18 August 2023: Clinical Research
Comparative Analysis of Mandibular and Cervical Mobility in Young Adults with Temporomandibular Joint Disorders: A Case-Control Study
Andżelina Wolan-NierodaDOI: 10.12659/MSM.940653
Med Sci Monit 2023; 29:e940653
Abstract
BACKGROUND: Temporomandibular joint disorders (TMJD) affect the muscles of the mandible or the temporomandibular joint (TMJ). The objective of this case-control study was to compare mandibular and cervical joint mobility in young adults diagnosed with TMJD to a healthy control group.
MATERIAL AND METHODS: We enrolled 60 participants aged 18-30 years, split evenly between 30 TMJD patients and 30 healthy controls. We employed a millimeter gauge to measure TMJ mobility and a tape-based tool for assessing the range of cervical mobility.
RESULTS: Our data revealed that TMJD patients exhibited a significantly reduced range of mobility in both the TMJ and cervical spine compared to controls. Controls demonstrated a greater mean cervical mobility through left and right lateral flexion movements (P<0.01 and P<0.05 respectively), as well as right and left rotations (P<0.05). Additionally, they showed significantly higher mandibular mobility across all tested parameters (P<0.001). Within the TMJD group, we observed a significant correlation between cervical and mandibular mobility (P<0.05).
CONCLUSIONS: Our findings underline that TMJD patients possess significantly diminished mandibular and cervical mobility, particularly in lateral movements and rotations, compared to those without the disorder. The observed correlation between cervical and mandibular mobility in the TMJD group implies the necessity to consider these interconnected aspects when designing rehabilitation programs, thereby enhancing patient quality of life and impeding further mobility deterioration.
Keywords: Cervical Atlas, Temporomandibular Joint Disorders, Range of Motion, Articular, Humans, young adult, Case-Control Studies, Quality of Life, Neck, Mandible
Background
Temporomandibular joint disorders (TMJD) involve the muscles of the jaw or the temporomandibular joint (TMJ). There are various causes of this problem, such as genetic factors, trauma, muscle dysfunction, stress, and uneven bite [1–3].
Reduced mobility of the cervical spine and mandible can adversely affect daily activities such as eating, speaking, or laughing [4–6]. Earlier studies have shown an association between TMJD and limitations in mobility of the cervical spine, suggesting that disorders in one area may affect the other [7,8].
The exact cause of TMJD can frequently be linked to multiple factors such as injury to the jaw, teeth grinding or clenching, joint degeneration, and stress leading to increased muscle tension. Other contributing factors may include malocclusion, systemic diseases such as rheumatoid arthritis and genetic predispositions [9].
The process of diagnosing TMJD can be difficult because of the various symptoms and the lack of a standardized diagnostic protocol. The evaluation typically takes into account the patient’s detailed medical history, a physical examination of the head, neck, and TMJ area, and an assessment of the patient’s occlusion [3]. Imaging techniques such as X-rays, magnetic resonance imaging (MRI), and computed tomography (CT) can be used to further examine the joints and surrounding structures. In some cases, additional diagnostic tools may be used, such as surface electromyography (sEMG) or joint vibration analysis (JVA) [10].
The management and treatment of TMJD depends on the specific cause, the severity of the symptoms, and the individual needs of the patient. Management of TMJD comprises the following aspects: patient education and self-care, as well as advice related to correct posture, coping with stress, and avoiding activities that exacerbate TMJD symptoms [9]. Treatment of TMJD includes pharmacological interventions and, most importantly, physiotherapy, which includes exercises and manual techniques to improve mandible function and reduce pain. Additionally, the treatment is often supplemented with oral appliances such as occlusal stabilization splints or guards to help reduce teeth grinding and clenching, as well as decrease muscle tension [11]. Surgical intervention can be considered if conservative treatment does not provide relief [12].
The literature related to TMJD presents a number of methods enabling assessment of TMJ mobility and range of cervical mobility, including highly precise techniques involving the use of advanced equipment [13,14] and more subjective methods without use of such instruments [15–25]. The purpose of the present study was to assess and compare the range of TMJ mobility and cervical mobility using simple and easily accessible tools such as a millimeter gauge and a centimeter tape. The current study focused on the functional, rather than structural, assessment of these areas, due to which the authors used methods that are inexpensive, do not require a lot of time and instruments, and are commonly used both in clinical practice and in research, as shown by numerous scientific reports [15–25]. The methods used in the study have been shown to be reliable and valid by a number of studies [19–25]. Researchers have shown that these methods (ie, the tape-based approach) provide results that are consistent with and comparable to the information obtained from the use of objective tools such as the Cervical Range of Motion (CROM) goniometer [22,23].
Some studies related to this issue describe the relationship between posture and TMJD [26–28]. It has been suggested that abnormal masticatory muscle tone can be linked to head posture, and may cause dysfunction in the paraspinal muscles in the neck, which can lead to restricted cervical mobility [16,29–33]. A possible explanation could involve the neurophysiological connections between the cervical spine and the temporomandibular area, such as the convergence of trigeminal and superior afferent inputs in the area of the trigeminal nucleus [32].
Despite the fact that TMJD are rather common, there are few studies investigating mobility in TMJ in comparison to distant joints, such as the cervical spine [15,34], and this subject has generally been overlooked in the Polish literature, which provided a motivation for the current research project. Therefore, this case-control study aimed to evaluate mandibular and cervical mobility in 30 patients aged 18–30 years with TMJD.
Material and Methods
ETHICS STATEMENT:
The study was approved by the Commission for Ethics in Scientific Research at the University of Warmia and Mazury in Olsztyn, Poland (9/2018). All the procedures were performed in conformity with the 1964 Declaration of Helsinki, as amended. Additionally, before the study was conducted, all participants were informed about the aims, methods, and potential benefits, as well as risks resulting from their involvement in the study. Each individual gave informed and voluntary consent to participate in the study, which was documented on the consent forms.
DESIGN:
This case-control study was conducted in the Spine Kinesiology Laboratory at the University of Rzeszów, Poland to evaluate mandibular and cervical mobility in 30 patients with TMJD and 30 healthy controls aged 18–30 years.
PARTICIPANTS:
The study group comprised 30 patients, ranging in age from 18 to 30 years, with TMJD. The participants were selected from among patients visiting a dental clinic and reporting symptoms of TMJD, such pain, reduced mandibular mobility, joint inflammation or degenerative lesions, muscular conditions such as bruxism, and excessive teeth clenching. As a result, the study focused on a broad spectrum of problems related to TMJD, taking into account both joint and muscle functions (Figure 1). Owing to this, the results obtained in this group of patients provided better insight into the causes of pain and reduced mobility in this area, and made it possible to evaluate the effectiveness of the diagnostic methods applied. Temporomandibular disorders (TMJD) were evaluated based on the diagnostic criteria described by Dworkin and LeResche [35]. These criteria include: pain in the TMJ area, reduced mandibular mobility, and cracking in the joints during mandibular movements [35]. Eligibility criteria for potential participants of the study included: pain experienced for a duration of at least 3 months, pain intensity of at least 4/10 according to the visual analogue scale (VAS), and informed and voluntary consent to participate in the study. Criteria for exclusion were as follows: lack of informed consent to participate in the study, age outside the range of 18–30 years, cervical spine injury within the 12 months before the study, regular use of painkillers or steroids, diagnosed developmental and degenerative abnormalities of the cervical spine, and other coexisting neurological, orthopedic, rheumatological diseases possibly affecting cervical mobility.
The control group consisted 30 of healthy subjects without pain, matched for age and gender to the study group.
PROCEDURES AND OUTCOME MEASURES:
All measurements were performed once, by 1 examiner, under the same conditions, ensuring consistency and reliability in the data collection process. The study employed methods which are easy to use, do not require a lot of time and instruments, and are commonly used in clinical practice and research [15–25]. The methods appear to be reliable and valid, as reported by a number of studies [15–25].
Mobility of the TMJ was assessed using a linear measurement, for which a millimeter gauge was applied. This method has been shown to be reliable and valid in assessing TMJ mobility [16–20]. The examination included the assessment of mouth opening (also referred to as mandibular abduction) and lateral movements to the left and to the right. The subjects were seated in an upright position on a chair. Mandibular abduction was assessed at the maximum active mouth opening, with the distance between the edges of the upper and lower incisors being measured. In the cases where the subject’s upper and lower teeth were misaligned, the irregularity was measured and added to the value identified for mandibular abduction. Lateral movements were measured at the maximum active left and right mandibular protrusion. For this purpose, the examiner measured the distance between the maxillary midline and the mandibular midline displaced to the side [16].
The range of cervical mobility was measured using a tape-based tool, which has been demonstrated to be a reliable and valid method in scientific research, and researchers have demonstrated that the tape-based approach provides results comparable to the information obtained from use of objective tools, such as the CROM goniometer [21–23] and the related intraclass correlation coefficient values were reported to range from 0.89 to 0.98 [24,25]. During the examination, the subjects were seated with back support, and the assessment took into account active flexion, extension, right and left lateral flexion, and right and left rotation.
The distances were identified in centimeters, using a tape measure, in the following conditions:
SAMPLE SIZE:
A sample size calculator (“PLUS module” from Statistica 13.3 software) was applied to determine the minimum sample size for the population studied. The following formula was used in this process:
STATISTICAL ANALYSIS:
Statistical analyses were performed using IBM SPSS Statistics 25. Distributions of the investigated variables were examined for normality using the Shapiro-Wilk W test. When a lack of normal distributions was identified, the nonparametric Mann-Whitney U test was used to determine if there were statistically significant differences between 2 independent groups (ie, the group of patients with TMJD and the control group of healthy individuals) in the range of cervical and mandibular mobility. Correlations between 2 variables, where at least 1 of these did not meet the normality criterion, were calculated using the Spearman rank correlation coefficient. Analysis of Spearman correlations showed whether there was a statistically significant relationship between the variables examined (ie, cervical mobility and mandibular mobility) in the group of patients with TMJD and the control group of healthy individuals. It was assumed that the results were statistically significant if
Results
DEMOGRAPHIC CHARACTERISTICS OF THE PARTICIPANTS:
Patients with TMJD (n=30) and the controls (n=30) were matched for age and gender. The mean age of patients with TMJD was 28.55±1.72 years, and 28.79±1.43 years in the control group. Each group comprised 11 female and 19 male subjects. The average duration of pain symptoms in the study group was 16.05±3.22 weeks and average pain intensity was 6/10 on a VAS scale. No statistically significant differences were found in the baseline characteristics of participants in the 2 groups. The characteristics of the study participants are shown in Table 1.
CERVICAL AND MANDIBULAR RANGE OF MOTION IN THE GROUPS:
Patients with TMJD had significantly poorer cervical mobility in all parameters: cervical flexion was significantly lower in patients with TMJD (2.48±0.95 cm) compared to the controls (2.58±0.66 cm); P<0.05. Extension in the study group and the control group amounted to 6.68±1.79 cm, and 7.22±1.14 cm, respectively (P<0.05). Right and left lateral flexion of the cervical spine was also significantly less in patients with TMJD (4.5±1.21/4.75±1.33 cm) compared to the control group (5.7±1.07/5.73±0.97 cm); p<0.001. There were also significant differences in right and left rotation between patients with TMJD (6.52±1.94/6.4±1.9 cm) and the controls (7.4±1.19/7.3±1.36 cm) (P<0.05) (Table 2).
Maximum mouth opening was significantly smaller in patients with TMJD (38.37±2.76 mm) compared to the control group (46.26±3.12 mm); P<0.001. Lateral mobility was also significantly reduced in patients with TMJD (8.78±1.76 mm to the left; P<0.001, 8.57±2.16 mm to the right; P<0.001) compared to the controls (10.92±1.37 mm to the left; p<0.001 i 11.27±2.06 mm to the right; P<0.001) (Table 3).
ASSOCIATION BETWEEN CERVICAL AND MANDIBULAR RANGE OF MOTION IN THE GROUPS:
We also investigated whether there was a statistically significant relationship between cervical mobility and mandibular mobility in the study and control groups. The findings in the control group show no statistically significant correlation between mandibular mobility and cervical mobility (P>0.05) (Table 4).
In the study group the findings showed the following significant positive correlations: greater range of cervical flexion to the left corresponds to greater lateral movement of the mandible to the left (R=0.45; P<0.05), greater range of cervical flexion to the right corresponds to greater lateral movement of the mandible to the right (R=0.46; P<0.05) and to the left (R=0.44; p<0.05), and greater head turn to the left corresponds to greater lateral movement of the mandible to the left (R=0.46; P<0.05), greater head turn to the right corresponds to greater lateral movement of the mandible to the right (R=0.44; P<0.05) (Table 5).
Discussion
LIMITATIONS:
Although our study provides important information on the associations between mandibular and cervical mobility and TJMD, there are several limitations to consider. The first limitation relates to the methods applied to measure mandibular and cervical mobility. Although these methods are based on earlier scientific reports, and research has shown that the methods are highly reliable and are commonly applied as a standard in clinical practice [15–25], they may be subject to measurement errors that affect the results obtained. Further research could employ more advanced measurement techniques such as MRI to obtain more precise results. Notably however, the state-of-the-art quantitative diagnostic methods, which are very costly, are not available in many facilities in Poland. For this reason, the current study used methods that are easy to use, as well as cost- and time-effective, and which do not require complicated instruments, and therefore are widely used in clinical practice, and in scientific research, as shown by numerous publications [15–25].
Secondly, the study group consisted of only 30 patients, which may affect the generalizability of the evidence to a larger population. Further research with a larger number of participants may provide more reliable results. Notably, however, the sample size calculation was carried out for the study and showed that the sample of 30 participants was adequately powered for the feasibility study.
Thirdly, the study involved a narrow age cohort. Therefore, it is necessary to continue the related research investigating more age groups, including older individuals, and taking into account the severity of degenerative changes in the cervical spine.
Finally, the present study did not take into account other factors potentially affecting mandibular and cervical mobility, such as lifestyle or posture habits. In future studies it would be worthwhile to consider these factors to gain better understanding of the effect of TMJD on mandibular and cervical mobility and potential interactions between these factors.
Conclusions
The findings show significantly lower mobility of the mandible in all the planes and reduced cervical mobility in patients with TMJD, particularly in the case of lateral movements and rotation, compared to healthy individuals. Importantly, the current findings suggest that problems related to TMJD can also affect certain distant structures, such as the cervical spine. This fact should be taken into account by those designing rehabilitation programs for patients with this disorder. Our results suggest it is necessary to continue research related to this issue to gain better understanding of these relationships and to develop more effective treatment strategies addressing both TMJD-related problems and the impact of TMJD on cervical spine mobility.
Tables
Table 1. Characteristics of study participants.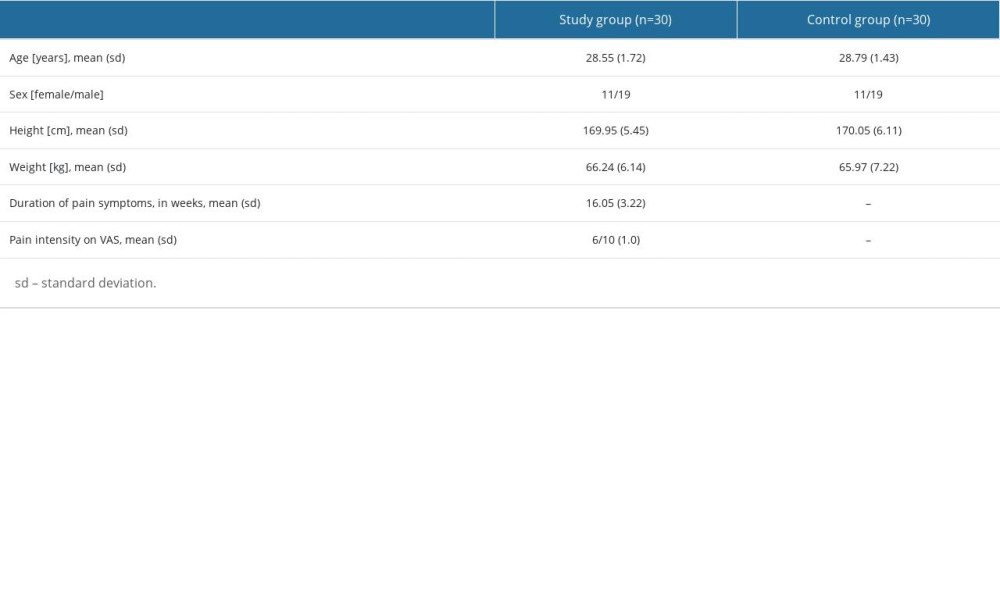 Table 2. Comparison of cervical mobility in the group of patients with TMJD and the control group.
Table 2. Comparison of cervical mobility in the group of patients with TMJD and the control group.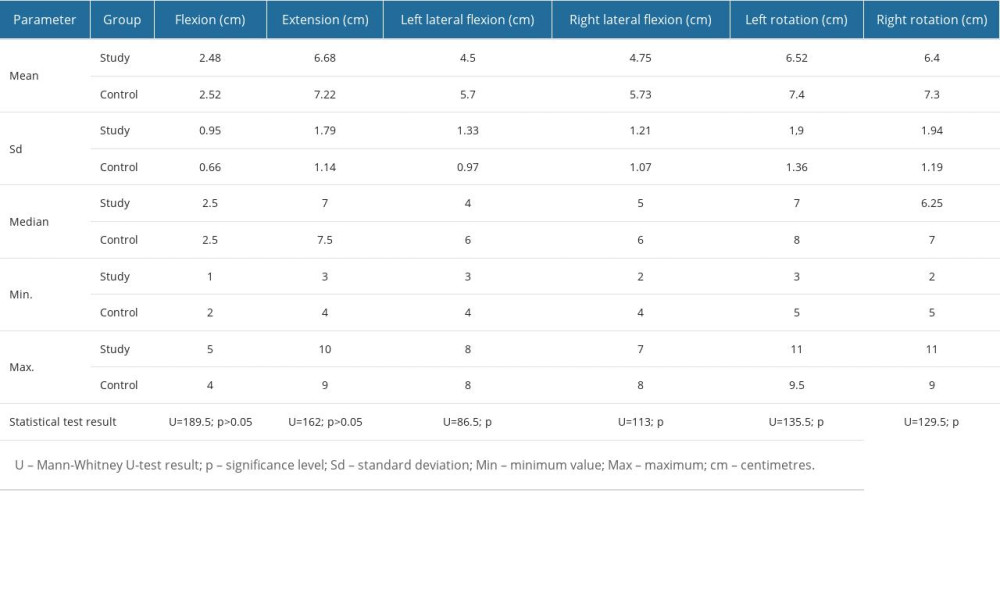 Table 3. Comparison of mandibular mobility in the patients with TMJD and the control group.
Table 3. Comparison of mandibular mobility in the patients with TMJD and the control group.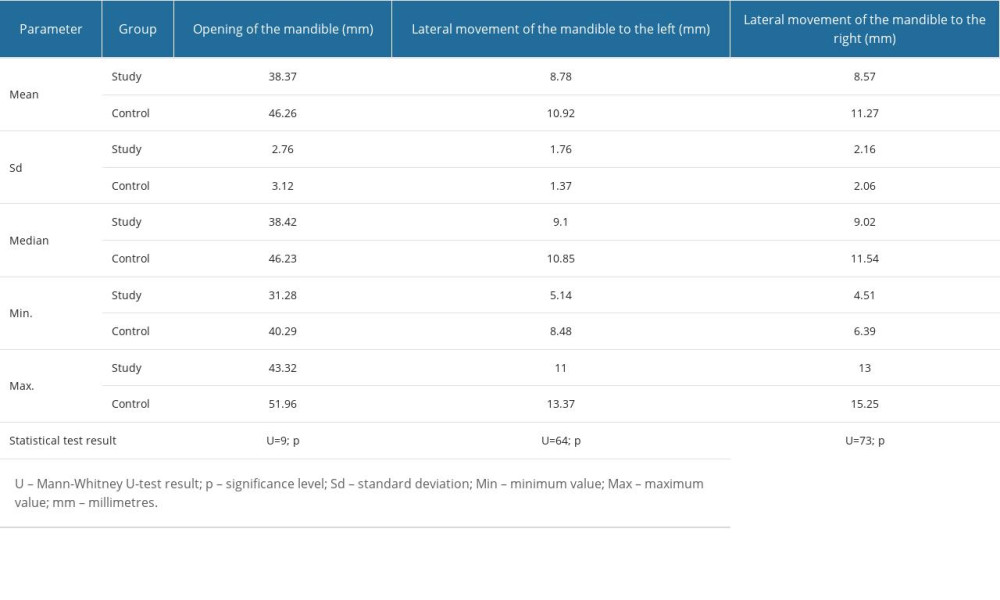 Table 4. Association between mandibular mobility and cervical mobility in the control group.
Table 4. Association between mandibular mobility and cervical mobility in the control group.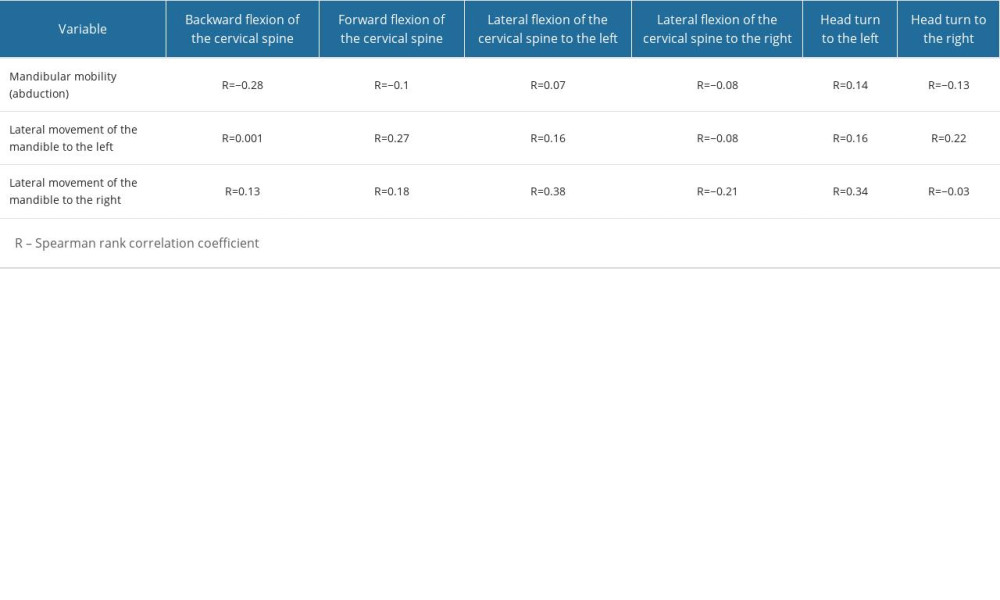 Table 5. Association between mandibular mobility and cervical mobility in the study group.
Table 5. Association between mandibular mobility and cervical mobility in the study group.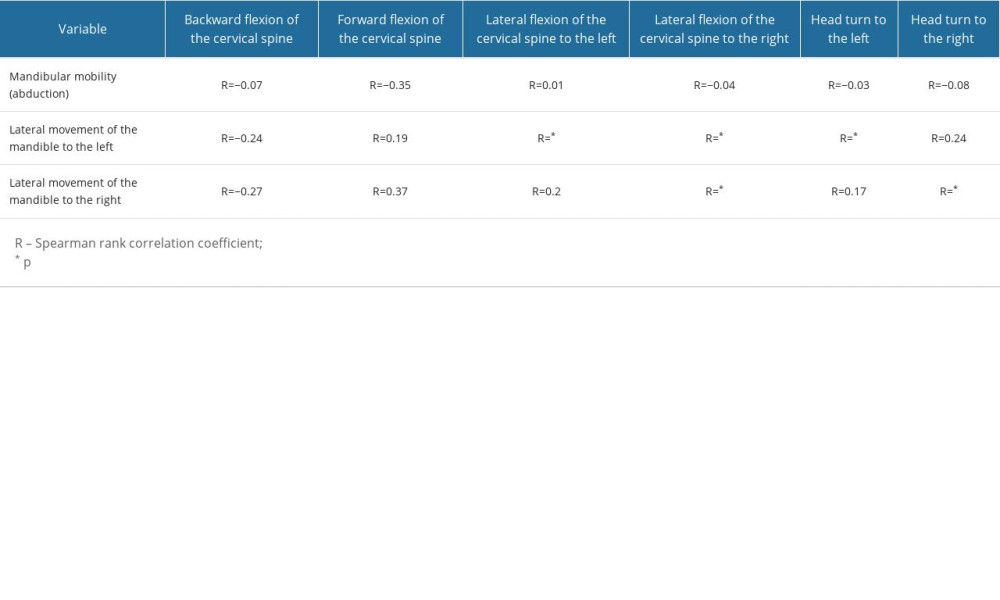
References
1. Schiffman E, Ohrbach R, Truelove E, Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: Recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group: J Oral Facial Pain Headache, 2014; 28(1); 6-27
2. Schiffman E, Ohrbach R, Executive summary of the Diagnostic Criteria for Temporomandibular Disorders for clinical and research applications: J Am Dent Assoc, 2016; 147(6); 438-45
3. Manfredini D, Guarda-Nardini L, Winocur E, Diagnostic criteria for temporomandibular disorders: A systematic review of axis and epidemiologic findings: Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2011; 112(4); 453-62
4. Ahmad M, Hollender L, Anderson Q, Research diagnostic criteria for temporomandibular disorders (RDC/TMD): Development of image analysis criteria and examiner reliability for image analysis: Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2009; 107(6); 844-60
5. Badel T, Marotti M, Pavicin IS, Basić-Kes V, Temporomandibular disorders and occlusion: Acta Clin Croat, 2012; 51(3); 419-24
6. Chisnoiu AM, Picos AM, Popa S, Factors involved in the etiology of temporomandibular disorders – a literature review: Clujul Med, 2015; 88(4); 473-78
7. De Laat A, Meuleman H, Stevens A, Verbeke G, Correlation between cervical spine and temporomandibular disorders: Clin Oral Investig, 1998; 2(2); 54-57
8. Evcik D, Aksoy O, Correlation of temporomandibular joint pathologies, neck pain and postural differences: J Phys Ther Sci, 2000; 12(2); 97-100
9. Scrivani SJ, Keith DA, Kaban LB, Temporomandibular disorders: N Engl J Med, 2008; 359(25); 2693-705
10. Emshoff R, Bertram S, Strobl H, Gassner R, Magnetic resonance imaging findings of internal derangement, osteoarthrosis, effusion, and bone marrow edema before and after performance of arthrocentesis and hydraulic distention of the temporomandibular joint: Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2003; 95(6); 755-61
11. De Rossi SS, Greenberg MS, Temporomandibular disorders: Evaluation and management: Med Clin North Am, 2013; 97(6); 1051-69
12. Mercuri LG, Surgical management of temporomandibular joint disorders: Oral Maxillofac Surg Clin North Am, 2011; 23(2); 253-66
13. Dijkstra PU, de Bont LG, Stegenga B, Boering G, Temporomandibular joint mobility assessment: A comparison between four methods: J Oral Rehabil, 1995; 22(6); 439-44
14. Moreno AJ, Utrilla G, Marin J, Cervical spine assessment using passive and active mobilization recorded through an optical motion capture: J Chiropr Med, 2018; 17(3); 167-81
15. Oleksy Ł, Kielnar R, Mika A, Impact of cervical spine rehabilitation on temporomandibular joint functioning in patients with idiopathic neck pain: Biomed Res Int, 2021; 2021; 6886373
16. Manfredini D, Arveda N, Guarda-Nardini L, Distribution of diagnoses in a population of patients with temporomandibular disorders: Oral Surg Oral Med Oral Pathol Oral Radiol, 2012; 113(5); 661-67
17. Stegenga B, de Bont LG, Boering G, van Willigen JD, Assessment of mandibular function impairment associated with temporomandibular joint osteoarthrosis and internal derangement: J Orofac Pain, 1991; 5(2); 133-41
18. Suvinen TI, Kemppainen P, Review of clinical EMG studies related to muscle and occlusal factors in healthy and TMD subjects: J Oral Rehabil, 2007; 34(9); 631-44
19. Walker N, Bohannon RW, Cameron D, Discriminant validity of temporomandibular joint range of motion measurements obtained with a ruler: J Orthop Sports Phys Ther, 2000; 30(8); 484-92
20. Steenks MH, de Wijer A, Validity of the Research Diagnostic Criteria for Temporomandibular Disorders Axis I in clinical and research settings: J Orofac Pain, 2009; 23(1); 9-16
21. Audette I, Dumas JP, Côté JN, De Serres SJ, Validity and between-day reliability of the cervical range of motion (CROM) device: J Orthop Sports Phys Ther, 2010; 40(5); 318-23
22. Maksymowych WP, Mallon C, Richardson R, Development and validation of a simple tape-based measurement tool for recording cervical rotation in patients with ankylosing spondylitis: Comparison with a goniometer-based approach: J Rheumatol, 2006; 33(11); 2242-49
23. Viitanen JV, Kokko ML, Heikkilä S, Kautiainen H, Neck mobility assessment in ankylosing spondylitis: A clinical study of nine measurements including new tape methods for cervical rotation and lateral flexion: Br J Rheumatol, 1998; 37(4); 377-81
24. Hoving JL, Pool JJ, van Mameren H, Reproducibility of cervical range of motion in patients with neck pain: BMC Musculoskelet Disord, 2005; 6; 59
25. Jordan K, Assessment of published reliability studies for cervical spine range-of-motion measurement tools: J Manipulative Physiol Ther, 2000; 23(3); 180-95
26. Silveira A, Gadotti IC, Armijo-Olivo S, Jaw dysfunction is associated with neck disability and muscle tenderness in subjects with and without chronic temporomandibular disorders: Biomed Res Int, 2015; 2015; 512792
27. Kummoona J, Surgical managements of subluxation and dislocation of the temporomandibular joint: Clinical and experimental studies: J Craniofac Surg, 2010; 21(6); 1692-97
28. Loster J, Wieczorek A, Majewski S, The emotional state of patients with temporomandibular dysfunction syndrome and other dental disorders: J Stoma, 2012; 65(1); 39-47
29. Khare N, Patil SB, Kale SM, Normal mouth opening in an adult Indian population: J Maxillofac Oral Surg, 2012; 11(3); 309-13
30. Svechtarov V, Hristova M, Nencheva-Svechtarova S, Tonchev T, Mandibular range of motion and its relations to temporomandibular disorders: Scripta Medicine Dentalis, 2015; 1(1); 21-26
31. Huggare JA, Raustia AM, Head posture and cervicovertebral and craniofacial morphology in patients with craniomandibular dysfunction: Cranio, 1992; 10(3); 173-79
32. Bragatto MM, Bevilaqua-Grossi D, Regalo SC, Sousa JD, Chaves CT, Associations among temporomandibular disorders, chronic neck pain and neck pain disability in computer office workers: A pilot study: J Oral Rehabil, 2016; 43(5); 321-32
33. Murray GM, Phanachet I, Uchida S, Whittle T, The human lateral pterygoid muscle: A review of some experimental aspects and possible clinical relevance: Aust Dent J, 2004; 49(1); 2-8
34. Catanzariti JF, Debuse T, Duquesnoy B, Chronic neck pain and masticatory dysfunction: Joint Bone Spine, 2005; 72(6); 515-19
35. Dworkin SF, LeResche L, Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications: Crit Rev Oral Biol Med, 1992; 3(4); 248-76
36. Kitsoulis P, Marini A, Iliou K, Signs and symptoms of temporomandibular joint disorders related to the degree of mouth opening and hearing loss: BMC Ear Nose Throat Disord, 2011; 11; 5
37. Kielnar R, Mika A, Bylina D, The influence of cervical spine rehabilitation on bioelectrical activity (sEMG) of cervical and masticatory system muscles: PLoS One, 2021; 16(4); e0250746
38. Cortese S, Mondello A, Galarza R, Biondi A, Postural alterations as a risk factor for temporomandibular disorders: Acta Odontol Latinoam, 2017; 30(2); 57-61
39. Forsberg CM, Hellsing E, Linder-Aronson S, Sheikholeslam A, EMG activity in neck and masticatory muscles in relation to extension and flexion of the head: Eur J Orthod, 1985; 7(3); 177-84
40. Calixtre LB, Oliveira AB, de Sena Rosa LR, Effectiveness of mobilisation of the upper cervical region and craniocervical flexor training on orofacial pain, mandibular function and headache in women with TMD. A randomised, controlled trial: J Oral Rehabil, 2019; 46(2); 109-19
41. Śmiga-Witas A, Kostrzewa-Janicka J, Brożyński M, Relationship between temporomandibular and cervical spine disorders: Protet Stomatol, 2011; 61(6); 466-75
42. Cuccia AM, Caradonna C, The relationship between the stomatognathic system and body posture: Clinics (Sao Paulo), 2009; 64(1); 61-66
43. Munhoz WC, Marques AP, de Siqueira JT, Evaluation of body posture in individuals with internal temporomandibular joint derangement: Cranio, 2005; 23(4); 269-77
44. Silva AG, Punt TD, Sharples P, Vilas-Boas J, Johnson MJ, Head posture and neck pain of chronic nontraumatic origin: A comparison between patients and pain-free persons: Arch Phys Med Rehabil, 2009; 90(4); 669-74
45. Armijo-Olivo S, Silvestre RA, Fuentes JP, Patients with temporomandibular disorders have increased fatigability of the cervical extensor muscles: Clin J Pain, 2012; 28(1); 55-64
Tables
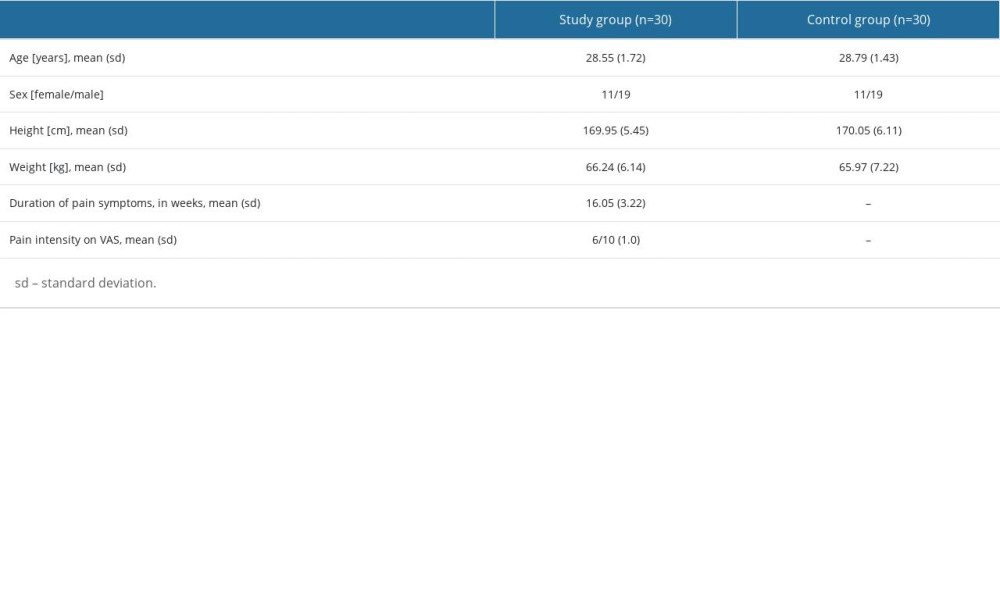 Table 1. Characteristics of study participants.
Table 1. Characteristics of study participants.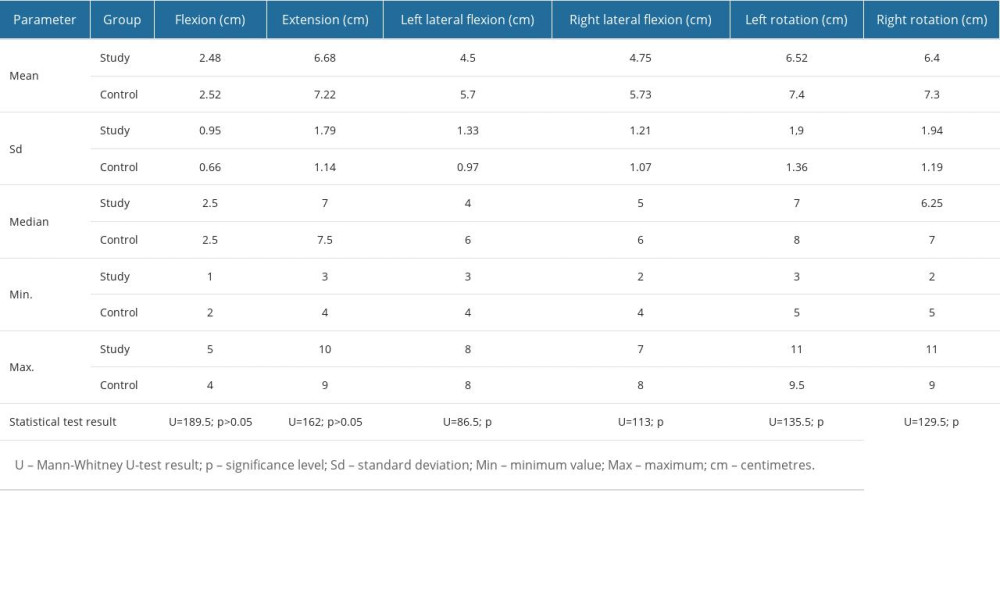 Table 2. Comparison of cervical mobility in the group of patients with TMJD and the control group.
Table 2. Comparison of cervical mobility in the group of patients with TMJD and the control group.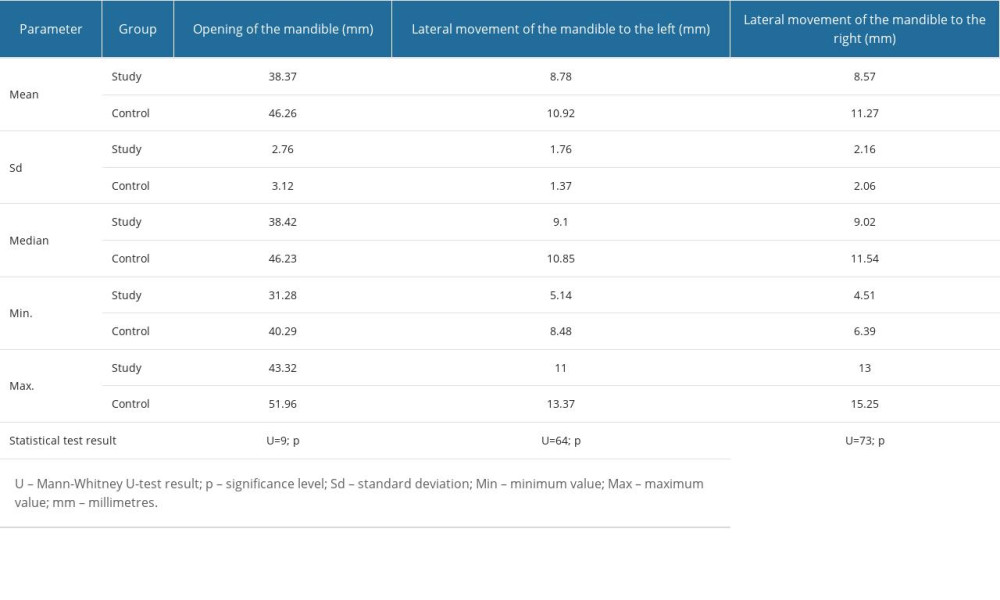 Table 3. Comparison of mandibular mobility in the patients with TMJD and the control group.
Table 3. Comparison of mandibular mobility in the patients with TMJD and the control group.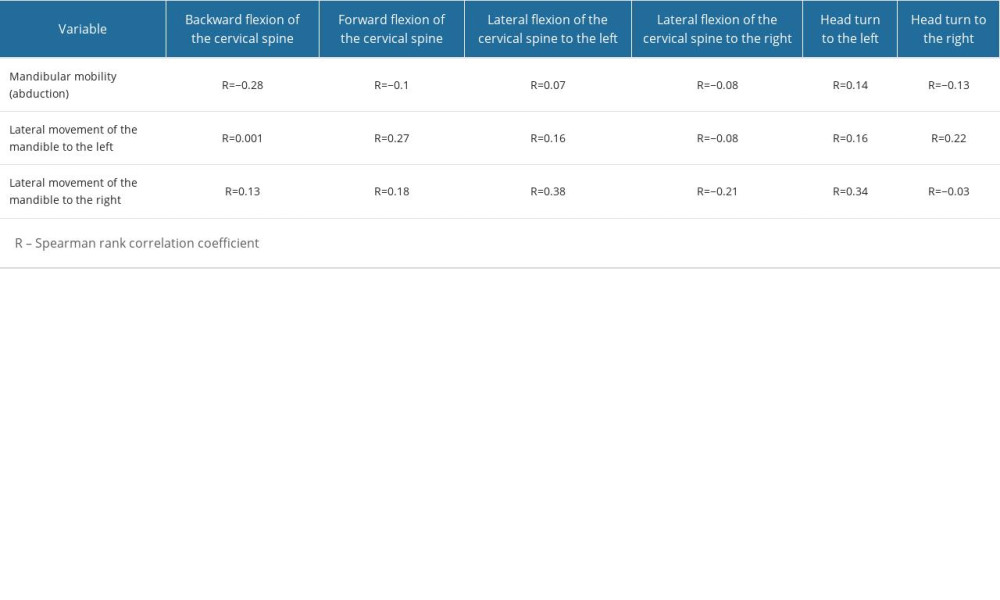 Table 4. Association between mandibular mobility and cervical mobility in the control group.
Table 4. Association between mandibular mobility and cervical mobility in the control group.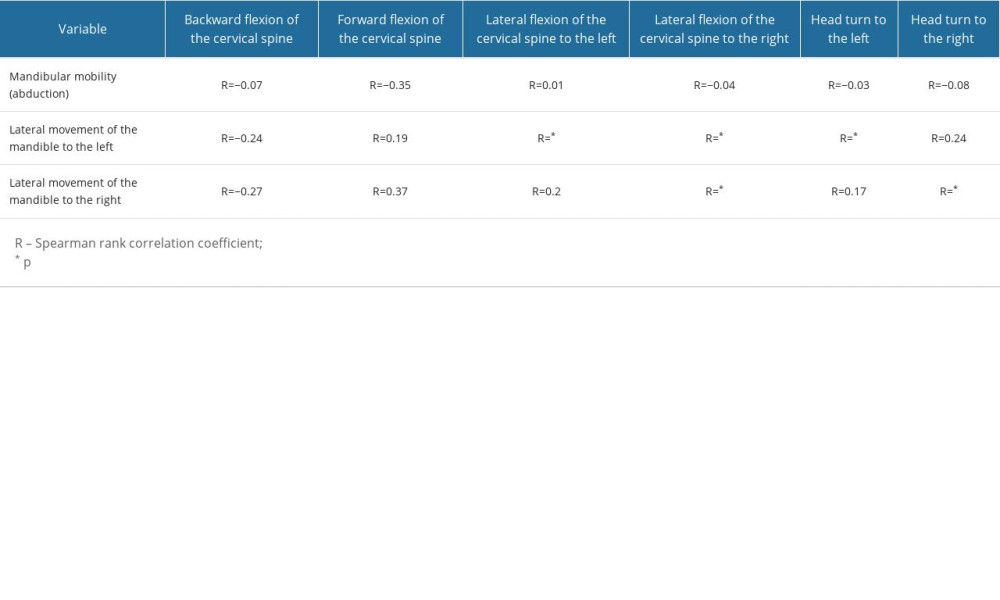 Table 5. Association between mandibular mobility and cervical mobility in the study group.
Table 5. Association between mandibular mobility and cervical mobility in the study group.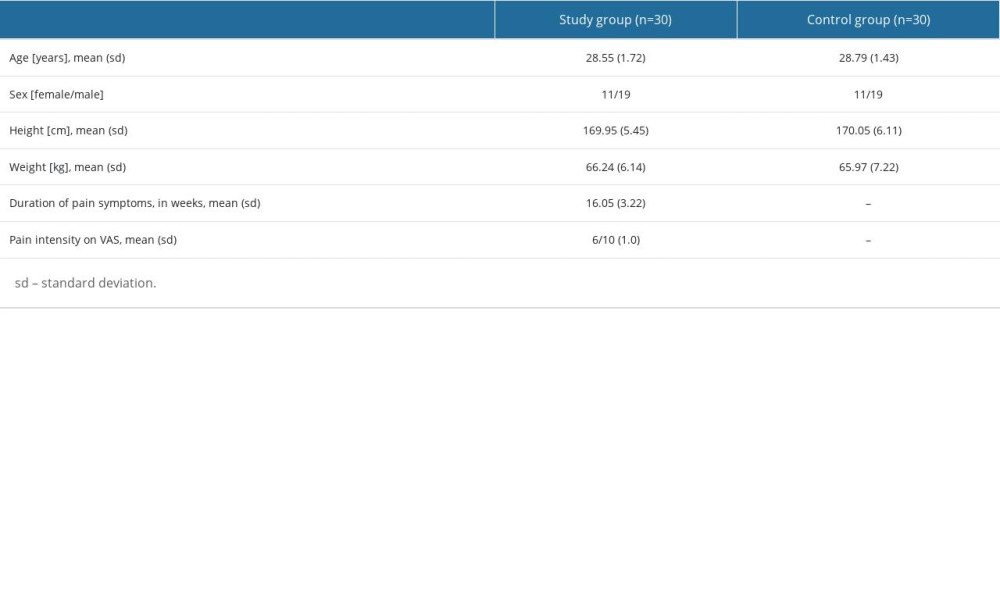 Table 1. Characteristics of study participants.
Table 1. Characteristics of study participants.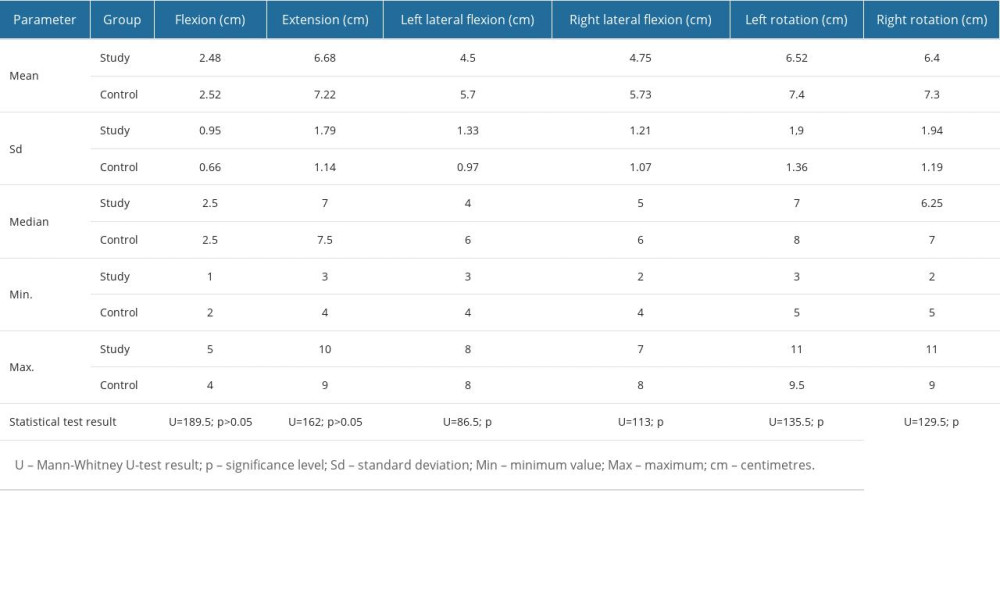 Table 2. Comparison of cervical mobility in the group of patients with TMJD and the control group.
Table 2. Comparison of cervical mobility in the group of patients with TMJD and the control group.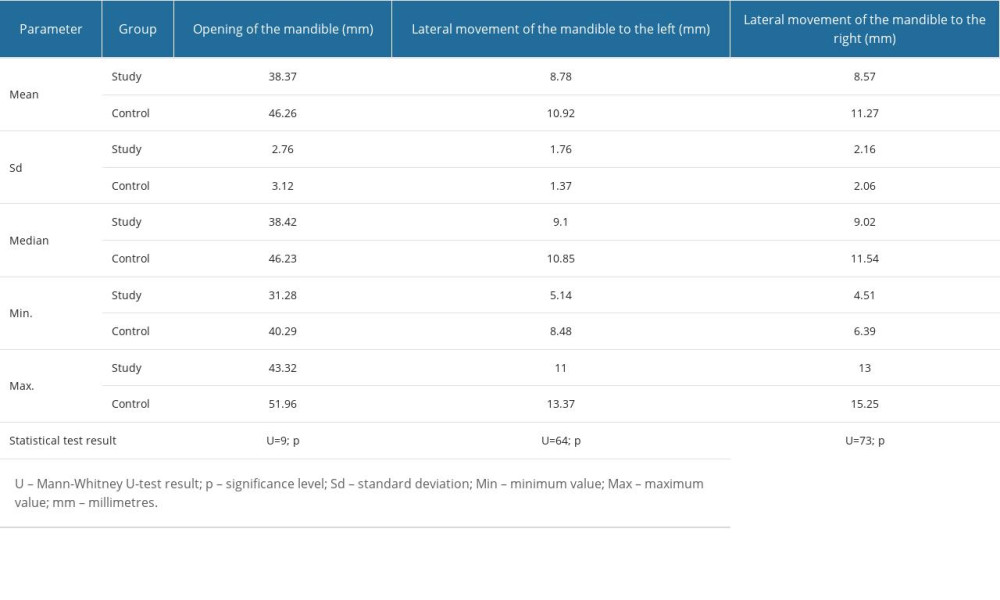 Table 3. Comparison of mandibular mobility in the patients with TMJD and the control group.
Table 3. Comparison of mandibular mobility in the patients with TMJD and the control group.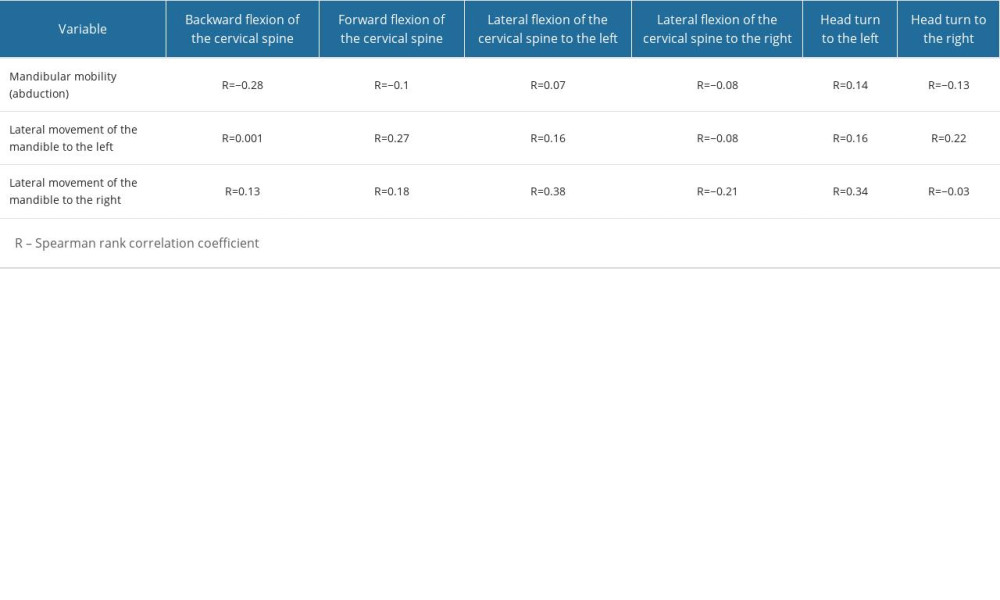 Table 4. Association between mandibular mobility and cervical mobility in the control group.
Table 4. Association between mandibular mobility and cervical mobility in the control group.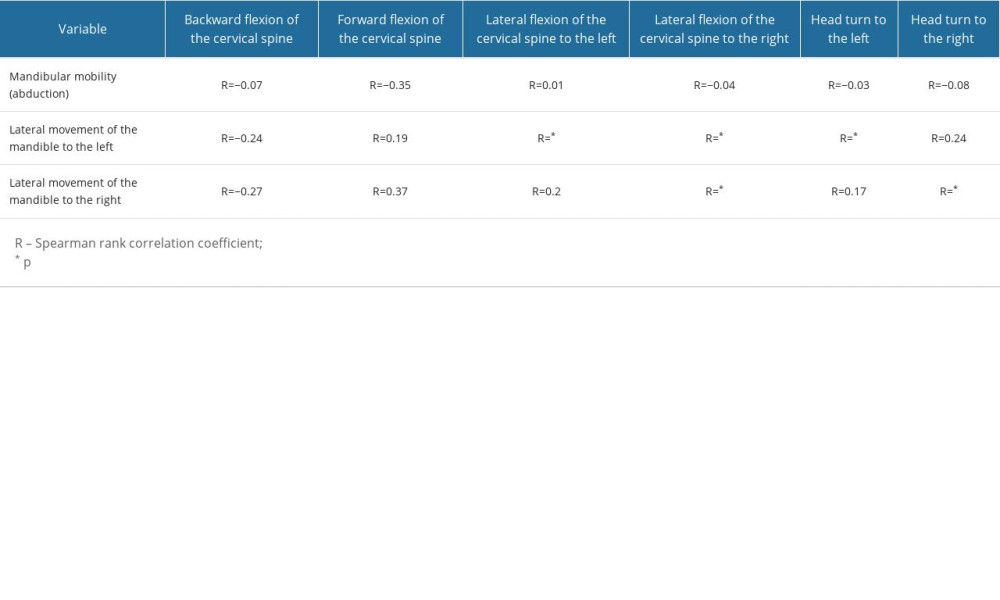 Table 5. Association between mandibular mobility and cervical mobility in the study group.
Table 5. Association between mandibular mobility and cervical mobility in the study group. In Press
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952









