23 December 2023: Clinical Research
Assessment of Sleeping Disorders, Characteristics, and Sleeping Medication Use Among Pharmacy Students in Saudi Arabia: A Cross-Sectional Quantitative Study
Wajid SyedDOI: 10.12659/MSM.942147
Med Sci Monit 2023; 29:e942147
Abstract
BACKGROUND: Insomnia is a growing problem, especially among university students, and is associated with sleep disorders, poor academic performance, and quality of sleep. The purpose of this study was to assess the prevalence of insomnia sleeping characteristics, managing techniques, and attitudes toward sleeping pill usage among pharmacy students.
MATERIAL AND METHODS: A cross-sectional web-based study was conducted among pharmacy students of King Saud University, College of Pharmacy, Riyadh, Saudi Arabia between February and March 2023. SPSS version 26 was used for data analysis. A P value of <0.05 and was considered statistically significant.
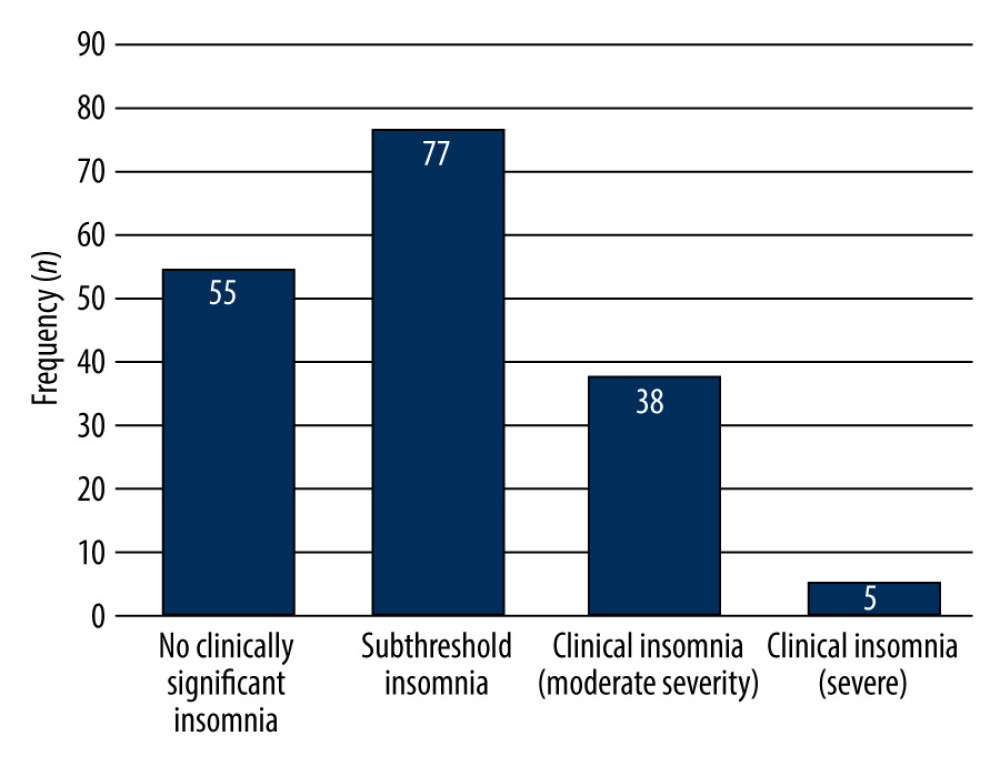
RESULTS: In this study, 61.7% (n=108) of the students’ slept an average of 6-10 h and 35.4% (n=62) slept an average of 6 h. Regarding sleeping patterns, nearly two-thirds (n=112, 64%) of the students had day and night sleeping patterns while more than one-third (n=63, 36%) had only night sleeping patterns. In this study, 2.9% (n=5) of the students had severe clinical insomnia, while 21.7% (n=38) reported moderately severe clinical insomnia, 44% (n=77) of them had subthreshold insomnia, and 31.4% (n= 55) had no clinically significant insomnia. The mean scores of the insomnia severity index were significantly related to the usage of stimulants (P=0.048), average hours of sleep (P=0.0001), and average minutes needed to fall asleep (P=0.0001).
CONCLUSIONS: The current findings demonstrated varying levels of insomnia among students, yet few students used sleeping pills.
Keywords: Acetaminophen, Narcolepsy 1, Problem-Based Learning, Sleep Initiation and Maintenance Disorders, sleep quality
Background
There is a strong relationship between sleep quality and mental health [1]. Lack of sleep is linked to various neurological disorders, restless legs syndrome, and obstructive sleep apnea [2]. According to the National Institute of Neurologic Disorders and Stroke, sleep is a sedentary state of mind; more broadly, it is a state of altered consciousness with comparatively reduced sensory muscle activity, and diminished interactions with the environment [3]. Furthermore, it is known that during the process of sleeping, the ability to respond to stimuli is lessened compared to alertness, although it is still more responsive than in a coma or other diseases of consciousness [3].
According to the literature, individuals in their daily routine spend one-third of their time in sleeping, and sleep is an important phenomenon in everyone’s life, comparable to food and water [3]. Sleep deprivation can hurt many organs in the human body, including the brain, heart, lungs, and metabolism. Additionally, the literature suggests that sleep deprivation affects immunity, disease resistance, and mood [3]. The problem of insomnia is not limited to adults and the elderly, as it is now more common among young university students [4]. For instance, a previous study among medical students reported a prevalence of 23.1% of hypersomnia, and 18.3% of the students reported insomnia [4]. Similarly, another study revealed that 54.7% of students obtained less than 7 h of sleep at night during a typical school week, while 81.7% of students did not sleep on the night before an examination [5]. Furthermore, various factors were found to be associated with sleep disorders, including gender, obesity, and poor academic performance [4].
In the context of academia, undergraduates can experience high levels of struggle in their everyday activities due to a variety of factors such as the high level of subjective content to be learned, practicals and theoretical classes, grades, presentations, and quizzes, which all need to completed in relatively short periods, which sometimes cause the students to worry about their education, which can lead to disturbed sleep and anxiety [6]. Previous findings demonstrated that students have high stress levels due to frequent exams, presentations, and heavy academic load, which also significantly contribute to inadequate sleep [6,7]. Furthermore, students with higher stress levels may get less sleep than recommended [7]. Many studies reported that undergraduates had suboptimal durations of sleep, and many studies reported that students got fewer than 7 h of sleep [7–10]. Poor sleep affects cognitive ability and hurts academic performance [7–12], and interferes with concentration on education, which can affect a student’s grades and quality of life [12].
According to the literature, academic load, student attitudes, individual stressful situations, and habits such as excessive use of the internet and social media were more common among young adults and students, resulting in poor sleep quality [4,5,7]. Other studies have found that educational structure and curricula, as well as cultural, personal, and lifestyle factors, can all have an impact on students’ sleep quality [7]. Furthermore, besides the educational stress, many students smoke tobacco, abuse drugs, and consume caffeine, energy drinks, and stimulants [13], which can be associated with poor sleeping habits [7]. However, it is difficult to extrapolate this information to all health profession students, including pharmacy students, both nationally and internationally [5–7]. Therefore, the present study was performed to assess the prevalence of insomnia sleeping characteristics, managing techniques, and attitudes toward sleeping pill use among pharmacy students at KSU in Riyadh, Saudi Arabia.
Material and Methods
SAMPLE SIZE:
The sample size was calculated using a web-based tool (http://www.raosoft.com/samplesize.html) that has been used in prior studies [15–20]. Around 300 senior students were enrolled in the College of Pharmacy on the KSU campus. The required sample size of 162 was obtained by assuming a 5% non-response rate, 95% confidence intervals (CI), and a 5% margin of error (ME). Nonetheless, to improve dependability, we eventually enrolled 180 students in our study.
AN INSTRUMENT FOR DATA COLLECTION:
The questionnaire aimed to assess the prevalence of insomnia and attitudes toward sleeping pill use among pharmacy students was adopted from similar studies published elsewhere [4,8,21] and grouped into sections and coded as follows. Demographic characteristics of the undergraduates, including age, gender, parent’s monthly household income, year of study, physical activity, smoking status, and use of stimulants. The second part of the study deals with the sleeping pattern and its related information, with 4 items: average hours of sleep, average time needed to fall asleep, sleeping pattern, and sleep quality. The third part of the study deals with the assessment of insomnia severity among students, with a total of 7 items. For example, how difficult falling asleep and staying asleep are. All these questionnaires were measured on a five-point scale of 0 to 4, where 0 indicates none or not much noticeable, while 4 indicates very severe or very noticeable\very dissatisfied. The last part of the study deals with the attitudes of students toward use of sleeping pills.
Following the completion of the final questionnaire drafts, 2 professionals in the field – a researcher from a clinical pharmacy and an academician from a medical college – provided independent feedback on the questions’ suitability to evaluate the questionnaire’s validity. Subsequently, a pilot study was carried out with a randomly chosen sample of students (n=20) to verify the conceptual and linguistic comprehension of the questions as well as the projected time needed to finish the survey. The questionnaire’s reliability was evaluated using Cronbach’s alpha coefficient, which yielded a score of 0.76.
The data collection was carried out online as a Google form in English language and took approximately 15 min to complete. To participate in the study, an invitation with a questionnaire link was sent to undergraduates from a mailing list or to their mobile phone number, which was obtained from the group leader before the start of the study. The study’s objectives were clearly stated, and participation was entirely optional by simply clicking on the link. Students who agreed to participate by filling out the questionnaire were included, while undergraduates who refused to participate and did not finish the surveys were excluded from the study.
The insomnia score was calculated and further divided according to the severity. All 7 questions for assessing the insomnia severity were given a score according to students’ answers to each question. For example, for the question about difficulty falling asleep, students who answered ‘none’ were given a score of ‘0’, while mild was given a score of ‘1’ and moderate, severe, and very severe were given a score of ‘2’, ‘3’, and ‘4’, respectively. To calculate the total insomnia score, alle scores for the 7 insomnia items were computed together. The overall score was further classified as no clinically significant insomnia (0–7, subthreshold insomnia (8–14), clinical insomnia of moderate severity (15–21), or severe insomnia (22–28) [22].
DATA ANALYSIS:
Students’ responses were evaluated, categorical data were described using frequencies (
Results
CHARACTERISTICS OF STUDENTS:
One hundred and seventy-five (n=175) students completed the survey. Table 1 shows the socio-demographic characteristics of the students. Most of the students were male (n=124, 70.9%) and aged 18–25 years (98.3%, n=172) and third-year students (n=90, 51.4%), followed fourth-year students (n=85, 48.6%). Most students (n=149, 85.1%) wer nonsmokers and almost half exercised daily. A large proportion of the students (n=158. 90.3%) did not use any stimulants.
QUALITY OF SLEEP:
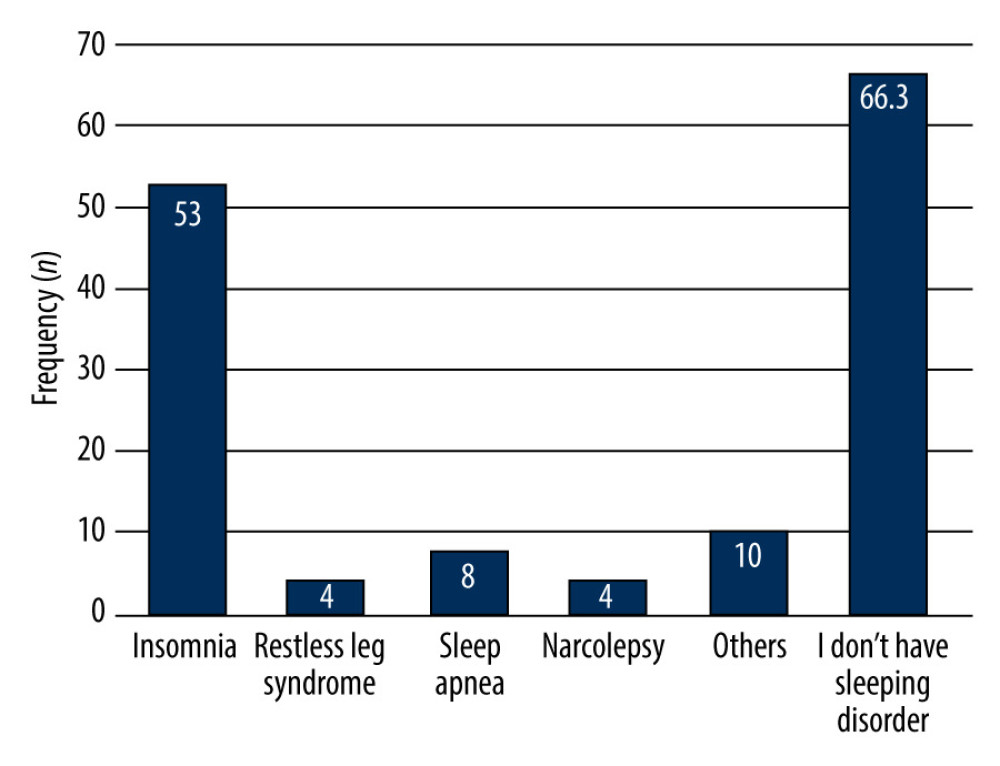
About two-thirds of the students (n=108, 61.7%) slept 6–10 h per night, followed by <6 h per night (n=62, 35.4%). Slightly under half of students (n= 79, 45.1%) needed 10–20 min to fall asleep. Regarding sleeping patterns, more than two-thirds (n=112, 64%) of the students had day and night sleeping patterns, while more than one-third (n=63, 36%) had only night sleeping patterns. In this study, 74.3% (n=130) of the students had good or excellent sleep quality, while 25.7% (n=45) of the students reported having poor sleep quality, over one-third of the students (n=60, 34.3%) needed a moderate amount of time to fall asleep, and 12.5% (n=23) had severe or very severe problem of falling asleep. Furthermore, 28.7% (n=52) of students had moderate difficulty in staying asleep, while 9.7% (n=17) had severe or very severe difficulty staying asleep. We found that 32% (n=56) of the students have severe or very severe problems staying asleep and woke up too early. Details on the quality of sleep of the students can be found in Table 2. In this study, the most common sleeping disorder among students was insomnia (n=53, 30.3%), followed by other sleeping disorders (n=10, 5.7%), sleep apnea (n=8, 4.6%), restless legs syndrome (n=4; 2.3%), and narcolepsy (n=4, 2.3%). Detailed information is shown in Figure 1.
SLEEP PATTERN SATISFACTION:
In terms of satisfaction, the majority of students (n= 59, 33.7%) were moderately satisfied with their sleeping patterns, while 11.4% were very satisfied with their current sleeping patterns. Over a one-quarter (29.7%) of the students reported having a sleep problem that was impairing quality of life and was somewhat noticeable to others. One-third (30.3%; n=53) of the students reported not being at all worried about sleeping, and a similar percentage were worried a little (30.3%; n=53). Over one-quarter of the students reported having a sleep problem that somewhat interfered with daily activities or functioning (n= 52, 29.7%). When we asked students about their use of sleeping pills over the past 2 weeks, 20.5% (n=36) had used sleeping medicine, and when asked about the frequency of use of sleeping medicine over the past 2 weeks, 4.6% (n=8) of them used it 1 day, followed by 2.9% (n= 5) who took it 2 days, and 7.4% (n=13) took it about every other day. Most of the students (n=139, 79.4%) did not currently use any sleeping medicine. Only 12.6% and 10.9% currently used Panadol Night and herbal medicines/home remedies, respectively. Table 3 shows the level of satisfaction with sleep patterns.
In this study, 2.9% (n=5) of the students had clinical insomnia (severe), 21.7% (n=38) had moderately severe clinical insomnia, 44% (n=77) had subthreshold insomnia, and 31.4% (n=55) had no clinically significant insomnia (Figure 2).
The relationship between socio-demographic characteristics and insomnia severity score is demonstrated in Table 4. Similar insomnia severity mean scores were observed for male and female students (10.71±5.86 and 10.84±5.79, respectively), with no statistically significant difference (P=0.801). There were no statistically significant associations between insomnia severity mean scores and age groups (P=0.111), nationality (P=0.383), level of education (P=0.382), exercise status (P=0.471), and sleeping pattern (P=0.798). The mean scores of insomnia severity were significantly associated with use of stimulants (P=0.048), average hours of sleep (P=0.0001), and average minutes falling asleep (P=0.0001).
Discussion
It is well known that individuals at some point in their lives suffer from sleeping problems such as poor sleep, difficulty getting appropriate sleep, and insomnia. However, an estimate of the prevalence of insomnia relies upon how we define insomnia and, more importantly, the population being studied. In this study, the overall mean insomnia severity score among students was 10.75±5.82 (SD) (median=11; range 0–27), while 44% (n=77) had subthreshold insomnia, and more than one-third (31.4%, n=55) had no clinically significant insomnia. However, 21.7% (n=38) and 2.9% (n=5) had clinical insomnia with moderate severity and clinical insomnia severity, respectively. These findings were are similar to previous findings by Mbous et al among college students, Alqudah et al among medical and paramedical students, Chowdhury et al among university students, and AlHadi et al among undergraduates [23–26]. For instance, Mbous et al reported a prevalence of 26.4% of insomnia [23]. Similarly, another study among medical and paramedical students in Jordan reported a 26% prevalence of clinical insomnia [24], and 49.9% had subthreshold insomnia [24]. A recent study among Saudi university students revealed a 41% frequency of moderate to severe insomnia [26]. A recent systematic review of studies on the prevalence of insomnia among university students in southern Asian countries found a 35.4% to 70% prevalence. In another study, insomnia was reported to occur in 52.1% of university students [25]. Thus, the literature shows insomnia is common among university students in Saudi Arabia and around the world. This very high prevalence of insomnia may be due to students believing they needed extra hours of sleep to perform well on tests and to concentrate on their studies and achieve academic success. More emphasis should be placed on factors that influence insomnia among university students to identify the fundamental causes and implement effective remedies.
In this research, 61.7% of students reported sleeping at least 6–10 h, whereas 35.4% reported sleeping 6 h. In contrast, a prior survey found that 26.1% of students got more than 7 h of sleep every night, and 42% of students got less than 6 h [24]. Similarly, another study on a large sample of college students found that 25% of students receive less than 6.5 h of sleep per night and 29.4% got more than 8 h [27]. A healthy adult aged 18–60 years requires at least 7 h of sleep, while individuals aged 61–64 require 7–9 h [28].
The sleeping pattern in the current study somewhat differs from previous findings. Most of our students slept during both day and night, few students reported having narcolepsy in our population, and this may be due to cultural norms. For instance, many people in Saudi Arabia sleep in the afternoon after lunch [29], during the severe midday heat, but because of the intense academic schedule at university, some students may no longer be able to indulge in this habit. This, combined with the fact that most students enjoy staying up late at night, may cause some students to feel tired throughout the day. This could explain the prevalence of daytime sleepiness other investigations have shown [30]. Additional research is required to corroborate this finding and investigate additional causes for the disparity in daytime sleeping and narcolepsy rates between our study and those carried out in other nations.
We found that 36% of the students sleep at night only, and 64% slept both at night and day. Similar findings were reported in a previous study among pharmacy students in Saudi Arabia, where 23.2% of the pharmacy students always had daytime sleepiness [31]. These findings also suggested that most of the students slept for the average number of hours required for young adults [24]. The variation in the sleeping pattern and duration of sleep may be explained by the fact that university students can have high levels of stress at the time of data collection, during the exam season, and on normal days. Another reason may be that 71% of our sample students were males who were not physically active, few students were smokers, some used stimulants, and all these factors may have led to a higher prevalence of insomnia in the current study compared to other studies. Furthermore, the difference in findings may be explained by use of different assessment tools and different populations (health care students vs university students vs the public). Furthermore, previous reports revealed university students, especially health care students and pharmacy students, were in stressful conditions [6] due to competition with each other to succeed in exams and courses, which ultimately contribute to insomnia or use of sleeping medicine among students [32,33].
In this study, the most common sleeping disorders among students were insomnia (n=53, 30.3%), followed by sleep apnea (n=8, 4.6%), restless legs syndrome (n=4, 2.3%), and narcolepsy (n=4, 2.3%). A previous study reported that 76.7% had insomnia, followed by 23.3% with restless legs syndrome, 11.3% with narcolepsy, and 6 (4%) with other sleeping disorders, including waking up frequently and excessive daytime sleepiness [34]. Similarly, another study among university students in Oman reported narcolepsy, restless leg syndrome, insomnia, and obstructive sleep apnea were the most common sleep disorders, while sleepwalking and nightmares were infrequently reported [35].
We found that more than two-thirds of the students (65.1%) did not use any sleeping medicine, while 12.6% of the students used Panadol Night and 10. 9% of them used herbal medicines/home remedies. In contrast, Alasmari et al reported a high prevalence of sleeping pill use (24.85%) among students [34], and we found that 17.7% of students used sleeping medicine without a physician’s prescription. These findings were still better than previous findings by Alasmari et al among medical students, who reported that 21.3% of the students used sleeping medicine without a prescription [34]. Other previous finding revealed that sleeping pill use was associated with the use of stimulants, good grades, among senior students, and among students who needed a longer average time to fall asleep [34].
Although self-prescribing is common practice in Saudi Arabia and other developed countries, especially among healthcare students, it is not safe, but self-prescribed medications can have some benefits when used appropriately. The availability and accessibility of several forms of over-the-counter medications, such as Panadol Night and melatonin was the reason for the excessive use of self-prescribed medication among students and other individuals [35–38]. Although self-prescribed drugs can have some benefits when used correctly, it is a dangerous practice that can delay an accurate medical diagnosis and result in unpleasant effects, drug interactions, and building dependence, thereby exacerbating the problem intended to be treated.
Our study has some limitations. First, it was limited to KSU Pharmacy College students and focused on assessing prevalence, sleeping patterns, and satisfaction, and use of sleeping medicine among students in the pharmacy college. Second, given the small sample size, the study lacks generalizable results. Despite these limitations, our study is important in that it assessed student’s sleeping patterns and the results can subsequently help remedy any problems found. Our study is the first of its kind and will establish a foundation for research on this issue.
Conclusions
We found varying levels of insomnia among students, but most had a sleeping pattern recommended by health guidelines. Although sleep disorders were associated with negative academic performance and disturbed quality of life, adequate diagnosis and management of sleep disorders may solve this issue. Furthermore, a larger emphasis on the student’s mental health is encouraged, which can increase students’ academic satisfaction, well-being, and academic achievement. Additionally, there are a range of approaches available to help college students feel less stressed, including messaging, coping therapy, and social support from family. To overcome sleeping problems, students must develop a regulated sleeping time, a sleeping pattern to combat insomnia, avoid using social media or the internet before bed, and, finally, adopt relaxing techniques that may aid in overcoming sleeping problems. We propose an additional study of pharmacy students with a large sample size to address this essential issue.
References
1. Van Dongen HP, Maislin G, Mullington JM, Dinges DF, The cumulative cost of additional wakefulness: Dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation: Sleep, 2003; 26(2); 117-26 Erratum in: Sleep. 2004;27(4):600
2. Zolfaghari S, Yao C, Thompson C, Effects of menopause on sleep quality and sleep disorders: Canadian Longitudinal Study on Aging: Menopause, 2020; 27(3); 295-304
3. National Institute of neurologic disorders and stroke: Brain Basics: Understanding Sleep Available at https://www.ninds.nih.gov/health-information/public-education/brain-basics/brain-basics-understanding-sleep
4. Yassin A, Al-Mistarehi AH, Beni Yonis O, Prevalence of sleep disorders among medical students and their association with poor academic performance: A cross-sectional study: Ann Med Surg (Lond), 2020; 58; 124-29
5. Zeek ML, Savoie MJ, Song M, Sleep duration and academic performance among student pharmacists: Am J Pharm Educ, 2015; 79(5); 63
6. Samreen S, Siddiqui NA, Mothana RA, Prevalence of anxiety and associated factors among pharmacy students in Saudi Arabia: A cross-sectional study: Biomed Res Int, 2020; 2020; 2436538
7. Mnatzaganian CL, Atayee RS, Namba JM, The effect of sleep quality, sleep components, and environmental sleep factors on core curriculum exam scores among pharmacy students: Curr Pharm Teach Learn, 2020; 12(2); 119-26
8. Ahrberg K, Dresler M, Niedermaier S, The interaction between sleep quality and academic performance: J Psychiatr Res, 2012; 46(12); 1618-22
9. Abdulghani HM, Alrowais NA, Bin-Saad NS, Sleep disorder among medical students: Relationship to their academic performance: Med Teach, 2012; 34(Suppl 1); S37-41
10. Christodoulou N, Maruani J, d’Ortho MP, Sleep quality of medical students and relationships with academic performances: Encephale, 2023; 49(1); 9-14
11. Veldi M, Aluoja A, Vasar V, Sleep quality and more common sleep-related problems in medical students: Sleep Med, 2005; 6(3); 269-75
12. Syed W, Iqbal A, Siddiqui NA, Attitudes and associated demographic factors contributing towards the abuse of illicit drugs: A cross-sectional study from health care students in Saudi Arabia: Medicina (Kaunas), 2022; 58(2); 322
13. Bastien CH, Vallières A, Morin CM, Validation of the Insomnia Severity Index as an outcome measure for insomnia research: Sleep Med, 2001; 2(4); 297-307
14. Mayo Clinic, Insomnia: Overview Available at https://www.mayoclinic.org/diseases-conditions/insomnia/symptoms-causes/syc-20355167#:~:text=It%27s%20usually%20the%20result%20of,put%20up%20with%20sleepless%20nights
15. Samreen S, Siddiqui NA, Wajid S, Prevalence and use of dietary supplements among pharmacy students in Saudi Arabia: Risk Manag Healthc Policy, 2020; 13; 1523-31
16. Samreen S, Sales I, Bawazeer G, Assessment of beliefs, behaviors, and opinions about blood donation in Telangana, India – a cross sectional community-based study: Front Public Health, 2021; 9; 785568
17. Bashatah A, Syed W, Al-Rawi MBA, Knowledge of cardiovascular disease risk factors and its primary prevention practices among the saudi public – a questionnaire-based cross-sectional study: Int J Gen Med, 2023; 16; 4745-56
18. Alobaid AM, Syed W, Al-Rawi MBA, Evaluation of headache trends among undergraduate first responders for medical emergencies at Saudi University in Riyadh, Saudi Arabia: Medicina (Kaunas), 2023; 59(9); 1522
19. Qhadi OA, Albothi GK, Fallatah R, Navigating health literacy and practices: A cross-sectional study on nursing undergraduates in Riyadh, Saudi Arabia: Med Sci Monit, 2023; 29; e941632
20. Syed W, Al-Rawi MBA, Community pharmacists’ awareness, perceptions, and opinions of artificial intelligence: A cross-sectional study in Riyadh, Saudi Arabia: Technol Health Care, 2023 Online ahead of print
21. Blais FC, Gendron L, Mimeault V, Morin CMEvaluation of insomnia: Validity of 3 questionnaires: Encephale, 1997; 23(6); 447-53 in French
22. Morin CM, Belleville G, Bélanger L, Ivers H, The Insomnia Severity Index: Psychometric indicators to detect insomnia cases and evaluate treatment response: Sleep, 2011; 34(5); 601-8
23. Mbous YPV, Nili M, Mohamed R, Dwibedi N, Psychosocial correlates of insomnia among college students: Prev Chronic Dis, 2022; 19; 220060
24. Alqudah M, Balousha SAM, Al-Shboul O, Insomnia among medical and paramedical students in Jordan: Impact on academic performance: Biomed Res Int, 2019; 2019; 7136906
25. Chowdhury AI, Ghosh S, Hasan MF, Prevalence of insomnia among university students in South Asian Region: A systematic review of studies: J Prev Med Hyg, 2021; 61(4); E525-E29
26. AlHadi AN, Alhuwaydi AM, Insomnia prevalence and associated factors among university students in Saudi Arabia during the COVID-19 pandemic and lockdown: A large-scale survey: Nat Sci Sleep, 2022; 14; 1651-63
27. Lund HG, Reider BD, Whiting AB, Prichard JR, Sleep patterns and predictors of disturbed sleep in a large population of college students: J Adolesc Health, 2010; 46(2); 124-32
28. Chaput JP, Dutil C, Sampasa-Kanyinga H, Sleeping hours: What is the ideal number and how does age impact this?: Nat Sci Sleep, 2018; 10; 421-30
29. Shokry SM, El Wakeel EE, Al-Maflehi N, Association between self-reported bruxism and sleeping patterns among dental students in Saudi Arabia: A cross-sectional study: Int J Dent, 2016; 2016; 4327081
30. Spoormaker VI, Verbeek I, van den Bout J, Klip EC, Initial validation of the SLEEP-50 questionnaire: Behav Sleep Med, 2005; 3(4); 227-46
31. Thabit AK, Alsulami AA, Impact of sleep pattern of pharmacy college students on academic performance: Sleep Vigil, 2023 Online ahead of print
32. Garber MC, Huston SA, Breese CR, Sources of stress in a pharmacy student population: Curr Pharm Teach Learn, 2019; 11(4); 329-37
33. Opoku-Acheampong A, Kretchy IA, Acheampong F, Perceived stress and quality of life of pharmacy students in University of Ghana: BMC Res Notes, 2017; 10(1); 115
34. Alasmari MM, Alkanani RS, Alshareef AS, Medical students’ attitudes toward sleeping pill usage: A cross-sectional study: Front Psychiatry, 2022; 13; 1007141
35. Al Salmani AA, Al Shidhani A, Al Qassabi SS, Prevalence of sleep disorders among university students and its impact on academic performance: Int J Adolesc Youth, 2020; 25(1); 974-81
36. Mahmoud MA, Wajid S, Naqvi AA, Self-medication with antibiotics: A cross-sectional community-based study: Latin American Journal of Pharmacy, 2020; 39(2); 348-53
37. Alfadly S, Ballaswad MR, Amra AS, Self-medication with antibiotic amongst adults attending community pharmacies in Mukalla district, Yemen: Lat Am J Pharm, 2017; 36(2); 224-28
38. Aljohani EM, Aldughaither AA, The prevalence of sleeping pills and factors associated with their use among primary care patients, in Riyadh, Saudi Arabia: International Journal of Medicine in Developing Countries, 2019; 3; 83-89
Tables
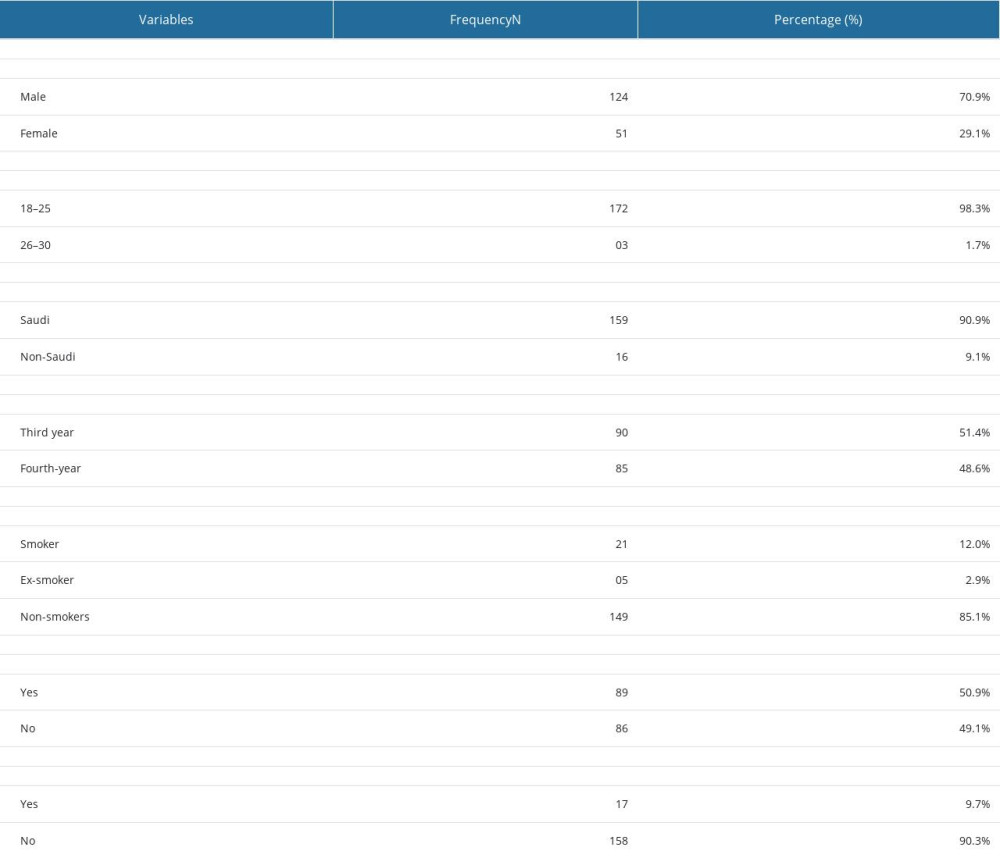 Table 1. Socio-demographic characteristics of the students.
Table 1. Socio-demographic characteristics of the students.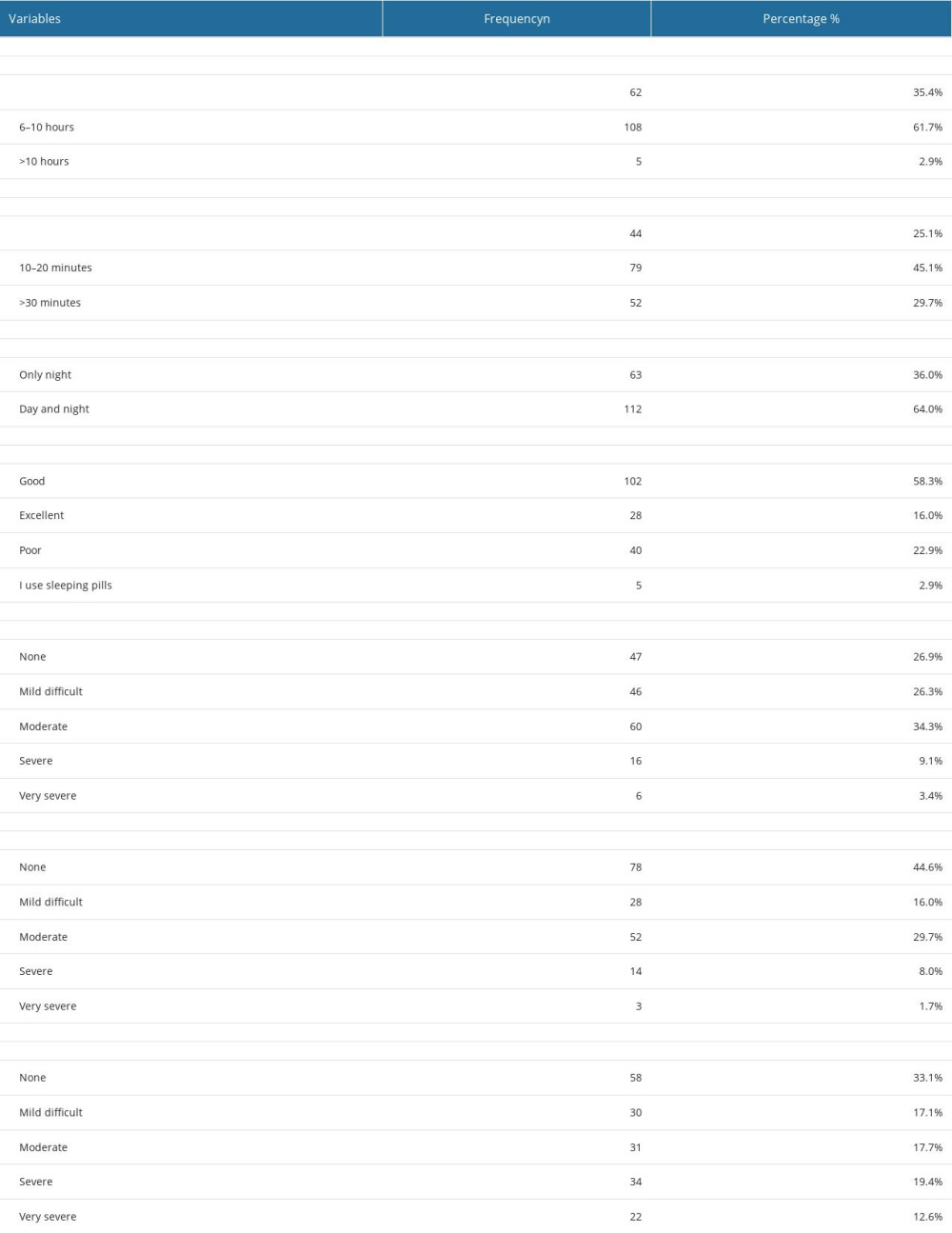 Table 2. Responses towards the quality of sleep of the students.
Table 2. Responses towards the quality of sleep of the students.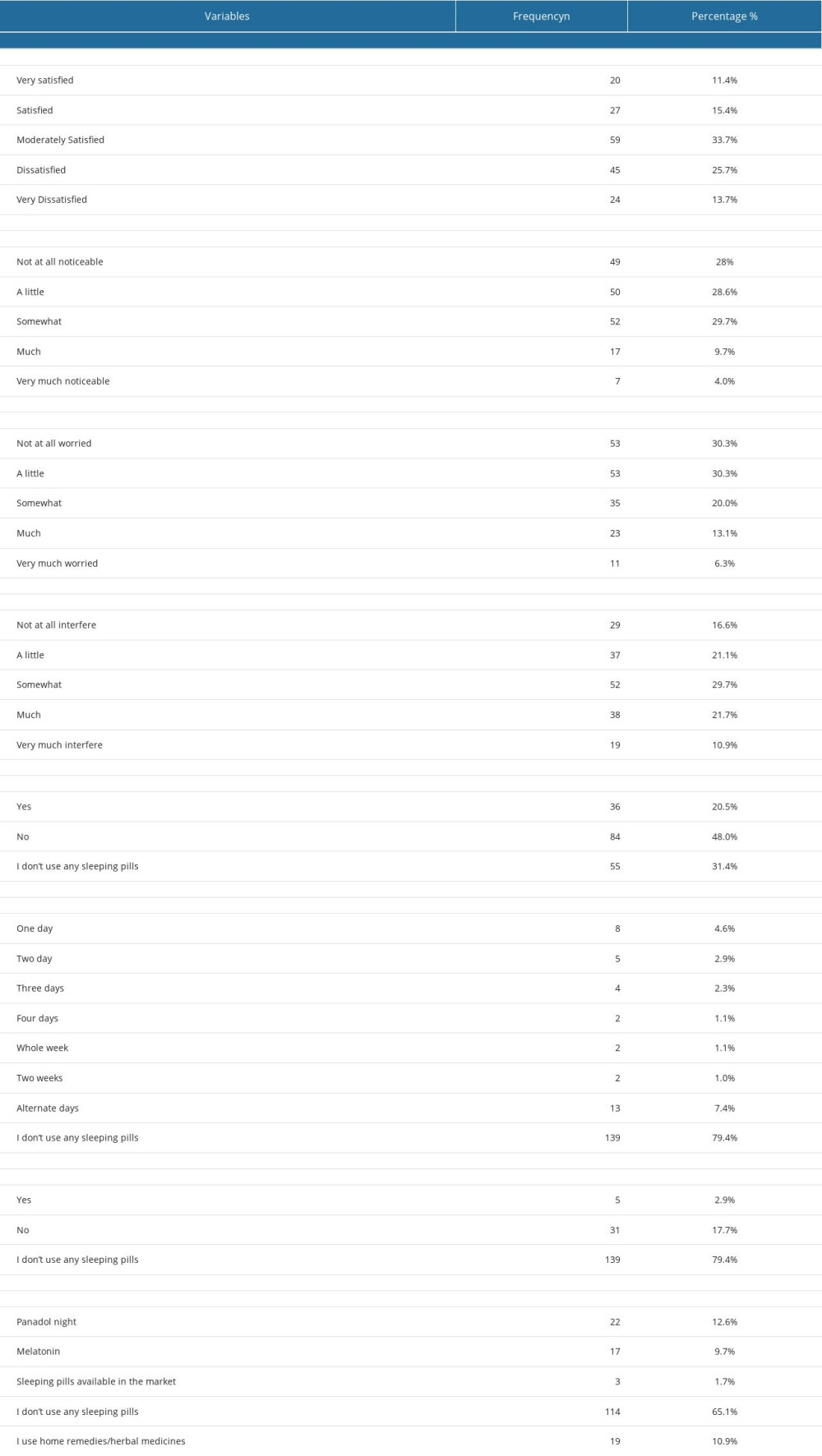 Table 3. Students’ responses towards sleep pattern satisfaction.
Table 3. Students’ responses towards sleep pattern satisfaction.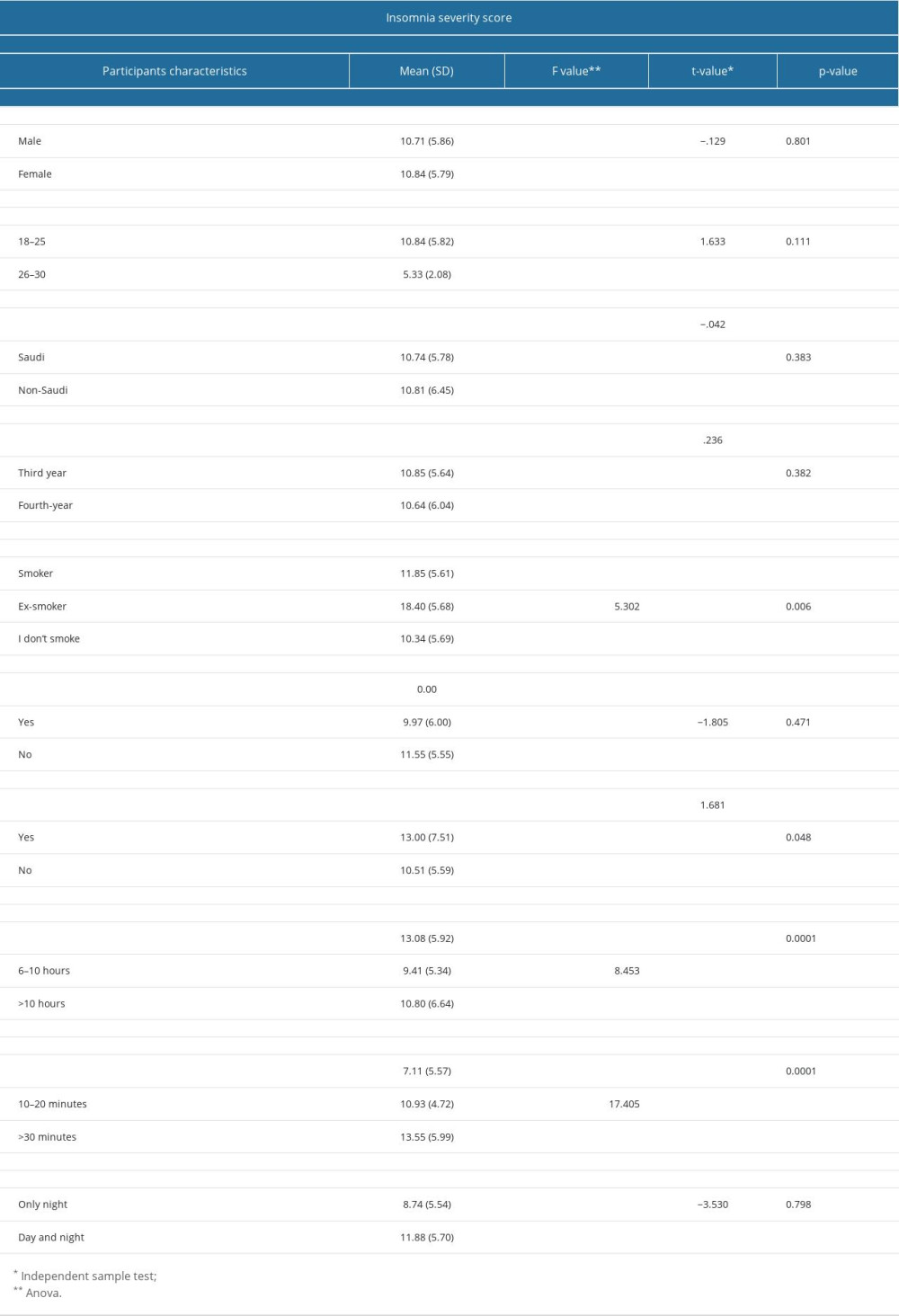 Table 4. Association between insomnia severity scores and participant’s characteristics.
Table 4. Association between insomnia severity scores and participant’s characteristics.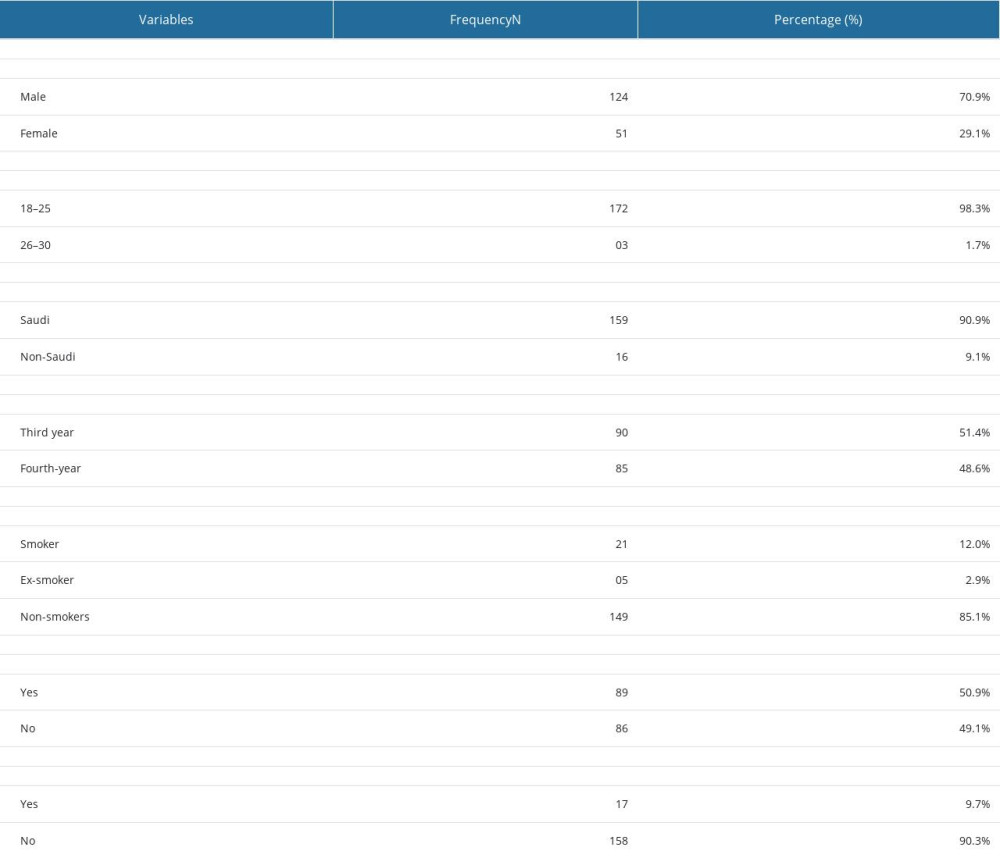 Table 1. Socio-demographic characteristics of the students.
Table 1. Socio-demographic characteristics of the students.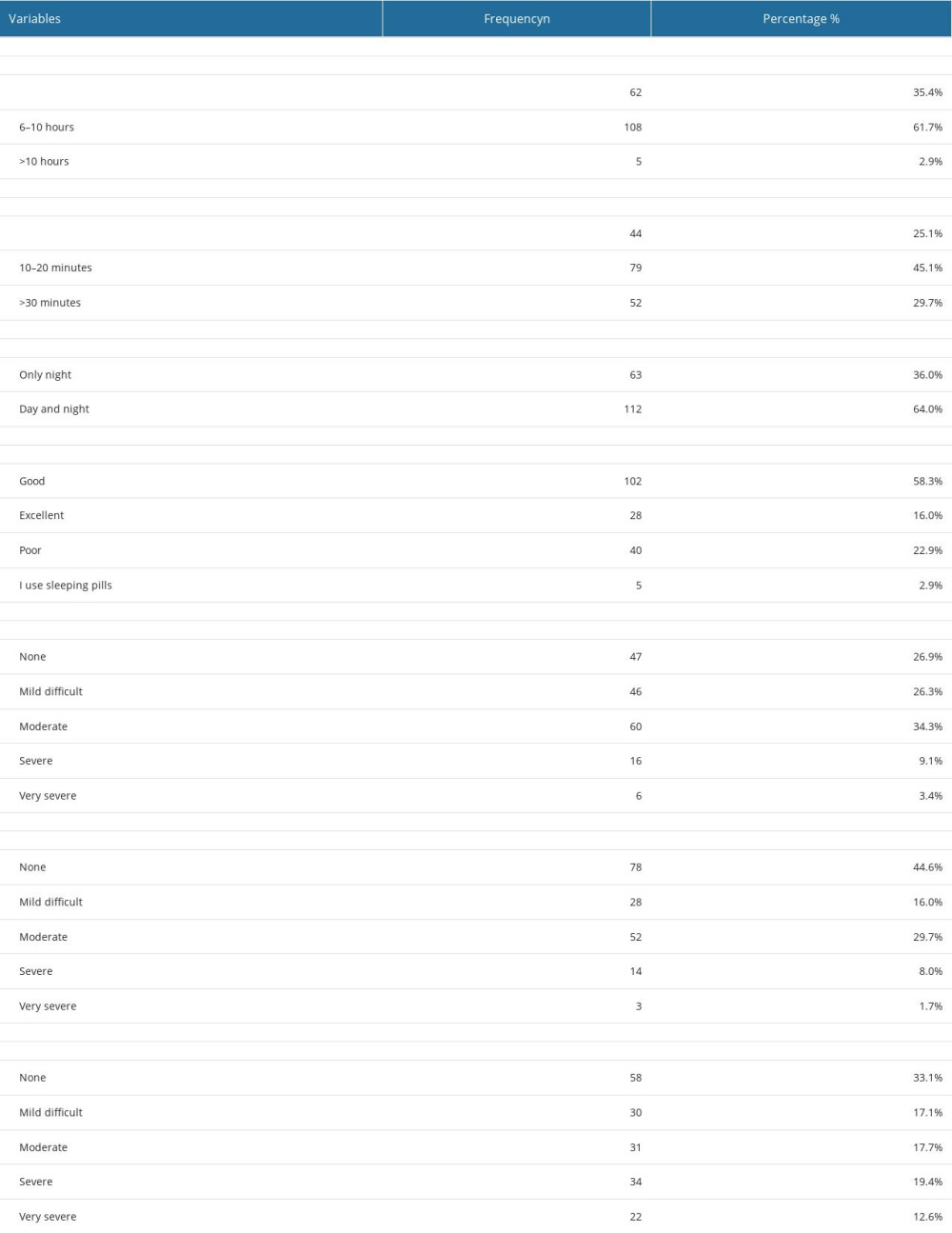 Table 2. Responses towards the quality of sleep of the students.
Table 2. Responses towards the quality of sleep of the students.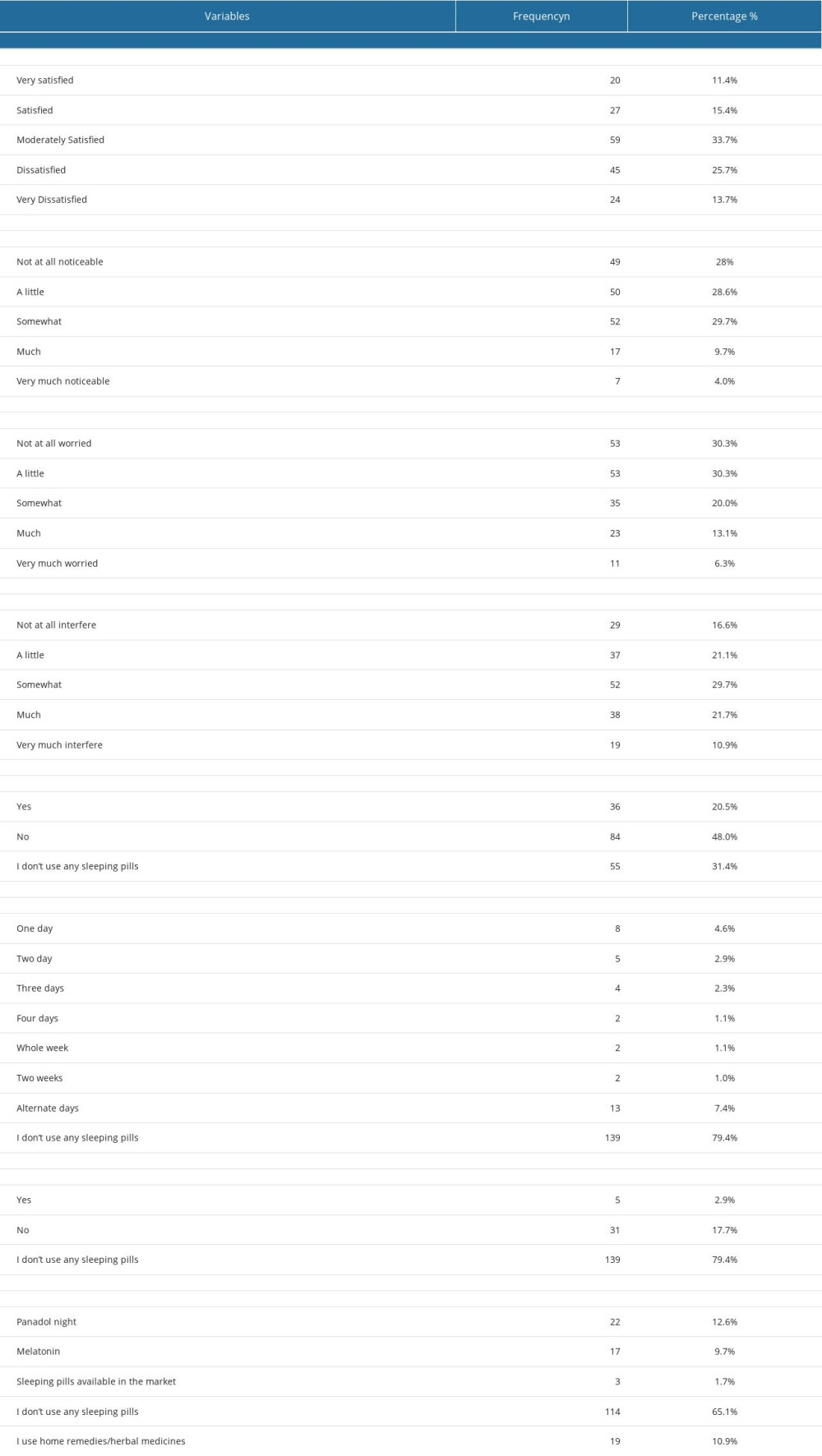 Table 3. Students’ responses towards sleep pattern satisfaction.
Table 3. Students’ responses towards sleep pattern satisfaction.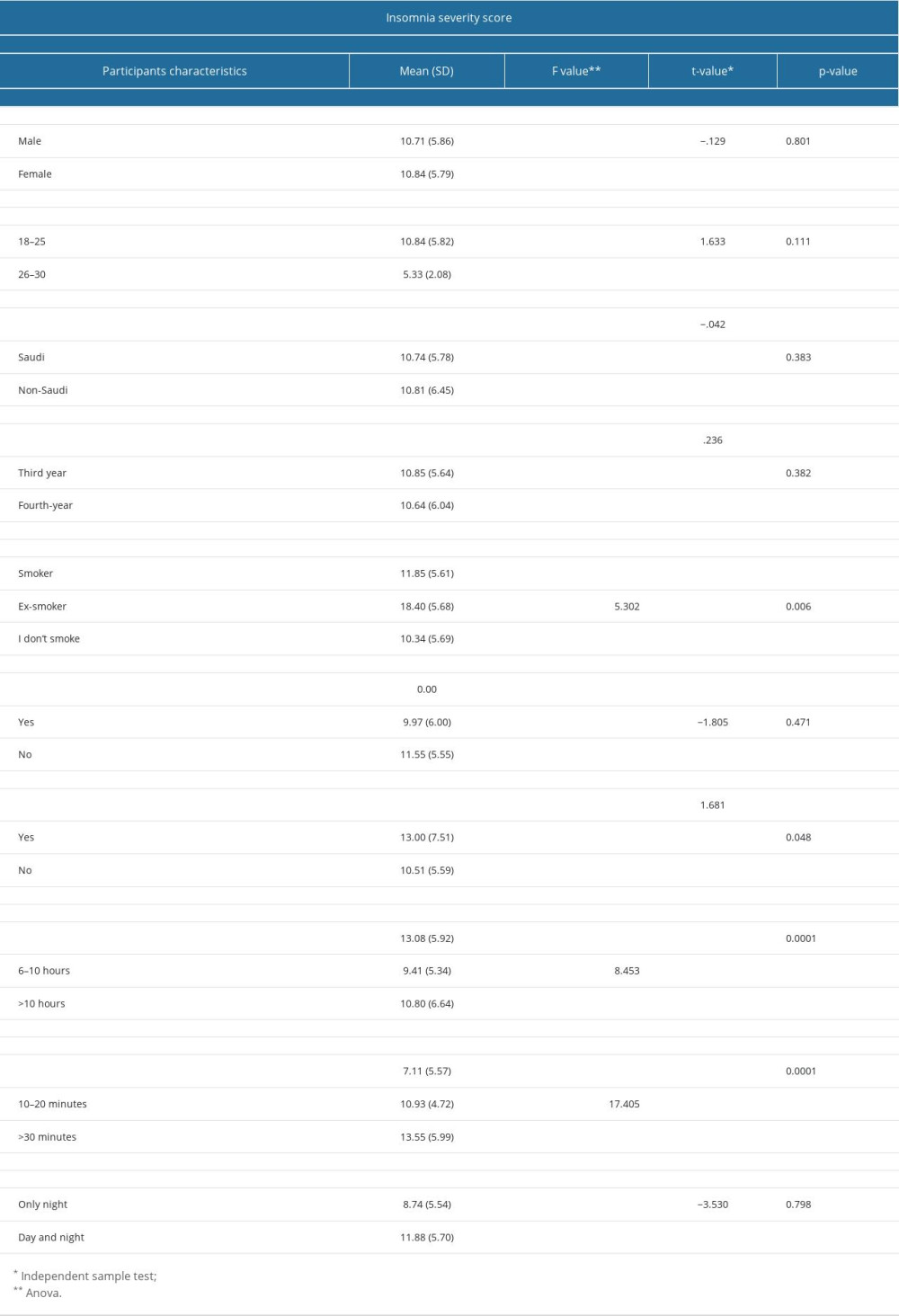 Table 4. Association between insomnia severity scores and participant’s characteristics.
Table 4. Association between insomnia severity scores and participant’s characteristics. In Press
12 Mar 2024 : Clinical Research
Tissue Inhibitors of Metalloproteinase 1 (TIMP-1) and 3 (TIMP-3) as New Markers of Acute Kidney Injury Afte...Med Sci Monit In Press; DOI: 10.12659/MSM.943500
12 Mar 2024 : Review article
Optimizing Behçet Uveitis Management: A Review of Personalized Immunosuppressive StrategiesMed Sci Monit In Press; DOI: 10.12659/MSM.943240
12 Mar 2024 : Clinical Research
Metabolomic Alterations in Methotrexate Treatment of Moderate-to-Severe PsoriasisMed Sci Monit In Press; DOI: 10.12659/MSM.943360
14 Mar 2024 : Clinical Research
Renal Dysfunction Increases Risk of Adverse Cardiovascular Events in 5-Year Follow-Up Study of Intermediate...Med Sci Monit In Press; DOI: 10.12659/MSM.943956
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952