12 January 2021: Clinical Research
Limb-Salvage Outcomes of Arterial Repair Beyond Time Limit at Different Lower-Extremity Injury Sites
Li Yu1ABCDEF, Linglong Deng1ABCDEF, Shaobo Zhu1BCD, Kai Deng1BCD, Guorong Yu1BCD, Chunquan Zhu1BCD, Baiwen Qi1ABCDEF, Zhenyu Pan1ABCDEF*DOI: 10.12659/MSM.927652
Med Sci Monit 2021; 27:e927652
Abstract
BACKGROUND: The purpose of this study was to analyze the outcomes of revascularization exceeding 12 h after arterial injury at different sites of the lower extremity.
MATERIAL AND METHODS: From January 2009 to April 2017, 58 patients with 58 lower-limb arterial injuries who underwent revascularization over 12 h after trauma were included in our study. Outcomes measured, including mortality, amputation, complications, and other parameters (gait, length discrepancy, the range of movement of the knee and ankle joint, and muscle wasting) were analyzed.
RESULTS: External iliac artery injury (EIAI) or femoral artery injury (FAI) was affected in 4 patients, superficial femoral artery injury (SFAI) in 18, and popliteal artery injury (PAI) (including proximal gastrocnemius muscle vascular (PGMV) and proximal gastrocnemius muscle vascular [PGMV]) in 36. The median time of arterial injury was 72 h (interquartile range, 59.5). No mortality was found. Amputations were performed in 16 patients due to non-viable limbs, progressing infection, or muscle necrosis. All patients were followed up (median, 52 months; interquartile range, 5.5). Of the 42 limb-salvage patients, most had a limp, muscle wasting, or ankle and knee dysfunctions, and 26 patients with knee or ankle dysfunction underwent secondary surgery.
CONCLUSIONS: Although limited recanalization of blood vessels may lead to limb complications or amputations over time, the high success rate of limb salvage still merits the surgeon’s best efforts.
Keywords: Amputation, Femoral Artery, Iliac Artery, Leg Injuries, Popliteal Artery, Gait, Limb Salvage, Mortality, Postoperative Complications, Reoperation
Background
The management of lower-extremity trauma remains challenging and is highly associated with limb loss [1]. Amputation following lower-extremity trauma has been variously ascribed to extent of soft tissue damage or bone defect, ischemia-related vascular injuries, and development of compartment syndrome [2–4]. Among many associated factors, traumatic artery injury presents the most significant threat to limb survival, with amputation rates reported as high as 70% [5], particularly in resource-limited developing countries such as China, where amputation rates may be even higher. Overwhelmingly, saving the patient’s life and improving the rate of limb salvage are the goals [6]. Prior studies have documented factors that affect limb salvage after arterial injury [7], of which the duration of ischemia is the most influential [8,9]. The golden time for arterial repair, widely accepted by scholars and researchers, is less than 6 h [10]. Hence, essential management for substantial improvement in limb salvage rates includes attention to minimizing delayed repair of vascular injury [11]. This is somewhat low given the fact that most of the revascularizations were done after the golden period had passed [12]. Due to technical and medical limitations or delays in diagnosis at local primary hospitals, most patients were transferred to tertiary care centers for revascularization later than 6 h after injury [13].
In addition to a higher amputation rate, delayed revascularization is associated with a poor prognosis for sensory and motor function [14]. Nonetheless, recent studies suggest that delayed intervention (later than 6 h) also presented acceptable outcomes [15,16]. Silva et al. [15] studied the retention of limb motor function after vascular time-out reconstruction (mean, 10 h) in selected cases. However, the reasons why muscles remain viable after prolonged ischemia have been largely unclear. In our institution, we found that similar traumatic violence, but in different sites of the lower extremity, resulted in different outcomes (e.g., amputation rate, limb function, limb deformity). For example, some patients with vascular injury still maintained muscle viability for 2–3 days or even 1 week, while others developed more severe muscle necrosis within 10 h. To the best of our knowledge, there have been few studies exploring how limbs undergoing revascularization with prolonged ischemia could still survive.
In the present study, we evaluated the efficacy of delayed revascularization (beyond 12 h) in patients with arterial injury and attempted to better understand the associated factors.
Material and Methods
STATISTICAL ANALYSIS:
Outcomes were compared across 3 principal aspects: (1) vascular repair sites and mechanisms, (2) primary and secondary amputation, and (3) long-term functions of the affected limb. Data were analyzed using SPSS 19.0 statistical software. Independent-samples
Results
All 58 patients were diagnosed with artery injuries accompanied by prolonged ischemia at least 12 h after trauma (median, 72 h; interquartile range, 59.5). The external iliac artery injury (EIAI) and femoral artery injury (FAI) were involved in 4 patients (6.90%), superficial femoral artery injury (SFAI) in 18 patients (31.03%), and popliteal artery injury (PAI) in 36 patients (62.07%). In the PAI group, 15 cases of arterial injury occurred in the proximal part of the gastrocnemius muscle vasculature (PGMV) and 21 cases of arterial injury occurred in the distal part of the gastrocnemius muscle vasculature (DGMV) (Figure 2). Mechanisms of injury were categorized as blunt trauma in 79.31%, stab wound in 15.52%, and gunshot wound in 5.17%. No significant differences existed between these groups (
There was no pre- or post-operative mortality. Three patients (1 SFAI, 1 PGMVI, and 1 DGMVI) presented with non-viable limbs and underwent primary amputation. Primary amputation was not significantly different between the 4 groups (
Among the 44 patients with limb salvage, 26 had related complications, including 6 patients (15.38%) with chronic osteomyelitis, 3 patients (7.69%) with nonunion, 10 patients with soft-tissue infection, and 7 patients with muscle necrosis, respectively. Compared with the other 3 groups, the DGMV group had the lowest complication rate (
In the long-term follow-up, the sensory and motor functions of most patients with limb salvage were seriously affected (Table 2). Motor dysfunctions, including limp, length discrepancy, RMK, RMA, and muscle wasting, were noted in all 4 groups. Except that KRM in DGMVI group was superior to the other 3 groups (
Finally, for patients with partial knee or ankle joint loss due to muscle necrosis or fibrosis, further surgeries were required by 2 patients in the EIAI (Figure 3) or FAI group, 3 patients in the SFAI group (Figure 4), 4 patients in the PGMVI group, and 8 patients in the DGMVI group (Figure 5).
Discussion
Based on the replantation time of the amputated limb, the optimal golden time of revascularization was less than 6 h [12,20]. Unlike amputated limbs, which may resist up to a typical 6 h of ischemia because of complete disruption of blood supply, limbs with arterial injuries could survive longer due to collateral circulation. However, prolonged ischemia of an injured limb (longer than 6 h) is associated with a 4-fold increased risk of secondary amputation [10]. Therefore, whether revascularization is worth more than 6 h after arterial injury has been a controversial issue. Prior studies have reported that limbs with revascularization later than 24 h (or even one week) after arterial injury could be salvaged successfully [12,21], but the reasons why the limbs that underwent revascularization with prolonged ischemia time can survive is less well understood.
After the trunk vascular injury, the tissue blood supply is seriously reduced and insufficient, which makes the tissue enter into the ischemic tolerance period. At this point, collateral circulation begins to play a critical role in pathophysiological processes, providing a small amount of blood supply to tissue metabolism. In other words, collateral circulation, to a certain extent, determines the prospects of limb salvage in patients with delayed revascularization after vascular injury. In the lower extremity, the abundance of collateral branches varies in different anatomical sites, which indicates that delayed vascular repair after trunk vascular injury at different anatomical sites may present distinct limb salvage effects. Perkins et al. [8] identified the anatomical site of the arterial injury as a risk factor for amputation after a meta-analysis reviewing the prognostic factors for surgical repair of lower-extremity vascular trauma. In our study, we classified the vascular injury of lower limbs according to the anatomic sites to explore the limb-salvage outcomes after revascularization for more than 12 h.
Accordingly, we found that compared with EIAI, FAI, and PGMVI, SFAI and DGMVI presented encouraging limb salvage outcomes with lower rates of primary and secondary amputation, which is consistent with the literature [22,23] Traupe et al. [24] quantified function of collateral arteries by balloon occlusion of the superficial femoral artery, and concluded that the superficial femoral artery has abundant collateral circulation, which plays a key role in the pathophysiological process of limb ischemia. Indeed, the superficial femoral artery and the profunda femoris artery form a collateral bed between the ileo-femoral segment and the popliteal artery. Consequently, among patients with SFAI lasting more than 12 h, the majority (94.44%) had successful revascularization and avoided primary amputation. Due to anatomic factors of the thigh, prophylactic and therapeutic osteofascial operations are generally not required, which reduces the incidence of complications such as infection and osteomyelitis, resulting in a low rate (11.11%) of secondary amputation. Therefore, compared with popliteal artery injury, superficial femoral artery injury has the innate advantage of limb salvage. Inevitably, superficial femoral arterial injury was followed by the disruption of blood supply to the calf muscles. So, in our study, as the result of the anterior and posterior muscles ischemic necrosis or nerve injury, some patients lost most of their knee and ankle joint functions, and developed clubfoot deformity.
In contrast, the occurrence of limb salvage effects like SFAI in EIAI or FAI seems relatively rare. As a consequence of the absence of corresponding collateral circulation in the proximal femoral artery and the external iliac artery, high amputation rates, especially in secondary amputation, occurred in our series. Accordingly, in 4 EIAI or FAI patients, 2 had amputation due to massive toxin absorption, with no remission on dialysis. Although the other 2 patients had their limbs salvaged after hemodialysis and multiple debridements, their knee and ankle functions were almost completely lost. Hence, in this scenario, revascularization should be performed as early as possible, especially where there is little collateral circulation.
Among all vascular injuries in the lower limbs, popliteal artery injury is considered to be the most serious threat to limb survival [25]. In our study, according to the anatomical positions between the popliteal artery and the gastrocnemius, popliteal artery injuries were classified into PGMVI and DGMVI. Since the popliteal artery has relatively few branching loops before entering the gastrocnemius, popliteal artery injury in PGMV has significant and severe symptoms of lower-limb ischemia. If the PGMVI were missed or delayed in repair, the likelihood of amputation would be very high. In most cases, popliteal artery injury, which often resulted from high-energy injury, is frequently associated with the knee fracture, dislocations, and severe tissue swelling. In this context, anastomotic vessels are prone to embolize again. Moreover, most patients had to undergo prophylactic and therapeutic fasciotomy, which can increase the risk of osteomyelitis and aggravating infections. Logically, it can be assumed that the secondary amputation rate increased because of the above complications, and this may account for the high amputation rates in patients with PGMVI. However, due to the abundant collateral circulation of the popliteal artery in the gastrocnemius segment, when the popliteal artery is injured at DGMV, even in the posterior deep muscle, the blood supply is still not completely interrupted. In our study, following vascular anastomosis, the amputation rate (9.52%) in the DGMV group was lower than that in the PGMV group (46.67%), which was attributed to better vascular bed. Moini et al. [25] assessed the outcomes of delayed vascular repair from 3 aspects: motor loss, sensory loss, and muscle viability. They concluded that a high success rate of vascular recanalization and limb salvage would be achieved in the presence of viable gastrocnemius muscle after popliteal artery injury. Jagdish et al. [12] also determined that delayed revascularization after popliteal injury in some cases resulted in improved sensory and motor functions under the condition of gastrocnemius vitality. In our study, due to popliteal artery injury, the posterior tibial muscle had ischemic necrosis, which more or less affected the lower-extremity motor function of patients, such as foot deformity, limp, and limited joint activity.
Several studies have delineated factors affecting sensor functions after vascular injury; time to revascularization is one of the crucial factors [26]. In our series, we observed 4 groups of varying degrees of sensory impairment. Since sensory dysfunction is mainly caused by nerve injury, and some patients had nerve injury on admission, we cannot accurately judge the effect of delayed vascular repair at different sites on sensory function. Therefore, early vascular repair may avoid aggravating sensory dysfunctions.
Additionally, modern techniques have made limb salvage possible, but many people have been skeptical about the long-term disability it brings [27]. Although major advances in medicine have improved the technical capacity to reconstruct severely injured limbs, concurrent development of bioengineering in prosthetics also can provide good function for amputees [28]. Therefore, patients with severe trauma may face the challenge of choosing between amputation and limb salvage. Attempts to save limbs necessitate multiple operations, often resulting in partial or complete loss of functions, which imposes a greater financial and psychological burden on patients. However, some patients still prefer limb salvage because of psychological rejection of prosthetic limbs. Several studies also have reported significant disability following limb salvage of such injuries, with patients often complaining of severe pain while walking, difficulty returning to work, and, in some cases, permanent disability [29,30]. Mitchell et al. [30] observed the outcomes of amputation versus limb salvage following major lower-extremity trauma and found that the functional prognosis of amputees after wearing a prosthesis was better than that of patients with limb salvage. If such patients can return to normal activities after amputation and early postoperative prosthesis, avoiding the sufferings of poor limb function after limb salvage, this is in line with the concept of accelerated rehabilitation. The purpose of surgery is to obtain the best limb function outcome in patients with severe limb injury that is not life threatening. Therefore, amputation and early postoperative prosthesis may be a consideration for lower-extremity vascular injury with poor prognostic function if patients can accept the prosthesis psychologically.
The outcomes of delayed repair of damaged vasculature are closely related to collateral circulation at the sites of vascular injury. Abundant vascular branches could provide the possibility of limb salvage beyond the time limit after arterial injury, but poor sensory and motor function may ultimately still be unavoidable. Therefore, in the face of vascular injury, it is important to complete revascularization as early as possible if limb salvage is planned.
Conclusions
Early diagnosis and timely revascularization are still the basic principles in the treatment of vascular injury. Vascular recanalization beyond the time limit is not necessarily an absolute indication for amputation. In terms of limb salvage, once a lower-limb arterial injury is diagnosed, even delayed revascularization can still be actively considered because of the relatively high success rate. However, considering the unsatisfactory functions of the limb after limb salvage, this is still a dilemma that patients have to face.
Figures
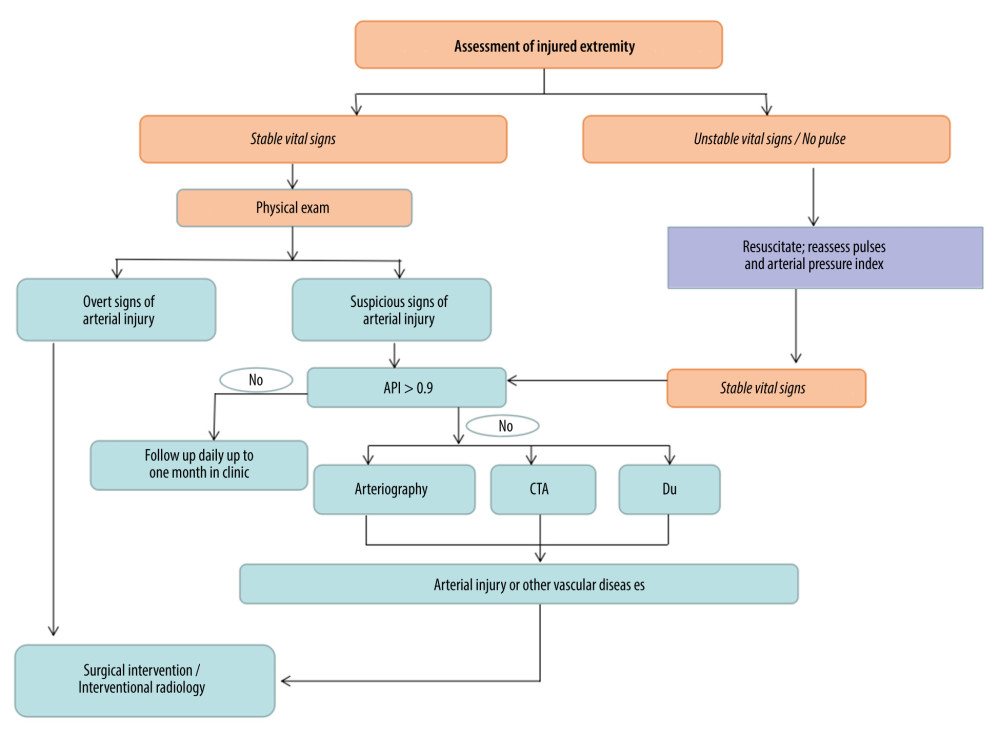 Figure 1. Algorithm for evaluation of patient with possible vascular injury. DU – Doppler ultrasonography; API – Doppler arterial pressure distal to injury/Doppler arterial pressure in uninvolved upper extremity.
Figure 1. Algorithm for evaluation of patient with possible vascular injury. DU – Doppler ultrasonography; API – Doppler arterial pressure distal to injury/Doppler arterial pressure in uninvolved upper extremity. 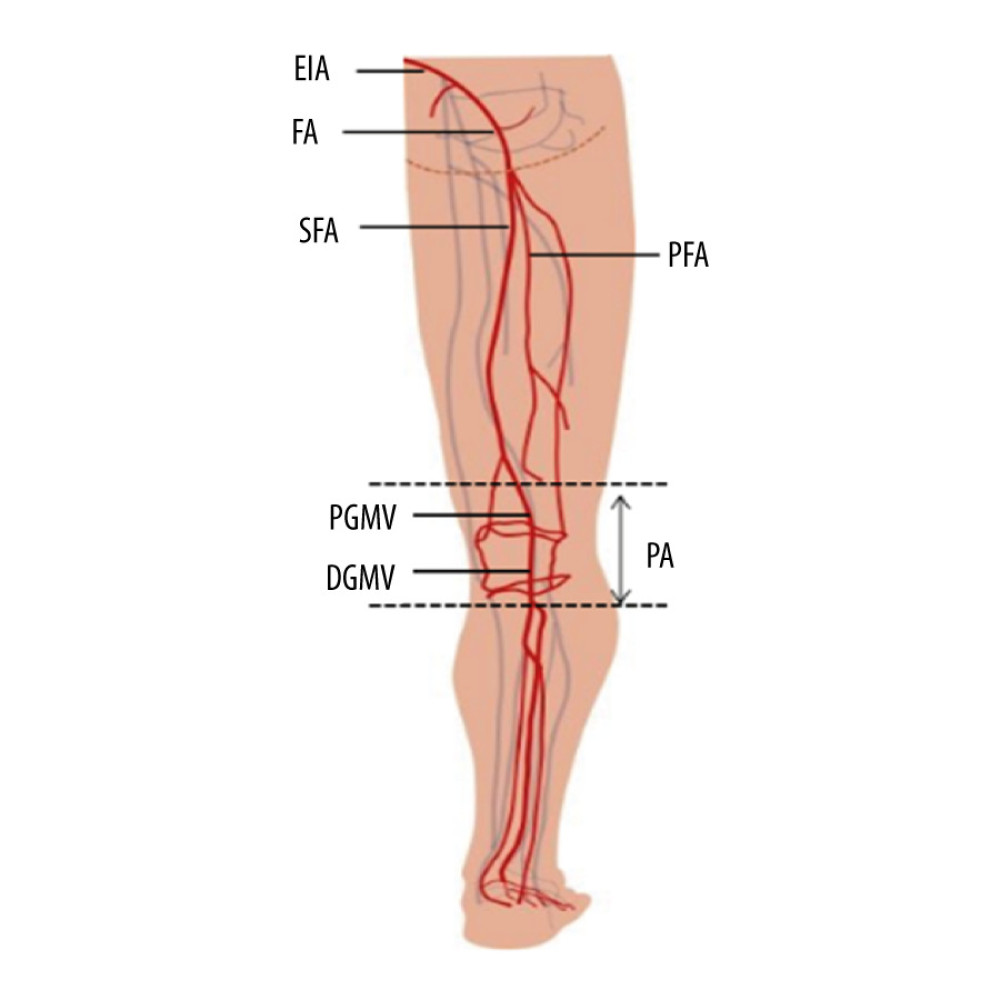 Figure 2. Schematic illustration of vascular injury sites in lower extremity. EIA – extemal iliac artery; FA – femoral artery; PFA – profounda femoral artery; SFA – superficial femoral artery; PA – popliteal artery; PGMV – proximaI gastrocnemius muscle vascular; DGMV – distal gastrocnemius muscle vascular.
Figure 2. Schematic illustration of vascular injury sites in lower extremity. EIA – extemal iliac artery; FA – femoral artery; PFA – profounda femoral artery; SFA – superficial femoral artery; PA – popliteal artery; PGMV – proximaI gastrocnemius muscle vascular; DGMV – distal gastrocnemius muscle vascular.  Figure 3. A typical example of delayed repair of EIAI (27 h): A 10-year-old boy sustained a car accident, open pelvic fracture, and extensive avulsion of the abdomen and right thigh. After local hospital debridement, the patient was transferred to our hospital. As a result of intractable hypotension, exploratory surgery was immediately prepared. We found a rupture in the right external iliac artery, and then revascularized the damaged artery using a saphenous vein graft (SVG). After 1 week of dialysis, 4 debridements, and a skin graft, his life and lower limbs were saved. At the 10th year of follow-up, there were many scars in his inguinal region and right thigh (A). His motor function was severely impaired, including a maximum knee flexion of 80 degrees (B) and a clubfoot deformity (C). Achilles tendon release surgery and subtalar-talonavicular joint fusion were performed to correct the deformities (D).
Figure 3. A typical example of delayed repair of EIAI (27 h): A 10-year-old boy sustained a car accident, open pelvic fracture, and extensive avulsion of the abdomen and right thigh. After local hospital debridement, the patient was transferred to our hospital. As a result of intractable hypotension, exploratory surgery was immediately prepared. We found a rupture in the right external iliac artery, and then revascularized the damaged artery using a saphenous vein graft (SVG). After 1 week of dialysis, 4 debridements, and a skin graft, his life and lower limbs were saved. At the 10th year of follow-up, there were many scars in his inguinal region and right thigh (A). His motor function was severely impaired, including a maximum knee flexion of 80 degrees (B) and a clubfoot deformity (C). Achilles tendon release surgery and subtalar-talonavicular joint fusion were performed to correct the deformities (D). 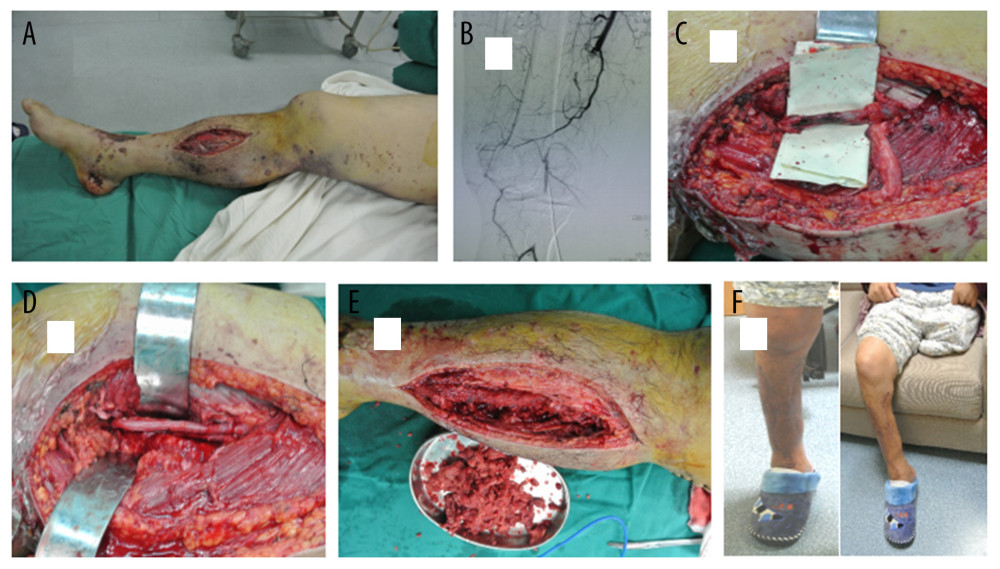 Figure 4. A typical example of delayed repair of SFAI (72 h). A 41-year-old man was struck by a car. In a local hospital, a closed dislocation of his right knee joint was reduced 8 h after the injury and an amputation was performed in his left leg due to the severity of the injury. Three days later, the patient was transferred to our hospital to treat the limb ischemia. A few mottling and some muscle-necrosis wounds were found on his foot (A). The angiography demonstrated injury to the superficial femoral artery, but the lateral branches of the deep femoral artery and the anterior and posterior tibial arteries were clearly presented (B). Intraoperatively, SFAI with long-segment embolus (C) was revascularized by SVG (D). After multiple debridements to remove necrotic tissue (E), the incision of the decompression of compartment was sutured. Lower extremity follow-up at 32 months showed good ankle and knee functions (F).
Figure 4. A typical example of delayed repair of SFAI (72 h). A 41-year-old man was struck by a car. In a local hospital, a closed dislocation of his right knee joint was reduced 8 h after the injury and an amputation was performed in his left leg due to the severity of the injury. Three days later, the patient was transferred to our hospital to treat the limb ischemia. A few mottling and some muscle-necrosis wounds were found on his foot (A). The angiography demonstrated injury to the superficial femoral artery, but the lateral branches of the deep femoral artery and the anterior and posterior tibial arteries were clearly presented (B). Intraoperatively, SFAI with long-segment embolus (C) was revascularized by SVG (D). After multiple debridements to remove necrotic tissue (E), the incision of the decompression of compartment was sutured. Lower extremity follow-up at 32 months showed good ankle and knee functions (F). 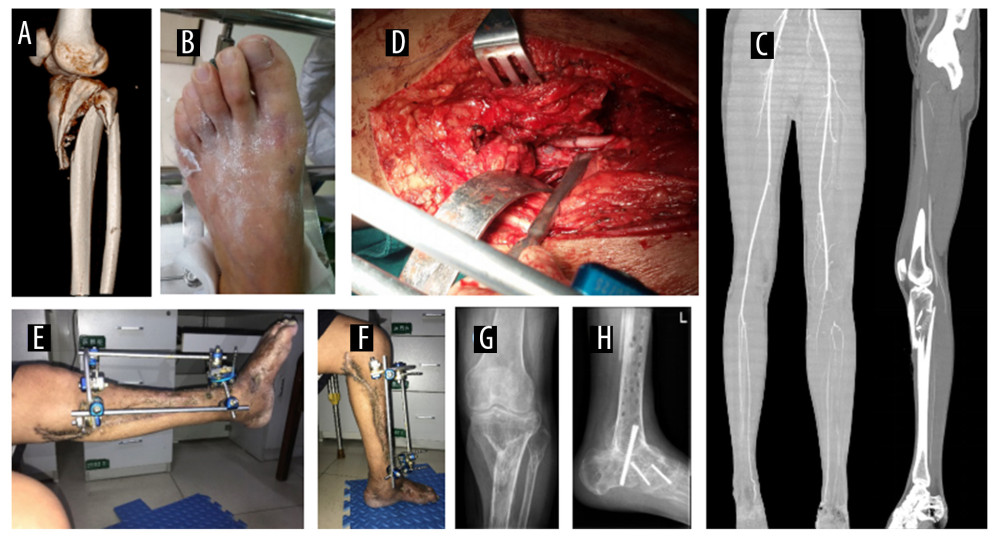 Figure 5. A typical example of delayed repair of PAI at DGMV (60 h). A 41-year-old man was admitted to a local hospital due to a traffic accident, suffering tibia and fibula fractures with a popliteal artery injury of his left leg (A). At 2 days after trauma, the patient was transferred to our hospital. The skin color of the left foot seemed normal but there was no pulse (B). CTA revealed popliteal artery embolization at DGMV, but the blood signal of the gastrector artery, the calf artery, and the collateral circulation were very clear (C). The PAI was confirmed intra-operatively, and revascularization was performed by end-to-end anastomosis (D). After external fixation of the fracture, good knee function was presented (E, F). However, 1 year after fracture healing, poor ankle function (clubfoot deformity) was corrected by four-joint fusion (G, H).
Figure 5. A typical example of delayed repair of PAI at DGMV (60 h). A 41-year-old man was admitted to a local hospital due to a traffic accident, suffering tibia and fibula fractures with a popliteal artery injury of his left leg (A). At 2 days after trauma, the patient was transferred to our hospital. The skin color of the left foot seemed normal but there was no pulse (B). CTA revealed popliteal artery embolization at DGMV, but the blood signal of the gastrector artery, the calf artery, and the collateral circulation were very clear (C). The PAI was confirmed intra-operatively, and revascularization was performed by end-to-end anastomosis (D). After external fixation of the fracture, good knee function was presented (E, F). However, 1 year after fracture healing, poor ankle function (clubfoot deformity) was corrected by four-joint fusion (G, H). References
1. Low EE, Inkellis E, Morshed S, Complications and revision amputation following trauma-related lower limb loss: Injury, 2017; 48(2); 364-70
2. Azouz SM, Castel NA, Vijayasekaran A, Lower-limb reconstruction with chimeric flaps: The quad flap: Microsurgery, 2019; 39(2); 182-87
3. Chimutengwende-Gordon M, Mbogo A, Khan W, Limb reconstruction after traumatic bone loss: Injury, 2017; 48(2); 206-13
4. Almasri J, Adusumalli J, Asi N, A systematic review and meta-analysis of revascularization outcomes of infrainguinal chronic limb-threatening ischemia: J Vasc Surg, 2018; 68(2); 624-33
5. Yan H, Zhao B, Kolkin J, The management of lower extremity multilevel arterial injuries: A 10-year experience: PLoS One, 2015; 10(3); e0121769
6. Feliciano DV, For the patient-evolution in the management of vascular trauma: J Trauma Acute Care Surg, 2017; 83(6); 1205-12
7. Hafez HM, Woolgar J, Robbs JV, Lower extremity arterial injury: Results of 550 cases and review of risk factors associated with limb loss: J Vasc Surg, 2001; 33(6); 1212-19
8. Perkins ZB, Yet B, Glasgow S, Meta analysis of prognostic factors for amputation following surgical repair of lower extremity vascular trauma: Journal of Vascular Surgery, 2015; 62(1); 265-65
9. Micari A, Sbarzaglia P, Meeks MDME, New imaging modalities in peripheral interventions: European Heart Journal Supplements, 2015; 17(Suppl A); A18-22
10. Baghi I, Herfatkar MR, Shokrgozar L, Assessment of vascular injuries and reconstruction: Trauma Mon, 2015; 20(4); e30469
11. Maithel S, Fujitani RM, Grigorian A, Outcomes and predictors of popliteal artery injury in pediatric trauma: Ann Vasc Surg, 2020; 66; 242-49
12. Jagdish K, Paiman M, Nawfar A, The outcomes of salvage surgery for vascular injury in the extremities: A special consideration for delayed revascularization: Malays Orthop J, 2014; 8(1); 14-20
13. Kohli A, Singh G, Management of extremity vascular trauma: Jammu experience: Asian Cardiovasc Thorac Ann, 2008; 16(3); 212-14
14. Franz RW, Shah KJ, Halaharvi D, A 5-year review of management of lower extremity arterial injuries at an urban level I trauma center: J Vasc Surg, 2011; 53(6); 1604-10
15. de Silva W, Ubayasiri RA, Weerasinghe CW, Challenges in the management of extremity vascular injuries: A wartime experience from a tertiary centre in Sri Lanka: World J Emerg Surg, 2011; 6; 24
16. Huynh TT, Pham M, Griffin LW, Management of distal femoral and popliteal arterial injuries: an update: Am J Surg, 2006; 192(6); 773-78
17. Slauterbeck JR, Britton C, Moneim MS, Mangled extremity severity score: An accurate guide to treatment of the severely injured upper extremity: J Orthop Trauma, 1994; 8(4); 282-85
18. Feliciano DV, Moore FA, Moore EE, Evaluation and management of peripheral vascular injury. Part 1. Western Trauma Association/critical decisions in trauma: J Trauma, 2011; 70(6); 1551-56
19. Langer V, Management of major limb injuries: ScientificWorldJournal, 2014; 2014 640430
20. Imerci A, Özaksar K, Gürbüz Y, Popliteal artery injury associated with blunt trauma to the knee without fracture or dislocation: Western Journal of Emergency Medicine Integrating Emergency Care with Population Health, 2014; 15(2); 145-48
21. Moini M, Hamedani K, Rasouli MR, Outcome of delayed brachial artery repair in patients with traumatic brachial artery injury: Prospective study: Int J Surg, 2008; 6(1); 20-22
22. Stanley BB, Teague B, Raptis S, Efficacy of balloon angioplasty of the superficial femoral artery and popliteal artery in the relief of leg ischemia: J Vasc Surg, 1996; 23(4); 679-85
23. Jawas A, Abbas AK, Nazzal M, Management of war-related vascular injuries: Experience from the second gulf war: World J Emerg Surg, 2013; 8(1); 22
24. Traupe T, Ortmann J, Stoller M, Direct quantitative assessment of the peripheral artery collateral circulation in patients undergoing angiography: Circulation, 2013; 128(7); 737-44
25. Moini M, Takyar MA, Rasouli MR, Revascularization later than 24h after popliteal artery trauma: Is it worthwhile?: Injury, 2007; 38(9); 1098-101
26. Mullenix PS, Steele SR, Andersen CA, Limb salvage and outcomes among patients with traumatic popliteal vascular injury: An analysis of the National Trauma Data Bank: J Vasc Surg, 2006; 44(1); 94-100
27. Bosse MJ, Teague D, Reider L, Outcomes after severe distal tibia, ankle, and/or foot trauma: Comparison of limb salvage versus transtibial amputation (OUTLET): J Orthop Trauma, 2017; 31(Suppl 1); S48-55
28. , Section 2: Limb Salvage and Amputation After Major Lower Limb Trauma: J Orthop Trauma, 2017; 31(Suppl 1); S39
29. Shawen SB, Keeling JJ, Branstetter J, The mangled foot and leg: Salvage versus amputation: Foot Ankle Clin, 2010; 15(1); 63-75
30. Mitchell SL, Hayda R, Chen AT, The Military Extremity Trauma Amputation/Limb Salvage (METALS) Study: Outcomes of amputation compared with limb salvage following major upper-extremity trauma: J Bone Joint Surg Am, 2019; 101(16); 1470-78
Figures
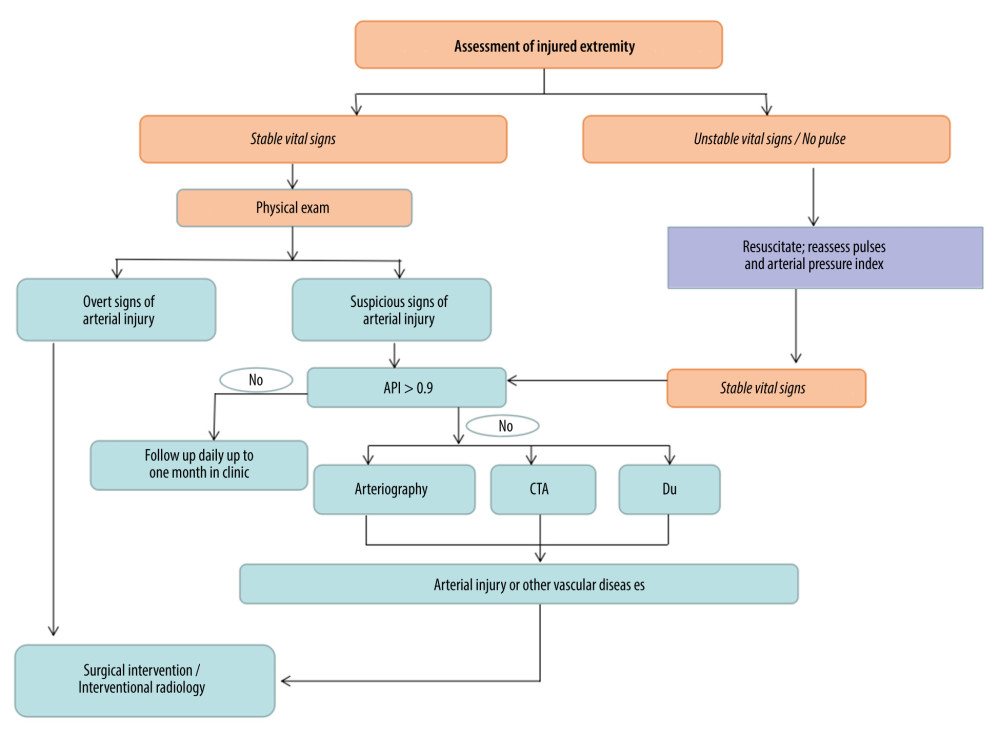 Figure 1. Algorithm for evaluation of patient with possible vascular injury. DU – Doppler ultrasonography; API – Doppler arterial pressure distal to injury/Doppler arterial pressure in uninvolved upper extremity.
Figure 1. Algorithm for evaluation of patient with possible vascular injury. DU – Doppler ultrasonography; API – Doppler arterial pressure distal to injury/Doppler arterial pressure in uninvolved upper extremity.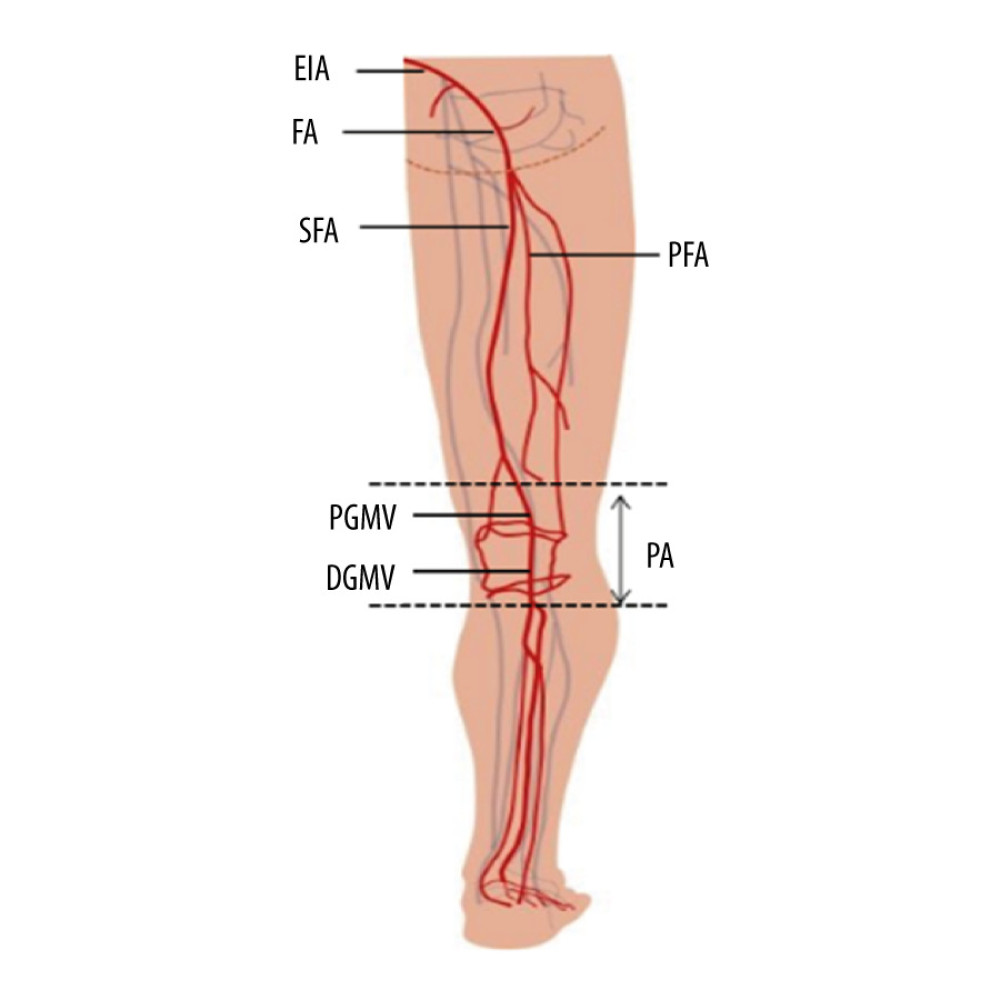 Figure 2. Schematic illustration of vascular injury sites in lower extremity. EIA – extemal iliac artery; FA – femoral artery; PFA – profounda femoral artery; SFA – superficial femoral artery; PA – popliteal artery; PGMV – proximaI gastrocnemius muscle vascular; DGMV – distal gastrocnemius muscle vascular.
Figure 2. Schematic illustration of vascular injury sites in lower extremity. EIA – extemal iliac artery; FA – femoral artery; PFA – profounda femoral artery; SFA – superficial femoral artery; PA – popliteal artery; PGMV – proximaI gastrocnemius muscle vascular; DGMV – distal gastrocnemius muscle vascular. Figure 3. A typical example of delayed repair of EIAI (27 h): A 10-year-old boy sustained a car accident, open pelvic fracture, and extensive avulsion of the abdomen and right thigh. After local hospital debridement, the patient was transferred to our hospital. As a result of intractable hypotension, exploratory surgery was immediately prepared. We found a rupture in the right external iliac artery, and then revascularized the damaged artery using a saphenous vein graft (SVG). After 1 week of dialysis, 4 debridements, and a skin graft, his life and lower limbs were saved. At the 10th year of follow-up, there were many scars in his inguinal region and right thigh (A). His motor function was severely impaired, including a maximum knee flexion of 80 degrees (B) and a clubfoot deformity (C). Achilles tendon release surgery and subtalar-talonavicular joint fusion were performed to correct the deformities (D).
Figure 3. A typical example of delayed repair of EIAI (27 h): A 10-year-old boy sustained a car accident, open pelvic fracture, and extensive avulsion of the abdomen and right thigh. After local hospital debridement, the patient was transferred to our hospital. As a result of intractable hypotension, exploratory surgery was immediately prepared. We found a rupture in the right external iliac artery, and then revascularized the damaged artery using a saphenous vein graft (SVG). After 1 week of dialysis, 4 debridements, and a skin graft, his life and lower limbs were saved. At the 10th year of follow-up, there were many scars in his inguinal region and right thigh (A). His motor function was severely impaired, including a maximum knee flexion of 80 degrees (B) and a clubfoot deformity (C). Achilles tendon release surgery and subtalar-talonavicular joint fusion were performed to correct the deformities (D).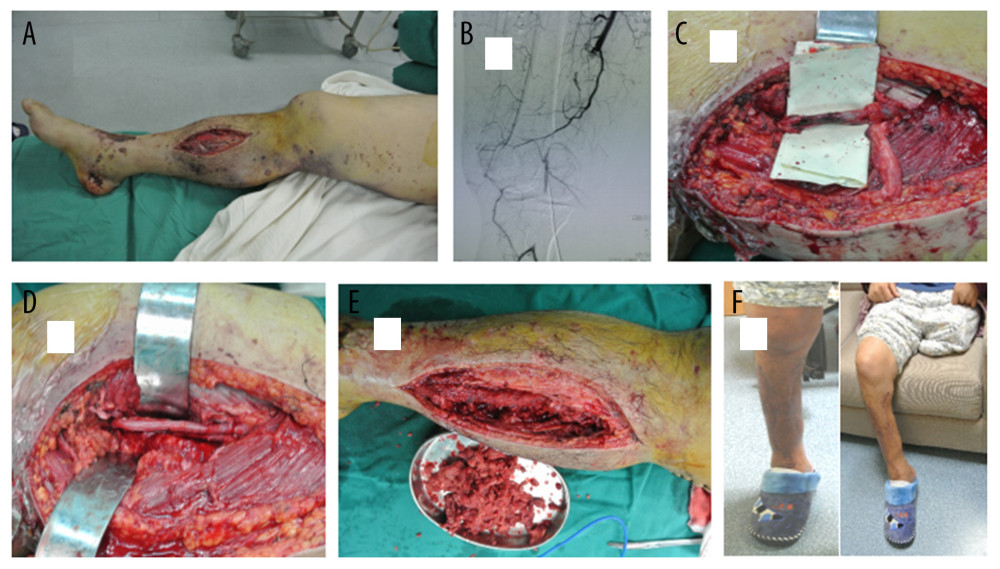 Figure 4. A typical example of delayed repair of SFAI (72 h). A 41-year-old man was struck by a car. In a local hospital, a closed dislocation of his right knee joint was reduced 8 h after the injury and an amputation was performed in his left leg due to the severity of the injury. Three days later, the patient was transferred to our hospital to treat the limb ischemia. A few mottling and some muscle-necrosis wounds were found on his foot (A). The angiography demonstrated injury to the superficial femoral artery, but the lateral branches of the deep femoral artery and the anterior and posterior tibial arteries were clearly presented (B). Intraoperatively, SFAI with long-segment embolus (C) was revascularized by SVG (D). After multiple debridements to remove necrotic tissue (E), the incision of the decompression of compartment was sutured. Lower extremity follow-up at 32 months showed good ankle and knee functions (F).
Figure 4. A typical example of delayed repair of SFAI (72 h). A 41-year-old man was struck by a car. In a local hospital, a closed dislocation of his right knee joint was reduced 8 h after the injury and an amputation was performed in his left leg due to the severity of the injury. Three days later, the patient was transferred to our hospital to treat the limb ischemia. A few mottling and some muscle-necrosis wounds were found on his foot (A). The angiography demonstrated injury to the superficial femoral artery, but the lateral branches of the deep femoral artery and the anterior and posterior tibial arteries were clearly presented (B). Intraoperatively, SFAI with long-segment embolus (C) was revascularized by SVG (D). After multiple debridements to remove necrotic tissue (E), the incision of the decompression of compartment was sutured. Lower extremity follow-up at 32 months showed good ankle and knee functions (F).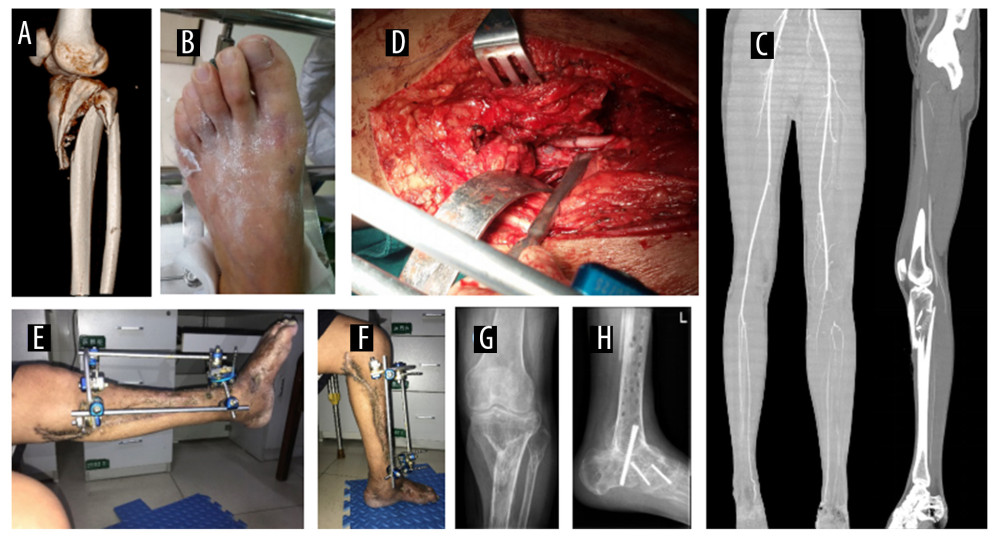 Figure 5. A typical example of delayed repair of PAI at DGMV (60 h). A 41-year-old man was admitted to a local hospital due to a traffic accident, suffering tibia and fibula fractures with a popliteal artery injury of his left leg (A). At 2 days after trauma, the patient was transferred to our hospital. The skin color of the left foot seemed normal but there was no pulse (B). CTA revealed popliteal artery embolization at DGMV, but the blood signal of the gastrector artery, the calf artery, and the collateral circulation were very clear (C). The PAI was confirmed intra-operatively, and revascularization was performed by end-to-end anastomosis (D). After external fixation of the fracture, good knee function was presented (E, F). However, 1 year after fracture healing, poor ankle function (clubfoot deformity) was corrected by four-joint fusion (G, H).
Figure 5. A typical example of delayed repair of PAI at DGMV (60 h). A 41-year-old man was admitted to a local hospital due to a traffic accident, suffering tibia and fibula fractures with a popliteal artery injury of his left leg (A). At 2 days after trauma, the patient was transferred to our hospital. The skin color of the left foot seemed normal but there was no pulse (B). CTA revealed popliteal artery embolization at DGMV, but the blood signal of the gastrector artery, the calf artery, and the collateral circulation were very clear (C). The PAI was confirmed intra-operatively, and revascularization was performed by end-to-end anastomosis (D). After external fixation of the fracture, good knee function was presented (E, F). However, 1 year after fracture healing, poor ankle function (clubfoot deformity) was corrected by four-joint fusion (G, H). Tables
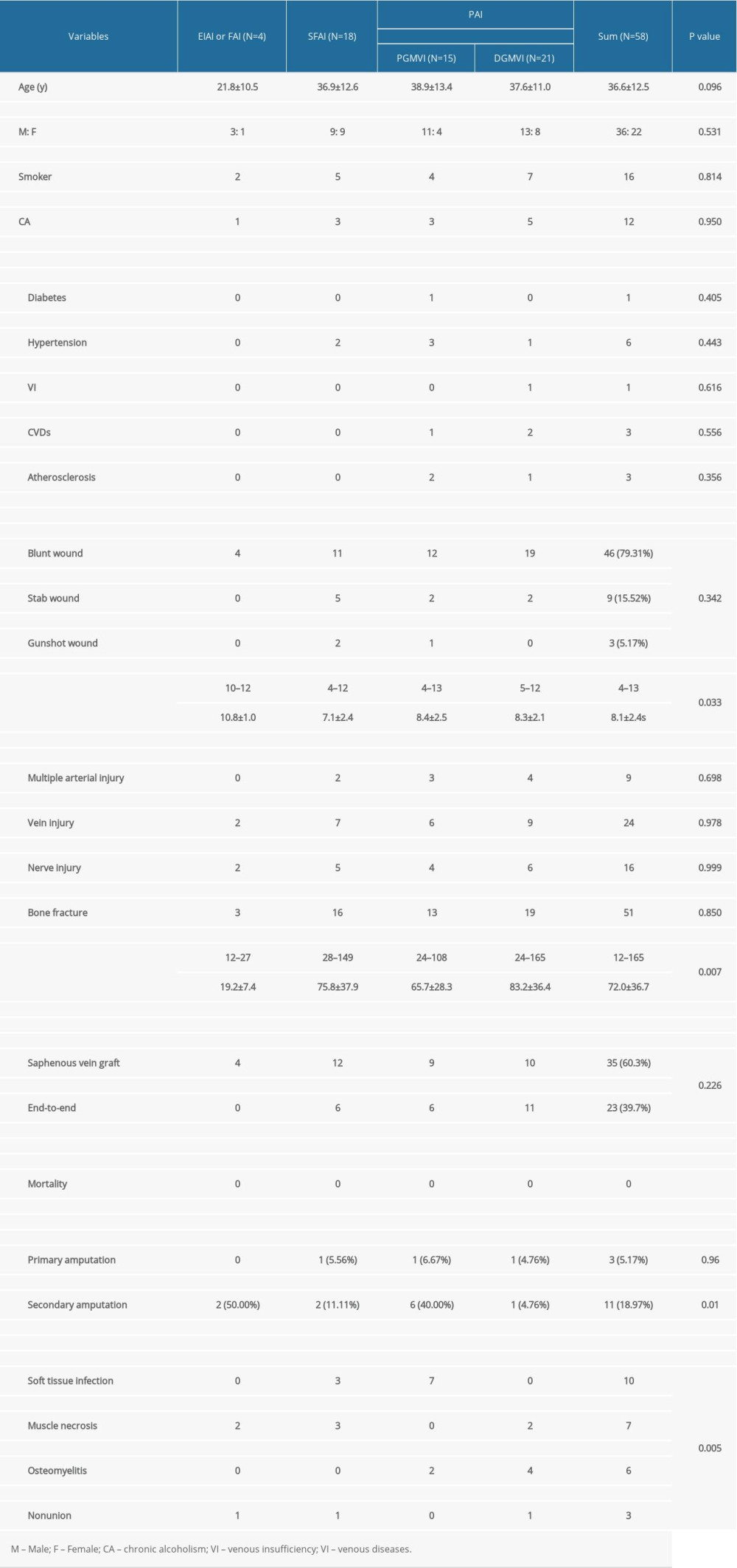 Table 1. Demographic data of different vascular injure site.
Table 1. Demographic data of different vascular injure site.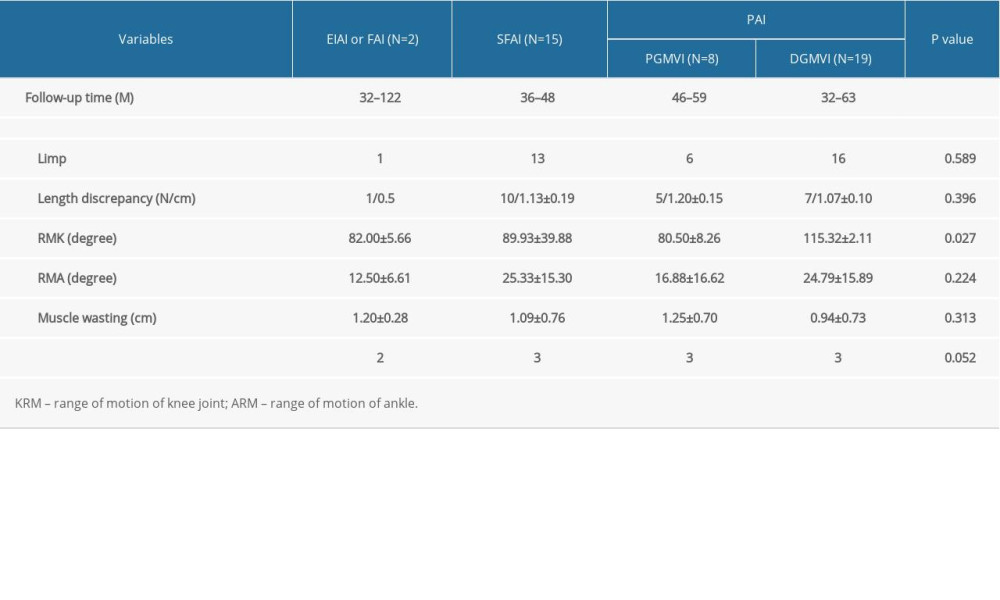 Table 2. Long-term follow-up of limb salvage patients with arterial injury at different sites.
Table 2. Long-term follow-up of limb salvage patients with arterial injury at different sites.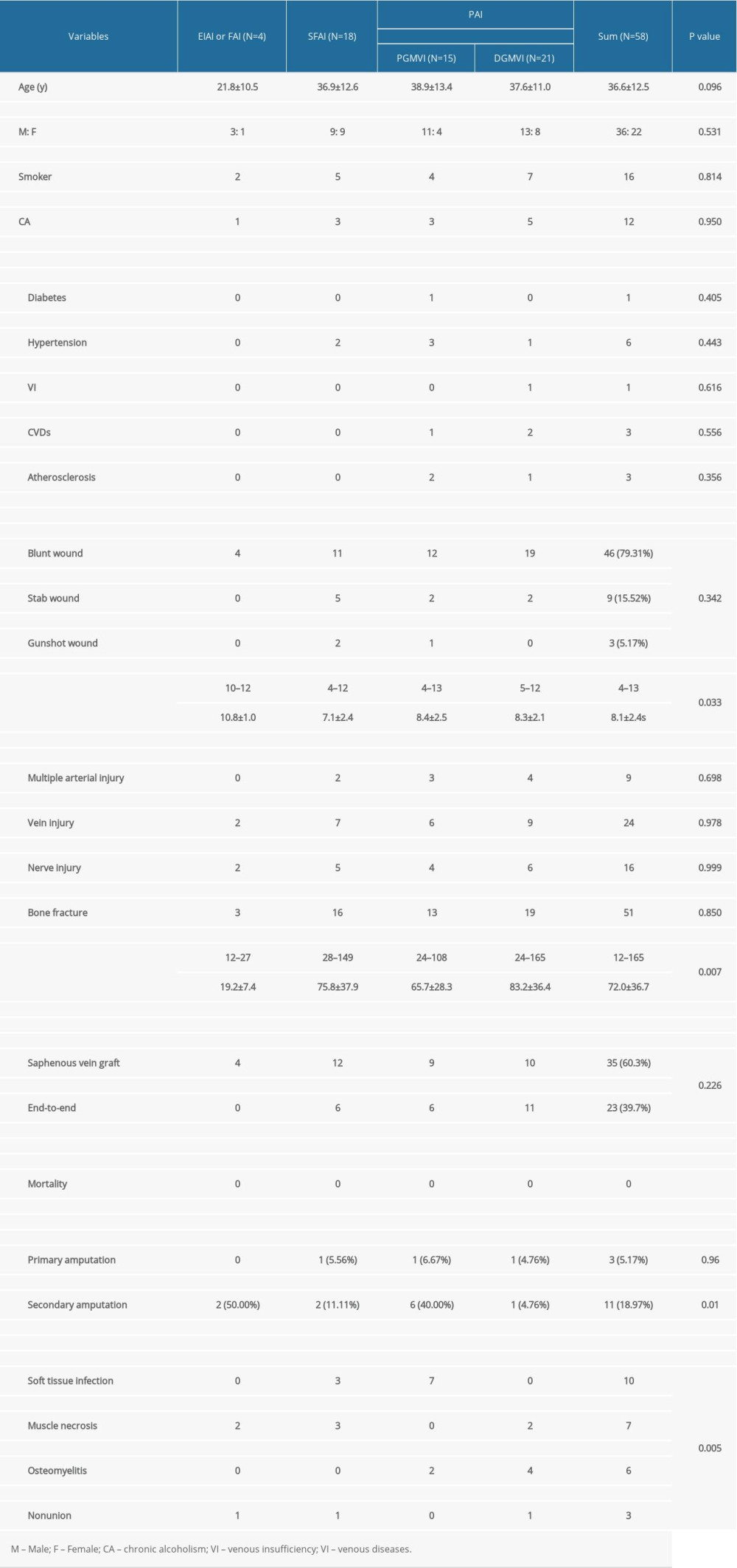 Table 1. Demographic data of different vascular injure site.
Table 1. Demographic data of different vascular injure site.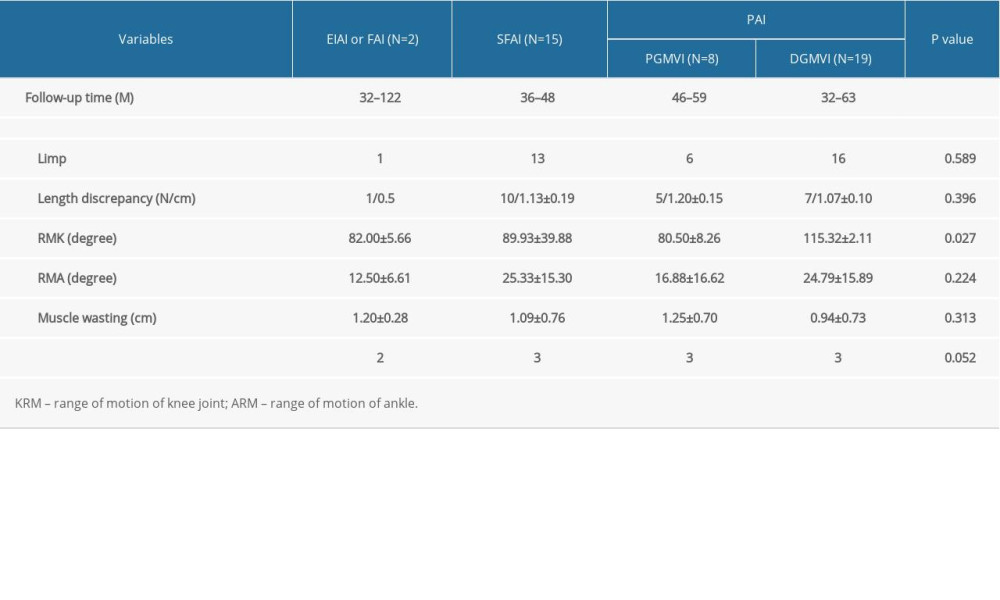 Table 2. Long-term follow-up of limb salvage patients with arterial injury at different sites.
Table 2. Long-term follow-up of limb salvage patients with arterial injury at different sites. In Press
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








