23 October 2023: Clinical Research
Comparative Evaluation of Metallic and Biodegradable Suture Anchors in Arthroscopic Repair of Anterior Talofibular Ligament Injury: A Short-term Study on Clinical and Functional Outcomes
Lei ZhangABG, Xiaogao TangABC, Guixuan YouBCDE, Xueyi ChenEF, Siyi YangDF, Houyin ShiF, Guoyou WangAEDOI: 10.12659/MSM.939830
Med Sci Monit 2023; 29:e939830
Abstract
BACKGROUND: With the development of arthroscopy and suture anchor, the modified Brostrӧm technique has made remarkable progress. However, it is unclear which material is most suitable for treating anterior talofibular ligament injury (ATFL). This study evaluated the short-term efficacy of 2 suture anchors (metal vs biodegradable materials) in arthroscopic ATFL repair.
MATERIAL AND METHODS: From January 2018 to December 2019, 82 patients with ankle disorders (51 men and 31 women) with ATFL injury received arthroscopic repair with suture anchor through the Brostrӧm-Gould procedure. The mean age was 38.70±9.35 years (range, 18-54 years). Each patient was followed up. American Orthopedic Foot and Ankle Society score (AOFAS), Karlsson Ankle Functional Score (KAFS), and the Visual Analogue Scale (VAS) were used to evaluate functional status and pain.
RESULTS: All patients were followed up for 21.21±2.19 months (range, 18-25 months). No complications were found either group. Preoperative clinical and functional scores in both groups had no significant difference (P>0.05). The functional score increased significantly in both groups (P<0.001). At the last follow-up, the mean AOFAS score was 93.00 (90.00, 96.00) in the Biodegradable group and 93.50 (91.00, 96.00) in the Metallic group (P=0.31). The mean KAFS score was 91.50 (85.00, 95.00) in the Biodegradable group and 93.00 (90.00, 95.50) in the Metallic group (P=0.10); the mean VAS score was 1.50 (1.00, 1.80) in the Biodegradable group and 1.30 (0.98, 1.70) in the Metallic group (P=0.22).
CONCLUSIONS: Arthroscopic repair of ATFL injury with suture anchors can improve the prognosis of CAI. There were no statistically significant differences in clinical and functional outcomes with metal or biodegradable suture anchors at short-term follow-up.
Keywords: Ankle, Ankle Injuries, Arthroscopy, Lateral Ligament, Ankle, Postoperative Period, Suture Anchors, Male, Humans, Female, Adult, Middle Aged, Retrospective Studies, Joint Instability, Ankle Joint
Background
Ankle sprain is one of the most common sports injuries of the ankle [1]. In the US, data from emergency department visits suggest an incidence rate of 2 to 7 acute ankle sprains/1000 person-years. Reports show that lateral sprain account for approximately 85% of ankle sprains [2] and up to 80% of patients have an ATFL injury [3]. Additionally, approximately 20% of patients progress to chronic ankle instability (CAI) [4]. In case of failure of conservative treatment, it is necessary to use surgical treatment for anatomical repair or reconstruction of the ATFL to provide good clinical results. An increasing number of surgeons are using suture anchors to repair the ATFL arthroscopically to treat chronic ankle instability [5,6].
Regarding suture anchors, there are differences in the choice of suture anchor material among different surgeons, but in the current study most of them are the choice of the number of anchors, the difference of suture knot mode, or insertion angle [7–10]. In terms of anchor materials, most of them focus on rotator cuff injury repair, and little information has been provided to evaluate differences between various materials in repairing the ATFL. Hembree et al [11] reported that an innovative suture-based anchor had a greater peak load to failure compared with a bioabsorbable anchor in the fibula. Therefore, it is important to determine whether there are differences in clinical and functional outcomes after ATFL repair with biodegradable and metallic suture anchors.
Thus, the study was designed to compare the short period clinical and functional outcomes of the arthroscopic modified Broström-Gould procedure that uses metallic or biodegradable suture anchor to repair AFTL injuries. We hypothesized that no differences in clinical and functional outcomes based on suture anchor type would be observed.
Material and Methods
Patient Selection
INCLUSION CRITERIA:
(1) All the patients had an obvious medical history of ankle sprain, and all cases had pain, swelling, and obvious ankle movement limitation when admitted to hospital. (2) All cases received conservative treatment for more than 6 months, but without improved symptoms. (3) Varus stress anteroposterior radiographs showed tibial talus inclination over 15°, and anteroposterior drawer lateral radiographs showed tibial talus inclination over 10 mm, with ligamentous disruption discovered on plain MRI. (4) No medical history of previous ankle fracture or surgery; (5) Complete surgery and follow-up record.
EXCLUSION CRITERIA:
(1) Combined deformity, ipsilateral ankle fracture(s), revision operation, not suitable for surgery due to infectious disease and other ligament injuries; (2) Ankle and subtalar osteochondral injury or osteoarthritis which affected the motor function of the lower limbs; (3) Severe underlying diseases such as chronic wasting disease that cannot tolerate surgery; (4) Acute ankle sprain without conservative management for more than 6 months.
THE GENERAL INFORMATION OF PARTICIPANTS:
From January 2018 to December 2019, 132 consecutive CAI patients who underwent arthroscopic repair with suture anchors via the modified Broström-Gould procedure by the same group of senior foot and ankle surgeons were invited to participate in this study.
Ultimately, a total of 82 patients completed their follow-up in this study. Five patients were followed up for shorter than 18 months, and 10 patients had withdrawn from the study, 20 patients had a history of ankle operation, and 15 patients had other ankle diseases. Demographic details and general preoperative data of the patients enrolled in the study are shown in Table 1.
MATERIAL:
The introduction of suture anchors details materials in this study are shown in Figure 1 and Table 2.
SURGERIES:
All surgeries were performed by the same group of surgeons. The specific surgical approach used the technique of Tun Hing Lui et al.
The patient was placed in the supine position, and the affected thigh was tied with a pneumatic tourniquet to prevent excessive blood loss during the operation so that the surgical field was clean. The ankle joint was fixed in neutral position. The approach and important tissue surface markers were marked before the operation to avoid injury of the superficial peroneal nerve, deep peroneal nerve, anterior tibial artery and vein, and anterior tibial tendon. The median approach and the anterolateral approach were established as the operating approach. Among them, the median approach was 5 mm lateral to the anterior tibial tendon at the ankle joint space plane, and the anterolateral approach was about 15 mm in front of the fibula tip.
The ankle arthroscopy was performed using the standard anterolateral and median approach (Figure 2A), followed by debriding hyperplasia tissue in the articular cavity to ensure excellent exposure. The intra-articular structures damage including cartilage and ligaments was fully evaluated (Figure 2B). Subsequently, the attachment site for the ATFL on the fibula was examined and exposed. The suture anchor (Table 2) (Osteoraptor 2.9 mm, Smith & nephew; Twinfix Ti 3.5 mm, Smith & nephew) was placed in the middle of the fibula footprint site through the anterolateral approach (Figure 2C). We confirmed the pull-out resistance of the anchor by pulling the anchor wire (Figure 2D). Under direct arthroscopic visualization, No. 2 Nylon loop threads carried by a needle served as a suture passer and were introduced via the accessory anterolateral portal (Figure 2E). With the assistance of the grab loop, the ATFL was sutured and fixed to the distal fibula (Figure 2F).
POSTOPERATIVE MANAGEMENT:
The ankle joint was immobilized by cast in mild dorsal expansion and eversion for 2 weeks. Early non-weightbearing functional exercise such as performing primary range of motion (ROM) (mostly dorsiflexion) and isometric exercises of the lower limb was encouraged on the second day after surgery. The plaster cast was changed to an ankle brace 2 weeks after surgery, and patients were permitted to gradually start partial weight-bearing functional exercises after removal of the skin sutures. Balance and endurance training commenced in 6 weeks and transitioned to full weight-bearing.
FOLLOW-UP AND EVALUATION INDEXES:
Wound healing, postoperative complications, and ankle stability were assessed during follow-up and recorded in the 2 groups. Postoperative outcomes were assessed in all participants at 2 weeks, 12 weeks, and last follow-up. The AOFAS and KAFS scores were used to evaluate the clinical and functional results, and the VAS score was used to assess pain.
STATISTICAL ANALYSIS:
SPSS version 25.0 for Windows (SPSS, Inc., Chicago, IL, USA) was used to analyze the data. Shapiro-Wilk tests were conducted to assess data normality. The continuous normally distributed variables are expressed as mean±standard deviation (SD) and non-normally distributed variables are represented by medians (interquartile range, IQR). The independent samples
Results
Patients in both groups were followed up for 21.21±2.19 months (range, 18–25 months). All incisions healed successfully without wound complication, foreign body reaction, or vascular or nerve injury. Preoperative clinical and functional scores were not significantly different in either group (
Discussion
This study compared the short-term functional and clinical outcomes of an arthroscopic modified Broström-Gould procedure using metallic or biodegradable suture anchors to repair AFTL injuries. With both types of suture anchor material, ankle function was improved after ATFL repair at the early postoperative stage.
Patients with superior quality of tissue of the ATFL remnant tended to choose ligament stump repair technology. With the development of arthroscopic technology, ankle arthroscopic technology has also developed rapidly, making it possible to carry out the anatomical repair of lateral collateral ligament of the ankle under all-arthroscopy [12–14]. Suture anchors used in foot and ankle surgery have provide a good choice for surgeons in minimally invasive surgery. Currently, the arthroscopic Broström-Gould procedure is widely used to repair the ATFL. Previous studies have shown that it is a reasonable alternative to the CAI treatment regimen, and can obtain the same short-term functional results as classical Broström-Gould surgery [15].
Gang Zeng et al [16] evaluated early therapeutic efficacy and cost between open Broström-Gould repair (n=10) and all-arthroscopic anatomical repair (n=17) of the ATFL for chronic lateral ankle instability, and both groups had comparable therapeutic efficacy for CAI, but the arthroscopic group had a smaller incision, while the open group had a shorter surgery duration and lower cost.
Few clinical studies have compared different implant materials, which are useful for surgeons to evaluate the short-term clinical efficacy of patients [17].
The first type of suture anchors in our study used for repairing was metallic. Using metal anchors can be associated with complications such as anchor loosening and migration, cartilage injury, and metal allergy [18–20]. Another major drawback is artifacts in MRI evaluation [21]. The other is biodegradable suture anchors which have been widely used since the 1990s. Those anchors have not the drawbacks of previously used metallic anchors and those devices provide the necessary initial strength, and their mechanical characteristics during degradation decline slowly. Biodegradable suture anchors have stability and fixability comparable to metal. Moreover, compared to metallic anchors, biodegradable anchors are associated with simpler revision procedures, better postoperative imaging, and higher biocompatibility, and do not require removal procedures [22–24]. It has excellent radiolucency, which can be utilized to properly evaluate the bony conditions by plain radiography and CT [20]. However, as a nonmetallic implant, there are still shortcomings, such as cyst formation, soft-tissue inflammation, loosening of implant fragments in the joint, and local osteolysis [25–27].
In our study, there were no significant differences in function and pain scores in either group at each follow-up period, and those improved significantly in both groups at the final follow-up. It indicated that there was no significant difference in functional recovery after arthroscopic repair of ATFL despite the use of anchors of different materials. The main advantage of this study was that the same group of well-trained surgeons utilized mature technology and the same type of metal or biodegradable suture anchor for all operations.
This study has a few limitations. Firstly, the study was designed retrospectively, which may have created selection bias, since the anchors used during surgery were not randomized among the 2 different types of suture anchors. Moreover, the observation time was short, meaning that a long-term functional follow-up is not clear and the outcome might not be applicable to internal implants of other materials. Thirdly, postoperative images of the 2 types of anchors were evaluated only by X-ray without other aspects of the anchors, such as biomechanics. Future studies need to include additional biomechanical studies and appropriate randomized controlled trials, as well as long-term follow-up to better understand the true benefits of biodegradable implants relative to metal implants in arthroscopic repair.
Conclusions
Arthroscopic repair of ATFL injury with suture anchors can improve the prognosis of CAI. There was no statistically significant difference in postoperative outcomes between metallic and biodegradable anchors when using all-inside arthroscopic modified Broström-Gould procedure to repair ATFL.
Figures
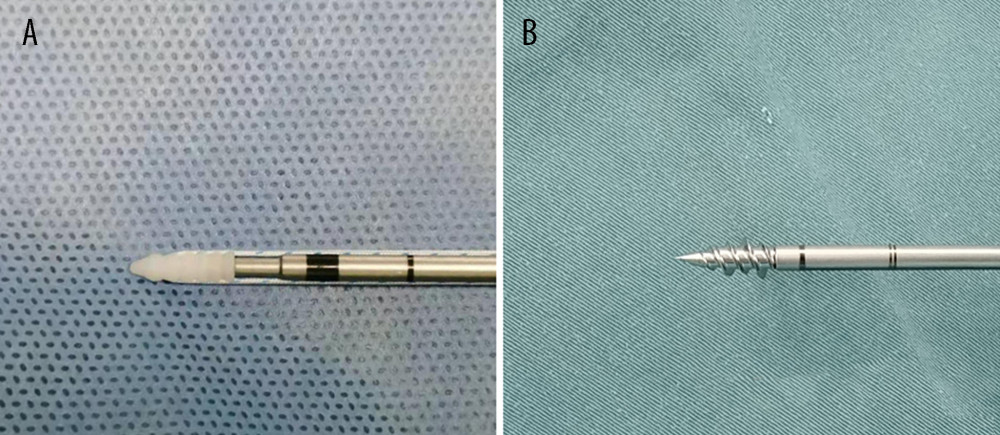 Figure 1. (A) The appearance of PEEK anchor. (B) The appearance of Titanium alloy. All figures are processed using PS (Adobe Photoshop CC, Adobe Systems, California, USA).
Figure 1. (A) The appearance of PEEK anchor. (B) The appearance of Titanium alloy. All figures are processed using PS (Adobe Photoshop CC, Adobe Systems, California, USA). 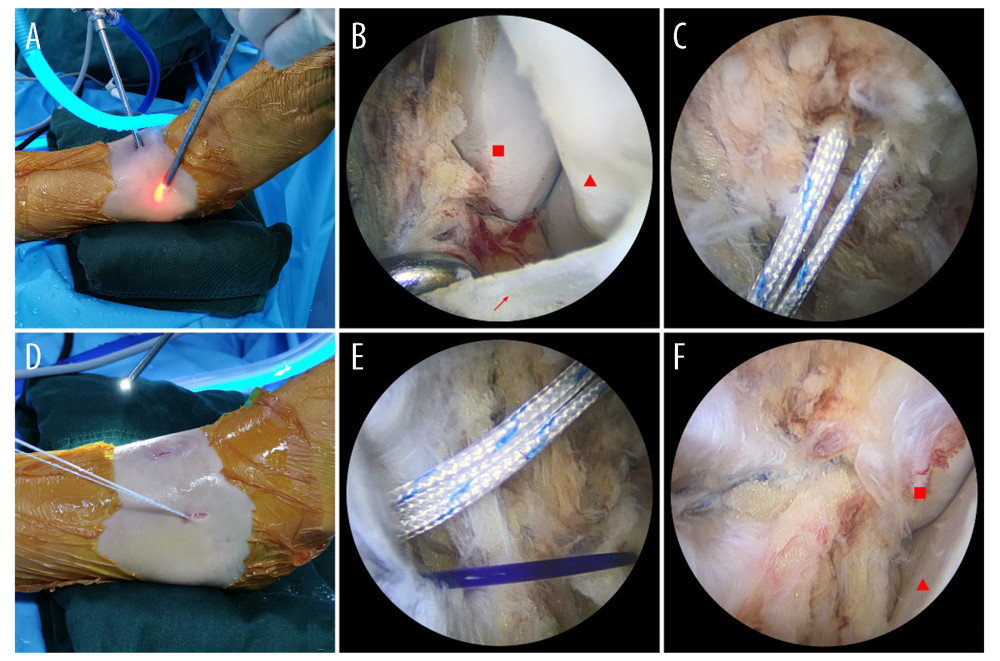 Figure 2. (A) Standard anterolateral and anteromedial ankle arthroscopic approaches were established. (B) Use the probe hooks to detect ATFL (red arrow) damage ( fibula, Talus). (C). The double suture anchor was inserted into the middle of the fibula footprint area. (D) Confirm the pull-out resistance of the anchor by pulling the anchor wire. (E) Use nylon wire to guide the anchor wire through the ATFL. (F) Confirm the effectiveness of the suture under the arthroscopic visualization and check the stability of the ankle ( fibula, Talus). All figures were created using PS (Adobe Photoshop CC, Adobe Systems, California, USA).
Figure 2. (A) Standard anterolateral and anteromedial ankle arthroscopic approaches were established. (B) Use the probe hooks to detect ATFL (red arrow) damage ( fibula, Talus). (C). The double suture anchor was inserted into the middle of the fibula footprint area. (D) Confirm the pull-out resistance of the anchor by pulling the anchor wire. (E) Use nylon wire to guide the anchor wire through the ATFL. (F) Confirm the effectiveness of the suture under the arthroscopic visualization and check the stability of the ankle ( fibula, Talus). All figures were created using PS (Adobe Photoshop CC, Adobe Systems, California, USA). References
1. Waterman BR, Owens BD, Davey S, The epidemiology of ankle sprains in the United States: J Bone Joint Surg Am, 2010; 92(13); 2279-84
2. Maffulli N, Ferran NA, Management of acute and chronic ankle instability: J Am Acad Orthop Surg, 2008; 16(10); 608-15
3. Matsui K, Burgesson B, Takao M, Minimally invasive surgical treatment for chronic ankle instability: A systematic review: Knee Surg Sport Tr A, 2016; 24(4); 1040-48
4. Matheny LM, Johnson NS, Liechti DJ, Clanton TO, Activity level and function after lateral ankle ligament repair versus reconstruction: Am J Sports Med, 2016; 44(5); 1301-8
5. Ahn H-W, Lee K-B, Comparison of the modified Broström procedure for chronic lateral ankle instability with and without subfibular ossicle: Am J Sports Med, 2016; 44(2); 3158-64
6. Acevedo JI, Mangone P, Ankle instability and arthroscopic lateral ligament repair: Foot Ankle Clin, 2015; 20(1); 59-69
7. Hong L, Hua Y, Li H, Chen S, Anterior talofibular ligament (ATFL) repair using two suture anchors produced better functional outcomes than using one suture anchor for the treatment of chronic lateral ankle instability: Knee Surg Sports Traumatol Arthrosc, 2020; 28(1); 221-26
8. Zhi X, Zhang Y, Li W, Absorbable suture anchor and knotless anchor techniques produced similar outcomes in arthroscopic anterior talofibular ligament repair: Knee Surg Sports Traumatol Arthrosc, 2022; 30(6); 2158-65
9. Barber FA, Herbert MA, Crates JM, A comparison of lateral ankle ligament suture anchor strength: Foot Ankle Surg, 2013; 19(2); 108-11
10. Weiss WM, Saucedo RP, The effect of suture anchor insertion angle on calcaneus pullout strength: challenging the deadman’s angle: Foot Ankle Spec, 2017; 10(5); 411-14
11. Hembree WC, Tsai MA, Comparison of suture-based anchors and traditional bioabsorbable anchors in foot and ankle surgery: J Foot Ankle Surg, 2017; 56(1); 3-7
12. Jo J, Lee JW, Arthroscopic all-inside anterior talofibular ligament repair with and without inferior extensor retinacular reinforcement: A prospective randomized study: J Bone Joint Surg Am, 2021; 103(17); 1578-87
13. Vega J, Malagelada F, Arthroscopic all-inside ATFL and CFL repair is feasible and provides excellent results in patients with chronic ankle instability: Knee Surg Sports Traumatol Arthrosc, 2020; 28(1); 116-23
14. Li D, Tang Q, Liu Q, Arthroscopic anterior talofibular ligament repair with Internal Brace and lasso-loop technique for chronic ankle lateral instability: Int Orthop, 2022; 46(12); 2821-28
15. Feng SM, Maffulli N, Ma C, Oliva F, All-inside arthroscopic modified Broström-Gould procedure for chronic lateral ankle instability with and without anterior talofibular ligament remnant repair produced similar functional results: Knee Surg Sports Traumatol Arthrosc, 2021; 29(8); 2453-61
16. Zeng G, Hu X, Liu W, Open Broström-Gould repair vs arthroscopic anatomical repair of the anterior talofibular ligament for chronic lateral ankle instability: Foot Ankle Int, 2020; 41(1); 44-49
17. Li H, Xu H, Hua Y, Anatomic knot suture anchor versus knotless suture anchor technique for anterior talofibular ligament repair: A biomechanical comparison: Orthop J Sports Med, 2020; 8(1); 2325967119898125
18. Maestro A, Pipa I, Safety and performance of titanium suture anchors used in knee ligament repair procedures: Medicina (Kaunas), 2021; 57(3); 287
19. Uluyardımcı E, Öçgüder DA, All-suture anchors versus metal suture anchors in the arthroscopic treatment of traumatic anterior shoulder instability: A comparison of mid-term outcomes: Jt Dis Relat Surg, 2021; 32(1); 101-7
20. Kaar TK, Schenck RC, Wirth MA, Rockwood CA, Complications of metallic suture anchors in shoulder surgery: A report of 8 cases: Arthroscopy, 2001; 17(1); 31-37
21. Marquardt B, Witt KA, Long-term results of arthroscopic Bankart repair with a bioabsorbable tack: Am J Sports Med, 2006; 34(12); 1906-10
22. Longo UG, Petrillo S, Loppini M, Metallic versus biodegradable suture anchors for rotator cuff repair: A case control study: BMC Musculoskelet Disord, 2019; 20(1); 477
23. Ro K, Pancholi S, Perianchor cyst formation after arthroscopic rotator cuff repair using all-suture-type, bioabsorbable-type, and PEEK-type anchors: Arthroscopy, 2019; 35(8); 2284-92
24. Milano G, Grasso A, Salvatore M, Arthroscopic rotator cuff repair with metal and biodegradable suture anchors: A prospective randomized study: Arthroscopy, 2010; 26(9); S112-19
25. Barber FA, Complications of biodegradable materials: Anchors and interference screws: Sports Med Arthrosc Rev, 2015; 23(3); 149-55
26. Dhawan A, Ghodadra N, Karas V, Complications of bioabsorbable suture anchors in the shoulder: Am J Sports Med, 2012; 40(6); 1424-30
27. Cobaleda Aristizabal AF, Sanders EJ, Barber FA, Adverse events associated with biodegradable lactide-containing suture anchors: Arthroscopy, 2014; 30(5); 555-60
Figures
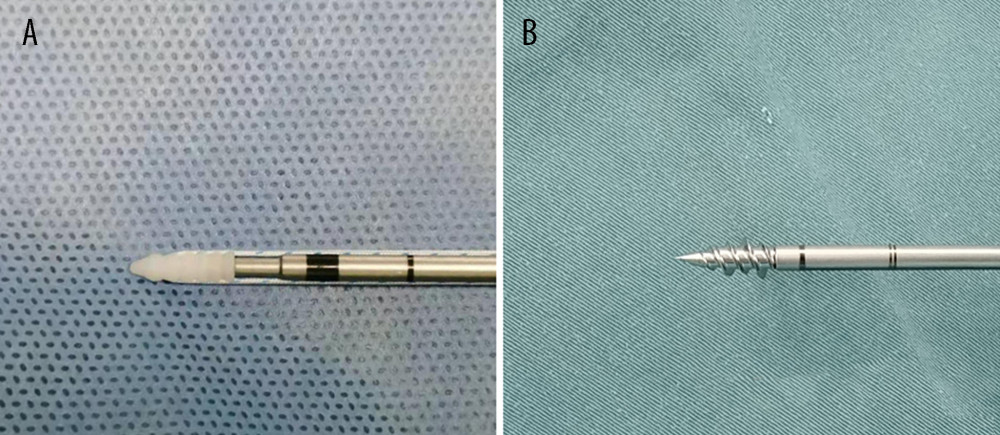 Figure 1. (A) The appearance of PEEK anchor. (B) The appearance of Titanium alloy. All figures are processed using PS (Adobe Photoshop CC, Adobe Systems, California, USA).
Figure 1. (A) The appearance of PEEK anchor. (B) The appearance of Titanium alloy. All figures are processed using PS (Adobe Photoshop CC, Adobe Systems, California, USA).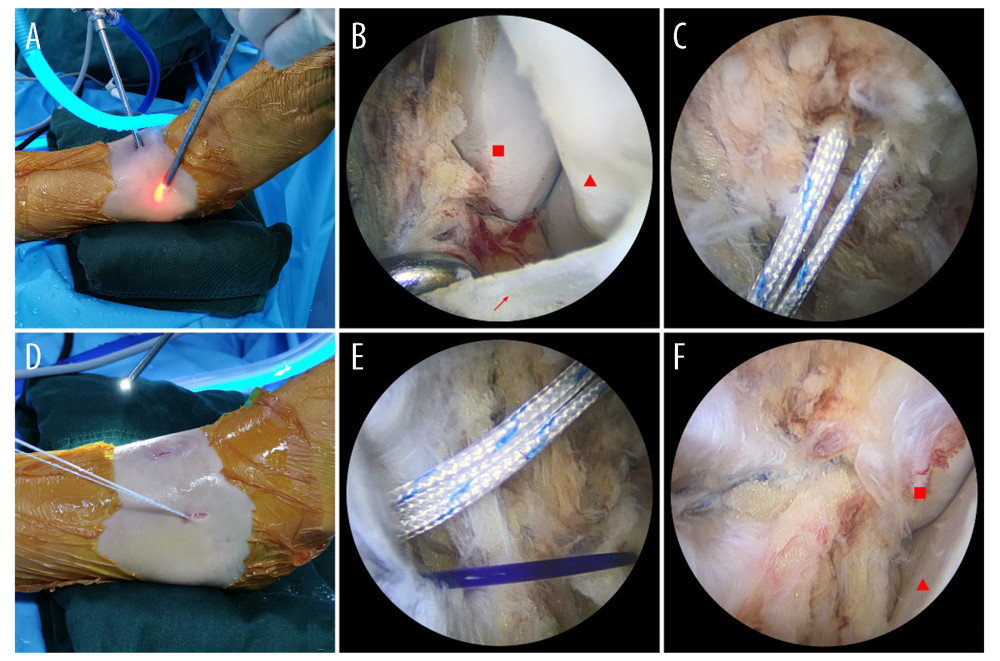 Figure 2. (A) Standard anterolateral and anteromedial ankle arthroscopic approaches were established. (B) Use the probe hooks to detect ATFL (red arrow) damage ( fibula, Talus). (C). The double suture anchor was inserted into the middle of the fibula footprint area. (D) Confirm the pull-out resistance of the anchor by pulling the anchor wire. (E) Use nylon wire to guide the anchor wire through the ATFL. (F) Confirm the effectiveness of the suture under the arthroscopic visualization and check the stability of the ankle ( fibula, Talus). All figures were created using PS (Adobe Photoshop CC, Adobe Systems, California, USA).
Figure 2. (A) Standard anterolateral and anteromedial ankle arthroscopic approaches were established. (B) Use the probe hooks to detect ATFL (red arrow) damage ( fibula, Talus). (C). The double suture anchor was inserted into the middle of the fibula footprint area. (D) Confirm the pull-out resistance of the anchor by pulling the anchor wire. (E) Use nylon wire to guide the anchor wire through the ATFL. (F) Confirm the effectiveness of the suture under the arthroscopic visualization and check the stability of the ankle ( fibula, Talus). All figures were created using PS (Adobe Photoshop CC, Adobe Systems, California, USA). Tables
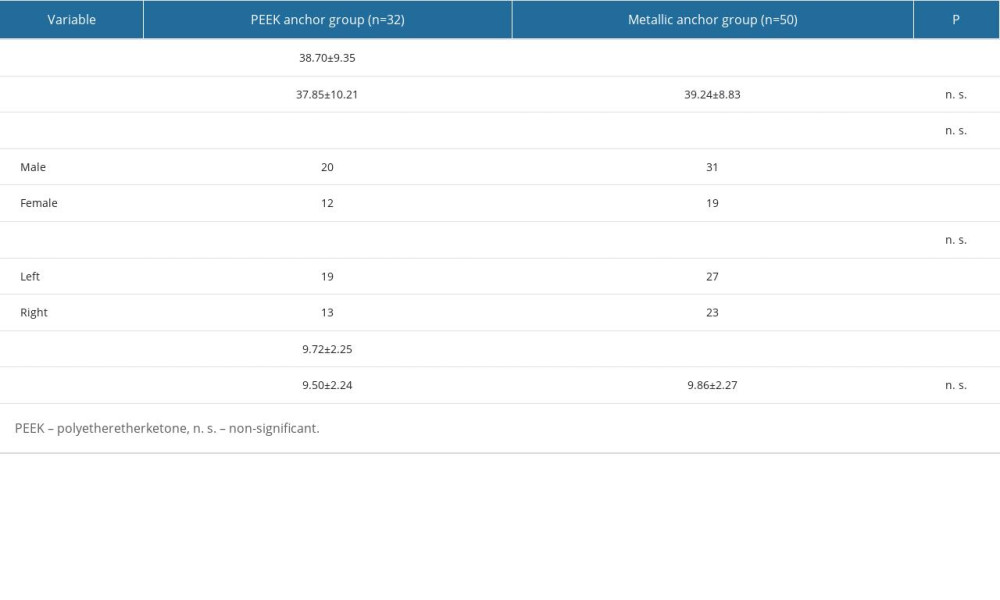 Table 1. Demographic and surgical details.
Table 1. Demographic and surgical details.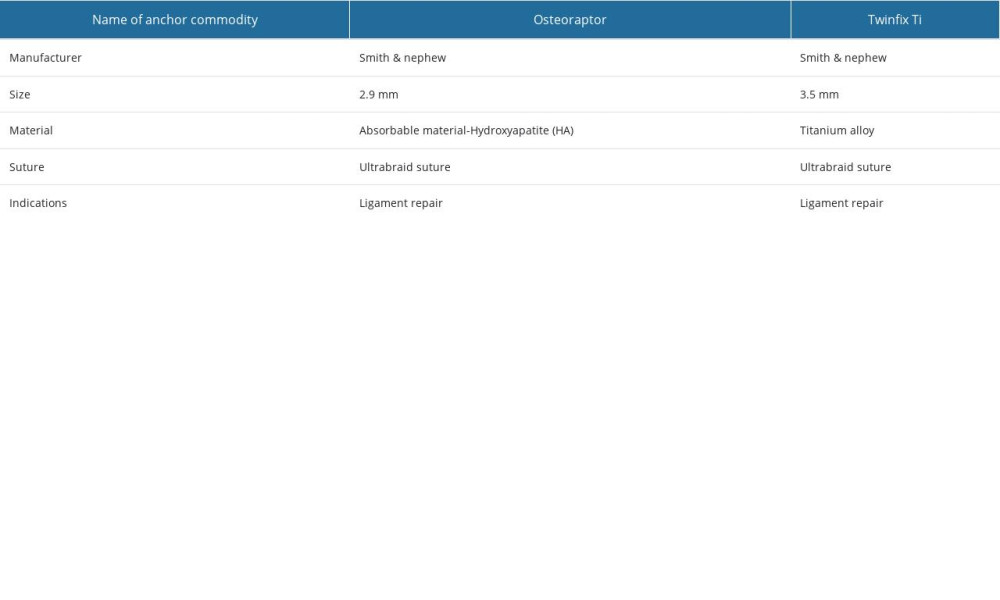 Table 2. The introduction of suture anchors.
Table 2. The introduction of suture anchors.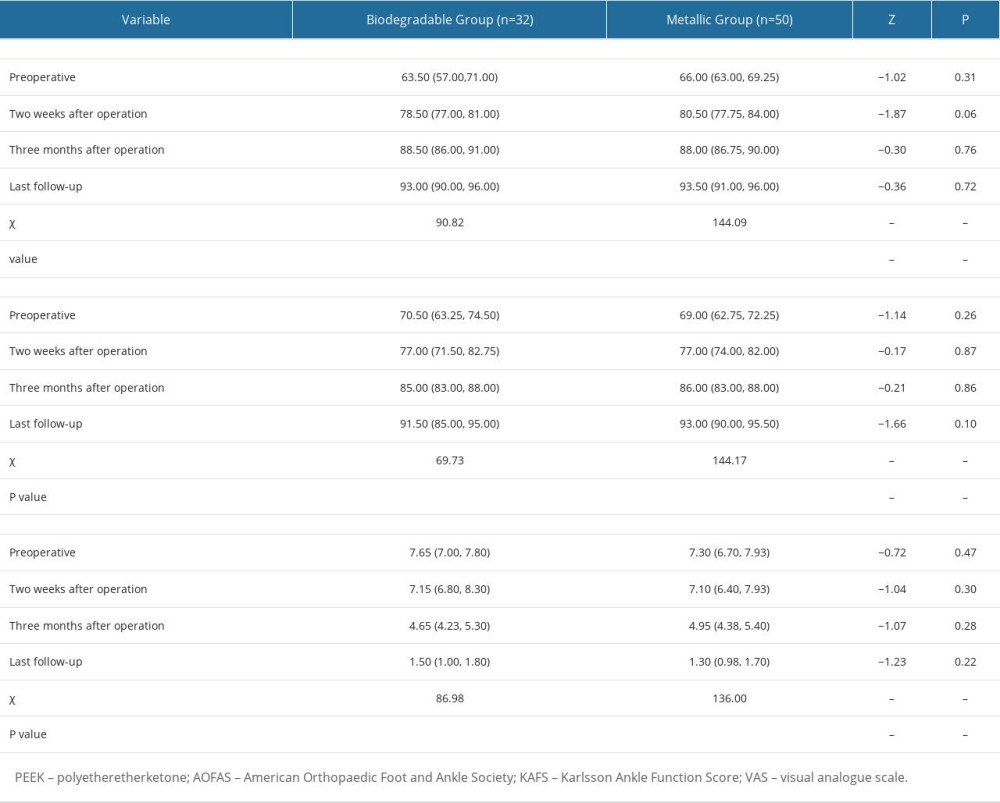 Table 3. Functional and clinical outcomes comparison of the 2 groups.
Table 3. Functional and clinical outcomes comparison of the 2 groups.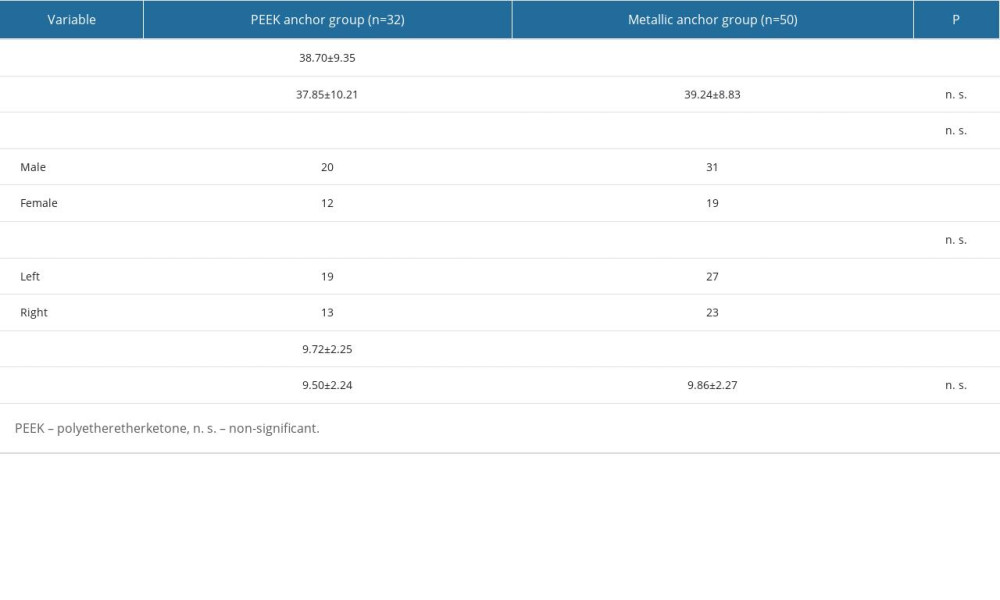 Table 1. Demographic and surgical details.
Table 1. Demographic and surgical details.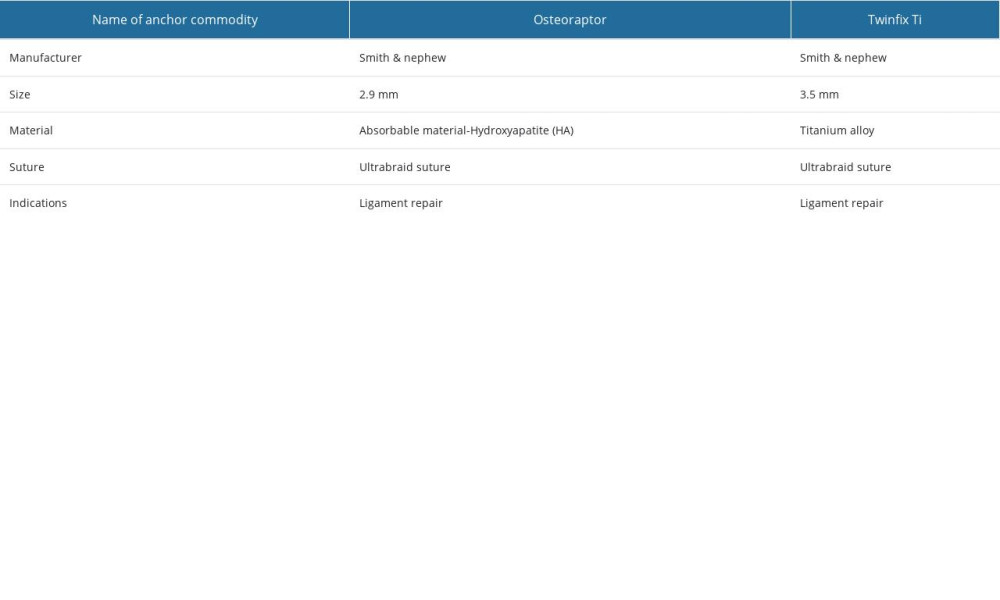 Table 2. The introduction of suture anchors.
Table 2. The introduction of suture anchors.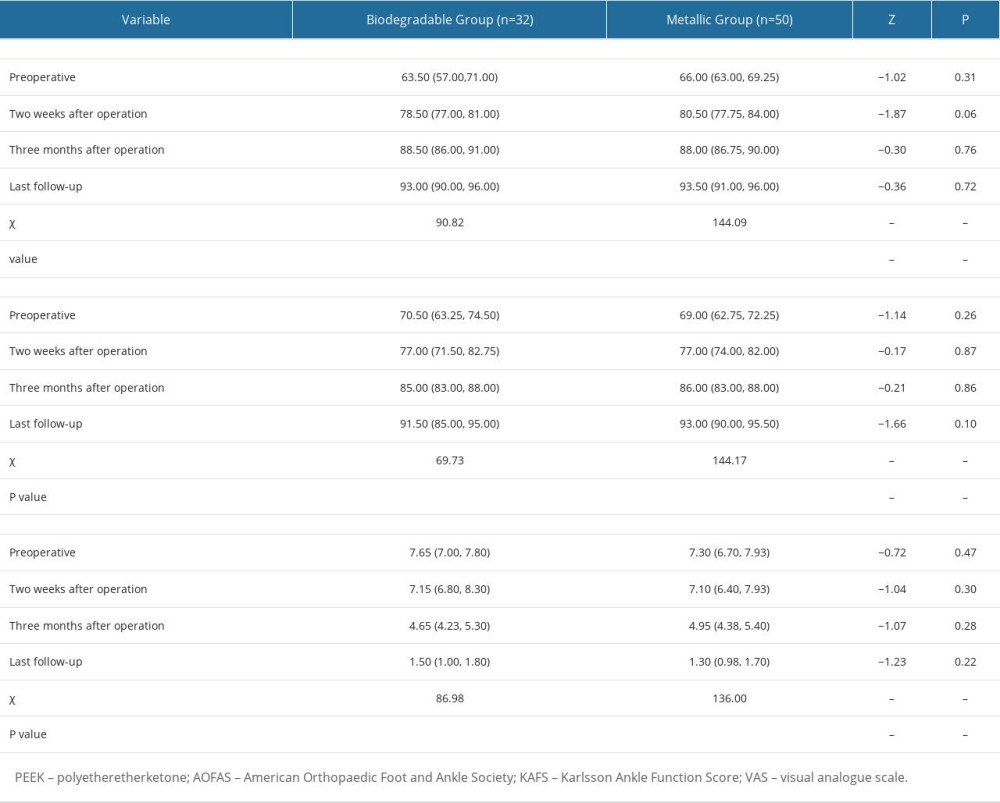 Table 3. Functional and clinical outcomes comparison of the 2 groups.
Table 3. Functional and clinical outcomes comparison of the 2 groups. In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








