03 May 2022: Clinical Research
Retrospective Study of 23 Patients with Traumatic Posterolateral Tibial Plateau Fracture Treated in a Single Center Between 2017 and 2019 with Lateral Arthrotomy, Reduction, and Plate Fixation Using the Frosch Approach
Fukang Zhu1ABCDEF, Chenyao Wu1BCF, Qihong Wu1BCF, Yucheng Huang1DE, Yi Liu1DE, Jing Jiao1DEG, Junwen Wang1ADEG*DOI: 10.12659/MSM.935377
Med Sci Monit 2022; 28:e935377
Abstract
BACKGROUND: The Frosch approach is a posterolateral surgical procedure performed with or without osteotomy of the fibula for the treatment of posterolateral tibial plateau fractures (PLFs). This retrospective study from a single center aimed to evaluate 23 patients with PLFs who underwent surgical reduction with the Frosch approach between January 2017 and October 2019.
MATERIAL AND METHODS: Twenty-three patients, 4 with Schatzker type V and 19 with Schatzker type II fractures were enrolled. Postoperative radiographs were performed regularly to measure the medial proximal tibial angle (MTPA), lateral posterior slope angle (LPSA), medial posterior slope angle (MPSA), and articular step-off to evaluate the fracture reduction. At the last follow-up, the Hospital for Special Surgery (HSS) knee score and knee range of motion (ROM) were used to assess knee function.
RESULTS: Radiograph examinations indicated excellent reduction and fixation of fractures in all patients. The average HSS scores and ROM of the 23 patients were 88.0±3.5 and 131.8±7.8°, respectively, with an average of 30.5±4.6 months of follow-up. Skin numbness occurred in 3 patients but was recovered within 6 months. One patient sustained superficial wound infection, and another patient had superficial adipose tissue liquefaction necrosis.
CONCLUSIONS: This experience from a single center demonstrated the advantage of the Frosch approach in visualizing the posterolateral and lateral tibial plateau from a single surgical incision and resulted in excellent postoperative outcomes at follow-up when evaluated by the HSS score, ROM, and radiographic evaluation of the MTPA, LPSA, and MPSA.
Keywords: Knee Injuries, Tibial Fractures, Bone Plates, Fibula, Fracture Fixation, Internal, Humans
Background
Reduction of the articular surface, restoration of lower limb alignment, and the achievement of stable internal fixation concerning the soft tissue envelope should be considered as prerequisites for excellent treatment outcomes of tibial plateau fractures [1]. Inadequate exposure of the articular surface is the main risk factor for the poor prognosis of patients [2]. With the development of 3-dimensional computed tomography (CT) and reconstruction techniques, the classification of tibial plateau fracture types has evolved from the traditional planar Schatzker [3] and AO classifications [4] to the 3-dimensional Three-Column classification [5]. This theory divides the tibial plateau into lateral, medial, and posterior columns. The fractures involving the lateral part of the posterior column are called posterolateral tibial plateau fractures (PLFs).
Tibial plateau fractures occur in 10.3 per 100 000 annually, of which AO type 41-B3 is the most common, accounting for up to 35%. People aged 40 to 60 years have the highest frequency of fractures, with men more likely to have falls and auto accidents, and women more likely to have accidents from cycling or indoor activities [6]. Up to 66.1% of tibial plateau fractures involve the posterolateral column [7]. PLFs are difficult to expose through traditional anterolateral approaches, and double incisions are required when fractures extend the anterior articular surface. For this type of injury, it is necessary to correctly choose the surgical approach to achieve the best articular congruity and stable internal fixation. Direct visualization of the fragments is a key factor in achieving this goal [8]. In recent years, scholars have had extensive discussions on this issue. Tarng et al [9] reached the posterior region through a reverse L incision and treated anterior injury in combination with an anterolateral approach, which differed from the more invasive osteotomy procedures used by some other authors [10–12]. Verona et al [13] used arthroscopically assisted reduction and internal fixation to treat simple tibial plateau fractures and achieved encouraging results. This supported the view that the available treatment outcomes were not contradicted approaches aiming to limit soft tissue injuries and treat associated intra-articular lesions simultaneously [14]. However, none of the above approaches could simultaneously meet the requirements of less trauma and direct visualization of fragments. While it changed in 2010, the innovative posterolateral approach, which was also called the Frosch approach, attracted extensive attention from orthopedic surgeons for ensuring the visualization of the posterolateral and anterolateral articular surfaces without osteotomy to protect the surrounding soft tissues. The Frosch approach provides 2 surgical windows from 1 incision, the lateral arthrotomy window for articular surface inspection, and the posterolateral window for fragment reduction and buttress fixation [15]. Yi et al [16] also reported successful cases of using the Frosch approach to place a “Barrel hoop plate” in the treatment of posterolateral depression fractures. Subsequently, for the requirement of additional osteotomy in some patients in the previous study, and in the face of the problem of poor mobility of the common peroneal nerve (CPN) [15], Mancini et al [17] made modifications based on this technique. With patients laying in a three-quarter dorsolateral position, the surgeons could better expose the articular surface of the posterolateral tibial plateau. However, reports on the treatment of this surgical technique were of all small samples with a short follow-up. Therefore, this retrospective study from a single center aimed to evaluate 23 patients with PLFs who underwent surgical reduction with the Frosch approach between 2017 and 2019.
Material and Methods
ETHICAL STATEMENT:
This study has been approved by the Ethics Committee of Wuhan Fourth Hospital (no. KY2021-083-01), and all patients provided informed consent.
PATIENT SELECTION CRITERIA:
The inclusion criteria for patients were as follows: 1) patients diagnosed with fresh PLFs between January 2017 and October 2019 in our institution, and 2) patients underwent the Frosch approach or Frosch combined with a posteromedial approach for Schatzker V tibial plateau fracture. The exclusion criteria were as follows: 1) patients with pathological fracture; 2) patients with a history of knee surgery or injury; 3) patients with neurovascular injury or compartment syndrome, and 4) patients with polytrauma.
PREOPERATIVE MANAGEMENT:
All patients were treated with leg braces or calcaneal traction and mannitol when necessary. Low-molecular-weight heparin 0.4 mg a day was given to prevent deep vein thrombosis. Knee joint X-ray (Wandong, Beijing, China) and 3-dimensional CT reconstruction (Toshiba, CA, USA) radiological examinations were completed before surgery. One typical case from our study was demonstrated in Figure 1. All patients underwent surgery after the presence of a wrinkled sign on the skin.
SURGICAL APPROACH:
The fibula head and lateral joint line were marked on the knee joint, as they were important anatomical markers, so that we could prevent damage to the CPN and locate exactly where we needed to operate. Following administration of general anesthesia, the patient was placed in the lateral decubitus position. When the fracture type was Schatzker V, the patient was placed prone for surgery. Skin incision began 3 cm above the articular and extended distally along with the fibula head (Figure 2). After opening the subcutaneous tissue and fascial layer, we could identify the CPN, which was at the rear edge of the biceps femoris muscle. The nerve needed to be isolated from surrounding soft tissue until it could be fully moved without any possible injury (Figure 3). To get a surgical window for the exposure of the anterolateral articular surface, the tractus iliotibial was partially detached from Gerdy’s tubercle. After incision of the lateral capsule, a suture was used to pull the lateral meniscus. Therefore, the entire lateral tibial plateau articular surface could be easily inspected (Figure 4). When necessary, a cortical window could be made on the anterolateral tibial epiphyseal to help restore the articular surface height according to the characteristic of the fracture [16]. Then, dissection was performed between the interval of the posterior margin of the biceps femoris muscle and the lateral head of the gastrocnemius muscle, and the lateral head of the gastrocnemius muscle was used to fully protect the vascular nerve tract at the popliteal fossa. The inferior lateral genicular artery was routinely ligated. Satisfactory exposure of the PLFs could be achieved after partial dissection of the soleus muscle distally to the approximate level of the fibula neck [15] (Figure 5). During this process, the CPN might be seen crossing the interosseous membrane from here. In addition, the presence of the anterior tibial artery approximately 5 cm distal to the articular surface should have been noted. Reduction and fixation were further determined using a C-arm machine (Figure 6A, 6B) after placing a distal radial T-shaped pre-bent plate posteriorly and a lateral locking plate (Figure 7). Finally, the incision was sutured by layers after irrigation and the placing of drainage.
POSTOPERATIVE MANAGEMENT AND REHABILITATION:
Second-generation cephalosporin 1.5 mg twice a day was used for prophylactic anti-infective therapy, and low-molecular-weight heparin 0.4 mg a day was administered after surgery. The drainage was removed within 48 h after surgery. Active knee extension was encouraged to start 1 day after surgery. Sixth weeks later, patients were allowed to partial toe-touch, weight-bearing gradually. The time of full weight-bearing was required to satisfy radiographic or clinical criteria for fracture union.
FOLLOW-UP AND EVALUATION INDICATORS:
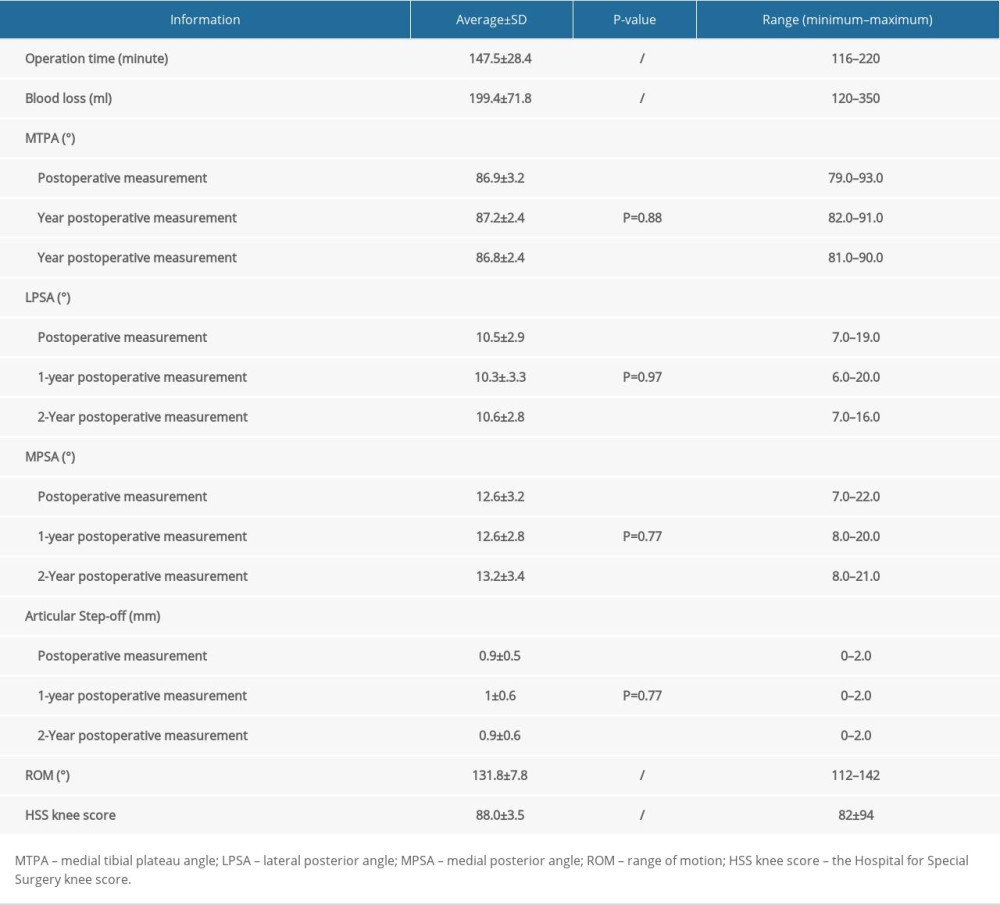
Standard anteroposterior and lateral knee X-ray radiographs that required a slight internal rotation of the lower limb to ensure the anterior position of the patella were obtained to evaluate the reduction immediately after surgery and 1 and 2 years after surgery. The Neusoft Picture Archiving and Communication System (Dongruan Dalian China) was used to measure the medial proximal tibial angle (MTPA), lateral posterior slope angle (LPSA), medial posterior slope angle (MPSA), and articular step-off on X-rays during follow-up [18]. Bone malreduction is defined as a tibial plateau step-off ≥2 mm; MTPA ≥95° or ≤80°; and PSA ≥15° or ≤-5°. Secondary loss of reduction is indicated with a change of articular surface depression >2 mm or 1 of the measured angles >5° during follow-up [19]. We conducted the knee function assessment during outpatient appointments at the last follow-up. The Hospital for Special Surgery (HSS) knee score [20] was evaluated by questionnaire and subjective measurement. A goniometer (Tnagshi Huaian, China) was used to measure ROM.
STATISTICAL ANALYSIS:
The statistical analyses of the data were performed using SPSS (version 22.0, IBM Corp, Armonk, NY, USA). Continuous variables were shown by mean±standard deviation and were compared by one-way ANOVA. A value of
Results
DEMOGRAPHIC INFORMATION:
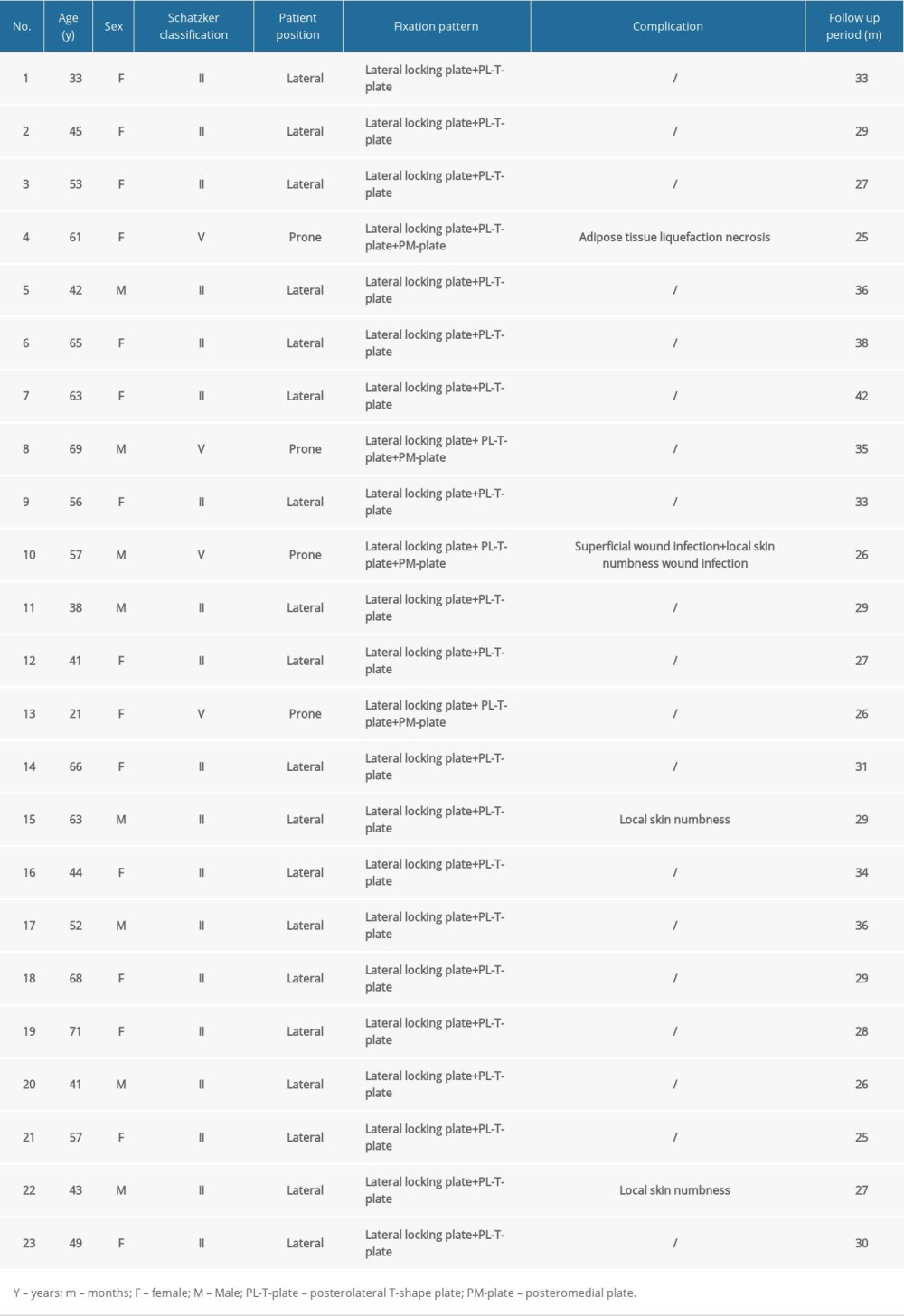
A total of 15 women and 8 men (23 knees), 4 with Schatzker type V and 19 with Schatzker type II fractures who were treated by the same senior surgeon using the Frosch approach for PLFs were enrolled. The average age of the patients was 52.1±13.0 years. The patients were followed up for an average of 30.5±4.6 months. Patients with Schatzker type II fractures were fixed with a lateral locking plate and posterolateral T-shape plate, while for the Schatzker V fractures, another posteromedial plate was added. All of the information was accessed from the medical records. The detailed demographic information of patients was listed in Table 1.
RADIOGRAPHIC MEASUREMENT AND KNEE OUTCOME:
The postoperative MTPA, LPSA, and MPSA measurements were 86.9±3.2°, 10.5±2.9°, and 12.6±3.2°, respectively. At the 1-year and 2-year follow-up visits, the MTPA was measured as 87.2±2.4° and 86.8±2.4°, respectively, and the LPSA was 10.3±3.3° and 10.6±2.8°, respectively. The results of MPSA were 12.6±2.8° and 13.2±3.4° at 1 and 2 years, respectively. The MTPA (P=0.88), LPSA (P=0.97), and MPSA (P=0.77) showed no significant differences throughout the follow-up period. The results of the articular step-off also showed no significant difference (P=0.69). The radiograph examinations indicated excellent reduction and stable fixation in all patients. After progressive functional exercises, all patients achieved satisfactory ROM with an average of 131.8± 7.8° (Figure 8A, 8B). The average HSS score was as high as 88.0±3.5. The detailed treatment information of the patients was described in Table 2.
COMPLICATIONS:
Three patients developed superficial skin numbness during treatment, which returned to normal within 6 months, without special intervention. One patient developed a superficial wound infection, which healed well after debridement and prolonged antibiotic therapy. Another patient developed superficial adipose tissue liquefaction necrosis. There were no serious neurovascular iatrogenic injuries in any of the patients.
Discussion
The main finding of the present study was that the Frosch approach was effective in the treatment of PLFs, with satisfactory outcomes for all patients. This was due to the direct visualization of the posterolateral articular surface by the Frosch approach and the most stable buttress fixation of the PLFs [21], with full respect for soft tissue. To the best of our knowledge, this was the first study with a relatively larger sample and longer follow-up period to report the effects of the Frosch approach in the treatment of PLFs.
During the follow-up, none of the patients appeared to have a reduction in the loss of fragments. Although the results of a few patients reached the definition range of malreduction or secondary loss, it may have been caused by measurement errors or nonstandard imaging positions of patients, which did not have practical significance. At the last follow-up, we measured an MTPA of 86.8±2.4°, which was similar to the 86.7±1.9° measured by Shetty et al [22] in healthy Asian adults. Also, the mean difference of LPSA and MPSA was 2.6°, which was highly consistent with the data measured by Chiu et al [23] in cadaveric specimens. Although the mean values of LPSA and MPSA measured by Chiu were 11.8° and 14.8°, respectively, these differences are acceptable considering differences in the sample patients] and measurement methods. These imaging data demonstrated that the Frosch approach fully restored normal lower extremity alignment and flat articular surface in PLFs, might help us to delay the progression of traumatic osteoarthritis [24] and decrease the risk of mid- to long-term postoperative knee pain [25]. These beneficial results stemmed from the fact that the Frosch approach not only fully exposed the fractures for stable buttress fixation, but also protected the posterolateral complex structure and minimized the impact on the blood supply of the fractures [15].
There are many studies of PLFs treated by the anterolateral approach [26–29]. Because the PLFs are too close to the lateral plateau edge, the conventional plates placed anteriorly have the problem of a bare area unsupported by rafting screws in the posterolateral articular [30]. To solve this, Cho et al [26] and Ren et al [28] used new self-made plates to treat PLFs anteriorly and achieve positive results. Meanwhile, Verona et al [13] reported the treatment of PLFs via an anterolateral arthroscopic approach. However, the above methods are contraindicated for complex comminuted PLFs. Some authors had described osteotomy approaches to better expose the posterolateral articular surface from the anterior direction. Both anterolateral intra-articular and fibular osteotomy increase the severity of fractures [10]. Fibular osteotomy is more invasive and will damage the posterolateral complex. Anterolateral osteotomy further damages articular cartilage, which may accelerate the progression of postoperative traumatic osteoarthritis. In addition, a few authors have performed the lateral femoral condyle osteotomy to expose the PLFs [12,31]. In the cadaver study by Frosch et al [8], this procedure directly exposed approximately 80% area of the lateral plateau of the tibia. The disadvantages are that it is not possible to directly observe the fractures in the metaphysis of the posterior tibia during surgery, there are few reports about the treatment of femoral lateral condyle osteotomy [32,33], and it is difficult to evaluate its therapeutic effect. What is noteworthy is that none of the above approaches can achieve stable buttress plate fixation [34].
As for the posteromedial approach, the intraoperative position needs to be changed when the anterolateral tibial plateau is involved, which increases the operative time and postoperative infection risk. The indications needed to choose a posteromedial approach or posterolateral approach for isolated posterior fractures is an interesting point. Orapiriyakul et al [35] conducted an anatomical study on cadavers and found that the optimal exposure range for the posteromedial approach was the medial 44% area between the lateral tibial spine and the lateral plateau rim located anterior to the fibular head. When the fracture is closer to the lateral area, a posterolateral approach is recommended.
Compared with previous studies focusing on the Frosch approach, our study enrolled the largest sample, which was followed for the longest time. None of the patients required additional osteotomy to better expose the surgical field, but 3 patients developed superficial skin numbness, which further suggested that we must follow the anatomic course of the CPN as much as possible and avoid stretching the CPN during reduction and fixation. However, this will happen even if the CPN is dissected accurately, and fortunately, it usually recovers spontaneously within 6 months [17]. Future studies should focus on the therapeutic differences between the Frosch approach and other approaches in prospective controlled studies of similar fracture types.
Additionally, the anterior tibial artery courses through the interosseous membrane of the lower leg distally to the articular surface and the fibular head at 50.9±6.9 mm and 36.5±6.0 mm, respectively [35,36]. There are certain differences between individuals. The surgeons should be familiar with the anatomical structure around the knee joint and master the exposure techniques to avoid iatrogenic vascular injuries. At the same time, pre-bending of the plate is necessary before the fixation of the fragments.
The main limitations of this study were as follows. First, it was a retrospective study, and therefore confounding factors that can affect the results were inevitable. For example, the type of bone graft and the degree of cartilage damage in patients could not be controlled because the study was limited to patients with Schatzker type II and V tibial plateau fractures to minimize the influence of these confounding factors. Secondly, it was a single-center retrospective study and did not prospectively compare with other approaches. Finally, the number of patients was small. However, the relevant data was sufficient to demonstrate the effectiveness of the Frosch approach in the treatment of PLFs.
Conclusions
In conclusion, the Frosch approach completed by a single center provided sufficient visualization of the posterolateral and lateral articular surfaces from only 1 incision in the treatment of PLFs and resulted in excellent radiographic parameters and knee function outcomes. Therefore, we believe that the Frosch approach is therapeutic and practical.
Figures
References
1. Mthethwa J, Chikate A, A review of the management of tibial plateau fractures: Musculoskelet Surg, 2018; 102(2); 119-27
2. Krause M, Preiss A, Meenen NM, “Fracturoscopy” is superior to fluoroscopy in the articular reconstruction of complex tibial plateau fractures-an arthroscopy assisted fracture reduction technique: J Orthop Trauma, 2016; 30(8); 437-44
3. Taşkesen A, Demirkale İ, Okkaoğlu MC, Intraobserver and interobserver reliability assessment of tibial plateau fracture classification systems: Eklem Hastalik Cerrahisi, 2017; 28(3); 177-81
4. Marsh JL, Slongo TF, Agel J, Fracture and dislocation classification compendium – 2007: Orthopaedic Trauma Association classification, database and outcomes committee: J Orthop Trauma, 2007; 21(10 Suppl); S1-133
5. Wang Y, Luo C, Zhu Y, Updated Three-Column Concept in surgical treatment for tibial plateau fractures – a prospective cohort study of 287 patients: Injury, 2016; 47(7); 1488-96
6. Elsoe R, Larsen P, Nielsen NP, Population-based epidemiology of tibial plateau fractures: Orthopedics, 2015; 38(9); e780-86
7. Yao X, Xu Y, Yuan J, Classification of tibia plateau fracture according to the “four-column and nine-segment”: Injury, 2018; 49(12); 2275-83
8. Krause M, Frings J, Isik H, Comparison of extended lateral approaches to the tibial plateau: The articular exposure of lateral epicondyle osteotomy with and without popliteus tendon vs. fibula osteotomy: Injury, 2020; 51(8); 1874-78
9. Tarng Y-W, Lin K-C, A combined prone and supine approaches for complex three column tibial plateau fracture with posterolateral articular injury: Injury, 2019; 50(10); 1756-63
10. Chen L, Xiong Y, Yan C, Fibular neck osteotomy approach in treatment of posterolateral tibial plateau fractures: A retrospective case series: Med Sci Monit, 2020; 26; e927370
11. Johnson EE, Timon S, Osuji C, Surgical technique: Tscherne-Johnson extensile approach for tibial plateau fractures: Clin Orthop Relat Res, 2013; 471(9); 2760-67
12. Kfuri M, Schatzker J, Castiglia MT, Extended anterolateral approach for complex lateral tibial plateau fractures: J Knee Surg, 2017; 30(3); 204-11
13. Verona M, Marongiu G, Cardoni G, Arthroscopically assisted reduction and internal fixation (ARIF) versus open reduction and internal fixation (ORIF) for lateral tibial plateau fractures: A comparative retrospective study: J Orthop Surg Res, 2019; 14(1); 155
14. McNamara IR, Smith TO, Shepherd KL, Surgical fixation methods for tibial plateau fractures: Cochrane Database Syst Rev, 2015(9); CD009679
15. Frosch K-H, Balcarek P, Walde T, A new posterolateral approach without fibula osteotomy for the treatment of tibial plateau fractures: J Orthop Trauma, 2010; 24(8); 515-20
16. Yi Z, Hui S, Binbin Z, A new strategy to fix posterolateral depression in tibial plateau fractures: Introduction of a new modified Frosch approach and a “Barrel hoop plate” technique: Injury, 2020; 51(3); 723-34
17. Mancini N, Salvato D, Delmastro E, A modified Frosch approach for posterior tibial plateau fractures: Technical note and case series: Injury, 2021 [Online ahead of print]
18. Luo C-F, Reference axes for reconstruction of the knee: Knee, 2004; 11(4); 251-57
19. Wicky S, Blaser PF, Blanc CH, Comparison between standard radiography and spiral CT with 3D reconstruction in the evaluation, classification and management of tibial plateau fractures: Eur Radiol, 2000; 10(8); 1227-32
20. Insall JN, Dorr LD, Scott RD, Rationale of the Knee Society clinical rating system: Clin Orthop Relat Res, 1989(248); 13-14
21. Zhang W, Luo C-F, Putnis S, Biomechanical analysis of four different fixations for the posterolateral shearing tibial plateau fracture: Knee, 2012; 19(2); 94-98
22. Shetty GM, Mullaji A, Bhayde S, Factors contributing to inherent varus alignment of lower limb in normal Asian adults: Role of tibial plateau inclination: Knee, 2014; 21(2); 544-48
23. Chiu KY, Zhang SD, Zhang GH, Posterior slope of tibial plateau in Chinese: J Arthroplasty, 2000; 15(2); 224-27
24. Parkkinen M, Madanat R, Mustonen A, Factors predicting the development of early osteoarthritis following lateral tibial plateau fractures: Mid-term clinical and radiographic outcomes of 73 operatively treated patients: Scand J Surg, 2014; 103(4); 256-62
25. Biz C, Maso G, Gambato M, Challenging surgical treatment of displaced articular tibial plateau fractures: Do early knee radiographic features have a predictive value of the mid-term clinical functional outcomes?: Orthop Surg, 2019; 11(6); 1149-62
26. Cho J-W, Samal P, Jeon Y-S, Rim plating of posterolateral fracture fragments (PLFs) through a modified anterolateral approach in tibial plateau fractures: J Orthop Trauma, 2016; 30(11); e362-68
27. Hu S-J, Chang S-M, Zhang Y-Q, The anterolateral supra-fibular-head approach for plating posterolateral tibial plateau fractures: A novel surgical technique: Injury, 2016; 47(2); 502-7
28. Ren D, Liu Y, Lu J, A novel design of a plate for posterolateral tibial plateau fractures through traditional anterolateral approach: Sci Rep, 2018; 8(1); 16418
29. Delcogliano M, Marin R, Deabate L, Arthroscopically assisted and three-dimensionally modeled minimally invasive rim plate osteosynthesis via modified anterolateral approach for posterolateral tibial plateau fractures: Knee, 2020; 27(3); 1093-100
30. Kim Y, Yoon Y-C, Cho J-W, Rim plate augmentation of the posterolateral bare area of the tibial plateau using a 3.5-mm precontoured locking compression plate: A cadaveric study: J Orthop Trauma, 2018; 32(5); e157-60
31. Yoon Y-C, Sim J-A, Kim D-H, Combined lateral femoral epicondylar osteotomy and a submeniscal approach for the treatment of a tibial plateau fracture involving the posterolateral quadrant: Injury, 2015; 46(2); 422-26
32. Kfuri M, Schatzker J, Castiglia MT, Extended anterolateral approach for complex lateral tibial plateau fractures: J Knee Surg, 2017; 30(3); 204-11
33. Bowers AL, Huffman GR, Lateral femoral epicondylar osteotomy: An extensile posterolateral knee approach: Clin Orthop Relat Res, 2008; 466(7); 1671-77
34. Sun H, He Q-F, Zhang B-B, A biomechanical evaluation of different fixation strategies for posterolateral fragments in tibial plateau fractures and introduction of the ‘magic screw’: Knee, 2018; 25(3); 417-26
35. Orapiriyakul W, Apivatthakakul T, Phornphutkul C, Posterolateral tibial plateau fractures, how to buttress? Reversed L posteromedial or the posterolateral approach: A comparative cadaveric study: Arch Orthop Trauma Surg, 2018; 138(4); 505-13
36. May H, Kastan O, Emre TY, Anterior tibial artery and its clinical importance in the posterolateral approach to the tibial plateau: An angiographic study on 219 lower limbs: J Knee Surg, 2020 [Online ahead of print]
Figures
In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952