17 December 2020: Clinical Research
Group Music Intervention Using Percussion Instruments to Reduce Anxiety Among Elderly Male Veterans with Alzheimer Disease
Mu-N Liu1234ABDG, Ying-Jay Liou12AC, Wan-Chuan Wang56ABCD, Kuan-Chen Su5DEF, Heng-Liang Yeh7B, Chi‐ieong Lau89101112FG, Li-Yu Hu12DF, Shih-Jen Tsai123ADEG*, Hsin-Yi Chen513ADGDOI: 10.12659/MSM.928714
Med Sci Monit 2021; 27:e928714
Abstract
BACKGROUND: This study aimed to assess the impact of a group music intervention on anxiety and depression of elderly male veterans with dementia.
MATERIAL AND METHODS: In total, 50 elderly men with Alzheimer disease were randomly divided into intervention and control groups. Patients in the intervention group attended a 60-minute group music session that used percussion instruments with familiar music in the morning once a week for 12 weeks, whereas those in the control group received a rest and reading session at the same intervals and under the same conditions. The Hamilton Anxiety Rating Scale and Geriatric Depression Scale were used to assess anxiety and depression at baseline, week 6, and week 12. The Primary Measures of Music Audiation (PMMA) was used to assess musical aptitude at the baseline.
RESULTS: A significant reduction in the anxiety level following the 12-week music sessions was observed in the intervention group (P<.001), but there was no significant change in the control group. However, the change in depressive symptoms between the 2 groups was nonsignificant. In the intervention group, when stratifying patients based on music aptitude determined through PMMA assessment, patients with high PMMA scores had significantly reduced anxiety symptoms over time compared with those with low scores.
CONCLUSIONS: For elderly male veterans with dementia, participating in a group music intervention reduced anxiety symptoms. In patients with high musical aptitude, the treatment effects on anxiety reduction were satisfactory. Measures of music aptitude may provide valuable information regarding patients’ response to music intervention.
Keywords: Alzheimer Disease, Anxiety, Aptitude, Music, Veterans, Age Factors, Aged, 80 and over, Anxiety Disorders, Music Therapy, Taiwan
Background
Dementia is a clinical syndrome defined as a cluster of symptoms including memory difficulties, language and other cognitive function disturbances, behavior changes, and impairment of daily living activities [1]. The number of patients with dementia is expected to double every 20 years, reaching 43.2 million by 2020 and 81.1 million by 2040 [2]. Alzheimer disease (AD) is a chronic and progressive neurodegenerative disorder, and is the most common type of dementia [1]. With the anticipated 2-fold increase in the number of cases in the next few decades, this progressive disease has become a major public health problem.
Although cognitive decline is the cardinal characteristic of AD, neuropsychiatric symptoms associated with AD account for increased disability rates and seriously affect patient and caregiver quality of life [3]. Untreated depression and anxiety can contribute to worsening of functional status and may trigger behavioral disturbance in those with AD, which may further lead to institutionalization [3]. Patients with dementia and depression and/or anxiety are often managed with antidepressant and anxiolytic medications [3]. However, because of concerns regarding adverse effects from psychotropic medication and the relatively high likelihood of patients with dementia failing to comply with treatment [4], the use of nonpharmacological care strategies is vital in managing neuropsychiatric symptoms of patients with AD [5,6].
Music is a major means of triggering emotions. Music-based intervention stimulates intellectual function and reduces anxiety and depression, and thus significantly improves autonomy in patients with neurodegenerative disorders [5–8]. This is because the music is chosen on the basis of personal experience, with an aim of stimulating memory by evoking autobiographical events [9]. Several studies have assessed the effect of different types of music interventions on depression and anxiety symptoms for people with AD, such as passively listening to music alone or together with others and singing or playing instruments in a group setting [7]. Among these music approaches, playing percussion instruments may create a rich and stimulating music experience for patients with dementia [10], making it a beneficial and nonpharmacological intervention to alleviate neuropsychiatric symptoms [11].
Measures of musical aptitude provide valuable information about likely patient response that can be used for designing music intervention and strategies. Moreover, the effect of music intervention is greater among people with high musical aptitude because they are inclined to appreciate music and receive happiness and satisfaction when listening to it, as opposed to those with low musical aptitude [12]. Furthermore, a study indicated that people with high musical aptitude have a superior ability to process and transform auditory stimulation related to emotions than those without such aptitude [13]. Therefore, investigating the effect of baseline musical aptitude on response to music intervention is critical.
Most elderly Taiwanese veterans came to Taiwan during their teenage years toward the end of the 1940s from hometowns throughout mainland China [14]. Most of them are men, have a minimal extent of formal education, and live in government-sponsored long-term care institutions known as veterans’ homes. Because of the passage of time and changing social structures, elderly veterans now lack a support system and have become a distinct minority group in Taiwan [15]. In addition, elderly veterans are vulnerable to dementia and neuropsychiatric symptoms [16] and prone to adverse effects from medications [4]. Therefore, the efficacy of nonpharmacological interventions should be explored in this vulnerable population [6]. To the best of our knowledge, few studies have assessed the impact of group music percussion interventions on male veterans with dementia. This study aimed to determine (1) whether the use of percussion in group music intervention could reduce depression and anxiety levels in elderly male veterans with AD and (2) whether the baseline musical aptitude could affect the response to a music intervention. Our findings can serve as a foundation for future nonpharmacological programs for elderly men with AD.
Material and Methods
PATIENTS:
We selected 50 patients from veterans’ homes in northern Taiwan. The patients usually lived in the veteran’s homes in a long-term stay setting or dementia center. All patients had to meet the following inclusion criteria: (1) a resident of veterans’ homes; (2) male gender, (3) aged 75 years or older; (4) meeting the diagnostic criteria for probable AD according to the National Institute of Neurological and Communicative Disorders [17], in a mild or moderate stage based on the Clinical Dementia Rating scale (CDR, 1 and 2); (5) in a mild level of anxiety based on HAMA score below 17 [18]; (6) receiving stable psychotropic or anxiolytic treatment for 3 months; (7) able to communicate in Mandarin or Taiwanese; (8) no severe hearing impairment; (9) able to follow simple instructions and participate in easy and simple activities, and (10) capable of engaging in the evaluation and intervention. Patients and their relatives and caregivers at the veteran’s homes signed informed consent forms prior to inclusion in the study. The study was approved by the Ethics Committee of Taipei Veterans’ General Hospital.
RANDOMIZATION:
Patients with AD were randomized into an intervention or a control group with a 1: 1 ratio after matching by age and CDR level. An external expert who had no direct contact with the patients generated the randomization list using a spreadsheet software program and kept each patient’s allocation concealed. The assessor, the music facilitator, and the participants were not able to know the group allocation in advance. Only the outcome assessor was blinded to the group allocation throughout the trial. At the time of assessments, participants were reminded not to reveal their allocation to the assessor.
STUDY DESIGN:
In the intervention group, patients received 12 weeks of music intervention once per week (a total of 12 sessions). In the control group, without active participation in music intervention, patients participated in a rest and reading session, at the same intervals and under the same conditions. All participants were assessed for level of depression and for anxiety severity using the Geriatric Depression Scale – short form (GDS) [19], and the Hamilton Anxiety Rating Scale (HAMA) [20] at baseline, week 6, and week 12. Musical aptitude was assessed using the Primary Measures of Music Audiation (PMMA) at baseline. Within the intervention group, patients were further stratified into 2 groups categorized by PMMA overall scores; 0–20 (low musical aptitude subgroup) or 21–100 (high musical aptitude subgroup) [21].
GROUP MUSIC INTERVENTION:
In the intervention group, patients received the 60-minute group music intervention delivered by a trained music facilitator in the morning once a week for 12 weeks in the activity room in the veterans’ homes. The intervention contained a 10-minute warm-up session of fingers and upper-extremities exercises and breathing exercises. Then, the participants used percussion instruments to practice simple rhythmic patterns, engaged in a 40-minute group music session with familiar music, and finally engaged in a 10-minute review session in which they returned to earlier rhythmic patterns used during the same day’s session. A collection of preferred and familiar songs from participants, which were assessed prior to the intervention by asking them, their caregivers, family members, or institutional staff, was used with the music session. The music collections contained pleasant rhythm and moderate tempo from 1930–1970s’ Chinese and Taiwanese popular songs. Participants were asked to follow the instruction to play various kinds of percussion instruments (such as wrist bell, tambourine, maracas, triangle, double-tone woodblock, hand drum, castanet) by moving their upper extremities with their familiar songs.
OUTCOME MEASUREMENTS:
HAMA is a 14-item scale designed to assess anxiety severity, measured on a 5-point Likert scale ranging from 0 (not present) to 4 (severe), with the total score ranging from 0 to 56 [20]. The survey of GDS score consisted of 15 questions with a set of yes or no answers. The total possible score ranges from 0 to 15; each ‘yes’ response received 1 positive point. The GDS score has been used to represent the degree of depression severity [19]. The PMMA contains 40 pairs of audio clips, whereas participants were asked to compare the difference of tonal sequence or rhythmic pattern within each pair of clips [21].
DATA ANALYSIS:
Data are presented with means±standard deviations for continuous variables or with numbers and percentages for categorical variables. Normality of distribution was confirmed through Kolmogorov-Smirnov testing. The unpaired
Repeated-measures analysis of variance (repeated-measure ANOVA) was performed to compare the differences in HAMA and GDS scores between the intervention and control groups over time. There were 3 time-points (baseline, week 6, and week 12) throughout the trial. Time-dependent effects of the music intervention on HAMA or GDS between intervention and control groups were assessed by fitting a “time x group” interaction term. If the “time x group” interaction effect on GDS or HAMA was statistically significant, a post hoc
Results
Fifty elderly male veterans with AD were randomly divided into 2 groups: a music intervention group (n=25) or a control group (n=25). In each group, dementia was mild in 9 patients (CDR=1) and moderate in 16 patients (CDR=2). The average age was 86.6±4.5 years for the intervention group and 86.9±5.7 years for the control group. The 2 groups were homogeneous in terms of age, education, frequency distribution of dementia severity, and baseline clinical symptoms (Table 1).
Regarding the change in clinical symptoms between groups before and after the intervention, time (
Within the intervention group, time (
Discussion
LIMITATIONS:
Study limitations must be considered when interpreting these results. The small sample size of participants with AD and restrictions in the population sample (only male veterans in Taiwan) are the main limitations of the study. Subsequent studies should include a larger sample size with other populations; for example, nonveterans, females, and non-Han populations. Secondly, not all participants received brain imaging before enrollment; therefore, the possibility of “vascular dementia” was excluded only through clinical history and physical examination. Future research should use magnetic resonance imaging examinations to exclude cancer, vascular dementia, or other neurological illness. Thirdly, we enrolled patients with mild- or moderate-stage AD, and the PMMA musical aptitude test might be too lengthy for patients with late-stage AD to complete. Therefore, the current result may not be applied to patients with severe AD. Fourthly, except for musical aptitude, we did not explore other music elements that could affect response to music intervention, such as musical perception, musical preferences, and attention to or enjoyment of music [26]. Fifthly, the HAMA is not a criterion standard to examine anxiety in dementia, and valid tools are needed to assess the level of anxiety in persons with dementia. Finally, we did not assess other neuropsychiatric symptoms such as behavioral disturbances, delusions, or hallucinations. The impact of music interventions on these symptoms must be evaluated in future studies.
Conclusions
The results from this study suggest that the music intervention was effective in treating anxiety in elderly male veterans with AD. Moreover, patients’ musical aptitude may be related to their therapeutic response. The musical aptitude of patients with dementia must be considered and assessed before providing a group music intervention. Music interventions are a low-cost approach that staff at veterans’ homes can introduce in their everyday activities to reduce neuropsychiatric symptoms and alleviate caregivers’ stress and burden of care. Further studies are needed to verify our conclusions.
Figures
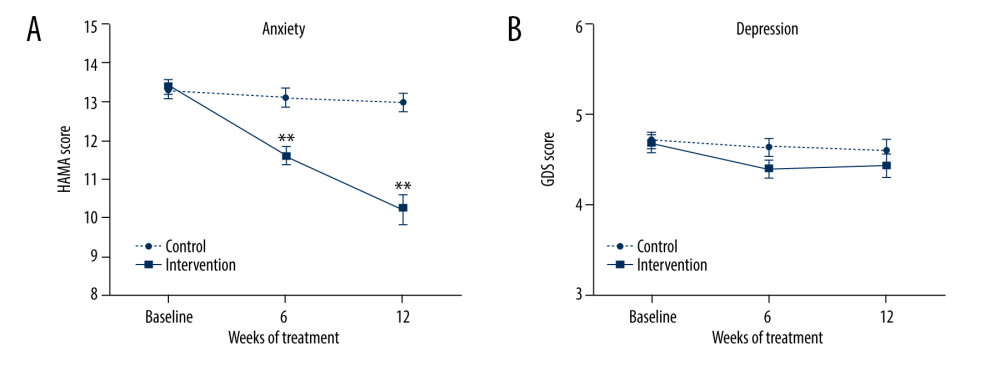 Figure 1. Effects of group music intervention. (A) Hamilton Anxiety Rating Scale (HAMA) score. (B) Geriatric Depression Scale (GDS) score. Intervention group: solid line (n=25); control group: dashed line (n=25). Values are expressed as mean±standard error of the mean. Repeated-measures ANOVA and post hoc analyses with independent t tests: ** P<0.001 to compare the intervention group with control group.
Figure 1. Effects of group music intervention. (A) Hamilton Anxiety Rating Scale (HAMA) score. (B) Geriatric Depression Scale (GDS) score. Intervention group: solid line (n=25); control group: dashed line (n=25). Values are expressed as mean±standard error of the mean. Repeated-measures ANOVA and post hoc analyses with independent t tests: ** P<0.001 to compare the intervention group with control group. 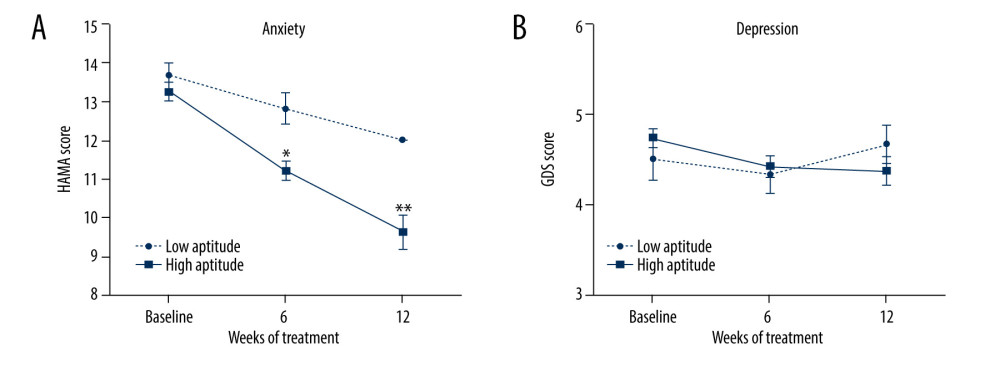 Figure 2. Effect of musical aptitude on the response to music intervention. (A) Hamilton Anxiety Rating Scale (HAMA) score. (B) Geriatric Depression Scale (GDS) score. High musical aptitude subgroup: solid line (n=19); low musical aptitude subgroup: dashed line (n=6). Values are expressed as mean±standard error of the mean. Repeated-measures ANOVA and post hoc analyses with independent t tests: * P<0.01, ** P<0.001 to compare high- and low-aptitude subgroups.
Figure 2. Effect of musical aptitude on the response to music intervention. (A) Hamilton Anxiety Rating Scale (HAMA) score. (B) Geriatric Depression Scale (GDS) score. High musical aptitude subgroup: solid line (n=19); low musical aptitude subgroup: dashed line (n=6). Values are expressed as mean±standard error of the mean. Repeated-measures ANOVA and post hoc analyses with independent t tests: * P<0.01, ** P<0.001 to compare high- and low-aptitude subgroups. References
1. Qiu C, Kivipelto M, von Strauss E, Epidemiology of Alzheimer’s disease: Occurrence, determinants, and strategies toward intervention: Dialogues Clin Neurosci, 2009; 11(2); 111
2. Ferri C, Prince M, Brayne C, Alzheimers Disease International: Global prevalence of dementia: A Delphi consensus study: Lancet, 2005; 366(9503); 2112-17
3. Lyketsos CG, Carrillo MC, Ryan JM, Neuropsychiatric symptoms in Alzheimer’s disease: Alzheimers Dement, 2011; 7(5); 532-39
4. Phan SV, Osae S, Morgan JC, Neuropsychiatric symptoms in dementia: Considerations for pharmacotherapy in the USA: Drugs RD, 2019; 19(2); 93-115
5. Feast AR, White N, Candy B, The effectiveness of interventions to improve the care and management of people with dementia in general hospitals: A systematic review: Int J Geriatr Psychiatry, 2020; 35(5); 463-88
6. Kishita N, Backhouse T, Mioshi E, Nonpharmacological interventions to improve depression, anxiety, and quality of life (QoL) in people with dementia: An overview of systematic reviews: J Geriatr Psychiatry Neurol, 2020; 33(1); 28-41
7. Van der Steen JT, Smaling HJ, Van der Wouden JC, Music-based therapeutic interventions for people with dementia: Cochrane Database Syst Rev, 2018; 7(7); CD003477
8. Pereira APS, Marinho V, Gupta D, Music therapy and dance as gait rehabilitation in patients with parkinson disease: A review of evidence: J Geriatr Psychiatry Neurol, 2019; 32(1); 49-56
9. Irish M, Cunningham CJ, Walsh JB, Investigating the enhancing effect of music on autobiographical memory in mild Alzheimer’s disease: Dement Geriatr Cogn Disord, 2006; 22(1); 108-20
10. Bell J, Music therapy and percussion for persons with dementia: A systematic literature review: Concordia University, 2016
11. Sung Hc, Lee Wl, Li Tl, A group music intervention using percussion instruments with familiar music to reduce anxiety and agitation of institutionalized older adults with dementia: Int J Geriatr Psychiatry, 2012; 27(6); 621-27
12. Hoffer C: Introduction to music education, 2017, Waveland Press
13. Steele J, The relationship between music aptitude, empathy, and sensitivity to emotional prosody: An ERP Investigation, 2020
14. Lin SW, From soldier to veteran: institution-building of state and the formation of demographic categories in Taiwan (1949–1970): Taiwan: A Radical Quarterly in Social Studies, 2003; 52; 187-254
15. Chang HT, Liu LF, Chen CK, Correlates of institutionalized senior veterans’ quality of life in Taiwan: Health Qual Life Outcomes, 2010; 8(1); 70
16. Byers AL, Yaffe K, Depression and dementias among military veterans: Alzheimers Dement, 2014; 10(3 Suppl); S166-73
17. McKhann G, Drachman D, Folstein M, Clinical diagnosis of Alzheimer’s disease: Report of the NINCDS-ADRDA Work Group* under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease: Neurology, 1984; 34(7); 939-39
18. Matza LS, Morlock R, Sexton C, Identifying HAM-A cutoffs for mild, moderate, and severe generalized anxiety disorder: Int J Methods Psychiatr Res, 2010; 19(4); 223-32
19. Mui AC, Geriatric Depression Scale as a community screening instrument for elderly Chinese immigrants: Int Psychogeriatr, 1996; 8(3); 445-58
20. Hamilton M, The assessment of anxiety states by rating: Br J Med Psychol, 1959; 32(1); 50-55
21. Gordon E, Primary measures of music audiation. Chicago: GIA Pub: In: Inc, 1979
22. Raglio A, Bellelli G, Traficante D, Efficacy of music therapy in the treatment of behavioral and psychiatric symptoms of dementia: Alzheimer Dis Assoc Disord, 2008; 22(2); 158-62
23. Hall GR, Progressively lowered stress threshold; A conceptual model for care of adults with Alzheimer’s disease: Arch Psychiatr Nurs, 1987; 1(6); 399-406
24. Suzuki M, Kanamori M, Watanabe M, Behavioral and endocrinological evaluation of music therapy for elderly patients with dementia: Nurs Health Sci, 2004; 6(1); 11-18
25. Mead N, Lester H, Chew-Graham C, Effects of befriending on depressive symptoms and distress: Systematic review and meta-analysis: Br J Psychiatry, 2010; 196(2); 96-101
26. Wilson BL, Smith DS, Music therapy assessment in school settings: A preliminary investigation: J Music Ther, 2000; 37(2); 95-117
Figures
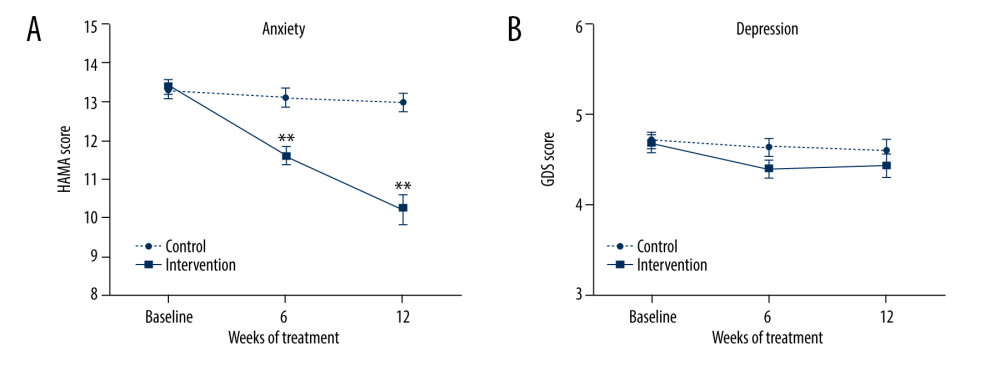 Figure 1. Effects of group music intervention. (A) Hamilton Anxiety Rating Scale (HAMA) score. (B) Geriatric Depression Scale (GDS) score. Intervention group: solid line (n=25); control group: dashed line (n=25). Values are expressed as mean±standard error of the mean. Repeated-measures ANOVA and post hoc analyses with independent t tests: ** P<0.001 to compare the intervention group with control group.
Figure 1. Effects of group music intervention. (A) Hamilton Anxiety Rating Scale (HAMA) score. (B) Geriatric Depression Scale (GDS) score. Intervention group: solid line (n=25); control group: dashed line (n=25). Values are expressed as mean±standard error of the mean. Repeated-measures ANOVA and post hoc analyses with independent t tests: ** P<0.001 to compare the intervention group with control group.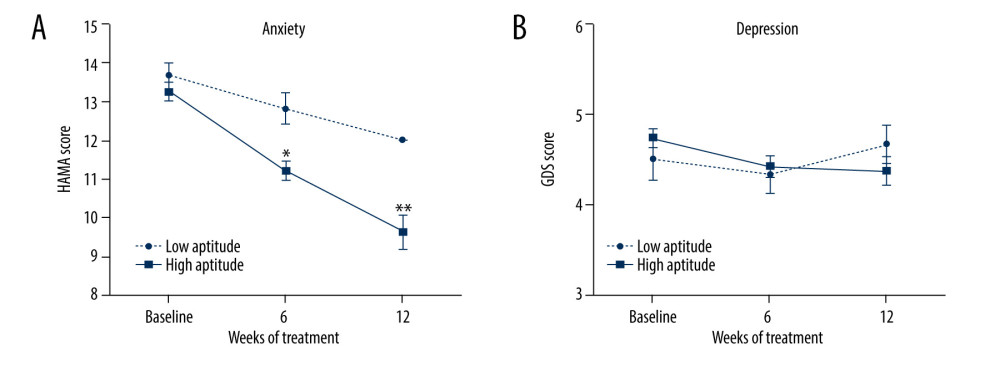 Figure 2. Effect of musical aptitude on the response to music intervention. (A) Hamilton Anxiety Rating Scale (HAMA) score. (B) Geriatric Depression Scale (GDS) score. High musical aptitude subgroup: solid line (n=19); low musical aptitude subgroup: dashed line (n=6). Values are expressed as mean±standard error of the mean. Repeated-measures ANOVA and post hoc analyses with independent t tests: * P<0.01, ** P<0.001 to compare high- and low-aptitude subgroups.
Figure 2. Effect of musical aptitude on the response to music intervention. (A) Hamilton Anxiety Rating Scale (HAMA) score. (B) Geriatric Depression Scale (GDS) score. High musical aptitude subgroup: solid line (n=19); low musical aptitude subgroup: dashed line (n=6). Values are expressed as mean±standard error of the mean. Repeated-measures ANOVA and post hoc analyses with independent t tests: * P<0.01, ** P<0.001 to compare high- and low-aptitude subgroups. Tables
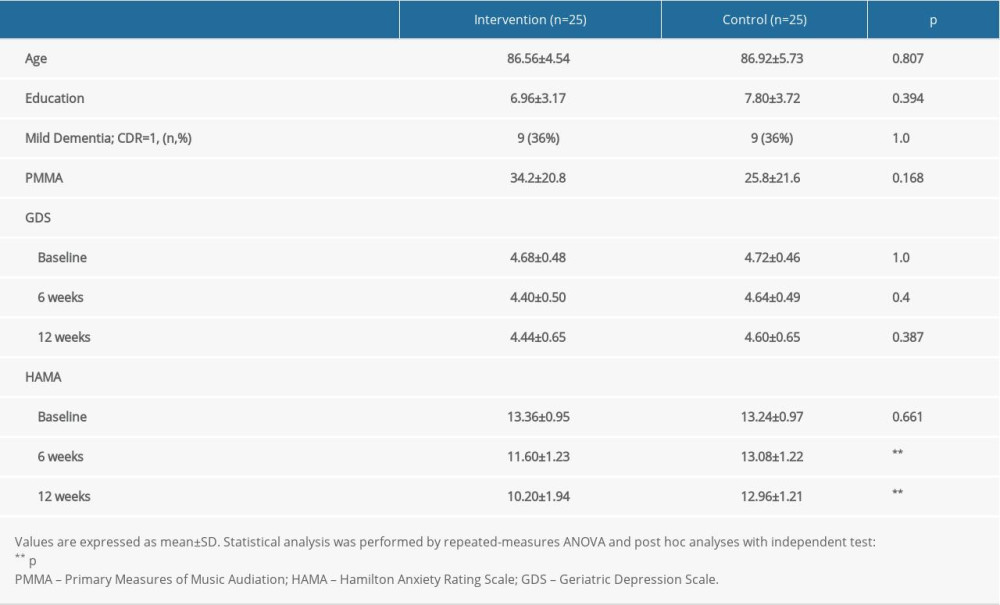 Table 1. Demographic characteristics and measurements of depression and anxiety of patients with Alzheimer disease in the intervention and control groups.
Table 1. Demographic characteristics and measurements of depression and anxiety of patients with Alzheimer disease in the intervention and control groups.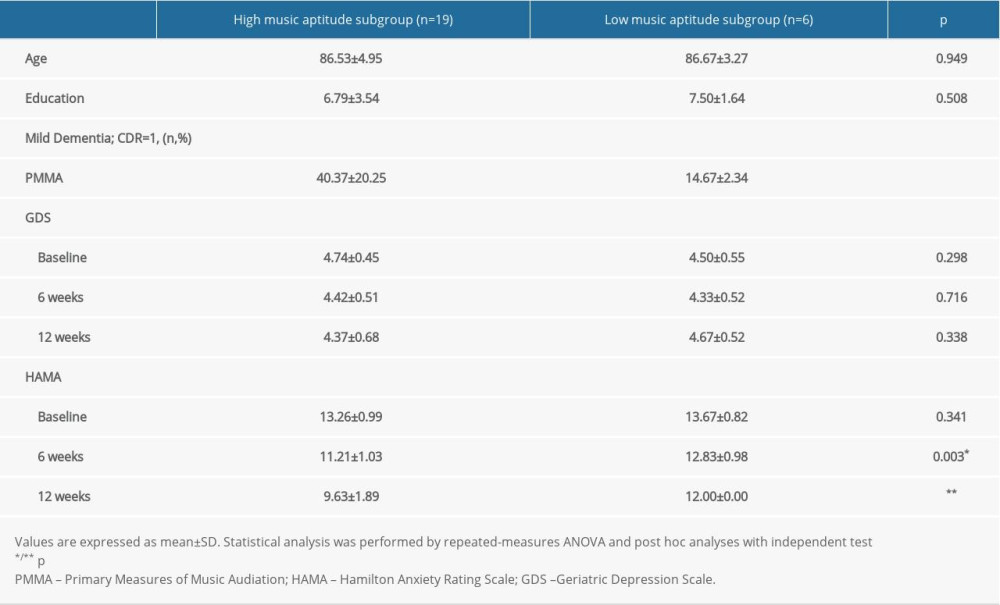 Table 2. Demographic characteristics and measurements of depression and anxiety in the high and low musical aptitude subgroups.
Table 2. Demographic characteristics and measurements of depression and anxiety in the high and low musical aptitude subgroups.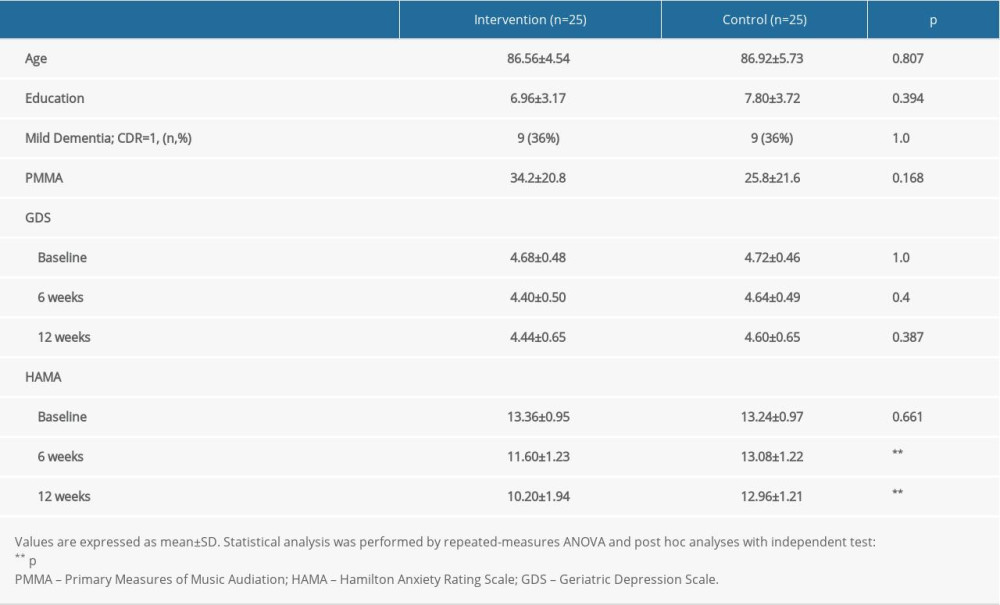 Table 1. Demographic characteristics and measurements of depression and anxiety of patients with Alzheimer disease in the intervention and control groups.
Table 1. Demographic characteristics and measurements of depression and anxiety of patients with Alzheimer disease in the intervention and control groups.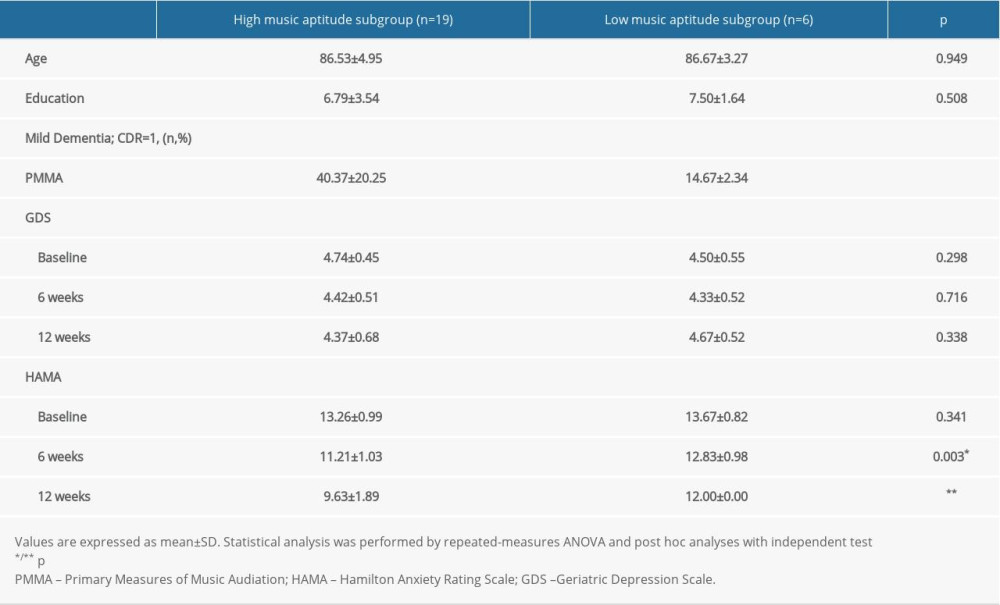 Table 2. Demographic characteristics and measurements of depression and anxiety in the high and low musical aptitude subgroups.
Table 2. Demographic characteristics and measurements of depression and anxiety in the high and low musical aptitude subgroups. In Press
05 Mar 2024 : Clinical Research
Role of Critical Shoulder Angle in Degenerative Type Rotator Cuff Tears: A Turkish Cohort StudyMed Sci Monit In Press; DOI: 10.12659/MSM.943703
06 Mar 2024 : Clinical Research
Comparison of Outcomes between Single-Level and Double-Level Corpectomy in Thoracolumbar Reconstruction: A ...Med Sci Monit In Press; DOI: 10.12659/MSM.943797
21 Mar 2024 : Meta-Analysis
Economic Evaluation of COVID-19 Screening Tests and Surveillance Strategies in Low-Income, Middle-Income, a...Med Sci Monit In Press; DOI: 10.12659/MSM.943863
10 Apr 2024 : Clinical Research
Predicting Acute Cardiovascular Complications in COVID-19: Insights from a Specialized Cardiac Referral Dep...Med Sci Monit In Press; DOI: 10.12659/MSM.942612
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








