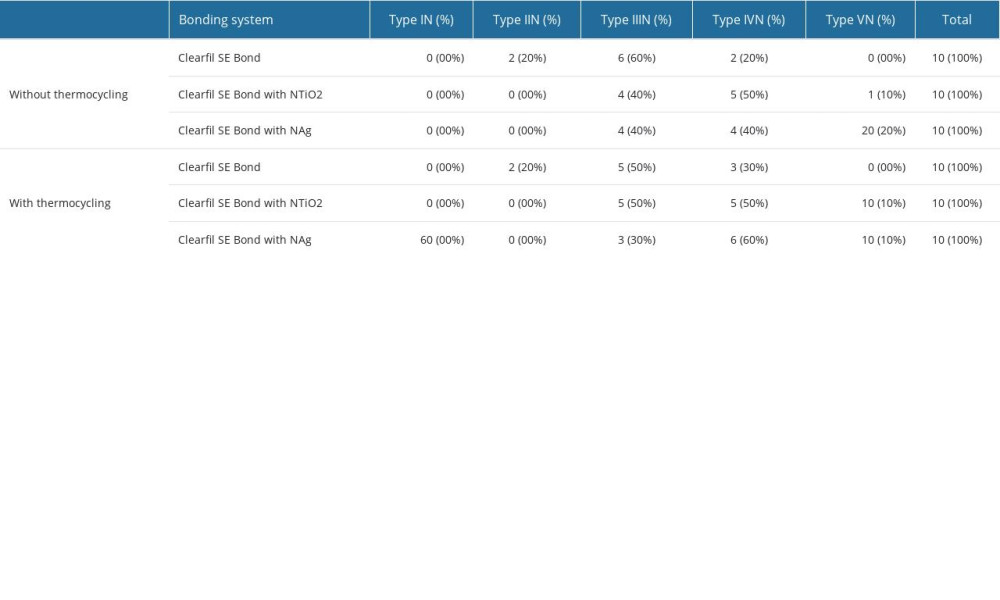
References
1. Perdigao J, Gomes G, Augusto V, The effect of dowel space on the bond strengths of fiber posts: J Prosth Dent, 2007; 16; 154-64
2. Erdemir A, Ari H, Güngüneş H, Belli S, Effect of medications for root canal treatment on bonding to root canal dentin: J Endod, 2004; 30; 113-16
3. Gomez M, Llido B, Rivero A, Rio J, Celemin A, A 10-year retrospective study of the survival rate of teeth restored with metal prefabricated posts versus cast metal posts and cores: J Dent, 2010; 38; 916-20
4. Zarone F, Sorrentino R, Apicella D, Evaluation of the biomechanical behavior of maxillary central incisors restored by means of endo-crowns compared to a natural tooth: A 3D static linear finite elements analysis: Dent Mat J, 2006; 22; 1035-44
5. Rasimick B, Wan J, Musikant B, Deutsch A, A review of failure modes in teeth restored with adhesively luted endodontic dowels: J Prosth, 2010; 19; 639-46
6. Omiri M, Wahadni A, An ex vivo study of the effects of retained coronal dentine on the strength of teeth restored with composite core and different post and core systems: Int Endo J, 2006; 39; 890-99
7. Santos P, Castro C, Silva G, Effects of post system and length on the strain and fracture resistance of root filled bovine teeth: Int Endod J, 2008; 41; 493-501
8. Schwartz R, Adhesive dentistry and endodontics. Part 2: Bonding in the root canal system-the promise and the problems: A review: J Endod, 2006; 32; 1125-34
9. Malyk Y, Kaaden C, Hickel R, Ilie N, Analysis of resin tags formation in root canal dentine: a cross sectional study: Int Endod J, 2010; 43; 47-56
10. Gu X, Mao C, Kern M, Effect of different irrigation on smear layer removal after post space preparation: J Endod, 2009; 35; 583-86
11. Nima G, Makishi P, Fronza BM, Polymerization kinetics, shrinkage stress, and Bond strength to dentin of conventional and self-adhesive resin cements: J Adhes Dent, 2022; 24(1); 355-66
12. Tay F, Loushine R, Lambrechts P, Geometric factors affecting dentin bonding in root canals: A theoretical modeling approach: J Endod, 2005; 31; 584-89
13. Dharma HNC, Jaafar J, Widiastuti N, A review of titanium dioxide (TiO2)-based photocatalyst for oilfield-produced water treatment: Membranes (Basel), 2022; 12(3); 345
14. Younis AB, Milosavljevic V, Fialova T, Synthesis and characterization of TiO2 nanoparticles combined with geraniol and their synergistic antibacterial activity: BMC Microbiol, 2023; 23(1); 207
15. Sodagar A, Kassaee MZ, Pourakbari B, Anti-cariogenic effect of polymethylmethacrylate with in situ generated silver nanoparticles on planktonic and biofilm bacteria: Annals of Biological Research, 2013; 4(8); 7
16. Pant HR, Pandeya DR, Nam KT, Photocatalytic and antibacterial properties of a TiO2/nylon-6 electrospun nanocomposite mat containing silver nanoparticles: J Hazard Mate, 2011; 189; 465-71
17. Wang J, Jiang W, Liang J, Ran S, Influence of silver nanoparticles on the resin-dentin bond strength and antibacterial activity of a self-etch adhesive system: J Prosthet Dent, 2022; 128(6); 1363e1-e10
18. Shafiei F, Memarpour M, Jowkar Z, Effect of silver antibacterial agents on bond strength of fiber posts to root dentin: Brazilian Dental J, 2020; 31; 409-16
19. Cheng L, Weir M, Zhang K, Antibacterial nanocomposite with calcium phosphate and quaternary ammonium: J Dent Res, 2012; 91; 460-66
20. Morones J, Elechiguerra J, Camacho A, The bactericidal effect of silver nanoparticles: Nanotechnology, 2005; 16; 2346-53
21. Alkahtany MF, Extrusion bond strength of glass fiber post to radicular dentin after final irrigation using MTAD, EDTA, Pineapple peel extract, and Riboflavin: Photodiagnosis Photodyn Ther, 2022; 39; 102982
22. Başaran G, Göncü Başaran E, Ayna E, Microtensile bond strength of root canal dentin treated with adhesive and fiber-reinforced post systems: Braz Oral Res, 2019; 33; e027
23. Raafat W, Kheiralla L, Nabil M, Effect of laser surface treatment of glass fiber posts on their bond strength to intra-radicular dentin at different root levels: An in-vitro study: IJADS, 2023; 9(1); 149-55
24. Zhu L, Li Y, Chen YC, Carrera CA, Comparison between two post-dentin bond strength measurement methods: Sci Rep, 2018; 8(1); 2350
25. Al-Ahmari MM, Alzahrani AH, Effect of miswak derivatives on color changes and mechanical properties of polymer-based computer-aided design and computer-aided manufactured (CAD/CAM) dental ceramic materials: Med Sci Monit, 2022; 28; e936892
26. Alves PB, Jurema ALB, Torres CRG, Bond strength evaluation between different glass fiber post systems to restore weakened roots: J Compos Sci, 2022; 6; 252
27. Alves Dos Santos GN, Silva-Sousa YTC, Alonso ALL, Evaluation of the push-out bond strength of an adjustable fiberglass post system to an endodontically treated oval root canal: Dent Mater J, 2023; 42(4); 532-41
28. Bertolini GR, Alves dos Santos GN, Garcia-Paula FW, Impact of the removal of filling material from the post space with ultrasonic insert and magnification with a surgical microscope on the bond strength and adhesive interface of multifilament fiberglass posts onto flat-oval root canals: J Mech Behav Biomed Mater, 2022; 132; 105264
29. Plotino G, Grande N, Bedini R, Flexural properties of endodontic posts and human root dentin: Dent Mat J, 2007; 23; 1129-35
30. Bitter K, Neumann K, Kielbassa A, Effects of pretreatment and thermocycling on bond strength of resin core materials to various fiber-reinforced composite posts: J Adh Dent, 2008; 10; 481-89
31. Aleisa K, Ziad N, Rawda A, Charles J, Effect of luting agents on the tensile bond strength of glass fi ber posts: An in vitro study: J Prosth Dent, 2013; 110; 216-22
32. Naumann M, Sterzenbach G, Rosentritt M, Is adhesive cementation of endodontic posts necessary?: J Endod, 2008; 34; 1006-10
33. Bonfante G, Kaizer O, Pegoraro L, Valle A, Tensile bond strength of glass fi ber posts luted with different cements: Braz Oral Res, 2007; 21; 159-64
34. Salameh Z, Sorrentino R, Papacchini F, Fracture resistance and failure patterns of endodontically treated mandibular molars restored using resin composite with or without translucent glass fi ber posts: J Endod, 2006; 32; 752-55
35. Marshall S, Bayne S, Baier R, A review of adhesion science: Dent Mater, 2010; 26; 11-16
36. Tay F, Pashley D, Monoblocks in root canals. A hypothetical or a tangible goal: J Endod, 2007; 33; 391-98
37. Rene G, Rogelio J, Rosalía C, Mechanical, antibacterial and bond strength properties of nano-titanium-enriched glass ionomer cement: J Appl Oral Sci, 2015; 23; 321-28
38. Al-Saleh S, Alateeq A, Alshaya AH, Influence of TiO2 and ZrO2 nanoparticles on adhesive Bond strength and viscosity of dentin polymer: A physical and chemical evaluation: Polymers (Basel), 2021; 13(21); 3794
39. Sun J, Petersen EJ, Watson SS, Biophysical characterization of functionalized titania nanoparticles and their application in dental adhesives: Acta Biomater, 2017; 53; 585-97
40. Esteban Florez FL, Kraemer H, Hiers RD, Sorption, solubility and cytotoxicity of novel antibacterial nanofilled dental adhesive resins: Sci Rep, 2020; 10; 13503
41. Cheng Y, Zeiger D, Howarter J, In situ formation of silver nanoparticles in photo cross linking polymers: J Bio Mat Res, 2011; 97; 124-31
42. Cheng L, Zhang K, Melo M, Anti-biofi lm dentin primer with quaternary ammonium and silver nanoparticles: J Dent Res, 2012; 91; 598-604
43. Chou C, Hsu S, Chang H, Tseng S, Lin H, Enhanced thermal and mechanical properties and biostability of polyurethane containing silver nanoparticles: Polym Degrad Stab, 2006; 91; 1017-24
44. Fatemeh K, Mohammad Javad M, Samaneh K, The effect of silver nanoparticles on composite shear bond strength to dentin with different adhesion protocols: J Appl Oral Sci, 2017; 25; 367-73
45. Klein-Junior CA, Zimmer R, Coelho-de-Souza FH, Influence of the incorporation of titanium dioxide nanofibers net on bond strength and morphology of a total etching adhesive system: J Clin Exp Dent, 2023; 15(9); e714-e19
46. Jowkar Z, Fattah Z, Ghanbarian S, Shafiei F, The effects of silver, zinc oxide, and titanium dioxide nanoparticles used as dentin pretreatments on the microshear Bond strength of a conventional glass ionomer cement to dentin: Int J Nanomedicine, 2020; 15; 4755-62
47. Al-Saleh S, Vohra F, Alateeq A, Strength of fiber posts with experimental TiO2 and ZrO2 particle bonding – an SEM, EDX, rheometric and push-out strength study: Coatings, 2022; 12; 1176
48. Moussaoui H, El Mesbahi N, Nadour M, Bennani A, Effect of different final irrigants applied on intraradicular dentin on the Bond strength to fiber post: A review: Open Access Library J, 2023; 10; e10309
49. Moreno-Sánchez PL, Ramírez-Álvarez M, Ayala-Ham AdR, Dental surface conditioning techniques to increase the micromechanical retention to fiberglass posts: A literature review: Appl Sci, 2023; 13; 8083
50. Silva AM, Alencar CM, Jassé FFA, Effect of post-space irrigation with acid solutions on Bond strength and dentin penetrability using a self-adhesive cementation system: J Clinic Experimental Dent, 2021; 13; e564-e71
51. Sheikh GM, Khoroushi M, Feiz A, Effect of calcium hypochlorite and sodium hypochlorite as root canal irrigants on push-out Bond strength of fiber post cemented with etch-and-rinse resin cement: An in vitro study: Front Dent, 2021; 18 Article No. 18
Figures
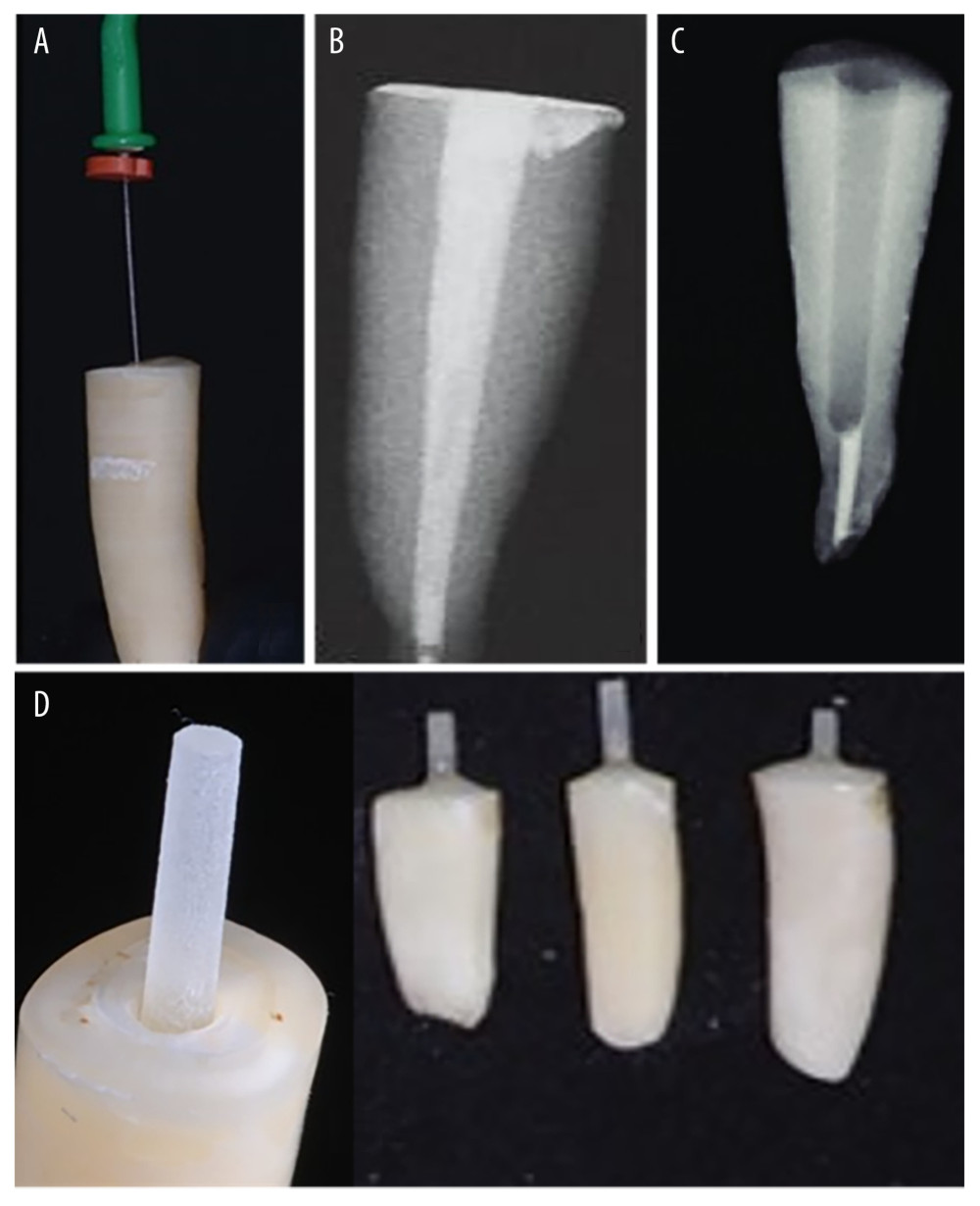 Figure 1. During endodontic treatment, (A) working length, (B) filling the canal with gutta percha, (C) post space preparation, and (D) after cementation of posts.
Figure 1. During endodontic treatment, (A) working length, (B) filling the canal with gutta percha, (C) post space preparation, and (D) after cementation of posts.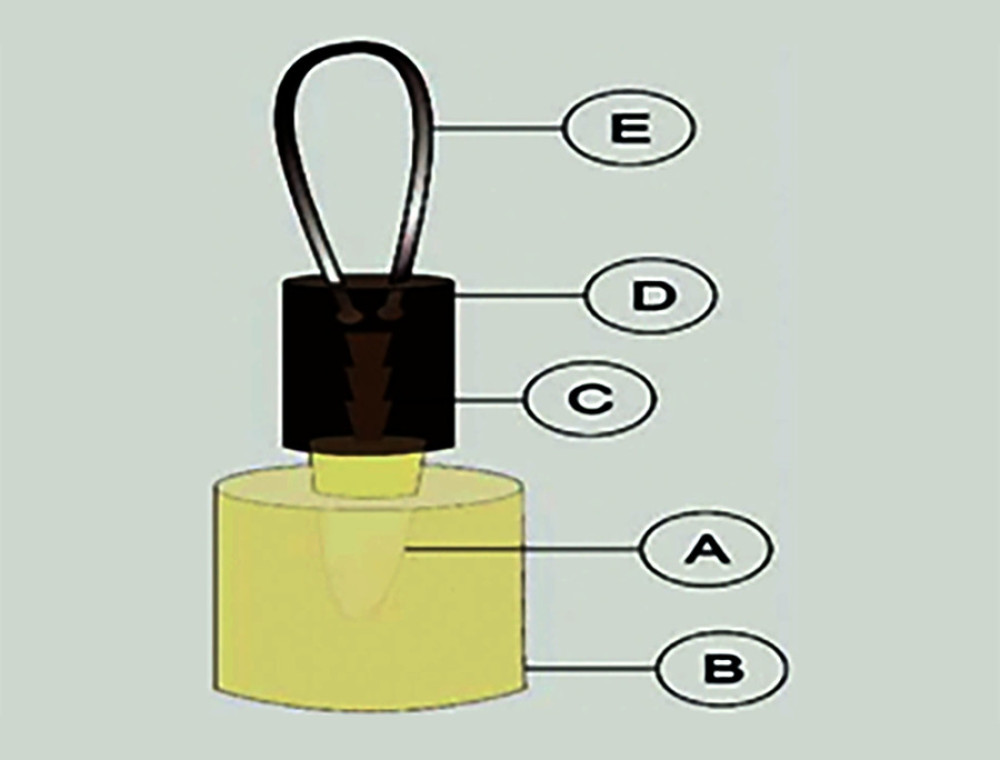 Figure 2. Sample ready for tensile bond strength test, A) human root; B) acrylic resin; C) glass fiber post; D) acrylic resin cylinder; E) metallic loop.
Figure 2. Sample ready for tensile bond strength test, A) human root; B) acrylic resin; C) glass fiber post; D) acrylic resin cylinder; E) metallic loop.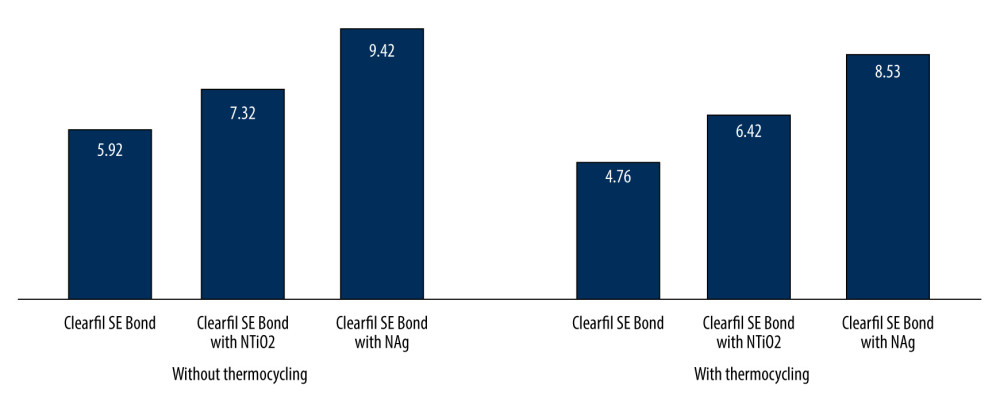 Figure 3. Bar chart of mean tensile bond strength in (MPa) of the tested bond adhesive system groups with and without thermocycling.
Figure 3. Bar chart of mean tensile bond strength in (MPa) of the tested bond adhesive system groups with and without thermocycling.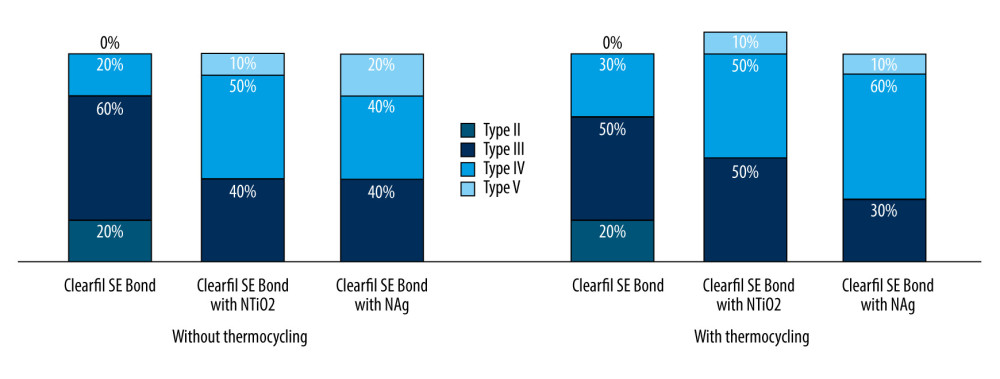 Figure 4. Percentage of the failure pattern of the tested bond adhesive system groups with and without thermocycling.
Figure 4. Percentage of the failure pattern of the tested bond adhesive system groups with and without thermocycling. Tables
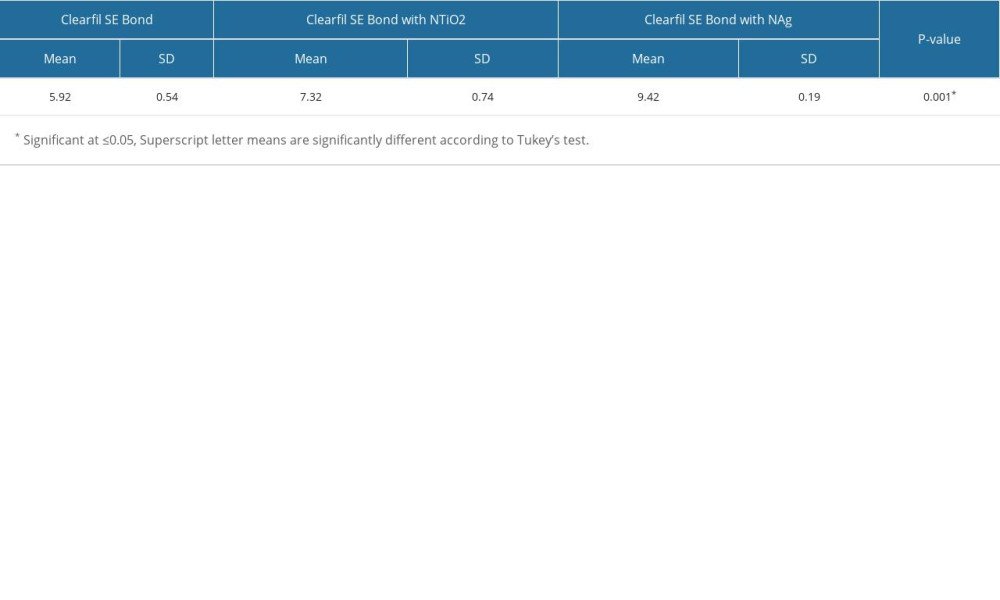 Table 1. Comparison of the mean tensile strengths for non-thermocycling samples of tested adhesive systems in MPa.
Table 1. Comparison of the mean tensile strengths for non-thermocycling samples of tested adhesive systems in MPa.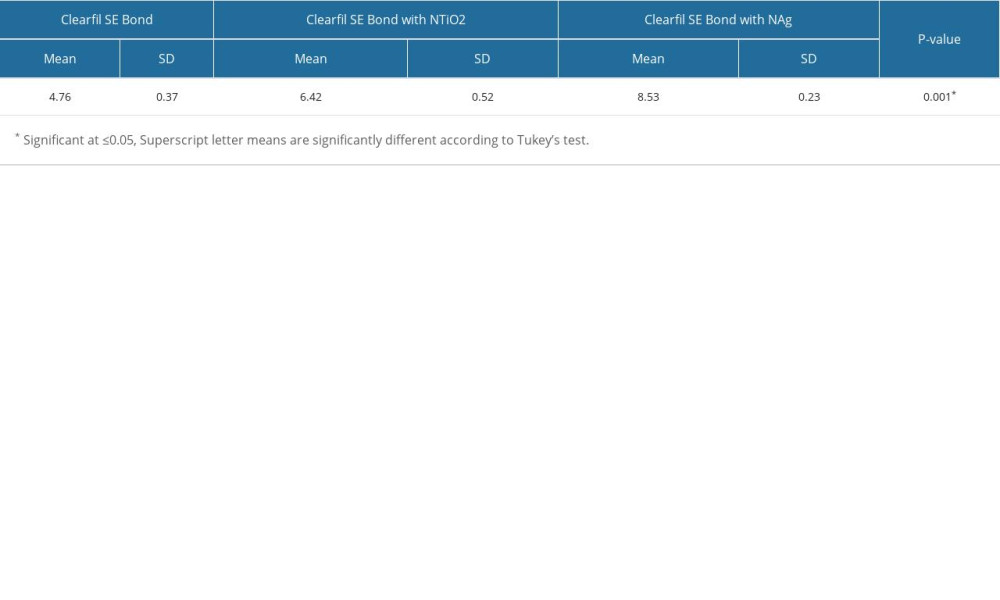 Table 2. Comparison of the mean tensile strengths for samples underwent for thermocycling of tested adhesive systems in MPa.
Table 2. Comparison of the mean tensile strengths for samples underwent for thermocycling of tested adhesive systems in MPa.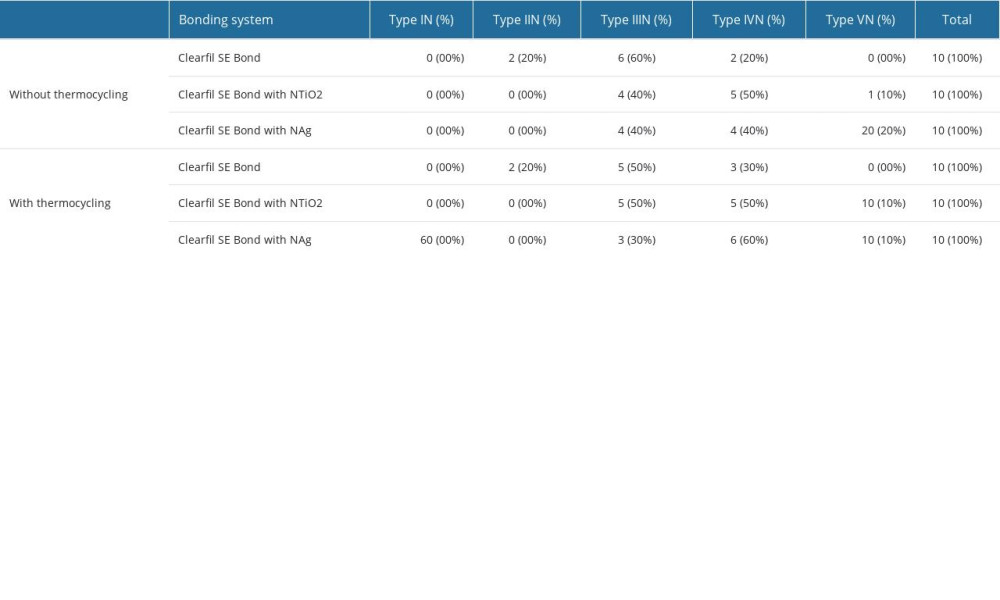 Table 3. Descriptive of the failure types of all tested samples.
Table 3. Descriptive of the failure types of all tested samples.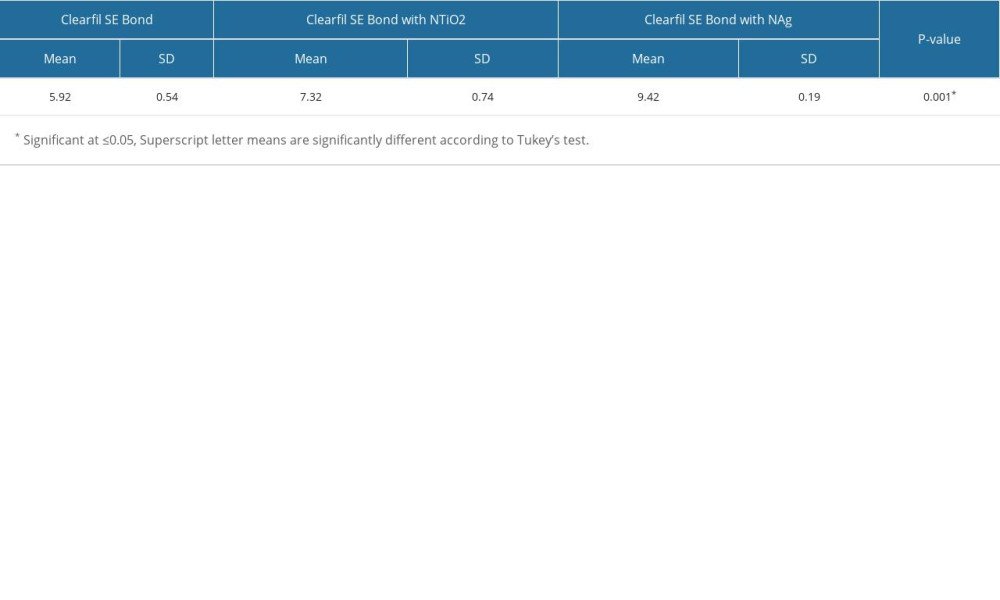 Table 1. Comparison of the mean tensile strengths for non-thermocycling samples of tested adhesive systems in MPa.
Table 1. Comparison of the mean tensile strengths for non-thermocycling samples of tested adhesive systems in MPa.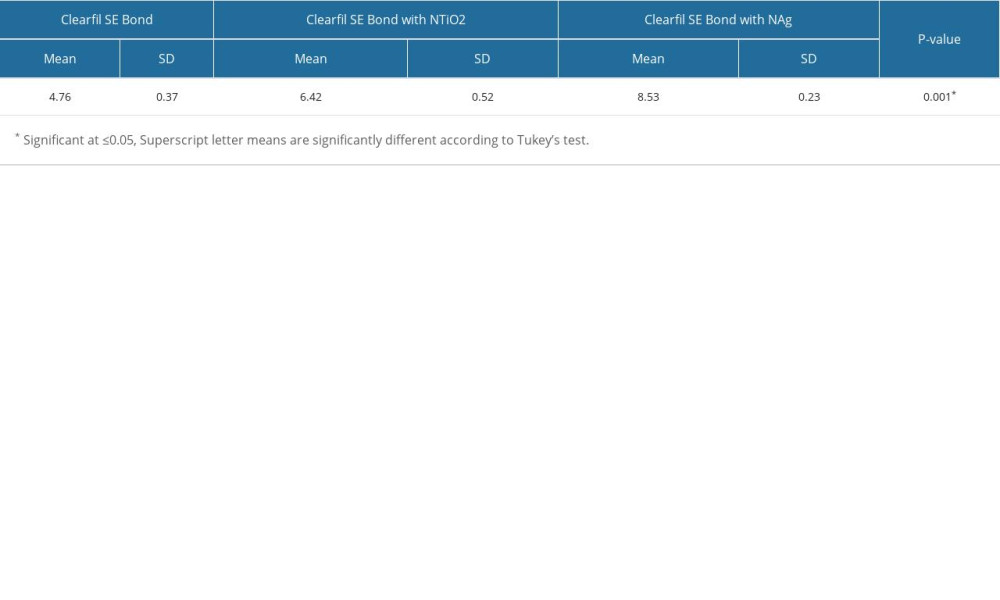 Table 2. Comparison of the mean tensile strengths for samples underwent for thermocycling of tested adhesive systems in MPa.
Table 2. Comparison of the mean tensile strengths for samples underwent for thermocycling of tested adhesive systems in MPa.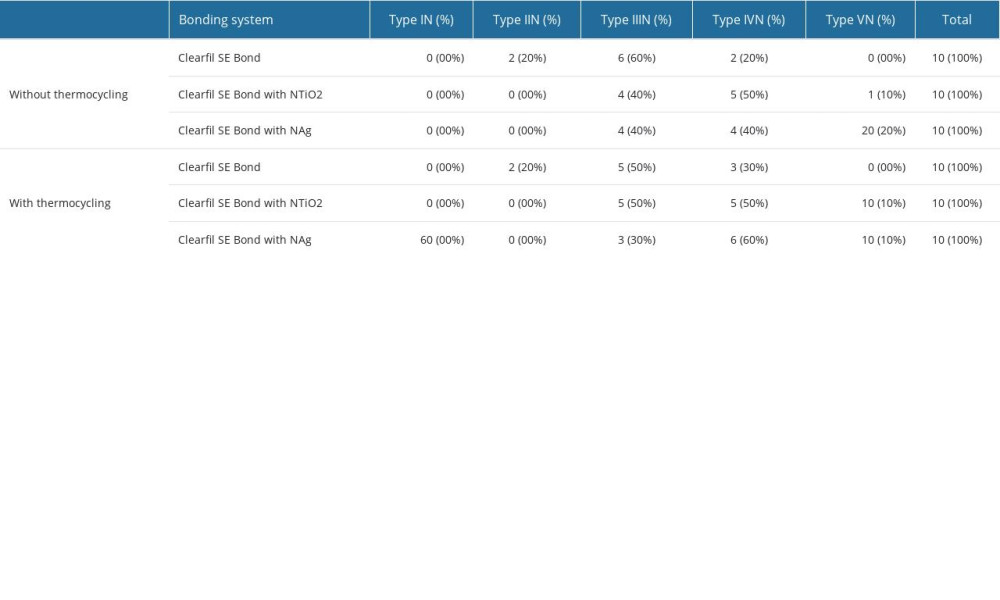 Table 3. Descriptive of the failure types of all tested samples.
Table 3. Descriptive of the failure types of all tested samples. In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








