15 March 2022: Clinical Research
Chain Mediation Model of Perceived Stress, Resilience, and Social Support on Coping Styles of Chinese Patients on Hemodialysis During COVID-19 Pandemic Lockdown
Lu Peng1AE, Yuling Ye1AC, Lingzhen Wang1C, Wanling Qiu1B, Sicheng Huang1B, Lixing Wang1F, Fengling He2B, Lili Deng3F, Jingxia Lin4F*DOI: 10.12659/MSM.935300
Med Sci Monit 2022; 28:e935300
Abstract
BACKGROUND: The recurrence of COVID-19 and the continuous escalation of prevention and control policies can lead to an increase in mental health problems. This study aimed to investigate the perceived stress, coping style, resilience, and social support among patients on maintenance hemodialysis (MHD) during the COVID-19 epidemic lockdown in China.
MATERIAL AND METHODS: This cross-sectional observational study enrolled 197 patients on MHD from the Guangdong Province Traditional Chinese Medical Hospital and the Hedong Hospital of Guangzhou Liwan District People’s Hospital during July 2021. AMOS 24.0 and PROCESS Macro 3.1 model 6 were used for analyses of moderating mediating effects.
RESULTS: Perceived stress was negatively correlated with positive coping style (r=-0.305, P<0.001) and resilience (r=-0.258, P<0.001), whereas resilience (r=0.631, P<0.001) and social support (r=0.300, P<0.001) were positively correlated with positive coping style among patients on MHD. In the moderated mediating model, perceived stress had significant direct predictive effects on positive coping style (95% CI -0.33, -0.07), and perceived stress had significant indirect predictive effects on positive coping styles through resilience (95% CI -0.26, -0.06) or social support (95% CI 0.01, 0.06). Perceived stress had significant indirect predictive effects on positive coping style through both resilience and social support (95% CI -0.04, -0.01).
CONCLUSIONS: Perceived stress not only predicted coping style directly, but also indirectly predicted coping style through resilience and social support. Coping style was affected by internal and external factors during the COVID-19 pandemic lockdown period.
Keywords: COVID-19, Hemodialysis, Home, Resilience, Psychological, Social Support, Stress, Psychological, Adaptation, Psychological, Adult, Asian People, COVID-19, China, Communicable Disease Control, Cross-Sectional Studies, Female, Humans, Kidney Diseases, Male, Pandemics, Renal Dialysis, SARS-CoV-2, Surveys and Questionnaires
Background
COVID-19 is highly a contagious disease with a fast spread and multiple channels that make the population susceptible; it has caused serious health threats worldwide [1]. In May 2021, India’s B.1.617 mutant strain spread for the first time in the Liwan District of Guangzhou, China. It had a short incubation period, fast transmission, high viral load, and long duration until patients had a negative test result. Its suddenness and dissemination in the community posed a huge threat and impact on peoples’ lives. To further strengthen the prevention and control of the COVID-19 epidemic in Guangzhou, the Guangzhou New Coronavirus Pneumonia Epidemic Prevention and Control Headquarters locked down the Liwan District and other places according to the risk level on June 4, 2021 [2].
During the COVID-19 pandemic lockdown period, patients on maintenance hemodialysis (MHD) still needed to have dialysis in the hospital weekly. It is reported that the prevalence of hemodialysis in China was 402.18 per million, and the corresponding number of patients on hemodialysis was approximately 553 000 in 2015 [3]. Dialysis is unable to fully compensate for the metabolic activities of people, and this is considered one of the potential stress factors among patients on dialysis [4]. Previous research has shown that patients on hemodialysis were dealing with many psychological tensions in addition to the problems related to treatment [5]. In dialysis treatment, patients receiving MHD deal with significant stresses due to the aggravation of chronic renal failure, and since the treatment of this disease is a long-term process, it affects the patients’ psychosocial function [6,7]. Many psychiatric disorders are seen in patients on MHD, such as stress, depression, and anxiety. Since the dialysis centers have a large flow of people with unknown contact history, and with the COVID-19 epidemic outbreak and the continuous escalation of prevention, patients on MHD experienced additive psychosocial pressure. It has been reported that some patients were seriously affected in their daily lives from the excessive stress [8]. In addition to dialysis treatment, the COVID-19 outbreak, lack of understanding of chronic kidney disease, and commuting to and from the hospital exposed patients to the prominent contradictions of handling a chronic disease within a pandemic. This fact could lead to a series of physical and mental problems and then affect the prognosis of the disease.
Perceived stress occurs when individuals consider their relationship with the environment to be overwhelming or threatening in a way which could affect well-being [9]. It is the confusion or uncertainty that the individual generates when assessing the threat posed by a stressful event, including tension and loss of control [10]. The stress-response theory points out that when an individual is faced with a stressful event, the event will be perceived by the individual at first, and then the individual will make a preliminary assessment of the degree of stress caused by the stressful event, combine it with the experience and evaluation of other response resources, and finally produce corresponding coping behaviors [11]. Studies shows that positive and mature coping styles can improve the mental health of the general population [12]. Therefore, helping patients on MHD take an active response during the lockdown period to reduce the perceived stress has great significance in improving their mental health. The risk of mental health impairment is significantly increased without good coping styles and effective social support under high stress [13]. Patients on MHD need tangible and emotional social support. When they feel the understanding and support from the society and family members, they could take more active measures to relieve the negative emotions; social support helps patients on MHD to better cope with external pressure [14]. Social support can directly affect an individual’s mental health, but it can also act on an individual’s internal psychological factors, and even mental health. Studies have shown that the predictive effect of social support on mental health is achieved through resilience [15]. Better resilience helps people actively cope with the pressure encountered in work and life [16]. García-Martínez et al have confirmed that resilience is one of the important predictors of perceived stress [17]. Therefore, the development of interventions to promote resilience may have a positive impact on the perceived stress of patients on MHD.
The psychological state of patients on MHD changed from indifference and disbelief to fear and excessive tension, and finally toward relaxation during the COVID-19 epidemic [8]. Whether resilience and social support, as an internal driving force and valuable external resource, respectively, could improve patients’ pressure perception and impact coping style is worth studying. This study aimed to investigate the perceived stress, coping style, resilience, and social support among patients on MHD during the COVID-19 pandemic lockdown in China as well as the underlying possible mediating and moderating mechanisms. We also aimed to explore psychological care measures to improve the mental health of patients during the lockdown period. Additionally, we examined a chain mediating model of resilience and social support for the relationship between perceived stress and coping style (Figure 1).
Material and Methods
PARTICIPANTS:
All patients on MHD who were treated at the Guangdong Province Traditional Chinese Medical Hospital and the Hedong Hospital of Guangzhou Liwan District People’s Hospital during the lockdown period (June 4–24, 2021) were invited to participate in this study. The inclusion criteria were as follows: (1) patient met the diagnostic criteria of stage 5 chronic kidney disease in the clinical guidelines of the US Kidney Disease Prognosis Quality Initiative [18]; (2) patients was between 25 and 85 years old; (3) patient’s regular dialysis time ≥3 months; and (4) patients was willing to cooperate with the study. The exclusion criteria were as follows: (1) severe liver disease, heart disease, or other systemic diseases; and (2) mental illness or cognitive dysfunction.
STUDY DESIGN:
We conducted a cross-sectional, observational survey. The survey was approved by the Ethics Committee of Guangdong Provincial Traditional Chinese Medical Hospital (no. ZE2021-157-01). This study was performed following institutional guidelines, and all procedures followed were in accordance with the Helsinki Declaration of 1975 in its most recent version. Participation in the study was voluntary and all participants gave their written informed consent.
SETTING:
The COVID-19 lockdown period in Fangcun was from June 4, 2021 to June 24, 2021. Due to the requirements of pandemic prevention, this study was not allowed to be officially carried out until lockdown ended, so the data were collected in July 2021. When the investigation was officially conducted, the investigator introduced the method and purpose of the study to the patients who met the inclusion criteria and signed the informed consent form. The questionnaires were issued to patients before or during the treatment, and the patients were guided with a standard procedure to complete the questionnaire independently according to their actual situation and subjective feelings. For patients with special conditions who could not fill out the questionnaire by themselves, a qualified nurse read the contents of the questionnaire to them, the patient chose the answers, and then a researcher recorded the answers on the questionnaire.
PERCEIVED STRESS ASSESSMENT: The Perceived Stress Scale [10] was used to assess perceived stress. The scale measured the extent of self-awareness of stress and the belief that one’s life had been overloaded or was unpredictable or uncontrollable during the previous month. The survey includes 2 dimensions of loss of control and tension, and the 10 items are answered on a 5-point Likert scale. The minimum and maximum points are 0 and 40 points, respectively, with a higher score representing greater mental stress. The scale has shown high validity and reliability in the Chinese population [19], with a Cronbach’s alpha of 0.82 [20].
COPING STYLE ASSESSMENT: The Chinese version of the Simplified Coping Style Questionnaire [21] was used to measure coping style. The 20-item scale consists of 2 dimensions: positive and negative coping. The first 12 items cover positive coping, and the latter 8 items cover negative coping. The score is based on a 4-point Likert scale, the minimum and maximum points are 0 and 60 points, respectively, and higher scores indicates greater positive or negative coping. The scale has shown high reliability and validity in a Chinese population [13], with a Cronbach alpha of 0.916 for positive coping and 0.808 for negative coping [21].
RESILIENCE ASSESSMENT: The Connor-Davidson Resilience Scale [22] was used to measure resilience, which consists of 3 factors: toughness, strength, and optimism. The scale has a total of 25 items rated on a 5-point Likert scale ranging from 1 (not at all) to 4 (always). The minimum and maximum points are 0 and 100 points, respectively, and a higher score indicates better resilience. The scale has shown high validity and reliability in a Chinese population [23], with a Cronbach’s alpha of 0.882 [24].
SOCIAL SUPPORT ASSESSMENT: The Social Support Rating Scale [25], which consists of 10 items, was used to assess social support. The scale includes 3 dimensions: objective support, subjective support, and availability of support. The minimum and maximum points are 14 and 74 points, respectively, with higher scores reflecting more social support. The scale has shown high validity and reliability in a Chinese population, with a Cronbach’s alpha of 0.949 [26].
SAMPLE SIZE:
The study was designed as a cross-sectional survey, so we sought to include all available patients at our hospitals. Since we did not evaluate the effects of any particular intervention, we did not conduct a sample size calculation. All patients undergoing MHD at the Guangdong Province Traditional Chinese Medical Hospital and the Hedong Hospital of Guangzhou Liwan District People’s Hospital were invited to participate in this study during the lockdown period (June 4–24, 2021). A total of 197 patients agreed to take part in the study.
STATISTICAL ANALYSIS:
SPSS Statistics for Windows v21.0 (IBM Corp, Armonk, NY, USA), IBM SPSS Amos 24.0, and IBM SPSS macro program PROCESS v3.1 were used for the statistical analyses of this study. We compared continuous variables using the Kruskal-Wallis test; data are expressed as mean±standard deviation. We compared categorical variables using the chi-squared test or Fisher’s exact test for variables with low expected counts; data are described as n (%). The Pearson-product moment correlational analysis was performed using SPSS, structural equation model was conducted with AMOS 24.0, and analyses of moderating mediating effect was performed with the PROCESS v3.1 Model 6 [27]. Finally, bootstrapping using 5000 resamples with a 95% confidence interval (CI) was used to analyze the significance of moderated mediating model. A P value less than 0.05 was considered statistically significant.
Results
BASELINE CHARACTERISTICS OF THE PARTICIPANTS:
A total of 197 patients undergoing MHD participated in this study. Among the participants were 106 men (53.8%) and 91 women (46.2%), and the age range was from 25 to 85 years. There were 15 (7.6%) participants living alone, while 182 (92.4%) were living with their families. During the lockdown period, transportation to the hospital was by walking (67%), self-driving (16.2%), ambulance (12.2%), and wheelchair and walking (4.6%). Participants had nucleic acid detected either every 2 days (56.3%) or every day (40.6%). The baseline participant characteristics are shown in Table 1.
DESCRIPTIVE STATISTICS AND CORRELATIONS:
Table 2 presents the results of the correlational analysis of perceived stress, resilience, social support, and coping style of participants. Patients on MHD scored an average of 15.72±4.58 on the Perceived Stress Scale, 31.09±6.54 on the Simplified Coping Style Questionnaire, 58.28±10.74 on the Connor-Davidson Resilience Scale, and 36.87±6.81 on the Social Support Rating Scale. It was found that perceived stress was negatively correlated with positive coping style (r=−0.305, P<0.001) and resilience (r=−0.258, P<0.001), whereas resilience (r=0.631, P<0.001) and social support (r=0.300, P<0.001) were positively correlated with positive coping style.
STRUCTURAL EQUATION MODEL ANALYSIS:
The structural equation model is illustrated in Figure 2. With perceived stress as an independent variable and positive coping style as the dependent variable, the structural equation model was constructed to assess the hypothesis model. It showed good fit based on the chi-squared statistic (χ2/df=2.414) and CFI=0.954, GFI=0.954, TLI=0.920, IFI=0.955, NFI=0.926, and RMSEA=0.085 (0.051–0.120).
CHAIN MEDIATION EFFECTS ANALYSIS:
This study examined the chain mediating roles of resilience and social support on perceived stress and coping styles (Table 3). Perceived stress was used as an independent variable, coping style was used as a dependent variable, resilience and social support were used as mediating variables, and the PROCESS Macro 3.1 model 6 was used to test the chain mediating effect (Table 4). The results showed that: (1) perceived stress had significant direct predictive effects on positive coping style, with a direct effect value of −0.20 (95% CI [−0.33, −0.07]); (2) perceived stress had significant indirect predictive effects on positive coping styles through resilience, and the indirect effect value was −0.16 (95% CI [−0.26, −0.06]); (3) perceived stress has significant indirect predictive effects on positive coping style through social support, and the indirect effect value was 0.03 (95% CI [0.01, 0.06]); and (4) perceived stress had significant indirect predictive effects on positive coping style through resilience and social support, and the indirect effect value was −0.01 (95% CI [−0.04, −0.01]). Four variables that were significantly correlated were modeled as chain mediators. A bias-corrected percentile Bootstrap (5000 replicate samples) was used to determine the role of resilience and social support in mediating the chain variables between perceived stress and positive coping style. The standardized path coefficients were calculated to reduce Type 1 errors due to distribution [29]. The results of the chain mediation model analysis are shown in Figure 3.
Discussion
STUDY LIMITATIONS:
Despite the valuable contributions of this study, there were several limitations. First, the convenience sampling technique may have led to selection bias. Hence, generalization of the results to other populations is limited. Second, collecting data face to face may have limited the number of participants and the generalization of the results since participants were limited to those willing to voluntarily participate. Future studies should consider this factor. Third, our cross-sectional study could not capture changes in psychological distress during the lockdown period of the COVID-19 pandemic. Therefore, future studies should conduct a follow-up for the current situation and engage in a more consistent analysis of the long-term psychological effects of the COVID-19 pandemic in patients on MHD. Such work should also more generally explore the ability of resilience and social support to mediate the effects of the COVID-19 pandemic on perceived stress and coping style. Nonetheless, the present findings lay the groundwork for further studies on these issues in this part of the world.
Conclusions
Perceived stress not only predicted coping style directly, but also indirectly predicted coping style through resilience and social support. Coping style was affected by internal and external factors during the COVID-19 pandemic lockdown period among patients on MHD. Therefore, the development of interventions to promote resilience and social support may have a positive impact on perceived stress in patients on MHD.
Figures
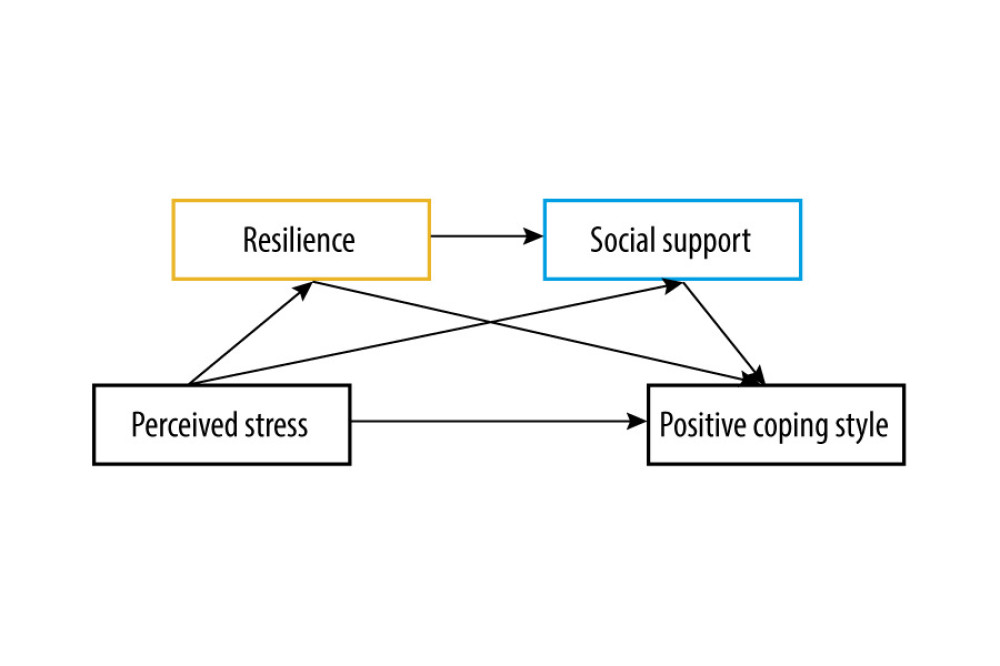 Figure 1. The prediction of a chain mediating model of resilience and social support on the relationship between perceived stress and coping style among patients on MHD in China during the COVID-19 pandemic lockdown period. Resilience and social support may have a certain mediating effect between perceived stress and coping styles (IBM SPSS macro program PROCESS v3.1 Model 6).
Figure 1. The prediction of a chain mediating model of resilience and social support on the relationship between perceived stress and coping style among patients on MHD in China during the COVID-19 pandemic lockdown period. Resilience and social support may have a certain mediating effect between perceived stress and coping styles (IBM SPSS macro program PROCESS v3.1 Model 6). 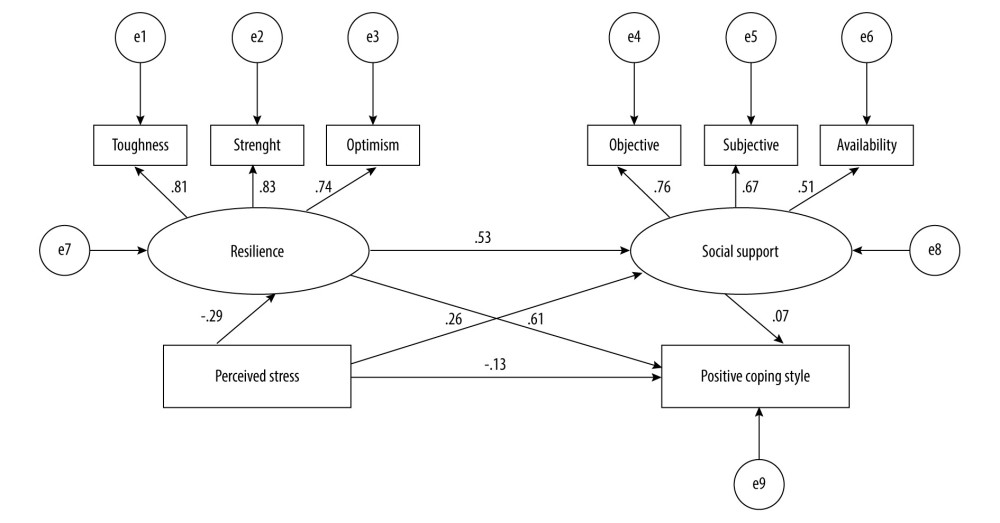 Figure 2. The structural equation model of the study. The numbers on the arrows represent standardized regression coefficients (path coefficients), and e1~e9 represent unobserved variables. There is a path relationship among the 4 main observation variables: perceived stress, resilience (including 3 dimensions), social support (including 3 dimensions), and positive coping style. Resilience and social support play a mediating role between perceived stress and positive coping style (IBM SPSS Amos 24.0).
Figure 2. The structural equation model of the study. The numbers on the arrows represent standardized regression coefficients (path coefficients), and e1~e9 represent unobserved variables. There is a path relationship among the 4 main observation variables: perceived stress, resilience (including 3 dimensions), social support (including 3 dimensions), and positive coping style. Resilience and social support play a mediating role between perceived stress and positive coping style (IBM SPSS Amos 24.0). 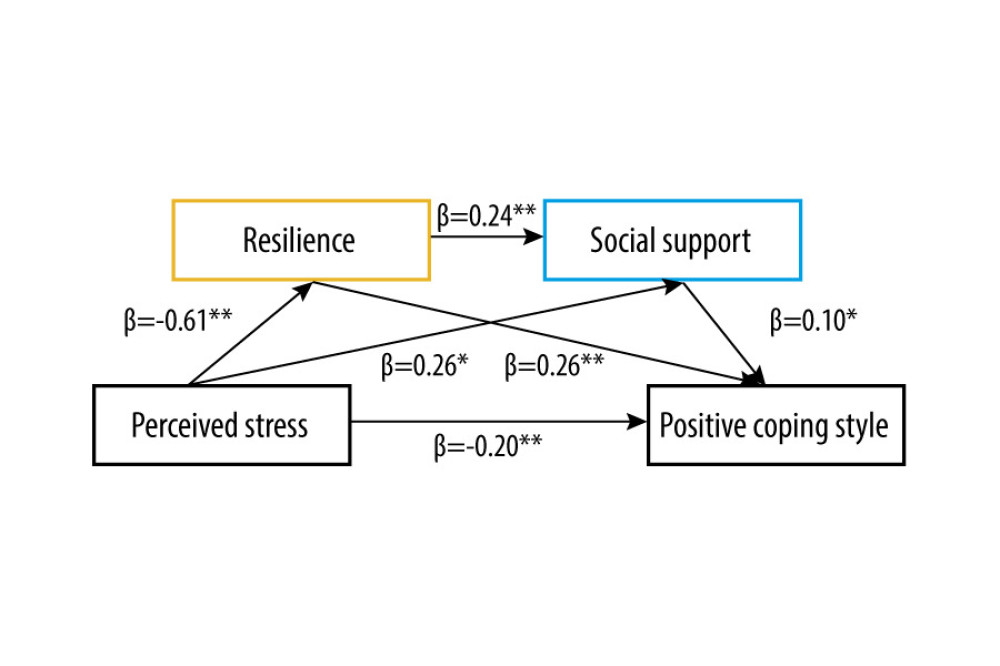 Figure 3. The role of resilience and social support as chain mediators in the relationship between perceived stress and positive coping style with standardized beta (IBM SPSS macro program PROCESS v3.1 Model 6). * P<0.05, ** P<0.01. Values on paths are path coefficients (standardized βs).
Figure 3. The role of resilience and social support as chain mediators in the relationship between perceived stress and positive coping style with standardized beta (IBM SPSS macro program PROCESS v3.1 Model 6). * P<0.05, ** P<0.01. Values on paths are path coefficients (standardized βs). Tables
Table 1. Sociodemographic characteristics of participants. Survey of patients on maintenance hemodialysis (MHD) at the Guangdong Province Traditional Chinese Medical Hospital and the Hedong Hospital of Guangzhou Liwan District People’s Hospital during the COVID-19 pandemic lockdown period in China, 2021.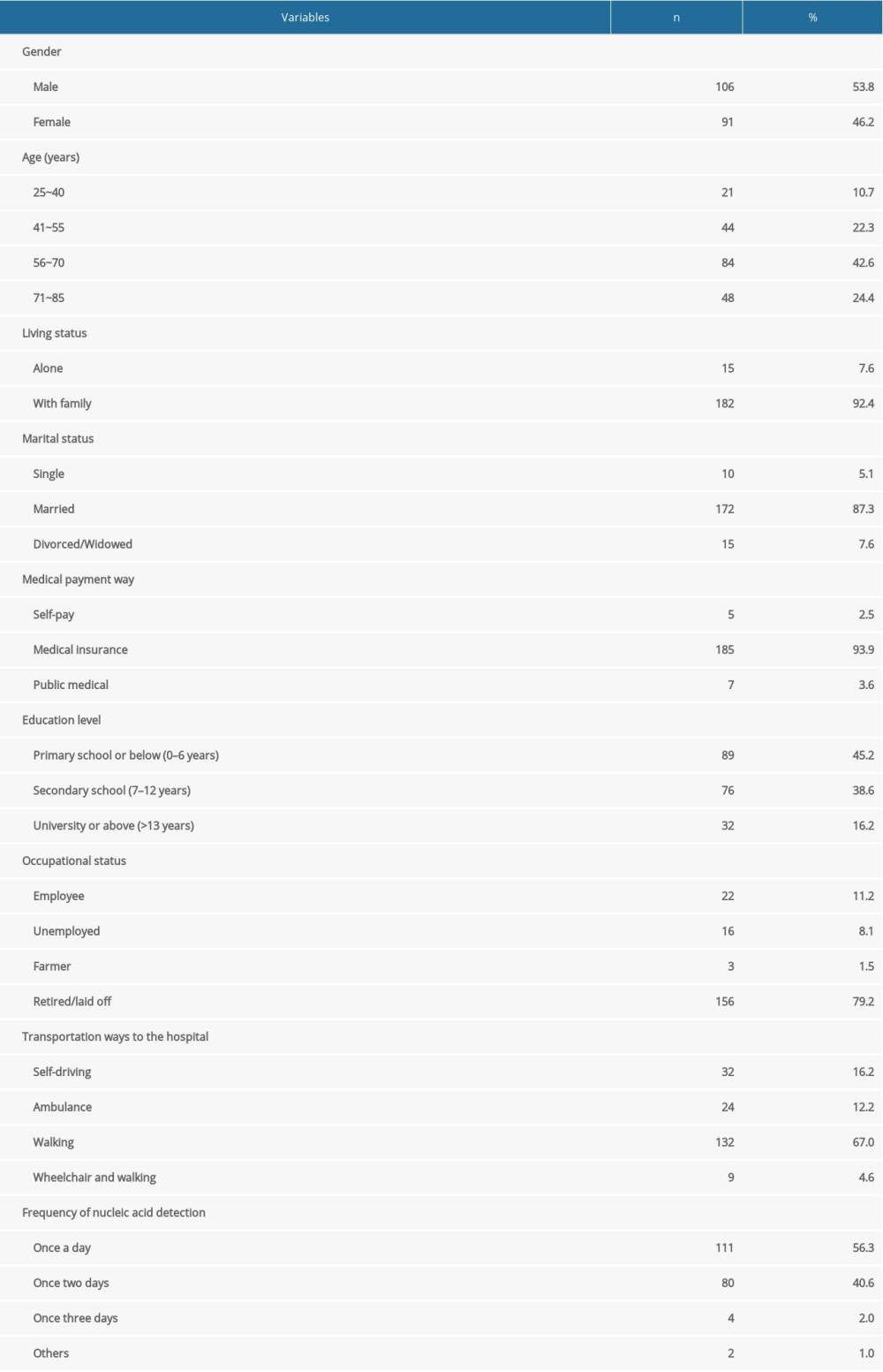 Table 2. Correlational matrix of perceived stress, resilience, social support, and coping style of participants. Survey of patients on maintenance hemodialysis (MHD) at the Guangdong Province Traditional Chinese Medical Hospital and the Hedong Hospital of Guangzhou Liwan District People’s Hospital during the COVID-19 pandemic lockdown period in China, 2021.
Table 2. Correlational matrix of perceived stress, resilience, social support, and coping style of participants. Survey of patients on maintenance hemodialysis (MHD) at the Guangdong Province Traditional Chinese Medical Hospital and the Hedong Hospital of Guangzhou Liwan District People’s Hospital during the COVID-19 pandemic lockdown period in China, 2021.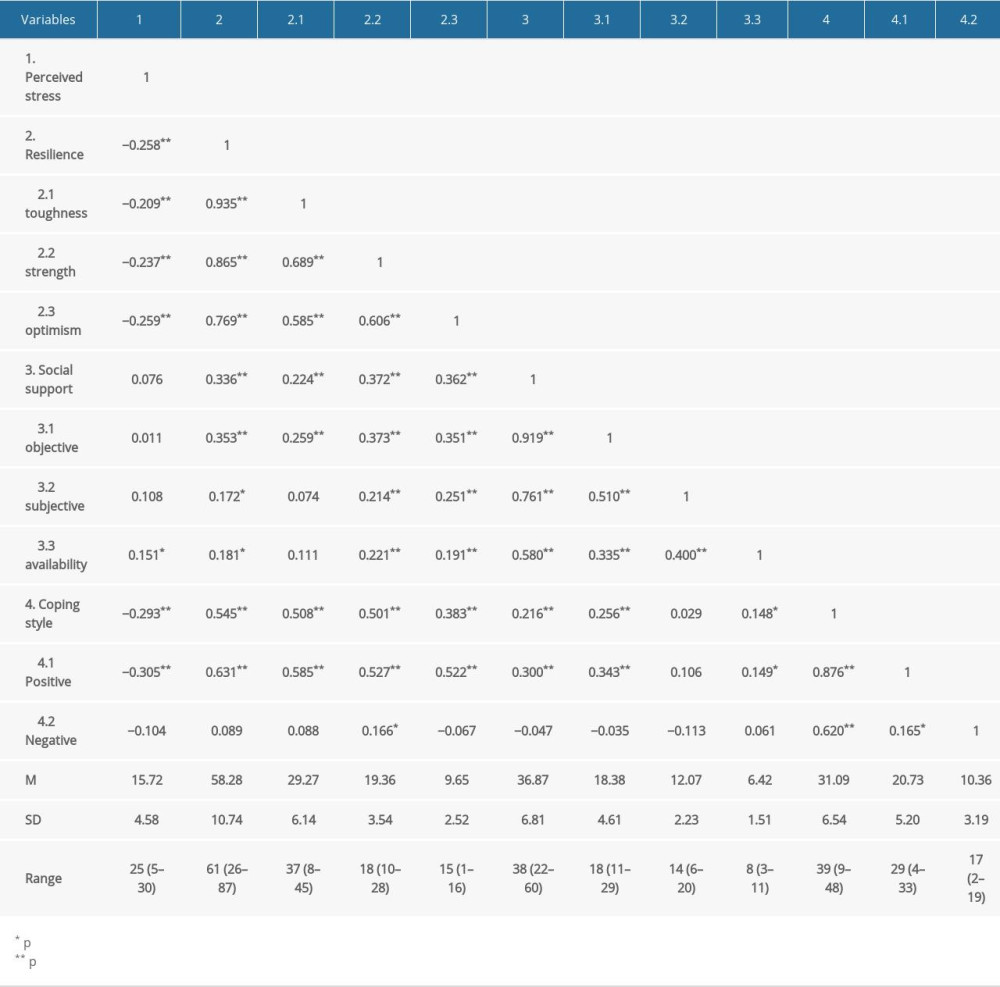 Table 3. The chain mediating model of perceived stress, resilience, social support and positive coping style. Survey of patients on maintenance hemodialysis (MHD) at the Guangdong Province Traditional Chinese Medical Hospital and the Hedong Hospital of Guangzhou Liwan District People’s Hospital during the COVID-19 pandemic lockdown period in China, 2021.
Table 3. The chain mediating model of perceived stress, resilience, social support and positive coping style. Survey of patients on maintenance hemodialysis (MHD) at the Guangdong Province Traditional Chinese Medical Hospital and the Hedong Hospital of Guangzhou Liwan District People’s Hospital during the COVID-19 pandemic lockdown period in China, 2021.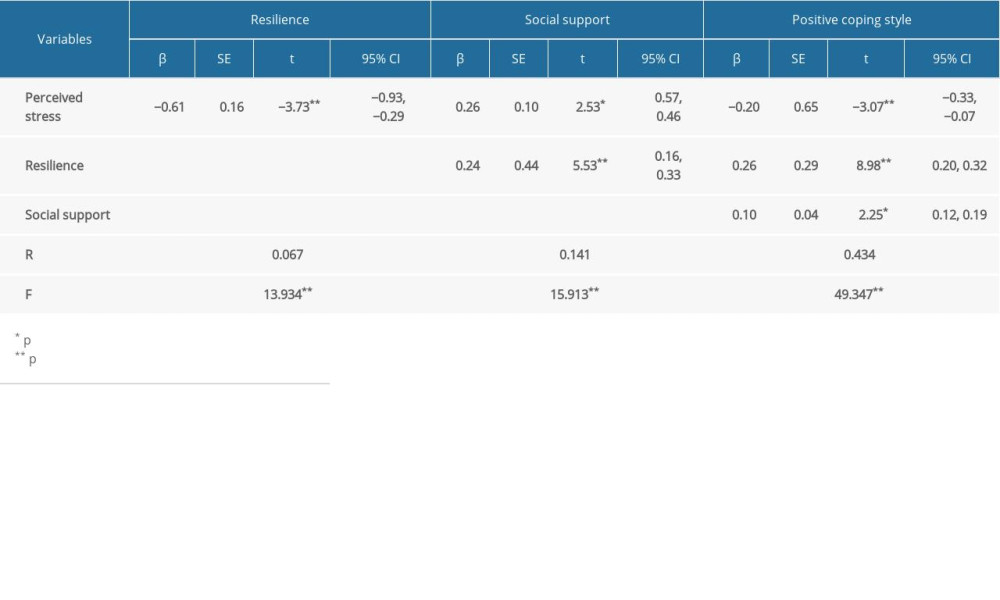 Table 4. The analysis of the chain mediating effect of resilience and social support to perceived stress and positive coping style. Survey of patients on maintenance hemodialysis (MHD) at the Guangdong Province Traditional Chinese Medical Hospital and the Hedong Hospital of Guangzhou Liwan District People’s Hospital during the COVID-19 pandemic lockdown period in China, 2021.
Table 4. The analysis of the chain mediating effect of resilience and social support to perceived stress and positive coping style. Survey of patients on maintenance hemodialysis (MHD) at the Guangdong Province Traditional Chinese Medical Hospital and the Hedong Hospital of Guangzhou Liwan District People’s Hospital during the COVID-19 pandemic lockdown period in China, 2021.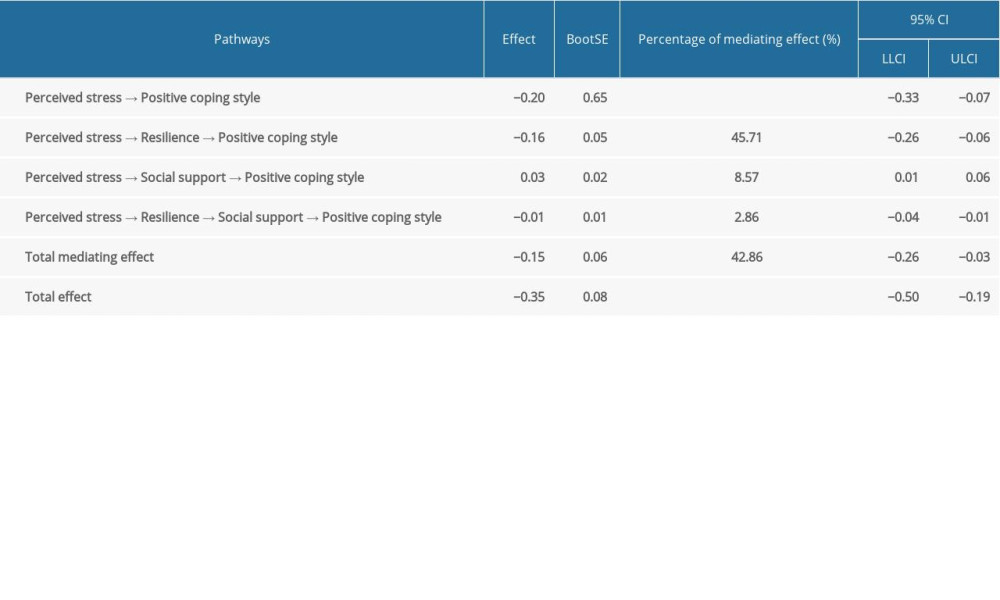
References
1. Ali SA, Baloch M, Ahmed N, The outbreak of coronavirus disease 2019 (COVID-19)-An emerging global health threat: J Infect Public Health, 2020; 13; 644-46
2. Guangzhou New Coronavirus Pneumonia Epidemic Prevention and Control Headquarters: Notice of Guangzhou New Coronavirus Pneumonia Epidemic Prevention and Control Headquarters on Further Strengthening the Prevention and Control of New Coronary Pneumonia Epidemics by Classification [No.16] 06 04, 2021 Available: http://wjw.gz.gov.cn/ztzl/xxfyyqfk/fktzgg/content/post7314687.html
3. Wang F, Yang C, Long J, Executive summary for the 2015 Annual Data Report of the China Kidney Disease Network (CK-NET): Kidney Int, 2019; 95(3); 501-5
4. Clarke AL, Yates T, Smith AC, Chilcot J, Patient’s perceptions of chronic kidney disease and their association with psychosocial and clinical outcomes: A narrative review: Clin Kidney J, 2016; 9; 494-502
5. Ghaffari M, Morowatisharifabad MA, Mehrabi Y, What are the hemodialysis patient’ style in coping with stress? A directed content analysis: Int J Community Based Nurs Midwifery, 2019; 7(4); 309-18
6. Morowatisharifabad MA, Ghaffari M, Mehrabi Y, Experiences of stress appraisal in hemodialysis patients: A theory-guided qualitative content analysis: Saudi J Kidney Dis Transpl, 2020; 31(6); 1294-302
7. Ghaffari M, Morowatisharifabad MA, Jadgal MS, The effectiveness of intervention based on the transactional model on improving coping efforts and stress moderators in hemodialysis patients in Tehran: A randomized controlled trial: BMC Nephrol, 2021; 22(1); 377
8. Cui H, Ding H, Zhang Y, Psychological status and nursing methods of hemodialysis patients in different periods of the development of new coronary pneumonia: J Qilu Nurs, 2020; 26(12); 61-63
9. Lazarus RS: Stress and emotion: A new synthesis, 2006, New York (NY), Springer Publishing Company
10. Cohen S, Kamarck T, Mermelstein R, A global measure of perceived stress: J Health Soc Behav, 1983; 24(4); 385-96
11. Lazaru RS: Folkman Stress, appraisal and coping, 1984, New York (NY), Springer
12. Besirli A, Erden SC, Atilgan M, The Relationship between anxiety and depression levels with perceived stress and coping strategies in health care workers during the COVID-19 pandemic: Sisli Etfal Hastan Tip Bul, 2021; 55(1); 1-11
13. Li Z, Yi X, Zhong M, Psychological distress, social support, coping style, and perceived stress among medical staff and medical students in the early stages of the COVID-19 epidemic in China: Front Psychiatry, 2021; 12; 664808
14. Hoang VL, Green T, Bonner A, Examining social support, psychological status and health-related quality of life in people receiving haemodialysis: J Ren Care, 2021 [Online ahead of print]
15. Wilks SE, Croom B, Perceived stress and resilience in Alzheimer’s disease caregivers: Testing moderation and mediation models of social support: Aging Ment Health, 2008; 12(3); 357-65
16. Haeffel GJ, Vargas I, Resilience to depressive symptoms: The buffering effects of enhancing cognitive style and positive life events: J Behav Ther Exp Psychiatry, 2011; 42(1); 13-18
17. García-Martínez P, Ballester-Arnal R, Gandhi-Morar K, Perceived stress in relation to quality of life and resilience in patients with advanced chronic kidney disease undergoing hemodialysis: Int J Environ Res Public Health, 2021; 18(2); 536
18. National Kidney Foundation, K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification: Am J Kidney Dis, 2002; 39(2 Suppl 1); S1-266
19. Huang F, Wang H, Wang Z, Psychometric properties of the perceived stress scale in a community sample of Chinese: BMC Psychiatry, 2020; 20; 130
20. Zhao X, Lan M, Li H, Perceived stress and sleep quality among the non-diseased general public in China during the 2019 coronavirus disease: A moderated mediation model: Sleep Med, 2020; 21; 339-45
21. Xie YN, A preliminary study of the reliability and validity of the simplified coping style questionnaire (in Chinese): Chin J Clin Psychol, 1998; 6; 114-15
22. Connor KM, Davidson JR, Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC): Depress Anxiety, 2003; 18(2); 76-82
23. Yu XN, Lau JT, Mak WW, Factor structure and psychometric properties of the Connor-Davidson Resilience Scale among Chinese adolescents: Compr Psychiatry, 2011; 52(2); 218-24
24. Freire de Medeiros CM, Arantes EP, Tajra RD, Resilience, religiosity and treatment adherence in hemodialysis patients: A prospective study: Psychol Health Med, 2017; 22(5); 570-77
25. Xiao H, Zhang Y, Kong D, The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China: Med Sci Monit, 2020; 26; e923549
26. Liu JW, Li FY, Lian YLReliability and validity of social support rating scale: J Xinjiang Med Univ, 2008; 1; 4-6 [in Chinese]
27. Hayes AF: Introduction to mediation, moderation, and conditional process analysis: A regression-based approach, 2018, New York (NY), Guilford Press
28. Babore A, Lombardi L, Viceconti ML, Psychological effects of the COVID-2019 pandemic: Perceived stress and coping strategies among healthcare professionals: Psychiatry Res, 2020; 293; 113366
29. Alharbi H, Alshehry A, Perceived stress and coping strategies among ICU nurses in government tertiary hospitals in Saudi Arabia: A cross-sectional study: Ann Saudi Med, 2019; 39(1); 48-55
30. Zhao X, Lan M, Li H, Perceived stress and sleep quality among the non-diseased general public in China during the 2019 coronavirus disease: A moderated mediation model: Sleep Med, 2020; 21; 339-45
31. Noghan N, Akaberi A, Pournamdarian S, Resilience and therapeutic regimen compliance in patients undergoing hemodialysis in hospitals of Hamedan, Iran: Electron Physician, 2018; 10(5); 6853-58
32. Sahu M, Gandhi S, Sharma MK, Marimuthu P, Perceived stress and resilience and their relationship with the use of mobile phone among nursing students: Invest Educ Enferm, 2019; 37; e05
33. Sarrionandia A, Ramos-Diaz E, Fernandez-Lasarte O, Resilience as a mediator of emotional intelligence and perceived stress: A cross-country study: Front Psychol, 2018; 9; 2653
34. Mandzuk LL, McMillan DE, A concept analysis of quality of life: Orthop Nurs, 2005; 9; 12-18
35. Zhang LL, Xu J, Zhu AHInfluence of perceived social support on college students coping style: Chain mediating effect of meaning in life and psychological resilience: Chin J Health Psychol, 2021; 29(5); 758-61 [in Chinese]
36. Liu YM, Chang HJ, Wang RH, Role of resilience and social support in alleviating depression in patients receiving maintenance hemodialysis: Ther Clin Risk Manag, 2018; 14; 441-51
37. Gurklis JA, Menke EM, Chronic hemodialysis patients’ perceptions of stress, coping, and social support: Anna J, 1995; 22(4); 381-87
38. Labrague LJ, Psychological resilience, coping behaviours and social support among health care workers during the COVID-19 pandemic: A systematic review of quantitative studies: J Nurs Manag, 2021; 29(7); 1893-905
Figures
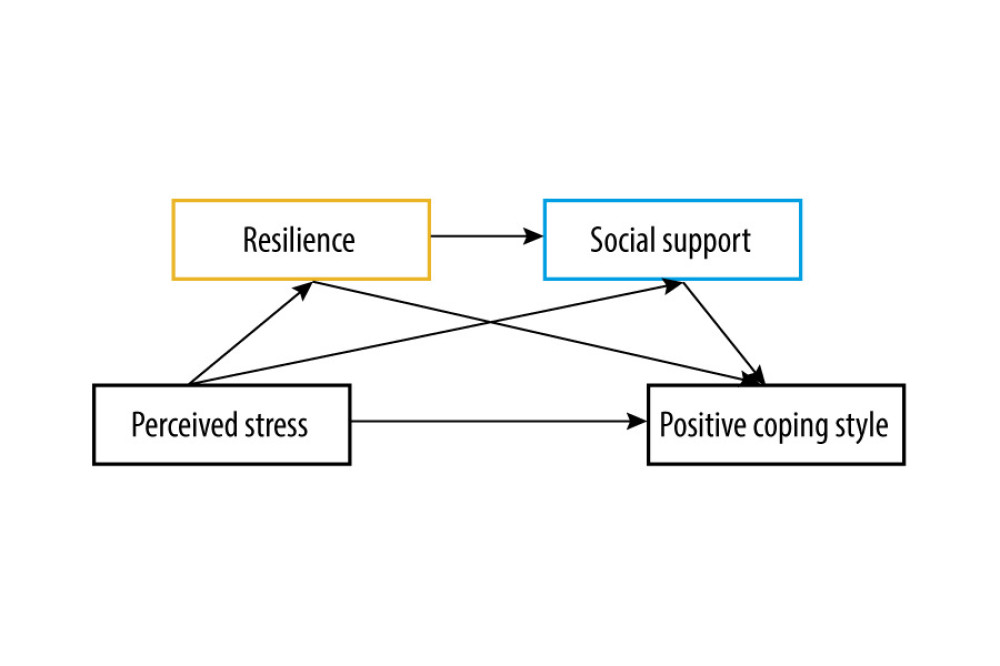 Figure 1. The prediction of a chain mediating model of resilience and social support on the relationship between perceived stress and coping style among patients on MHD in China during the COVID-19 pandemic lockdown period. Resilience and social support may have a certain mediating effect between perceived stress and coping styles (IBM SPSS macro program PROCESS v3.1 Model 6).
Figure 1. The prediction of a chain mediating model of resilience and social support on the relationship between perceived stress and coping style among patients on MHD in China during the COVID-19 pandemic lockdown period. Resilience and social support may have a certain mediating effect between perceived stress and coping styles (IBM SPSS macro program PROCESS v3.1 Model 6).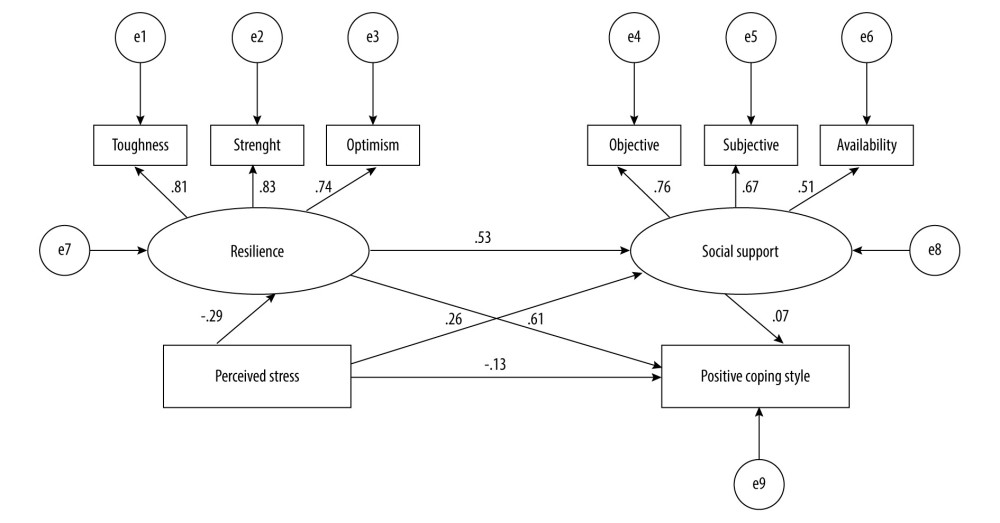 Figure 2. The structural equation model of the study. The numbers on the arrows represent standardized regression coefficients (path coefficients), and e1~e9 represent unobserved variables. There is a path relationship among the 4 main observation variables: perceived stress, resilience (including 3 dimensions), social support (including 3 dimensions), and positive coping style. Resilience and social support play a mediating role between perceived stress and positive coping style (IBM SPSS Amos 24.0).
Figure 2. The structural equation model of the study. The numbers on the arrows represent standardized regression coefficients (path coefficients), and e1~e9 represent unobserved variables. There is a path relationship among the 4 main observation variables: perceived stress, resilience (including 3 dimensions), social support (including 3 dimensions), and positive coping style. Resilience and social support play a mediating role between perceived stress and positive coping style (IBM SPSS Amos 24.0).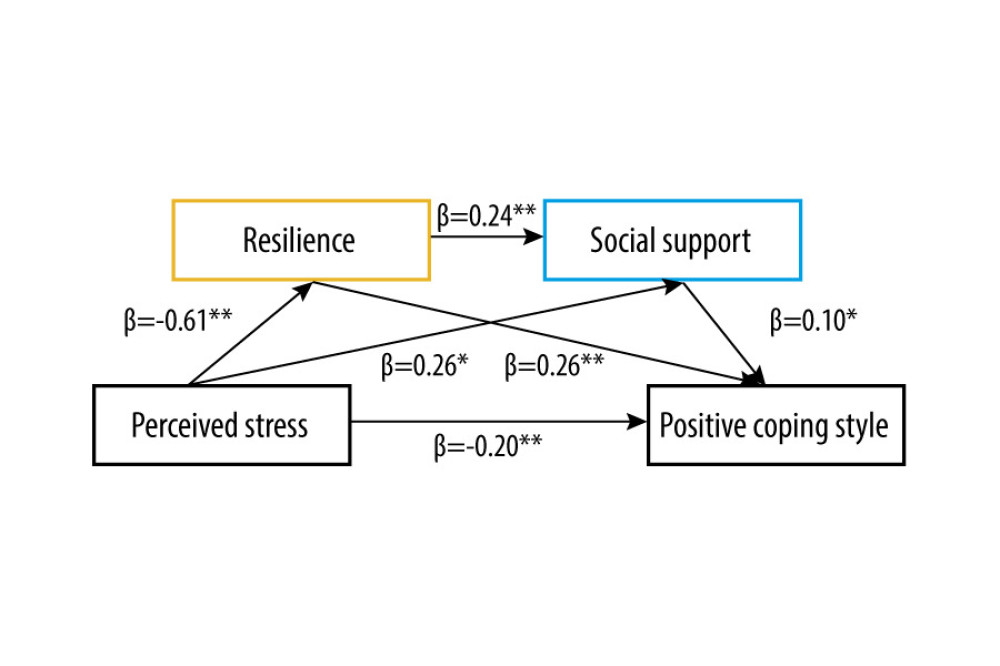 Figure 3. The role of resilience and social support as chain mediators in the relationship between perceived stress and positive coping style with standardized beta (IBM SPSS macro program PROCESS v3.1 Model 6). * P<0.05, ** P<0.01. Values on paths are path coefficients (standardized βs).
Figure 3. The role of resilience and social support as chain mediators in the relationship between perceived stress and positive coping style with standardized beta (IBM SPSS macro program PROCESS v3.1 Model 6). * P<0.05, ** P<0.01. Values on paths are path coefficients (standardized βs). Tables
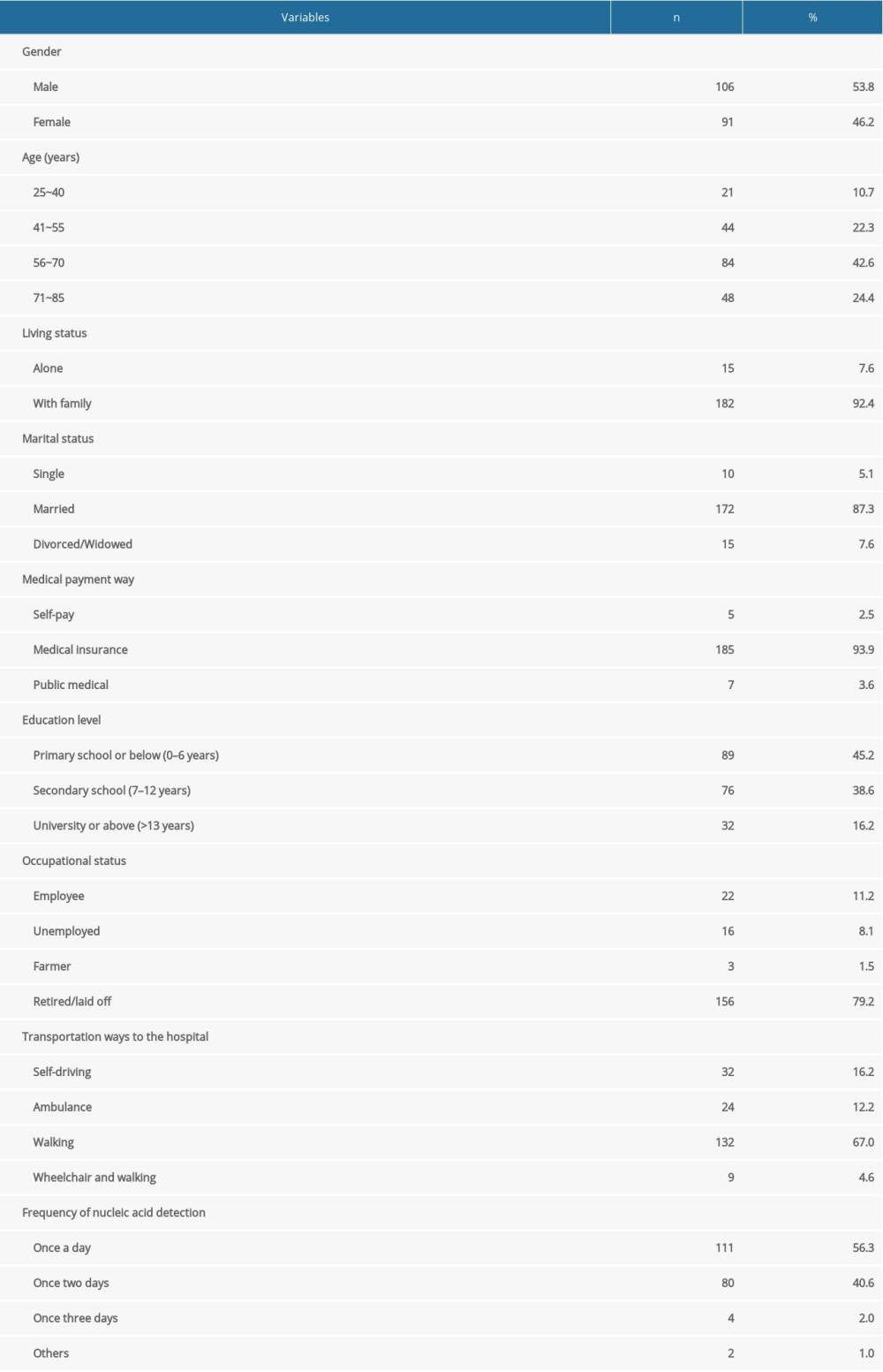 Table 1. Sociodemographic characteristics of participants. Survey of patients on maintenance hemodialysis (MHD) at the Guangdong Province Traditional Chinese Medical Hospital and the Hedong Hospital of Guangzhou Liwan District People’s Hospital during the COVID-19 pandemic lockdown period in China, 2021.
Table 1. Sociodemographic characteristics of participants. Survey of patients on maintenance hemodialysis (MHD) at the Guangdong Province Traditional Chinese Medical Hospital and the Hedong Hospital of Guangzhou Liwan District People’s Hospital during the COVID-19 pandemic lockdown period in China, 2021.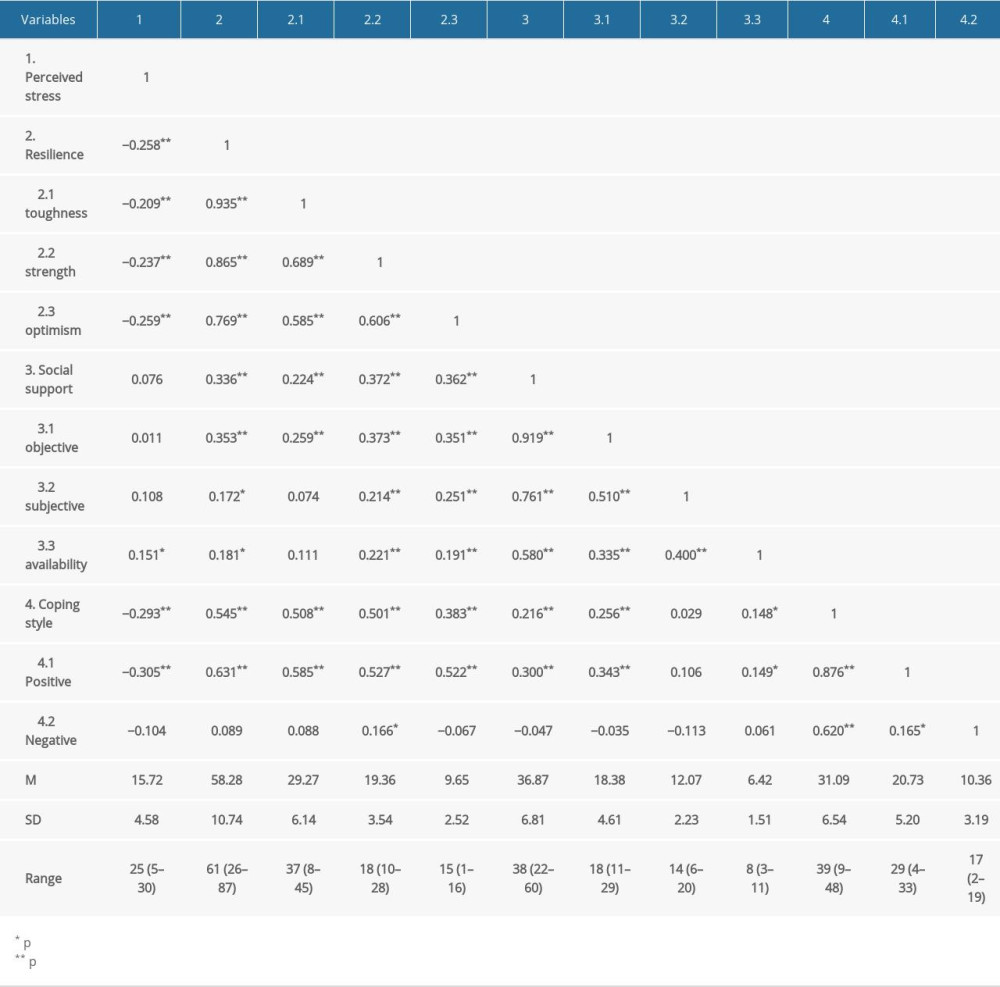 Table 2. Correlational matrix of perceived stress, resilience, social support, and coping style of participants. Survey of patients on maintenance hemodialysis (MHD) at the Guangdong Province Traditional Chinese Medical Hospital and the Hedong Hospital of Guangzhou Liwan District People’s Hospital during the COVID-19 pandemic lockdown period in China, 2021.
Table 2. Correlational matrix of perceived stress, resilience, social support, and coping style of participants. Survey of patients on maintenance hemodialysis (MHD) at the Guangdong Province Traditional Chinese Medical Hospital and the Hedong Hospital of Guangzhou Liwan District People’s Hospital during the COVID-19 pandemic lockdown period in China, 2021.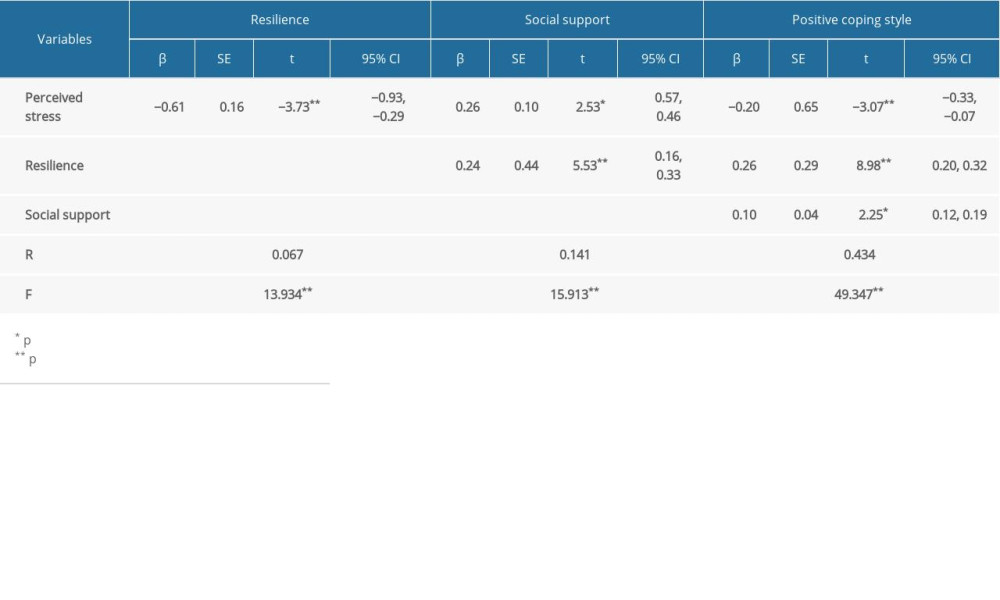 Table 3. The chain mediating model of perceived stress, resilience, social support and positive coping style. Survey of patients on maintenance hemodialysis (MHD) at the Guangdong Province Traditional Chinese Medical Hospital and the Hedong Hospital of Guangzhou Liwan District People’s Hospital during the COVID-19 pandemic lockdown period in China, 2021.
Table 3. The chain mediating model of perceived stress, resilience, social support and positive coping style. Survey of patients on maintenance hemodialysis (MHD) at the Guangdong Province Traditional Chinese Medical Hospital and the Hedong Hospital of Guangzhou Liwan District People’s Hospital during the COVID-19 pandemic lockdown period in China, 2021.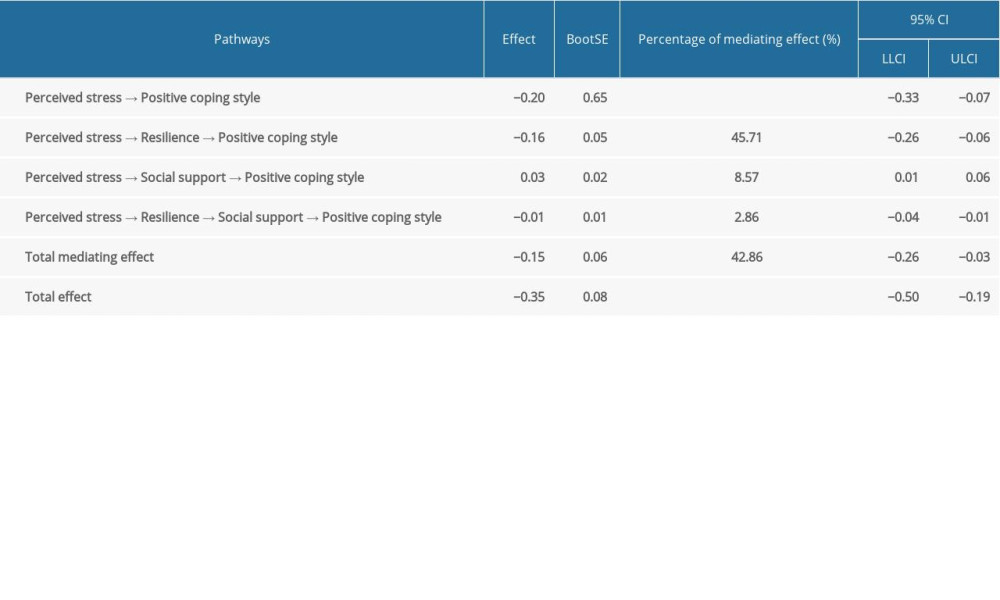 Table 4. The analysis of the chain mediating effect of resilience and social support to perceived stress and positive coping style. Survey of patients on maintenance hemodialysis (MHD) at the Guangdong Province Traditional Chinese Medical Hospital and the Hedong Hospital of Guangzhou Liwan District People’s Hospital during the COVID-19 pandemic lockdown period in China, 2021.
Table 4. The analysis of the chain mediating effect of resilience and social support to perceived stress and positive coping style. Survey of patients on maintenance hemodialysis (MHD) at the Guangdong Province Traditional Chinese Medical Hospital and the Hedong Hospital of Guangzhou Liwan District People’s Hospital during the COVID-19 pandemic lockdown period in China, 2021.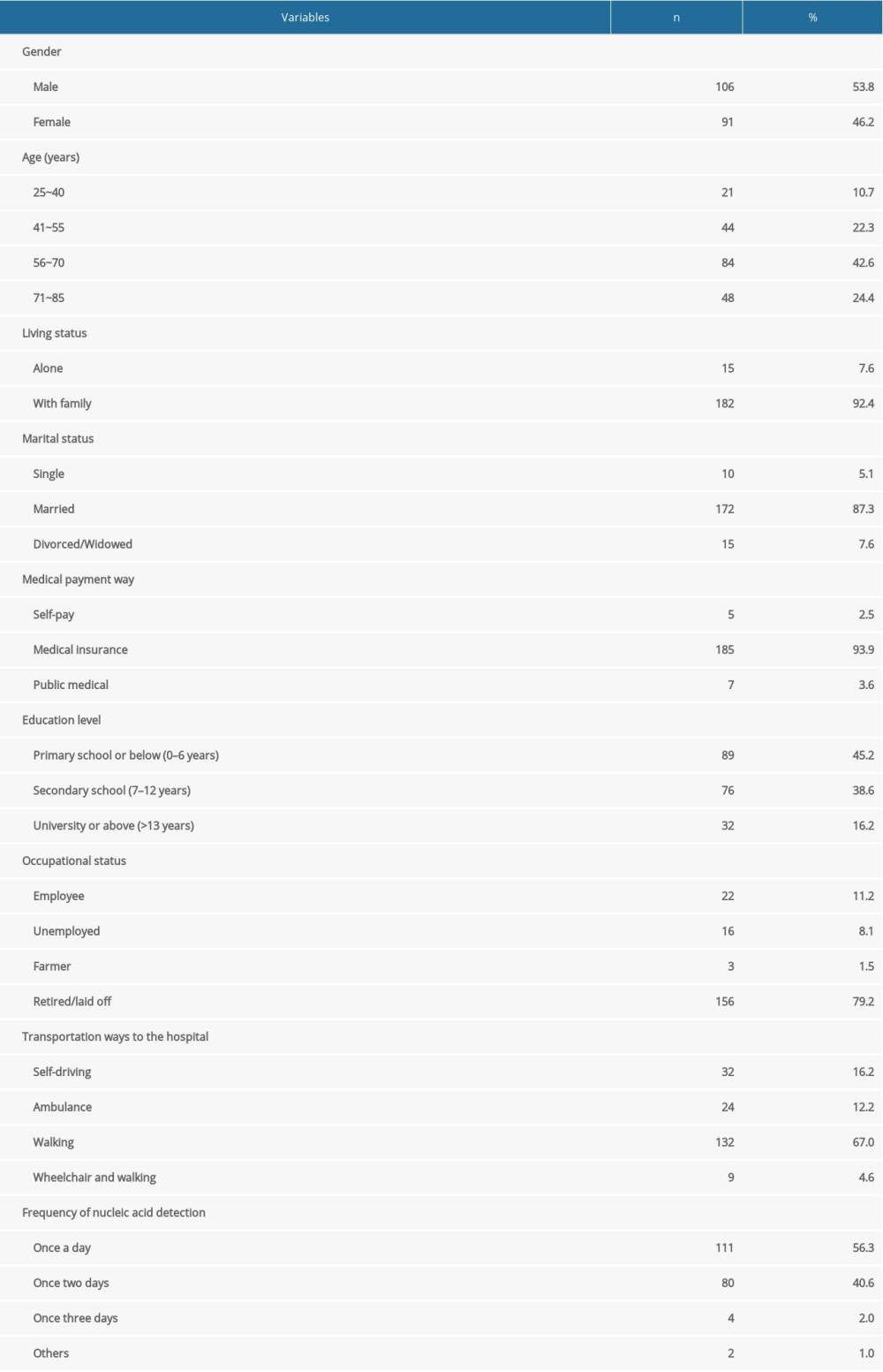 Table 1. Sociodemographic characteristics of participants. Survey of patients on maintenance hemodialysis (MHD) at the Guangdong Province Traditional Chinese Medical Hospital and the Hedong Hospital of Guangzhou Liwan District People’s Hospital during the COVID-19 pandemic lockdown period in China, 2021.
Table 1. Sociodemographic characteristics of participants. Survey of patients on maintenance hemodialysis (MHD) at the Guangdong Province Traditional Chinese Medical Hospital and the Hedong Hospital of Guangzhou Liwan District People’s Hospital during the COVID-19 pandemic lockdown period in China, 2021.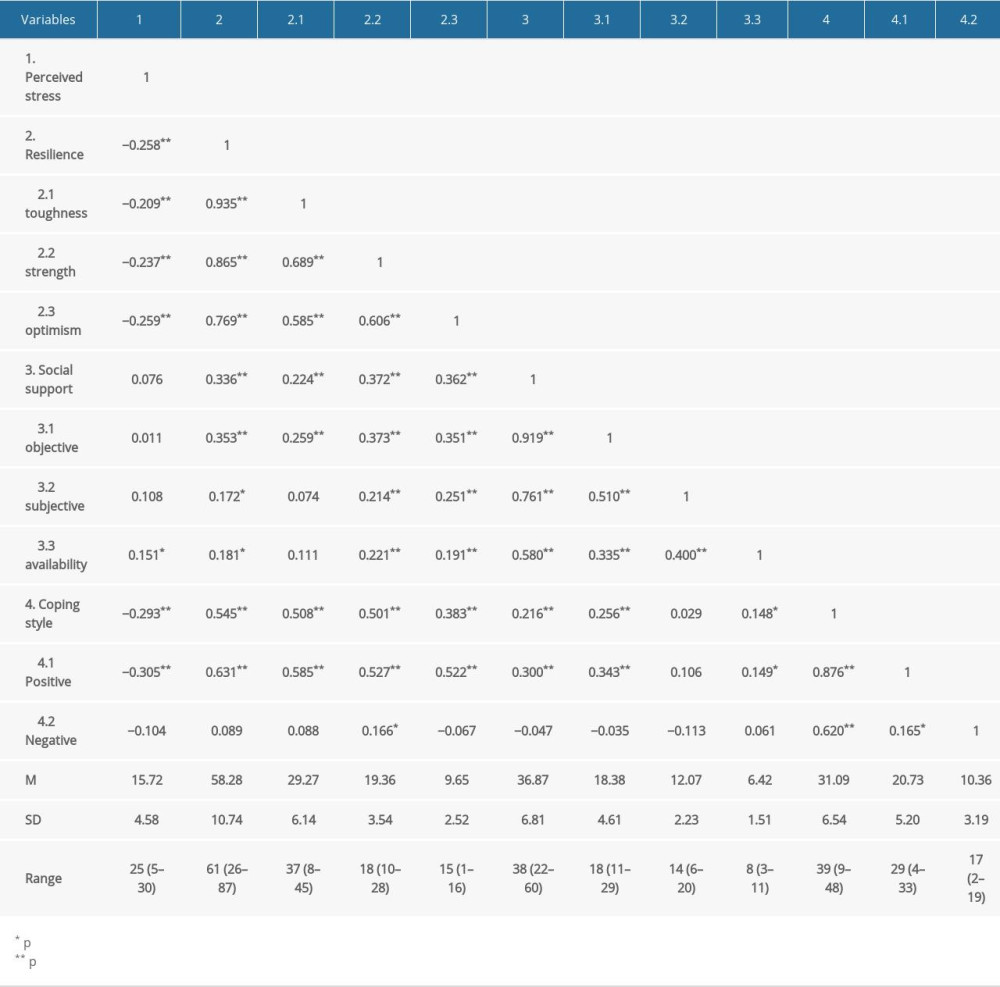 Table 2. Correlational matrix of perceived stress, resilience, social support, and coping style of participants. Survey of patients on maintenance hemodialysis (MHD) at the Guangdong Province Traditional Chinese Medical Hospital and the Hedong Hospital of Guangzhou Liwan District People’s Hospital during the COVID-19 pandemic lockdown period in China, 2021.
Table 2. Correlational matrix of perceived stress, resilience, social support, and coping style of participants. Survey of patients on maintenance hemodialysis (MHD) at the Guangdong Province Traditional Chinese Medical Hospital and the Hedong Hospital of Guangzhou Liwan District People’s Hospital during the COVID-19 pandemic lockdown period in China, 2021.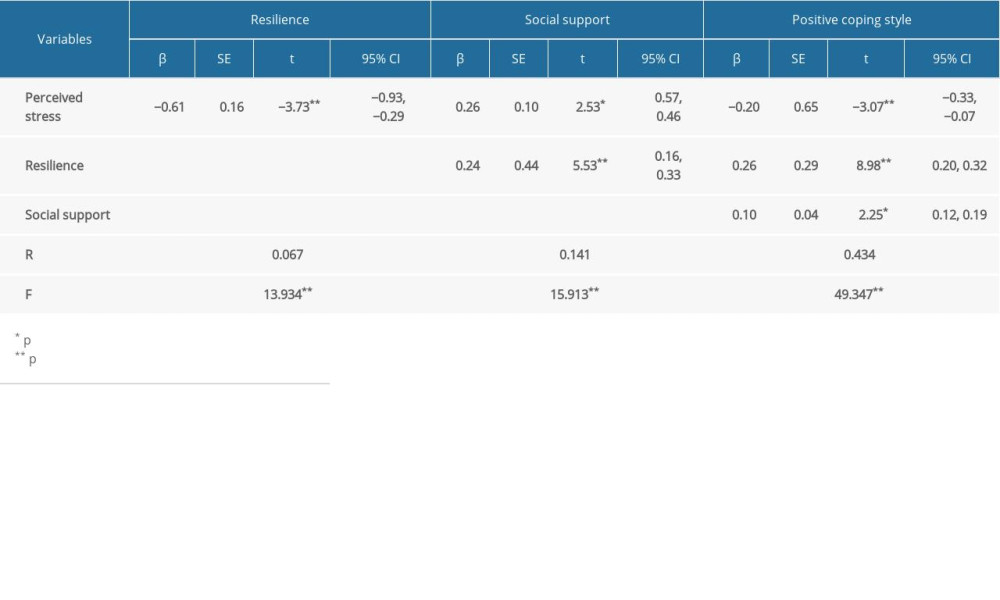 Table 3. The chain mediating model of perceived stress, resilience, social support and positive coping style. Survey of patients on maintenance hemodialysis (MHD) at the Guangdong Province Traditional Chinese Medical Hospital and the Hedong Hospital of Guangzhou Liwan District People’s Hospital during the COVID-19 pandemic lockdown period in China, 2021.
Table 3. The chain mediating model of perceived stress, resilience, social support and positive coping style. Survey of patients on maintenance hemodialysis (MHD) at the Guangdong Province Traditional Chinese Medical Hospital and the Hedong Hospital of Guangzhou Liwan District People’s Hospital during the COVID-19 pandemic lockdown period in China, 2021.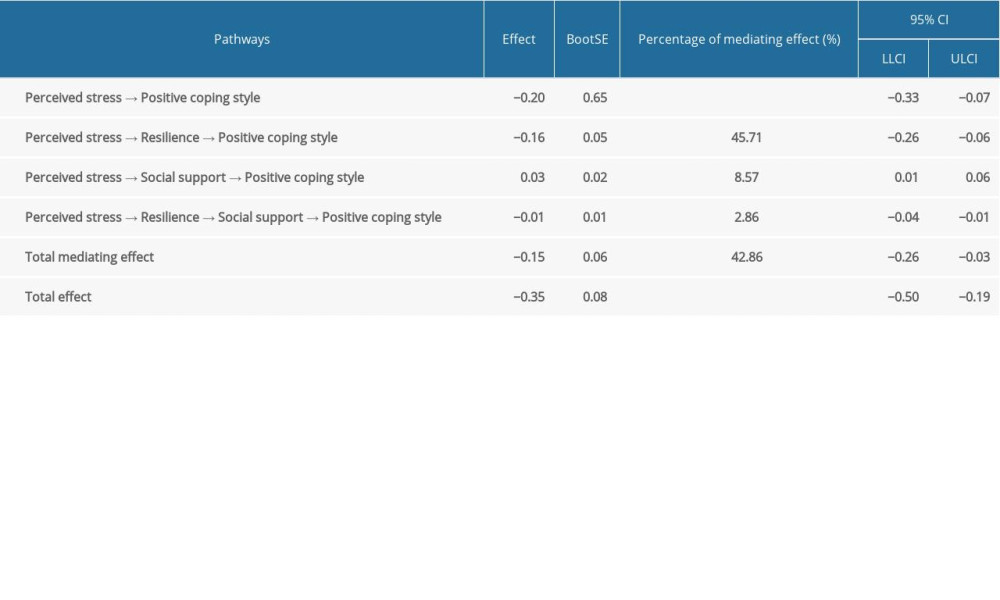 Table 4. The analysis of the chain mediating effect of resilience and social support to perceived stress and positive coping style. Survey of patients on maintenance hemodialysis (MHD) at the Guangdong Province Traditional Chinese Medical Hospital and the Hedong Hospital of Guangzhou Liwan District People’s Hospital during the COVID-19 pandemic lockdown period in China, 2021.
Table 4. The analysis of the chain mediating effect of resilience and social support to perceived stress and positive coping style. Survey of patients on maintenance hemodialysis (MHD) at the Guangdong Province Traditional Chinese Medical Hospital and the Hedong Hospital of Guangzhou Liwan District People’s Hospital during the COVID-19 pandemic lockdown period in China, 2021. In Press
15 Apr 2024 : Laboratory Research
The Role of Copper-Induced M2 Macrophage Polarization in Protecting Cartilage Matrix in OsteoarthritisMed Sci Monit In Press; DOI: 10.12659/MSM.943738
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








