11 August 2023: Clinical Research
Immediate Effects of Ankle Mobilization on Range of Motion, Balance, and Muscle Activity in Elderly Individuals with Chronic Ankle Instability: A Pre-Post Intervention Study
Sunmin KimDOI: 10.12659/MSM.941398
Med Sci Monit 2023; 29:e941398
Abstract
BACKGROUND: This study aimed to identify the immediate effect of applying ankle mobilization to the elderly with chronic ankle instability on the range of joint motion, balance, and lower extremity muscle activity.
MATERIAL AND METHODS: This study, the Cumberland Ankle Instability Tool (CAIT) was used to evaluate chronic ankle instability, and as a result, 65-year-olds with a score of 24 or less were conducted. In this study, the grade III of Maitland mobilization was used to increase the range of joint motion in older people with chronic ankle instability. And four joint mobilizations were administered for a total of 40 minutes, 10 minutes per run. In the pre-examination, the range of motion of ankle joints, balance, and lower extremity muscle activity in the Limit of Stability (LOS) position prior to ankle mobilization. The reexamination was taken a right after the intervention to see the immediate effect of applying joint mobilization. This study was conducted after receiving the approval of the Institutional Review Board of the Korea National University of Transportation.
RESULTS: The study results show that, as a result of applying the ankle mobilization intervention, the range of dorsi flexor and plantar flexor motion increased, resulting in the improvement of balance and an immediate effect on the lower extremity muscle activity when measuring the Limit of Stability.
CONCLUSIONS: The conclusion of this study is ankle mobilization may be a useful intervention method in preventing falls and improving balance in older adults with chronic ankle instability.
Keywords: Ankle Joint, Electromyography, Joint Instability, postural balance, Range of Motion, Articular, Humans, Aged, Ankle, Muscles
Background
A fall can occur at any age, but the elderly and those with mobility difficulties may be severely injured or even die because of complications from a fall [1]. Physical damage caused by a fall incurs a considerable cost to individuals, families, society, and the economy, and recent research has reported a steady increase in mortality from falls in older people [2]. Some falls in the elderly have a single cause, but most falls result from a combination of multiple causes. Age-related declines in vision, vestibular sense, proprioception, muscles, and reaction time result in loss of balance, which increases the risk of falls [3]. Although older people generally go have reduction of postural control and an increase of body shaking, the relationship between simultaneous contraction of muscles and balance ability is unclear. However, simultaneous contractions of adequate muscles are important factors for maintaining posture [4]. Clinically, limiting the range of motion in older people’s joints is the primary cause of lifestyle restriction and structural defects in older people, and is associated with reduced balance and falls due to age-related decline in proprioception [5]. Although it is difficult to eliminate all these various causes of risk, modifying 1 risk factor may be a valuable therapeutic goal to reduce the fall risk in the elderly [6]. Many previous studies have shown that movement of the foot, ankle joints, and soles plays a crucial role in balance and gait [7]. Elderly people who have had falls often have a severe decline in ankle muscle mass and have impaired balance. Among distal muscles, the dorsiflexor is the biggest risk factor for a fall, and falls can be predicted by the strength of the dorsiflexor [8]. The range of motion of ankle joints tends to decrease with aging, so the range of motion of the ankle joints in dorsiflexion, plantar flexion, inversion, and eversion also decreases with aging [9]. Previous studies have reported that causes of falls in older people include dorsiflexor weakness [10] and reduced ankle joint range of motion [11], and depending whether the patient had fallen, there was a statistically significant difference in dorsiflexor strength [12], lower extremity muscles [13], and balance ability [14]. Holland (2002) [15] also reported that the range of motion of the ankle dorsiflexor decreased by 6 degrees in the elderly compared to younger people, and as the range narrows, dynamic balance and postural control ability decreases, increasing the risk of falls [16]. In addition to falls, older people also tend to have chronic ankle instability and frequent sprained ankles, caused by chronic weakness of ligaments due to repeated injury to the ankle joints. This reduces the range of motion of ankle dorsiflexors and dynamic balance, leading to recurrent ankle injury and had a negative impact on movement control of peripheral nerves, thereby increasing the risk of falls [17].
Although 80% of acute ankle sprains of the elderly fully recover through conservative treatment, 20% develop into chronic ankle instability (CAI), in which repeated ankle injury occurs due to the lack of normal recovery of the initial treatment and rehabilitation after acute injury [18]. There are 2 leading causes of ankle instability. First, mechanical instability arises either via an acute injury or chronic repetitive stress resulting in attenuation and alteration of the mechanical structures of the ligaments. The most common mechanism of injury in lateral ankle sprain occurs with a plantar flexion force on an inverted ankle as the body moves over the foot. Second, functional instability is the feeling of ankle instability or recurrent symptomatic ankle sprains due to proprioceptive deficits. Functional classification divides ankle instability into 3 grades. In Grade I the patient can fully bear weight and walk, in Grade II the patient walks with a noticeable limp, and in Grade III the patient is unable to walk. In this study, we aimed to improve the functional ankle instability grade to Grade I by applying ankle joint mobilization [19]. Patients with chronic ankle instability have structural problems of the tarsal bone and damage to various structures such as the joint capsule, nerves, ligaments, and tendons. As a result, coordination ability and postural control ability are reduced, resulting in a decline in balance [20]. For these reasons, the range of movement of the foot and ankle joints is critical for balance and mobility, and Mechagni (2000) [6] reported a significant correlation between the range of movement of joints and balance. Recent literature on the management of ankle instability includes rest, ice, elevation, compression, initial range of motion, progressive weight-bearing guided by symptom tolerance, and physical therapy. Even with proper functional rehabilitation, 10–40% of patients go on to develop chronic ankle instability following acute ankle sprains. Multiple studies have shown the benefits of conservative therapy as well as surgical treatment for cases that do not adequately respond to conservative treatment [19]. Many previous studies show that the normal range of motion of ankle joints is the most critical factor to prevent a fall with maintaining balance. From this point of view, the intervention that can improve these factors is expected to contribute significantly to preventing falls in the elderly. Ju (2011) [21] reported that the use of ankle mobilization in older men resulted in an improved range of motion of ankle joints and balance ability, which helped prevent falls and improved balance in older people. Hoch (2011) [16] also reported that joint mobilization enhances neuromuscular function that contributes to activating afferent information and joint stabilization, which improves postural control and stimulates cutaneous receptors to increase activation of sensory input information and joint mobility, leading to the improvement of the body’s postural control. Previous studies reported that intervening with Talocrural and Subtalar Joint Mobilization in the elderly immediately improves the range of joint motion [7]. Many interventions have been recently studied to prevent falls in older people, including strengthening muscles, increasing flexibility, cardio, and balance training programs [22]. The application of therapy to improve mobility in the foot, ankle joints, and soles may increase the expansibility of noncontractile capsules and ligament tissues and stimulate the mechanoreceptor in the joints, improving the transfer of afferent information. An improved range of joint motion also promotes postural control and improves balance [7]. However, there have been few studies on interventions to improve mobility, and most studies have had a limited duration of intervention. Few studies have found immediate effects of ankle mobilization. The purpose of this study was to verify the immediate effect on ankle joint range of motion balance and muscle activity when Maitland joint mobilization Grade III was applied to 10 patients with chronic ankle instability with a score of 24 or less on the Cumberland Ankle Instability Tool.
Material and Methods
SUBJECTS:
The selection of participants in this study was conducted after approval by the Institutional Review Board, and subjects who agreed to participate in the study proceeded after receiving explanations about the purpose and experimental method of this study. Consent to participate in the study was obtained by signing the research participation consent form. We selected people aged 65 years or older with chronic ankle instability, staying at hospital S in Cheongju City, Korea (Table 1). The criteria for selection and exclusion of subjects were: scores lower than 24 using the Cumberland Ankle Instability Tool (CAIT), which measures ankle instability; those who have experienced ankle sprain and suffered a recurrent ankle injury at least once; or who currently do not receive a therapeutic intervention. We excluded those who experienced ankle damage within the last 3 months, who had a pathological ankle condition, or had orthopedic problems other than ankle sprain. Out of the 13 individuals who were willing to participate in the study after being informed about the purpose and methods of the study, a total of 10 subjects were selected after excluding 3 who had CAIT scores of 24 or more.
PROTOCOL:
Talocrural joint anteroposterior mobilization and Talocrural joint posteroanterior mobilization were applied to improve dorsiflexion and plantar flexion of ankle joints, while Subtalar joint mediolateral mobilization and Subtalar joint lateromedial mobilization were applied to improve inversion and eversion. The Maitland mobilization technique was applied, which is used to relieve pain and increase the flexibility of joints and connective tissues around joints. The Maitland mobilization grade ranges from I–IV, and Grade I refers to the intensity of very small oscillations applied at the beginning of the joint range of motion with no load on the connective tissue. It is often used for severe pain. On the other hand, Grade II indicates the strength to which a slightly larger oscillation is applied and is applied from the start point to the midpoint of the joint range of motion. Grades I and II have the effect of stimulating mechanoreceptors and thus reduce joint pain by limiting harmful stimuli. Grade III applies to large oscillation at the midpoint of the joint range of motion, and application starts at the joint range of motion limit point. Finally, Grade IV is applied for tissue resistance at small oscillations with a limited range of joint range of motion. Grades III and IV are used to provide a stretching effect by increasing the range of motion of the joint, which functions to relieve shortened tissue stiffness [23]. In this study, the subject lay down on a flat mat with the applied ankle slightly protruding off of the mat. After fixing the intervening leg with a strap, the therapist holds the anterior part above the ankle with one hand and holds the anterior part of the talus bone between the thumb and forefinger with the other hand, and applies glide from anterior to posterior direction. The sliding in the medial direction and the lateral posterior direction changes the patient’s lying position and applies the same [24]. The pre-examination assesses the range of motion of ankle joints, balance, and lower extremity muscle activity in the Limit of Stability (LOS) position prior to ankle mobilization. The reexamination was performed right after the intervention to assess the immediate effect of applying joint mobilization. Ankle mobilization was performed by a skilled physical therapist with more than 10 years of physiotherapy experience, and 4 joint mobilizations were administered for a total of 40 minutes, 10 minutes per run. This study was conducted after receiving the approval of the Institutional Review Board of the Korea National University of Transportation (approval number KNUT IRB 2022-82).
TALOCRURAL JOINT A-P MOBILIZATION: The patient is in the supine position, and the therapist stands at the side of the patient’s feet. The backside of the calves is on the bed and the ankle joint is placed over the edge of the bed, and the therapist applies the Grade III Maitland mobilization by moving the heel down with the toes on the floor (Figure 1).
TALOCRURAL JOINT P-A MOBILIZATION: The patient is lying prone on the therapy bed while the therapist stands on the side of the patient’s feet. The patient’s tibia and talus are fixed on the therapy bed, and the therapist fixes the patient’s foot sole with the left hand. The therapist uses the right hand to hold the patient’s foot with the therapist’s index finger on the talus with the left hand on the calcaneus. The therapist then applies Grade III Maitland mobilization by slightly bending the knee joint and pushing the talus forward (Figure 2).
SUBTALAR JOINT M-L MOBILIZATION: The patient is in the lateral position, and the therapist is in a standing position toward the sole to be treated. With the lateral sides of the calf and talus on the bed, the joint below the talus is placed in the open pack position, and the talus is fixed on the therapy bed. The therapist applies Grade III Maitland mobilization by holding the patient’s instep with the left hand, and holding the back calcaneus that is the closest to the joint cleft with the right hand and pulling it toward the fibula (Figure 3).
CUMBERLAND ANKLE INSTABILITY TOOL (CAIT): The Cumberland Ankle Instability Tool is the questionnaire that scored the extent of ankle instability for the first time, consisting of 9 questions. Scores 0 to 3 are allotted to 5 questions, 0 to 4 are allotted to 2 questions, 0 to 5 are allotted to one question, and 0 to 2 are allotted to one question. The total score is 30 points, and more than 28 points mean stable ankles, while less than 24 points mean ankle instability. This questionnaire has sensitivity is 82.9% and a specificity is 74.7%. Test-retest reliability was excellent (ICC=.96). CAIT is, therefore, a simple, valid, and reliable tool to measure the severity of functional ankle instability [25].
ASSESSMENT OF THE RANGE OF MOTION OF ANKLE JOINTS (CLINOMETER): The measurement of the active ankle dorsiflexion and plantar flexion angles was based on a study that showed a strong correlation between them and the Goniometer, the criterion standard method of measuring joint angles. We used the smartphone application, Clinometer (Clinometer + bubble level, PlaincordTM, Stephanskirchen, Germany), to measure joint angles. The subject is in the supine position, and we put the smartphone on the lateral side of the fifth metatarsal bone and measured the dorsiflexion and plantar flexion angles by displaying active movement in the sagittal plane. The measurement of ankle joint angles using the smartphone application is a useful assessment tool that has proven reliability (r=.80) and validity (r=.83) [26] (Figure 5).
BT-4 (PSA, PSL, LOS): We measured postural sway area (PSA), postural sway length (PSL), and limit of stability (LOS) values using the BT-4 (Hur lab, Finland), a balance measurement system, to measure balance ability. The values of PSA and PSL are the main result values used in static balance ability and mean the area (mm2) where the movement path line is drawn for postural fluctuations at the center of pressure. The LOS value is the maximum movement distance when moving the body in a standing posture. The BT-4 balance measurement system has a rectangular shape and has measurement sensors at both ends to measure the center of pressure (COP), PSA, and PSL over time. This equipment analyzed and measured all data using Smart-suit Balance software 1.4. The subjects were standing on the BT-4 platform, with feet 2 cm apart and feet facing outward at a 15-degree angle. In addition, the hands were naturally positioned, and in this study, the static balance was measured at 30 degrees with the eyes closed. It is interpreted that the better the static balance, the lower the PSA and PSL values, and the worse the static balance, the higher the PSA and PSL values [27]. In the evaluation of dynamic balance ability, each subject’s LOS value was measured while leaning forward, backward, left, and right without moving the feet in a standing position. It is interpreted that the better the dynamic balance ability, the higher the range of movement value, and the worse the dynamic balance ability, the lower the range of movement value (Figure 6).
WIRELESS SURFACE EMG SYSTEM (FREEEMG1000, BTS): The wireless surface EMG system (freeEMG1000, BTS bioengineering, Milano, Italy) was used to measure muscle activity of the tibialis anterior muscle and gastrocnemius muscle. The sampling rate of the signal is set to 1024 Hz. We used a 60 Hz notch filter and a 30 to 500 Hz band pass filter to minimize noise. The collected signals were processed by root mean square (RMS) and the electrodes to the tibialis anterior muscles are attached outward from the medial shaft of the tibia with a 2 cm horizontal space. The calves EMG electrodes were also placed under the knees, 2 cm from the medial and lateral sides of the centerline behind the back calves, to place the electrodes on the medial and lateral gastrocnemius muscle fibers. When measuring the LOS value, the muscle activity of the tibialis anterior muscle and gastrocnemius muscle was measured during forward, backward, leftward, and rightward movement. Out of muscle activities measured for 5 seconds, the muscle activity values for 3 seconds were extracted, excluding 1 second from the start and 1 second from the end (Figure 7).
STATISTICAL METHODS:
The SPSS Win. 21.0 Package was used to process and analyze collected data in this study. The Kolmogorov-Smirnov test was used to verify the normality, and the chi-squared test was used to compare the subjects’ general characteristics. Data collection in this study was performed before and after Maitland joint mobilization. The matching sample
Results
CHANGES IN POSTURAL SWAY AREA AND LENGTH ACCORDING TO THE INTERVENTION:
Changes in static balance (PSA, PSL) after applying ankle mobilization to elderly patients with chronic ankle instability are as follows (Table 2). With eyes open, the PSA value decreased significantly from 254.31 mm2 before mobilization to 213.91 mm2 after mobilization, showing a meaningful increase of static balance (P<.01), and the PSL value decreased significantly from 332.62 mm before mobilization to 305.57 mm after mobilization, showing a meaningful increase of static balance (P<.05). With eyes closed, the PSA value decreased significantly from 457.53 mm2 before mobilization to 380.34 mm2 after mobilization, showing a meaningful increase of static balance (P<.01), and the PSL value decreased significantly from 553.28 mm before mobilization to 496.34 mm after mobilization, showing a meaningful increase of static balance (P<.05).
CHANGES IN LIMIT OF STABILITY (LOS) ACCORDING TO THE INTERVENTION:
Changes in dynamic balance (LOS) after applying ankle mobilization to elderly patients with chronic ankle instability are as follows (Table 2). The forward stability limit (FLOS) value increased from 3.23 mm before joint mobilization to 3.53 mm after joint mobilization, but there was no statistically significant difference (P>.05). The backward stability limit (BLOS) value increased from 2.77 mm before joint mobilization to 3.00 mm after joint mobilization, and there was a statistically significant difference (P<.01), and the left limit of stability (LLOS) value increased from 3.47 mm before joint mobilization to 3.95 mm after joint mobilization, and there was a statistically significant difference (P<.05). On the other hand, the right limit of stability (RLOS) value decreased from 3.85 mm before mobilization to 3.80 mm after mobilization, with no significant difference (P>.05).
CHANGES IN ANKLE ROM FOLLOWING INTERVENTION:
Changes in the range of motion of ankle joints (ROM) after applying ankle mobilization to the elderly with chronic ankle instability were as follows (Table 3). The range of motion of the left dorsiflexor significantly increased from 5.55° before mobilization to 10.33° after mobilization (P<.01), and the range of motion of the right dorsiflexor significantly increased from 9.03° before mobilization to 12.58° after mobilization (P<.001). The range of motion of the left plantar flexor significantly increased from 25.47° before mobilization to 32.91° after mobilization (P<.001), and the range of motion of the right plantar flexor significantly increased from 28.47° before mobilization to 33.02° after mobilization (P<.001).
CHANGES IN MUSCLE ACTIVITY FOLLOWING INTERVENTION:
Changes in the muscle activity of the tibialis anterior muscle and gastrocnemius muscle in the LOS measuring position after applying ankle mobilization to elderly patients with chronic ankle instability were as follows (Table 4). When measuring the FLOS, the muscle activity of the tibialis anterior muscle increased significantly from 36.75 μV before mobilization to 41.35 μV after mobilization, and the muscle activity of the gastrocnemius muscle also increased significantly from 28.03 μV before mobilization to 33.71 μV after mobilization (P<.001). When measuring the BLOS, the muscle activity of the tibialis anterior muscle increased significantly from 36.41 μV before mobilization to 43.61μV after mobilization, and the muscle activity of the gastrocnemius muscle also increased significantly from 28.45 μV before mobilization to 32.82 μV after mobilization (P<.01). When measuring the LLOS, the muscle activity of the tibialis anterior muscle increased from 35.06 μV before mobilization to 38.72 μV after mobilization, showing a widened range of joint motion, but there was no significant difference (P>.05). The muscle activity of the gastrocnemius muscle increased significantly from 26.70 μV before mobilization to 30.39 μV after mobilization (P<.001). When measuring the RLOS, the muscle activity of the tibialis anterior muscle increased from 36.96 μV before mobilization to 38.44 μV after mobilization, showing an increased range of joint motion, but there was no significant difference (P>.05). The muscle activity of the gastrocnemius muscle increased significantly from 26.87 μV before mobilization to 32.11 μV after mobilization (P<.001).
CHANGES IN CAIT FOLLOWING INTERVENTION:
Changes in scores of the CAIT, the tool to assess functional ankle instability, after applying ankle mobilization to elderly patients with chronic ankle instability were as follows (Table 5). The CAIT score increased significantly from 18.40 before mobilization to 25.40 after mobilization (P<.001).
Discussion
Given the qualitative aspects of the life of the elderly in the aging society of Korea, physical functioning is a very important factor in living an independent life. However, falling is a major health problem that leads to physical injuries like fractures, dysfunction, and death in the elderly, limiting their activity, affecting their ability to live independently, and restricting their social activities due to fear of falling. Although there are many causes falling, the range of joint motion is considered the most important factor related to ankle joint stability [28], and functional ankle instability leads to recurrent sprains and reduced balance [29]. For this reason, this study aimed to provide basic information for prevention of falls in older people by identifying the immediate impact of applying ankle mobilization to elderly patients with chronic ankle instability on the range of motion, balance, and lower extremity muscle activity. The elderly’s vision in balance control, vestibular sense, and proprioceptive sense decline due to aging, and it is quite difficult to artificially improve the senses in the balance control system. The study also aimed to apply ankle mobilization and improve the range of motion of ankle joints and balance control, focusing on the epidemiological changes from a normal range of joint motion [30] due to the joint dysfunction caused by reduced functions in the musculoskeletal system. According to this study, the BT-4 balance measurement system measures static balance by conducting the Romberg’s test with eyes open and closed. As a result of applying ankle mobilization to older people with chronic ankle instability, the PSA and PSL values significantly decreased, showing the improvement of static balance. This is consistent with the results of previous studies, and Ju (2011) [21] reported that the use of ankle mobilization in older people resulted in improved range of motion of ankle joints and balance, which helped prevent falls and improve balance in older people. It is considered that the increased ankle mobility through ankle mobilization prevents older people with a reduced range of motion of ankle joints from having alternative motion patterns to complement the balance, improving their balance ability.
This study measured the dynamic balance using the BT-4 balance measurement system to measure the FLOS, BLOS, LLOS, and RLOS after applying ankle mobilization. The FLOS value showed improvement of the range of motion, but there was no statistically significant difference (
The immediate changes in the range of motion of ankle joints after applying the ankle mobilization include meaningful increases in dorsiflexion and plantar flexion on both feet. Chevutschi (2014) [7] researched the immediate effect of the intervention of Talocrural and Subtalar Joint Mobilization in the elderly on the range of joint motion, reporting that there was an immediate improvement in the range of joint motion, which is consistent with this study’s results. It was also reported that widening the range of dorsiflexor motion in patients with chronic ankle instability contributes to the dynamic balance [17]. It is believed that the widened range of motion of ankle joints would have contributed to the balance, and provided information on the postural control ability of joint receptors such as the ligaments or joint capsules around the ankle, thereby addressing ankle joint instability to improve the balance control ability. The ankle mobilization intervention is associated with the improvement in the range of motion and ankle muscles, bringing about postural stability [33]. An improved range of motion can promote postural control and improve balance [7]. Mecagni (2000) [6] reported that the range of motion of ankle joints was important not only for balance but also for mobility, and that there was a significant correlation between the range of motion and balance.
When measuring the LOS, we chose the tibialis anterior muscle, which is in charge of anterior-medial stability of the ankle, and the gastrocnemius muscle which is in charge of the posterior stability of the ankle to measure muscle activity. The gastrocnemius muscle contributes to dynamic balance while walking and the tibialis anterior muscle contributes to the ankle stability by acting as the antagonistic muscle of the gastrocnemius muscle. The gastrocnemius muscle has the ability to maintain posture while standing statically in response to the line of gravity that passes directly in front of the ankle joint [34]. This study showed a significant increase in the muscle activity of the tibialis anterior muscle and gastrocnemius muscle in the FLOS and BLOS. The muscle activity of the tibialis anterior muscle and gastrocnemius muscle had a meaningful increase in the LLOS and RLOS, but there was no significant difference. Yang’s research (2012) [35] reported that when it comes to the LOS, there is a meaningful correlation between the muscle activity of the tibialis anterior muscle and gastrocnemius muscle, and that the increased muscle activity of the ankle joints affected an increase in balance. Arampatzis (2006) [36] reported that the angle of the ankle joint had a significant effect on the action of the dorsiflexor and plantar flexor, and muscle activities of these muscles increase with aging. These differences in muscle activity are explained by changes in epidemiological factors of ankle joints, changes in muscle volume, and changes in the action of agonistic and antagonistic muscle muscles depending on angles. It is considered that the increased range of motion of ankle joints following the use of ankle mobilization, as shown above, may have contributed to the increased muscle activity of the tibialis anterior muscle and gastrocnemius muscle in the elderly with chronic instability when measuring the FLOS, BLOS, LLOS, and RLOS.
According to the results of the latest previous study, it was reported that the balance and ankle range of motion of patients with chronic ankle instability were improved when Maitland joint mobilization was applied, which is consistent with the results of this study. However, the limitations of previous studies suggested that additional research is needed to measure the muscle activity of the lower extremities related to daily life [37]. Therefore, unlike in previous studies, in this study, muscle activity, as well as balance and joint range of motion, were measured in subjects with chronic ankle instability to overcome the limitations of previous studies. Also, Norouzi (2021) [38] reported that Maitland joint mobilization significantly improved ankle range of motion and pain in patients with ankle sprains due to ankle instability.
The ankle mobilization increased the range of motion of ankle joints in the elderly with chronic ankle instability, which contributed to the balance and the lower extremity muscle activity in the elderly. In addition, the ankle joint instability score also improved significantly after the intervention to more than 24. In sum, it is an improvement in pain and instability that may occur in everyday activities, such as going up the stairs or suddenly changing directions. Limitations of the study include that it is impossible to know how long the improvements will last because this study looked at immediate changes after applying the ankle mobilization without an intervention period; and that it is difficult to generalize the results because the number of subjects was small. Further studies should be conducted to determine how long the effect of ankle mobilization with the intervention period will last, and to determine the correlation between the range of joint motion, foot and ankle muscles, and psychological factors and the balance and muscle activity of older people with chronic ankle instability.
Conclusions
The conclusion of this study is ankle mobilization may be a useful intervention method in preventing falls and improving balance in older adults with chronic ankle instability.
Figures
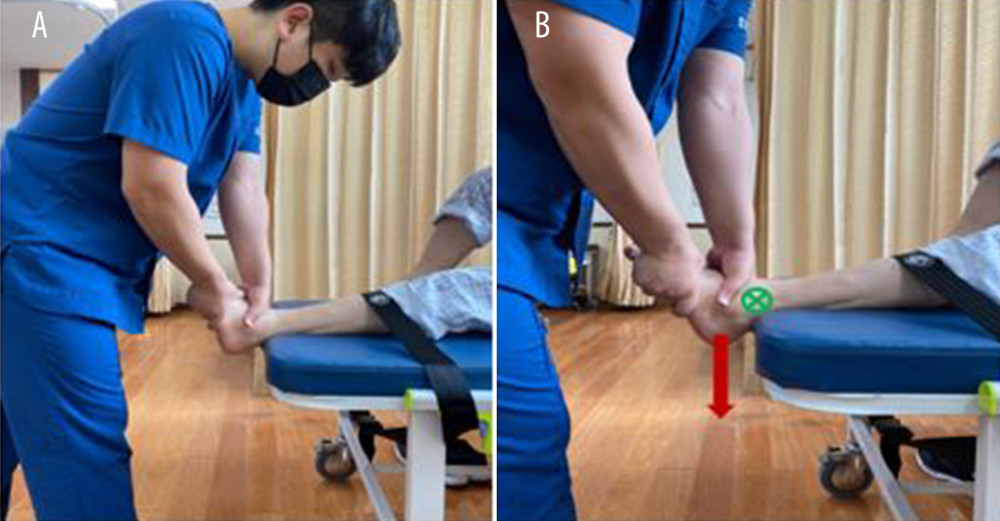 Figure 1. Talocrural joint A-P mobilization. (A) A-P mobilization Grade III starting position (B) Glide direction by force when A-P mobilization is applied.
Figure 1. Talocrural joint A-P mobilization. (A) A-P mobilization Grade III starting position (B) Glide direction by force when A-P mobilization is applied. 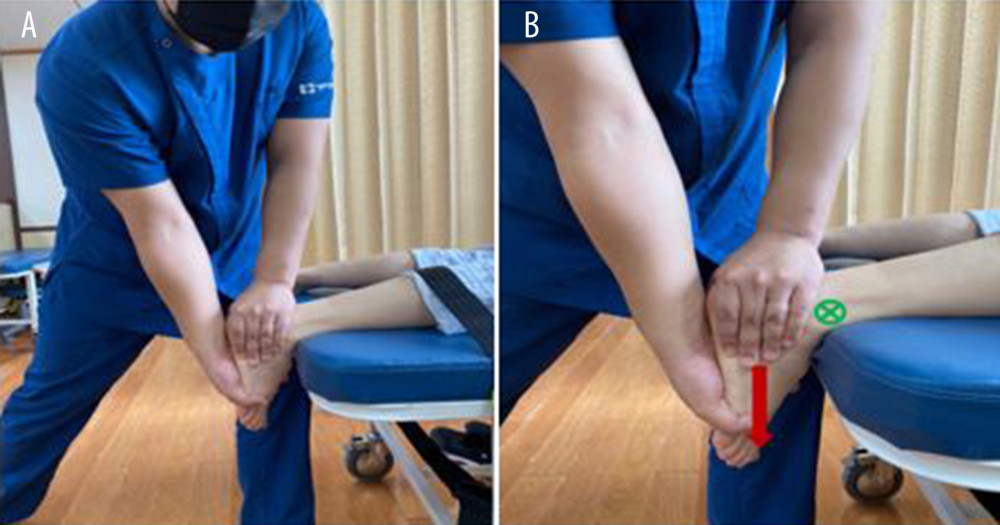 Figure 2. Talocrural joint P-A mobilization. (A) P-A mobilization Grade III starting position (B) Glide direction by force when P-A mobilization is applied.
Figure 2. Talocrural joint P-A mobilization. (A) P-A mobilization Grade III starting position (B) Glide direction by force when P-A mobilization is applied. 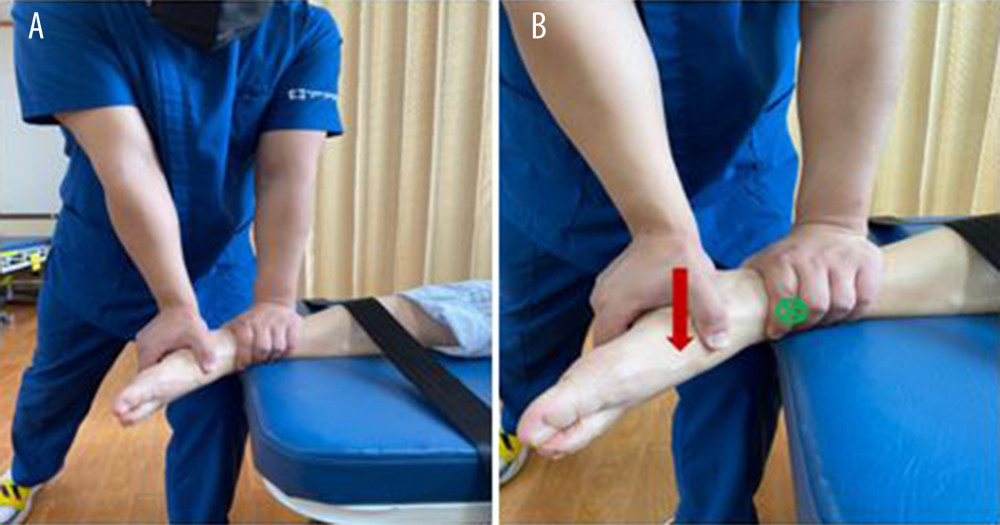 Figure 3. Subtalar joint M-L mobilization. (A) M-L mobilization Grade III starting position (B) Glide direction by force when M-L mobilization is applied.
Figure 3. Subtalar joint M-L mobilization. (A) M-L mobilization Grade III starting position (B) Glide direction by force when M-L mobilization is applied.  Figure 4. Subtalar joint L-M mobilization. (A) L-M mobilization Grade III starting position (B) Glide direction by force when L-M mobilization is applied.
Figure 4. Subtalar joint L-M mobilization. (A) L-M mobilization Grade III starting position (B) Glide direction by force when L-M mobilization is applied. 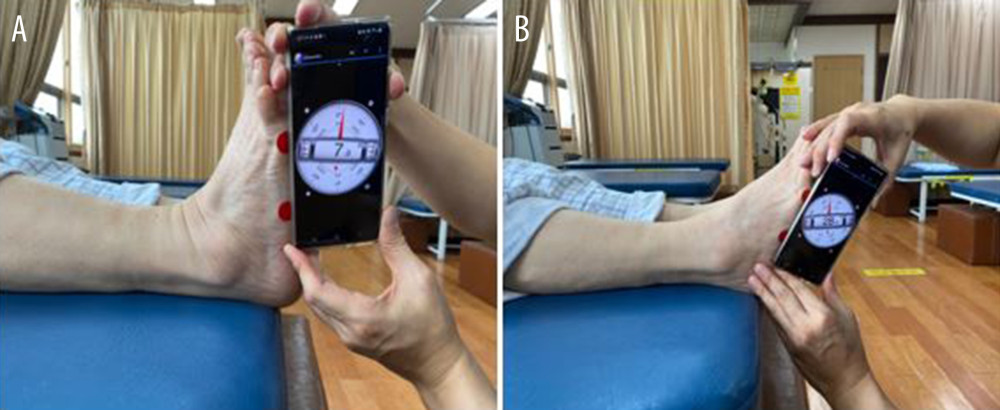 Figure 5. Ankle Rage of Motion (ROM) measurement (A) ankle dorsiflexion ROM measurement (B) ankle plantar flexion ROM measurement.
Figure 5. Ankle Rage of Motion (ROM) measurement (A) ankle dorsiflexion ROM measurement (B) ankle plantar flexion ROM measurement.  Figure 6. Measurement of balance ability (BT-4): Static balance and dynamic balance measurements.
Figure 6. Measurement of balance ability (BT-4): Static balance and dynamic balance measurements. 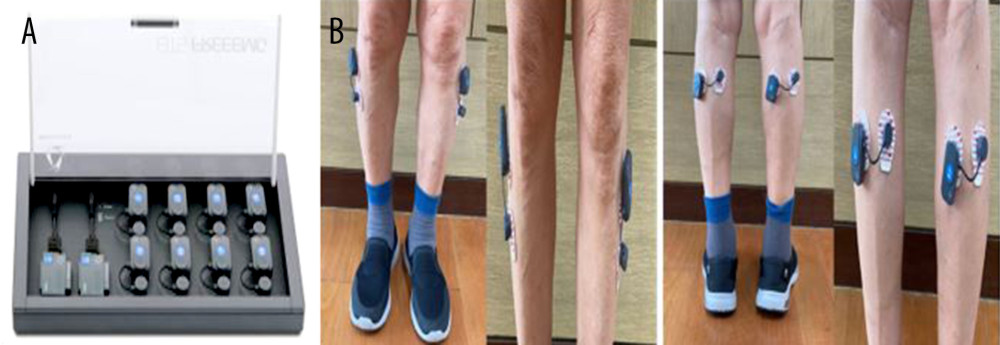 Figure 7. (A) Electromyogram (EMG) measuring device (B) measurement of electromyogram.
Figure 7. (A) Electromyogram (EMG) measuring device (B) measurement of electromyogram. References
1. Karlsson MK, Magnusson H, von Schewelov T, Rosengren BE, Prevention of falls in the elderly – a review: Osteoporos Int, 2013; 24; 747-62
2. Burns E, Kakara R, Deaths from falls among persons aged ≥65 years – United States, 2007–2016: MMWR, 2018; 67(18); 509
3. Seidler RD, Bernard JA, Burutolu TB, Motor control and aging: Links to age-related brain structural, functional, and biochemical effects: Neurosci Biobehav Rev, 2010; 34(5); 721-33
4. Nagai K, Yamada M, Uemura K, Differences in muscle coactivation during postural control between healthy older and young adults: Arch Gerontol Geriatr, 2011; 53(3); 338-43
5. Abate M, Schiavone C, Pelotti P, Salini V, Limited joint mobility (LJM) in elderly subjects with type II diabetes mellitus: Arch Gerontol Geriatr, 2011; 53(2); 135-40
6. Mecagni C, Smith JP, Roberts KE, O’Sullivan SB, Balance and ankle range of motion in community-dwelling women aged 64 to 87 years: A correlational study: Phys Ther, 2000; 80(10); 1004-11
7. Chevutschi A, D’houwt J, Pardessus V, Thevenon A, Immediate effects of talocrural and subtalar joint mobilization on balance in the elderly: Physiother Res Int, 2015; 20(1); 1-8
8. Whipple R, Wolfson L, Amerman P, The relationship of knee and ankle weakness to falls in nursing home residents: An isokinetic study: J Am Geriatr Soc, 1987; 35(1); 13-20
9. Vandervoort AA, Chesworth BM, Cunningham DA, Age and sex effects on mobility of the human ankle: J Gerontology, 1992; 47(1); M17-21
10. Bae S-Y, Ko D-S, Noh J-S, Relation of physical activity and health-related quality of life in Korean elderly: The Journal of the Korea Contents Association, 2010; 10(10); 255-66
11. Lee S-E, Effects of increasing ankle range of motion program on ambulation and balance for the elderly with balance disorder: Phys Ther Korea, 2005; 12(2); 28-36
12. Nitz JC, Choy NL, The relationship between ankle dorsiflexion range, falls and activity level in women aged 40 to 80 years: New Zealand Journal of Physiotherapy, 2004; 32(3); 121
13. Sohng K-Y, Choi D-W, Instrumental activities of daily living, leg muscle strength, cognitive and visual function according to demographic variables and the experience of falling in community resident elderly Koreans: J Korean Acad Fundam Nurs, 2007; 14(2); 221-29
14. Yoo Y, Falls and functional levels associated with falls in older people living in the community: J Korean Gerontol Nurs, 2010; 12(1); 40-50
15. Holland GJ, Tanaka K, Shigematsu R, Nakagaichi M, Flexibility and physical functions of older adults: A review: J Aging Phys Act, 2002; 10(2); 169-206
16. Hoch MC, McKeon PO, Normative range of weight-bearing lunge test performance asymmetry in healthy adults: Man Ther, 2011; 16(5); 516-19
17. Basnett CR, Hanish MJ, Wheeler TJ, Ankle dorsiflexion range of motion influences dynamic balance in individuals with chronic ankle instability: Int J Sports Phys Ther, 2013; 8(2); 121-28
18. Abe Y, Sugaya T, Sakamoto M, The postural control characteristics of individuals with and without a history of ankle sprain during single-leg standing: Relationship between center of pressure and acceleration of the head and foot parameters: J Phys Ther Sci, 2014; 26(6); 885-88
19. Cerezal A, Ocampo R, Llopis E, Cerezal L: Ankle instability update Seminars in musculoskeletal radiology, 2023, New York, NY, Thieme Medical Publishers, Inc
20. Olmsted LC, Carcia CR, Hertel J, Shultz SJ, Efficacy of the star excursion balance tests in detecting reach deficits in subjects with chronic ankle instability: J Athl Train, 2002; 37(4); 501-6
21. Ju S-B, Gong W-T, Park G-D, Lee H-Y, The effects of the range of motion of the ankle joint and balance control ability after the application of the ankle joint mobilization technique for elderly men: Korean Journal of Sports Science, 2011; 20(5); 1037-45
22. Thomas E, Battaglia G, Patti A, Physical activity programs for balance and fall prevention in elderly: A systematic review: Medicine, 2019; 98(27); e16218
23. Pennetti A, A multimodal physical therapy approach utilizing the Maitland concept in the management of a patient with cervical and lumbar radiculitis and Ehlers-Danlos syndrome-hypermobility type: A case report: Physiother Theory Pract, 2018; 34(7); 559-68
24. Hoch MC, Andreatta RD, Mullineaux DR, Two-week joint mobilization intervention improves self-reported function, range of motion, and dynamic balance in those with chronic ankle instability: J Orthop Res, 2012; 30(11); 1798-804
25. Hiller CE, Refshauge KM, Bundy AC, The Cumberland ankle instability tool: A report of validity and reliability testing: Arch Phys Med Rehabil, 2006; 87(9); 1235-41
26. Williams CM, Caserta AJ, Haines TP, The TiltMeter app is a novel and accurate measurement tool for the weight bearing lunge test: J Sports Sci Med, 2013; 16(5); 392-95
27. Borg FG, Laxåback G, Entropy of balance-some recent results: J Neuroeng Rehabil, 2010; 7; 1-11
28. Takao M, Uchio Y, Naito K, Arthroscopic assessment for intra-articular disorders in residual ankle disability after sprain: Am J Sports Med, 2005; 33(5); 686-92
29. Eils E, Rosenbaum D, A multi-station proprioceptive exercise program in patients with ankle instability: Med Sci Sports Exerc, 2001; 33(12); 1991-98
30. Paris S, Loubert P: Foundations of clinical orthopaedics, 1999, St Augustine, University of St Augustine for Health Sciences
31. Park J-M, The effects of somatosensory stimulations with joints mobilization in foot on balance and gait speed in some elderly women-case survey: Kor Acad Ortho Man Phys Ther, 2013; 19(2); 67-71
32. Shumway-Cook A, Horak FB, Rehabilitation strategies for patients with vestibular deficits: Neurol Clin, 1990; 8(2); 441-57
33. Slatyer MA, Hensley MJ, Lopert R, A randomized controlled trial of piroxicam in the management of acute ankle sprain in Australian Regular Army recruits: The Kapooka Ankle Sprain Study: Am J Sports Med, 1997; 25(4); 544-53
34. Soderberg GL: Kinesiology: Application to pathological motion, 1997, Lippincott Williams & Wilkins
35. Yang D-J, Kim J-H, Jung Y-S, Correlation between balance and lower extremity muscle activity in stroke patients: J Kor Acad Clin Elec, 2012; 10(1); 1-5
36. Arampatzis A, Karamanidis K, Stafilidis S, Effect of different ankle-and knee-joint positions on gastrocnemius medialis fascicle length and EMG activity during isometric plantar flexion: J Biomech, 2006; 39(10); 1891-902
37. Yin Y, Yu Z, Wang J, Sun J, Effectiveness of the rehabilitation training combined with maitland mobilization for the treatment of chronic ankle instability: A randomized controlled trial: Int J Environ Health Res, 2022; 19(22); 15328
38. Norouzi A, Delkhoush CT, Mirmohammadkhani M, Bagheri R, A comparison of mobilization and mobilization with movement on pain and range of motion in people with lateral ankle sprain: A randomized clinical trial: J Bodyw Mov Ther, 2021; 27; 654-60
Figures
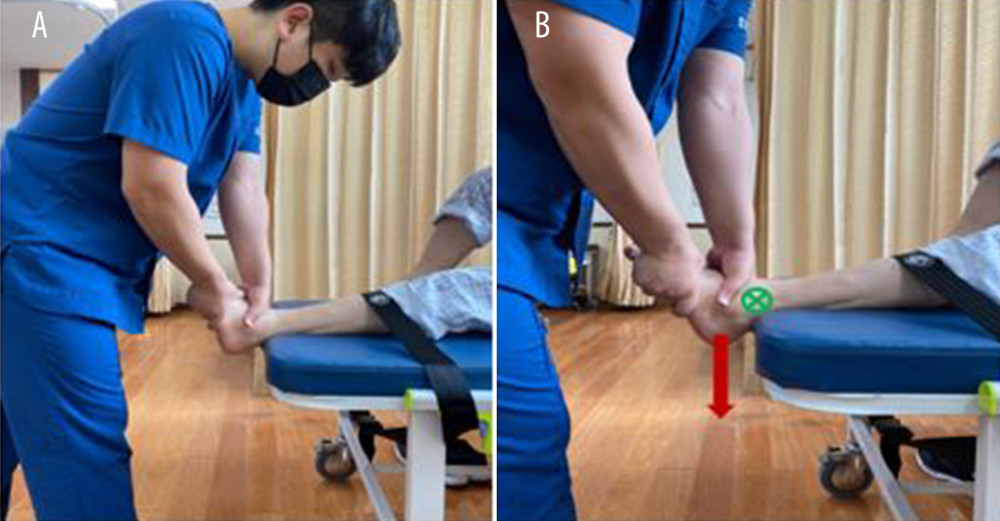 Figure 1. Talocrural joint A-P mobilization. (A) A-P mobilization Grade III starting position (B) Glide direction by force when A-P mobilization is applied.
Figure 1. Talocrural joint A-P mobilization. (A) A-P mobilization Grade III starting position (B) Glide direction by force when A-P mobilization is applied.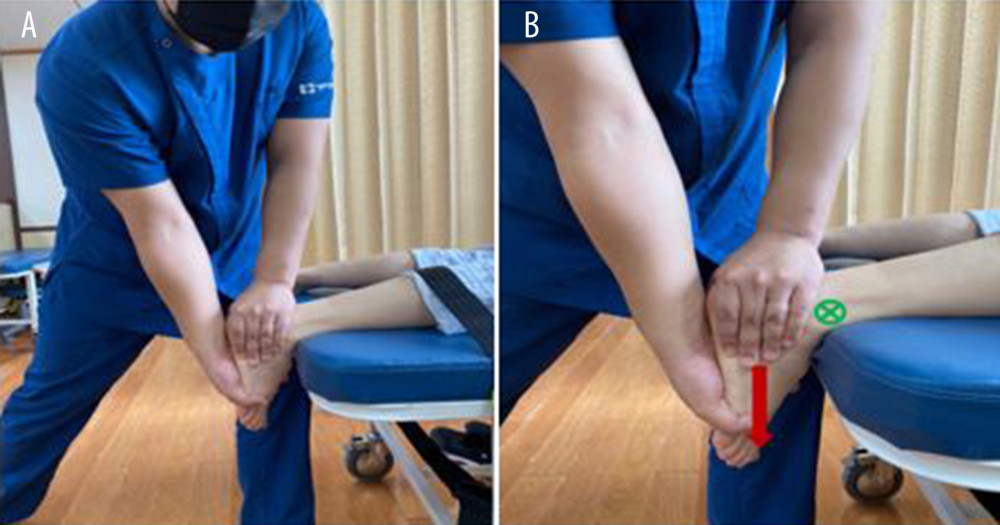 Figure 2. Talocrural joint P-A mobilization. (A) P-A mobilization Grade III starting position (B) Glide direction by force when P-A mobilization is applied.
Figure 2. Talocrural joint P-A mobilization. (A) P-A mobilization Grade III starting position (B) Glide direction by force when P-A mobilization is applied.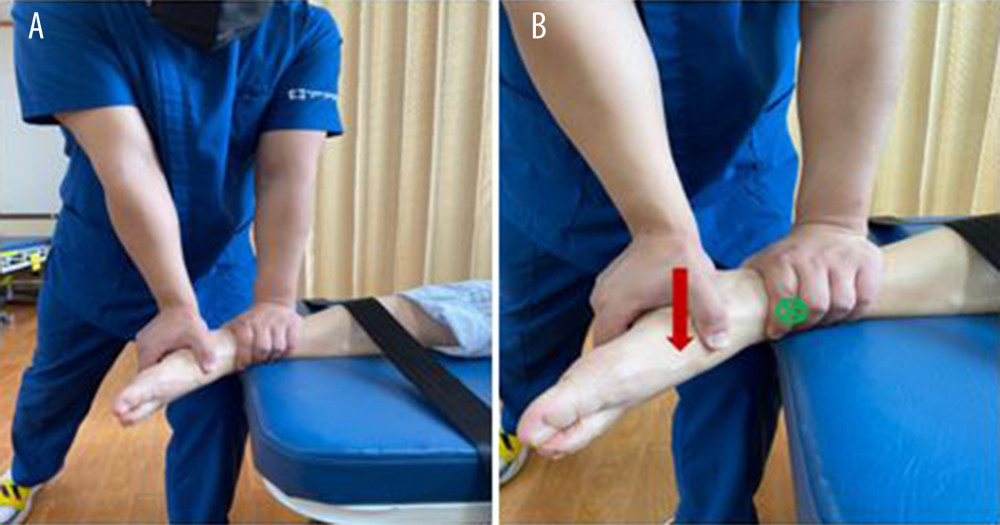 Figure 3. Subtalar joint M-L mobilization. (A) M-L mobilization Grade III starting position (B) Glide direction by force when M-L mobilization is applied.
Figure 3. Subtalar joint M-L mobilization. (A) M-L mobilization Grade III starting position (B) Glide direction by force when M-L mobilization is applied. Figure 4. Subtalar joint L-M mobilization. (A) L-M mobilization Grade III starting position (B) Glide direction by force when L-M mobilization is applied.
Figure 4. Subtalar joint L-M mobilization. (A) L-M mobilization Grade III starting position (B) Glide direction by force when L-M mobilization is applied.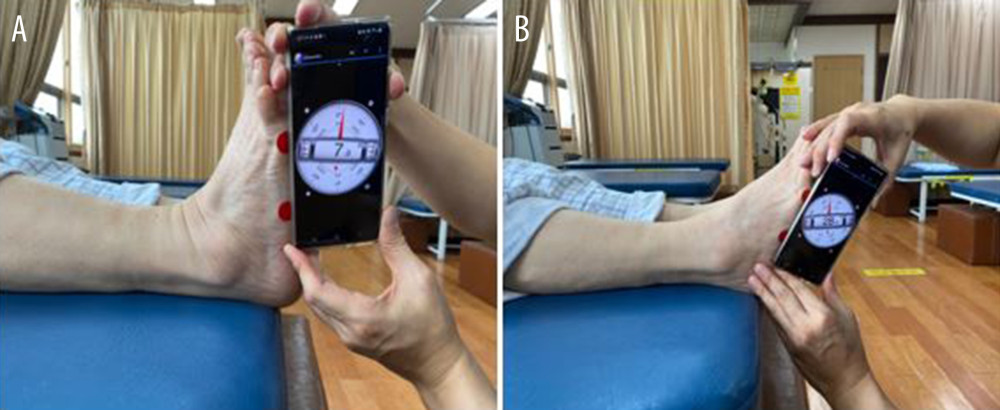 Figure 5. Ankle Rage of Motion (ROM) measurement (A) ankle dorsiflexion ROM measurement (B) ankle plantar flexion ROM measurement.
Figure 5. Ankle Rage of Motion (ROM) measurement (A) ankle dorsiflexion ROM measurement (B) ankle plantar flexion ROM measurement. Figure 6. Measurement of balance ability (BT-4): Static balance and dynamic balance measurements.
Figure 6. Measurement of balance ability (BT-4): Static balance and dynamic balance measurements.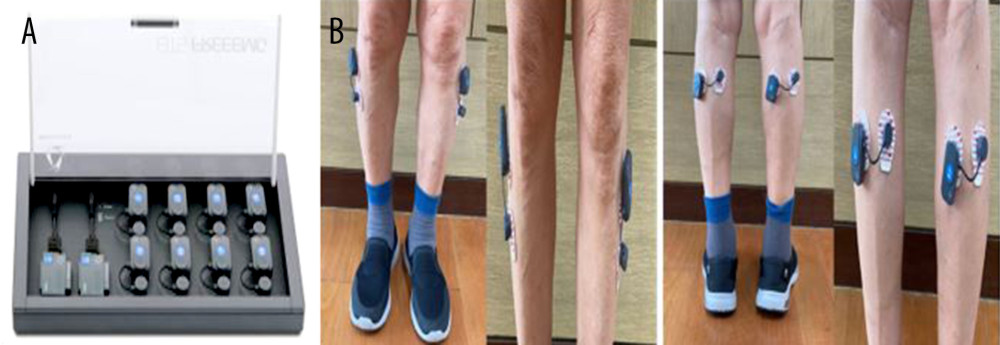 Figure 7. (A) Electromyogram (EMG) measuring device (B) measurement of electromyogram.
Figure 7. (A) Electromyogram (EMG) measuring device (B) measurement of electromyogram. Tables
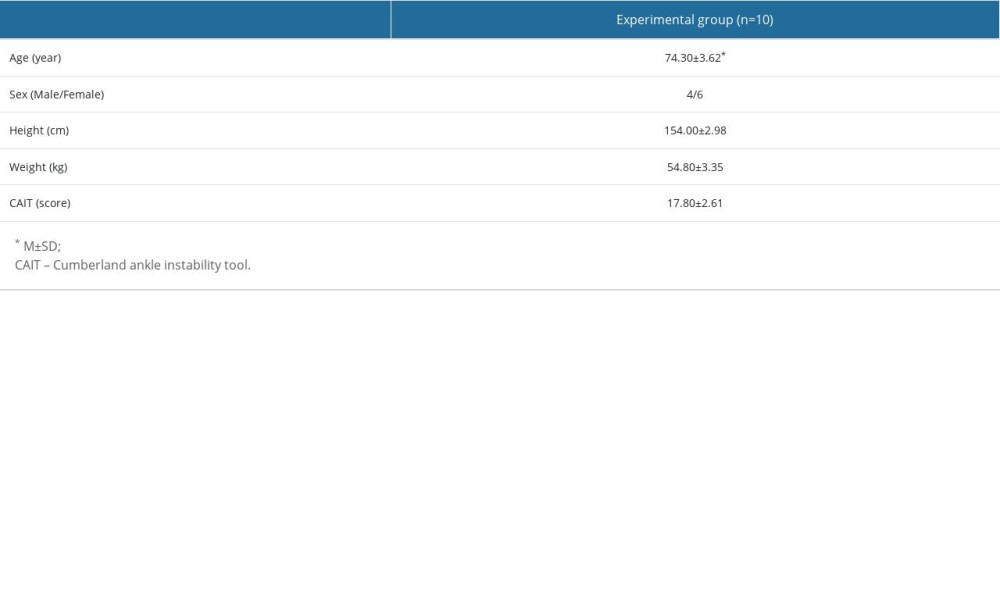 Table 1. General characteristics of subjects.
Table 1. General characteristics of subjects.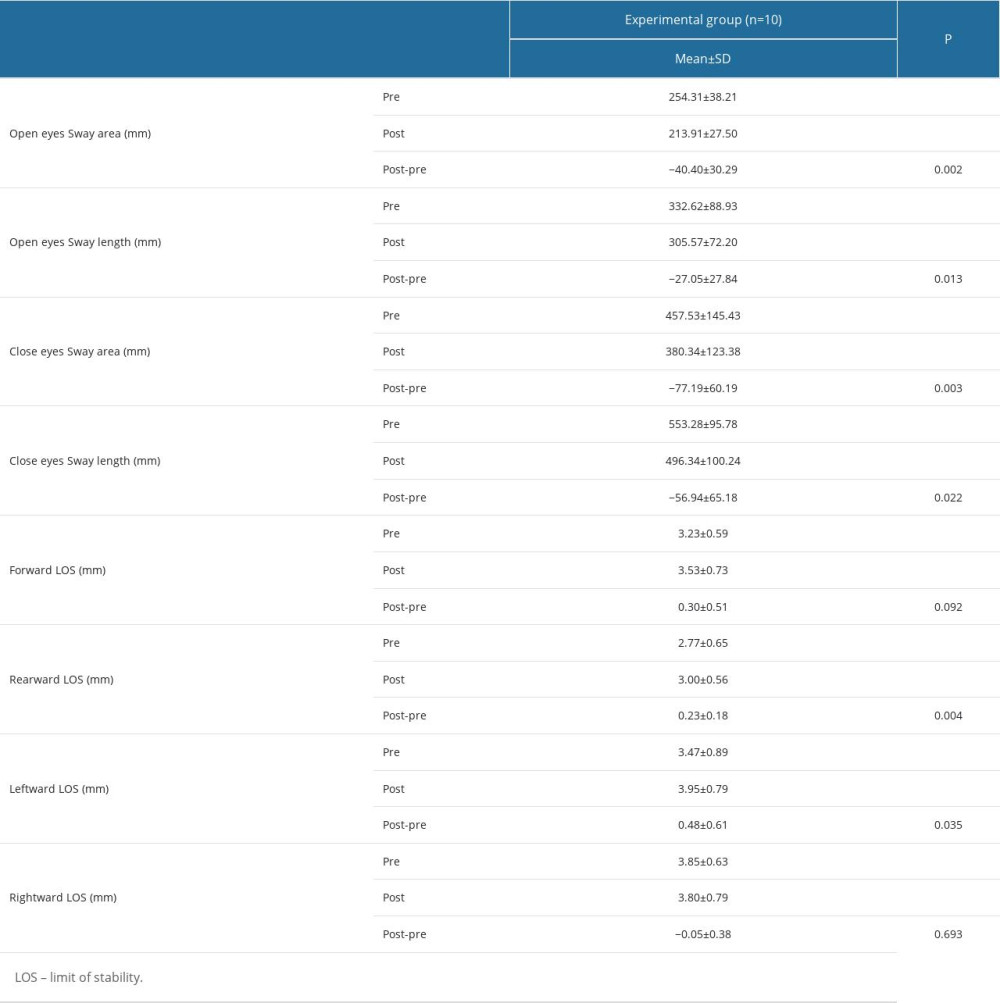 Table 2. Changes in balance following intervention.
Table 2. Changes in balance following intervention.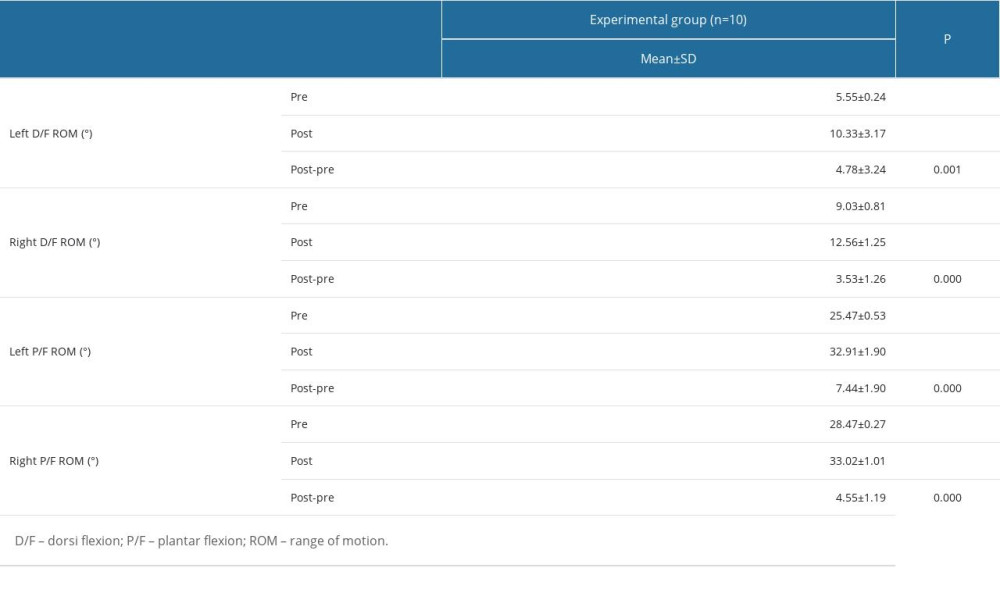 Table 3. Changes in ROM following intervention.
Table 3. Changes in ROM following intervention. Table 4. Changes in muscle activity following intervention.
Table 4. Changes in muscle activity following intervention.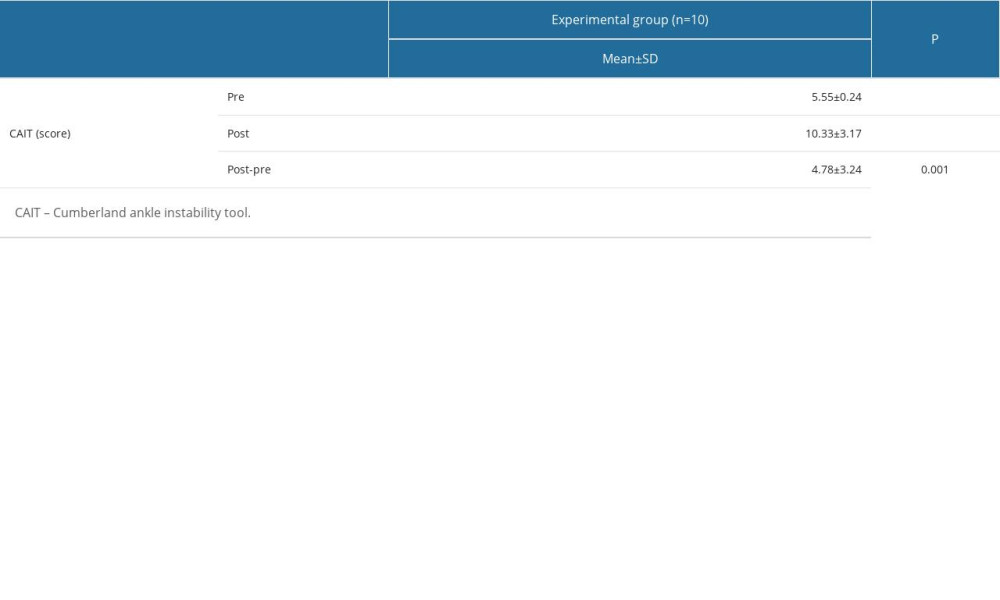 Table 5. Changes in CAIT following intervention.
Table 5. Changes in CAIT following intervention.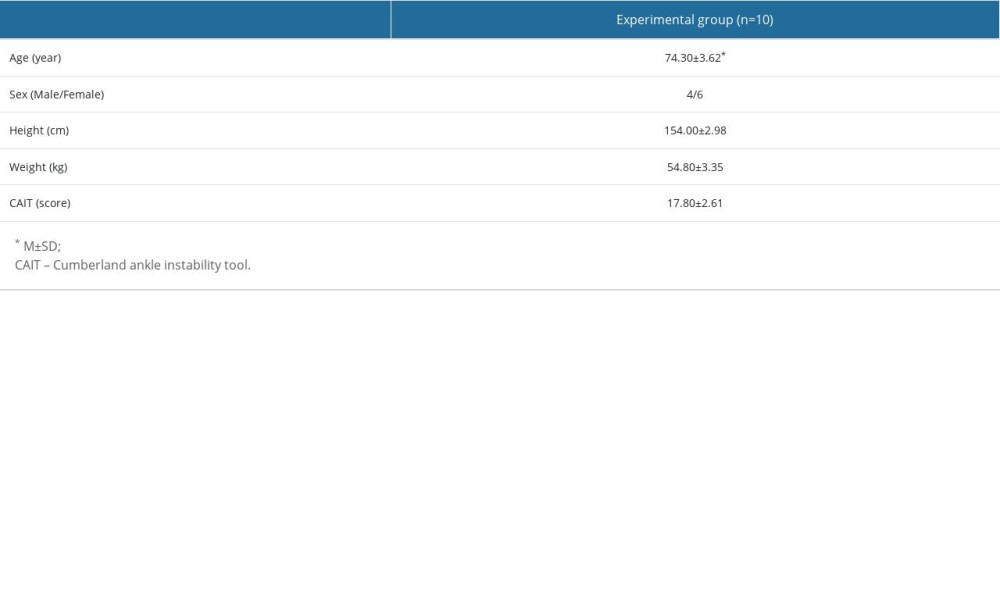 Table 1. General characteristics of subjects.
Table 1. General characteristics of subjects.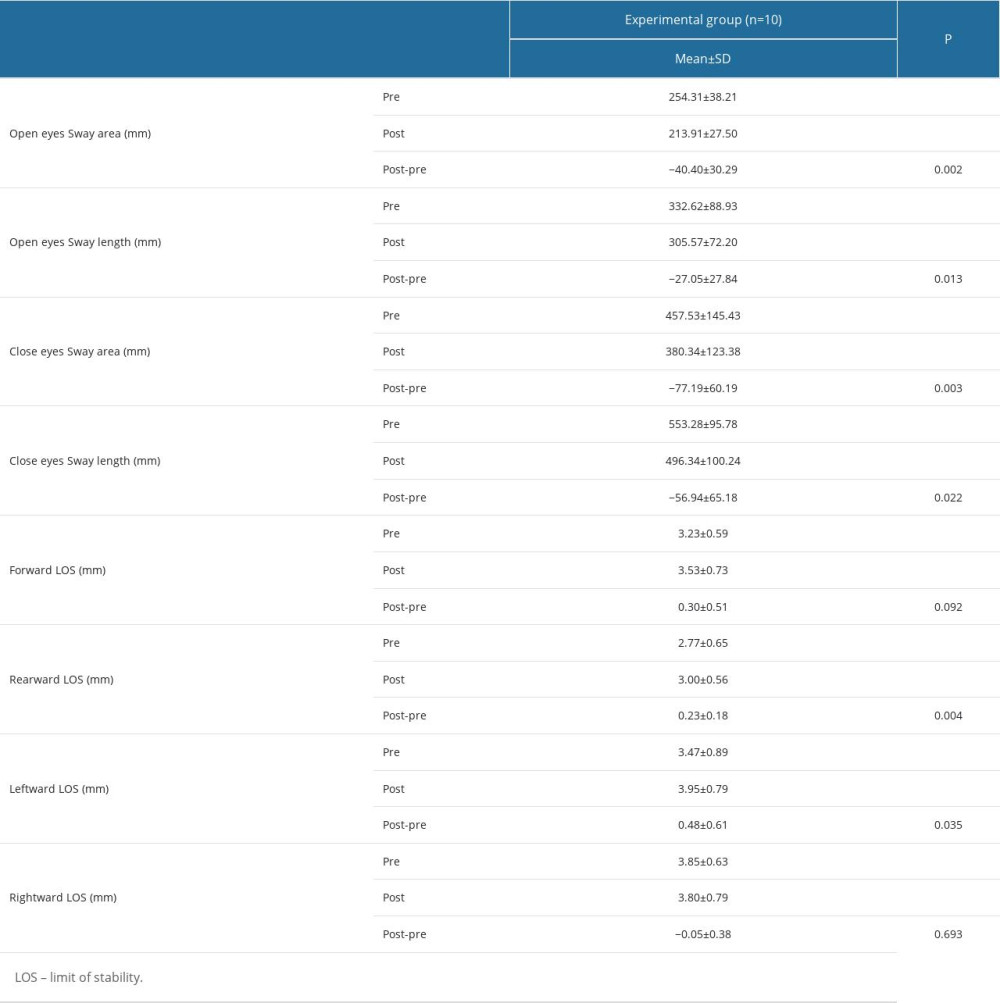 Table 2. Changes in balance following intervention.
Table 2. Changes in balance following intervention.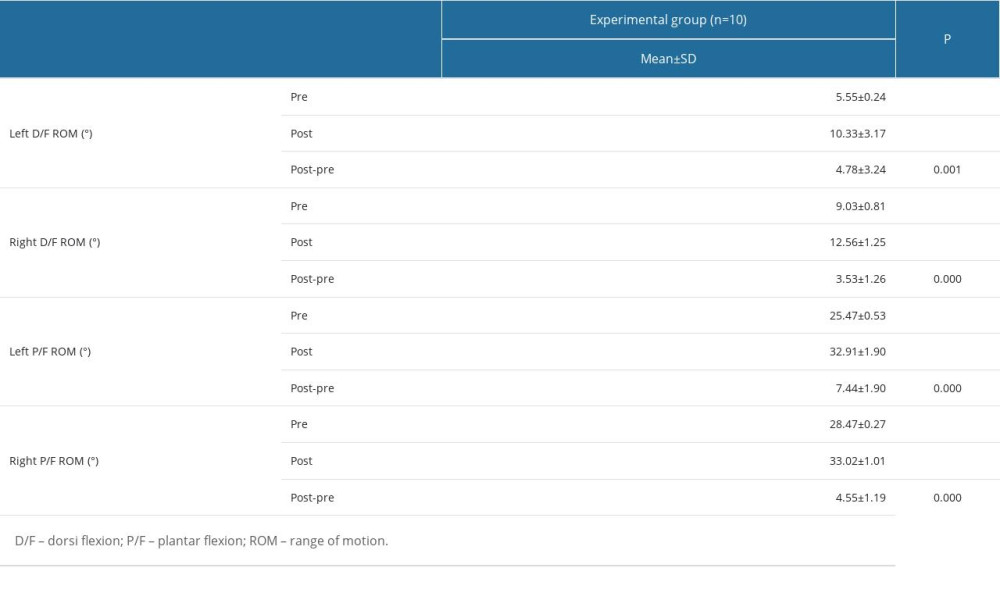 Table 3. Changes in ROM following intervention.
Table 3. Changes in ROM following intervention. Table 4. Changes in muscle activity following intervention.
Table 4. Changes in muscle activity following intervention.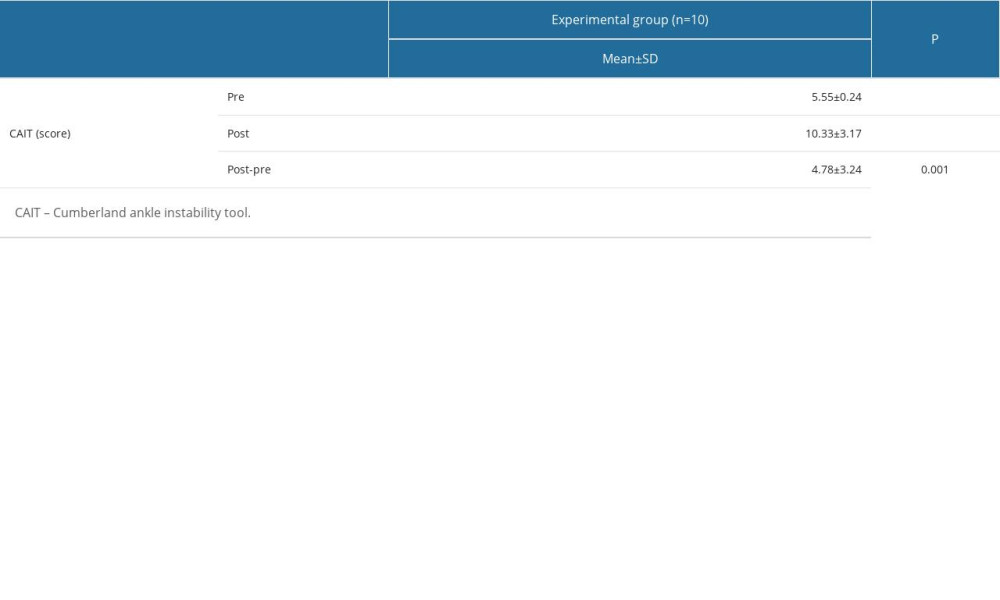 Table 5. Changes in CAIT following intervention.
Table 5. Changes in CAIT following intervention. In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








