21 October 2023: Clinical Research
Paravertebral Muscle Morphology in L4-L5 Disc Herniation: Insights from the Michigan State University Classification
Pei-yu Du1AB, Yong-wang Zhang2AB, Xu-hao Cao3B, Yue-lin Liu3C, Yun-tao Yan2CD, Lu Liu2EF, Shuang-qing Du2AFG*DOI: 10.12659/MSM.941937
Med Sci Monit 2023; 29:e941937
Abstract
BACKGROUND: Lumbar disc herniation (LDH) at L4-L5 impacts paravertebral muscle morphology. Intervertebral disc degeneration is linked to paravertebral muscle changes, affecting LDH treatment outcomes. This study explored L4-L5 LDH paravertebral muscle alterations, specifically in the erector spinae, multifidus, and psoas major, using Michigan State University’s classification to guide LDH treatment.
MATERIAL AND METHODS: The study enrolled 160 patients, including 39 normal patients and 121 L4-L5 LDH patients. Patients with LDH were grouped according to MSU classification and compared to the normal group according to demographics and imaging changes.
RESULTS: In patients with L4-L5 herniation in Zone B, the FI of the ES muscle at L3-L4 level, L4-L5 level, and L5-S1 level was higher than that of normal people (P=0.018, P=0.043, P=0.010, respectively), and there was no difference between FI of MF and normal people. The Zone B patients also had a smaller CSA of the ES muscle at L4-L5 level than that in the normal group (P=0.049). Patients in the Zone C group were older than those in the normal group (P=0.014). The CSA of the PM of patients with Grade 3 herniation differed from that of the normal group at the L4-L5 and L5-S1 level. They were higher than in normal people at L4-L5 level (P=0.011) and lower at L5-S1 level (P=0.028).
CONCLUSIONS: In patients with L4-L5 herniation in Zone B, the FI of ES at L3-S1 level was higher than in normal people, and the CSA at L4-L5 level was smaller than in normal people. In patients with Grade3 herniation, PM CSA was larger at L4-L5 level and smaller at L5-S1 level than in normal people.
Keywords: Lumbar Stenosis, Familial, Lumbar Vertebrae, Muscle Fibers, Skeletal, Humans, Intervertebral Disc Displacement, Michigan, Universities, Magnetic Resonance Imaging, intervertebral disc degeneration, Psoas Muscles
Background
Lumbar disc herniation (LDH) is a common clinical disease, occurring in people of all ages. It causes pain and results in a very large economic burden, so prevention of LDH is very important [1]. Many previous studies [2,3] have shown that intervertebral disc degeneration is associated with the paravertebral muscle. Studies [4] have also shown that exercise of the paravertebral muscle can reduce the symptoms of LDH, and the preoperative cross-sectional area (CSA) and fat infiltration (FI) of the paravertebral muscle can also affect postoperative efficacy; therefore, identifying the changes of the paravertebral muscle in LDH patients can help in treatment of LDH.
The paravertebral muscles are mainly divided into the psoas major muscle (PM), multifidus muscle (MF), and erector spinae muscles (ES) and play a very important role in lumbar spine stability [5]. When there is fat infiltration, the muscle contractions of the paravertebral muscles are impaired, resulting in loss of muscle function [6,7]; therefore, FI is a commonly used measure of muscle function. Paravertebral muscle degeneration is closely related to spinal diseases such as chronic low back pain and scoliosis. Previous studies [8,9] only explored the relationship between the rate of fat infiltration of paravertebral muscle and lumbar disc herniation, but the relationship between different degrees and different positions of herniation and paravertebral muscle has not been studied. Therefore, the purpose of this study was to explore the morphological differences of among ES, MF, and PM in patients with only L4–L5 LDH under different Michigan State University (MSU) classifications, so as to better reveal the relationship between LDH and paravertebral muscles to further reveal the causes and guide the treatment of LDH.
Material and Methods
STUDY COHORT:
This retrospective, cross-sectional, radiographic study was approved by the local ethics review committee and performed in accordance to the guidelines specified in the Declaration of Helsinki. The inclusion criteria of LDH patients were: diagnosed as LDH only at L4–L5 level or diagnosed as normal, and had complete radiographic data. The exclusion criteria were: neuromuscular diseases, hip joint or knee joint disease, history of spinal surgery, neuromuscular diseases, tumor, infection, fracture, or spinal deformity. The people in the normal group had no lumbar disc herniation according to MRI diagnosis of the lumbar spine by 2 senior spinal surgeons, and also had no degeneration or Modic changes of intervertebral discs at the L4–L5 level. This retrospective study on coded data was exempt by the ethics review committee from seeking informed consent from patients without general consent or dissent.
DATA COLLECTION AND RADIOGRAPHIC MEASUREMENT:
Demographic information, including age and sex, was extracted from patient records. We used a 3.0-T imaging system, and clinical T2-weighted magnetic resonance imaging (MRI) scans were collected. The patients were graded by MSU classification on the coronal image (Figure 1) and images were uploaded to Image J software (Version 1.43u, Wayne Rasband, NIH, USA) for measuring the CSA and FI of the bilateral paraspinal muscle. The cross-sectional areas of the bilateral PM, MF, and ES muscles were measured and the mean value was calculated (Figure 2). The mean value of the cross-sectional area of the same muscle on both sides was defined as the CSA of the muscle. Images for L1–2, L2–3, L3–L4, L4–L5, L4–L5, and L5–S1 intervertebral disc levels of the patients were collected and measured. The FI of the PM was not measured because PM often has little fat infiltration [10].
STATISTICAL ANALYSIS:
SPSS version 22.0 (IBM company) was used to analyze the collected data. Multiple logistic regression analysis was used to compare the differences of paravertebral muscle CSA and FI between the LDH patients and the normal group under different zones and grades. Due to the data volume, 3 groups of muscle CSA and FI at 5 levels were included into the 2 models together with age and sex.
Results
We collected data on160 patients, including 39 normal patients and 121 patients with single-level L4–L5 LDH. According to the MSU classification, the patients were divided into Zone 1, 2, and 3 groups according to the different zones, and Grade 1, 2, and 3 groups according to the degree of herniation (Table 1).
The FI of MF and ES of normal people and patients with L45 LDH, as well as age and sex, were included in the model to explore their differences in different regions with different salience degrees. The mean comparison of FI between patients in different zones and the normal group is shown in Figure 3, and the differences are shown in Table 2. It can be seen that the paravertebral muscle indexes, sex, and age of Zone A patients were not significantly different from the normal group. In patients with L4–L5 herniation in Zone B, the FI of the ES muscle at L3–L4 level, L4–L5 level, and L5–S1 level was higher than that of normal people (
The mean comparison of FI between patients with different degrees of herniation and the normal group is shown in Figure 4, and the differences are shown in Table 3. It can be seen that there is no significant difference in the FI in the MF and ES at different levels compared with normal people, regardless of the degree of herniation of the patients.
The CSA, age, and sex of MF, ES, and PM of normal people and patients with L4–L5 herniation were included in the model to explore their differences in different regions and different degrees of outburst. Figure 5 shows the comparison of the values of different levels and different muscles of patients under different zones, and Table 4 shows the differences compared with the normal group, showing that the CSA of the ES muscle at L45 level in patients with L45 herniation in Zone B was significantly different from that in the normal group (
The comparison of mean muscle CSA between patients with different degrees of herniation and the normal group is shown in Figure 6, and the differences are shown in Table 5. It can be seen that the paravertebral muscle CSA of patients with Grade 1 and Grade 2 herniation has no significant difference compared with the normal group, while the CSA of the PM of patients with Grade 3 herniation differed from that of the normal group at the L4–L5 and L5–S1 levels, and they were higher than in normal people at L4–L5 level (
Discussion
LDH is a common disease of the lumbar spine and is the most common cause of radiculopathy. Surgical treatment is required when symptoms are severe and conservative treatment is not effective [11]. To more accurately describe the degree and location of prominence, Mysliwiec et al [12] proposed the MSU classification, using 1–2–3 and A–B–C to describe the size and location of herniation. Many previous studies have demonstrated an association between lumbar disc herniation and the paravertebral muscle, but no studies have linked MSU grade to the paravertebral muscle. In our study, in terms of age and sex, patients in Zone 3 were significantly older than those in the normal group, and with herniation in Zone C representing extreme lateral herniation, first reported by Abdullah et al [13] in 1974, it tends to occur in elderly patients, which is consistent with our conclusion.
Patients in Zone B often require surgery because their symptoms are more pronounced [12]. However, our study found that the FI of the ES muscle in patients with Zone B herniation was larger at L3–L4, L4–L5, L5–S1 levels than that in the normal group, and the CSA of the ES muscle at L4–L5 was smaller than that in normal people. Although the causal relationship between paravertebral degeneration and LDH has not been established, it is generally believed that compression of nerve roots causes paravertebral degeneration. In LDH patients with Zone B herniation, the herniation may stimulate nerve roots more obviously, and the biological effect of skeletal muscle denervation may lead to muscle fiber atrophy and adipose tissue replacement, leading to paravertebral muscle degeneration, which is mainly manifested by increased FI and decreased CSA [14,15].
The L4–L5 herniation is located in Zone B, where the corresponding nerve root is compressed, and the nerve root innervates the paravertebral muscle at the same level anatomically, resulting in paravertebral muscle degeneration at the same level. Dong Sun et al [16] also came to a similar conclusion. However, we found that compression of the nerve roots only resulted in degeneration of the ES, not of the MF and PM. In addition to the corresponding L4–L5 levels, the FI of ES at L3–L4 and L5–S1 levels also increased. Of course, another cause of muscle degeneration is disuse, and patients with Zone B have obvious symptoms, resulting in reduced activity [17] and degeneration of the ES. The function of the MF muscle is more to maintain the stability of the lumbar segment [18], so the degeneration may not be significant.
Mazda et al [19] studied MRI in 19 patients with symptomatic single-level and unilateral lumbar root disease and found that MF degeneration was independent of the severity of root compression and duration of compression. Cooley [20] performed a meta-analysis of paravertebral muscles and found no relationship between FI of MF and nerve root compression, which was similar to our conclusion that nerve root compression was only associated with ES degeneration, not with the MF muscle. The ES are formed in the loin by the longissimus muscle on the medial side and the iliocostal muscle on the lateral side, and span 1 or more vertebrae longitudinally [21]. According to our conclusion, the FI of ES at the L3–L4 and L5–S1 levels may be related to the longitudinal span of multiple vertebral bodies of ES innervated by compressed nerve roots. In addition, muscle degeneration should be mainly in the form of fat change rather than muscle atrophy, otherwise it is insufficient to explain the fact that the CSA of ES muscle at the level of L3–L4 and L5–S1 did not decrease significantly, but FI increased significantly, which needs to be assessed in future basic research.
As one of the paravertebral muscles, the PM is less studied than the ES and MF muscles. Juraj et al [10] found in their study on PM in intervertebral disc degeneration that patients with intervertebral disc degeneration and Modic changes had a smaller PM than normal people, and it was inferred that the reduction of activity caused by pain led to a decrease in PM CSA. In this regard, the research of Parkkola et al [22] and Cui et al [23] also reached the same conclusion. However, previous studies have not linked the degree of lumbar disc herniation with CSA of PM. Our study found that patients with Grade 1 and Grade 2 herniation did not differ significantly from the normal group, while in patients with Grade 3 herniation, the L4–L5 level had a large CSA and the L5–S1 level had a small CSA. This is a very strange finding. Why did the same muscle yield opposite results at different levels? Apparently, innervation does not explain this anymore. After consideration, we believe that Grade 3 herniation is generally caused by intense exercise and violent injury, rather than due to degenerative factors. The CSA of the PM at the L4–L5 and L5–S1 levels is correlated with curvature of the spine, because the lordosis apex is generally at the L4 vertebrae level, so when lumbar lordosis (LL) increases, the angle of the disc at the L4–L5 level and horizontal line will be larger and the CSA of the PM at the section will therefore be larger. Similarly, when the sacral slope (SS) is small, the angle between the L5–S1 level disc and the horizontal plane decreases, resulting in a decrease in the CSA of the PM in this section. Our conclusions suggest that patients with large LL and small SS are prone to sports and violent injuries, leading to severe (Grade3) LDH. This also suggests the shortcomings of previous studies, which did not consider spinal parameters in relation to disc degeneration, herniation, and the paravertebral muscle.
This study has some limitations. First, this was a retrospective study with insufficient sample size, and further prospective studies are needed. Second, spinal sequence parameters were not included, which may have led to inaccurate results. Third, in MSU grading, the zone and grade of herniation should be considered at the same time, but due to the small sample size, our study could only discuss these 2 aspects separately.
Conclusions
Patients in the Zone C group were significantly older than in the normal group. In patients with L4–L5 herniation in Zone B, the FI of ES at the L3–S1 level was higher than normal, and the CSA at L4–L5 level was smaller than normal. In patients with Grade3 herniation, PM CSA was larger at the L4–L5 level and smaller at the L5–S1 level than in normal people.
Figures
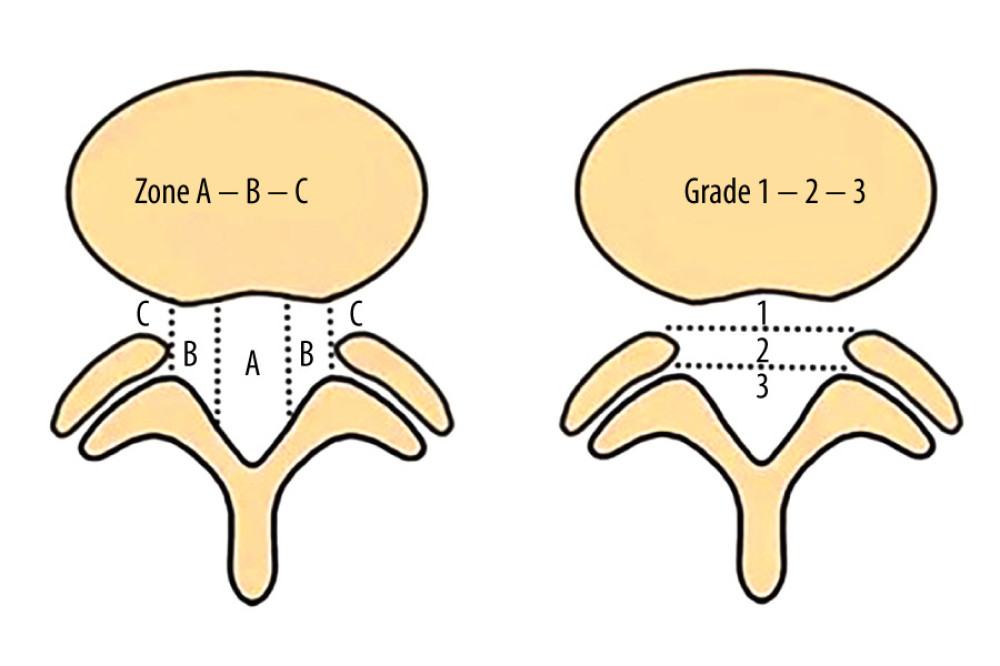 Figure 1. MSU classification results from combination of size and location of LDH: grading LDH for size with growing impact on nerve compression from grades 1 to 3 and medial to lateral LDH location from zone A to zone C. MSU – Michigan State University; LDH – lumbar disc herniation.
Figure 1. MSU classification results from combination of size and location of LDH: grading LDH for size with growing impact on nerve compression from grades 1 to 3 and medial to lateral LDH location from zone A to zone C. MSU – Michigan State University; LDH – lumbar disc herniation. 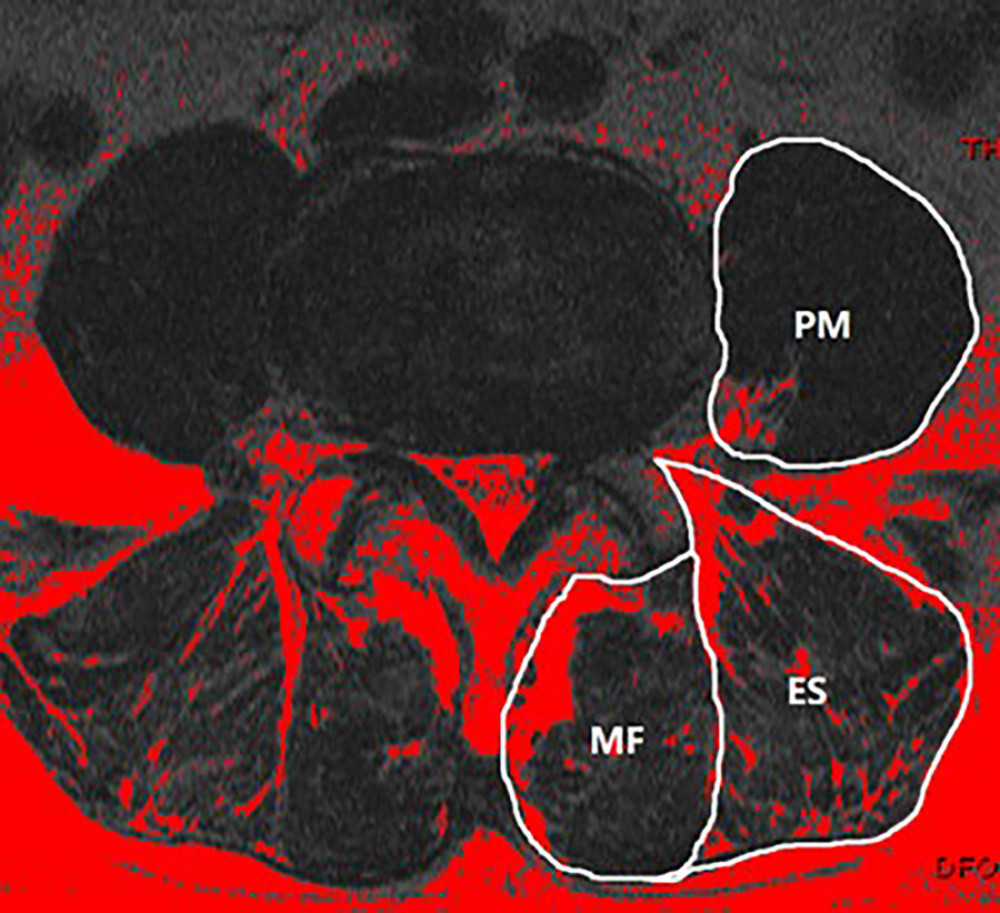 Figure 2. At the L4–L5 level, paraspinal muscle related parameters were measured using Image J software (version 1.43u).
Figure 2. At the L4–L5 level, paraspinal muscle related parameters were measured using Image J software (version 1.43u). 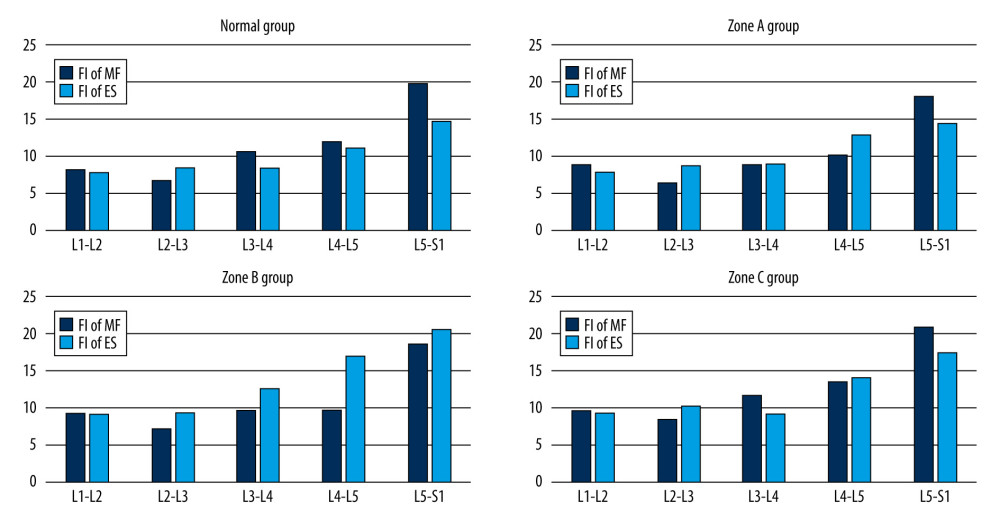 Figure 3. Mean value of fat infiltration in different zone of L4–L5 herniation patients and normal people.
Figure 3. Mean value of fat infiltration in different zone of L4–L5 herniation patients and normal people. 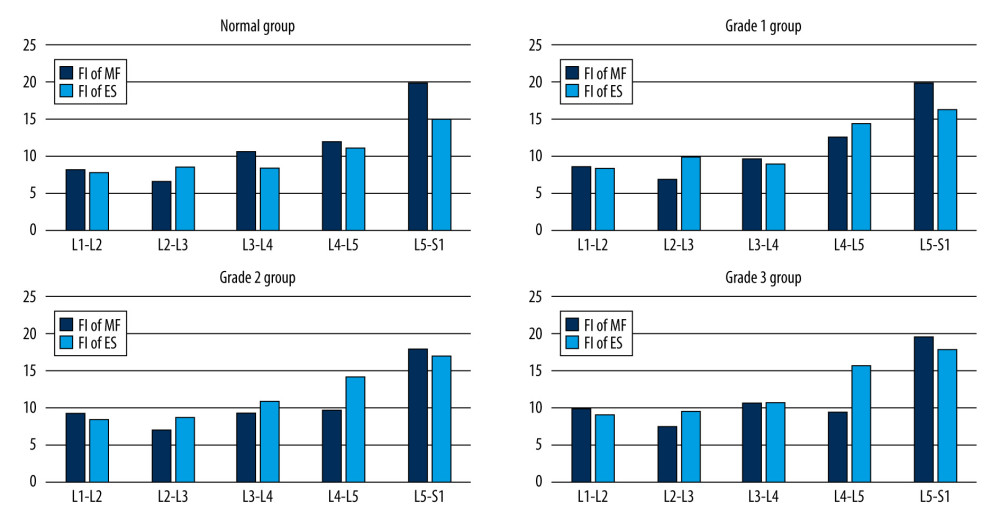 Figure 4. Mean value of fat infiltration in different grade of L4–L5 herniation patients and normal people.
Figure 4. Mean value of fat infiltration in different grade of L4–L5 herniation patients and normal people. 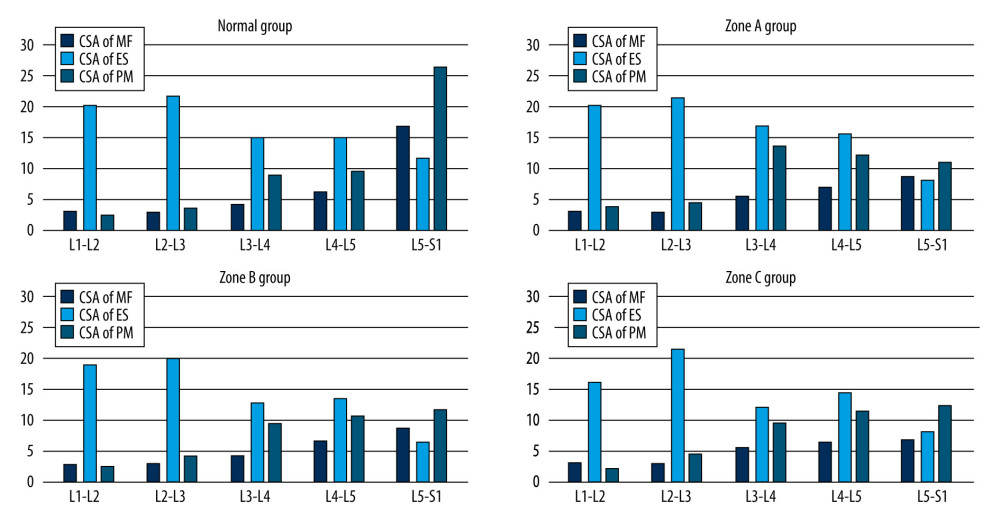 Figure 5. Mean value of cross-sectional area in different zone of L4–L5 herniation patients and normal people.
Figure 5. Mean value of cross-sectional area in different zone of L4–L5 herniation patients and normal people. 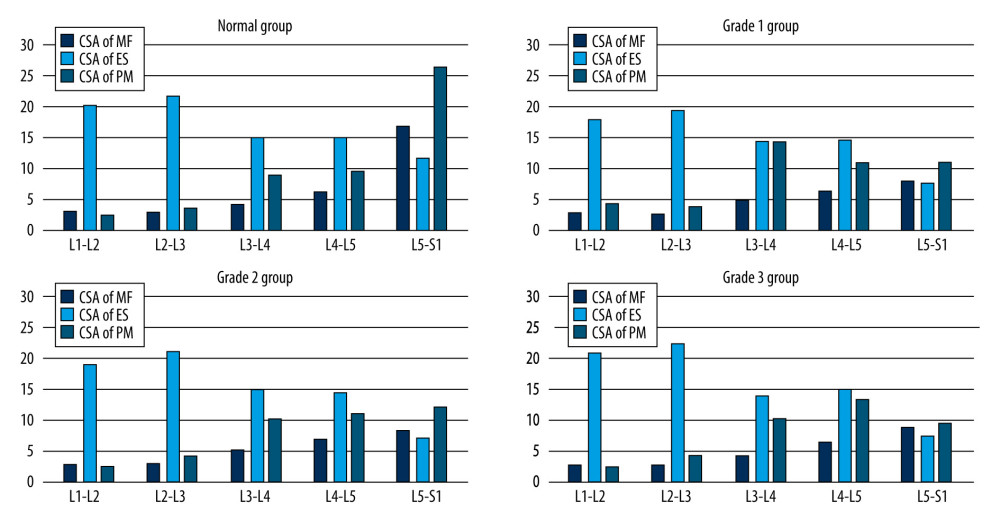 Figure 6. Mean value of cross-sectional area in different grade of L4–L5 herniation patients and normal people.
Figure 6. Mean value of cross-sectional area in different grade of L4–L5 herniation patients and normal people. Tables
Table 1. Michigan State University classification of 121 L4–L5 lumbar disc herniation patients.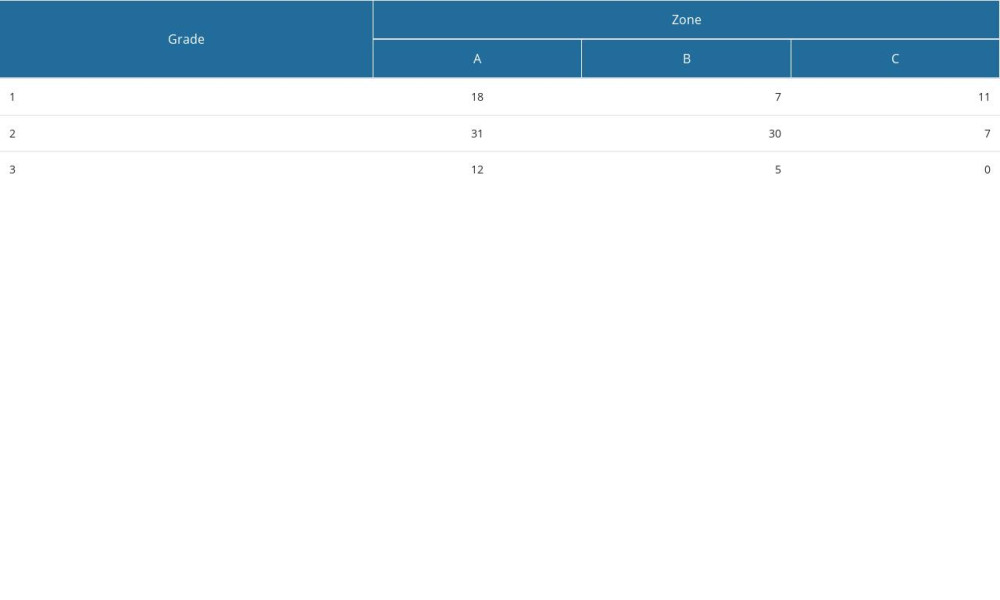 Table 2. Fat infiltration of patients with L4–L5 herniation in different zone compared with normal people.
Table 2. Fat infiltration of patients with L4–L5 herniation in different zone compared with normal people.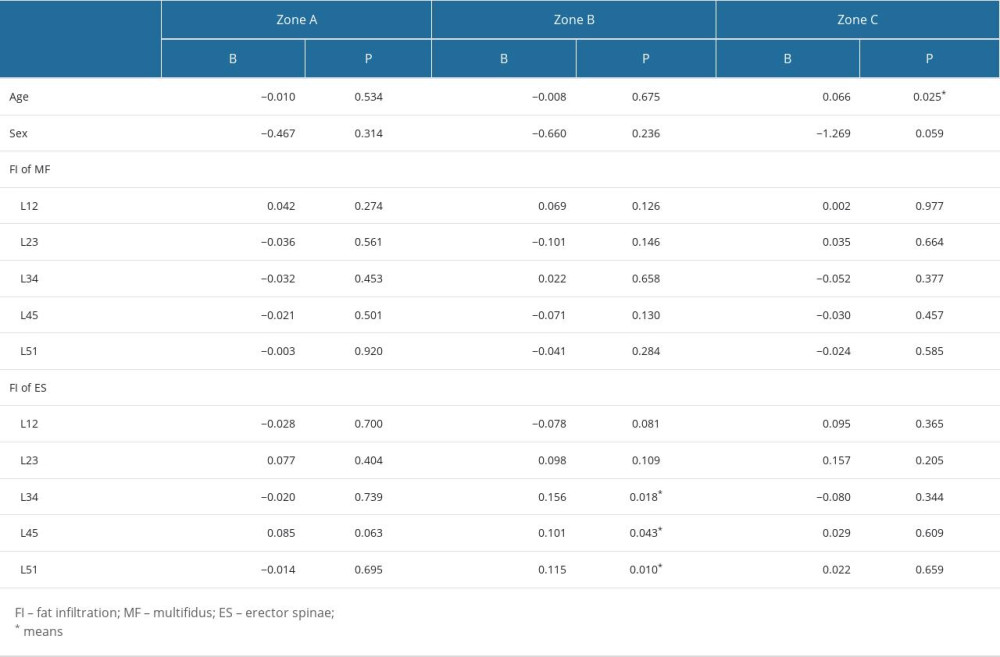 Table 3. Fat infiltration of patients with L4–L5 herniation in different grade compared with normal people.
Table 3. Fat infiltration of patients with L4–L5 herniation in different grade compared with normal people.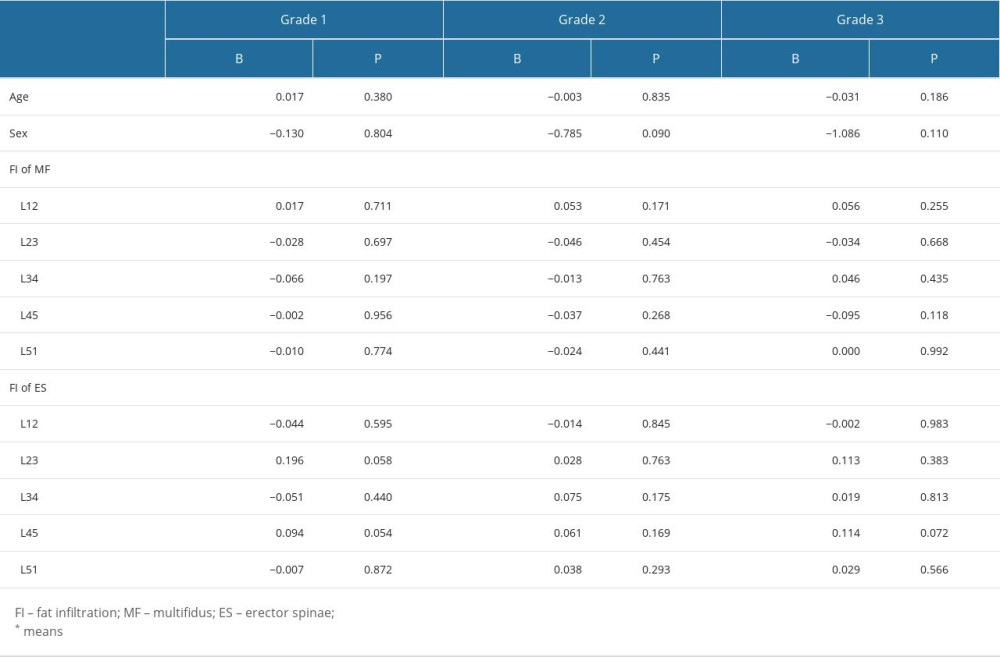 Table 4. Cross-sectional area of patients with L4–L5 herniation in different zone compared with normal people.
Table 4. Cross-sectional area of patients with L4–L5 herniation in different zone compared with normal people.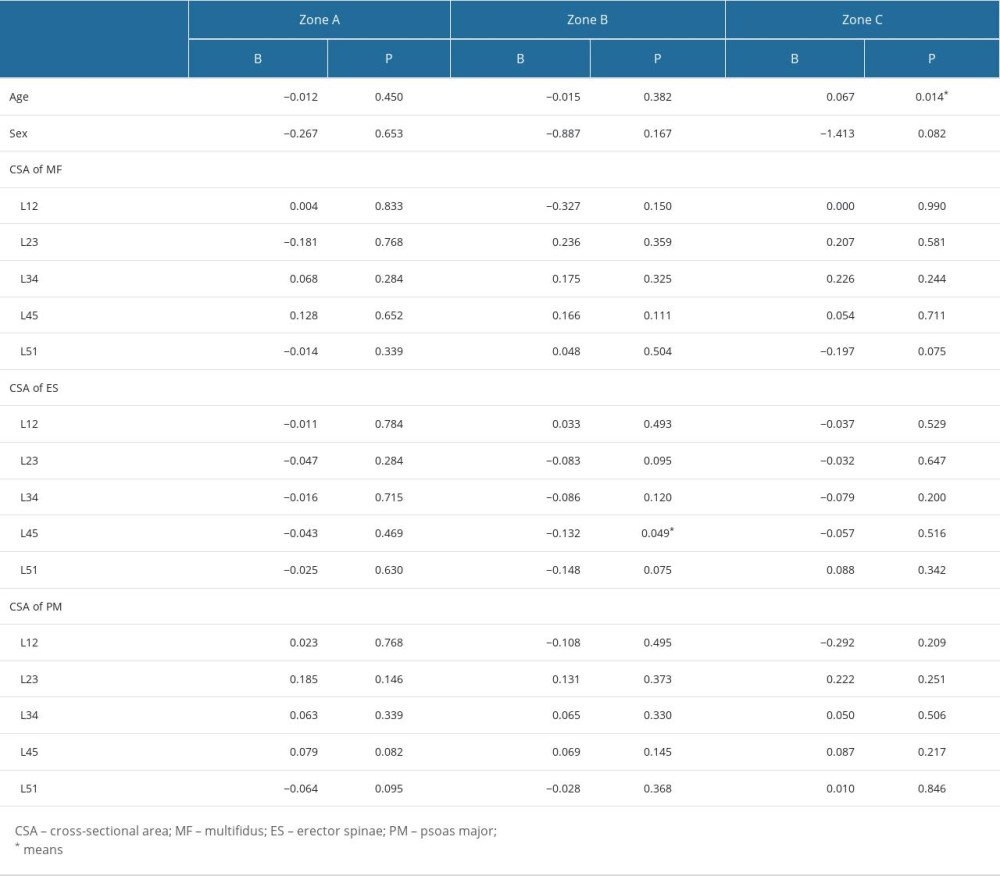 Table 5. Cross-sectional area of patients with L4–L5 herniation in different grades compared with normal people.
Table 5. Cross-sectional area of patients with L4–L5 herniation in different grades compared with normal people.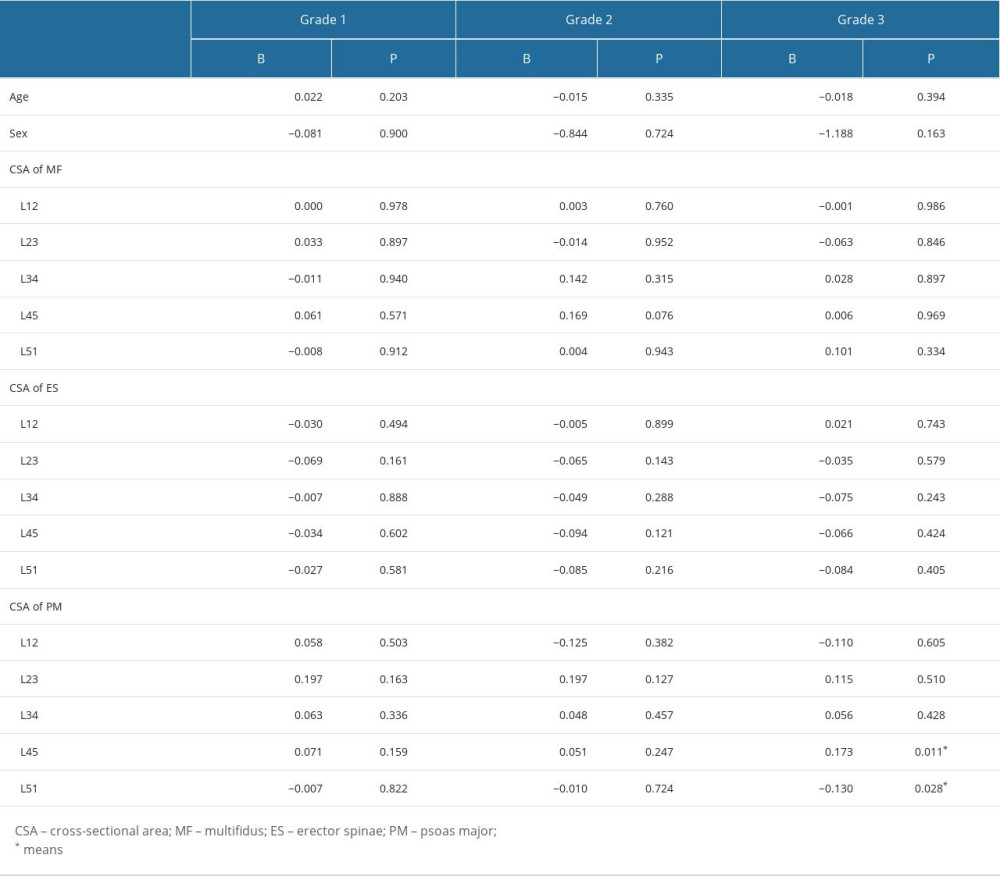
References
1. Long DM, BenDebba M, Torgerson WS, Persistent back pain and sciatica in the United States: Patient characteristics: J Spinal Disord, 1996; 9(1); 40-58
2. Faur C, Patrascu JM, Haragus H, Anglitoiu B, Correlation between multifidus fatty atrophy and lumbar disc degeneration in low back pain: BMC Musculoskelet Disord, 2019; 20(1); 414
3. Fortin M, Lazáry À, Varga PP, Paraspinal muscle asymmetry and fat infiltration in patients with symptomatic disc herniation: Eur Spine J, 2016; 25(5); 1452-59
4. Stanuszek A, Jędrzejek A, Gancarczyk-Urlik E, Preoperative paraspinal and psoas major muscle atrophy and paraspinal muscle fatty degeneration as factors influencing the results of surgical treatment of lumbar disc disease: Arch Orthop Trauma Surg, 2022; 142(7); 1375-84
5. Hides JA, Belavý DL, Stanton W, Magnetic resonance imaging assessment of trunk muscles during prolonged bed rest: Spine (Phila Pa 1976), 2007; 32(15); 1687-92
6. Hamrick MW, McGee-Lawrence ME, Frechette DM, Fatty infiltration of skeletal muscle: Mechanisms and comparisons with bone marrow adiposity: Front Endocrinol (Lausanne), 2016; 7; 69
7. Le Cara EC, Marcus RL, Dempsey AR, Morphology versus function: The relationship between lumbar multifidus intramuscular adipose tissue and muscle function among patients with low back pain: Arch Phys Med Rehabil, 2014; 95(10); 1846-52
8. Zhao X, Liang H, Hua Z, The morphological characteristics of paraspinal muscles in young patients with unilateral neurological symptoms of lumbar disc herniation: BMC Musculoskelet Disord, 2022; 23(1); 994
9. Kulig K, Scheid AR, Beauregard R, Multifidus morphology in persons scheduled for single-level lumbar microdiscectomy: Qualitative and quantitative assessment with anatomical correlates: Am J Phys Med Rehabil, 2009; 88(5); 355-61
10. Arbanas J, Pavlovic I, Marijancic V, MRI features of the psoas major muscle in patients with low back pain: Eur Spine J, 2013; 22(9); 1965-71
11. Hahne AJ, Ford JJ, McMeeken JM, Conservative management of lumbar disc herniation with associated radiculopathy: A systematic review: Spine (Phila Pa 1976), 2010; 35(11); E488-504
12. Mysliwiec LW, Cholewicki J, Winkelpleck MD, Eis GP, MSU classification for herniated lumbar discs on MRI: Toward developing objective criteria for surgical selection: Eur Spine J, 2010; 19(7); 1087-93
13. Abdullah AF, Ditto EW, Byrd EB, Williams R, Extreme-lateral lumbar disc herniations. Clinical syndrome and special problems of diagnosis: J Neurosurg, 1974; 41(2); 229-34
14. Yarjanian JA, Fetzer A, Yamakawa KS, Correlation of paraspinal atrophy and denervation in back pain and spinal stenosis relative to asymptomatic controls: PM R, 2013; 5(1); 39-44
15. Yoshihara K, Shirai Y, Nakayama Y, Uesaka S, Histochemical changes in the multifidus muscle in patients with lumbar intervertebral disc herniation: Spine (Phila Pa 1976), 2001; 26(6); 622-26
16. Sun D, Liu P, Cheng J, Correlation between intervertebral disc degeneration, paraspinal muscle atrophy, and lumbar facet joints degeneration in patients with lumbar disc herniation: BMC Musculoskelet Disord, 2017; 18(1); 167
17. Crombez G, Vervaet L, Lysens R, Avoidance and confrontation of painful, back-straining movements in chronic back pain patients: Behav Modif, 1998; 22(1); 62-77
18. Ding JZ, Kong C, Li XY, Different degeneration patterns of paraspinal muscles in degenerative lumbar diseases: A MRI analysis of 154 patients: Eur Spine J, 2022; 31(3); 764-73
19. Farshad M, Gerber C, Farshad-Amacker NA, Asymmetry of the multifidus muscle in lumbar radicular nerve compression: Skeletal Radiol, 2014; 43(1); 49-53
20. Cooley JR, Walker BF, Ardakani EM, Relationships between paraspinal muscle morphology and neurocompressive conditions of the lumbar spine: A systematic review with meta-analysis: BMC Musculoskelet Disord, 2018; 19(1); 351
21. Macintosh JE, Bogduk N, 1987 Volvo award in basic science. The morphology of the lumbar erector spinae: Spine (Phila Pa 1976), 1987; 12(7); 658-68
22. Parkkola R, Rytökoski U, Kormano M, Magnetic resonance imaging of the discs and trunk muscles in patients with chronic low back pain and healthy control subjects: Spine (Phila Pa 1976), 1993; 18(7); 830-36
23. Cui M, Zhang Q, Chen X, Wu H, Analysis of CT imaging changes of psoas major muscles in patients with lumbar disc herniation mainly based on low back pain and lower limb pain: Front Surg, 2022; 9; 1022903
Figures
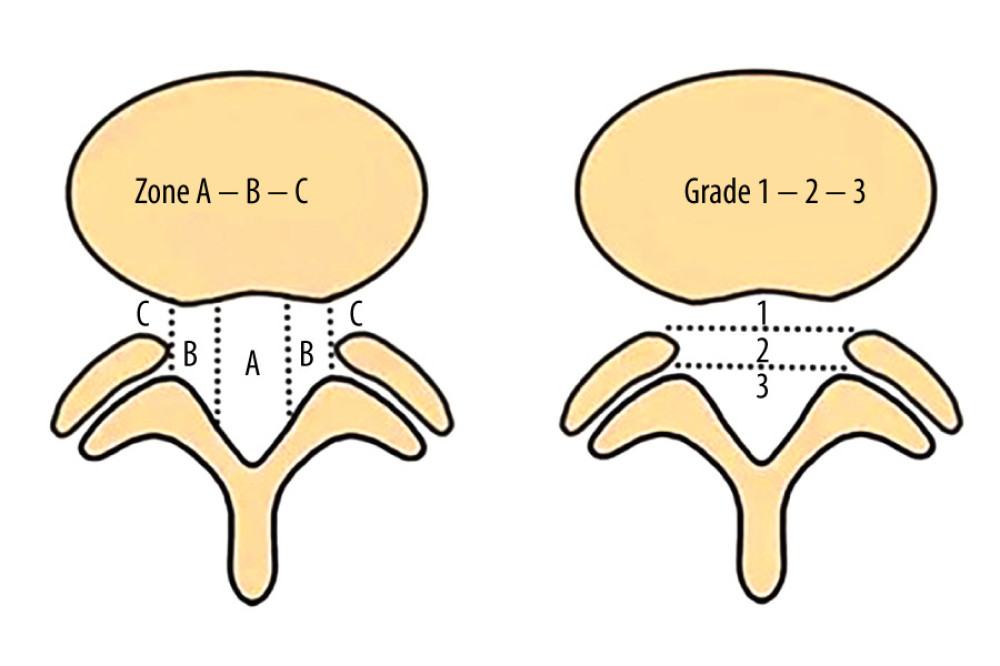 Figure 1. MSU classification results from combination of size and location of LDH: grading LDH for size with growing impact on nerve compression from grades 1 to 3 and medial to lateral LDH location from zone A to zone C. MSU – Michigan State University; LDH – lumbar disc herniation.
Figure 1. MSU classification results from combination of size and location of LDH: grading LDH for size with growing impact on nerve compression from grades 1 to 3 and medial to lateral LDH location from zone A to zone C. MSU – Michigan State University; LDH – lumbar disc herniation.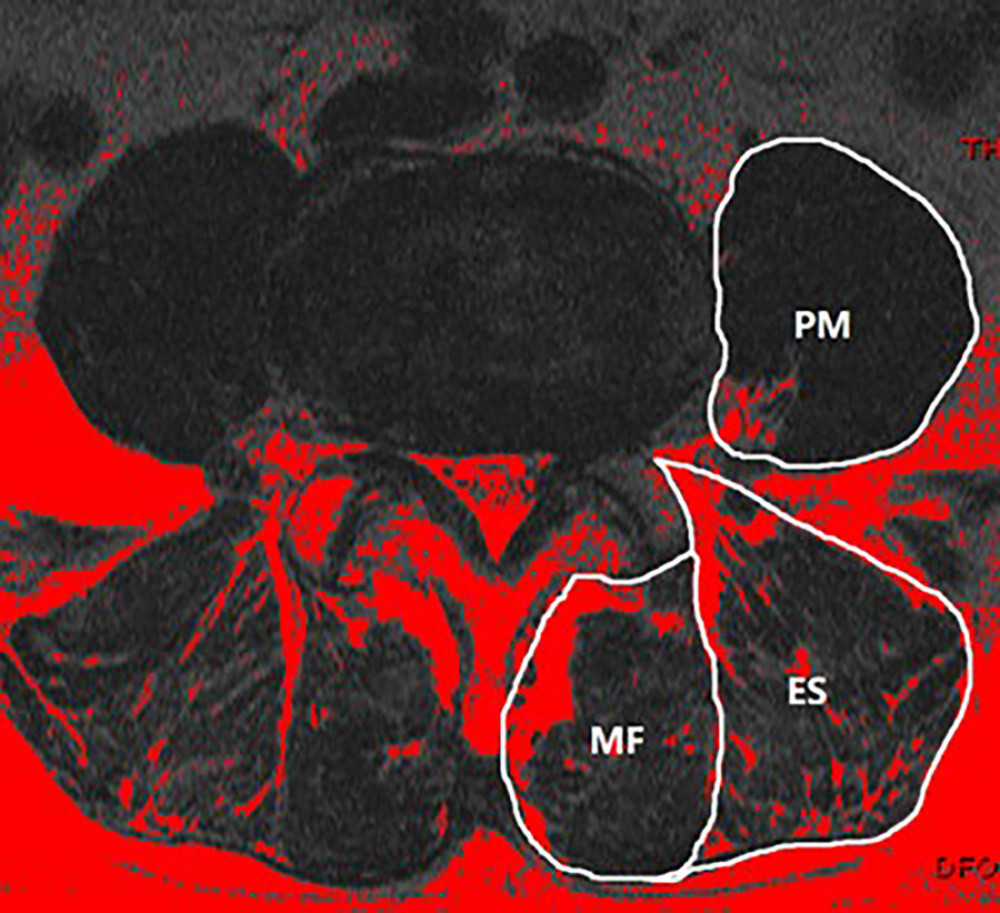 Figure 2. At the L4–L5 level, paraspinal muscle related parameters were measured using Image J software (version 1.43u).
Figure 2. At the L4–L5 level, paraspinal muscle related parameters were measured using Image J software (version 1.43u).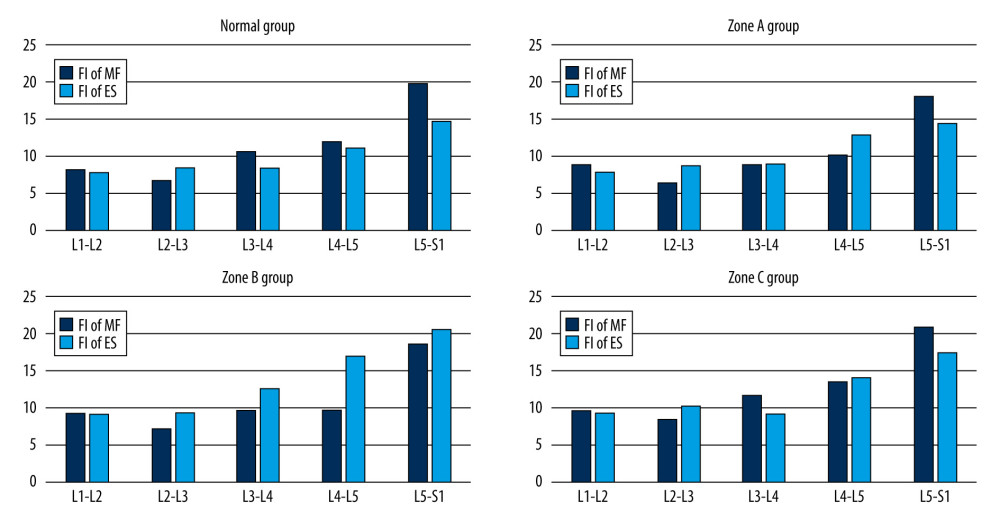 Figure 3. Mean value of fat infiltration in different zone of L4–L5 herniation patients and normal people.
Figure 3. Mean value of fat infiltration in different zone of L4–L5 herniation patients and normal people.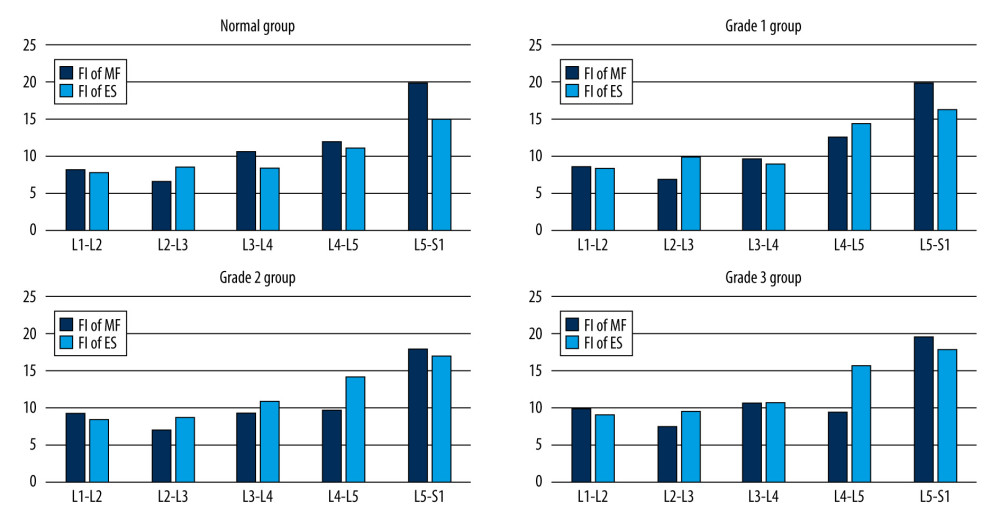 Figure 4. Mean value of fat infiltration in different grade of L4–L5 herniation patients and normal people.
Figure 4. Mean value of fat infiltration in different grade of L4–L5 herniation patients and normal people.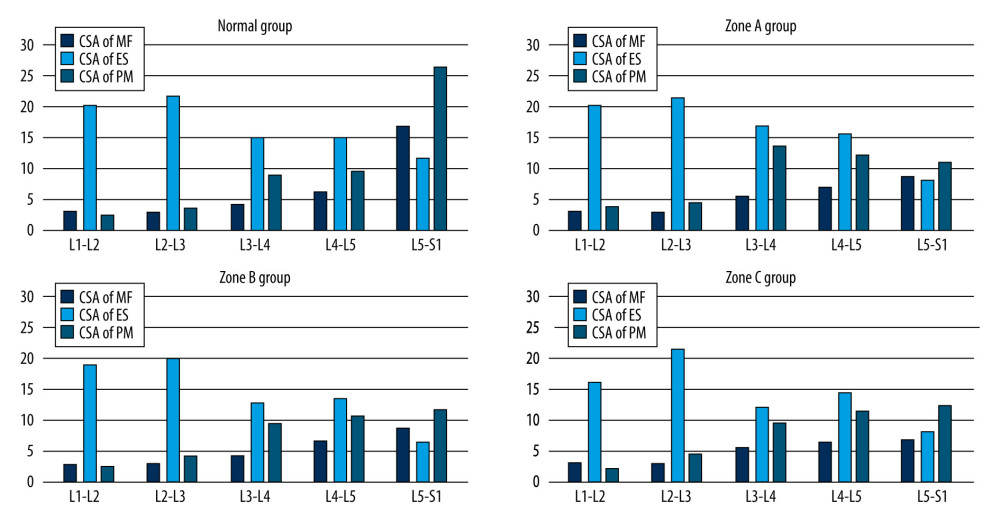 Figure 5. Mean value of cross-sectional area in different zone of L4–L5 herniation patients and normal people.
Figure 5. Mean value of cross-sectional area in different zone of L4–L5 herniation patients and normal people.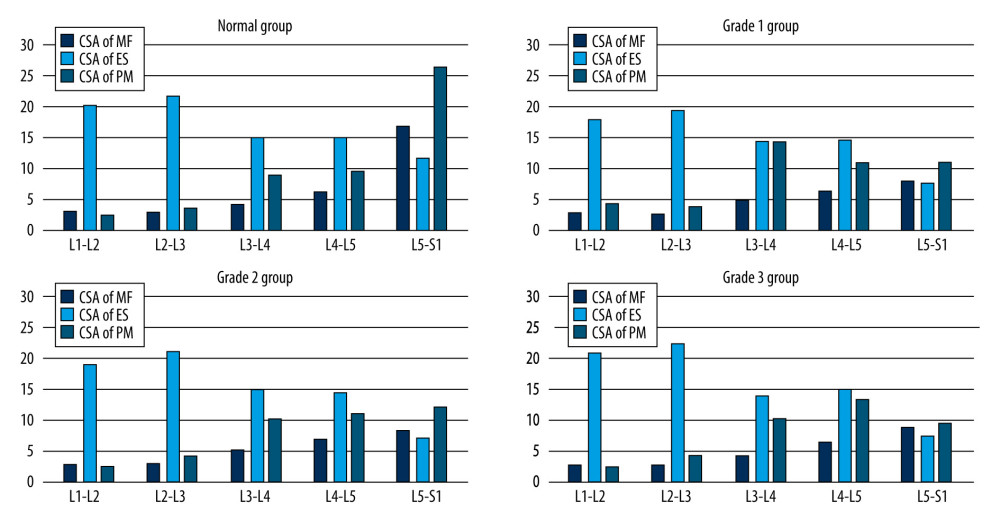 Figure 6. Mean value of cross-sectional area in different grade of L4–L5 herniation patients and normal people.
Figure 6. Mean value of cross-sectional area in different grade of L4–L5 herniation patients and normal people. Tables
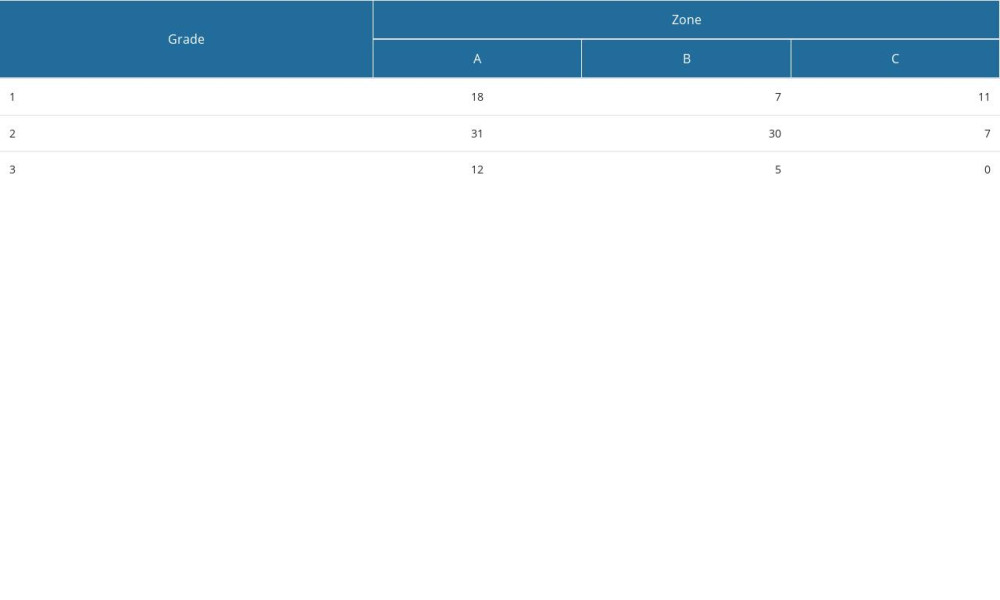 Table 1. Michigan State University classification of 121 L4–L5 lumbar disc herniation patients.
Table 1. Michigan State University classification of 121 L4–L5 lumbar disc herniation patients.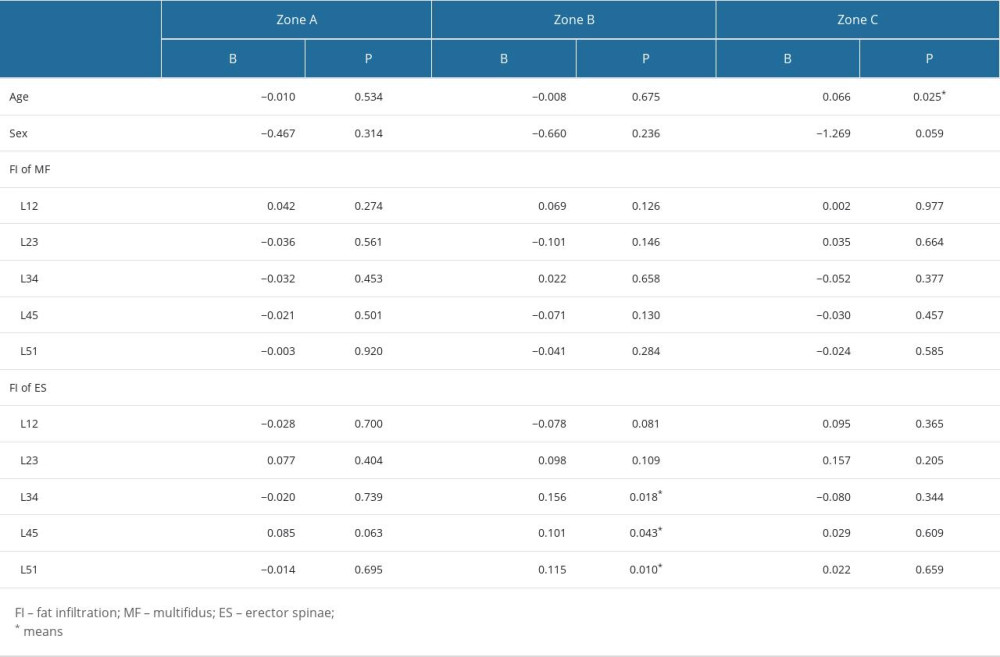 Table 2. Fat infiltration of patients with L4–L5 herniation in different zone compared with normal people.
Table 2. Fat infiltration of patients with L4–L5 herniation in different zone compared with normal people.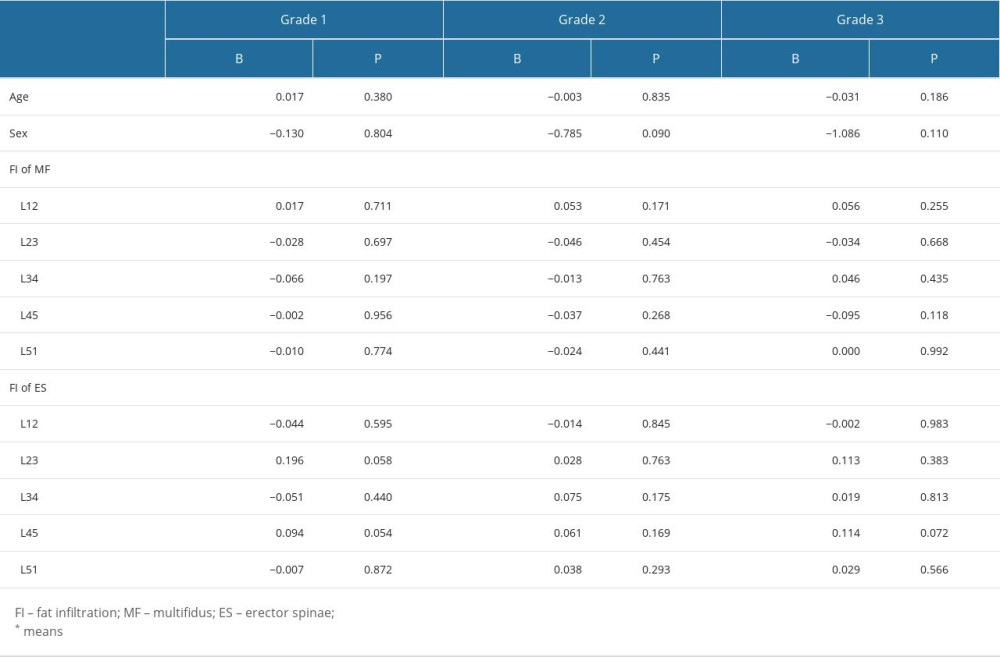 Table 3. Fat infiltration of patients with L4–L5 herniation in different grade compared with normal people.
Table 3. Fat infiltration of patients with L4–L5 herniation in different grade compared with normal people.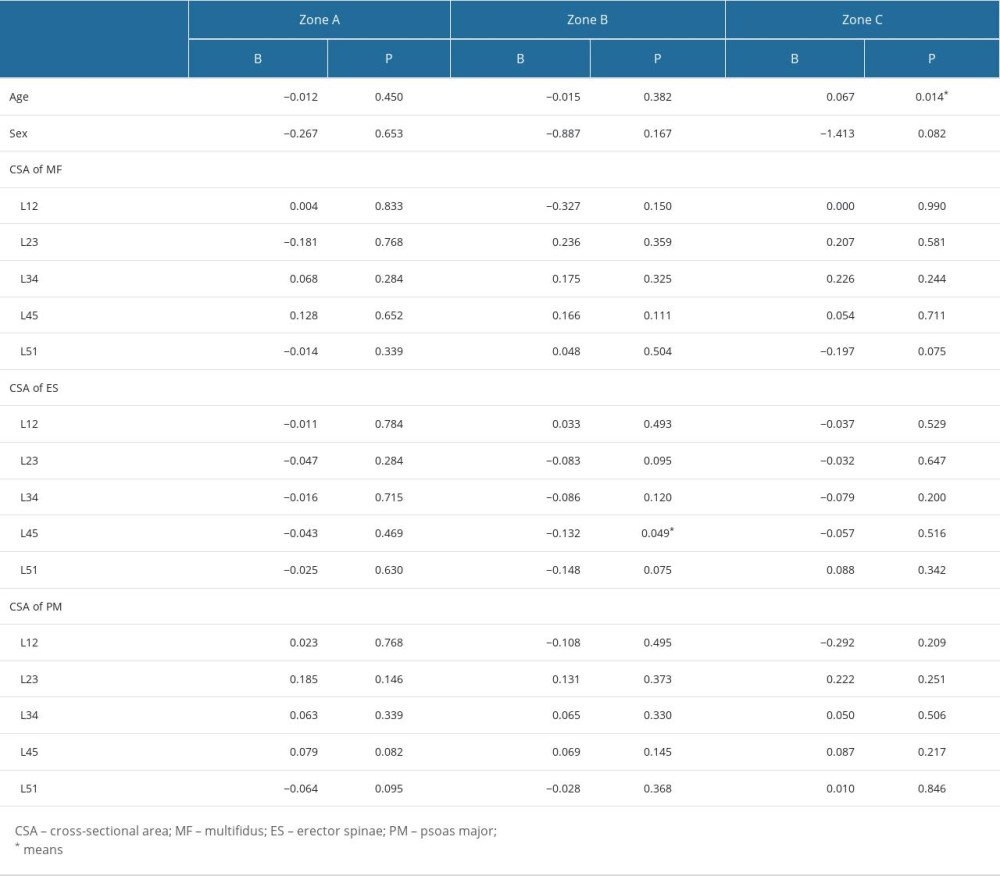 Table 4. Cross-sectional area of patients with L4–L5 herniation in different zone compared with normal people.
Table 4. Cross-sectional area of patients with L4–L5 herniation in different zone compared with normal people.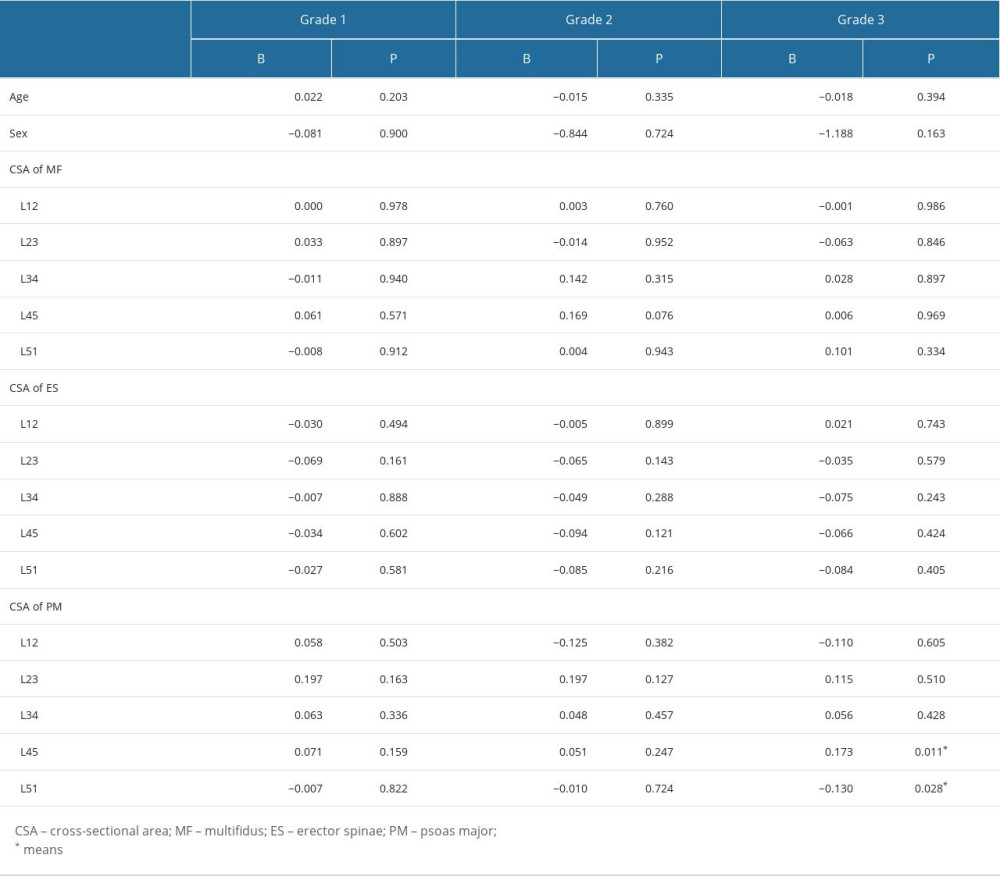 Table 5. Cross-sectional area of patients with L4–L5 herniation in different grades compared with normal people.
Table 5. Cross-sectional area of patients with L4–L5 herniation in different grades compared with normal people.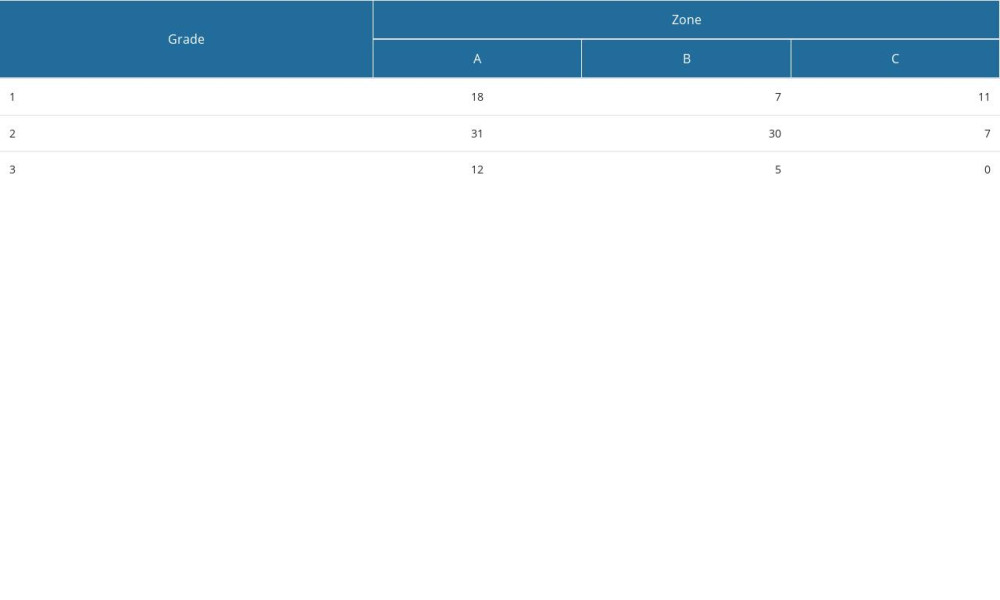 Table 1. Michigan State University classification of 121 L4–L5 lumbar disc herniation patients.
Table 1. Michigan State University classification of 121 L4–L5 lumbar disc herniation patients.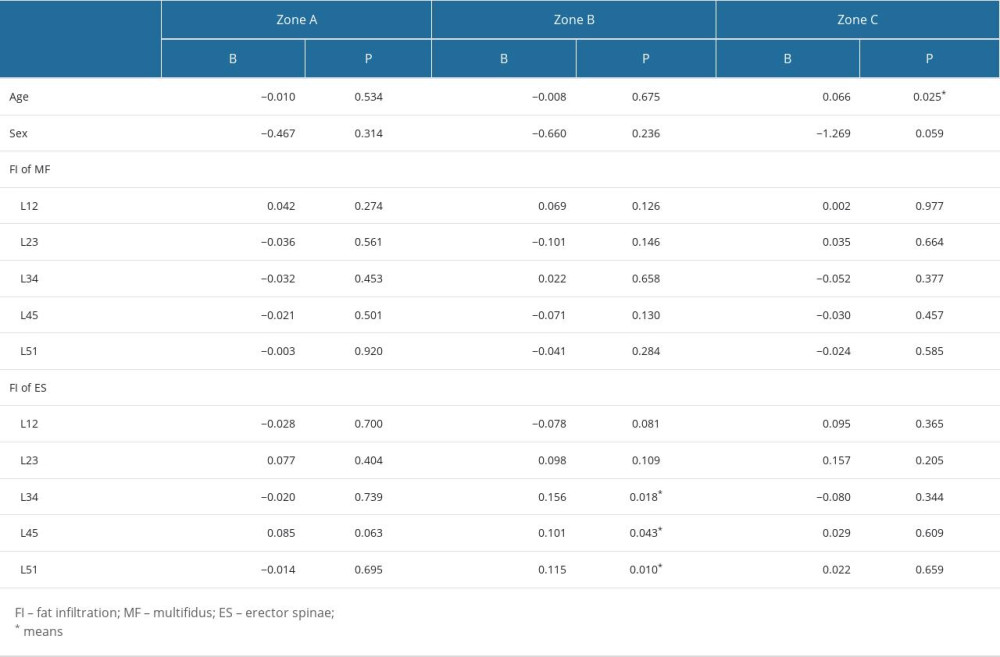 Table 2. Fat infiltration of patients with L4–L5 herniation in different zone compared with normal people.
Table 2. Fat infiltration of patients with L4–L5 herniation in different zone compared with normal people.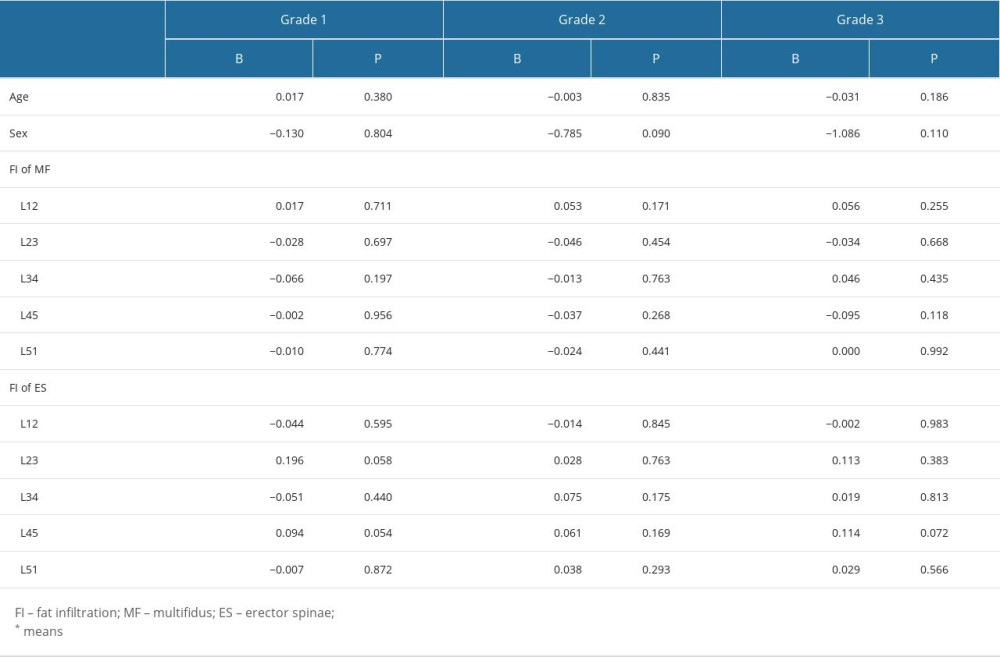 Table 3. Fat infiltration of patients with L4–L5 herniation in different grade compared with normal people.
Table 3. Fat infiltration of patients with L4–L5 herniation in different grade compared with normal people.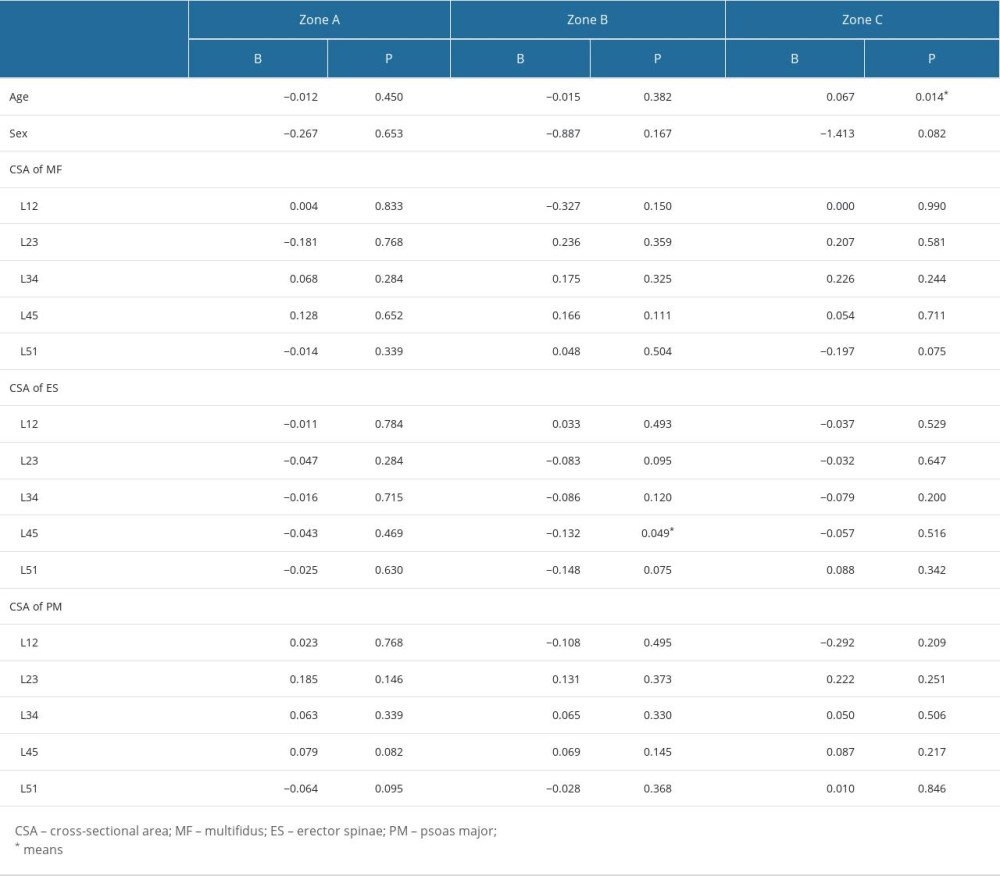 Table 4. Cross-sectional area of patients with L4–L5 herniation in different zone compared with normal people.
Table 4. Cross-sectional area of patients with L4–L5 herniation in different zone compared with normal people.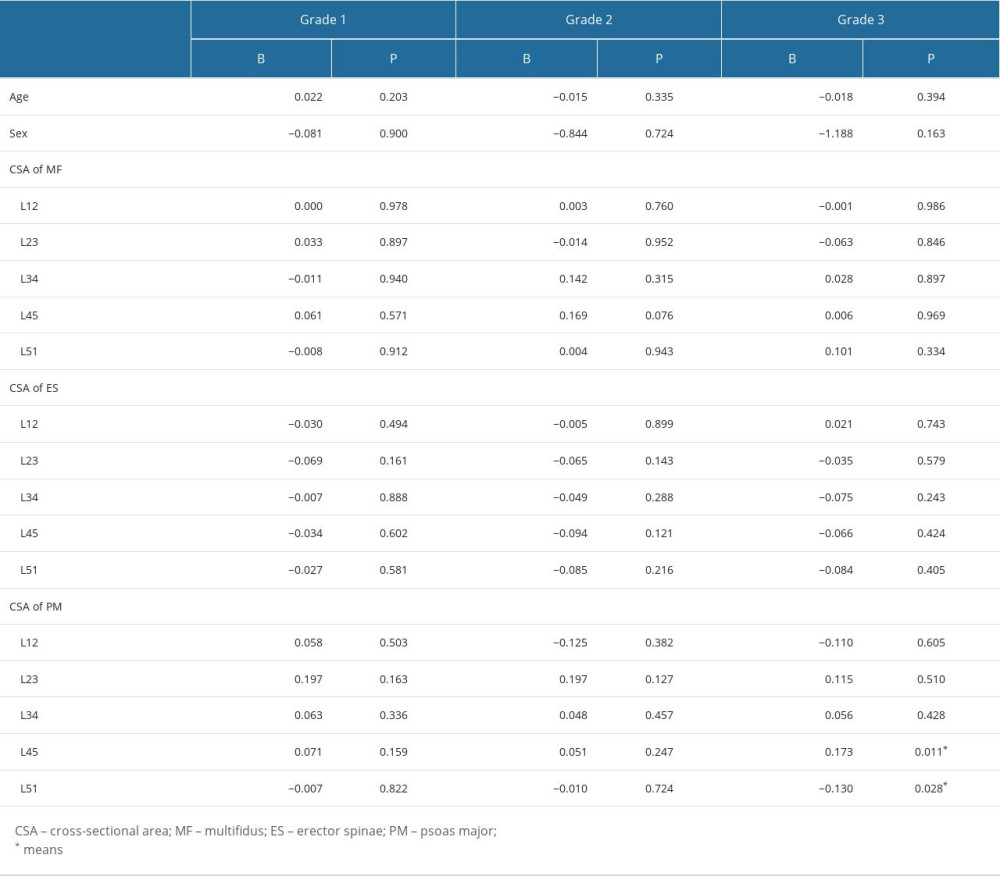 Table 5. Cross-sectional area of patients with L4–L5 herniation in different grades compared with normal people.
Table 5. Cross-sectional area of patients with L4–L5 herniation in different grades compared with normal people. In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








