24 May 2023: Database Analysis
Relationship Between Physical Activity and Adult Asthma Control Using NHANES 2011–2020 Data
Wei Ye1ABDF*, Xingxing Li2BCFG, Yuenuo Huang3ABFDOI: 10.12659/MSM.939350
Med Sci Monit 2023; 29:e939350
Abstract
BACKGROUND: The purpose of this study was to determine whether PA is associated with asthma control using data from the National Health and Nutrition Examination Survey (NHANES) for 2011-2020. We did not find a relationship between physical activity (PA) and asthma control.
MATERIAL AND METHODS: In this study, we measured asthma control by counting asthma attacks and emergency room visits for asthma in the past year. Physical activity was divided into recreational physical activity and work physical activity. A total of 3158 patients (≥20 years old) were included in the study, of which 2375 were in the asthma attack group and 2844 were in the emergency care group, with indicators of asthma control and physical activity as dichotomous variables. Multiple sets of covariates were selected, such as age, gender, and race. Multiple logistic regression analysis and subgroup analysis were used to analyze the data.
RESULTS: Active workload was significantly correlated with acute asthma attacks, but the relationship with emergency care was not statistically significant. We found that the relationship between physical activity and emergency care was influenced by race, education, and economic level.
CONCLUSIONS: The amount of work activity was correlated with acute asthma attacks, and the relationship between physical activity and emergency case was influenced by race, education, and economic level.
Keywords: Asthma, Sedentary Behavior, Humans, Adult, young adult, Nutrition Surveys, Exercise, Educational Status, Emergency Medical Services
Background
Asthma is a common disease in children and adults, characterized by airway inflammation and obstruction due to increased mucus production, and is associated with a serious global health burden [1]. According to GINA 2020, asthma affects approximately 300 million people worldwide, which is responsible for a global disease burden of 11 million years of life lost (YLLs) and 25 million disability-adjusted life years (DALYs) per year [2,3]. Asthma is a public health problem that imposes significant administrative costs on health systems worldwide. In 2010, approximately 8.2% of U.S. adults had asthma, and of those, 49.1% had an asthma attack in the past year [4]. This highlights the importance of symptom management and disease control [4]. Asthma seriously affects people’s physical and mental health, resulting in reduced learning efficiency, limited physical activity, and reduced quality of life [5]. Therefore, to improve the awareness of the risk of asthma, how to effectively treat asthma has become an important goal of asthma prevention and treatment in recent years. Multiple factors contribute to the development of asthma, such as unhealthy lifestyle factors, including lack of physical activity/exercise, increased sedentary time, and poor nutrition, and obesity may play a role [6]. The difference between physical exercise and physical activity should be pointed out. According to the World Health Organization definition: Physical activity is any bodily movement that results from the expenditure of energy by the skeletal muscular system. Exercise is a planned, structured, repetitive and purposeful physical activity that seeks to improve or maintain one or even several elements of physical fitness. For asthma patients, physical training is a widely accepted adjunct to both pharmacologic and non-pharmacologic therapy [7]. However, the effect of physical activity on asthma is controversial. Many previous studies have shown that exercise is a trigger for asthma and reducing exercise is an effective means of controlling asthma symptoms [8]. However, recent studies have demonstrated that daily exercise can help improve asthma symptoms [9]. Combined exercise training (resistance and aerobic exercise) was found to improve cardiopulmonary function and muscle strength in children and adolescents with asthma in a 12-week randomized trial [10]. Aerobic exercise training was found to potentially improve asthma control and lung function, but not airway inflammation, in a meta-study [11].
The National Health and Nutrition Examination Survey (NHANES) is a population-based cross-sectional survey designed to collect information on the health and nutrition status of adults and children in the United States. The unique feature of this survey is that it combines interviews and physical examinations. To determine the causality of physical activity in the development of asthma, we used NHANES data from 2011 to 2020 to examine the relationship between exercise intensity and acute asthma attacks/emergency room admission in adults with asthma, and to assess whether this relationship was influenced by potential confounding factors.
Material and Methods
DATA SOURCES:
In this study, we used the cross-sectional survey of NHANES in 5 cycles(2011–2012, 2013–2014, 2015–2016, 2017–2018, and 2019–2020). The data we used was obtained from publicly available databases. The inclusion criteria were as follows: 1) NHANES participants were 20 years old and above; 2) NHANES participants diagnosed with asthma were identified. Exclusion criteria were as follows: 1) Acute attacks or incomplete visits to the emergency department for asthma in the past year; 2) Participants with incomplete indicators of work activity or recreational activity; 3) A very small number of participants lacked covariates, such as gender, education, marriage, and hypertension. The study design and inclusion and exclusion criteria are shown in Figure 1. Only public datasets were used in this study, and ethics approval was not required. The NHANES protocols were approved by the NCHS Research Ethics Review Board, and written informed consent forms were provided by all participants. More information is available at http://www.cdc.gov/nchs/nhanes.htm.
PHYSICAL ACTIVITY ASSESSMENT:
The World Health Organization (WHO) defines physical activity as the production of physical activity by any skeletal muscle that requires the expenditure of energy. In this study, we included work activities and recreational activities.
Work activity: Work activity was measured in the “Physical Activity” questionnaire. In the “Physical Activity” questionnaire, each participant was asked about vigorous work activity, number of days vigorous work/number of days moderate work, and minutes of vigorous-intensity work/minutes moderate-intensity work. Physical Activity Guidelines recommended at least 75 minutes of high-intensity exercise per week or 150 minutes of appropriate exercise per week. The weekly amount of exercise was calculated through the questions, which was then divided into active (≥ recommended amount of activity), less active (< recommended amount of activity), and inactive according to the above suggestions.
Recreational activity: Work activity was measured in the “Physical Activity” questionnaire. In the “Physical Activity” questionnaire, each participant was asked about vigorous work activity, number of days vigorous recreational activities/number of days moderate recreational activities, and minutes vigorous-intensity work/minutes moderate-intensity recreational activities. Physical Activity Guidelines recommended at least 75 minutes of vigorous exercise per week or 150 minutes of appropriate exercise per week. The weekly amount of exercise was calculated through the questions, which was then divided into active (≥ recommended amount of activity), less active (< recommended amount of activity), and inactive according to the above suggestions.
EVALUATION OF COVARIATES:
We comprehensively screened for 12 confounding factors that might be associated with physical activity and asthma control, including age, race, gender, history of alcohol use, marital history, educational history, smoking history, hypertension, history of high cholesterol, diabetes, and BMI. We divided each covariate into a reference group and other groups for easy contrast analysis. In addition, we set Don’t Know/Refused/Undetectable to Unknow group and removed invalid values. The following data processing was performed:
Gender: Male and female.
Age: It was a continuous variable and was not grouped.
Ethnicity/race: Race was divided into non-Hispanic white (reference group), non-Hispanic black, Mexican-American, and other Hispanic.
Marital history: Married, cohabiting with partner, widowed, divorced, separated, never married.
Drinking Behavior: Drinking behavior was measured on the “Alcohol Use” questionnaire, in which each respondent was asked how many times they had consumed alcoholic beverages in the past 12 months, and was asked about the average amount of water consumed on those days when they consumed alcoholic beverages. Based on these questions, the average number of alcoholic beverages consumed per week during the past 12 months could be calculated. According to the National Institute on Alcohol Abuse and Alcoholism (NIAAA), the average number of alcoholic beverages consumed per week was classified as moderate (1 drink for women or 1–2 drinks for men), heavy (2–3 drinks for women or 3–4 drinks for men), and binge (≥4 drinks for women or ≥5 drinks for men).
Smoking history: Smoking behavior was measured in the “Smoking: Cigarette Use” questionnaire, in which participants were asked whether they had smoked at least 100 cigarettes in their life, and whether they had smoked cigarettes when asked. Based on answers to these questions, smoking history was categorized as non-smoker, former smoker, and current smoker.
BMI status: Body mass index was calculated as weight/height2 based on measured height and weight, and then classified as not overweight (<25), overweight (25–30), and obese (≥30).
Diabetes: History of diabetes was measured in the “Diabetes” questionnaire, which asked “Has a doctor told you that you have diabetes?” Depending on the answer, diabetes was classified as yes or no.
History of hypertension: History of hypertension was measured in the “hypertension & hyperlipidemia” questionnaire, in which participants were asked “Have you ever been told you have high blood pressure?” According to the answer, history of hypertension was categorized as yes or no.
History of hyperlipidemia: History of hyperlipidemia was measured in the “hypertension & hyperlipidemia” questionnaire, in which participants were asked “Has a doctor ever told you that you have high cholesterol?” Depending on the answer, the history of hyperlipidemia was categorized as yes or no.
Household income-to-poverty ratio: An index defined as the ratio of household income to poverty. The ratio was categorized as 1–5 and ≥5.
ASTHMA CONTROL CONDITION:
We evaluated asthma control through 2 dimensions: 1) asthma attack within 1 year: Asthma attacks were measured in the “Medical Conditions” questionnaire, in which each respondent was asked “Have you ever been told you have asthma?” Based on answers to these questions, asthma attacks were divided into an asthma attack subgroup and a no asthma attack subgroup; 2) Emergency care visits for asthma in the past year: Asthma attacks were measured in the “Medical Conditions” questionnaire, in which each respondent was asked “During the past 12 months, did you visit an emergency room or urgent care center because of asthma?” According to responses to these questions, asthma attacks were divided into an emergency care subgroup and a no emergency care subgroup.
STATISTICAL ANALYSIS:
We used data from the NHANES (2011–2020) database. Continuous variables were expressed as mean±standard deviation, while categorical variables were expressed as percentage (95% CI). According to the categorization and distribution of the variables and data, the chi-square test or the
Results
CHARACTERISTICS OF PARTICIPANTS:
In this study, a total of 2375 cases were included in the asthma attack subgroup, and 2844 were included in the emergency care subgroup (Tables 1, 2). In the asthma attack subgroup, the mean age of the group was 44.665. There were differences in age, gender, race, marriage, hypertension, high cholesterol, and BMI between the 2 subgroups. The asthma attack subgroup tended to be more female, Other Hispanic White, Widowed, and more likely to be obese and have high cholesterol. In the emergency care group, the mean age within the group was 47.360 years. There were differences in age, sex, race, education, household income-to-poverty ratio, and BMI between the 2 subgroups. The patients in the emergency care subgroup were predominately female, with some college or AA degree, household income-to-poverty ratio of 1 to 5, and were more likely to be obese.
RELATIONSHIP BETWEEN PHYSICAL ACTIVITY AND ASTHMA CONTROL:
This study analyzed the relationship between work activities and recreational activities and asthma attacks and emergency room admission due to asthma. For analysis, we divided the level of physical activity into 3 categories: active, less active, and not active. The correlation between physical activity and asthma control is shown in Table 3. In the asthma attack work activities group, we found that within the unadjusted group, the active work activities subgroup was more likely to have an asthma attack within 1 year compared to the no active work activities subgroup. In model 2, age, gender, and race were slightly adjusted. In model 3, age, race, gender, alcohol consumption history, marital history, education history, smoking history, hypertension, high cholesterol history, and diabetes were slightly adjusted. The results of OR values in both models were consistent with the trend of OR values in the unadjusted model group, indicating that active workload was more likely to cause acute asthma attacks. In the emergency care group, the 3 models showed the same results: recreational work was not significantly associated with acute asthma attacks within 1 year. We used the same method to construct 3 models (Model 1, Model 2, Model 3) to assess the relationship between physical activity and emergency room visits due to asthma attacks, and the results showed that there was no significant association between physical activity and emergency care.
SUBGROUP ANALYSIS:
We found no significant correlation between physical activity and emergency room admissions for asthma. Therefore, we further analyzed the factors affecting the correlation between the 2 groups. The subgroup analysis of work activities revealed that the correlation between the 2 was affected by gender, race, education, economic level, and smoking history, as shown in Table 4. Female, current smoker, high school graduate/GED or equivalent, active work activities with asthma were more likely to be seen in the emergency room with an acute episode of the disease, while asthma patients with high cholestasis, a household income to poverty ratio of 5, and non-Hispanic Black asthma patients were be more likely to present to the emergency department for acute episodes of the disease. The correlation between the recreational activity and emergency admissions was influenced by gender, education, and marriage (Table 5). People who were female, college graduate or above, divorced, and had recreational and work activities with asthma were more likely to be seen in the emergency room for asthma.
Discussion
Asthma is a common, chronic, lower respiratory disease worldwide. For patients with asthma, physical training is widely accepted as an adjunct to pharmacological and non-pharmacological treatment. The effect of physical training on the symptoms of asthma patients is controversial. In this study, active work exercise induced acute asthma attacks, while recreational exercise was not significantly associated with acute asthma attacks. Further analysis suggested that the association between physical training and emergency room visits was influenced by gender, race, education, economic level, and smoking history.
Poorly controlled asthma is a common problem, often resulting in missed school, absenteeism, emergency room visits, and hospitalizations. In a population-based study, people with asthma performed less physical activity and were more likely to be sedentary on a daily basis compared to non-asthmatic populations [11]. During exercise, asthma symptoms are often worsened because of excessive physical activity and limited physical conditions. High-intensity workload can lead to acute asthma attacks, which fits with our study. Lifestyle changes, particularly reduced physical activity, are one of the reasons for the increased incidence and severity of asthma [6]. In a study of 201 adults with asthma, daily physical activity was associated with decreased lung function within 12 years of asthma diagnosis. Annual declines in FEV1 and FVC were slower in the high physical activity group than in the low physical activity group [12]. Russell et al found that lighter physical activity may have long-term benefits, while increased activity intensity did not significantly improve asthma [13]. Our study results do not suggest an appropriate workload for asthma symptom control. Most studies on physical training interventions for asthma patients have focused on various types of aerobic exercise, such as jogging, resistance exercise, and walking, and have been conducted in professional settings under the guidance of physical therapists, making it difficult to generalize to real-world situations. A limitation of our study is that it did not exclude participants with other systemic diseases, which may have biased the results.
Interestingly, in our study, low cholesterol was a risk factor for acute asthma attacks in the active exercise group. Vigorous physical activity had a causal effect on HDL, LDL, total cholesterol, and triglycerides. We can assume that the active exercise group is mostly dominated by people with low cholesterol. However, a Mendelian randomized analysis found no correlation between lifestyle factors and HDL, LDL, total cholesterol, and triglycerides [14]. However, there are some studies that seem to refute this conclusion. In a 130-year prospective cohort study of individuals from 17 high-income, middle-income, and low-income countries, higher recreational and non-recreational physical activity was associated with a lower risk of mortality and cardiovascular disease events [15]. In a cohort study with 5-year follow-up, higher levels of recreational physical activity were strongly, hierarchically, and inversely associated with the risk of acute myocardial infarction [16].
In addition, there was no significant relationship between adult asthma emergency department visits and physical activity in this study. Several studies have confirmed racial and socioeconomic differences in emergency room visits among adult asthma participants [17]. We believe that adult emergency room visits for asthma are not determined by asthma symptom control, but by other factors such as race and economic level that play a dominant role. This agrees with our study. In a study analyzing data from the National Hospital Ambulatory Medical Care Survey (NHAMCS) between 2010 and 2015, asthma-related emergency room visits and post-emergency hospitalizations were more frequent in children, Blacks, and Hispanics [18]. Therefore, national governments should develop effective interventions to reduce ethnic or socioeconomic health disparities. Helen et al showed racial differences in childhood asthma. Racial disparities in childhood asthma were reduced after controlling for factors of physical hardship. In particular, poor housing quality was strongly associated with asthma prevalence. Policymakers may consider improving housing quality as a means of reducing asthma disparities[19].
This study has the following limitations. First, it was a cross-sectional study with some limitations. The results of this study only assessed the association between physical activity and asthma attacks/emergency admissions, and specific types of physical activity were not taken into account. Second, the NHANSE statistics from which the data were sourced are subject to geographical limitations. Third, there are some missing data in this study, which may have caused the results to be biased. Fourth, this was a cross-sectional study and has limitations in determining the causal relationship between asthma-related variables and adult asthma control. Finally, our study included only living asthma patients; patients who died due to acute asthma attack were not included in the survey, which may have created a self-selection bias.
Conclusions
The amount of work exercise is correlated with acute asthma attacks. Active workload can make asthma attacks more likely, while recreational activity is not correlated with acute asthma attacks. In contrast, gender, race, education, and economic level have a greater impact on emergency room visits for asthma. National governments should develop effective interventions to reduce other health disparities based on race or socioeconomic factors.
Figures
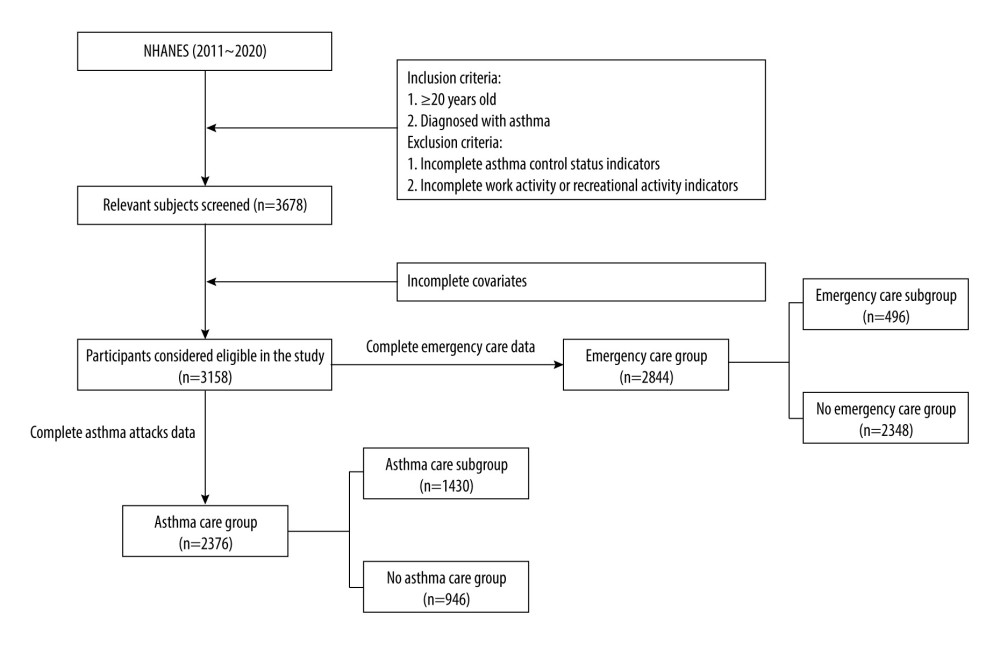 Figure 1. Flow chart.
Figure 1. Flow chart. Tables
Table 1. Baseline characteristics of asthma patients with different asthma attack subgroup.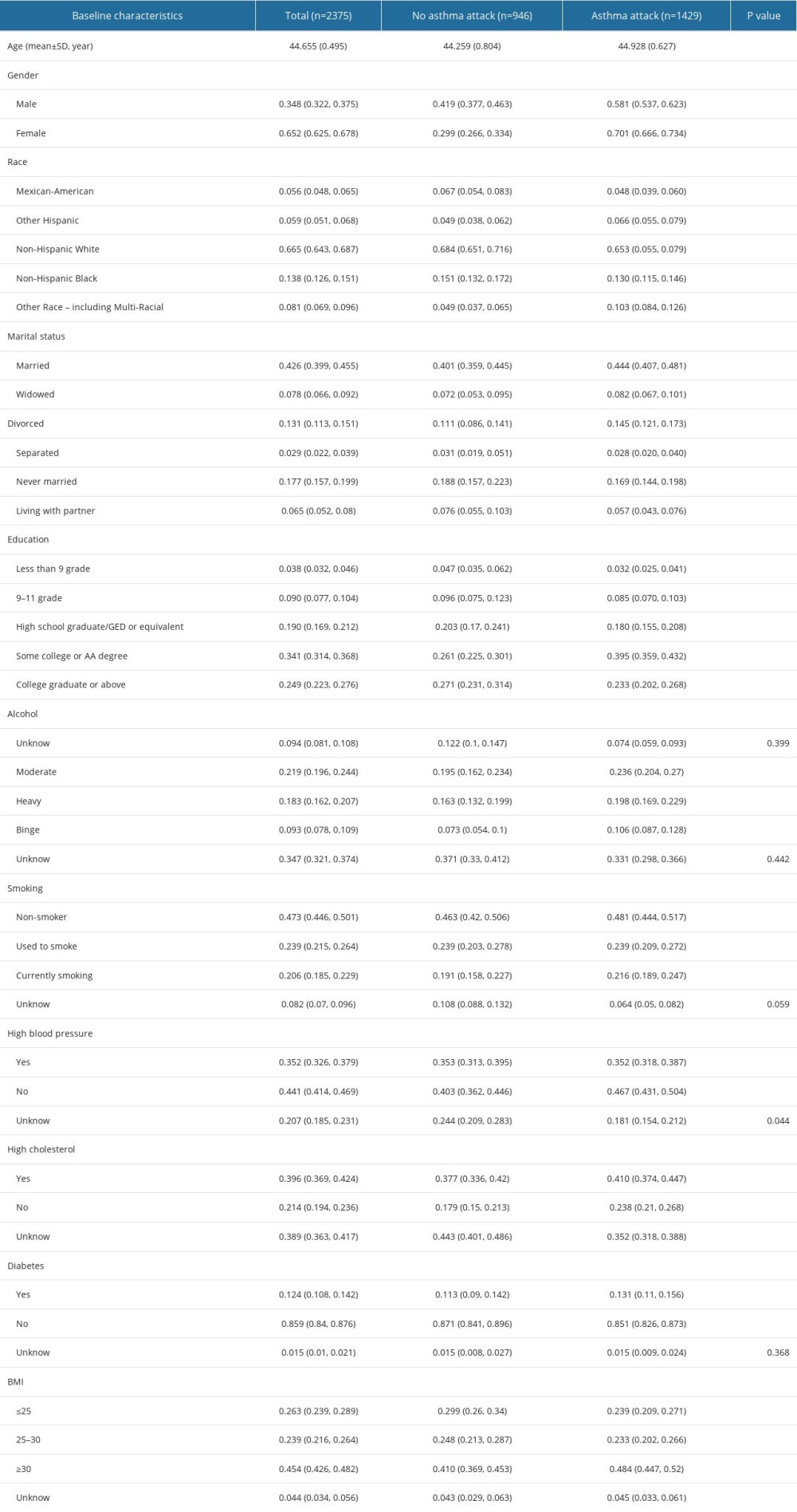 Table 2. Baseline characteristics of asthma patients with different Emergency cases subgroup.
Table 2. Baseline characteristics of asthma patients with different Emergency cases subgroup.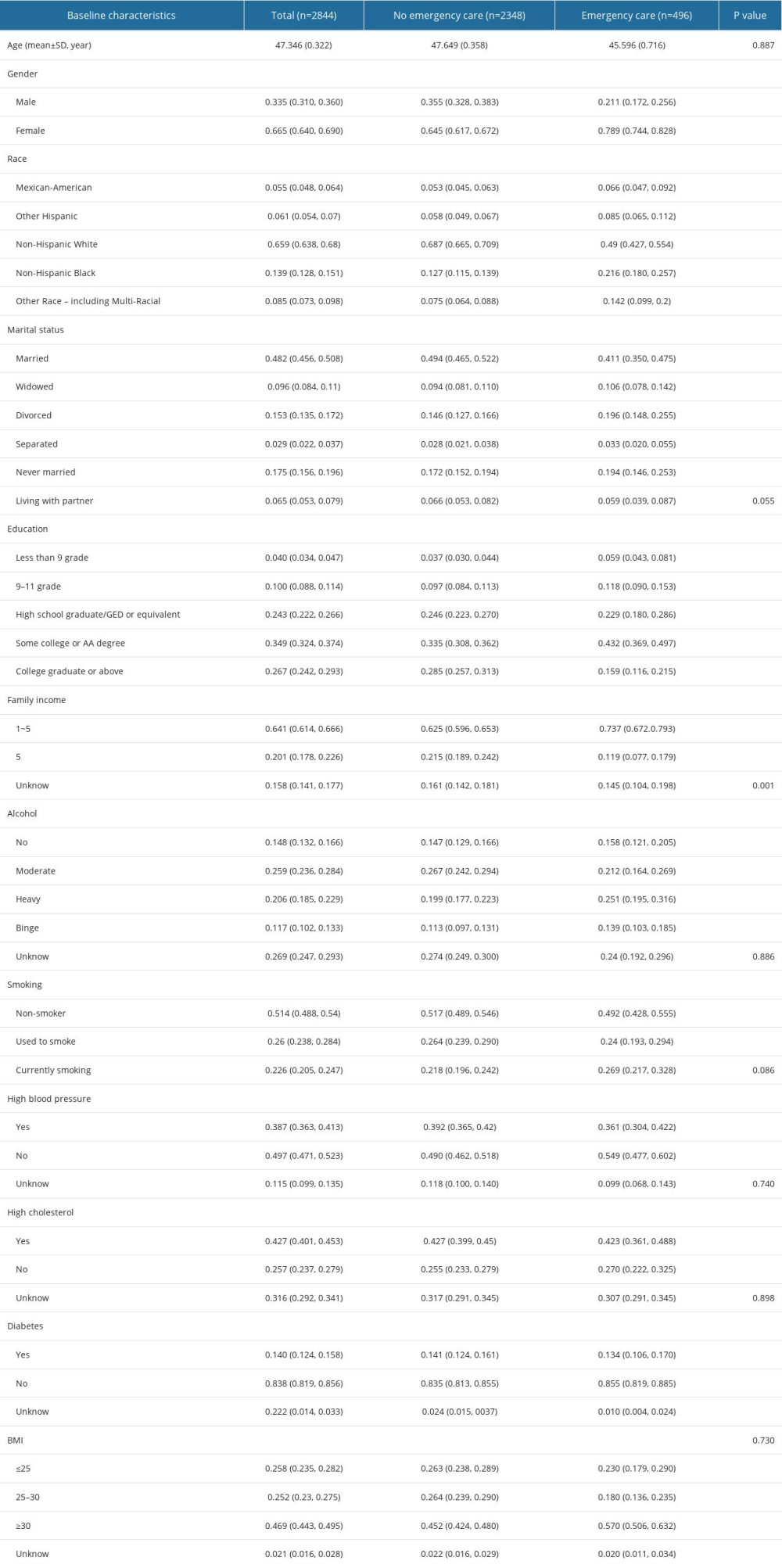 Table 3. The relationship between physical activity and asthma control und er different models.
Table 3. The relationship between physical activity and asthma control und er different models.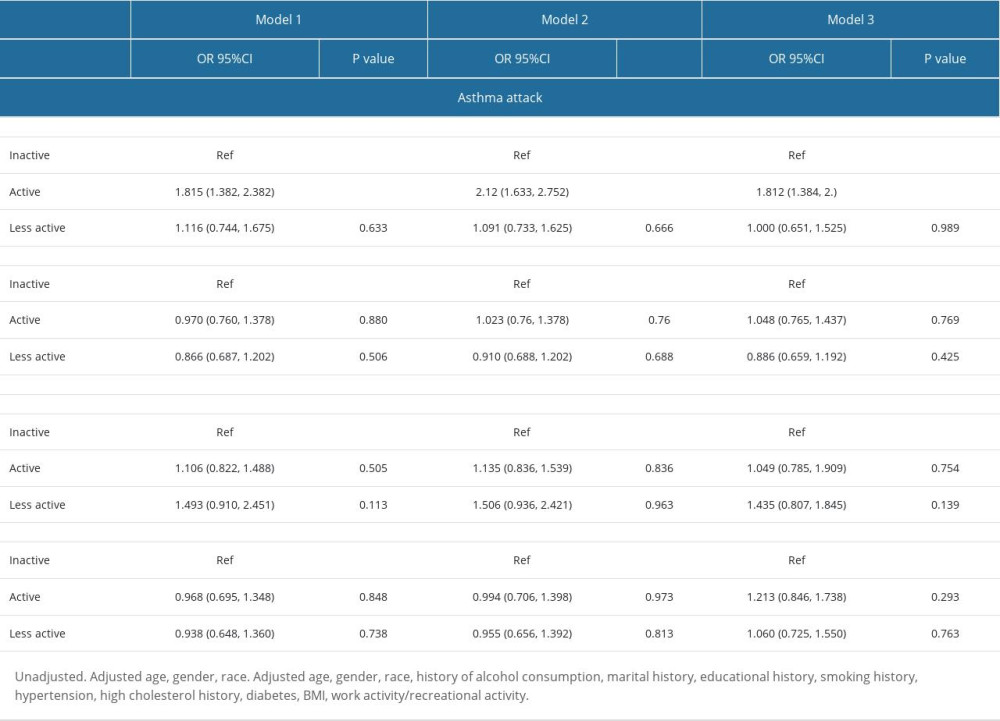 Table 4. Work activities-emergency care subgroup analysis.
Table 4. Work activities-emergency care subgroup analysis.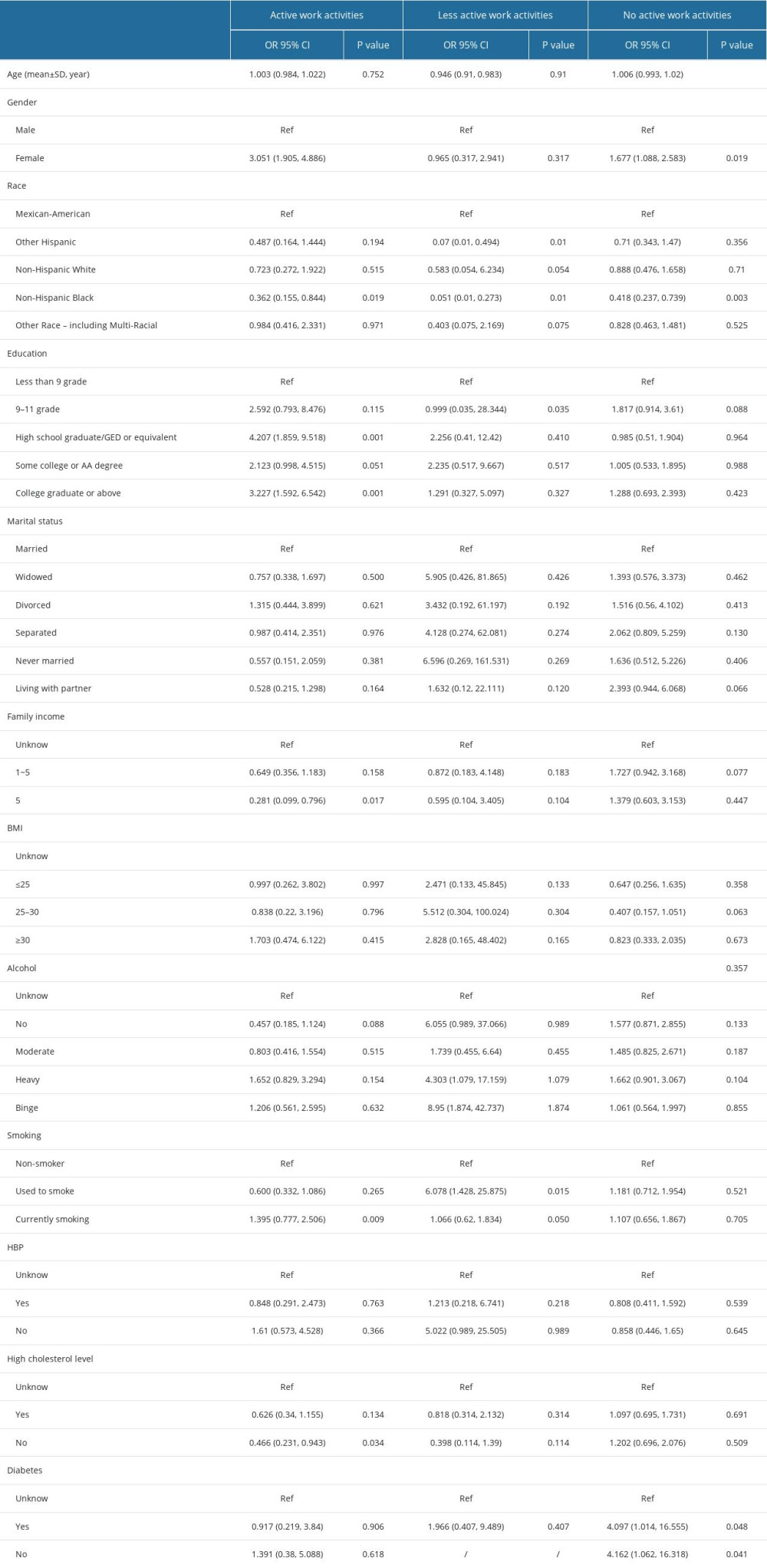 Table 5. Recreational activities – emergency care subgroup analysis.
Table 5. Recreational activities – emergency care subgroup analysis.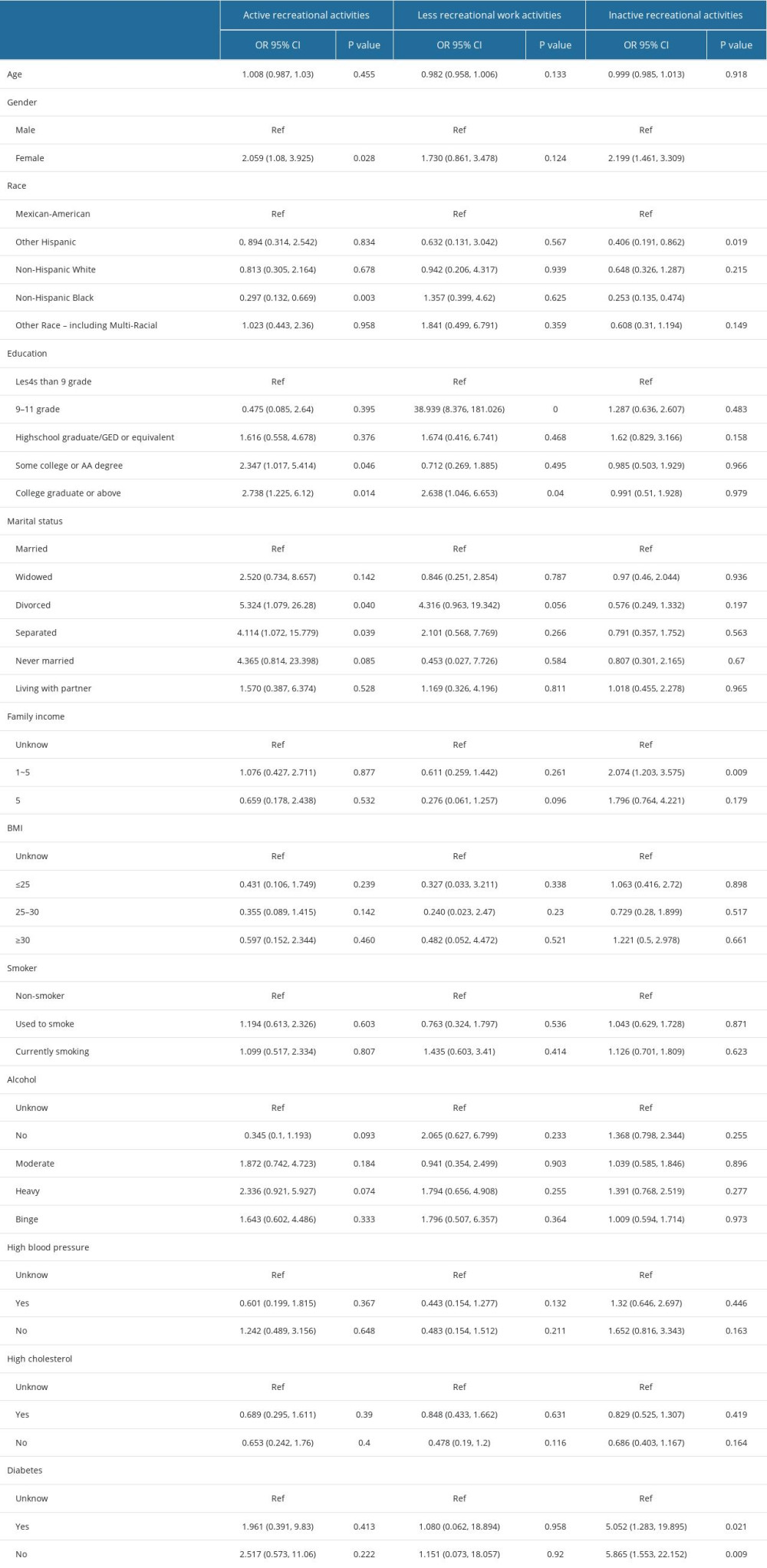
References
1. Agache I, Eguiluz-Gracia I, Cojanu C, Advances and highlights in asthma in 2021: Allergy, 2021; 76(11); 3390-407
2. Collaborators GBDCRD, Prevalence and attributable health burden of chronic respiratory diseases, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017: Lancet Respir Med, 2020; 8(6); 585-96
3. Ish P, Malhotra N, Gupta N, GINA 2020: What’s new and why?: J Asthma, 2021; 58(10); 1273-77
4. Mazurek JM, Syamlal G, Prevalence of asthma, asthma attacks, and Emergency Department visits for asthma among working adults – National Health Interview Survey, 2011–2016: Morb Mortal Wkly Rep, 2018; 67(13); 377-86
5. Patel SJ, Teach SJ, Asthma: Pediatr Rev, 2019; 40(11); 549-67
6. Nyenhuis SM, Dixon AE, Ma J, Impact of lifestyle interventions targeting healthy diet, physical activity, and weight loss on asthma in adults: What is the evidence?: J Allergy Clin Immunol Pract, 2018; 6(3); 751-63
7. Ding S, Zhong C, Exercise and asthma: Adv Exp Med Biol, 2020; 1228; 369-80
8. Hansen ESH, Pitzner-Fabricius A, Toennesen LL, Effect of aerobic exercise training on asthma in adults: A systematic review and meta-analysis: Eur Respir J, 2020; 56(1); 2000146
9. Lang JE, The impact of exercise on asthma: Curr Opin Allergy Clin Immunol, 2019; 19(2); 118-25
10. Sanz-Santiago V, Diez-Vega I, Santana-Sosa E, Effect of a combined exercise program on physical fitness, lung function, and quality of life in patients with controlled asthma and exercise symptoms: A randomized controlled trial: Pediatr Pulmonol, 2020; 55(7); 1608-16
11. Avallone KM, McLeish AC, Asthma and aerobic exercise: A review of the empirical literature: J Asthma, 2013; 50(2); 109-16
12. Loponen J, Ilmarinen P, Tuomisto LE, Daily physical activity and lung function decline in adult-onset asthma: A 12-year follow-up study: Eur Clin Respir J, 2018; 5(1); 1533753
13. Russell MA, Janson C, Real FG, Physical activity and asthma: A longitudinal and multi-country study: J Asthma, 2017; 54(9); 938-45
14. Zhuang Z, Gao M, Yang R, Association of physical activity, sedentary behaviours and sleep duration with cardiovascular diseases and lipid profiles: A Mendelian randomization analysis: Lipids Health Dis, 2020; 19(1); 86
15. Lear SA, Hu W, Rangarajan S, The effect of physical activity on mortality and cardiovascular disease in 130 000 people from 17 high-income, middle-income, and low-income countries: the PURE study: Lancet, 2017; 390(10113); 2643-54
16. Yu Q, Huang H, Zhang Z, The association between pelvic asymmetry and non-specific chronic low back pain as assessed by the global postural system: BMC Musculoskelet Disord, 2020; 21(1); 596
17. Boudreaux ED, Emond SD, Clark S, Camargo CA, Acute asthma among adults presenting to the emergency department: the role of race/ethnicity and socioeconomic status: Chest, 2003; 124(3); 803-12
18. Zook HG, Payne NR, Puumala SE, Racial/ethnic variation in Emergency Department care for children with asthma: Pediatr Emerg Care, 2019; 35(3); 209-15
19. Drewek R, Mirea L, Rao A, Asthma treatment and outcomes for children in the emergency department and hospital: J Asthma, 2018; 55(6); 603-8
Figures
Tables
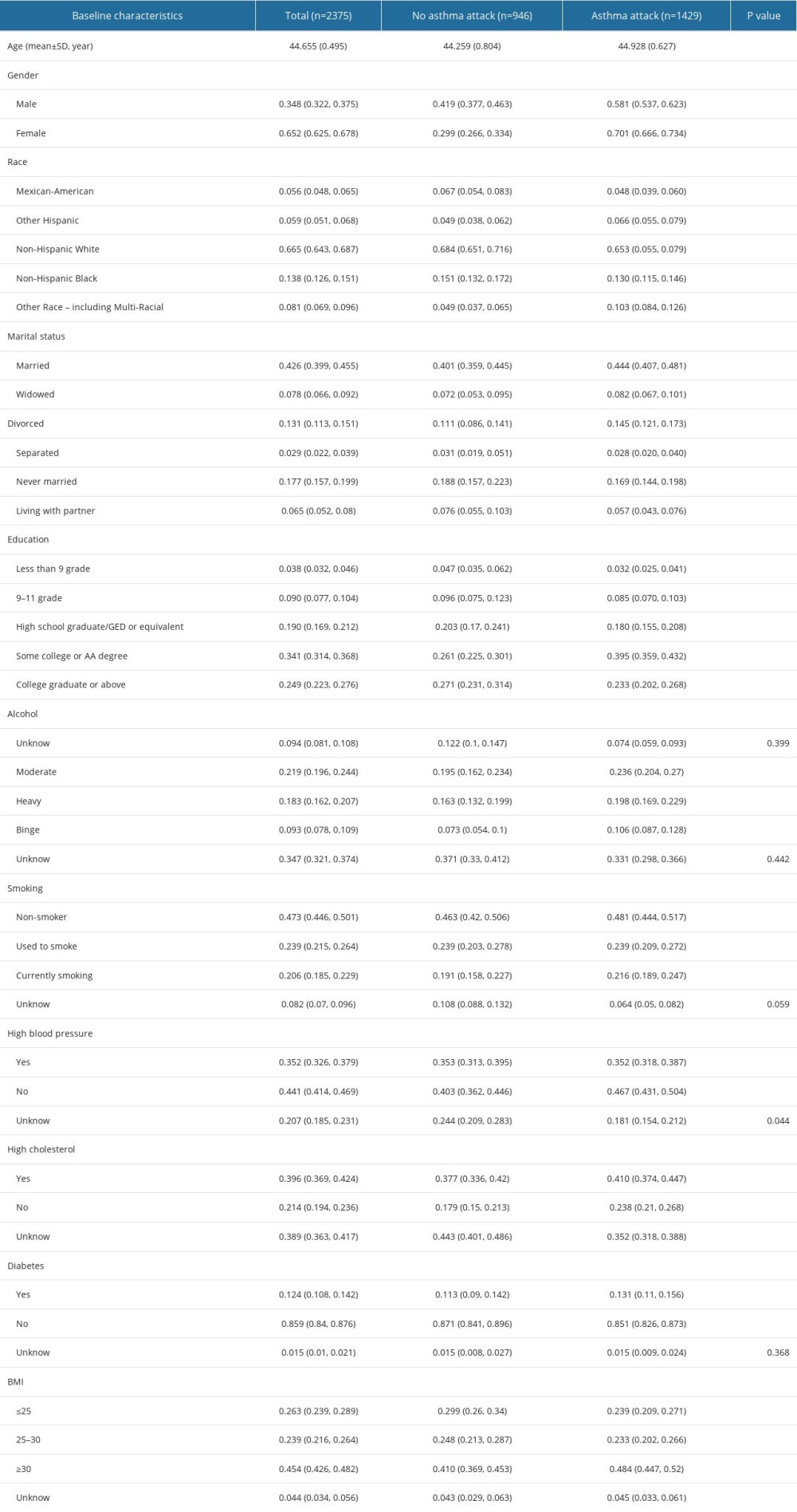 Table 1. Baseline characteristics of asthma patients with different asthma attack subgroup.
Table 1. Baseline characteristics of asthma patients with different asthma attack subgroup.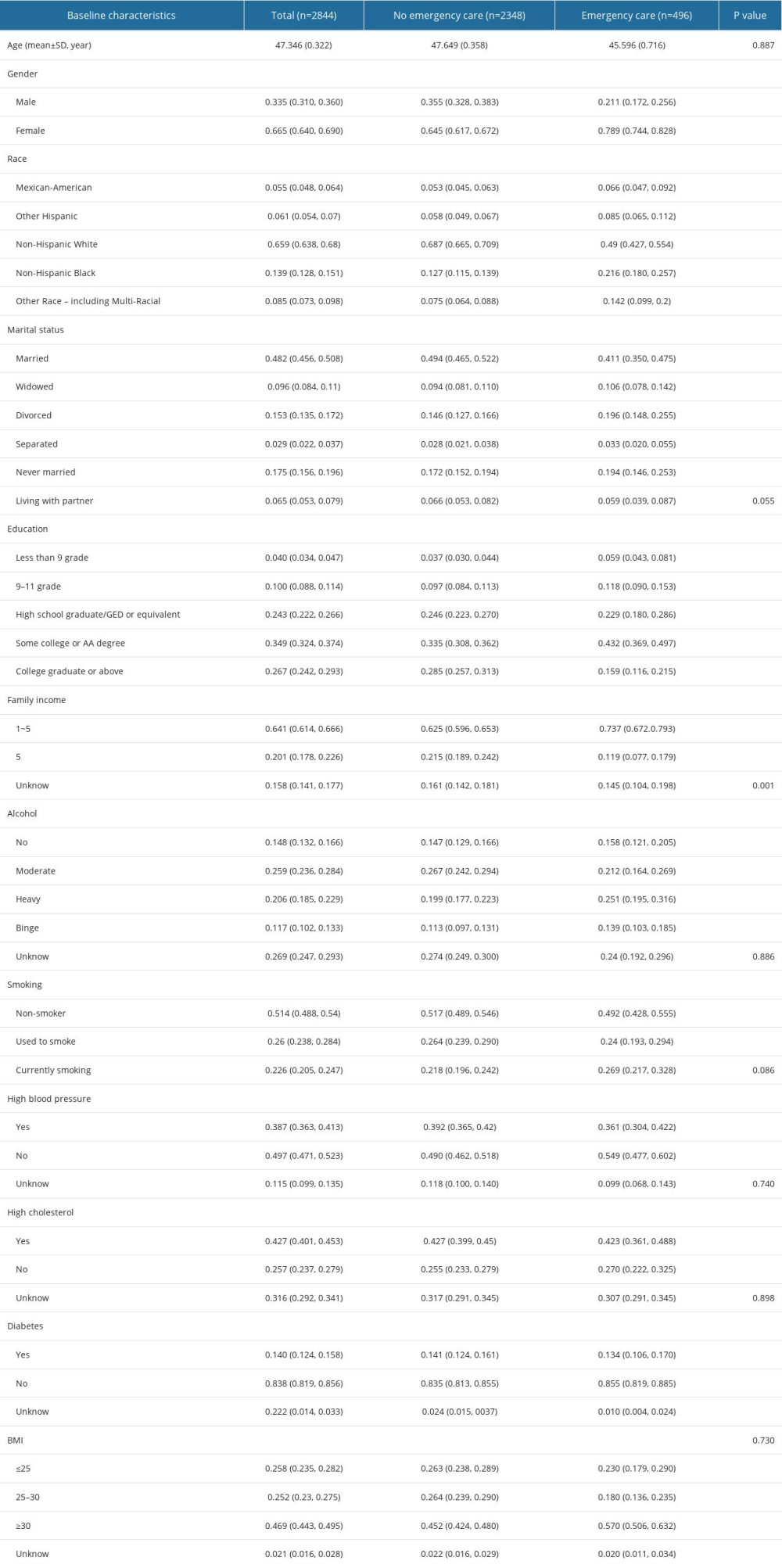 Table 2. Baseline characteristics of asthma patients with different Emergency cases subgroup.
Table 2. Baseline characteristics of asthma patients with different Emergency cases subgroup.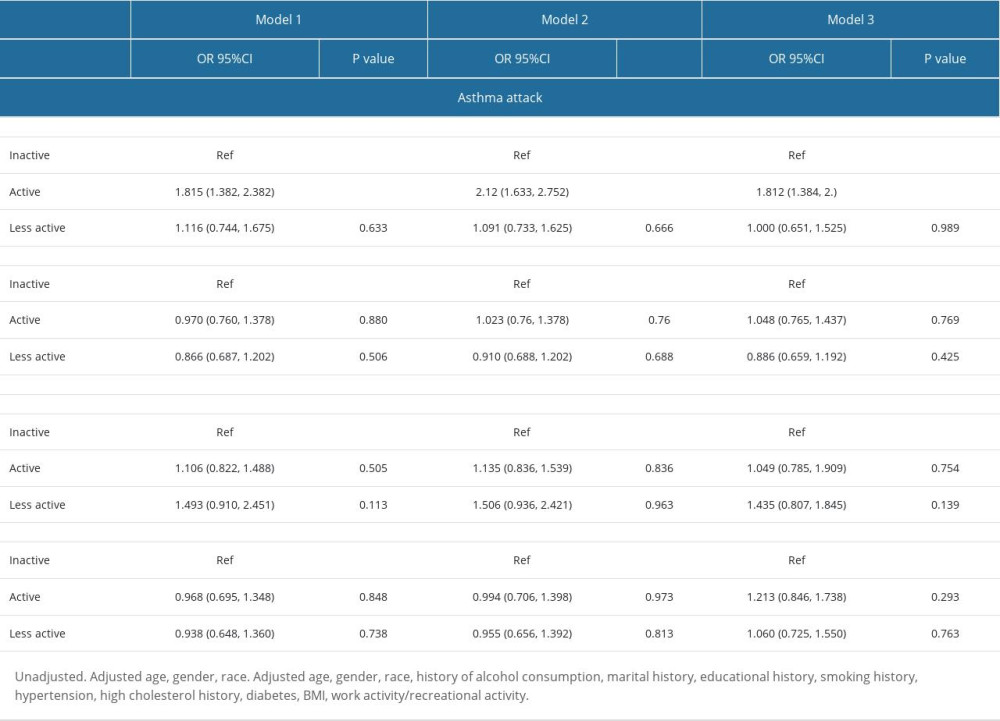 Table 3. The relationship between physical activity and asthma control und er different models.
Table 3. The relationship between physical activity and asthma control und er different models.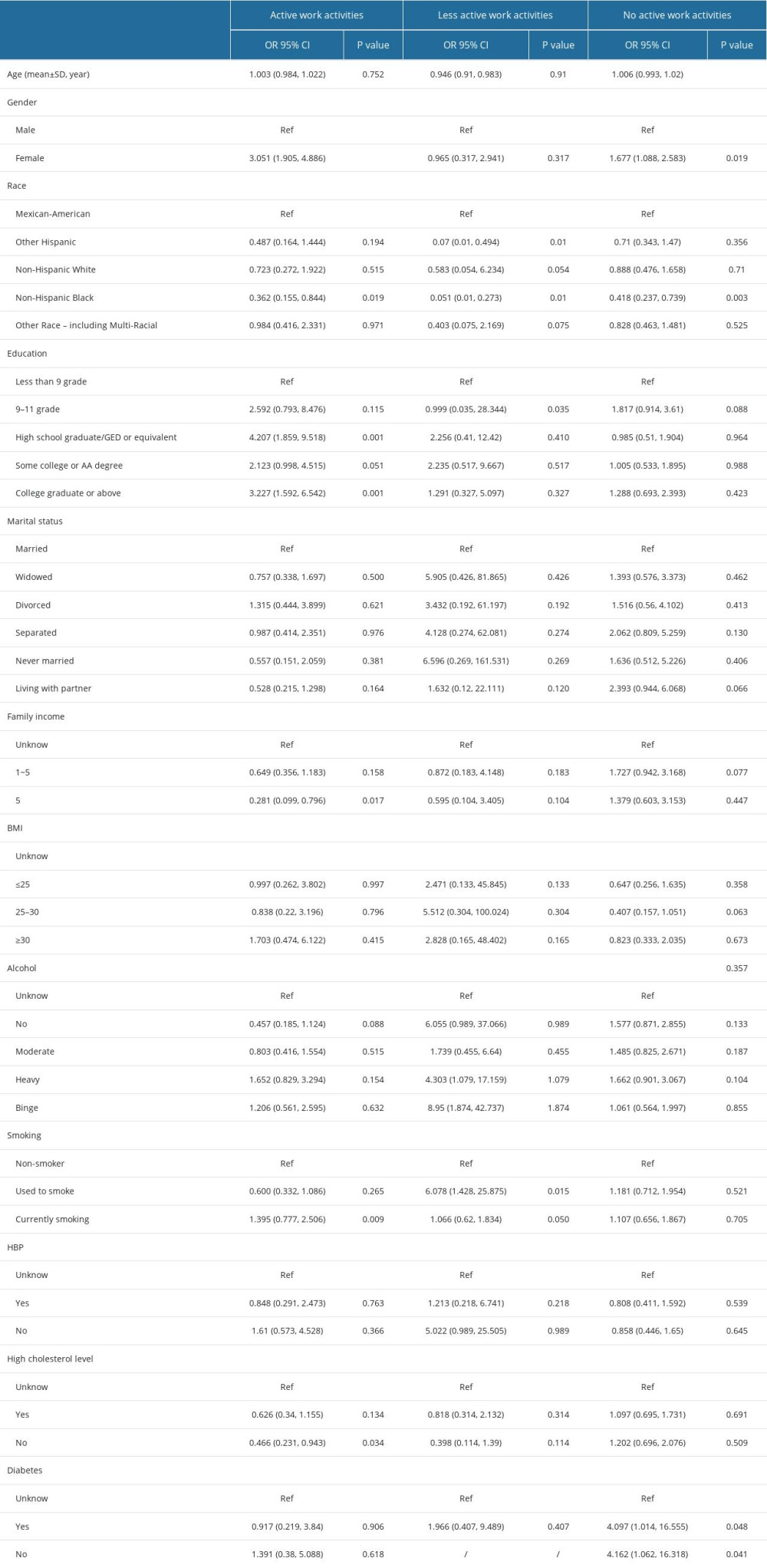 Table 4. Work activities-emergency care subgroup analysis.
Table 4. Work activities-emergency care subgroup analysis.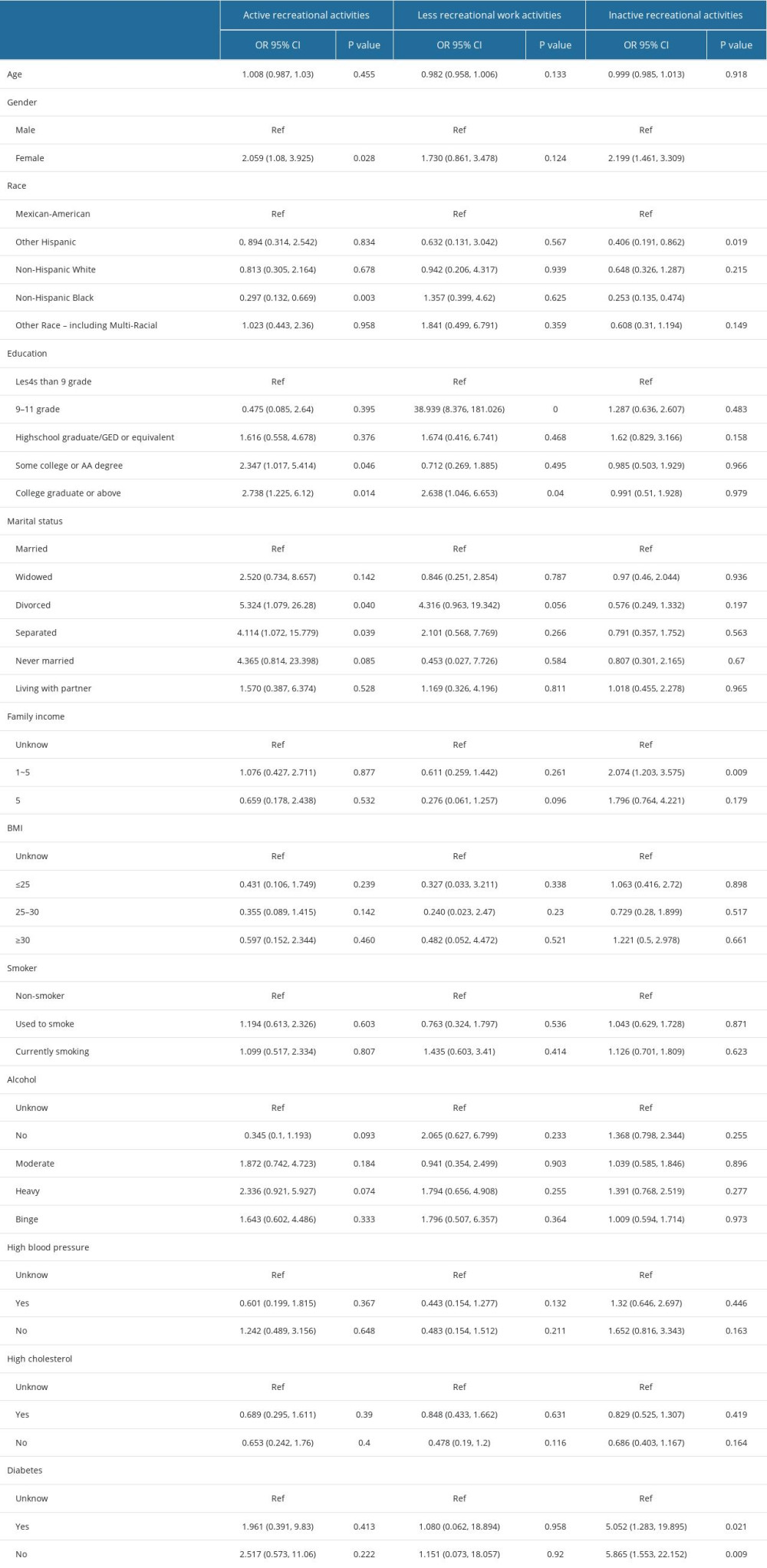 Table 5. Recreational activities – emergency care subgroup analysis.
Table 5. Recreational activities – emergency care subgroup analysis.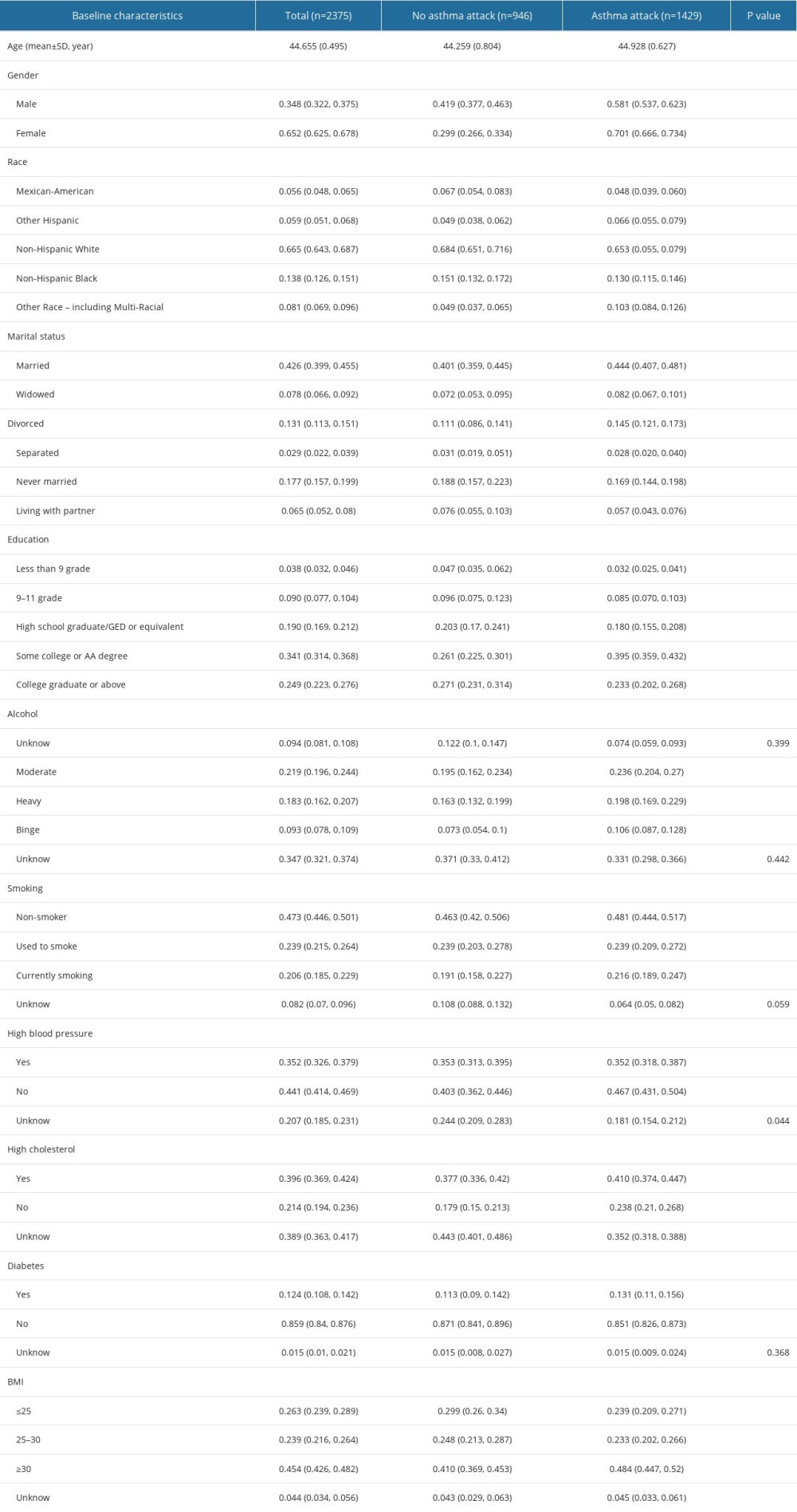 Table 1. Baseline characteristics of asthma patients with different asthma attack subgroup.
Table 1. Baseline characteristics of asthma patients with different asthma attack subgroup.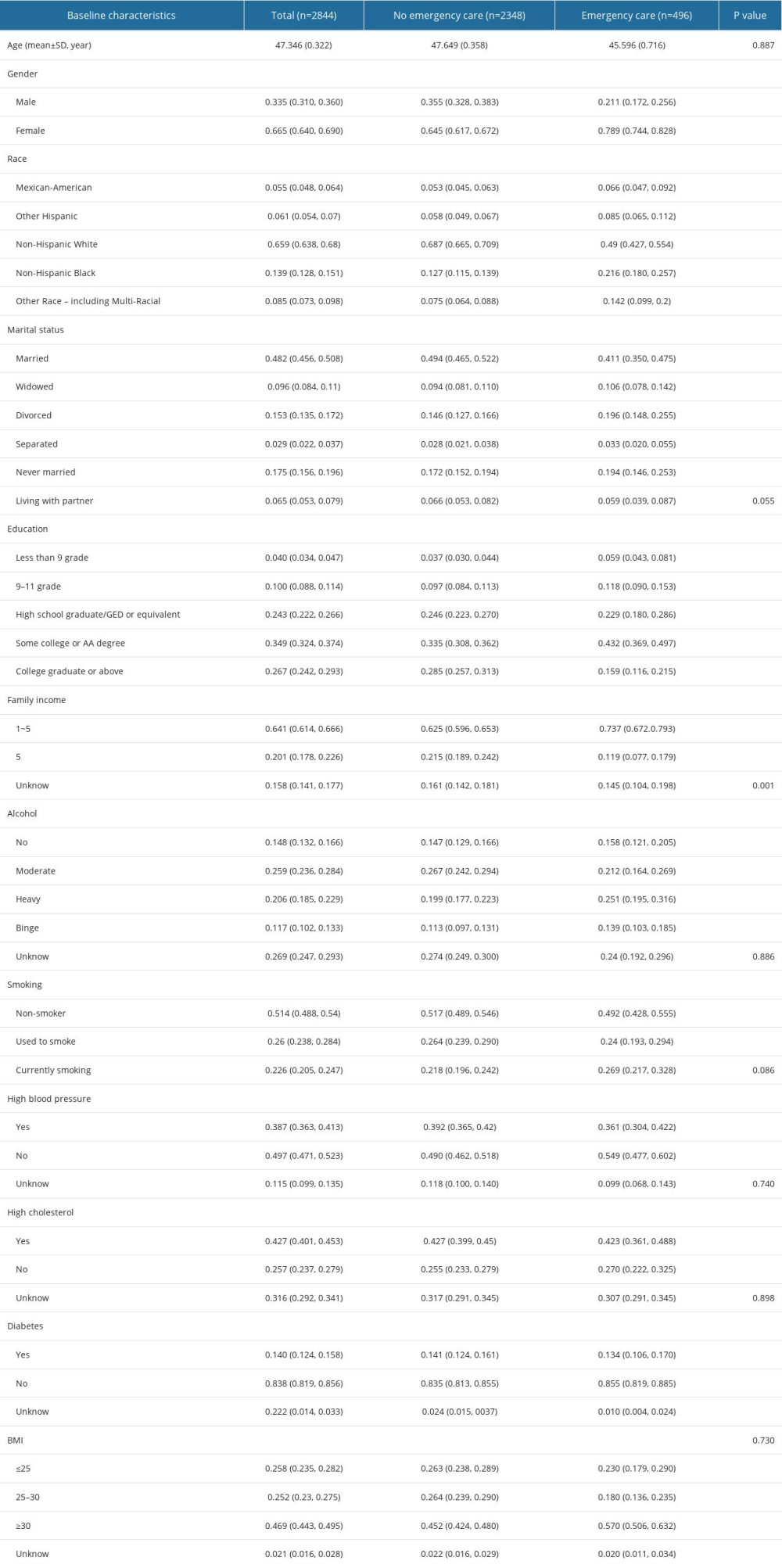 Table 2. Baseline characteristics of asthma patients with different Emergency cases subgroup.
Table 2. Baseline characteristics of asthma patients with different Emergency cases subgroup.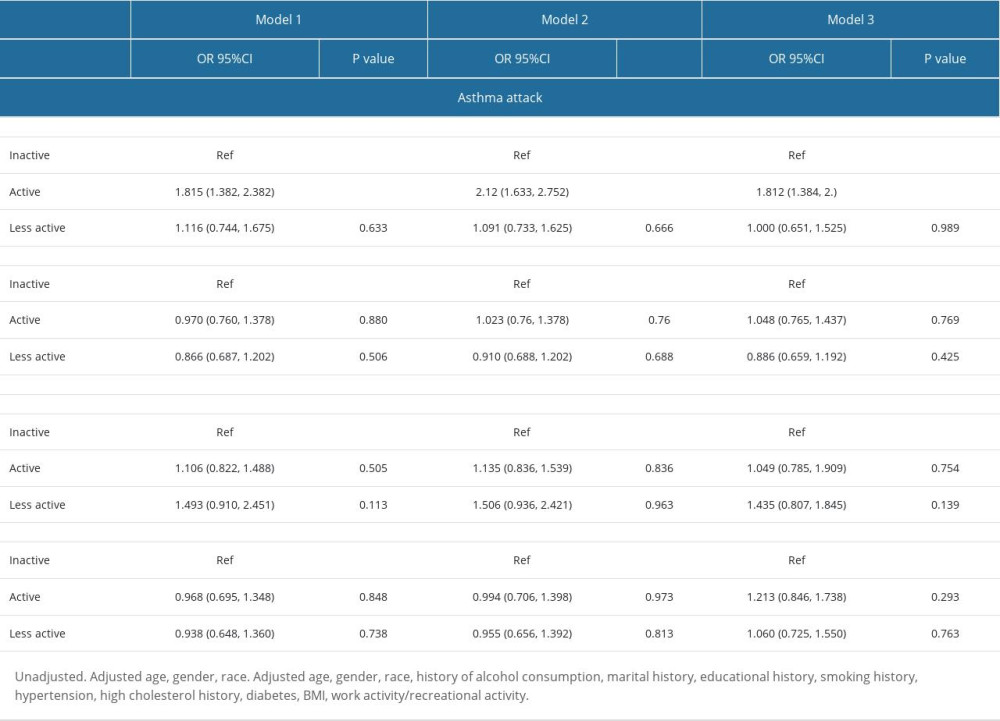 Table 3. The relationship between physical activity and asthma control und er different models.
Table 3. The relationship between physical activity and asthma control und er different models.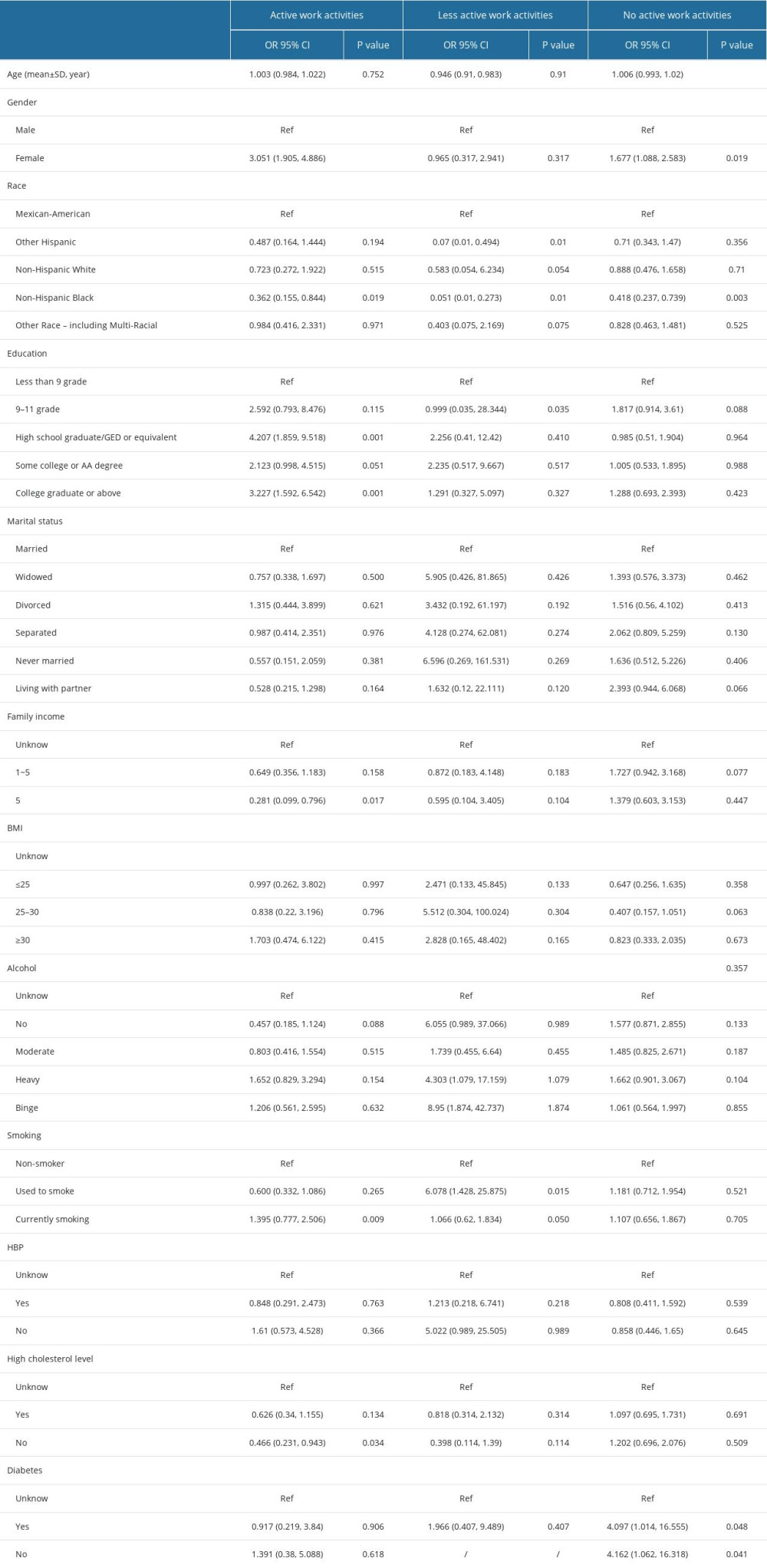 Table 4. Work activities-emergency care subgroup analysis.
Table 4. Work activities-emergency care subgroup analysis.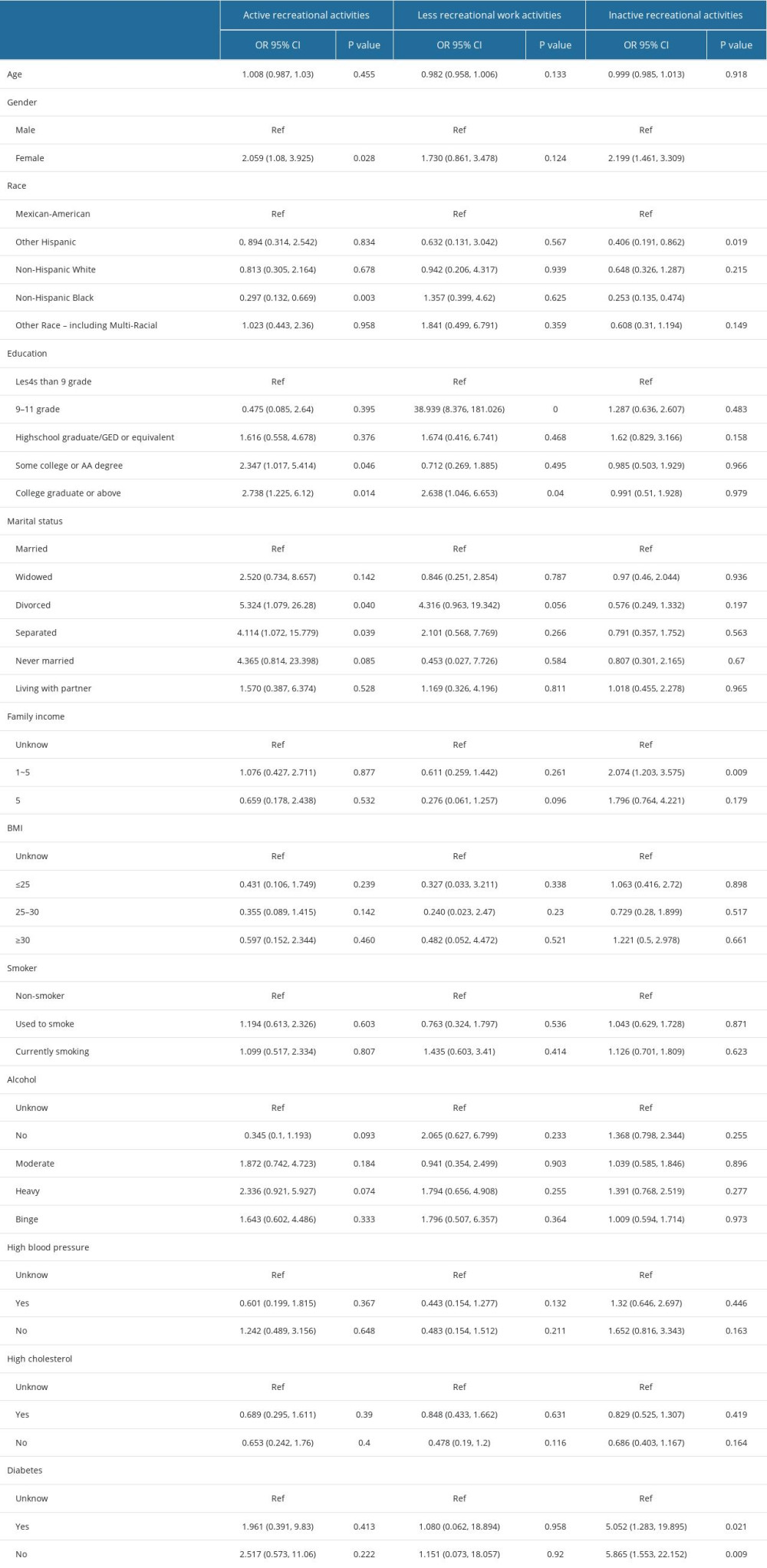 Table 5. Recreational activities – emergency care subgroup analysis.
Table 5. Recreational activities – emergency care subgroup analysis. In Press
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
06 Mar 2024 : Clinical Research
Enhanced Surgical Outcomes of Popliteal Cyst Excision: A Retrospective Study Comparing Arthroscopic Debride...Med Sci Monit In Press; DOI: 10.12659/MSM.941102
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








