04 March 2024: Clinical Research
Comparison of Modified Shock Index and Shock Index for Predicting Massive Transfusion in Women with Primary Postpartum Hemorrhage: A Retrospective Study
Hyojeong Kwon1CDEF, Chang Hwan Sohn1ABCDEF*, Sang-Min Kim1CDF, Youn-Jung Kim1DF, Seung Mok Ryoo1DF, Shin Ahn1DF, Dong-Woo Seo1DF, Won Young Kim1DFDOI: 10.12659/MSM.943286
Med Sci Monit 2024; 30:e943286
Abstract
BACKGROUND: The modified shock index (MSI) is calculated as the ratio of heart rate (HR) to mean arterial pressure (MAP) and has been used to predict the need for massive transfusion (MT) in trauma patients. This retrospective study from a single center aimed to compare the MSI with the traditional shock index (SI) to predict the need for MT in 612 women diagnosed with primary postpartum hemorrhage (PPH) at the Emergency Department (ED) between January 2004 and August 2023.
MATERIAL AND METHODS: The patients were divided into the MT group and the non-MT group. The predictive power of MSI and SI was compared using the areas under the receiver operating characteristic curve (AUC). The sensitivity, specificity, positive predictive value (PPV), and negative predictive value were calculated.
RESULTS: Out of 612 patients, 105 (17.2%) required MT. The MT group had higher median values than the non-MT group for MSI (1.58 vs 1.07, P<0.001) and SI (1.22 vs 0.80, P<0.001). The AUC for MSI, with a value of 0.811 (95% confidence interval [CI], 0.778-0.841), did not demonstrate a significant difference compared to the AUC for SI, which was 0.829 (95% CI, 0.797-0.858) (P=0.066). The optimal cutoff values for MSI and SI were 1.34 and 1.07, respectively. The specificity and PPV for MT were 77.1% and 40.2% for MSI, and 83.2% and 45.9% for SI.
CONCLUSIONS: Both MSI and SI were effective in predicting MT in patients with primary PPH. However, MSI did not demonstrate superior performance to SI.
Keywords: Blood Transfusion, Postpartum Hemorrhage, Predictive Value of Tests
Background
Primary postpartum hemorrhage (PPH) is a major cause of maternal morbidity and mortality in both developed and developing countries [1]. To reduce maternal morbidity and mortality from PPH, it is essential to accurately and promptly predict the severity of PPH and provide timely resuscitation. However, previous studies have demonstrated the inaccuracy of estimating the severity of PPH based solely on blood loss [2–6]. This presents challenges for emergency physicians and obstetricians. Dealing with patients transferred from other hospitals, particularly in the emergency department (ED), can further complicate this challenge. Thus, ensuring the swift and accurate identification of patients at risk of severe hemorrhagic shock, particularly those who require immediate massive transfusion (MT) during the initial phase of resuscitation, is crucial for optimizing patient outcomes.
The traditional shock index (SI), which is calculated as the ratio of heart rate (HR) to systolic blood pressure (SBP), has been used as a parameter to assess hemodynamic instability [7–9]. Recently, it has also been used to predict the need for MT in traumatic, surgical, and obstetric emergencies [10,11]. The modified shock index (MSI) is calculated by substituting mean arterial pressure (MAP) for SBP in the SI [12]. This adjustment takes into account the importance of diastolic blood pressure (DBP) when evaluating patients’ clinical condition. It has been shown to have better predictive performance for mortality compared to SI [12]. Some studies have indicated that MSI is more effective than SI in predicting outcomes for adult trauma patients [12,13]. Although studies have compared MSI and SI for predicting the need for MT in trauma patients, no similar investigations have been conducted for PPH patients.
Therefore, this retrospective study from a single center aimed to compare the modified shock index with the shock index to predict the need for MT in 612 women diagnosed with primary PPH between January 2004 and August 2023.
Material and Methods
ETHICS STATEMENT:
The study protocol was approved by the Institutional Review Board of Asan Medical Center, and the requirement for informed consent was waived due to the retrospective nature of the study (No. 2023-1596).
STUDY DESIGN AND SETTING:
This retrospective observational study was conducted in an ED with an annual census of approximately 120 000 visits at a university-affiliated teaching hospital in South Korea. All patients with primary PPH who visited the ED between January 2004 and August 2023 were included. Primary PPH is defined as bleeding that requires a blood transfusion or fluid resuscitation within the first 24 hours after delivery [14]. None of the patients included in this study underwent delivery at our medical institution. Instead, patients were referred to our ED from other medical facilities or obstetric clinics for the assessment and management of primary PPH. The primary outcome was the need for MT, which was defined as receiving 10 or more units of packed red blood cells (pRBC) within the first 24 hours [15]. Patients were divided into the MT group and the non-MT group.
DATA COLLECTION:
We reviewed the electronic medical records to collect demographic and clinical data, including age, parity, type of delivery, initial mental status, initial vital signs (SBP, DBP, HR, respiratory rate, and body temperature), and initial laboratory findings. MSI and SI were calculated using the initial vital signs obtained upon the patient’s arrival at the ED during the triage process. The MSI was calculated as the ratio of HR to MAP, represented as (SBP+2×DBP)/3. The SI was calculated by dividing HR by SBP. The study evaluated clinical outcomes, including embolization, hysterectomy, duration of hospital stay, admission to the intensive care unit (ICU), and in-hospital mortality. We measured the total amount of blood transfused before the patient’s admission to the ED and the amount of blood transfused after their arrival. This included encompassing transfusions given in the ED as well as in subsequent care settings like the ICU or general ward, to identify cases of MT. The decision of whether a blood transfusion was necessary, the specific blood type required, and the amount of blood given to patients with primary PPH was solely based on the clinical judgment of the attending emergency physicians or obstetricians.
STATISTICAL ANALYSIS:
Continuous variables were summarized using either the mean and standard deviation or the median and interquartile range, depending on the normality of the distribution as determined by the Kolmogorov-Smirnov test. The categorical data were presented as absolute counts and percentages. The characteristics of the groups were compared using either the Mann-Whitney U test or the t test for continuous variables, and the chi-square or Fisher’s exact tests for categorical variables. The ability of MSI and SI to predict MT was evaluated using a receiver operating characteristic (ROC) curve, with the area under the curve (AUC) indicating predictive accuracy. The optimal cutoff values for MSI and SI in predicting MT were determined using Youden’s index. High accuracy was defined as an AUC greater than 0.9, while moderate accuracy was indicated by an AUC ranging from 0.7 to 0.9. Low accuracy was determined when the AUC was below 0.7 [16]. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio (PLR), and negative likelihood ratio (NLR) were calculated to compare the performance of MSI and SI for predicting MT. The comparison of the 2 independent ROC curves was conducted using DeLong’s test [17]. A two-tailed P value of less than 0.05 was considered statistically significant. All statistical analyses were performed using IBM SPSS Statistics for Windows, Version 21.0 (IBM Corp., Armonk, NY, USA) and MedCalc® Statistical Software version 20.116 (MedCalc Software Ltd, Ostend, Belgium).
Results
BASELINE CHARACTERISTICS:
A total of 612 patients with primary PPH visited the ED during the study period, and all of them were included in the analysis. Out of these, 105 (17.2%) required MT. Table 1 shows the baseline demographics and clinical characteristics of the patients. There were no significant differences in age, parity, type of delivery, or body temperature between the groups. However, there was a significant difference in the initial mental status between the 2 groups (P<0.001). The MT group had significantly lower SBP, DBP, and MAP, and higher HR upon their arrival at the ED compared to the non-MT group. The initial MSI and SI were significantly higher in the MT group compared to the non-MT group, with values of 1.58 vs 1.07 (P<0.001) and 1.22 vs 0.80 (P<0.001), respectively.
COMPARISON OF CLINICAL PARAMETERS BETWEEN THE MT AND NON-MT GROUPS:
The comparison of initial laboratory findings, blood transfusion amounts, and clinical outcomes between the 2 groups is presented in Table 2. The MT group had significantly lower levels of hemoglobin, hematocrit, and platelet count, as well as a prolonged prothrombin time, compared to the non-MT group. The MT group received a significantly higher amount of pRBCs within the first 24 hours, with a median of 13.0 (11.0–20.0) units, compared to the non-MT group, which received 3.0 (1.0–5.0) units (P<0.001). Additionally, the MT group received significantly larger quantities of other blood components, such as fresh frozen plasma (FFP) and platelet concentrate (PC). In the MT group, there were higher frequencies of embolization and hysterectomy compared to the non-MT group. Additionally, the MT group had a higher rate of ICU admissions and longer hospital stays. In-hospital mortality showed a significant difference between the 2 groups, with all deaths occurring only in the MT group.
PREDICTIVE PERFORMANCE OF MSI AND SI FOR PREDICTING MT:
The ROC curve analysis showed that the AUC value for predicting the need for MT in MSI was 0.811 (95% confidence interval [CI], 0.778–0.841; P<0.001), indicating moderate accuracy. The value showed no significant difference compared to the AUC for SI, which was 0.829 (95% CI, 0.797–0.858; P<0.001) (P=0.066) (Figure 1). Table 3 shows the optimal cutoff values of MSI and SI to predict MT. The MSI higher than 1.34 had a sensitivity of 74.3%, specificity of 77.1%, PPV of 40.2%, NPV of 93.5%, PLR of 3.25, and NLR of 0.33 in predicting MT. The SI, with a cutoff value of 1.07, predicted the MT with a sensitivity of 68.6%, specificity of 83.2%, PPV of 45.9%, NPV of 92.7%, PLR of 4.09, and NLR of 0.38.
Discussion
In this study, we compared the accuracy of MSI and SI in predicting MT in ED patients with primary PPH. Both MSI and SI calculated from the initial vital signs showed moderate accuracy in predicting MT. There was no significant difference in the predictive power of MSI compared to SI.
The prompt recognition of severe hemorrhage in patients with PPH and the timely initiation of resuscitation are essential for improving patient care, efficiently managing resources, and determining the appropriate patient management plan [14]. Vogt et al found that early activation of a MT protocol during resuscitation has a dual advantage: it improves patient outcomes and reduces the need for blood components, leading to a decrease in associated complications [18]. However, identifying high-risk patients who require MT during severe hemorrhage has been challenging. Factors such as SI, lactate, and delta neutrophil index have been reported to be associated with the need for MT in patients with primary PPH [10,15,19].
SI, calculated as HR divided by SBP, is a readily accessible parameter for assessing hemodynamic instability [7–9]. The clinical value of SI has been systematically assessed as a predictive tool for various medical conditions. These include detecting ongoing intraoperative bleeding, determining the need for urgent interventions in cases of gastrointestinal hemorrhage, recognizing sepsis early, and differentiating between major and minor injuries [20–22]. The SI, typically ranging from 0.5 to 0.7, is a clinical marker used to identify hypovolemic shock upon arrival at the ED. It is particularly useful in determining the need for transfusion and hemostatic resuscitation [23]. Le Bas et al [24] conducted an assessment to establish the standard range for the ‘obstetric shock index’ after childbirth. They determined that the normal range for the shock index is between 0.7 and 0.9. Additionally, they suggested that a shock index greater than 1.0 is a useful indicator for estimating blood loss in cases of severe PPH and for predicting the need for blood transfusions. We found that the initial SI was independently associated with the need for MT in ED patients with primary PPH, with an odds ratio of 9.47 (95% CI, 1.75–51.28;
However, SI, which only considers SBP, overlooks the important role of DBP in evaluating a patient’s clinical severity. Conversely, MAP, which includes both SBP and DBP, is widely recognized as a clinical indicator of organ perfusion [25–29]. Liu et al introduced the MSI as a method to predict the severity of critically ill patients. Instead of using SBP, MSI divides HR by MAP, resulting in an improved ability to predict outcomes. An MSI of 1.3 or higher is associated with increased ICU admission and mortality [12]. Several studies have compared MSI and SI as tools for assessing hemodynamic instability and predicting patient outcomes. Liu et al showed that MSI is a superior predictor of mortality among ED patients compared to SI, HR, and blood pressure alone [12]. Similarly, Singh et al found that MSI is a more effective predictor of hospital mortality in adult trauma patients in the ED compared to using HR, SBP, DBP, and SI as standalone indicators [13]. Several studies have evaluated the accuracy of MSI and SI in predicting the need for MT in trauma patients. Rau et al evaluated the predictive abilities of MSI and SI in predicting MT in trauma patients. The predictive power of MSI was not higher than that of SI, with AUCs of 0.756 (sensitivity: 0.615 and specificity: 0.823) and 0.760 (sensitivity: 0.563 and specificity: 0.876), respectively [30]. Similarly, Sharma et al [31] and Wang et al [32] have shown that prehospital MSI and prehospital SI are equally effective in predicting MT in trauma patients.
To the best of our knowledge, this study is the first to compare MSI and SI in predicting MT in patients presenting to ED with primary PPH, analyzing data spanning over 2 decades. Both MSI and SI showed moderate accuracy in predicting MT, with AUC values of 0.811 (95% CI, 0.778–0.841) and 0.829 (95% CI, 0.797–0.858), respectively. However, MSI did not demonstrate superior discriminative power compared to SI in predicting MT (
This study has several limitations. Firstly, the retrospective design of the study introduced potential biases and confounding factors. Secondly, the analysis was limited to patients who presented at the ED of a single medical center, which limits the generalizability of the results to patients in other settings, such as labor and delivery units, obstetric clinics, or different healthcare institutions. A well-designed prospective study is required to validate the findings of the study. Finally, the 20-year duration of the study may have led to variations in clinical outcomes. However, it is important to note that the definitions for the relevant terms remained unchanged, making it unlikely that any differences in outcomes can be attributed to this factor. Despite this, advancements in clinical practices and changes in treatment guidelines may have influenced the clinical outcomes of primary PPH.
Conclusions
Both MSI and SI were effective in predicting MT in patients with primary PPH. However, MSI did not demonstrate superior performance to SI.
Tables
Table 1. Baseline demographic and clinical characteristics of the study patients.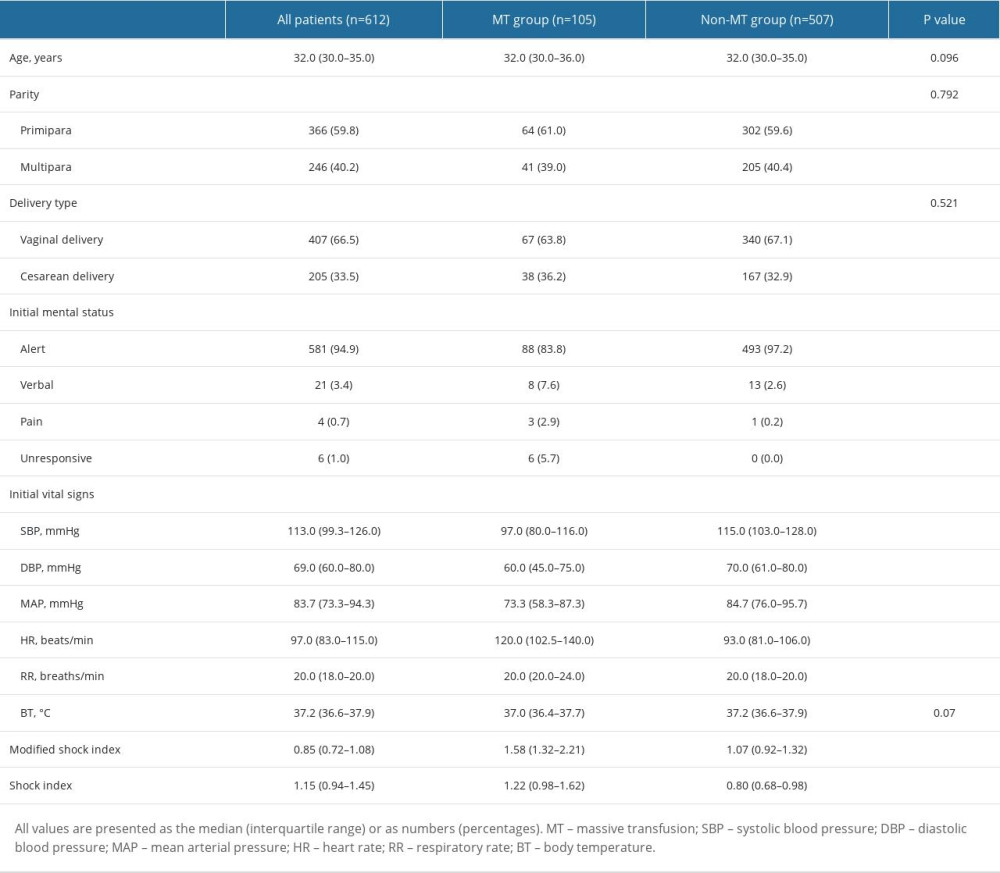 Table 2. A comparison of laboratory findings, blood transfusion amounts, and clinical outcomes based on massive transfusion in patients with primary postpartum hemorrhage.
Table 2. A comparison of laboratory findings, blood transfusion amounts, and clinical outcomes based on massive transfusion in patients with primary postpartum hemorrhage.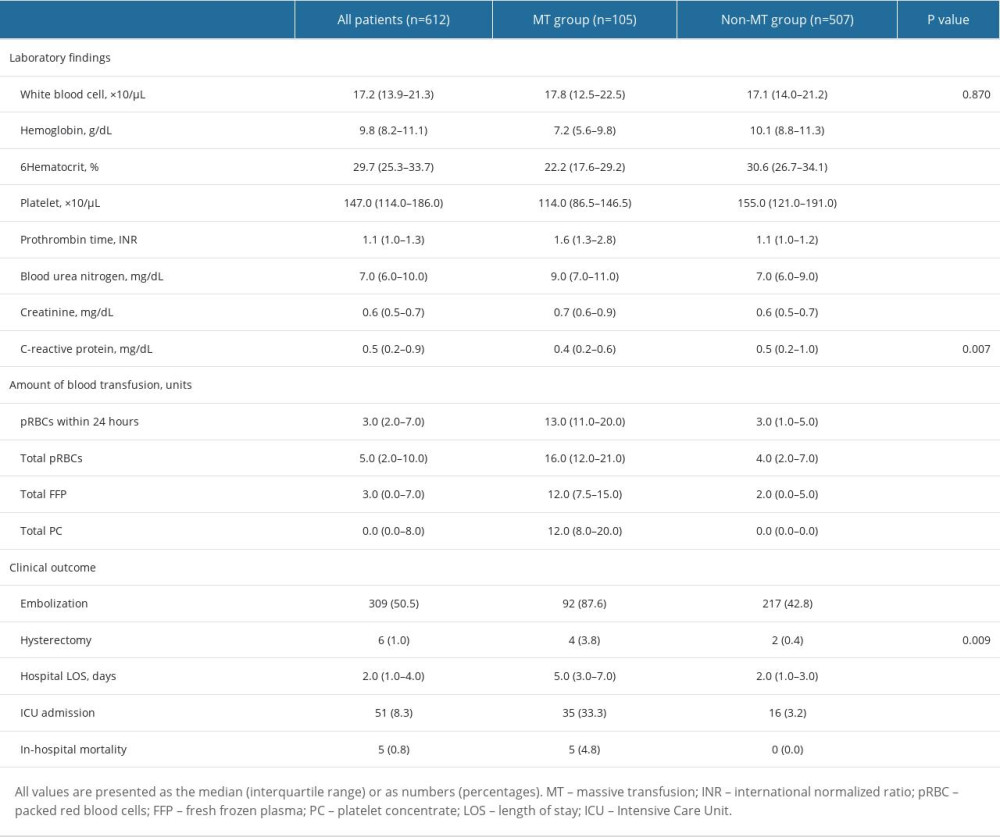 Table 3. Optimal cutoff value and predictive power of modified shock index and shock index for massive transfusion in primary postpartum hemorrhage.
Table 3. Optimal cutoff value and predictive power of modified shock index and shock index for massive transfusion in primary postpartum hemorrhage.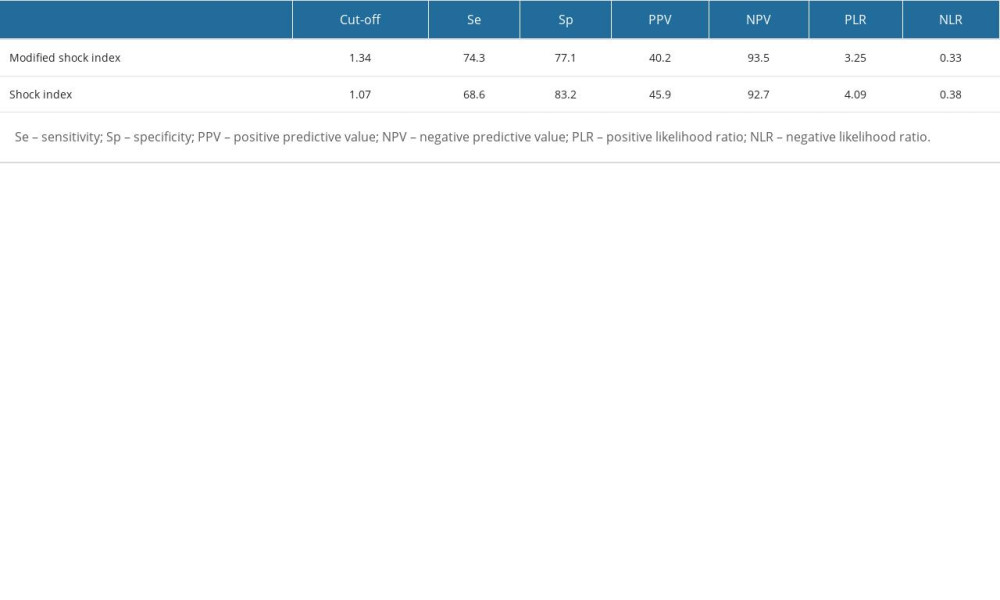
References
1. Mousa HA, Blum J, El Abou Senoun G, Treatment for primary postpartum haemorrhage: Cochrane Database Syst Rev, 2014; 2014(2); CD003249
2. Brant H, Precise estimation of postpartum haemorrhage: Difficulties and importance: Br Med J, 1967; 1(5537); 398-400
3. Duthie SJ, Ven D, Yung GL, Discrepancy between laboratory determination and visual estimation of blood loss during normal delivery: Eur J Obstet Gynecol Reprod Biol, 1991; 38(2); 119-24
4. Larsson C, Saltvedt S, Wiklund I, Estimation of blood loss after cesarean section and vaginal delivery has low validity with a tendency to exaggeration: Acta Obstet Gynecol Scand, 2006; 85(12); 1448-52
5. Strote J, Mayo M, Townes D, ED patient estimation of blood loss: Am J Emerg Med, 2009; 27(6); 709-11
6. Ashburn JC, Harrison T, Ham JJ, Strote J, Emergency physician estimation of blood loss: West J Emerg Med, 2012; 13(4); 376-79
7. Mitra B, Fitzgerald M, Chan J, The utility of a shock index ≥1 as an indication for pre-hospital oxygen carrier administration in major trauma: Injury, 2014; 45(1); 61-65
8. McNab A, Burns B, Bhullar I, An analysis of shock index as a correlate for outcomes in trauma by age group: Surgery, 2013; 154(2); 384-87
9. DeMuro JP, Simmons S, Jax J, Gianelli SM, Application of the shock index to the prediction of need for hemostasis intervention: Am J Emerg Med, 2013; 31(8); 1260-63
10. Sohn CH, Kim WY, Kim SR, An increase in initial shock index is associated with the requirement for massive transfusion in Emergency Department patients with primary postpartum hemorrhage: Shock, 2013; 40(2); 101-5
11. Lee SY, Kim HY, Cho GJ, Use of the shock index to predict maternal outcomes in women referred for postpartum hemorrhage: Int J Gynaecol Obstet, 2019; 144(2); 221-24
12. Liu Y-c, Liu J-h, Fang ZA, Modified shock index and mortality rate of emergency patients: World J Emerg Med, 2012; 3(2); 114-17
13. Singh A, Ali S, Agarwal A, Srivastava RN, Correlation of shock index and modified shock index with the outcome of adult trauma patients: a prospective study of 9860 patients: N Am J Med Sci, 2014; 6(9); 450-52
14. Sohn C, Kim Y-J, Seo D, Blood lactate concentration and shock index associated with massive transfusion in Emergency Department patients with primary postpartum haemorrhage: Br J Anaesth, 2018; 121(2); 378-83
15. Sohn CH, Kim SR, Kim Y-J, Disseminated intravascular coagulation in Emergency Department patients with primary postpartum hemorrhage: Shock, 2017; 48(3); 329-32
16. Akobeng AK, Understanding diagnostic tests 3: Receiver operating characteristic curves: Acta Paediatr, 2007; 96(5); 644-47
17. DeLong ER, DeLong DM, Clarke-Pearson DL, Comparing the areas under two or more correlated receiver operating characteristic curves: A nonparametric approach: Biometrics, 1988; 44(3); 837-45
18. Vogt K, Van Koughnett J, Dubois L, The use of trauma transfusion pathways for blood component transfusion in the civilian population: A systematic review and meta-analysis: Transfus Med, 2012; 22(3); 156-66
19. Kong T, Lee HS, Jeon SY, Delta neutrophil index and shock index can stratify risk for the requirement for massive transfusion in patients with primary postpartum hemorrhage in the Emergency Department: PLoS One, 2021; 16(10); e0258619
20. Asaari H, Value of shock index in prognosticating the short term outcome of death for patients presenting with severe sepsis and septic shock in the Emergency Department: Med J Malaysia, 2012; 67(4); 406-11
21. Rady MY, Smithline HA, Blake H, A comparison of the shock index and conventional vital signs to identify acute, critical illness in the Emergency Department: Ann Emerg Med, 1994; 24(4); 685-90
22. King RW, Plewa MC, Buderer NMF, Knotts FB, Shock index as a marker for significant injury in trauma patients: Acad Emerg Med, 1996; 3(11); 1041-45
23. Mutschler M, Nienaber U, Münzberg M: Crit Care, 2013; 17(4); R172
24. Le Bas A, Chandraharan E, Addei A, Arulkumaran S, Use of the “obstetric shock index” as an adjunct in identifying significant blood loss in patients with massive postpartum hemorrhage: Int J Gynaecol Obstet, 2014; 124(3); 253-55
25. LeDoux D, Astiz ME, Carpati CM, Rackow EC, Effects of perfusion pressure on tissue perfusion in septic shock: Crit Care Med, 2000; 28(8); 2729-32
26. Maheshwari K, Nathanson BH, Munson SH, The relationship between ICU hypotension and in-hospital mortality and morbidity in septic patients: Intensive Care Med, 2018; 44(6); 857-67
27. Dünser MW, Takala J, Ulmer H, Arterial blood pressure during early sepsis and outcome: Intensive Care Med, 2009; 35(7); 1225-33
28. Khanna AK, Maheshwari K, Mao G, Association between mean arterial pressure and acute kidney injury and a composite of myocardial injury and mortality in postoperative critically ill patients: A retrospective cohort analysis: Crit Care Med, 2019; 47(7); 910-17
29. Varpula M, Tallgren M, Saukkonen K, Hemodynamic variables related to outcome in septic shock: Intensive Care Med, 2005; 31(8); 1066-71
30. Rau CS, Wu SC, Kuo SC, Prediction of massive transfusion in trauma patients with shock index, modified shock index, and age shock index: Int J Environ Res Public Health, 2016; 13(7); 683
31. Sharma A, Satish UN, Tevatia M, Singh S, Prehospital shock index, modified shock index, and pulse pressure heart rate ratio as predictors of massive blood transfusions in modern warfare injuries: A retrospective analysis: Med J Armed Forces India, 2019; 75(2); 171-75
32. Wang I-J, Bae B-K, Park S-W, Pre-hospital modified shock index for prediction of massive transfusion and mortality in trauma patients: Am J Emerg Med, 2020; 38(2); 187-90
Tables
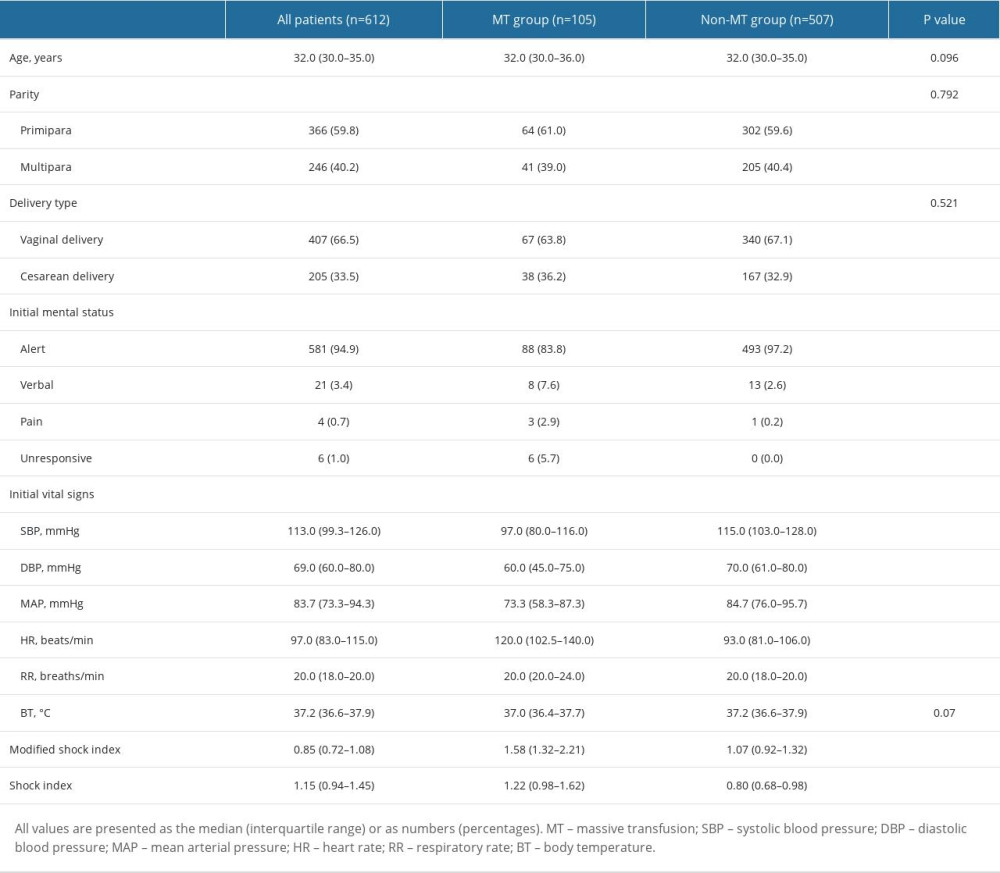 Table 1. Baseline demographic and clinical characteristics of the study patients.
Table 1. Baseline demographic and clinical characteristics of the study patients.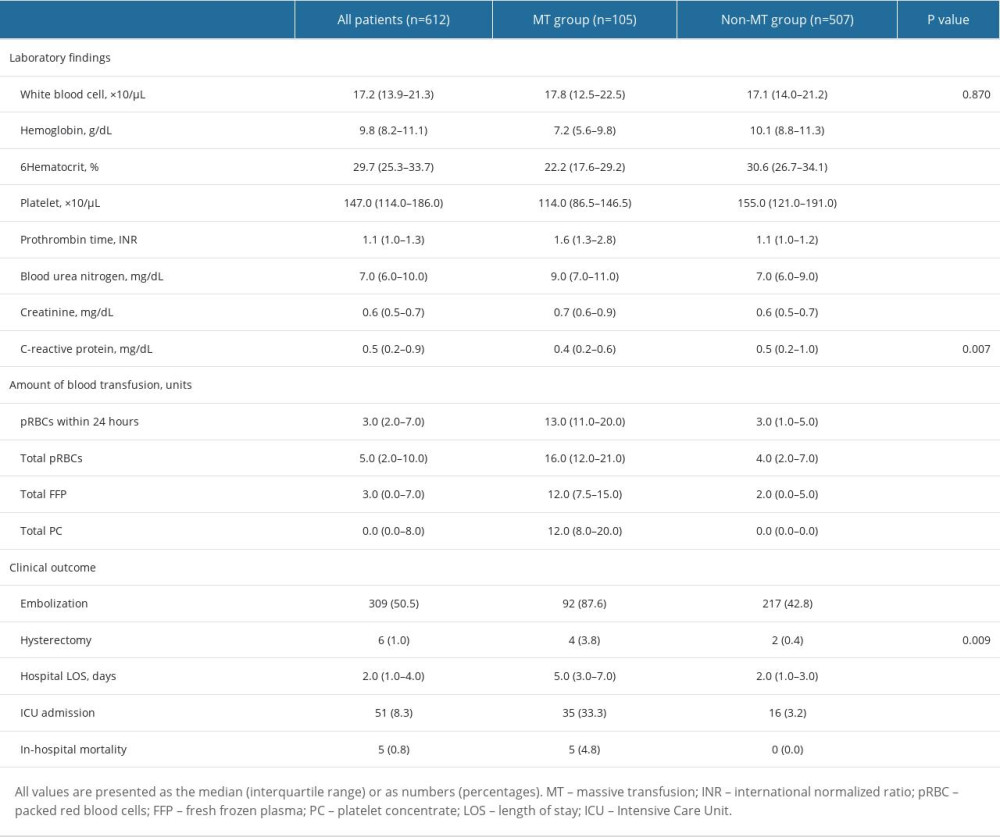 Table 2. A comparison of laboratory findings, blood transfusion amounts, and clinical outcomes based on massive transfusion in patients with primary postpartum hemorrhage.
Table 2. A comparison of laboratory findings, blood transfusion amounts, and clinical outcomes based on massive transfusion in patients with primary postpartum hemorrhage.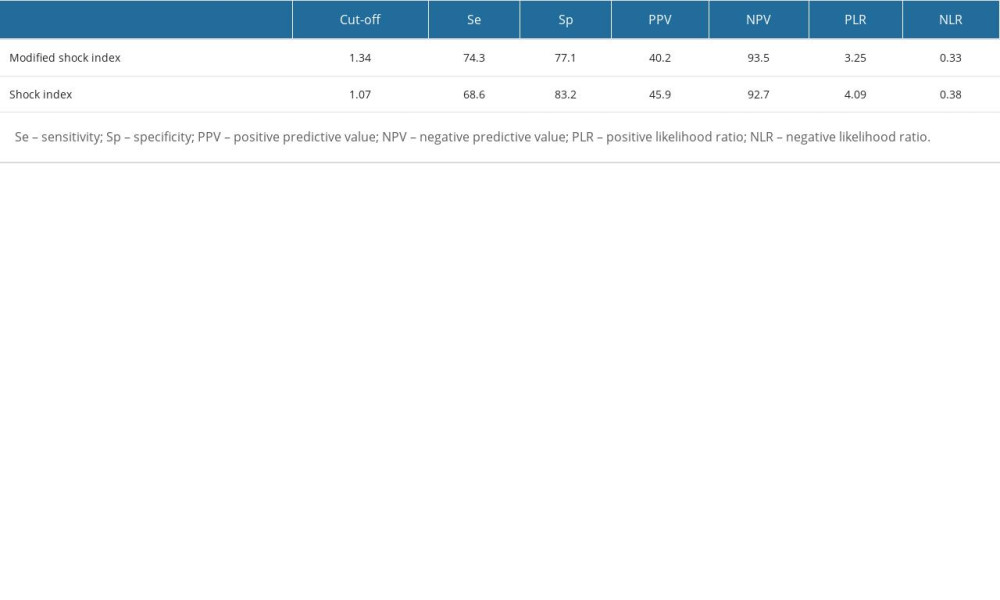 Table 3. Optimal cutoff value and predictive power of modified shock index and shock index for massive transfusion in primary postpartum hemorrhage.
Table 3. Optimal cutoff value and predictive power of modified shock index and shock index for massive transfusion in primary postpartum hemorrhage.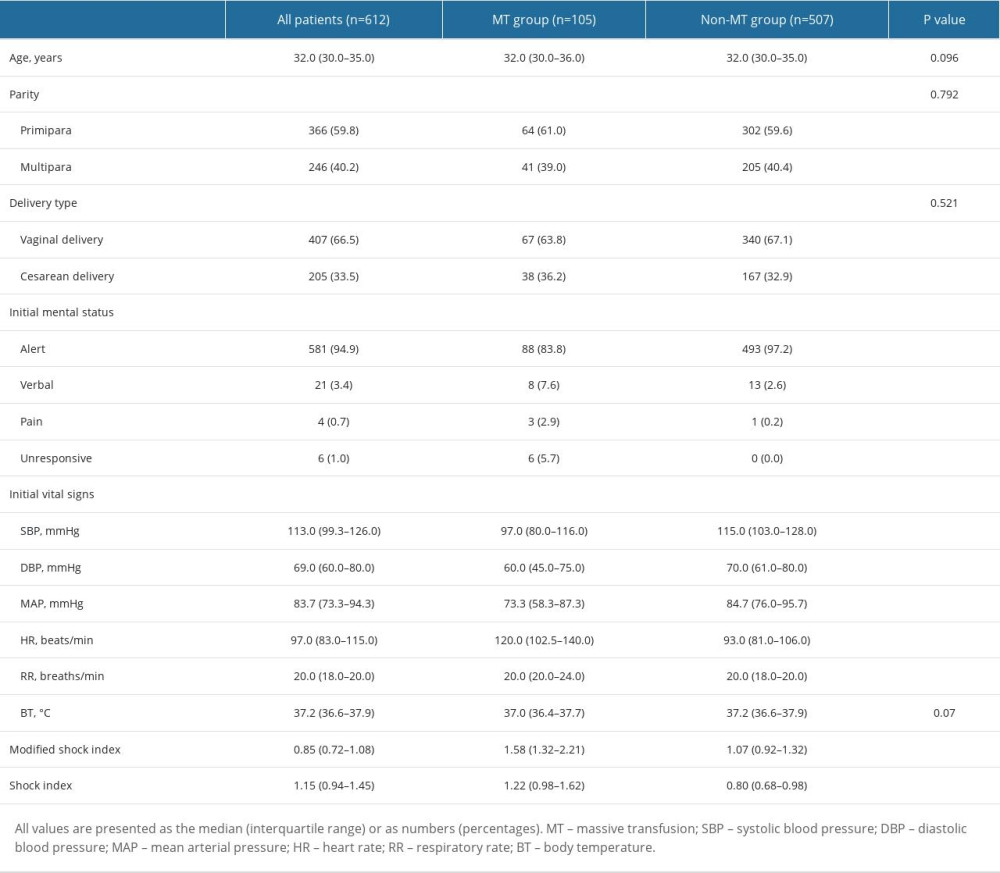 Table 1. Baseline demographic and clinical characteristics of the study patients.
Table 1. Baseline demographic and clinical characteristics of the study patients.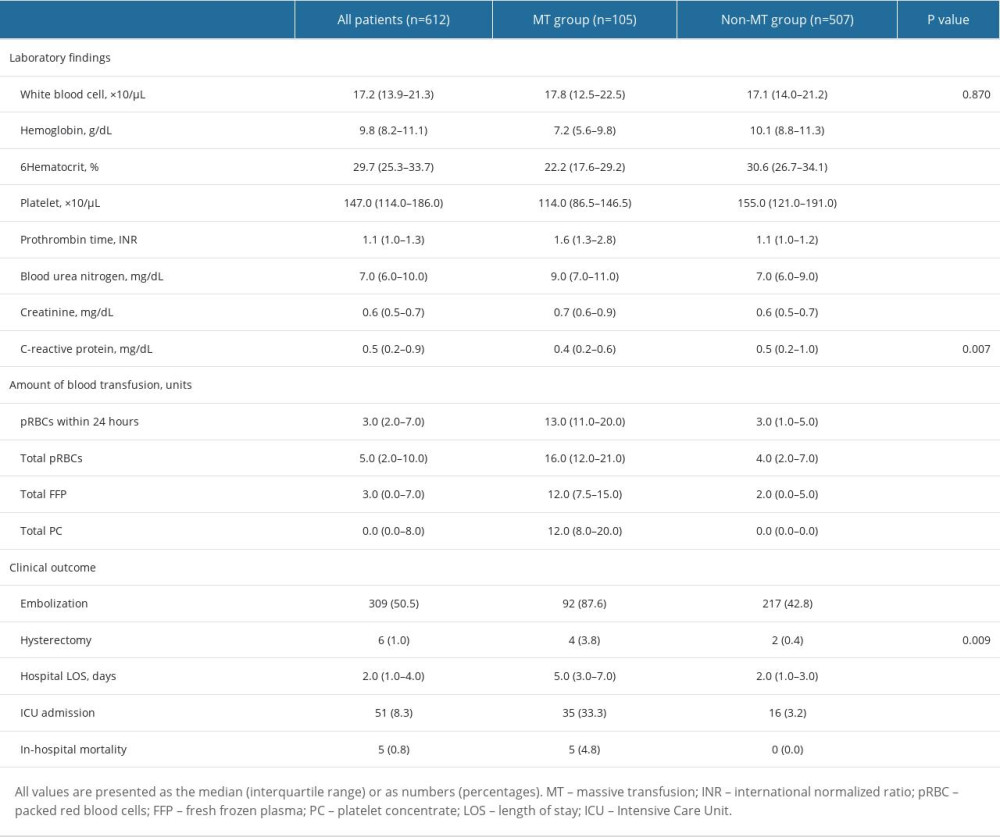 Table 2. A comparison of laboratory findings, blood transfusion amounts, and clinical outcomes based on massive transfusion in patients with primary postpartum hemorrhage.
Table 2. A comparison of laboratory findings, blood transfusion amounts, and clinical outcomes based on massive transfusion in patients with primary postpartum hemorrhage.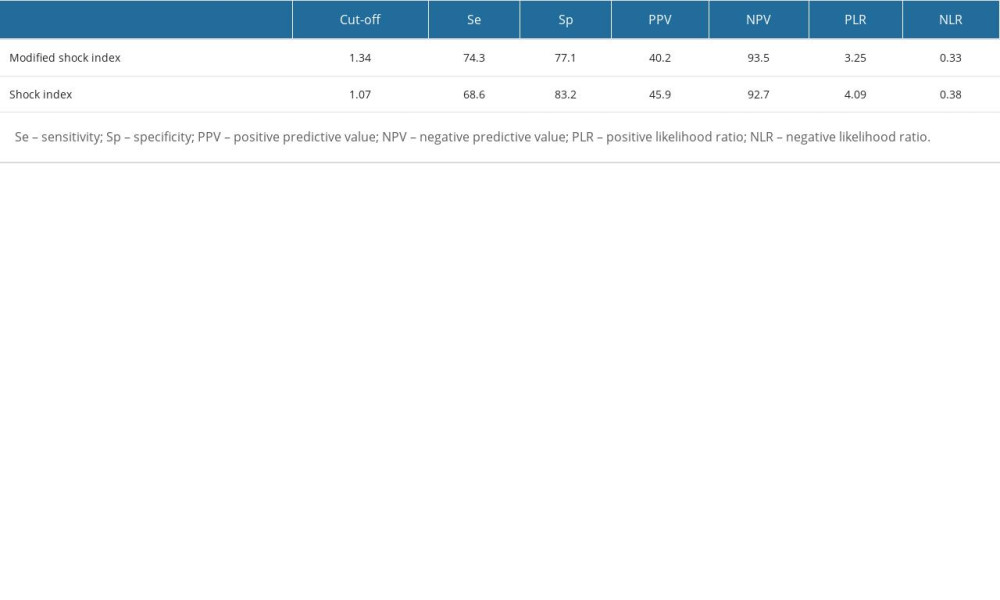 Table 3. Optimal cutoff value and predictive power of modified shock index and shock index for massive transfusion in primary postpartum hemorrhage.
Table 3. Optimal cutoff value and predictive power of modified shock index and shock index for massive transfusion in primary postpartum hemorrhage. In Press
12 Mar 2024 : Clinical Research
Tissue Inhibitors of Metalloproteinase 1 (TIMP-1) and 3 (TIMP-3) as New Markers of Acute Kidney Injury Afte...Med Sci Monit In Press; DOI: 10.12659/MSM.943500
12 Mar 2024 : Review article
Optimizing Behçet Uveitis Management: A Review of Personalized Immunosuppressive StrategiesMed Sci Monit In Press; DOI: 10.12659/MSM.943240
12 Mar 2024 : Clinical Research
Metabolomic Alterations in Methotrexate Treatment of Moderate-to-Severe PsoriasisMed Sci Monit In Press; DOI: 10.12659/MSM.943360
14 Mar 2024 : Clinical Research
Renal Dysfunction Increases Risk of Adverse Cardiovascular Events in 5-Year Follow-Up Study of Intermediate...Med Sci Monit In Press; DOI: 10.12659/MSM.943956
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








