01 November 2022: Clinical Research
Questionnaire-Based Study of 81 Patients in Poland to Evaluate the Course of Inflammatory Bowel Disease and the Effects of the COVID-19 Pandemic on Quality of Life and Mental State from February to June 2021
Natalia OwsiankoDOI: 10.12659/MSM.938243
Med Sci Monit 2022; 28:e938243
Abstract
BACKGROUND: The COVID-19 pandemic affected many people worldwide, including those with chronic diseases. Our objective was to analyze its influence on medical care and the course of inflammatory bowel disease (IBD) in Poland.
MATERIAL AND METHODS: In 2021, 81 patients in Poland with IBD completed an original anonymous questionnaire about the impact of the COVID-19 pandemic on the course of their disease and mental status. The printed questionnaire was distributed to IBD patients treated at the Gastroenterology Outpatient Clinic of the University Clinical Hospital in Białystok, and an online questionnaire was sent to patients via social media. Statistical analysis was performed using the chi-squared test, with a significance level of P<0.05.
RESULTS: The study group consisted of 46 women and 35 men with a mean age of 32.42 years. Fifty-nine patients had ulcerative colitis and 22 had Crohn disease. Patients reported significant deterioration in medication availability (50.62%) and restricted access to gastroenterology outpatient clinics (51.90%) (P<0.05). Of patients who contracted COVID-19, 89.47% did not require hospitalization, 32.10% (26/81) were asymptomatic, mild, or moderate, despite immunosuppressive biological treatment (27.16%, 22/81), or steroids (18.52%, 15/81). Over 50% of respondents stated the pandemic negatively affected their mental state and 30% of them associated that with worsening IBD.
CONCLUSIONS: During the pandemic, respondents were mainly concerned with difficulties in accessing the gastroenterology clinic and limited drug availability. The pandemic negatively affected patients’ mental state. In cases of COVID-19 disease, patients with IBD were mostly asymptomatic and did not require hospitalization, despite therapy affecting the immune system.
Keywords: Colitis, Ulcerative, COVID-19, Crohn Disease, Inflammatory Bowel Diseases, Poland, Male, Humans, Female, Adult, Pandemics, Quality of Life, Surveys and Questionnaires, Chronic Disease
Background
In December 2019, a new variant of coronavirus emerged in Wuhan, China [1]. It was later named by the International Committee on Taxonomy of Viruses as SARS-CoV-2 [2]. This new virus had spread worldwide in early 2020 and led to the World Health Organization identifying the COVID-19 outbreak as a pandemic on March 11, 2020 [3]. The most common symptoms of COVID-19 disease are fever, dry cough, and fatigue, but there are also less specific symptoms, such as different types of skin rash, nausea, vomiting, and diarrhea [4]. In Poland, from January 3, 2020, to January 12, 2022, there have been 4 248 559 reported cases of COVID-19, with 100 938 associated deaths [5].
The pandemic has had a negative impact on the global economy, healthcare, and everyday life [6]. The pandemic was especially challenging for people with chronic diseases, considering that some of the hospitals were focused on patients with COVID-19 patients, and therefore, diagnostic tests and hospital admissions for patients with chronic diseases were postponed [7]. Inflammatory bowel disease (IBD) is a group of disorders that consists of 2 forms: Crohn disease (CD) and ulcerative colitis (UC). These conditions are characterized by chronic inflammation of the gastrointestinal tract that is caused by a defective immune system. Poland is considered to have a moderate prevalence of IBD, which affects approximately 157 of 100 000 individuals [8]. Most patients with IBD require long-term treatment, regular medical appointments, and diagnostic tests, all of which may have been disrupted by the pandemic [9]. Recently, major international organizations published guidelines and strategies for the management of patients with IBD during the pandemic [10,11]. The incidence of COVID-19 in patients with IBD was low and similar to that of the general population. Unfortunately, in patients infected with SARS-CoV-2, treatment with corticosteroids or mesalamine was significantly associated with worse outcomes, compared with that of anti-TNF therapies [12,13].
This questionnaire-based study of 81 patients in Poland with a diagnosis of IBD aimed to evaluate the course of the disease and the effects of the COVID-19 pandemic on patients’ quality of life and mental state from February to June 2021.
In this study, we analyzed the impact of the COVID-19 pandemic on medical care and the course of IBD in patients using a questionnaire-based analysis. Our hypothesis assumed that the COVID-19 pandemic caused limited access to specialist treatment and negatively affected the course of IBD.
Material and Methods
ETHICAL APPROVAL AND INFORMED CONSENT:
This investigation was reviewed and approved by the local ethics committee (approval no. APK.002.247.2021), and was conducted in accordance with the Helsinki Declaration. All patients were informed about the conducted research and data collection, and a written informed consent form was obtained from each patient. Participation in the study was voluntary and the participants could withdraw at any time during the study.
STUDY DESIGN AND POPULATION:
An observational, anonymous survey study was conducted using a questionnaire to evaluate the impact of the COVID-19 pandemic on access to medications and treatment, including difficulties in obtaining consultations at gastroenterology (outpatient) clinics in patients with the 2 forms of IBD: CD and UC. Additionally, the study was designed to investigate the impact of SARS-CoV-2 infection on the course of IBD and the influence of the pandemic on the mental well-being of patients. The study group consisted of patients with IBD who were admitted to the Gastroenterology and Internal Medicine Department and Outpatient Clinic and patients from all over Poland who voluntarily responded to a questionnaire posted via social media from February to June 2021. Clinical symptoms, biochemical testing, such as blood counts, C-reactive protein, and liver enzymes, imaging, endoscopic, histopathological (analysis of endoscopy-derived sections), and stool (fecal calprotectin) examinations were all used to identify IBD in patients [14]. The CDAI scale and Mayo scale were used to assess disease activity in CD and UC, respectively.
STUDY PROTOCOL:
The study was conducted from February to June 2021 in the form of a personalized questionnaire, which was created by the authors of the study, at the Department of Gastroenterology and Internal Medicine, Medical University of Białystok (Table 1). The questionnaire was addressed to patients with IBD who were aged over 16 years and from Białystok (printed questionnaire) and all over Poland (online questionnaire). The group of respondents consisted of 81 patients.
The online questionnaire, designed in the Polish language using Google Forms, was electronically distributed on February 15, 2021, via social media and applications (Facebook, WhatsApp, Instagram) to patients with IBD, as well as via medical groups associated with patients with CD and UC. The printed questionnaire, also designed in the Polish language using Microsoft Word, was distributed from February to June 2021 to patients with UC and CD treated at the Department of Gastroenterology and Internal Medicine outpatient clinic of the University Clinical Hospital in Białystok. The duration of data collection and analysis was 5 months.
The original questionnaire was divided into 3 parts and contained 32 questions. The first part contained basic information on sex, age, level of education, and questions about past history of IBD, namely, date of diagnosis, predominant symptoms, current treatment, and flares of the disease. The second part concerned medical care during the COVID-19 pandemic and included questions about difficulties in obtaining medical care at the gastroenterology outpatient clinic, telemedicine, access to medications, and hospitalizations related to diagnostic procedures, exacerbation of symptoms, and treatment modifications for IBD. Questions about SARS-CoV-2 infection, the severity level of infection, and its influence on UC and CD courses were also included. The third part of the proprietary questionnaire concerned the effects of the COVID-19 pandemic on the mental health of patients with IBD. Questions also analyzed the influence of changes in mental well-being on the course of the underlying disease.
To determine the effect on mental health in the era of the COVID-19 pandemic, a 5-step visual analog scale was used, where 1 indicated that there was no negative effect on mental health and/or the course of IBD, and 5 indicated there was a major negative impact. This scale was intended to allow a subjective assessment of the mental state of patients before and during the COVID-19 pandemic. The questions prepared by the authors were reviewed by an expert gastroenterologist for consistency and appropriateness. Table 1 shows a summary of questions from the questionnaire.
STATISTICAL ANALYSIS:
The data were collected in Excel and then manually verified by the investigators. To avoid duplication of data, each respondent was assigned a unique Email address. Then, statistical analysis was performed with Statistica 13 software. Results were presented as mean±SD or number of patients and percentage of the total study group. The chi-square test was used to determine possible pandemic-induced changes in access to medications and difficulty obtaining consultations at gastroenterology clinics in patients with IBD. Continuous variables, such as age, were analyzed by establishing a defined data cut-off point to create 2 comparable groups. A
Results
DISEASE ACTIVITY AND TREATMENT:
At the time of completing the questionnaire, 56.80% of respondents declared that their disease was currently in clinical remission (UC 33/59, 55.93%, CD 13/22, 59.09%). The remaining 43.20% were in active disease, based on symptoms. Patients with CD most frequently reported abdominal pain (18/22), weight loss (11/22), weakness (8/22), diarrhea (8/22), ulcers (8/22), fissures (6/22), and perianal fistulas (6/22). The most frequently used forms of therapy in patients with CD were biological treatment (10/22), aminosalicylates (8/22), and immunosuppressive drugs (7/22), or no treatment (4/22). In contrast, patients with UC reported mostly diarrhea (52/59), blood in the stool (49/59), weakness (41/59), abdominal pain (40/59), and weight loss (30/59). Patients with UC most commonly used aminosalicylates (51/59), immunosuppressants (19/59), steroids (15/59), biological treatment (12/59), or no medication (2/59).
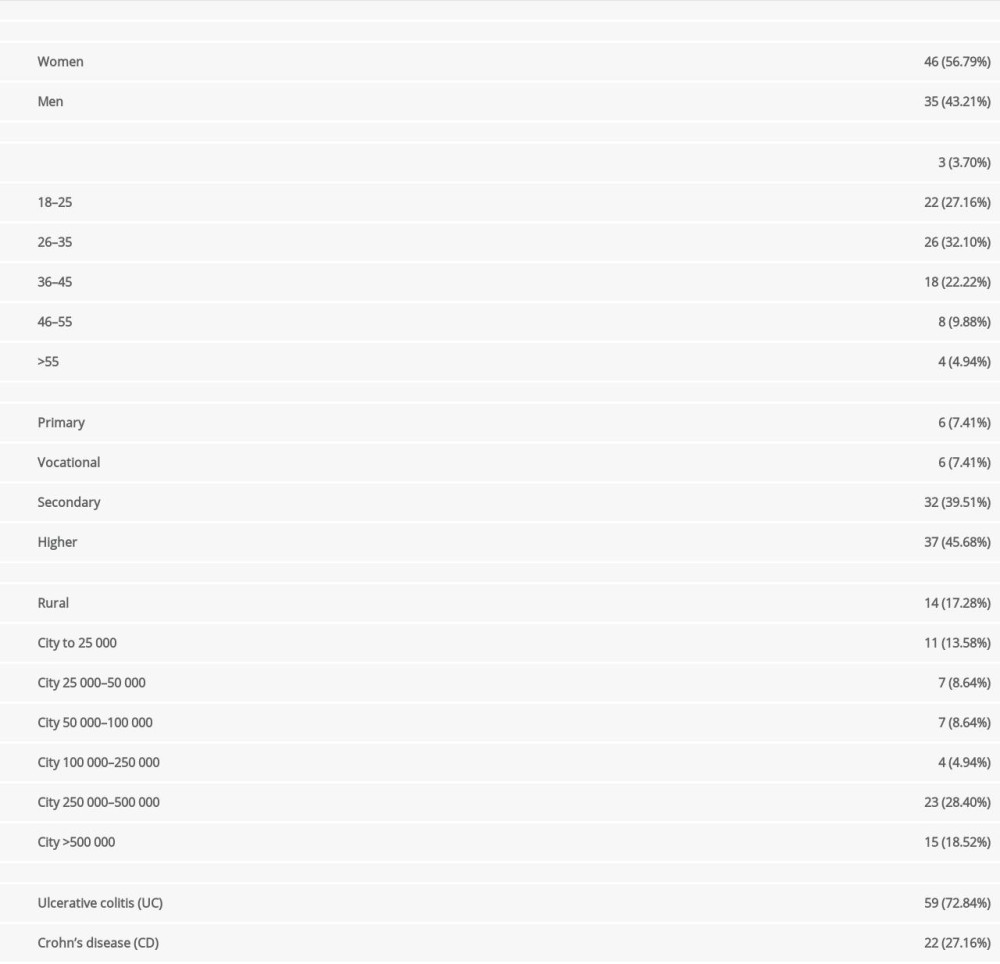
Exacerbation of disease during the COVID-19 pandemic in patients with UC (43/59, 72.90%) was significantly more frequent than in those with CD (9/22, 41.00%), with P<0.05. During the pandemic, nearly 40% of patients reported changes in IBD treatment, with 44.07% (26/59) of patients with UC and 27.27% with CD (6/22). The most common change (68.75%) was in the form of adding a new drug, changing 1 or more drugs to another (37.50%), modifying the dosage of a previously used drug (34.38%), or discontinuing a drug (21.88%) (Figure 1).
Almost one-half of patients (40/81, 49.40%; IBD-y 12/25, 48.00%; and IBD-o 28/56, 50.00%) were hospitalized during the pandemic (from March 2020 to June 2021) due to the IBD course. The most frequent reasons for hospitalization included disease exacerbation, diagnostics related to the severity of the inflammatory bowel disease, or change in treatment.
FACTORS INFLUENCING IBD CONTROL:
From March 2020, there was a statistically significant deterioration in availability to gastroenterological treatment compared with the time before the pandemic (P<0.05). Overall, 51.90% (42/81; CD-y 4/8; CD-o 7/14; UC-y 11/17; and UC-o 20/42) of respondents reported a problem in treatment availability, independent of IBD type (CD 50.00% vs UC 52.00%, P>0.05), patient age (older 48.20% vs younger 60.00%, P>0.05), disease activity (active disease 43.20% vs 56.80% remission, P>0.05), place of residence (>250 000 inhabitants vs <250 000 inhabitants, P>0.05), and educational status (higher education vs primary + secondary education, P>0.05). Among the reported problems in obtaining a consultation by a gastroenterologist, the most frequently mentioned were difficulties in scheduling (73.81%), postponing an appointment (38.10%), and hospitalization (33.33%), and difficult access to examinations (33.33%). Other concerns included cancellation of an appointment (21.43%), hospitalization (16.67%), and change of attending physician (14.29%) (Figure 2).
For 58.02% (47/81) of patients, appointments were performed with the use of telemedicine technology regardless of the IBD type (CD 54.50% vs UC 59.00%) and patient age (older 52.00% (29/56) vs younger 72.00% (18/25),
COVID-19 AND THE COURSE OF IBD:
Seventeen patients (20.99%, including 20.00% IBD-y and 21.42% IBD-o) had COVID-19, but the majority (15/17, 88.24%, CD-y 2/2, CD-o 3/3, UC-y 2/3, UC-o 8/9) did not require hospitalization and assessed the course of the disease as asymptomatic, mild, or moderate. However, 7 of 17 infected patients (41.18%) declared that the infection negatively affected the course of the underlying disease, with noticeable exacerbation of existing symptoms (6/17, 35.29%; IBD-y 1/5, 20.00%; and IBD-o 5/12, 41.65%), appearance of new symptoms (2/17, 11.76%; only IBD-o 2/12, 16.67%), and the need for hospitalization (2/17, 11.76%; only IBD-o 2/12, 16.67%) in the gastroenterology department.
From all respondents, 53.09% (43/81, IBD-y 18/25, 72.00% and IBD-o 25/56, 44.64%,) believed that the pandemic had influenced their mental well-being (IBD-y vs IBD-o, P<0.05), and 83.72% (36/43) of them (IBD-y 14/18, 77.78% and IBD-o 22/25, 88.00%, P>0.05) determined this impact was negative (Figure 3). Among those patients, 58.13% (25/43; IBD-y 9/25, 36.00%; and IBD-o 16/25, 64.00%) associated the decrease of mental well-being with a worse course of IBD.
Discussion
We conducted a survey to investigate the impact of the COVID-19 pandemic on the medical care of patients with IBD in Poland. The results indicated that the pandemic had multiple effects on those patients. We observed difficulties in accessing gastroenterology outpatient clinics, in scheduling hospitalization, and in accessing prescribed medications. Our results also suggested that most patients had mild to moderate SARS-CoV-2 infection and did not require hospitalization for COVID-19. In addition, we observed that only a small fraction of patients actually contracted SARS-CoV-2 infection. More than one-half of patients pointed out that online consultations replaced regular visits in the gastroenterology outpatient clinic. Moreover, the majority indicated that they were satisfied with this form of contact with doctors, regardless of the patient’s age. Finally, an analysis of the questionnaire showed that more than one-half of the patients observed that the COVID-19 pandemic affected their mental well-being, most of them negatively.
Many of the patients in our study, due to the changing epidemiological situation, experienced difficulties accessing gastroenterology clinics and making follow-up appointments. They also indicated problems with postponed or rescheduled hospitalizations. Another published study also showed a significant decrease in hospitalizations in patients with IBD, mainly during the initial phase of the COVID-19 pandemic, primarily due to the heavy burden of patients with COVID-19 filling hospital beds [15]. It is remarkable that the incidence of hospitalization of patients with UC and CD has decreased considerably in the last decade, especially in patients under 40 years of age; therefore, it is not possible to say whether our results prove the impact of the pandemic on this factor [16]. In a study conducted by in an Italian center, the results were comparable to ours, with more than one-half of the patients being seen for a scheduled appointment and one-fifth having their appointments rescheduled [17]. In the present study, some patients mentioned that the intravenous administration of biological drug was postponed, as this procedure requires a 1-day hospitalization in Poland for formal reasons. This problem was also observed in another study [18].
Patients in the present study also reported having a problem with access to prescribed medications, most likely due to stock shortages and logistical difficulties, which could also affect the underlying disease. However, a survey conducted in 27 countries indicated that only 8.9% of the respondents had problems with the availability of essential medications [19]. However, that questionnaire had several limitations, such as a diverse group of patients and use of the vague term “essential medications”. Due to the limited nature of the aforementioned study, as well as the limitations of our study, we cannot clearly indicate what these differences in drug availability result from.
Most of the patients in the present study had a mild to moderate SARS-CoV-2 infection and did not require hospitalization for this reason, despite the fact that the treatment used for IBD affects the immune system, modulates immunity, and can contribute to a higher risk of infection [20]. We speculate that this may be related to the fact that not every immunosuppressive treatment can cause clinical deterioration, because drugs exhibit different mechanisms of action. Other reports indicated that TNF-α is also overexpressed in SARS infection, so that biologic treatment with adalimumab (a monoclonal antibody anti-TNF-α) may paradoxically be a protective factor against severe COVID-19 [21–23]. Another study also indicated that biologic therapies can lessen the likelihood of adverse COVID-19 implications, such as cytokine storm syndrome [12]. Also, it has been reported that TNF inhibitors can be effective in reducing organ damage. This effect is achieved by the reduced excretion of the ectodomain of angiotensin-converting enzyme 2 (ACE2), which is essential for SARS-CoV-2 entry into the cell [24]. Studies reported that only long-term steroid use worsened clinical outcomes, and patients on steroidal treatment were more likely to be admitted to intensive care units [25]. In another study it was found that the use of either steroids or mesalazine was associated with a worse course of infection [13]. However, in our study, of the 15 patients using steroids, only 3 had COVID-19 and none of them required hospitalization. In view of these results, it seems reasonable to recommend to patients with IBD the same methods of prevention and treatment of COVID-19 as in the general population. In addition, only a minority of infected patients reported that the infection adversely affected the course of the underlying disease, with exacerbation of existing symptoms or appearance of new ones. This is consistent with the results of other published studies [26,27]. In our results, only a small proportion of patients acquired SARS-CoV-2 infection, which agrees with the results of other studies that have been performed [24,28,29] and contradicts the concern that patients with IBD were at greater risk of being infected with SARS-CoV-2. Concerns have been raised in studies that found increased expression of the soluble form of ACE2 by which coronaviruses bind to target cells in the human body [28]. It is currently speculated that the soluble form of ACE2 does not anchor to the membrane and circulates in small amounts in the blood. Therefore, it may competitively capture SARS-CoV-2 and prevent the viral particle from binding to full-length ACE2, allowing it to enter the body and develop infection. However, further studies on a large group of patients with pharmacodynamic analysis of the effects of drugs used in IBD are needed to definitively verify and clarify this relationship.
Taking into consideration the course of COVID-19 disease in patients with IBD, most of our respondents did not require hospitalization and assessed the course of the disease as asymptomatic or mild. When comparing the older and younger groups in terms of the impact of COVID-19 on underlying disease, we noted that mainly older patients reported an exacerbation of existing symptoms of IBD, as well as the appearance of new ones, and were more likely to require hospitalization for this reason. Similar results were reported by Brenner et al [25].
Our survey also indicated that 59.25% (48/81) of patients had an online consultation instead of an in-person visit in a gastroenterology outpatient clinic. Online consultation and telemedicine have become the most common solutions, as was observed in other studies [18,24,28,30]. Telemedicine has many advantages, including access to the general practitioner from home, cost savings by not having to travel, and reduced risk of SARS-CoV-2 transmission by avoiding groups of people in the clinic. There are also limitations to telemedicine, primarily because the physician relying on the patient’s interpretation of the problem and verbal communication from a distance is not always effective [30]. In patients with IBD, this is particularly important because they do not have access to physical, laboratory, or endoscopic examination when the consultation takes place online. However, it is worth mentioning that more than one-half of the patients in the present study positively evaluated this form of contact with a physician. Other studies also showed high trust, satisfaction, and good accessibility to telemedicine and its management of gastroenterological diseases, such as IBD, celiac disease, and HCV infection. This indicates a high probability of expanding this form of contact with the gastroenterological patient in the future [31,32]. According to our results, patient age had no influence on the use of telemedicine counseling. However, other studies have indicated that this form of contact has been chosen more frequently by younger patients [33,34].
Another issue we assessed in our study was the impact of the COVID-19 worldwide outbreak on the mental well-being of patients. Our results indicated that in more than one-half of patients surveyed the COVID-19 pandemic significantly and negatively affected the mental well-being of most patients. One-third of patients associated mental deterioration with the pandemic’s negative impact on their control of the underlying disease. Other studies also confirmed the deterioration of mental status among patients with chronic diseases, especially those associated with immunosuppression, which is likely due to concerns about the severity and occurrence of complications of COVID-19 infection [35]. In addition, patients with other chronic diseases, such as asthma, diabetes, hypertension, and heart failure, were more likely to experience stress, anxiety and to develop depression than healthy control individuals [36,37]. Other studies indicated that social isolation increased negative emotions and psychological outcomes, including confusion, anger, anxiety, and depression [38–41]. In addition, prolonged exposure to loneliness is a critical risk factor for post-traumatic stress disorder symptoms [38]. A number of factors, including age, have also been shown to increase the likelihood of mental disorders; however, reports on this topic are conflicting, with some sources citing younger age as a risk factor, while other sources found that mental health problems are more prevalent among the elderly [39,42]. Other risk factors include female sex, education, occupation, economic conditions, and close contact with SARS-CoV-2-infected individuals [40,41].
Our results suggested that special emphasis should be placed on good contact between health professionals and patients with IBD during the COVID-19 pandemic to effectively guide treatment and prevent complications. This is crucial because, in most cases, continuation of current therapy and ongoing contact with a gastroenterologist helped to avoid relapse and unnecessary hospitalizations. In addition, psychological support should be provided to patients, as a change in mental status due to the pandemic situation can also worsen the course of the disease. We believe that further multicenter studies are needed to thoroughly evaluate the risk of COVID-19 in IBD patients and the efficacy and dangers of their immunomodulating drugs. This can significantly affect the milder course of infection and prevent exacerbations, hospitalizations, and mental state deterioration.
Our study had several limitations. The short follow-up period could have caused errors in estimating the long-term care of patients with IBD. Also, the relatively small study group did not represent an overall picture of patients with IBD in general, because their concerns, comorbidities, and additional treatments can affect the course of the underlying disease and that of COVID-19. Further, the small group of patients did not allow for a detailed assessment of the effectiveness of the medications used and their impact on the course of COVID-19. Finally, the small number of included patients also means that the statistical analysis may not have identified significant findings with adequate sensitivity.
Conclusions
Based on the survey results, the main concerns of patients with IBD during the COVID-19 pandemic were difficulties in accessing medicine and gastroenterology clinics. Therefore, the data has shown that the healthcare system needs to be better prepared for extreme situations occurring in the world in order to provide long-term medical care for patients with IBD and other chronic diseases. In terms of mental health, most patients felt that the pandemic negatively affected their mental well-being and was associated with an exacerbation of their primary condition. Although patients completing the questionnaire may have had long-term use of drugs that affect the immune system, most respondents did not report having SARS-CoV-2 infection. Moreover, the course of COVID-19, in the opinion of patients with IBD, was assessed as mild or moderate, and in most cases, did not require hospitalization.
Figures
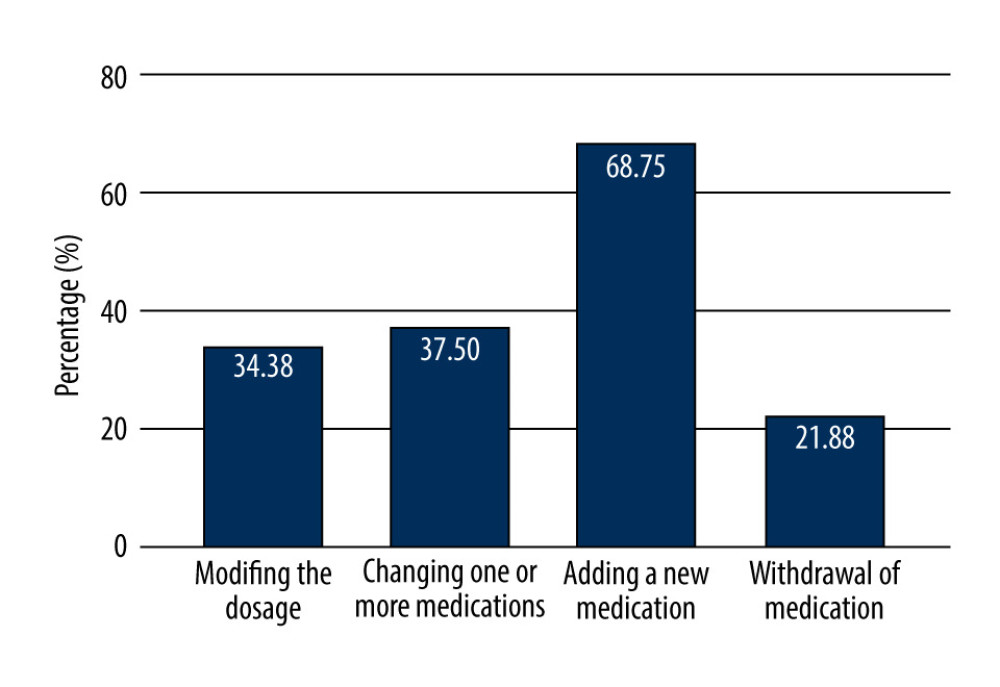 Figure 1. Changes in treatment in patients with inflammatory bowel diseases during the COVID-19 pandemic (Word 2021, Microsoft office).
Figure 1. Changes in treatment in patients with inflammatory bowel diseases during the COVID-19 pandemic (Word 2021, Microsoft office).  Figure 2. Difficulties reported by patients with inflammatory bowel diseases in obtaining consultation by a gastroenterologist during the COVID-19 pandemic. (Word 2021, Microsoft office).
Figure 2. Difficulties reported by patients with inflammatory bowel diseases in obtaining consultation by a gastroenterologist during the COVID-19 pandemic. (Word 2021, Microsoft office). 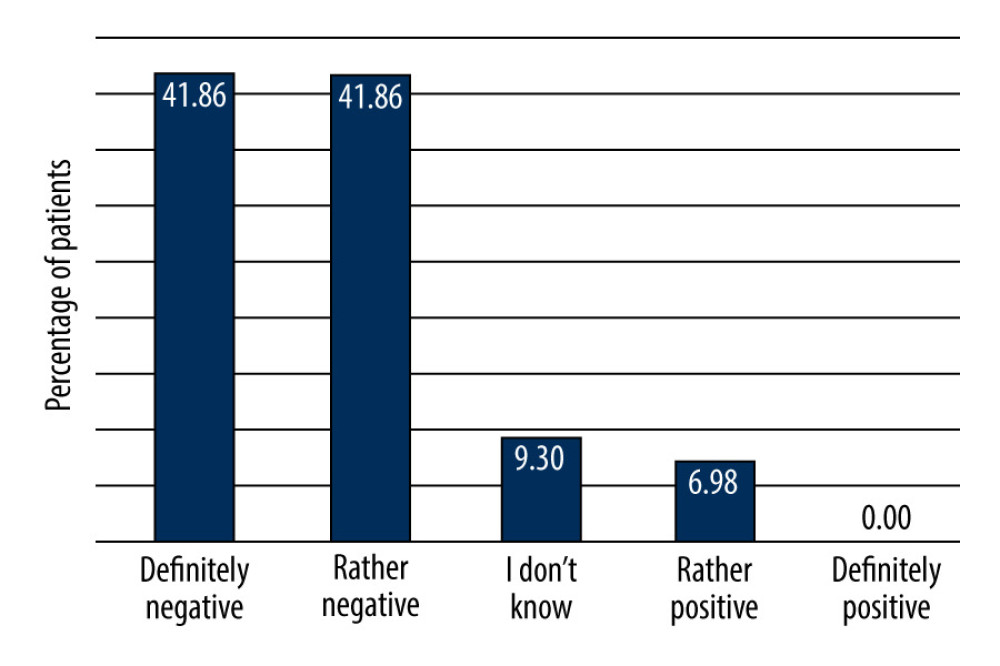 Figure 3. Questionnaire scoring of the mental state of patients with inflammatory bowel disease during the COVID-19 pandemic: 1, definitely negative impact of pandemic on the mental status; 2, rather negative impact of pandemic on the mental status; 3, difficult to assess impact of pandemic on the lowering of mental status; 4, rather positive impact of pandemic on the mental status; 5, definitely positive impact of pandemic on the mental status (Word 2021, Microsoft office).
Figure 3. Questionnaire scoring of the mental state of patients with inflammatory bowel disease during the COVID-19 pandemic: 1, definitely negative impact of pandemic on the mental status; 2, rather negative impact of pandemic on the mental status; 3, difficult to assess impact of pandemic on the lowering of mental status; 4, rather positive impact of pandemic on the mental status; 5, definitely positive impact of pandemic on the mental status (Word 2021, Microsoft office). References
1. Zhou P, Yang XL, Wang XG, A pneumonia outbreak associated with a new coronavirus of probable bat origin: Nature, 2020; 579; 270-73
2. Coronaviridae Study Group of the International Committee on Taxonomy of Viruses, The species Severe acute respiratory syndrome-related coronavirus: Classifying 2019-nCoV and naming it SARS-CoV-2: Nat Microbiol, 2020; 5(4); 536-44
3. Sharma A, Ahmad Farouk I, Lal SK, COVID-19: A review on the novel coronavirus disease evolution, transmission, detection, control and prevention: Viruses, 2021; 13(2); 202
4. Ochani R, Asad A, Yasmin F, COVID-19 pandemic: from origins to outcomes. A comprehensive review of viral pathogenesis, clinical manifestations, diagnostic evaluation, and management: Infez Med, 2021; 29(1); 20-36
5. World Health Organization: Poland: WHO Coronavirus Disease (COVID-19) Dashboard With Vaccination Data Available from: https://covid19.who.int/region/euro/country/pl
6. Nabi G, Resurgence of COVID-19 pandemic: Challenging situation of economics vs. healthcare: Scott Med J, 2021; 66(1); 1-2
7. Alyammahi SK, Abdin SM, Alhamad DW, The dynamic association between COVID-19 and chronic disorders: An updated insight into prevalence, mechanisms and therapeutic modalities: Infect Genet Evol, 2021; 87; 104647
8. Holko P, Kawalec P, Stawowczyk E, Prevalence and drug treatment practices of inflammatory bowel diseases in Poland in the years 2012–2014: An analysis of nationwide databases: Eur J Gastroenterol Hepatol, 2018; 30(4); 456-64
9. Pithadia AB, Jain S, Treatment of inflammatory bowel disease (IBD): Pharmacol Rep, 2011; 63(3); 629-42
10. Abreu MT, Peyrin-Biroulet L, Providing guidance during a global viral pandemic for the care of patients with inflammatory bowel disease: J Crohns Colitis, 2020; 14(14 Suppl 3); S767-68
11. Neumann H, Emura F, Bokemeyer B, Practical advice for management of inflammatory bowel diseases patients during the COVID-19 pandemic: World Endoscopy Organization Statement: Dig Endosc, 2020; 32(5); 658-62
12. Kumric M, Ticinovic Kurir T, Martinovic D, Impact of the COVID-19 pandemic on inflammatory bowel disease patients: A review of the current evidence: World J Gastroenterol, 2021; 27(25); 3748-61
13. Tripathi K, Godoy Brewer G, Thu Nguyen M, COVID-19 and outcomes in patients with inflammatory bowel disease: Systematic review and meta-analysis: Inflamm Bowel Dis, 2022; 28(8); 1265-79
14. Maaser C, Sturm A, Vavricka SREuropean Crohn’s and Colitis Organisation [ECCO] and the European Society of Gastrointestinal and Abdominal Radiology [ESGAR], ECCO-ESGAR Guideline for Diagnostic Assessment in IBD Part 1: Initial diagnosis, monitoring of known IBD, detection of complications: J Crohns Colitis, 2019; 13(2); 144-64
15. Ellen Kuenzig M, Windsor JW, Barrett L, Crohn’s and Colitis Canada’s 2021 impact of COVID-19 and inflammatory bowel disease in Canada: Executive summary: J Can Assoc Gastroenterol, 2021; 4(Suppl 2); S1-S9
16. Scaldaferri F, Papa A, Napolitano D, Changes in admissions, and hospitalization outcomes of IBD patients in an Italian tertiary referral center over a 13-year period: Eur Rev Med Pharmacol Sci, 2021; 25(18); 5826-35
17. Scaldaferri F, Pugliese D, Privitera G, Impact of COVID-19 pandemic on the daily management of biotechnological therapy in inflammatory bowel disease patients: Reorganisational response in a high-volume Italian inflammatory bowel disease centre: United European Gastroenterol J, 2020; 8(7); 775-81
18. Zhang YF, Qiu Y, He JS, Impact of COVID-19 outbreak on the care of patients with inflammatory bowel disease: A comparison before and after the outbreak in South China: J Gastroenterol Hepatol, 2021; 36(3); 700-9
19. Mikocka-Walus A, Skvarc D, van Tilburg MAL, COVID-19-related personal product shortages are associated with psychological distress in people living with gastrointestinal disorders: A cross-sectional survey: Neurogastroenterol Motil, 2022; 34(3); e14198
20. Kirchgesner J, Lemaitre M, Carrat F, Risk of serious and opportunistic infections associated with treatment of inflammatory bowel diseases: Gastroenterology, 2018; 155(2); 337-46e10
21. Tursi A, Angarano G, Monno L, COVID-19 infection in Crohn’s disease under treatment with adalimumab: Gut, 2020; 69(7); 1364-65
22. de León-Rendón JL, Hurtado-Salazar C, Yamamoto-Furusho JK, Aspects of inflammatory bowel disease during the COVID-19 pandemic and general considerations: Rev Gastroenterol Mex (Engl Ed), 2020; 85(3); 295-302
23. Sultan K, Mone A, Durbin L, Review of inflammatory bowel disease and COVID-19: World J Gastroenterol, 2020; 26(37); 5534-42
24. Magro F, Rahier JF, Abreu C, Inflammatory bowel disease management during the COVID-19 outbreak: The ten do’s and don’ts from the ECCO-COVID Taskforce: J Crohns Colitis, 2020; 14(14 Suppl 3); S798-806
25. Brenner EJ, Ungaro RC, Gearry RB, Corticosteroids, but not TNF antagonists, are associated with adverse COVID-19 outcomes in patients with inflammatory bowel diseases: results from an international registry: Gastroenterology, 2020; 159(2); 481-91e3
26. Wetwittayakhlang P, Albader F, Golovics PA, Clinical outcomes of COVID-19 and impact on disease course in patients with inflammatory bowel disease: Can J Gastroenterol Hepatol, 2021; 2021; 7591141
27. Baryah ANS, Midha V, Mahajan R, Sood A, Impact of Corona Virus Disease-19 (COVID-19) pandemic on gastrointestinal disorders: Indian J Gastroenterol, 2020; 39(3); 214-19
28. Anikhindi SA, Kumar A, Arora A, COVID-19 in patients with inflammatory bowel disease: Expert Rev Gastroenterol Hepatol, 2020; 14(12); 1187-93
29. Monteleone G, Ardizzone S, Are Patients with inflammatory bowel disease at increased risk for COVID-19 infection?: J Crohns Colitis, 2020; 14(9); 1334-36
30. Colbert GB, Venegas-Vera AV, Lerma EV, Utility of telemedicine in the COVID-19 era: Rev Cardiovasc Med, 2020; 21(4); 583-87
31. Costantino A, Bortoluzzi F, Giuffrè M, Correct use of telemedicine in gastroenterology, hepatology, and endoscopy during and after the COVID-19 pandemic: Recommendations from the Italian association of hospital gastroenterologists and endoscopists (AIGO): Dig Liver Dis, 2021; 53(10); 1221-27
32. Perisetti A, Goyal H, Successful distancing: Telemedicine in gastroenterology and hepatology during the COVID-19 pandemic: Dig Dis Sci, 2021; 66(4); 945-53
33. Reed ME, Huang J, Graetz I, Patient characteristics associated with choosing a telemedicine visit vs office visit with the same primary care clinicians: JAMA Netw Open, 2020; 3(6); e205873
34. Lahat A, Shatz Z, Telemedicine in clinical gastroenterology practice: What do patients prefer?: Therap Adv Gastroenterol, 2021; 14; 1756284821989178
35. Avčin T, Avguštin Avčin B, Addressing mental health issues in immunocompromised adolescents with chronic diseases during the COVID-19 pandemic: J Pediatr (Rio J), 2022; 98(4); 323-25
36. Sayeed A, Kundu S, Al Banna MH, Mental health outcomes of adults with comorbidity and chronic diseases during the COVID-19 pandemic: A matched case-control study: Psychiatr Danub, 2020; 32(3–4); 491-98
37. Melaku T, Assefa D, Bayisa B, Legese N, Research and intervention priorities for mental health of people living with chronic disease(s) in the midst of the COVID-19 pandemic in low resource settings: A commentary: Ann Med Surg (Lond), 2020; 57; 268-69
38. Chen PJ, Pusica Y, Sohaei D, An overview of mental health during the COVID-19 pandemic: Diagnosis (Berl), 2021; 8(4); 403-12
39. Chew NWS, Lee GKH, Tan BYQ, A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak: Brain Behav Immun, 2020; 88; 559-65
40. Hossain MM, Tasnim S, Sultana A, Epidemiology of mental health problems in COVID-19: A review: F1000Res, 2020; 9; 636
41. Gloster AT, Lamnisos D, Lubenko J, Impact of COVID-19 pandemic on mental health: An international study: PLoS One, 2020; 15(12); e0244809
42. Huang Y, Zhao N, Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey [published correction appears in Psychiatry Res. 2021;299:113803]: Psychiatry Res, 2020; 288; 112954
Figures
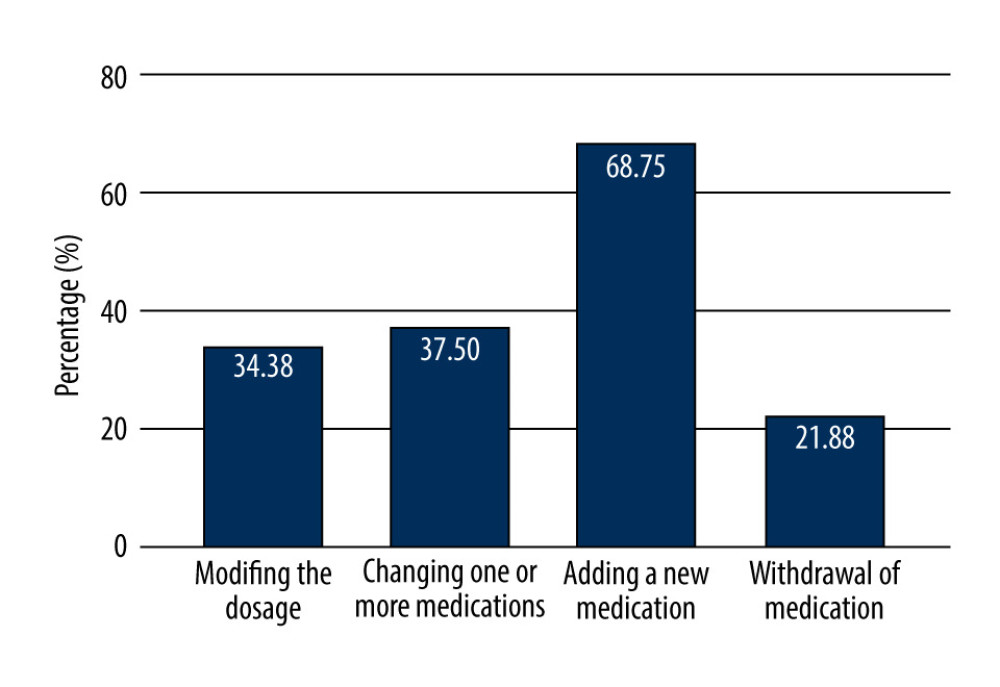 Figure 1. Changes in treatment in patients with inflammatory bowel diseases during the COVID-19 pandemic (Word 2021, Microsoft office).
Figure 1. Changes in treatment in patients with inflammatory bowel diseases during the COVID-19 pandemic (Word 2021, Microsoft office).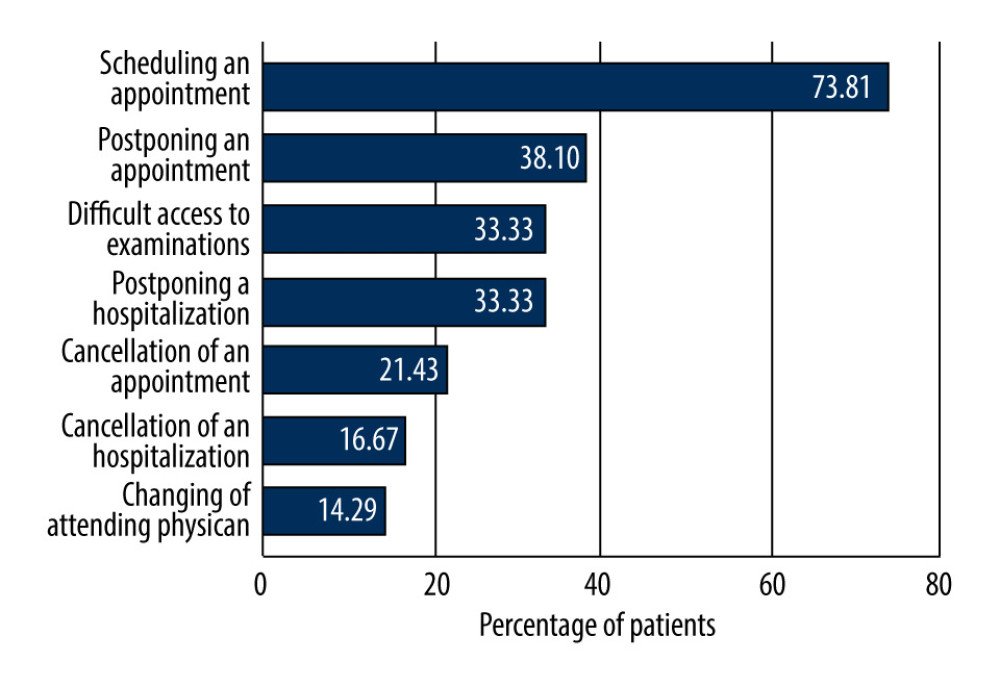 Figure 2. Difficulties reported by patients with inflammatory bowel diseases in obtaining consultation by a gastroenterologist during the COVID-19 pandemic. (Word 2021, Microsoft office).
Figure 2. Difficulties reported by patients with inflammatory bowel diseases in obtaining consultation by a gastroenterologist during the COVID-19 pandemic. (Word 2021, Microsoft office).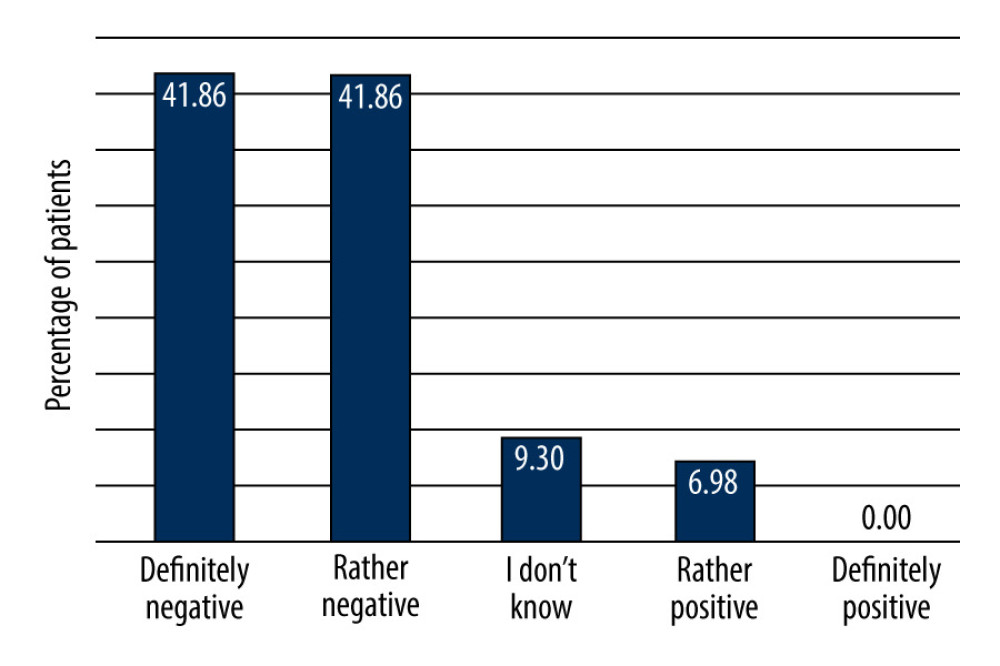 Figure 3. Questionnaire scoring of the mental state of patients with inflammatory bowel disease during the COVID-19 pandemic: 1, definitely negative impact of pandemic on the mental status; 2, rather negative impact of pandemic on the mental status; 3, difficult to assess impact of pandemic on the lowering of mental status; 4, rather positive impact of pandemic on the mental status; 5, definitely positive impact of pandemic on the mental status (Word 2021, Microsoft office).
Figure 3. Questionnaire scoring of the mental state of patients with inflammatory bowel disease during the COVID-19 pandemic: 1, definitely negative impact of pandemic on the mental status; 2, rather negative impact of pandemic on the mental status; 3, difficult to assess impact of pandemic on the lowering of mental status; 4, rather positive impact of pandemic on the mental status; 5, definitely positive impact of pandemic on the mental status (Word 2021, Microsoft office). In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952