11 December 2023: Clinical Research
Comprehensive Comparison of Therapeutic Efficacy of Radiofrequency Thermocoagulation and Pulsed Radiofrequency in Treatment of Elderly Patients with Thoracic Postherpetic Neuralgia
Shiyu Wang1AE, Hui Wang1BG, Huan Wang1AC, Dandan Zhang2CF, Huiyong Nie1AEF*DOI: 10.12659/MSM.942108
Med Sci Monit 2023; 29:e942108
Abstract
BACKGROUND: We comprehensively compared the therapeutic efficacy of radiofrequency thermocoagulation (RFT) and pulsed radiofrequency (PRF) in the treatment of elderly patients with thoracic postherpetic neuralgia (PHN).
MATERIAL AND METHODS: We divided 149 elderly patients with thoracic PHN into 2 groups – the RFT group (n=79) and the PRF group (n=70) – based on the radiofrequency mode administered. The Visual Analog Scale (VAS), Athens Insomnia Scale (AIS), Generalized Anxiety Disorder 7 items (GAD-7), and Patient Health Questionnaire 9 items (PHQ-9) were used to analyze the degree of pain, sleep quality, and psychological state of patients before and 1 week, 1 month, 3 months, 6 months, and 12 months after treatment.
RESULTS: VAS, AIS, GAD-7, and PHQ-9 scores were significantly decreased after RFT and PRF treatment (P<0.001). There was no significant difference in VAS scores between the 2 groups at 1 week and 1 month after treatment (P>0.05). Then, VAS scores in the RFT group were significantly lower than those in the PRF group at 3, 6, and 12 months after treatment (P<0.001). At 1 week after treatment, there were no significant differences in AIS, GAD-7, and PHQ-9 scores between the 2 groups (P>0.05). However, the RFT group had significantly lower AIS, GAD-7, and PHQ-9 scores than the PRF group at 1, 3, 6, and 12 months after treatment (P<0.05).
CONCLUSIONS: RFT and PRF both effectively reduced pain in the distribution area of thoracic spinal neuropathy and improved the sleep quality and psychological state of elderly patients with thoracic PHN, but RFT had a better long-term effect.
Keywords: Pulsed Radiofrequency Treatment, Radiofrequency Therapy, Neuralgia, Postherpetic, Aged, Quality of Life
Background
Herpes zoster (HZ) is an acute skin disease caused by reactivation and replication of varicella-zoster virus (VZV) lurking in the dorsal root ganglion (DRG). It mainly occurs in middle-aged and elderly people and people with weakened immunity. It is mainly manifested as clustered blisters distributed along nerve segments on one side of the body, accompanied by pain and paresthesia [1]. Postherpetic neuralgia (PHN) is one of the most important complications of herpes zoster. In China, about 29.8% of HZ patients develop PHN, and the prevalence increases with age [2]. With the progression of population aging, the number of elderly patients with PHN is increasing yearly. Long-term chronic pain seriously affects the quality of life of elderly patients, especially those with chronic diseases or tumors [3].
The mechanism of PHN is complex and lacks an effective method of treatment. The recommended clinical treatment methods include drug therapy and minimally invasive treatment. Commonly used drugs for the treatment of PHN include calcium channel modulators (eg, gabapentin and pregabalin), tricyclic antidepressants (eg, amitriptyline and nortriptyline), and topical lidocaine patches. The pharmacotherapy of neuropathic pain is challenging and frequently unsatisfactory [4]. Elderly patients have increased sensitivity to CNS drugs. Therefore, the central adverse effects of some drugs may limit their use [5,6]. The minimally invasive methods commonly used by clinicians to treat PHN include nerve block, radiofrequency thermocoagulation (RFT), pulsed radiofrequency (PRF), and nerve electrical stimulation, which have an essential role in pain relief. A number of studies have confirmed that both RFT and PRF can relieve pain and paresthesia in PHN patients [6–9]. However, there is no comparative study on the efficacy of these 2 methods in elderly patients with PHN. The present study comprehensively analyzed the analgesic effects of RFT and PRF in the treatment of PHN in elderly patients, as well as the effects on sleep quality and psychological state of patients.
Material and Methods
PATIENTS:
This retrospective study included 158 elderly patients (>60 years old) with PHN who were hospitalized in the Pain Department of the First Affiliated Hospital of Xi’an Jiaotong University from March 2020 to March 2022. A total of 149 patients completed the follow-up, including 79 in the RFT group and 70 in the PRF group. Nine patients were lost to follow-up, including 7 patients lost to follow-up due to changing telephone number, and 2 patients died (Figure 1). We recorded data on age, gender, disease duration, height, weight, preoperative VAS score, smoking, drinking, hypertension, diabetes, and postoperative complications. The patients were followed up at 1 week, 1 month, 3 months, 6 months, and 12 months after the operation. The pain score (VAS), sleep quality (AIS), and psychological state (GAD-7, PHQ-9) of the 2 groups were compared and analyzed. This study was approved by the Ethics Committee of the First Affiliated Hospital of Xi’an Jiaotong University (KYLLSL-2022–205).
Inclusion criteria were: (1) PHN arising from thoracic spinal nerves (T2–T12); (2) history of herpes zoster over 3 months; (3) persistent intense pain, with/without local skin hyperalgesia, and sensory abnormalities even after complete healing of skin lesions; (4) pain not controlled with standard pharmacotherapy (antiepileptic drugs, antidepressants, opioids) or physical treatments as recommended by the International Association for the Study of Pain; and (5) 24-hour visual analog scale (VAS) score ≥5. Exclusion criteria were: (1) history of malignant tumor; (2) history of systemic immune diseases; (3) incomplete follow-up data; (4) received other interventional therapy before surgery or during follow-up; (5) mental or psychological disorders.
SURGICAL PROCEDURE:
Patients in the prone position were routinely monitored with electrocardiography and oxygen saturation. The area to be treated was routinely disinfected. The surgeon located the puncture point according to the affected spinal nerve segment and performed local infiltration anesthesia with 0.5% lidocaine. Under C-arm guidance, the radiofrequency needle (5 mm at the bare end) was punctured through the skin layer by layer into the DRG (Figure 2), at which time the patient may experience abnormal sensation in the area of previous pain. Then, the RF device was turned on and sensory tests were performed (50 Hz, 0.5 ms, <0.2 v) and motor test (2 Hz, 1.0 ms, <0.5 v). The pain and muscle twitch in the corresponding lesion site were elicited and completely covered, which proved that the location was accurate. The RFT group received standard radiofrequency mode, and the parameters were set as: 80°C and 180 s. The PRF group received pulsed RF mode, and the parameters were set as: 42°C, pulse width 50 ms, and 300 s. At the end of the treatment, the patients were locally sterilized, pasted with sterile excipients, and sent back to the ward for close observation.
All surgical procedures were performed by the same surgeon. Whether a doctor provided a RFT or PRF procedure to a patient depended on 3 factors: (1) Patient’s tolerance to pain in daily life (pain is more obvious during RFT), (2) Patients’ acceptance of postoperative complications(numbness may occur after RFT), and (3) Patients with cardiovascular and cerebrovascular risk were recommended to receive PRF therapy.
OBSERVATIONS AND FOLLOW-UP:
The Visual Analog Scale (VAS) was used to assess the patient’s pain. A 10-cm straight line was used, and the 2 ends were marked with “no pain” (0) and “severe pain” (10). The distance from the starting point to the mark was the pain intensity score.
The Athens Insomnia Scale (AIS) was used to evaluate the effect of pain on patients’ sleep. The total score was 24 points, with more than 6 points indicating insomnia, 4–6 points indicating suspected insomnia, and <4 points indicating no sleep disorder.
Generalized Anxiety Disorder 7 items (GAD-7) and Patient Health Questionnaire 9 items (PHQ-9) were used to evaluate the degree of anxiety and depression of patients. GAD-7 score was defined as normal (0–4), anxiety tendency (5–6), mild anxiety (7–10), moderate anxiety (11–17), and severe anxiety (18–21). The PHQ-9 score was defined as normal (0–4), mild depression (5–9), moderate depression (10–14), moderate to severe depression (15–19), and severe depression (20–27).
The patients were followed up at 1 week, 1 month, 3 months, 6 months, and 12 months after treatment through outpatient, telephone, and Internet communication. The patients’ pain degree, sleep quality, and psychological state were analyzed and evaluated.
STATISTICAL ANALYSIS:
SPSS 27.0 software was used for statistical analysis. The normally distributed measurement data were described as mean±standard deviation (χ̆ ±s). The age, course of disease, height, and weight of the 2 groups were compared by independent samples
Results
PATIENT CHARACTERISTICS:
According to the inclusion and exclusion criteria, a total of 149 patients completed the study, including 79 patients in the RFT group and 70 patients in the PRF group. There was no significant difference in age, disease duration, height, weight, and preoperative VAS score between the 2 groups (P>0.05). In addition, the patients’ smoking, drinking, hypertension, diabetes, and postoperative complications were also recorded. The 2 groups did not significantly differ in terms of smoking, alcohol consumption, hypertension, or diabetes. However, patients in the RFT group had more postoperative complications than those in the PRF group (P=0.044). Seven patients had local numbness, and 4 patients had local short-term hyperalgesia in the RFT group, which are normal complications of surgery (Table 1).
According to the number of patients included in this study and the 12-month VAS score data, the statistical power calculated was greater than 99.9% with α=0.05; therefore, the study sample was much larger than the minimum sample size required.
POSTOPERATIVE VAS SCORES:
The postoperative VAS scores of all patients were significantly lower than those before the operation (P<0.001). There was no significant difference in VAS scores between the RFT group and PRF group at 1 week and 1 month after the operation (P>0.05). However, with the extension of follow-up time, the VAS score in the RF group continued to decrease, while the VAS score in the PRF group increased slightly. At 3, 6, and 12 months after surgery, the VAS scores between the 2 groups were significantly different (P<0.001, Figure 3). Repeated measures ANOVA between the 2 groups led to the same conclusion. The time effect between the 2 groups was statistically significant (F=867.661, P<0.001), and the time*group effect was statistically significant (F=43.291, P<0.001), indicating that RFT was superior to PRF in reducing the VAS score (Table 2).
POSTOPERATIVE AIS SCORES:
The postoperative AIS scores of all patients were significantly lower than those before surgery (P<0.001). There was no significant difference in AIS scores between the RFT group and the PRF group at 1 week after surgery (P> 0.05). At 1, 3, 6, and 12 months after surgery, the AIS score in the RFT group was lower than that in the PRF group (P<0.05, Figure 4). The results of repeated measures analysis of variance (Table 3) showed that the postoperative AIS score was significantly lower than that before surgery (F=1539.372, P<0.001). The time*group effect showed that the AIS score of the RFT group decreased more than that of the PRF group, meaning that the sleep improvement of the RFT group was more significant (F=51.585, P<0.001).
POSTOPERATIVE GAD-7 AND PHQ-9 SCORES:
Postoperative GAD-7 and PHQ-9 scores of all patients were significantly lower than those before surgery (P<0.001), with significant improvement in anxiety and depression. The GAD-7 and PHQ-9 scores of patients in the RFT group showed a gradual downward trend after surgery, while those in the PRF group showed a slight increase after 1 month after surgery (Figure 5). There was no significant difference in GAD-7 and PHQ-9 scores between the RFT group and PRF group at 1 week after surgery (P>0.05). GAD-7 and PHQ-9 scores in the RFT group were significantly lower than those in the PRF group at 1, 3, 6, and 12 months after surgery (P<0.001). Repeated measures analysis of variance showed that the time effect of GAD-7 (F=1299.504, P<0.001) and PHQ-9 (F=1791.680, P<0.001) scores were statistically significant, meaning that anxiety and depression in the 2 groups were significantly improved after surgery. While the time*group effect suggested that the GAD-7 (F=36.351, P<0.001) and PHQ-9 (F=32.104, P<0.001) scores were significantly lower than in the PRF group, which means that with the extension of follow-up time, the anxiety and depression of patients after RFT were more improved than those of the PRF group (Table 4).
Discussion
INTRODUCTION TO HZ:
Varicella-zoster virus (VZV) is a double-stranded DNA virus belonging to the human herpesvirus (HHV3) family. When a susceptible person inhales virus-containing droplets or aerosols, the virus replicates rapidly in the T cells of the Waldeyer ring and then causes systemic blisters through hematogenous dissemination. Immunocompromised persons may develop severe conditions such as disseminated herpes, viral pneumonia, or involvement of internal organs [10,11]. Subsequently, the virus migrates retrograde from the infected skin lesions to the dorsal root ganglion cells of the spinal cord to incubate. With age, when the body’s immunity declines, the virus lurking in the ganglion is reactivated and replicated, and then clusters of blisters appear along the nerve segments on one side of the body, and the thoracic spinal cord segment is the most vulnerable. Currently available recombinant herpes zoster vaccines reduce the incidence of herpes zoster by about 90% [12–14]. Studies [15,16] have shown that COVID-19 infection can increase the risk of neuralgia in patients with herpes zoster, especially in the elderly. However, during the study period (March 2020 to March 2022), the Chinese government adopted strict quarantine measures, so the enrolled patients did not test positive for SARS-CoV-2 during the study.
MECHANISMS OF PAIN IN PHN:
Postherpetic neuralgia (PHN), defined as local pain lasting more than 3 months after healing of herpes zoster (HZ), is the most common complication of HZ. At present, the mechanism of pain caused by PHN is not completely clear, and the existing research mainly includes peripheral nerve sensitization and central nerve sensitization. VZV activates and proliferates and destroys axons in DRG, causing nerve demyelination and ion channel dysfunction, leading to spontaneous abnormal nerve discharge and abnormal excitation. VZV can enhance nociceptive signals, increase the production and release of pro-inflammatory mediators and pro-inflammatory cytokines, and lead to peripheral nerve sensitization [17,18]. However, pro-inflammatory mediators and cytokines activate C-fibers in the central nervous system and lead to central nervous sensitization. Peripheral and central nervous sensitization complement and interact with each other [19,20]. The enhancement of pain signal, proliferation, and activation of pathological microglia, interleukin-6 (IL-6), interleukin-10 (IL-10), and other cytokines and abnormalities of multiple signaling pathways are involved in the occurrence of pain in PHN patients [21].
The pain caused by PHN seriously affects the sleep quality and psychological state of patients. Du et al [22] showed that 69.0% (456/661) of PHN patients had anxiety and 65.8% (435/661) had depression, and female gender, pain intensity, eruption onset time, and extent of rash spread were significantly related to anxiety and depression in PHN patients [22]. Studies have shown that activated inflammatory processes can affect multiple aspects of central nervous system function, leading to behavioral changes in patients with depression, and immune abnormalities in patients with PHN may be related to the occurrence of depression [23]. Moreover, people with greater psychological stress are at higher risk of HZ and PHN, and interventions targeting the psychological state of AHZ patients may help to slow the progression of PHN [24,25].
MECHANISMS OF RFT AND PRF IN THE TREATMENT OF PHN:
The treatment of PHN mainly includes drug therapy and minimally invasive interventional therapy. Drug therapy, as the preferred method for pain relief, has been clinically proven to be effective. However, due to the poor efficacy and adverse effects, there are still many patients whose pain cannot be well controlled. Especially in the elderly, increased sensitivity to CNS drugs leads to increased adverse effects [6]. Minimally invasive interventional therapy mainly includes nerve block, RFT, PRF, and spinal cord electrical stimulation (SCS), which can be used as a second-line option to relieve pain to a certain extent. Targeted DRG therapy has some effect on relieving PHN, and the pain relief time is longer than that of nerve block. Therefore, interventional therapies such as RFT, PRF, and SCS have good prospects for development [20].
Current studies suggest that PRF can relieve pain by modulating neuronal activity, altering neuronal excitability, affecting synaptic transmission and neurotransmitter release, and altering the number of pathological microglia [26,27]. Although the treatment of PRF causes little damage to patients, the recurrence rate is high. This was confirmed by the follow-up results of 67 patients, in which the recurrence rate in the PRF group was 37.31% within 3 months after surgery, and the total recurrence rate was 44.78% [28]. RF can relieve pain by blocking pain transmission and causing tissue and protein damage through the heat produced. It can treat a variety of acute and chronic pain and neuropathic pain, and produce more lasting effects. Zhang [29] showed that the 1-year effective rate of RFT in the treatment of PHN was 75.6%, and Zhu [7] showed that the pain relief effect of bipolar RFT with 5-mm spacing was better than that of single-stage, which was more complete and had better pain relief time and effect. Our results also showed that RFT had a longer lasting effect on pain relief than PRF.
It should be pointed out that RFT causes irreversible nerve damage and may cause complications such as local numbness and paresthesia. Although the clinical application of RFT is controversial at present, we suggest that RFT treatment can be performed according to the situation for patients with recurrence and refractory, unbearable pain who are willing to accept the possible complications such as numbness. After all, RFT provides better and longer pain relief.
SIGNIFICANCE OF RESEARCH:
Our study shows that RFT is superior to PRF in alleviating PHN in elderly patients, and the effect can be extended to 12 months after surgery. In addition, we investigated the effects of different radiofrequency modes on sleep quality and psychological state of patients. The psychological state changes caused by PHN have a great impact on the life of patients. Many patients suffer from chronic pain, and in serious cases, patients may even have a suicidal tendency. Many elderly PHN patients are complicated with multiple chronic diseases. Our study found that patients with PHN had better improvement in anxiety, depression, and sleep symptoms after RFT, which may be related to the reduction of pain in patients with PHN, but the specific mechanism needs to be studied further.
LIMITATIONS OF THE STUDY:
Our study has certain limitations. First, this was a single-center study with a relatively limited clinical sample. Second, the follow-up period of our study was up to 12 months after surgery, and further follow-up studies are needed to clarify the long-term effect of RFT treatment. In addition, we did not study the extent to which the combination of RF or PRF with nerve block or oral, topical agents improved patient pain levels. As a retrospective study, the results may also have been affected by other treatments that patients received during follow-up. The patient’s socioeconomic status, education level, and family support should also be considered. The above deficiencies will be addressed in future studies.
PROSPECTS FOR THE FUTURE:
RFT and PRF have great research prospects for the relief of chronic neuropathic pain. In addition to PHN, other neuropathic pain such as trigeminal neuralgia (TN) [30,31], complex regional pain syndrome [32], sympathetic chain syndrome [33], and other neuropathic pain [34] can choose RF or PRF to relieve pain, and clinical research is of great significance.
Conclusions
RFT and PRF can effectively reduce the pain in the distribution area of thoracic spinal neuropathy, and improve sleep quality and psychological state of elderly patients with thoracic PHN, and RFT has a better long-term effect.
Figures
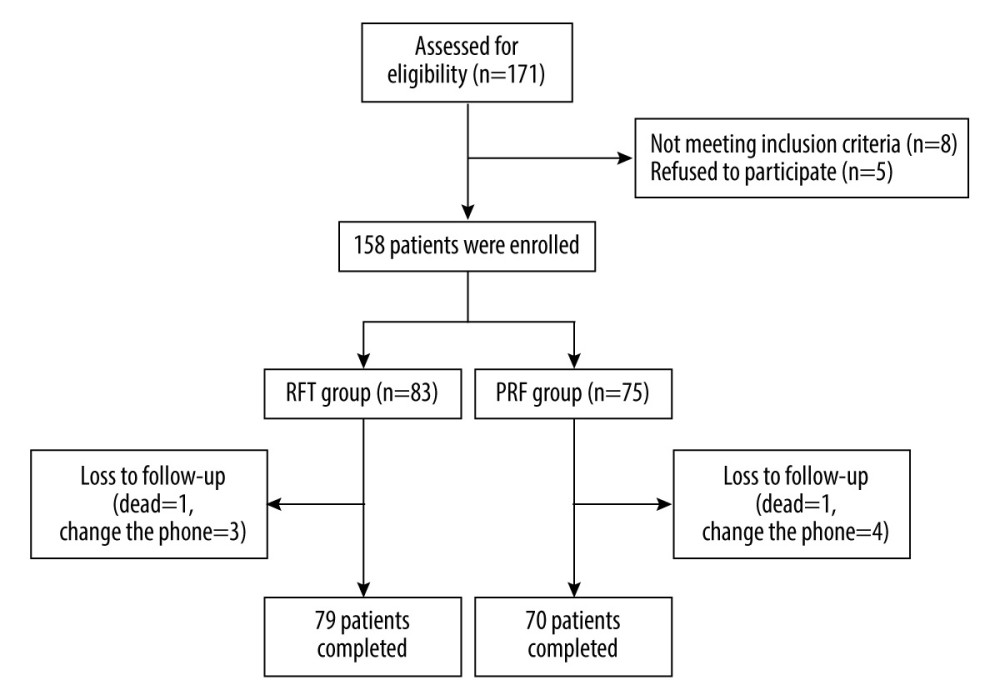 Figure 1. Flow chart of patient enrollment and follow-up (Office 2007, Microsoft Corporation).
Figure 1. Flow chart of patient enrollment and follow-up (Office 2007, Microsoft Corporation). 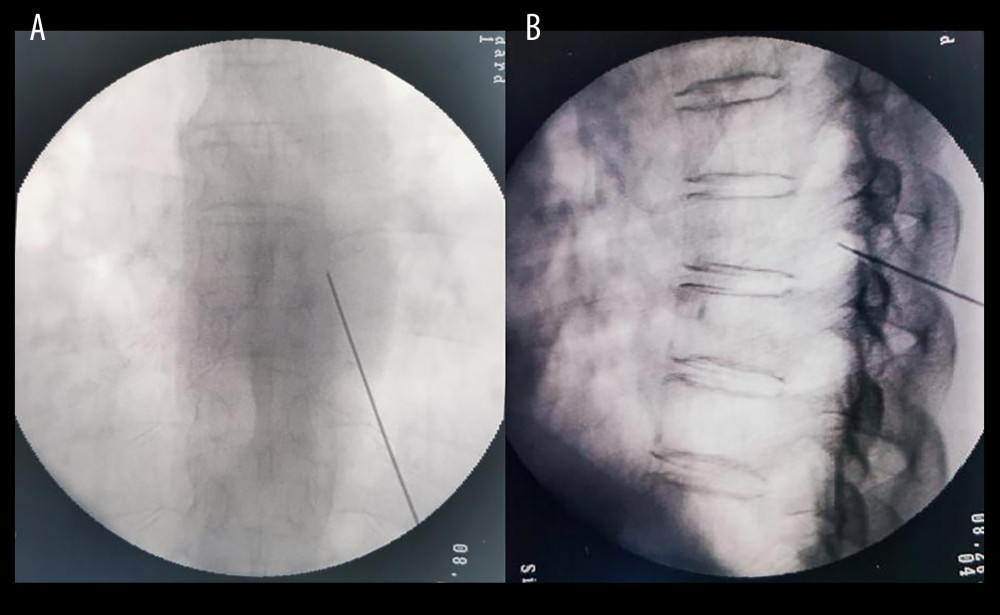 Figure 2. C-arm guided DRG puncture (A for anteroposterior radiography, B for lateral radiography. DRG – dorsal root ganglion) (C-Arm, Siemens AG, Germany).
Figure 2. C-arm guided DRG puncture (A for anteroposterior radiography, B for lateral radiography. DRG – dorsal root ganglion) (C-Arm, Siemens AG, Germany). 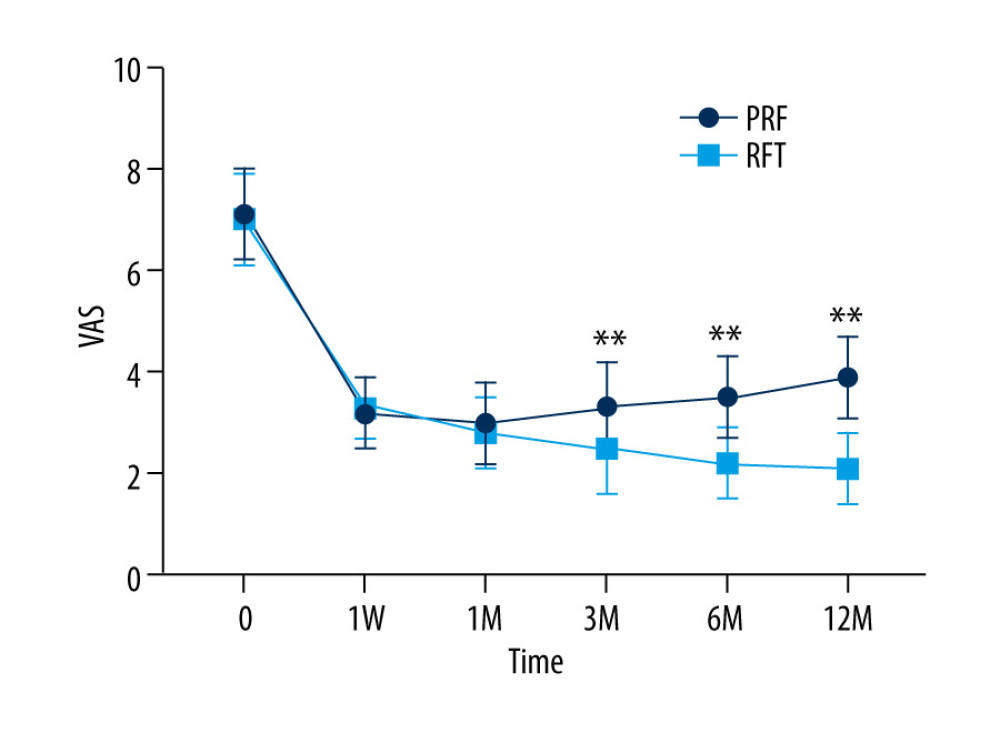 Figure 3. VAS score of RFT and PRF groups (** P<0.001, RFT vs PRF) (GraphPad Prism 8, GraphPad).
Figure 3. VAS score of RFT and PRF groups (** P<0.001, RFT vs PRF) (GraphPad Prism 8, GraphPad). 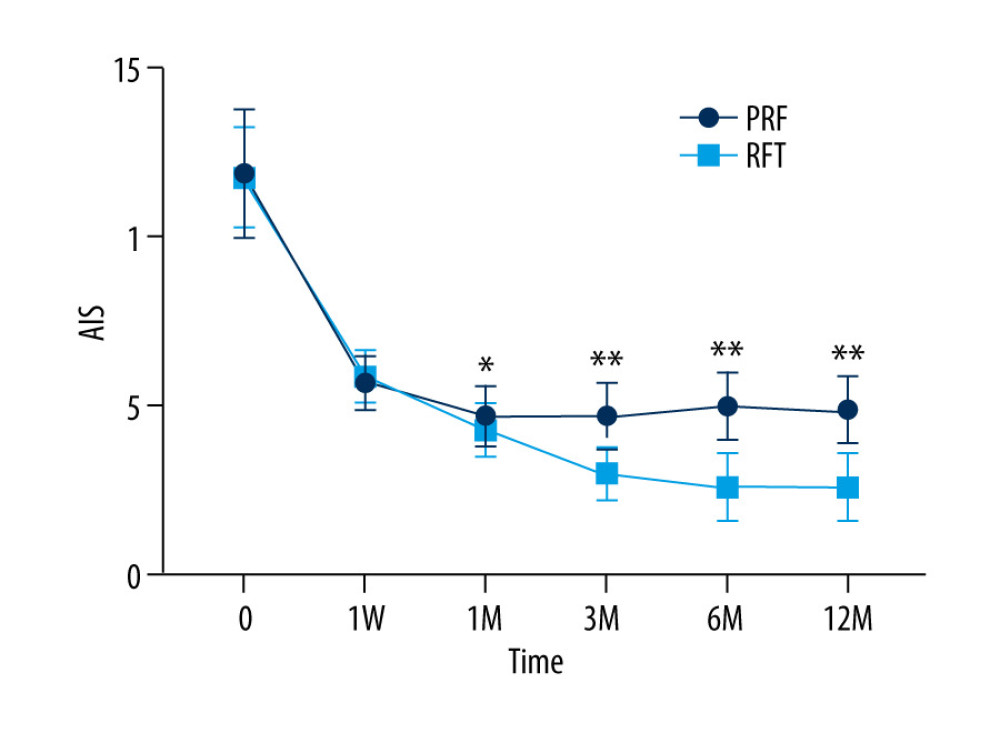 Figure 4. AIS in RFT and PRF groups (* P<0.05/** P<0.001, RF vs PRF) (GraphPad Prism 8, GraphPad).
Figure 4. AIS in RFT and PRF groups (* P<0.05/** P<0.001, RF vs PRF) (GraphPad Prism 8, GraphPad). 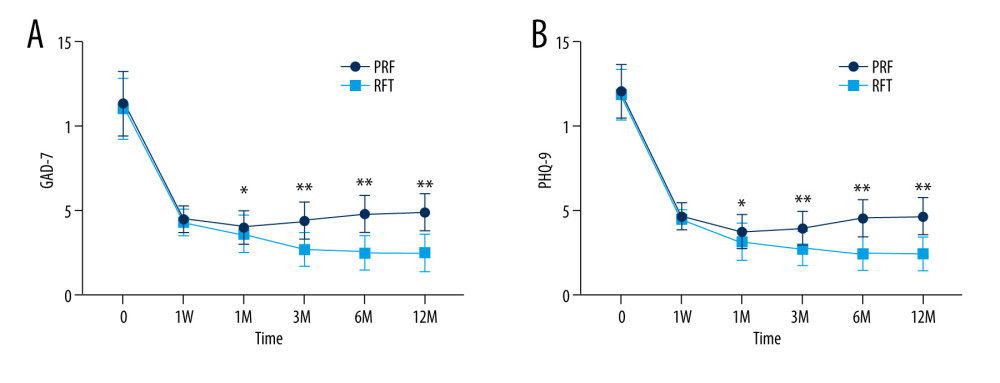 Figure 5. GAD-7 (A) and PHQ-9 (B) of RFT and PRF groups (* P<0.05/** P<0.001, RF vs PRF) (GraphPad Prism 8, GraphPad).
Figure 5. GAD-7 (A) and PHQ-9 (B) of RFT and PRF groups (* P<0.05/** P<0.001, RF vs PRF) (GraphPad Prism 8, GraphPad). References
1. John AR, Canaday DH, Herpes zoster in the older adult: Infect Dis Clin North Am, 2017; 31(4); 811-26
2. Yang F, Yu S, Fan B, The epidemiology of herpes zoster and postherpetic neuralgia in China: Results from a cross-sectional study: Pain Ther, 2019; 8(2); 249-59
3. Pickering G, Leplege A, Herpes zoster pain, postherpetic neuralgia, and quality of life in the elderly: Pain Pract, 2011; 11(4); 397-402
4. Kremer M, Salvat E, Muller A, Antidepressants and gabapentinoids in neuropathic pain: Mechanistic insights: Neuroscience, 2016; 338; 183-206
5. Mallick-Searle T, Snodgrass B, Brant JM, Postherpetic neuralgia: Epidemiology, pathophysiology, and pain management pharmacology: J Multidiscip Healthc, 2016; 9; 447-54
6. Huang X, Ma Y, Wang W, Efficacy and safety of pulsed radiofrequency modulation of thoracic dorsal root ganglion or intercostal nerve on postherpetic neuralgia in aged patients: A retrospective study: BMC Neurol, 2021; 21(1); 233
7. Zhu J, Luo G, He Q, Evaluation of the efficacy of unipolar and bipolar spinal dorsal root ganglion radiofrequency thermocoagulation in the treatment of postherpetic neuralgia: Korean J Pain, 2022; 35(1); 114-23
8. Sheng L, Liu Z, Zhou W, Short-term spinal cord stimulation or pulsed radiofrequency for elderly patients with postherpetic neuralgia: A prospective randomized controlled trial: Neural Plast, 2022; 2022; 7055697
9. Li D, Sun G, Sun H, Combined therapy of pulsed radiofrequency and nerve block in postherpetic neuralgia patients: A randomized clinical trial: PeerJ, 2018; 6; e4852
10. Ehrenstein B, Diagnosis, treatment and prophylaxis of herpes zoster: Z Rheumatol, 2020; 79(10); 1009-17
11. Patil A, Goldust M, Wollina U, Herpes zoster: A review of clinical manifestations and management: Viruses, 2022; 14(2); 192
12. Schmader K, Herpes zoster: Ann Intern Med, 2018; 169(3); ITC19-ITC31
13. Meister W, Neiss A, Gross G, Demography, symptomatology, and course of disease in ambulatory zoster patients. A physician-based survey in Germany: Intervirology, 1998; 41(6); 272-77
14. Koshy E, Mengting L, Kumar H, Epidemiology, treatment and prevention of herpes zoster: A comprehensive review: Indian J Dermatol Venereol Leprol, 2018; 84(3); 251-62
15. Joshi D, Gyanpuri V, Pathak A, Neuropathic pain associated with COVID-19: A systematic review of case reports: Curr Pain Headache Rep, 2022; 26(8); 595-603
16. Aknin LB, De Neve JE, Dunn EW, The neurological consequences of contracting COVID-19: Acta Neuropsychologica, 2021; 19(3); 301-5
17. Watson P, Postherpetic neuralgia: Am Fam Physician, 2011; 84(6); 690-92
18. Ji RR, Nackley A, Huh Y, Neuroinflammation and central sensitization in chronic and widespread pain: Anesthesiology, 2018; 129(2); 343-66
19. Basbaum AI, Bautista DM, Scherrer G, Cellular and molecular mechanisms of pain: Cell, 2009; 139(2); 267-84
20. Meacham K, Shepherd A, Mohapatra DP, Neuropathic pain: Central vs. Peripheral mechanisms: Curr Pain Headache Rep, 2017; 21(6); 28
21. Baron R, Binder A, Wasner G, Neuropathic pain: Diagnosis, pathophysiological mechanisms, and treatment: Lancet Neurol, 2010; 9(8); 807-19
22. Du J, Sun G, Ma H, Prevalence and risk factors of anxiety and depression in patients with postherpetic neuralgia: A retrospective study: Dermatology, 2021; 237(6); 891-95
23. Irwin MR, Miller AH, Depressive disorders and immunity: 20 years of progress and discovery: Brain Behav Immun, 2007; 21(4); 374-83
24. Koga R, Yamada K, Ishikawa R, Association between treatment-related early changes in psychological factors and development of postherpetic neuralgia: J Anesth, 2019; 33(6); 636-41
25. Takao Y, Okuno Y, Mori Y, Associations of perceived mental stress, sense of purpose in life, and negative life events with the risk of incident herpes zoster and postherpetic neuralgia: The SHEZ study: Am J Epidemiol, 2018; 187(2); 251-59
26. Sam J, Catapano M, Sahni S, Pulsed radiofrequency in interventional pain management: Cellular and molecular mechanisms of action – an update and review: Pain Physician, 2021; 24(8); 525-32
27. Park D, Chang MC, The mechanism of action of pulsed radiofrequency in reducing pain: A narrative review: J Yeungnam Med Sci, 2022; 39(3); 200-5
28. Luo G, Zhang Z, Zhu J, Association between the risk of relapse and the type of surgical procedure for herpes zoster-related pain: Pain Physician, 2021; 24(8); E1227-36
29. Zhang Z, Xia Z, Luo G, Analysis of efficacy and factors associated with reccurence after radiofrequency thermocoagulation in patients with postherpetic neuralgia: A long-term retrospective and clinical follow-up study: Pain Ther, 2022; 11(3); 971-85
30. Hong T, Ding Y, Yao P, Long-term efficacy and complications of radiofrequency thermocoagulation at different temperatures for the treatment of trigeminal neuralgia: Biochem Res Int, 2020; 2020; 3854284
31. Liao C, Visocchi M, Yang M, Pulsed radiofrequency: A management option for recurrent trigeminal neuralgia following radiofrequency thermocoagulation: World Neurosurg, 2017; 97; 760e765-e767
32. Park J, Lee YJ, Kim ED, Clinical effects of pulsed radiofrequency to the thoracic sympathetic ganglion versus the cervical sympathetic chain in patients with upper-extremity complex regional pain syndrome: A retrospective analysis: Medicine (Baltimore), 2019; 98(5); e14282
33. Kim ED, Yoo WJ, Kim YN, Ultrasound-guided pulsed radiofrequency treatment of the cervical sympathetic chain for complex regional pain syndrome: A retrospective observational study: Medicine (Baltimore), 2017; 96(1); e5856
34. Carralero-Martínez A, Muñoz Pérez MA, Kauffmann S, Efficacy of capacitive resistive monopolar radiofrequency in the physiotherapeutic treatment of chronic pelvic pain syndrome: A randomized controlled trial: Neurourol Urodyn, 2022; 41(4); 962-72
Figures
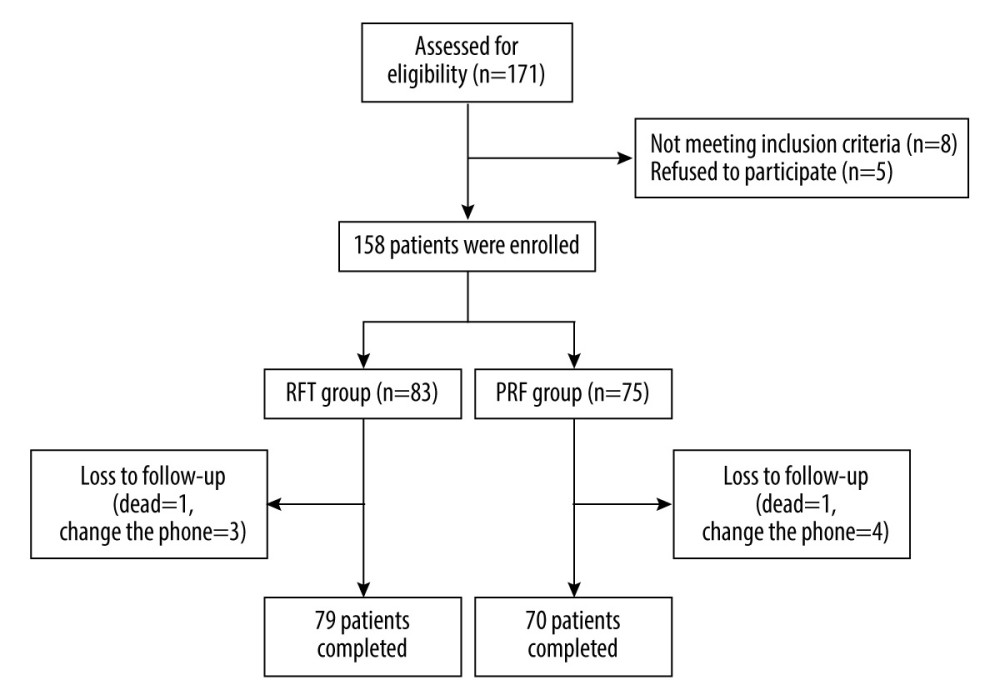 Figure 1. Flow chart of patient enrollment and follow-up (Office 2007, Microsoft Corporation).
Figure 1. Flow chart of patient enrollment and follow-up (Office 2007, Microsoft Corporation).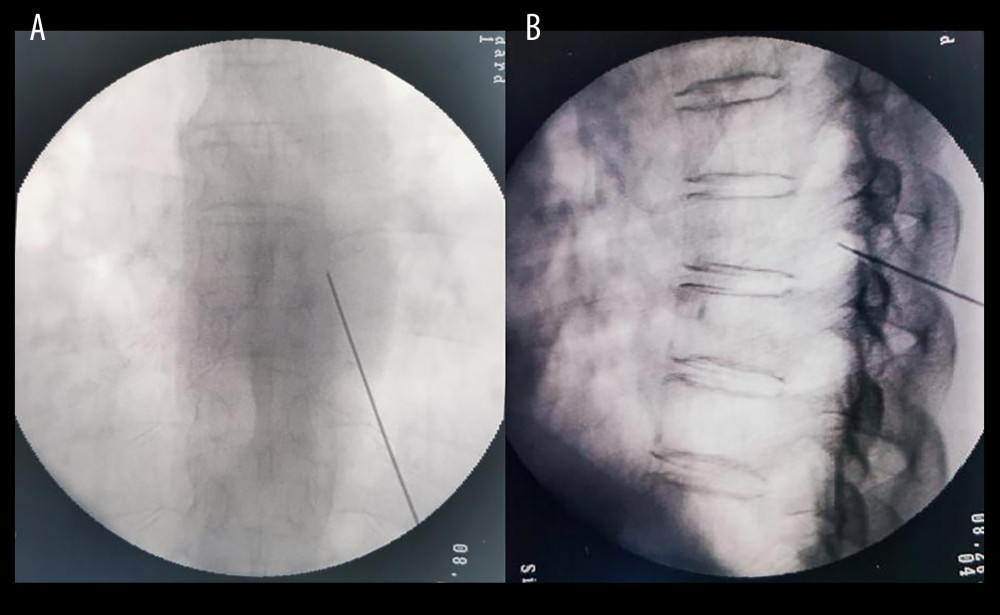 Figure 2. C-arm guided DRG puncture (A for anteroposterior radiography, B for lateral radiography. DRG – dorsal root ganglion) (C-Arm, Siemens AG, Germany).
Figure 2. C-arm guided DRG puncture (A for anteroposterior radiography, B for lateral radiography. DRG – dorsal root ganglion) (C-Arm, Siemens AG, Germany).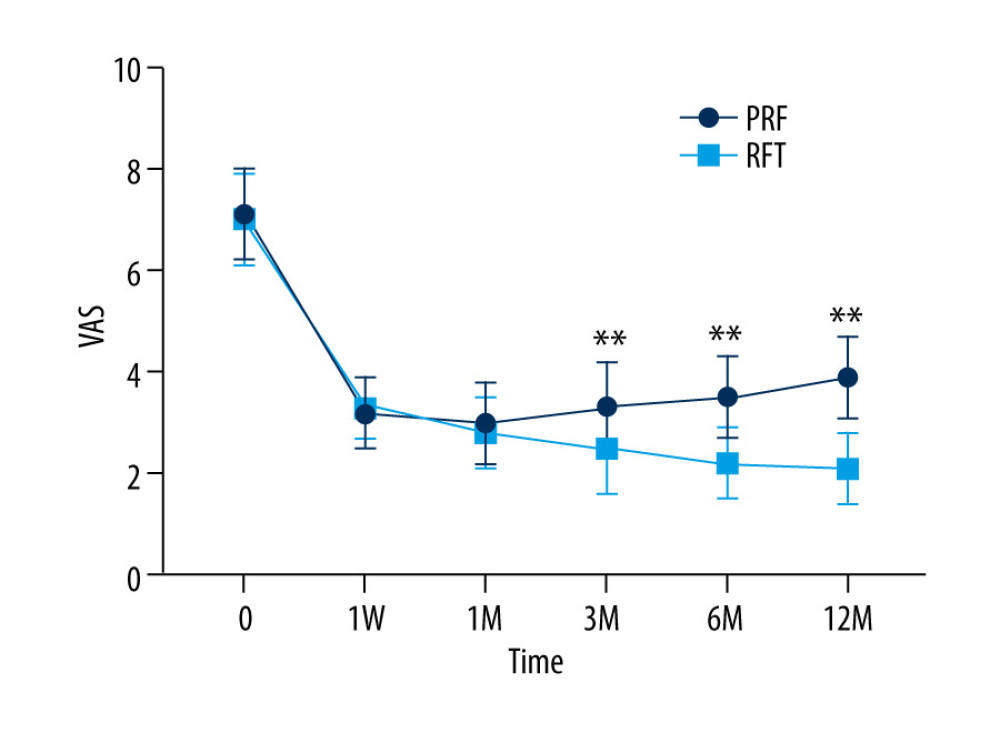 Figure 3. VAS score of RFT and PRF groups (** P<0.001, RFT vs PRF) (GraphPad Prism 8, GraphPad).
Figure 3. VAS score of RFT and PRF groups (** P<0.001, RFT vs PRF) (GraphPad Prism 8, GraphPad).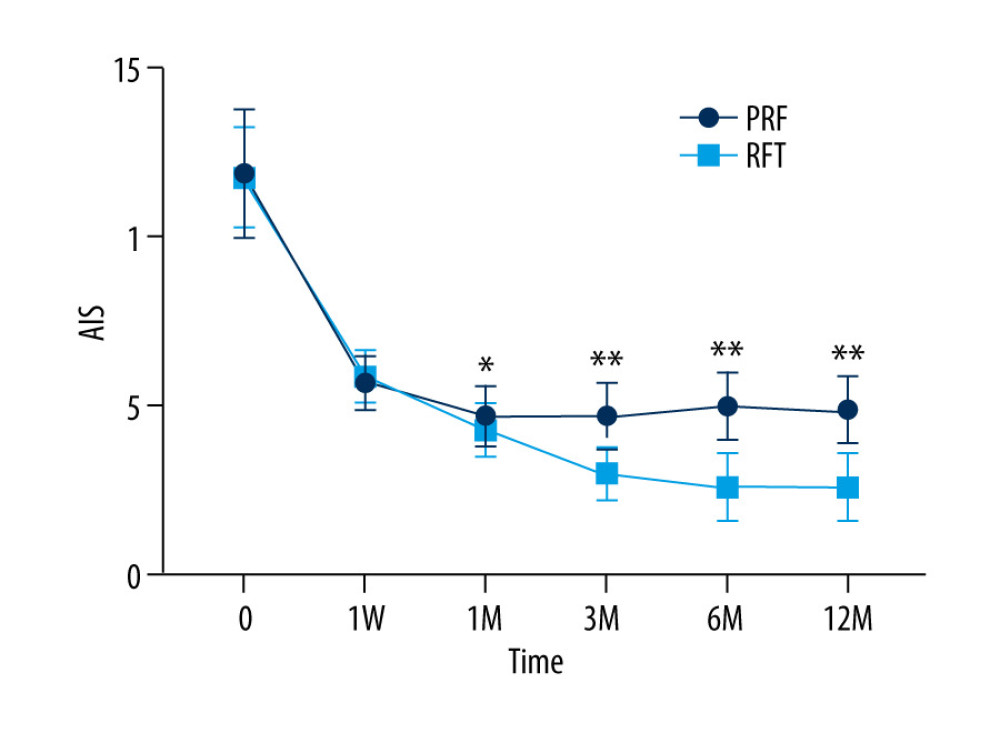 Figure 4. AIS in RFT and PRF groups (* P<0.05/** P<0.001, RF vs PRF) (GraphPad Prism 8, GraphPad).
Figure 4. AIS in RFT and PRF groups (* P<0.05/** P<0.001, RF vs PRF) (GraphPad Prism 8, GraphPad). Figure 5. GAD-7 (A) and PHQ-9 (B) of RFT and PRF groups (* P<0.05/** P<0.001, RF vs PRF) (GraphPad Prism 8, GraphPad).
Figure 5. GAD-7 (A) and PHQ-9 (B) of RFT and PRF groups (* P<0.05/** P<0.001, RF vs PRF) (GraphPad Prism 8, GraphPad). Tables
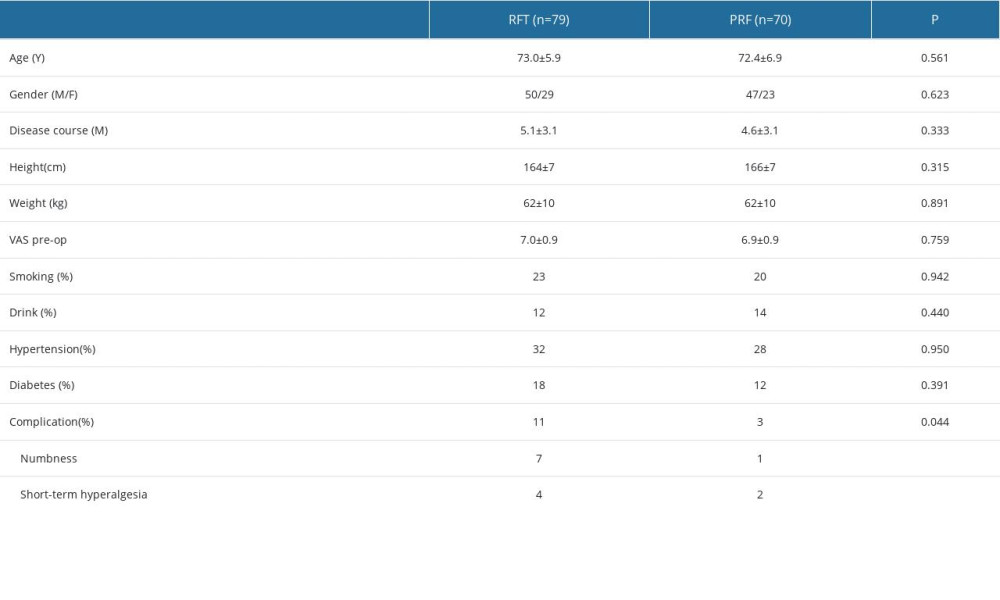 Table 1. General information about RFT and PRF groups.
Table 1. General information about RFT and PRF groups.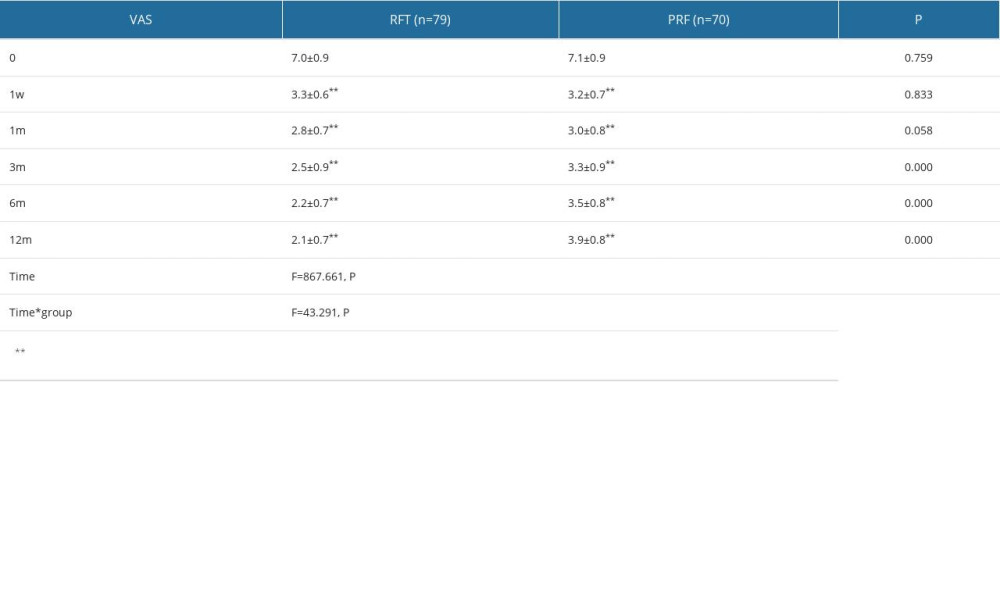 Table 2. VAS score of RFT and PRF groups.
Table 2. VAS score of RFT and PRF groups.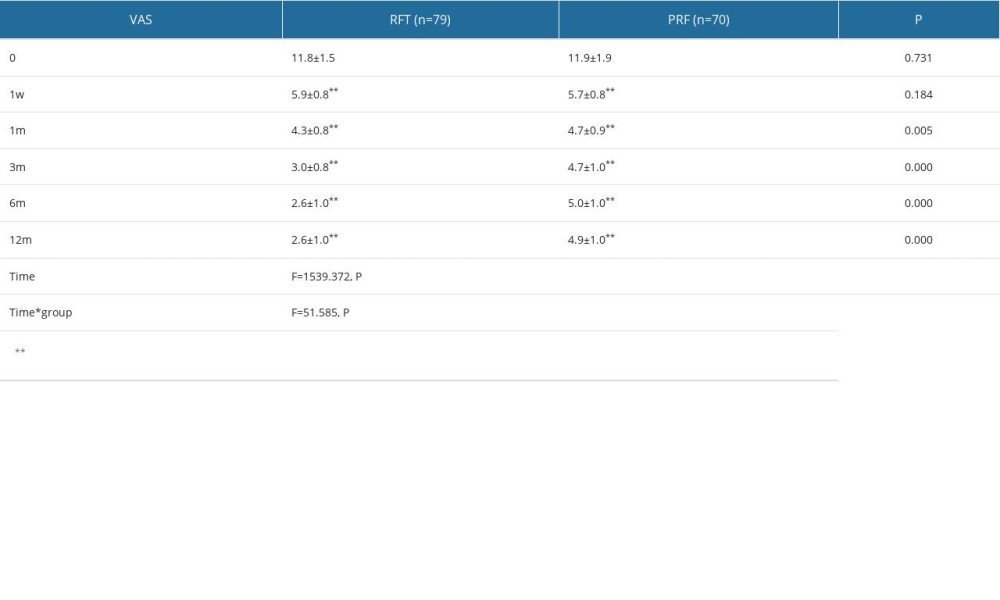 Table 3. Postoperative AIS in RFT and PRF groups.
Table 3. Postoperative AIS in RFT and PRF groups.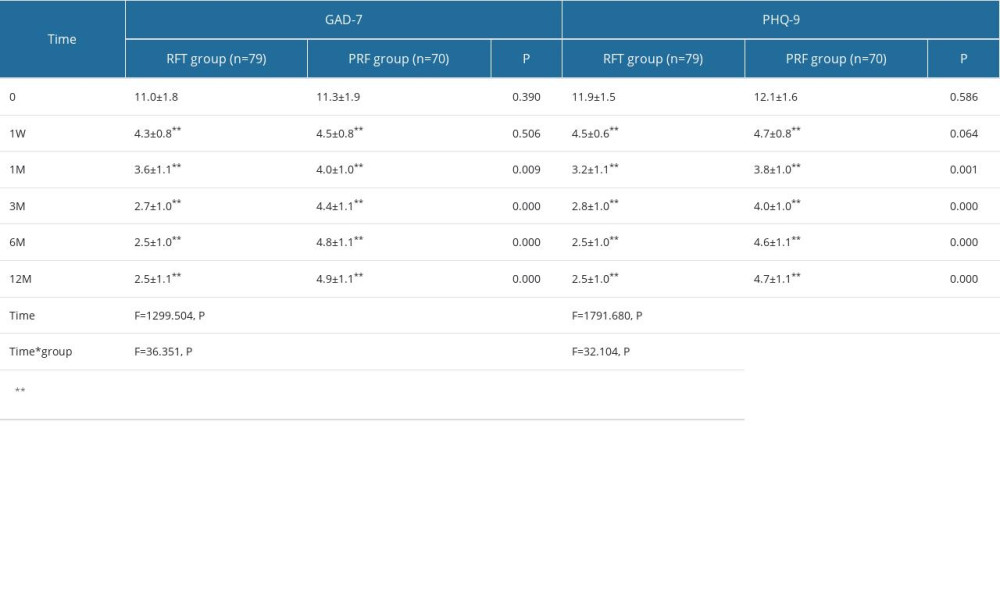 Table 4. GAD-7 and PHQ-9 of RFT and PRF groups.
Table 4. GAD-7 and PHQ-9 of RFT and PRF groups.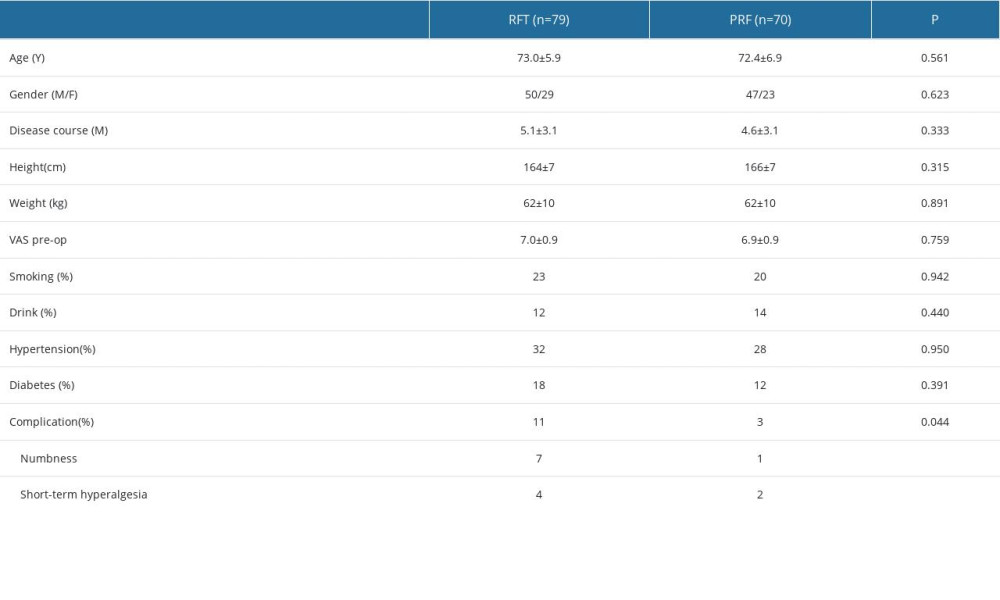 Table 1. General information about RFT and PRF groups.
Table 1. General information about RFT and PRF groups.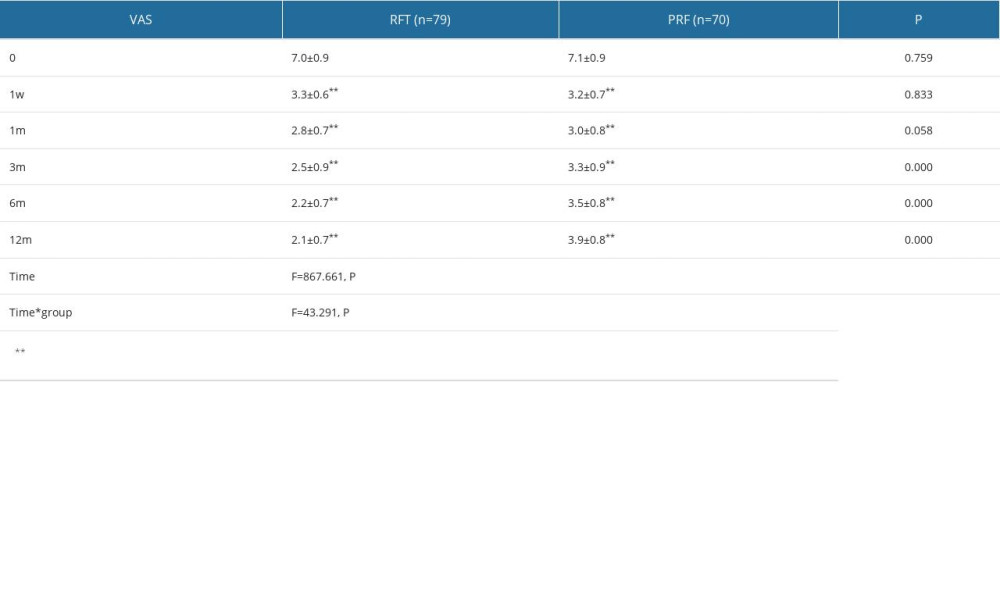 Table 2. VAS score of RFT and PRF groups.
Table 2. VAS score of RFT and PRF groups.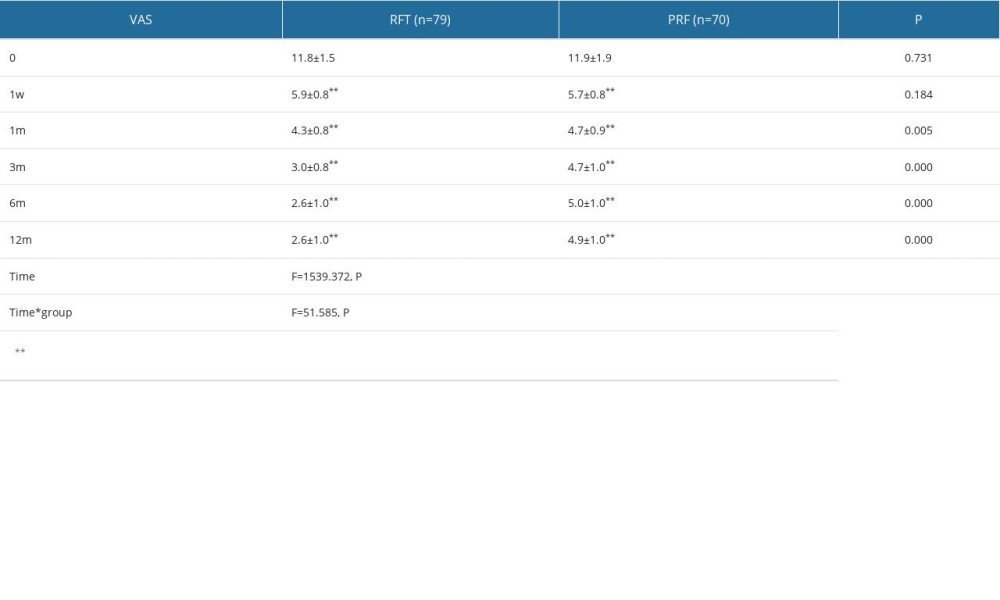 Table 3. Postoperative AIS in RFT and PRF groups.
Table 3. Postoperative AIS in RFT and PRF groups.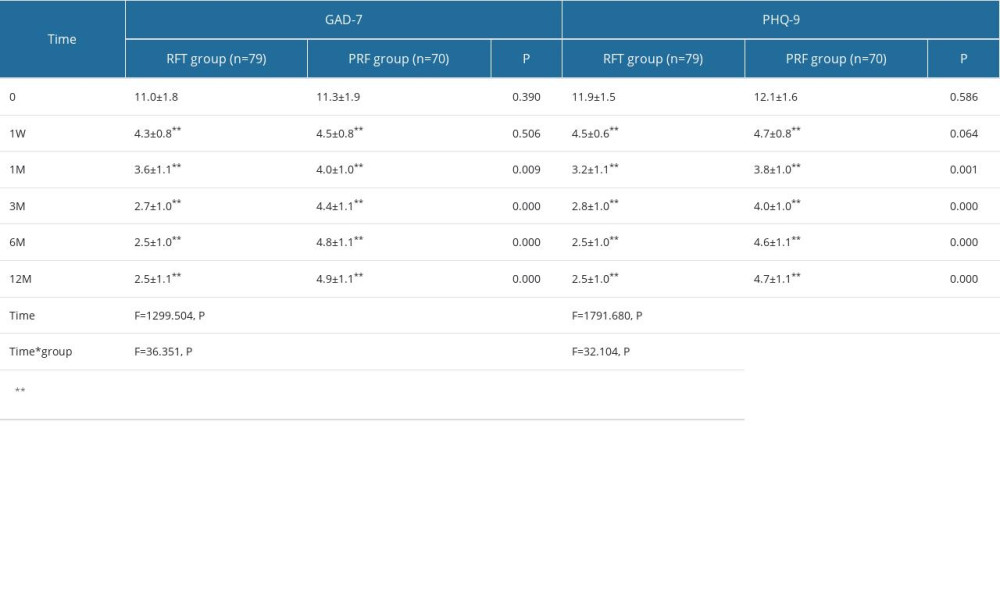 Table 4. GAD-7 and PHQ-9 of RFT and PRF groups.
Table 4. GAD-7 and PHQ-9 of RFT and PRF groups. In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








