04 July 2023: Clinical Research
Periapical Lesions and Missed Canals in Endodontically Treated Teeth: A Cone-Beam Computed Tomographic Study of a Chinese Subpopulation
Jing Hao1BCDEG, He Liu2ACDEF*, Ya Shen2DEFDOI: 10.12659/MSM.940533
Med Sci Monit 2023; 29:e940533
Abstract
BACKGROUND: Periapical lesions (PL) are a common complication of endodontically treated teeth (ETT), which can result from a missed canal (MC). This study aimed to assess the prevalence of PL and MC in the ETT of a Chinese subpopulation and investigate potential associations between them.
MATERIAL AND METHODS: A total of 561 cone-beam computed tomography images were selected and analyzed. A total of 1024 endodontically treated posterior teeth excluding third molars were evaluated for the presence of PL and MC. The chi-square test or Fisher’s exact test, as well as the odds ratio test, were used to determine whether there was an association and risk relationship between the incidence of PL and the occurrence of MC.
RESULTS: The overall prevalence of PL and MC in ETT was 56.1% and 19.0%, respectively. In endodontically treated molars, the incidence of PL and MC was 64.1% and 27.6%, whereas in premolars, it was 42.1% and 4.27%. The maxillary first molar showed the highest frequency of PL (71.5%) and MC (65.7%), with the mesiobuccal second canal being the most missed (78.8%). Teeth with an MC were found to be 3.658 times (95% confidence interval=2.541-5.301, P<0.0001) more likely to be associated with a PL.
CONCLUSIONS: Endodontically treated teeth with missed canals are associated with higher risks of periapical lesions. The high prevalence of these complications in a Chinese subpopulation underscores the importance of implementing enhanced diagnostic and treatment methods for root canal treatment or retreatment.
Keywords: Cone-Beam Computed Tomography, Endodontics, Periapical Periodontitis, Root Canal Therapy, Tooth, Nonvital, Humans, Dental Pulp Cavity, East Asian People, Molar, Tooth Root
Background
Post-treatment periapical lesions (PL) are commonly associated with unsuccessful endodontic treatment outcomes, either due to persistent infection in necrotic teeth or secondary infection in non-infected vital teeth [1]. A plethora of prognostic studies have attempted to identify potential risk factors that can impact the outcome of endodontic treatment [2–9]. These risk factors can be grouped into 3 categories: pre-operative factors (such as patient demographics and systemic health, tooth characteristics and root canal anatomy, diagnosis, and the presence of PL) [2–5]; intra-operative factors (such as the procedures used for chemomechanical preparation, the quality of root canal filling, the operator’s experience, skills, and protocol) [6–9]; and postoperative factors (such as the quality of the post-operative restoration) [7–9]. Among these factors, understanding complex tooth morphology and utilizing magnification and troughing are especially essential to avoid missing canals [9]. However, most of these studies have used 2-dimensional X-ray examination as the assessment tool or criteria to evaluate the periapical status and technical quality of the root-filled teeth. The limitations of using 2-dimensional radiographic images to assess the complex configurations and morphologies of the 3-dimensional root canal system are well-established [10].
In recent years, the use of cone-beam computed tomography (CBCT) in endodontics has become increasingly prevalent, proving to be a valuable tool for diagnosis, treatment planning, and assessment of treatment outcomes [10]. Studies have shown that endodontic outcome predictors identified using CBCT differ from those identified using periapical radiographs [11,12]. Additionally, CBCT has been found to be more sensitive and accurate than periapical radiographs in detecting PL and technical errors, such as deficiencies in the root canal filling [12–15]. Previous research has shown that CBCT can detect all PL that are visible during surgery [14]. In an animal study evaluating healing after apical surgery, CBCT results were consistent with histological results [15]. CBCT imaging is particularly helpful in identifying additional canals with complex anatomy. Failure to detect and treat these canals can result in infection and the formation of bacterial biofilms. These infections can host bacterial pathogens and eventually lead to complications such as the development of PL [16,17]. Several cross-sectional studies have utilized CBCT to evaluate the prevalence of PL and MC in endodontically treated teeth (ETT) and investigated their associations [18–23]. While these studies have been conducted in various populations, to the best of our knowledge, no such study has been published on a Chinese population.
Previous research has identified variations in tooth configurations between the Chinese population and other races [24]. Additionally, different regions and countries have varying treatment quality guidelines and standards [25–27]. Therefore, the aim of this study was to fill this gap in the literature and provide valuable insights into the prevalence and associations of these factors specifically in the Chinese population. The first objective of the study was to evaluate the prevalence of PL and MC in ETT of a Chinese population. The second objective was to investigate the potential association between MC and the incidence of PL. It is worth noting that this study is cross-sectional in nature and therefore does not provide any information regarding the failure rate.
Material and Methods
PARTICIPANTS:
This cross-sectional study was conducted in compliance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [28]. The protocol of this study was approved by the Medical Ethics Committee of Hangzhou Stomatology Hospital (Permit: 2022–12–02). Prior to CBCT imaging, informed consent was obtained from the participants. The CBCT images initially screened in this study were obtained from the archive of the Hangzhou Stomatology Hospital between January 2018 and December 2021, which were taken for reasons unrelated to this study, using an OP300–1 machine (KaVo Dental GmbH, Warthausen, Germany) with a 6×8 cm field of view and a voxel size of 0.2 mm. The selection of CBCT images and subsequent analysis of teeth were conducted using OnDemand3D Dental software (Cybermed, Seoul, Korea). The CBCT scans that contained at least 1 root-filled tooth were included in the study. Teeth that showed no indication of previous root canal treatment (RCT), which were determined by the lack of radiopaque filling material within the canal, inadequate imaging quality, and the presence of CBCT artifacts, were excluded from the analysis. Additionally, teeth that had undergone RCT were excluded if they had experienced marginal bone loss greater than 4 mm, had undergone previous endodontic surgery, exhibited fused roots, suffered from root fracture, or had significant external root resorption that altered the root anatomy [18–20].
SAMPLE SIZE CALCULATION:
The sample size was determined using G*Power 3.1 software (Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany), with an effect size of 0.3, a type I error rate of 0.05, a power of 0.8, and 1 degree of freedom. Based on these parameters from a previous study, a total sample size of 88 (ETT) was calculated [20]. Figure 1 shows the flow diagram on the selection of eligible participants and the conduction of the trial.
CBCT ANALYSIS:
The CBCT images were viewed in a black environment on a 19-inch LED monitor (ThinkVision™ LT1953; Lenovo, Beijing, China) with a resolution of 1440×900 pixels, a brightness of 250 nits, a contrast ratio of 1000: 1, and a response time of 5 ms. The axial, sagittal, and coronal images of each root were oriented with respect to vertical (canal orifice to apex) and horizontal (mesial to distal) reference lines that were parallel to the long axis of each canal. We first examined the axial views for any unfilled canal spaces, and then verified the observations by reviewing the sagittal and coronal views. Canals that were not filled and extended from the cementoenamel junction to the apex, including any canals that branched off from a main canal at the coronal, middle, or apical third, were regarded as MC [18–20]. A PL was identified through the detection of a disrupted lamina dura and a radiolucent area around the radiographic apex that was at least twice as wide as the periodontal ligament space [18–20]. Figure 2 shows CBCT images demonstrating PL and MC.
INTRA-EXAMINER REPRODUCIBILITY CONTROL:
All ETT included in this study were analyzed by an experienced endodontic expert on CBCT images. To calibrate the intra-examiner reliability, the analysis of 100 teeth was repeated for identification of PL and MC after an interval of 14 days. The results showed very good reliability, with an intra-class correlation coefficient of 0.919 for PL and 0.931 for MC.
STATISTICAL ANALYSIS:
Prism 9.0 software (GraphPad Software, Boston, MA, USA) was utilized to conduct the data analysis. The intra-class correlation coefficient was used to calibrate the intra-examiner reliability for the presence of MC and PL. The chi-square test or Fisher’s exact test was used to determine the associations between the incidence of PL and MC. Specifically, Fisher’s exact test was used if the sample size was less than 10. The odds ratio was calculated to assess the probability of a PL developing in a tooth or root with at least an MC, as opposed to in a root where all canals were treated.
Results
PREVALENCE OF PERIAPICAL LESIONS:
The prevalence of PL overall was found to be 56.1% (574/1024). There was slightly higher prevalence of PL in maxillary (288/511, 56.4%) than in mandibular posterior teeth (286/513, 55.8%). The highest prevalence of PL was observed in the maxillary first molars (123/172, 71.5%) and mandibular first molars (174/250, 69.6%), while the lowest prevalence was found in the mandibular first and second premolars, with rates of 38.8% (19/49) and 36.9% (38/103), respectively, as shown in Table 1.
PREVALENCE OF MISSED CANALS:
Among 1024 endodontically treated premolars and molars excluding third molars, 19.0% (195) had at least 1 MC. Maxillary first molars had the highest frequency of MC (65.7%, 113/172), followed by mandibular first molars (16.4%, 41/250), mandibular second molars (11.7%, 13/111), and maxillary second molars (10.3%, 12/116). The incidence of MC in mandibular and maxillary premolars was low, as shown in Table 1. The mesiobuccal (MB) roots of maxillary first molars were found to have the highest frequency of MC (63.4%, 109/172), with the mesiobuccal second (MB2) canals being the most often missed (78.8%, 104/132), as indicated in Table 2.
ASSOCIATIONS BETWEEN THE INCIDENCE OF PERIAPICAL LESIONS AND MISSED CANALS:
The presence of at least 1 MC in teeth was associated with a 3.658-fold increase in the likelihood of PL [95% confidence interval (CI)=2.541–5.301, P<0.0001], as indicated in Table 3. Specifically, maxillary first molars with MC were 3.957 times more likely to have PL (95% CI=2.004–7.682, P<0.0001). Moreover, the MB roots of maxillary first molars with MC were found to be 13.91 times more likely to have PL (95% CI=6.590–28.50, P<0.0001), as shown in Table 4.
Discussion
This cross-sectional study is the first to investigate PL and MC in ETT in a Chinese population. Assessing the prevalence of these issues is crucial for dental practitioners because it can provide valuable insights into the effectiveness of current endodontic treatment protocols and identify areas for improvement. Furthermore, investigating potential associations between these issues can help identify risk factors and inform treatment planning and management decisions to prevent or minimize their occurrence. The results of this study and previous research are summarized in Table 5, providing a valuable reference for clinicians and researchers in this field.
In the present study, we analyzed 1024 endodontically treated posterior teeth, excluding third molars, in a Chinese subpopulation and found a 19.0% prevalence of MC. This result is consistent with previous reports on the same tooth type from different populations, including Karabucak et al (23.1%) in a North American population, Mashyakhy et al (18%) in a Saudi Arabian population, Baruwa et al (17.0%) in a population from several regions, and Costa et al (17.0%) in a Brazilian population [18–21]. In their study, do Carmo et al reported the highest prevalence (53.6%) of MC in maxillary first and second molars in a population from the Southeast Region of Brazil, while Alnowailaty et al reported the lowest prevalence (12.47%) in a Saudi Arabian population [22,23]. The prevalence of MC in endodontically treated maxillary and mandibular premolars in the present study was 5.8% and 2.0%, respectively. These findings are similar to those reported by Costa et al (6.3% and 4.2%) and Baruwa et al (3.3% and 3.6%) [19–20]. Karabucak et al and Mashyakhy et al reported the two highest prevalence rates of MC in maxillary premolars (9.5% and 8.9%), while Alnowailaty et al reported the lowest prevalence (1.9%) [18,23]. The highest prevalence of MC in mandibular premolars was reported by Karabucak et al (10.7%), while Mashyakhy et al and Alnowailaty et al reported no MC in mandibular premolars [18,21,23].
Based on the present study and previous research, it is inconclusive whether there is a difference in the prevalence of MC between maxillary and mandibular premolars. Maxillary first premolars are more susceptible to a 2-rooted configuration, whereas maxillary second premolars and mandibular premolars are more commonly found with a single root [29–32]. Multi-rooted configurations, including 3-rooted configurations, have been reported in both maxillary and mandibular premolars [29–32]. These variations in root morphology may contribute to the complexity of the root canal system and increase the likelihood of MC. The high prevalence of MC in endodontically treated premolars reported by Karabucak et al highlights the importance of considering the anatomical complexity of premolars, which may not be fully captured in 2-dimensional periapical radiographs [18]. It is widely recognized in the dental profession that molars exhibit intricate root canal anatomy, which represents a significant obstacle for successful endodontic treatment [24,33]. The elaborate structure of these teeth enhances the probability of MC and persistent infections relative to other types of teeth [29,30]. Among posterior teeth that have undergone endodontic treatment in the present study, excluding third molars, the maxillary first molars had the highest frequency of MC (65.7%), which is consistent with findings from Baruwa et al (59.6%), do Carmo et al (55.2%), Costa et al (54.5%), Karabucak et al (44.2%), and Mashyakhy et al (40.6%) [18–22]. Alnowailaty et al reported that the incidence of MC was lowest in maxillary first molars, at 15.1%, whereas maxillary second molars had the highest incidence of MC, at 38.1% [23]. In the present study, the MB root of maxillary first molars was found to have the highest frequency of missed treated canals (63.4%), with the MB2 canal being the most often missed (78.8%), which has been confirmed by previous studies [18–21]. Despite variations in the prevalence of the MB2 canal across different regions and patient demographics, this study and previous research have reported a high incidence of missed MB2 canals, underscoring the importance for clinicians to assume that maxillary first molars typically have 4 canals. This highlights the need for skilled dental practitioners to effectively manage these complexities to achieve optimal treatment outcomes. To accomplish this, efforts should be made to demonstrate the presence or absence of the MB2 canal through the use of advanced 3-dimensional preoperative diagnosis and intraoperative navigation techniques, appropriate access cavity design to ensure direct access to the pulp chamber floor, and magnification and illumination tools to facilitate optimal visualization [9]. The use of a dental operating microscope is highly recommended to locate the MB2 canal during RCT or retreatment [34]. It has been reported that using a dental operating microscope and ultrasonic instruments together can detect a significantly greater number of MB2 canals than in cases in which no microscope was utilized [34].
Limited field-of-view CBCT imaging, which has a high resolution and low radiation dose, is the preferred method for imaging teeth with complex root canal systems and for non-surgical retreatment cases in which untreated canals are suspected [35,36]. Karabucak et al recommend using limited field-of-view CBCT prior to retreatment cases to identify any untreated canals [18]. However, a clinical study by Parker et al found that using CBCT alone had limited effectiveness in locating additional MB2 canals in maxillary molars and suggested the use of a dental operating microscope in conjunction with selective troughing and CBCT imaging [37]. Another study showed that directly accessing the tooth resulted in significantly more MB2 canals being found than using CBCT imaging alone [38]. Therefore, a preoperative CBCT scan may not be necessary for every patient but should be considered when a MB2 canal cannot be found clinically, as it can significantly increase the chances of locating it [38].
In this study, the prevalence of PL in endodontically treated posterior teeth excluding third molars was found to be 56.1%, which is consistent with previous studies by Karabucak et al (59.5%) on endodontically treated posterior teeth and Baruwa et al (55.5%) on all tooth types excluding third molars [18,20]. However, higher prevalence rates were reported by Costa et al (88%) on all tooth types, do Carmo et al (77.7%) on maxillary first and seconds molars, and Mashyakhy et al (74.5%) on posterior teeth excluding third molars, while the lowest was reported by Alnowailaty et al (15.84%) on posterior teeth excluding third molars [19,21–23]. The prevalence of PL increased to 79.0% in ETT with MC, making them 3.658 times more likely to be associated with PL than those without MC. The odds ratio noted in this study was consistent with previous research by Karabucak et al (4.38) and Baruwa et al (4.4) and do Carmo et al (2.57) but lower than the study by Costa et al (6.25) [18–20,22]. The presence of MC in multirooted molars is associated with a higher proportion of PL in individual roots. Among the roots of these molars, the MB root of the maxillary first molar is the most affected. When the MB root contains a missed MB2 canal, the prevalence of PL is significantly higher than that in the distobuccal and palatal roots of the same tooth. The above statement implies that overlooking the presence of the MB2 canal can significantly increase the likelihood of RCT failure. Our study’s findings are consistent with those of a retrospective CBCT study by Colakoglu et al that examined the potential associations between PL and missed MB2 canals [39]. The study revealed that endodontically treated maxillary molars with missed MB2 canals had a 5.5 times higher risk of PL than those without missed MB2 canals. Peña-Bengoa et al conducted a CBCT study to determine the prevalence of missed MB2 canals and PL in maxillary molars among a subpopulation in Chile [40]. The study found that 45.78% of endodontically treated molars had missed MB2 canals, and among them, 70% were associated with PL, a statistically significant higher percentage than those without missed MB2 canals. Such an untreated canal is linked to a higher incidence of PL compared to any other root, irrespective of the particular tooth involved. The results are consistent with previous research, which found that the occurrence of an untreated canal was the second most common reason for failure in all types of teeth and the leading cause of failure in molars [41]. MC can provide a breeding ground for primary bacterial infections or act as a location for secondary infections within the canal system. Following infection, the level and strength of bacteria can result in or sustain apical periodontitis, depending on whether they can infiltrate the surrounding periradicular tissues [1,16]. Thus, the strong associations between periapical pathologies and untreated canals underscores the importance of identifying and treating all canals to prevent RCT failure.
Discrepancies between the present and previously reported data may be due to variations in tooth configuration and root canal system, as well as differences in the quality and standards of RCT across various regions and races [25–27,29–32]. It has been reported that the percentage of maxillary first premolars with a 2-root configuration was 80.9% in Saudi Arabian, 61% in Brazilian, and 41.5% in Chinese populations [29]. A multicenter CBCT study revealed that the prevalence of the MB2 canal in maxillary first molars was 76.4% in the Chinese population, compared with a range of 48.0% to 97.6% of other races [24].
Compared with a longitudinal study, this cross-sectional study had a larger sample size design that helped to distribute errors evenly, resulting in more accurate results. Furthermore, this study was either more cost-effective or less prone to bias. Nevertheless, this study was subject to certain limitations. First, since it was a cross-sectional study, data collection and tooth evaluation were limited to a specific time and single observation period. This meant that it was impossible to ascertain whether PL were progressing or regressing after treatment. Second, information on RCT, such as the treatment standards, was not available, and many factors that could affect treatment were not considered. Historically in China, resinifying therapy was a popular method for treating teeth, which involved instrumenting root canals with stainless hand files and filling them with phenol-formaldehyde liquid. However, this technique is no longer considered the standard of treatment in modern endodontics, as it fails to provide sufficient cleaning, shaping, and filling of the root canal system. Additionally, CBCT images cannot determine if a root canal has been filled with phenol-formaldehyde liquid, resulting in some root canals treated with this technique being classified as missed canals in this study. Thus, the association between PL and MC could be established, but not the cause-effect relationship. Third, while CBCT has shown superior sensitivity and accuracy in detecting PL, it cannot determine the histologic nature of these lesions.
Conclusions
With the limitations of this study, it can be concluded that ETT with ML are associated with higher risks of PL. As such, clinicians must have a comprehensive understanding of root canal anatomy and configurations to avoid missing canals during treatment. The high prevalence of these complications in a Chinese population stresses the importance of implementing improved diagnostic and treatment approaches. Additionally, the strong associations between MC and PL underscores the critical need to identify and treat MC to attain the optimal treatment outcomes.
Figures
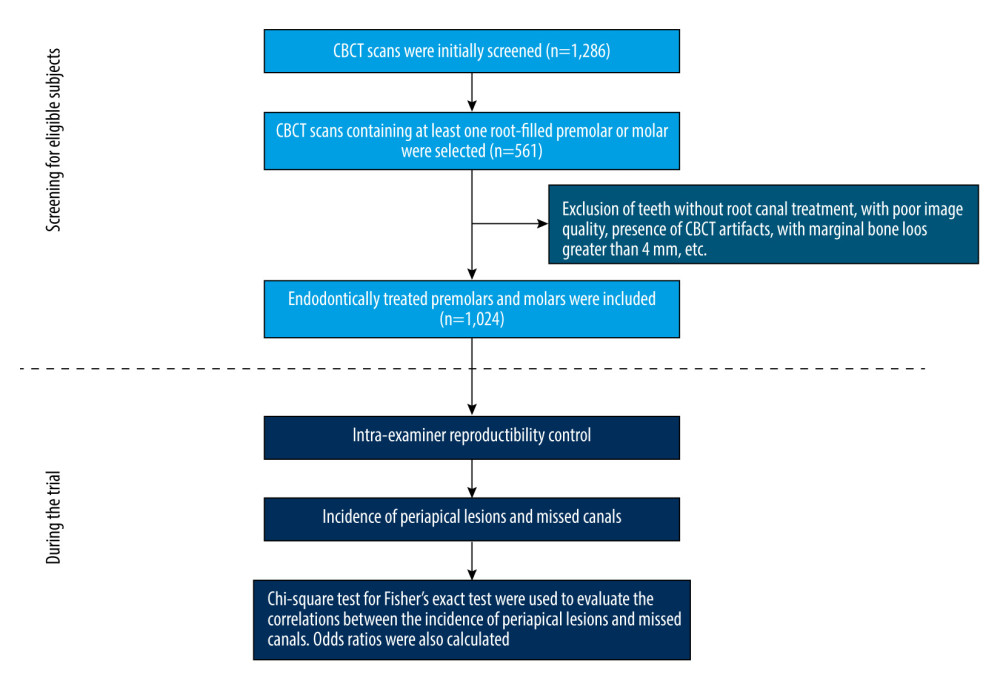 Figure 1. Flow diagram showing the selection of eligible subjects and the conduction of the trial. CBCT – cone-beam computed tomography. Prism 9.0 software (GraphPad Software, Boston, MA, USA) was used to create this figure.
Figure 1. Flow diagram showing the selection of eligible subjects and the conduction of the trial. CBCT – cone-beam computed tomography. Prism 9.0 software (GraphPad Software, Boston, MA, USA) was used to create this figure. 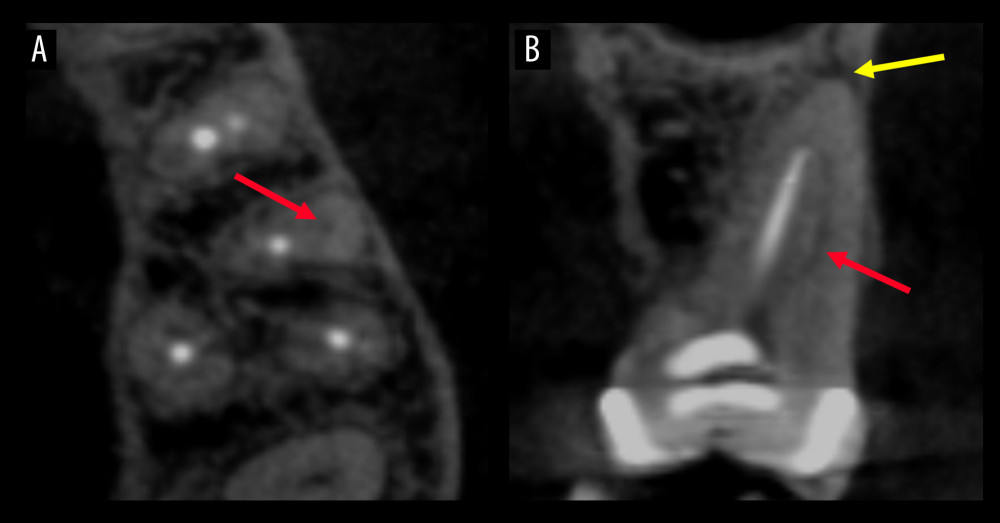 Figure 2. Cone-beam computed tomography images demonstrating a missed canal and a periapical lesion. The axial plane (A) and the coronal plane (B) of a maxillary first molar with an untreated mesiobuccal canal (indicated by red arrow) and periapical lesion (indicated by yellow arrow). OnDemand3D Dental software (Cybermed, Seoul, Korea) and Adobe Photoshop version 23.4.1 software (Adobe Inc., San Jose, CA, USA) were used to create this figure.
Figure 2. Cone-beam computed tomography images demonstrating a missed canal and a periapical lesion. The axial plane (A) and the coronal plane (B) of a maxillary first molar with an untreated mesiobuccal canal (indicated by red arrow) and periapical lesion (indicated by yellow arrow). OnDemand3D Dental software (Cybermed, Seoul, Korea) and Adobe Photoshop version 23.4.1 software (Adobe Inc., San Jose, CA, USA) were used to create this figure. Tables
Table 1. Periapical lesions and missed canals in endodontically treated posterior teeth excluding third molars.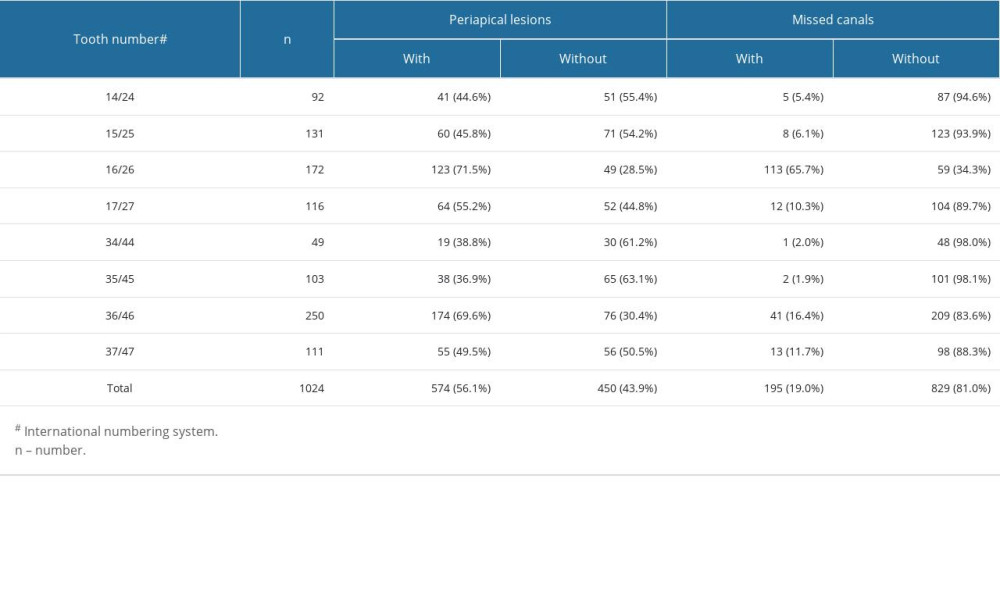 Table 2. Missed canals in maxillary first molars.
Table 2. Missed canals in maxillary first molars.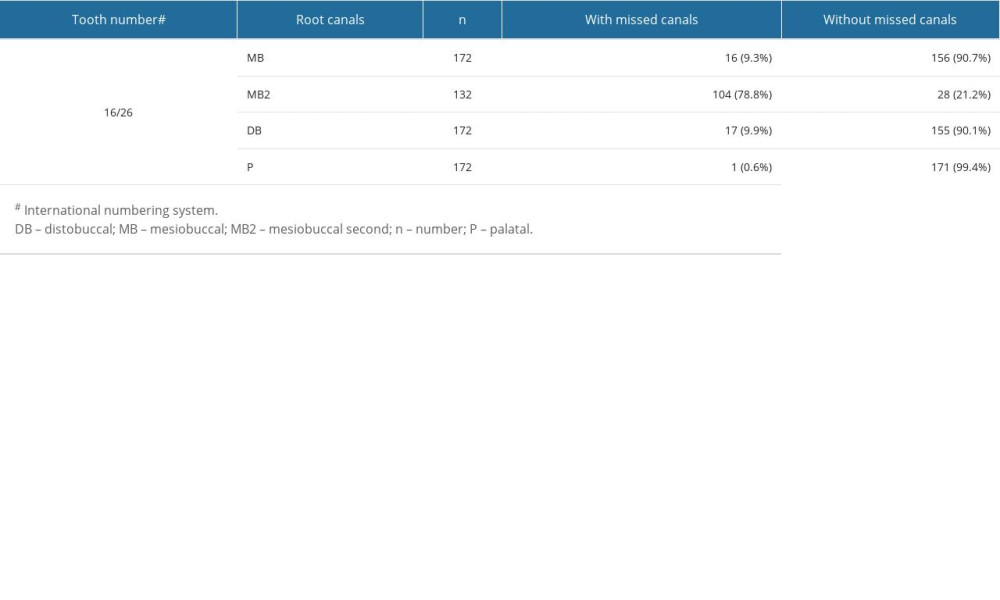 Table 3. Associations between the incidence of periapical lesions and missed canals.
Table 3. Associations between the incidence of periapical lesions and missed canals.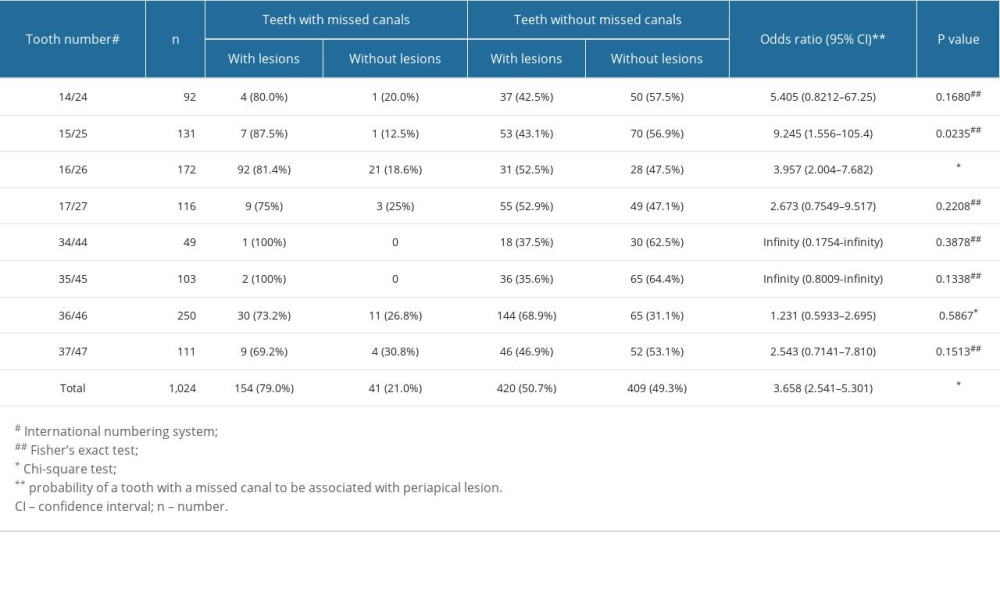 Table 4. Associations between missed canals and the incidence of periapical lesions in different roots of maxillary first molars.
Table 4. Associations between missed canals and the incidence of periapical lesions in different roots of maxillary first molars.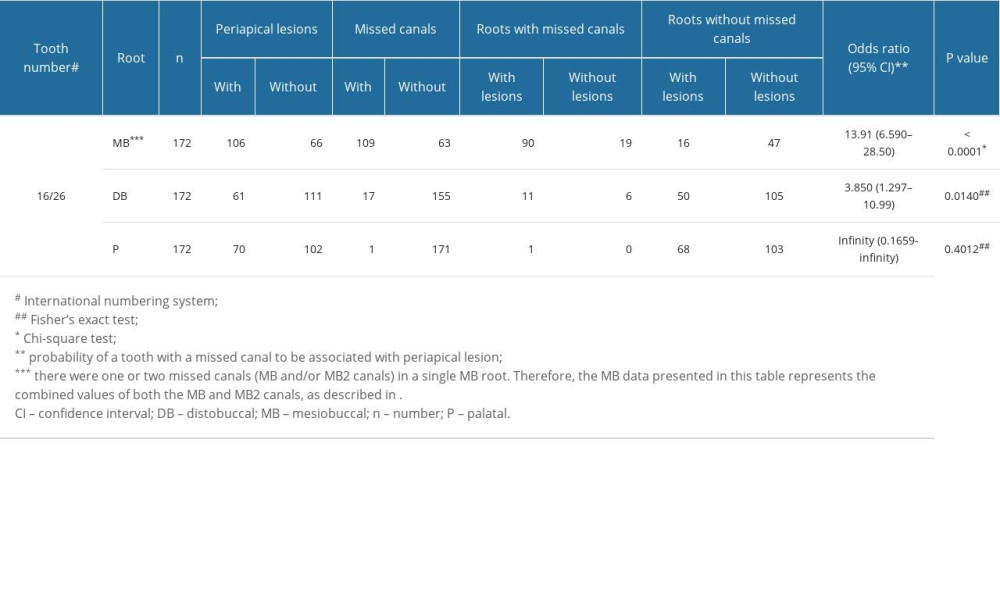 Table 5. A summary of results from previous research and the present study.
Table 5. A summary of results from previous research and the present study.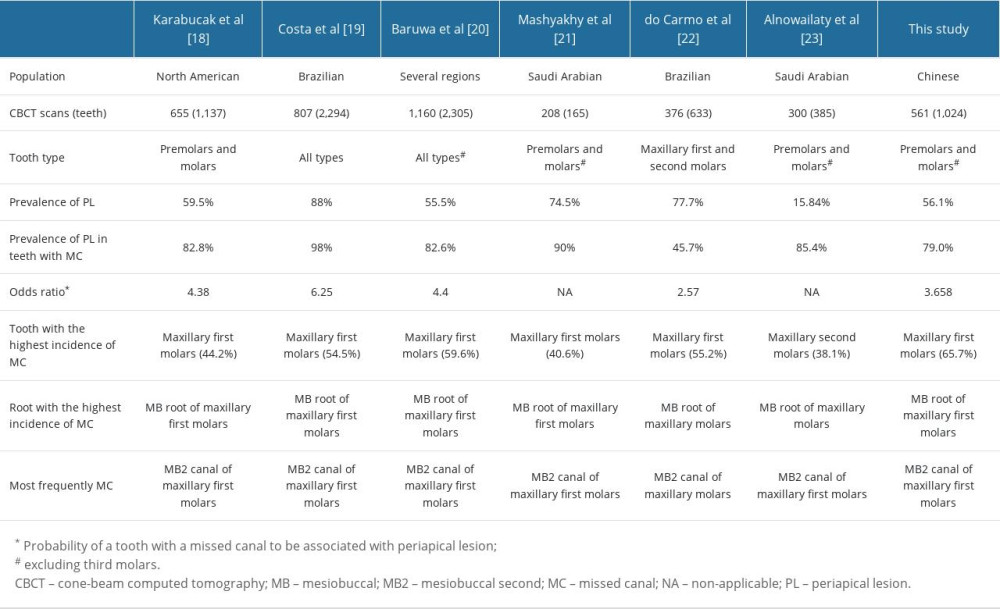
References
1. Haapasalo M, Shen Y, Ricucci D, Reasons for persistent and emerging post-treatment endodontic disease: Endod Topics, 2008; 18; 31-50
2. Bystrom A, Happonen RP, Sjogren U, Sundqvist G, Healing of periapical lesions of pulpless teeth after endodontic treatment with controlled asepsis: Endod Dent Traumatol, 1987; 3; 58-63
3. Ray HA, Trope M, Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration: Int Endod J, 1995; 28; 12-18
4. Chugal NM, Clive JM, Spångberg LS, A prognostic model for assessment of the outcome of endodontic treatment: Effect of biologic and diagnostic variables: Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2001; 91; 342-52
5. Chugal NM, Clive JM, Spångberg LS, Endodontic infection: Some biologic and treatment factors associated with outcome: Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2003; 96; 81-90
6. Cheung GS, Liu CS, A retrospective study of endodontic treatment outcome between nickel-titanium rotary and stainless steel hand filing techniques: J Endod, 2009; 35; 938-43
7. Ng YL, Mann V, Gulabivala K, A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: Part 1: Periapical health: Int Endod J, 2011; 44; 583-609
8. Ng YL, Mann V, Gulabivala K, A prospective study of the factors affecting outcomes of non-surgical root canal treatment: Part 2: Tooth survival: Int Endod J, 2011; 44; 610-25
9. Gulabivala K, Ng YL, Factors that affect the outcomes of root canal treatment and retreatment – a reframing of the principles: Int Endod J, 2023; 56(Suppl 2); 82-115
10. Patel S, Brown J, Pimentel T, Cone beam computed tomography in endodontics – a review of the literature: Int Endod J, 2019; 52; 1138-52
11. Liang YH, Li G, Wesselink PR, Wu MK, Endodontic outcome predictors identified with periapical radiographs and cone-beam computed tomography scans: J Endod, 2011; 37; 326-31
12. Fernández R, Cadavid D, Zapata SM, Impact of three radiographic methods in the outcome of nonsurgical endodontic treatment: A five-year follow-up: J Endod, 2013; 39; 1097-103
13. Patel S, Wilson R, Dawood A, Mannocci F, The detection of periapical pathosis using periapical radiography and cone beam computed tomography – part 1: Pre-operative status: Int Endod J, 2012; 45; 702-10
14. Velvart P, Hecker H, Tillinger G, Detection of the apical lesion and the mandibular canal in conventional radiography and computed tomography: Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2001; 92; 682-88
15. Chen I, Karabucak B, Wang C, Healing after root-end microsurgery by using mineral trioxide aggregate and a new calcium silicate-based bioceramic material as root-end filling materials in dogs: J Endod, 2015; 41; 389-99
16. Cantatore G, Berutti E, Castellucci A, Missed anatomy: frequency and clinical impact: Endod Topics, 2006; 15; 3-31
17. Li H, Liu H, Zhang L, Evaluation of extracellular polymeric substances matrix volume, surface roughness and bacterial adhesion property of oral biofilm: J Dent Sci, 2023 [in Press]
18. Karabucak B, Bunes A, Chehoud C, Kohli MR, Setzer F, Prevalence of apical periodontitis in endodontically treated premolars and molars with untreated canal: A cone-beam computed tomography study: J Endod, 2016; 42; 538-41
19. Costa FFNP, Pacheco-Yanes J, Siqueira JF, Association between missed canals and apical periodontitis: Int Endod J, 2019; 52; 400-6
20. Baruwa AO, Martins JNR, Meirinhos J, The influence of missed canals on the prevalence of periapical lesions in endodontically treated teeth: A cross-sectional study: J Endod, 2020; 46; 34-39
21. Mashyakhy M, Hadi FA, Alhazmi HA, Prevalence of missed canals and their association with apical periodontitis in posterior endodontically treated teeth: A CBCT study: Int J Dent, 2021; 2021; 9962429
22. do Carmo WD, Verner FS, Aguiar LM, Missed canals in endodontically treated maxillary molars of a Brazilian subpopulation: Prevalence and association with periapical lesion using cone-beam computed tomography: Clin Oral Investig, 2021; 25; 2317-23
23. Alnowailaty Y, Alghamdi F, Prevalence of endodontically treated premolars and molars with untreated canals and their association with apical periodontitis using cone-beam computed tomography: Cureus, 2022; 14; e25619
24. Martins JNR, Alkhawas MAM, Altaki Z, Worldwide analyses of maxillary first molar second mesiobuccal prevalence: A multicenter cone-beam computed tomographic study: J Endod, 2018; 44; 1641-49
25. Society of Cariology and Endodontology CS, Guidelines for Root Canal Therapy: Chin J Dent Res, 2015; 18; 213-16
26. European Society of Endodontology, Quality guidelines for endodontic treatment: Consensus report of the European Society of Endodontology: Int Endod J, 2006; 39; 921-30
27. Dahlkemper PE: American Association of Endodontists: Guide to clinical endodontics, 2016, Chicago, USA
28. Von Elm E, Altman DG, Egger M, The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies: Lancet, 2007; 370; 1453-57
29. Ahmad IA, Alenezi MA, Root and root canal morphology of maxillary first premolars: A literature review and clinical considerations: J Endod, 2016; 42; 861-72
30. Yan Y, Li J, Zhu H, CBCT evaluation of root canal morphology and anatomical relationship of root of maxillary second premolar to maxillary sinus in a western Chinese population: BMC Oral Health, 2021; 21; 358
31. Cleghorn BM, Christie WH, Dong CC, The root and root canal morphology of the human mandibular first premolar: A literature review: J Endod, 2007; 33; 509-16
32. Cleghorn BM, Christie WH, Dong CC, The root and root canal morphology of the human mandibular second premolar: A literature review: J Endod, 2007; 33; 1031-37
33. Cleghorn BM, Christie WH, Dong CC, Root and root canal morphology of the human permanent maxillary first molar: A literature review: J Endod, 2006; 32; 813-21
34. Alaçam T, Tinaz AC, Genç O, Kayaoglu G, Second mesiobuccal canal detection in maxillary first molars using microscopy and ultrasonics: Aust Endod J, 2008; 34; 106-9
35. AAE and AAOMR Joint Position Statement, Use of cone beam computed tomography in endodontics 2015 update: J Endod, 2015; 41; 1393-96
36. Patel S, Brown J, Semper M, Abella F, Mannocci F, European Society of Endodontology position statement: Use of cone beam computed tomography in Endodontics: European Society of Endodontology (ESE) developed by: Int Endod J, 2019; 52; 1675-78
37. Parker J, Mol A, Rivera EM, Tawil P, CBCT uses in clinical endodontics: The effect of CBCT on the ability to locate MB2 canals in maxillary molars: Int Endod J, 2017; 50; 1109-15
38. Hiebert BM, Abramovitch K, Rice D, Torabinejad M, Prevalence of second mesiobuccal canals in maxillary first molars detected using cone-beam computed tomography, direct occlusal access, and coronal plane grinding: J Endod, 2017; 43; 1711-15
39. Colakoglu G, Kaya Buyukbayram I, Elcin MA, Association between second mesiobuccal canal and apical periodontitis in retrospective cone-beam computed tomographic images: Aust Endod J, 2023; 49; 20-26
40. Peña-Bengoa F, Cáceres C, Niklander SE, Meléndez P, Association between second mesiobuccal missed canals and apical periodontitis in maxillary molars of a Chilean subpopulation: J Clin Exp Dent, 2023; 15; e173-76
41. Song M, Kim HC, Lee W, Kim E, Analysis of the cause of failure in nonsurgical endodontic treatment by microscopic inspection during endodontic microsurgery: J Endod, 2011; 37; 1516-19
Figures
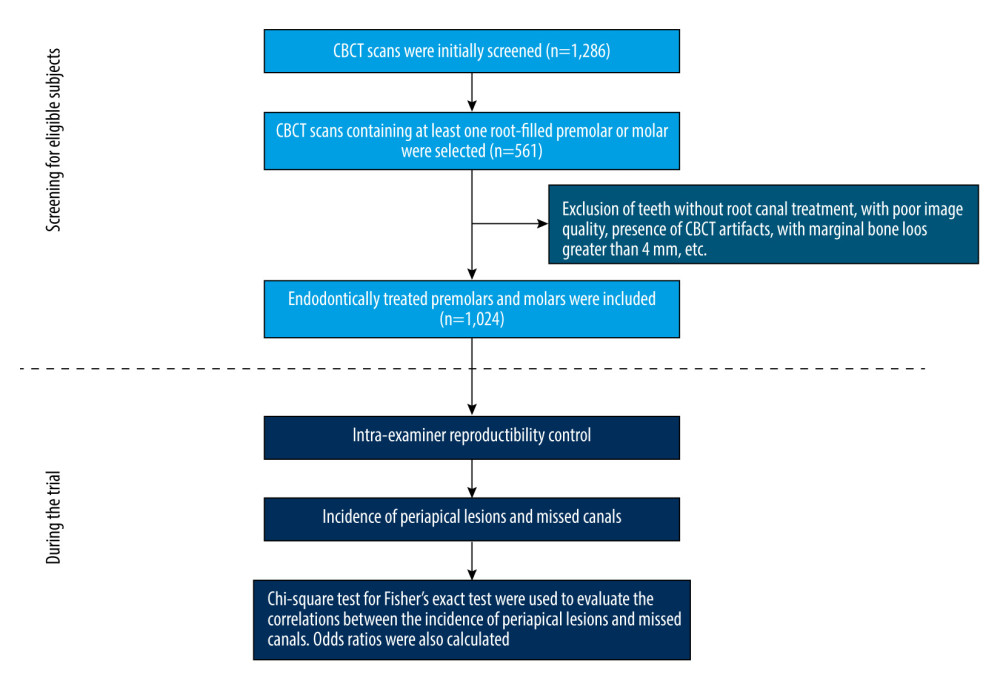 Figure 1. Flow diagram showing the selection of eligible subjects and the conduction of the trial. CBCT – cone-beam computed tomography. Prism 9.0 software (GraphPad Software, Boston, MA, USA) was used to create this figure.
Figure 1. Flow diagram showing the selection of eligible subjects and the conduction of the trial. CBCT – cone-beam computed tomography. Prism 9.0 software (GraphPad Software, Boston, MA, USA) was used to create this figure.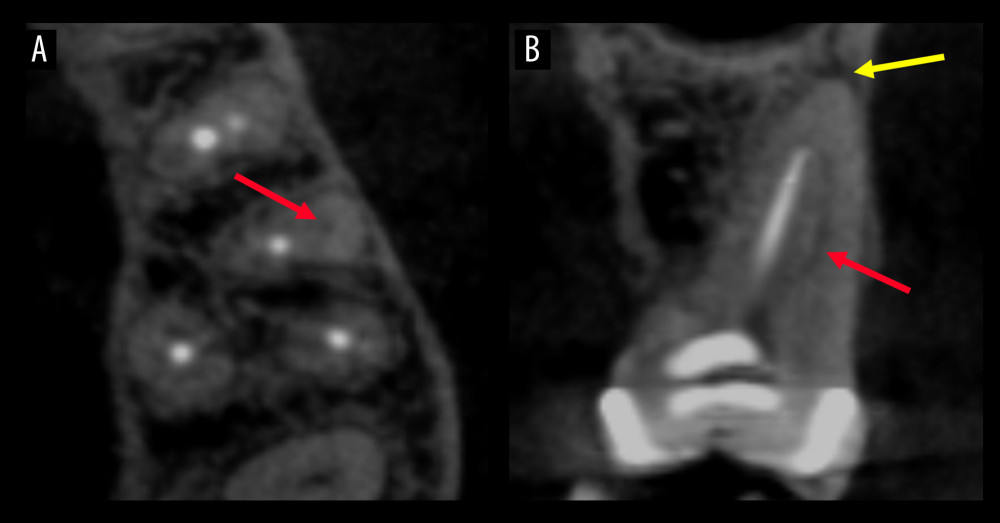 Figure 2. Cone-beam computed tomography images demonstrating a missed canal and a periapical lesion. The axial plane (A) and the coronal plane (B) of a maxillary first molar with an untreated mesiobuccal canal (indicated by red arrow) and periapical lesion (indicated by yellow arrow). OnDemand3D Dental software (Cybermed, Seoul, Korea) and Adobe Photoshop version 23.4.1 software (Adobe Inc., San Jose, CA, USA) were used to create this figure.
Figure 2. Cone-beam computed tomography images demonstrating a missed canal and a periapical lesion. The axial plane (A) and the coronal plane (B) of a maxillary first molar with an untreated mesiobuccal canal (indicated by red arrow) and periapical lesion (indicated by yellow arrow). OnDemand3D Dental software (Cybermed, Seoul, Korea) and Adobe Photoshop version 23.4.1 software (Adobe Inc., San Jose, CA, USA) were used to create this figure. Tables
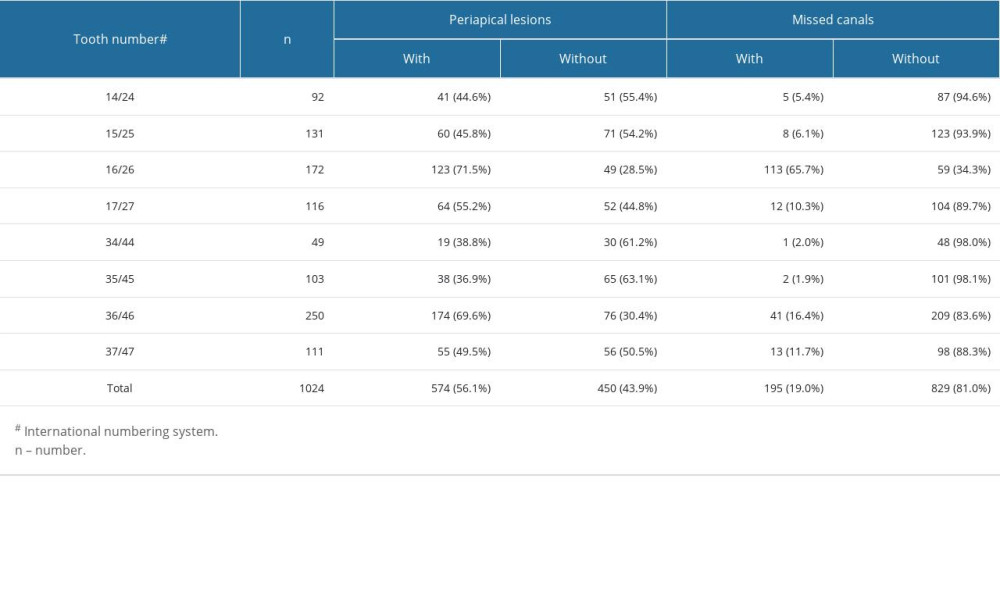 Table 1. Periapical lesions and missed canals in endodontically treated posterior teeth excluding third molars.
Table 1. Periapical lesions and missed canals in endodontically treated posterior teeth excluding third molars.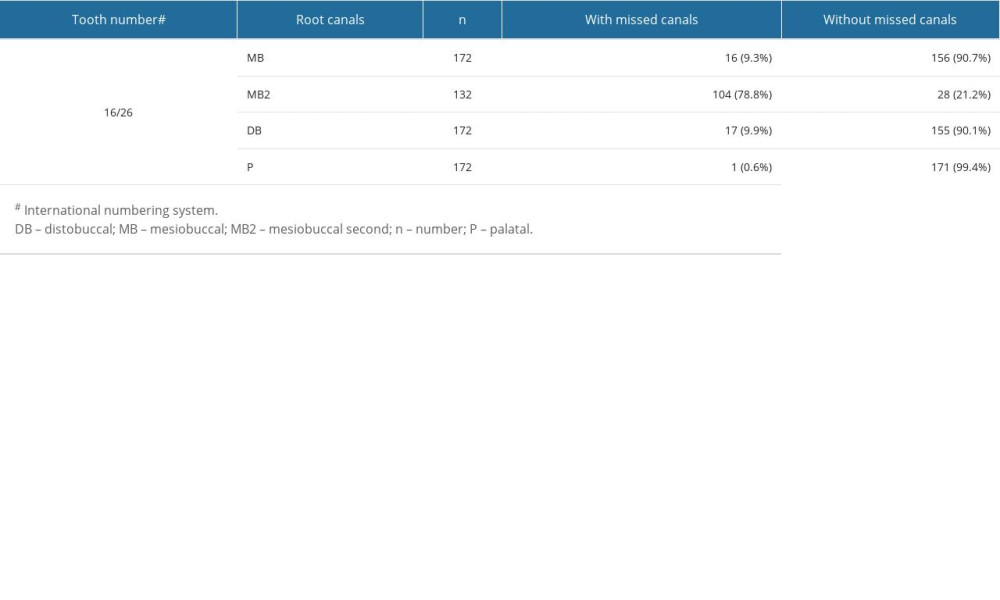 Table 2. Missed canals in maxillary first molars.
Table 2. Missed canals in maxillary first molars.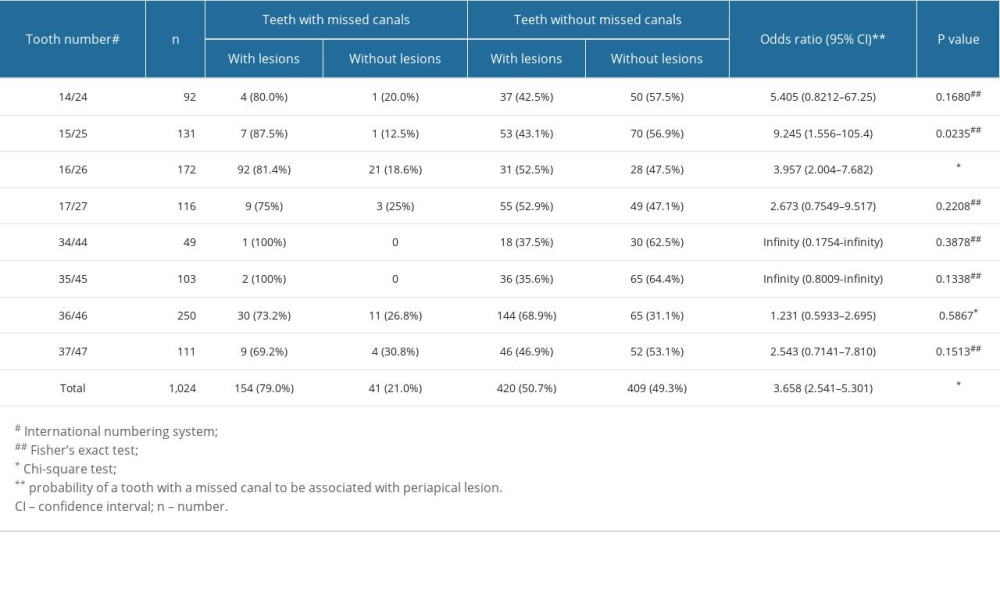 Table 3. Associations between the incidence of periapical lesions and missed canals.
Table 3. Associations between the incidence of periapical lesions and missed canals.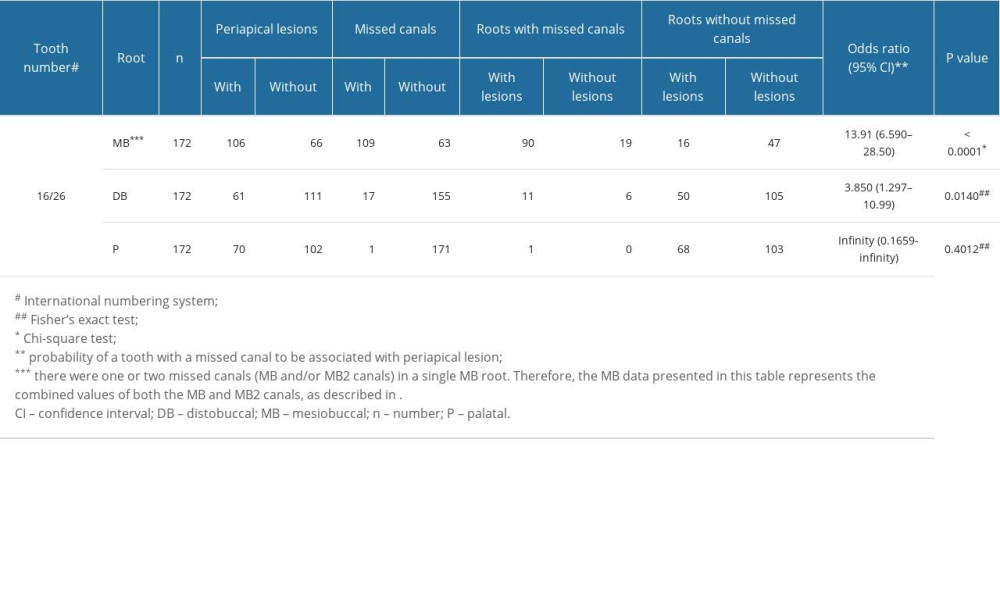 Table 4. Associations between missed canals and the incidence of periapical lesions in different roots of maxillary first molars.
Table 4. Associations between missed canals and the incidence of periapical lesions in different roots of maxillary first molars.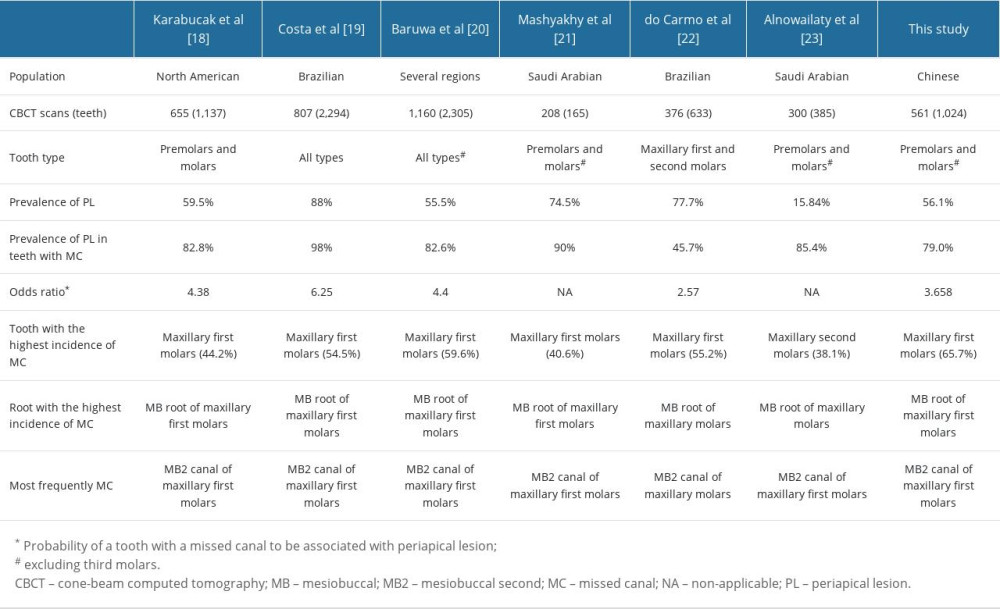 Table 5. A summary of results from previous research and the present study.
Table 5. A summary of results from previous research and the present study.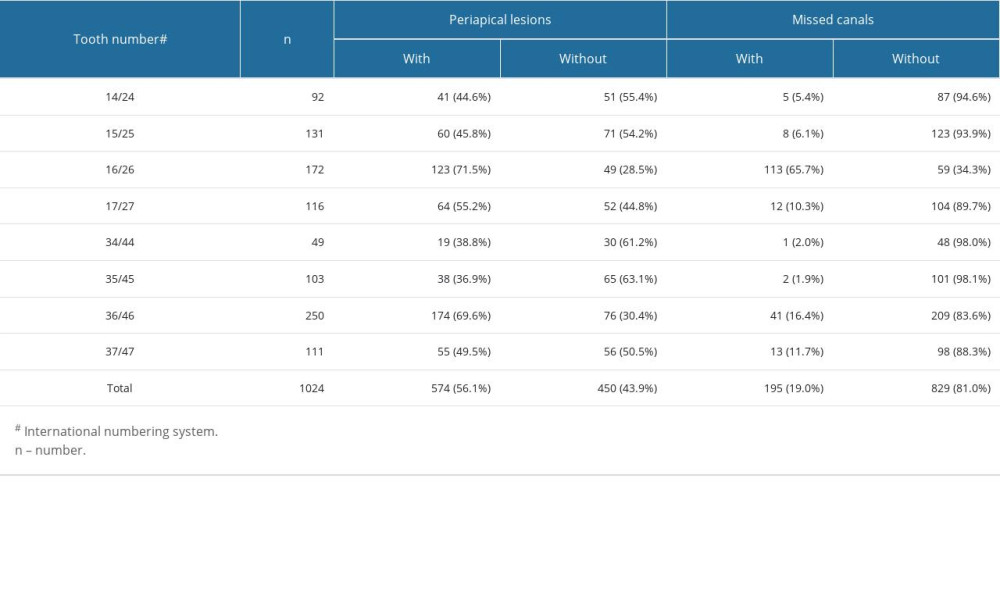 Table 1. Periapical lesions and missed canals in endodontically treated posterior teeth excluding third molars.
Table 1. Periapical lesions and missed canals in endodontically treated posterior teeth excluding third molars.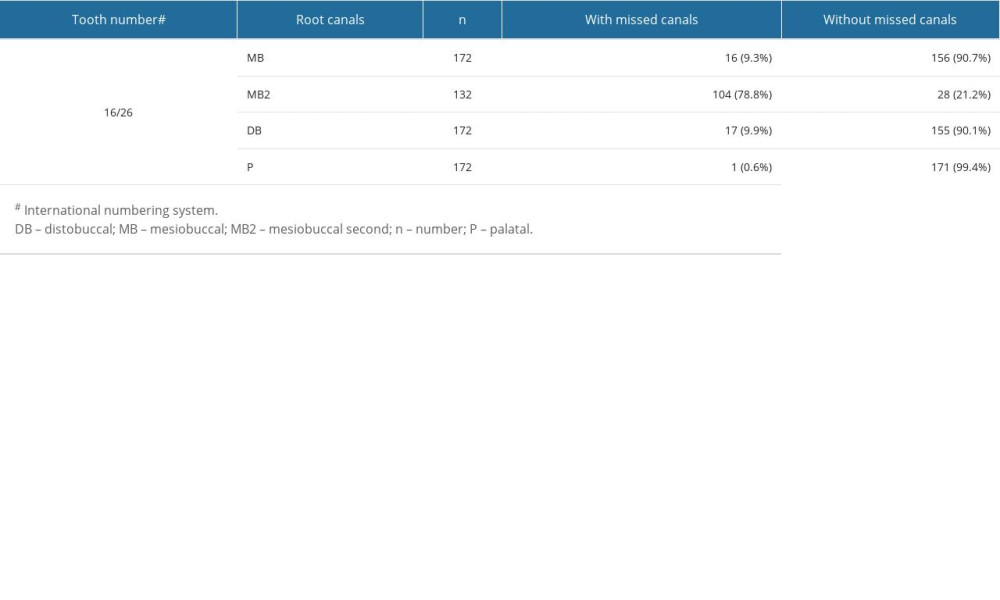 Table 2. Missed canals in maxillary first molars.
Table 2. Missed canals in maxillary first molars.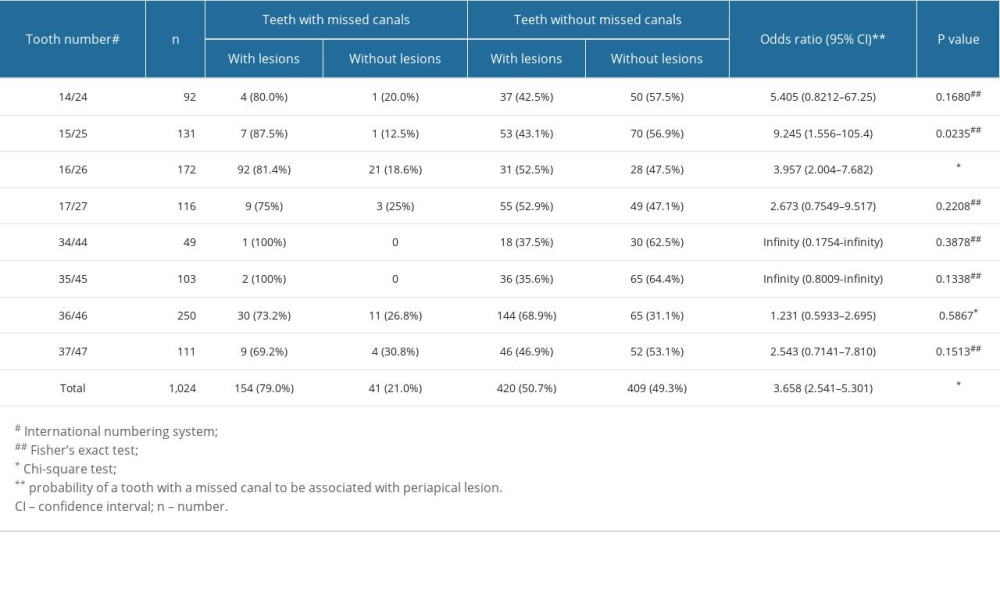 Table 3. Associations between the incidence of periapical lesions and missed canals.
Table 3. Associations between the incidence of periapical lesions and missed canals.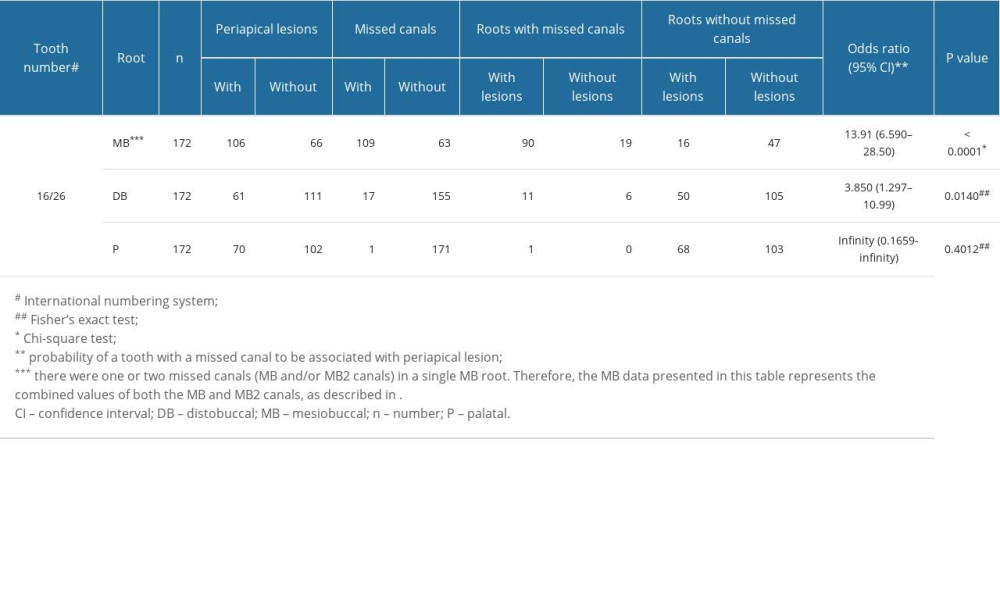 Table 4. Associations between missed canals and the incidence of periapical lesions in different roots of maxillary first molars.
Table 4. Associations between missed canals and the incidence of periapical lesions in different roots of maxillary first molars.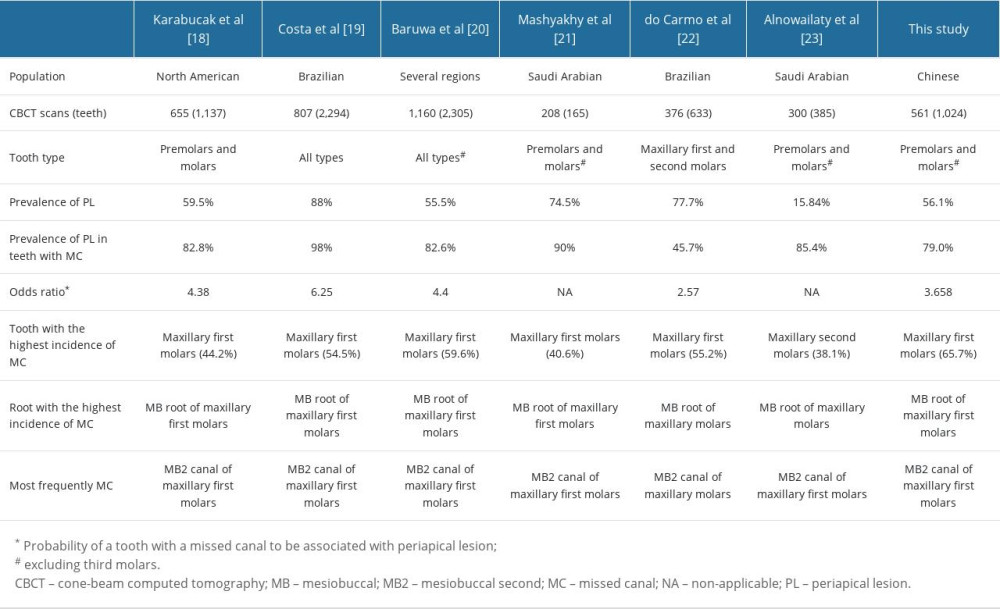 Table 5. A summary of results from previous research and the present study.
Table 5. A summary of results from previous research and the present study. In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








