01 August 2021: Clinical Research
Factors Associated with Emergency Department Length of Stay in Critically Ill Patients: A Single-Center Retrospective Study
Zhiwei Yang1AE, Kun Song1B, Hang Lin1F, Changluo Li1D, Ning Ding1CD*DOI: 10.12659/MSM.931286
Med Sci Monit 2021; 27:e931286
Abstract
BACKGROUND: Length of stay (LOS) in the emergency department (ED) should be measured and evaluated comprehensively as an important indicator of hospital emergency service. In this study, we aimed to analyze clinical characteristics of critically ill patients admitted to the ED and identify the factors associated with LOS.
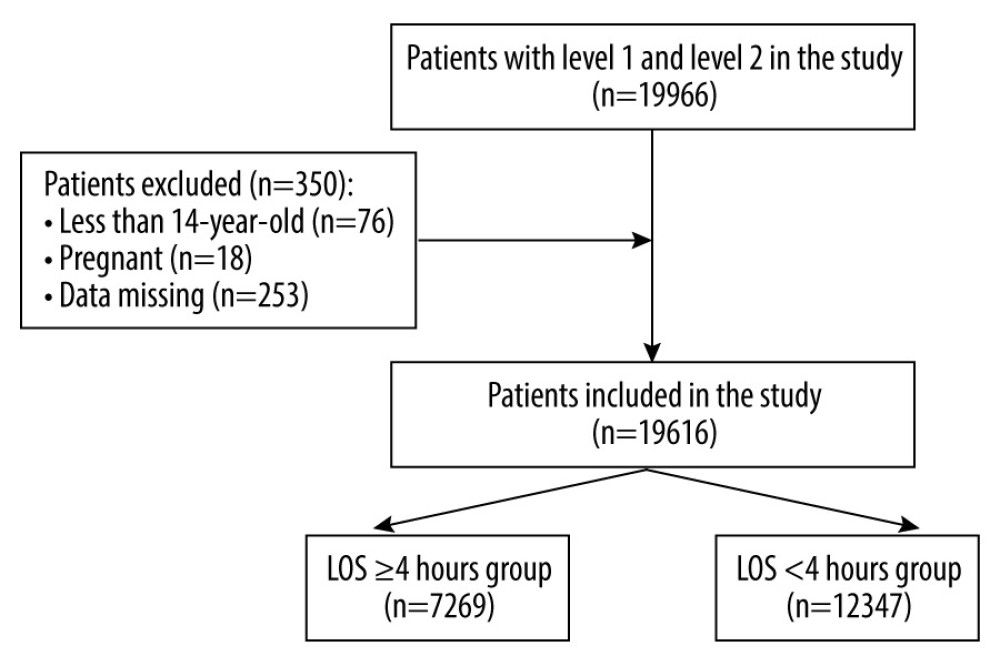
MATERIAL AND METHODS: All patients with level 1 and level 2 of the Emergency Severity Index who were admitted to the ED from January 2018 to December 2019 were included in this retrospective study. The patients were divided into 2 groups: LOS ≥4 h and LOS <4 h. Variables were comprehensively analyzed and compared between the 2 groups.
RESULTS: A total of 19 616 patients, including 7269 patients in the LOS ≥4 h group and 12 347 patients in the LOS <4 group, were included. Advanced age, admission in winter and during the night shift, and diseases excluding nervous system diseases, cardiovascular diseases, and trauma were associated with higher risk of LOS. Nervous system diseases, cardiovascular diseases, trauma, and procedures including tracheal intubation, surgery, percutaneous coronary intervention, and thrombolysis were associated with lower risk of LOS.
CONCLUSIONS: Prolonged LOS in the ED was associated with increased age and admission in winter and during the night shift, while shortened LOS was associated with nervous system diseases, cardiovascular diseases, and trauma, as well as with procedures including tracheal intubation, surgery, percutaneous coronary intervention, and thrombolysis. Our findings can serve as a guide for ED physicians to individually evaluate patient condition and allocate medical resources more effectively.
Keywords: Critical Illness, Emergency Medical Services, Length of Stay, Age Factors, Emergencies, Emergency Service, Hospital, Health Care Rationing, Needs Assessment, Patient Selection, Seasons, Shift Work Schedule
Background
Overcrowding in the hospital Emergency Department (ED), which can decrease the efficiency of ED staff and lead to patient management delays and poor clinical outcomes, is considered a public health problem worldwide [1,2]. The imbalance of a rapid increase in the number of patients, especially critically ill patients, and insufficient medical resources exacerbates the problem [3]. A multicenter retrospective research study including 995 379 ED patients concluded that ED crowding is associated with increased in-hospital mortality and prolonged length of stay (LOS) [4]. Conversely, prolonged LOS in the ED was detrimental to quality of treatment, especially in time-sensitive disorders, including trauma [5], heart failure [6], and acute coronary syndrome [7]. Previous studies revealed that factors linked with LOS in the ED include patient-specific factors such as age, triage level, and severity of disorder and hospital-specific factors such as hospital size and specialist consultation [8,9]. A maximum length of ED stay of 4 h was confirmed to be associated with improved quality of medical care in the ED as well as with patient satisfaction [10]. Another retrospective study clarified that an LOS in the ED longer than 4 h could make the ED crowded. As ED volume increased, some ED patients did not receive treatment in a proper and timely manner [11].
Therefore, LOS in the ED is an important indicator of hospital emergency service, which should be comprehensively measured and evaluated so that medical management and resources can be implemented and allocated more effectively. It is critical for physicians to identify the essential factors needed to assess, at an early stage, the likelihood of a longer LOS after admission. In our study, we aimed to analyze clinical characteristics of patients with critical illness admitted to the ED and identify the factors associated with LOS.
Material and Methods
STUDY DESIGN AND PATIENTS:
Initially, all patients admitted to the ED from January 2018 to December 2019 were included in this retrospective study. Only patients with a critical illness of level 1 and level 2 according to the Emergency Severity Index (ESI), which has a 5-level triage system [12], were enrolled in the study. Exclusion criteria were the following: age <14 years, pregnancy, and patients with data missing. The included patients were divided into 2 groups: LOS ≥4 h and LOS <4 h. Variables were comprehensively analyzed and compared between the 2 groups.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE:
The study was approved by the Ethics Committee of Changsha Central Hospital of University of South China (Changsha, China). All research was performed in accordance with the relevant guidelines and regulations. Owing to the retrospective nature of the study, informed consent was waived, which was also approved by the Ethics Committee of Changsha Central Hospital of University of South China.
DATA COLLECTION:
The collected data included the baseline and clinical characteristics of the patients admitted to the ED. Patient characteristics included the following: sex, age, time of presenting (including month and day) to the ED, diagnosis after admission, treatments including tracheal intubation, mechanical ventilation, cardiopulmonary resuscitation (CPR), surgery, interventional therapy, and thrombolysis, clinical outcomes including hospitalization, observation in ED, discharge home, and transfers, and in-hospital mortality.
DEFINITIONS:
Based on the climatic characteristics of southern in China, 4 seasons were classified as follows: winter (December to February), spring (March to May.), summer (June to August), and autumn (September to November). Based on the schedule of the ED, 24 h were divided into 3 different shifts as follows: day shift (8: 00 AM to 4: 00 PM), afternoon shift (4: 00 PM to midnight), and night shift (midnight to 8: 00 AM).
STATISTICAL ANALYSIS:
Statistical results were expressed in mean±standard deviation for normally distributed data, while for non-normally distributed data, interquartile range (IQR) and median were employed. Categorical data were expressed as a percentage and number. The
Significant factors associated with LOS ≥4 h (
Results
GENERAL CHARACTERISTICS OF PATIENTS:
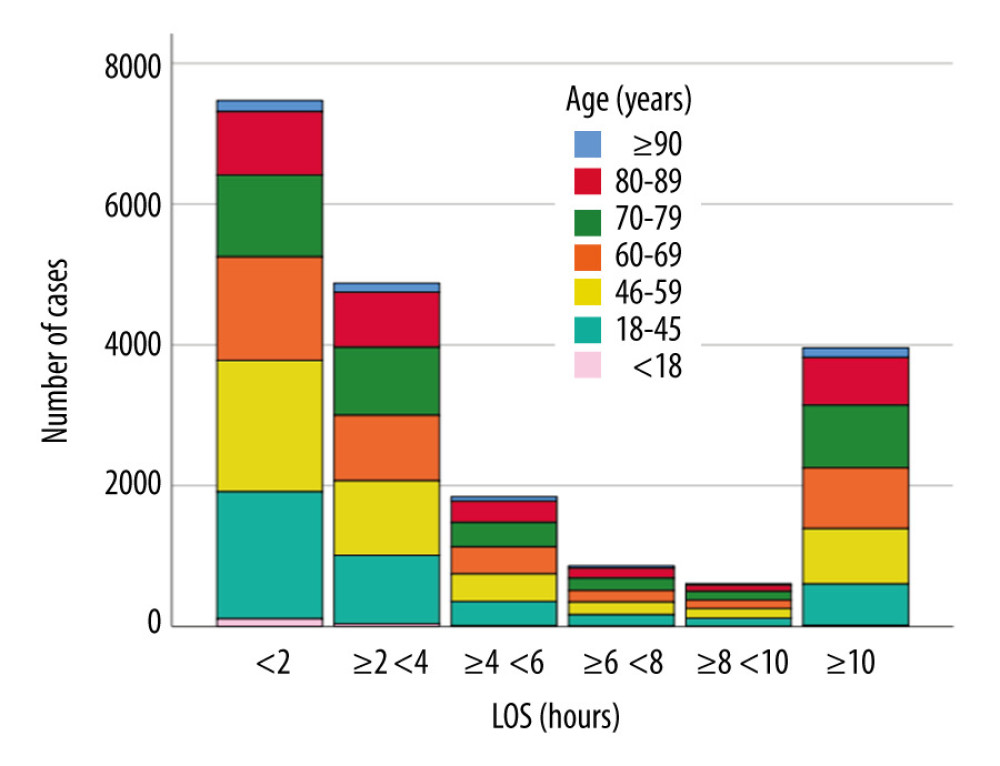
At first, a total of 19 966 patients admitted to the ED were enrolled in this study. Based on the exclusion criteria, 350 patients were excluded and 19 616 patients with critical illness were finally included (Figure 1). The distribution of subgroups based on LOS is shown in Figure 2. The LOS proportions were <2 h (38.1%), 2 to 4 h (24.9%), 4 to 6 h (9.4%), 6 to 8 h (4.4%), 8 to 10 h (3.1%), and ≥10 h (20.1%). The mean patient age was 60.5 years and the in-hospital mortality was 1.9%. Male patients and elderly patients (≥60 years) accounted for 62.9% and 56.2% of patients, respectively. The proportion of ESI level 1 and level 2 were 11.7% and 88.3%, respectively. The mean time of LOS was 2.7 h. The top 5 disease categories ranked as follows: nervous system (25.6%), respiratory system (21.0%), cardiovascular system (14.3%), digestive system (11.6%), and trauma (9%). The incidence of tracheal intubation, mechanical ventilation, and CPR were 5.2%, 5%, and 2.4%, respectively. Surgery, PCI, and thrombolysis were performed in 377 (1.9%), 615 (3.1%), and 273 (1.4%) patients, respectively. More than 60% of patients were hospitalized (Table 1).
COMPARISON OF VARIABLES BETWEEN LOS ≥4 H AND LOS <4 H GROUPS:
The clinical characteristics of the 7269 patients in the LOS ≥4 h group and the 12 347 patients in the LOS <4 h group are shown in Table 2. There were significant differences in sex between the 2 groups (P=0.038). Patients in the LOS ≥4 h group were older (P<0.001). Comparing 6 subgroups of age, the LOS ≥4 h group had more patients in the 4 subgroups ≥60 years. The number of patients in the LOS ≥4 h group admitted in winter (December to February) and spring (March to May) was significantly higher than patients in the LOS <4 h group admitted during those seasons. Moreover, significant differences were found between the 2 groups in admissions by all seasons (all P<0.001). The proportion of patients in the LOS ≥4 h group admitted to the ED during the night shift (midnight to 8: 00 AM) was significantly higher than those in the LOS <4 h group (20.8% vs 15.1%, P<0.001), while the LOS ≥4 h group admissions were lower at the other times (day and afternoon shifts). Comparing the top 5 disease categories at presentation between the 2 groups, patients with respiratory diseases (32.1%) and digestive diseases (13.8%) were more likely to have longer stays in the ED, while those with nervous system diseases (31.7%), cardiovascular diseases (16.4%), and trauma (11.7%) had shorter stays in the ED (all P<0.001). The proportion of patients with tracheal intubation (3.0%), mechanical ventilation (3.4%), CPR (1.1%), surgery (0.2%), interventional therapy (1.8%), and thrombolysis (0.2%) was significantly lower in the LOS ≥4 h group than in the LOS <4 h group (all P<0.001). More patients were hospitalized (75.4%) or discharged home (16.6%) in the LOS ≥4 h group than in the LOS <4 h group (both P<0.001). The in-hospital mortality rates of the LOS ≥4 h and LOS <4 h groups were 1.1% and 2.5%, respectively (P<0.001).
UNIVARIATE AND MULTIVARIATE ANALYSES FOR FACTORS ASSOCIATED WITH LOS:
Factors associated with LOS were determined by univariate and multivariate logistic regression analyses, as shown in Table 3. Age >60 years, admission in winter and during the night shift, and diseases excluding nervous system diseases, cardiovascular diseases, and trauma were associated with the higher risk of LOS. Nervous system diseases, cardiovascular diseases, trauma, and procedures including tracheal intubation, surgery, PCI, and thrombolysis were associated with the lower risk of LOS. In age subgroups, the OR increased with increasing age, and the OR in the group over 90 years old was the highest (OR 2.320, 95% CI 1.426–3.776). For time of admission, patients admitted in the winter (December to February) and during the night shift (midnight to 8: 00 AM) were more likely to stay longer in the ED (OR 1.602, 95% CI 1.459–1.759 and OR 1.642, 95% CI 1.493–1.806, respectively). Three categories of diseases were negatively associated with LOS, including cardiovascular diseases (OR 0.188, 95% CI 0.104–0.341), nervous system diseases (OR 0.612, 95% CI 0.544–0.689), and trauma (OR 0.541, 95% CI 0.456–0.640). Patients with tracheal intubation (OR 0.564, 95% CI 0.329–0.967), surgery (OR 0.097, 95% CI 0.054–0.174), PCI (OR 0.046, 95% CI 0.028–0.077), and thrombolysis (OR 0.170, 95% CI 0.103–0.281) had a significantly lower risk of longer LOS.
Discussion
In this retrospective cohort study of critically ill patients admitted to the ED in 2018 and 2019, patient clinical characteristics were analyzed and factors associated with LOS were identified. Prolonged LOS was associated with increased age and admission in winter and during the night shift, whereas shortened LOS was associated with nervous system diseases, cardiovascular diseases, and trauma as well as with procedures including tracheal intubation, surgery, PCI, and thrombolysis.
Our study showed that with increasing age, the risk of prolonged LOS increased, and the group of patients aged 90 years or older had the highest risk. A study with 5025 elderly patients in the ED indicated that prolonged LOS is best predicted by several indicators, which include being aged 90 years or older [13]. Another study revealed that of 16 791 ED presentations made by older patients, 4192 experienced a longer LOS, and increased age was associated with an increasing LOS in the ED [14]. Elderly patients are likely to stay in the ED longer because of poor communication with physicians, multiple chronic disorders, an atypical presentation with delayed symptoms, and unstable vital signs. Compared with younger patients, older patients admitted in the ED have multiple and complex presenting symptoms and conditions, which lead to more diagnostic tests and procedures as well as consultation services [15].
In the present study, patients admitted in winter and during the night shift had a higher risk of staying longer in the ED. One study investigated the relationship between the relative risk of ED visitation and seasonal temperature and concluded that in cold weather, the total number of patients in the hospital declined by 15%, but ED visits increased by 4% [16]. A study of 17 298 ED visits for respiratory infection indicated that significantly fewer visits were recorded in warm months than in cold months (OR 0.23; 95% CI 0.29–0.18;
In the present study, among the most common categories of disorders presenting in the ED, nervous system diseases, cardiovascular diseases, and trauma were negatively associated with LOS. Moreover, tracheal intubation, surgery, PCI, and thrombolysis showed the same relationship with LOS. Our hospital is a tertiary hospital as well as a stroke, chest pain, and trauma center. For several years, effective and convenient emergency medicine processes have been constructed for time-sensitive disorders including stroke, acute coronary syndrome, acute heart failure, and trauma. For those patients, multidiscipline consultation and management are implemented quickly as are hospitalizations and transfers, which could explain why patients with mechanical intubation, surgery, PCI, and thrombolysis had a comparatively lower risk of prolonged LOS. In a study on stroke, evidence showed that endovascular stroke therapy and thrombolysis were inversely associated with the LOS in the ED [25]. In a mature trauma center with standardized activation protocols, trauma activation and subsequent management and procedures, including surgery, could mitigate the negative effects of prolonged LOS in the ED [26].
Overall, factors associated with LOS in the ED in a large sample of critically ill patients were analyzed. Our findings can serve as a guide for ED physicians to individually evaluate patients’ condition and allocate medical resources more effectively. There were several limitations in our study. First, it was a single-center retrospective study, so caution should be exercised when applying the results to other centers with different situations and policies. Second, only categories of diseases were included and analyzed in this study, with subgroups of diseases not divided and compared, which to a certain extent might have affected our results. Third, because of some missing data, not all factors associated with LOS in the ED of patients were mentioned in this study, including marital status, medical insurance, socioeconomical status, and educational background. Further research with more clinical variables should be considered.
Conclusions
Prolonged LOS in the ED was associated with increased age and admission in winter and during the night shift, while shortened LOS was linked with nervous system diseases, cardiovascular diseases, and trauma as well as with procedures including tracheal intubation, surgery, PCI, and thrombolysis. Our findings can serve as a guide for ED physicians to individually evaluate patients’ conditions and allocate medical resources more effectively.
References
1. Prather J, Alexander B, Halstrom J, Factors affecting Emergency Department visits, readmissions, and reoperations within 30 days of ankle fracture surgery – an institutional retrospective study: Injury, 2020; 51(11); 2698-702
2. Oh HC, Chow WL, Gao Y, Factors associated with inappropriate attendances at the emergency department of a tertiary hospital in Singapore: Singapore Med J, 2020; 61(2); 75-80
3. Tangkulpanich P, Yuksen C, Kongchok W, Jenpanitpong C, Clinical predictors of emergency department revisits within 48 hours of discharge: A case control study: Arch Acad Emerg Med, 2021; 9(1); e1
4. Sun BC, Hsia RY, Weiss RE, Effect of emergency department crowding on outcomes of admitted patients: Ann Emerg Med, 2013; 61(6); 605-11.e6
5. Hymel G, Leskovan JJ, Thomas Z, Emergency department boarding of non-trauma patients adversely affects trauma patient length of stay: Cureus, 2020; 12(9); e10354
6. Sricharoen P, Phinyo P, Patumanond J, Clinical predictors influencing the length of stay in emergency department patients presenting with acute heart failure: Medicina (Kaunas), 2020; 56(9); 434
7. Chen H-C, Lee W-C, Chen Y-L, The impacts of prolonged emergency department length of stay on clinical outcomes of patients with ST-segment elevation myocardial infarction after reperfusion: Intern Emerg Med, 2015; 11(1); 107-14
8. Strada A, Bolognesi N, Manzoli L, Diagnostic anticipation to reduce emergency department length of stay: A retrospective cohort study in Ferrara University hospital, Italy: BMC Health Serv Res, 2020; 20(1); 624
9. Chen CH, Hsieh JG, Cheng SL, Early short-term prediction of emergency department length of stay using natural language processing for low-acuity outpatients: Am J Emerg Med, 2020; 38(11); 2368-73
10. Dadeh AA, Phunyanantakorn P, Factors affecting length of stay in the emergency department in patients who presented with abdominal pain: Emerg Med Int, 2020; 2020; 5406516
11. Fee C, Weber EJ, Maak CA, Bacchetti P, Effect of emergency department crowding on time to antibiotics in patients admitted with community-acquired pneumonia: Ann Emerg Med, 2007; 50(5); 501-9
12. Mistry B, Stewart De Ramirez S, Kelen G, Accuracy and reliability of emergency department triage using the Emergency Severity Index: An international multicenter assessment: Ann Emerg Med, 2018; 71(5); 581-7.e3
13. Curiati PK, Gil-Junior LA, Morinaga CV, Predicting hospital admission and prolonged length of stay in older adults in the emergency department: The PRO-AGE Scoring System: Ann Emerg Med, 2020; 76(3); 255-65
14. Sweeny A, Keijzers G, O’Dwyer J, Predictors of a long length of stay in the emergency department for older people: Intern Med J, 2020; 50(5); 572-81
15. Jusmanova K, Rice C, Bourke R, Impact of a specialist service in the emergency department on admission, length of stay and readmission of patients presenting with falls, syncope and dizziness: QJM, 2020; 114(1); 32-38
16. Davis R, Markle E, Windoloski S, A comparison of the effect of weather and climate on emergency department visitation in Roanoke and Charlottesville, Virginia: Environ Res, 2020; 191; 110065
17. Ferrero F, Abrutzky R, Ossorio MF, Torres F, Effects of contamination and climate in the Pediatric Emergency Department visits for acute respiratory infection in the City of Buenos Aires: Arch Argent Pediatr, 2019; 117(6); 368-74
18. Chen X, Shang W, Huang X, The effect of winter temperature on patients with ischemic stroke: Med Sci Monit, 2019; 25; 3839-45
19. Shibuya J, Kobayashi N, Asai K, Comparison of coronary culprit lesion morphology determined by optical coherence tomography and relation to outcomes in patients diagnosed with acute coronary syndrome during winter-vs-other seasons: Am J Cardiol, 2019; 124(1); 31-38
20. Beard JD, Beck C, Graham R, Winter temperature inversions and emergency department visits for asthma in Salt Lake County, Utah, 2003–2008: Environ Health Perspect, 2012; 120(10); 1385-90
21. Christiaens H, Charpentier S, Houze-Cerfon CH, Balen F, Winter virus season impact on acute dyspnoea in the emergency department: Clin Respir J, 2019; 13(11); 722-27
22. Zhou Y, Yang G, He H, Pan X, Association between admission time and in-hospital mortality in acute aortic dissection patients: A retrospective cohort study: Heart Lung, 2020; 49(5); 651-59
23. Ahmed AA, Ibro SA, Melkamu G, Length of stay in the emergency department and its associated factors at Jimma Medical Center, southwest Ethiopia: Open Access Emerg Med, 2020; 12; 227-35
24. Sariyer G, Ataman MG, Kiziloglu I, Analyzing main and interaction effects of length of stay determinants in emergency departments: Int J Health Policy Manag, 2020; 9(5); 198-205
25. Minaeian A, Patel A, Essa B, Emergency department length of stay and outcome after ischemic stroke: J Stroke Cerebrovasc Dis, 2017; 26(10); 2167-73
26. Siletz A, Jin K, Cohen M, Emergency department length of stay in critical nonoperative trauma: J Surg Res, 2017; 214; 102-8
Figures
Tables
 Table 1. General characteristics of total patients.
Table 1. General characteristics of total patients.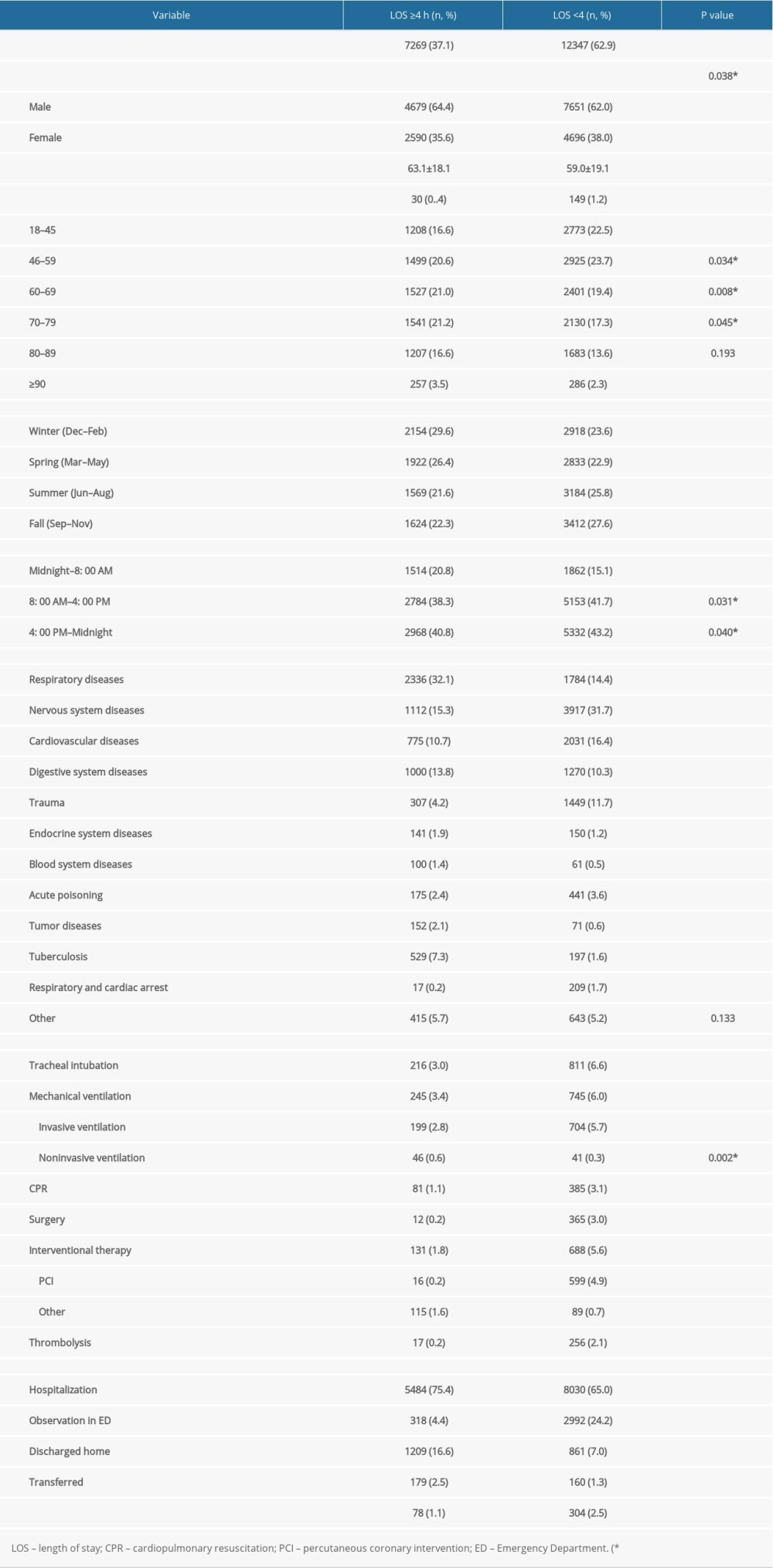 Table 2. Comparison of variables between LOS ≥4 h and LOS <4 h groups.
Table 2. Comparison of variables between LOS ≥4 h and LOS <4 h groups.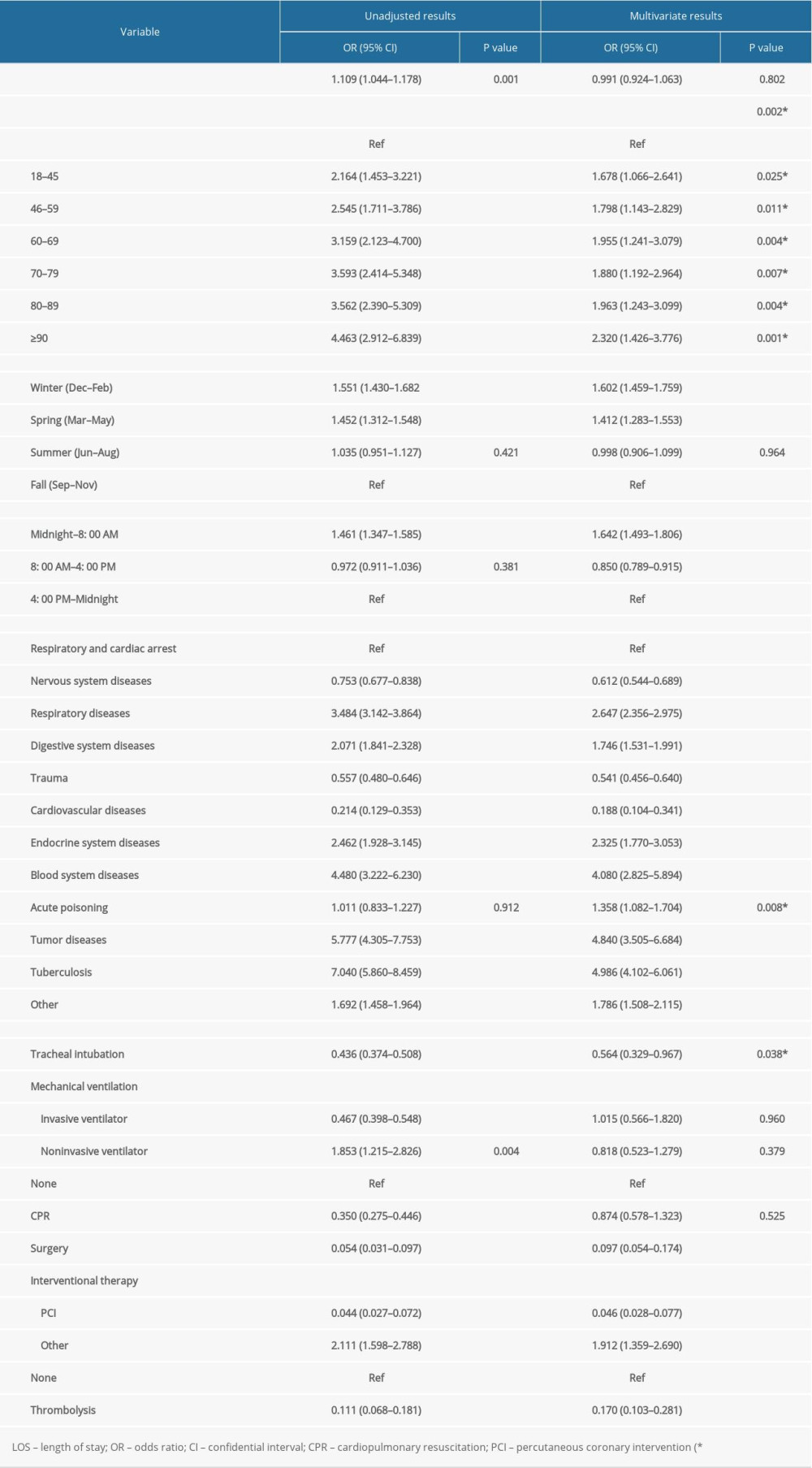 Table 3. Univariate and multivariate analyses for factors associated with LOS.
Table 3. Univariate and multivariate analyses for factors associated with LOS. Table 1. General characteristics of total patients.
Table 1. General characteristics of total patients.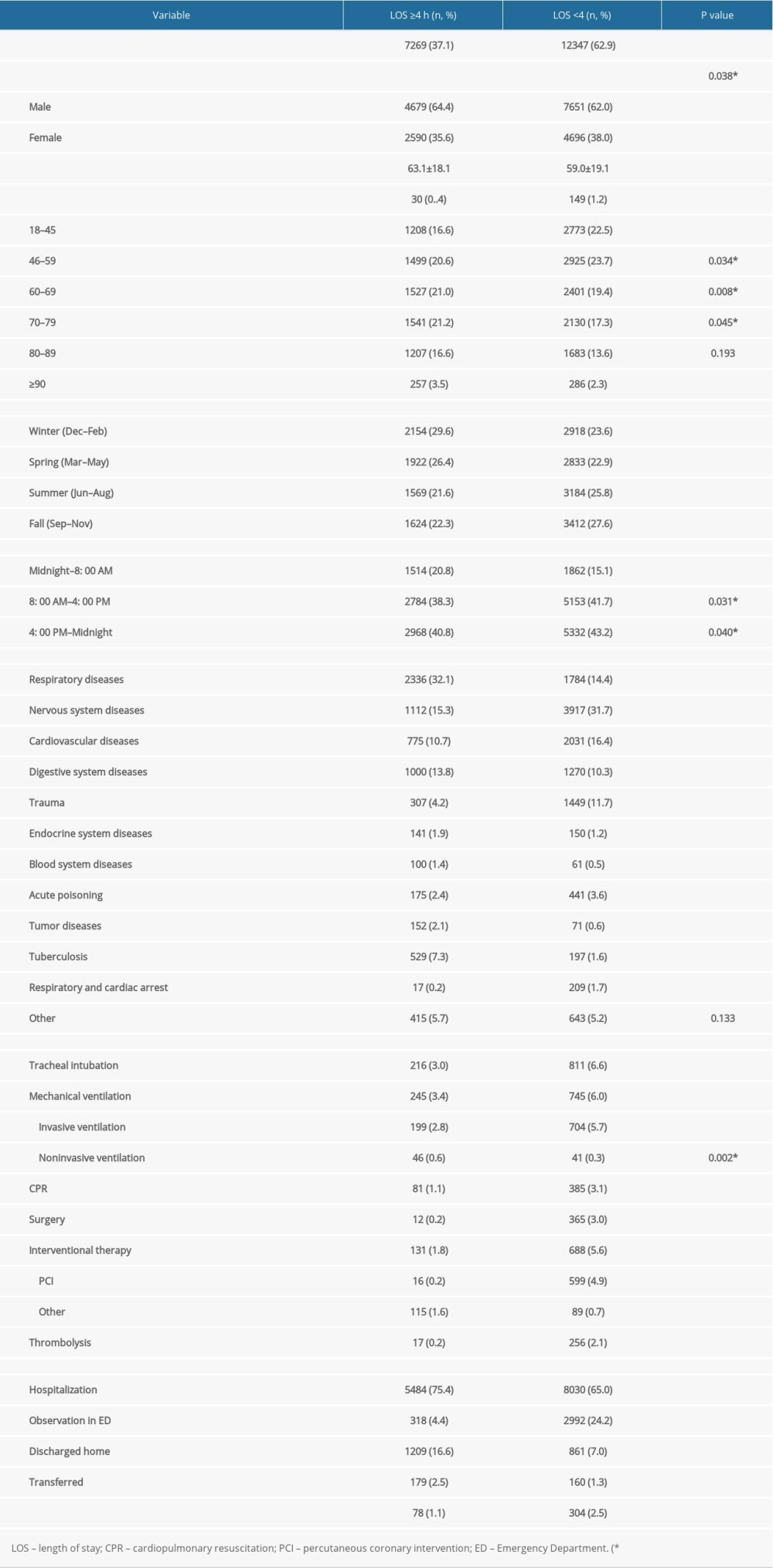 Table 2. Comparison of variables between LOS ≥4 h and LOS <4 h groups.
Table 2. Comparison of variables between LOS ≥4 h and LOS <4 h groups.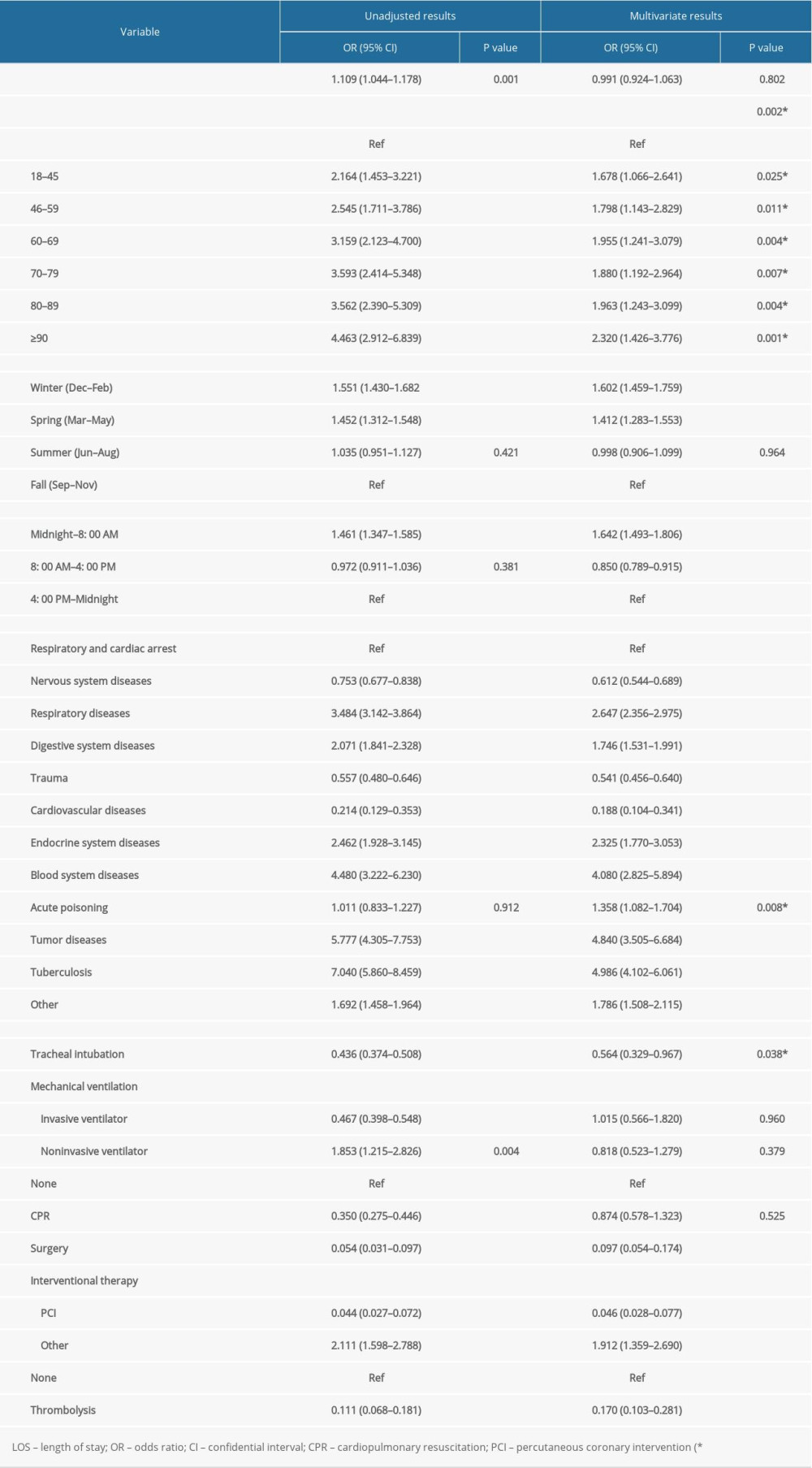 Table 3. Univariate and multivariate analyses for factors associated with LOS.
Table 3. Univariate and multivariate analyses for factors associated with LOS. In Press
07 Mar 2024 : Clinical Research
Knowledge of and Attitudes Toward Clinical Trials: A Questionnaire-Based Study of 179 Male Third- and Fourt...Med Sci Monit In Press; DOI: 10.12659/MSM.943468
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952