03 December 2020: Clinical Research
Development and Validation of Predictive Models for Vaginal Birth After Cesarean Delivery in China
Shilei Bi1ACDEF, Lizi Zhang2ACDEF, Jingsi Chen134AC, Lijun Huang1BF, Shanshan Zeng1BF, Jinping Jia5B, Suiwen Wen6B, Yinli Cao7B, Shaoshuai Wang8B, Xiaoyan Xu8B, Feng Ling8B, Xianlan Zhao9B, Yangyu Zhao10B, Qiying Zhu11B, Hongbo Qi12B, Lanzhen Zhang13B, Hongtian Li14CD, Lili Du134ACEG*, Zhijian Wang2AG, Dunjin Chen134AGDOI: 10.12659/MSM.927681
Med Sci Monit 2020; 26:e927681
Abstract
BACKGROUND: The rate of delivery by cesarean section is rising in China, where vaginal birth after cesarean (VBAC) is in its early stages. There are no validated screening tools to predict VBAC success in China. The objective of this study was to identify the variables predicting the likelihood of successful VBAC to create a predictive model.
MATERIAL AND METHODS: This multicenter, retrospective study included 1013 women at ≥28 gestational weeks with a vertex singleton gestation and 1 prior low-transverse cesarean from January 2017 to December 2017 in 11 public tertiary hospitals within 7 provinces of China. Two multivariable logistic regression models were developed: (1) at a first-trimester visit and (2) at the pre-labor admission to hospital. The models were evaluated with the area under the receiver operating characteristic curve (AUC) and internally validated using k-fold cross-validation. The pre-labor model was calibrated and a graphic nomogram and clinical impact curve were created.
RESULTS: A total of 87.3% (884/1013) of women had successful VBAC, and 12.7% (129/1013) underwent unplanned cesarean delivery after a failed trial of labor. The AUC of the first-trimester model was 0.661 (95% confidence interval [CI]: 0.61–0.712), which increased to 0.758 (95% CI: 0.715–0.801) in the pre-labor model. The pre-labor model showed good internal validity, with AUC 0.743 (95% CI: 0.694–0.785), and was well calibrated.
CONCLUSIONS: VBAC provides women the chance to experience a vaginal delivery. Using a pre-labor model to predict successful VBAC is feasible and may help choose mode of birth and contribute to a reduction in cesarean delivery rate.
Keywords: Cesarean Section, Repeat, Pregnancy Complications, Trial of Labor, Vaginal Birth after Cesarean, Calibration, Labor, Obstetric, Models, Biological, nomograms, Pregnancy, ROC Curve, Reproducibility of Results
Background
The rate of delivery by cesarean section has increased worldwide. From 1970 to 2016, the cesarean section rate in the United States increased from 5% to 31.9% [1,2]. In Germany, studies reported that the cesarean section rate increased from 25.3% in 2002 to 33% in 2012 [3]. In China, the cesarean rate increased from 28.8% in 2008 to 34.9% in 2014 [4]. These rates are far from the World Health Organization (WHO) recommended cesarean section rate of 10% to 15% of total births [5]. The increase in cesarean rate is due partly to an increased rate of repeat cesarean delivery (RCD). Currently, the high cesarean section rate and the complications involved with cesarean delivery are serious public health problems, and it is crucial to reduce both. The promotion of vaginal birth after cesarean (VBAC) is one way to reduce the overall number of cesarean deliveries worldwide.
In 1982, the American College of Obstetrics and Gynecology recommended VBAC as a safe and acceptable birthing option [6]. In 1985, the National Consensus Conference on Aspects of Cesarean Birth in Canada recommended that women with no indication for cesarean section be offered a trial of labor [7]. Many studies have shown that, with strict indications for VBAC, its success rate could reach 60% to 80% [2,3]. However, from 1996 to 2010, the rate of VBAC decreased from 28% to 8%, which was thought to be largely related to the high legal risks for obstetricians and midwives when offering VBAC [8].
The National Institutes of Health of the United States [6] and the American Association of Obstetricians and Gynecologists [9] encouraged and guaranteed support for pregnant women with cesarean section history to attempt trial of labor after cesarean delivery (TOLAC) when conditions permit [2]. For women with a previous cesarean delivery (CD), the decision to proceed with RCD or TOLAC is based on multiple factors. The assessment of individual risks and the likelihood of VBAC success is, therefore, critical in identifying appropriate candidates for TOLAC [10]. There are several published models available to predict the probability of a successful VBAC in women who undergo TOLAC [11–13].
In 2016, the enactment of the 2-child policy in China was expected to increase the rate of cesarean section because of RCDs [14], and women with cesarean section history were facing the difficult decision of choosing delivery modes. China was at the early stage of dealing with TOLAC. There were no large multicenter studies of VBAC screening tools to provide a consistent and validated ability to predict the success of VBAC in China. Although some VBAC nomograms and prediction models have been developed in other countries, their accuracy decreased when applied to different datasets [15–17], which may be due in part to geographic diversity or to the models being calibrated to lower predicted probabilities of success [11].
The aim of this study was to analyze and identify variables affecting VBAC success and to develop 2 predictive tools for VBAC, the first for use during the first trimester and the second at the pre-labor hospital admission, using multicenter, retrospective clinical data from hospitals in China. Our goal is to help obstetricians make accurate clinical treatment decisions and decrease the high rate of RCD in China.
Material and Methods
STATISTICS ANALYSIS:
Statistical analysis was performed using R software (version 3.6.1) and IBM SPSS v25.0. Missing values were imputed using the Random Forests algorithm. Quantitative data were examined for normal distribution, and normally distributed variables were represented as mean±SD, and the
Results
The study included 11 958 pregnant women with uterine scarring from cesarean section who delivered again. Among these women, 91.5% (10 945/11 958) opted for RCDs and 8.5% (1013/11 958) opted for TOLAC. From the 1013 women attempting a TOLAC, 87.3% (884/1013) achieved a vaginal delivery, which included 854 cases of normal vaginal delivery and 30 cases of instrumental vaginal delivery, and 12.7% (129/1013) underwent an unplanned cesarean delivery (Figure 1). Table 1 shows the maternal and neonatal outcomes in the unplanned cesarean and successful vaginal delivery groups. The median blood loss in the unplanned cesarean delivery group was higher than that in the successful vaginal delivery group (395 mL
Table 2 shows the characteristics of the pregnant women. There were 17 variables collected at the first-trimester visit and an additional 28 variables collected at the hospital pre-labor and delivery visit. Table 3 summarizes the most significant variables included in the 2 simple models at these 2 timepoints.
Figure 2 shows the receiver operating characteristic curves of the 4 models. At each timepoint (first-trimester and pre-labor visits), 2 models were established: (1) a full model using all variables and (2) a simple model using independent risk factors. At the first-trimester visit, the AUC of the full model was 0.672 (95% confidence interval [CI]: 0.622–0.723) and the AUC of the simple model was 0.661 (95% CI: 0.61–0.712). The full and simple models achieved 5-fold cross-validation mean AUCs of 0.607 (95% CI: 0.546–0.659) and 0.652 (95% CI: 0.599–0.703), respectively. At the pre-labor visit, the AUCs of the full and simple models were 0.8 (95% CI: 0.763–0.838) and 0.758 (95% CI: 0.715–0.801), respectively; and the full and simple models achieved 5-fold cross-validation mean AUCs of 0.703 (95% CI: 0.653–0.752) and 0.743 (95% CI: 0.694–0.785), respectively. The calibration curve of the pre-labor model for the probability of vaginal birth demonstrated agreement between prediction and observation (Figure 3).
In Figure 4, the pre-labor model is presented as a graphical calculator (nomogram). The clinical impact curve for the pre-labor model is presented in Figure 5. Of 1000 patients, the red solid line shows the total number who were deemed high risk for each risk threshold. The blue dashed line shows how many of those were true positives (cases).
Discussion
In this multicenter retrospective study, the proportion of successful deliveries by TOLAC was 87.3% (884/1013). The prediction of the simple model with 5 variables at the first-trimester visit was limited, with an AUC of 0.661 (95% CI: 0.61–0.712). The pre-labor model increased the prediction accuracy, with an AUC of 0.758 (95% CI: 0.715–0.801) and a validation curve that adhered more closely to the ideal validation line from the addition of variables before labor. Logistic multivariate analysis indicated that gravity, parity, number of spontaneous abortions, source of patient referral, premature rupture of membrane, antepartum hemorrhage, placenta accrete spectrum, preeclampsia, neonatal weight, and oxytocin induction influenced the success of VBAC. The total incidence rate of uterine rupture was 0.39% (4/1013). There were no maternal deaths in the 2 groups and there was 1 neonatal death in the cesarean group.
Although China is in the early stages of dealing with TOLAC, the success rate of VBAC in China found in the present study should help increase the frequency with which TOLAC is offered. Our results are also comparable with other reports. Fonseca et al. in Columbia reported that, of 203 women who had a TOLAC, 174 (85.7%) had a successful delivery [6]. Haumonte et al. reported a 65% (240/367) VBAC success rate in France [20]. Xu et al. reported that 85.2% (456/535) of women had successful VBAC in China [21]. Lipschuetz et al. reported the success rate of VBAC was 77.4% (5787/7473) in a study in Israel [22]. As these studies show, VBAC is feasible for most pregnant women, even in China where there is a high rate of CD. Women with a previous CD should be recommended TOLAC to reduce the rate and complications of RCD.
At present, many researchers have collected clinical data to construct predictive models that can provide physicians with a useful tool to accurately predict the success of VBAC for a given woman. Grobman et al. developed a nomogram with an AUC of 0.754 (95% CI: 0.742–0.766) from the first prenatal check-up [21], which increased to 0.774 (95% CI: 0.764–0.784) when the features at the delivery unit were added. Lipschuetz et al. used machine learning to build a tool that had an AUC of 0.745 (95% CI: 0.728–0.762) in a first-trimester model, which increased to an AUC of 0.793 (95% CI: 0.778–0.808) in the pre-labor model [22]. Some researchers reported that the accuracy of the predictive models decreased when they were applied to other datasets [15,23,24], which could have been due in part to geographic diversity or that the model had been calibrated to lower predicted probabilities of success [11]. Therefore, in the present study, it was necessary to develop predictive models using clinical data collected from pregnant women in China.
To the best of our knowledge, this was the first multicenter retrospective study using screening tools to predict the success of VBAC in China. Our results agreed with previously published models in which adding variables that were available before delivery increased the predictive accuracy of VBAC. It is worth noting that some of the predictors of VBAC in the present study had already been described in the literature. The presence of preeclampsia [20], induction of labor [20], advanced gestational age [12,25], and increased fetal weight [25] decreased the chance of VBAC. Parity [12] and no maternal complications [26] increased the success of VBAC. Contrary to the results of Denham et al. [26], we found that previous antepartum hemorrhage was associated with more VBAC occurrence. In our study, we found that some new variables, including less gravity and more spontaneous abortions, were related to the success of VBAC, while referral patients complicated with premature rupture of membranes or placenta accrete spectrum were not conducive to vaginal delivery. These results should be investigated in more extensive, prospective trials. Whether there are other factors influencing the success of VBAC also requires further study.
Although the Bishop score was commonly used as a discriminatory tool to predict the success of VBAC in some published models [13,22], this implied that the opportunity of VBAC may have been offered to women with a high Bishop score. Many women with unfavorable cervices chose RCD directly. For those women with unfavorable cervices, induction of labor may improve the cervical condition. The American College of Obstetrics and Gynecology Practice Bulletin (Number 205) recommends that the induction of labor remain an option for women undergoing TOLAC [2]. In this study, we used oxytocin induction and a mechanical method of cervical ripening for women with unfavorable cervices intending to TOLAC. Our pre-labor model considered numerous variables in addition to cervical status, given the large number of women with unfavorable cervices having VBAC after induction of labor.
Our study had several strengths. The study was based on the multicenter database from 11 public tertiary hospitals, including 7 provinces, municipalities, and autonomous regions in China in 2017, which effectively avoided the selection bias of single-center and small-sample studies. Therefore, to some extent, the data could be generalized to more heterogeneous populations. The model’s ease of use by obstetricians is enhanced by its representation as a graphical nomogram, and its validity was tested with results showing moderate discrimination and good calibration. The clinical impact curves visually show the estimated numbers of pregnant women who were deemed vaginal birth and true positives with different threshold probabilities.
However, our study had some limitations. First, this is a retrospective study. Second, data from different centers were not always ideal and complete. Therefore, we excluded cases with important missing data. Other missing values were imputed using the Random Forests algorithm. More complete data may provide more accurate outcomes.
Conclusions
In conclusion, VBAC provides a chance for women to experience a vaginal delivery after CD. Additionally, using a pre-labor model to predict successful VBAC by comprehensively assessing the previous and current pregnancy and fetal features is feasible. The prediction nomogram based on gravity, parity, number of spontaneous abortions, source of patient referral, premature rupture of membranes, antepartum hemorrhage, placenta accrete spectrum, preeclampsia, neonatal weight, and oxytocin induction could help obstetricians and pregnant women in the decision-making process about the mode of birth after CD and can reduce of the rate of RCD.
Figures
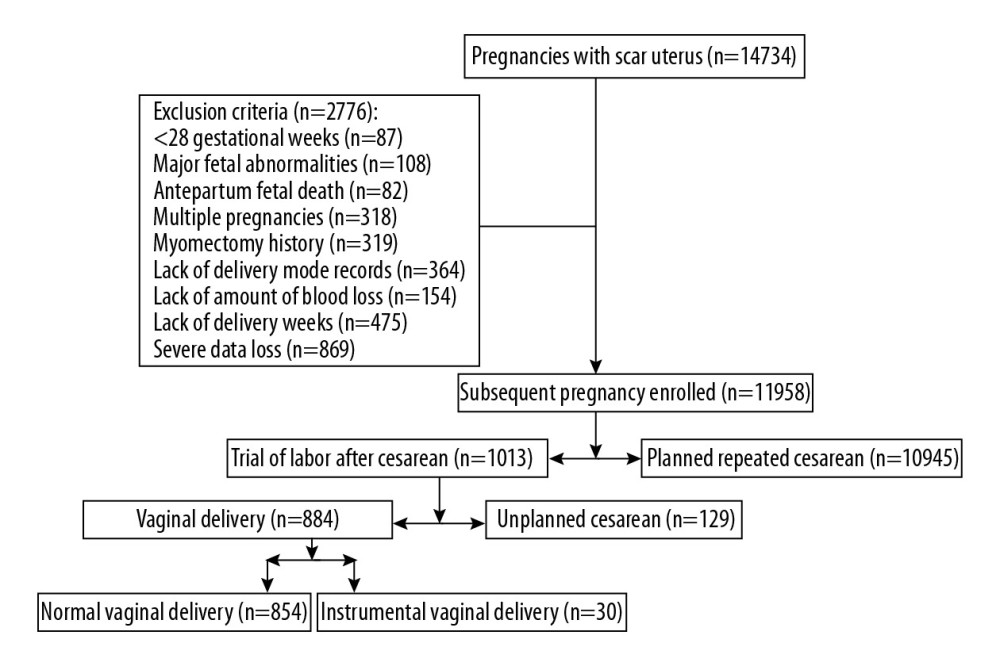 Figure 1. Flow diagram of the patients’ enrollment process.
Figure 1. Flow diagram of the patients’ enrollment process. 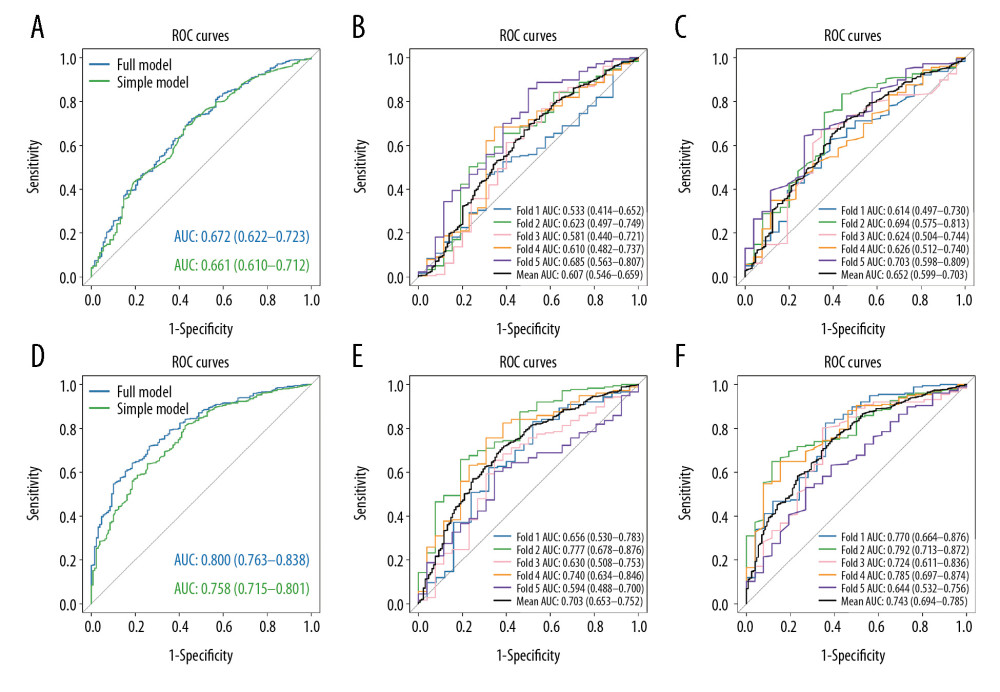 Figure 2. The receiver operating characteristic (ROC) curves of the 4 models. The first trimester period: (A–C); 5-fold cross validation of full model; 5-fold cross validation of first trimester model. The pre-labor period: (D–F); 5-fold cross validation of full model; 5-fold cross validation of pre-labor model.
Figure 2. The receiver operating characteristic (ROC) curves of the 4 models. The first trimester period: (A–C); 5-fold cross validation of full model; 5-fold cross validation of first trimester model. The pre-labor period: (D–F); 5-fold cross validation of full model; 5-fold cross validation of pre-labor model. 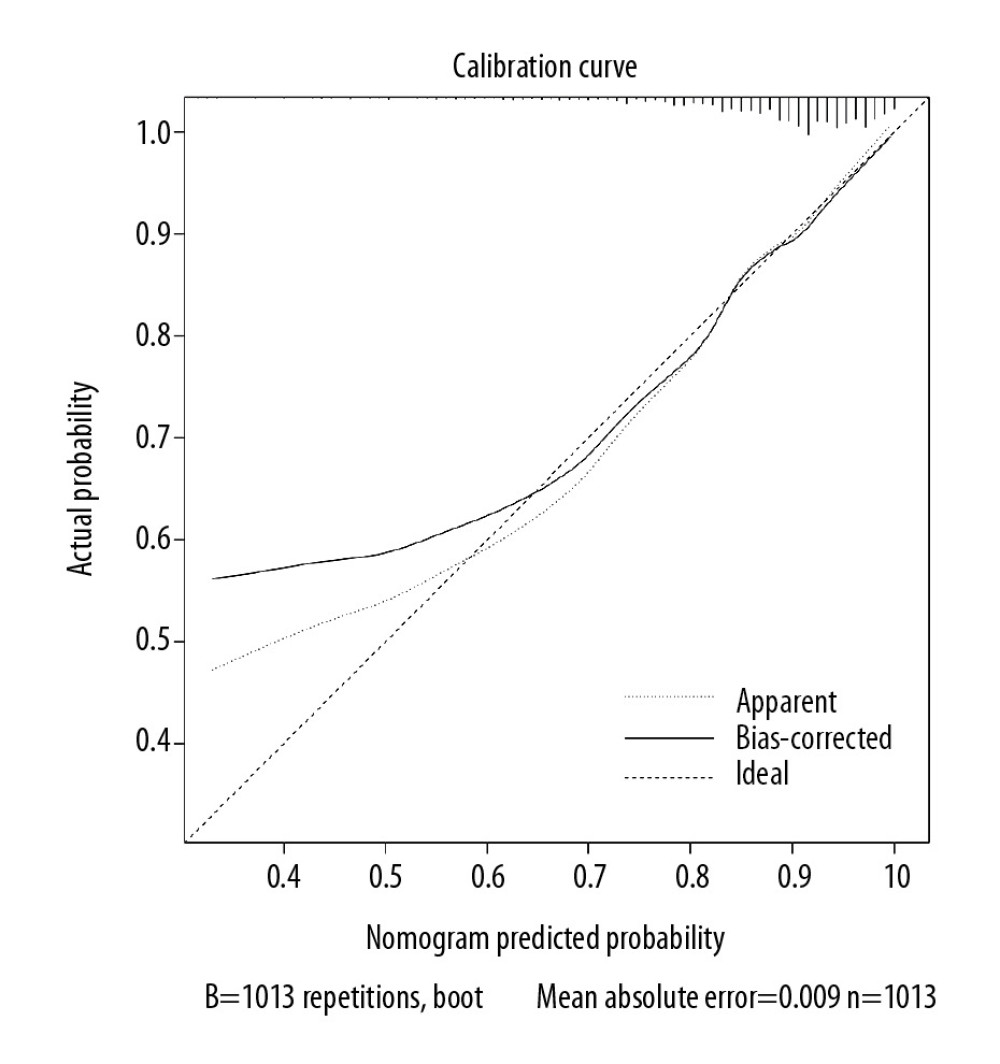 Figure 3. The calibration curve of the pre-labor model.
Figure 3. The calibration curve of the pre-labor model. 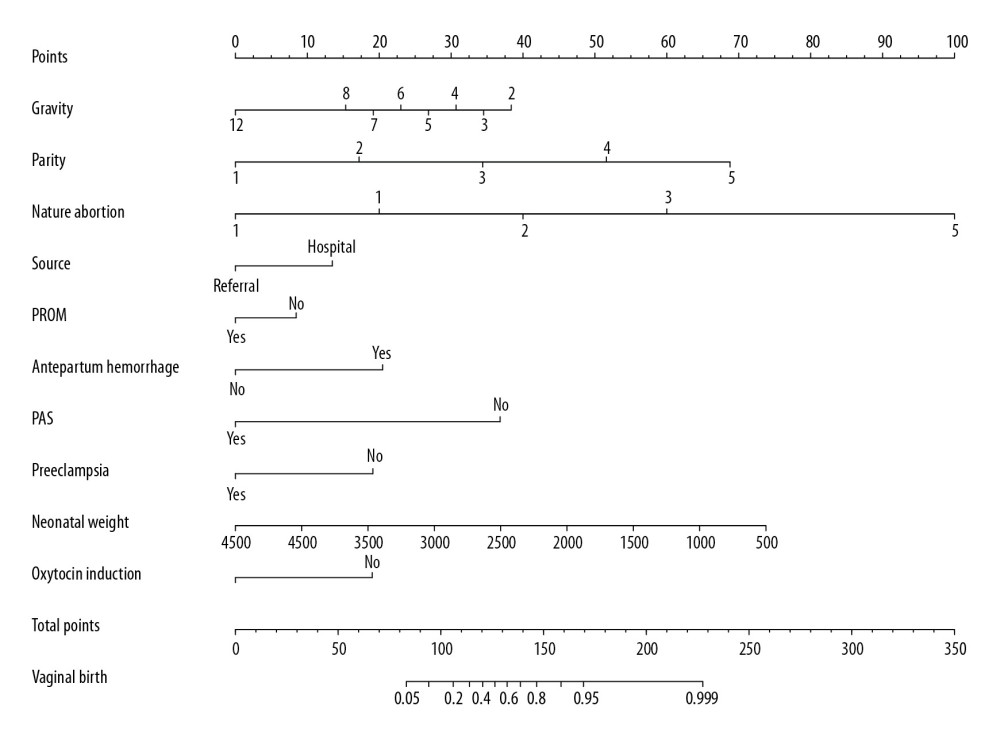 Figure 4. The nomogram of the pre-labor model. The nomogram converts each risk predictor into a 0 to 100 scale that is proportional to the derived adjusted log odds. These points are added across predictors to derive the „total points”, which are converted to predict the probabilities of vaginal birth.
Figure 4. The nomogram of the pre-labor model. The nomogram converts each risk predictor into a 0 to 100 scale that is proportional to the derived adjusted log odds. These points are added across predictors to derive the „total points”, which are converted to predict the probabilities of vaginal birth. 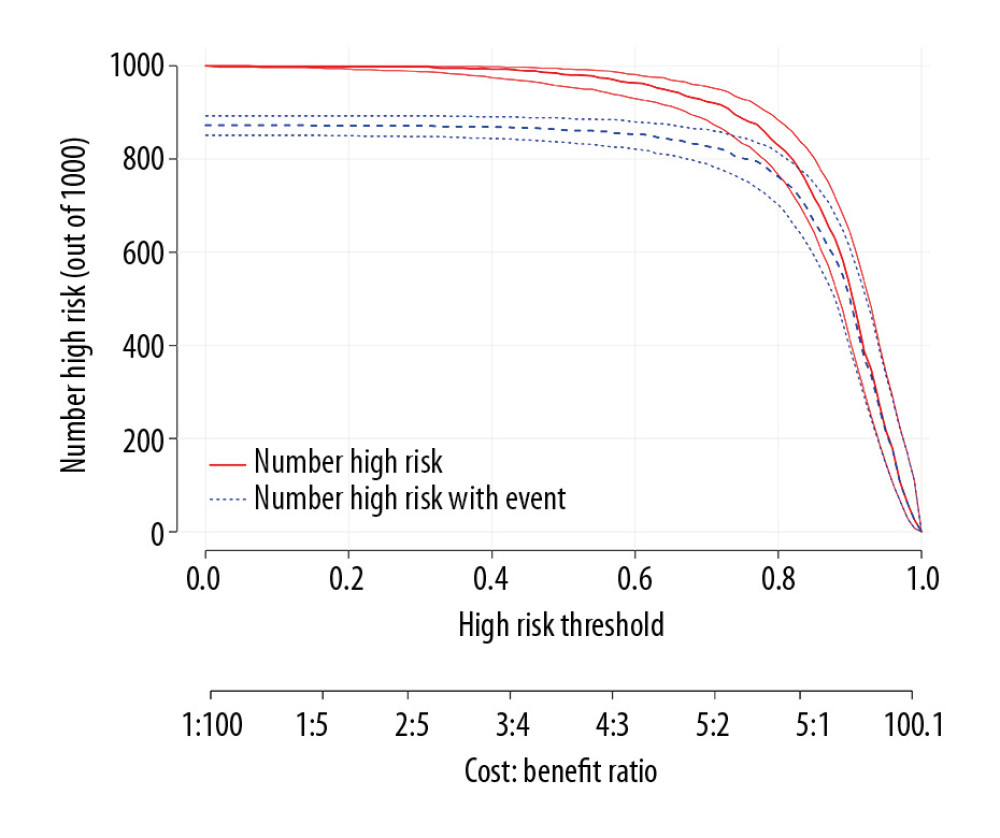 Figure 5. The clinical impact curve for the pre-labor model. Of 1000 patients, the red solid line shows the total number who would be deemed high risk for each risk threshold. The blue dashed line shows how many of those would be true positives (cases).
Figure 5. The clinical impact curve for the pre-labor model. Of 1000 patients, the red solid line shows the total number who would be deemed high risk for each risk threshold. The blue dashed line shows how many of those would be true positives (cases). References
1. Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Births final data for 2018: Natl Vital Stat Rep, 2019; 68; 1-47
2. , american college of obstetrics and gynecology practice bulletin no. 205 summary: vaginal birth after cesarean delivery: Obstet Gynecol, 2019; 133; 393-95
3. Beckmann L, Dorin L, Metzing S, Hellmers CZ, Vaginal birth after cesarean section in out-of-hospital settings: A literature review: Geburtshilfe Neonatol, 2014; 218; 195-202
4. Li HT, Luo S, Trasande L, Geographic variations and temporal trends in cesarean delivery rates in China, 2008–2014: JAMA, 2017; 317; 69-76
5. World Health Organization, Appropriate technology for birth: Lancet, 1985; 2; 436-37
6. Fonseca JE, Rodriguez JL, Maya Salazar D, Validation of a predictive model for successful vaginal birth after cesarean section: Colomb Med (Cali), 2019; 50; 13-21
7. , Indications for cesarean section: Final statement of the panel of the National Consensus Conference on Aspects of Cesarean Birth: CMAJ, 1986; 134; 1348-52
8. Cox KJ, Providers’ perspectives on the vaginal birth after cesarean guidelines in Florida, United States: A qualitative study: BMC Pregnancy Childbirth, 2011; 12; 72
9. , American College of Obstetrics and Gynecology Practice Bulletin No. 205: Vaginal birth after cesarean delivery: Obstet Gynecol, 2019; 133; e110-27
10. , American College of Obstetrics and Gynecology Practice Bulletin No. 115: Vaginal birth after previous cesarean delivery: Obstet Gynecol, 2010; 116; e450-63
11. Harris BS, Heine RP, Park J, Are prediction models for vaginal birth after cesarean accurate?: Am J Obstet Gynecol, 2019; 220; 492.e1-7
12. Alavifard S, Meier K, Shulman Y, Derivation and validation of a model predicting the likelihood of vaginal birth following labour induction: BMC Pregnancy Childbirth, 2019; 19; 130
13. Li YX, Bai Z, Long DJ, Predicting the success of vaginal birth after caesarean delivery: A retrospective cohort study in China: BMJ Open, 2019; 9; e027807
14. Zeng Y, Hesketh T, The effects of China’s universal two-child policy: Lancet, 2016; 388; 1930-38
15. Annessi E, Del Giovane C, Magnani L, A modified prediction model for VBAC, in a European population: J Matern Fetal Neonatal Med, 2016; 29; 435-39
16. Mone F, Harrity C, Mackie A, Vaginal birth after caesarean section prediction models: A UK comparative observational study: Eur J Obstet Gynecol Reprod Biol, 2015; 193; 136-39
17. Xie X, Beihua K, Duan T, Obstetrics and gynecology: Manegement of labor and delivery, 2018; 171-77, People’s Medical Publishing House
18. Brown MA, Magee LA, Kenny LC, Hypertensive disorders of pregnancy: ISSHP classification, diagnosis, and management recommendations for international practice: Pregnancy Hypertens, 2018; 13; 291-310
19. Xie X, Beihua K, Duan T, Obstetrics and gynecology: Abnormal uterine action, 2018; 181-84, People’s Medical Publishing House
20. Haumonte JB, Raylet M, Christophe M, French validation and adaptation of the Grobman nomogram for prediction of vaginal birth after cesarean delivery: J Gynecol Obstet Hum Reprod, 2018; 47; 127-31
21. Xu P, Feng Y, Shen H, Verification a model of predicting vaginal birth after cesarean delivery in Chinese pregnant women: Medicine (Baltimore), 2019; 98; e18421
22. Lipschuetz M, Guedalia J, Rottenstreich A, Prediction of vaginal birth after cesarean deliveries using machine learning: Am J Obstet Gynecol, 2020; 222; 613.e1-12
23. Grobman WA, Lai Y, Landon MB, Development of a nomogram for prediction of vaginal birth: Obstet Gynecol, 2007; 109; 806-12
24. Grobman WA, Lai Y, Landon MB, Does information available at admission for delivery improve prediction of vaginal birth after cesarean?: Am J Perinatol, 2009; 26; 693-701
25. Lin J, Hou Y, Ke Y, Establishment and validation of a prediction model for vaginal delivery after cesarean and its pregnancy outcomes-Based on a prospective study: Eur J Obstet Gynecol Reprod Biol, 2019; 242; 114-21
26. Denham SH, Humphrey T, deLabrusse C, Dougall N, Mode of birth after caesarean section: individual prediction scores using Scottish population data: BMC Pregnancy Childbirth, 2019; 19; 84
Figures
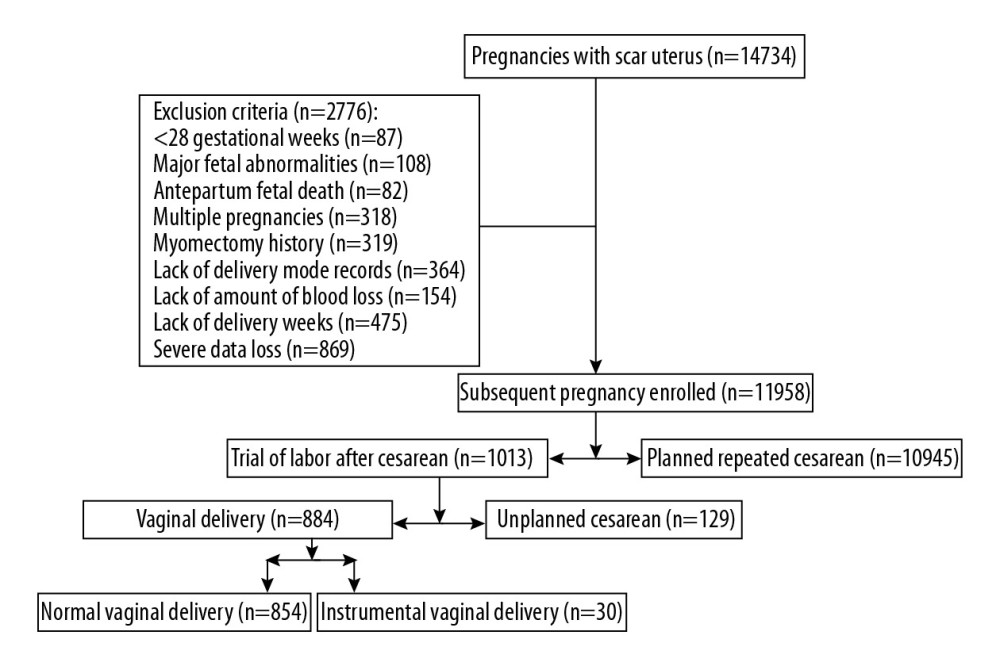 Figure 1. Flow diagram of the patients’ enrollment process.
Figure 1. Flow diagram of the patients’ enrollment process.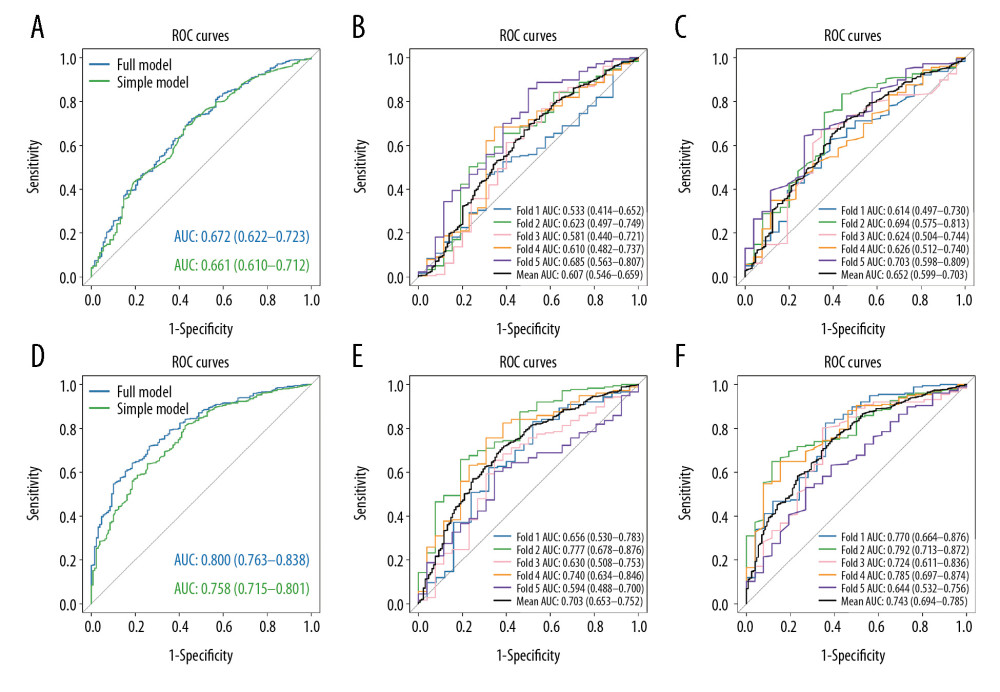 Figure 2. The receiver operating characteristic (ROC) curves of the 4 models. The first trimester period: (A–C); 5-fold cross validation of full model; 5-fold cross validation of first trimester model. The pre-labor period: (D–F); 5-fold cross validation of full model; 5-fold cross validation of pre-labor model.
Figure 2. The receiver operating characteristic (ROC) curves of the 4 models. The first trimester period: (A–C); 5-fold cross validation of full model; 5-fold cross validation of first trimester model. The pre-labor period: (D–F); 5-fold cross validation of full model; 5-fold cross validation of pre-labor model.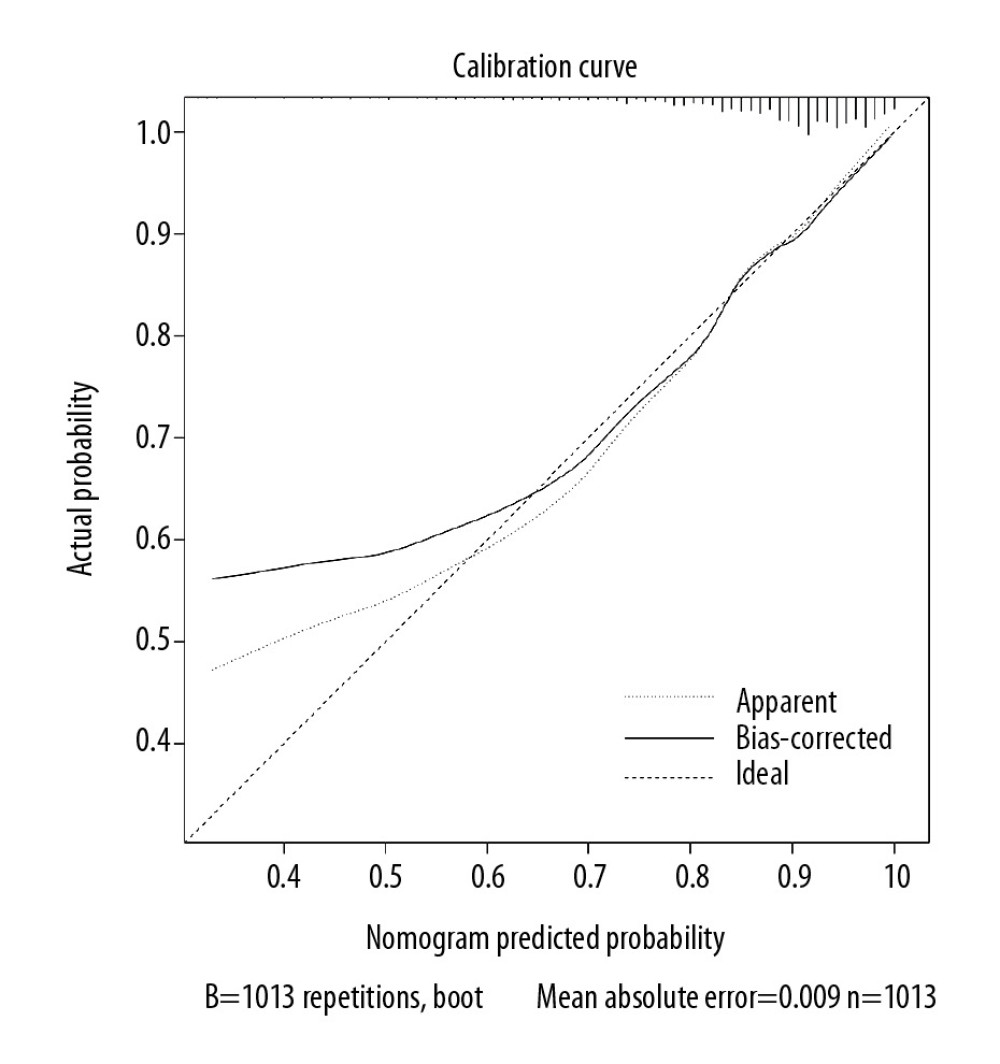 Figure 3. The calibration curve of the pre-labor model.
Figure 3. The calibration curve of the pre-labor model.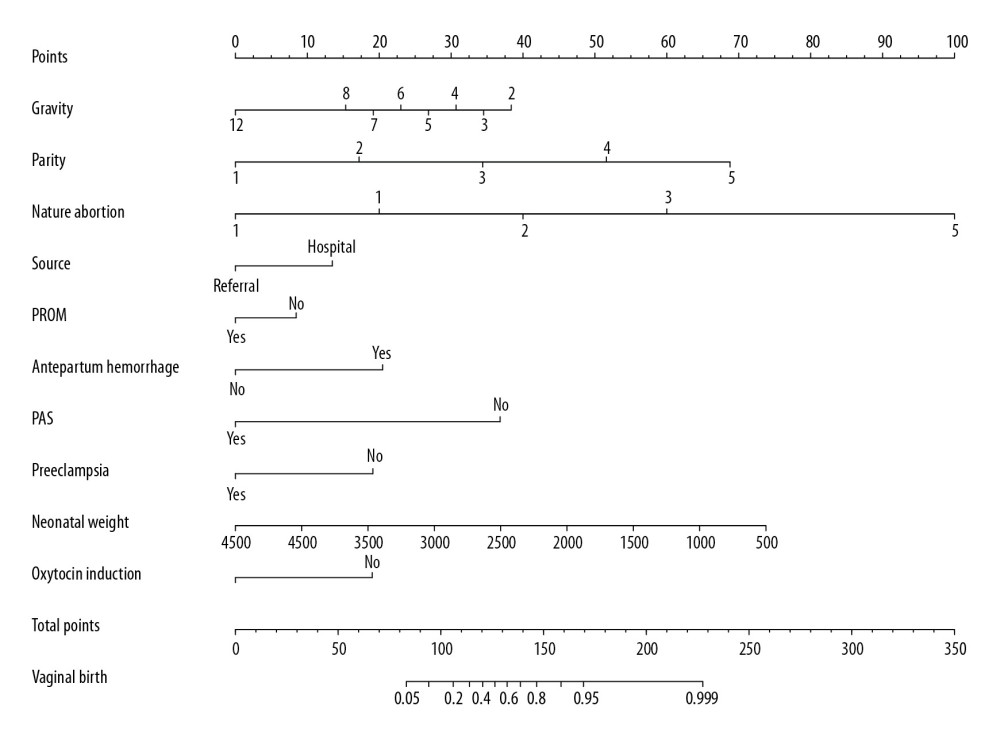 Figure 4. The nomogram of the pre-labor model. The nomogram converts each risk predictor into a 0 to 100 scale that is proportional to the derived adjusted log odds. These points are added across predictors to derive the „total points”, which are converted to predict the probabilities of vaginal birth.
Figure 4. The nomogram of the pre-labor model. The nomogram converts each risk predictor into a 0 to 100 scale that is proportional to the derived adjusted log odds. These points are added across predictors to derive the „total points”, which are converted to predict the probabilities of vaginal birth.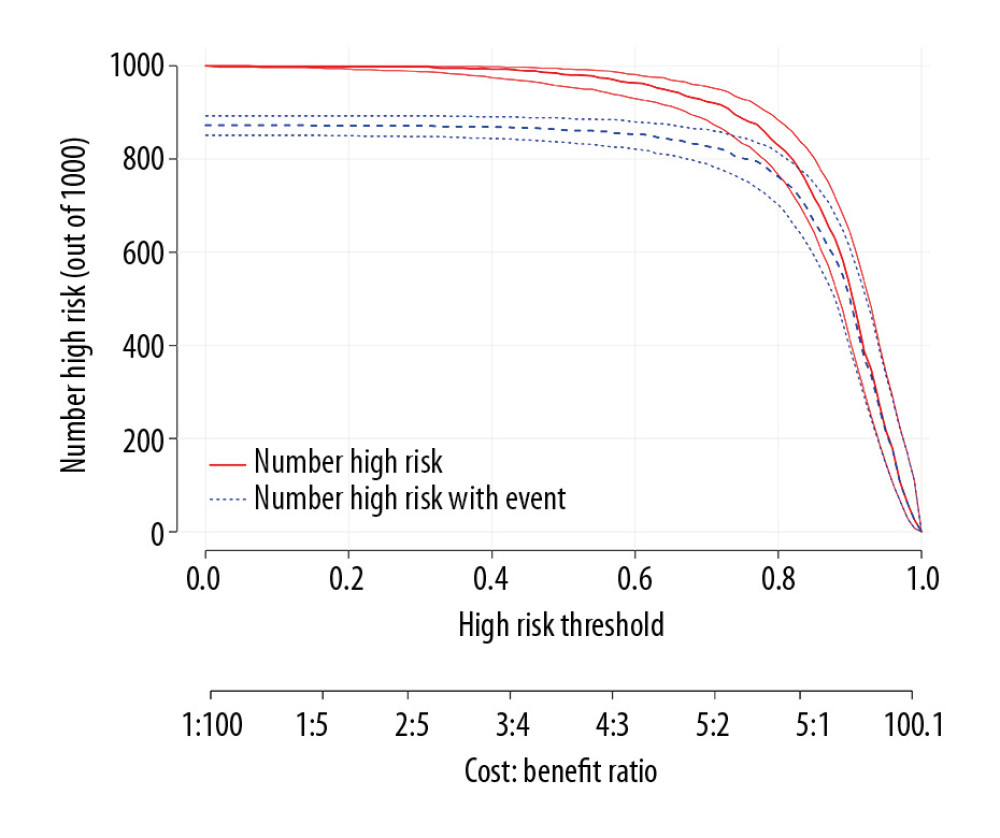 Figure 5. The clinical impact curve for the pre-labor model. Of 1000 patients, the red solid line shows the total number who would be deemed high risk for each risk threshold. The blue dashed line shows how many of those would be true positives (cases).
Figure 5. The clinical impact curve for the pre-labor model. Of 1000 patients, the red solid line shows the total number who would be deemed high risk for each risk threshold. The blue dashed line shows how many of those would be true positives (cases). Tables
 Table 1. Maternal and neonatal outcomes.
Table 1. Maternal and neonatal outcomes.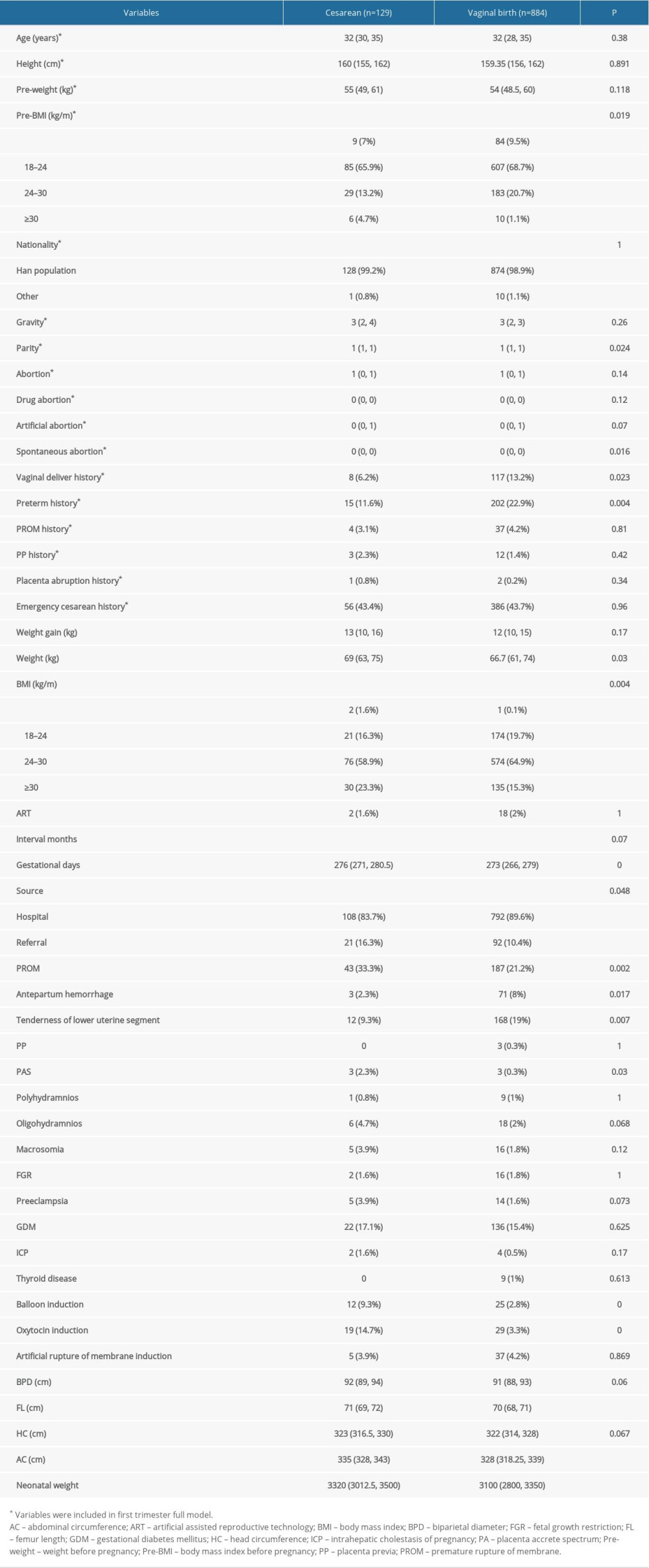 Table 2. Characteristics of the pregnant women.
Table 2. Characteristics of the pregnant women.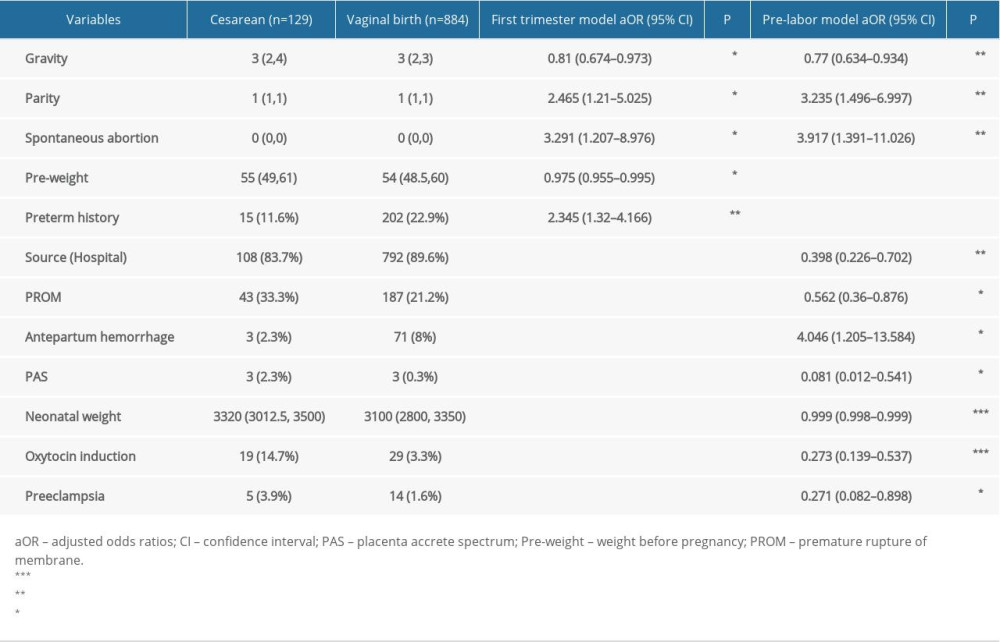 Table 3. The most significant variables included in the 2 models.
Table 3. The most significant variables included in the 2 models. Table 1. Maternal and neonatal outcomes.
Table 1. Maternal and neonatal outcomes.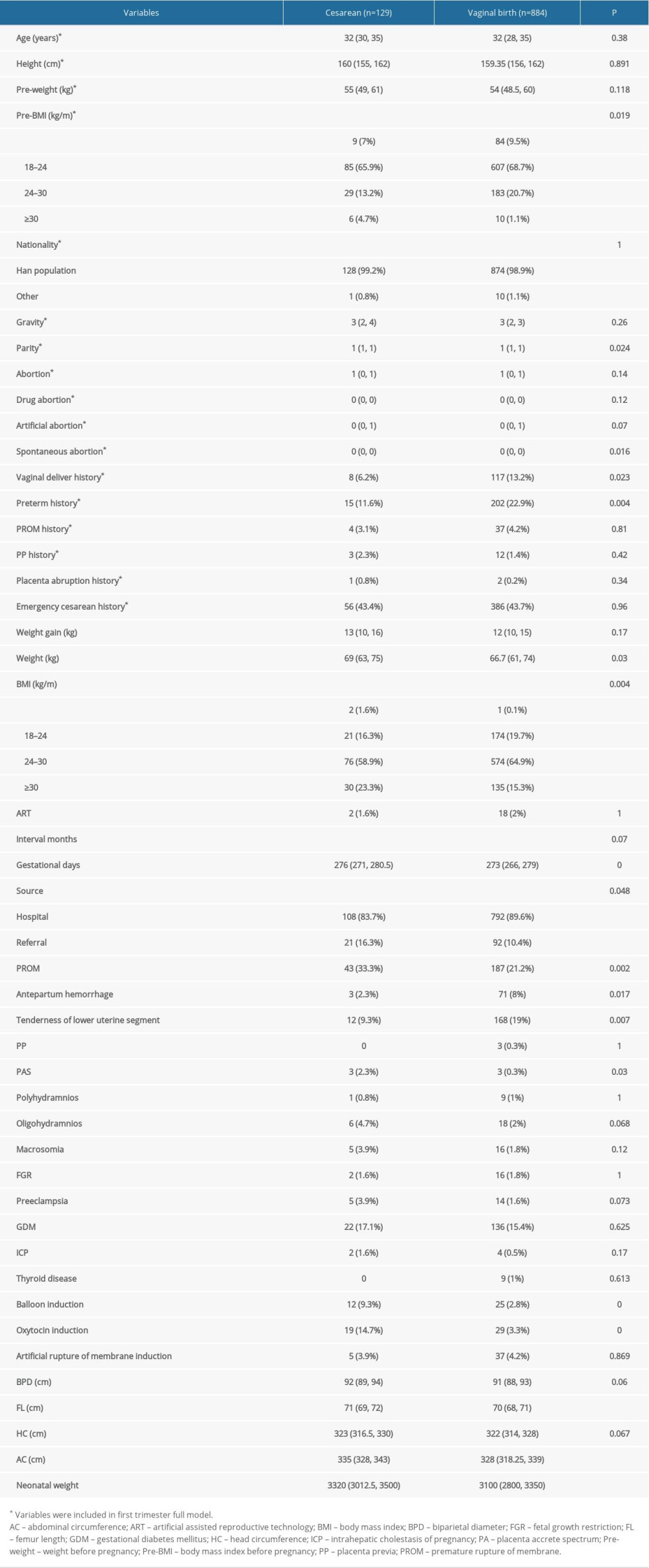 Table 2. Characteristics of the pregnant women.
Table 2. Characteristics of the pregnant women.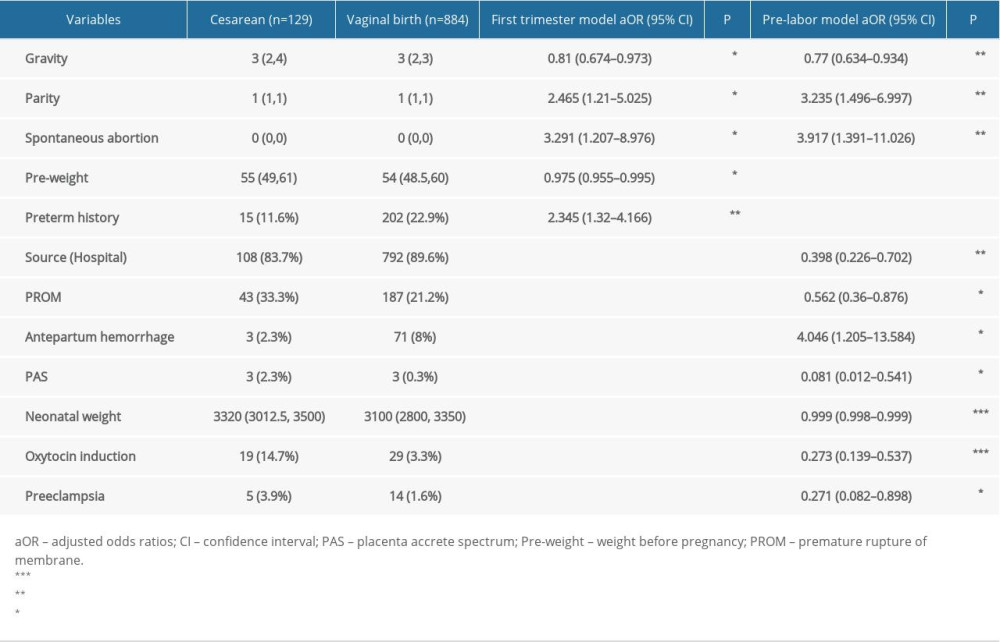 Table 3. The most significant variables included in the 2 models.
Table 3. The most significant variables included in the 2 models. In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








