24 January 2021: Clinical Research
Elevated Plasma Angiopoietinlike Protein 5 (ANGPTL5) Is More Positively Associated with Glucose Metabolism Disorders in Patients with Metabolic Syndrome
Chang Liu123ABCD, Xin Yi123AEG, Yongnan Lyu123CF, Wei Ren4CD, Yi Zhou123BF, Gaoke Feng123E, Weiguo Wan123B, Xue-jun Jiang123AEG*DOI: 10.12659/MSM.929626
Med Sci Monit 2021; 27:e929626
Abstract
BACKGROUND: Angiopoietinlike protein 5 (ANGPTL5) is an adipocytokine and has an important role in metabolic processes including lipid metabolism, obesity, and type 2 diabetes mellitus. On the basis of these roles, the present study aimed to investigate the level and role of plasma ANGPTL5 in metabolic syndrome (MS) patients.
MATERIAL AND METHODS: A total of 139 participants was enrolled in this study; 69 of them were diagnosed with MS. Plasma ANGPTL5 levels were measured by enzyme-linked immunosorbent assay. Sex, age, and other laboratory tests were compared statistically. Correlations between ANGPTL5 and biochemical parameters such as lipid levels and insulin resistance were all evaluated statistically.
RESULTS: In patients with MS, plasma ANGPTL5 levels were higher than in those without MS (P<0.05). Moreover, after adjusting for the glucose profiles, positive correlations were found between plasma ANGPTL5 levels and body mass index (BMI), waist circumference, and waist-hip ratio (WHR); a weak negative correlation was found between ANGPTL5 concentration and high-density lipoprotein cholesterol. After controlling the lipid profiles, positive correlations were found between ANGPTL5 concentration and BMI, WHR, fasting plasma glucose, fasting insulin, glycated hemoglobin, and homeostatic model assessment (HOMA) of insulin resistance; a negative correlation was found between plasma ANGPTL5 concentration and HOMA of β-cell function. The area under the curve was approximately 0.912 in receiver operating characteristic curve analysis.
CONCLUSIONS: The findings in the present study showed that plasma ANGPTL5 was more positively correlated with glucose metabolism disorders than with lipid metabolism disorders in patients with MS, which suggested that ANGPTL5 might serve as a potential and useful clinical predictor of MS.
Keywords: Glucose Metabolism Disorders, lipid metabolism disorders, Metabolic Syndrome X, Angiopoietin-like Proteins
Background
Metabolic syndrome (MS), also variously known as syndrome X, is a cluster of cardiovascular disease risk factors that is manifested in the clinical syndromes of obesity, dyslipidemia, hyperglycemia, and hypertension [1]. As it progresses, it promotes the occurrence and development of cardiovascular diseases such as type 2 diabetes, nonalcoholic fatty liver disease, and some tumors [2,3]. Cases of MS have rapidly increased, so effective diagnostic and therapeutic approaches are of great clinical value for the prevention and treatment of MS [1]. Currently, biomarkers are widely used in clinical diagnosis, evaluation, and prognosis [4–6]. Therefore, exploring novel biomarkers for MS has important clinical value that could further promote diagnosis and treatment strategies for MS.
A novel family of proteins has been identified and recognized as “angiopoietinlike proteins” (ANGPTLs), which exhibit structural similarities to antigenic-regulating factors [7–9]. Many studies have found that the ANGPTL family has autocrine or paracrine activities in endocrine metabolism such as lipid regulation, glucose metabolism, inflammation, and angiogenesis [10–13]. ANGPTL3, ANGPTL4, and ANGPTL8 have been confirmed to regulate serum triacylglycerol levels, which are potential targets for reducing triacylglycerol levels and improving lipid metabolism-related diseases [14–16]. Additionally, reducing the levels of ANGPTL4 and ANGPTL8 could improve glucose tolerance [11]. Therefore, ANGPTLs as predictive biomarkers related to glucose and lipid metabolism have become current research hot spots in metabolic diseases.
ANGPTL5 was extracted by Zeng et al. in 2003 [17]. Similar to others, ANGPTL5 has a classic N-terminal coil-coillike domain and a C-terminal fibrinogenlike domain [13]. Loss-of-function mutations of ANGPTL5, ANGPTL3, and ANGPTL4 could significantly reduce the plasma triglyceride (TG) concentration, which suggested that ANGPTL5 may be closely related to regulation of TGs [18]. Recently, Alghanim et al. found that compared with nonobese type 2 diabetes patients, the plasma ANGPTL5 concentration was increased in obese patients with type 2 diabetes. It was also positively correlated with fasting plasma glucose (FPG), TG, and homeostatic model assessment of insulin resistance (HOMA-IR) [19]. These suggest that ANGPTL5 may be related to glucose and lipid metabolism, obesity, and diabetes, and is expected to become one of the important biomarkers for the above diseases. Therefore, the present study aimed to detect plasma ANGPTL5 levels in patients with MS and further investigate the correlations of ANGPTL5 with MS-related components such as glucose and lipid profiles and obesity indicators.
Material and Methods
STUDY POPULATION:
The study included 139 patients, 70 with MS and 69 without MS, who were recruited from June 2018 to June 2019 in the Department of Cardiology at Renmin Hospital of Wuhan University (Wuhan, China). The present study was approved by the Medical Ethics Review Committee of Renmin Hospital and was conducted in line with the principles of the Declaration of Helsinki.
The inclusion criteria for MS patients in the study were the presence of 3 or more of the following: (1) central obesity, waist ≥90 cm (men) or ≥80 cm (women); (2) hypertriglyceridemia, TG ≥1.7 mmol/L; (3) high-density lipoprotein cholesterol (HDL-C) <1.04 mmol/L (men) or <1.30 mmol/L (women); (4) blood pressure ≥130/85 mmHg; (5) blood glucose >5.6 mmol/L [20]. Individuals were excluded if they had other severe illnesses such as thyroid disease, tuberculosis, liver and kidney dysfunction, malignant tumor, blood disease, infectious disease, or autoimmune disease.
All subjects were examined for the presence of diabetes, hypertension, cardiovascular disease, history of smoking, and family histories. Height, weight, and waist circumference were measured. After the measurement of height and weight, the calculation of body mass index (BMI) was achieved by dividing the weight (kg) by the squared height (m2). Insulin resistance was calculated using the HOMA-IR formula: FPG (mmol/L)×fasting insulin (FINS, (μU/mL)/22.5, and the calculation of HOMA of β-cell function (HOMA-β) was achieved by the following formula: 20×FINS (μU/mL)/(FPG [mmol/L]–3.5)×100%.
SAMPLE PREPARATION:
Blood was collected intravenously in the morning after overnight fasting within 24 h after hospital admission. Venous blood samples were collected into tubes and centrifuged at 3500 revolutions per minute for 15 min at room temperature. Next, the plasma was separated and then stored at −80°C until measurement.
MEASUREMENT OF BIOCHEMICAL PARAMETERS:
Concentrations of total cholesterol (TC), TG, HDL-C, low-density lipoprotein cholesterol (LDL-C), and glucose were measured using enzymatic methods with the Siemens Advia 2400 biochemistry analyzer. Concentration of high-sensitivity C-reactive protein (hs-CRP) was detected using a polyethylene glycol-enhanced immunoturbidimetric assay. Double antigen sandwich chemiluminescence detection was applied for insulin. High-performance liquid affinity chromatography was used for investigation of glycated hemoglobin (HbA1c). To assess the plasma level of human ANGPTL5, we adopted commercial enzyme-linked immunosorbent assay kits purchased from ELK Biotechnology (catalog no.: ELK8375). The test principle of this kit was sandwich enzyme immunoassay. The range of values detected by this assay was 62.5–4000 pg/mL. All measurements of plasma ANGPTL5 were performed in duplicate for each sample.
STATISTICAL ANALYSIS:
SPSS 22.0 (IBM, Armonk, NY, USA) and Graphpad Prism 8.0 were used for the statistical analysis. Data for continuous variables were summarized as mean value±standard deviation (SD), and categorical data were expressed as percentages or frequency. In comparisons between 2 groups, the statistical significance of differences in continuous variables was assessed using the independent-sample
Results
CHARACTERISTICS OF THE STUDY POPULATION:
The demographic and clinical characteristics of the subjects included in the present study are summarized in Table 1. In the obesity parameters, MS patients showed higher waist circumference, waist-hip ratio (WHR), and BMI. For glucose metabolism, the MS population displayed unfavorable glucose profiles, with higher concentrations of FPG, FINS, HbA1C, and HOMA-IR, and lower HOMA-β. Additionally, the MS individuals had unfavorable lipid profiles, with higher TC, TG, and LDL-C, and lower HDL-C levels. Plasma ANGPTL5 concentration of the MS group was nearly twice that of the non-MS group (Figure 1A). These results indicate that the MS subjects presented features of obesity, hyperlipidemia, abnormal glucose metabolism, and elevated plasma ANGPTL5.
PLASMA ANGPTL5 LEVEL ELEVATED IN SUBJECTS WITH GLUCOSE DISORDERS:
It was found that the plasma ANGPTL5 concentration of the diabetes patients was significantly higher than that of subjects without diabetes (Figure 1B). The ANGPTL5 level in the diabetes group was also higher than that of the prediabetes group (Figure 1C).
ELEVATED PLASMA ANGPTL5 MORE POSITIVELY CORRELATED WITH GLUCOSE METABOLISM DISORDERS:
Associations between plasma ANGPTL5 concentration and laboratory parameters were assessed. In unadjusted analyses, ANGPTL5 was strongly positively correlated with waist circumference, WHR, BMI, FPG, FINS, HbA1c, TC, TG, LDL-C, and HOMA-IR. ANGPTL5 had negative correlations with HDL-C and HOMA-β (Table 2, Figure 2). However, ANGPTL5 had no correlation with laboratory parameters including obesity and lipid and glucose metabolism in the non-MS group (Table 2).
As ANGPTL5 was significantly elevated in subjects with glucose disorders, this study further investigated the correlations of ANGPTL5 and lipid profiles after controlling for glucose profiles, and then again glucose profile correlations after controlling for lipid profiles. After adjustment of age and glucose profiles, ANGPTL5 was positively correlated with BMI, waist circumference, and WHR, but weakly negatively correlated with HDL-C (r=−0.180, P=0.039). Of interest, after adjustment for age and lipid profiles, ANGPTL5 was still strongly positively correlated with FPG (r=0.525, P<0.001), FINS (r=0.390, P<0.001), HbA1c (r=0.443, P<0.001), and HOMA-IR (r=0.556, P<0.001), whereas it showed a strong negative correlation with HOMA-β (r=−0.360, P<0.001) (Table 3). All of the above results indicated that elevated plasma ANGPTL5 presented a stronger association with glucose metabolism disorders than with lipid disorders.
MULTIVARIATE LINEAR REGRESSION ANALYSES:
As Table 4 shows, in the model of multiple linear regression, with MS-related indicators as the independent variable and ANGPTL5 as the dependent variable, ANGPTL5 was strongly correlated with these parameters, including FPG and HOMA-β (F=50.435, P<0.001, adjusted R2=0.591). These data further reveal that ANGPTL5 was more likely correlated with glucose metabolism in MS subjects.
MULTIVARIATE LOGISTIC REGRESSION ANALYSES:
Different logistic regression models were applied to assess the association between plasma concentration of ANGPTL5 and MS (Table 5). In unadjusted analysis, ANGPTL5 concentration was associated with the presence of MS; the odds ratio (OR) per SD increase was 1.026 (95% confidence interval [CI] 1.018–1.035, P<0.001). The association persisted after adjustment for conventional MS risk indicators including sex, age, BMI, family history of diabetes, family history of hypertension, smoking, and hs-CRP; the OR per SD increase was 1.044 (95% CI 1.013–1.075, P=0.005). Furthermore, to assess the incremental power of ANGPTL5, ROC curve analysis was performed. As shown in Figure 3, the area under the curve was approximately 0.912. Thus, plasma ANGPTL5 might be combined with other characteristics to help identify patients at higher risk of MS.
Discussion
Consistent with previous studies, when compared with non-MS individuals in the present study, subjects with MS were accompanied by a series of clinical symptoms of metabolic disorders such as central obesity, hypertension, hyperglycemia, insulin resistance, and dyslipidemia [1–3]. Most important, the present study was the first to evaluate the potential association between plasma ANGPTL5 and MS. It was observed that the plasma ANGPTL5 level was elevated in MS subjects in a cohort of the Chinese population. ANGPTL5 concentration was also increased in subjects with glucose disorders. Plasma ANGPTL5 concentration was positively associated with the parameters of glucose metabolism disorders even after adjustment for lipid factors.
In 2019, Alghanim et al. found that the plasma ANGPTL5 concentration of obese patients was higher than that of nonobese patients; compared with nonobese patients with type 2 diabetes, the plasma ANGPTL5 concentration was significantly higher in obese patients with type 2 diabetes, which was closely related to insulin resistance [19]. In 2020, it was further found that ANGPTL5 levels were elevated in obese adolescents, and associated with cardiovascular disease risk factors including hs-CRP and oxidized LDL [21]. It jointly suggested that the concentration of ANGPTL5 might be strongly correlated with obesity, diabetes, and lipid metabolism, and is expected to become a powerful biomarker or an important therapeutic tool for metabolic diseases. However, the role and mechanism of ANGPTL5 in the above metabolic diseases need to be discussed in depth.
ANGPTL5 has a classic N-terminal coil-coillike domain and a C-terminal fibrinogenlike domain [13]. As mentioned before, loss-of-function mutations of ANGPTL5, ANGPTL3, and ANGPTL4 could significantly reduce the level of TG; however, whether the mechanism of ANGPTL5 in mediating metabolism is closely related to ANGPTL3 or ANGPTL4 is still unknown [18]. ANGPTL3 is known as the downstream target of the liver X receptor (LXR), which plays a critical role in lipid metabolism by regulating the expression of ANGPTL3 [22]. When treated with LXR activator T0901317, the concentration of ANGPTL3 in HepG2 cells was elevated significantly, and the levels of TC and TG were also markedly increased [23]. Inducement of the expression of LXR in the liver by intervening LXR ligand could promote the production of ANGPTL3 and fatty acid enzymes, which leads to a large accumulation of TG in mice. However, when the LXR ligands interfered, it did not cause the development of hypertriglyceridemia in ANGPTL3-deficient mice. Additionally, ANGPTL3 could also significantly inhibit the activity of lipoprotein lipase (LPL), which then could lead to a significant increase in TG [24]. Similarly, ANGPTL4 is a potent LPL inhibitor, and plays an important role in regulating LPL activity. ANGPTL4-null mice exhibited lower plasma TG and increased plasma LPL activity; conversely, transgenic overexpression of ANGPTL4 increased plasma TG and inhibited the activity of LPL [25]. However, here, it was found that ANGPTL5 was weakly correlated with HDL-C when controlling for the glucose profiles. ANGPTL5 presented more correlation with glucose and insulin metabolism than that of TG and other lipid profiles. In other words, differently from ANGPTL3 and ANGPTL4, ANGPTL5 might regulate lipid metabolism through other pathways in the process of MS.
Free fatty acid (FFA) is an important factor leading to insulin resistance. It has been reported that ANGPTL3 can decompose fat cells; the decomposed fat cells release a large amount of FFA [26]. The accumulated FFA will affect glucose metabolism, which then could result in the occurrence of insulin resistance. The expression of ANGPTL3 was significantly increased in the liver of insulin-deficient mice, and the injection of insulin could gradually decrease the level of ANGPTL3 and control the blood glucose within the normal range in the insulin-deficient mice. Insulin sensitivity was increased in ANGPTL3 knockout mice, indicating that ANGPTL3 could affect insulin sensitivity and then play an important role in the process of glucose metabolism [27]. Further, we found that plasma ANGPTL5 was more correlated with glucose disorders. Collectively, this indicates that the role and mechanism of ANGPTL5 in insulin resistance and insulin sensitivity can be observed, which then can reveal information on its role and mechanism in glucose metabolism in the process of MS.
However, certain limitations exist in the present study. First, a limited number of MS patients were recruited at a single center. Although we have proposed the association of the ANGPTL5 level with MS-related factors in Chinese patients, this has prevented us from drawing conclusions about the causal relationship between the ANGPTL5 level and MS pathogenesis. Therefore, future prospective studies with large-scale populations or other genetically distinct populations will be needed, which can then be applied to determine at what point ANGPTL5 concentration begins to rise to enable early diagnosis or assessment of MS. This will help determine the role of ANGPTL5 in the pathophysiological mechanism of MS. Second, MS is a common cause of many chronic diseases including macrovascular diseases, cerebrovascular diseases, and microvascular diseases, which can cause damage to important organs such as the heart, brain, kidney, and liver. Therefore, the correlations between elevated ANGPTL5 levels and various components or survival-indicating factors (such as B-type natriuretic peptide, proteinuria) of MS should be further investigated. This study could not determine which biochemical factors might be responsible for elevated plasma ANGPTL5 level in MS patients. In other words, upstream factors involved in the regulation of ANGPTL5 expression are little known, and focused studies to delineate the potential regulatory mechanism are required.
Conclusions
In summary, plasma ANGPTL5 level is elevated in MS patients. The results of the present study suggest that elevated plasma ANGPTL5 concentration is more associated with the parameters of glucose metabolism disorders than with lipid factors, and is expected to become one of the novel biomarkers for evaluating glucose metabolism disorders in MS subjects.
Figures
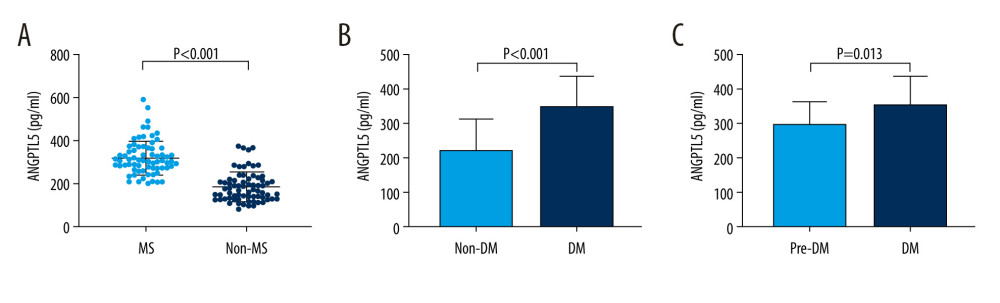 Figure 1. Characterization of plasma angiopoietinlike protein 5 (ANGPTL5) levels in patients with metabolic syndrome (MS) or without MS. (A) Level of plasma ANGPTL5 in the MS group and the non-MS group. (B) Plasma ANGPTL5 concentration of the diabetes and the non-diabetes subjects. (C) Plasma ANGPTL5 level of patients with diabetes and prediabetes.
Figure 1. Characterization of plasma angiopoietinlike protein 5 (ANGPTL5) levels in patients with metabolic syndrome (MS) or without MS. (A) Level of plasma ANGPTL5 in the MS group and the non-MS group. (B) Plasma ANGPTL5 concentration of the diabetes and the non-diabetes subjects. (C) Plasma ANGPTL5 level of patients with diabetes and prediabetes. 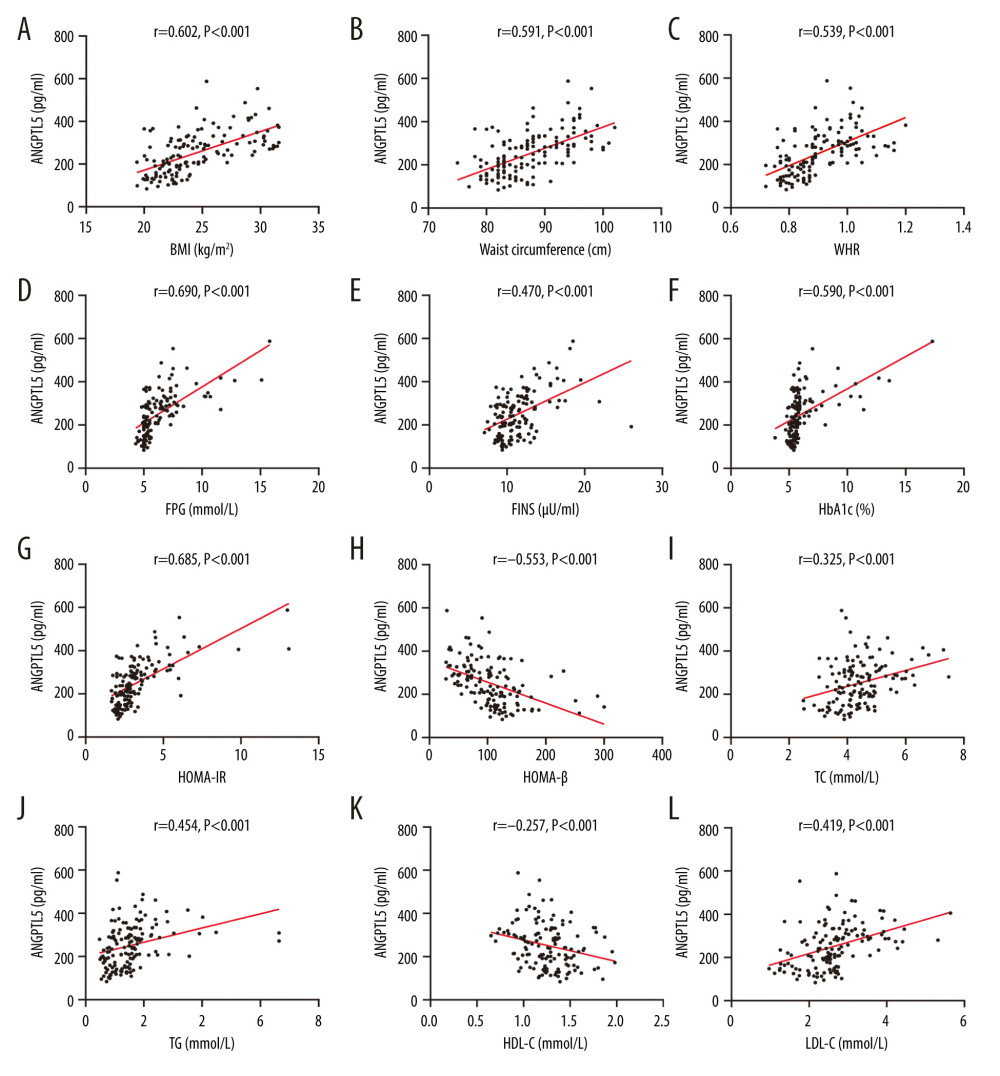 Figure 2. (A–L) Correlations between angiopoietinlike protein 5 level and obesity, glucose, and lipid metabolism indicators in participants.
Figure 2. (A–L) Correlations between angiopoietinlike protein 5 level and obesity, glucose, and lipid metabolism indicators in participants. 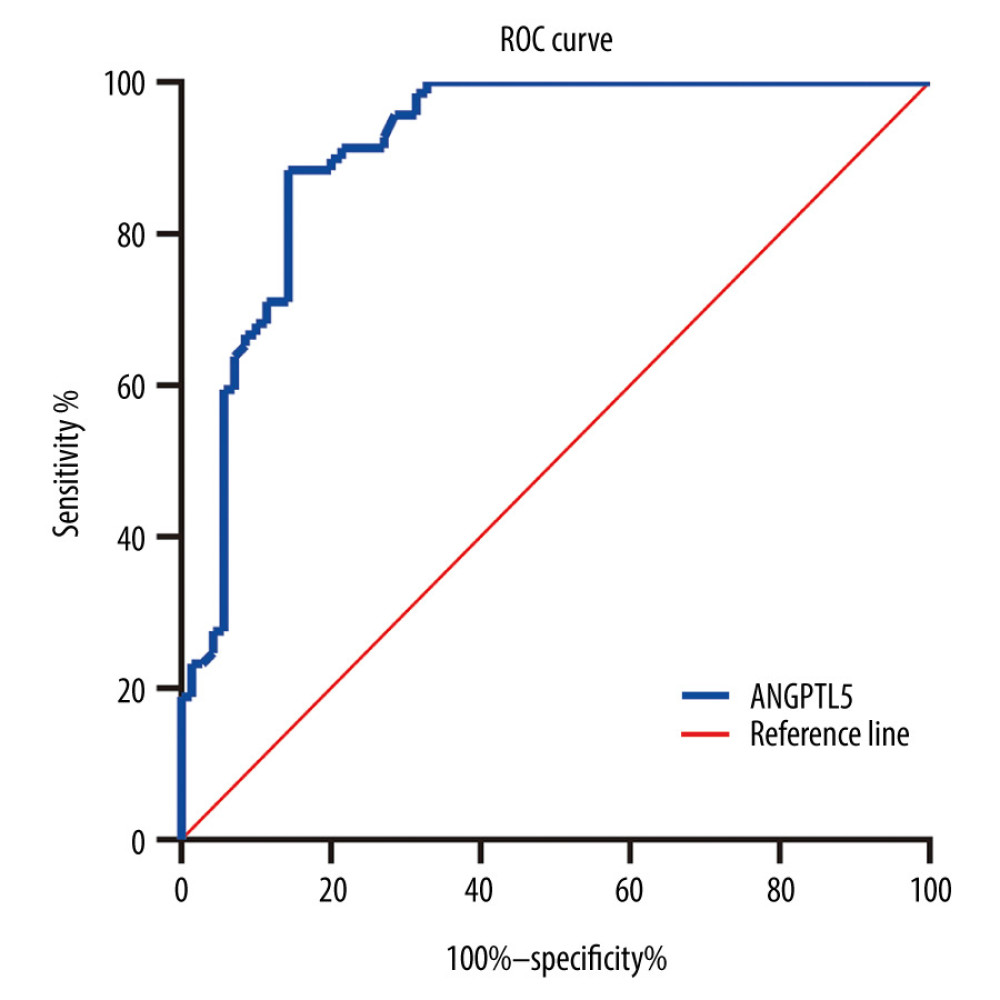 Figure 3. Receiver operating characteristic curve of angiopoietinlike protein 5 (ANGPTL5) to identify patients at higher risk of metabolic syndrome. ANGPTL5: area under the curve=0.912, P<0.001, 95% confidence interval 0.862–0.962.
Figure 3. Receiver operating characteristic curve of angiopoietinlike protein 5 (ANGPTL5) to identify patients at higher risk of metabolic syndrome. ANGPTL5: area under the curve=0.912, P<0.001, 95% confidence interval 0.862–0.962. Tables
Table 1. Demographic and clinical characteristics of subjects included.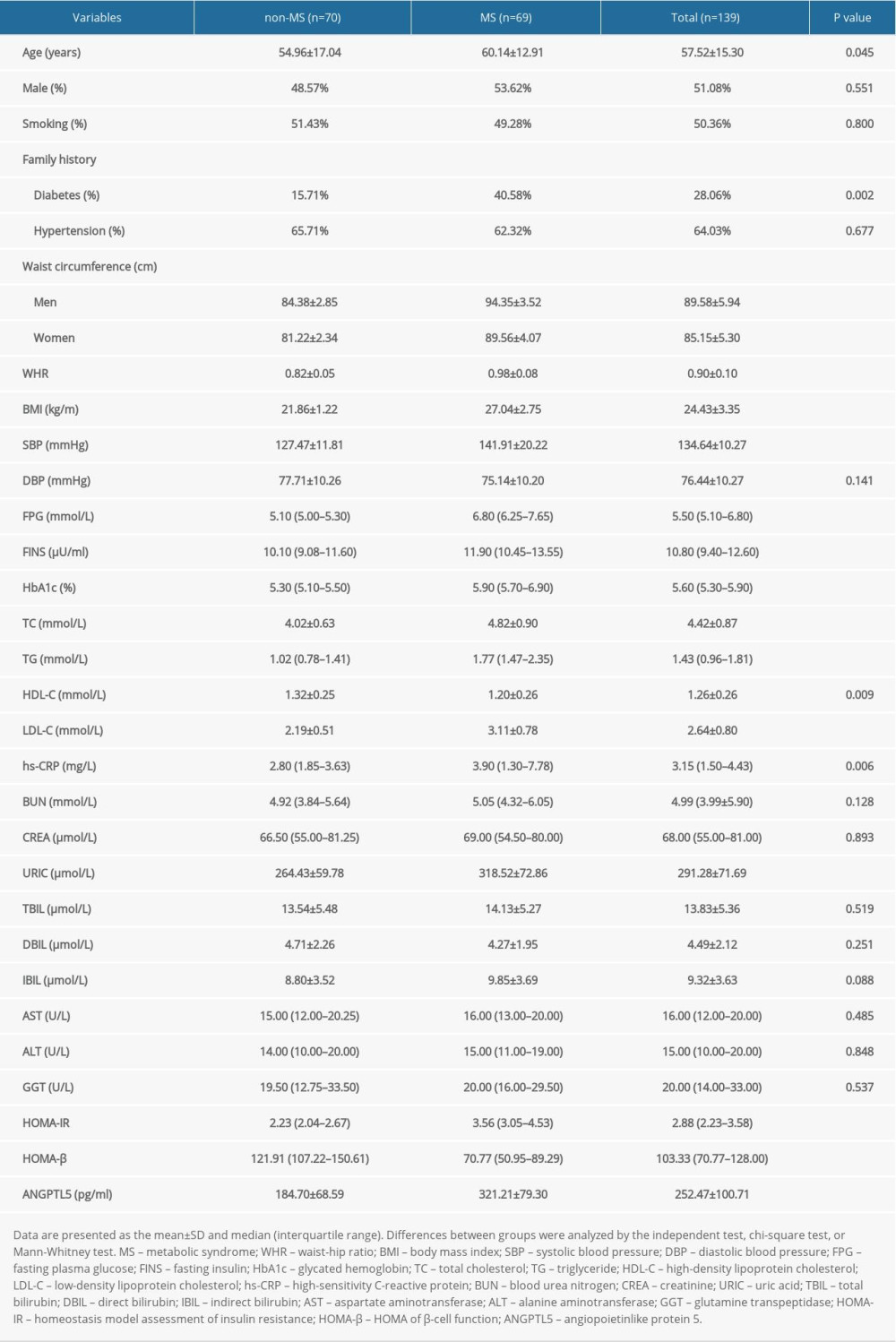 Table 2. Correlations of plasma angiopoietinlike protein 5 (ANGPTL5) with laboratory parameters in patients with metabolic syndrome (MS).
Table 2. Correlations of plasma angiopoietinlike protein 5 (ANGPTL5) with laboratory parameters in patients with metabolic syndrome (MS).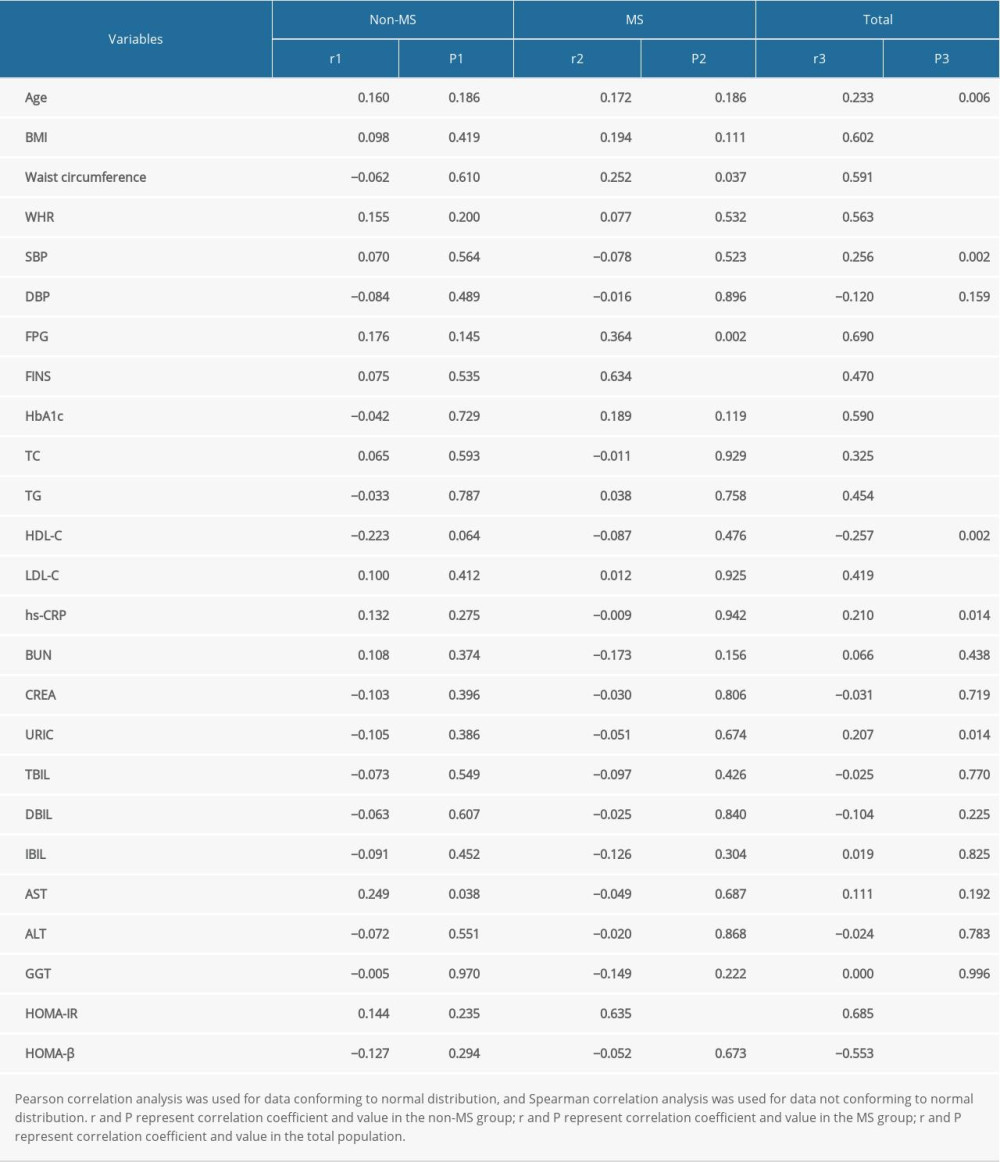 Table 3. Correlations of plasma angiopoietinlike protein 5 (ANGPTL5) with laboratory parameters after controlling for the lipid or glucose profiles.
Table 3. Correlations of plasma angiopoietinlike protein 5 (ANGPTL5) with laboratory parameters after controlling for the lipid or glucose profiles.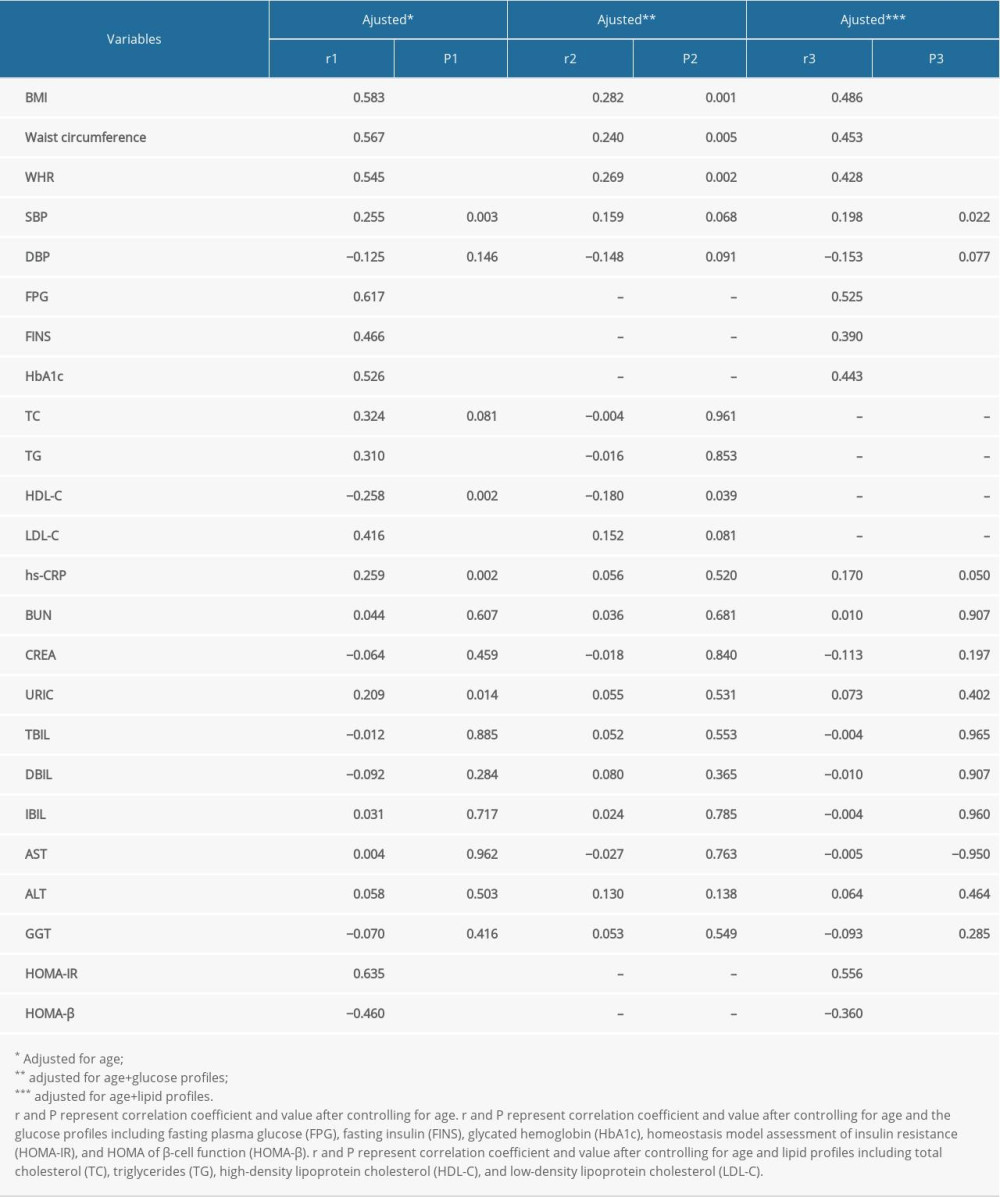 Table 4. Multivariate linear regression to examine association of metabolic syndrome (MS)-related indicators with plasma angiopoietinlike protein 5 (ANGPTL5).
Table 4. Multivariate linear regression to examine association of metabolic syndrome (MS)-related indicators with plasma angiopoietinlike protein 5 (ANGPTL5).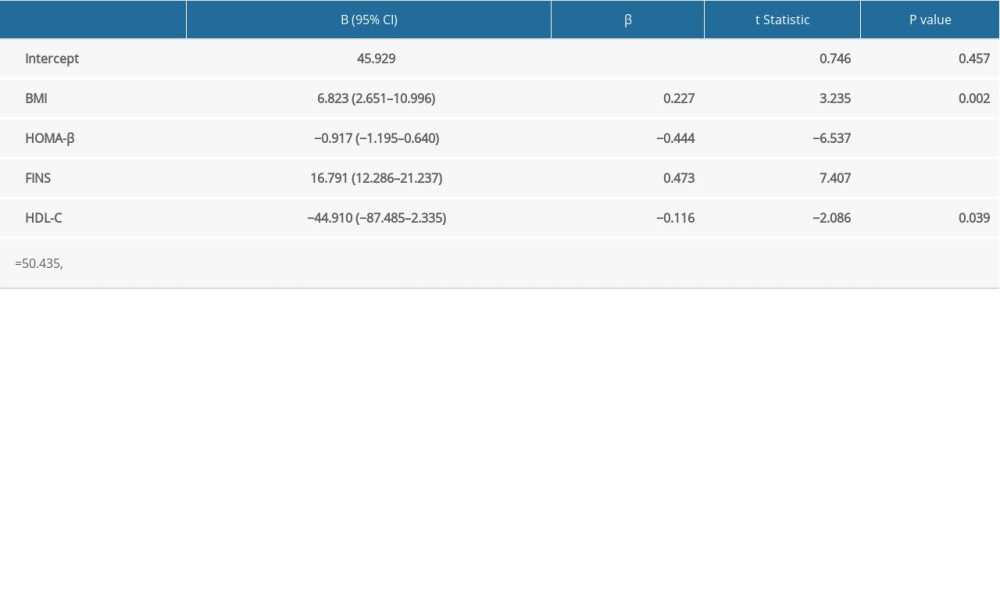 Table 5. Multivariate logistic regression to assess association of plasma angiopoietinlike protein 5 (ANGPTL5) with the risk of metabolic syndrome (MS).
Table 5. Multivariate logistic regression to assess association of plasma angiopoietinlike protein 5 (ANGPTL5) with the risk of metabolic syndrome (MS).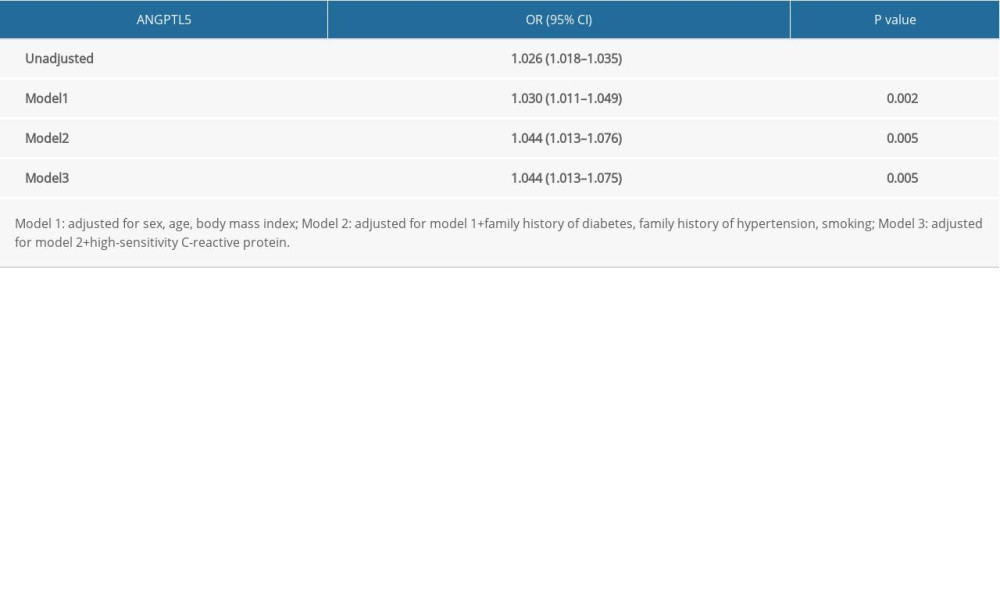
References
1. Saklayen MG, The global epidemic of the metabolic syndrome: Curr Hypertens Rep, 2018; 20; 12
2. Grundy SM, Metabolic syndrome pandemic: Arterioscler Thromb Vasc Biol, 2008; 28; 629-36
3. Kassi E, Pervanidou P, Kaltsas G, Metabolic syndrome: Definitions and controversies: BMC Med, 2011; 9; 48
4. Barrea L, Annunziata G, Muscogiuri G, Trimethylamine-N-oxide (TMAO) as novel potential biomarker of early predictors of metabolic syndrome: Nutrients, 2018; 10; 1971
5. Chen PY, Cripps AW, West NP, A correlation-based network for biomarker discovery in obesity with metabolic syndrome: BMC Bioinformatics, 2019; 20; 477
6. Ghadge AA, Khaire AA, Leptin as a predictive marker for metabolic syndrome: Cytokine, 2019; 121; 154735
7. Dijk W, Kersten S, Regulation of lipid metabolism by angiopoietin-like proteins: Curr Opin Lipidol, 2016; 27; 249-56
8. Santulli G, Angiopoietin-like proteins: A comprehensive look: Front Endocrinol (Lausanne), 2014; 5; 4
9. Zheng J, Umikawa M, Cui C, Inhibitory receptors bind ANGPTLs and support blood stem cells and leukaemia development: Nature, 2012; 485; 656-60
10. Barja-Fernandez S, Folgueira C, Castelao C, ANGPTL-4 is associated with obesity and lipid profile in children and adolescents: Nutrients, 2019; 11; 1340
11. Davies BSJ, Can targeting ANGPTL proteins improve glucose tolerance?: Diabetologia, 2018; 61; 1277-81
12. Qin L, Zhang R, Yang S, Knockdown of ANGPTL-4 inhibits inflammatory response and extracellular matrix accumulation in glomerular mesangial cells cultured under high glucose condition: Artif Cells Nanomed Biotechnol, 2019; 47; 3368-73
13. Carbone C, Piro G, Merz V, Angiopoietin-like proteins in angiogenesis, inflammation and cancer: Int J Mol Sci, 2018; 19; 431
14. Xu YX, Redon V, Yu H, Role of angiopoietin-like 3 (ANGPTL3) in regulating plasma level of low-density lipoprotein cholesterol: Atherosclerosis, 2018; 268; 196-206
15. Cushing EM, Chi X, Sylvers KL, Angiopoietin-like 4 directs uptake of dietary fat away from adipose during fasting: Mol Metab, 2017; 6; 809-18
16. Kovrov O, Kristensen KK, Larsson E, On the mechanism of angiopoietin-like protein 8 for control of lipoprotein lipase activity: J Lipid Res, 2019; 60; 783-93
17. Zeng L, Dai J, Ying K, Identification of a novel human angiopoietin-like gene expressed mainly in heart: J Hum Genet, 2003; 48; 159-62
18. Miida T, Hirayama S, Impacts of angiopoietin-like proteins on lipoprotein metabolism and cardiovascular events: Curr Opin Lipidol, 2010; 21; 70-75
19. Alghanim G, Qaddoumi MG, Alhasawi N, Higher levels of ANGPTL5 in the circulation of subjects with obesity and type 2 diabetes are associated with insulin resistance: Front Endocrinol (Lausanne), 2019; 10; 495
20. Grundy SM, Cleeman JI, Daniels SR, Diagnosis and management of the metabolic syndrome: An American Heart Association/National Heart, Lung, and Blood Institute scientific statement: Executive Summary: Crit Pathw Cardiol, 2005; 4; 198-203
21. Hammad MM, Abu-Farha M, Al-Taiar A, Correlation of circulating ANGPTL5 levels with obesity, high sensitivity C-reactive protein and oxidized low-density lipoprotein in adolescents: Sci Rep, 2020; 10; 6330
22. Matsusue K, Miyoshi A, Yamano S, Ligand-activated PPARbeta efficiently represses the induction of LXR-dependent promoter activity through competition with RXR: Mol Cell Endocrinol, 2006; 256; 23-33
23. Kaplan R, Zhang T, Hernandez M, Regulation of the angiopoietin-like protein 3 gene by LXR: J Lipid Res, 2003; 44; 136-43
24. Inaba T, Matsuda M, Shimamura M, Angiopoietin-like protein 3 mediates hypertriglyceridemia induced by the liver X receptor: J Biol Chem, 2003; 278; 21344-51
25. Koster A, Chao YB, Mosior M, Transgenic angiopoietin-like (angptl)4 overexpression and targeted disruption of angptl4 and angptl3: Regulation of triglyceride metabolism: Endocrinology, 2005; 146; 4943-50
26. Shimamura M, Matsuda M, Kobayashi S, Angiopoietin-like protein 3, a hepatic secretory factor, activates lipolysis in adipocytes: Biochem Biophys Res Commun, 2003; 301; 604-9
27. Inukai K, Nakashima Y, Watanabe M, ANGPTL3 is increased in both insulin-deficient and -resistant diabetic states: Biochem Biophys Res Commun, 2004; 317; 1075-79
Figures
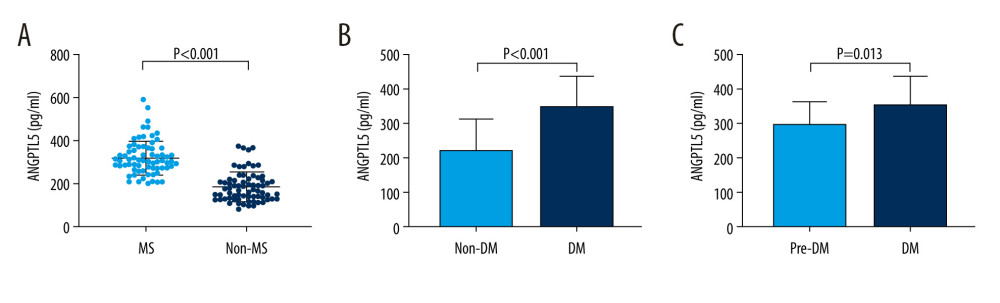 Figure 1. Characterization of plasma angiopoietinlike protein 5 (ANGPTL5) levels in patients with metabolic syndrome (MS) or without MS. (A) Level of plasma ANGPTL5 in the MS group and the non-MS group. (B) Plasma ANGPTL5 concentration of the diabetes and the non-diabetes subjects. (C) Plasma ANGPTL5 level of patients with diabetes and prediabetes.
Figure 1. Characterization of plasma angiopoietinlike protein 5 (ANGPTL5) levels in patients with metabolic syndrome (MS) or without MS. (A) Level of plasma ANGPTL5 in the MS group and the non-MS group. (B) Plasma ANGPTL5 concentration of the diabetes and the non-diabetes subjects. (C) Plasma ANGPTL5 level of patients with diabetes and prediabetes.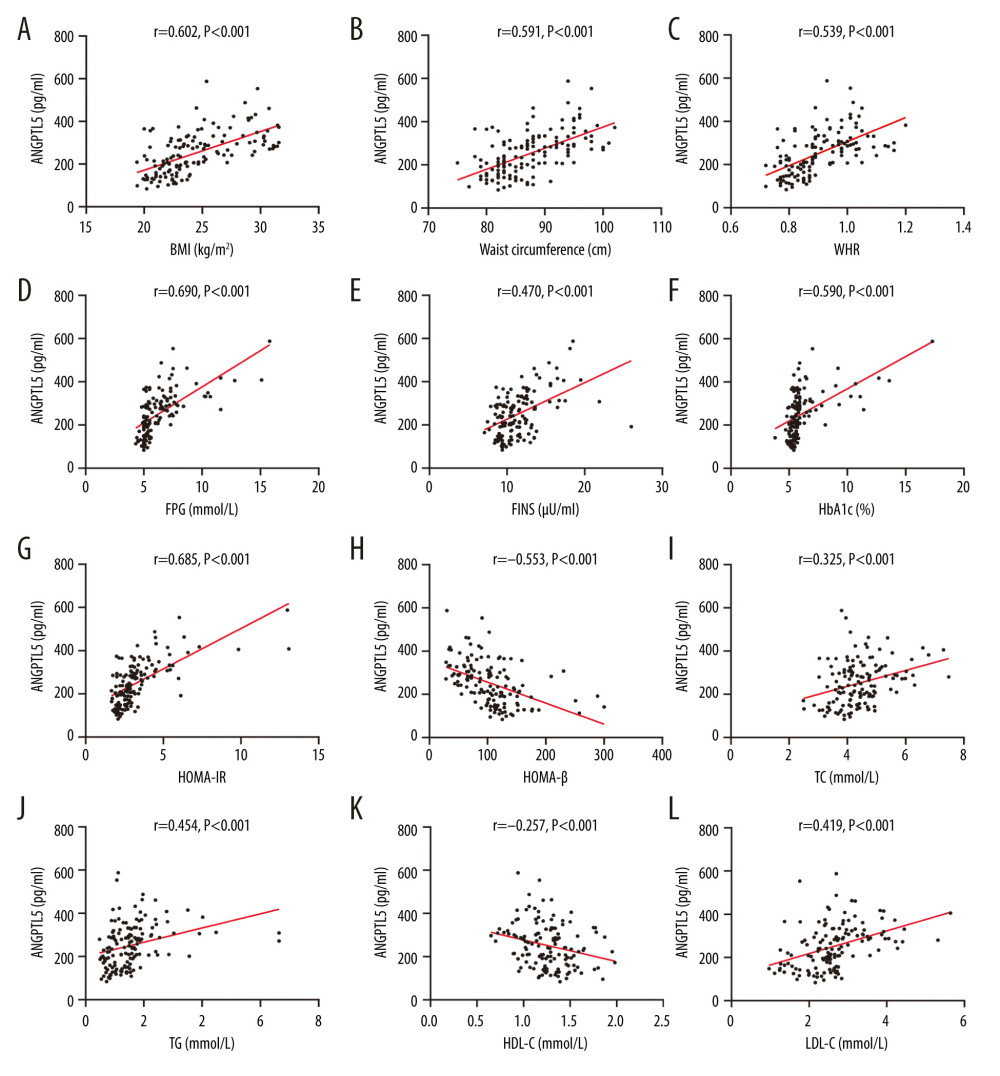 Figure 2. (A–L) Correlations between angiopoietinlike protein 5 level and obesity, glucose, and lipid metabolism indicators in participants.
Figure 2. (A–L) Correlations between angiopoietinlike protein 5 level and obesity, glucose, and lipid metabolism indicators in participants.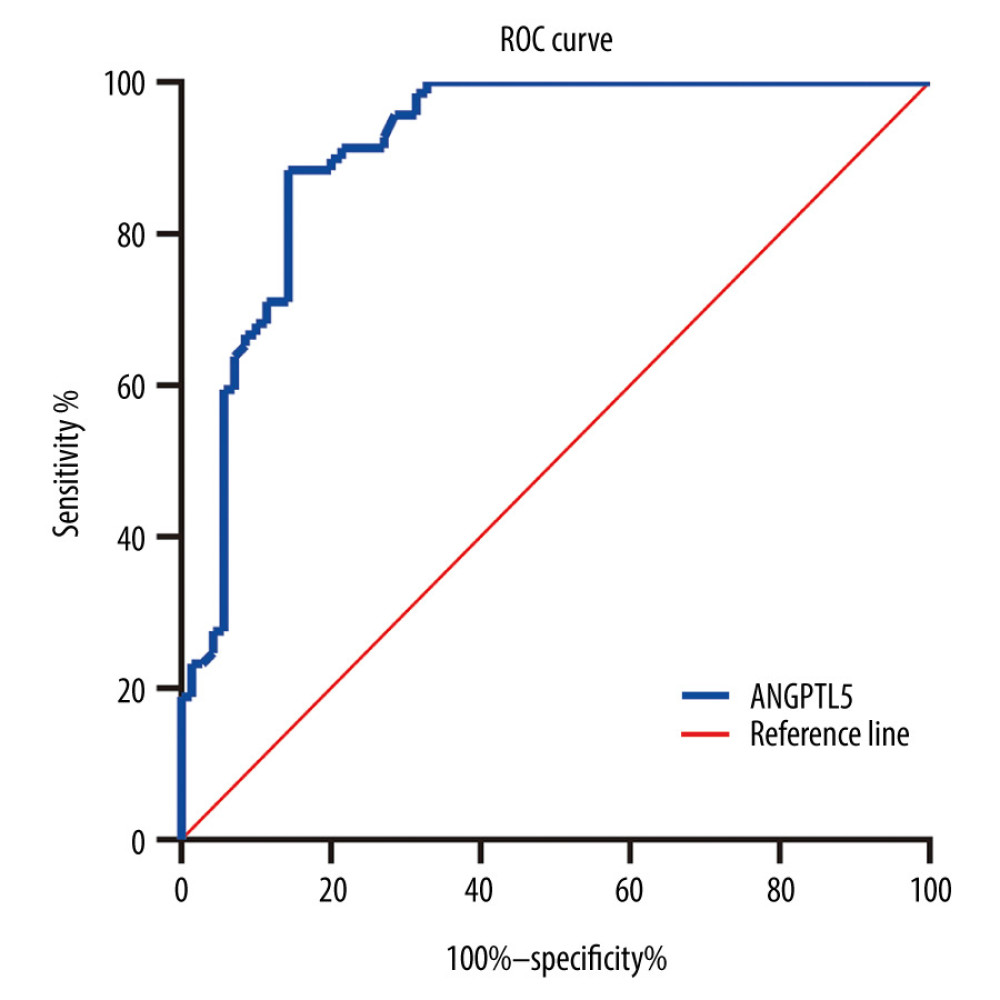 Figure 3. Receiver operating characteristic curve of angiopoietinlike protein 5 (ANGPTL5) to identify patients at higher risk of metabolic syndrome. ANGPTL5: area under the curve=0.912, P<0.001, 95% confidence interval 0.862–0.962.
Figure 3. Receiver operating characteristic curve of angiopoietinlike protein 5 (ANGPTL5) to identify patients at higher risk of metabolic syndrome. ANGPTL5: area under the curve=0.912, P<0.001, 95% confidence interval 0.862–0.962. Tables
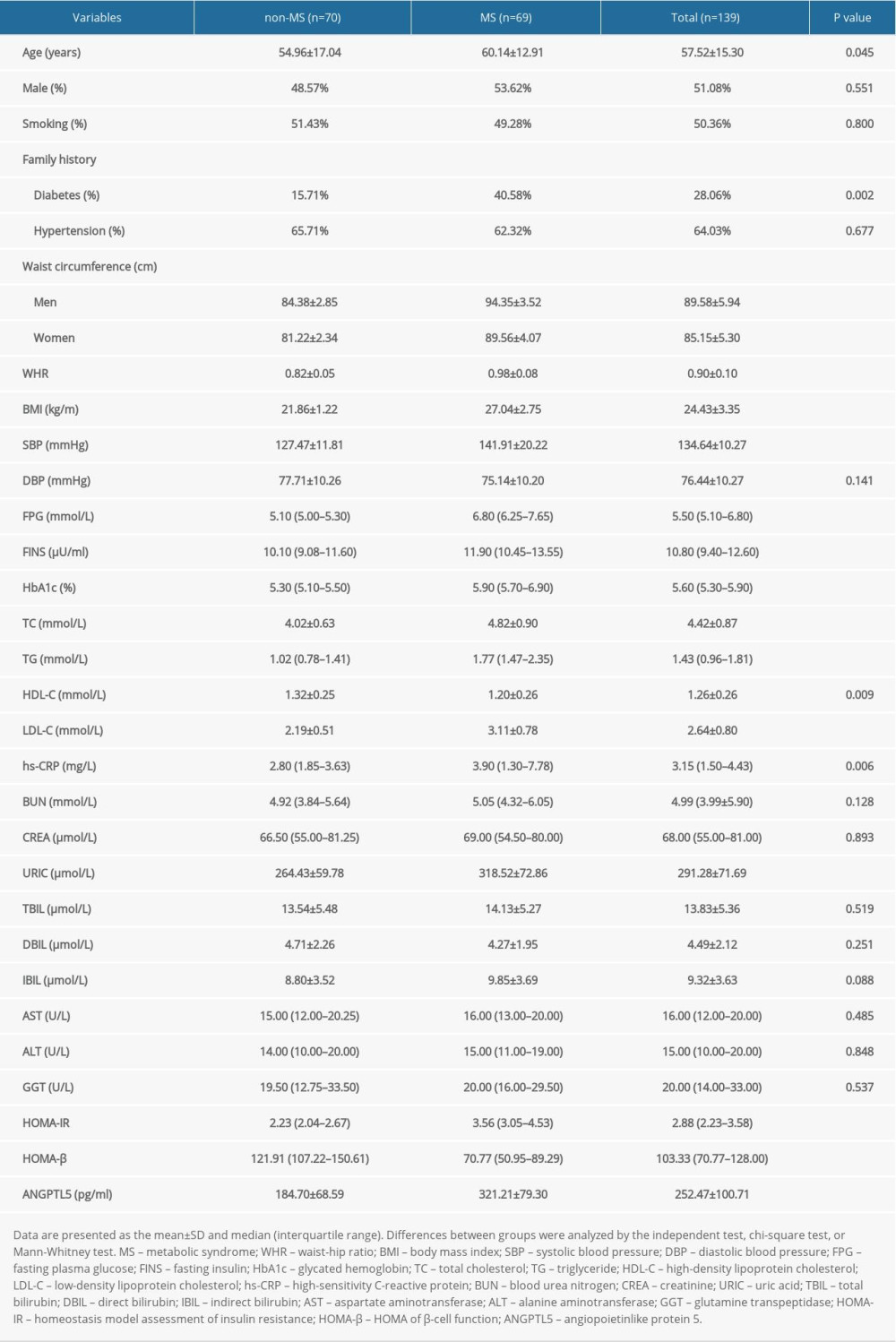 Table 1. Demographic and clinical characteristics of subjects included.
Table 1. Demographic and clinical characteristics of subjects included.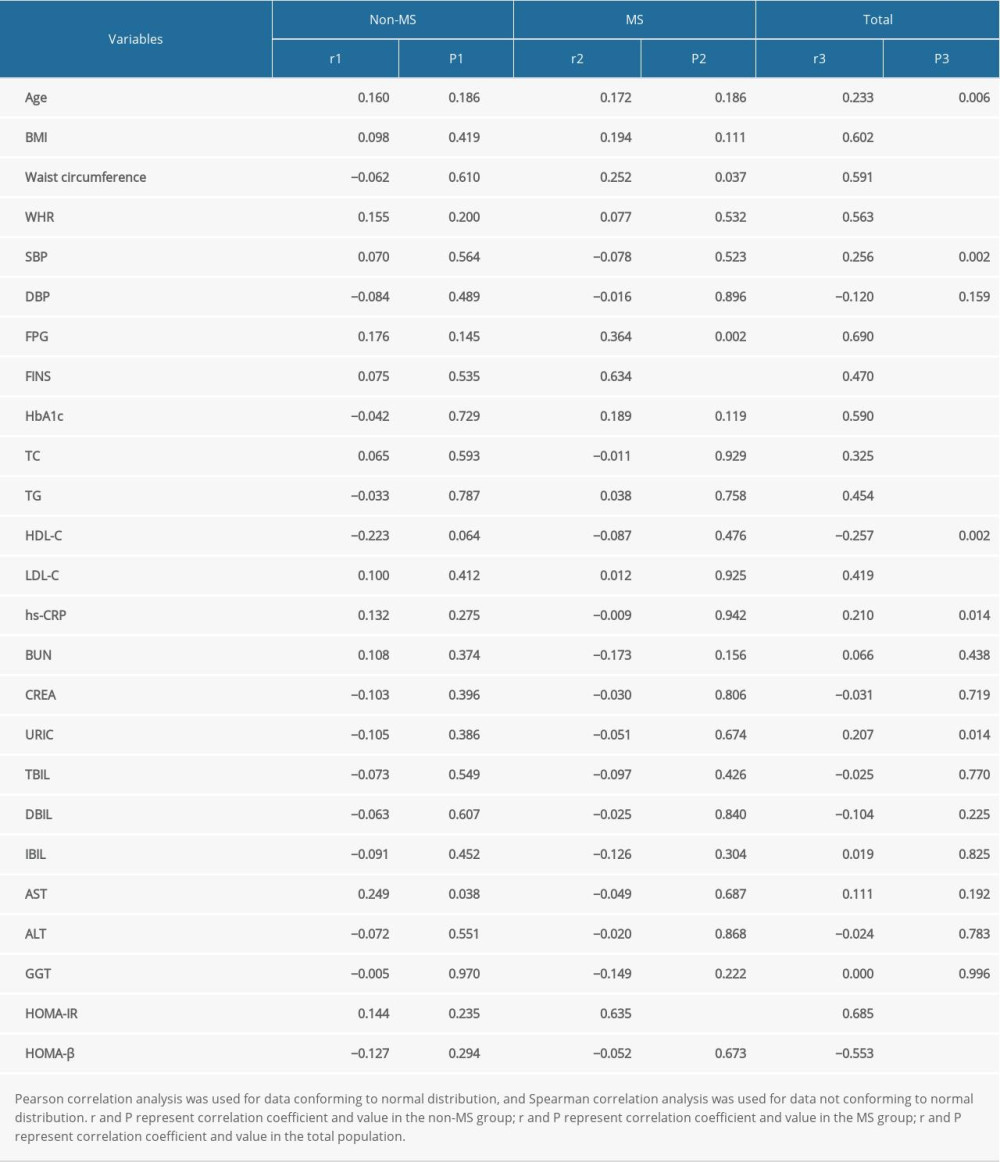 Table 2. Correlations of plasma angiopoietinlike protein 5 (ANGPTL5) with laboratory parameters in patients with metabolic syndrome (MS).
Table 2. Correlations of plasma angiopoietinlike protein 5 (ANGPTL5) with laboratory parameters in patients with metabolic syndrome (MS).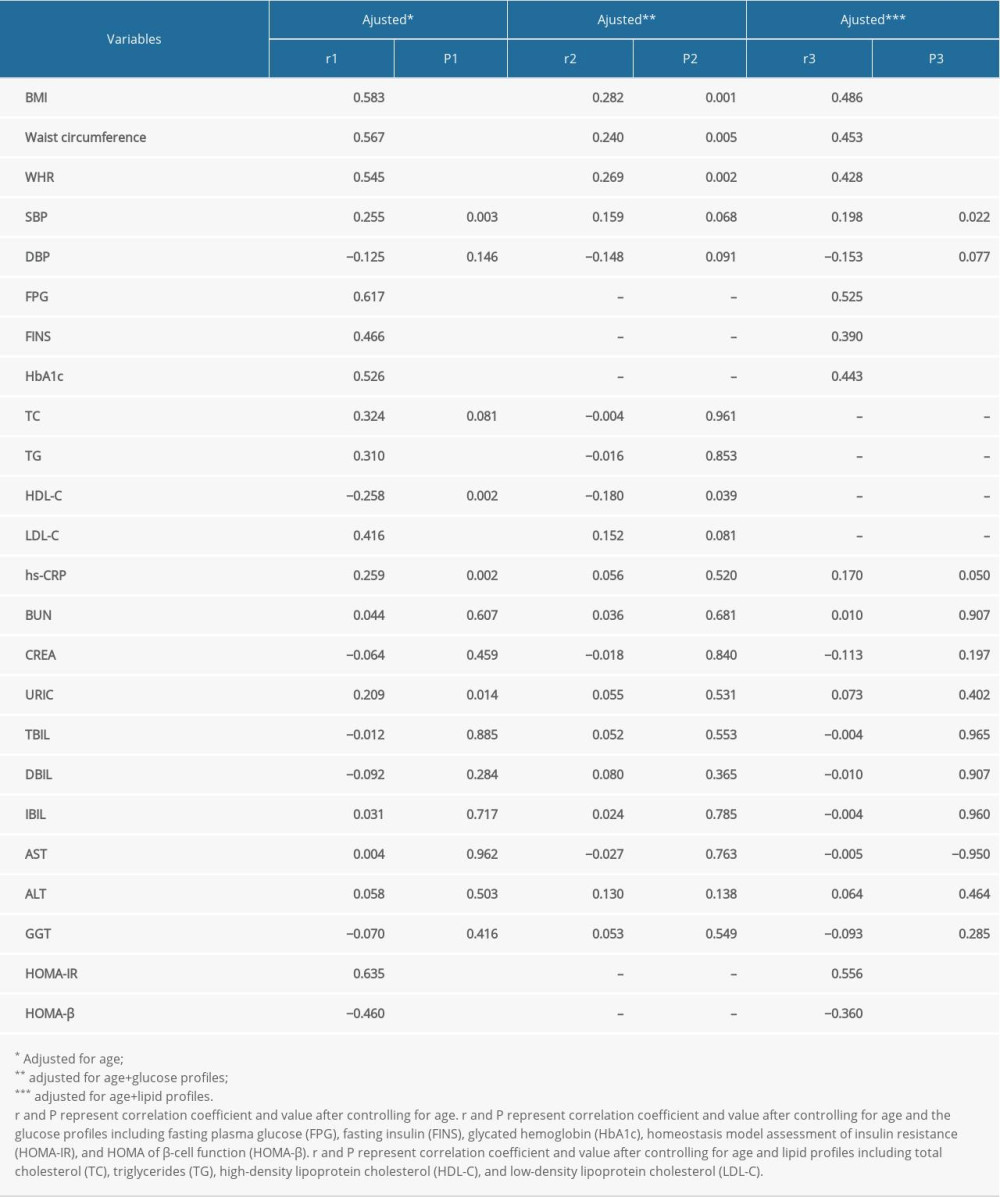 Table 3. Correlations of plasma angiopoietinlike protein 5 (ANGPTL5) with laboratory parameters after controlling for the lipid or glucose profiles.
Table 3. Correlations of plasma angiopoietinlike protein 5 (ANGPTL5) with laboratory parameters after controlling for the lipid or glucose profiles.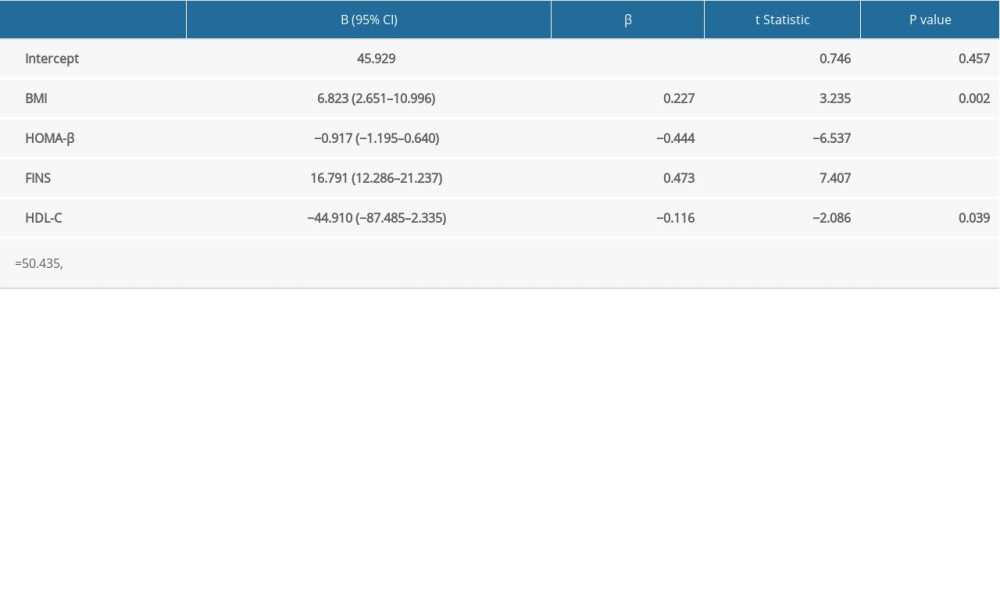 Table 4. Multivariate linear regression to examine association of metabolic syndrome (MS)-related indicators with plasma angiopoietinlike protein 5 (ANGPTL5).
Table 4. Multivariate linear regression to examine association of metabolic syndrome (MS)-related indicators with plasma angiopoietinlike protein 5 (ANGPTL5).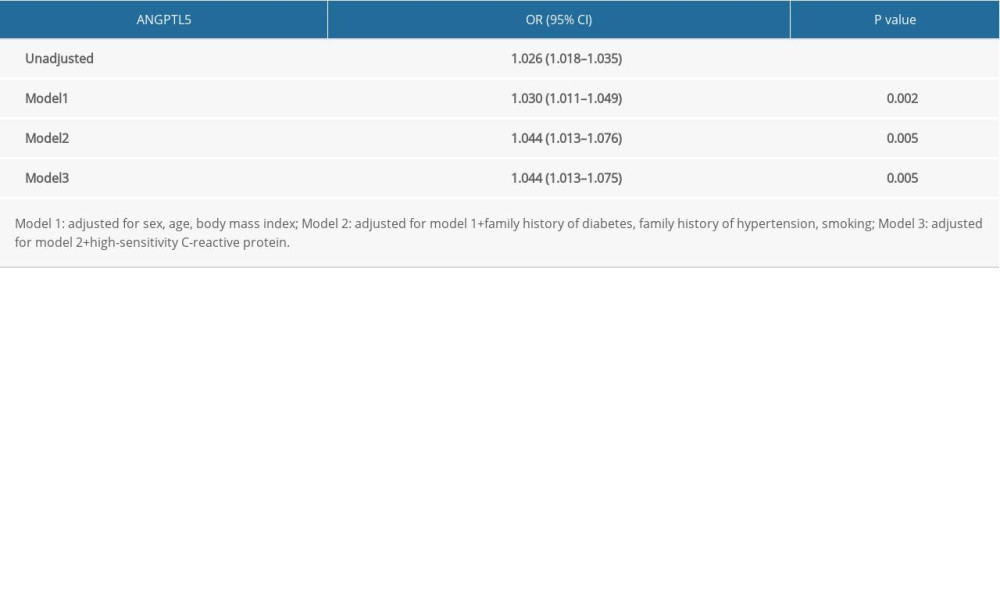 Table 5. Multivariate logistic regression to assess association of plasma angiopoietinlike protein 5 (ANGPTL5) with the risk of metabolic syndrome (MS).
Table 5. Multivariate logistic regression to assess association of plasma angiopoietinlike protein 5 (ANGPTL5) with the risk of metabolic syndrome (MS).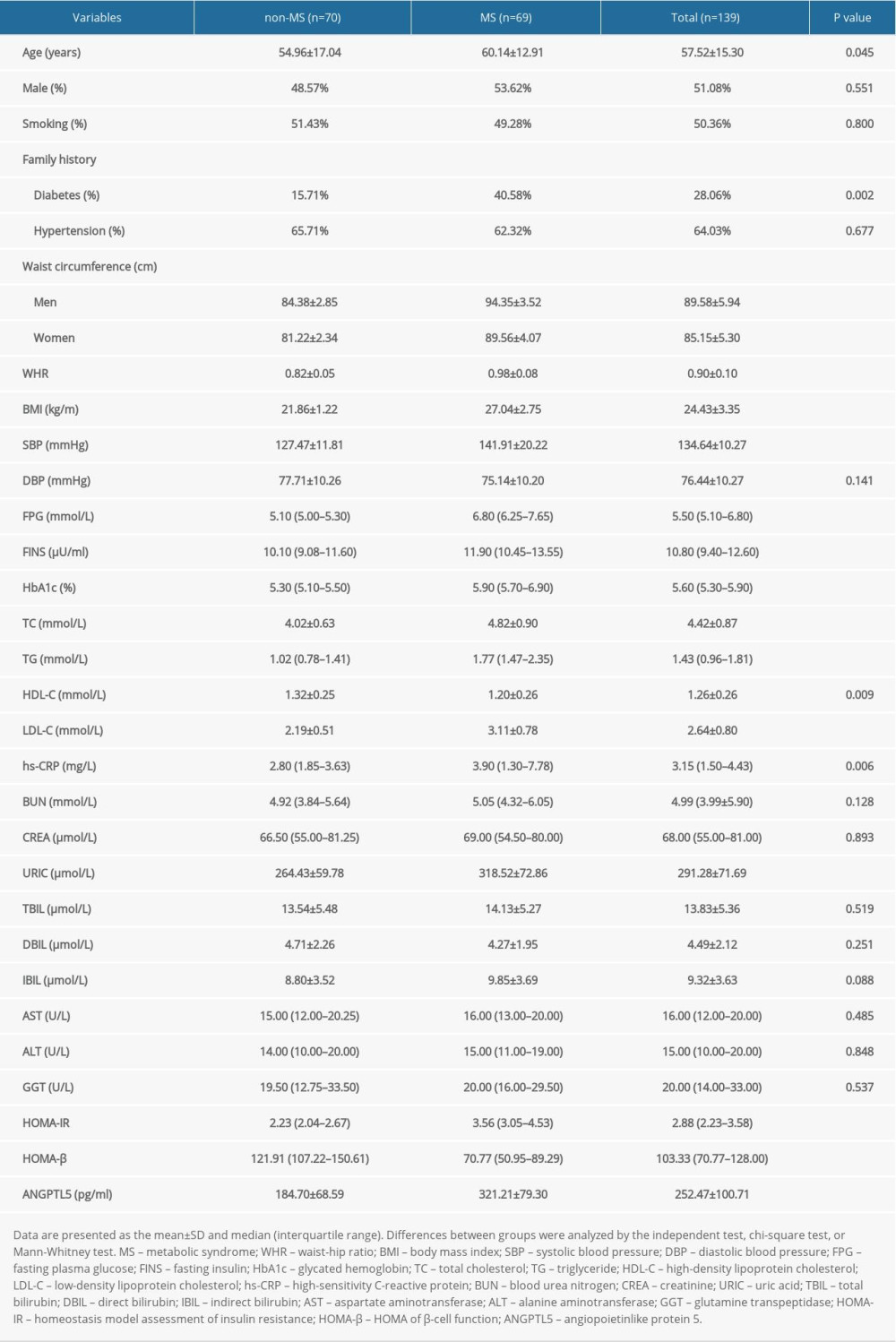 Table 1. Demographic and clinical characteristics of subjects included.
Table 1. Demographic and clinical characteristics of subjects included.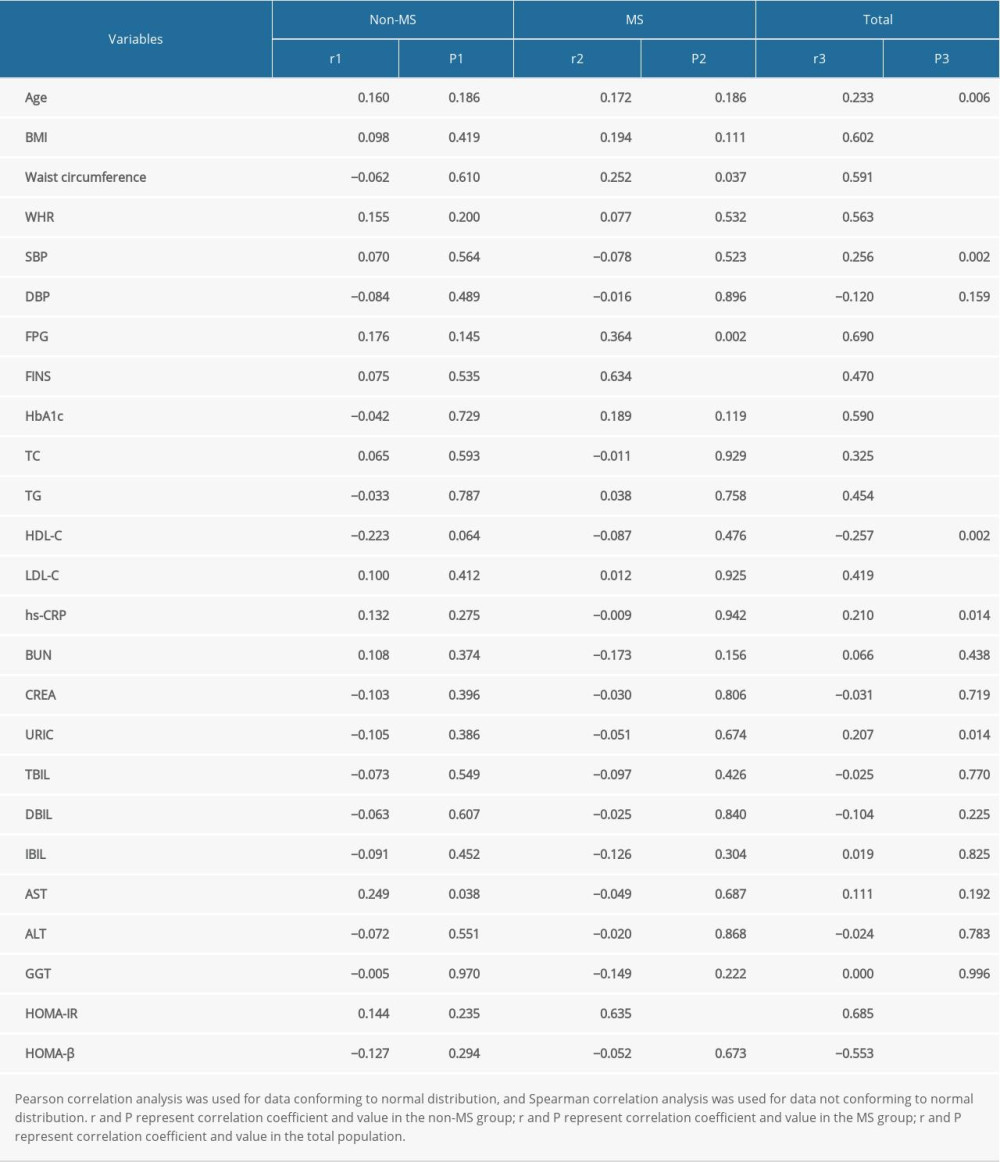 Table 2. Correlations of plasma angiopoietinlike protein 5 (ANGPTL5) with laboratory parameters in patients with metabolic syndrome (MS).
Table 2. Correlations of plasma angiopoietinlike protein 5 (ANGPTL5) with laboratory parameters in patients with metabolic syndrome (MS).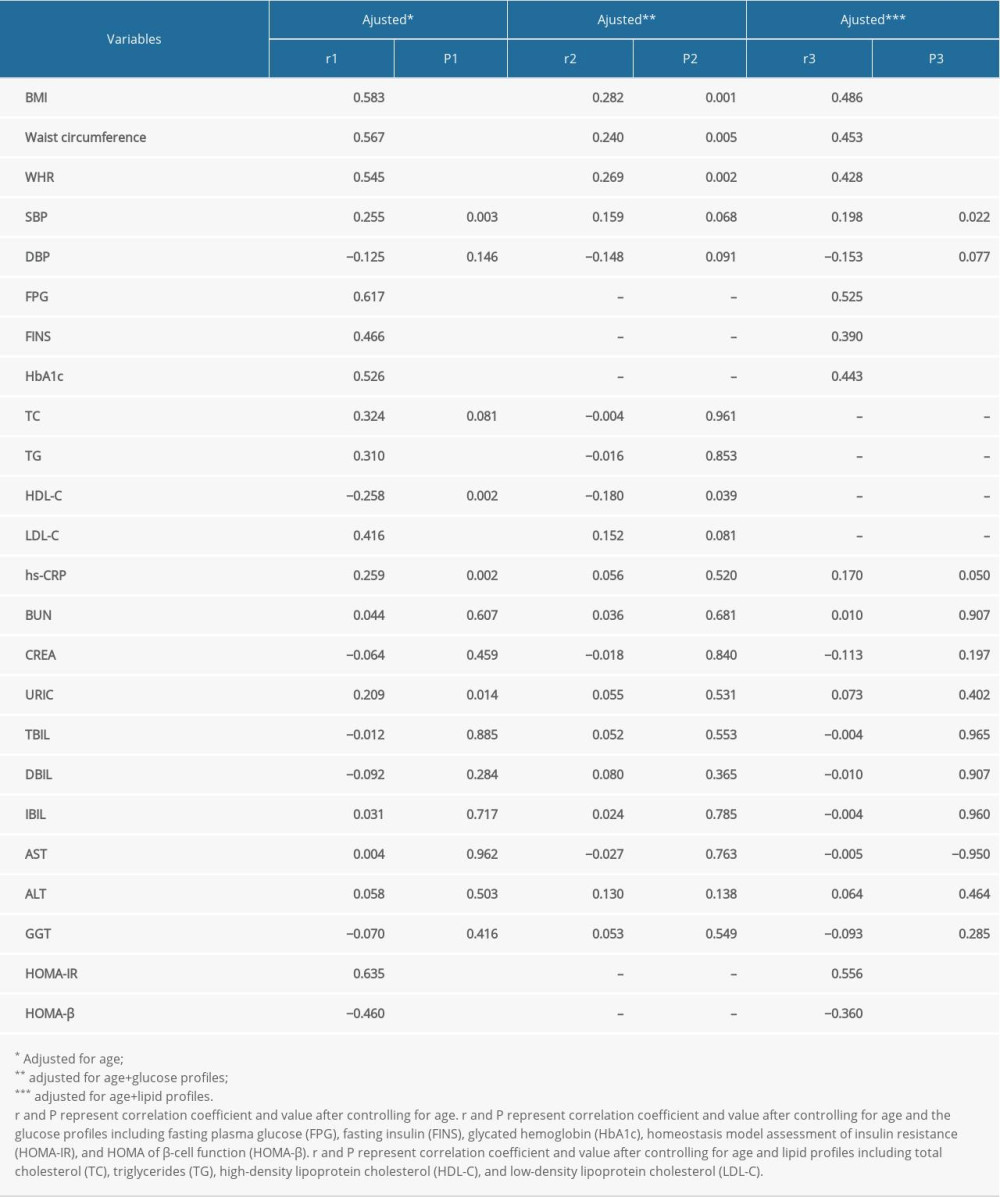 Table 3. Correlations of plasma angiopoietinlike protein 5 (ANGPTL5) with laboratory parameters after controlling for the lipid or glucose profiles.
Table 3. Correlations of plasma angiopoietinlike protein 5 (ANGPTL5) with laboratory parameters after controlling for the lipid or glucose profiles.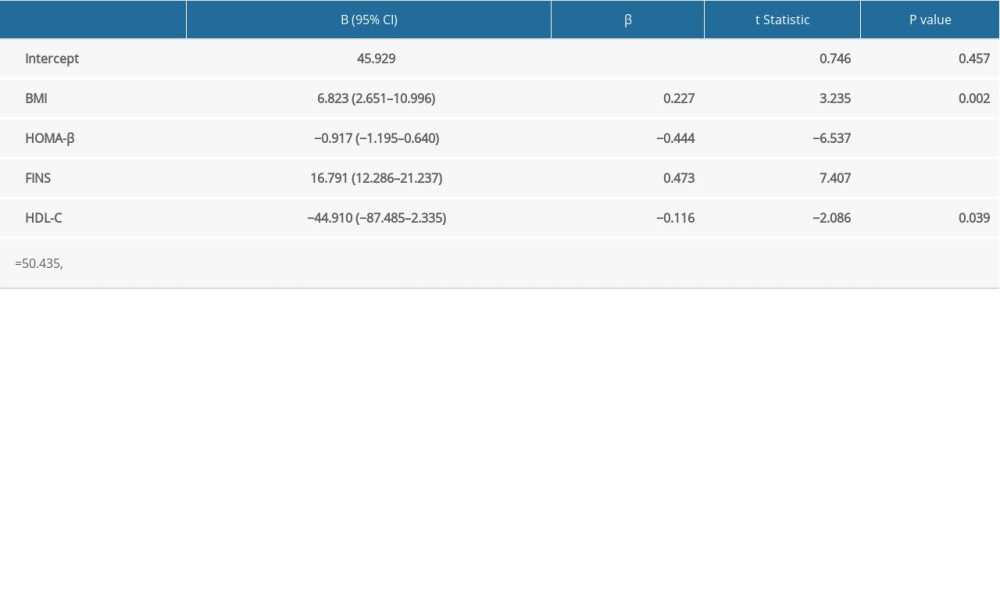 Table 4. Multivariate linear regression to examine association of metabolic syndrome (MS)-related indicators with plasma angiopoietinlike protein 5 (ANGPTL5).
Table 4. Multivariate linear regression to examine association of metabolic syndrome (MS)-related indicators with plasma angiopoietinlike protein 5 (ANGPTL5).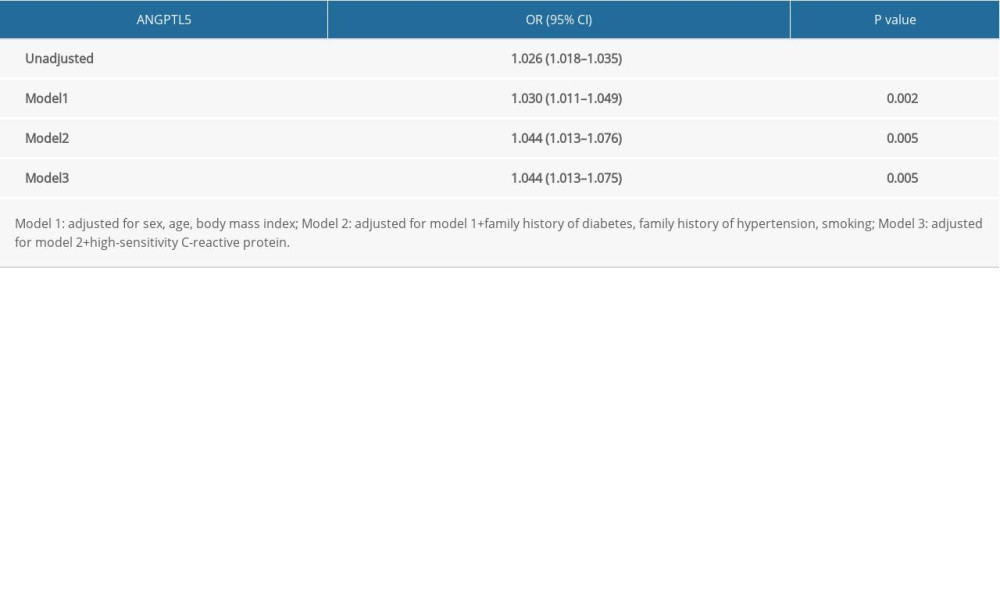 Table 5. Multivariate logistic regression to assess association of plasma angiopoietinlike protein 5 (ANGPTL5) with the risk of metabolic syndrome (MS).
Table 5. Multivariate logistic regression to assess association of plasma angiopoietinlike protein 5 (ANGPTL5) with the risk of metabolic syndrome (MS). In Press
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








