20 January 2024: Clinical Research
Impact of Fluorodeoxyglucose-Positron Emission Tomography/Computed Tomography on Therapeutic Decisions and Radiotherapy Planning in Head and Neck Squamous Carcinoma: A Retrospective Study of 46 Patients
Anh Pham1ABDF*, Ildiko Garai2ADE, Kovács Árpád3A, Ádám Dér3DE, Erika Szanto3DE, Zsolt Hascsi2A, Ferenc Bátyi2B, Ervin Berényi2A, Thong Minh Pham1ADOI: 10.12659/MSM.942122
Med Sci Monit 2024; 30:e942122
Abstract
BACKGROUND: Positron emission tomography/computed tomography (PET/CT) using fluorodeoxyglucose (FDG) is essential in oncology for precise tumor delineation. This study evaluated FDG PET/CT’s impact on therapeutic decisions in head and neck cancer, comparing metabolic tumor volumes (MTV) measured by different methods with radiotherapy targets, crucial for treatment planning and patient outcomes.
MATERIAL AND METHODS: We retrospectively analyzed 46 patients with histologically confirmed head and neck cancer who underwent FDG PET/CT examination before radiotherapy. The mean age was 62 years (46-78 years). Then, we calculated MTV of the primary tumor or local recurrence using a local threshold of 41% of the standard uptake volume (SUV) corrected for lean body mass (SULmax) of the lesion and absolute threshold of SUV 2.5. Descriptive analysis of the recruited patients was assessed based on the clinical database (Medsol).
RESULTS: The study included 45 patients with squamous carcinoma and 1 with sarcoid cell carcinoma. PET/CT examination led to therapeutic decision changes in 11 cases. No significant difference was found in median values of Gross Tumor Volume (GTV) and MTV absolute (p=0.130). However, significant differences were observed in MTV local, MTV absolute, and GTV median values (p<0.001), with both MTVs showing significant correlation with GTV (p<0.01), especially MTV absolute (r=0.886).
CONCLUSIONS: FDG PET/CT examination prior to radiotherapy significantly influences therapeutic decisions in head and neck cancer patients. Based on our findings, the absolute threshold method (SUV: 2.5) appears to be an effective approach for calculating MTV for radiotherapy planning purposes.
Keywords: Head and Neck Neoplasms, Positron Emission Tomography Computed Tomography, Radiotherapy Planning, Computer-Assisted, Radiotherapy, Carcinoma, Squamous Cell, Positron-Emission Tomography
Background
According to global data in 2012, head and neck cancer is the 6th most common malignancy globally, accounting for 5% of total cancer [1]. Based on histological classification, squamous cell carcinoma is the most common type.
The management of head and neck cancer requires a complex multi-disciplinary approach, in which imaging for radiotherapy planning has an important role [2]. The intricate geometry and high radiation-associated toxicity of the head and neck make them excellent targets for conformal radiotherapy. Often, there are only a few millimeters separating the gross tumor volume (GTV) or the clinical target volume (CTV), which represents areas at high risk of microscopic illness, from important tissues such the optic nerve, spinal cord, brainstem, and salivary gland [3].
Curative radiation for head and neck cancer requires precise delineation of the primary tumor and the associated lymph nodes. Thus, one of the most important first steps toward better radiation therapy is improving tumor target volumes. At present, structural imaging techniques such as computed tomography and magnetic resonance imaging are considered the gold standard for tumor identification. MRI can provide additional information to help physicians detect soft tissue tumors and nodal diseases as it has superior soft tissue contrast resolution [4].
However, these techniques have several limitations such as poor contrast between tumor and normal tissues; or fail to detect the microscopic extent of the disease, as well as inability to detect metastatic lymph nodes of small size [5]. For these reasons, a visual method using fused PET/CT has been increasingly used and proved to perform better than CT or MRI in identifying tumor extension, nodal disease, and staging. The use of 2-deoxy-2-[fluorine-18]fluoro-D-glucose (18F-FDG), an analogue of glucose, in Positron Emission Tomography (PET) offers useful functional information based on the increased uptake of glucose and glycolysis of cancer cells. It also shows metabolic anomalies prior to morphological modifications. 18F-FDG PET/CT has an impact on the assessment of both newly diagnosed and previously treated patients with head and neck cancer [6]. When Syed, N Bomanji, N Nagabhushan et al. looked at the effects of combined FDG PET/CT on HNC in 24 patients, they found that PET/CT dramatically improved the confidence in disease localization of FGD-avid lesions by 51% and increased interobserver agreement [7]. Van den Wyngaert, Helsen N, Carp L, et al confirmed that FDG PET/CT can rule out residual neck illness, but its sensitivity is highly time-dependent, and this was shown 12 weeks following concurrent radiochemotherapy. In other words, PET/CT has a high sensitivity for detecting residual disease in patients who relapse up to 9 months after imaging, but its sensitivity is lower for individuals in whom residual disease was diagnosed up to twelve months after imaging (59.7%). The widely varying follow-up times in this significant finding may account for part of the heterogeneity observed in the literature now under publication [8]. Nevertheless, pre-therapeutic FDG PET/CT is currently only recommended to assess distant extension and/or to detect synchronous primary cancer (SPC) in advanced HNSCC and not in early-stage cancers [9]. The potential impact of FDG PET/CT on therapeutic decisions still remains largely unresolved.
Various methods to quantify tumor metabolic activity using 18 FDG PET/CT have been introduced. In these methods, metabolic tumor volume (MTV) delineation has been increasingly used and has been shown effective in many tumor types. However, the volumetric parameters of FDG PET/CT have not yet been added to the routine procedure in clinical practice. The main reason behind this is that the publication of an accurate and optimal segmentation method for quantifying the volumetric measurements of FDG PET/CT has not been established [10]. Therefore, this retrospective study of 46 patients with HNSCC at Department of Nuclear Medicine in Debrecen, Hungary aimed to evaluate the role of FDG PET on therapeutic decisions as well as to find the most suitable method to support radiotherapy treatment planning by measuring metabolic tumor volumes (MTV) using local threshold of 41% of SULmax and absolute threshold of SUV: 2.5 on FDG PET/CT images and make a comparison to radiotherapy target volumes (GTV).
Material and Methods
PATIENT SELECTION:
The study was conducted in accordance with the Declaration of Helsinki, and approved by the local Ethics Committee of the University of Debrecen (Ethical approval: H.0158-2019) for involving humans. Due to ethics approval of this retrospective trial, the requirement for separate patient consent was waived.
Patients who underwent a pre-therapeutic FDG PET/CT in Debrecen Nuclear Medicine Department were retrospectively included. They were enrolled between September 2019 and September 2020. These patients were candidates for radiotherapy treatment. All patients who underwent a whole body FDG PET/CT were diagnosed with head and neck cancer. Exclusion criteria included: previous resection of primary or nodal disease; prior radiotherapy to the head and neck district; other primary cancers. A detailed medical history of the patients was obtained. The clinical data recording included age, gender, histology, primary tumor site, indication for FDG PET/CT procedure, and presence of distant metastasis.
SCANNING PROTOCOL:
Patients with known or suspected head and neck cancer were scanned using Philips Gemini PET/CT machine. FDG PET/CT scan was done at the Department of Nuclear Medicine by using our standard procedure. All patients were instructed to be fasted for at least 4 hours (preferably 6 hours) prior to FDG injection. The patient’s blood glucose level was maintained below 200mg/dl. After 70 minutes of FDG injection, FDG PET/CT scan was performed.
TARGET VOLUME DEFINITION AND MARGINS:
The gross tumor volume (GTV) was delineated in Radiology department using data from clinical examination and imaging modalities. FDG PET/CT examination was done based on modified oncological protocol using the same position as later did. Scans were reviewed and analyzed by one researcher and a skilled oncology radiologist. During the evaluation, we used the threshold-based method: local threshold of 41%SULmax and absolute threshold of SUV2.5 to calculate MTV of the primary tumor and recurrent tumor (Figure 1).
STATISTICAL ANALYSIS:
Statistical analyses were performed using SPSS 19.0 statistical software. Descriptive analysis of the recruited patients was assessed based on clinical history from clinical database (Medsol). We used Shapiro-Wilk test to assess normality of the tumor volumes (GTV, MTVs). Later, we used Wilcoxon Signed Ranks test to compare median values of GTV, MTV measured by absolute threshold, and MTV measured by local threshold. Finally, we run a non-parametric Spearman’s rho correlation test to examine the monotonic relationship between paired data. The two-tailed P value was significant at the level <0.05.
Results
PATIENT CHARACTERISTICS:
The characteristics of the patients are shown in Table 1. There were total of 46 patients in our study population which was predominantly male, accounted for 95.65%. The number of female patients accounted for 4.35%. Mean age of patients was 62 years, ranging from 46 to 78 years (Table 1).
Oropharynx tumor, which made up 48%, was considerably the most common location of head and neck cancer in our study. Hypopharynx (26%) was slightly more common than oral cavity tumor, which made up 22%. Nasopharynx is the least common location, with 4%. Squamous carcinoma accounted for the majority of patients (97.8%) (Figure 2).
ROLE OF FDG PET/CT IN THERAPEUTIC DECISION CHANGING:
Following the results of FDG PET/CT scan, we found that there were changes in therapeutic decisions in 11/46 cases (24%). We discovered that in 64% of these patients, the tumor’s distant metastases required an alteration in treatment to systemic therapy. In 18% of cases, no viable primary tumor was found hence no irradiation was needed. In the last 18%, there was no obvious tumor in the primary site, however other sites were suspected. Treatment was changed to extended irradiation (Figure 3).
COMPARISON OF DIFFERENT IMAGE SEGMENTATION METHODS:
P value <0.05 showed a non-normal distribution in GTV, MTV_absolut and MTV_local. Wilcoxon Signed rank test was performed to compare the median values between GTV, MTV measured by absolute threshold of SUV2.5 and MTV measured by local threshold of SUL41%. P<0.05, we found significant differences between MTV_absolut threshold and MTV local threshold as well as between GTV and MTV_local. However, when we compared GTV and MTV_absolut value, P>0.05 showed that there was no significant different of median values btw GTV and MTV_absolut. Descriptive analysis was performed to measure mean, median, Std deviation, minimum, maximum and range value of GTV, MTV_aboslut and MTV_local. The median value measured by MTV_local was 27.2500, which was the smallest volume compared to tumor volumes delineated using other 2 methods. There were not many differences between median value measured by MTV_absolut (62.950) and GTV (59.8750). MTV_absolut is significant and showed a high correlation (p<0.001, r=0.885) with GTV. There is also a significant and high correlation between MTV_local and GTV (p<0.001, r=0.776) (Figures 4, 5).
Discussion
SUMMARY OF FINDINGS:
The patients in our study were those receiving radiotherapy for head and neck cancer. It was shown that a noteworthy proportion of patients had their treatment modified subsequent to FDG PET/CT scans (24%). The discovery of metastases led to an alteration in treatment to systemic therapy in 64% of these instances. Due to suspected other regions of concern, the therapy was altered for an additional 18% of patients to extended irradiation. Since the primary tumor could not be located in the remaining 18% of instances, no irradiation was necessary. This indicates that FDG PET/CT examination before radiotherapy does have an influence on radiotherapy treatment in head and neck cancer.
In the next part of our study, we measured MTV values of all patients using local threshold of 41%SULmax and absolute threshold of SUV2.5. We found that between MTV measured by local threshold (27.2500 cm3) and MTV measured by absolute threshold (62.950 cm3), the median value of MTV_absolut were much closer to the median value of GTV (66.3188 cm3) provided by radiotherapists. This indicated that MTV measured by absolute threshold was a better method to segment the tumor tissue. Until now, segmentation methods using local threshold of 41% SULmax and absolute threshold of SUV2.5 applied to calculate MTV value for head and neck cancer remain unclear.
In order to further examine the accuracy of these methods, Spearman’s rho correlation test was run to determine the association between data. Both MTV_absolut and MTV_local showed a significant (p<0.001) and high correlation (r=0.885 in MTV_absolut; r=0.776 in MTV_local) to GTV value. This suggested that volumetric parameters were reliable, even though the MTV values were consistently smaller than GTV values.
COMPARISON TO PREVIOUS STUDIES:
As far as we know, there are approximately 10% of patients who presents metastasis in head and neck cancer with an additional 20–30% of cases who will develop metastasis over the course of their disease [13]. In the majority of patients, distant metastatic diseases will be clinically silent. The tumor burden might be an important prognostic value. Many studies have shown the success of FDG PET/CT in detecting occult distant cancer. Syed, N Bomanji, N Nagabhushan et al. looked at the effects of combined FDG PET/CT on HNC in 24 patients, 18F-FDG-avid metastatic cervical lymph nodes were accurately detected in this investigation, 2 (22%) contralateral and 7 (78%) ipsilateral. Furthermore, 2 non-nodal metastases were found [7]. Goerres and colleagues showed distant metastases and secondary primary cancer were found in 24% of their patients who were newly diagnosed with squamous cell carcinoma of the oral cavity initially screened by clinical exam, CT, and chest x-ray [14]. Another study was run by Ha and colleagues which found that 31% of their patients had TNM modified after PET/CT scanning [15]. These results show a correlation to our result, emphasizing the ability to detect suspected primary cancer and distant metastasis. Moreover, various studies have demonstrated the ability of PET/CT to detect residual lesions as well as recurrent cancer with high specificities, ranging from 92% to 97%. This method was much more reliable compared to conventional imaging [16]. Therefore, FDG PET/CT is a helpful method for monitoring treatment response in head and neck cancer.
Results from previous studies demonstrate that MTV was computed using a maximum percentage threshold of 40–50%. Moreover, other studies used a fixed SUV threshold, most commonly SUV2.5, where SUV>2.5 is the absolute threshold (MTV2.5) for tumors. This method was identified as a reasonable decision in several prior studies. However, these studies only claimed a high correlation to other cancer types such as cervical cancer, pancreatic cancer or small cell lung carcinoma [17]. As a result, we hypothesized that the 41% of SULmax and absolute threshold of SUV2.5 would be reliable and provide an accurate MTV value. This would be an independent prognostic factor in head and neck cancer. Ha and colleagues also demonstrated that the GTV was consistently larger than the MTV because it contained the entirety of the visualized disease when using CT whereas they assigned a 50% threshold of maximum SUV for the semi-automated delineation of the MTV [15]. GTV included both the primary tumor and involved lymph nodes and these values were highly correlated with MTV. The correlation coefficient was 0.73 (p<0.001). Chung M.K et al also used SUV 2.5 as the method to segment pharyngeal tumors and a positive correlation between SUV2.5 and GTV was identified with Spearman correlation coefficient 0.621 and P<0.001 [18]. The positive correlation they found was shown not as strong as the correlation between SUV2.5 and GTV in our method (r=0.885). This might be due to their patient’s selection including the heterogeneity of treatment modalities with a longer period of time to follow up. Nevertheless, their investigation showed concordance with the result of our study and has further strengthened the validity of our methods.
LIMITATIONS OF THE STUDY:
We are aware that our research might have some limitations, including the retrospective nature of our study design, the heterogeneity of primary tumor location, the small sample size of the patients, and the inability to follow up. An additional source of error was that the procedure to measure the tumor volumes was executed in 2 different departments. GTV values were provided by radiotherapists in Radiology department while MTV values were calculated in the Nuclear Medicine Department. The ideal procedure would be to measure both these tumor volumes with the same software program. Despite these difficulties, we have found further evidence to support the usage of FDG PET/CT to diagnose and perform treatment planning in head and neck cancer patients. Moreover, we revealed highly significant results which demonstrated the correlation between the methods to calculate MTV using local threshold of 41% SULmax, absolute threshold of SUV2.5 and the GTV value obtained from clinical examination and anatomical imaging. After the detailing assessment, we believe that MTV measured by absolute threshold will be better than MTV measured by local threshold to segment the tumor tissue. Analyses with larger numbers of cases and with a period of follow-up in prospective trials are required to confirm the reliability of MTV in predicting outcomes and to test the validity of the present study are necessary.
Conclusions
In conclusion, FDG PET/CT examination before radiotherapy has a great influence on therapeutic decisions in head and neck cancer patients. MTV values calculated by different threshold methods show a correlation with GTV. Especially, MTV_absolute at threshold 2.5 seems to be a more suitable and simple segmentation method that provides metabolic data for radiotherapy planning. We suggest applying MTV_absolut at threshold 2.5 in standard clinical practice for radiotherapy treatment planning in head and neck cancer.
Figures
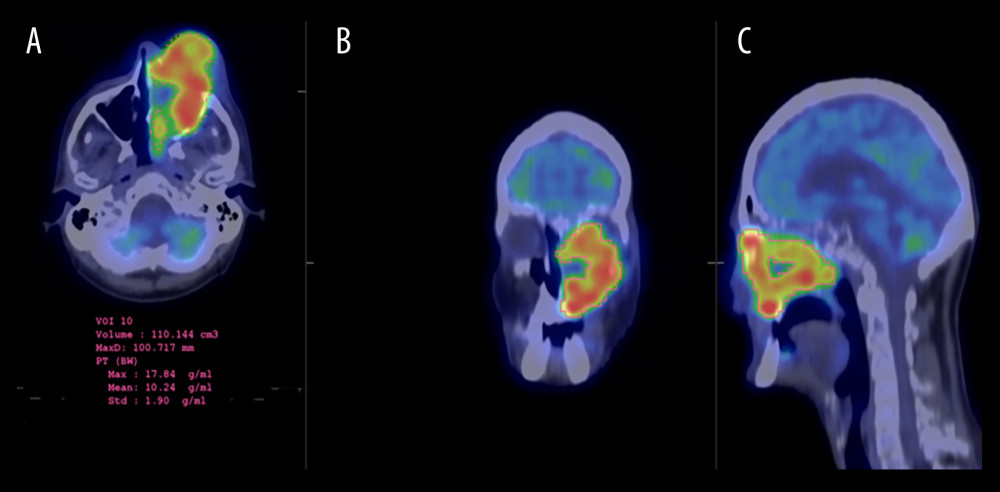 Figure 1. 49 y/o patient with squamous cell carcinoma of the left nasal cavity and nasopharynx. Tumor target delineation using local threshold of 41% of the standard uptake volume (SUV) corrected for lean body mass (SULmax) of the lesion and absolute threshold of SUV2.5 was done on 18F-FDG PET/CT scan. Absolute threshold of SUV 2.5 delineation is seen on axial (A) coronal (B) and sagittal (C) fused PET/CT images with 270.5 ccm3.
Figure 1. 49 y/o patient with squamous cell carcinoma of the left nasal cavity and nasopharynx. Tumor target delineation using local threshold of 41% of the standard uptake volume (SUV) corrected for lean body mass (SULmax) of the lesion and absolute threshold of SUV2.5 was done on 18F-FDG PET/CT scan. Absolute threshold of SUV 2.5 delineation is seen on axial (A) coronal (B) and sagittal (C) fused PET/CT images with 270.5 ccm3. 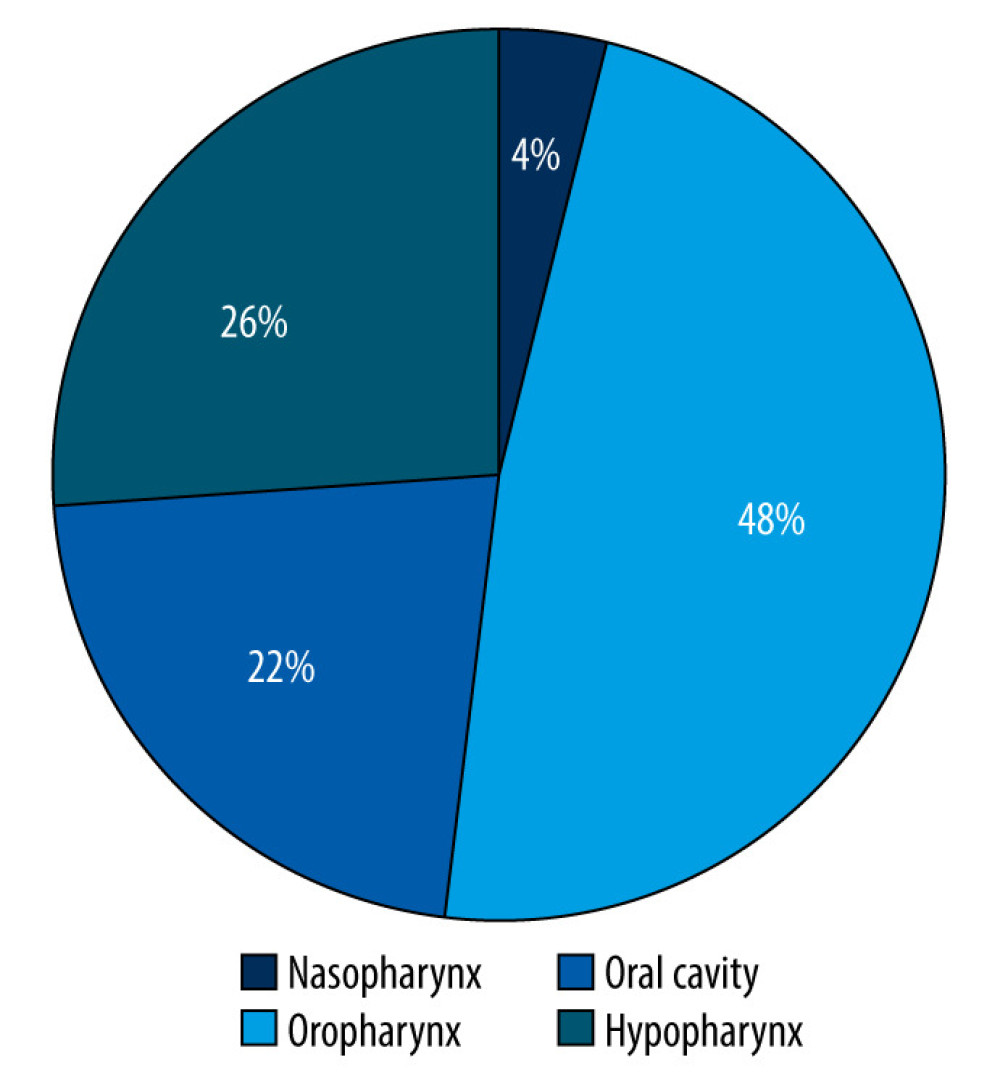 Figure 2. Primary locations of head and neck cancer in the study population.
Figure 2. Primary locations of head and neck cancer in the study population. 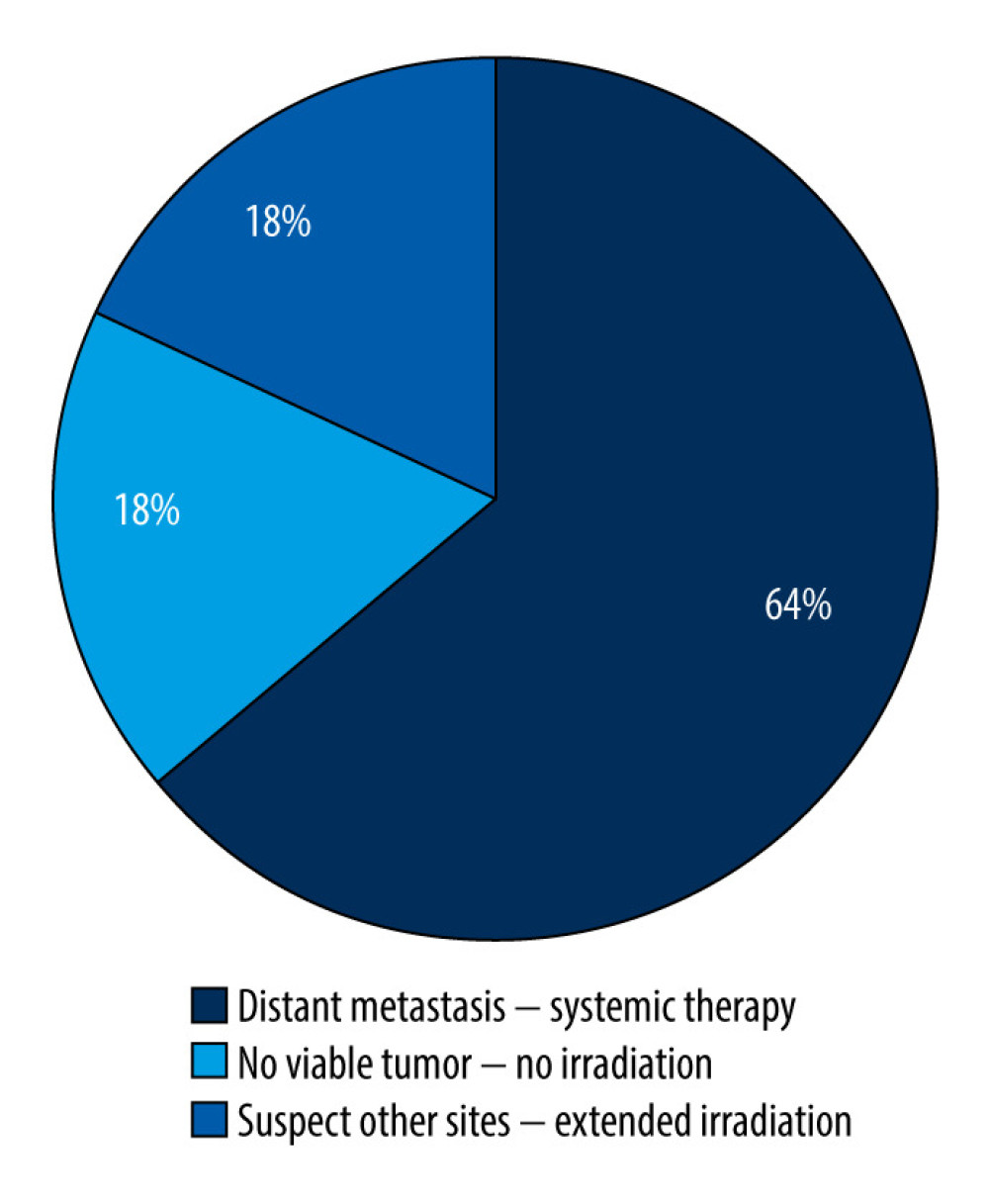 Figure 3. Reasons for therapeutic changes.
Figure 3. Reasons for therapeutic changes. 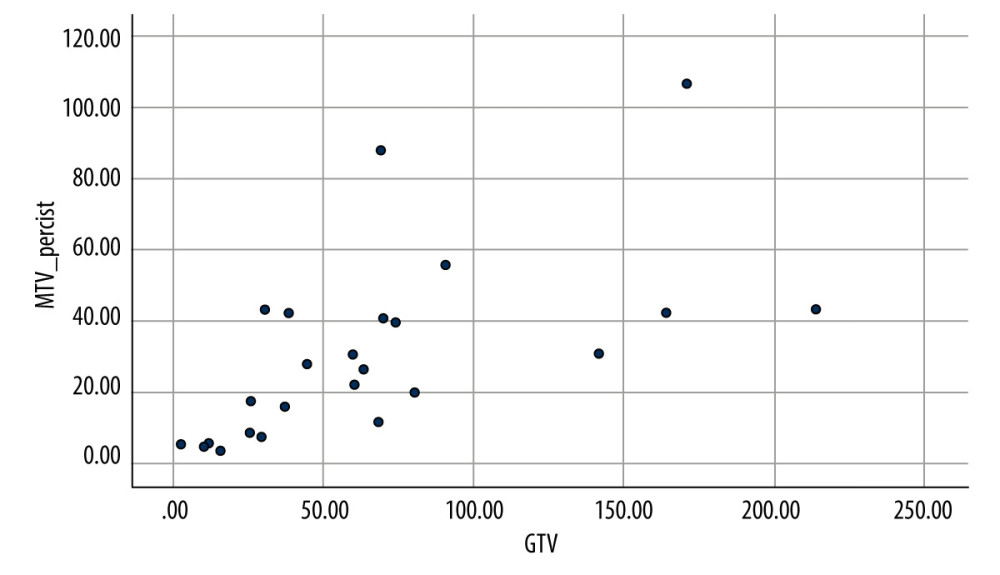 Figure 4. Correlation between Gross Tumor Volume (GTV) (x) and Metabolic Tumor Volume (MTV) absolute threshold of SUV2.5 (y).
Figure 4. Correlation between Gross Tumor Volume (GTV) (x) and Metabolic Tumor Volume (MTV) absolute threshold of SUV2.5 (y). 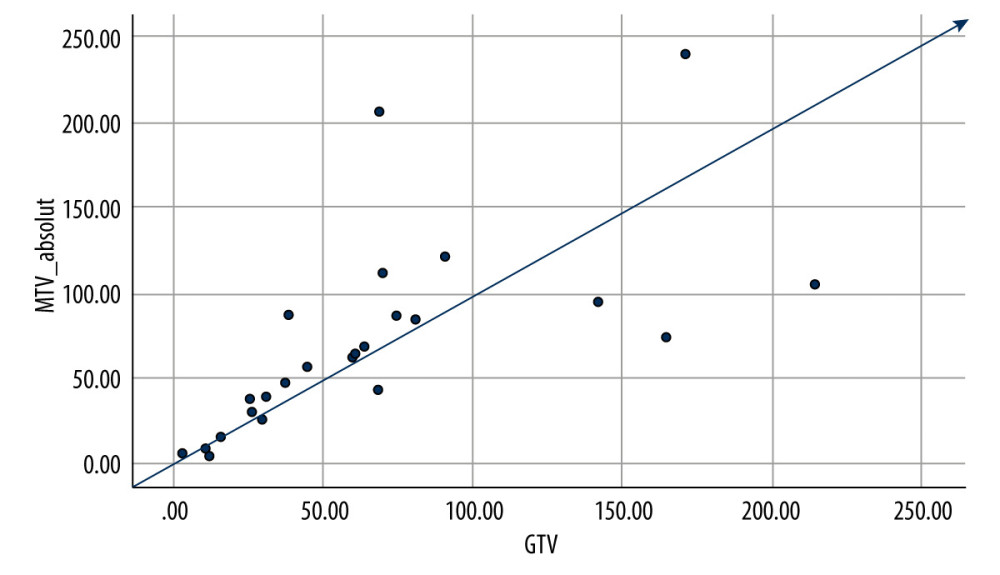 Figure 5. Correlation between Gross Tumor Volume (GTV) (x) and Metabolic Tumor Volume (MTV) local threshold of 41% SULmax (y).
Figure 5. Correlation between Gross Tumor Volume (GTV) (x) and Metabolic Tumor Volume (MTV) local threshold of 41% SULmax (y). References
1. Torre LA, Bray F, Siegel RL, Ferlay J, Global cancer statistics, 2012: Cancer J Clin, 2015; 65(2); 87-108
2. Schwartz DL, Garden AS, Thomas J, Adaptive radiotherapy for head-and-neck cancer: Initial clinical outcomes from a prospective trial: Int J Radiat Oncol Biol Phys, 2012; 83(3); 986-93
3. Nuyts S, Defining the target for radiotherapy of head and neck cancer: Cancer Imaging , 2007; 7(Spec No A(Special issue A)); S50-55
4. Pedraza S, Ruiz-Alonso A, Hernández-Martínez AC, 18F-FDG PET/CT in staging and delineation of radiotherapy volume for head and neck cancer: Rev Esp Med Nucl Imagen Mol (Engl Ed), 2019; 38(3); 154-59
5. International Atomic Energy Agency (IAEA): The role of PET/CT in radiation treatment planning for cancer patient treatment. October, 2008; 86-97
6. Almuhaideb A, Papathanasiou N, Bomanji J, 18 F-FDG PET/CT imaging in oncology: Ann Saudi Med, 2011; 31(1); 3-13
7. Syed R, Bomanji JB, Nagabhushan N, Impact of combined 18F-FDG PET/CT in head and neck tumours: Br J Cancer, 2005; 92(6); 1046-50
8. Van den Wyngaert T, Helsen N, Carp L, Fluorodeoxyglucose-positron emission tomography/computed tomography after concurrent chemoradiotherapy in locally advanced head-and-neck squamous cell cancer: The ECLYPS study: J Clin Oncol, 2017; 35(30); 3458-64
9. Leclere JC, Delcroix O, Rousset J, Integration of 18-FDG PET/CT in the initial work-up to stage head and neck cancer: Prognostic significance and impact on therapeutic decision making: Front Med (Lausanne), 2020; 7; 273
10. Im HJ, Bradshaw T, Solaiyappan M, Cho SY, Current methods to define metabolic tumor volume in positron emission tomography: Which one is better: Nucl Med Mol Imaging, 2018; 52(1); 5-15
11. Al-Ibraheem A, Buck A, Krause BJ, Clinical applications of FDG PET and PET/CT in head and neck cancer: J Oncol, 2009; 2009; 208725
12. Buck AK, Herrmann K, Stargardt T, Economic evaluation of PET and PET/CT in oncology: Evidence and methodologic approaches: J Nucl Med Technol, 2010; 38(1); 6-17
13. Pisani P, Airoldi M, Allais A, Metastatic disease in head & neck oncology: Acta Otorhinolaryngol Ital, 2020; 40(Suppl 1); S1-S86
14. Goerres GW, Schmid DT, Grätz KW, von Schulthess GK, Eyrich GK, Impact of whole body positron emission tomography on initial staging and therapy in patients with squamous cell carcinoma of the oral cavity: Oral Oncol, 2003; 39(6); 547-51
15. La TH, Filion EJ, Turnbull BB, Metabolic tumor volume predicts for recurrence and death in head-and-neck cancer: Int J Radiat Oncol Biol Phys, 2009; 74(5); 1335-41
16. Ryan WR, Fee WE, Le QT, Pinto HA, Positron-emission tomography for surveillance of head and neck cancer: Laryngoscope, 2005; 115(4); 645-50
17. Ma W, Wang M, Li X, Quantitative 18F-FDG PET analysis in survival rate prediction of patients with non-small cell lung cancer: Oncol Lett, 2018; 16(4); 4129-36
18. Chung MK, Jeong HS, Park SG, Metabolic tumor volume of [18F]-fluorodeoxyglucose positron emission tomography/computed tomography predicts short-term outcome to radiotherapy with or without chemotherapy in pharyngeal cancer: Clin Cancer Res, 2009; 15(18); 5861-68
Figures
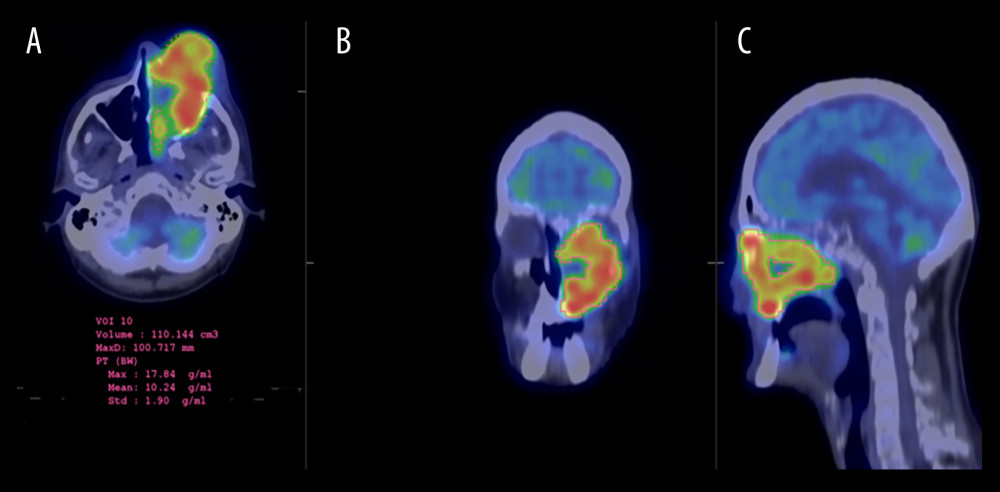 Figure 1. 49 y/o patient with squamous cell carcinoma of the left nasal cavity and nasopharynx. Tumor target delineation using local threshold of 41% of the standard uptake volume (SUV) corrected for lean body mass (SULmax) of the lesion and absolute threshold of SUV2.5 was done on 18F-FDG PET/CT scan. Absolute threshold of SUV 2.5 delineation is seen on axial (A) coronal (B) and sagittal (C) fused PET/CT images with 270.5 ccm3.
Figure 1. 49 y/o patient with squamous cell carcinoma of the left nasal cavity and nasopharynx. Tumor target delineation using local threshold of 41% of the standard uptake volume (SUV) corrected for lean body mass (SULmax) of the lesion and absolute threshold of SUV2.5 was done on 18F-FDG PET/CT scan. Absolute threshold of SUV 2.5 delineation is seen on axial (A) coronal (B) and sagittal (C) fused PET/CT images with 270.5 ccm3.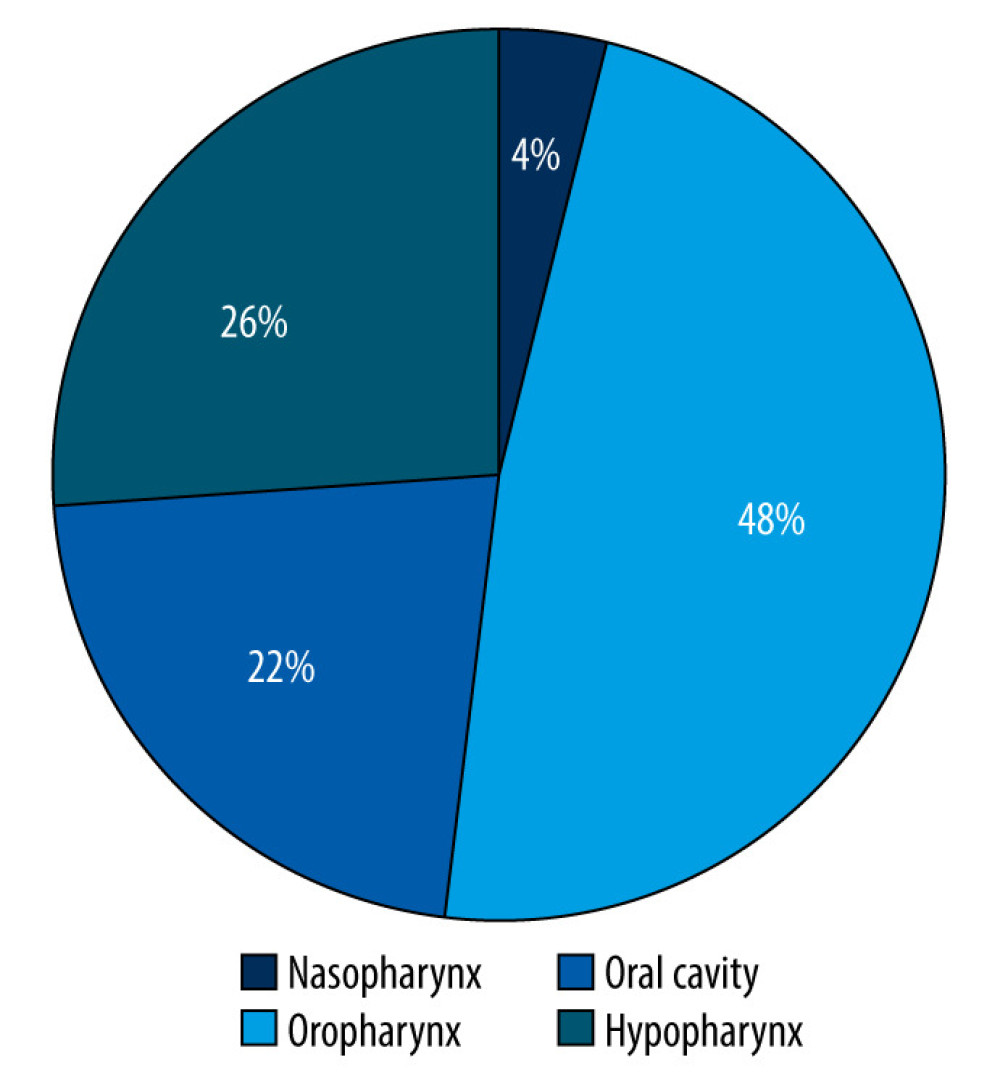 Figure 2. Primary locations of head and neck cancer in the study population.
Figure 2. Primary locations of head and neck cancer in the study population.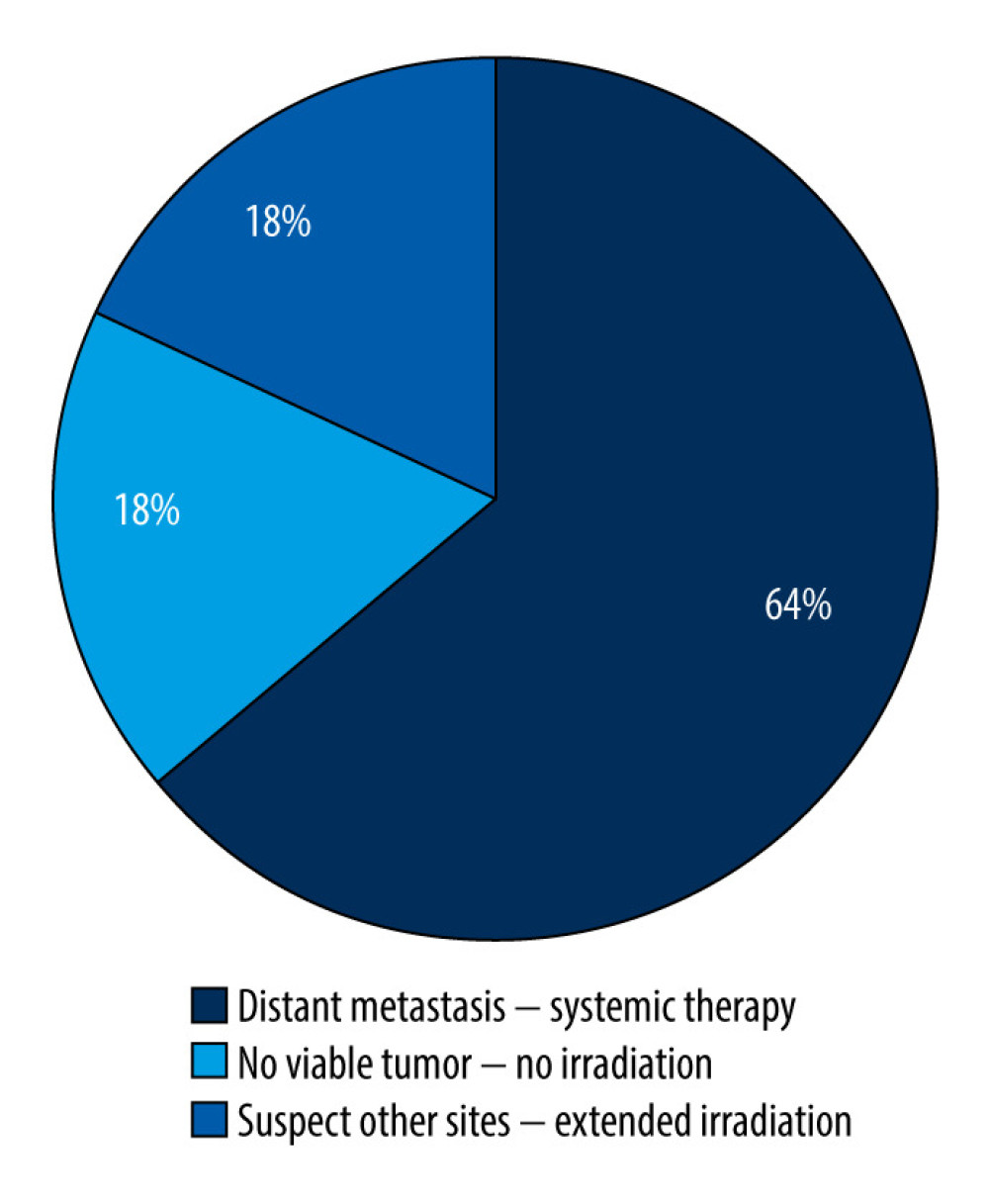 Figure 3. Reasons for therapeutic changes.
Figure 3. Reasons for therapeutic changes.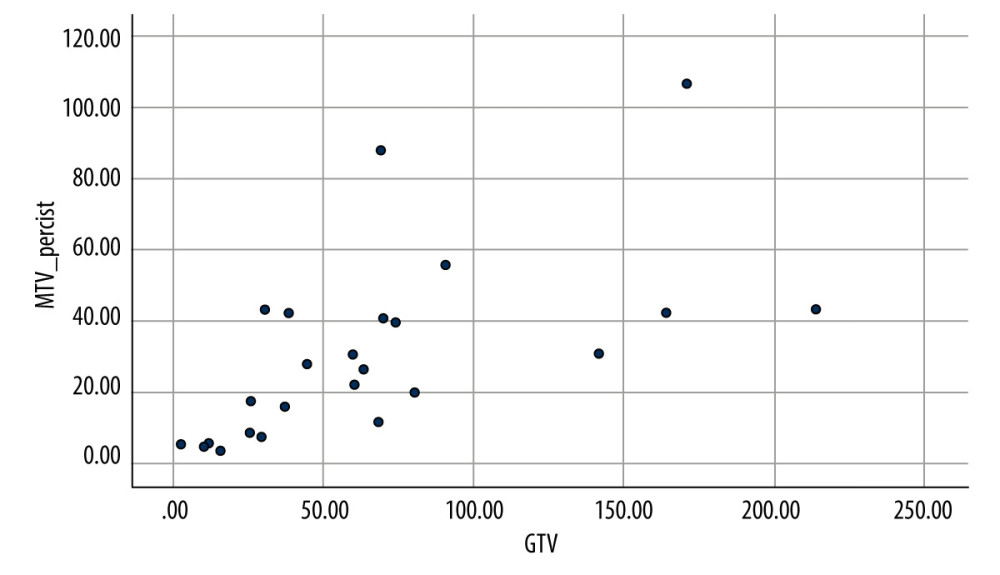 Figure 4. Correlation between Gross Tumor Volume (GTV) (x) and Metabolic Tumor Volume (MTV) absolute threshold of SUV2.5 (y).
Figure 4. Correlation between Gross Tumor Volume (GTV) (x) and Metabolic Tumor Volume (MTV) absolute threshold of SUV2.5 (y).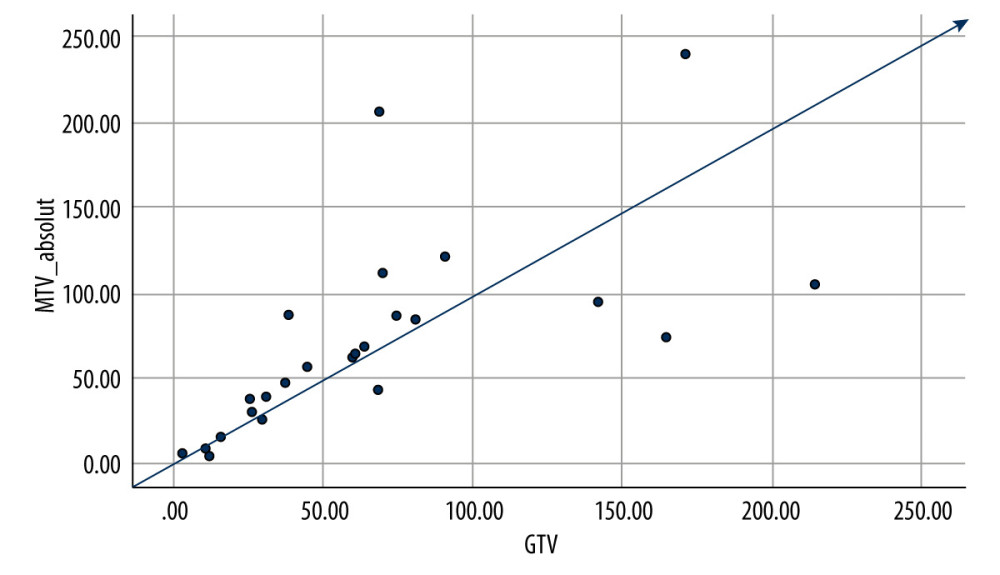 Figure 5. Correlation between Gross Tumor Volume (GTV) (x) and Metabolic Tumor Volume (MTV) local threshold of 41% SULmax (y).
Figure 5. Correlation between Gross Tumor Volume (GTV) (x) and Metabolic Tumor Volume (MTV) local threshold of 41% SULmax (y). In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952









