04 May 2023: Clinical Research
Assessment of Periodontal Health Among Removable and Fixed Partial Denture Wearers in Aseer Region of Saudi Arabia
Asim Alsir Elmahdi1ABD, Mohamed Fadul A. ElagibDOI: 10.12659/MSM.940322
Med Sci Monit 2023; 29:e940322
Abstract
BACKGROUND: Prosthetic rehabilitation will have harmful effects on periodontal structure if the patient fails to maintain an oral hygiene protocol. This study aimed to evaluate oral hygiene in fixed and removable partial denture wearers in the Aseer Province of Saudi Arabia.
MATERIAL AND METHODS: This was a cross-sectional study done on 286 prosthesis wearers aged between 25 and 55 years; 142 were men and 144 women. Clinical examination was done using 3 periodontal parameters: plaque index, gingival index, and calculus surface index.
RESULTS: It was found that 72% and 25% of patients used fixed and removable partial prostheses, respectively. Most patients were in the 45-55 year age group (38.1%), were medically fit (78%), and used toothbrush and paste (70.6%). Most patients were instructed regarding the use of oral hygiene measures for their prostheses (71.3%). However, around half of the study group (52.8%) had odor from their prostheses. Most fixed prostheses were in the posterior teeth (73.2%) and had 3 units or more (58.7%). Removable partial dentures were mostly tooth-tissue supported (74%). A statistically significant difference was found for plaque index and gingival index between natural teeth and abutments in terms of various prosthetic parameters (P£0.001). The higher prevalence of gingival inflammation, plaque, and calculus accumulation in this study may be correlated to improper oral hygiene methods used by patients.
CONCLUSIONS: It can be concluded that there is a need to reinforce meticulous oral hygiene practices among patients using prosthodontic appliances.
Keywords: periodontal diseases, Saudi Arabia, Dental Prosthesis, Dental Prosthesis Design, Male, Humans, Female, Adult, Middle Aged, Cross-Sectional Studies, Toothbrushing, Denture, Partial, Fixed, Denture, Partial, Removable
Background
Prosthodontics is a branch of dental surgery that deals with the replacement of damaged and missing teeth. The word prosthodontics originates from 2 separate words “prostho,” which means to replace, and “dontist,” which means someone who deals with teeth. Prosthetic replacement of the missing teeth using fixed or removable partial dentures (RPD) to restore the function and esthetic of the oral cavity will have an insidious harmful effect if the patient does not meticulously follow oral hygiene procedures to preserve and prevent further deterioration of the complex and soft dental structure [1,2].
A fundamental concept of up-to-date dental prosthetics is for the applied prosthetic rehabilitation to enhance the structural and biological durability of oral health and to not induce any harmful effects to either the remaining natural teeth structure or the health of the dental periodontium. Many factors associated with prosthodontic treatment, such as a history of oral disease, age, and additional retentive areas, present prosthodontic patients with a risk of dental plaque accumulation.
Recall and maintenance visits for the patient wearing a removable or fixed partial denture is of great importance to prevent and treat any dental disease that can affect and compromise the life span of the abutment teeth and adjacent remaining natural teeth. Bidara et al [1] observed minimal evidence related to recall schedules in patients with removable and fixed partial prostheses. Zlataric et al [2] noted that the values obtained for the abutment teeth were significantly higher for all periodontal variables than the values obtained for non-abutment teeth. Momiaz et al [3], in their study evaluating the periodontal status of denture wearers in a rural Brazilian community, found that all denture wearers displayed periodontal problems in the sextant, where the denture was recorded. Do Amaral et al [4], after a longitudinal assessment over 12 months of the periodontal condition of the abutment and non-abutment teeth in patients with RPD, found that the abutment teeth showed higher values for probing depth, gingival recession, gingival inflammation, and plaque. Yeung et al [5] showed a higher prevalence of plaque, gingivitis, and gingival recession, especially on surfaces near the RPD elements. Correia et al [6] found that abutment teeth had higher values of all periodontal variables (
Periodontal and gingival indices for fixed partial denture abutment teeth are higher than those of non-abutment teeth. This problem is exaggerated with other factors such as patient age, duration of the prosthesis, and location of the crown margin. Al-Sinaidi and Preethanath [7] and Ayoub and Rashid [8] evaluated the periodontal status of abutment teeth compared with their respective teeth in another side of the arch, and reached the same conclusion regarding periodontal status and association with age of the patient, duration of prosthesis, and position of the finish margin. Periodontal status is linked to the presence or absence of an oral hygiene practice and pathogenic bacteria and increased specific inflammatory mediators, such as interleukins, prostaglandins, and C-reactive protein (CRP) [9]. It has also been found that these cytokines cause the upregulation of endothelin secretions (secreted by endothelial cells) after exposure to pathogenic bacteria and represent potential mediators of inflammation and vasoconstriction. [10]. Some studies have shown a correlation between high levels of nitrous oxide [10,11] and vitamin C with elevated levels of CRP and resultant endothelial damage in periodontitis patients [12,13].
Nevertheless, tooth decay, gingival inflammation, and periodontal disease are quoted as the most common biological complications of fixed prosthodontic appliances [14,15]. The risk of the periodontal problems and caries of the abutment teeth in a patient wearing a prosthodontic appliance is well known by every dental practitioner. However, there is currently less awareness about structured periodontal maintenance after RPD delivery [16]. The patient with a fixed partial denture has little awareness about the need for interdental brushes and floss to clean abutment teeth and pontics, owing to ignorance of their benefit and lack of instructions from their dentist concerning the maintenance of a fixed partial denture [17].
In 2018, AlQahtani discussed patient awareness and acceptance of dental implants as a treatment modality for replacement of missing teeth in the Aseer region of Saudi Arabia [18], while in 2023, Rownaq et al presented the assessment of current knowledge, awareness, and attitudes toward dental implants as a treatment option for replacement of missing teeth in the Riyadh region of Saudi Arabia [19]. However, there is no published data in the Aseer region of Saudi Arabia covering the conventional prosthetic replacement of missing teeth.
Therefore, the present study aimed to evaluate the oral hygiene level in 286 fixed prosthesis and removable partial denture wearers in the Aseer region of Saudi Arabia, and to develop a follow-up protocol to help patients maintain their prostheses, remaining teeth, and oral hygiene. The null hypothesis was that there was no difference in the oral hygiene levels of patients who used dental prostheses and those who did not use them in our community.
Material and Methods
ETHICS APPROVAL AND PATIENT CONSENT:
The Institutional Review Board and the Scientific Research Committee of the College of Dentistry of King Khalid University, Abha, Saudi Arabia, approved the study (IRB/REG/2019-2020/24). The study participants signed informed consent before the start of the study.
STUDY DESIGN:
The study was a prospective cross-sectional clinical survey conducted on 286 patients who wore prosthodontic appliances and attended the Diagnostic clinic at College of Dentistry, King Khalid University, Abha, Saudi Arabia, from May 2021 to November 2021. Those patients between the ages of 25 and 55 years were considered for further examination. Exclusion criteria included patients with any systemic conditions except diabetes mellitus, periodontal therapy in the last 6 months, systemic antibiotics within the last 3 months, and pregnancy and lactation.
PATIENT CHARACTERISTICS:
A detailed description of study patients’ characteristics was collected by using various parameters to understand the factors that may account for observed differences in prevalence of periodontal problems across studied parameters In this study, the following data were recorded: age (25–34, 35–44, and 45–55 years); sex (male or female); the presence of any previous medical history (no and yes); duration since prosthesis was used (Less than 1 year, 1 year, 2 years, and 3 years and more); oral hygiene habits (none, once daily, twice daily, and after every meal); method of oral hygiene (none, miswak, toothbrush and paste, and both); whether instructions were given by treating dentist for the hygiene of prosthesis (no and yes); use of oral hygiene aids to clean (no and yes); and odor from the prosthesis (no and yes). Details regarding prosthesis distribution based on various regions and units, periodontal status based on various characteristics of the prosthesis, and periodontal parameters of natural and retainer teeth in different types of prostheses were collected. Following this, the periodontal parameters of plaque index (PI), gingival index (GI), and calculus surface index (CSI) were recorded.
STATISTICAL ANALYSIS:
A subject-level analysis was performed for each of the parameters using the Statistical Package for the Social Sciences (SPSS) software for Windows, version 16.0 (IBM Corp, Armonk, NY, USA). Frequency and percentage were calculated as summary measures for condensing the raw data. A pairwise comparison using a paired-sample
Results
DEMOGRAPHIC CHARACTERISTICS OF PARTICIPANTS:
This study included 286 patients (142 men and 144 women) aged between 25 and 55 years old. Most patients were in the 45–55 year age group (38.1%) and had no medical history (78%). More than half of the patients (60.5%) gave a history of using the removable or fixed prosthesis for over 3 years. Oral hygiene habits varied among the patients, including a minor proportion (1.4%) that neglected it. However, most of these patients (70.6%) used toothbrush and paste. Most patients (71.3%) reported having been instructed regarding the use of oral hygiene measures for their prostheses. A total of 25% of patients used various oral hygiene aids (floss, tape) to clean their teeth and fixed prostheses. However, around half of the study group (52.8%) complained of odor from their prostheses (Table 1).
DISTRIBUTION OF PROSTHESES:
Table 2 shows the distribution of prostheses based on various regions and units. While 72% of patients used fixed prostheses and 25% used removable partial dentures, only 3% had both. Most of the fixed prostheses were in the posterior teeth (73.2%) and had 3 units or more (58.7%). Removable partial dentures were mostly tooth-tissue supported (74%).
PERIODONTAL STATUS BASED AROUND PROSTHESES:
Table 3 shows the periodontal status of patients using different types of prostheses. There was a statistically significant difference in the PI and CSI (P=0.026 and P=0.002, respectively) for different types of prostheses (fixed and removable). A difference was not observed for GI between different types of prostheses (P=0.230). Based on the fixed prosthesis location, PI (P=0.001) and GI (P=0.001) showed a statistically significant difference. However, no significant difference was found for CSI (P=0.407). PI (P=0.001), GI (P=0.001), and CSI (P=0.016) showed a statistically significant difference based on the number of fixed prosthesis units observed. Removable partial dentures, type of support, number of abutment teeth, and number of edentulous areas showed no statistically significant difference in periodontal parameters tested in this study.
COMPARISON OF PERIODONTAL PARAMETERS WITH DIFFERENT TYPES OF PROSTHESES:
Table 4 shows a comparison of periodontal parameters of natural and retainer teeth in different types of prostheses. A statistically significant difference was found for PI and GI between natural teeth and abutments (P≤0.001). Similarly, the comparison between the natural teeth and abutments for fixed partial dentures when the bridge was anterior, posterior, and a combination of anterior or posterior showed a statistically significant P value for all periodontal parameters. Several fixed prostheses, either for crowns or retainers for the bridge, when comparing natural and abutment teeth, showed statistically significant P values for both PI and GI (P≤0.001). CSI showed only a statistically significant value (P=0.03) with a bridge replacing a missing tooth or teeth.
COMPARISON OF PERIODONTAL PARAMETERS WITH REMOVABLE SUPPORT:
Table 5 shows a comparison of periodontal parameters of natural and abutment teeth according to removable support type. Periodontal parameters compared in the remaining natural teeth and abutment for tooth-supported and tooth-tissue-supported removable partial dentures showed a statistically significant difference for PI and GI (P≤0.001). In contrast, CSI showed a significant difference (P=0.023) with tooth-supported removable partial dentures only. Similarly, a comparison between natural teeth and abutment for removable partial dentures according to the number of edentulous areas showed a statistically significant difference (P≤0.001) in PI and GI but not for CSI. PI for the abutment teeth of removable partial dentures compared with that of remaining natural teeth showed a significant difference (P≤0.001) when the abutment teeth were located posteriorly. Compared with the GI of the remaining natural teeth, GI for abutment teeth of removable partial dentures was statistically significant wherever the abutment was positioned. CSI showed a significant difference when the abutment teeth were located anteriorly compared with the remaining natural teeth (P=0.034).
Discussion
This study was performed to evaluate the oral hygiene of the patients who had removable and fixed prostheses and compare 3 periodontal indices (PI, GI, and CSI) of the abutment teeth with those of the controlled non-abutment teeth. While a small group of patients in the present study stated that they were not instructed on oral hygiene methods for their prostheses by their treating dentist, most were instructed to use oral hygiene measures for their prostheses. This result agrees with that of the study by Al Qabba and Rayyan [20], in which a similar proportion (75%) of patients were instructed on a particular procedure of oral hygiene regarding their prostheses. Contrary to this, Almutairi [21] reported that only a small proportion of patients received instructions about cleaning the pontics and involved teeth of their fixed partial denture. A few among them failed to follow instructions.
The harmful effects of partial dentures in patients who did not maintain periodontal health through meticulous oral hygiene have been thoroughly discussed by many authors. It is apparent that there is a relationship between partial dentures and the accumulation of plaque [22]. Amaral et al recognized the association between periodontal damage of the teeth in a group with direct and indirect retainers compared with a control group [4]; the position and number of replaced missing teeth of fixed partial denture abutment in this study showed a statistically significant difference for PI and GI between the anterior and posterior teeth. Al-Sinaidi and Preethanath [7] reported a similar result and noted that the abutment teeth scored significantly higher PI, GI and probing pocket depth than non-abutment teeth (
The higher prevalence of gingival inflammation, plaque, and calculus accumulation in the present study group may be correlated with the improper oral hygiene methods used by the patients and lack of post-prosthetic instructions regarding methods and demonstrations of the cleansing of the prosthesis. This result is consistent with that of Geiballa et al [17], who reported inadequate post-prosthetic instructions regarding the fixed partial denture hygiene. Al Qabba and Rayyan [20] showed that most of their patients did not receive fixed denture oral hygiene instructions, while Harini et al [24] concluded that many patients (75%) did not use any interdental aids to clean their fixed partial dentures.
In the present study, the prevalence of gingival inflammation, plaque and calculus accumulation for abutment teeth of fixed partial dentures compared with that of adjacent natural remaining teeth showed statistically significant differences, except for the PI of the anterior abutment teeth. This may be explained by the visibility of the involved teeth and easy accessibility of the patient to remove debris. Periodontal parameters for removable partial dentures showed statistically significant differences according to abutment position, several edentulous areas, and support type. A similar finding was reported by Zlataric et al [2], Do Amaral et al [4], and Correia et al [6], who showed that the abutment teeth for removable partial dentures had a higher value in all periodontal variables when compared with adjacent non-abutment teeth. Yeung et al [5] found that the periodontal parameter of the periodontium is significantly affected in the abutment tooth’s side adjacent to removable partial denture elements by less than 3 mm. This result does not agree with results of other studies that reported no statistically significant difference in periodontal variables between the abutment teeth and non-abutment teeth in the oral cavity [25,26].
It is well documented that the control of gingival inflammation, plaque, and calculus accumulation can improve overall oral health. Comprehensive therapeutic methods, such as mechanical and chemical plaque control methods, including toothbrush, dentifrice, and mouthwash, are indicated to control dental plaque [27]. Oral hygiene measures cause improvement in gingival inflammation and in mucocutaneous lesions, such as lichen planus [28]. Furthermore, many studies have reported the association between bone diseases, periodontal pathogens, and periodontal diseases. Specific periodontal pathogens induce the activation of the immune response in our body, which in turn controls periodontal disease and related diseases, such as osteoporosis and rheumatoid arthritis [29].
It should be emphasized that periodontal disease is multifactorial in origin. Although plaque is the primary etiological factor causing this disease, the immune pathway’s altered response possibly modulates the body’s response toward pathogenic bacteria in the plaque [9]. Damage to the endothelium, which leads to activation of specific heat shock proteins and the resultant cross-reactive T cells, is a possible periodontal destructive mechanism. Some studies also show that in periodontitis, there is an imbalance in salivary nitrous oxide levels [30] and that inflamed periodontal tissues produce elevated levels of nitrous oxide against the periodontopathogens. Decreased vitamin C levels have also been found to have deleterious effects on endothelial dysfunction and altered immune response during the periodontal destructive pathway [9].
The present study was aimed to evaluate periodontal status in conventional prosthetic wearers in the Aseer region of Saudi Arabia. This study points out the need for developing a follow-up protocol to help patients maintain their prosthesis, remaining teeth, and oral hygiene. However, this study’s results should be interpreted with caution in terms of the removable prosthesis, as most patients had fixed prostheses. Future investigations would include details of medically compromised patients and a broader age group to increase generalizability results.
From the results of the present study, it is evident that oral hygiene and daily care was the main problem for the fixed and removable prosthodontic wearers. Therefore, emphasis should be on teaching our patients about proper oral hygiene methods and the use of dental floss for the remaining natural teeth and prosthesis before delivery. A regular follow-up protocol and recall visits specially designed for every prosthodontics patient to check his/her personal compliance with their specific instructions is recommended. We recommend conducting a more detailed study with a larger sample size, including dental implant patients, and using new updates to classify periodontal diseases and conditions.
Limitations were that the COVID-9 pandemic and lockdown delayed the start of the study, it was only a clinical examination for periodontal parameters, and no radiographic examination was carried out to evaluate the quality of bone and bone loss around the abutment teeth of prostheses. Another limitation was the small sample size, which may have affected the power of the study. Also, the cross-sectional design of the study limited our ability to relate the time pattern with the present periodontal status of the patients. We failed to include implant prostheses in our study; however, today, the use of implants is increasing exponentially for the replacement of missing teeth. We can incorporate implant prostheses in future studies. This study considered only clinical examination for periodontal parameters, and no radiographic examination was carried out to evaluate the quality of bone and bone loss around the abutment teeth.
Conclusions
The findings from the present study showed that there is a need for meticulous oral hygiene measures by patients with prosthodontic appliances. It should be emphasized that follow-up visits for the patient are equally essential to preserve and maintain their remaining natural teeth. Our results showed that, in our community, there indeed is a difference in the oral hygiene levels of the patients who used dental prosthesis and those who did not use them. Furthermore, awareness of the treating dentist regarding prosthodontics instruction and demonstration of oral hygiene aids indicated for the prosthodontics appliances are necessary.
Tables
Table 1. Demographic data of the patients.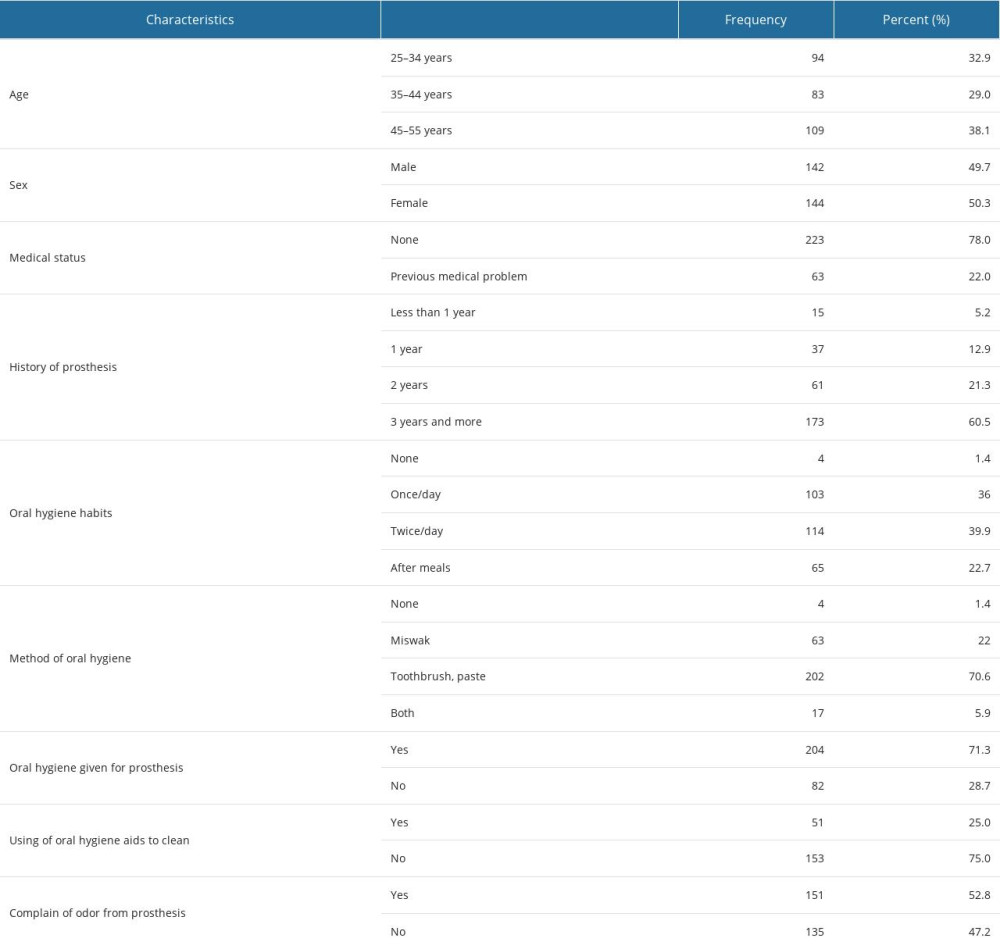 Table 2. Distribution of prostheses based on various regions and units.
Table 2. Distribution of prostheses based on various regions and units.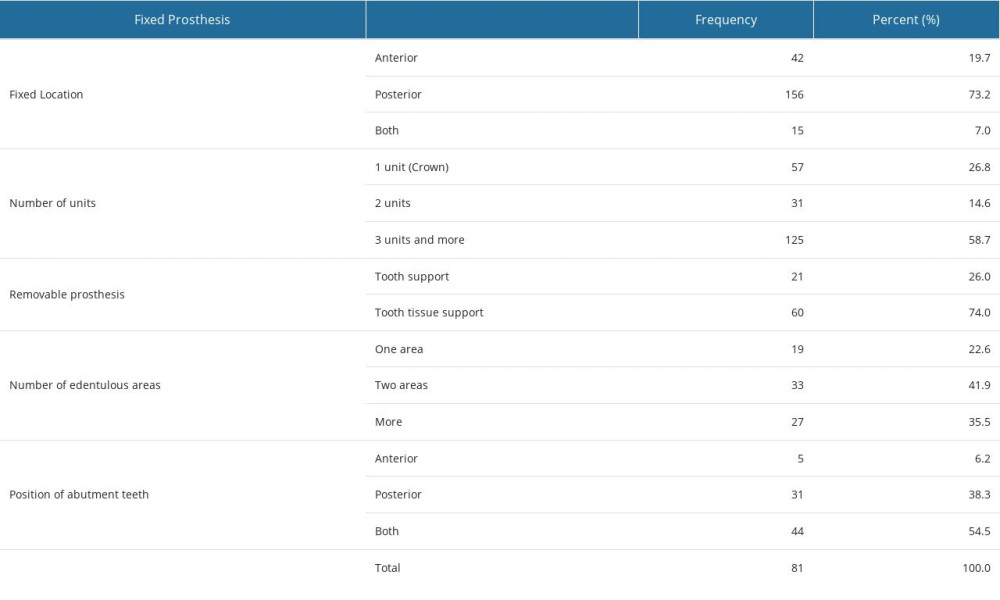 Table 3. Periodontal status based on various characteristics of prostheses.
Table 3. Periodontal status based on various characteristics of prostheses.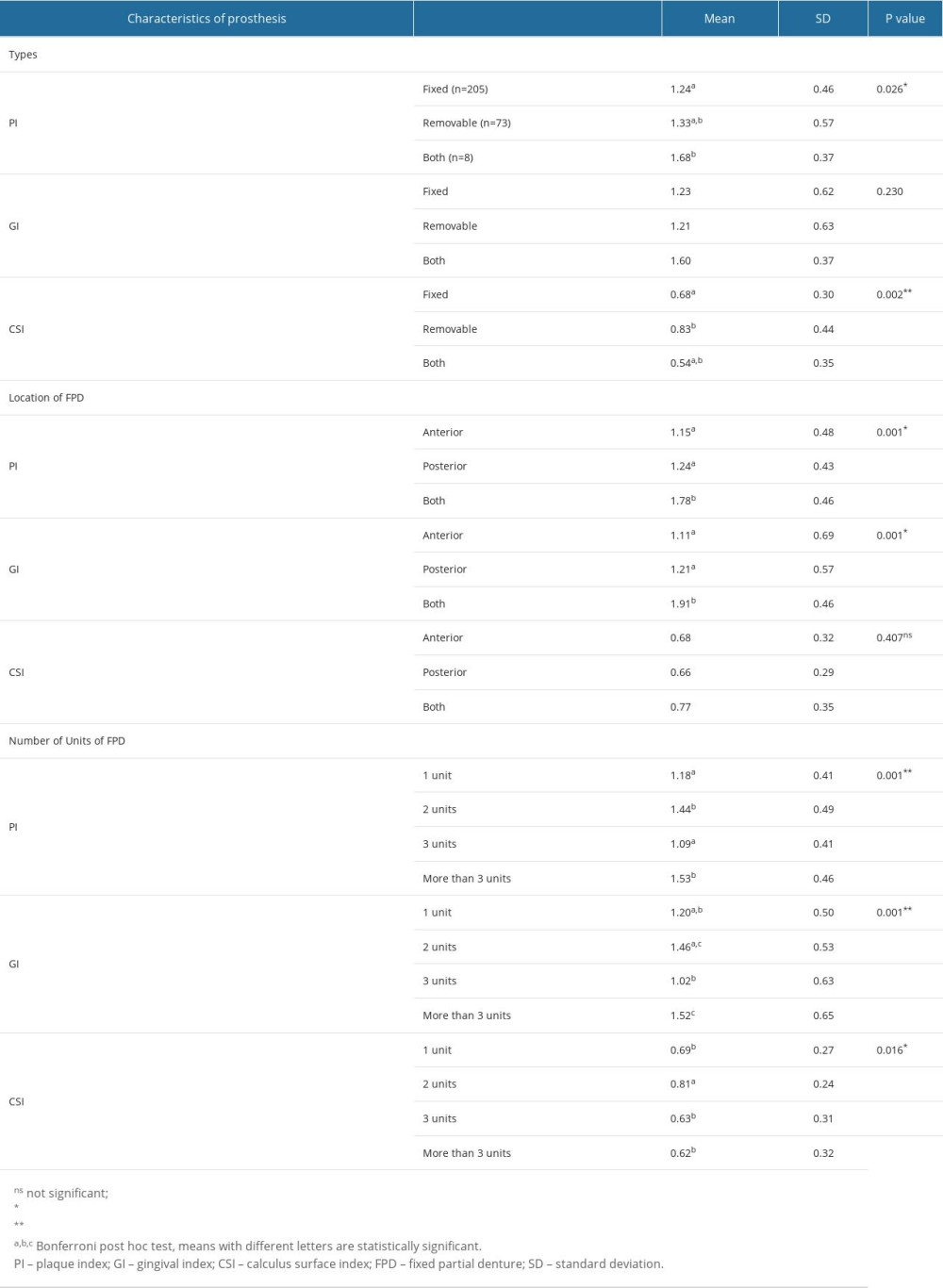 Table 4. Comparison of periodontal parameters of natural and retainer teeth in different types of prostheses.
Table 4. Comparison of periodontal parameters of natural and retainer teeth in different types of prostheses.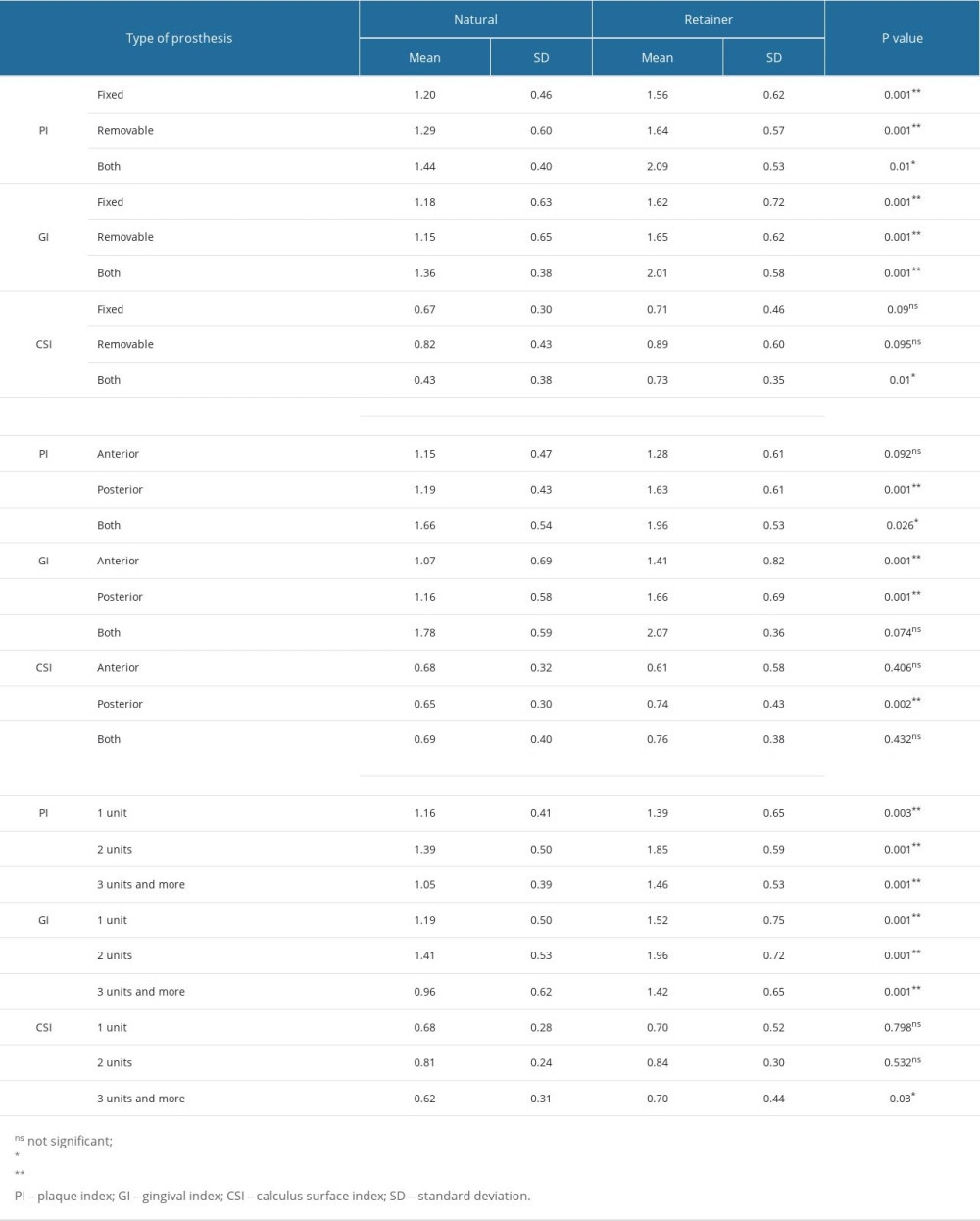 Table 5. Comparison of periodontal parameters of natural and abutment teeth according to removable support.
Table 5. Comparison of periodontal parameters of natural and abutment teeth according to removable support.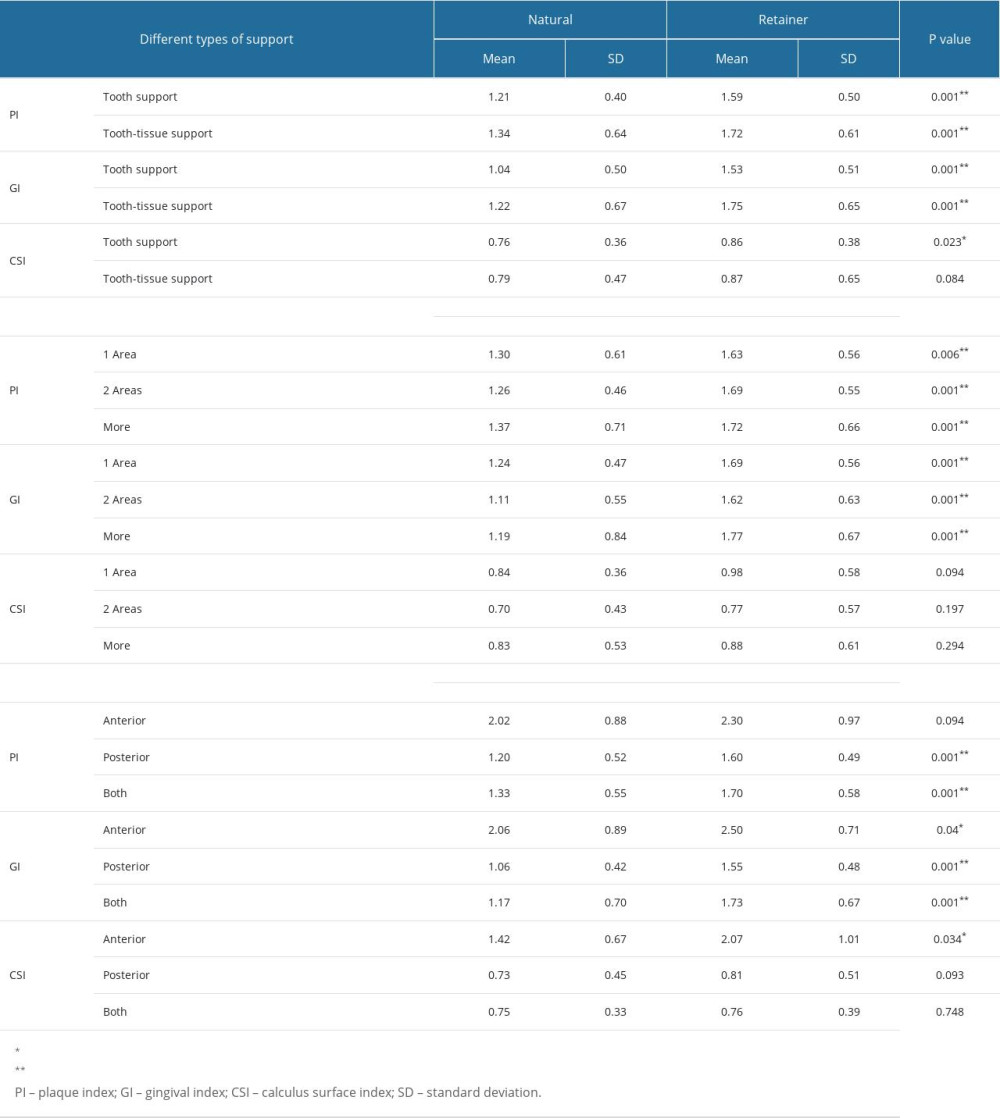
References
1. Bidra AS, Daubert DM, Garcia LT, A systematic review of the recall regimen and maintenance regimen of patients with dental restorations. Part 2: Implant-borne restorations: J Prosthodont, 2016; 25(S1); S16-31
2. Zlatarić DK, Čelebić A, Valentić-Peruzović M, The effect of removable partial dentures on periodontal health of abutment and non-abutment teeth: J Periodontol, 2002; 73(2); 137-44
3. Moimaz SA, Saliba NA, Saliba O, Association between dental prosthesis and periodontal disease in a rural Brazilian community: Braz J Oral Sci, 2006; 5(19); 1226-31
4. do Amaral BA, Barreto AO, Gomes Seabra E, A clinical follow-up study of the periodontal conditions of RPD abutment and non-abutment teeth: J Oral Rehabil, 2010; 37(7); 545-52
5. Yeung AL, Lo EC, Chow TW, Clark RK, Oral health status of patients 5–6 years after placement of cobalt-chromium removable partial dentures: J Oral Rehabil, 2000; 27(3); 183-89
6. Correia ARM, da Silva Lobo FD, Miranda MCP, Evaluation of the periodontal status of abutment teeth in removable partial dentures: Int J Periodontics Restorative Dent, 2018; 38(5); 755-60
7. Al-Sinaidi A, Preethanath RS, The effect of fixed partial dentures on periodontal status of abutment teeth: Saudi J Dent Res, 2014; 5(2); 104-8
8. Ayoub W, Rashid R, The effect of fixed partial dentures on periodontal status of abutment teeth: Int J Appl Dent Sci, 2017; 3(4); 103-6
9. Isola G, Polizzi A, Alibrandi A, Analysis of endothelin-1 concentrations in individuals with periodontitis: Sci Rep, 2020; 10(1); 1652
10. Amiri F, Virdis A, Neves MF, Endothelium-restricted overexpression of human endothelin-1 causes vascular remodeling and endothelial dysfunction: Circulation, 2004; 110(15); 2233-40
11. Toczewska J, Konopka T, Zalewska A, Nitrosative stress biomarkers in the non-stimulated and stimulated saliva, as well as gingival crevicular fluid of patients with periodontitis: Review and clinical study: Antioxidants, 2020; 9(3); 259
12. Mah E, Matos MD, Kawiecki D, Vitamin C status is related to proinflammatory responses and impaired vascular endothelial function in healthy, college-aged lean and obese men: J Am Diet Assoc, 2011; 111; 737-43
13. Nishida M, Grossi SG, Dunford RG, Dietary vitamin C and the risk for periodontal disease: J Periodontol, 2000; 71; 1215-23
14. Brägger U, Aeschlimann S, Bürgin W, Biological and technical complications and failures with fixed partial dentures (FPD) on implants and teeth after four to five years of function: Clin Oral Implants Res, 2001; 12(1); 26-34
15. Hämmerle CH, Ungerer MC, Fantoni PC, Long-term analysis of biologic and technical aspects of fixed partial dentures with cantilevers: International J Prosthodont, 2000; 13(5); 409-15
16. Milward P, Katechia D, Morgan MZ, Knowledge of removable partial denture wearers on denture hygiene: Br Dent J, 2013; 215(10); E20
17. Geiballa GH, Abubakr NH, Ibrahim YE, Patients’ satisfaction and maintenance of fixed partial denture: Eur J Dent, 2016; 10(2); 250
18. AlQahtani Saeed M, Awareness and acceptance of dental implants as a treatment modality for replacement of missing teeth among patients in Aseer Region, Kingdom of Saudi Arabia: Int J Oral Health Sci, 2018; 6(1); 58-64
19. Rownaq AM, Alzaidi TA, Yaqoub AR, Assessment of current knowledge, awareness and attitude towards dental implants as a treatment option for replacement of missing teeth in Riyadh, Saudi Arabia: Cureus, 2023; 15(1); e34189
20. AlQabbaa LM, Rayyan MR, Oral hygiene and maintenance habits among fixed partial denture wearers: Saudi J Oral Sci, 2018; 5(2); 115
21. Almutairi MN, Assessment of level of satisfaction and problems in patients treated with fixed partial denture in Alkharj City (Kingdom of Saudi Arabia), 2017; 3(5); 2454-9142
22. Devlin H, Replacement of missing molar teeth - a prosthodontic dilemma: Br Dent J, 1994; 176(1); 31-33
23. Edalia LG, Kassim BA, Oteino F, Complications associated with crowns and fixed partial denture provided to patients at teaching hospital: Int J Multidiscip Res Rev, 2017; 1(32); 19-24
24. Harini K, Ganapathy D, Visalakshi RM, Knowledge, attitude, and awareness on oral hygiene practice among patients wearing fixed partial denture: Drug Invent Today, 2019; 12(5); 1110-13
25. Vanzeveren C, D’Hoore W, Bercy P, Influence of removable partial denture on periodontal indices and microbiological status: J Oral Rehabil, 2002; 29(3); 232-39
26. Piwowarczyk A, Köhler KC, Bender R, Prognosis for abutment teeth of removable dentures: A retrospective study: J Prosthodont, 2007; 16(5); 377-82
27. Tandelilin RT, Jonarta AL, Widita E, The efficacy of anticalculus mouth rinse in moderate gingivitis patients with and without professional intervention: J Int Oral Health, 2018; 10(3); 148
28. Alsarraf A, Mehta K, Khzam N, The gingival oral lichen planus: A periodontal-oral medicine approach: Case Rep Dent, 2019; 2019; 4659134
29. Kanzaki H, Makihira S, Suzuki M, Soluble RANKL cleaved from activated lymphocytes by TNF-α-converting enzyme contributes to osteoclastogenesis in periodontitis: J Immunol, 2016; 197(10); 3871-83
30. Hampton TG, Amende I, Fong J, Basic FGF reduces stunning via a NOS2-dependent pathway in coronary-perfused mouse hearts: Am J Physiol Heart Circ Physiol, 2000; 279(1); H260-68
Tables
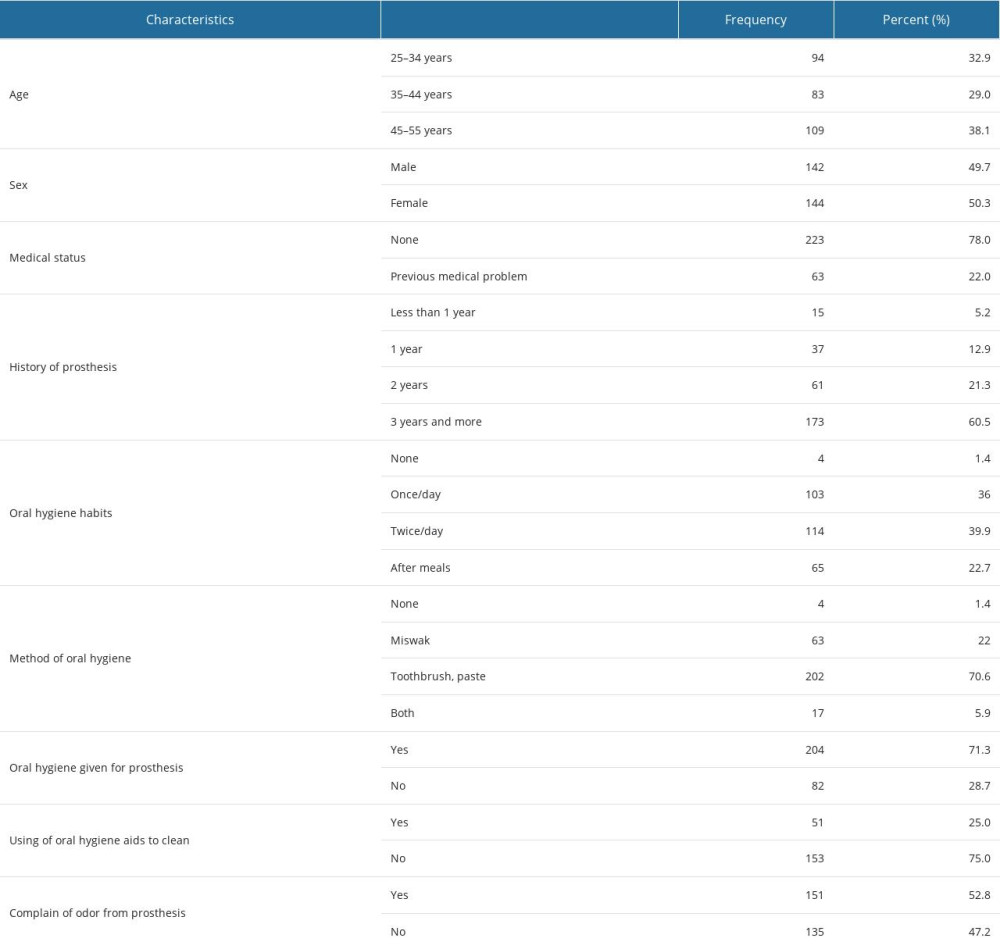 Table 1. Demographic data of the patients.
Table 1. Demographic data of the patients.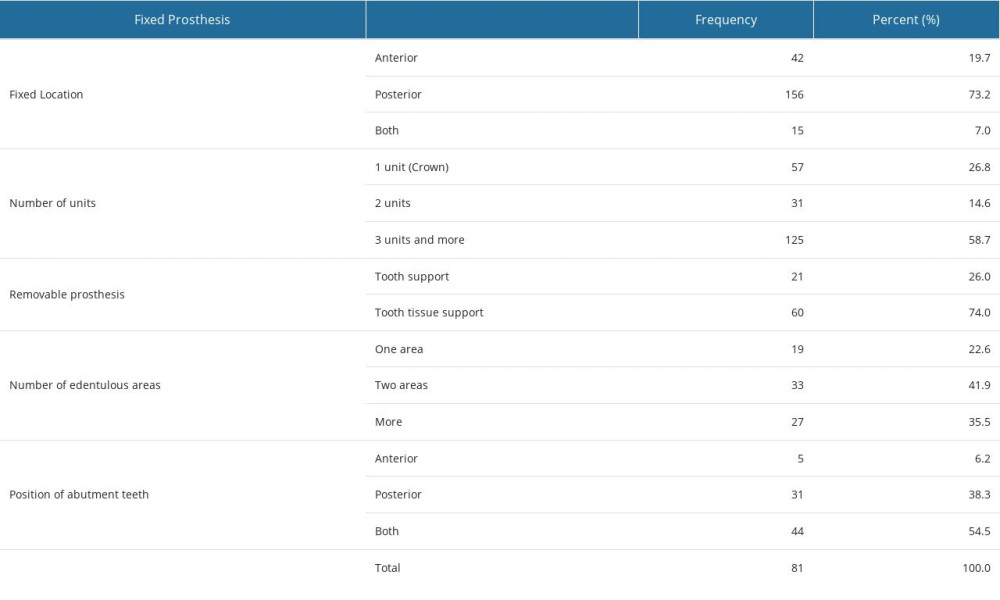 Table 2. Distribution of prostheses based on various regions and units.
Table 2. Distribution of prostheses based on various regions and units.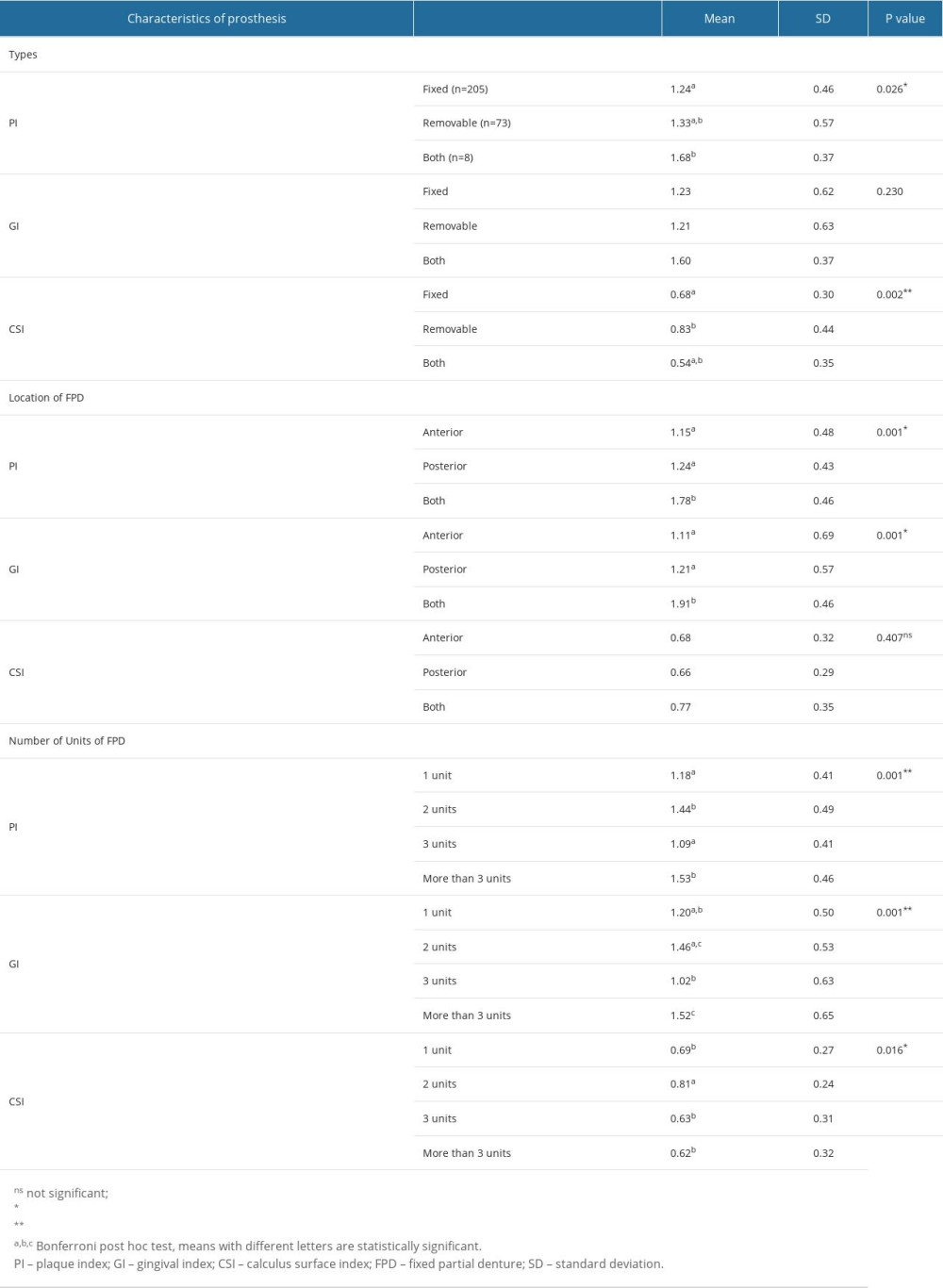 Table 3. Periodontal status based on various characteristics of prostheses.
Table 3. Periodontal status based on various characteristics of prostheses.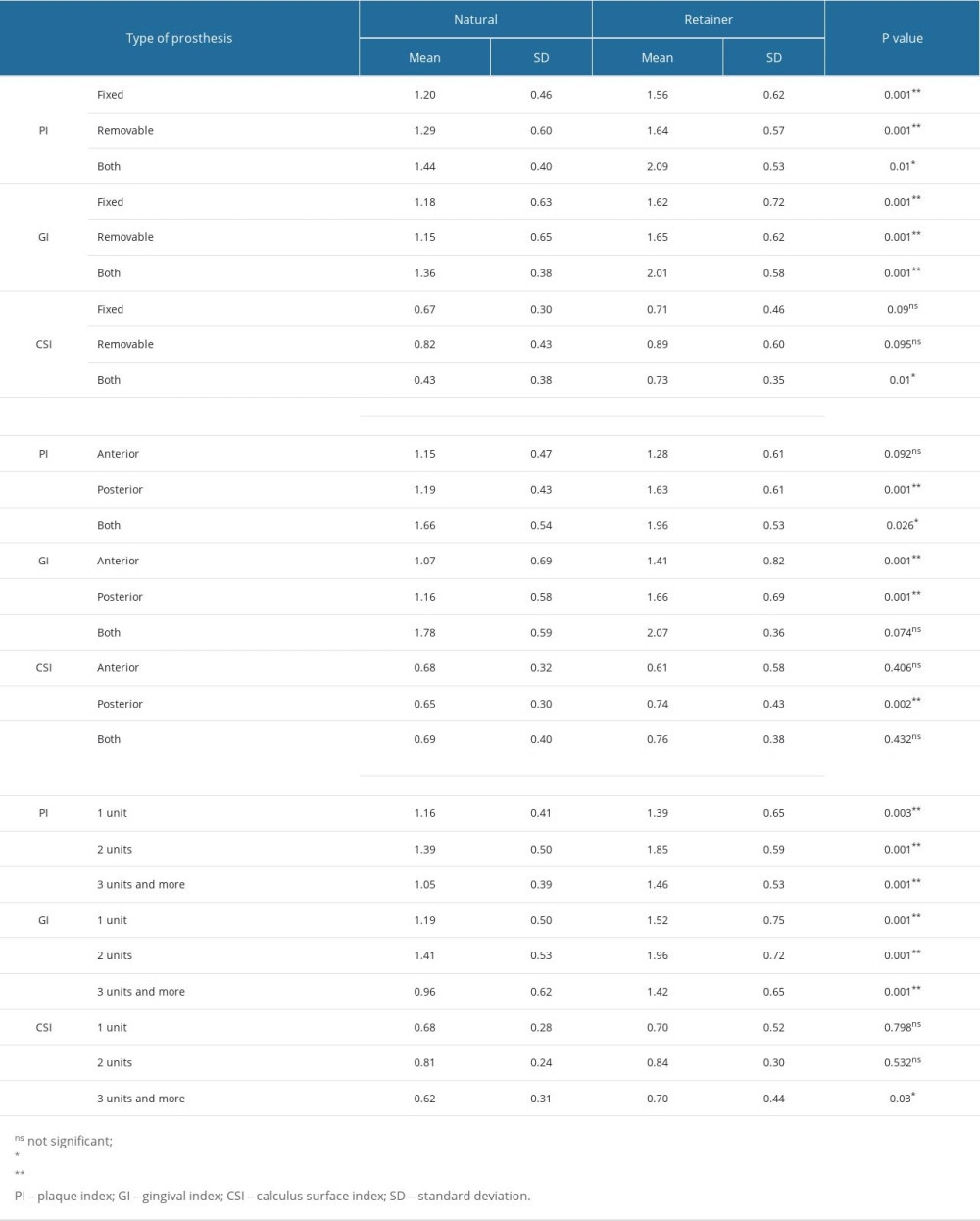 Table 4. Comparison of periodontal parameters of natural and retainer teeth in different types of prostheses.
Table 4. Comparison of periodontal parameters of natural and retainer teeth in different types of prostheses.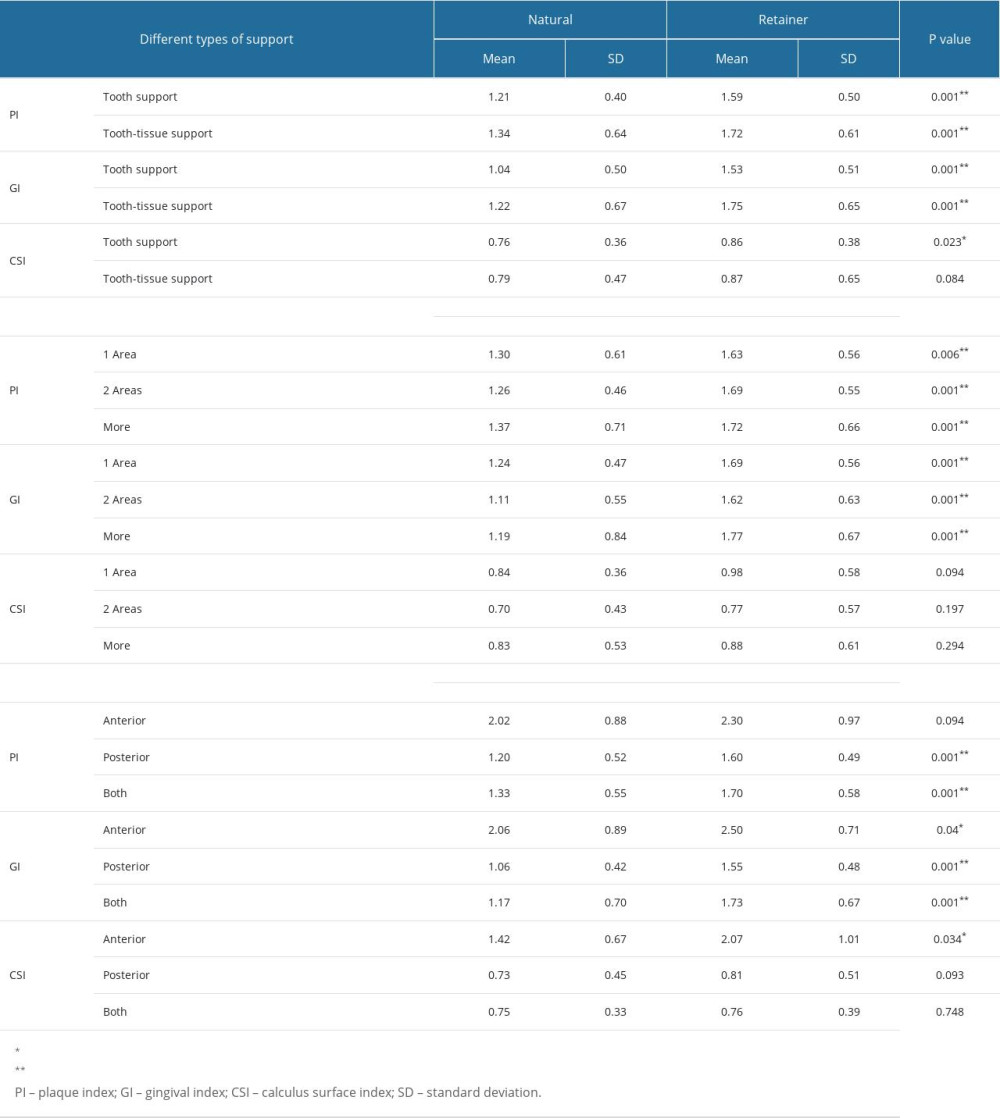 Table 5. Comparison of periodontal parameters of natural and abutment teeth according to removable support.
Table 5. Comparison of periodontal parameters of natural and abutment teeth according to removable support. In Press
06 Mar 2024 : Clinical Research
Prevalence and Variation of Medical Comorbidities in Oral Surgery Patients: A Retrospective Study at Jazan ...Med Sci Monit In Press; DOI: 10.12659/MSM.943884
08 Mar 2024 : Clinical Research
Evaluation of Foot Structure in Preschool Children Based on Body MassMed Sci Monit In Press; DOI: 10.12659/MSM.943765
15 Apr 2024 : Laboratory Research
The Role of Copper-Induced M2 Macrophage Polarization in Protecting Cartilage Matrix in OsteoarthritisMed Sci Monit In Press; DOI: 10.12659/MSM.943738
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








