24 December 2023: Clinical Research
Prevalence and Risk Factors of Osteoporosis in a Chinese Population: A Cross-Sectional Study in Xi’an, Shaanxi Province, China
Jidong Song1ACDE, Jiaxin Zhao1CE*, Tun Liu1BC, Yongwei Li1BC, Xiaoqian Dang1C, Wei Wang1ADOI: 10.12659/MSM.942346
Med Sci Monit 2023; 29:e942346
Abstract
BACKGROUND: Osteoporosis is a systemic chronic disease characterized by bone mineral density (BMD) reduction. This study aimed to assess the prevalence of osteoporosis and fracture risks in northwestern China and investigate the related anthropometric risk factors.
MATERIAL AND METHODS: Between July 2022 and August 2022, 1429 participants (1295 females, 134 males) with measured BMD were recruited to participate in this cross-sectional study. Data on height, weight, and T score were collected. Spearman’s correlation and multiple linear regression analysis were used to investigate the relationships between various demographic factors and BMD and the 10-year risk of major osteoporotic fracture (MO) and hip fracture (HP).
RESULTS: The overall prevalence of osteoporosis in northwest China was 42.34%, with 44.56% in females and 20.90% in males. Age negatively affects females’ T scores (r=-0.304, P<0.05), and height positively influences both sexes’ T scores (r=0.059 P<0.05). Age (r=0.148, P<0.05) and height were positive predictors of MO (r=0.027, P<0.05), while weight was a negative predictor (r=-0.035, P<0.05). The conclusion for HP was consistent with that of MO, except for the T score, which was a positive predictor of HP (r=0.014, P<0.05).
CONCLUSIONS: The prevalence of osteoporosis in northeast China is high. The association between anthropometric parameters and osteoporosis in adults in northwest China is different between sexes.
Keywords: Osteoporosis, Bone Density, Fractures, Bone, China
Background
Osteoporosis is a systemic disease characterized by bone mineral density (BMD) reduction, bone fragility, and skeletal tissue deterioration [1]. It can lead to pain, disability, a decline in quality of life, and even shortened life expectancy [2]. It is estimated that approximately 200 million people worldwide suffer from osteoporosis [3], and the prevalence of this disease increases with age and is higher in females than in males [4]. A research report predicted the number of people at high risk of osteoporosis fractures will rise from 158 million currently to 319 million by 2040 [5]. In China, the morbidity rate of osteoporosis has increased for decades, affecting approximately one-third of people aged 50 years and older [4]. Currently, an estimated 10.9 million men and 49.3 million women in China suffer from osteoporosis [6].
Bone mineral density (BMD) is an important indicator of bone strength, and its reduction is reliable for diagnosing and evaluating osteoporosis [7]. The T score and the Z-score are used to express the condition of BMD, with a T score −2.5 or below the score indicating osteoporosis, a T score between −2.5 and −1 indicating osteopenia, and a T score of −1 or above indicating normal bone mass [8]. Dual-energy X-ray absorptiometry (DXA) is considered the criterion standard for diagnosis of osteoporosis [9], but it is expensive and involves some exposure to radiation, making it less suitable for screening for changes in bone density [10]. Studies have shown that radius quantitative ultrasound (QUS) is a more practical and non-radiational tool to assess osteoporosis, providing a reference for improved fracture risk assessment [11].
Various non-modifiable, modifiable, and lifestyle factors affect osteoporosis [12]. Non-modifiable factors, such as genes, advanced age, female sex, and familial predisposition, play a significant role in the majority of the risk of osteoporosis [5]. Some studies have confirmed that age, sex, weight, and BMI are important predictors of osteoporosis, but the exact association has not been fully determined in Chinese people [13].
We conducted a cross-sectional study following 1429 participants to assess the prevalence of osteoporosis using QUS and calculated their fracture risks using FRAX tool in a population of both sexes in Xi’an, Shaanxi Province, China. We investigated the effects of age, sex, weight, height, and BMI on BMD and fracture risks through multiple linear regression analysis to provide a general description of osteoporosis in the population of northwest China. This study aimed to determine the characteristics of osteoporosis and fracture risks in northwest China, to assess the sex differences in osteoporosis in the population, and to draw relevant conclusions. We also studied the association of age, BMI, and other factors with osteoporosis and fracture risks.
Material and Methods
ETHICS APPROVAL:
The study protocol was approved by the Ethics Committee of the Second Affiliated Hospital of Xi’an Jiaotong University (No. 2023264), and written informed consent was obtained from each participant.
STUDY DESIGN AND POPULATION:
This was a cross-sectional study. A total of 1295 female and 134 male participants aged 30 years or older who had undergone routine physical check-ups were recruited from our hospital in Xi’an, Shaanxi province of China between July 2022 and August 2022. Each participant underwent anthropometric and wrist BMD measurements. Exclusion criteria were metabolic bone disease history, history of diseases affecting body composition or weights, and lack of data for necessary items or written informed consent could not be obtained.
DATA COLLECTION:
A general anthropometric measurement was performed for all participants. Weight and height were measured wearing thin clothes and removing shoes. BMI was calculated as weight (kg) divided by height squared (m2).
The BMD of the right wrist was measured using a dry quantitative ultrasound device (BMD-A3, Pinyuan Tec., Xuzhou, China). The instruments were calibrated daily according to the operating instruction before measurement and each participant was measured twice on the right wrist by a well-trained doctor, and the mean value was used for further analysis. The output paraments include speed of sound (SOS, m/s), T score, and Z-score. T scores and Z-scores of BMD were calculated using data on healthy Chinese as a reference.
The World Health Organization (WHO) introduced the fracture risk assessment tool (FRAX) in 2008 to estimate the absolute risk of osteoporotic fractures in a certain range of patients [14], using the interaction of risk factors such as height, weight, age, sex, family, and personal history [15]. The FRAX score was used to determine the participants’ 10-year risk of major osteoporotic fracture and hip fracture. It was calculated using sex, age, weight (kg), and height (cm) with the FRAX tool online calculator of the Center for Metabolic Bone Diseases, University of Sheffield, UK (https://www.sheffield.ac.uk/FRAX/index.aspx).
DEFINITION:
A diagnosis of osteoporosis is made based on the WHO definition. According to the WHO, the T score represents the number of standard deviations (SD) below or above the average BMD. Participants were classified as normal (T score > −1.0), having osteopenia (−2.5 < T score < −1.0), and having osteoporosis (T score < −2.5) [16].
STATISTICAL ANALYSIS:
Statistical analyses were performed using the SPSS version 26 (SPSS, Inc., Chicago, IL, USA). Continuous variables are expressed as mean±SD and categorical data are presented as percentages. We used unpaired and paired
Results
BASELINE CHARACTERISTICS OF OVERALL POPULATION:
The baseline characteristics of overall population are presented in Table 1. A total of 1429 participants (1295 women and 134 men, mean BMI 23.37±2.72 kg/m2) were included in this cross-sectional study. According to Table 1, there was no significant difference in the mean BMI between the sexes. The prevalence of osteoporosis among all participants was 42.34%, with a higher prevalence in females (44.56%) than in males (20.90%).
The fracture risks were also assessed in the study population using sex, age, weight (kg) and height (cm) with the FRAX tool. The 10-year risk of major osteoporotic fracture was (3.57±1.21)% for the total population and (1.02±0.79)% for hip fracture. In females, the 10-year risk of major osteoporotic fracture was (3.70±1.17)% and (1.05±0.81)% for hip fracture. Conversely, in males, the 10-year risk of major osteoporotic fracture was (2.21±0.55)% and (0.72±0.53)% for hip fracture (Table 1).
SPEARMAN’S CORRELATION ANALYSIS FOR THE ASSOCIATION BETWEEN SEX, AGE, WEIGHT, HEIGHT, BMI AND T SCORE:
Based on the results shown in Table 2, for the overall population, it is evident that sex, age, height, and weight were significantly associated with T scores (P<0.05), while there was no correlation between BMI and T score (P>0.05). Spearman’s correlation analysis revealed a positive correlation between height, weight, and T score, indicating that individuals with higher heights and weights tend to have higher T scores. Conversely, a negative correlation was observed between age and T score, indicating that older individuals tend to have lower T scores.
Further analysis of the subgroups by sex revealed intriguing findings. Specifically, in females, spearman’s correlation analysis showed that age, height, and weight were significantly associated with T score (P<0.05), indicating that these variables play a crucial role in determining T scores in females. In contrast, in males, only age was found to be significantly associated with T score (P<0.05), while height and weight did not have a significant impact. This suggests that the determinants of T score differ between males and females, and further exploration is required to understand the underlying factors that influence T scores in each sex (Table 2).
ASSOCIATION BETWEEN SEX, AGE, WEIGHT, HEIGHT, BMI, AND T SCORE:
According to the results of our statistical analysis, as demonstrated in Table 3, the univariate linear regression analysis revealed that sex, age, height, and weight were all associated with the T score in the overall study population (P<0.001), while there was no significant correlation between BMI and T score (P>0.05). Moreover, the multivariate linear regression analysis showed that sex, age, and height remained significant predictors of T scores, even after controlling for the effects of the other variables. However, the relationship between body weight and the T score was no longer significant in the multivariate model (Table 3).
Additionally, separate univariate and multivariate linear regression analyses on females were conducted (Table 4). In this subgroup analysis, age, height, and weight were found to be significant predictors of T scores (P<0.001), whereas BMI were not significantly correlated with T scores (P>0.05). The findings regarding age and height were further supported by the multiple linear regression analysis, which showed that age was negatively correlated with T scores (P<0.001) and height was positively correlated with T scores (P<0.05) (Table 4).
ASSOCIATION BETWEEN SEX, AGE, WEIGHT, HEIGHT, AND T SCORE AND FRACTURE RISKS:
Multiple linear regression analysis was conducted to investigate the relationships between various demographic factors and the 10-year risk of major osteoporotic fracture (MO) and hip fracture (HP). The results showed that sex, age, weight, and height were significantly related to MO in the total population. In particular, age and height were positively correlated with MO, while weight was negatively correlated with MO (Table 5). Furthermore, our analysis revealed that sex, age, weight, height, and T score were significantly associated with HP in the total population. In particular, age, height, and T score were positively correlated with HP, while weight was negatively correlated with HP (Table 5).
After our analysis of the total population, we then carried out subgroup analyses for females. According to Table 6, in females, age, height, weight, and T score were all significantly associated with both MO and HP. Specifically, age, height, and T score were positively correlated with both MO and HP, while weight was negatively correlated with both MO and HP (Table 6).
Discussion
This cross-sectional study aimed to investigate the characteristics of osteoporosis and fracture risks in northwest China by assessing the prevalence of osteoporosis using QUS and calculated their fracture risks using the FRAX tool. A total of 1429 participants (1295 women and 134 men) were included, and the effects of age, sex, and anthropometric measurements on BMD and fracture risks were examined to provide a general description of osteoporosis in the population of northwest China. Our study revealed an overall prevalence of osteoporosis of 42.34%, with a higher prevalence among females (44.56%) compared to males (20.90%). In terms of BMD, sex, age, and height were significant predictors of T score, with age negatively predicting T scores in females and height positively predicting T scores in both sexes. In terms of fracture risks, age and height were positive predictors of MO, while weight was a negative predictor. The results regarding HP were consistent with those for MO, except for the T score, which was a positive predictor of HP.
The prevalence of osteoporosis and related fracture risks pose a significant public health concern, albeit with considerable variability noted across different investigations. The distribution of BMD and osteoporosis populations in the northwest region has not been systematically studied. In China, Zhang et al compiled a reference BMD database in 2014 by pooling data from139 912 Chinese adults, revealing that the age-standardized prevalence of osteoporosis was 23.9% and 12.5% in women and 3.2% and 5.3% in men aged >50 years at the lumbar spine and femoral neck, respectively[17]. A recent comprehensive cross-sectional study on the prevalence of osteoporosis among 20 416 participants in mainland China, assessing clinical fracture and related factors, estimated that the prevalence of osteoporosis among those aged 40 years or older was 5.0% in men and 20.6% in women [18]. A study conducted in Jilin Province, Northern China, examining the prevalence of osteoporosis defined by BMD at the distal forearm, reported a prevalence of 19.8% in men and 36.9% in women aged over age 50 years [19]. In our study, which utilized radial QUS to assess the prevalence of osteoporosis in northwest China, we found an overall prevalence of 42.34%, with higher prevalence among females (44.56%) than males (20.90%), consistent with the findings in Jilin Province. However, another study, defined by BMD at radius, conducted in Gansu, another province in northwest China, yielded a prevalence of 9.65% for postmenopausal women and 8.08% for men [20], which is much lower than in other reports. Differences in inclusion and exclusion criteria, population size, regions, genetic factors, and measurement methods and sites all can affect the distribution of BMD and osteoporosis in a population, making the production of representative studies one of the current challenges. The present study supplements the literature on the characteristics of osteoporosis in northwest China.
Our study suggests that demographic factors, such as sex, age, height, and weight, play a role in determining BMD and the development of osteoporotic fractures, and this relationship may vary by sex. In terms of BMD, sex, age, and height were significant predictors of T score, with age negatively predicting T score in females, similar to previous findings, and height positively predicting T score in both sexes. The predictive value of height for BMD is controversial. In a 15-year follow-up including 1421 postmenopausal women, Forsmo et al found that shorter height was accompanied by a lower forearm BMD, and height was somewhat predictive of BMD [21], and this was similar to our findings. However, some studies found that height does not correlate with BMD [22]. Nichotson et al found no association between shorter height and lower BMD in a cross-sectional study of 222 individuals [23]. The relationship between height and BDM may need to be assessed by studies with larger sample sizes.
In addition, we included the fracture risk score to complement the description of the study population, and found the 10-year risk of major osteoporotic fracture was (3.57±1.21)% for the total population and (1.02±0.79)% for hip fracture. We found that the risk of fracture was higher in women than in men, which is similar to previous findings [24,25]. However, the prevention and treatment of osteoporotic fracture in men should not be neglected because they tend to have worse outcomes and poorer treatment rates. In addition, we believe the FRAX model may underestimate the actual fracture probability in China [26,27]. Our study found that multiple demographic and clinical factors play important roles in the development of osteoporotic fractures, and that these relationships may vary by sex. In particular, our results highlight the importance of age, height, weight, and T score as key predictors of fracture risk, and suggest that heavier weight may have a protective effect against fractures in females. Our findings are consistent with previous research [28,29].
In addition to the factors we focused on, other confounding factors, including dietary patterns, lifestyle choices, medication usage, and stress levels, may contribute to the difference in prevalence of risk factors between our study and other studies in China. The role of diet is particularly significant in relation to osteoporosis, as it is one of the few modifiable risk factors. The Mediterranean diet has proven to be beneficial to BMD [30], and Dietary Approaches to Stop Hypertension may improve lumbar spine BMD [31]. The diet pattern is the high-carbohydrate diet that is common in northwest China. The types of foods consumed were generally lacking diversity and the main energy sources were rice and noodles. A cross-sectional study in northwest China found that a high-carbohydrate diet was associated with a higher risk of frailty and pre-frailty [32]. This may account for part of the vast regional difference. Maintaining a healthy lifestyle, characterized by physical activity and sun exposure, is also beneficial for the preservation and enhancement of bone density. Conversely, unhealthy lifestyle habits such as smoking and excessive alcohol consumption can decrease bone density. In terms of medication usage, calcium and vitamin D play a crucial role in osteoporosis prevention, and engaging in outdoor activities promotes exposure to sunlight, which aids vitamin D synthesis. Low vitamin D status is prominent in mainland China, especially among adults [33]. A cross-sectional study including 11157 healthy participants found that vitamin D deficiency is highly prevalent in northwest China (82.5% in men and 81.1% in women), especially among young physically inactive and overweight women with limited sunlight exposure [34]. Notably, Follis et al discovered a potential correlation between heightened social stress and bone loss in a study involving 11 020 postmenopausal women [35]. However, the relationship between regional differences in these confounding factors and BMD requires larger epidemiological studies.
It is important to note some potential limitations of this study. First, an analysis of a northwestern Chinese population led us to our conclusion. Therefore, the results of the study should not be generalized to all regions of China. Second, the number of females and males in the study population failed to ensure quantitative consistency, so further studies with larger sample sizes are needed to investigate the prevalence of osteoporosis in the Chinese population and its associated factors.
Conclusions
We found an overall prevalence of osteoporosis of 42.34%, with a higher prevalence among females (44.56%) compared to males (20.90%) in northwest China. In terms of BMD, sex, age and height were significant predictors of T score, with age negatively predicting T score in females and height positively predicting T score in both sexes. In terms of fracture risks, age and height were positive predictors of MO, while weight was a negative predictor. The conclusion for HP was consistent with that of MO, except for the T score, which was a positive predictor of HP.
Tables
Table 1. Baseline characteristics of overall populations.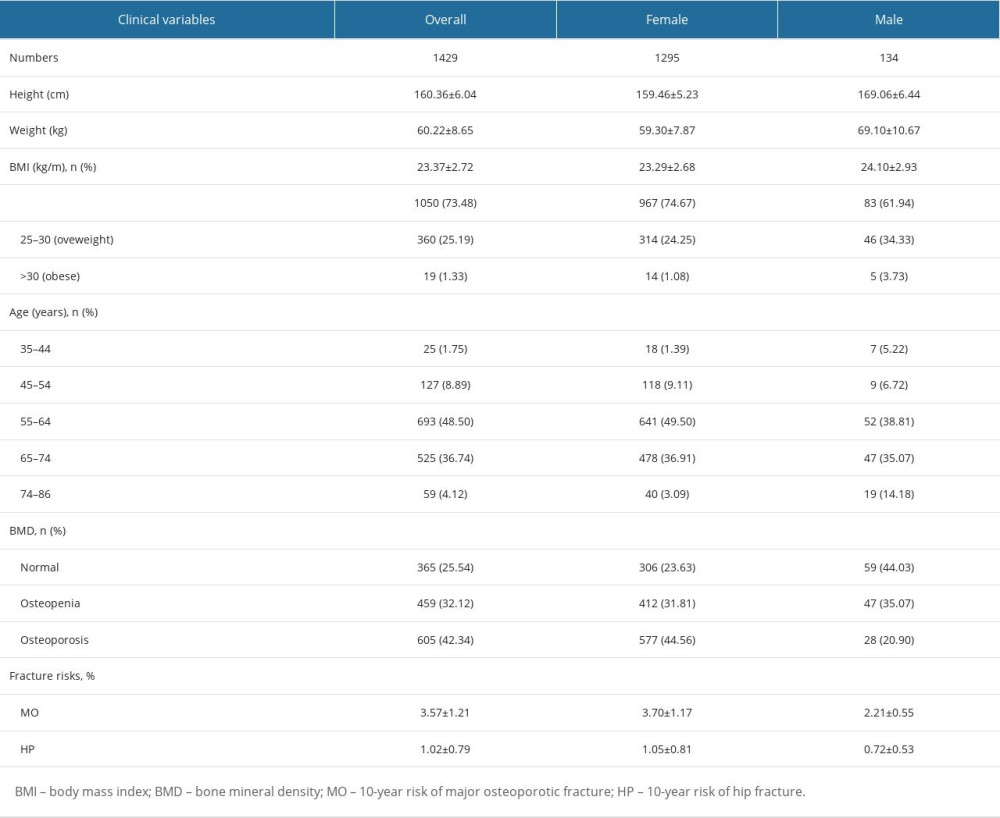 Table 2. Spearman’s rank correlation coefficient for T score.
Table 2. Spearman’s rank correlation coefficient for T score.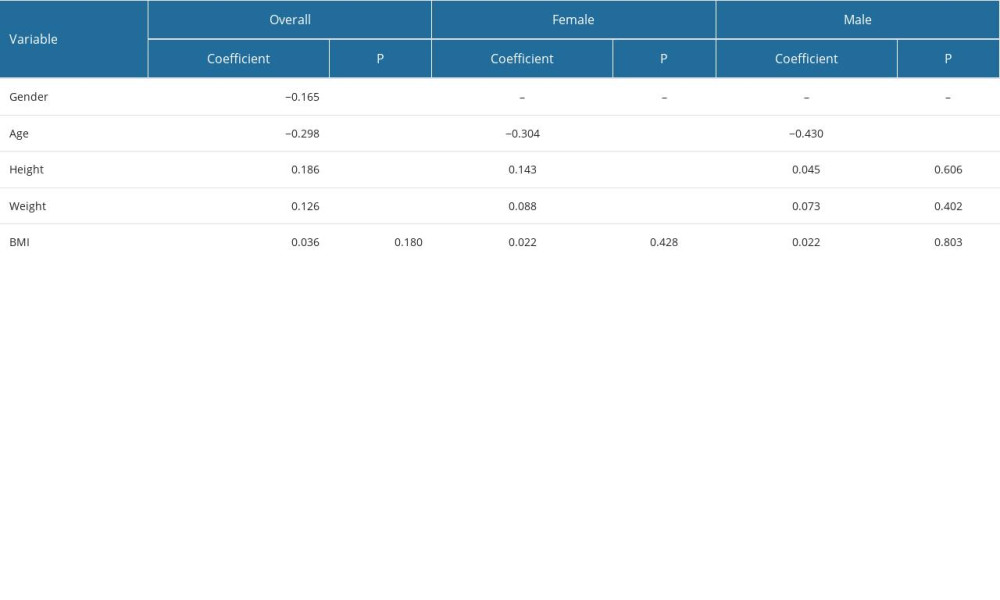 Table 3. Linear regression analysis for overall T score.
Table 3. Linear regression analysis for overall T score.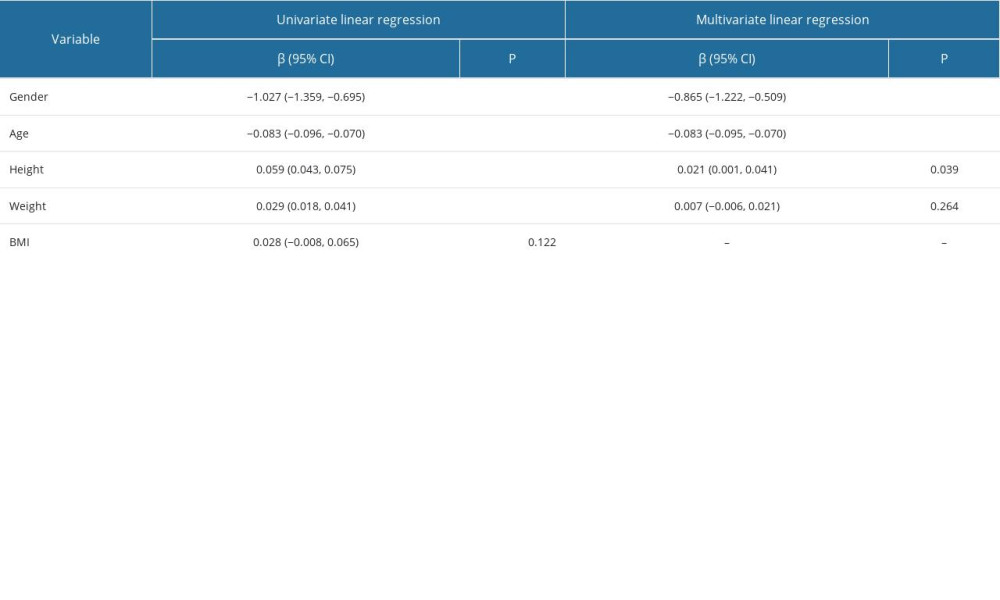 Table 4. Linear regression analysis for the female T score.
Table 4. Linear regression analysis for the female T score.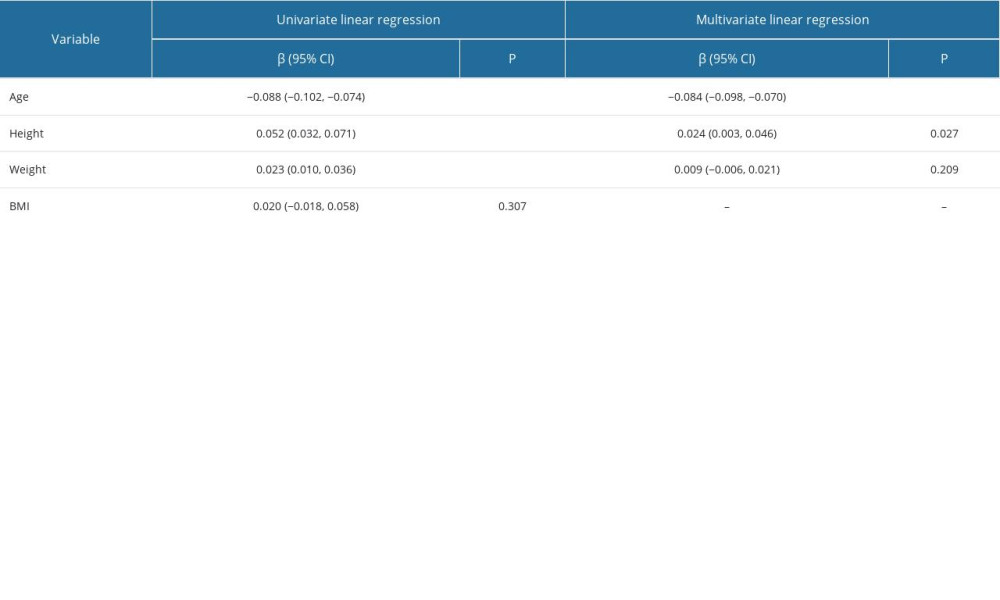 Table 5. Multivariate linear regression analysis for overall fracture risks.
Table 5. Multivariate linear regression analysis for overall fracture risks.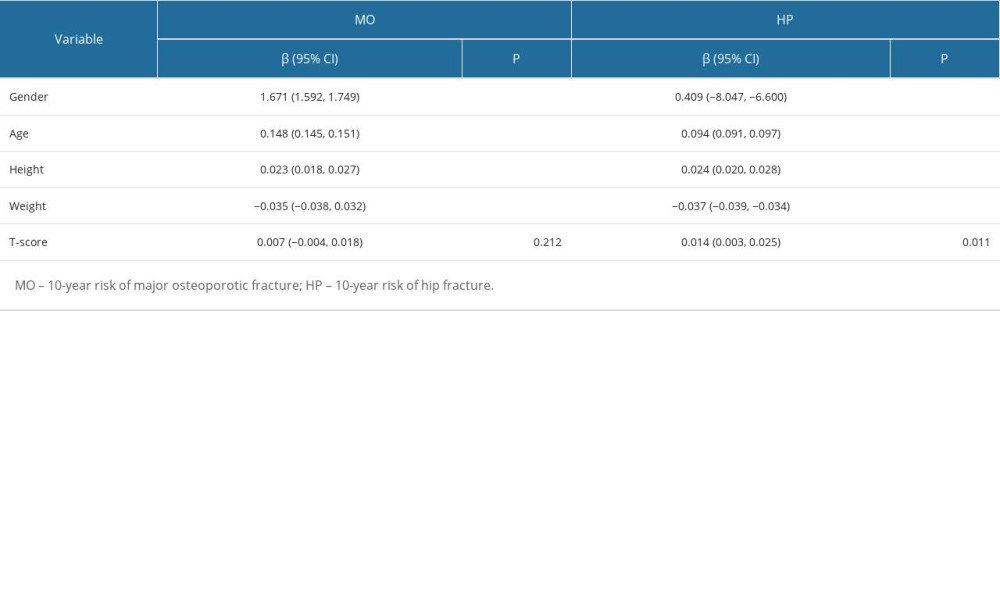 Table 6. Multivariate linear regression analysis for female fracture risks.
Table 6. Multivariate linear regression analysis for female fracture risks.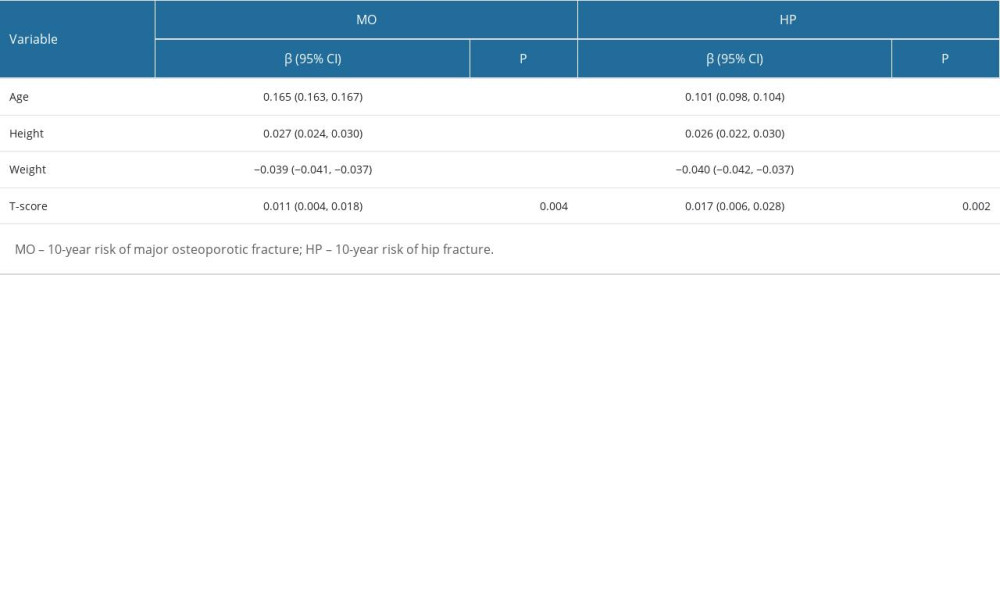
References
1. Leslie WD, Morin SN, Osteoporosis epidemiology 2013: Implications for diagnosis, risk assessment, and treatment: Curr Opin Rheumatol Jul, 2014; 26(4); 440-46
2. Johnston CB, Dagar M, Osteoporosis in Older Adults: Med Clin North Am, 2020; 104(5); 873-84
3. Aaseth J, Boivin G, Andersen O, Osteoporosis and trace elements – an overview: J Trace Elem Med Biol, 2012; 26(2–3); 149-52
4. Chen P, Li Z, Hu Y, Prevalence of osteoporosis in China: A meta-analysis and systematic review: BMC Public Health, 2016; 16(1); 1039
5. Tanski W, Kosiorowska J, Szymanska-Chabowska A, Osteoporosis – risk factors, pharmaceutical and non-pharmaceutical treatment: Eur Rev Med Pharmacol Sci, 2021; 25(9); 3557-66
6. Zeng Q, Li N, Wang Q, The prevalence of osteoporosis in China, a nationwide, multicenter DXA survey: J Bone Miner Res, 2019; 34(10); 1789-97
7. Li Y, Huang Z, Gong Y, Retrospective analysis of the relationship between bone mineral density and body composition in a health check-up Chinese population: Front Endocrinol (Lausanne), 2022; 13; 965758
8. Ulivieri FM, Rinaudo L, Messina C, Bone Strain Index: Preliminary distributional characteristics in a population of women with normal bone mass, osteopenia and osteoporosis: Radiol Med, 2022; 127(10); 1151-58
9. Clo A, Gibellini D, Damiano D, Calcaneal quantitative ultrasound (QUS) and dual X-ray absorptiometry (DXA) bone analysis in adult HIV-positive patients: New Microbiol, 2015; 38(3); 345-56
10. Cournil A, Eymard-Duvernay S, Diouf A, Reduced quantitative ultrasound bone mineral density in HIV-infected patients on antiretroviral therapy in Senegal: PLoS One, 2012; 7(2); e31726
11. Raum K, Grimal Q, Varga P, Ultrasound to assess bone quality: Curr Osteoporos Rep, 2014; 12(2); 154-62
12. Nawrat-Szoltysik A, Miodonska Z, Zarzeczny R, Osteoporosis in Polish older women: Risk factors and osteoporotic fractures: A cross-sectional study: Int J Environ Res Public Health, 2020; 17(10); 3725
13. Cui R, Zhou L, Li Z, Assessment risk of osteoporosis in Chinese people: Relationship among body mass index, serum lipid profiles, blood glucose, and bone mineral density: Clin Interv Aging, 2016; 11; 887-95
14. Kanis JA, Johnell O, Oden A, FRAX and the assessment of fracture probability in men and women from the UK: Osteoporos Int, 2008; 19(4); 385-97
15. Lin J, Yang Y, Fei Q, Validation of three tools for identifying painful new osteoporotic vertebral fractures in older Chinese men: Bone mineral density, Osteoporosis Self-Assessment Tool for Asians, and fracture risk assessment tool: Clin Interv Aging, 2016; 11; 461-69
16. Berger A, Bone mineral density scans: BMJ, 2002; 325(7362); 484
17. Zhang ZQ, Ho SC, Chen ZQ, Reference values of bone mineral density and prevalence of osteoporosis in Chinese adults. Osteoporosis international: A journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA, 2014; 25(2); 497-507
18. Wang L, Yu W, Yin X, Prevalence of osteoporosis and fracture in China: The China osteoporosis prevalence Study: JAMA Netw Open, 2021; 4(8); e2121106
19. GCL , MYZ , CML , Investigation and analysis of incidence of osteoporosis for 9735 cases of bone mineral density population in Jilin city region: Chin J Front Med Sci (Electronic Version), 2014; 6; 90-93
20. Tian L, Yang R, Wei L, Prevalence of osteoporosis and related lifestyle and metabolic factors of postmenopausal women and elderly men: A cross-sectional study in Gansu province, Northwestern of China: Medicine, 2017; 96(43); e8294
21. Forsmo S, Hvam HM, Rea ML, Height loss, forearm bone density and bone loss in menopausal women: A 15-year prospective study. The Nord-Trondelag Health Study, Norway: Osteoporos Int, 2007; 18(9); 1261-69
22. Thornton MJ, Sedlak CA, Doheny MO, Height change and bone mineral density: Revisited: Orthop Nurs, 2004; 23(5); 315-20
23. Nicholson PH, Haddaway MJ, Davie MW, Evans SF, Vertebral deformity, bone mineral density, back pain and height loss in unscreened women over 50 years: Osteoporos Int, 1993; 3(6); 300-7
24. Cawthon PM, Gender differences in osteoporosis and fractures: Clin Orthop Relat Res, 2011; 469(7); 1900-5
25. Fujiwara S, Nakamura T, Orimo H, Development and application of a Japanese model of the WHO fracture risk assessment tool (FRAX™): Osteoporosis Int, 2008; 19(4); 429-35
26. Min YK, Lee DY, Park YS, A FRAX experience in Korea: Fracture risk probabilities with a country-specific versus a surrogate model: J Bone Metab, 2015; 22(3); 113-18
27. Wang J, Wang X, Fang Z, The effect of FRAX on the prediction of osteoporotic fractures in urban middle-aged and elderly healthy Chinese adults: Clinics, 2017; 72(5); 289-93
28. Morin S, Tsang JF, Leslie WD, Weight and body mass index predict bone mineral density and fractures in women aged 40 to 59 years: Osteoporos Int, 2009; 20(3); 363-70
29. Shapses SA, Riedt CS, Bone, body weight, and weight reduction: What are the concerns?: J Nutr, 2006; 136(6); 1453-56
30. Andreo-López MC, Contreras-Bolívar V, García-Fontana B, The influence of the mediterranean dietary pattern on osteoporosis and sarcopenia: Nutrients, 2023; 15(14); 3224
31. Chen H, Avgerinou C, Association of alternative dietary patterns with osteoporosis and fracture risk in older people: A scoping review: Nutrients, 2023; 15(19); 4255
32. Li X, Wang Q, Guo L, Associations between low-carbohydrate diets and low-fat diets with frailty in community-dwelling aging Chinese adults: Nutrients, 2023; 15(14); 3084
33. Liu W, Hu J, Fang Y, Vitamin D status in Mainland of China: A systematic review and meta-analysis: EClinicalMedicine, 2021; 38; 101017
34. Liu J, Ma W, Wei L, Adult serum 25(OH)D3 in Gansu province, northwest China: A cross-sectional study: Asia Pac J Clin Nutr, 2018; 27(4); 832-39
35. Follis SL, Bea J, Klimentidis Y, Psychosocial stress and bone loss among postmenopausal women: Results from the Women’s Health Initiative: J Epidemiol Community Health, 2019; 73(9); 888-92
Tables
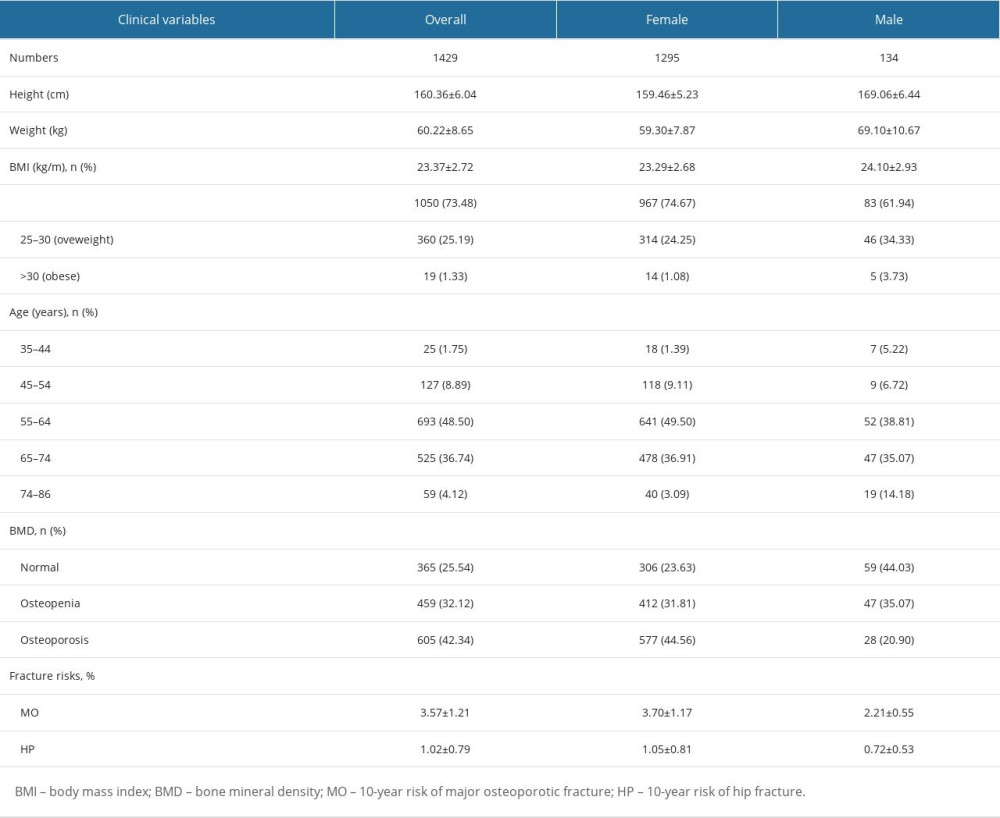 Table 1. Baseline characteristics of overall populations.
Table 1. Baseline characteristics of overall populations.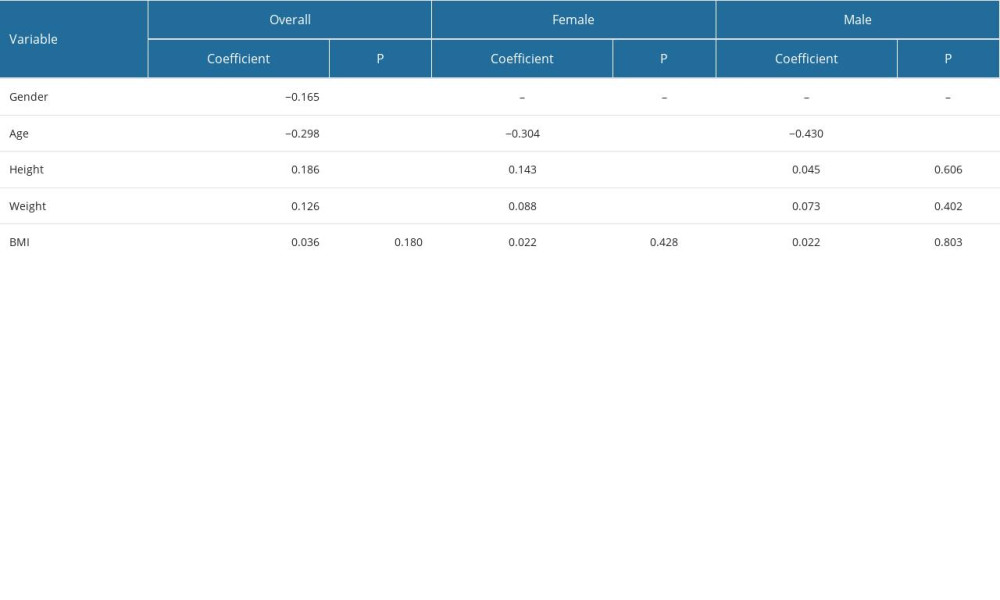 Table 2. Spearman’s rank correlation coefficient for T score.
Table 2. Spearman’s rank correlation coefficient for T score.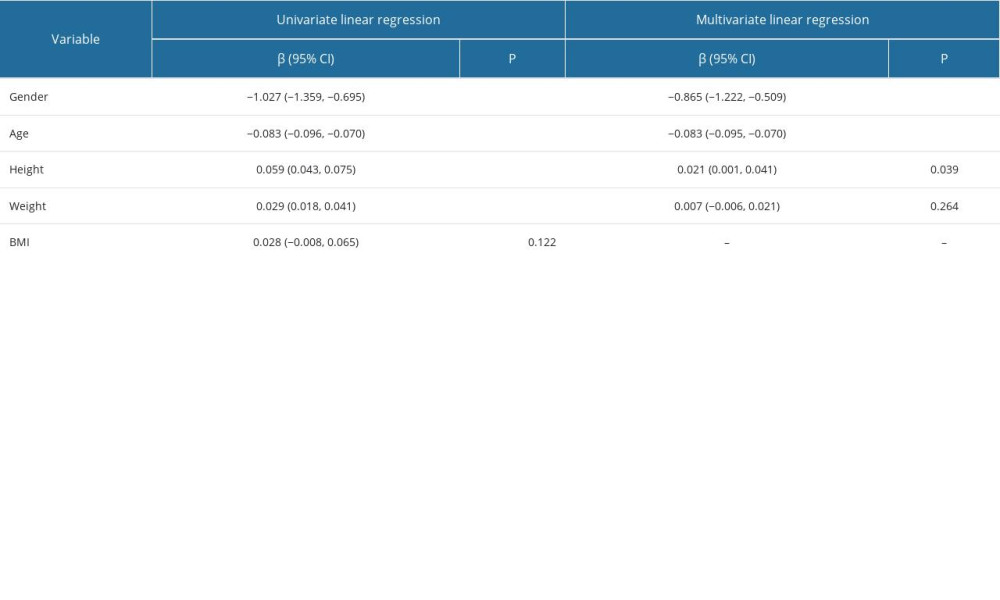 Table 3. Linear regression analysis for overall T score.
Table 3. Linear regression analysis for overall T score.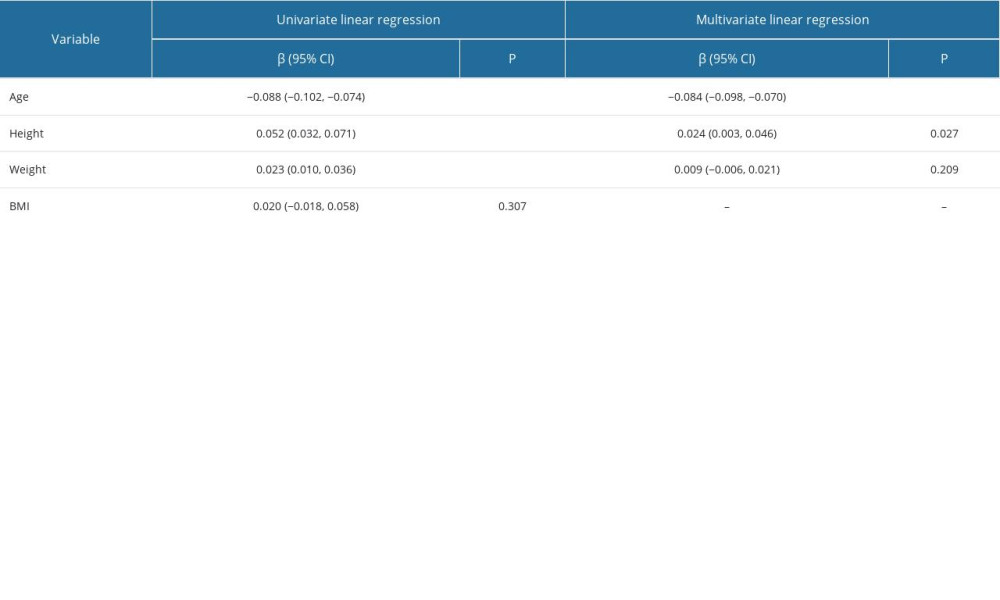 Table 4. Linear regression analysis for the female T score.
Table 4. Linear regression analysis for the female T score.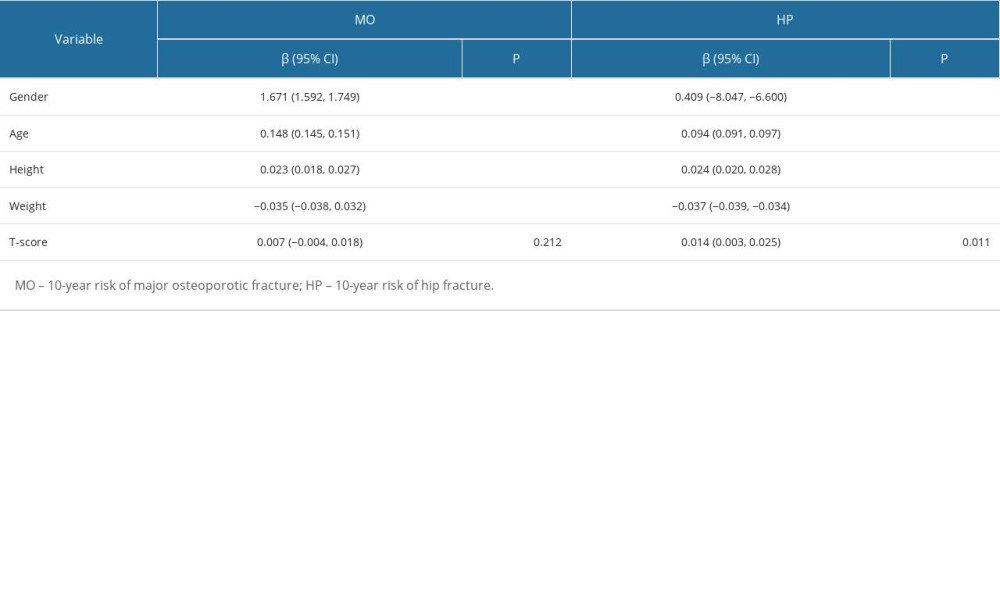 Table 5. Multivariate linear regression analysis for overall fracture risks.
Table 5. Multivariate linear regression analysis for overall fracture risks.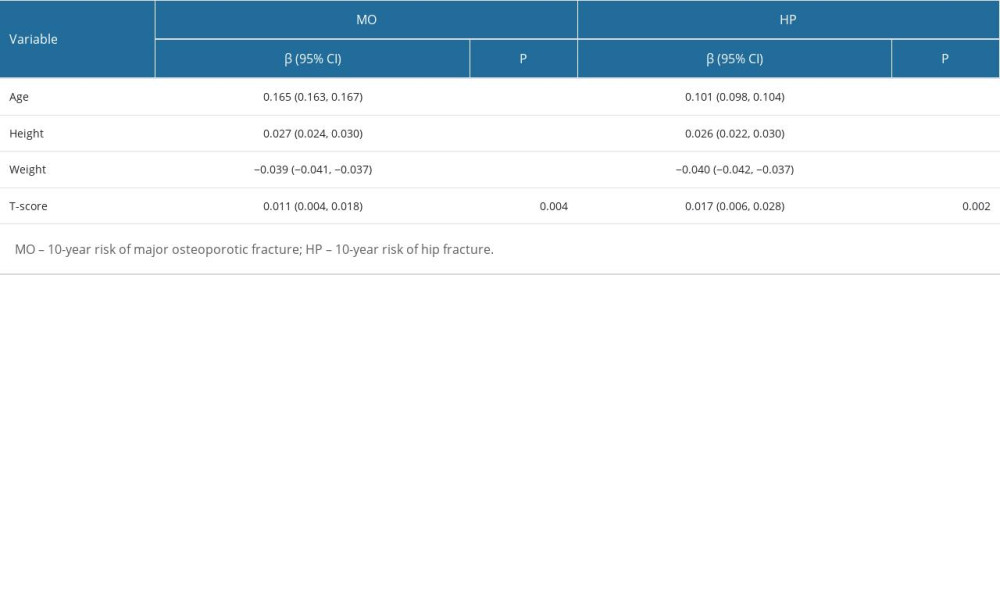 Table 6. Multivariate linear regression analysis for female fracture risks.
Table 6. Multivariate linear regression analysis for female fracture risks. In Press
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
12 Mar 2024 : Clinical Research
Comparing Neuromuscular Blockade Measurement Between Upper Arm (TOF Cuff®) and Eyelid (TOF Scan®) Using Miv...Med Sci Monit In Press; DOI: 10.12659/MSM.943630
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








