18 January 2024: Clinical Research
Enhancing Efficacy and Safety in Laparoscopic Partial Nephrectomy for Localized Renal Tuberculosis: The Skirted Continuous Suture Technique
Xin Tong1ABCDEFG, Jian Zhang1BCDF, Yuzhe Tang2BCDF, Tao Yu3BCDF, Zhijia Liu4CDF, Hongwei Bai4CDF, Qiang Wang12BCDG*DOI: 10.12659/MSM.940146
Med Sci Monit 2024; 30:e940146
Abstract
BACKGROUND: Limited research has been conducted on laparoscopic partial nephrectomy for kidney tuberculosis. This study aimed to evaluate the effectiveness of the skirted continuous suture technique in laparoscopic partial nephrectomy for localized renal tuberculosis.
MATERIAL AND METHODS: Five patients with kidney tuberculosis underwent standard retroperitoneal laparoscopic partial nephrectomy after computed tomography evaluation. The skirted continuous suture technique was utilized during the procedure. This retrospective study analyzed the outcomes of these patients who received treatment between January 2011 and December 2020 at Beijing Tsinghua Changgung Hospital and Eighth Medical Center of Chinese People’s Liberation Army General Hospital.
RESULTS: The surgical success rate was 100%. Renal function was well preserved, with a decrease of glomerular filtration rate by 9.6±9.0 ml/min. Only 1 patient experienced postoperative urinous infiltration and lymphatic fistula, while the others did not have any surgical complications. Antituberculous therapy was continued postoperatively, and 1 patient had recurrence during follow-up.
CONCLUSIONS: The laparoscopic continuous suturing technique offers a reliable and straightforward method for extensively closing incision edges of the renal parenchyma in laparoscopic surgery. It contributes to the improved efficacy and safety of treating localized renal tuberculosis with exceptional application.
Keywords: Kidney, Nephrectomy, Kidney Tubules, Laparoscopy, Suture Techniques
Background
According to the Global Tuberculosis Report 2019 released by the World Health Organization, tuberculosis (TB) ranked first among causes of death by single-pathogen diseases, and roughly 10 million new TB patients emerge annually worldwide [1]. Based on the report, China had the second largest burden of TB in the world. Extrapulmonary TB accounted for 10% of cases in China and the proportion continues to increase. Urogenital TB accounted for 30–40% of all forms of extrapulmonary TB, among which kidney TB is the most common [2].
In localized or cavitation kidney TB patients, the tuberculous focus is located at 1 pole or 1 fragment of the kidney, without destruction of the whole kidney, which means that the affected kidney remains functional.
Given the severe fibrosis in the perinephric cavity caused by TB, tissue dissection and separation become technically challenging under laparoscopy. Laparoscopic technology has successfully replaced open surgery for removal of end-stage tuberculous kidneys [6]. Although experience with laparoscopic partial nephrectomy has accumulated, few studies on laparoscopic partial nephrectomy for kidney TB have been conducted [7,8]. Thus, this study aimed to evaluate the efficacy and safety of the skirted continuous suture technique in retroperitoneal laparoscopic partial nephrectomy for localized kidney TB.
Material and Methods
PATIENTS:
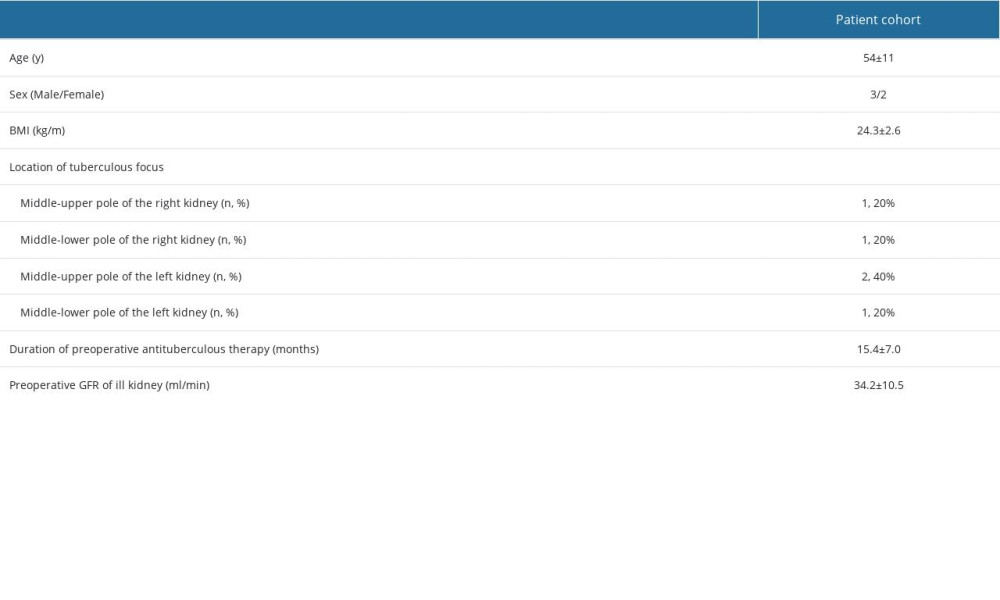
This study retrospectively reviewed 5 kidney TB-infected patients who received a retroperitoneal laparoscopic partial nephrectomy at Beijing Tsinghua Changgung Hospital and Eighth Medical Center of Chinese People’s Liberation Army General Hospital between January 2011 and December 2020. Characteristics of patients are shown in Table 1. All patients were subjected to a quadruple antituberculous therapy before surgery. Contrast-enhanced computed tomography (CT) was used for diagnosis and localization of tuberculous focus. Renal dynamic imaging (99mTc-DTPA- 5mci)-mediated measurement of glomerular filtration rate (GFR) was conducted to assess the split renal function. The diagnosis of focal renal tuberculosis is based on a combination of clinical manifestations, imaging, and laboratory tests. Clinically, patients may experience symptoms such as hematuria, lumbar pain, frequent urination, and urinary urgency. Systemic symptoms such as low fever, chills, night sweats, and loss of appetite may also occur. Common imaging methods include renal CT scan, renal ultrasound, and radionuclide nephrography. Normally, the kidney should be uniform and translucent, but in the case of focal renal tuberculosis, imaging manifestations such as renal necrosis, calcification, abscesses, and stones may be seen. Urinalysis is an important part of routine laboratory testing. Abnormalities such as pus, leukocytosis, red blood cells, titularity, and crystals may be present in urine. In addition, ultrasound, urine Mycobacterium tuberculosis culture and urine TB antibody testing can be used as an aid to diagnosis.
SURGICAL METHODS:
The study was approved by unanimous vote of the Ethics Committee members and all patients gave their informed consent. Surgical approach and access, trocar sites, and methods for identification of tuberculous renal anatomy were consistent with our previous reports [6,8].
Patients received general anesthesia to ensure they were pain-free during the procedure. Positioning and access are established by the surgeon making a small incision in the abdomen and then inserting the laparoscope and other necessary surgical tools. The laparoscope was placed through the abdominal cavity to visualize the kidney and perform the operation. For tethered dissection, the surgeon gently cut the fatty muscle tissue around the kidney to expose the kidney. To deal with the kidney’s blood vessels, the surgeon identified and separated the blood vessels of the kidney to remove the part of the kidney. The surgeon used special clamps or electric cutting tools. Nephrectomy was performed depending on the patient’s specific disease, and the surgeon removed a portion of the kidney, ensuring that enough healthy tissue was retained to keep the kidney functioning.
For incision closure, after the surgery was completed, the surgeon carefully inspected the incision to make sure there was no bleeding or other complications. Then, the surgeon closed the incision with sutures. Localized kidney TB showed inflammatory changes in the perinephric cavity, and the renal parenchyma was fibrotic and lacked blood supply. The abscess was clearly protruding with a white wall, which was easily identified under endoscopy (Figure 1A). After blocking of the renal artery, the tuberculous focus was dissected and completely removed along the abscess wall (Figure 1B).
STITCHING METHOD:
The renal collecting system was sutured to avoid occurrence of postoperative urinary fistula, using V-Loc 3-0 (V-Loc wound closure device, Covidien, Mansfield, MA) absorbable barbed suture. Thereafter, the skirted continuous suture technique was used to perform whole-layer suture of the margin of the renal parenchyma with V-Loc 2-0 absorbable barbed suture as follows (Figure 1C). Before taking the first stitch, the suture was fixed with a Hem-o-lock clip (Teleflex, Research Triangle Park, NC) on its thread, and then the first stitch went through the renal parenchyma on the whole layer, and the margin of renal parenchyma was sutured with a continuous circular lockstitch as shown in the schematic illustration. The final stitch was also locked by a Hem-o-lock clip. After suturing, the kidney was re-perfused (Figure 1D).
STATISTICAL METHODS:
Statistical analysis was performed using SPSS software (version 26.0). Continuous variables were expressed either as mean±standard deviation for normal distributions or median (range) for non-normal distributions. The Shapiro-Wilk test was applied to determine whether continuous variables were normally distributed.
Results
SURGICAL SUCCESS RATE:
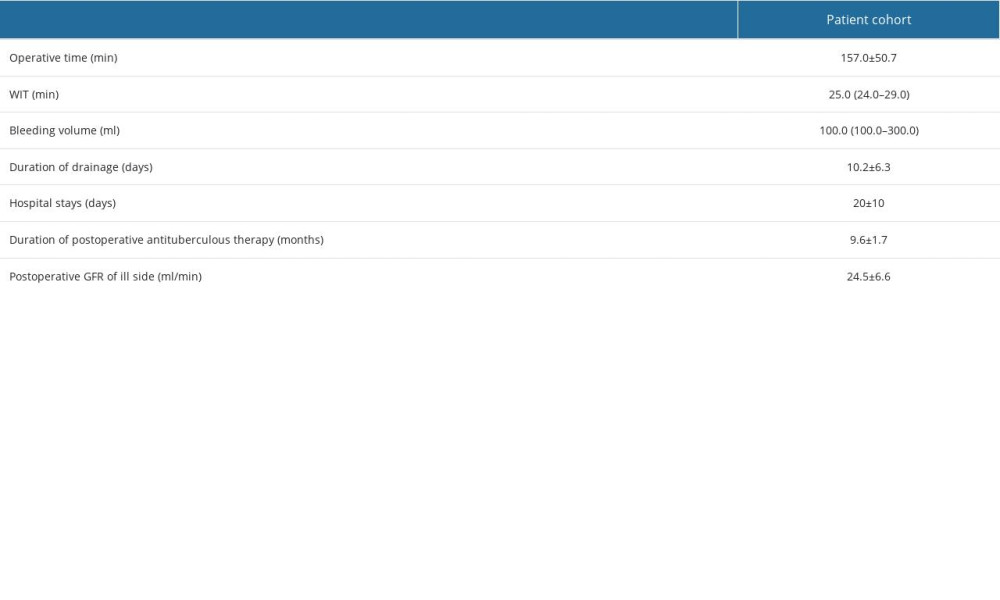
All patients received a quadruple antituberculous therapy, including Rifampicin/Rifapentine, Isoniazid aminosalicylate, ethambutol hydrochloride, and pyrazinamide. All surgeries were successful, with allowable warm ischemic time (WIT) and bleeding volume. Intra- and postoperative parameters are shown in Table 2.
POSTOPERATIVE EXAMINATION RESULTS:
Acid-fast bacilli test results were negative after the operation in all patients. Renal function was well preserved, with a mean decrease of GFR by 9.6±9.0 ml/min. TB was confirmed by pathology. Urinous infiltration and lymphatic fistula occurred in 1 patient. Kidney antituberculous therapy was continued postoperatively. Recurrence was found in 1 patient during follow-up and the patient received Rifapentine, Pasiniazid, Moxifloxacin and Pyrazinamide for drug-resistant TB.
Discussion
The surgical success rate is 100%. Renal function was well preserved, with a decrease of glomerular filtration rate by 9.6±9.0 ml/min. Except for 1 patient with postoperative urinous infiltration and lymphatic fistula, no surgical complications were observed in any of the other patients. Antituberculous therapy was continued postoperatively and recurrence was found in 1 patient during follow-up. According to the extent of tissue destruction, pathology of kidney TB can be classified into 4 stages, from stage 1 to stage 4 [9]. The manifestations of our patients were consistent with stage 3 (destructive form), which refers to cavernous kidney TB. The treatment of kidney TB consistently depended on the antituberculous drugs (ATDs), while surgery was generally performed as a supplementary therapy. Partial nephrectomy for kidney TB was recommended to limit the presence of localized calcified focus, including non-responsiveness to 6 weeks of intensive chemotherapy, or a gradual increase in the size of the calcified area, which may eventually damage the entire kidney [4,10]. However, when localized, kidney TB was effectively treated with chemotherapy, as a cicatrized tuberculous focus might result in structural damage to the kidney, such as scar formation, fibrosis of the renal calyceal neck and infundibula, and other secondary changes that might lead to intrarenal stenosis in severe cases. Poor drainage and even mechanical obstruction of the calyceal neck might cause decreased blood supply to the focus and significantly increase the probability of secondary lithiasis, mixed bacterial infections, and tumors [3]. These forms of renal structural damage and disorders of blood circulation directly affect the effective drug concentration of localized ATDs, resulting in residual
The criteria for nephron-preservation surgery included GFR >15 ml/min and renal cortex thickness >10 mm [12]. Partial nephrectomy for kidney TB was introduced in the 1940s, which was questioned due to conflicting results from Europe [3]. Meanwhile, many patients with kidney TB were cured by ATDs, so that the number of patients treated with partial nephrectomy decreased significantly. However, the progression of calcification was an important indication for partial nephrectomy [10,15]. Although cavernotomy was highly preferred over partial nephrectomy for localized kidney TB because of its safety [3,15], it was considered more suitable for localized hydrops or empyema foci, which were relatively large and easy to locate. Small tuberculous foci and calcifications were likely to be missed, resulting in disease progression. Furthermore, interconnection between the foci and renal pelvis was considered a surgical contraindication, which was difficult to identify. A procedure known as pan-renal ileostomy, in which the entire renal system is drained into the bladder using an ileal loop, has been reported in a related study [5]. This in vivo urinary diversion was adopted to treat severe renal stenosis in renal tuberculosis. However, it was traumatic and increased the risk of water electrolyte disorder and repeated infection.
Exposure of the tuberculous focus was inevitable intra-operatively. The occurrence of secondary TB infection depended on the sufficiency of preoperative antituberculous therapy. A previous study suggested a minimum 4-week ATDs administration before the operation, such as nephrectomy, nephrostomy, or ureteral stent placement [10]. Regarding partial nephrectomy, ATDs should be administered for 2–6 months pre-operatively to better control systemic infection and other small foci of the renal parenchyma, and reduce complications of TB such as urinary fistula, infection spread, and sinus formation [14]. In our study, all patients received preoperative antituberculous therapy for at least 6 months and the postoperative acid-fast bacilli test was negative, indicating that antituberculous therapy was effective.
Suturing the renal stump through laparoscopy was the key technique in partial nephrectomy for kidney TB. Due to the large wound after laparoscopic partial nephrectomy, implementation of a traditional double-layer suture or figure-8-shaped suture was difficult. Zhang et al [16] reported the efficacy of the ring suture technique in partial nephrectomy for hilar or large tumors, showing that the kidney tuberculous focus involved almost half of the kidney and that anastomosis and suture of the renal parenchyma was difficult after removal of the focus. Thus, taking the ring suture technique as a reference, we adopted the skirted continuous suture technique in partial nephrectomy for kidney TB (Figure 1C, 1D). The efficacy of the technique was satisfactory, with a good hemostatic effect. Except for 1 patient with postoperative urinous infiltration and lymphatic fistula, none of the surgical complications were observed in the others. The expected clinical outcomes of tuberculous focus resection and maximum preservation of renal function were successfully achieved.
Based on the premise of standard ATDs therapy, partial nephrectomy could be an important adjuvant therapy for localized kidney TB. The elimination of concealed tuberculous foci could prevent recurrence of TB and progression of infection, and secondary injury caused by cicatrization of kidney tuberculous focus after ATDs therapy could be avoided. The present study presented a minimally-invasive surgical method for maximizing preservation of renal function in patients with kidney TB. However, because of the limited number of patients, various parameters, including the indications for partial nephrectomy, preoperative window period of antituberculous therapy, and operative timing, need to be further explored. This study has limitations due to the small sample size and technical limitations.
Conclusions
Laparoscopic continuous suturing technique can be extensively used to close the incision edges of the renal parenchyma, which is easy and reliable to operate in laparoscopic surgery, and it can improve the efficacy and safety of treating localized renal tuberculosis with excellent effects.
References
1. Wold Health Organization (WHO): Global tuberculosis report 2019 October 15, 2019 Available at: https://www.who.int/publications/i/item/9789241565714
2. Gozdas HT, Caliskan S, Challenges in the diagnosis of renal tuberculosis: Kaohsiung J Med Sci, 2015; 31(9); 493-95
3. Ljunggren E, Indications for nephrectomy, nephro-ureterectomy and partial nephrectomy in renal tuberculosis: J Urol, 1957; 78(5); 499-504
4. Figueiredo AA, Lucon AM, Srougi M, Urogenital tuberculosis: Microbiol Spectr, 2017; 5(1); 120-24
5. Wong SH, Chan YT, Pan-caliceal ileoneocystostomy – a new operation for intrapelvic tuberculotic strictures of the renal pelvis: J Urol, 1981; 126(6); 734-36
6. Li X, Liu ZJ, Liu JW, A clinical comparative analysis of retroperitoneal laparoscopic tuberculous nephrectomy and open tuberculous nephrectomy: J Laparoendosc Adv Surg Tech A, 2019; 29(7); 909-13
7. Campbell S, Uzzo RG, Allaf ME, Renal mass and localized renal cancer: AUA guideline: J Urol, 2017; 198(3); 520-29
8. Finelli A, Ismaila N, Russo P, Management of small renal masses: American Society of Clinical Oncology clinical practice guideline summary: J Oncol Pract, 2017; 13(4); 276-78
9. Muneer A, Macrae B, Krishnamoorthy S, Urogenital tuberculosis – epidemiology, pathogenesis and clinical features: Nat Rev Urol, 2019; 16(10); 573-98
10. Cek M, Lenk S, Naber KG, EAU guidelines for the management of genitourinary tuberculosis: Eur Urol, 2005; 48(3); 353-62
11. Fischer M, Flamm J, The value of surgical therapy in the treatment of urogenital tuberculosis: Urologe A, 1990; 29(5); 261-64
12. Ramanathan R, Kumar A, Kapoor R, Relief of urinary tract obstruction in tuberculosis to improve renal function. Analysis of predictive factors: Br J Urol, 1998; 81(2); 199-205
13. Wong SH, Lau WY, The surgical management of non-functioning tuberculous kidneys: J Urol, 1980; 124(2); 187-91
14. Puigvert A, Gittes RF, Partial nephrectomy in the solitary kidney. II. Experience with 20 cases of renal tuberculosis: J Urol, 1968; 100(3); 243-50
15. Hanley HG, Cavernotomy and paral nephrectomy in renl tuberculosis: Br J Urol, 1970; 42(6); 661-66
16. Zhang C, Cao J, Li XRing suture technique for renorrhaphy during partial nephrectomy in the management of renal hilar cancer: Zhonghua Wai Ke Za Zhi, 2015; 53(11); 852-55 [in Chinese]
In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952