16 January 2024: Clinical Research
Outcomes of Lumbosacral Fixation in Patients with Suicidal Jumper’s Fractures: A Retrospective Study from a Single Center in Turkey
Ramazan Atiç1ABCF*, Celil Alemdar2ABDF, Sait Anıl Ulus3ABCE, Cihan Yazar1BCDE, Fatih Durgut4ACEF, Şafak Sayar5BDEF, Abdülkadir Aydın6ABCEDOI: 10.12659/MSM.942831
Med Sci Monit 2024; 30:e942831
Abstract
BACKGROUND: Suicide attempts that involve jumping from a great height may not be fatal but can result in lumbosacral facture-dislocations. This retrospective study aimed to present the experience from a single center in Turkey of 21 patients with lumbosacral facture-dislocations, or suicidal jumper fractures, treated with lumbosacral fixation between 2015 and 2022.
MATERIAL AND METHODS: The study included 21 patients. The diagnosis was established through X-ray and computed tomography (CT) examinations. Neurological damage was assessed using the Gibbons score. Among the patients, 2 were classified as Roy-Camille type 1, 12 as Roy-Camille type 2, and 7 as Roy-Camille type 3. Morphologically, 8 patients had H-type fractures, 7 had T-type fractures, and 6 had U-type fractures. Bilateral spinopelvic fixation was performed. Functional outcomes were evaluated using the Majeed score.
RESULTS: The average Injury Severity Score (ISS) was 31.6±12.2. The mean duration of surgery was 123.6±44.9 minutes. According to the Majeed score, excellent results were observed in 8 individuals (40%), good results in 5 individuals (25%), fair results in 5 individuals (25%), and poor results in 2 individuals (10%). Out of 18 patients with neurological deficits, 14 showed improvement after surgery, while 4 continued to experience deficits.
CONCLUSIONS: The findings from this study highlight the importance of obtaining a clear history of the cause of lumbosacral facture-dislocation, as attempted suicide by jumping from a height can cause specific types of injury to the lumbar spine and sacrum that require rapid diagnosis and management to reduce the incidence of permanent paraplegia.
Keywords: Decompression, Sacrum, Spinal Fractures, Lumbosacral Region
Background
Spinopelvic dissociation is a condition in which the upper sacrum and spine separate from the pelvis as a result of a transverse sacral fracture combined with a vertical sacral fracture on both sides [1]. Although spinopelvic dissociation is a rare injury (about 3–5% of all sacral fractures), it is associated with a high incidence of neurological impairments that impair the function of the lower extremities, including the bladder, colon, and bowel [2]. The most frequent cause of traumatic spinopelvic dissociations is high-energy trauma, which includes car crashes and falls from heights [3]. Because a typical mechanism of injury is a jump from height during a suicide attempt, Roy-Camille refers to them as the “suicidal jumper’s fracture”. Three categories of fractures were established by Roy-Camille. Type 1 is a flexion fracture in which the upper sacrum fragments simply bend in front. Type 2 is a flexion fracture in which the upper fragment moves posteriorly and becomes more or less horizontal, settling on the lower fragment’s fractured surface. Type 3 is an extension fracture in which the upper fragment moves anteriorly and becomes more or less vertical, slipping downward in front of the lower fragment [4]. Subsequently, the S1 crush fracture was added to the classification by Stronge-Vongsen and Lebech [5]. The addition of sagittal fracture lines to transverse fractures led to the emergence of U-, H-, and T-shaped fracture patterns. These fractures are typically unstable and result from high-energy injuries, often accompanied by neurological deficits, hemodynamic disturbances, and additional injuries to the musculoskeletal system and organs [6–9].
These high-energy fractures frequently result in spinal cord injury. The autonomic nervous system and the conduction of sensory and motor impulses across the lesion site(s) are both impacted by spinal cord injury (SCI). According to the sacral-sparing definition, injuries are generally categorized as either neurologically “complete” or “incomplete”. The phrase “sacral-sparing” describes the preservation of light touch or pin prick sensation at the S4–S5 dermatome, deep anal pressure, or voluntary anal sphincter contraction, as well as the presence of sensory or motor function in the most caudal sacral segments, as determined by the examination. Sacral-sparing, or the preservation of sensory and/or motor function in the lowest sacral segments, S4–S5, is described as the absence of a complete damage, while the presence of sacral-sparing, or some preservation of sensory and/or motor function at S4–S5, is classified as an incomplete injury [10]. Depending on the severity of the neurologic loss and the anatomical level of the damage, traumatic spinal cord injuries can have different neurologic repercussions. The lowest cord segment with normal motor and sensory function determines the level. Although there are other methods for grading severity, the most widely used one is the American Spinal Injury Association Impairment Scale (AIS), which uses a five-point rating system to go from A (total loss of neurologic function below the afflicted level) to E (normal function) [11].
Jumping from a height subjects the spine to flexion due to the body weight and gravitational force. After the fracture, the iliopsoas maintain the flexed posture. Due to displacement and instability, these injuries disrupt spinopelvic continuity, necessitating surgical intervention [12]. Early mobilization, low complication rates, strong stability, and restoration of pelvic anatomy are the primary goals of surgical treatment. Generally, cannulated screws, posterior tension bands, and spinopelvic fixation are commonly used surgical methods for sacral fractures. Among them, spinopelvic fixation is considered more reliable in providing fixation strength and maintaining lumbar spine-pelvic continuity in such injuries [6].
Therefore, this retrospective study aimed to present the experience from a single center in Turkey of 21 patients with lumbosacral facture-dislocations, or suicidal jumper’s fractures, treated with lumbosacral fixation between 2015 and 2022.
Material and Methods
ETHICS APPROVAL:
The Ethics Review Committee of Biruni University Hospital granted approval for this study (number: 2023/83-03). Written informed consent was obtained from the participants or their families, and the study was carried out in accordance with the Declaration of Helsinki’s ethics guidelines.
PATIENTS AND DATA COLLECTION:
In the study, 21 patients who developed sacral fractures following suicide attempts and underwent lumbosacral fixation between 2015 and 2022 were retrospectively evaluated. With the aid of electronic medical data, patient demographics, surgical specifics, and results were reviewed and gathered. Age, sex, particular surgical method, associated injuries, neurological status, Roy-Camille type, injury severity score, Gibbons score, and Majeed score were among the data points. The mean age of patients was 22.8±9.4 years. There were 14 females and 7 males. Patient information is provided in Table 1.
DIAGNOSTIC IMAGING AND CLASSIFICATION:
Standard direct radiographs and three-dimensional computed tomography (CT) scans were obtained for all patients. CT was used to assess the shape of the deformity, displacement, sacral foramina, and spinal canal. Roy-Camille classification was utilized for fracture classification. Morphologically, fractures were categorized as H-type, T-type, and U-type based on CT findings. Patients with neurological deficits also underwent magnetic resonance imaging (MRI).
PEROPERATIVE CARE AND INJURY SCORES:
The severity of trauma was determined using the Injury Severity Score (ISS). Advanced trauma life support protocol was applied to all patients. Patients who underwent initial evaluation and interventions in the emergency department were admitted to the intensive care unit or ward based on their overall condition. Isolated sacral fractures were present in 5 patients. Additional orthopedic injuries were observed in 16 patients, and 10 patients had non-skeletal injuries. Among the patients with non-orthopedic injuries, 6 had pneumothorax, 1 had rib fracture, 1 had a burn, 1 had a spleen laceration, and 1 had a nasal fracture. Surgery timing was determined considering hemodynamic stability, neurological damage, and additional injuries. Patients without open wounds received standard antibiotic prophylaxis with cefazolin 1 g 4×1 for 24 hours. The first dose was administered 1 hour before surgery. All patients wore anti-embolic stockings. Additionally, thromboembolism prophylaxis was administered with low-molecular-weight heparin. Patients in suitable overall condition were mobilized on the first postoperative day.
SURGICAL TECHNIQUE:
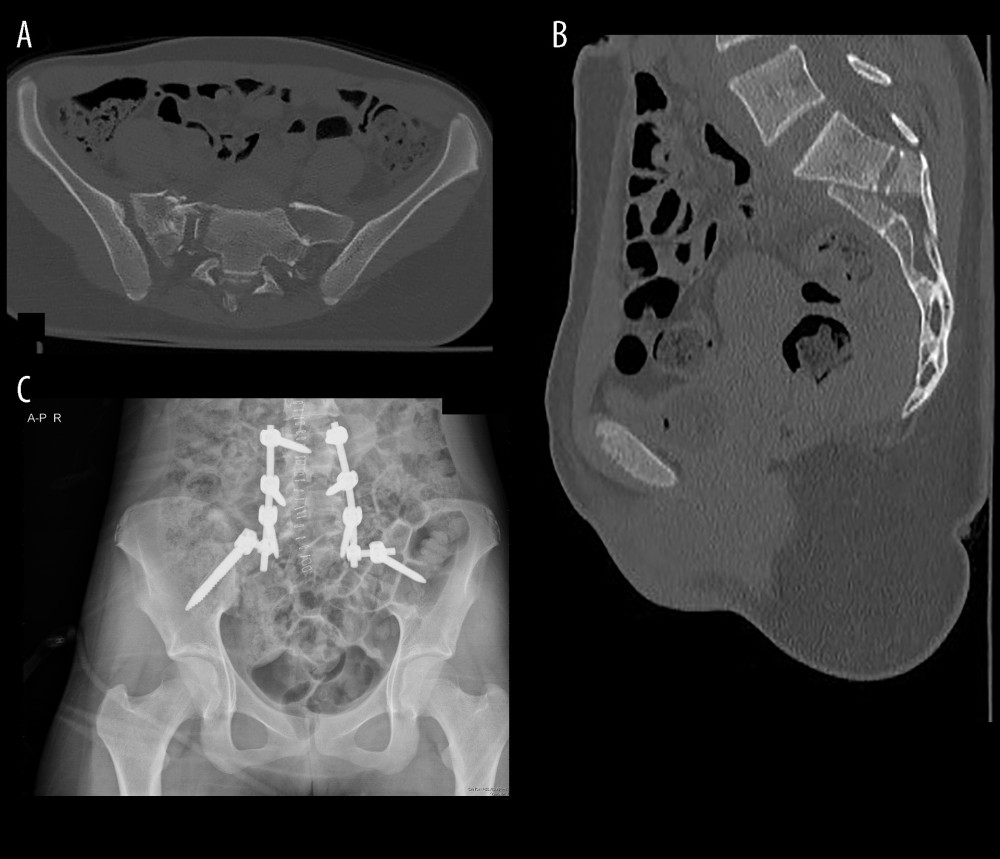
The patients were taken to surgery under general anesthesia in the prone position. Following draping and painting, a midline incision was made between L4 and S3. Paraspinal muscles were dissected using cautery and elevator, and pedicles were reached. L4–L5 pedicle screws were placed under fluoroscopic guidance. Subsequently, the posterior superior iliac crests were identified, and supraacetabular trajectories were used for placing iliac screws under fluoroscopic guidance. Decompression was additionally performed in patients with neurological deficits or fragments compressing the canal, foramen, or roots identified in preoperative evaluation. Reduction was achieved. Suitable-length rods were placed on both sides with lordosis, and secured to the pedicle screws. Confirmation of maintained reduction was done using fluoroscopy. System stability was checked and hemostasis was confirmed. A Hemovac drain was placed, and the incision was closed. In Figure 1, preoperative, and postoperative images of one of our cases are presented.
POSTOPERATIVE EVALUATION:
The neurological examination included evaluation of perineal sensation, anal tone, sphincter functions, and lower-extremity motor functions. Gibbons score [13] was used to determine the level of injury (Table 2). Early postoperative images were obtained, and reduction was evaluated. After surgery, patients were able to walk with help in 2 to 5 days. Patients were scheduled for regular follow-ups until fracture consolidation. Fracture consolidation was evaluated using direct radiographs. Implants were removed 1 year after surgery to eliminate movement restrictions. Functional outcomes were assessed using the Majeed scoring system [14], and clinical outcomes were graded as follows: excellent (85–100), good (70–84), fair (55–69), and poor (<55).
STATISTICAL ANALYSIS:
The distribution of the data was assessed using the Kolmogorov-Smirnov test. Normally distributed continuous data are presented as mean (SD), whereas non-normally distributed data are presented as median (interquartile range [IQR]). Statistical significance was set at a two-sided p-value <0.05. Data analysis was performed using SPSS version 22.0 (IBM Corp., Armonk, New York, USA).
Results
CHARACTERISTICS OF FRACTURES AND NEUROLOGICAL ASSESSMENT:
Among the patients, 2 were classified as Roy-Camille type 1, 12 as Roy-Camille type 2, and 7 as Roy-Camille type 3. Morphologically, 8 patients had H-type, 7 had T-type, and 6 had U-type fractures. The mean Injury Severity Score (ISS) was calculated as 31.6±12.2. The average preoperative sacral kyphosis angle was 42.2±21.9 degrees. The horizontal displacement measured 12.9±7.5 mm, and the mean sagittal displacement was 12.4±7.4 mm. Neurological deficits were present in 18 patients at the preoperative assessment. According to the Gibbons score, 3 patients scored 1, 14 scored 2, and 4 scored 4. Among the 18 patients with neurological deficits, the neurological condition improved in 14 after surgery, while 4 patients continued to experience neurological deficits.
OPERATIONAL PARAMETERS:
Bilateral fixation was applied to all patients. Seven patients with stable general conditions underwent surgery on the same day. The remaining 15 patients were operated on within an average of 3.5 (1–20) days after admission. The average duration of surgery was 123.6±44.9 minutes. Nineteen patients received blood transfusions with an average of 5.2±2.5 units of blood. The average length of hospital stay was 9.7±5.3 days (Table 3).
PRIMARY FUNCTIONAL OUTCOMES:
The number of patients presenting with jump injuries significantly increased during the COVID-19 pandemic period from 2019 to 2021. One patient was lost due to COVID-19, and postoperative follow-up was not available. Union was achieved in the other 20 patients with an average union time of 140±72.8 days. The Majeed score was calculated as 72.8±22.9. Majeed scores were excellent in 8 (40%) individuals, good in 5 (25%), moderate in 5 (25%), and poor in 2 (10%).
COMPLICATIONS:
Four patients experienced complications requiring intervention; these patients exhibited signs of discharge and infection at the wound site. One of these patients underwent revision surgery on the first postoperative day due to improper screw positioning observed in the postoperative computed tomography. Another patient with infection also developed a decubitus ulcer. Two patients exhibited mild implant irritation, which was managed conservatively without routine removal.
Discussion
The study retrospectively evaluated 21 patients who experienced sacral fractures following suicide attempts and underwent lumbosacral fixation between 2015 and 2022. Two-thirds of the patients were female. The fractures were classified based on Roy-Camille types and morphological characteristics. The mean Injury Severity Score (ISS) was 31.6, and preoperative assessments indicated neurological deficits in 18 patients. The Gibbons score showed varying levels of neurological impairment. Surgical interventions included bilateral fixation, with a mean surgery duration of 123.6 minutes. Postoperatively, 14 patients with neurological deficits showed improvement, while 4 continued to experience deficits. The study reported an increase in jumping injuries during the COVID-19 pandemic. Out of 21 patients, one was lost due to COVID-19. The average union time was 140 days, and 20 patients achieved union. The Majeed score indicated outcomes ranging from excellent to poor, with complications observed in 4 patients, including wound site issues and implant irritation. Overall, the study demonstrated the challenges and outcomes of lumbosacral fixation in patients with sacral fractures following suicide attempts.
Suicidal jumper’s fractures of the sacrum are high-energy injuries. The classification of jumper’s fractures into 3 zones, as described by Dennis, does not fully explain the mechanism of these fractures. The primary mechanism of these fractures is vertical loading, leading to horizontal fractures in the sacrum [15]. The classification proposed by Roy-Camille, which focuses on vertical instability and is based on flexion and displacement, has been widely accepted for evaluating these injuries [16]. These fractures are generally unstable and often involve neurological impairment. The main reason for neurological involvement is the fracture line passing through the sacral foramina and canal.
In sacral fractures, options for treatment include spinopelvic fixation, tension band application, and cannulated screw fixation. Studies have demonstrated the success of tension band and screw application in sacral fractures. However, in vertically unstable fractures, maintaining the stability of lumbopelvic continuity is crucial. While the tension band provides stabilization between the iliac wings, it fails to ensure spinopelvic stability. Cannulated screw fixation, especially advantageous in patients with posterior skin issues, provides adequate fixation in zone 1 sacral fractures but might not be sufficient in complex and unstable vertical fractures. Moreover, compression achieved with screws can worsen the neurological condition. Therefore, spinopelvic fixation is the preferred approach in vertical unstable sacral fractures [17].
The most significant biomechanical advantage of spinopelvic fixation is its ability to create a bridge between the intact lumbar vertebra and the intact iliac wings, restoring spinopelvic dissociation. A study by Linhard et al [18], involving 24 cases, reported achieving ideal anatomical reduction in all patients and did not encounter signs of screw loosening or implant insufficiency during follow-ups. Defects and fragmentation in the sacrum do not significantly impair the strength of fixation. A robust fixation system allows for early load-bearing, does not exert compressive effects on the sacral area, and provides a suitable workspace for decompression and root liberation in the canal and foramen. Sobhan et al [19] published the results of 14 patients who underwent spinopelvic fixation, indicating the method’s effectiveness and safety, low complication rates, and nearly all patients (85%) returning to work. In another study, Okuda et al [20] emphasized the successful correction of vertical displacement with spinopelvic fixation in a series of 16 cases, achieving fusion in all cases. Our patients were injured between 2019 and 2021. The economic and psychological impact of the COVID-19 pandemic may have triggered suicidal tendencies, potentially explaining the increase in patients. We lost 1 patient shortly after surgery due to COVID-19, but all of the other patients achieved fusion. Kano et al demonstrated that psychological disorders increase the likelihood of suicide and the incidence of suicidal jumper’s fractures. They compared cases of spinal injury in suicidal and non-suicidal high fall incidents, noting that 67% of suicidal jumpers were young women. They indicated that 77% of their patients had mental disorders, including schizophrenia and depression. Additionally, they mentioned a higher frequency of extremity injuries in suicidal jumpers compared to non-suicidal high falls [21–23]. In our study, 66% of patients were young women, and extremity injuries accompanied most jumper’s fractures.
Neurological deficit is a common condition in unstable sacral fractures. Particularly, highly fragmented and displaced fractures are more risky in terms of neurological deficits. Usually, L5 and sacral roots are affected. Due to the affected roots, urinary and fecal incontinence can develop, severely affecting the patient’s quality of life. During surgery in patients with deficits, decompression and liberation up to the root foraminal exit are crucial. Decompression eliminates nerve compression. Miyamoto et al [24] reported excellent clinical outcomes in cases where they performed decompression through laminectomy. Maki et al [25] reported significant improvement in neurological symptoms after spinopelvic fixation and decompression. In contrast, in the study by Nonne et al, neurological deficits were present in 4 out of 5 treated patients, and improvement was observed only in the patient with sphincter deficit. The time interval between injury and definitive surgery in their patients exceeded 10 days; therefore, they did not perform decompression. They emphasized the importance of early spinopelvic fixation in their study [5]. In our study, the average time from injury to definitive surgery was 3.5 days, and improvement was observed in 14 out of 18 patients with neurological deficits. We believe that this difference is attributable to early surgical fixation and decompression in our approach.
The disadvantages of spinopelvic fixation have been evaluated in many studies. Due to its open surgical nature, it introduces an additional inflammatory burden. In cases accompanied by myofascial injuries such as bleeding, especially Morel-Lavallée lesions, there is a high risk of infection. This situation has directed surgeons towards minimally-invasive spinopelvic fixation (SPF) methods, and some authors have reported that complication rates can be reduced with minimally-invasive approaches. Pearson et al [26] compared the results of 16 patients who underwent percutaneous spinopelvic fixation with open surgery. They reported that the group treated with percutaneous SPF had fewer infection and wound problems, less blood loss, and shorter hospital stays. However, especially in closed surgical applications, the inability to fully meet the requirements for reduction and decompression, and additional radiation exposure, are significant handicaps. Williams et al [27], while listing the advantages of percutaneous surgery, pointed out the necessity of not avoiding open surgery and decompression when needed, especially by excluding patients with neurological deficits from the target group.
The severity of the injury and systemic or local complications related to surgery can be observed. Locally, wound infections and wound healing problems, hematomas, and implant-related issues are common. Mendel et al [28] reported deaths of 2 patients due to pulmonary embolism and 1 patient due to gastric perforation in a series of 73 cases. They also reported revision surgery in 1 patient due to hematoma, and encountering mild urinary tract infections in 4 patients. Li et al [29] reported encountering 3 complications in a series of 6 cases, including superficial infection in 1 patient, severe posterior implant irritation in 1 patient, and recurrent Morel-Lavallée lesions after surgery in another patient. Welle et al [30] reported encountering mild implant irritation in 3 patients and severe implant irritation in 1 patient. We experienced complications in 4 of our patients, who developed wound site discharge and infection. One was taken back to surgery on the first postoperative day for revision due to improper screw placement observed in the postoperative CT scan. In another patient with infection, a decubitus ulcer developed. In the 2 patients with implant irritation, routine management was maintained due to the mild nature of their concerns.
Our study has some limitations, such as being retrospective and conducted at a single center. These 2 characteristics reduce the generalizability of the data. The heterogeneity of accompanying injuries in patients has made it challenging to examine the impact of these injuries on functional life and treatment outcomes. Due to the rarity of these injuries, our case count has followed the literature averages. Methodologically, having a control group with unilateral fixation or minimally-invasive surgery could have allowed us to obtain more comparable results. The study partially coinciding with the COVID-19 period has added complexity to the incidence of suicide, although this incidence has not been thoroughly examined. Socio-demographic characteristics that could affect the postoperative rehabilitation of patients have not been adequately investigated. Posterior spinopelvic instrumentation is a surgery prone to complications.
Conclusions
In the case of unstable sacral fractures, the restoration of anatomy and stability is quite important in terms of radiological and functional outcomes. Spinopelvic fixation provides strong and sustainable fixation between the lumbar vertebra and iliac wings, ensuring continuity of the spinopelvic skeleton. Its ability to allow early weight-bearing and maintain a low complication rate renders this method reliable and effective. The findings from this study highlight the importance of obtaining a clear history of the cause of lumbosacral facture-dislocation, as attempted suicide by jumping from a height can cause specific types of injury to the lumbar spine and sacrum that require rapid diagnosis and management to reduce the incidence of permanent paraplegia.
References
1. Yi C, Hak DJ, Traumatic spinopelvic dissociation or U-shaped sacral fracture: A review of the literature: Injury, 2012; 43(4); 402-8
2. Petryla G, Bobina R, Uvarovas V, Functional outcomes and quality of life after surgical treatment of spinopelvic dissociation: A case series with one-year follow-up: BMC Musculoskelet Disord, 2021; 22(1); 795
3. Chou DTS, El-Daly I, Ranganathan A, Spinopelvic dissociation: A retrospective case study and review of treatment controversies: J Am Acad Orthop Surg, 2018; 26(14); e302-12
4. Roy-Camille R, Saillant G, Gagna G, Mazel C, Transverse fracture of the upper sacrum. Suicidal jumper’s fracture: Spine, 1985; 10(9); 838-45
5. Nonne D, Capone A, Sanna F, Suicidal jumper’s fracture – sacral fractures and spinopelvic instability: A case series: J Med Case Reports, 2018; 12; 186
6. Mohd Asihin MA, Bajuri MY, Spinopelvic fixation supplemented with gullwing plate for multiplanar sacral fracture with spinopelvic dissociation: A case series with short term follow up: Front Surg, 2019; 6; 42
7. Özkul E, Gem M, Alemdar CVascular injury following supracondylar humerus fractures in children: Ulus Travma Ve Acil Cerrahi Derg, 2016; 22(1); 84-89 [in Turkish]
8. Yiğit Ş, What should be the timing of surgical treatment of humeral shaft fractures?: Medicine (Baltimore), 2020; 99(17); e19858
9. Yazar C, Özkul E, Atiç R, Crush and compartment syndrome due to earthquake injury: Ulus Med J, 2023; 1(2); 26-30
10. Kirshblum SC, Burns SP, Biering-Sorensen F, International standards for neurological classification of spinal cord injury (revised 2011): J Spinal Cord Med, 2011; 34(6); 535-46
11. Ropper AE, Ropper AH, Acute spinal cord compression: N Engl J Med, 2017; 376(14); 1358-69
12. Matar HE, Hassan K, Duckett SP, Insufficiency sacral fracture-dislocation mimicking suicidal jumper’s fracture: BMJ Case Rep, 2016; 2016; bcr2016216587
13. Gibbons KJ, Soloniuk DS, Razack N, Neurological injury and patterns of sacral fractures: J Neurosurg, 1990; 72(6); 889-93
14. Majeed SA, Grading the outcome of pelvic fractures: J Bone Joint Surg Br, 1989; 71(2); 304-6
15. Liu Z, Hu Y, Tian W, Robot aided minimally ınvasive lumbopelvic fixation in treatment of traumatic spinopelvic dissociation: Orthop Surg, 2021; 13(2); 563-72
16. Dreizin D, Smith EB, CT of sacral fractures: Classification systems and management: Radiogr Rev Publ Radiol Soc N Am Inc, 2022; 42(7); 1975-93
17. Acklin YP, Zderic I, Richards RG, Biomechanical investigation of four different fixation techniques in sacrum Denis type II fracture with low bone mineral density: J Orthop Res, 2018; 36(6); 1624-29
18. Linhart C, Befrui N, Etzel L, Jumper’s fracture of the sacrum: A novel and reproducible way for successful reduction and fixation: Eur Spine J, 2022; 31(1); 18-27
19. Sobhan MR, Abrisham SMJ, Vakili M, Shirdel S, Spinopelvic fixation of sacroiliac joint fractures and fracture-dislocations: a clinical 8 years follow-up study: Arch Bone Jt Surg, 2016; 4(4); 381-86
20. Okuda A, Maegawa N, Matsumori H, Minimally invasive spinopelvic “crab-shaped fixation” for unstable pelvic ring fractures: technical note and 16 case series: J Orthop Surg, 2019; 14(1); 51
21. Kano H, Matsuo Y, Kubo N, Spinal ınjuries in suicidal jumpers: Spine, 2019; 44(1); E13-18
22. Cabrera-Pivaral CE, Clinical and social importance of stool RT-PCR: A follow-up test for COVID-19 and long COVID-19: Cir Cir, 2023; 91(5); 721-22
23. Akar MS, Ulus SA, Durgut F, Dönmez S, Complications and difficulties due to bonesetter in the treatment of pediatric distal humerus fractures: J Clin Trials Exp Investig, 2023; 2(1); 38-44
24. Miyamoto AK, Graells XSI, Sebben AL, Complex fractures of the sacrum with spinopelvic dissociation treated surgically with ıliolumbar fixation: Rev Bras Ortop, 2020; 55(3); 304-9
25. Maki S, Nakamura K, Yamauchi T, Lumbopelvic fixation for sacral ınsufficiency fracture presenting with sphincter dysfunction: Case Rep Orthop, 2019; 2019; 9097876
26. Pearson JM, Niemeier TE, McGwin G, Rajaram Manoharan S, Spinopelvic dissociation: Comparison of outcomes of percutaneous versus open fixation strategies: Adv Orthop, 2018; 2018; 5023908
27. Williams SK, Quinnan SM, Percutaneous lumbopelvic fixation for reduction and stabilization of sacral fractures with spinopelvic dissociation patterns: J Orthop Trauma, 2016; 30(9); e318-24
28. Mendel T, Ullrich BW, Hofmann GO, Progressive instability of bilateral sacral fragility fractures in osteoporotic bone: A retrospective analysis of X-ray, CT, and MRI datasets from 78 cases: Eur J Trauma Emerg Surg, 2021; 47(1); 11-19
29. Li-Jun L, Xiao-Man D, Xiao-Chen S, Jian J, Treatment of ‘suicidal jumper fractures’ with lumbopelvic fixation: A report of nine cases: J Hard Tissue Biol, 2021; 30(2); 205-10
30. Welle K, Khoury M, Prangenberg CMinimally invasive lumbopelvic stabilization of sacral fracture and sacroiliac injury: Oper Orthopadie Traumatol, 2021; 33(6); 538-45 [in Germany]
Tables
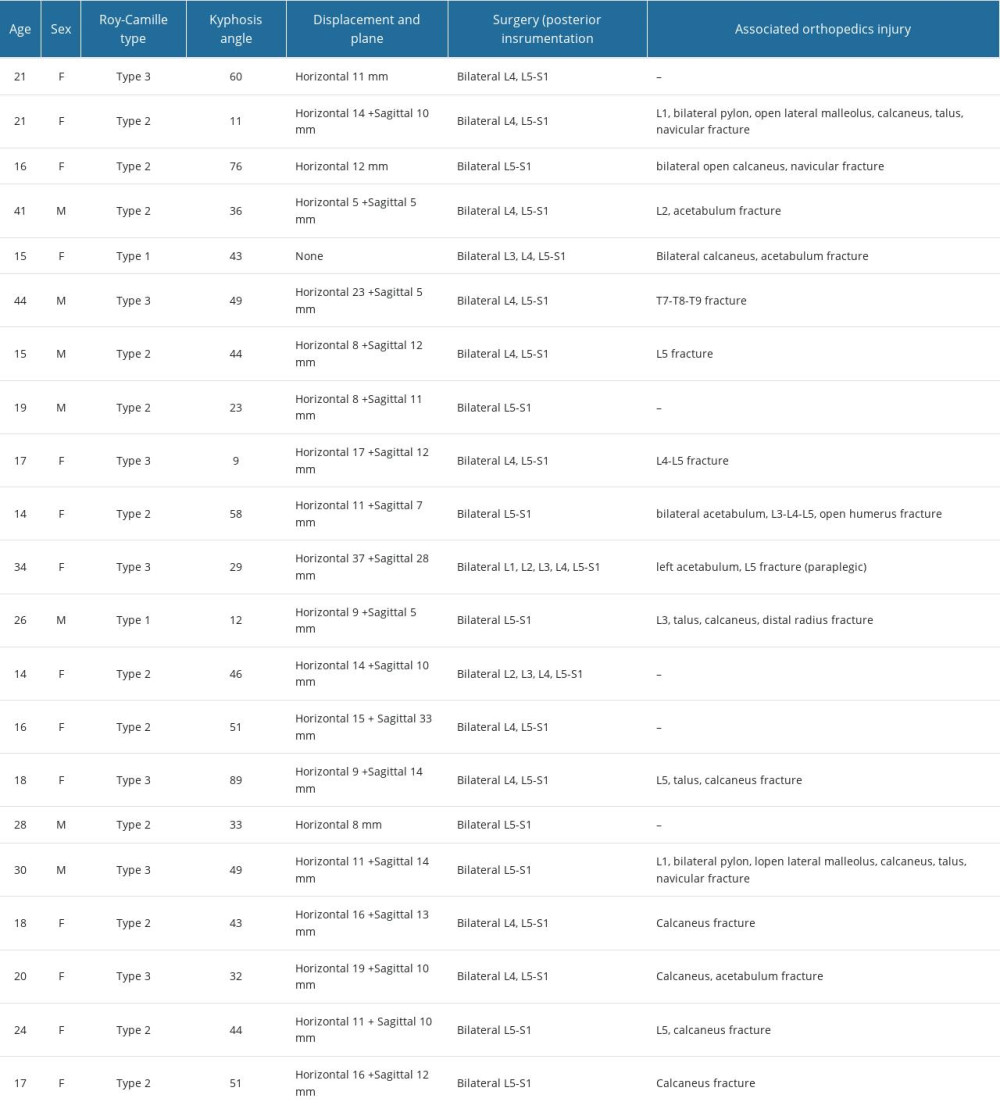 Table 1. Demographic characteristics and associated conditions of patients.
Table 1. Demographic characteristics and associated conditions of patients.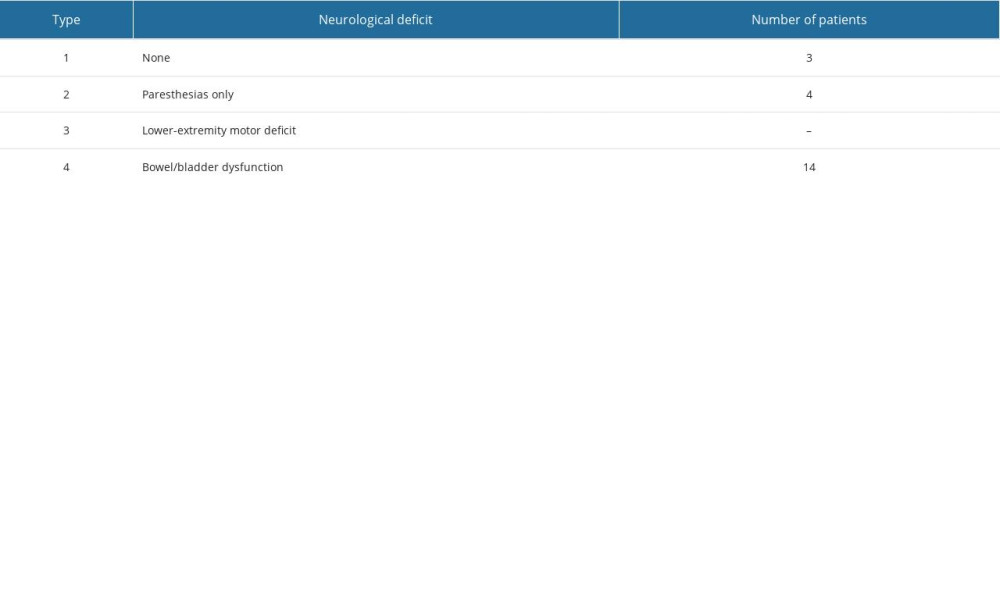 Table 2. Neurological assessment of the patients according to the Gibbons Classification.
Table 2. Neurological assessment of the patients according to the Gibbons Classification.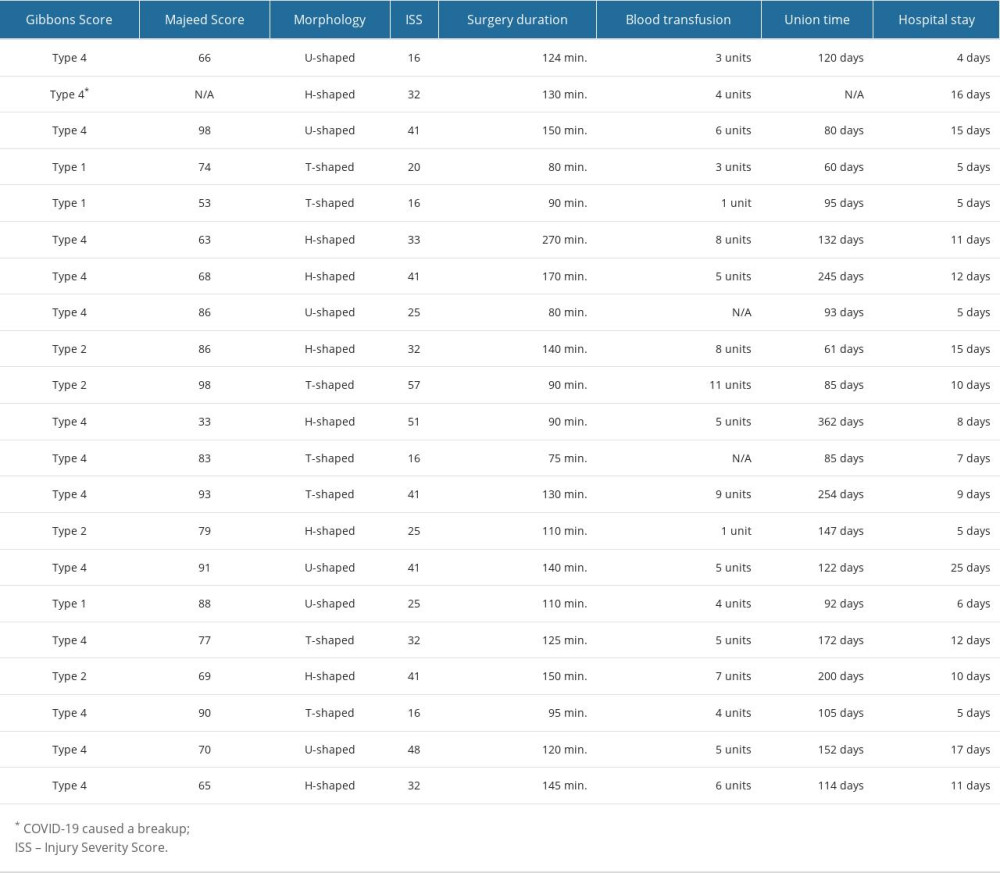 Table 3. The intraoperative and postoperative treatment outcomes of the patients.
Table 3. The intraoperative and postoperative treatment outcomes of the patients.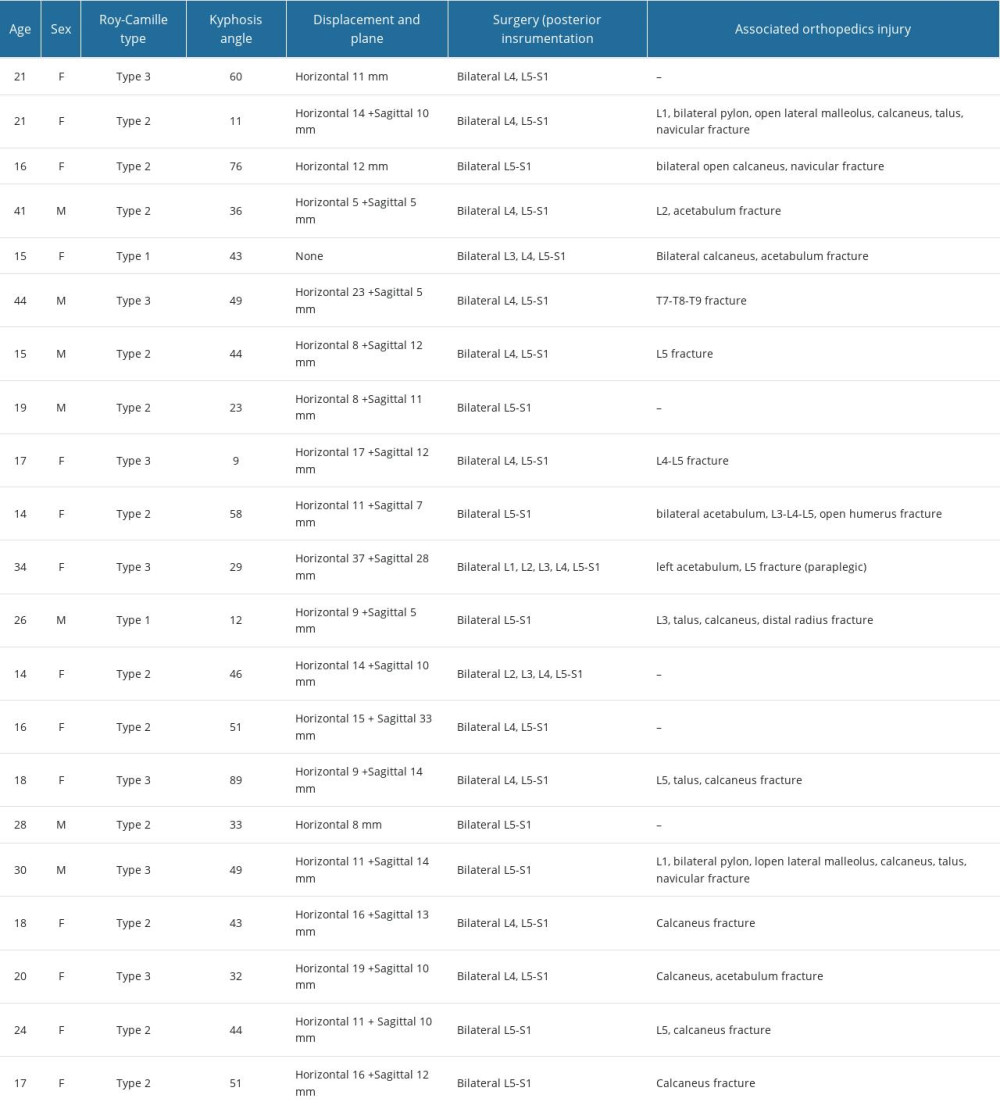 Table 1. Demographic characteristics and associated conditions of patients.
Table 1. Demographic characteristics and associated conditions of patients.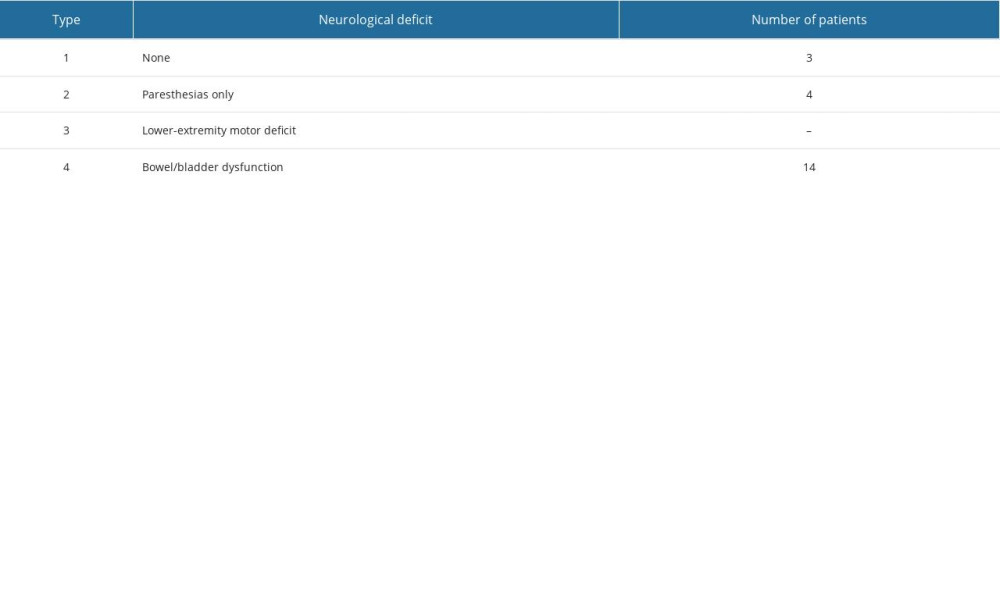 Table 2. Neurological assessment of the patients according to the Gibbons Classification.
Table 2. Neurological assessment of the patients according to the Gibbons Classification.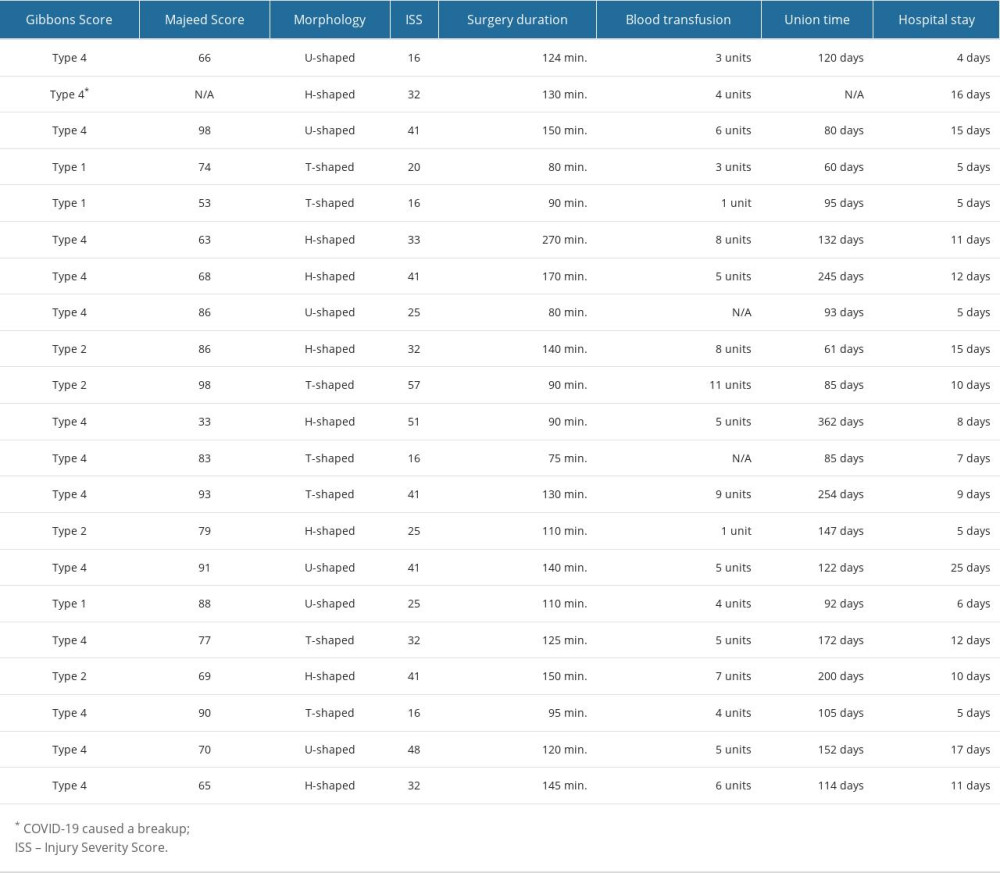 Table 3. The intraoperative and postoperative treatment outcomes of the patients.
Table 3. The intraoperative and postoperative treatment outcomes of the patients. In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952