12 December 2023: Clinical Research
Sleep Quality in Older People: The Impact of Age, Professional Activity, Financial Situation, and Chronic Diseases During the SARS-CoV-2 Pandemic
Grażyna PutoDOI: 10.12659/MSM.941648
Med Sci Monit 2023; 29:e941648
Abstract
BACKGROUND: The SARS-CoV-2 pandemic negatively affected health and social life, notably deteriorating sleep quality in older adults. Studies report inconsistent findings on sleep disturbances during this period, influenced by various physiological, emotional, and sociodemographic factors. This study aimed to identify these determining factors.
MATERIAL AND METHODS: The study was conducted among 342 people 60 years of age or older participating in online classes of randomly selected Senior Clubs and the University of the Third Age in the southern regions of Poland.
RESULTS: Sleep problems (PSQI >5 points) were diagnosed in 250 subjects (83.6%). Logistic regression analysis showed that the quality of sleep significantly depends on: age, as people aged 66-70 were more likely to have better sleep quality than people aged 60-65 (OR=3.07), and those over 70 scored better than people aged 60-65 (OR=2.87); current job – employed people have a better chance of better sleep quality (OR=3.08) than unemployed people; financial situation, people assessing their financial situation as very good/good had a better chance of better sleep quality (OR=2.00) compared to people assessing their financial situation as very bad, bad/average; chronic diseases, people without chronic diseases had a chance of better sleep quality (OR=2.45) than people with chronic diseases.
CONCLUSIONS: Age, financial situation, current job, and chronic disease were the most important factors determining sleep quality in older people. The identification of factors affecting sleep quality can be used as important data to develop interventions and programs to improve sleep quality.
Keywords: Chronic Disease, Frail Elderly, sleep quality, sociodemographic factors
Background
The SARS-CoV-2 virus pandemic, which turned into a global health crisis with high mortality worldwide, has had a negative impact on a number of areas of health and social life, including a particularly vulnerable group of older adults. One of the many affected areas in the older population is sleep.
Studies have shown that the deterioration of the sleep quality of older people during the SARS-CoV-2 virus pandemic was one of the most commonly reported ailments [1–4]. Systematic reviews and meta-analysis have shown that older adults report taking a long time to fall asleep, with more night awakenings and later awakening times, resulting in more time spent in bed but not longer sleep time, which ultimately resulted in poorer sleep quality during the pandemic compared to the period before the outbreak of SARS-CoV-2 virus pandemic [5–10].
A longitudinal study comparing the quality of sleep and the severity of insomnia between the pre-pandemic period and the first wave of the pandemic among older people showed that the incidence of insomnia symptoms increased from 25.4% to 32.2%, and the incidence of insomnia syndrome increased from 16.8% to 19% during the first wave of the pandemic [10]. These results contradict those of other longitudinal studies that do not support changes in sleep quality or insomnia rates in older adults during the pandemic [2,6,11]. Consequently, the change in the sleep quality of older people during the SARS-CoV-2 virus pandemic remains unclear.
In addition to age-related physiological changes leading to changes in the sleep-wake cycle, greater sleep fragmentation, and more frequent naps among older people, the SARS-CoV-2 pandemic has introduced additional factors that may negatively affect sleep in these people [12]. Poor sleep quality, especially if it is chronic, can adversely affect the immune system, disrupting the production of antibodies after vaccination or previous contact with a viral agent. This can lead to increased susceptibility to infectious diseases such as coronavirus disease (COVID-19) [13,14]. In addition, older people with pre-existing sleep problems are more likely to have a poorer prognosis after infection with SARS-COV-2 [14]. Fear of contagion can be considered to be another factor that can negatively affect overall well-being due to high rates of mortality among older people [15]. The pandemic also increased rates of anxiety and depression [15,16], symptoms of post-traumatic stress and intensification of chronic diseases, which in turn worsen the quality of sleep [17] and increase the risk of hospitalization and mortality [2,18,19].
Pandemic factors such as the lockdown and social isolation may increase feelings of loneliness and directly impact older people’s sleep [14]. Reduced exposure to light, less time spent outdoors, and increased exposure to light-emitting electronics disrupt circadian rhythms, causing or perpetuating insomnia [5,14]. The lack of stimuli related to family and social activity and a monotonous lifestyle may contribute to sleep problems. Another important factor among older people is loneliness. Social and emotional support for this population was important during the pandemic to reduce the emotional burden and consequently insomnia and other sleep-related symptoms [14,20]. Cross-sectional studies have shown that sociodemographic factors such as female gender, lower educational attainment, and greater financial burden caused by the COVID-19 pandemic were associated with poorer sleep quality among older adults [5,9,19,21].
The decline in sleep quality associated with the SARS-CoV-2 virus pandemic can have significant negative consequences for health and well-being, so it is extremely important to identify these factors as key health consequences of the global pandemic. Due to the pandemic-related limitations in this period, Computer Assisted Web Interview (CAWI) was used as the research technique in the study, which allowed for the dissemination of the online questionnaire. The aim of the study was to identify factors determining sleep quality of older people during the SARS-CoV-2 virus pandemic.
Material and Methods
DATA COLLECTION:
The presented results come from a cross-sectional study conducted in the years 2021–2022 on a sample of 342 community-dwelling older people (at least 60 years old). The study was conducted using a diagnostic survey. A link to the survey was made available to older people participating in online classes of randomly selected Senior Clubs and the University of the Third Age in the southern regions of Poland. The study used the Computer Assisted Web Interview (CAWI) research technique. This technique allows for the dissemination of the questionnaire via a link to the website, preserving full anonymity of the respondents and granting the possibility to answer questions at a convenient time and enabling the researcher to collect reliable data [22]. The survey was developed in Polish using the Google Forms tool. Completing online questionnaires is a well-established method in healthcare research. The data collection process is simplified and accelerated, ensuring greater completeness of data [23–25]. The data collected during this study were anonymized, which makes it impossible to identify the people participating in the study. At the beginning of the questionnaire there was a short introduction explaining the purpose of the study and instructions on how to complete it. The survey also contained information stating that the answers will be analyzed in aggregate statistical lists and will be used for scientific purposes only. Each person completing the survey was also informed about anonymity and the possibility to stop taking the survey at any time without giving a reason. The e-mail address of the study’s lead researcher was also included in the introduction to the survey in case of questions or concerns. The criteria for inclusion in the study were: expressing informed consent to participate in the study, being 60 years of age or older, and computer/internet access. The exclusion criteria were: lack of consent to participate in the study, age below 60, and no computer/internet access.
GENERAL CHARACTERISTICS:
The study used a questionnaire which included questions on demographic and social characteristics (age, gender, place of residence, marital status, structure of residence, education, current job, and financial situation), clinical status (presence of chronic diseases and scope of locomotion – moving independently/moving with the help of rehabilitation equipment), factors related to the SARS-CoV-2 virus pandemic (having been infected or coming into contact with people infected with the SARS-CoV-2 virus, loved ones infected/deceased during the pandemic, hospitalization related to COVID-19 infection, a sense of emptiness in life, limited contact with relatives, and a limitation of hobbies during this period).
PITTSBURGH SLEEP QUALITY INDEX – PSQI: Sleep quality over the previous 4 weeks was assessed using the Pittsburgh Sleep Quality Index (PSQI), which is the most widely used tool in clinical and research studies [26]. The questionnaire consists of 9 questions with sub-items (19 items in total). The first 4 questions concern the time of going to sleep, getting up, waiting to fall asleep, and the average sleep time, to which the subject answers by giving values. Responses are expressed in minutes or hours (quantitative assessment). Other questions concern the frequency of problems affecting sleep (eg, number of awakenings at night due to breathing difficulties, pain, coughing, snoring, or inappropriate temperature in the bedroom). Each of the items in this part is assessed on a 4-point scale corresponding to the severity of the given ailments (0 – no difficulties in the last weeks, 1 – difficulty less than once a week, 2 – difficulty once or twice a week, 3 – difficulty experienced 3 or more times a week).
The questionnaire enables the assessment of 7 parameters (components) of sleep: 1) subjective sleep quality – a qualitative assessment, 2) sleep latency – a quantitative assessment, analysis of the time needed to fall asleep (in minutes) and the number of nights when the time to fall asleep was longer than 30 minutes, 3) sleep duration – quantitative assessment, actual sleep duration (in hours), 4) sleep efficiency – quantitative assessment, ratio of the actual amount of sleep to the time spent in bed, 5) sleep problems – quantitative assessment of sleep problems resulting from specific ailments and inconveniences such as cough, pain, or cold, 6) use of sleep medication – quantitative assessment of used sleeping medications expressed in the number of doses taken, 7) daytime dysfunction – qualitative and quantitative assessment of sleepiness and alertness during daily activities [26].
The Global PSQI score for all components of the PSQI scale ranges from 0 to 21 points, with a higher score meaning poorer sleep quality. A score above 5 points denotes sleep problems (PSQI >5 points), while ≤5 points denotes a lack of sleep problems (PSQI ≤5 points). The Cronbach’s alpha reliability coefficient for the PSQI questionnaire was 0.83 [27].
STATISTICAL ANALYSIS:
Distributions of qualitative variables are described by the absolute number of individual categories (N) and their percentage share in the distribution of the variable (%). The average values of quantitative and ordinal variables are described using the mean and standard deviation (SD), as well as the median and the first and third quartiles (Q1–Q3). Correlations between qualitative variables are presented in the form of cross tables. The analysis of statistical significance of these correlations was performed using Pearson’s chi-square test. Comparison of the average values of variables with significantly different from normal distributions in 2 unrelated groups was performed using the Mann-Whitney (pM-W) test for dependent variables measured at the interval measurement level and the Kolmogorov-Smirnov test for dependent variables measured at the ordinal measurement level. As univariate analysis provided many significant correlations between sleep quality and other variables, additional analyses were conducted to exclude those which could be spurious correlations and to determine the factors affecting occurrence of sleep problems. These analyses were performed using a multivariate logistic regression model, the results of which are presented in the form of odds ratios (OR) and the corresponding 95% confidence intervals (95% CI) and the test probability value
Effects for which the
ETHICAL PROCEDURES:
The research procedure was carried out in accordance with the Helsinki Declaration of the World Medical Association [28] and the ethical codes of the Belmont Report [29]. Approval of the Jagiellonian University Bioethics Committee (No. 1072.6120.305.2021) was obtained.
Results
DEMOGRAPHICS AND SOCIAL CHARACTERISTICS OF STUDY GROUP:
Among the 342 people 60 years of age or older covered by the presented analysis (219 women, 123 men), women predominated (64%). The mean age in the study group was 70.3 years (±7.3; min. 60 years, max. 98 years). Women had a significantly lower mean age than men (69.4±6.93 vs 71.8 years±6.68; P=0.003). The demographic and social characteristics of the study group are presented in Table 1.
Sleep quality assessed using the Pittsburgh Sleep Quality Index (PSQI) showed no significant differences between men and women. The average time waiting to fall sleep (sleep latency) among women was longer than among men (33.15±25.76 vs 29.11±21.72 minutes), women also spent slightly more time in bed than men (8.41±25.76 1.22 vs 8.17±0.97 hours). Total sleep time was slightly higher among men than among women (6.77±0.97 vs 6.67±1.15 hours).
DEMOGRAPHIC AND SOCIAL VARIABLES DETERMINING SLEEP:
Sleep problems (PSQI >5 points) – were diagnosed in 250 subjects (83.6%). Among the demographic and social variables, a statistically significant correlation was found between sleep problems and:
There were no significant correlations between sleep problems and the analyzed demographic and social variables, such as: gender, age, place of residence and work (Table 2).
CLINICAL STATUS AND FACTORS RELATED TO THE SARS-COV-2 VIRUS PANDEMIC DETERMINING SLEEP IN THE STUDY GROUP:
The analysis of variables concerning the clinical condition of the subjects showed a statistically significant correlation between sleep problems and:
Among the analyzed variables regarding factors related to the SARS-CoV-2 virus pandemic, there were significant correlations between sleep problems and:
LOGISTIC REGRESSION ANALYSIS OF THE CORRELATIONS BETWEEN DEMOGRAPHIC AND SOCIAL VARIABLES, CLINICAL CONDITION, FACTORS CAUSED BY THE SARS-COV-2 VIRUS PANDEMIC, AND SLEEP QUALITY:
To determine the impact of demographic and social variables, clinical status, and the SARS-CoV-2 virus pandemic on the sleep quality of older people, multivariate logistic regression models were used.
Model 1 of the logistic regression included the assessment of the sleep quality of older people conditioned by demographic and social variables. The analysis of the model showed that the quality of sleep significantly depends on:
Clinical condition was included in logistic regression model 2. The analysis of this model showed that the quality of sleep significantly depends on the following factors:
Model 3 included the variables of model 2 and the factors related to the SARS-CoV virus pandemic. The analysis of the model showed that the quality of sleep significantly depends on the following factors:
Discussion
This study analyzed the factors determining sleep quality among older people during the SARS-CoV-2 virus pandemic. In the obtained results of the study conducted among 342 people over 60 years of age, the prevalence of sleep problems (PSQI >5 points) was 83.6%, which is a relatively high value.
Research conducted in Brazil confirms that sleep quality deteriorated during the COVID-19 pandemic, especially among people in quarantine, women, and older people. The authors of the study compared sleep parameters measured using the PSQI questionnaire before and during the COVID-19 pandemic. The results obtained during the COVID-19 pandemic showed later waking hours (increase from 5.91±1.04 vs 6.43±1.24 h), which resulted in longer time spent in bed (7.6±1.24 vs 8.25±1.54 h), but not in longer sleep time (6.87±1.52 vs 6.84±1.6 h). Sleep latency was also slightly longer (25.0±34.4 vs 33.4±38.4 min), while sleep efficiency was reduced (90.18±14.04 vs 83.63±16.27%). The authors of the study justify this, among others, by psychosocial factors (such as anxiety or social isolation) as well as environmental factors (reduced activity or exposure to light) [5]. In our own study conducted during the COVID-19 pandemic, the obtained results of the logistic regression analysis showed that people with a sense of emptiness in their lives caused by the SARS-CoV-2 virus pandemic were about 5 times less likely to have better sleep quality than people who did not experience this emptiness. People without chronic diseases were more likely to have better sleep quality compared to those with chronic diseases. The impact of chronic diseases on the quality of sleep during the SARS-CoV-2 virus pandemic has also been confirmed in other studies [12,30]. It was shown that older people with chronic diseases may experience pain that negatively affects the quality of sleep [12,30]. In addition, older people with chronic diseases often have a dry mouth (after taking medications, which results in the need to drink more water and thus leads to an increased number of awakenings at night, affecting the quality of sleep [31].
Studies have also shown that depression and anxiety are risk factors for poor sleep quality among older people [12]. However, a retrospective study conducted in China showed that poor sleep quality predisposes to the occurrence of severe inflammatory bowel disease [32]. Our own study did not assess the impact of depression and anxiety on the quality of sleep in the study group.
Studies show that sleep quality varies by gender and age [12,21]. Our study failed to confirm the dependence on gender. It can be assumed that this is related to the increase in the total prevalence of sleep problems (women 74%, men 71.5%). The more frequent occurrence of sleep disorders among women than men during the SARS-CoV-2 virus pandemic, also confirmed in other studies, may be associated with more frequent health problems among women [4]. The obtained results of the logistic regression analysis in our study regarding the correlation with age show a greater chance of better sleep quality among people aged 66–70 and over 70 than among people aged 60–65. In a study conducted in Egypt [33] the results of logistic regression analysis showed that sleep problems are less likely among people over age 75 compared to those aged 60–75. The authors of the study explain that people aged 60–75 have more responsibilities over family members when they are not working compared to those who are over age 75 [33].
The correlation between the presence of sleep problems and the level of education was also confirmed in the present study. People with primary/vocational education (83.8%) experienced sleep problems significantly more often than people with higher education (64.1%). A higher level of education is most often associated with a higher standard of living, better health awareness, and thus effective prevention of chronic diseases that disrupt the quality of sleep [34]. The correlation between the quality of sleep and the level of education and economic status is also confirmed by other studies [21]. Logistic regression analysis in the present study showed that people who are professionally active and in a better financial situation were more likely to have better quality of sleep than people who do not work. The impact of professional activity on sleep quality has also been confirmed in other studies. Professionally active older people had better sleep quality than people who stopped their professional activity, which might result in financial hardship aggravated by the frequent presence of comorbidities [5,9,19,21,34]. Retirement is associated not only with a decline in psychophysical activity but also with a change in daily rhythm, which rarely remains at the same level after retiring from professional activity.
The results of the logistic regression analysis of sleep problems in relation to the structure of residence obtained by us are consistent with the results of other authors [35,36]. They indicate a higher incidence of sleep problems among people living alone. In situations such as the recent SARS-CoV-2 virus pandemic, older people who live alone were particularly vulnerable to social isolation [19,37]. In a situation where face-to-face contact is difficult due to social distancing, participating in social gatherings and activities via smartphones can be an effective support system for older people living alone, which may ultimately lead to improved sleep quality [38].
According to the conducted systematic review and meta-analysis of research, one of the strongest sources of support for older people is a spouse, which can result in a healthy lifestyle, emotional support, better maintenance of living standards and, above all, a better quality of life compared to people living alone [19,20,37]. In addition, living with a spouse or family has been found to have a very positive correlation with mental health in old age, which can be explained by mutual support [20,37]. The correlation between marital status and sleep problems was confirmed in this study as well as in other studies [39]. Unmarried people are significantly more likely to have sleep problems than married people.
It should be emphasized that the present study has some limitations. The conducted study was cross-sectional, which makes it impossible to assess the correlation in terms of cause and effect; therefore, the links between the analyzed variables should be carefully interpreted. The study was conducted using the Computer Assisted Web Interview (CAWI) technique, which can only be used by people using information and communication technologies (a computer with access to the Internet). This technique, on the other hand, allows the respondent to maintain full anonymity, the ability to answer questions at a convenient time, and allows the researcher to collect reliable data. In addition, it should be noted that the surveyed group could not rely on the help of the interviewer, but only on the meticulously prepared instructions. Sleep problems were assessed only on the basis of subjective assessment, while environmental factors such as noise and light levels were not taken into account. In future research, it is necessary to investigate the factors that interfere with sleep in even greater detail. Further longitudinal studies are needed to explain the impact of factors determining sleep problems in relation to the functioning of older people.
Conclusions
Age, financial situation, current job, and chronic disease were the most important factors determining sleep quality in older people. In addition, the sense of emptiness in life during the SARS-CoV-2 virus pandemic was also a factor determining quality of sleep. The identification of factors which reduce sleep quality can be used as important data to develop interventions and programs to improve sleep quality. There is therefore a need for in-depth research on sleep problems in older people. It is necessary to educate this population in the field of sleep hygiene and to promote an active lifestyle or use of behavioral and cognitive therapy.
Tables
Table 1. Demographic and social characteristics of the study group.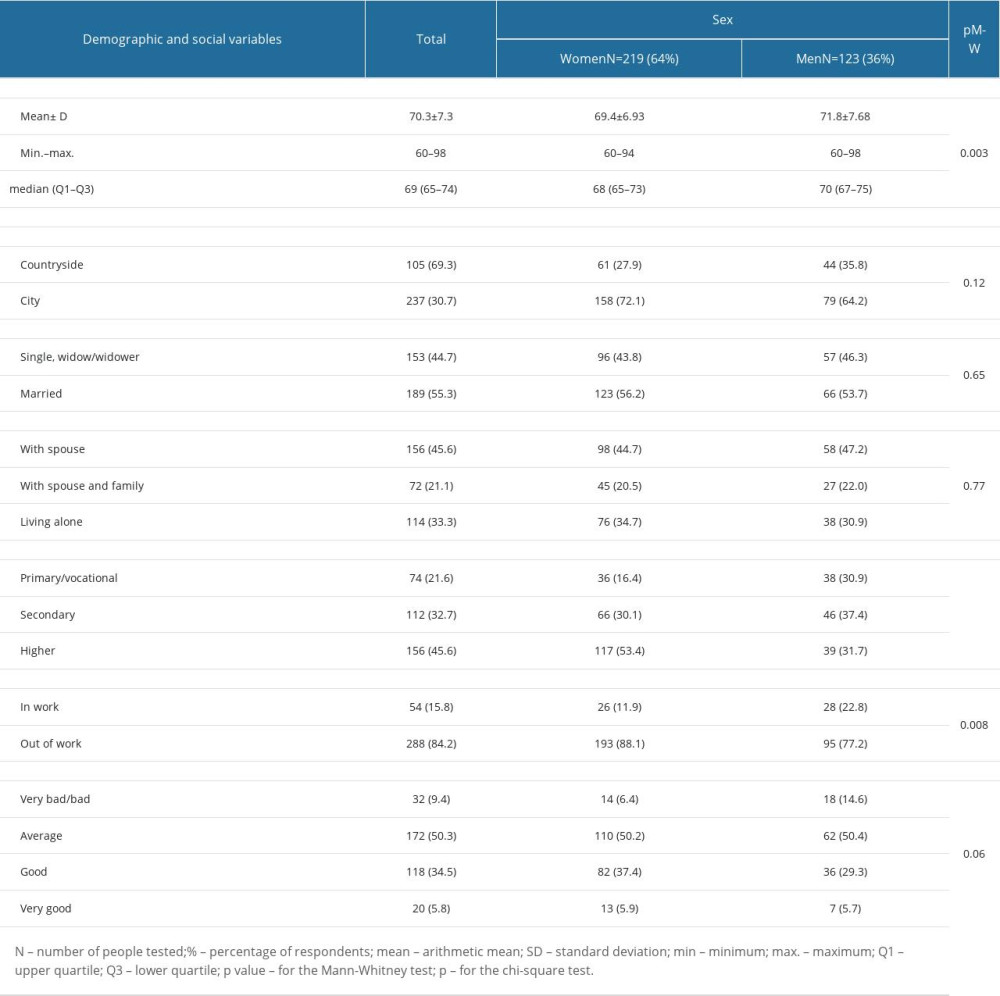 Table 2. Demographic and social variables determining sleep in the study group.
Table 2. Demographic and social variables determining sleep in the study group.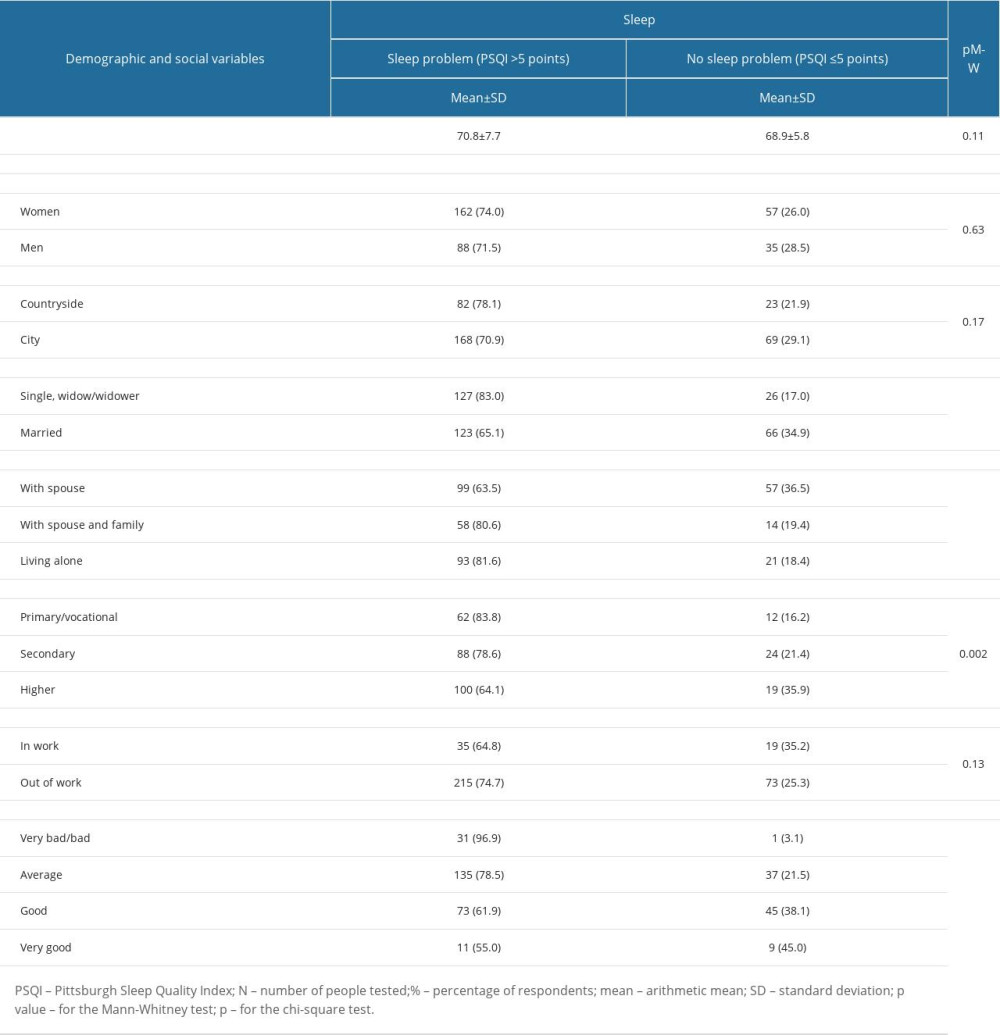 Table 3. Clinical status and factors related to the SARS-CoV-2 virus pandemic affecting sleep in the study group.
Table 3. Clinical status and factors related to the SARS-CoV-2 virus pandemic affecting sleep in the study group.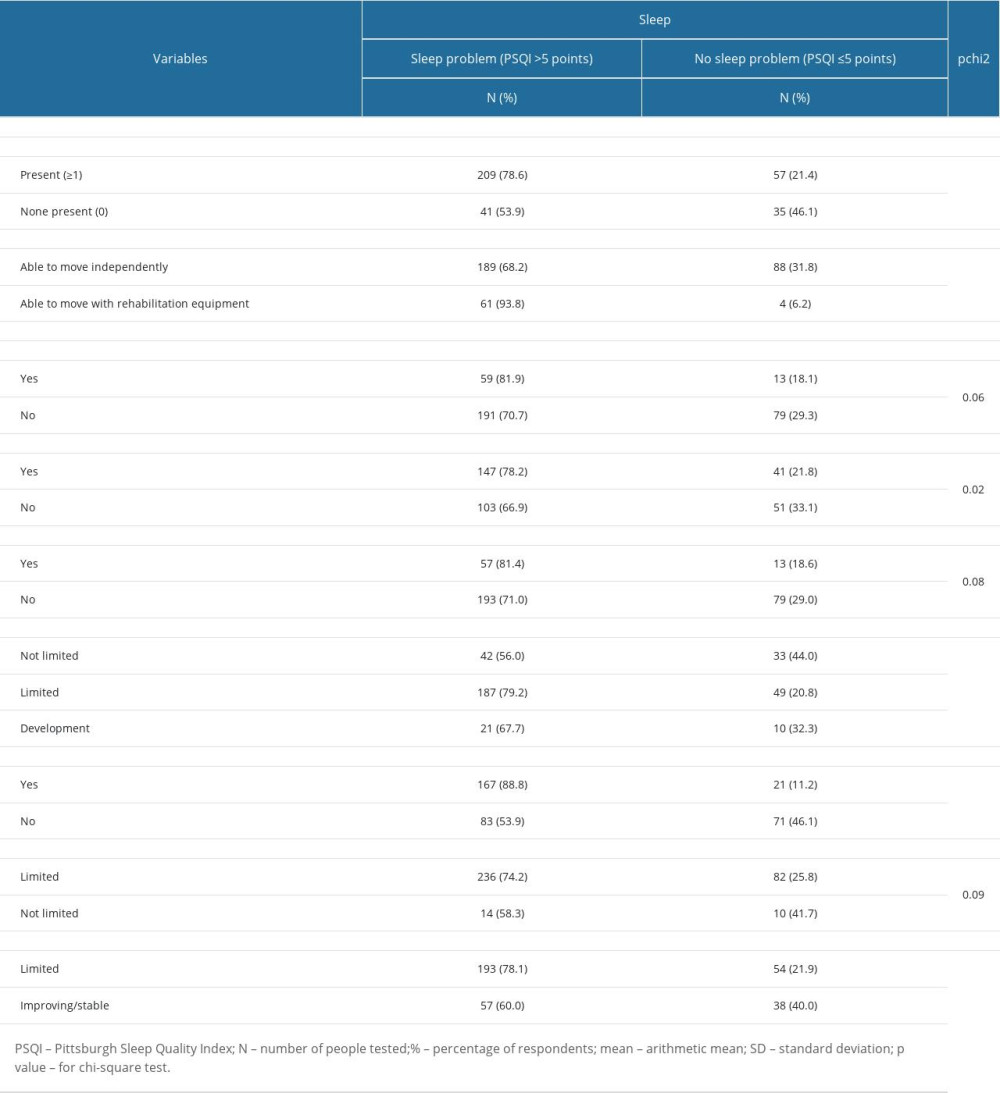 Table 4. Logistic regression analysis of the relationship between sleep quality and demographic and social variables, clinical status, and the factors caused by the SARS-CoV-2 virus pandemic.
Table 4. Logistic regression analysis of the relationship between sleep quality and demographic and social variables, clinical status, and the factors caused by the SARS-CoV-2 virus pandemic.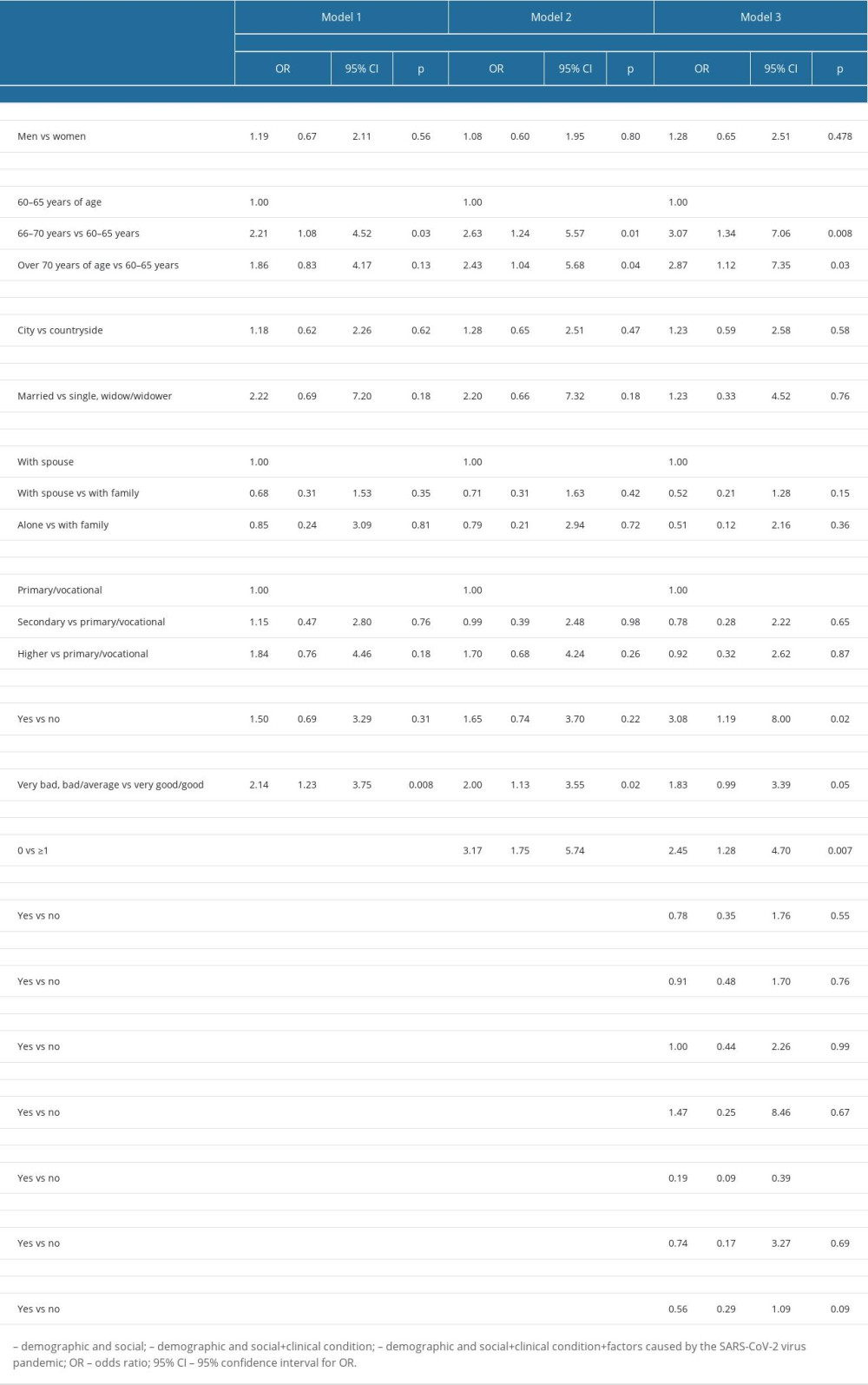
References
1. Wang J, Gong Y, Chen Z, Sleep disturbances among Chinese residents during the Coronavirus Disease 2019 outbreak and associated factors: Sleep Med, 2020; 74; 199-203
2. Parveen S, George SM, Chand S, Was sleep a problem for the elderly during COVID-19?: Sleep Vigil, 2021; 5(2); 197-203
3. Emerson KG, Coping with being cooped up: Social distancing during COVID-19 among 60+ in the United States: Rev Panam Salud Publica, 2020; 44; e81
4. de Almondes KM, Castro EAS, Paiva T, Morbidities Worsening Index to sleep in the older adults during COVID-19: Potential moderators: Front Psychol, 2022; 13; 913644
5. Taporoski TP, Beijamini F, Gómez LM, Subjective sleep quality before and during the COVID-19 pandemic in a Brazilian rural population: Sleep Health, 2022; 8(2); 167-74
6. Kocevska D, Blanken TF, Van Someren EJW, Rösler L, Sleep quality during the COVID-19 pandemic: not one size fits all: Sleep Med, 2020; 76; 86-88
7. Taillard J, Gronfier C, Bioulac S, Sleep in normal aging, homeostatic and circadian regulation and vulnerability to sleep deprivation: Brain Sci, 2021; 11; 1003
8. Trabelsi K, Ammar A, Masmoudi L, Sleep quality and physical activity as predictors of mental wellbeing variance in older adults during COVID-19 lockdown: ECLB COVID-19 International online survey: Int J Environ Res Public Health, 2021; 18; 4329
9. Mandelkorn U, Genzer S, Choshen-Hillel S, Escalation of sleep disturbances amid the COVID-19 pandemic: A cross-sectional international study: J Clin Sleep Med, 2021; 17(1); 45-53
10. Morin CM, Vézina-Im LA, Ivers H, Prevalent, incident, and persistent insomnia in a population-based cohort tested before (2018) and during the first-wave of COVID-19 pandemic (2020): Sleep, 2022; 45(1); zsab258
11. Amicucci G, Salfi F, D’Atri A, Viselli L, Ferrara M, The differential impact of COVID-19 lockdown on sleep quality, insomnia, depression, stress, and anxiety among late adolescents and elderly in Italy: Brain Sci, 2021; 11(10); 1336
12. Wang J, Qin W, Pang M, The effect of chronic disease and mental health on sleep quality among migrant elderly following children in Weifang City, China: Int J Environ Res Public Health, 2022; 19; 12734
13. Benedict C, Cedernaes J, Could a good night’s sleep improve COVID-19 vaccine efficacy?: Lancet Respir Med, 2021; 9(5); 447-48
14. Pires GN, Ishikura IA, Xavier SD, Sleep in older adults and its possible relations with COVID-19: Front Aging Neurosci, 2021; 13; 647875
15. Wong SYS, Zhang D, Sit RWS, Impact of COVID-19 on loneliness, mental health and health service utilisation: A prospective cohort study of older adults with multimorbidity in primary care: Br J Gen Pract, 2020; 70; e817-e24
16. Liao G, Huang B, Lee PM, Differences in sleep patterns and mental health problems during different periods of COVID-19 outbreak among community-dwelling older men in Hong Kong: Int J Public Health, 2022; 67; 1604363
17. Cipriani GE, Bartoli M, Amanzio M, Are sleep problems related to psychological distress in healthy aging during the COVID-19 pandemic? A review: Int J Environ Res Public Health, 2021; 18(20); 10676
18. Chao AM, Wadden TA, Clark JM, Changes in the prevalence of symptoms of depression, loneliness, and insomnia in U.S. older adults with type 2 diabetes during the COVID-19 pandemic: The look AHEAD study: Diabetes Care, 2022; 45(1); 74-82
19. Polenick CA, Daniel NR, Perbix EA, Factors associated with sleep disturbances related to the COVID-19 pandemic among older adults with chronic conditions: Am J Geriatr Psychiatry, 2021; 29(11); 1160-65
20. Deng M, Qian M, Lv J, Guo C, Yu M, The association between loneliness and sleep quality among older adults: A systematic review and meta-analysis: Geriatric Nursing, 2023; 49; 94-100
21. Li N, Xu G, Chen G, Zheng X, Sleep quality among Chinese elderly people: A population-based study: Arch Gerontol Geriatr, 2020; 87; 103968
22. SurvGo: Metodologia CAWI-technika badawcza Available from: . Updated: 2023www.survgo.com/blog/metodologia-cawi-technika-badawcza
23. Ebert JF, Huibers L, Christensen B, Paper- or web-based questionnaire invitations as a method for data collection: Cross-sectional comparative study of differences in response rate, completeness of data, and financial cost: J Med Internet Res, 2018; 20(1); e24
24. Uhlig CE, Seitz B, Eter N, Efficiencies of Internet-based digital and paper-based scientific surveys and the estimated costs and time for different-sized cohorts: PLoS One, 2014; 9(10); e108441
25. Arafa AE, Anzengruber F, Mostafa AM, Perspectives of online surveys in dermatology: J Eur Acad Dermatol Venereol, 2019; 33(3); 511-20
26. Mollayeva T, Thurairajah P, Burton K, The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis: Sleep Med Rev, 2016; 25; 52-73
27. Smith MT, Wegener ST, Measures of sleep: The Insomnia Severity Index, Medical Outcomes Study (MOS) Sleep Scale, Pittsburgh Sleep Diary (PSD), and Pittsburgh Sleep Quality Index (PSQI): Arthritis Care & Research, 2003; 49(5S); 184-96
28. World Medical Association, World Medical Association World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects: JAMA, 2013; 310(20); 2191-94
29. Department of Health, Education, and Welfare, National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research, The Belmont Report. Ethical principles and guidelines for the protection of human subjects of research: J Am Coll Dent, 2014; 81(3); 4-13
30. Roncoroni J, Wu Whitaker S, Wippold G, Sociodemographic and health correlates of sleep in U.S. Hispanic older adults: Sleep Med, 2020; 68; 213-17
31. Morita I, Morioka H, Abe YRelationship between the number of prescribed medications and oral dysfunction in elderly individuals: Nihon Koshu Eisei Zasshi, 2021; 68; 167-79 [in Japanese]
32. Xu J, Chen X, Ma K, Correlation between sleep, life, mood, and diet and severity of inflammatory bowel disease in China: A retrospective study: Med Sci Monit, 2021; 27; e930511
33. El-Gilany AH, Saleh N, Mohamed H, Prevalence of insomnia and its associated factors among rural elderly: A community based study: Int J Adv Nurs Stud, 2017; 6(1); 56-62
34. Wang P, Song L, Wang K, Prevalence and associated factors of poor sleep quality among Chinese older adults living in a rural area: A population-based study: Aging Clin Exp Res, 2020; 32(1); 125-31
35. Chu HS, Oh J, Lee K, The relationship between living arrangements and sleep quality in older adults: Gender differences: Int J Environ Res Public Health, 2022; 19(7); 3893
36. Lee YH, Chang YC, Chiang T, Living arrangements and sleep-related outcomes among older adults in China: A panel analytic approach: Int J Aging Hum Dev, 2020; 91(2); 111-26
37. Aleman A, Sommer I, The silent danger of social distancing: Psychol Med, 2020; 52(4); 789-90
38. Van Orden KA, Bower E, Lutz J, Strategies to promote social connections among older adults during “social distancing” restrictions: Am J Geriatr Psychiatry, 2021; 29(8); 816-27
39. Choi YJ, Lee KK, Lee SB, Association between sleep and loneliness in the elderly living alone: Korean J Psychosom Med, 2020; 28(2); 168-76
Tables
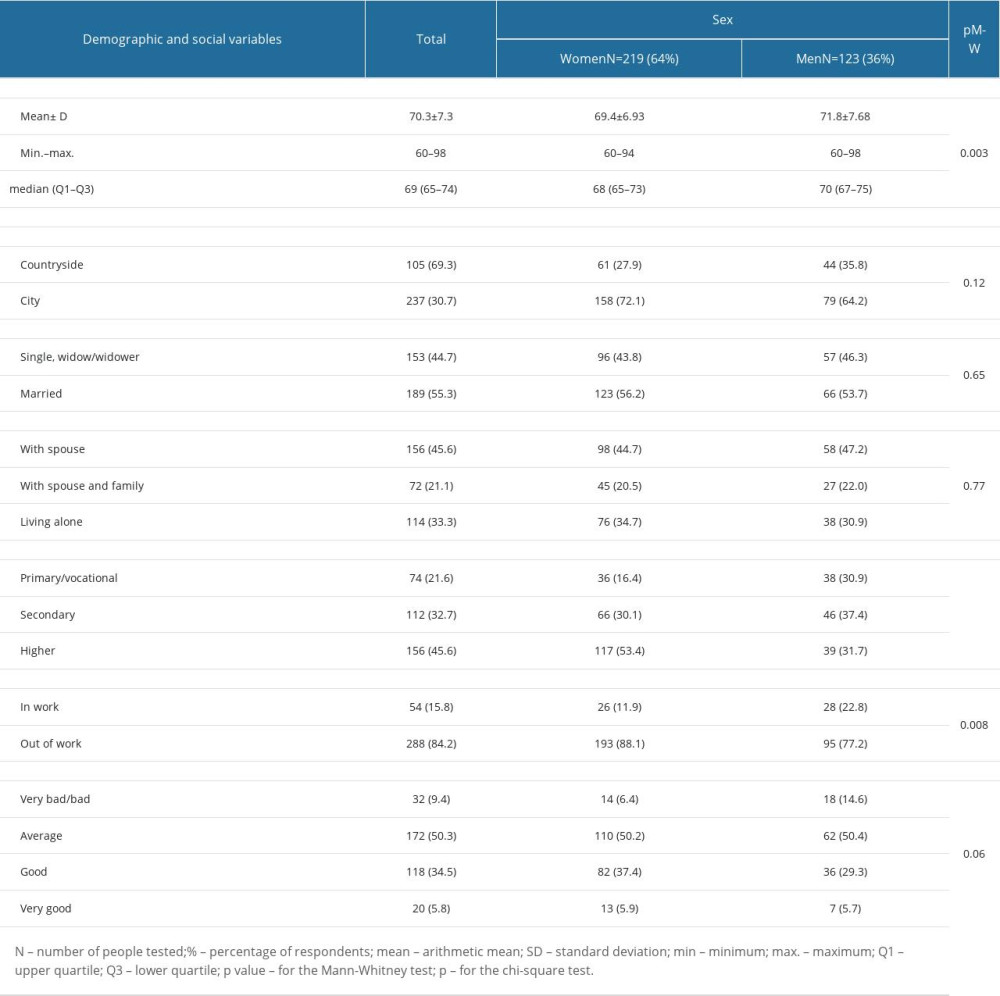 Table 1. Demographic and social characteristics of the study group.
Table 1. Demographic and social characteristics of the study group.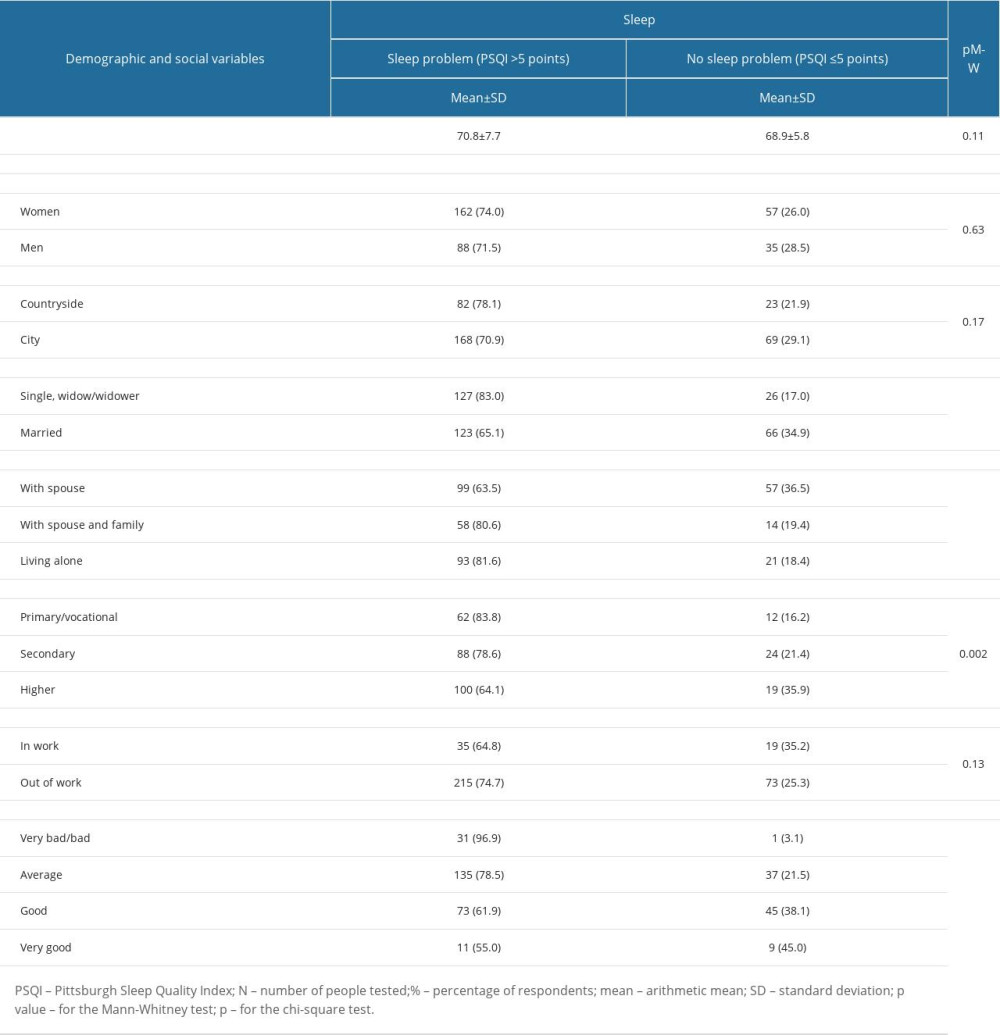 Table 2. Demographic and social variables determining sleep in the study group.
Table 2. Demographic and social variables determining sleep in the study group.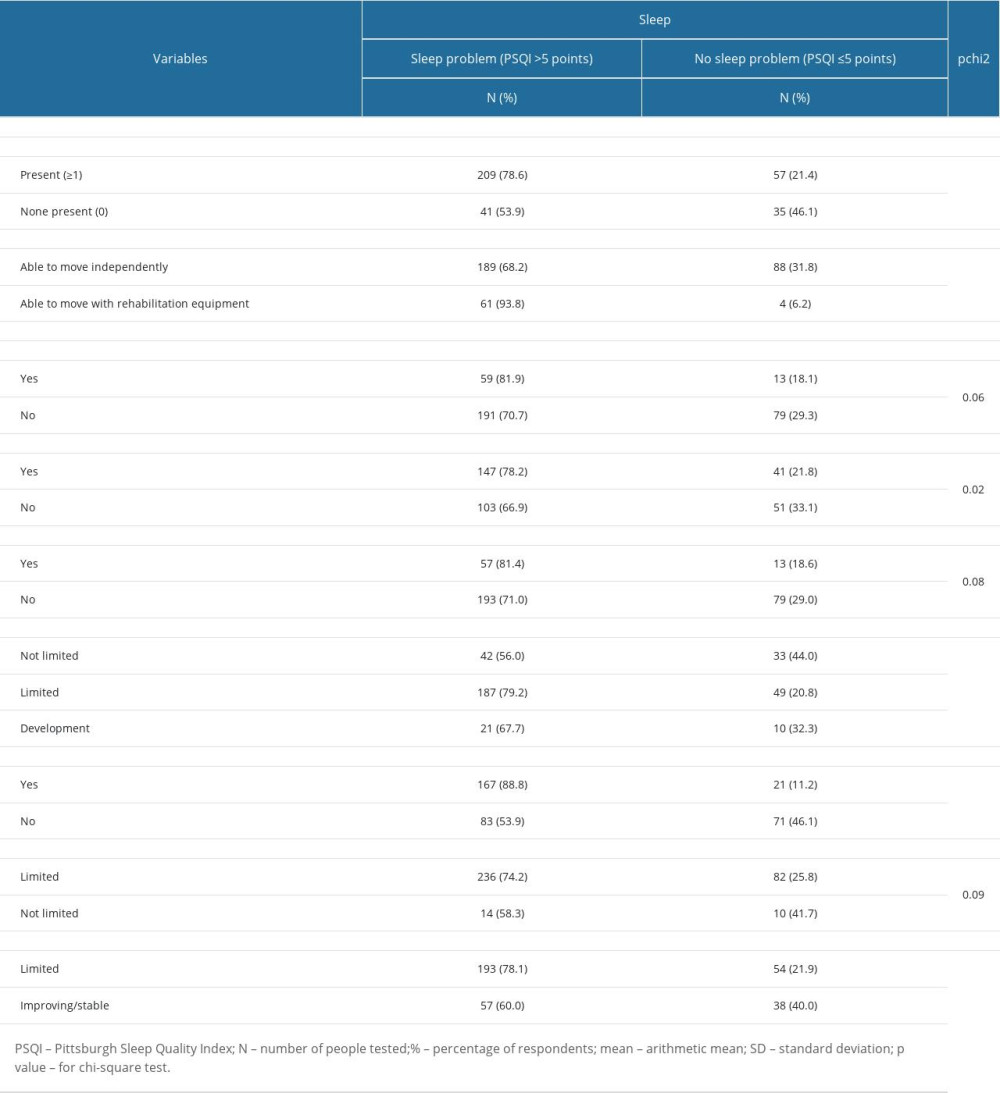 Table 3. Clinical status and factors related to the SARS-CoV-2 virus pandemic affecting sleep in the study group.
Table 3. Clinical status and factors related to the SARS-CoV-2 virus pandemic affecting sleep in the study group.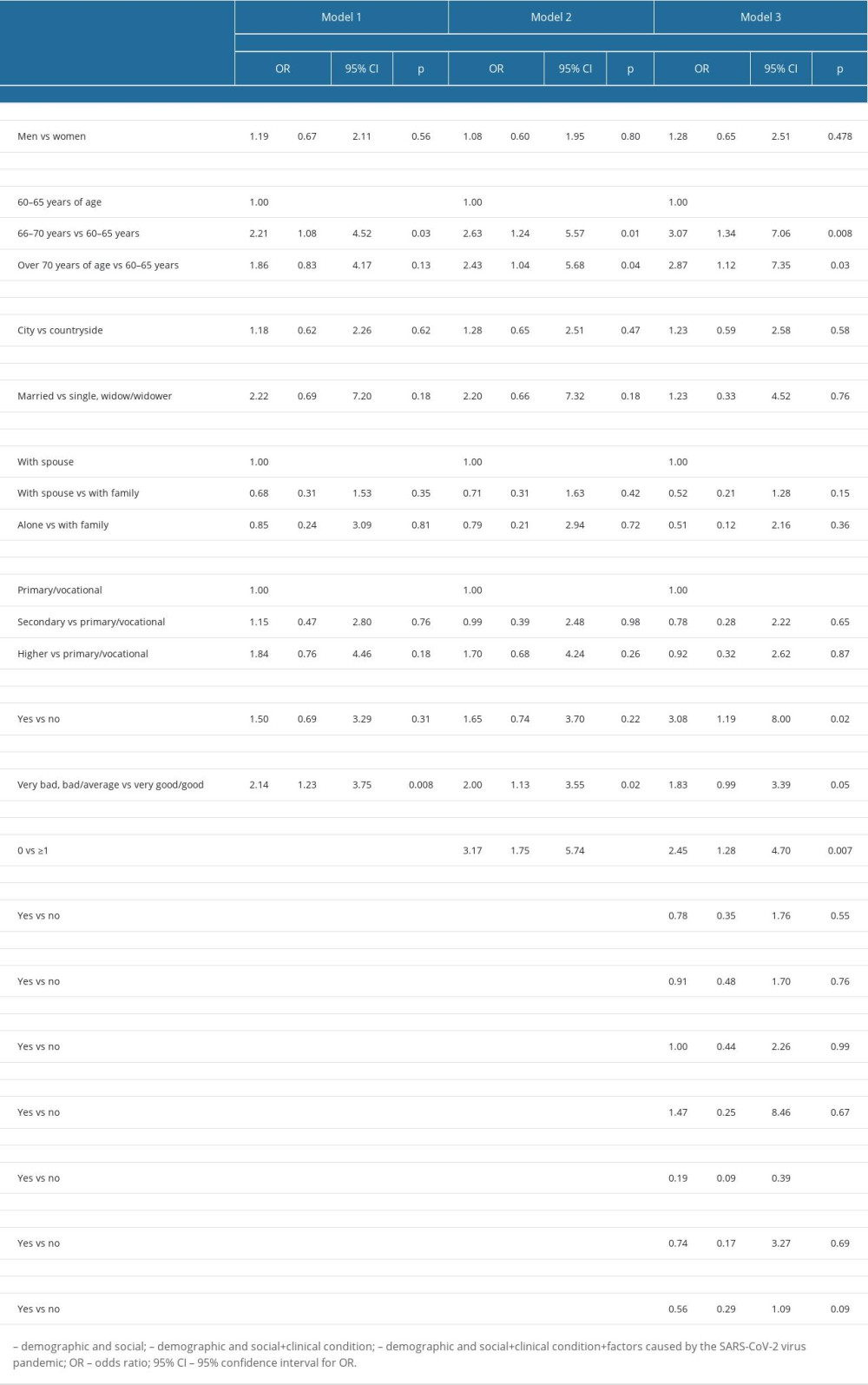 Table 4. Logistic regression analysis of the relationship between sleep quality and demographic and social variables, clinical status, and the factors caused by the SARS-CoV-2 virus pandemic.
Table 4. Logistic regression analysis of the relationship between sleep quality and demographic and social variables, clinical status, and the factors caused by the SARS-CoV-2 virus pandemic. In Press
11 Mar 2024 : Clinical Research
Enhancement of Frozen-Thawed Human Sperm Quality with Zinc as a Cryoprotective AdditiveMed Sci Monit In Press; DOI: 10.12659/MSM.942946
12 Mar 2024 : Database Analysis
Risk Factors of Age-Related Macular Degeneration in a Population-Based Study: Results from SHIP-TREND-1 (St...Med Sci Monit In Press; DOI: 10.12659/MSM.943140
12 Mar 2024 : Clinical Research
Preoperative Blood Transfusion Requirements for Hemorrhoidal Severe Anemia: A Retrospective Study of 128 Pa...Med Sci Monit In Press; DOI: 10.12659/MSM.943126
12 Mar 2024 : Clinical Research
Tissue Inhibitors of Metalloproteinase 1 (TIMP-1) and 3 (TIMP-3) as New Markers of Acute Kidney Injury Afte...Med Sci Monit In Press; DOI: 10.12659/MSM.943500
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








