19 September 2023: Clinical Research
Impact of Verbal Suggestions on Finger Flexor Activation and Strength in Healthy Individuals
Kamil ZaworskiDOI: 10.12659/MSM.941548
Med Sci Monit 2023; 29:e941548
Abstract
BACKGROUND: Words uttered by other people can have an enormous influence on how we perceive our surroundings, what we expect, what we experience, and how we behave. This study aimed to evaluate the effect of verbal reinforcement on the placebo effect in the context of finger flexor muscle activation measured with surface electromyography (sEMG) and hand grip strength measured with a hand dynamometer in healthy subjects.
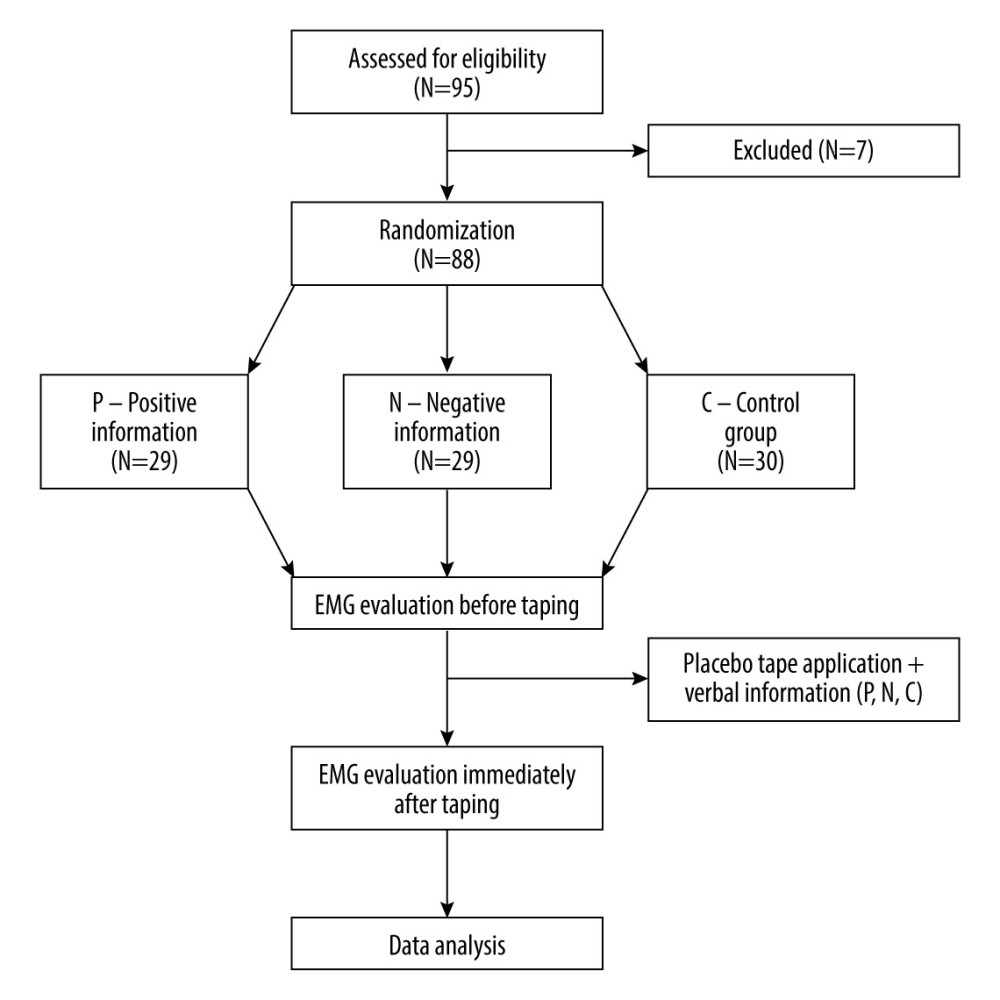
MATERIAL AND METHODS: Eighty-eight individuals aged 22.64±5.2 years took part in the study. For each person, paper tape was applied (placebo). The participants were randomly assigned to 1 of the 3 groups: positive information group (P) – “the tape increases hand muscle strength”, negative information group (N) – “the tape decreases hand muscle strength”, and control group (C) – “the effect of the tape on hand muscle strength is unknown.” The activation of muscles was assessed using surface electromyography (sEMG) while measuring the strength of wrist and finger flexors with a hand dynamometer. Each participant was examined twice – prior to and immediately after taping and providing verbal reinforcement.
RESULTS: Only group N manifested a decrease in muscle strength, from 39.7N to 37.6N (P=0.003). Group C displayed an increase in muscle strength from 34.3N to 36.4N (P=0.035). None of the groups demonstrated statistically significant changes in bioelectrical activity of the muscles. At no stage of examination were the differences between the groups significant.
CONCLUSIONS: Negative verbal information combined with the placebo intervention resulted in a significant decrease in the strength of finger flexors.
Keywords: Hand Strength, Nocebo Effect, Placebo Effect, Humans, Upper Extremity, Fingers, Hand, Muscle, Skeletal
Background
Perception and behavior are strongly influenced by verbal information (eg, verbal suggestions) provided by other individuals and by the learning mechanism (conditioning). The manner in which healthcare workers (including physiotherapists) inform patients about typical effects of a given treatment affects patients’ feelings and expectations as well as their subjective evaluation of treatment effects. Active interventions are more effective when patients are provided with verbal information in a manner that increases their expectations concerning positive outcomes [1]. Verbal reinforcement is a well-known phenomenon commonly used in training. As early as in 1983, Johansson et al noted an increase in isometric muscle contraction resulting from high-volume verbal commands [2]. Also, Belkhiria et al observed positive effects of verbal reinforcement on isometric force [3]. Positive verbal information associated with positive conditioning produces the placebo effect, while its negative counterpart leads to the nocebo effect. The word ‘placebo’ originates from Latin and means “I shall please.” It was used to define individuals hired to mourn during funerals. In the medical literature, it was first used in the 19th century in a medical dictionary published in 1811 [4]. The term ‘placebo’ refers to a neutral factor or activity that should not have any proven ability to produce physical or psychological effects. The placebo effect indicates a positive psychological or physical impact that can be attributed to placebo or processes (expectation or conditioning) owing to which placebo takes effect [5]. Placebo may produce tangible therapeutic benefits in numerous clinical states through the activity of different neurobiological pathways [6].
Most investigations into placebo and nocebo effects do not provide exact words used in verbal suggestions; however, large differences in effects point to the significance of particular terms. There is a strong need for further research into therapeutic effectiveness improvement using verbal suggestions. In this context, use of inappropriate words can either reduce or eliminate therapeutic effects, or even result in contrary effects. Therefore, the use of inappropriate words can affect the achievement of desired therapeutic aims [7].
It was also found that the application of a non-active drug or a therapy with expected negative outcomes (eg, increased fear, fatigue, or other symptoms) often leads to an increase in adverse symptoms. It was defined as the nocebo effect (“nocebo” means “I shall harm”) [8].
The nocebo effect occurs when information and expectations regarding negative effects of an intervention lead to negative (often significant) consequences [9]. Sports-related studies revealed that the nocebo effect can reduce sports performance [6,10,11]. It was observed that among trained athletes “subjects in a control group perform worse because they know they are in the control group” [12]. Research on placebo in athletes also showed that it can enhance their performance (also in elite athletes), and its influence goes beyond ordinary motivation of an athlete to perform better [11]. In their review, Hurst et al analyzed 32 studies that included 1513 participants, finding small to moderate placebo effects (Cohen’s d=0.36) and small to moderate nocebo effects (d=0.37) in elite athletes [11].
Electromyography (EMG) refers to the reception of the electric signal from muscles controlled by the nervous system. The EMG signal is the electric activity of motor units of a muscle. There are 2 types of EMG: surface EMG (sEMG) and intramuscular EMG. Currently, signals detected by means of sEMG are preferable in terms of obtaining data on the time and intensity of surface muscle activation. EMG signals are used as electrophysiological signals both in medicine and in engineering [13].
Hand dynamometers are widely used; it has been proved that they are valid and reliable for examining healthy individuals. These tools measure muscle peak strength. There are hydraulic and electronic dynamometers which make it possible to measure average grip strength in a given time period as well as grip strength at the end of this period [14].
Therefore, this study aimed to evaluate the effect of verbal reinforcement on the placebo effect in the context of finger flexor muscle activation measured with surface electromyography (sEMG) and hand grip strength measured with a hand dynamometer in healthy subjects.
Material and Methods
ETHICS STATEMENT:
The study was approved by the Bioethics Committee of the ABNS in Biała Podlaska (protocol code 5/2019) and was conducted in accordance with the ethical standards established in the 1964 Declaration of Helsinki.
Prior to the examinations, the participants were partly informed about the purpose of the study (they were informed that the study would focus on the effects of the applied tape on muscle strength and activation) and were made aware of being able to quit the study at any time. Moreover, they gave their written informed consent to use the data collected during the study for scientific purposes (publishing). Upon completing the study, the participants were fully informed about the study aim.
STUDY DESIGN:
This single-blinded, controlled, randomized, clinical trial was registered at Clinical Trials (NCT05206383).
The participants were randomly assigned to 1 of 3 groups: group P received positive verbal information, group N received negative verbal information, and group C (control group). Randomization was performed using opaque sealed envelopes. Each participant drew 1 envelope out of an opaque box, opened it and read out the symbol of the group (P, N, or C).
PARTICIPANTS:
A total of 91 individuals volunteered to participate in the study. However, 3 persons were excluded from the study because they did not meet the inclusion criteria (Figure 1).
Eighty-eight healthy white students aged 22.64 years (SD=5.2) took part in the study. The mean value of body mass index (BMI) was 23.5±3.22 kg/m2. Homogeneity of the groups under study is shown in Table 1.
Women constituted a slightly larger percentage of the study participants (61.4%). Detailed information is presented in Table 2. The vast majority of participants were right-handed (86.4%).
The inclusion criteria were as follows: the absence of pain or any signs of musculoskeletal dysfunction in the upper limbs, no use of any non-steroidal anti-inflammatory drugs (NSAIDs) for at least 1 week prior to study entry, age 19–24 years, written consent to participate in the study, absence of peripheral or central metabolic or neurological diseases, and lack of knowledge about kinesiology taping. The exclusion criteria were as follows: studying for a degree in physiotherapy, previous surgery on the examined upper limb, previous bone fractures in the examined upper limb, injury to the examined upper limb within 6 months before the start of the study, previous application of kinesiology taping, and allergic reaction to the tape application.
PROCEDURES:
A single-blinded (subject) study with a repeated-measure design was performed to evaluate the influence of verbal information on strength and activation of wrist and finger flexors.
The experiment was conducted in a standardized manner. Students’ dominant upper limbs were tested. Each participant sat on a chair without leaning forward, with the arm slightly adducted (15°), the elbow flexed at 90°, and the forearm in a neutral position (between supination and pronation).
The participants performed a 5-min warm-up that involved active exercises of fingers and wrists (flexion-extension, abduction-adduction, and circles, with 20 repetitions each).
Dynamometric measurements, performed with the use of the hand dynamometer KERN MAP 80K1S, were preceded by 3 warm-up attempts (duration – 3 s, interval between attempts – 1 min) that helped the participants learn how to use the dynamometer.
After a 10-min break, each participant was asked to hold the grip of the dynamometer as tight as possible for 3 s, with a 1-min rest interval between attempts. The values of 3 attempts were registered. Afterwards, paper tape was applied to the forearm of the dominating upper limb. In groups P and N, verbal information was provided, followed by an immediate request to perform the dynamometer test with maximum strength in the same standardized manner. Paper tape (Endura Fix Tape) 8 cm long was applied to the forearm in a neutral position on the lateral side in the long axis of the radius. Group P received positive verbal information – “the tape increases hand muscle strength.” Group N received negative verbal information – “the tape decreases hand muscle strength.” Group C received neutral verbal information – “the effect of the tape on hand muscle strength is unknown”.
At every stage of examination, measurements were also made using sEMG. Prior to placing electrodes on the body, the skin was cleaned with 90% alcohol solution. Ag/Ag electrodes 30 mm in diameter and with a conducting area of 16 mm (SORIMEX, Toruń, Poland) were placed on the anterolateral side of the forearm, 1 cm above the medial epicondyle of the humerus. The electrodes were placed along muscle fibers of wrist and finger flexors by experienced physiotherapists (K.Z. – author, and M.K.). All sEMG examinations were performed between 8 a.m. and 12 a.m. using the 8-channel Naroxon Ultium EMG system and mioMUSCLE system (Naroxon U.S.A., Inc.).
After completing the tests, the participants provided subjective feedback on how they felt their hand grip strength changed (definitely yes, rather yes, no change, rather not, definitely not).
DATA ANALYSES:
Statistical analysis was performed with the SPSS 17.0 software package (Atonicity, USA). The main tests used in statistical analyses were the
Correlations between quantitative variables were determined using r-Pearson coefficient, which informs about the strength of a correlation as well as its direction (either positive or negative). The value obtained ranges from −1 to 1, where (−1) points to strong negative correlation, while (1) indicates strong positive correlation.
Results
DYNAMOMETRIC MEASUREMENTS:
Dynamometric measurements revealed significant changes in muscle strength in groups N and C. In groups P and C, an increase in muscle strength was noted, (
MUSCLE ACTIVATION (SEMG):
None of the groups exhibited significant changes in muscle activation measured with sEMG (P>0.05). Detailed information is shown in Table 3.
DIFFERENCES BETWEEN THE GROUPS:
No significant differences in dynamometric and sEMG measurements between the studied groups were observed at any stage of examination (P>0.05). Detailed information is presented in Table 4.
In all groups, the highest number of participants (44.3% on average) did not feel any changes in muscle strength after the procedures were applied. No significant differences were noted between the groups in subjective evaluation of changes in muscle strength (P>0.05). Detailed information is shown in Table 5.
CORRELATIONS:
No correlations were found between subjective evaluation of muscle strength and dynamometric measurement results and sEMG in any of the examined groups (P>0.05). Detailed information is presented in Table 6.
Discussion
STUDY LIMITATIONS:
The present study has some limitations. To begin with, it only focused on effects observed immediately after taping and providing verbal suggestions. Moreover, it is important that we did not analyse the participants’ expectations, which considerably limits our interpretation of results with regard to this mechanism. Further research should be carried out taking this aspect into consideration. Also, we did not perform a double-blinded trial due to the impracticality of blinding the experimenter in our settings that included different verbal suggestions in placebo and nocebo groups.
It is worth noting that dynamometric measurements do not provide information on endurance and fatigue of grip [14]. In the measurement of muscle activation, a non-invasive method was used, in which amplitude is weakly associated to the effective neural drive to the muscles due to the effect of volume conductor, amplitude cancellation, and random positions of motor units in the muscle tissue [37].
Conclusions
The study revealed a significant decrease in the strength of finger flexors in the group with negative verbal information. It confirms that negative verbal information can cause the nocebo effect. At no stage of examination were the differences between the groups in dynamometric and sEMG measurements significant. From a practical standpoint, our findings may have serious implications for physiotherapists and coaches. For instance, if physiotherapists tell their patients that the therapy will make them feel sore, the likelihood of pain or functional state deterioration will be greater. Words associated with treatment should be chosen carefully to avoid negative consequences.
Tables
Table 1. Homogeneity of the groups under study (N=88).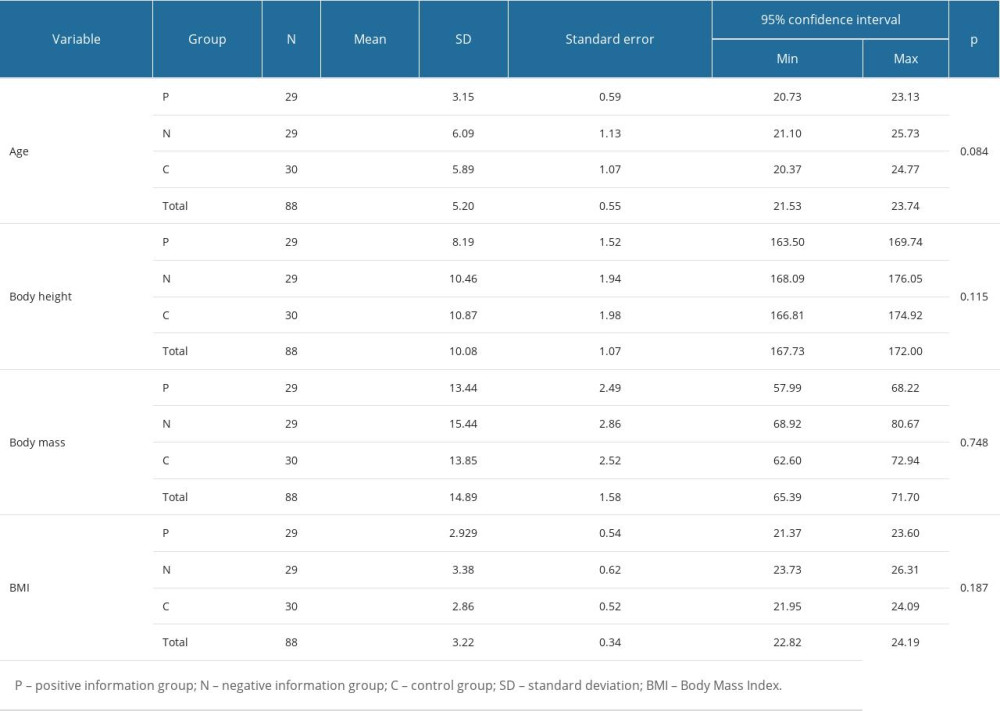 Table 2. Sex distribution in the groups under study (N=88).
Table 2. Sex distribution in the groups under study (N=88).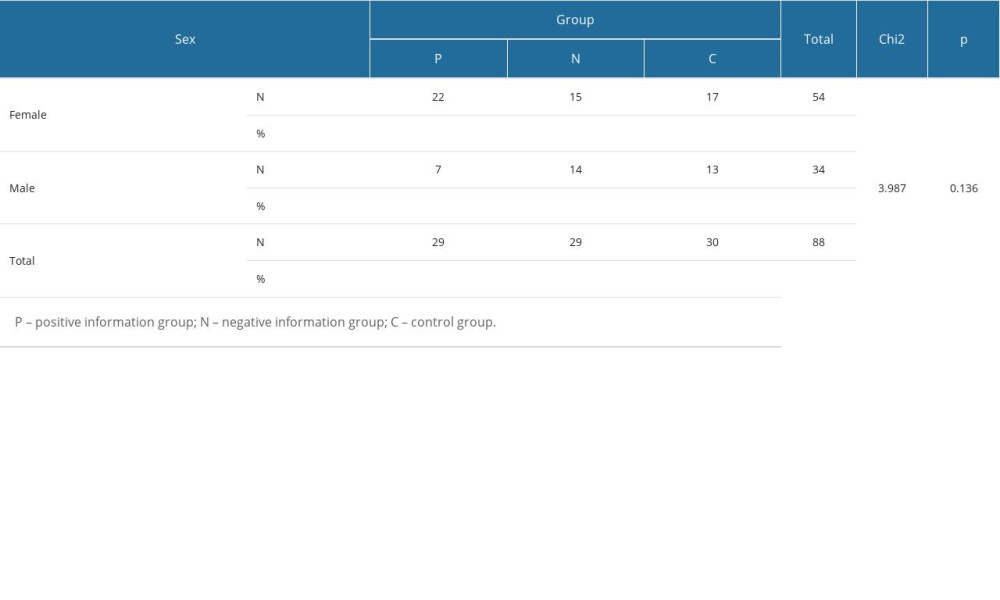 Table 3. Changes in muscle strength and activation in the groups under study (N=88).
Table 3. Changes in muscle strength and activation in the groups under study (N=88).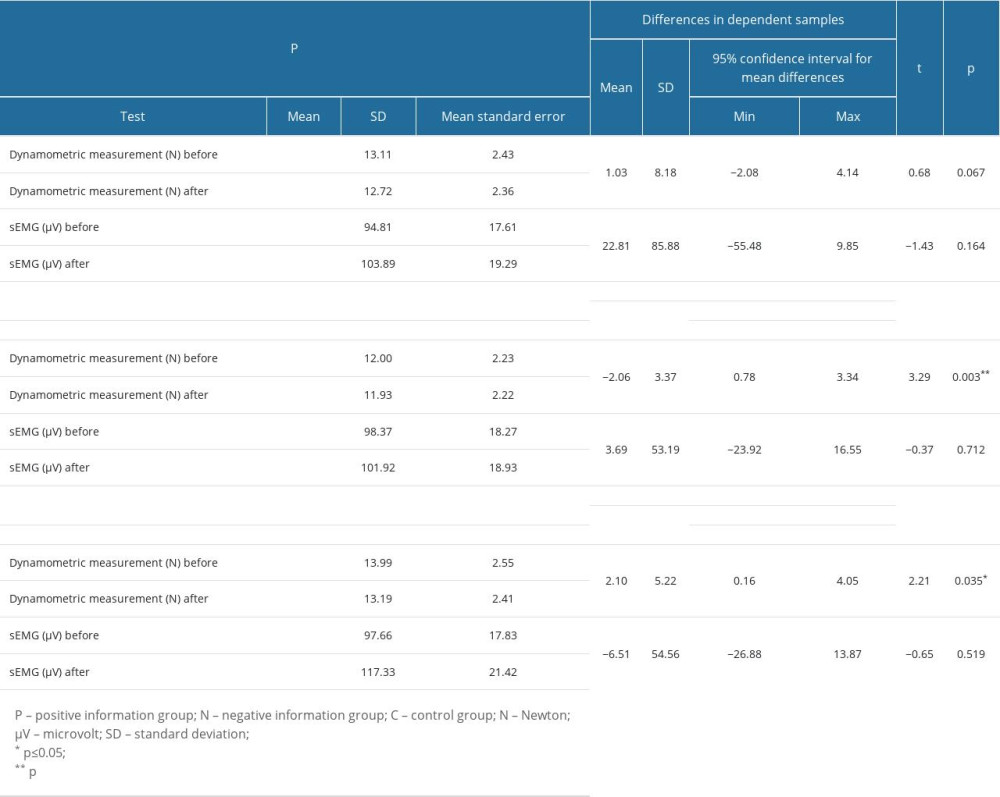 Table 4. Differences in results of dynamometric and sEMG measurements between the groups under study (N=88).
Table 4. Differences in results of dynamometric and sEMG measurements between the groups under study (N=88).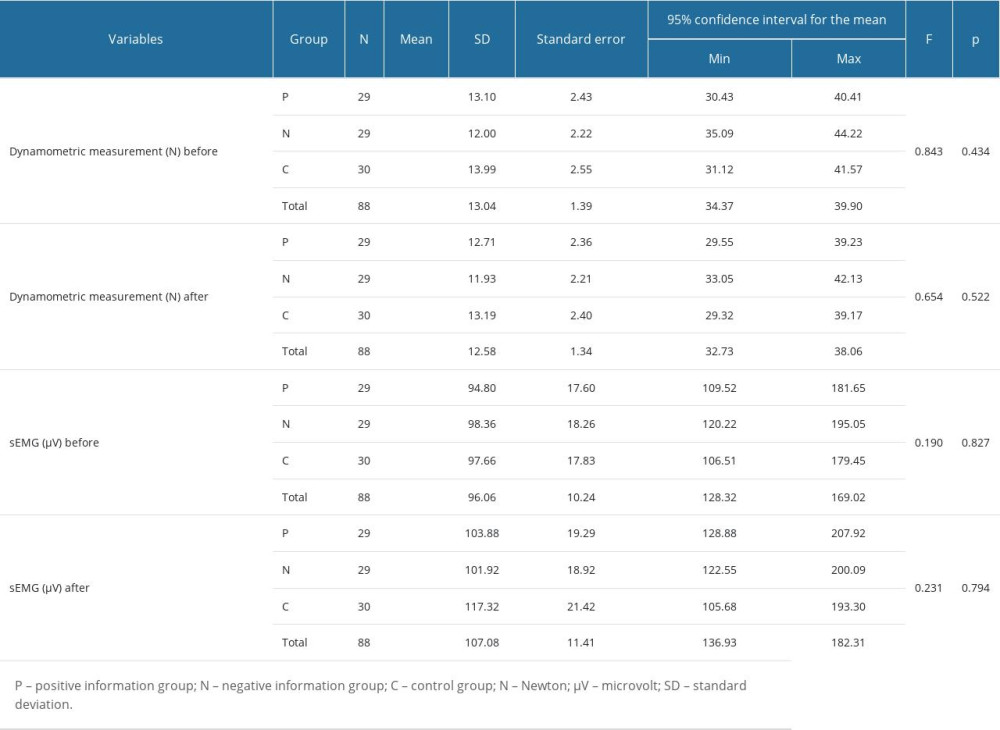 Table 5. Subjective evaluation of changes in muscle strength (N=88).
Table 5. Subjective evaluation of changes in muscle strength (N=88).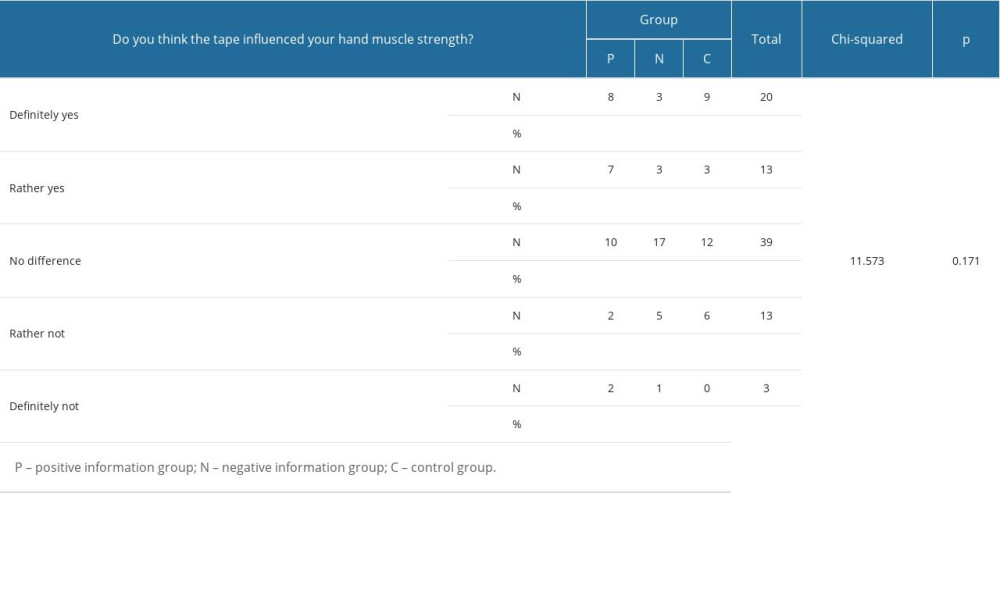 Table 6. Correlations between subjective evaluation of muscle strength and dynamometric and sEMG measurements (N=88).
Table 6. Correlations between subjective evaluation of muscle strength and dynamometric and sEMG measurements (N=88).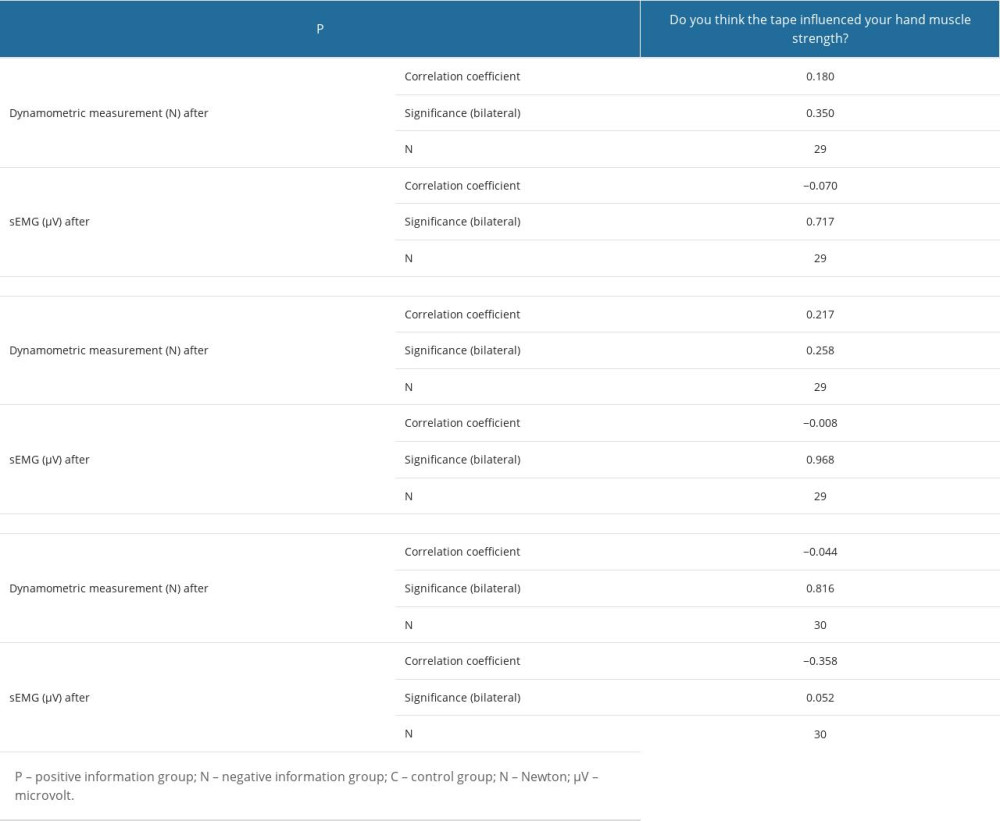
References
1. Koban L, Jepma M, Geuter S, Wager TD, What’s in a word? How instructions, suggestions, and social information change pain and emotion: Neurosci Biobehav Rev, 2017; 81; 29-42
2. Johansson CA, Kent BE, Shepard KF, Relationship between verbal command volume and magnitude of muscle contraction: Phys Ther, 1983; 63(8); 1260-65
3. Belkhiria C, De Marco G, Driss T, Effects of verbal encouragement on force and electromyographic activations during exercise: J Sports Med Phys Fitness, 2018; 58(5); 750-57
4. Guijarro C, A history of the placebo: Neurosciences and History, 2015; 3(2); 68-80
5. Hall KT, Loscalzo J, Kaptchuk TJ, Genetics and the placebo effect: The placebome: Trends Mol Med, 2015; 21(5); 285-94
6. Beedie C, Benedetti F, Barbiani D, Incorporating methods and findings from neuroscience to better understand placebo and nocebo effects in sport: Eur J Sport Sci, 2020; 20(3); 313-25
7. Hansen E, Zech N, Meissner KPlacebo and nocebo: How can they be used or avoided?: Internist (Berl), 2017; 58(10); 1102-10 [in German]
8. Benedetti F, Lanotte M, Lopiano L, Colloca L, When words are painful: Unraveling the mechanisms of the nocebo effect: Neuroscience, 2007; 147(2); 260-71
9. Faasse K, Cundy T, Gamble G, Petrie KJ, The effect of an apparent change to a branded or generic medication on drug effectiveness and side effects: Psychosom Med, 2013; 75(1); 90-96
10. Beedie CJ, Coleman DA, Foad AJ, Positive and negative placebo effects resulting from the deceptive administration of an ergogenic aid: Int J Sport Nutr Exerc Metab, 2007; 17(3); 259-69
11. Hurst P, Schipof-Godart L, Szabo A, The placebo and nocebo effect on sports performance: A systematic review: Eur J Sport Sci, 2020; 20(3); 279-92
12. Bonetti DL, Hopkins WG, Sea-level exercise performance following adaptation to hypoxia: A meta-analysis: Sports Med, 2009; 39(2); 107-27
13. Chowdhury RH, Reaz MB, Ali MA, Surface electromyography signal processing and classification techniques: Sensors (Basel), 2013; 13(9); 12431-66
14. Massy-Westropp N, Rankin W, Measuring grip strength in normal adults: Reference ranges and a comparison of electronic and hydraulic instruments: J Hand Surg Am, 2004; 29(3); 514-19
15. Colloca L, Petrovic P, Wager TD, How the number of learning trials affects placebo and nocebo responses: Pain, 2010; 151(2); 430-39
16. Benedetti F, Mayberg HS, Wager TD, Neurobiological mechanisms of the placebo effect: J Neurosci, 2005; 25(45); 10390-402
17. Beedie CJ, Foad AJ, The placebo effect in sports performance: A brief review: Sports Med, 2009; 39(4); 313-29
18. Corsi N, Emadi Andani M, Sometti D, When words hurt: Verbal suggestion prevails over conditioning in inducing the motor nocebo effect: Eur J Neurosci, 2019; 50(8); 3311-26
19. Pollo A, Carlino E, Vase L, Benedetti F, Preventing motor training through nocebo suggestions: Eur J Appl Physiol, 2012; 112(11); 3893-903
20. Emadi Andani M, Tinazzi M, Modulation of inhibitory corticospinal circuits induced by a nocebo procedure in motor performance: PLoS One, 2015; 10(4); e0125223
21. Maganaris CN, Collins D, Sharp M, Expectancy effects and strength training: Do steroids make a difference?: The Sport Psychologist, 2000; 14(3); 272-78
22. Häuser W, Hansen E, Enck P, Nocebo phenomena in medicine: Their relevance in everyday clinical practice: Dtsch Arztebl Int, 2012; 109(26); 459-65
23. Hansen E, Zech N, Nocebo effects and negative suggestions in daily clinical practice – forms, impact and approaches to avoid them: Front Pharmacol, 2019; 10; 77
24. Zech N, Seemann M, Grzesiek M, Nocebo effects on muscular performance – an experimental study about clinical situations: Front Pharmacol, 2019; 10; 219
25. Elsenbruch S, Enck P, Placebo effects and their determinants in gastrointestinal disorders: Nat Rev Gastroenterol Hepatol, 2015; 12(8); 472-85
26. Keltner JR, Furst A, Fan C, Isolating the modulatory effect of expectation on pain transmission: A functional magnetic resonance imaging study: J Neurosci, 2006; 26(16); 4437-43
27. Lee SY, Soltesz I, Cholecystokinin: A multi-functional molecular switch of neuronal circuits: Dev Neurobiol, 2011; 71(1); 83-91
28. Black CD, Dobson RM, Prior eccentric exercise augments muscle pain and perception of effort during cycling exercise: Clin J Pain, 2013; 29(5); 443-49
29. Li S, Kamper DG, Stevens JA, Rymer WZ, The effect of motor imagery on spinal segmental excitability: J Neurosci, 2004; 24(43); 9674-80
30. Pulvermüller F, Hauk O, Nikulin VV, Ilmoniemi RJ, Functional links between motor and language systems: Eur J Neurosci, 2005; 21(3); 793-97
31. Benedetti F, Amanzio M, Mechanisms of the placebo response: Pulm Pharmacol Ther, 2013; 26(5); 520-23
32. Freeman S, Yu R, Egorova N, Distinct neural representations of placebo and nocebo effects: Neuroimage, 2015; 112; 197-207
33. Amanzio M, Vase L, Mitsikostas DD, Editorial: Nocebo effects and their influence on clinical trials and practice: Modulating factors in healthy and pathological conditions: Front Pharmacol, 2020; 11; 100
34. Colloca L, Barsky AJ, Placebo and nocebo effects: N Engl J Med, 2020; 382(6); 554-61
35. Zaworski K, Baj-Korpak J, Kręgiel-Rosiak A, Gawlik K, Effects of kinesio taping and rigid taping on gluteus medius muscle activation in healthy individuals: A randomized controlled study: Int J Environ Res Public Health, 2022; 19(22); 14889
36. Reicherts P, Gerdes AB, Pauli P, Wieser MJ, Psychological placebo and nocebo effects on pain rely on expectation and previous experience: J Pain, 2016; 17(2); 203-14
37. Felici F, Del Vecchio A, Surface electromyography: What limits its use in exercise and sport physiology?: Front Neurol, 2020; 11; 578504
Figures
Tables
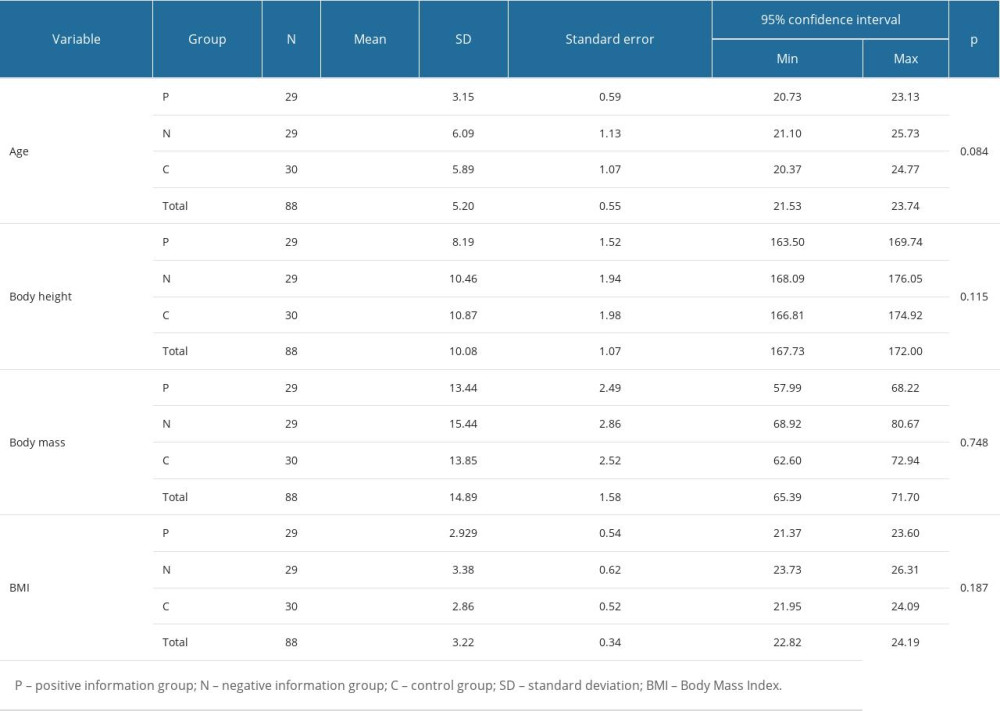 Table 1. Homogeneity of the groups under study (N=88).
Table 1. Homogeneity of the groups under study (N=88).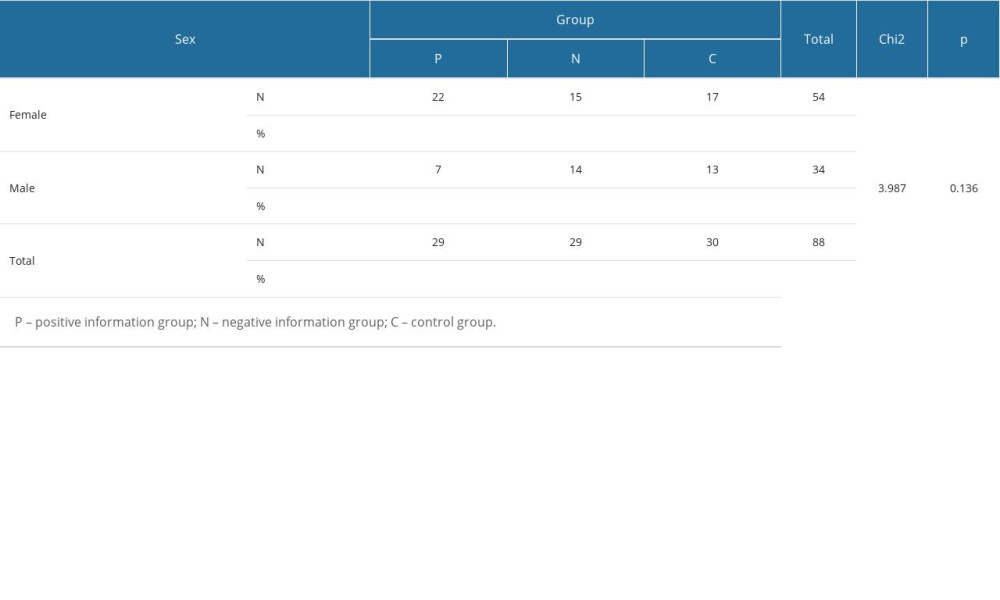 Table 2. Sex distribution in the groups under study (N=88).
Table 2. Sex distribution in the groups under study (N=88).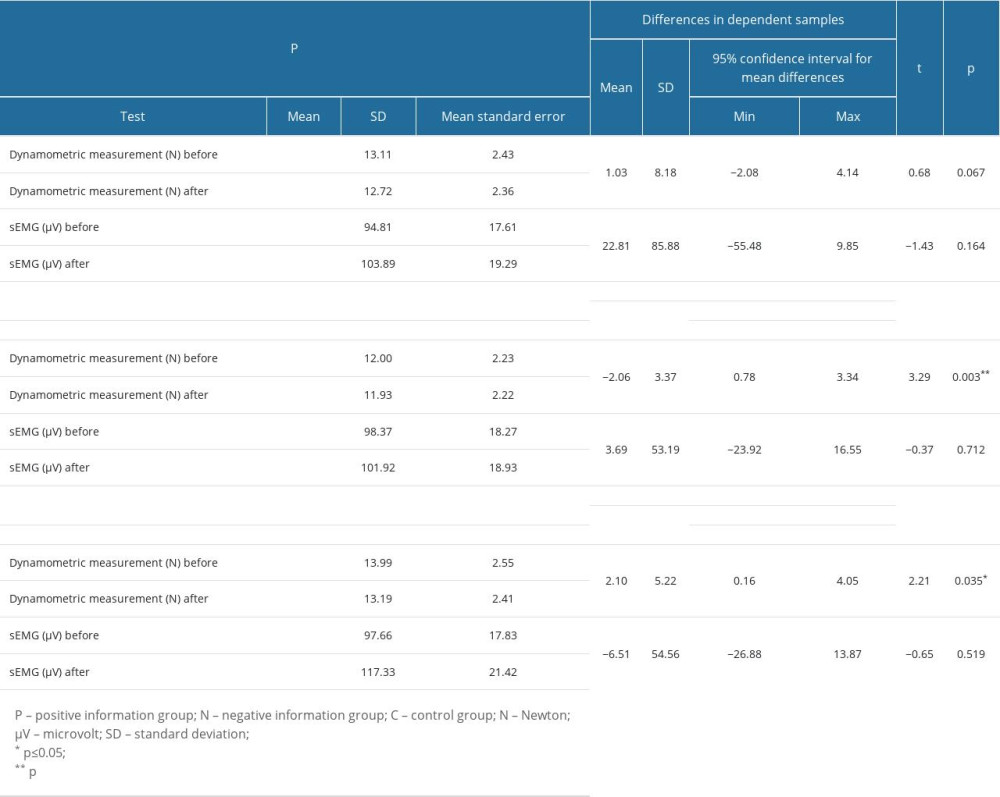 Table 3. Changes in muscle strength and activation in the groups under study (N=88).
Table 3. Changes in muscle strength and activation in the groups under study (N=88).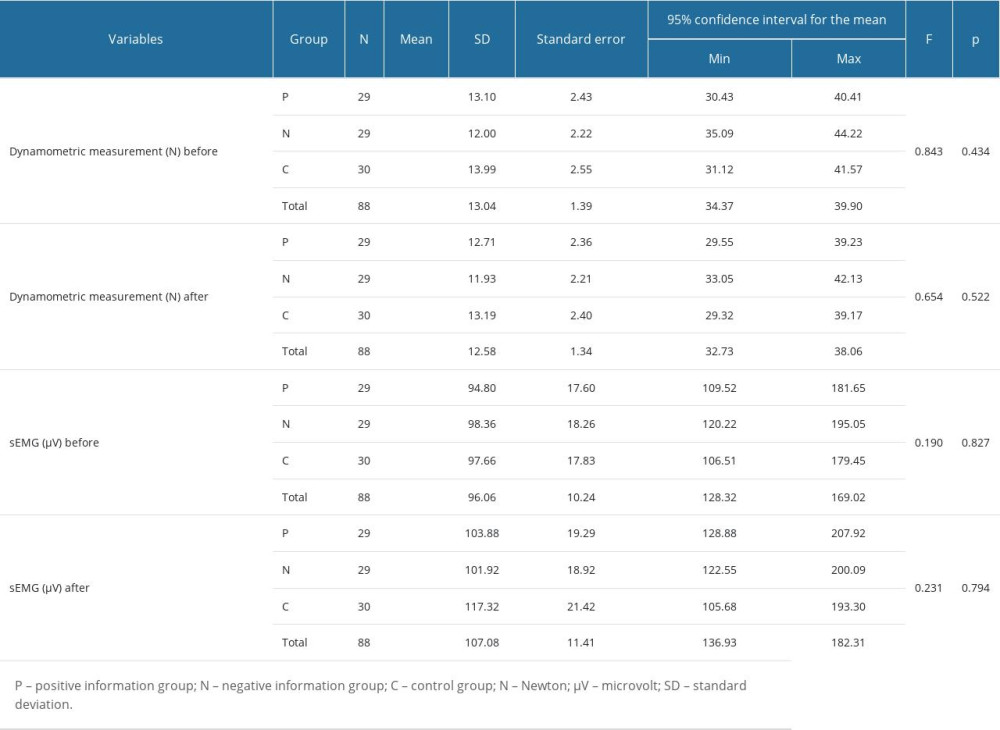 Table 4. Differences in results of dynamometric and sEMG measurements between the groups under study (N=88).
Table 4. Differences in results of dynamometric and sEMG measurements between the groups under study (N=88).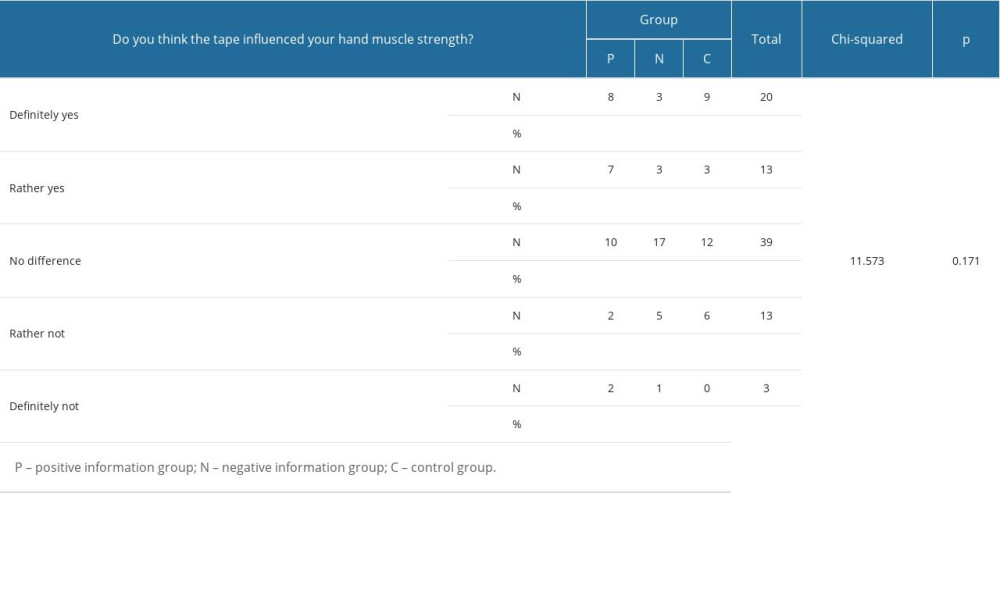 Table 5. Subjective evaluation of changes in muscle strength (N=88).
Table 5. Subjective evaluation of changes in muscle strength (N=88).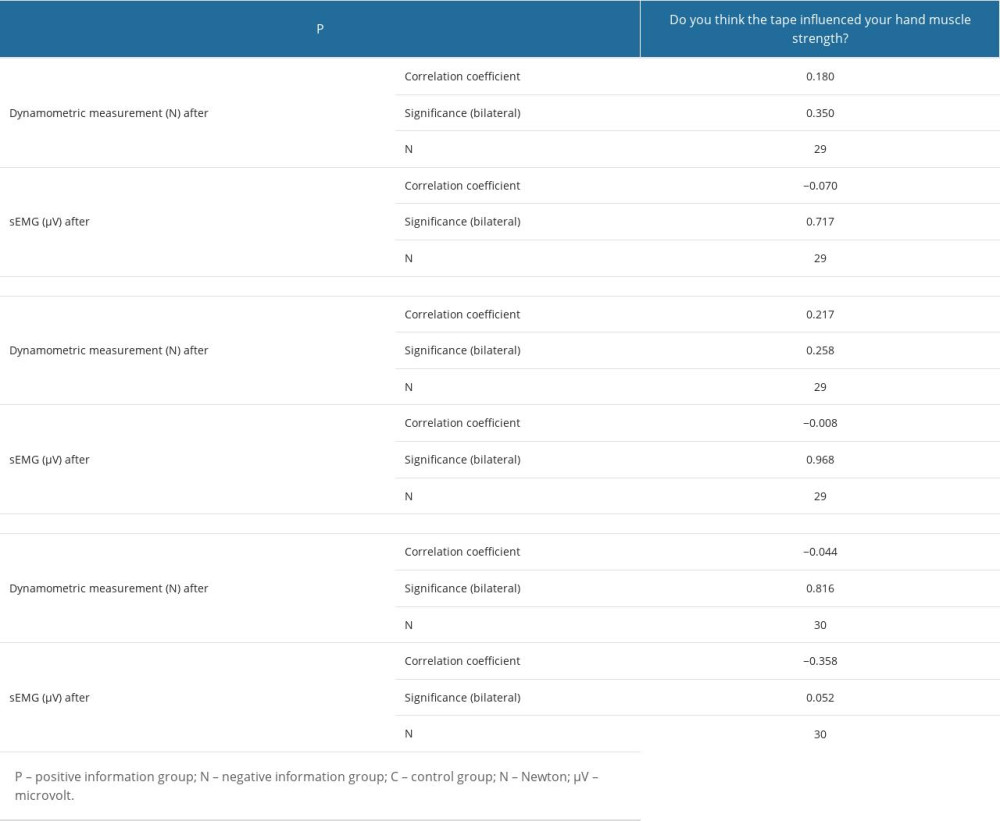 Table 6. Correlations between subjective evaluation of muscle strength and dynamometric and sEMG measurements (N=88).
Table 6. Correlations between subjective evaluation of muscle strength and dynamometric and sEMG measurements (N=88).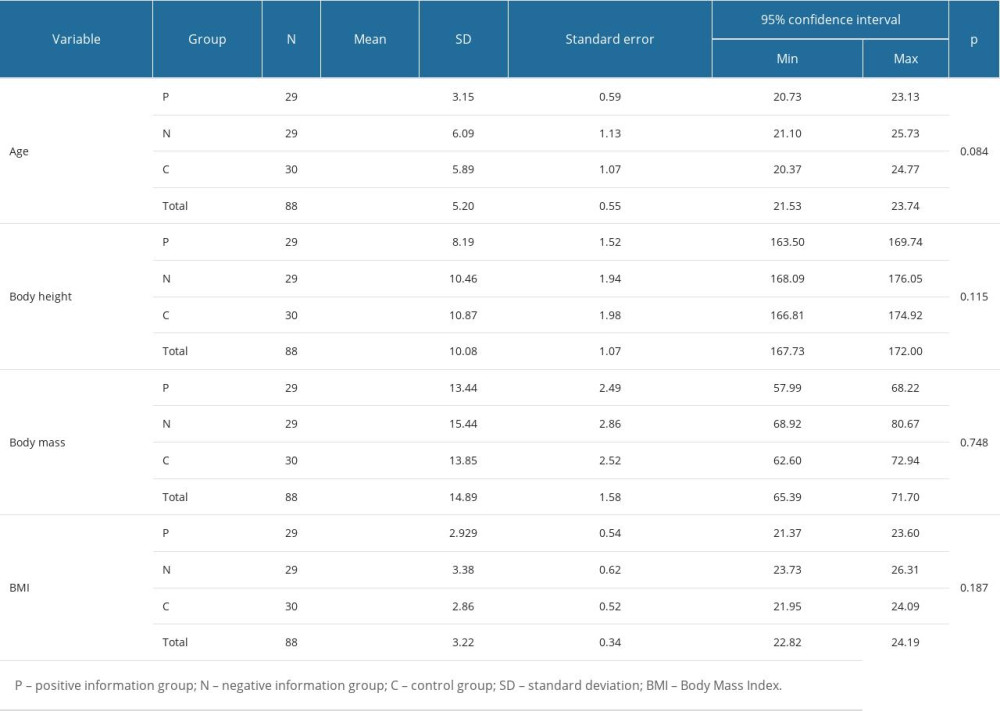 Table 1. Homogeneity of the groups under study (N=88).
Table 1. Homogeneity of the groups under study (N=88).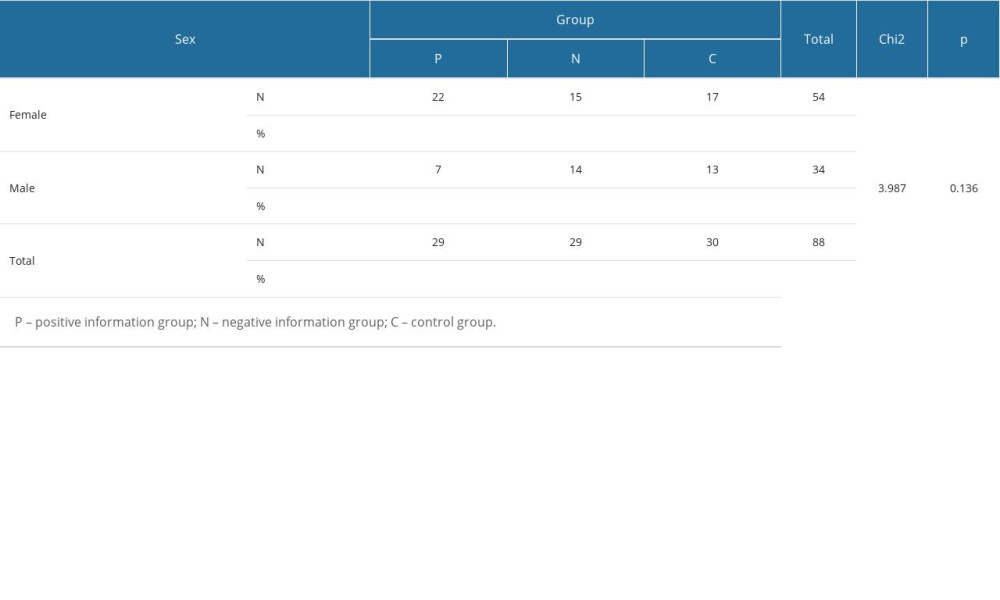 Table 2. Sex distribution in the groups under study (N=88).
Table 2. Sex distribution in the groups under study (N=88).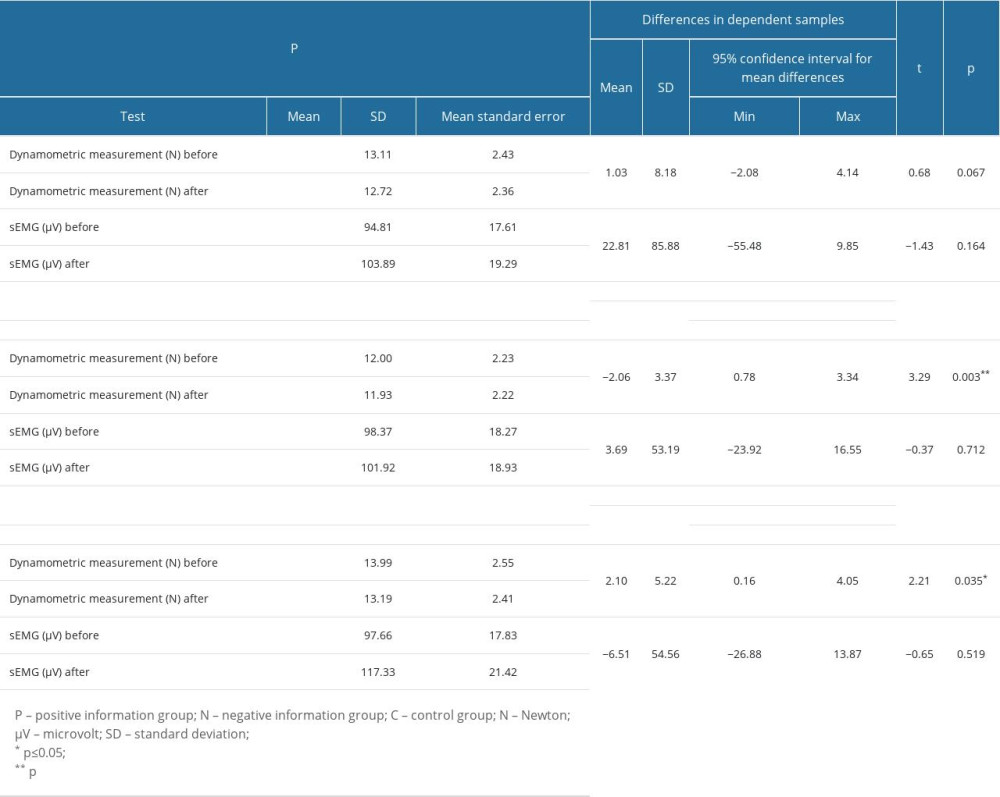 Table 3. Changes in muscle strength and activation in the groups under study (N=88).
Table 3. Changes in muscle strength and activation in the groups under study (N=88).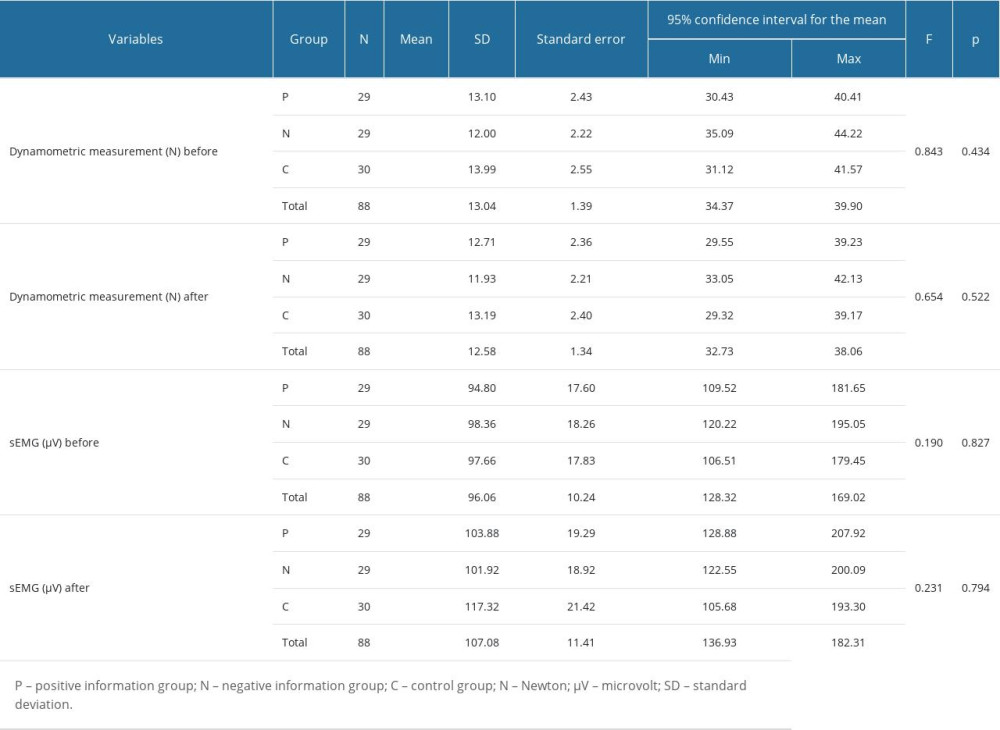 Table 4. Differences in results of dynamometric and sEMG measurements between the groups under study (N=88).
Table 4. Differences in results of dynamometric and sEMG measurements between the groups under study (N=88).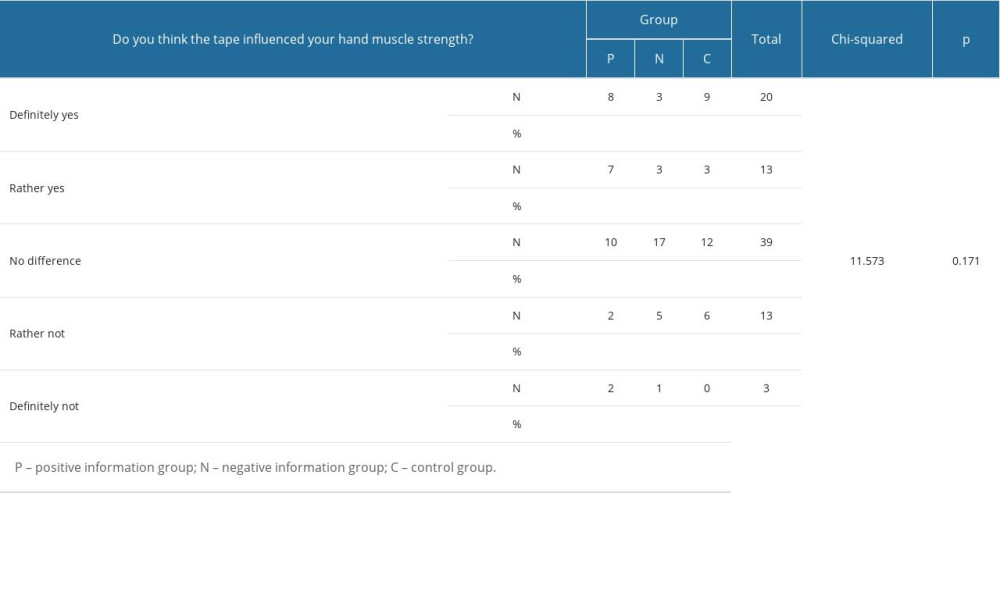 Table 5. Subjective evaluation of changes in muscle strength (N=88).
Table 5. Subjective evaluation of changes in muscle strength (N=88).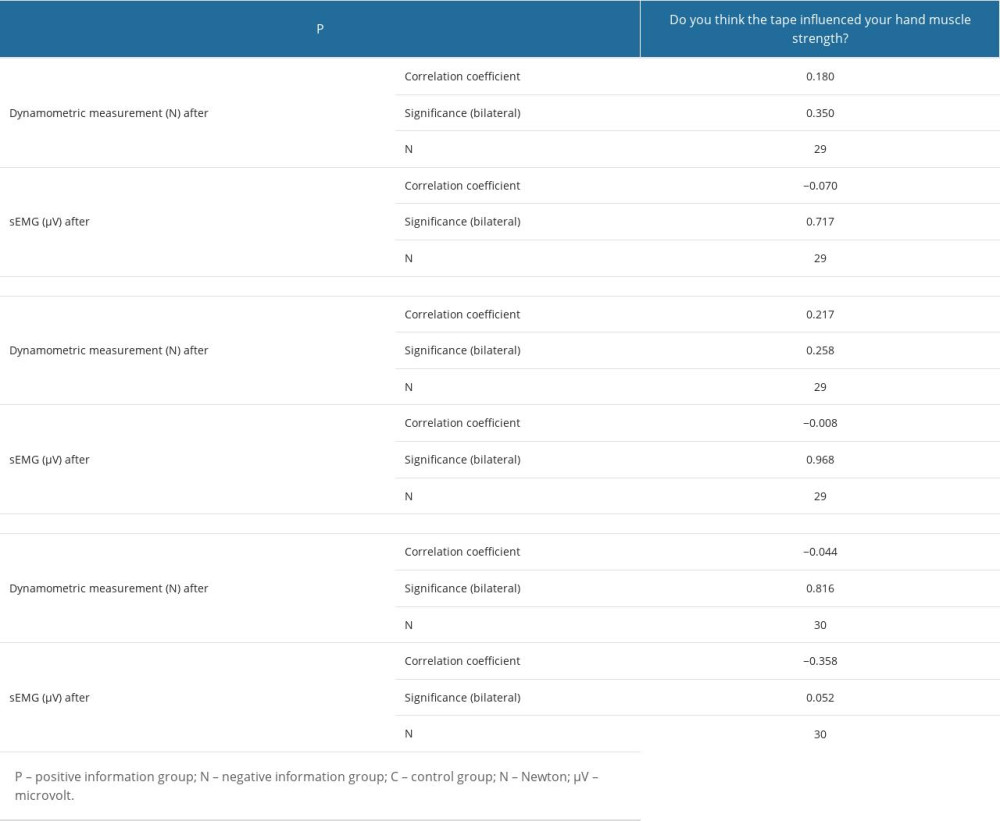 Table 6. Correlations between subjective evaluation of muscle strength and dynamometric and sEMG measurements (N=88).
Table 6. Correlations between subjective evaluation of muscle strength and dynamometric and sEMG measurements (N=88). In Press
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
12 Mar 2024 : Clinical Research
Tissue Inhibitors of Metalloproteinase 1 (TIMP-1) and 3 (TIMP-3) as New Markers of Acute Kidney Injury Afte...Med Sci Monit In Press; DOI: 10.12659/MSM.943500
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952