10 January 2024: Meta-Analysis
The Impact of Rationing Nursing Care on Patient Safety: A Systematic Review
Izabella UchmanowiczDOI: 10.12659/MSM.942031
Med Sci Monit 2024; 30:e942031
Abstract
BACKGROUND: Rationing of nursing care (RONC) has been associated with poor patient outcomes and is a growing concern in healthcare. The aim of this systematic study was to investigate the connection between patient safety and the RONC.
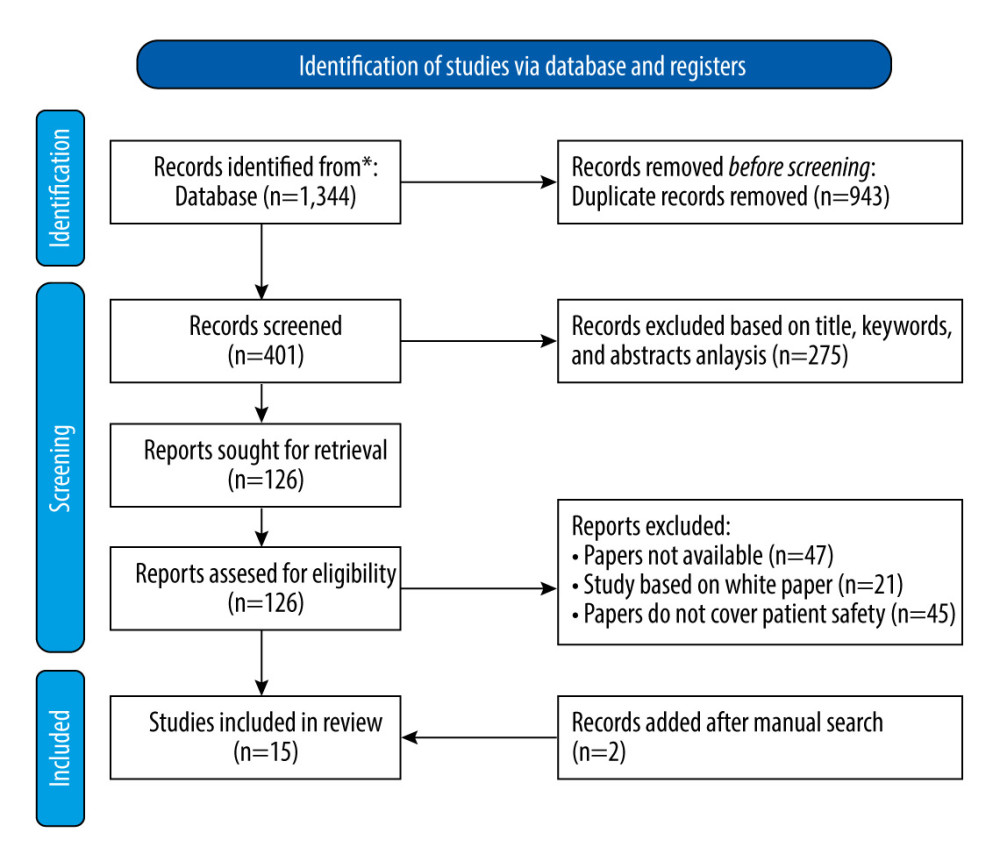
MATERIAL AND METHODS: A thorough search of electronic databases was done to find research that examined the relationship between restricting nurse services and patient safety. The systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Two reviewers (M.L. and A.P.) independently screened the titles and abstracts, and full-text articles were assessed for eligibility. Data were extracted, and a quality assessment was performed using appropriate techniques.
RESULTS: A total of 15 studies met the inclusion criteria. The studies included in the review demonstrated a correlation between rationing of nursing care and patient safety. The results of these studies revealed that there is an inverse relationship between rationing of nursing care and patient safety. The review found that when nursing care is rationed, there is a higher incidence of falls, medication errors, pressure ulcers, infections, and readmissions. In addition, the review identified that the work characteristics of nurses, such as workload, staffing levels, and experience, were associated with RONC.
CONCLUSIONS: RONC has a negative impact on patient safety outcomes. It is essential for healthcare organizations to implement effective strategies to prevent the RONC. Improving staffing levels, workload management, and communication amo0ng healthcare providers are some of the strategies that can support this.
Keywords: Nursing Care, Health Care Rationing, Patient safety
Background
OBJECTIVES:
The objective of this study was to provide a comprehensive and evidence-based understanding of the relationship between RONC and patient safety. This review aimed to identify and synthesize the available literature on the extent and causes of nursing care rationing, its impact on patient safety, and the potential strategies to mitigate its negative effects. By systematically analyzing and synthesizing relevant studies, this review will provide a more detailed and robust understanding of the complex relationship between RONC and patient safety, and thus offer insights and recommendations to support healthcare professionals, policymakers, and researchers to better address this important issue. The results of this review may also contribute to development of evidence-based guidelines and policies to improve patient safety and promote delivery of high-quality nursing care.
Material and Methods
SEARCH STRATEGY:
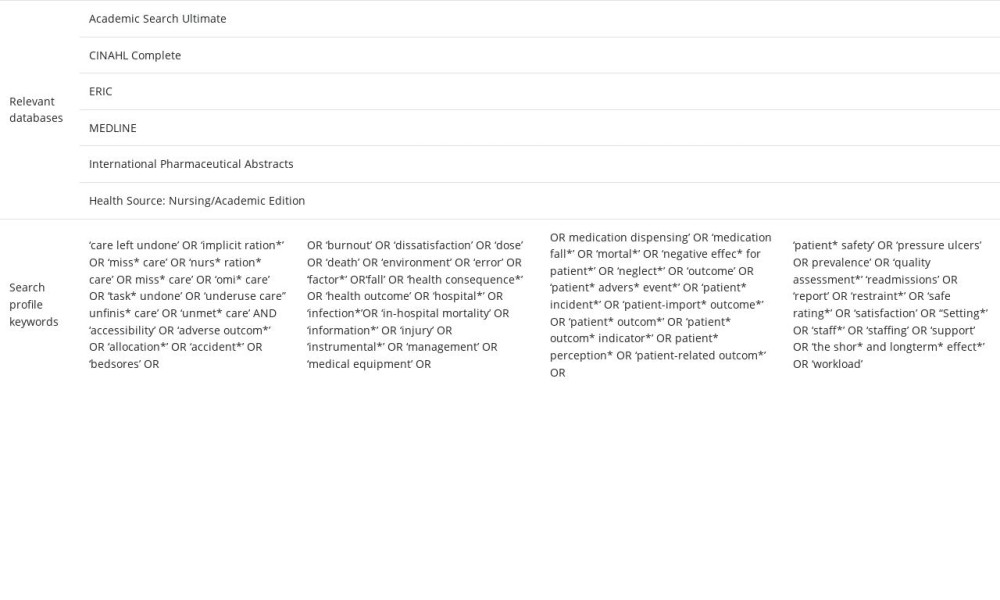
Two independent reviewers (M.L. and A.P.) conducted a comprehensive search in 6 electronic databases. The search strategy planning is shown in Table 1. The search was restricted to articles published in English from 2010 to the present. The search strategy was adapted to each database.
SELECTION CRITERIA:
The inclusion criteria for the studies were: (1) original research studies that evaluated the association between RONC and patient safety and patient outcomes, (2) studies that focused on acute care settings, (3) studies that included registered nurses as participants, and (4) studies published in English language. The exclusion criteria were: (1) studies that did not evaluate the association between RONC and patient safety, (2) studies that focused on non-acute care settings, (3) studies that did not include registered nurses as participants, and (4) studies published in languages other than English.
DATA EXTRACTION:
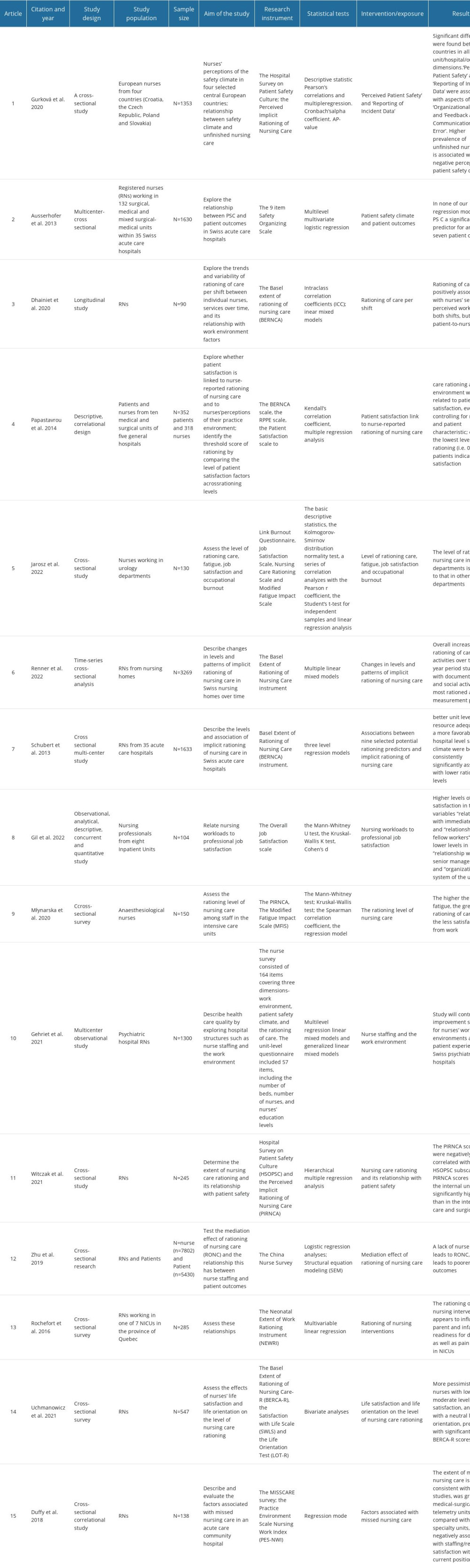
Two independent reviewers (M.L. and A.P.) screened the titles and abstracts of the identified articles and selected the articles that met the inclusion criteria. The full-texts of the selected articles were then reviewed, and data were extracted using a pre-defined data extraction form. The data extraction form included the following items: study design, study population, sample size, intervention/exposure, and key findings (Table 1). Discrepancies in the selection of articles and data extraction were resolved through discussion and consensus.
QUALITY ASSESSMENT:
The quality of the selected studies was assessed using the Cochrane Risk of Bias tool for randomized controlled trials and the Newcastle-Ottawa Scale for observational studies [18]. The quality assessment was conducted by 2 independent reviewers, and discrepancies were resolved through discussion and consensus.
DATA SYNTHESIS:
A narrative synthesis was conducted to summarize the findings of the selected studies. The studies were grouped according to the outcome measures, and findings were summarized and presented in tables and figures. Due to the heterogeneity of the studies in terms of research design, demographic, and outcome measures, a meta-analysis was not carried out.
PUBLICATION BIAS:
The funnel plots of the included studies were visually inspected to determine the likelihood of publication bias. Egger’s test was also employed to assess the funnel plots’ asymmetries. Egger’s test evaluates the significance of the constant α of the linear regression equation, where the dependent variable y is the standardized value of the effects of individual studies, and the independent variable x is the precision (ie, the inverse of the estimated standard error). The further away from 0 the value of the coefficient, the greater the asymmetry [19].
Results
CHARACTERISTICS OF THE INCLUDED STUDIES:
The 15 articles included in the analysis were published between 2010 and 2022, with 12 of the articles published between 2015 and 2022 [1,2,7,8,12,20–23,23–28]. The study designs varied from cross-sectional to longitudinal, observational, and quantitative. The study populations included registered nurses (RNs) from various healthcare settings such as medical, surgical, mixed surgical-medical, and psychiatric hospitals, nursing homes, and inpatient units. The sample sizes ranged from 90 to 7802 participants. The main intervention/exposure variables included perceived patient safety, incident report data, patient safety climate, rationing of care per shift, patient satisfaction, level of rationing of care, nursing workloads, nurse staffing, missed nursing care, and nursing interventions. Overall, the studies aimed to investigate the relationship between RONC and various outcomes such as patient safety, patient satisfaction, nursing workloads, professional job satisfaction, and missed nursing care.
Several studies examined the association between nursing care rationing and patient outcomes. Ausserhofer et al found that implicit RONC was a more robust predictor of patient outcomes than patient safety climate (PSC). Patient satisfaction probability significantly decreased as implied rationing of nursing services increased, and there was a significant increase in the odds of nurse-reported medication errors, bloodstream infections, and pneumonia [21]. In the article by Papastavrou et al, care rationing and work environment were linked to patient satisfaction even after controlling for nurse and patient variables. Even at the lowest degree of rationing, the modified regression model findings demonstrated that patients indicated low satisfaction [22]. Zhu et al found that nurses working in units with lower nurse-to-patient ratios reported higher scores on RONC, illustrating an increased level of withheld nursing care [26]. Rochefort, Bailey, and Sean revealed that 54.4% of respondents said pain was not well managed on their unit, and 15.2% of respondents believed parents and infants were not prepared for their discharge from NICU. According to multivariate analyses, reports of rationing parental support and teaching, as well as infant comfort care, were linked to less favorable perceptions of neonatal pain control, although RNs’ assessments of parent and infant preparedness for discharge was inversely correlated with limiting discharge planning [28]. The results of Duffy et al on deficient nursing care were consistent with other studies, showing it was more common on telemetry and medical-surgical units than on specialist units [27]. Some previous studies have investigated the rate of nursing care rationing and its association with workload and job satisfaction. Dhaini et al found that the rate of rationing of nursing activities exceeded 10% during day and night shifts. Rationing of care was positively associated with nurses’ self-perceived overwork in both shifts, but not with patient-to-nurse ratios [2]. Jarosz et al found that while nursing care is rarely rationed, the experience of fatigue ranged between sometimes and often. Job satisfaction is at an average level, and the level of rationing nursing care in urology departments is similar to that in other departments [7]. Schubert et al found that 98% of the participating nurses reported that they had to ration at least one of the nursing tasks listed in the Basel Extent of Rationing of Nursing Care for Nursing Homes (BERNCA). The mean rationing level of 1.69 indicates that on average the nurses reported ‘rarely’ being unable to perform the nursing tasks listed in the BERNCA [29]. Uchmanowicz et al found that nurses with low and moderate levels of life satisfaction, as well as those with a pessimistic or neutral life orientation, had higher scores on the BERCA-R than more optimistic nurses with high levels of life satisfaction [8]. Finally, Renner et al found that there were overall increases of rationing of care activities over the 5-year period studied, with documentation and social activities most rationed at both measurement points, and a considerable increase in rationing of activities of daily living was observed [23]. Młynarska et al found that sociodemographic factors did not affect the rationing level of nursing care in the intensive care unit; the average quality of patient care was 6.05/10 points, while the average job satisfaction rating was 7.13/10 points [25].
Discussion
STUDY LIMITATIONS:
Although we tried to include all relevant articles in this review, many articles could not be included due to the researchers’ lack of access to some databases; therefore, only open access English language articles were included. Based on researchers’ knowledge, even after searching various databases and sources, there is no adequate definition of nursing care rationing. In addition, it is recommended that researchers conduct more qualitative studies to develop an appropriate definition of nursing care rationing. An important aspect of care rationing research is structuration theory, which should be recommended in further research.
Conclusions
The results and conclusions from the studies we reviewed indicate that rationing of nursing care is a widespread issue in healthcare settings across different countries and specialties. The amount of nursing care that was missing is consistent with other research, with greater levels observed in medical-surgical and telemetry units, and higher levels of rationing were negatively associated with staffing/resources, job satisfaction, and collegial nurse-physician interactions.
The present review also indicates that higher levels of implicit rationing of nursing care are associated with significant decreases in patient satisfaction and significant increases in the odds of nurse-reported medication errors, bloodstream infections, and pneumonia. Determining the levels at which rationing begins to have a negative impact on patient outcomes may allow nurse managers to introduce interventions to keep rationing at a level where patient safety is not jeopardized. The variability in rationing activities was found to be associated with nurses’ self-perceived workload.
Implications
The present study highlights the need for urgent nurse leader action and future research to address the issue of nursing care rationing and to improve patient outcomes. Nursing homes, hospitals, and other healthcare settings need to consider regular monitoring of rationing of nursing care to assess nursing home care quality and determine adequate staffing levels and skill mixes. Additionally, employers should develop implementation programs for young workers to avoid burnout and invest in factors increasing nurses’ satisfaction, such as improving workplace culture. The links among organizational and environmental factors, care rationing, and patient satisfaction must also be confirmed by additional research.
Availability of Data and Materials
All relevant data are included in this article. If necessary, it is possible to contact the corresponding author to obtain additional materials.
References
1. Witczak I, Rypicz Ł, Karniej P, Rationing of nursing care and patient safety: Front Psychol, 2021; 12; 676970
2. Dhaini SR, Simon M, Ausserhofer D, Trends and variability of implicit rationing of care across time and shifts in an acute care hospital; A longitudinal study: J Nurs Manag, 2020; 28(8); 1861-72
3. Al-Jabri F, Kvist T, Sund R, Turunen H, Quality of care and patient safety at healthcare institutions in Oman; Quantitative study of the perspectives of patients and healthcare professionals: BMC Health Serv Res, 2021; 21(1); 1109
4. La Regina M, Guarneri F, Romano E, What quality and safety of care for patients admitted to clinically inappropriate wards; A systematic review: J Gen Intern Med, 2019; 34(7); 1314-21
5. Kalisch BJ, Landstrom GL, Hinshaw AS, Missed nursing care; A concept analysis: J Adv Nurs, 2009; 65(7); 1509-17
6. Schubert M, Glass TR, Clarke SP, Rationing of nursing care and its relationship to patient outcomes; The Swiss extension of the International Hospital Outcomes Study: Int J Qual Health Care, 2008; 20(4); 227-37
7. Jarosz K, Zborowska A, Młynarska A, Rationing care, job satisfaction, fatigue and the level of professional burnout of nurses in urology departments: Int J Environ Res Public Health, 2022; 19(14); 8625
8. Uchmanowicz I, Witczak I, Rypicz Ł, A new approach to the prevention of nursing care rationing; Cross-sectional study on positive orientation: J Nurs Manag, 2021; 29(2); 317-25
9. Chaboyer W, Harbeck E, Lee BO, Grealish L, Missed nursing care; An overview of reviews: Kaohsiung J Med Sci, 2021; 37(2); 82-91
10. Willis E, Brady C, The impact of “missed nursing care” or “care not done” on adults in health care; A rapid review for the Consensus Development Project: Nurs Open, 2022; 9(2); 862-71
11. Janatolmakan M, Khatony A, Explaining the consequences of missed nursing care from the perspective of nurses; A qualitative descriptive study in Iran: BMC Nurs, 2022; 21(1); 59
12. Gehri B, Bachnick S, Schwendimann R, Simon M, Matching registered nurse services with changing care demands in psychiatric hospitals; Protocol for a multicenter observational study (MatchRN Psychiatry Study): JMIR Res Protoc, 2021; 10(8); e26700
13. Wagner-Łosieczka B, Kolarczyk E, Młynarska A, The variables in the rationing of nursing care in cardiology departments: BMC Nurs, 2023; 22(1); 59
14. Griffiths P, Recio-Saucedo A, Dall’Ora C, The association between nurse staffing and omissions in nursing care; A systematic review: J Adv Nurs, 2018; 74(7); 1474-87
15. Griffiths P, Saville C, Ball J, Nursing workload, nurse staffing methodologies and tools; A systematic scoping review and discussion: Int J Nurs Stud, 2020; 103; 103487
16. McGowan J, Straus S, Moher D, Reporting scoping reviews-PRISMA ScR extension: J Clin Epidemiol, 2020; 123; 177-79
17. Moher D, Altman DG, Liberati A, Tetzlaff J, PRISMA statement: Epidemiology, 2011; 22(1); 128
18. Wee IJY, Syn NLX, Shabbir A, Enhanced recovery versus conventional care in gastric cancer surgery; A meta-analysis of randomized and non-randomized controlled trials: Gastric Cancer, 2019; 22(3); 423-34
19. Egger M, Smith GD, Schneider M, Minder C, Bias in meta-analysis detected by a simple, graphical test: BMJ, 1997; 315(7109); 629-34
20. Gurková E, Zeleníková R, Friganovic A, Hospital safety climate from nurses’ perspective in four European countries: Int Nurs Rev, 2020; 67(2); 208-17
21. Ausserhofer D, Schubert M, Desmedt M, The association of patient safety climate and nurse-related organizational factors with selected patient outcomes; A cross-sectional survey: Int J Nurs Stud, 2013; 50(2); 240-52
22. Papastavrou E, Andreou P, Tsangari H, Merkouris A, Linking patient satisfaction with nursing care; The case of care rationing – a correlational study: BMC Nurs, 2014; 13; 26
23. Renner A, Ausserhofer D, Zúñiga F, Increasing implicit rationing of care in nursing homes; A time-series cross-sectional analysis: Int J Nurs Stud, 2022; 134; 104320
24. Hellín Gil MF, Ruiz Hernández JA, Ibáñez-López FJ, Relationship between job satisfaction and workload of nurses in adult inpatient units: Int J Environ Res Public Health, 2022; 19(18); 11701
25. Młynarska A, Krawuczka A, Kolarczyk E, Uchmanowicz I, Rationing of nursing care in Intensive Care Units: Int J Environ Res Public Health, 2020; 17(19); 6944
26. Zhu X, Zheng J, Liu K, You L, Rationing of nursing care and its relationship with nurse staffing and patient outcomes; The mediation effect tested by structural equation modeling: Int J Environ Res Public Health, 2019; 16(10); 1672
27. Duffy JR, Culp S, Padrutt T, Description and factors associated with missed nursing care in an acute care community hospital: J Nurs Adm, 2018; 48(7–8); 361-67
28. Rochefort CM, Rathwell BA, Clarke SP, Rationing of nursing care interventions and its association with nurse-reported outcomes in the neonatal intensive care unit; a cross-sectional survey: BMC Nurs, 2016; 15; 46
29. Schubert M, Ausserhofer D, Desmedt M, Levels and correlates of implicit rationing of nursing care in Swiss acute care hospitals – a cross sectional study: Int J Nurs Stud, 2013; 50(2); 230-39
30. Jones T, Willis E, Amorim-Lopes M, Drach-Zahavy ARANCARE Consortium COST-CA 15208, Advancing the science of unfinished nursing care: Exploring the benefits of cross-disciplinary knowledge exchange, knowledge integration and transdisciplinarity: J Adv Nurs, 2019; 75(4); 905-17
31. Alvargonzález D, Multidisciplinarity, interdisciplinarity, transdisciplinarity, and the sciences: International Studies in the Philosophy of Science, 2011; 25(4); 387-403
In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952