14 August 2023: Clinical Research
A Simple and Accurate Model for Predicting Fall Injuries in Hospitalized Patients: Insights from a Retrospective Observational Study in Japan
Shizuka Yaita1ACDEF, Masaki TagoDOI: 10.12659/MSM.941252
Med Sci Monit 2023; 29:e941252
Abstract
BACKGROUND: While several predictive models for falls have been reported such as we reported in 2020, those for fall “injury” have been unreported. This study was designed to develop a model to predict fall injuries in adult inpatients using simple predictors available immediately after hospitalization.
MATERIAL AND METHODS: This was a single-center, retrospective cohort study. We enrolled inpatients aged ≥20 years admitted to an acute care hospital from April 2012 to March 2018. The variables routinely obtained in clinical practice were compared between the patients with fall injury and the patients without fall itself or fall injury. Multivariable analysis was performed using covariables available on admission. A predictive model was constructed using only variables showing significant association in prior multivariable analysis.
RESULTS: During hospitalization of 17 062 patients, 646 (3.8%) had falls and 113 (0.7%) had fall injuries. Multivariable analysis showed 6 variables that were significantly associated with fall injuries during hospitalization: age (P=0.001), sex (P=0.001), emergency transport (P<0.001), medical referral letter (P=0.041), history of falls (P=0.012), and abnormal bedriddenness ranks (all P≤0.001). The area under the curve of this predictive model was 0.794 and the shrinkage coefficient was 0.955 using the same data set given above.
CONCLUSIONS: We developed a predictive model for fall injuries during hospitalization using 6 predictors, including bedriddenness ranks from official Activities of Daily Living indicators in Japan, which were all easily available on admission. The model showed good discrimination by internal validation and promises to be a useful tool to assess the risk of fall injuries.
Keywords: Accidental Falls, Activities of Daily Living, Inpatients, Logistic Models, Wounds and Injuries, Adult, Humans, Retrospective Studies, Japan, Hospitalization, Risk Factors
Background
Fall injuries during hospitalization increase the cost of health care [1–4] due to the increased cost of hospitalization caused by extended hospital stays and the accompanying increased cost of treatment [1,5–6]. In addition, legal resolutions of falls considerably and seriously burden health care providers [7]. However, among the patients who fall while in hospital, 88% suffer no injuries and do not require any additional treatment [8]. Meanwhile, patients who do incur fall injuries are susceptible to limited activities of daily living (ADLs) or other long-term sequelae [9,10]. Therefore, it is more important to predict the occurrence of fall-related injuries than a fall itself without concomitant injuries. While many medical institutions in Japan use various tools to prevent a fall or fall injuries in inpatients, such as bed alarms, low beds, or hip protectors, medical resources available for such tools are limited [11–13]. Thus, the target population to be offered such preventive tools must inevitably be narrowed down to those patients more likely to have fall injuries. However, given that a reliable model to predict such patients remains to be established, medical practitioners in many medical institutions select their targets for intervention according to their previously developed risk assessment tools for falls. Therefore, development of a model that can accurately predict which patients are likely to have fall injuries would help medical practitioners worldwide to allocate finite human and material resources more effectively and efficiently.
Several predictive models for falls regardless of concomitant injuries have been reported, such as the St. Thomas Risk Assessment Tool, the Tinetti Mobility Test, the Hendrich II Fall Risk Model [14–16], and the Saga Fall Prediction Model we reported in 2020 [17]. In addition, studies targeting only patients who fall have reported various factors associated with fall injuries, such as being elderly, female, or visually impaired, and scoring rank A of bedriddenness ranks (BRs) from official ADLs scales of the Ministry of Health, Labour and Welfare (MHLW), Japan [8,18–20]. However, there have been no published reports on factors or models predicting fall injuries targeted to all adult inpatients. Because the risk of falling is reported to be highest within 1 week of admission [21], the predicting factors constituting a predictive model for fall injuries should be easily available on admission. Therefore, this retrospective study aimed to develop a predictive model for fall injuries targeting all inpatients aged ≥20 years by using simple predictors that were easily assessed on the day of admission.
Material and Methods
ETHICS STATEMENT:
This study complies with the Ethical Guidelines for Medical and Health Research Involving Human Subjects of the MHLW and the Ministry of Education, Culture, Sports, Science and Technology, Japan. This study was approved by the Research Ethics Committee of Yuai-Kai Foundation and Oda Hospital (No. 20180629_R1). Consent of all patients was obtained by the comprehensive consent method in the hospital, and patient anonymity was protected.
STUDY DESIGN AND POPULATION:
This was a single-center, retrospective cohort study. We enrolled all inpatients aged ≥20 years admitted to an acute care hospital (Yuai-Kai Foundation and Oda Hospital) from April 2012 to March 2018. The hospital is located in the rural city of Kashima, Saga Prefecture, Japan, serving a population of about 90 000. More than 3100 inpatients are treated annually in the hospital, with average length of stay of 12.1 days. The hospital comprises 10 departments and 111 beds, including the Departments of Internal Medicine, Surgery, Neurosurgery, and Cardiovascular Surgery.
VARIABLES AND SOURCES OF INFORMATION:
The data in this study were extracted from the hospital’s health records. The variables extracted have been reported as factors related to a fall or fall injuries in previous studies: age (continuous variable), sex (male or female), department of admission (Internal Medicine, Neurosurgery, or others), emergency admission (presence or absence), emergency transport (presence or absence), medical referral letter (presence or absence), history of falls (presence or absence), use of hypnotic medication (using or not using), visual impairment (presence or absence), parkinsonism (presence or absence), permanent damage by stroke (presence or absence), ability to eat, swallow, toileting, hold sitting, hold standing, transfer from bed to wheelchair/stretcher/portable toilet, move, bathe, and take prescribed medicine (independent or requiring assistance), and MHLW classifications for ADLs; BRs (normal, J, A, B, C), cognitive function scores (CFs) (normal, 1, 2, 3, 4, M) on admission and rehabilitation (presence or absence), surgery (presence or absence), fall (presence or absence), injury level caused by a fall (no injury and levels 1, 2, 3) [22], and dates of admission to and discharge from hospital. Among the variables we extracted, 8 variables – age, sex, emergency admission, department of admission, use of hypnotic medication, history of falls, ability to eat, BRs – had been reported as indicators in a predictive model for fall regardless of having concomitant injuries [17]. A sample size could not be calculated because a predictive model for fall injuries had not been previously reported.
DEFINITION OF FALL AND FALL INJURY:
The case of a patient’s fall during hospitalization is usually recorded in an incident/accident report by the attending nurse or the nurse who discovered the fall. “Falls” were defined as unexpected falls from any unplanned descent of a patient to the floor with or without injuries, from any height, and in any position, ie, on the floor, from stairs, chair, or bed, when standing, walking, or sitting, or even in recumbent position. Whether the patient had a fall or not was identified from the incident/accident reports described above. The severity of an injury caused by the fall was classified according to a part of “Reasons for Falls and Falls and Injury Severity Input Criteria” in the acute care indicators in the Maryland Hospital Association Center for Performance Sciences’ Quality Indicator Project (Table 1) [23]. We divided inpatients into 2 groups: the group “With fall injury” involving the patients with severe injuries more than injury level 1, and the group “Without fall injury” involving the patients who had not fallen or had fallen without having any injuries.
DEFINITION OF VARIABLES:
The variables history of falls, use of hypnotic medications, visual impairment, parkinsonism, permanent damage by stroke, ADLs, BRs, and CFs were routinely assessed by the attending nurse within 24 h after admission. MHLW BRs and CFs are official tools for assessing ADLs that have been used widely under the long-term care insurance system in Japan. BRs are classified into 5 major categories (normal; J, independence; A, house-bound; B, chair-bound; C, bed-bound) (Figure 1). CFs are classified into 6 major categories (normal; 1, independence; 2, attention needed; 3, intermittent care needed; 4, continuous care needed; M, specialized treatment needed) [8,22]. In the hospital, hypnotic medications were classified into benzodiazepines and nonbenzodiazepines, excluding melatonin receptor agonists and orexin receptor antagonists. Although “visual impairment” had not been defined clearly in this retrospective study, attending nurses determined a patient as being visually impaired when the patient’s ADLs were limited by some form of visual abnormality.
STATISTICAL ANALYSIS AND METHODS OF CREATING THE PREDICTIVE MODEL:
Univariable analysis for fall injury was performed by a chi-squared test with calculated odds ratio (OR), 95% confidence interval (95% CI), and
Results
CHARACTERISTICS OF THE PATIENTS AND INCIDENCE OF FALL INJURY:
During the study period, 17 687 inpatients were admitted. A total of 17 062 patients were analyzed, excluding 624 patients <20 years old and 1 patient without a record of outcome of fall injuries during hospitalization. The median age (interquartile range) was 77 (63–85) years; 8399 (49%) patients were men, and the median length of hospital stay (interquartile range) was 9 (4–17) days. There were 646 (3.8%) patients who had a fall during hospitalization (the incidence rate of falls was 5.33 per 1000 patient-days), and 113 patients were classified into the group “With fall injury” (0.7% of all hospitalized patients, or 1.21 per 100 000 patient-days, Figure 2). In the “With fall injury” group, the median age (interquartile range) was 85 (80–89) years, and 64 (57%) patients were male.
UNIVARIABLE ANALYSIS:
The results of univariable analysis are shown in Table 2. Patients with fall injuries were significantly older (85 vs 77 years) and had longer hospitalization (22 vs 9 days). In addition, the rates of the following factors were significantly higher in the “With fall injury” group: admission to Internal Medicine (64% vs 46%), emergency admission (69% vs 45%), absence of emergency transport (67% vs 40%), presence of medical referral letter (43% vs 29%), history of falls (30% vs 10%), requiring assistance in eating (35% vs 21%), requiring assistance in toileting (46% vs 27%), independence of sitting (73% vs 61%), requiring assistance in standing (30% vs 24%), independence of transfers from bed to wheelchair/stretcher/portable toilet (62% vs 42%), requiring assistance in moving (49% vs 31%), requiring assistance in bathing (59% vs 33%), BRs of J (12% vs 9.1%), A (38% vs 15%), and B (25% vs 11%), CFs of 1 (21% vs 10%), 2 (9.7% vs 3.1%), and 3 (35% vs 15%), undergoing rehabilitation during hospitalization (67% vs 40%), and without undergoing surgery during hospitalization (79% vs 69%).
COVARIATE SELECTION AND MULTIVARIABLE ANALYSIS:
Among all of the 24 collected factors, except for 3 indicators (surgery, rehabilitation, and length of hospital stay) that were impossible to access at the time of admission, the following 13 factors were selected as covariates for multivariable analysis, taking their collinearity into consideration: age (continuous variable), sex (male or female), department of admission (Internal Medicine, Neurosurgery, or others), emergency admission (presence or absence), emergency transport (presence or absence), medical referral letter (presence or absence), history of falls (presence or absence), use of hypnotic medications (using or not using), visual impairment (presence or absence), parkinsonism (presence or absence), permanent damage by stroke (presence or absence), ability to eat (independent or requiring assistance), and BRs (normal, J, A, B, C). The results of the binomial logistic regression analysis (forced entry method, Analysis 1) showed that 6 indicators were significantly associated with fall injuries (Table 3, Analysis 1): older age (OR 1.0, 95% CI 1.0–1.1, P=0.003), male (OR of female 0.5, 95% CI 0.4–0.8, P=0.001), absence of emergency transport (OR of presence 0.4, 95% CI 0.2–0.7, P=0.003), presence of medical referral letter (OR of presence 1.5, 95% CI 1.0–2.2, P=0.042), presence of history of falls (OR of presence 1.7, 95% CI 1.1–2.7, P=0.013), abnormal BRs: BR J (OR of J to normal 4.7, 95% CI 1.9–12, P=0.001), A (OR of A to normal 7.9, 95% CI 3.5–18, P<0.001), B (OR of B to normal 6.2, 95% CI 2.6–15, P<0.001), and C (OR of C to normal 4.1, 95% CI 1.6–11, P=0.004). Similar to Analysis 1, in the binomial logistic regression analysis (forced entry method, Analysis 2) using only the 6 covariates that were significant in Analysis 1, all of the 6 factors were significantly associated with fall injuries (Table 3, Analysis 2): older age (OR 1.0, 95% CI 1.0–1.1, P=0.001), male (OR of female 0.5, 95% CI 0.4–0.8, P=0.001), absence of emergency transport (OR of presence to absence 0.4, 95% CI 0.3–0.6, P<0.001), presence of medical referral letter (OR 1.5, 95% CI 1.0–2.2, P=0.041), presence of history of falls (OR 1.7, 95% CI 1.1–2.6, P=0.012), abnormal BRs: BR J (OR of J to normal 4.9, 95% CI 2.0–12, P=0.001), A (OR of A to normal 8.9, 95% CI 4.0–20, P<0.001), B (OR of B to normal 7.3, 95% CI 3.1–17, P<0.001), and C (OR of C to normal 4.5, 95% CI 1.9–11, P=0.001).
The predictive model for fall injuries we developed using the regression coefficients in Analysis 2 is as follows:
Score=−8.672+0.034 × (age) + (sex: female=−0.641) + (emergency transport: presence=−0.887, missing=−0.551) + (medical referral letter: presence=0.399, missing=1.189) + (history of falls: presence=0.542) + (BR: J=1.597, A=2.188, B=1.986, C=1.510, others=0.154).
INTERNAL VALIDATION OF PREDICTIVE MODEL:
The AUC as the predictive performance of this model calculated using data from the same population was 0.794 (95% CI 0.762–0.826, Figure 3). The cutoff values for the model with the 90% sensitivity and 54% specificity points was −5.27, and with the 35% sensitivity and 90% specificity points was −3.80. The score of the cutoff value with Youden’s Index was −5.08, with sensitivity 89% and specificity 56%. Predicted and measured incidence rates of fall injuries in each of 10 quartiles of the score are shown in Figure 4. The shrinkage coefficient was 0.955.
Discussion
We developed a new model to simply predict fall injuries during hospitalization using 6 predictors that were routinely obtained on admission in acute care settings in Japan. As predictive models for fall injuries have yet to be reported, the model developed in this study is the first predictive model for fall injuries to target all adult inpatients. Fall injuries during hospitalization lead to increased health care costs [1–4] and additional limitations of patients’ ADLs with possible long-term sequelae [9,10]. Although using hip protectors or multifaceted interventions based on risk assessment for a fall was reported to be effective in preventing a fall or fall injuries [13,24], it is unrealistic to apply such resources to all inpatients who are at risk of a fall in the setting of actual acute medical practice, owing to the limited supply of such equipment, medical resources, and time required. Therefore, several predictive models for a fall during hospitalization were developed and are duly employed, but without taking accompanying injuries into consideration [14–17]. However, 88% of patients who fell during hospitalization were reported to be uninjured without needing any additional treatment [8]. This fact suggests that preventive intervention should make more efficient and appropriate allocation of finite human and material resources to patients with a high probability of an injurious fall rather than to those at risk of a fall without concomitant injuries. In addition, assessment of the risk of fall injuries as early as possible is preferable because the highest incidence of falls is reported early after admission, especially within 1 week [21]. Considering these points, our prediction model focusing on the prediction of fall injuries rather than a fall itself regardless of the occurrence of concomitant injuries, which could be assessed immediately after admission using 6 simple predictors (age, sex, emergency transport, medical referral letter, history of falls, and BRs) available on admission, could be extremely useful in preventing fall injuries among inpatients in acute medical settings.
We used BRs, one of the official Japanese ADLs classifications, as one of our predictors. BRs have been widely used as a scale of disability among the aged population in medical and long-term care settings in Japan, and have also been used in several studies [8,25,26]. BRs classify the degree of ADLs decline roughly into 5 ranks through 3 steps [22], which is much easier to assess than the Katz Index with 7 ranks of overall rating requiring assessments of 7 items with 2 choices [27], or the Barthel Index requiring assessments of 10 items with 2 to 4 ranks [28]. BRs were also recently reported to have good inter-rater reliability and criterion-related validity, similar to the Katz Index and Barthel Index [22]. Thus, BRs are reasonable predictors to use in a predictive model that requires simplicity of use in clinical practice.
The multivariable analysis of this study identified the 6 variables – age, male, absence of emergency transport, presence of medical referral letter, presence of history of falls, and abnormal BR J, A, B, or C – as significant factors associated with fall injuries. The fact that age and BR of A are useful predictors for fall injuries is consistent with results previously reported [8,19,20], and in another study male was inconsistent [18]. Other remaining factors – absence of emergency transport, presence of medical referral letter, presence of history of falls, and abnormal BR J, B, or C – were new predictive factors for fall injury. The study that reported female as a predictive factor for fall injury was conducted only for patients who had fallen [18], which was different from our study that included patients who had not fallen. Male [16,17,29,30], presence of history of falls [31], and BR B or C had also been reported as factors associated with a fall itself regardless of having concomitant injuries [17], suggesting that these 3 factors could have predicted a fall itself, which was a matter-of-course prerequisite for having injuries. In addition, BRs are useful for predicting fall injuries among inpatients because of their higher OR for predicting fall injuries in comparison with other indicators in the model.
This study also showed that the absence of emergency transport and presence of a medical referral letter were 2 novel factors associated with fall injuries. The reason that the absence of emergency transport was associated with fall injuries could be the lower incidence of using physical restraint in such situations, which would naturally prevent a fall itself and subsequent related injuries. Physical restraint was reported to be more often used for young patients with psychiatric disorders or alcohol dependence or, on the contrary, aged patients with internal diseases, both of which tended to be transferred by ambulance [32]. Additionally, physical movements of patients being transferred by ambulance are often restricted because of their medical conditions or treatment modalities, such as bed rest after surgery or use of ventilator or infusion pump [33], which possibly lowers the incidence of a fall and fall injuries. In fact, the association between transported by ambulance and severity of fall injury was not significant in our previous study [8]. However, the proportion of patients transported by ambulance was markedly lower in the group with severe fall injuries than having mild or no injuries among inpatients who fell, which could mean that an insufficient sample size caused lower statistical power, thus preventing a possible significant difference. Concerning the other new factor, the presence of a medical referral letter, it is possible that it might have predicted only a fall without regarding concomitantly occurring injuries, consequently showing its significant relationship with fall injuries in this model. The percentage of patients having a medical referral letter with a fall in our previous study was higher (37–39%) than that of patients without a fall in another previous study we reported (33%) or in this study (29%) [8,17], although in our previous report the patients who fell showed no significant difference in the ratio of the presence of a medical referral between the patients with and without injuries [8]. Further research is required to decide whether the presence of a medical referral letter is an accurate predictor of a fall or to elucidate the reasons for the fact that a medical referral letter is associated with a fall, because all our studies already mentioned were conducted at the same institution in Japan, which was an unavoidable limitation.
This study has several limitations. There could be an overestimation bias because this study was a single-center, retrospective study without external validation, owing to the small sample size of patients with fall injuries. External validation using data from different populations with various backgrounds will be necessary to determine the proper prediction power and generalizability of this model because some predictors, including presence of emergency transport or medical referral letter, could have diverse indications in different medical settings, such as at different hospitals with various regional medical backgrounds. In addition, the ORs for fall injuries could have been underestimated because the influence of fall prevention procedures was not adjusted. These had been routinely implemented in the hospital according to its original risk assessment tool due to the failure of data collection.
Conclusions
We developed a new prediction model for fall injuries among inpatients using 6 predictors easily available on admission to hospital, including the subcategory BRs of the official ADLs scales in Japan. This is the first predictive model for fall injuries during hospitalization of adults in general hospitals, which could be useful for selecting priority targets of patients for fall prevention in busy clinical settings because of its simple and quick risk assessment.
Figures
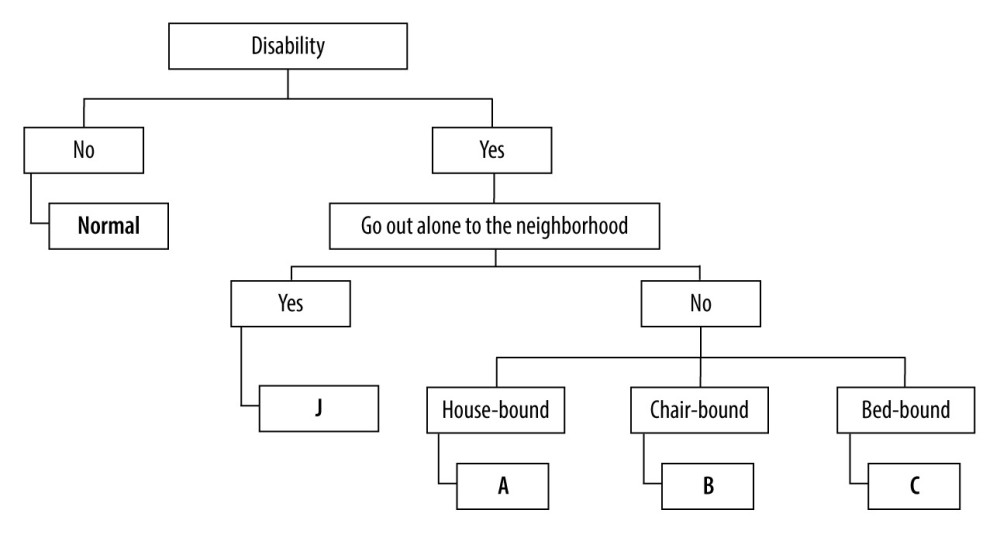 Figure 1. Flowchart for determining bedriddenness ranks. Bedriddenness ranks (BRs) is an official tool for assessing activities of daily living, which has been used widely under the long-term care insurance system in Japan. BRs are classified into 5 major categories (normal; J, independence; A, house-bound; B, chair-bound; C, bed-bound) by 3 steps. This figure was created using Microsoft® PowerPoint® for Microsoft 365 MSO (version 2305).
Figure 1. Flowchart for determining bedriddenness ranks. Bedriddenness ranks (BRs) is an official tool for assessing activities of daily living, which has been used widely under the long-term care insurance system in Japan. BRs are classified into 5 major categories (normal; J, independence; A, house-bound; B, chair-bound; C, bed-bound) by 3 steps. This figure was created using Microsoft® PowerPoint® for Microsoft 365 MSO (version 2305). 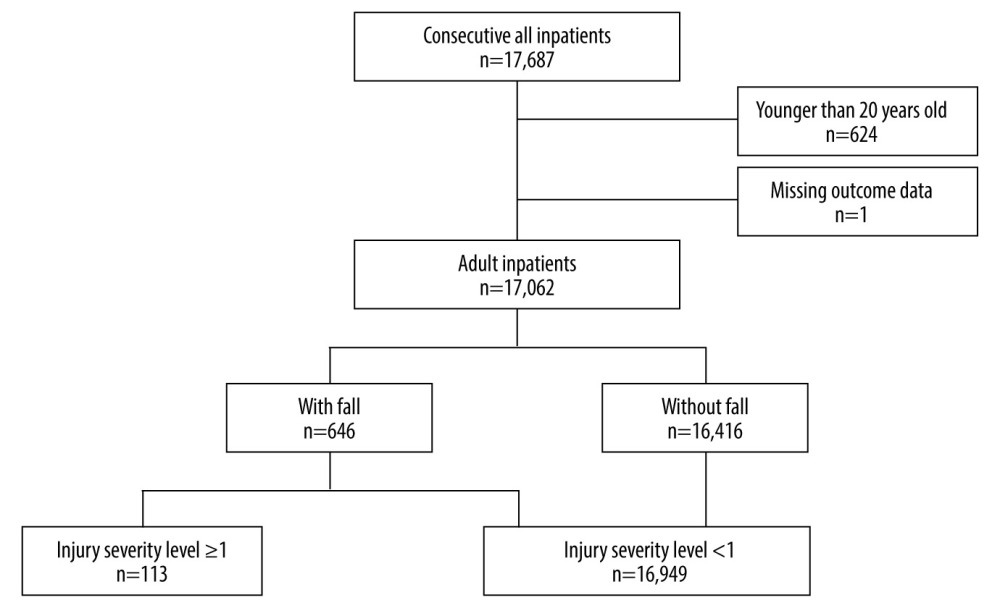 Figure 2. Data flow diagram. A total of 17 062 were eligible, of whom 646 fell; among these, 113 had an injury severity level of 1 or higher. This figure was created using Microsoft® PowerPoint® for Microsoft 365 MSO (version 2305).
Figure 2. Data flow diagram. A total of 17 062 were eligible, of whom 646 fell; among these, 113 had an injury severity level of 1 or higher. This figure was created using Microsoft® PowerPoint® for Microsoft 365 MSO (version 2305). 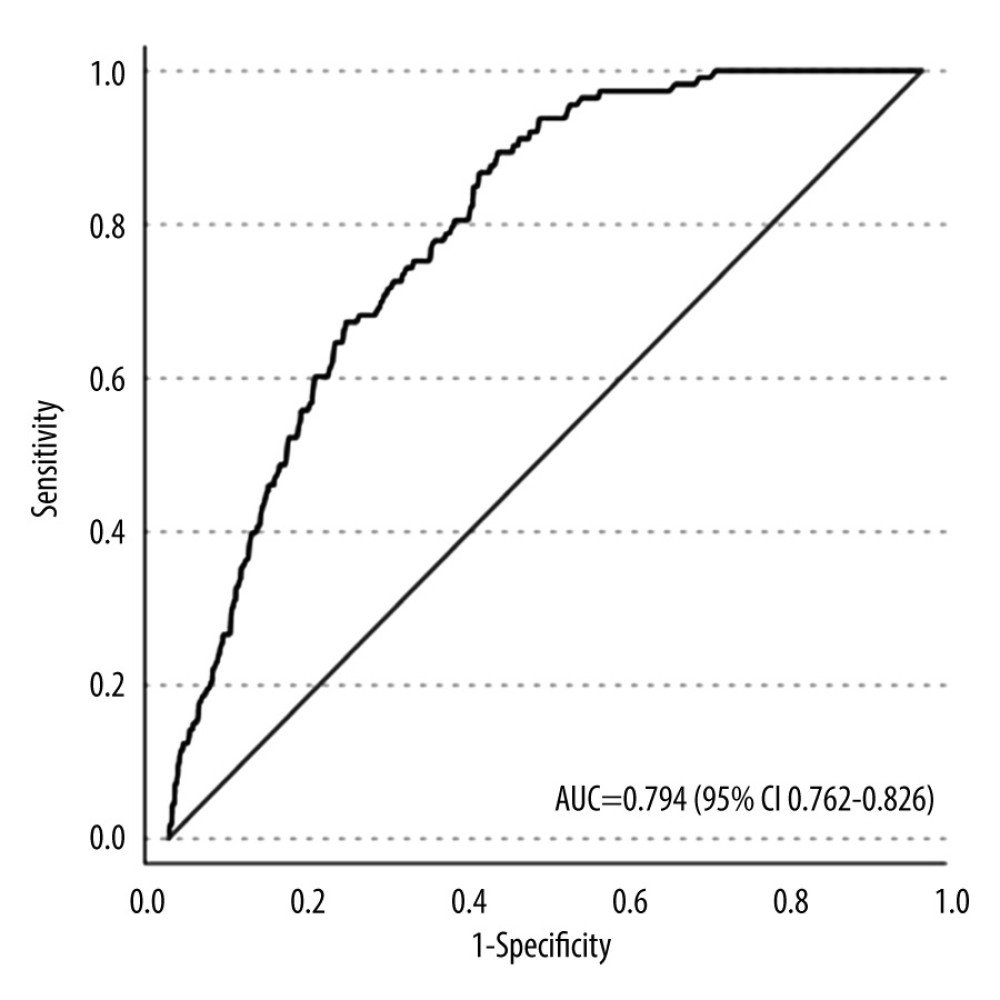 Figure 3. Receiver-operating characteristics. The performance of the predictive model, measured as area under the curve, was 0.794 (95% confidence interval 0.762–0.826). This figure was created using Microsoft® PowerPoint® for Microsoft 365 MSO (version 2305).
Figure 3. Receiver-operating characteristics. The performance of the predictive model, measured as area under the curve, was 0.794 (95% confidence interval 0.762–0.826). This figure was created using Microsoft® PowerPoint® for Microsoft 365 MSO (version 2305). 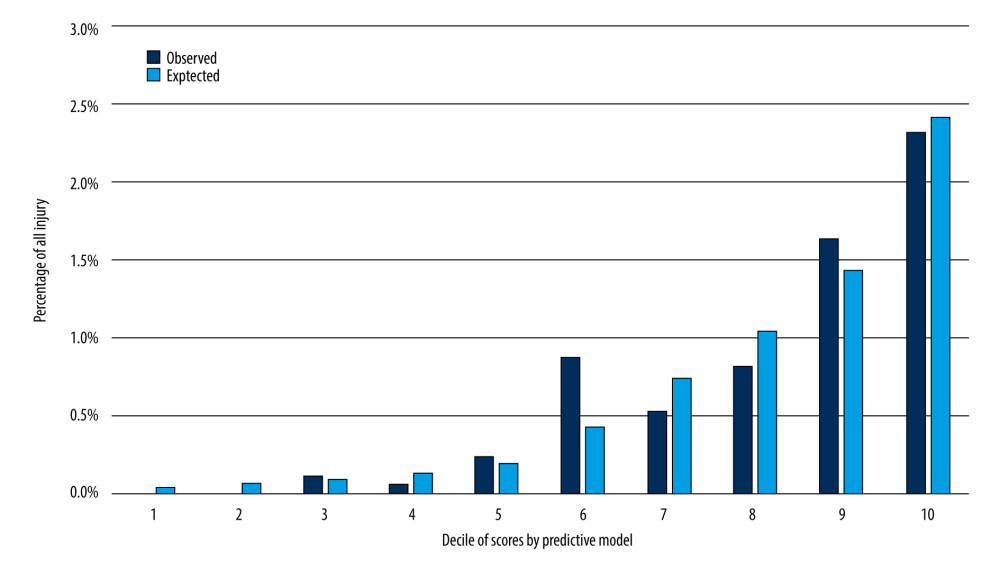 Figure 4. Observed and predicted rate of fall injury for each group of patients divided into 10 equal groups in the deciles of the calculated scores using the predictive model for fall injury. The gap between observed and predicted rates was not large for either group. Furthermore, the model was well calibrated, with a shrinkage coefficient of 0.955. This Figure was created using Microsoft® PowerPoint® for Microsoft 365 MSO (version 2305).
Figure 4. Observed and predicted rate of fall injury for each group of patients divided into 10 equal groups in the deciles of the calculated scores using the predictive model for fall injury. The gap between observed and predicted rates was not large for either group. Furthermore, the model was well calibrated, with a shrinkage coefficient of 0.955. This Figure was created using Microsoft® PowerPoint® for Microsoft 365 MSO (version 2305). Tables
Table 1. Entry criteria for reasons for falls and disability in the Maryland Hospital Association’s acute care indicators.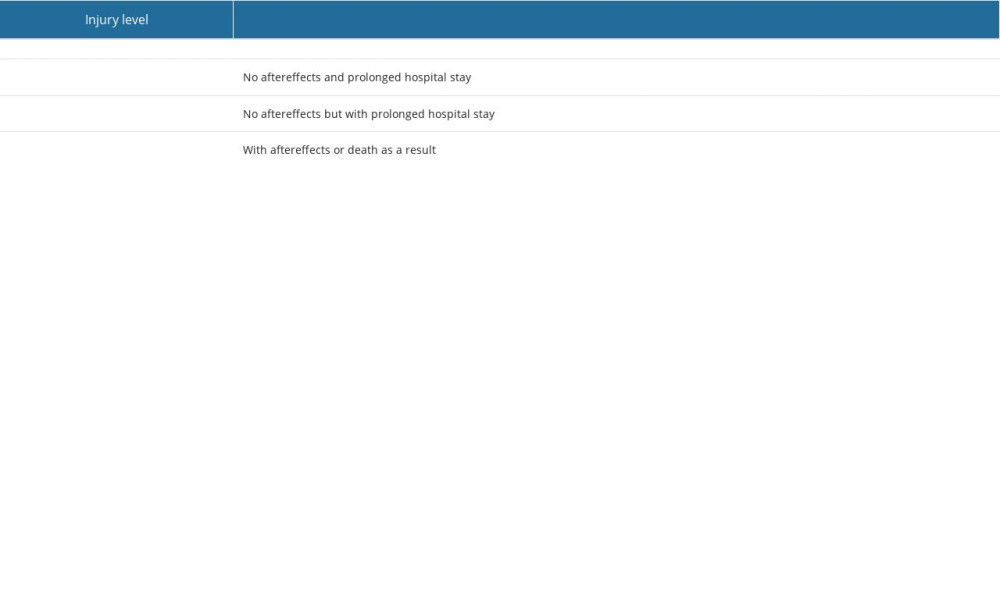 Table 2. Patients’ backgrounds with or without fall and the results of univariable analysis of chi-squared test.
Table 2. Patients’ backgrounds with or without fall and the results of univariable analysis of chi-squared test.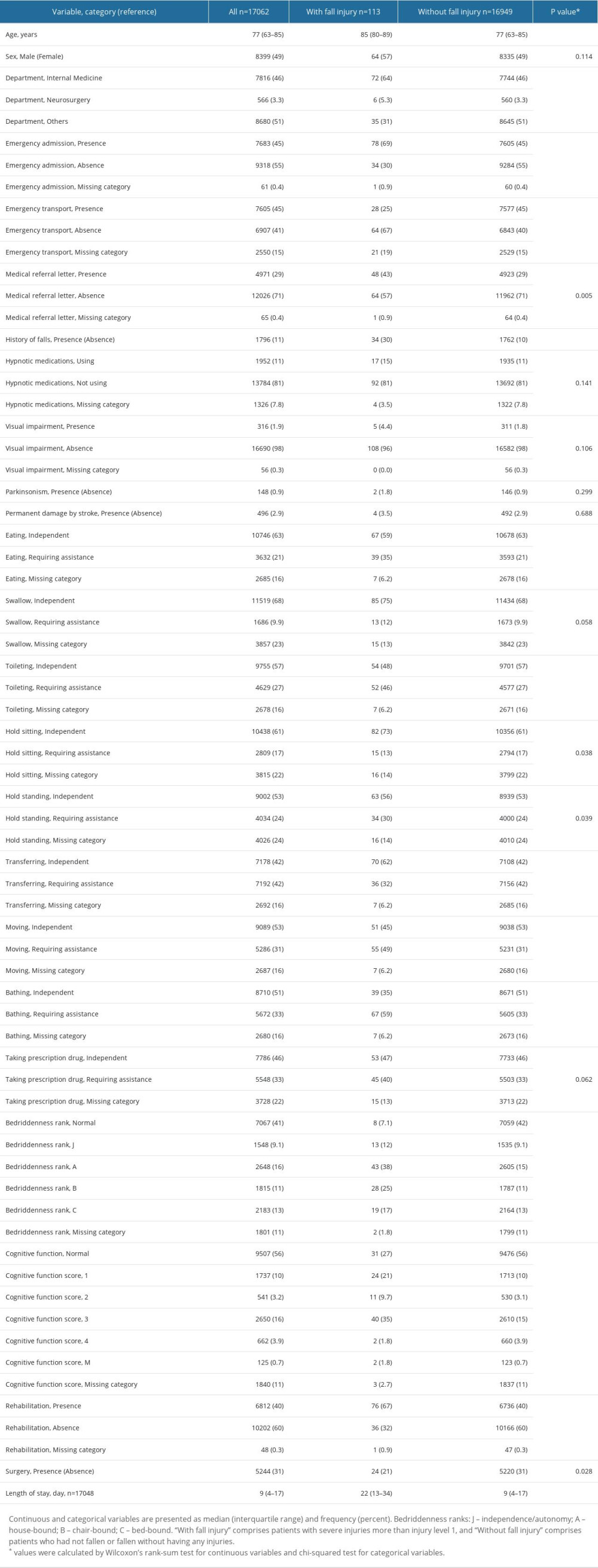 Table 3. Results of multivariable logistic regression analysis for fall injuries.
Table 3. Results of multivariable logistic regression analysis for fall injuries.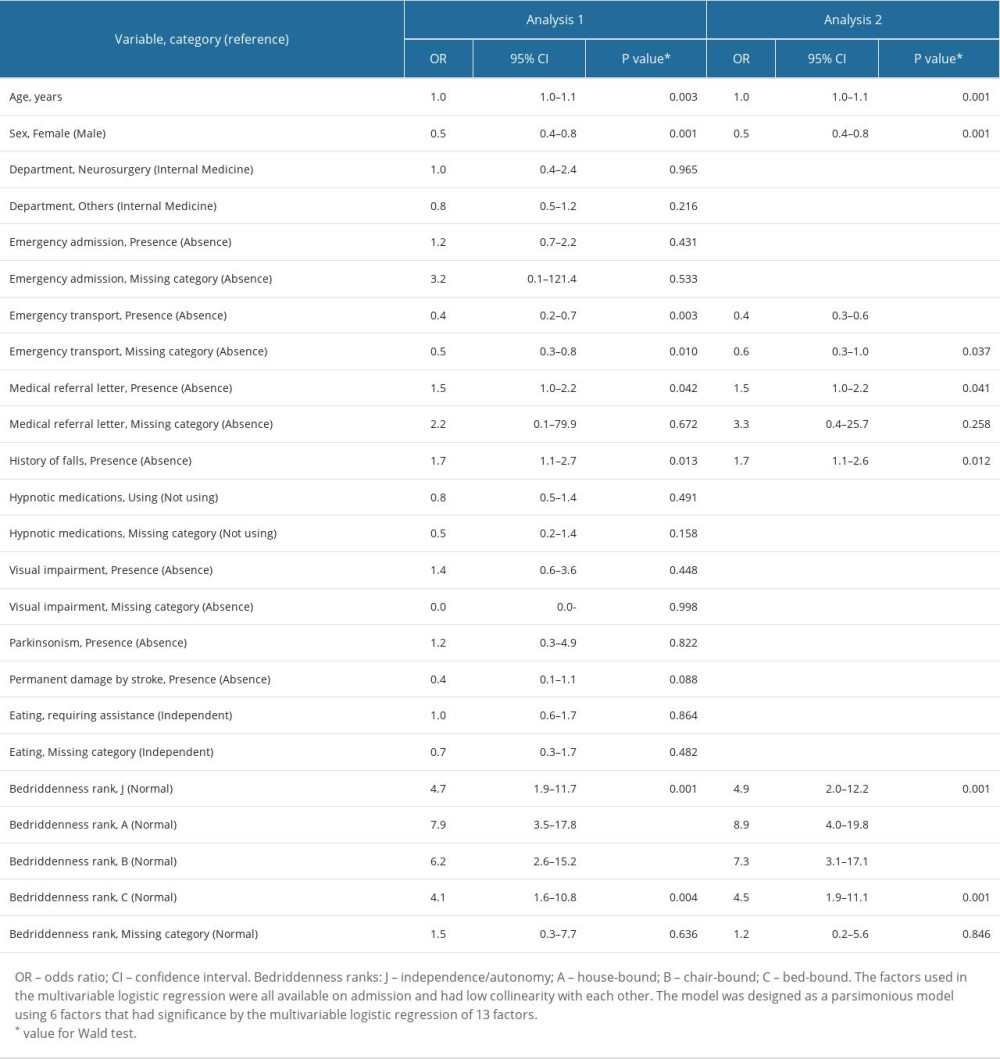
References
1. Burns ER, Stevens JA, Lee R, The direct costs of fatal and non-fatal falls among older adults – United States: J Safety Res, 2016; 58; 99-103
2. Egami K, Hirose M, Takemura T, Extra medical costs due to falls by using incident reporting and administrative profiling data at a teaching hospital in Japan: A retrospective case study: J Jpn Soc Heathcare Adm, 2011; 48; 157-69
3. Roudsari BS, Ebel BE, Corso PS, Molinari NA, Koepsell TD, The acute medical care costs of fall-related injuries among the U.S. older adults: Injury, 2005; 36(11); 1316-22
4. Hendrie D, Hall SE, Arena G, Legge M, Health system costs of falls of older adults in Western Australia: Aust Health Rev, 2004; 28(3); 363-73
5. Schwendimann R, Bühler H, De Geest S, Milisen K, Characteristics of hospital inpatient falls across clinical departments: Gerontology, 2008; 54(6); 342-48
6. Bates DW, Pruess K, Souney P, Platt R, Serious falls in hospitalized patients: Correlates and resource utilization: Am J Med, 1995; 99(2); 137-43
7. Stevenson DG, Studdert DM, The rise of nursing home litigation: findings from a national survey of attorneys: Health Aff (Millwood), 2003; 22(2); 219-29
8. Aihara H, Tago M, Oishi T, Visual impairment, partially dependent ADL and extremely old age could be predictors for severe fall injuries in acute care settings: Int J Gerontol, 2018; 12(3); 175-79
9. Choi K, Jeon GS, Cho SI, Prospective study on the impact of fear of falling on functional decline among community dwelling elderly women: Int J Environ Res Public Health, 2017; 14(5); 469
10. Thiamwong L, Suwanno J, Fear of falling and related factors in a community-based study of people 60 years and older in Thailand: Int J Gerontol, 2017; 11; 80-84
11. Shorr RI, Chandler AM, Mion LC, Effects of an intervention to increase bed alarm use to prevent falls in hospitalized patients: A cluster randomized trial: Ann Intern Med, 2012; 157(10); 692-99
12. Haines TP, Bell RA, Varghese PN, Pragmatic, cluster randomized trial of a policy to introduce low-low beds to hospital wards for the prevention of falls and fall injuries: J Am Geriatr Soc, 2010; 58(3); 435-41
13. Harada A, Mizuno M, Takemura M, Hip fracture prevention trial using hip protectors in Japanese nursing homes: Osteoporos Int, 2001; 12(3); 215-21
14. Aranda-Gallardo M, Morales Asencio JM, Canca-Sanchez JC, Group for preventing falls in Hospital Costa del Sol. Instruments for assessing the risk of falls in acute hospitalized patients: A systematic review protocol: J Adv Nurs, 2013; 69(1); 185-93
15. Curcio F, Basile C, Liguori I, Tinetti mobility test is related to muscle mass and strength in non-institutionalized elderly people: Age (Dordr), 2016; 38(5–6); 525-33
16. Hendrich AL, Bender PS, Nyhuis A, Validation of the Hendrich II Fall Risk Model: A large concurrent case/control study of hospitalized patients: Appl Nurs Res, 2003; 16(1); 9-21
17. Tago M, Katsuki NE, Oda Y, New predictive models for falls among inpatients using public ADL scale in Japan: A retrospective observational study of 7,858 patients in acute care setting: PLoS One, 2020; 15(7); e0236130
18. Hitcho EB, Krauss MJ, Birge S, Characteristics and circumstances of falls in a hospital setting: A prospective analysis: J Gen Intern Med, 2004; 19(7); 732-39
19. Mayo NE, Korner-Bitensky N, Levy AR, Risk factors for fractures due to falls: Arch Phys Med Rehabil, 1993; 74(9); 917-21
20. Fischer ID, Krauss MJ, Dunagan WC, Patterns and predictors of inpatient falls and fall-related injuries in a large academic hospital: Infect Control Hosp Epidemiol, 2005; 26(10); 822-27
21. Rapp K, Ravindren J, Becker C, Fall risk as a function of time after admission to sub-acute geriatric hospital units: BMC Geriatr, 2016; 16(1); 173
22. Tago M, Katsuki NE, Yaita S, High inter-rater reliability of Japanese bedriddenness ranks and cognitive function scores: A hospital-based prospective observational study: BMC geriatric, 2021; 21(1); 1-10
23. Kazandjian VA, Lawthers J, Cernak CM, Pipesh FC, Relating outcomes to processes of care: the Maryland Hospital Association’s Quality Indicator Project (QI Project): Jt Comm J Qual Improv, 1993; 19(11); 530-38
24. Cameron ID, Dyer SM, Panagoda CE, Interventions for preventing falls in older people in care facilities and hospitals: Cochrane Database Syst Rev, 2018; 9(9); CD005465
25. Kosaka K, Yamashita S, Ando C, Relationships among body mass index, activities of daily living and zinc nutritional status in disabled elderly patients in nursing facilities: J Nutr Sci Vitaminol, 2013; 59(5); 420-30
26. Kawase Y, Ogasawara T, Kawase S, Factors affecting the formation of membranous substances in the palates of elderly persons requiring nursing care: Gerodontology, 2014; 31(3); 184-93
27. Katz S, Ford AB, Moskowitz RW, Studies of illness in the aged. The Index of ADL: A standardized measure of biological and psychosocial function: JAMA, 1963; 185; 914-19
28. Mahoney FI, Barthel DW, Functional evaluation: The Barthel Index: Md State Med J, 1965; 14; 61-65
29. Neumann L, Hoffmann VS, Golgert S, In-hospital fall-risk screening in 4,735 geriatric patients from the LUCAS project: J Nutr Health Aging, 2013; 17(3); 264-69
30. Swartzell KL, Fulton JS, Friesth BM, Relationship between occurrence of falls and fall-risk scores in an acute care setting using the Hendrich II fall risk model: Medsurg Nurs, 2013; 22(3); 180
31. Oliver D, Daly F, Martin FC, McMurdo ME, Risk factors and risk assessment tools for falls in hospital in-patients: A systematic review: Age Ageing, 2004; 33(2); 122-30
32. Wong AH, Taylor RA, Ray JM, Bernstein SL, Physical restraint use in adult patients presenting to a General Emergency Department: Ann Emerg Med, 2019; 73(2); 183-92
33. Jöbges S, Mouton-Dorey C, Ricou B, Adult patients’ experience of coercion in intensive care: A scoping review: Research Square, 2021; 2021; rs.3.rs-396302/v1
Figures
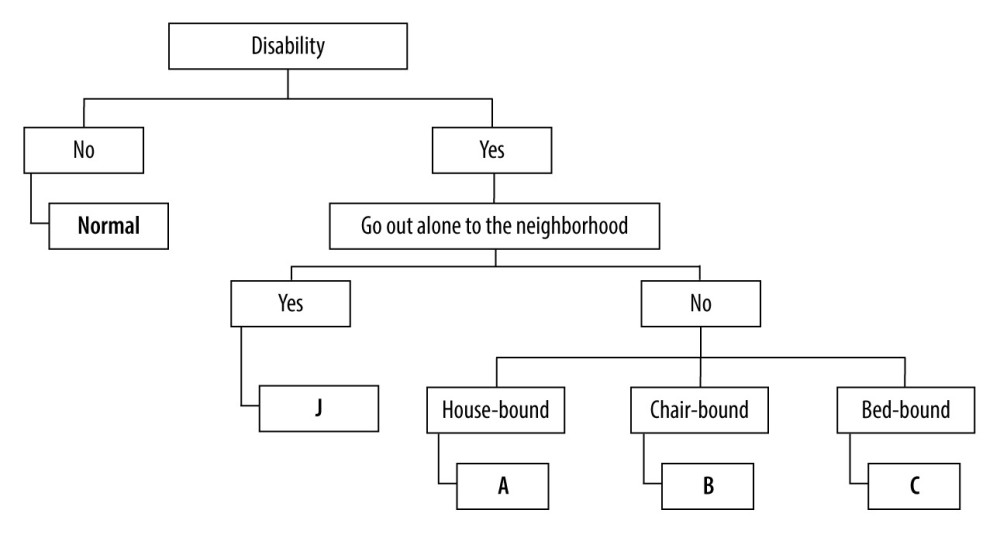 Figure 1. Flowchart for determining bedriddenness ranks. Bedriddenness ranks (BRs) is an official tool for assessing activities of daily living, which has been used widely under the long-term care insurance system in Japan. BRs are classified into 5 major categories (normal; J, independence; A, house-bound; B, chair-bound; C, bed-bound) by 3 steps. This figure was created using Microsoft® PowerPoint® for Microsoft 365 MSO (version 2305).
Figure 1. Flowchart for determining bedriddenness ranks. Bedriddenness ranks (BRs) is an official tool for assessing activities of daily living, which has been used widely under the long-term care insurance system in Japan. BRs are classified into 5 major categories (normal; J, independence; A, house-bound; B, chair-bound; C, bed-bound) by 3 steps. This figure was created using Microsoft® PowerPoint® for Microsoft 365 MSO (version 2305).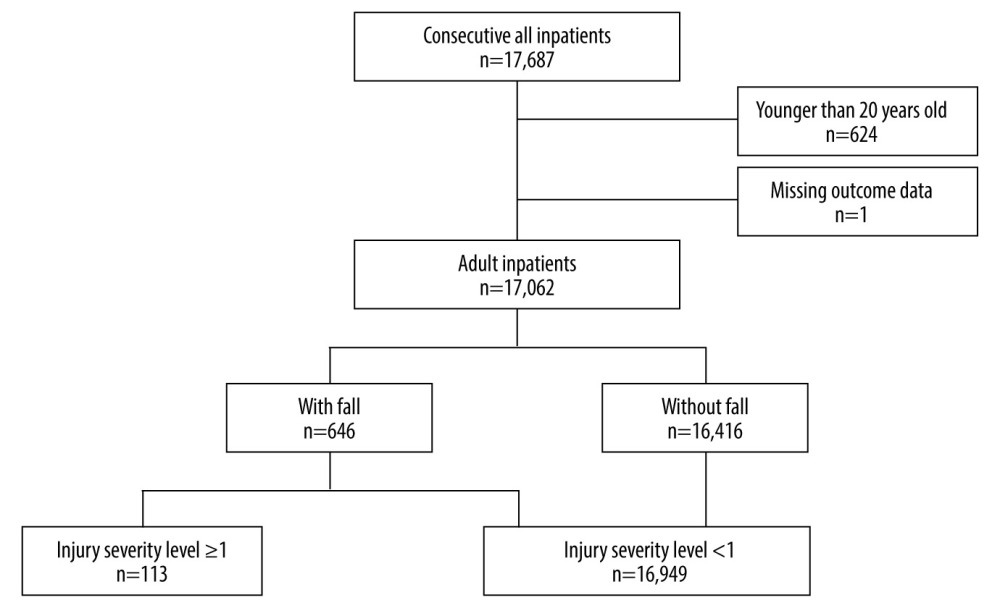 Figure 2. Data flow diagram. A total of 17 062 were eligible, of whom 646 fell; among these, 113 had an injury severity level of 1 or higher. This figure was created using Microsoft® PowerPoint® for Microsoft 365 MSO (version 2305).
Figure 2. Data flow diagram. A total of 17 062 were eligible, of whom 646 fell; among these, 113 had an injury severity level of 1 or higher. This figure was created using Microsoft® PowerPoint® for Microsoft 365 MSO (version 2305).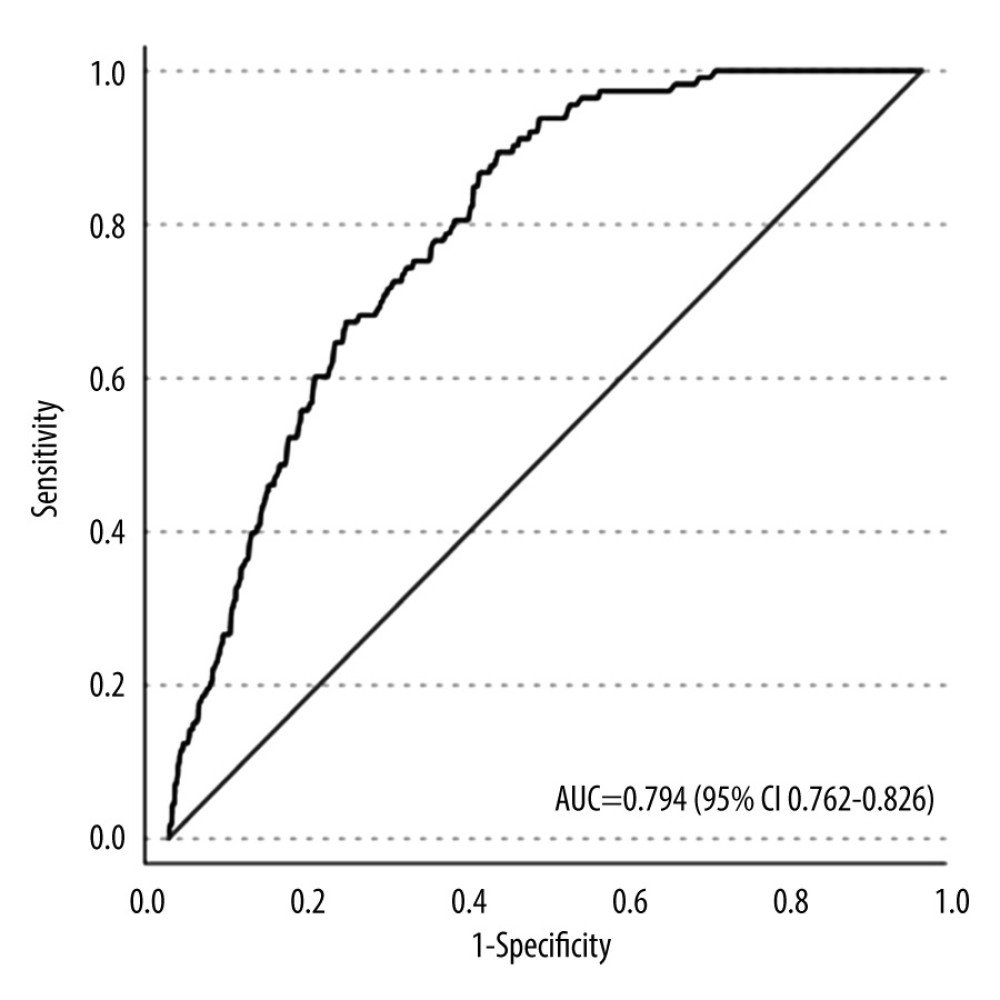 Figure 3. Receiver-operating characteristics. The performance of the predictive model, measured as area under the curve, was 0.794 (95% confidence interval 0.762–0.826). This figure was created using Microsoft® PowerPoint® for Microsoft 365 MSO (version 2305).
Figure 3. Receiver-operating characteristics. The performance of the predictive model, measured as area under the curve, was 0.794 (95% confidence interval 0.762–0.826). This figure was created using Microsoft® PowerPoint® for Microsoft 365 MSO (version 2305).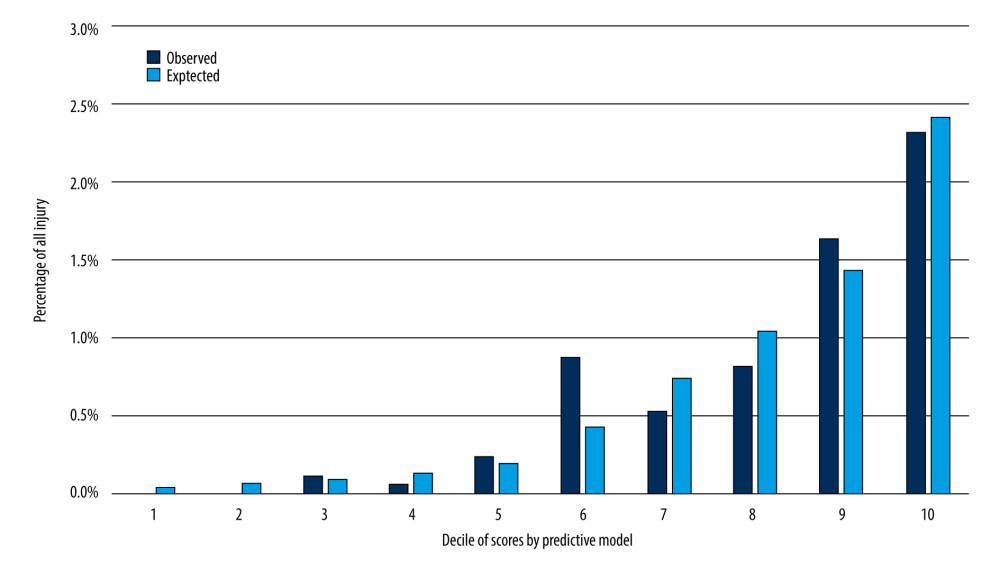 Figure 4. Observed and predicted rate of fall injury for each group of patients divided into 10 equal groups in the deciles of the calculated scores using the predictive model for fall injury. The gap between observed and predicted rates was not large for either group. Furthermore, the model was well calibrated, with a shrinkage coefficient of 0.955. This Figure was created using Microsoft® PowerPoint® for Microsoft 365 MSO (version 2305).
Figure 4. Observed and predicted rate of fall injury for each group of patients divided into 10 equal groups in the deciles of the calculated scores using the predictive model for fall injury. The gap between observed and predicted rates was not large for either group. Furthermore, the model was well calibrated, with a shrinkage coefficient of 0.955. This Figure was created using Microsoft® PowerPoint® for Microsoft 365 MSO (version 2305). Tables
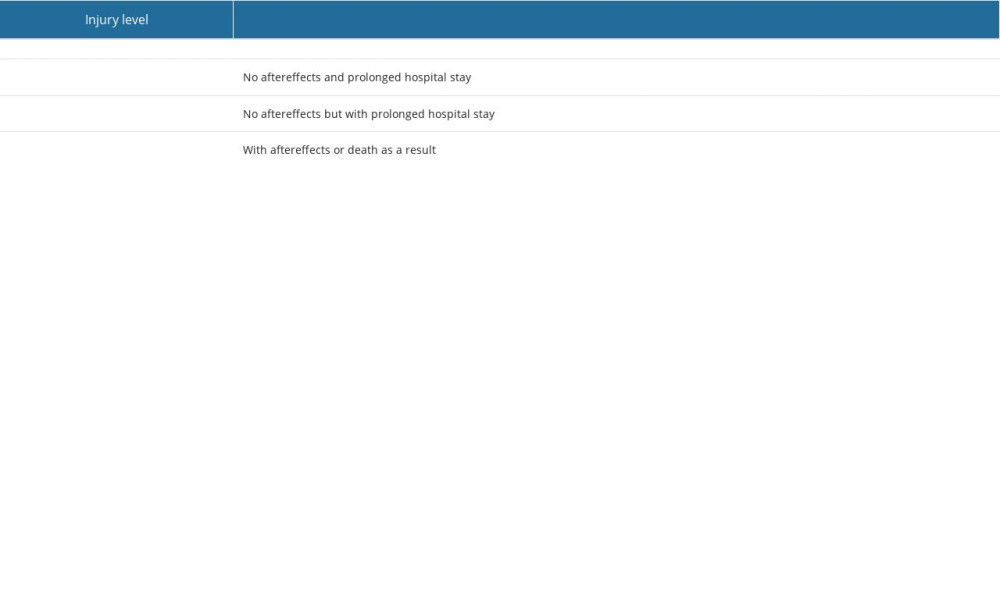 Table 1. Entry criteria for reasons for falls and disability in the Maryland Hospital Association’s acute care indicators.
Table 1. Entry criteria for reasons for falls and disability in the Maryland Hospital Association’s acute care indicators.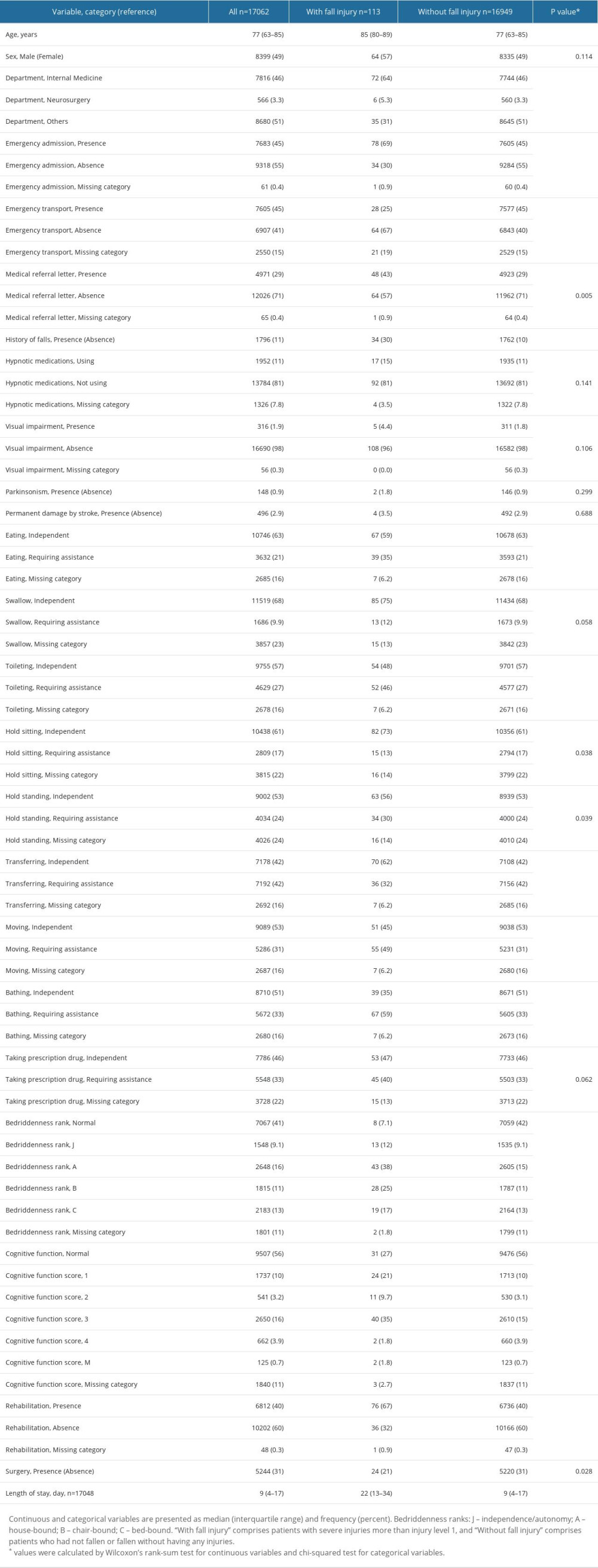 Table 2. Patients’ backgrounds with or without fall and the results of univariable analysis of chi-squared test.
Table 2. Patients’ backgrounds with or without fall and the results of univariable analysis of chi-squared test.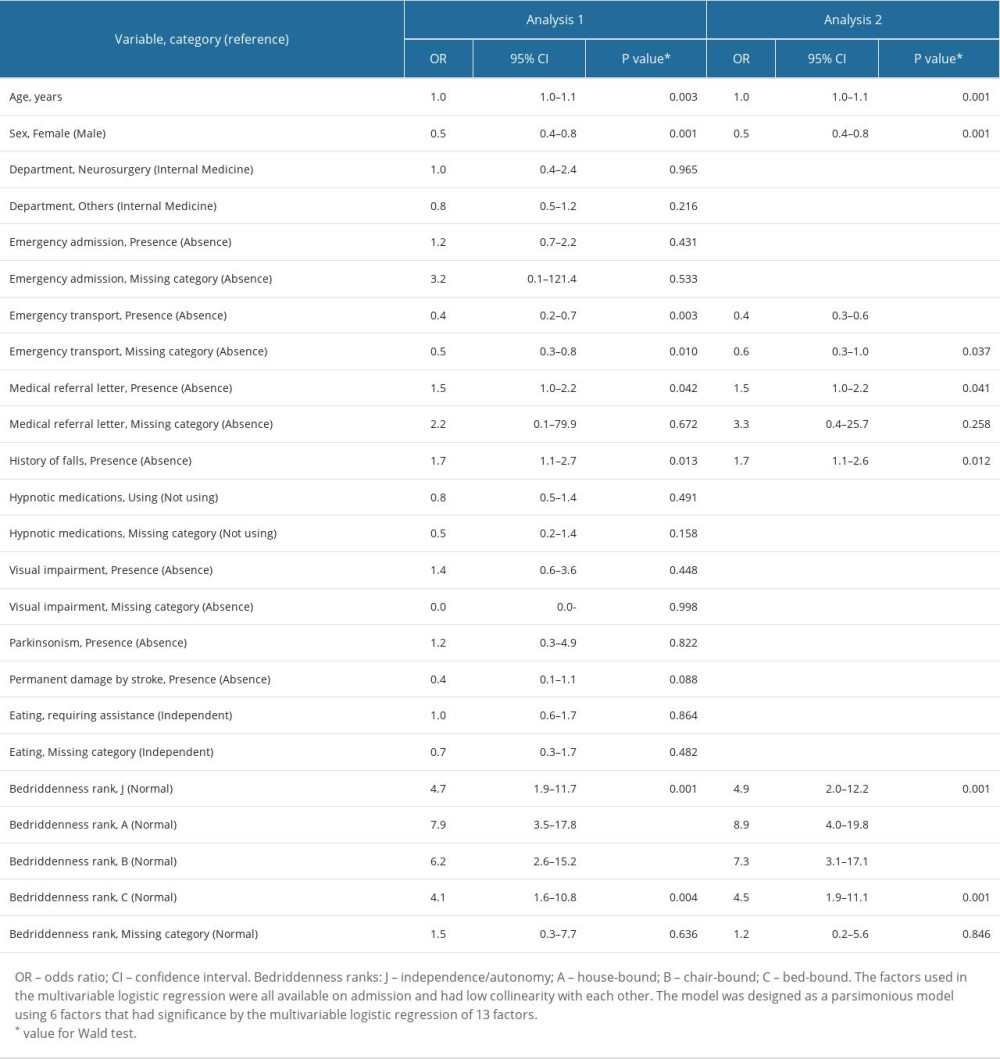 Table 3. Results of multivariable logistic regression analysis for fall injuries.
Table 3. Results of multivariable logistic regression analysis for fall injuries.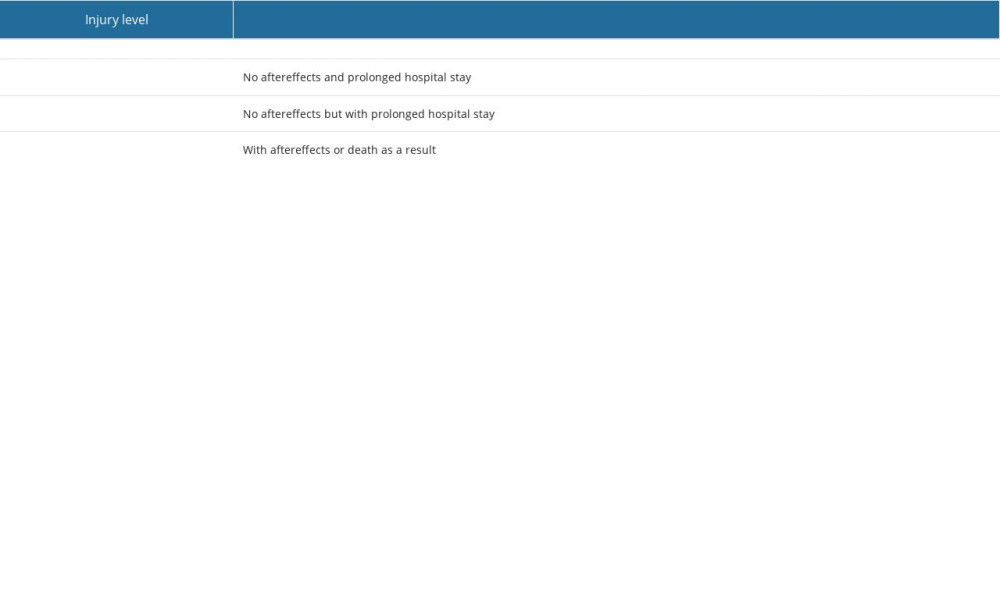 Table 1. Entry criteria for reasons for falls and disability in the Maryland Hospital Association’s acute care indicators.
Table 1. Entry criteria for reasons for falls and disability in the Maryland Hospital Association’s acute care indicators.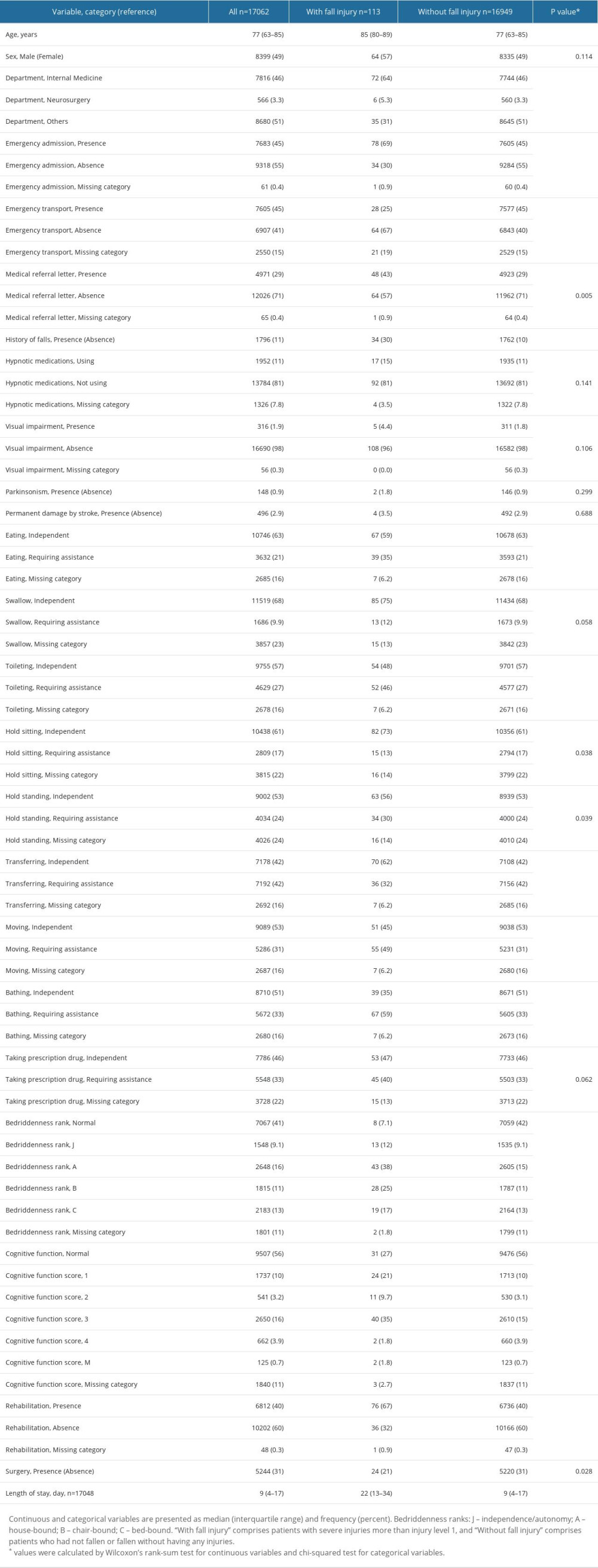 Table 2. Patients’ backgrounds with or without fall and the results of univariable analysis of chi-squared test.
Table 2. Patients’ backgrounds with or without fall and the results of univariable analysis of chi-squared test.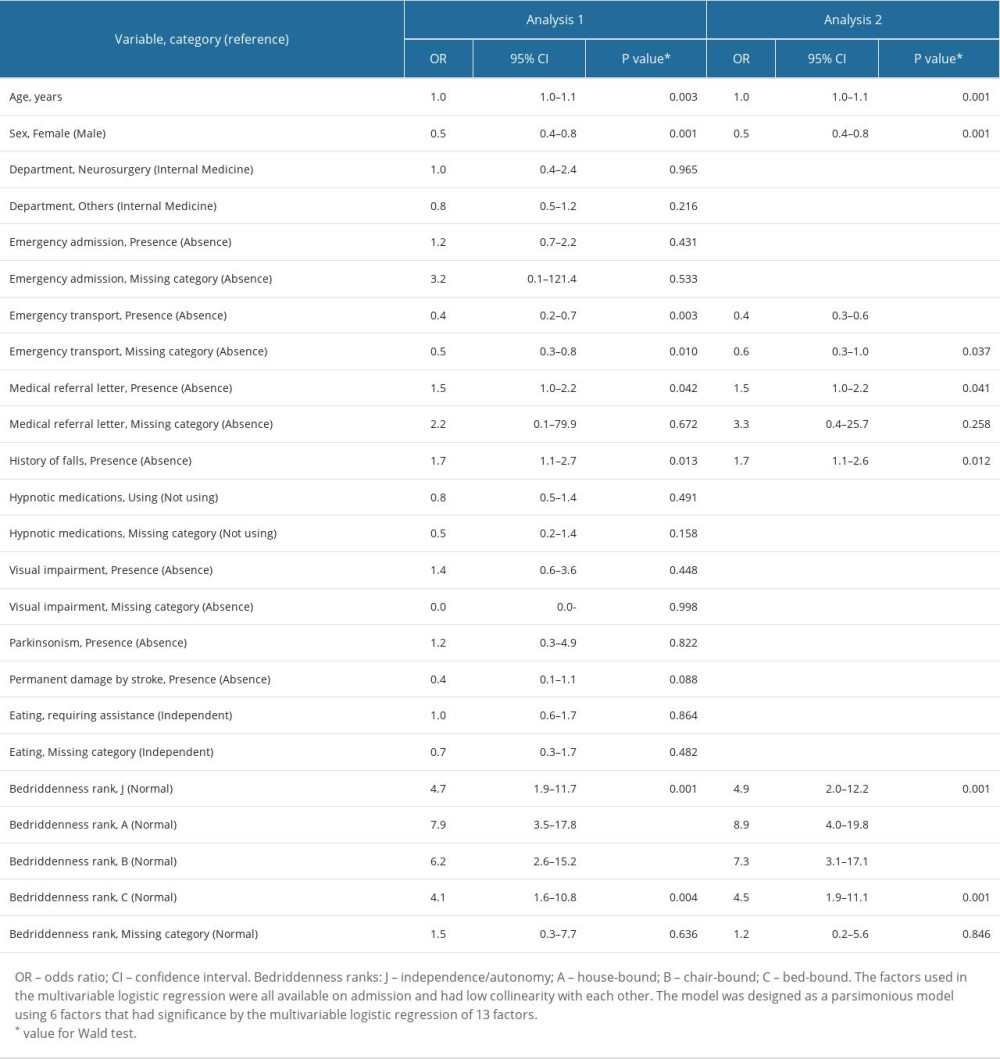 Table 3. Results of multivariable logistic regression analysis for fall injuries.
Table 3. Results of multivariable logistic regression analysis for fall injuries. In Press
12 Mar 2024 : Clinical Research
Metabolomic Alterations in Methotrexate Treatment of Moderate-to-Severe PsoriasisMed Sci Monit In Press; DOI: 10.12659/MSM.943360
14 Mar 2024 : Clinical Research
Renal Dysfunction Increases Risk of Adverse Cardiovascular Events in 5-Year Follow-Up Study of Intermediate...Med Sci Monit In Press; DOI: 10.12659/MSM.943956
15 Mar 2024 : Clinical Research
Impact of One-Lung Ventilation on Oxygenation and Ventilation Time in Thoracoscopic Heart Surgery: A Compar...Med Sci Monit In Press; DOI: 10.12659/MSM.943089
14 Mar 2024 : Clinical Research
Differential DHA and EPA Levels in Women with Preterm and Term Births: A Tertiary Hospital Study in IndonesiaMed Sci Monit In Press; DOI: 10.12659/MSM.943895
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








