16 December 2023: Database Analysis
Laparoscopic Sleeve Gastrectomy: Impact on Body Mass Index and Thyroid Hormones in Euthyroid Obese Patients
Omer Faruk BukDOI: 10.12659/MSM.942692
Med Sci Monit 2023; 29:e942692
Abstract
BACKGROUND: Obesity is still a major global public health problem and its incidence is increasing. Obesity leads to deterioration in thyroid functions. Even when they are within normal ranges, high normal levels of thyroid-stimulating hormone (TSH) increase morbidity and mortality. This study aimed to evaluate the body mass index (BMI) and TSH levels in 300 euthyroid patients with obesity before and after laparoscopic sleeve gastrectomy (LSG).
MATERIAL AND METHODS: A total of 300 euthyroid patients who underwent LSG between 2019 and 2021 were included in the study. Body mass index (BMI), thyroid-stimulating hormone (TSH), and free triiodothyronine (FT) 3 and tetraiodothyronine (FT4) levels were recorded before surgery and at 6 and 12 months after surgery and subsequently analyzed.
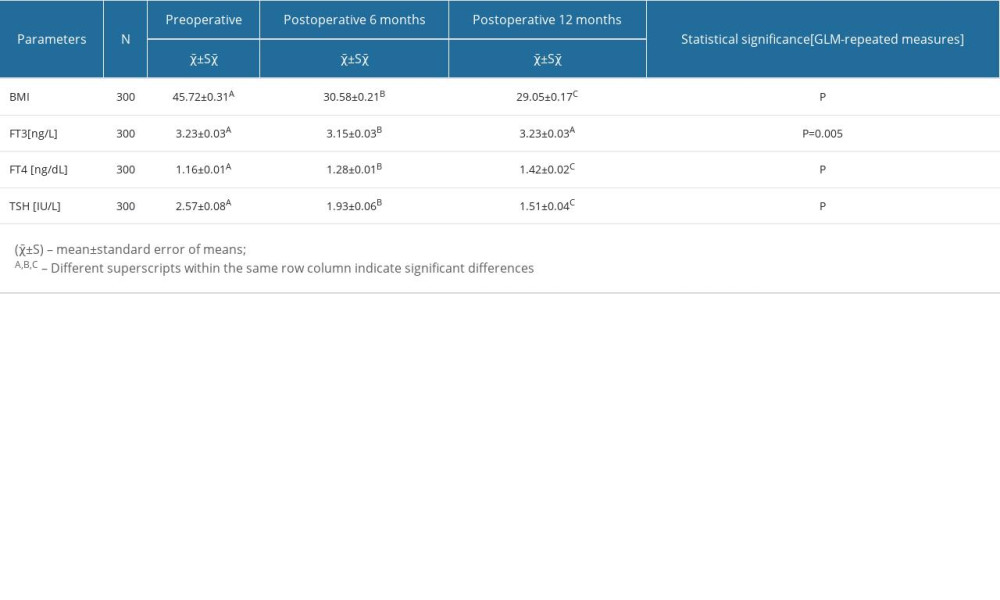
RESULTS: Mean BMI values were significantly lower at 6 and 12 months after surgery (P<0.001). There was a significant difference between mean TSH and FT4 levels before surgery and those at 6 and 12 months after surgery (P<0.001). However, mean FT3 levels remained unchanged 1 year after surgery (P=0.005).
CONCLUSIONS: LSG is not only effective in terms of weight loss, but also exhibits improving effects on thyroid hormone homeostasis in obese patients and provides protection against further adverse effects of TSH.
Keywords: Bariatric Surgery, Thyroid Function Tests, Obesity, Morbid
Background
Obesity is defined as having a body mass index (BMI) of 30 kg/m2 or higher and is classified as follows: class 1 obesity: BMI of 30–34.9; class 2 obesity: BMI of 35–39.9; and class 3 obesity: BMI of 40 or higher. Obesity is still a major global public health problem, and its prevalence has increased worldwide in recent years [1]. Weight loss improves the metabolic functions of various organs and leads to alterations in adipose tissue biological pathways [2].
There is a complex and bidirectional relationship between obesity and thyroid function. Hypothyroidism can lead to obesity, while obesity alters thyroid functions and the markers thereof in plasma, as shown in various studies in recent decades [3,4]. Weight gain causes a gradual increase in thyroid-stimulating hormone (TSH), and increased TSH levels are associated with increased visceral tissue rather than metabolic disturbance [5–7]. While free triiodothyronine (FT3) levels tend to increase in obese patients, free tetraiodothyronine (FT4) levels decrease [8–11]. Therefore, this study aimed to evaluate BMI and TSH levels in 300 euthyroid patients with obesity before and after laparoscopic sleeve gastrectomy (LSG).
Material and Methods
ETHICS STATEMENT:
This study was conducted at the Samsun Hospital Department of Surgery, Turkey, following receipt of approval from the local ethical committee (No. SUKAEK – 2022 11/9).
PATIENTS AND STUDY DESIGN:
Data for patients who underwent LSG between 2019 and 2021 were analyzed. Demographic characteristics and preoperative and 6-month and 12-month postoperative BMI values, excess weight loss rates, and thyroid function tests (TSH, FT3, and FT4 levels) were retrieved from the hospital database system. Patients who received thyroid hormone replacement preoperatively, who did not attend outpatient clinic visits regularly, or who had deficient laboratory results were excluded from the study. Data before surgery and at 6 and 12 months after surgery were compared.
SURGICAL PROCEDURE:
All the surgical procedures were performed by experienced bariatric surgeons, as previously described [12]. The patient was first placed in the supine position. A Veress needle was inserted below the left subcostal margin, and a 10-mm trocar was inserted in the left side of the umbilicus following Veress needle insufflation. Under direct visualization, a 10-mm trocar was inserted in the left anterior axillary line, and the other 5-mm and 12-mm trocars in the right midclavicular line. A Nathanson retractor is used for routine liver retraction in our institution in order to obtain a clear view of the hiatal region. By using bipolar energy devices (LigaSure Medtronic, Covidien product, Minneapolis, MN, USA), the greater curvature of the stomach was released up to the left crus proximally and 4 to 6 cm above to the pylorus. A 36 F bougie was then inserted, and sleeve gastrectomy was performed using tri-staples. Following the methylene blue leak test, the resected stomach was removed from the abdomen from the 12-mm trocar at the right midclavicular line. The trocars were removed under direct observation, and the procedure was completed. The patients were allowed to consume liquid on postoperative day 1 and were discharged on postoperative day 3 or 4.
SAMPLE COLLECTION:
All serum samples were collected after at least 8 h fasting into BD Vacutainer SST II Advance tubes, and thyroid function tests were measured by chemiluminescent immunoassay (Cobas Chemistry Analyzer Series, Roche Diagnostics). References values were as follows: TSH, 0.35–5 μIU/mL; FT3, 2.3–4.2 pg/mL; and FT4: 0.89–1.76 ng/dL.
STATISTICAL ANALYSIS:
Changes in preoperative thyroid function tests and complete blood count parameters and postoperative 6- and 12-month data from patients who underwent LSG were analyzed using general linear models and repeated measurements, and subsequently Tukey’s post-hoc test. The sphericity assumption (sphericity: homogeneity of variances for repeated measures) was assessed with the Mauchly test. Greenhouse-Geisser and Huynd-Feldt corrections were applied in cases in which the assumption of sphericity was not met. The results are expressed as mean±standard mean error. SPSS software (version 21, SPSS, IBM Corp, Armonk, NY, USA) was used for statistical analyses.
Results
PATIENT CHARACTERISTICS:
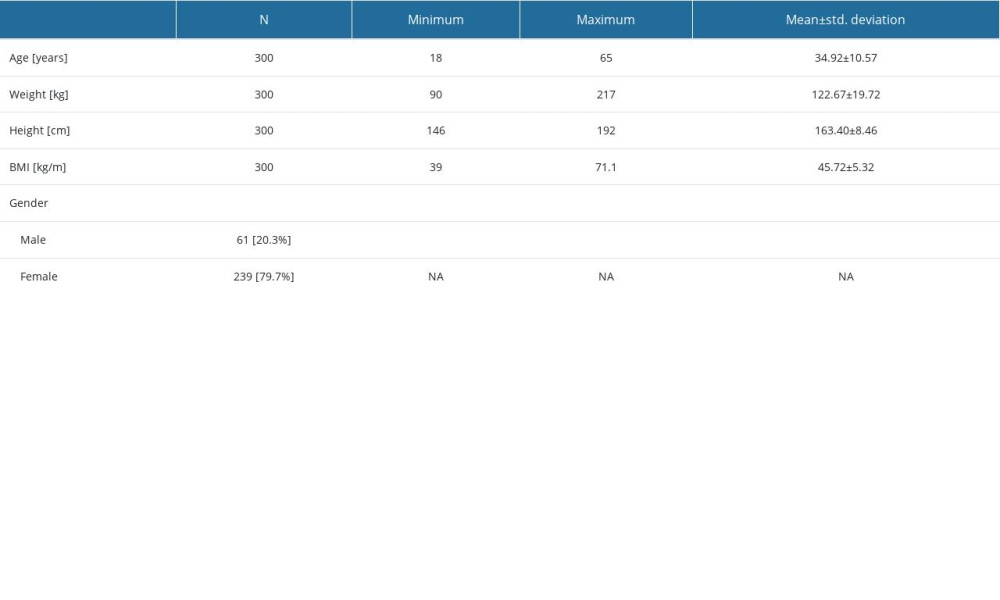
LSG was performed on 338 patients between 2019 and 2021. Eight patients were excluded for receipt of thyroid hormone replacement therapy and 30 were excluded because of loss to follow-up. The remaining 300 patients, 239 women and 61 men, were included in the study. Demographic and descriptive characteristics are summarized in Table 1.
BMI CHANGE:
Mean body BMI values were significantly lower at 6 and 12 months after surgery (
THYROID FUNCTION TESTS:
The mean TSH value was 2.57±0.08 IU/L before surgery, but decreased significantly at 6 and 12 months after surgery (P<0.001). FT3 levels differed significantly between baseline and 6 months after surgery, but no significant difference was observed between levels at baseline and 12 months after surgery. FT4 levels decreased significantly at 6 and 12 months after surgery compared with preoperative levels (P<0.001 for both). A summary of the parameters is shown in Table 2.
Discussion
Leptin is a hormone derived from adipose tissue that suppresses hunger and regulates energy balance. It regulates body weight as well energy expenditure through receptors located in the arcuate nucleus and paraventricular nucleus in the hypothalamus [12,13]. When a positive energy balance occurs in the body, leptin leads to a release of thyrotropin-releasing hormone from the pituitary gland, and thyroid hormone levels therefore rise in order to increase energy expenditure [13,14]. Increased adipose tissue and leptin levels in obesity are associated with the induced activation of the hypotalamo-pituitary-thyroid axis, which leads to an increase in TSH levels [15,16]. Although our patients’ TSH levels were within the reference range, the mean value exceeded 2 mIU/L. Weetman reported that TSH levels above 2 IU/L are associated with an increased risk of further hypothyroidism [17]. Even if within normal ranges, elevated TSH levels are associated with various metabolic alterations, including insulin resistance, elevated blood pressure, hyperlipidemia, inflammation, and hyperglycemia, according to a recent high-volume population-based study by Chang et al, whose findings were also in agreement with those of other studies [18–21]. In our series, postoperative TSH values decreased after LSG to 1.93 and 1.51 IU/L at 6 and 12 months, respectively. We therefore suggest that LSG improves thyroid functions in patients with obesity and also protects the human metabolism against the deleterious effects of TSH described above. Elevated TSH with normal FT3 and FT4 levels (subclinical hypothyroidism) result in endothelial dysfunction, which leads to various disorders, particularly cardiovascular diseases [22]. Some authors have suggested that high normal TSH levels (near the upper limit, >1.93) increase mortality associated with cardiovascular disease and malignancy [23,24]. Orouji et al and Delport et al suggested that high-normal TSH levels can cause infertility in women [25,26]. The European Thyroid Association recently recommended close follow-up of patients with TSH levels higher than 2.5 IU/L [27]. A significant decrease in TSH levels was achieved in our series, and the harmful effects of high-normal TSH levels described above were avoided in those patients.
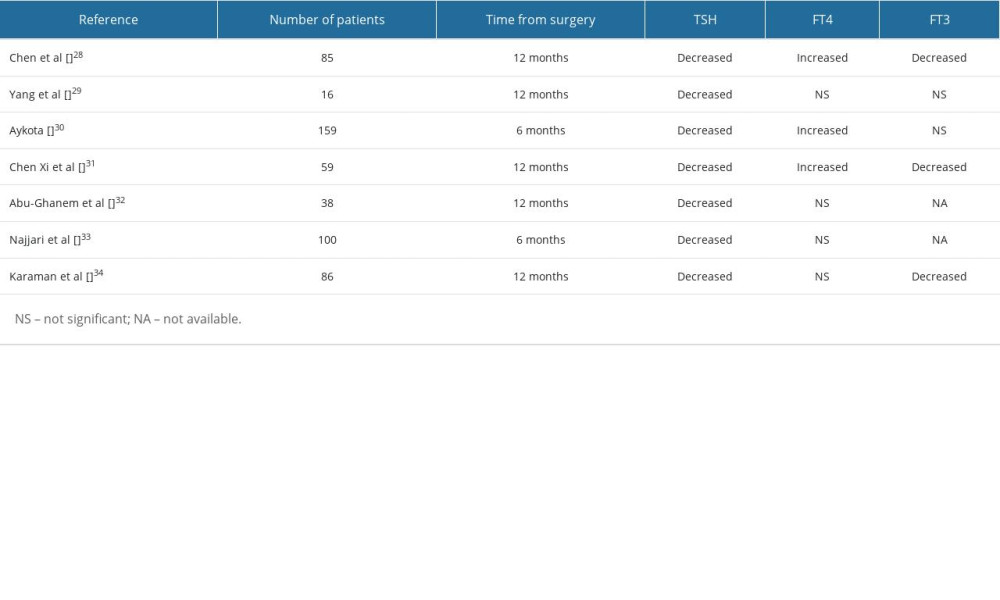
We observed a significant decrease in TSH levels in our cohort. These results were consistent with the results of previous studies, which are summarized in Table 3 [28–34]. However, inconsistent findings regarding FT3 and FT4 levels have been reported in previous studies. In the present study, while a significant increase was observed in FT4 levels, FT3 levels remained unchanged at 12 months after surgery. Published studies have reported inconsistent results. Although Chen Y et al, Chen Xi et al, and Karaman et al reported significant decreases in FT3 levels, Yang et al and Aykota et al reported non-significant increases [28,30–32,34]. In addition, Aykota et al and Chen Xi et al reported significant increases in FT4 levels, in agreement with our findings, although other authors found no significant difference [29–34]. These discrepancies can be related to various factors, including variations in surgical techniques (such as bougie size, distance to the pylorus, and the size of the remaining gastric fundus), BMI changes, individual fatty tissue alterations, and other unknown hormonal changes.
This study has a number of limitations that need to be addressed. First, it was conducted retrospectively and contained no control group including individuals with obesity who had not undergone bariatric surgery. Second, the patients were followed up for only 1 year, therefore the long-term effects of LSG on thyroid hormone status remain unclear. Third, only patients who underwent LSG were included in the study, and the effects of different types of bariatric surgery, including Roux-n-Y gastric bypass, one-anastomosis gastric bypass, and biliary-pancreatic diversion, on thyroid hormone functions could not therefore be compared. Further randomized controlled trials comparing these procedures are needed. Nevertheless, the high number of enrolled patients represents a particular strength of this study.
Conclusions
In conclusion, LSG reduces high normal TSH levels and increases FT4 levels in euthyroid obese patients, and these changes are beneficial for such patients in terms of providing protection against further adverse effects of TSH.
References
1. NCD Risk Factor Collaboration (NCD-RisC), Trends in adult body-mass index in 200 countries from 1975 to 2014: A pooled analysis of 1698 population-based measurement studies with 19·2 million participants: Lancet, 2016; 387(10026); 1377-96 Erratum in: Lancet. 2016;387(10032):1998
2. Magkos F, Fraterrigo G, Yoshino J, Effects of moderate and subsequent progressive weight loss on metabolic function and adipose tissue biology in humans with obesity: Cell Metab, 2016; 23(4); 591-601
3. Kitahara CM, Platz EA, Ladenson PW, Body fatness and markers of thyroid function among U.S. men and women: PLoS One, 2012; 7; e34979
4. Makepeace AE, Bremner AP, O’Leary P, Significant inverse relationship between serum free T4 concentration and body mass index in euthyroid subjects: Differences between smokers and nonsmokers: Clin Endocrinol (Oxf), 2008; 69; 648-52
5. Ren R, Jiang X, Zhang X, Association between thyroid hormones and body fat in euthyroid subjects: Clin Endocrinol (Oxf), 2014; 80; 585-90
6. Muscogiuri G, Sorice GP, Mezza T, High-normal TSH values in obesity: Is it insulin resistance or adipose tissue’s guilt?: Obes (Silver Spring), 2013; 21; 101-6
7. Lips MA, Pijl H, van Klinken JB, Roux-en-Y gastric bypass and calorie restriction induce comparable timedependent effects on thyroid hormone function tests in obese female subjects: Eur J Endocrinol, 2013; 169; 339-47
8. Reinehr T, de Sousa G, Andler W, Hyperthyrotropinemia in obese children is reversible after weight loss and is not related to lipids: J Clin Endocrinol Metab, 2006; 91; 3088-91
9. Nannipieri M, Cecchetti F, Anselmino M, Expression of thyrotropin and thyroid hormone receptors in adipose tissue of patients with morbid obesity and/or type 2 diabetes: Effects of weight loss: Int J Obes (Lond), 2009; 33; 1001-6
10. Rotondi M, Leporati P, La Manna A, Raised serum TSH levels in patients with morbid obesity: Is it enough to diagnose subclinical hypothyroidism?: Eur J Endocrinol, 2009; 160; 403-8
11. Marzullo P, Mele C, Mai S, The impact of the metabolic phenotype on thyroid function in obesity: Diabetol Metab Syndr, 2016; 8; 59
12. Seeras K, Sankararaman S, Lopez PP, Sleeve gastrectomy: StatPearls [Internet] Jan 23, 2023, Treasure Island (FL), StatPearls Publishing
13. Seoane LM, Carro E, Tovar S, Regulation of in vivo TSH secretion by leptin: Regul Pept, 2000; 92(1–3); 25-29
14. Martelli D, Brooks VL, Leptin increases: Physiological roles in the control of sympathetic nerve activity, energy balance, and the hypothalamic-pituitary-thyroid axis: Int J Mol Sci, 2023; 24(3); 2684
15. Feldt-Rasmussen U, Thyroid and leptin: Thyroid, 2007; 17(5); 413-19
16. Bétry C, Challan-Belval MA, Bernard A, Increased TSH in obesity: Evidence for a BMI-independent association with leptin: Diabetes Metab, 2015; 41; 248-51
17. Iacobellis G, Ribaudo MC, Zappaterreno A, Relationship of thyroid function with body mass index, leptin, insulin sensitivity and adiponectin in euthyroid obese women: Clin Endocrinol (Oxf), 2005; 62; 487-91
18. Weetman AP, Hypothyroidism: Screening and subclinical disease: Br Med J, 1997; 314(7088); 1175-78
19. Chang YC, Hua SC, Chang CH, High TSH level within normal range is associated with obesity, dyslipidemia, hypertension, inflammation, hypercoagulability, and the metabolic syndrome: A novel cardiometabolic marker: J Clin Med, 2019; 8(6); 817
20. Lai Y, Wang J, Jiang F, The relationship between serum thyrotropin and components of metabolic syndrome: Endocr J, 2011; 58; 23-30
21. Mehran L, Amouzegar A, Tohidi M, Serum free thyroxine concentration is associated with metabolic syndrome in euthyroid subjects: Thyroid, 2014; 24; 1566-74
22. Asvold BO, Bjøro T, Vatten LJ, Associations of TSH levels within the reference range with future blood pressure and lipid concentrations: 11-year follow-up of the HUNT study: Eur J Endocrinol, 2013; 169; 73-82
23. Lu M, Yang CB, Gao L, Mechanism of subclinical hypothyroidism accelerating endothelial dysfunction (review): Exp Ther Med, 2015; 9(1); 3-10
24. Zhu P, Lao G, Chen C, TSH levels within the normal range and risk of cardiovascular and all-cause mortality among individuals with diabetes: Cardiovasc Diabetol, 2022; 21(1); 254
25. Inoue K, Tsujimoto T, Saito J, Association between serum thyrotropin levels and mortality among euthyroid adults in the United States: Thyroid, 2016; 26(10); 1457-65
26. Orouji Jokar T, Fourman LT, Lee H, Higher TSH levels within the normal range are associated with unexplained infertility: J Clin Endocrinol Metab, 2018; 103(2); 632-39
27. Repelaer van Driel-Delprat CC, van Dam EWCM, van de Ven PM, Live birth rate after intrauterine insemination is not different between women with lower quartile versus higher quartile normal range thyroid stimulating hormone levels: Hum Reprod Open, 2019; 2019(1); hoz002
28. Poppe K, Bisschop P, Fugazzola L, A. 2021 European Thyroid Association Guideline on thyroid disorders prior to and during assisted reproduction: Eur Thyroid J, 2021; 9(6); 281-95 Erratum in: Eur Thyroid J. 2021;10(3):268
29. Chen Y, Zhang W, Pan YChinese obesity, metabolic surgery collaborative, Thyroid function before and after laparoscopic sleeve gastrectomy in patients with obesity: Obes Surg, 2022; 32(6); 1954-61
30. Yang J, Gao Z, Yang W, Effect of sleeve gastrectomy on thyroid function in Chinese euthyroid obese patients: Surg Laparosc Endosc Percutan Tech, 2017; 27(4); e66-e68
31. Aykota MR, Atabey M, Effect of sleeve gastrectomy on thyroid-stimulating hormone levels in morbidly obese patients with normal thyroid function: Eur Rev Med Pharmacol Sci, 2021; 25(1); 233-40
32. Chen X, Zhang C, Liu W, Laparoscopic sleeve gastrectomy-induced decreases in FT3 and TSH are related to fasting C-peptide in euthyroid patients with obesity: Diabetes Metab Syndr Obes, 2020; 13; 4077-84
33. Abu-Ghanem Y, Inbar R, Tyomkin V, Effect of sleeve gastrectomy on thyroid hormone levels: Obes Surg, 2015; 25(3); 452-56
34. Najjari K, Talebpour M, Mahmoudabadi HZ, Effect of laparoscopic sleeve gastrectomy vs. OAGB on thyroid function tests in patients with morbid obesity and subclinical or clinical hypothyroidism: Obes Surg, 2021; 31(11); 4808-14
35. Karaman K, Mansıroglu K, Subasi O, Thyroid hormone changes after sleeve gastrectomy with and without antral preservation: Obes Surg, 2021; 31(1); 224-31
36. Juiz-Valiña P, Outeiriño-Blanco E, Pértega S, Effect of weight loss after bariatric surgery on thyroid-stimulating hormone levels in euthyroid patients with morbid obesity: Nutrients, 2019; 11(5); 1121
In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952