21 February 2021: Clinical Research
Relationship Between Chronic Conditions and Balance Disorders in Outpatients with Dizziness: A Hospital-Based Cross-Sectional Study
Ruihua Zhang1ABCE, Bo Liu23ABDE*, Jingtao Bi23ABCF, Yiwen Chen1AEFDOI: 10.12659/MSM.928719
Med Sci Monit 2021; 27:e928719
Abstract
BACKGROUND: Balance dysfunction is common in adult outpatients with dizziness, especially those who are older, which can lead to catastrophic outcomes such as falls. The aim of this study was to investigate the association between chronic conditions and balance disorders in patients with dizziness, especially those who are elderly.
MATERIAL AND METHODS: A cross-sectional study was conducted in adult outpatients diagnosed with dizziness referred to the Department of Otolaryngology at Beijing Tongren Hospital from September 2017 to August 2018. All of the patients completed a self-administered, structured questionnaire. Demographic data and information on history of chronic conditions were collected and the patients were divided into 2 groups based on whether their balance was normal or abnormal.
RESULTS: Three hundred and thirty-two patients were included in this study, 168 in the normal balance group and 164 in the abnormal balance group. The incidence of chronic conditions, including hypertension and diabetes, in the abnormal balance group was higher than that in the normal balance group (all P<0.05). In subgroup analysis based on age, in those who were aged ≥60 years, the prevalence of chronic diseases was higher in the abnormal balance group than in the normal balance group (P=0.002), while there was no difference in age between the groups with abnormal and normal balance. Hypertension (OR: 2.268; 95%CI: 1.038–4.957; P<0.05) was a risk factor for balance disorders in elderly patients rather than those who were younger (P>0.05).
CONCLUSIONS: Our results show that chronic conditions are associated with balance function in older patients with dizziness. Thus, specialists should consider chronic conditions, especially hypertension, in elderly patients with dizziness.
Keywords: Chronic Disease, Dizziness, Accidental Falls, Cross-Sectional Studies, Hospitals, Outpatients, postural balance, Prevalence, Risk Factors, Surveys and Questionnaires, Vertigo
Background
Dizziness is a very common complaint in outpatients and one of the primary reasons for the creation of an outpatient service for elderly individuals. Every year, approximately 20% of elderly individuals in the United States experience problems with dizziness or balance disorders. Among these patients, 68% experience imbalance [1]. Balance disorders can severely limit daily activities and it is also associated with depression [2] and decreased quality of life [3]. It is also a major risk factor for falling, which can lead to fatal and nonfatal injuries, disability, and even death [4], as well as escalating medical costs [5]. The causes of dizziness are various, including vestibular and non-vestibular components. It is crucial to detect the factors leading to dizziness and imbalance to help patients remain mobile and avoid such secondary complications.
Maintenance of balance during everyday activities requires the interaction and coordination of the vestibular, visual, and proprioceptive systems. Disorders in function of any of these sensory systems can cause symptoms such as vertigo, dizziness, and balance disorders. Computerized dynamic posturography (CDP) is an established test of postural stability that quantitatively evaluates the integration of sensory information relevant to balance control by a patient. Studies have demonstrated the validity and value of CDP for assessment of balance disorders with high test-retest reliability [6,7]. CDP is a clinically proven and widely accepted and more sensitive method for assessing balancing abilities than some functional test and vestibular function tests, such as the Berg balance scale, the timed up and go test, and ocular motor, rotational chair, positional, and caloric findings [8,9]. The sensory organization test (SOT) is a CDP test protocol that assesses a subject’s ability to maintain balance under different stimulating conditions by employing visual, vestibular, and somatosensory inputs and monitoring the central compensatory state [10]. Clinicians and researchers can use the feedback from the test to obtain insight into an individual’s ability to maintain dynamic standing balance [11,12].
Chronic conditions are defined as conditions persisting for 12 months or more that limit self-care and independent living and require ongoing medical intervention [13,14]. Multiple chronic conditions are the presence of more than 1 chronic condition [15,16] and are termed as comorbidities, specifically in elderly people [17,18]. The majority of elderly patients with dizziness have chronic diseases, such as hypertension, diabetes mellitus (DM), dyslipidemia, and thyroid dysfunction [19].
Neuhauser et al examined the association of vestibular vertigo with sociodemographic factors and comorbid conditions in the general population. They found that hypertension and elevated levels of blood lipids had an independent effect on vestibular vertigo in the past 12 months [20]. Maarsingh et al found that cardiovascular disease was the most common major cause of dizziness in elderly patients in primary care [21]. Angela et al found that there was a statistically significant difference in the occurrence of Ménière’s disease (MD) attacks between patients with MD who did and did not have risk factors, which were defined as excessive body mass index, dyslipidemia, hypertension, smoking status and type 2 DM (T2DM) [22]. Li and his colleague found that patients with T2DM have a higher incidence of vestibular dysfunction. Vestibular dysfunction, visual system impairment, and a decline in motion control may be risk factors that lead to falls [23].
In adult outpatients with dizziness, however, the relationship between chronic conditions and balance disorders remains unclear. Thus, the present study attempted to investigate the association between chronic conditions and balance disorders.
Material and Methods
PATIENTS:
Adult outpatients complaining of dizziness who had been referred to the Department of Otolaryngology at Beijing Tongren Hospital from September 2017 to August 2018 were consecutively enrolled after approval from the Institutional Ethics Committee. Patients with cognitive decline who were unable to understand the procedure or perform the SOT safely due to poor nutritional status, blindness, cognitive impairment, or extremity disability; those with emergency conditions such as fever, unstable angina, and acute cerebral infarction; those unwilling to participate in the study; and those in other situations that the investigators judged made them unsuitable for the SOT protocol of the CDP test were excluded from the study. The study was explained to the patients and informed written consent was obtained.
The patients were divided into 2 groups based on balance function – abnormal balance and normal balance – according to SOT on CDP, which has been proven to diagnose balance function more accurately than a traditional vestibular function test [8].
QUESTIONNAIRE PROCEDURES:
A self-administered structured questionnaire was used to collect data on patient demographics (name, sex, age) and history of chronic diseases (defined as lasting >1 year), including hypertension, DM, dyslipidemia, hypothyroidism, chronic kidney disease, anemia, hyperthyroidism, and rheumatism. The patients received the questionnaires and the CDP examination application forms at the same time. They completed the questionnaires at home and returned them the day of the CDP examination.
SENSORY ORGANIZATION TEST FOR CDP:
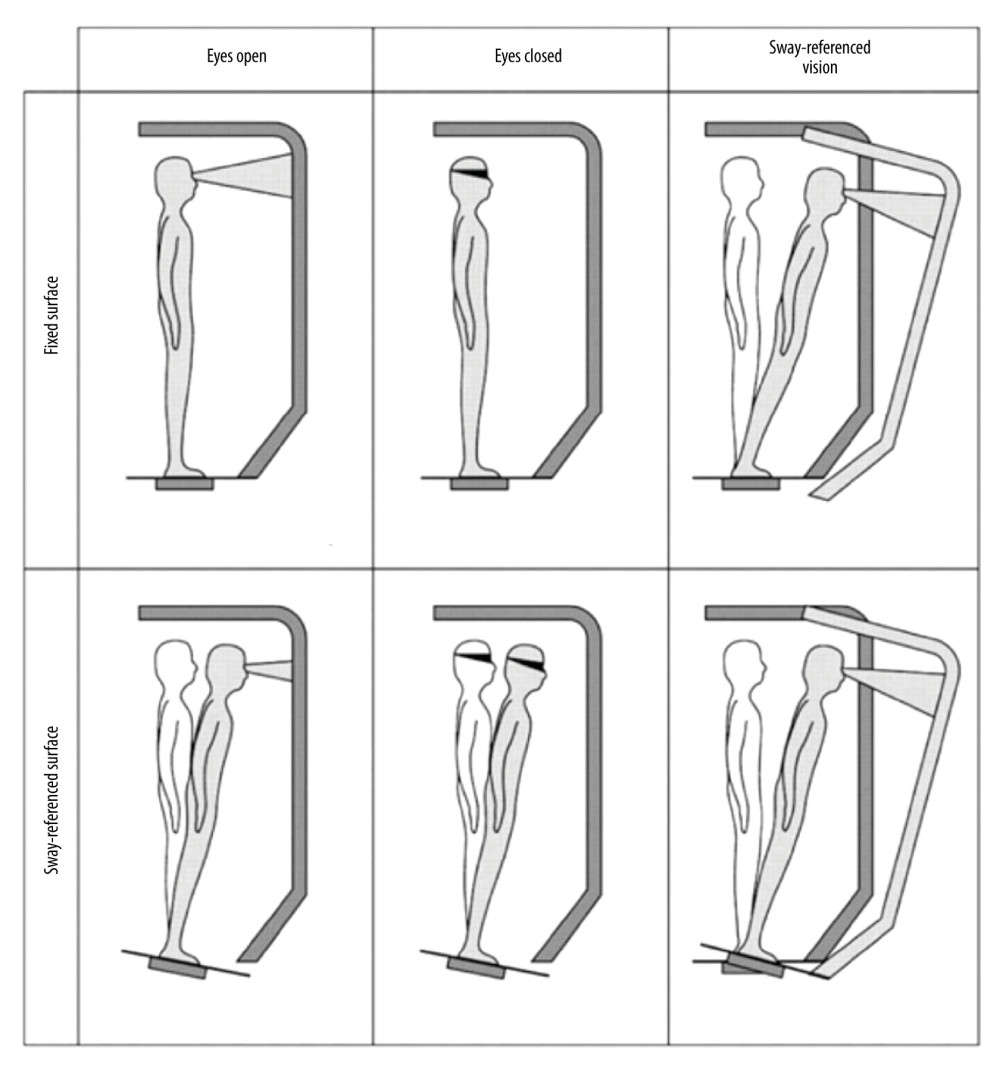
The NeuroCom Smart Balance Manager CDP platform (NeuroCom International; Oregon, United States) was used in this study. A patient was placed on the platform in the Romberg position, barefoot, with a safety harness. With the patient standing under 6 different conditions, movements from the center of pressure were recorded. The 6 conditions were as follows: 1) Fixed support, visual surround, and eyes open; 2) Fixed support and eyes closed; 3) Fixed support, eyes open, and moving visual surround; 4) Moving support, eyes open, and fixed visual surround; 5) Moving support and eyes closed; and 6) Moving support, eyes open, and moving visual surround (Figure 1). Each of these conditions was maintained for 20 seconds and each such test was repeated consecutively at least twice. If the patient did not pass the first 2 tests of a condition, the test was repeated a third time.
DATA ANALYSIS:
Balance outcomes for the SOT were analyzed using NeuroCom@ software. Equilibrium scores for each condition were calculated based on anterior-posterior peak-to-peak sway amplitude during the trial. The composite equilibrium score was calculated as a weighted average of the scores of the 6 conditions tested and a result was abnormal when the calculated score was lower than the score for the 95% age-matched control group. A score of 100 indicated no sway, whereas 0 indicated a fall [24].
STATISTICAL ANALYSIS:
Statistical analyses were performed using SPSS software version 25 (IBM SPSS Inc, Chicago, Illinois, United States). Continuous data were presented as means±SD (age) and were analyzed using a
Results
PATIENT CHARACTERISTICS:
Table 1 lists demographic data for all of the patients. A total of 332 patients were included in the present study, divided into 2 groups: normal balance (n=168) and abnormal balance (n=164). The average age was 52.92±14.07 years and the overall prevalence of balance disorders in the adult outpatient population was 49.4% in our study. Patients in the abnormal balance group were older than those in the normal balance group (56.15±13.37 vs 49.77±14.06, P<0.05). There was no difference between the 2 groups in terms of sex (P>0.05).
CHRONIC CONDITIONS:
As shown in Table 1, the prevalence of chronic diseases was higher in the abnormal than in the normal balance group (P<0.05). Hypertension, DM, and dyslipidemia were the most common chronic conditions in the 2 groups. The incidences of hypertension (41.5% vs 26.2%, P=0.003) and DM (16.5% vs 6.5%, P=0.005) were higher in the abnormal than in the normal balance group.
Based on the results described above, there was a significant difference in age between the normal and abnormal balance groups. Therefore, we divided all patients into younger (<60 years) and older (≥60 years) age groups for subgroup analysis. Data for younger patients are presented in Table 2. There was a significant difference in sex ratio between the normal and abnormal balance groups (P=0.012). However, there were no differences between the normal and abnormal balance groups in other indicators, including age and prevalence of chronic disease.
The incidence of imbalance in the elderly patients was 66.1% (Table 3). There was no significant difference between the 2 groups in either age or sex (P=0.983 and P=0.276, respectively). Unlike the younger patients, the older ones were more likely to have a chronic disease if they were in the abnormal balance than in the normal balance group (P=0.002). We observed that a history of hypertension was associated with a borderline significant increase in the odds of balance dysfunction (P=0.059). However, there was no significant difference between the 2 groups in the prevalence of other chronic diseases (DM, P=0.191; dyslipidemia, P=0.530; other diseases, P=0.450)
ASSOCIATION BETWEEN CHRONIC CONDITIONS AND BALANCE:
Logistic regression analyses were used to further explore the relationship between previous history of chronic conditions and balance disorder (Table 4). Note that age and sex were identified as confounding variables and thus were included in the models for adjustment. We observed that in the models adjusted for age and sex, hypertension (OR: 2.268; 95%CI: 1.038–4.957; P<0.05) was a risk factor for balance disorders in elderly but not in younger patients (P>0.05).
Discussion
The incidence of imbalance in the elderly group in our study was 66.1%, close to the rate reported by previous authors [1]. Balance disorders are very common in the elderly and they increase the risk of falling and pose a significant health concern. The results of the present study showed that the incidence of chronic conditions in elderly patients was higher than in younger patients. Hypertension was a risk factor for balance disorders in elderly but not in younger patients. Thus, clinicians should be alert for the presence of chronic conditions in elderly patients who have balance disorders.
In older people, dizziness is often a diagnostic challenge because the term can be used describe a variety of sensations and there are many potential causes [25]. Dizziness in the elderly is likely to constitute a geriatric syndrome, that is, an issue caused by multiple contributing factors that involve several organ systems [26]. Balance disorders in the elderly clearly can result from impairment in a number of systems, including sensory (vision, vestibular sense, proprioception, sensory integration), motor (strength, reaction time), and central processing systems (standing, leaning, gait, mobility, and transfers) [27]. One of the novel findings from the present study is that there was a significant association between chronic conditions and having a balance disorder. The incidences of hypertension (41.5% vs 26.2%, P=0.003) and DM (16.5% vs 6.5%, P=0.005) were higher in the abnormal than in the normal balance group. Among patients with dyslipidemia and other diseases, there were more individuals who had abnormal balance, but this difference was not significant.
Elderly outpatients with dizziness often present to a specialist, which increases the tendency to diagnose conditions in the clinician’s own field of experience (the “blind man and the elephant” phenomenon) [28]. The present study indicates that chronic conditions, particularly hypertension, should be considered in addition to common causes such as vestibular or neurological diseases. Doing so may help clinicians screen patients with abnormal balance function – especially those who are elderly – to determine whether they are at high risk of falling. In addition to treating illnesses that can cause dizziness, clinicians should counsel patients about measures to manage chronic conditions, assess their eyesight, and encourage them to exercise to improve their balance function.
There was another interesting result from our research. Many studies have found the prevalence of dizziness to be approximately 2 to 3 times higher in women than in men (consistent with our study). In the present study, however, among the younger outpatients with dizziness, the incidence of balance disorder was higher in men than in women. The same sex difference was not found in the elderly group.
Most studies have reported a significant association between hypertension and balance disorder [20,22,29,30], possibly because of the effect of hemodynamics on microcirculation in the inner ear, exposure to multiple drugs, and the well-known adverse effects of antihypertensive drugs. In addition, several authors have implicated metabolic disorders such as DM, dyslipidemia, and hypothyroidism in the etiology of balance disorders related to labyrinthine dysfunction through corresponding changes in hormone levels [23,31–34]. These studies partly explain the possible mechanism of abnormal balance function in patients with chronic conditions. However, with the exception of hypertension, which was significantly correlated with balance disorders in the elderly patients in our study, other chronic diseases did not have any significant influence on those patients. The probable reason is the insufficient sample size. Another possible reason is that balance function compensation is a very complex process involving multiple systems, such as the peripheral nervous system and the musculoskeletal system. Mechanisms of pathogenesis and development of various chronic diseases are diverse, leading to differing effects on balance function [35,36].
The main limitations of the present study are its single-center nature and small sample size. Another limitation of our study is that we considered only certain chronic conditions and not factors related to them, such as their duration and how they were managed. Some quantitative methods can be used to evaluate comorbidity. For example, the Charlson-Deyo comorbidity index is a weighted index that considers the number and intensity of comorbidities to estimate the risk of mortality. However, it takes into consideration 17 diseases, and because only a few chronic diseases were included in the present study, the applicability of the index to our research was poor. Furthermore, because we used a questionnaire to collect data on chronic disease history, the information is subject to recall error and inaccuracy. Finally, other factors that can affect balance function, such as relevant medications and arrythmia history, were not included in the present study. Further multicenter, prospective studies with larger sample sizes that take into consideration possible factors related to chronic disease would further strengthen our understanding of the relationship between chronic disease and balance disorders in elderly patients with dizziness.
Conclusions
Given the high prevalence and catastrophic consequences of balance problems in patients with dizziness, balance disorders merit special attention, particularly in the elderly population. The present study proved that an association exists between chronic conditions and balance function in older patients who have dizziness. Clinicians in all specialties should consider chronic conditions when they encounter elderly patients who complain of dizziness. In these cases, laboratory and diagnostic testing of blood lipids and thyroid hormones and a fasting blood glucose test should be ordered and the patient’s blood pressure should be measured. A multidisciplinary team approach to the management of dizziness is recommended, including consultation with otolaryngologic, neurologic, ophthalmologic, psychiatric, and geriatric departments.
Tables
Table 1. Comparison of demographic and medical conditions of all patients between different balance function.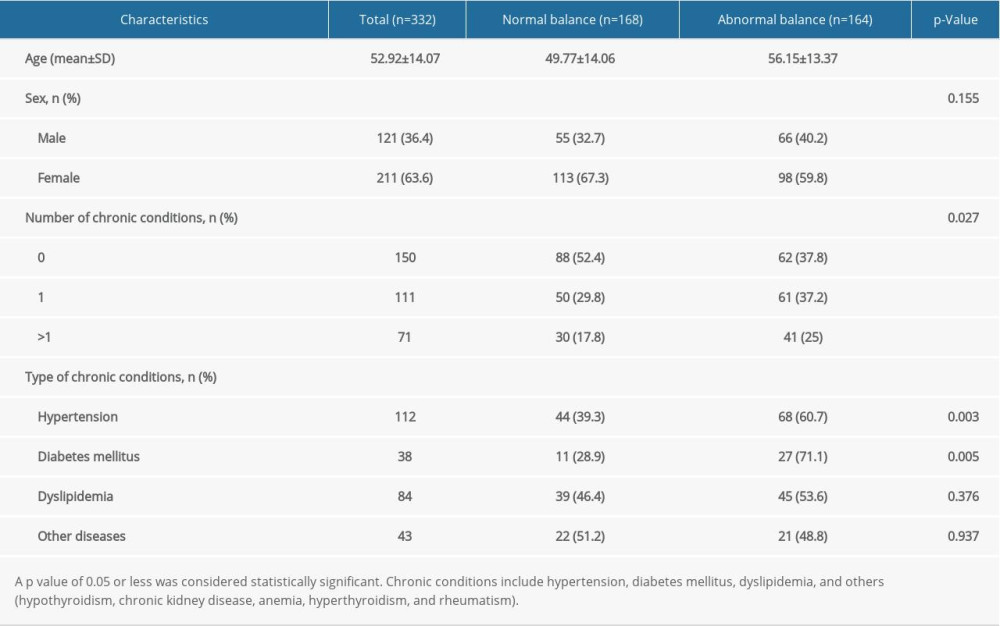 Table 2. Comparison of demographic and medical conditions of younger patients(<60 years) between different balance function.
Table 2. Comparison of demographic and medical conditions of younger patients(<60 years) between different balance function.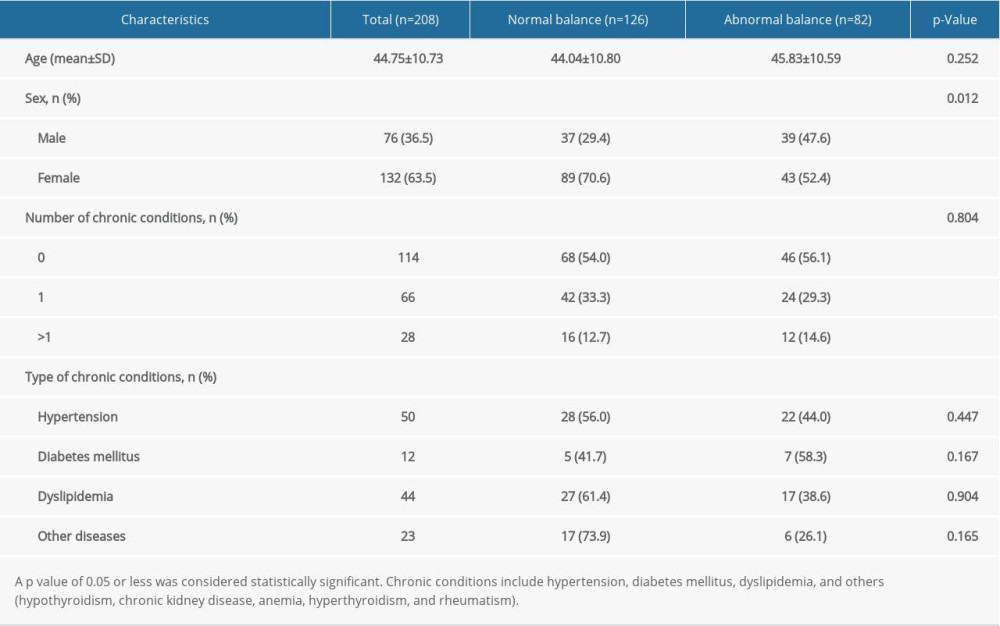 Table 3. Comparison of demographic and medical conditions of elderly patients (>=60 years) between different balance function.
Table 3. Comparison of demographic and medical conditions of elderly patients (>=60 years) between different balance function.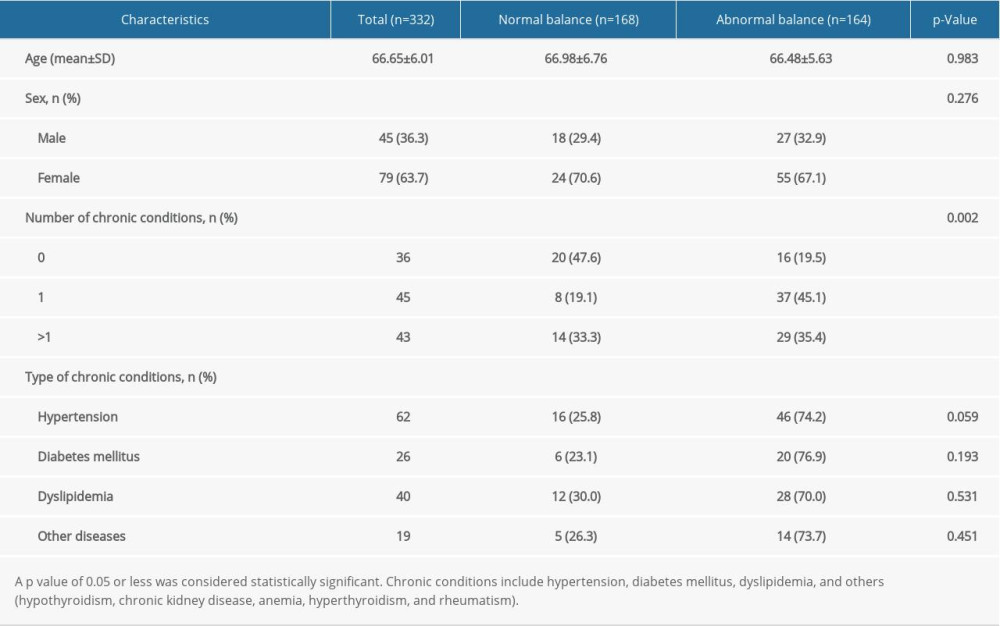 Table 4. Association between chronic conditions and balance function.
Table 4. Association between chronic conditions and balance function.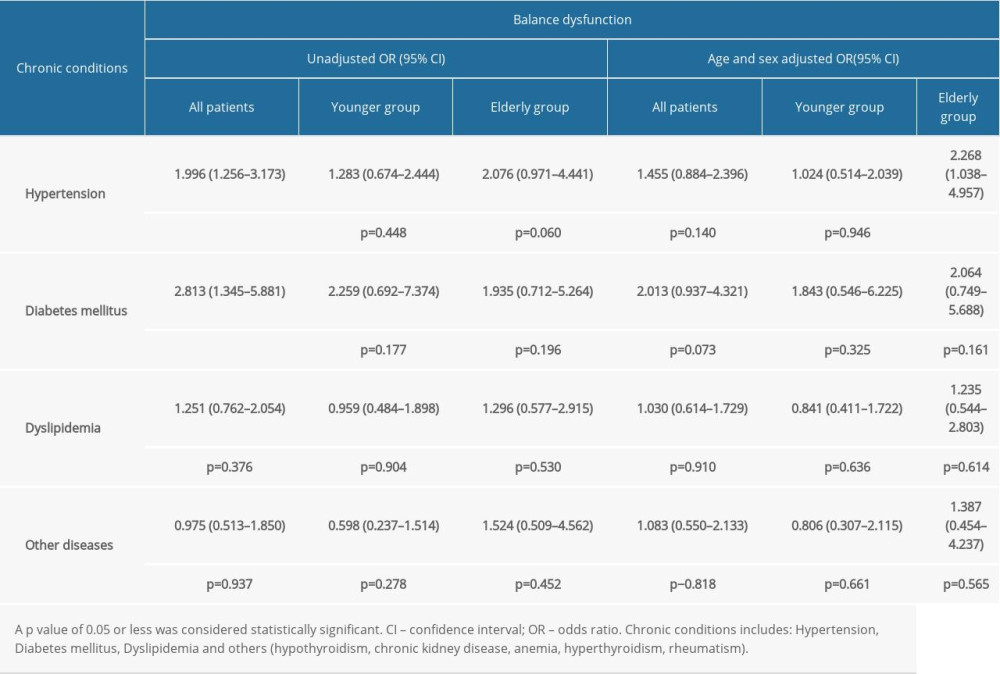
References
1. Lin HW, Bhattacharyya N, Balance disorders in the elderly: Epidemiology and functional impact: Laryngoscope, 2012; 122; 1858-61
2. Stam H, Wouden JC, Hugtenburg JG, Effectiveness of a multifactorial intervention for dizziness in older people in primary care: A cluster randomised controlled trial: PLoS One, 2018; 13(10); e0204876
3. Dros J, Maarsingh OR, Beem L, Impact of dizziness on everyday life in older primary care patients: A cross-sectional study: Health Qual Life Outcomes, 2011; 9(1); 44
4. Agrawal Y, Carey JP, Della Santina CC, Disorders of balance and vestibular function in US adults: Data from the National Health and Nutrition Examination Survey, 2001–2004: Arch Intern Med, 2009; 169; 938-44
5. Stevens JA, Corso PS, Finkelstein EA, The costs of fatal and non-fatal falls among older adults: Inj Prev, 2006; 12; 290-95
6. Carter ND, Khan KM, Petit MA, Results of a 10 week community based strength and balance training programme to reduce fall risk factors: A randomised controlled trial in 65–75 year old women with osteoporosis: Br J Sports Med, 2001; 35; 348-51
7. Pickerill ML, Harter RA, Validity and reliability of limits-of-stability testing: A comparison of 2 postural stability evaluation devices: J Athl Train, 2011; 46(6); 600-6
8. Petro B, Papachatzopoulou A, Kiss RM, Devices and tasks involved in the objective assessment of standing dynamic balancing – A systematic literature review: PLoS One, 2017; 12; e0185188
9. Whitney SL, Marchetti GF, Schade AI, The relationship between falls history and computerized dynamic posturography in persons with balance and vestibular disorders: Arch Phys Med Rehabil, 2006; 87; 402-7
10. Jacobson G, Shepard N, Computerized dynamic posturography: Balance function assessment and management, 2014; 451-79, San Diego, Plural Publishing Inc
11. Redfern MS, Chambers AJ, Sparto PJ, Inhibition and decision-processing speed are associated with performance on dynamic posturography in older adults: Exp Brain Res, 2019; 237(1); 37-45
12. Fong SS, Tsang WW, Ng GY, Altered postural control strategies and sensory organization in children with developmental coordination disorder: Hum Mov Sci, 2012; 31(5); 1317-27
13. Goodman RA, Posner SF, Huang ES, Defining and measuring chronic conditions: Imperatives for research, policy, program, and practice: Prev Chronic Dis, 2013; 10; E66
14. United States Department of Health and Human Services: HHS Initiative on Multiple Chronic Conditions, United States Department of Health and Human Services http://www.hhs.gov/ash/initiatives/mcc/
15. Parekh AK, Barton MB, The challenge of multiple comorbidity for the US health care system: JAMA, 2010; 303; 1303-4
16. Parekh AK, Goodman RA, Gordon C, HHS Interagency Workgroup on Multiple Chronic Conditions. Managing multiple chronic conditions: A strategic framework for improving health outcomes and quality of life: Public Health Rep, 2011; 126(4); 460-71
17. Yoon J, Zulman D, Scott JY, Costs associated with multimorbidity among VA patients: Med Care, 2014; 52(Suppl 3); S31-36
18. Steinman MA, Lee SJ, John Boscardin W, Patterns of multimorbidity in elderly veterans: J Am Geriatr Soc, 2012; 60; 1872-80
19. Hurwitz EL, Randhawa K, Yu HThe Global Spine Care Initiative, A summary of the global burden of low back and neck pain studies: Eur Spine J, 2018; 27; 796-801
20. Neuhauser HK, von Brevern M, Radtke A, Epidemiology of vestibular vertigo: A neurotologic survey of the general population \published correction appears in Neurology, 2006;67(8):1528]: Neurology, 2005; 65(6); 898-904
21. Maarsingh OR, Dros J, Schellevis FG, Causes of persistent dizziness in elderly patients in primary care: Ann Fam Med, 2010; 8(3); 196-205
22. Rego ÂR, Dias D, Pinto A, The cardiovascular aspects of a Ménière’s disease population – A pilot study: J Otol, 2019; 14(2); 51-56
23. Li J, Jiang J, Zhang Y, Impairment of vestibular function and balance control in patients with type 2 diabetes: Audiol Neurootol, 2019; 24(3); 154-60
24. NeuroCom Internacional Inc: Equitest system operator’s manual, 1998, Clackamas (OR), NeuroCom International
25. Alyono JC, Vertigo and dizziness: Understanding and managing fall risk: Otolaryngol Clin North Am, 2018; 51(4); 725-40
26. Tinetti ME, Williams CS, Gill TM, Dizziness among older adults: A possible geriatric syndrome: Ann Intern Med, 2000; 132(5); 337-44
27. Osoba MY, Rao AK, Agrawal SK, Balance and gait in the elderly: A contemporary review: Laryngoscope Investig Otolaryngol, 2019; 4(1); 143-53
28. Sloane PD, Dallara J, Clinical research and geriatric dizziness: The blind men and the elephant: J Am Geriatr Soc, 1999; 47(1); 113-14
29. Shen S, He T, Chu J, Uncontrolled hypertension and orthostatic hypotension in relation to standing balance in elderly hypertensive patients: Clin Interv Aging, 2015; 10; 897-906
30. Acar S, Demırbüken İ, Algun C, Is hypertension a risk factor for poor balance control in elderly adults?: J Phys Ther Sci, 2015; 27(3); 901-4
31. Lee H, Kim HA, Orthostatic hypertension: An underestimated cause of orthostatic intolerance: Clin Neurophysiol, 2016; 127; 2102-7
32. Maarsingh OR, Stam H, van de Ven PM, Predictors of dizziness in older persons. A 10-year prospective cohort study in the community: BMC Geriatr, 2014; 14; 133
33. Santos MD, Bittar RS, Vertigo and metabolic disorders: Int Tinnitus J, 2012; 17; 16-20
34. Lin ZM, Young YH, Investigating the causes of vertigo in breast cancer survivors: Eur Arch Otorhinolaryngol, 2005; 262; 432-36
35. Corrales CE, Bhattacharyya N, Dizziness and death: An imbalance in mortality: Laryngoscope, 2016; 126; 2134-36
36. Ammar H, Govindu R, Fouda R, Dizziness in a community hospital. central neurological causes, clinical predictors, and diagnostic yield and cost of neuroimaging studies: J Community Hosp Intern Med Perspect, 2017; 7; 73-78
Tables
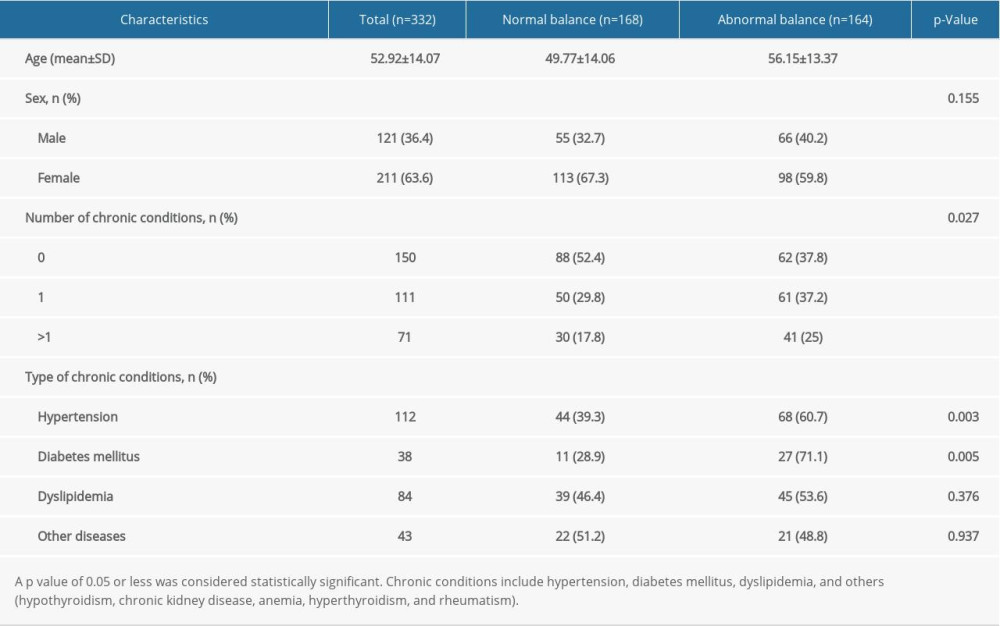 Table 1. Comparison of demographic and medical conditions of all patients between different balance function.
Table 1. Comparison of demographic and medical conditions of all patients between different balance function.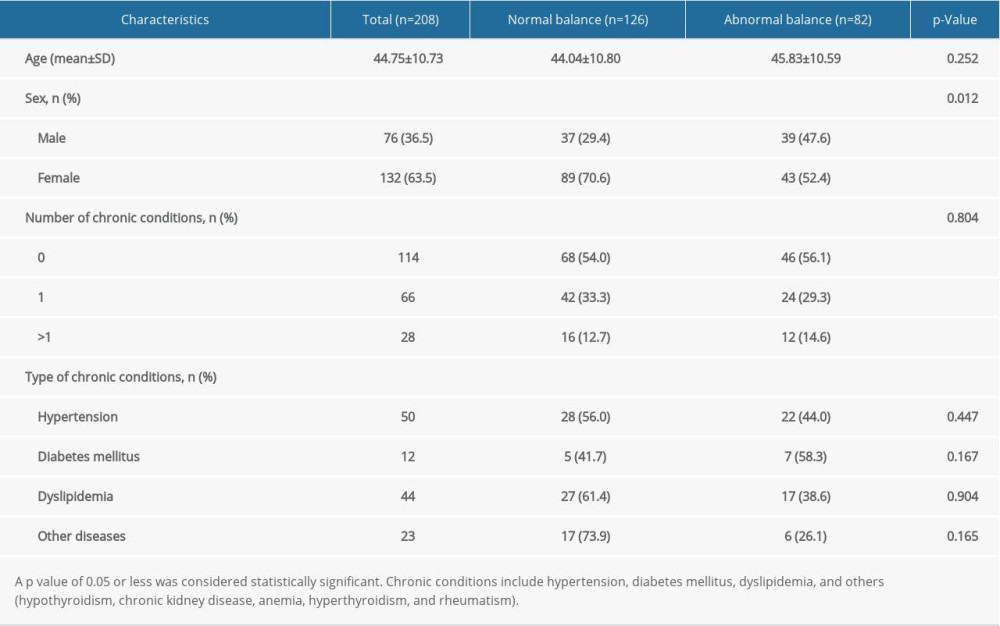 Table 2. Comparison of demographic and medical conditions of younger patients(<60 years) between different balance function.
Table 2. Comparison of demographic and medical conditions of younger patients(<60 years) between different balance function.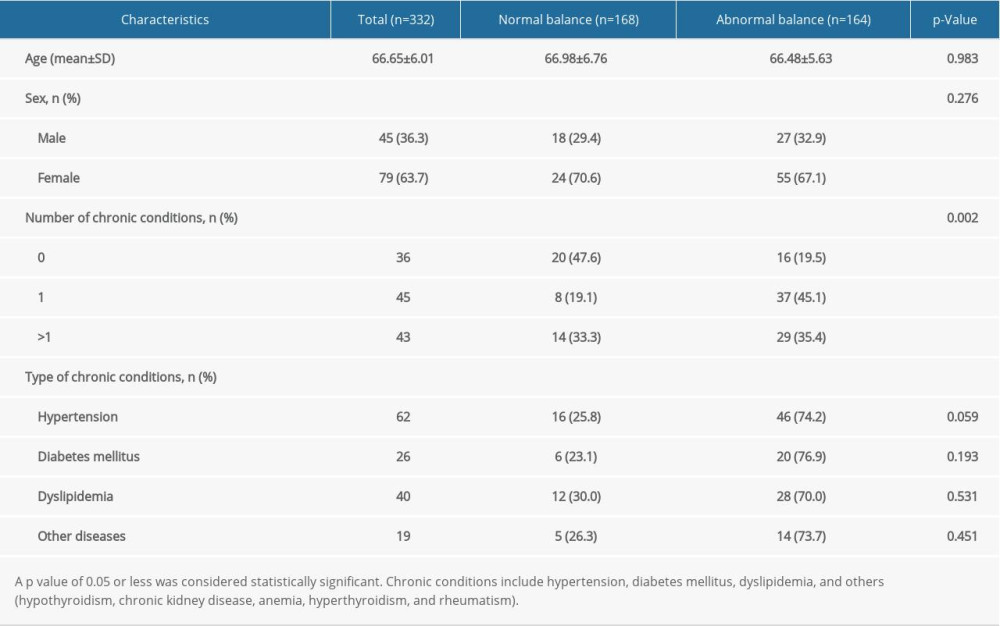 Table 3. Comparison of demographic and medical conditions of elderly patients (>=60 years) between different balance function.
Table 3. Comparison of demographic and medical conditions of elderly patients (>=60 years) between different balance function.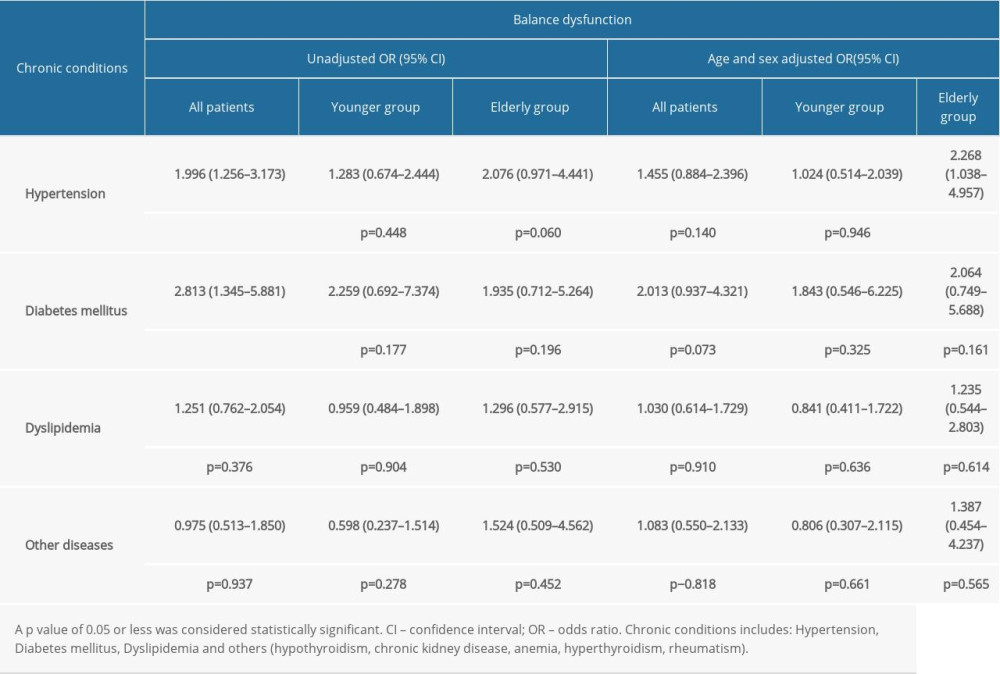 Table 4. Association between chronic conditions and balance function.
Table 4. Association between chronic conditions and balance function.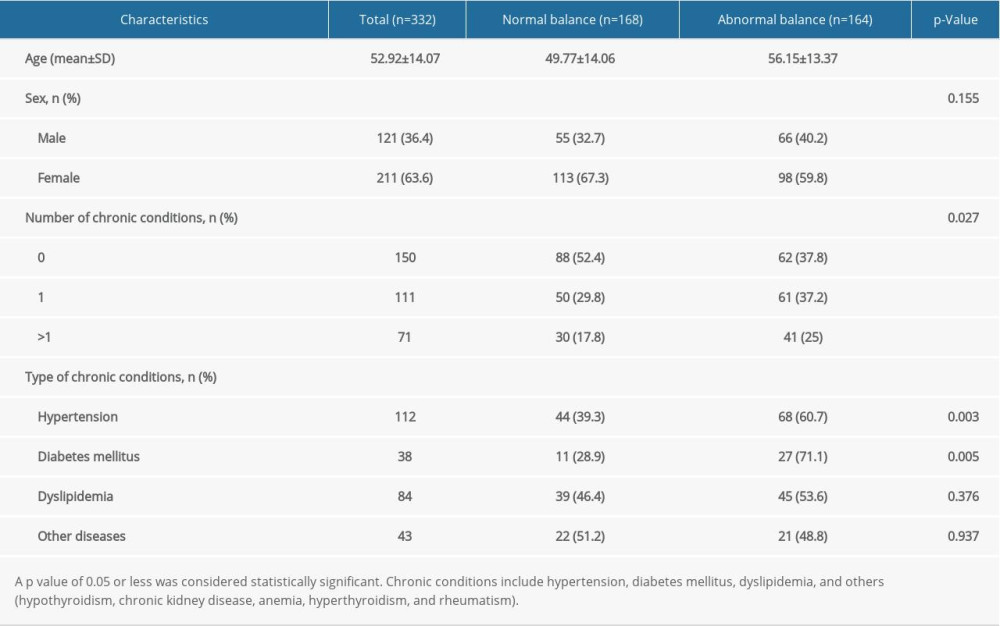 Table 1. Comparison of demographic and medical conditions of all patients between different balance function.
Table 1. Comparison of demographic and medical conditions of all patients between different balance function.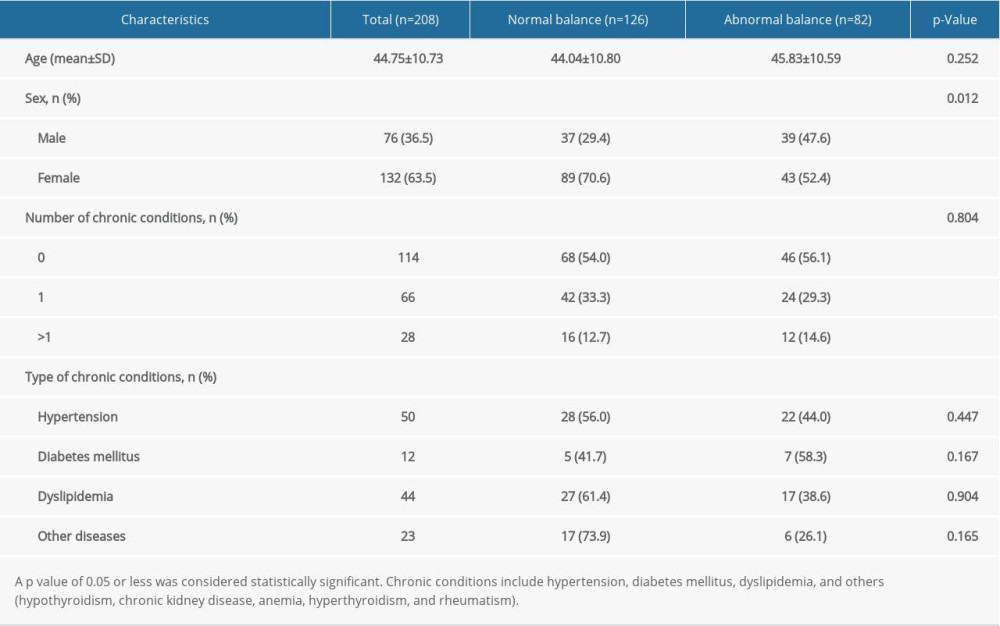 Table 2. Comparison of demographic and medical conditions of younger patients(<60 years) between different balance function.
Table 2. Comparison of demographic and medical conditions of younger patients(<60 years) between different balance function.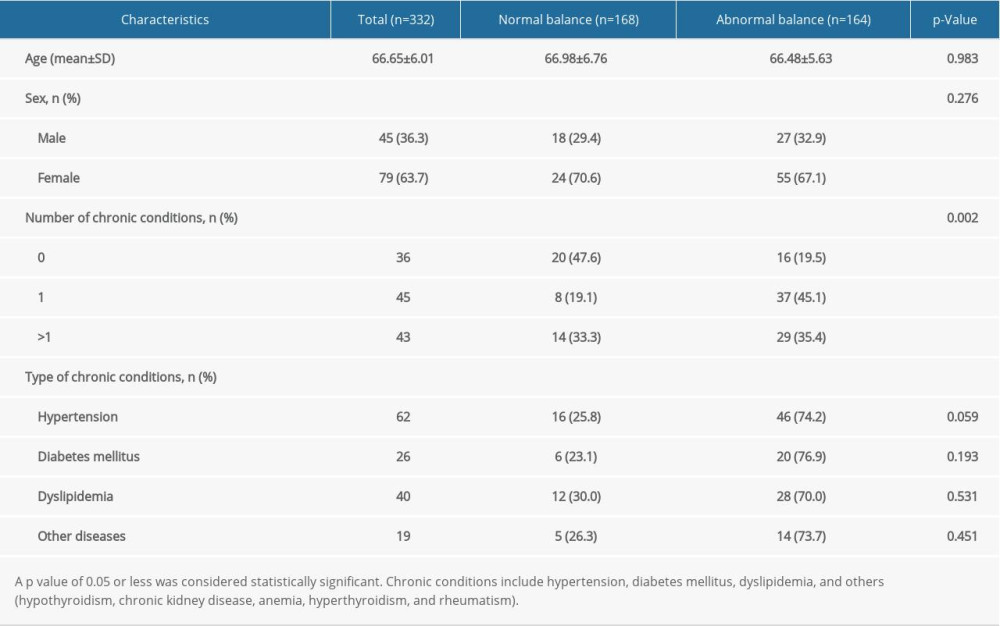 Table 3. Comparison of demographic and medical conditions of elderly patients (>=60 years) between different balance function.
Table 3. Comparison of demographic and medical conditions of elderly patients (>=60 years) between different balance function.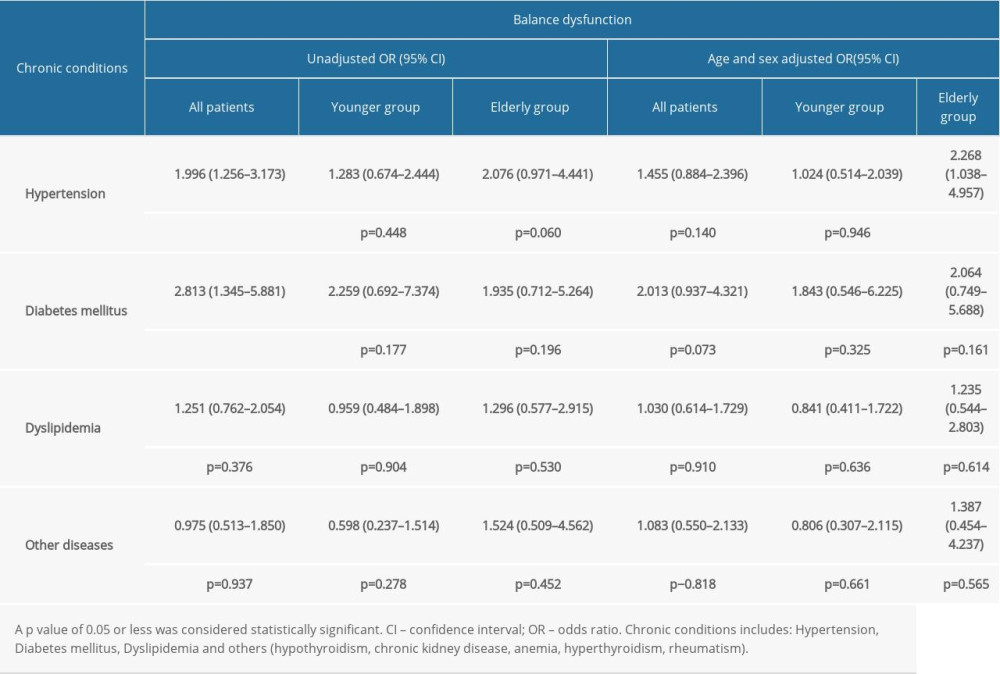 Table 4. Association between chronic conditions and balance function.
Table 4. Association between chronic conditions and balance function. In Press
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952