Abstract
BACKGROUND: The coronavirus disease 2019 (COVID-19) pandemic has impacted the health-related quality of life (HRQoL) and mental health worldwide. However, its impact on medical students in Indonesia has not been well documented. This study aimed to evaluate HRQoL and mental health in 729 Indonesian medical students during the COVID-19 pandemic.
MATERIAL AND METHODS: We conducted a cross-sectional study from 31 August to 30 September 2021. The study instrument was an online questionnaire that was distributed via social media platforms. The 12-item short form version 2 (SF12v2) was used to measure HRQoL, and the 21-item Depression, Anxiety, and Stress Scale (DASS-21) was used to measure mental health.
RESULTS: From 729 Indonesian medical students included in the analyses, 37.3% had impaired physical component and 66.9% had impaired mental component of HRQoL. The determinants were medical students’ island of residence, history of hospitalization, and family member’s hospitalization and death due to COVID-19. Concerning mental health, the prevalence of reported symptoms of depression, anxiety, and stress were 45.4%, 65.2%, and 60.9%, respectively. Sex, study method, grade, previous COVID-19 disease severity, comorbidities, previous learning experience, and history of family isolation were identified as the determinants of mental health.
CONCLUSIONS: This study highlights the adverse effects of COVID-19 on HRQoL and mental health in Indonesian medical students. The results identified key associations, including SARS-CoV-2 infection and comorbidities experienced by the students, the health of their families, including grief following bereavement, and the effects of social isolation during the pandemic.
Keywords: COVID-19, Indonesia, Mental Health, Quality of Life, Students, Medical, Humans, COVID-19, Pandemics, SARS-CoV-2, Cross-Sectional Studies, Depression, Stress, Psychological, Anxiety
Background
On 11 March 2020, the World Health Organization declared coronavirus disease 2019 (COVID-19) to be a pandemic due to its alarming levels of spread and severity [1]. To date, this disease has infected more than 600 million people, and caused the deaths of more than 6 million people worldwide [2]. In addition to the clinical consequences, this disease also causes a substantial impact on the mental health of the global population [3]. A previous meta-analysis and review showed that the prevalence of depression and anxiety during the COVID-19 pandemic in the general population was 26.93% and 27.77%, respectively [4]. However, healthcare workers (HCWs) are at higher risk of having mental health problems compared to the general population [5], as HCWs are more exposed to COVID-19 [6]. Previously, we have shown that the prevalence of depression, anxiety, and stress among HCWs was 29.4%, 44.9%, and 31.8%, respectively, when evaluated using 21-item depression, anxiety, and stress scale (DASS-21) [7].
Other than HCWs, there is another vulnerable group for developing mental health problems during the COVID-19 pandemic, that is, medical students. A recent systematic review and meta-analysis study concluded that the prevalence of mental health problems among medical students during the COVID-19 pandemic was relatively higher than among HCWs and the general population [8]. It was already known that medical students were susceptible to mental health problems, which is associated with and closely related to Health-Related Quality of Life (HRQoL) [9]. Previous studies conducted before the COVID-19 pandemic have demonstrated that medical students are highly susceptible to developing an extremely high level of depression, stress, and other deterioration of mental health compared to the general population [10–12]. During this unprecedented COVID-19 pandemic, these conditions worsened, as shown by the increasing prevalence of mental health problems among medical students compared to the pre-pandemic era [13]. Furthermore, compared to the early period, the prevalence of mental health problems was reported to be worsened in the later period of the COVID-19 pandemic [14,15].
Reflecting on the severe acute respiratory syndrome (SARS) outbreak in 2003, emotional distress conditions could persist 1–2 years after the outbreak has ended, which was marked by an increased incidence of burnout, anxiety, depression, and posttraumatic stress disorder [16]. Medical students are the future medical doctors who will become the backbone of the nation’s healthcare personnel. Therefore, mental health problems that can decrease the HRQoL of medical students, which may persist 1–2 years after the outbreak, will plausibly disturb the future of the health care system [16]. However, to the best of our knowledge, only 1 previous study has evaluated both the HRQoL and mental health of Indonesian medical students [17], and the study participants were from only 1 university. Therefore, the present study aimed to evaluate HRQoL and mental health in 729 Indonesian medical students during the COVID-19 pandemic.
Material and Methods
L2 ETHICS STATEMENT:
This study was conducted according to the principles of the Declaration of Helsinki. Ethics clearance from the Faculty of Medicine Universitas Airlangga Ethical Reviewer Board was obtained prior to data collection (Ethical approval number 164/EC/KEPK/FKUA/2021, approval date 30 August 2021). Participation in this study was voluntary, and all details that might disclose the identity of the respondents were omitted prior to data analyses to ensure respondents’ privacy. Informed consent was obtained from each respondent prior to their participation in the study.
STUDY DESIGN AND POPULATION:
This was a cross-sectional study using an open online questionnaire. The study population was Indonesian medical students. Inclusion criteria were active medical students and agreed to participate as respondents in this study. All participants were recruited using the snowball sampling technique, and the questionnaire was distributed through the most popular and accessible social media platforms in Indonesia: LINE®, WhatsApp®, and Instagram®. Data collection was from 31 August to 30 September 2021. During this period, Indonesia has experienced the peak of the second wave that was caused by the Delta variant outbreak, which placed Indonesia in the epicentrum of the pandemic in Asia [18,19].
The minimum required sample size was estimated using Raosoft software version 2.3 (Raosoft, Inc., Seattle, USA). As there are no precise data on the actual number of undergraduate medical students in Indonesia, we referred to a previous study that also involved medical students in Indonesia as their population [20]. A minimum of 382 participants were required to obtain sufficient statistical power with a 5% of margin error and 95% confidence interval.
STUDY INSTRUMENT:
The online questionnaire was constructed according to the CHERRIES checklist [21], and SurveyMonkey® was used as the survey platform. Each participant could fill out the questionnaire only once because the IP address was used to detect potential duplicate entries from the same respondent. The time required to complete all questionnaires was approximately 10–15 min. The questionnaire consisted of the following 3 sections: 1) sociodemographic background, 2) HRQoL, and 3) mental health. The sociodemographic characteristics comprised questions concerning the participant’s gender, age, institution, education batch and semester, education status (preclinical or clinical), place of residence, study method before and during the pandemic, class duration before and during the pandemic, grade point average (GPA) before and during the pandemic, history of self and family COVID-19 infection history, comorbidities, vaccination status, and stigma from society.
HRQoL was measured using the 12-item-short-form version 2 (SF12v2) health survey (license number: QM054173) [22]. This survey had previously been translated into Bahasa Indonesia and demonstrated good validity and reliability [23]. The SF12v2 measures both mental and physical components, which are divided into 8 health domain scales: general health (GH), social functioning (SF), role physical (RP), physical functioning (PF), bodily pain (BP), role emotional (RE), vitality (VT), and mental health (MH). These domain scales have been described in a previous study [23]. Vitality, social functioning, role emotional, and mental health have the greatest mental factor content, whereas physical functioning, role physical, bodily pain, and general health have the greatest physical factor content among the health domains [22]. The Optum® PROCoRE software (Optum PROCoRE 1.3 Smart Measurement System. Optum Inc., USA) was used to perform the scoring of SF12v2. This software calculates the score for each health domain, physical component summary (PCS), and mental component summary (MCS). Scores of less than 47 indicate significant impairment in the associated health domain [22].
Mental health was evaluated using the DASS-21. This is a self-administered instrument widely used to assess the full range of depression, anxiety, and stress disorders’ core symptoms [24]. This instrument is chosen because it can evaluate depression, anxiety, and stress with the fewest questions [5]. DASS-21 has been translated into Bahasa Indonesia with good validity and reliability [25]. It has 3 subscales (depression, anxiety, and stress) composed of 7 questions each (21 questions in total). The score of each question ranges from 0, indicating the lack of symptoms in the past week, to 3, indicating the presence of symptoms almost every day in the past week. Each subscale score must be multiplied by 2 to obtain the final score. The total score is then categorized into normal, mild, moderate, severe, and extremely severe, with the cut off values as follows: normal (0–9), mild (10–12), moderate (13–20), severe (21–27), and extremely severe (28–42) for depression; normal (0–6), mild (7–9), moderate (10–14), severe (15–19), and extremely severe (20–42) for anxiety; and normal (0–10), mild (11–18), moderate (19–26), severe (27–34), and extremely severe (25–42) for stress subscales [24].
STATISTICAL ANALYSES:
All collected data were processed for data cleaning, coding, and tabulation to simplify the visualization. Data analysis was conducted using IBM SPSS Statistics for Windows version 25.0. (IBM Corp., Armonk, NY, USA). Respondents who filled out only the first part of the questionnaire (the sociodemographic background section) were excluded from the analyses. Respondents who also filled out the HRQoL but not the mental health section were included for sociodemographic and HRQoL analyses but not for the mental health analyses. Nominal variables are expressed as frequency (valid percentage), whereas continuous variables are expressed as mean±standard deviation (SD) for normally distributed data and median (interquartile range [IQR]) for skewed data. Data distribution was evaluated using the one-sample Kolmogorov–Smirnov test.
For identification of determinants for impaired HRQoL and mental health condition, 2-step logistic regression analysis was performed. In the first phase, univariate regression analyses were used to identify independent variables associated with impaired HRQoL and mental health. Variables with a P of <0.1 were included in the second phase, where a multivariate regression analysis was conducted using backward selection. Variables with a P of <0.05 from the multivariate analysis were considered as the determinants [7]. During the analyses to identify the determinants, mental health variables were recategorized into dichotomous (normal or impaired) with the cut off values as follows: >9 for depression, >6 for anxiety, and >10 for stress [24].
Results
BASELINE CHARACTERISTICS:
The mean age of participants was 20±1.5 years, with a predominance of females (76%). The majority of participants were preclinical medical students (85.6%) and primarily resided in the main island (65.8%). Approximately one-fourth of the participants never experienced a direct face-to-face class before the pandemic. There were 158 (21.7%) participants who had ever been infected with COVID-19. Most participants have been fully vaccinated, and 125 (17.1%) respondents had at least 1 comorbidity. Table 1 shows the detailed characteristics of the study participants.
HRQOL:
The median [IQR] scores of PCS and MCS were 48.65 [45.63–51.53] and 42.67 [36.49–49.27], respectively. RE health domain had the lowest score compared with other health domain scales. Figure 2 shows the detailed scores of physical and mental health components and each health domain scale. A total of 272 (37.3%) medical students had an impairment in the physical component, and 488 (66.9%) students had an impairment in the mental component. PF was the most impaired health domain, followed by RE (Figure 3).
The univariate logistic regression analyses showed that medical students who experienced asymptomatic COVID-19 infection were more likely to have impaired MCS, as were medical students who had a family member hospitalized because of COVID-19. Regarding PCS, medical students with a history of hospitalization due to COVID-19 were more likely to have impaired PCS (Table 2).
The independent determinants of MCS and PCS were then analyzed using multivariate logistic regression analysis. Medical students who had a family member hospitalized (adjusted odds ratio [AOR]=1.64, P=0.034) and who died because of COVID-19 (AOR=1.71, P=0.024) were more likely to have impaired MCS. Students with a history of hospitalization were more likely to have impaired PCS (AOR=5.15, P=0.030), whereas medical students who resided outside main island were less likely to have impaired PCS (AOR=0.71, P=0.039) (Table 3).
MENTAL HEALTH:
The median (IQR) score for depression was 8 [4–14], for anxiety it was 10 [6–16], and for stress it was 14 [8–18]. Of 718 respondents, 326 (45.4%) reported symptoms of depression, 468 (65.2%) reported symptoms of anxiety, and 437 (60.9%) reported symptoms of stress. Data on the severity of each mental health component are presented in Figure 4.
The univariate logistic regression analyses revealed that medical students who had a history of moderate-severe COVID-19 infection, a comorbidity, and a family member with moderate-severe COVID-19 infection were more likely to report symptoms of depression, whereas medical students who had a high GPA were less likely to report symptoms of depression. Regarding anxiety, female medical students, those who had ever undergone self-isolation, those who had moderate-severe COVID-19 infection, those who had a comorbidity, and those who had a family member who underwent self-isolation or had moderate-severe COVID-19 infection were more likely to report symptoms of anxiety. In contrast, older medical students, medical students in their clinical year, those who learned in the hybrid method, and those who had ever experienced the normal (face-to-face) teaching method before the pandemic were less likely to report symptoms of anxiety. For stress, female medical students, those who had moderate-severe COVID-19 infection, those who had a comorbidity, and those who had a family member who underwent self-isolation or had moderate-severe COVID-19 infection were more likely to report symptoms of stress. However, older medical students, medical students in their clinical year, and those who learned in the hybrid method were less likely to report symptoms of stress (Table 4).
The independent determinants of depression, stress, and anxiety were then analyzed using multivariate logistic regression analysis. Those who had a comorbidity were more likely to report symptoms of depression (AOR=1.72, P=0.009), whereas those who had high GPAs were less likely to report symptoms of depression (AOR=0.43, P=0.004). Female medical students (AOR=1.75, P=0.003) and those who had a comorbidity (AOR=2.06, P=0.003) were more likely to report symptoms of anxiety. However, medical students who learned in the hybrid method (AOR=0.67, P=0.022) and had ever experienced offline classes before the pandemic (AOR=0.65, P=0.029) were less likely to report symptoms of anxiety. Female medical students (AOR=1.58, P=0.014), those who had moderate-severe COVID-19 infection (AOR=5.87, P=0.019), those who had a comorbidity (AOR=1.60, P=0.035), and those who had a family member who underwent self-isolation (AOR=1.47, P=0.031) were more likely to report symptoms of stress. In contrast, medical students who learned in the hybrid method (AOR=0.69, P=0.033) were less likely to report symptoms of stress (Table 5).
Discussion
Our study showed that among 729 Indonesian medicals students, 272 (37.3%) had impaired physical component and 488 (66.9%) had impaired mental component of HRQoL. All respondents had impairment in the PF health domain and 89% of respondents also had impairment in the RE health domain. The determinants of HRQoL in this study were medical students’ island of residence, history of hospitalization, and family member’s hospitalization and death due to COVID-19. Concerning mental health, 326 (45.4%) reported symptoms of depression, 468 (65.2%) reported symptoms of anxiety, and 437 (60.9%) reported symptoms of stress. Sex, study method, grade, previous COVID-19 disease severity, comorbidities, previous learning experience, and history of family isolation were identified as determinants of mental health problems.
Previous studies conducted in India and Brazil also reported that medical students have lower levels of HRQoL during the COVID-19 pandemic [26,27]. The deleterious effects of COVID-19 on the HRQoL of medical students in other countries are similar to the Indonesian circumstances. However, a previous study in Indonesia reported that low HRQoL, either in physical or psychological components, was only observed in a minority of the respondents [17]. The discrepancy from our findings might be caused by difference in study period, as the previous study was conducted in the earlier period of the pandemic (June–November 2020), when the number of cases and mortality rates were still relative low [28], whereas our study was conducted after the peak of the second wave [18,19]. The discrepancy in findings might also be due to the difference in the instruments used to assess the HRQoL. In the present study, we used SF12v2, while the previous study used a different instrument.
Our analysis revealed that residing on the main island was an independent risk factor for the HRQoL of medical students. Consistent with a previous study, medical students who lived in rural areas showed better HRQoL than those living in urban areas, especially for the physical health component [26]. During COVID-19 home quarantine, decreased physical activity and higher screen time or internet usage appeared to be the influential factors contributing to lower HRQoL in urban areas [29]. Moreover, the impacts of COVID-19 in rural areas are still low, as the transmission of COVID-19 in sparsely populated areas is much lower than that in urban areas, and, living close to nature could regenerate the senses and mind, which can improve HRQoL [30,31].
In this study, we found that medical students with a history of hospitalization due to COVID-19 had lower HRQoL. A previous study conducted in Bangladesh also found that patients hospitalized because of COVID-19 had significantly lower HRQoL [32]. Their physical components were also affected, such as difficulty in walking and lifting and carrying things, which are commonly found in hospitalized patients [33]. Additionally, persistence of symptoms, delayed recovery, and stress response in hospitalized patients also increase the risk of distress [32,34].
Experiences of close contact with patients with COVID-19, especially family, could potentially decrease HRQoL because of high rates of depression and fatigue [34]. Moreover, young people had a higher risk of negative psychological conditions caused by the restriction of social activities during the COVID-19 pandemic [35]. This finding was consistent with our study, which showed that medical students whose family members had COVID-19 had lower MCS. The fear of getting infected increased their anxiety and frustration, and the hospitalized family also induced worries and disrupted their concentration [36,37]. Facing the death of family members due to COVID-19 altered the self-efficacy and coping mechanisms of the medical students because the family member was the first-line support and the loss of their presence placed them in more stressful and frustrating situations [38,39].
The prevalence of depression, anxiety, and stress in our study were 45.4%, 65.2%, and 60.9%, respectively. The prevalence was higher than in previous studies. A study in India reported that the prevalences of depression, anxiety, and stress among undergraduate medical students during the COVID-19 pandemic were 33.5%, 33.2%, and 24.9%, respectively [13]. In a recent systematic review and meta-analysis, the pooled prevalence of depression and anxiety among medical students during the COVID-19 pandemic was 37.9% and 33.7%, respectively [8]. There are 3 previous studies from Indonesia that also evaluated the prevalence of mental health problems among medical students where the DASS-21 was also used as the study instrument; the prevalence of depression, anxiety, and stress was 13.5–18.6%, 15–48.1%, and 7.5–44.6%, respectively [17,30,40]. One of the possible explanations of the high prevalence in our study is because we collected the data shortly after Indonesia faced the peak of the second wave, which was caused by the Delta variant outbreak, and which placed Indonesia as the epicentrum of the pandemic in Asia [18,19].
Our analysis revealed that female gender was a significant independent predictor of anxiety and stress among medical students, which agrees with previous findings in the United Arab Emirates [41], France [42], and Morocco [43]. A worldwide cross-sectional study conducted in the general population has also consistently shown that women had more anxiety than men [44]. Additionally, it is stated that women are twice more likely to develop stress- and anxiety-related psychiatric disorders than men. Men and women have different fear and stress mechanisms because of hormonal influences [45]. Generally, the COVID-19 pandemic has in fact increased the incidence of mental health disorders significantly and being female is one of the risk factors. However, female gender is not the primary risk factor, as other variables such as personality type, lifestyle, and coping mechanisms also influence the levels of depression, anxiety, and stress [46–48].
We found that students with previous moderate or severe COVID-19 infection were more likely to exhibit depressive and stress symptoms than those who had never had the disease. Irrespective of being medical students, previous studies on general COVID-19 survivors have shown a high prevalence of psychiatric sequelae, including posttraumatic stress disorder, major depression, and anxiety [49,50]. Immunological responses to the infection and psychological factors, such as stigma, social isolation, concerns of infecting others, and mental impact due to a novel potentially fatal disease, might contribute to the development of post-COVID-19 psychiatric consequences [49]. Our results also showed that the presence of COVID-19-related medical comorbidities was highly associated with depression, anxiety, and stress. People with existing chronic illnesses were found to have poorer mental health during the COVID-19 pandemic. This association might be caused by the fact that individuals with comorbidities are more vulnerable to death due to COVID-19 and thus would likely have higher rates of psychiatric symptoms [51]. Our study also showed that some students with a family history of isolation were more susceptible to stress than those without a family history of isolation. Education level was considered to be related to the level of stress, which was higher among university students because of their capability of understanding the risk of SARS-CoV-2 infection and being more cautious of their surroundings [52]. Furthermore, some individuals, including students, were reported to have fears of getting infected from their family members who tested positive for COVID-19 and were extremely concerned about their own health, especially if they experienced any signs and/or symptoms related to any specific diseases during the associated pandemic [53]. The latter statement also well strengthened our finding that students’ stress was not significantly increased when the family members who tested positive for COVID-19 had their isolation periods in the hospital. When a family member was diagnosed with COVID-19, there were also some potential disruptions in the family relationship, routines, and rituals, which might further elevate the level of stress of the other family members [54].
In our study, lower rates of anxiety and stress were found in students who had experienced offline classes and had undergone the hybrid or blended learning method during the COVID-19 pandemic. A longer offline learning experience decreased the level of anxiety and stress among the medical students, as there were still more achievable clinical skills than those obtained with full online learning methods [55,56]. Our finding was also affected by the participants as our study sample was predominated by preclinical than clinical students, implying that preclinical students still did not understand the importance of offline classes compared with clinical students who require more offline clinical skill development rather than just discussing it online and will soon become professional medical health teams in the field [56–58]. Additionally, hybrid learning methods were likely to improve self-directed learning of the students as they had more time to learn medical skills and theory [58]. Consistent with our findings, a previous study also reported that students with lower GPAs were more likely to be depressed [59]. Thus, hybrid learning methods might decrease the levels of depression, anxiety, and stress, as there was more time for self-learning in the middle of having offline classes.
Depression is tightly associated with obesity, a phenomenon that was recently introduced as depreobesity (depression in the context of obesity) [60]. During the COVID-19 pandemic, previous studies have shown that depression is more prevalent in people with weight gain than in people with weight loss [61,62]. Compared to old individuals, young individuals are more likely to have increased bodyweight during the COVID-19 pandemic [63], possibly because of the unhealthy eating behaviors to cope with the pandemic, which is common among young people [64]. If no intervention is offered, especially among young people, including medical students, an upcoming epidemic of depreobesity can be expected in the near future [60,65].
This study has 3 important limitations to consider. First, the cross-sectional nature of the study precludes any causal inference or evaluation of longitudinal changes in HRQoL and mental health problems during the COVID-19 pandemic. Second, both instruments used in this study – DASS-21 to evaluate mental health and SF12v2 to evaluate HRQoL – are self-reported questionnaires; thus, this may under- or overestimate the prevalence of impaired HRQoL and mental health problems, and may not concur with objective assessment by health professionals. Third, as snowball sampling was used to recruit the respondents, this study was prone to selection bias, as only those with internet access and spare time were able to participate in this study. In addition, although the number of respondents in this study surpassed the minimum required number, the number of respondents was still small compared to the total number of medical students in Indonesia. Therefore, generalization of study findings to all medical students in Indonesia should be done cautiously.
Conclusions
This study of Indonesian medical students during the COVID-19 pandemic supports the findings from other studies on the adverse effects on HRQoL and mental health. The results identified key associations, including SARS-CoV-2 infection and comorbidities experienced by the students, the health of their families, including grief following bereavement, and the effects of social isolation during the pandemic. As medical students are essential for advancing the country’s health system and become the core of health services, we recommend that higher-learning institutions in Indonesia, in collaboration with the government, provide psychological assistance to medical students, especially to those who are at higher risk.
Figures
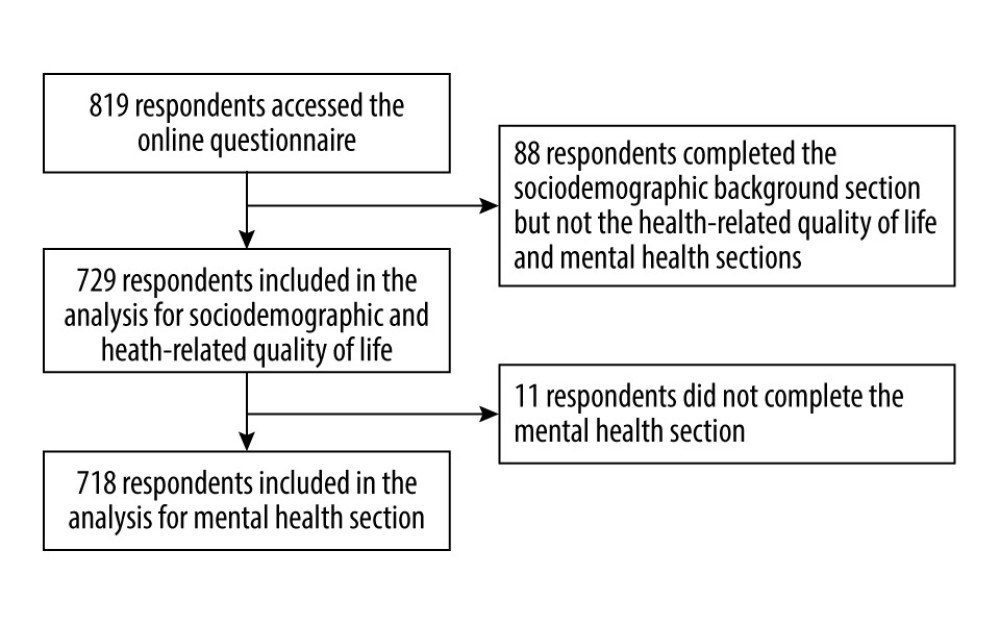 Figure 1. Flowchart of the study participants selection.
Figure 1. Flowchart of the study participants selection. 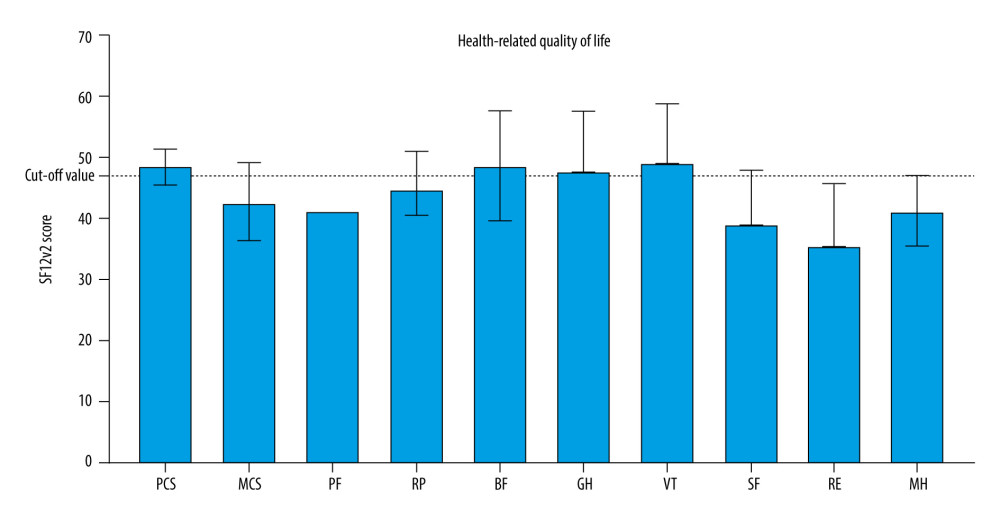 Figure 2. Median norm-based T-score of summary scores and each health domain scale of health-related quality of life among 729 medical students in Indonesia. BP – bodily pain; GH – general health; MCS – mental component summary; MH – mental health; PCS – physical component summary; PF – physical-function; RP – role-physical; SF – social functioning; SF12v2 – 12-item Short Form version 2; RE – role-emotional; VT – vitality. Health-related quality of life is evaluated using 12-item short form version 2.
Figure 2. Median norm-based T-score of summary scores and each health domain scale of health-related quality of life among 729 medical students in Indonesia. BP – bodily pain; GH – general health; MCS – mental component summary; MH – mental health; PCS – physical component summary; PF – physical-function; RP – role-physical; SF – social functioning; SF12v2 – 12-item Short Form version 2; RE – role-emotional; VT – vitality. Health-related quality of life is evaluated using 12-item short form version 2. 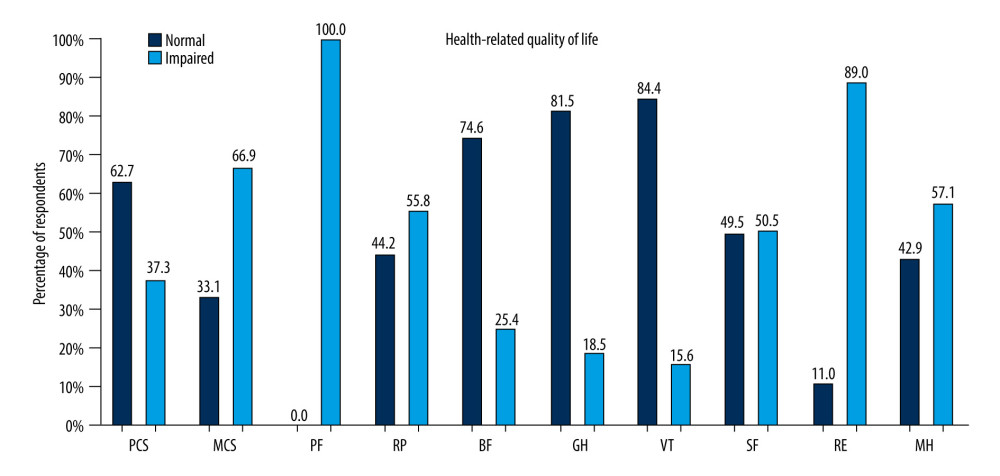 Figure 3. Prevalence of impaired health-related quality of life in physical and mental components in general and each health domain scale among 729 medical students in Indonesia. BP – bodily pain; GH – general health; MCS – mental component summary; MH – mental health; PCS – physical component summary; PF – physical-function; RP – role-physical; SF – social functioning; SF12v2 – 12-item Short Form version 2; RE – role-emotional; VT – vitality. Health-related quality of life is evaluated using 12-item short form version 2.
Figure 3. Prevalence of impaired health-related quality of life in physical and mental components in general and each health domain scale among 729 medical students in Indonesia. BP – bodily pain; GH – general health; MCS – mental component summary; MH – mental health; PCS – physical component summary; PF – physical-function; RP – role-physical; SF – social functioning; SF12v2 – 12-item Short Form version 2; RE – role-emotional; VT – vitality. Health-related quality of life is evaluated using 12-item short form version 2. 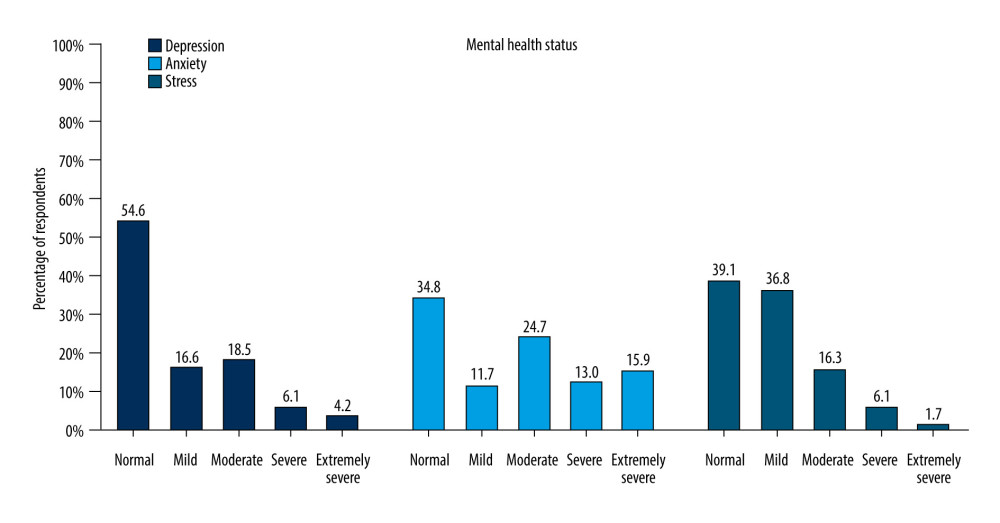 Figure 4. 0Prevalence of depression, anxiety, and stress among 718 medical students in Indonesia evaluated using 21-item Depression, Anxiety, and Stress Scale.
Figure 4. 0Prevalence of depression, anxiety, and stress among 718 medical students in Indonesia evaluated using 21-item Depression, Anxiety, and Stress Scale. Tables
Table 1. Characteristics of the study participants.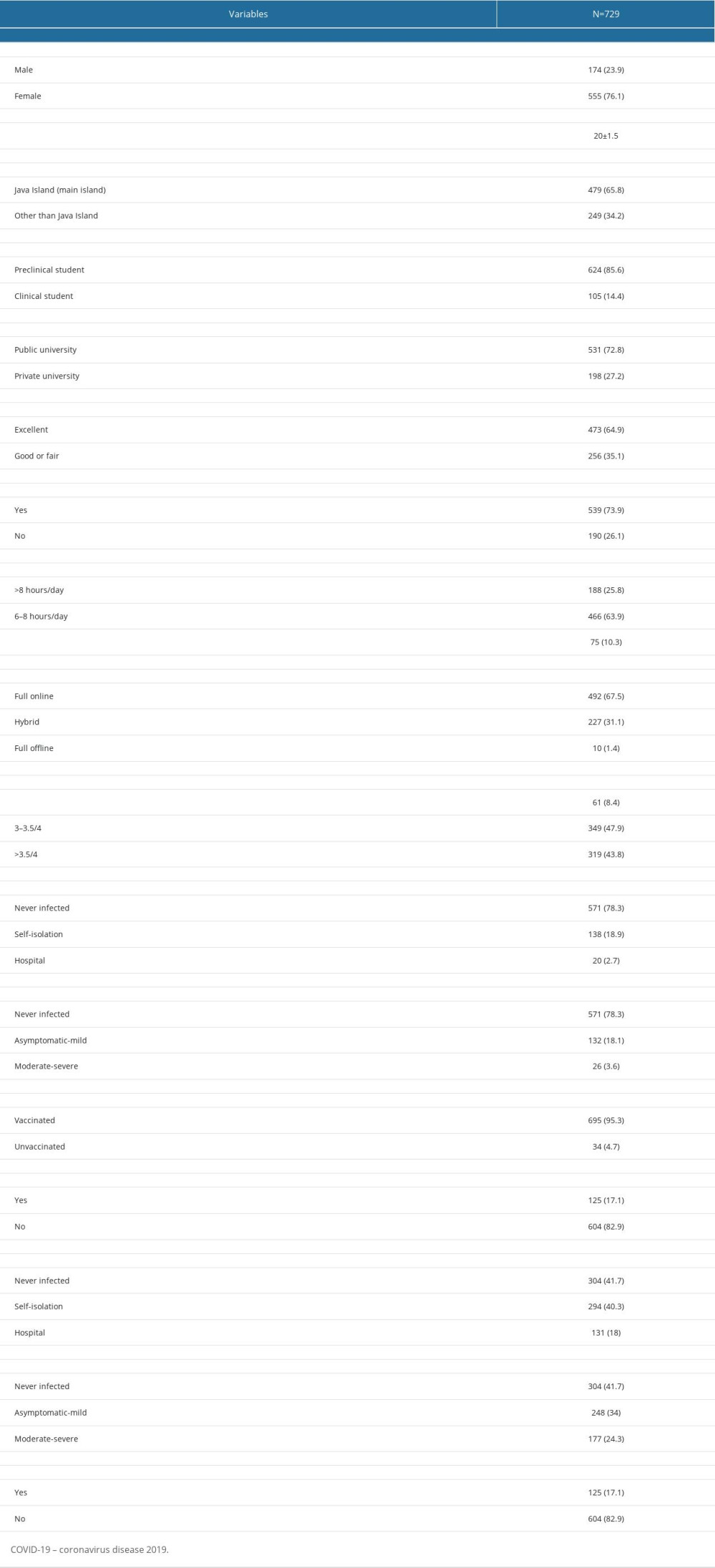 Table 2. Univariate logistic regression analysis for impaired health-related quality of life.
Table 2. Univariate logistic regression analysis for impaired health-related quality of life.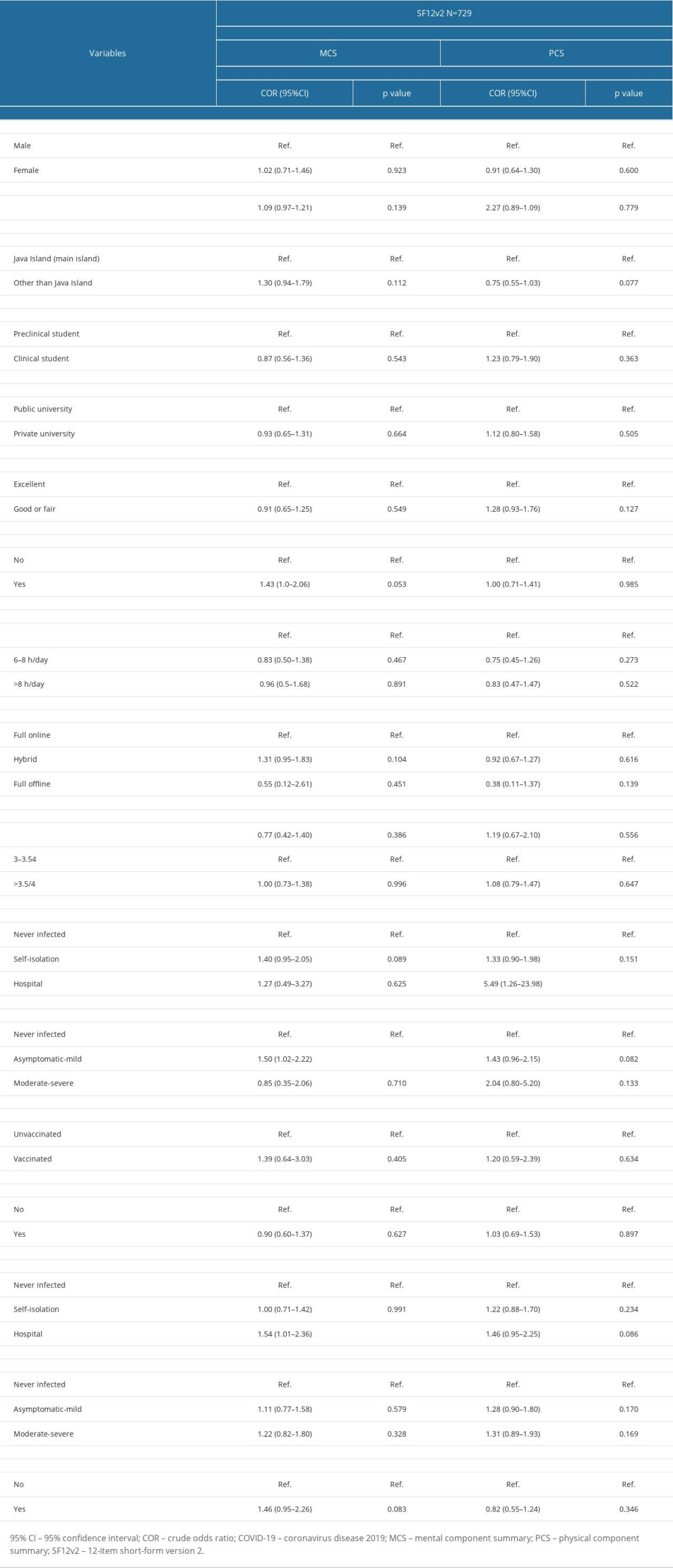 Table 3. Multivariate logistic regression analysis for impaired health-related quality of life.
Table 3. Multivariate logistic regression analysis for impaired health-related quality of life.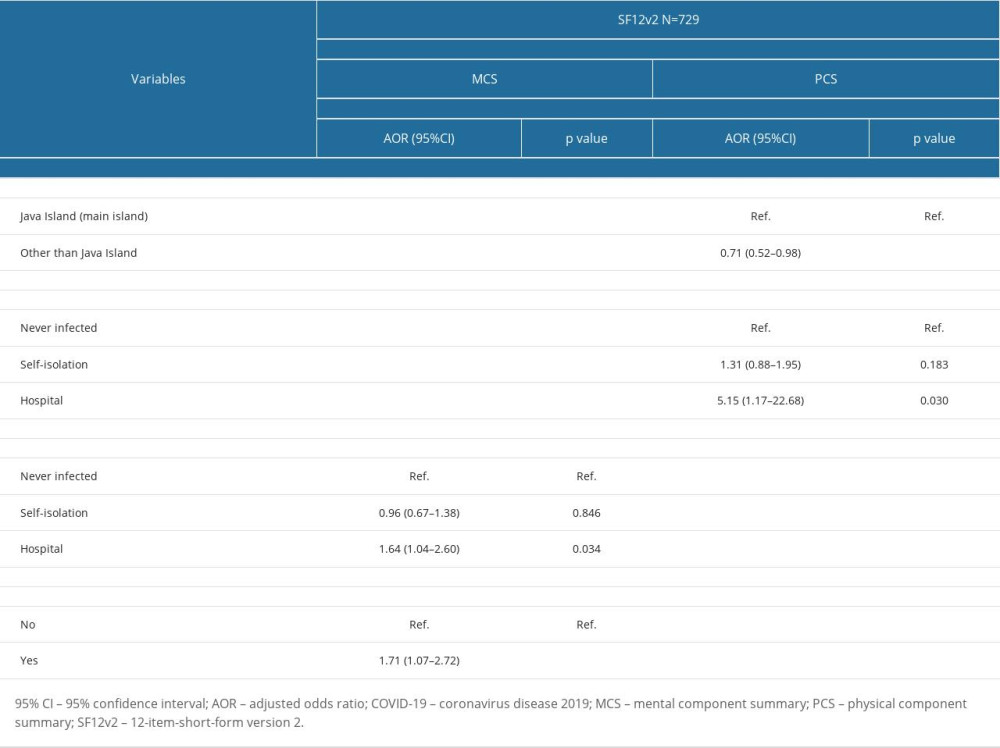 Table 4. Univariate logistic regression analysis for mental health problems.
Table 4. Univariate logistic regression analysis for mental health problems.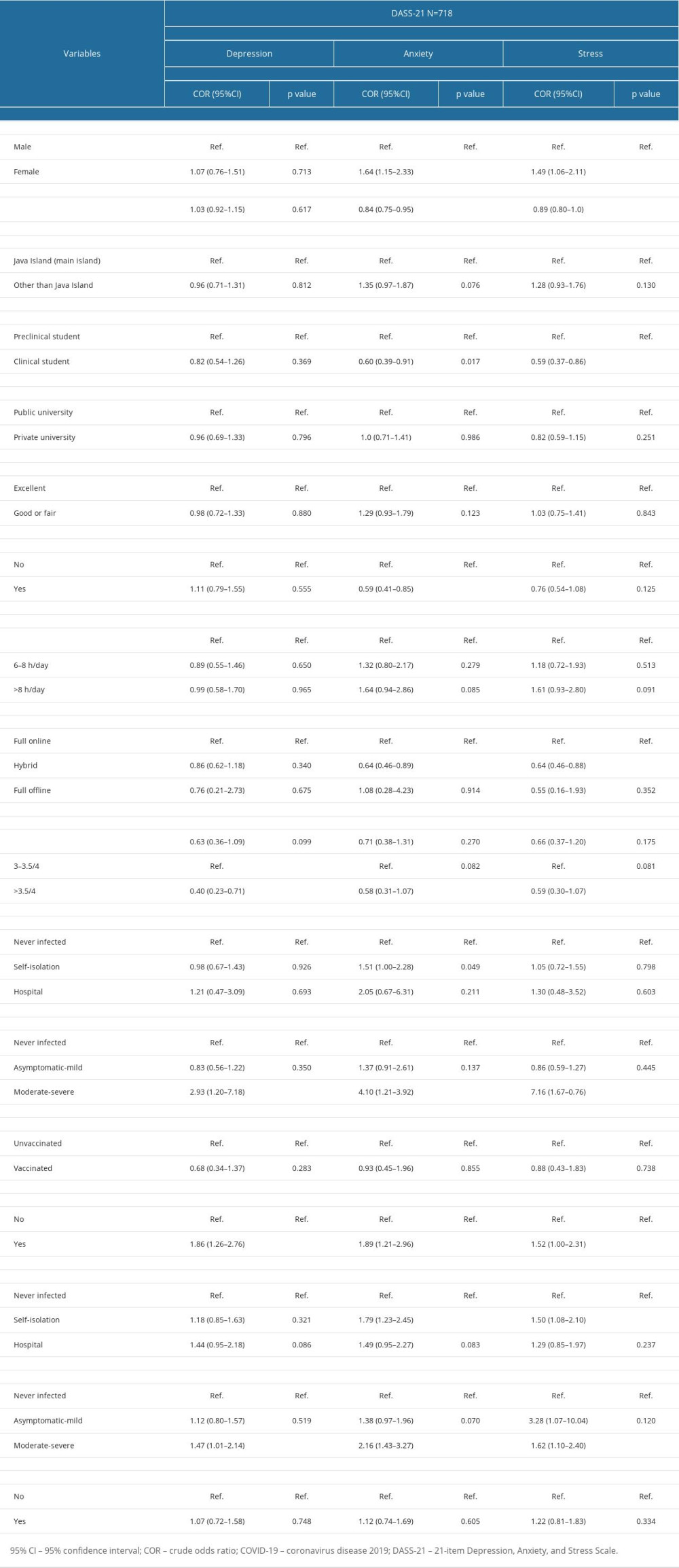 Table 5. Multivariate logistic regression analysis for mental health problems.
Table 5. Multivariate logistic regression analysis for mental health problems.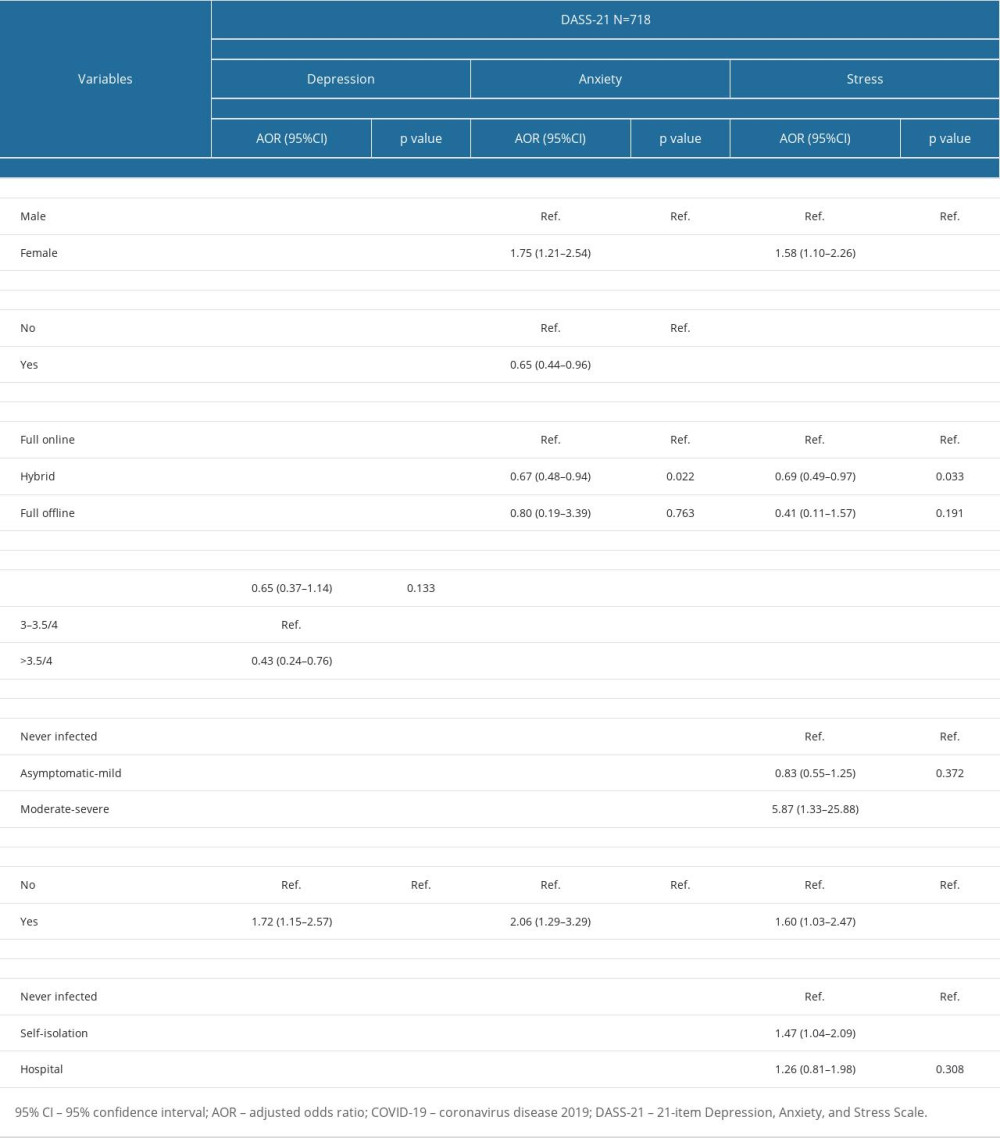
References
1. World Health Organization: Rolling updates on coronavirus disease (COVID-19) [updated 31 July 2020; cited 25 November 2022]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen
2. World Health Organization: Weekly epidemiological update on COVID-19 November 23, 2022 [updated 23 November 2022; cited 25 November 2022]. Available from: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---23-november-2022
3. COVID-19 Mental Disorders Collaborators, Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic: Lancet, 2021; 398(10312); 1700-12
4. de Sousa GM, Tavares VDO, de Meiroz Grilo MLP, Mental health in COVID-19 pandemic: A meta-review of prevalence meta-analyses: Front Psychol, 2021; 12; 703838
5. Lusida MAP, Salamah S, Jonatan M, Prevalence of and risk factors for depression, anxiety, and stress in non-hospitalized asymptomatic and mild COVID-19 patients in East Java province, Indonesia: PLoS One, 2022; 17(7); e0270966
6. Uphoff EP, Lombardo C, Johnston G, Mental health among healthcare workers and other vulnerable groups during the COVID-19 pandemic and other coronavirus outbreaks: A rapid systematic review: PLoS One, 2021; 16(8); e0254821
7. Syamlan AT, Salamah S, Alkaff FF, Mental health and health-related quality of life among healthcare workers in Indonesia during the COVID-19 pandemic: A cross-sectional study: BMJ Open, 2022; 12(4); e057963
8. Jia Q, Qu Y, Sun H, Mental health among medical students during COVID-19: A systematic review and meta-analysis: Front Psychol, 2022; 13; 846789
9. Moutinho ILD, Lucchetti ALG, Ezequiel ODS, Lucchetti G, Mental health and quality of life of Brazilian medical students: Incidence, prevalence, and associated factors within two years of follow-up: Psychiatry Res, 2019; 274; 306-12
10. Dyrbye LN, West CP, Satele D, Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population: Acad Med, 2014; 89(3); 443-51
11. Moir F, Yielder J, Sanson J, Chen Y, Depression in medical students: Current insights: Adv Med Educ Pract, 2018; 9; 323-33
12. Bergmann C, Muth T, Loerbroks A, Medical students’ perceptions of stress due to academic studies and its interrelationships with other domains of life: A qualitative study: Med Educ Online, 2019; 24(1); 1603526
13. Saraswathi I, Saikarthik J, Senthil Kumar K, Impact of COVID-19 outbreak on the mental health status of undergraduate medical students in a COVID-19 treating medical college: A prospective longitudinal study: Peer J, 2020; 8; e10164
14. Dominguez-Gonzalez AD, Guzman-Valdivia G, Angeles-Tellez FS, Depression and suicidal ideation in Mexican medical students during COVID-19 outbreak. A longitudinal study: Heliyon, 2022; 8(2); e08851
15. Zhang K, Lin Z, Peng Y, Li L, A longitudinal study on psychological burden of medical students during COVID-19 outbreak and remission period in China: Eur J Psychiatry, 2021; 35(4); 234-41
16. Lancee WJ, Maunder RG, Goldbloom DSCoauthors for the Impact of SARS Study, Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak: Psychiatr Serv, 2008; 59(1); 91-95
17. Tejoyuwono AAT, Nugraha RP, Fahdi FK, The effect of mental health status on the quality of life of faculty of medicine students during the pandemic coronavirus disease 2019 period: Open Access Macedonian Journal of Medical Sciences, 2021; 9(E); 645-52
18. Dyer O, COVID-19: Indonesia becomes Asia’s new pandemic epicentre as delta variant spreads: BMJ, 2021; 374; n1815
19. World Health Organization Indonesia: Coronavirus Disease 2019 (COVID-19) Situation Report – 78 [updated 27 October 2021; cited 27 November 2022]. Available from: https://www.who.int/indonesia/news/novel-coronavirus/situation-reports
20. Lazarus G, Findyartini A, Putera AM, Willingness to volunteer and readiness to practice of undergraduate medical students during the COVID-19 pandemic: A cross-sectional survey in Indonesia: BMC Med Educ, 2021; 21(1); 138
21. Eysenbach G, Improving the quality of Web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES): J Med Internet Res, 2004; 6(3); e34
22. Maruish ME: User’s manual for the SF-12v2 Health Survey, 2012, Lincoln, RI, QualityMetric Incorporated
23. Wicaksana AL, Maharani E, Hertanti NS, The Indonesian version of the Medical Outcome Survey – Short Form 12 version 2 among patients with cardiovascular diseases: Int J Nurs Pract, 2020; 26(2); e12804
24. Lovibond SH, Lovibond PF: Manual for the Depression Anxiety Stress Scales, 1995, Sydney, Australia, Psychology Foundation
25. El-Matury HJ, Lestari FA, Besral , Depression, anxiety and stress among undergraduate students in jakarta: Examining scores of the depression anxiety and stress scale according to origin and residency: Indian Journal of Public Health Research and Development, 2018; 9(2); 290-95
26. Chawla B, Chawla S, Singh H, Jain R, Arora I, Is coronavirus lockdown taking a toll on mental health of medical students? A study using WHOQOL-BREF questionnaire: J Family Med Prim Care, 2020; 9(10); 5261-66
27. Barreto FS, de Carvalho GO, da Silva LCN, Electronic tools for physical activity and quality of life of medical students during COVID-19 pandemic social isolation: Motriz: Revista de Educação Física, 2021; 27; e1021002121
28. Worldometer: Indonesia COVID – coronavirus statistics – Worldometer 2022 [18 September 2022]. Available from: https://www.worldometers.info/coronavirus/country/indonesia/
29. Biswas S, Bipeta R, Molangur U, Reshaboyina LR, A study to assess the quality of life of undergraduate medical students: Open J Psychiatry Allied Sci, 2019; 10; 19-25
30. Natalia D, Syakurah RA, Mental health state in medical students during COVID-19 pandemic: J Educ Health Promot, 2021; 10; 208
31. Hoegmark S, Andersen TE, Grahn P, The Wildman programme-rehabilitation and reconnection with nature for men with mental or physical health problems – a matched-control study: Int J Environ Res Public Health, 2021; 18(21); 11465
32. Hawlader MDH, Rashid MU, Khan MAS, Quality of life of COVID-19 recovered patients in Bangladesh: PLoS One, 2021; 16(10); e0257421
33. Jacobs LG, Gourna Paleoudis E, Lesky-Di Bari D, Persistence of symptoms and quality of life at 35 days after hospitalization for COVID-19 infection: PLoS One, 2020; 15(12); e0243882
34. Zhao YJ, Zhang SF, Li W, Mental health status and quality of life in close contacts of COVID-19 patients in the post-COVID-19 era: A comparative study: Transl Psychiatry, 2021; 11(1); 505
35. Li HY, Cao H, Leung DYP, Mak YW, The psychological impacts of a COVID-19 outbreak on college students in China: A longitudinal study: Int J Environ Res Public Health, 2020; 17(11); 3933
36. Leong Bin Abdullah MFI, Mansor NS, Quality of life and associated factors among university students during the COVID-19 pandemic: A cross-sectional study: BMJ Open, 2021; 11(10); e048446
37. Wheaton MG, Prikhidko A, Messner GR, Is fear of COVID-19 contagious? The effects of emotion contagion and social media use on anxiety in response to the coronavirus pandemic: Front Psychol, 2020; 11; 567379
38. Batley NJ, Bakhti R, Chami A, The effect of patient death on medical students in the emergency department: BMC Med Educ, 2017; 17(1); 110
39. Ho CY, Kow CS, Chia CHJ, The impact of death and dying on the personhood of medical students: A systematic scoping review: BMC Med Educ, 2020; 20(1); 516
40. Ramadianto AS, Kusumadewi I, Agiananda F, Raharjanti NW, Symptoms of depression and anxiety in Indonesian medical students: Association with coping strategy and resilience: BMC Psychiatry, 2022; 22(1); 92
41. Saddik B, Hussein A, Sharif-Askari FS, Increased levels of anxiety among medical and non-medical university students during the COVID-19 pandemic in the United Arab Emirates: Risk Manag Healthc Policy, 2020; 13; 2395-406
42. Wathelet M, Duhem S, Vaiva G, Factors associated with mental health disorders among university students in France confined during the COVID-19 pandemic: JAMA Netw Open, 2020; 3(10); e2025591
43. Essangri H, Sabir M, Benkabbou A, Predictive factors for impaired mental health among medical students during the early stage of the COVID-19 pandemic in Morocco: Am J Trop Med Hyg, 2021; 104(1); 95-102
44. Seedat S, Scott KM, Angermeyer MC, Cross-national associations between gender and mental disorders in the World Health Organization World Mental Health Surveys: Arch Gen Psychiatry, 2009; 66(7); 785-95
45. Maeng LY, Milad MR, Sex differences in anxiety disorders: Interactions between fear, stress, and gonadal hormones: Horm Behav, 2015; 76; 106-17
46. Perez-Cano HJ, Moreno-Murguia MB, Morales-Lopez O, Anxiety, depression, and stress in response to the coronavirus disease-19 pandemic: Cir Cir, 2020; 88(5); 562-68
47. Lee E, Kim Y, Effect of university students’ sedentary behavior on stress, anxiety, and depression: Perspect Psychiatr Care, 2019; 55(2); 164-69
48. Kim SC, Sloan C, Montejano A, Quiban C, Impacts of coping mechanisms on nursing students’ mental health during COVID-19 lockdown: A cross-sectional survey: Nurs Rep, 2021; 11(1); 36-44
49. Mazza MG, De Lorenzo R, Conte C, Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors: Brain Behav Immun, 2020; 89; 594-600
50. Taquet M, Luciano S, Geddes JR, Harrison PJ, Bidirectional associations between COVID-19 and psychiatric disorder: Retrospective cohort studies of 62 354 COVID-19 cases in the USA: Lancet Psychiatry, 2021; 8(2); 130-40
51. Sayeed A, Kundu S, Al Banna MH, Mental health outcomes of adults with comorbidity and chronic diseases during the COVID-19 pandemic: A matched case-control study: Psychiatr Danub, 2020; 32(3–4); 491-98
52. TMGH-Global COVID-19 Collaborative, Perceived stress of quarantine and isolation during COVID-19 pandemic: A globals: Front Psychiatry, 2021; 12; 656664
53. Brooks SK, Webster RK, Smith LE, The psychological impact of quarantine and how to reduce it: Rapid review of the evidence: Lancet, 2020; 395(10227); 912-20
54. Prime H, Wade M, Browne DT, Risk and resilience in family well-being during the COVID-19 pandemic: Am Psychol, 2020; 75(5); 631-43
55. Budiman AA, Lestari R, Yuliatun L, What is factor contributing to medical student learning anxiety during COVID-19 pandemic? A systematic review: International Journal of Public Health Science, 2021; 10(4); 898-905
56. TMS Collaborative, The perceived impact of the COVID-19 pandemic on medical student education and training – an international survey: BMC Med Educ, 2021; 21(1); 566
57. Lasheras I, Gracia-Garcia P, Lipnicki DM, Prevalence of anxiety in medical students during the COVID-19 pandemic: A rapid systematic review with meta-analysis: Int J Environ Res Public Health, 2020; 17(18); 6603
58. Aaraj S, Farooqi F, Saeed N, Khan S, Impact of COVID pandemic and hybrid teaching on final year MBBS students’ end of clerkship exam performance: Pak J Med Sci, 2022; 38(1); 113-17
59. Nakhostin-Ansari A, Sherafati A, Aghajani F, Depression and anxiety among iranian medical students during COVID-19 pandemic: Iran J Psychiatry, 2020; 15(3); 228-35
60. Mediouni M, Kaczor-Urbanowicz KE, Madiouni R, Future epidemic: Depreobesity: Obesity Medicine, 2020; 19; 100240
61. Almandoz JP, Xie L, Schellinger JN, Changes in body weight, health behaviors, and mental health in adults with obesity during the COVID-19 pandemic: Obesity (Silver Spring), 2022; 30(9); 1875-86
62. Khubchandani J, Price JH, Sharma S, COVID-19 pandemic and weight gain in American adults: A nationwide population-based study: Diabetes Metab Syndr, 2022; 16(1); 102392
63. Alshahrani SM, Alghannam AF, Taha N, The impact of COVID-19 pandemic on weight and body mass index in Saudi Arabia: A longitudinal study: Front Public Health, 2021; 9; 775022
64. Mason TB, Barrington-Trimis J, Leventhal AM, Eating to cope with the COVID-19 pandemic and body weight change in young adults: J Adolesc Health, 2021; 68(2); 277-83
65. Mediouni M, Madiouni R, Kaczor-Urbanowicz KE, COVID-19: How the quarantine could lead to the depreobesity: Obes Med, 2020; 19; 100255
Figures
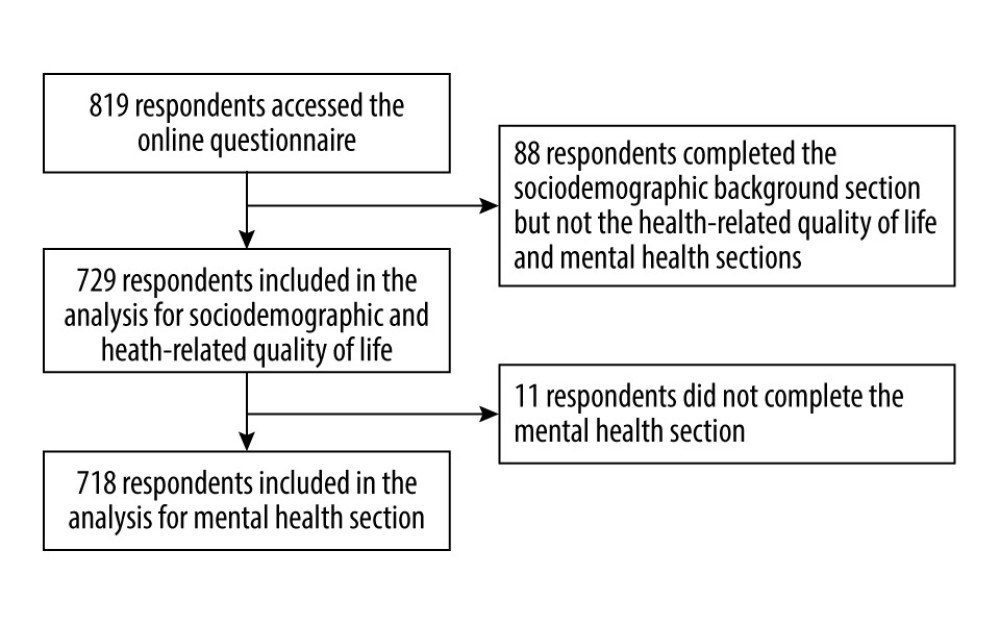 Figure 1. Flowchart of the study participants selection.
Figure 1. Flowchart of the study participants selection.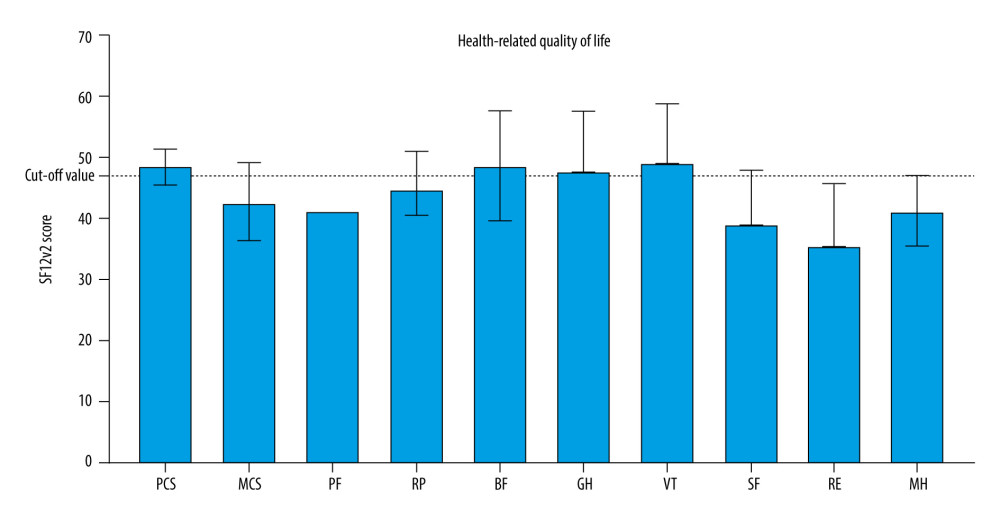 Figure 2. Median norm-based T-score of summary scores and each health domain scale of health-related quality of life among 729 medical students in Indonesia. BP – bodily pain; GH – general health; MCS – mental component summary; MH – mental health; PCS – physical component summary; PF – physical-function; RP – role-physical; SF – social functioning; SF12v2 – 12-item Short Form version 2; RE – role-emotional; VT – vitality. Health-related quality of life is evaluated using 12-item short form version 2.
Figure 2. Median norm-based T-score of summary scores and each health domain scale of health-related quality of life among 729 medical students in Indonesia. BP – bodily pain; GH – general health; MCS – mental component summary; MH – mental health; PCS – physical component summary; PF – physical-function; RP – role-physical; SF – social functioning; SF12v2 – 12-item Short Form version 2; RE – role-emotional; VT – vitality. Health-related quality of life is evaluated using 12-item short form version 2.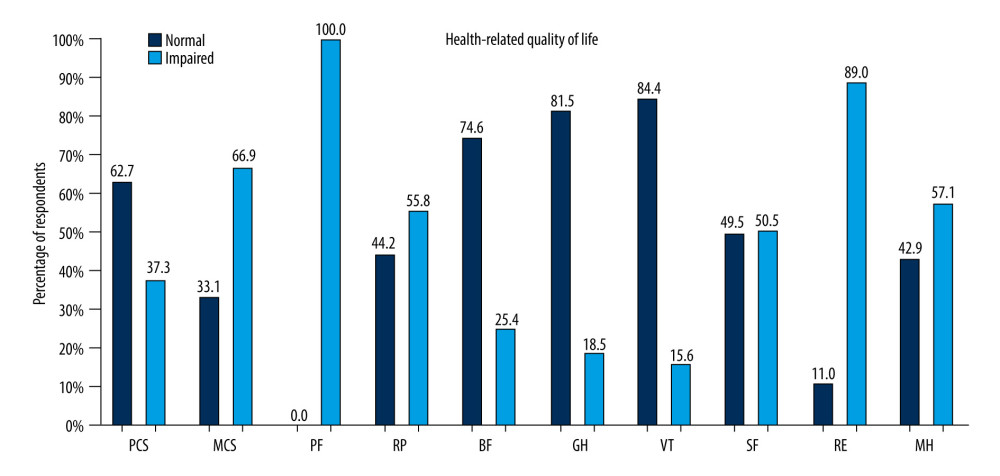 Figure 3. Prevalence of impaired health-related quality of life in physical and mental components in general and each health domain scale among 729 medical students in Indonesia. BP – bodily pain; GH – general health; MCS – mental component summary; MH – mental health; PCS – physical component summary; PF – physical-function; RP – role-physical; SF – social functioning; SF12v2 – 12-item Short Form version 2; RE – role-emotional; VT – vitality. Health-related quality of life is evaluated using 12-item short form version 2.
Figure 3. Prevalence of impaired health-related quality of life in physical and mental components in general and each health domain scale among 729 medical students in Indonesia. BP – bodily pain; GH – general health; MCS – mental component summary; MH – mental health; PCS – physical component summary; PF – physical-function; RP – role-physical; SF – social functioning; SF12v2 – 12-item Short Form version 2; RE – role-emotional; VT – vitality. Health-related quality of life is evaluated using 12-item short form version 2.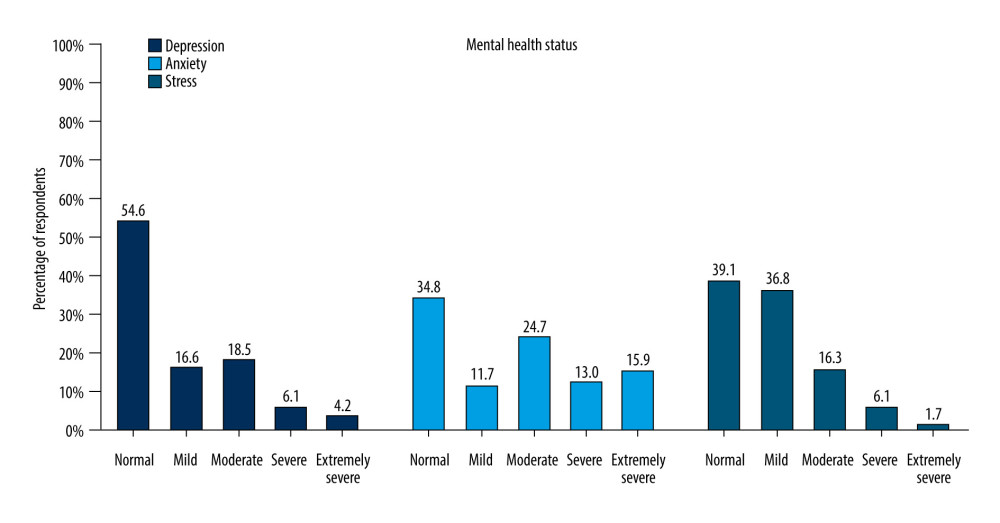 Figure 4. 0Prevalence of depression, anxiety, and stress among 718 medical students in Indonesia evaluated using 21-item Depression, Anxiety, and Stress Scale.
Figure 4. 0Prevalence of depression, anxiety, and stress among 718 medical students in Indonesia evaluated using 21-item Depression, Anxiety, and Stress Scale. Tables
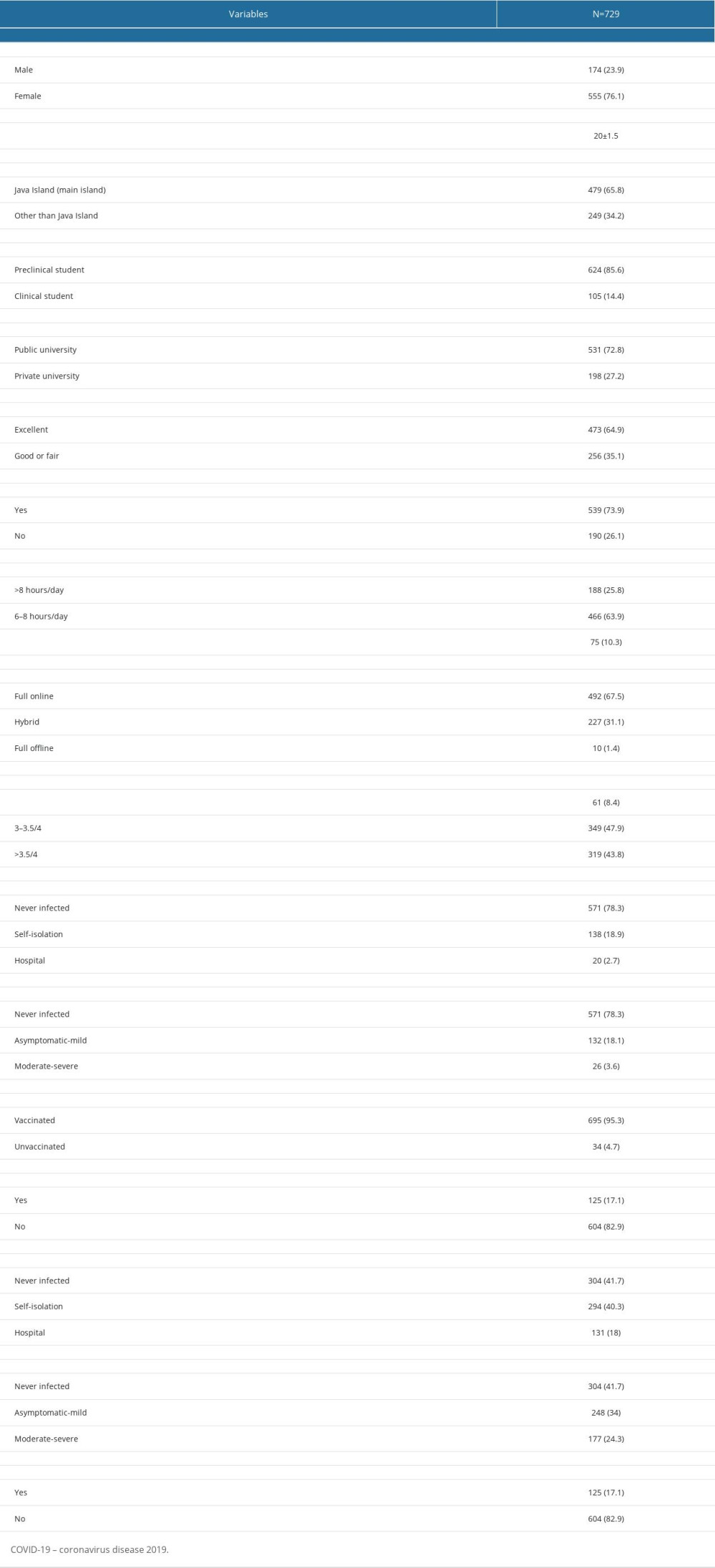 Table 1. Characteristics of the study participants.
Table 1. Characteristics of the study participants.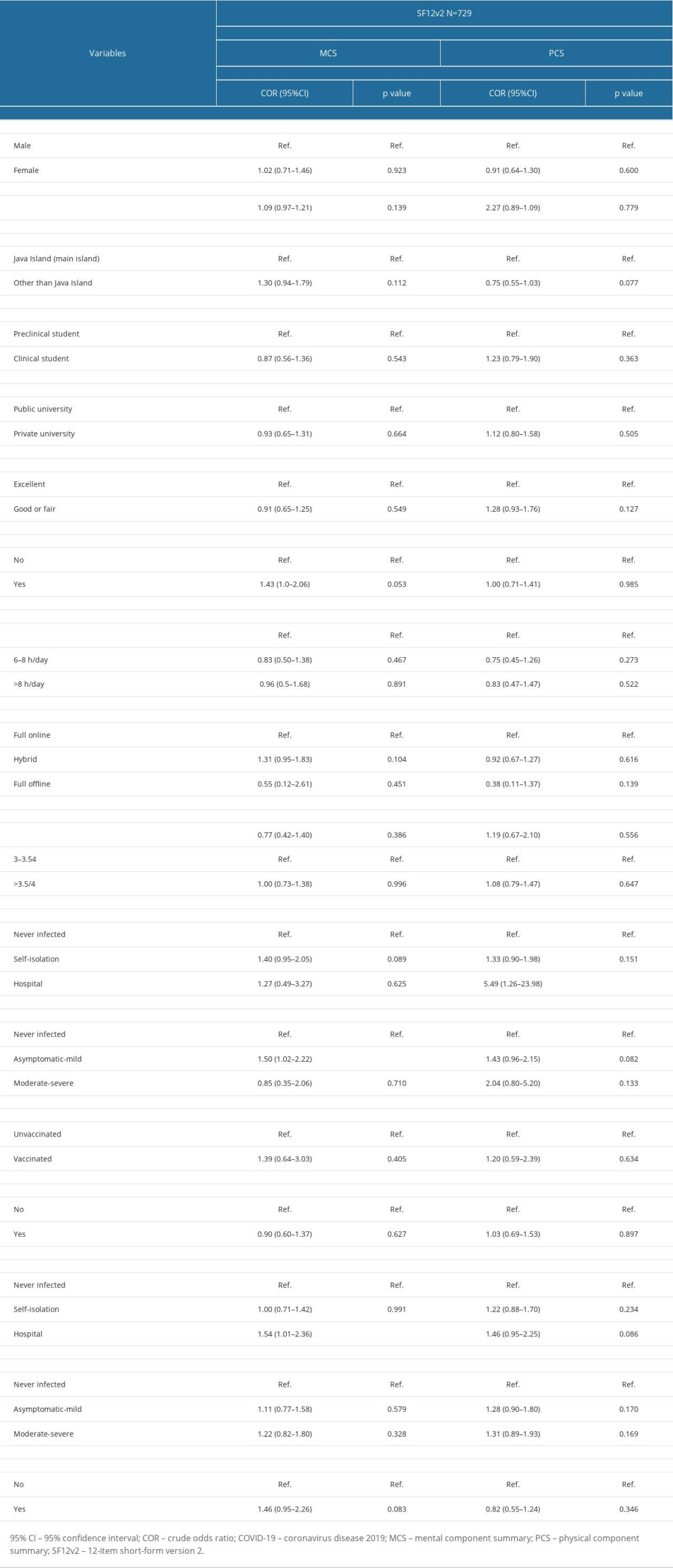 Table 2. Univariate logistic regression analysis for impaired health-related quality of life.
Table 2. Univariate logistic regression analysis for impaired health-related quality of life.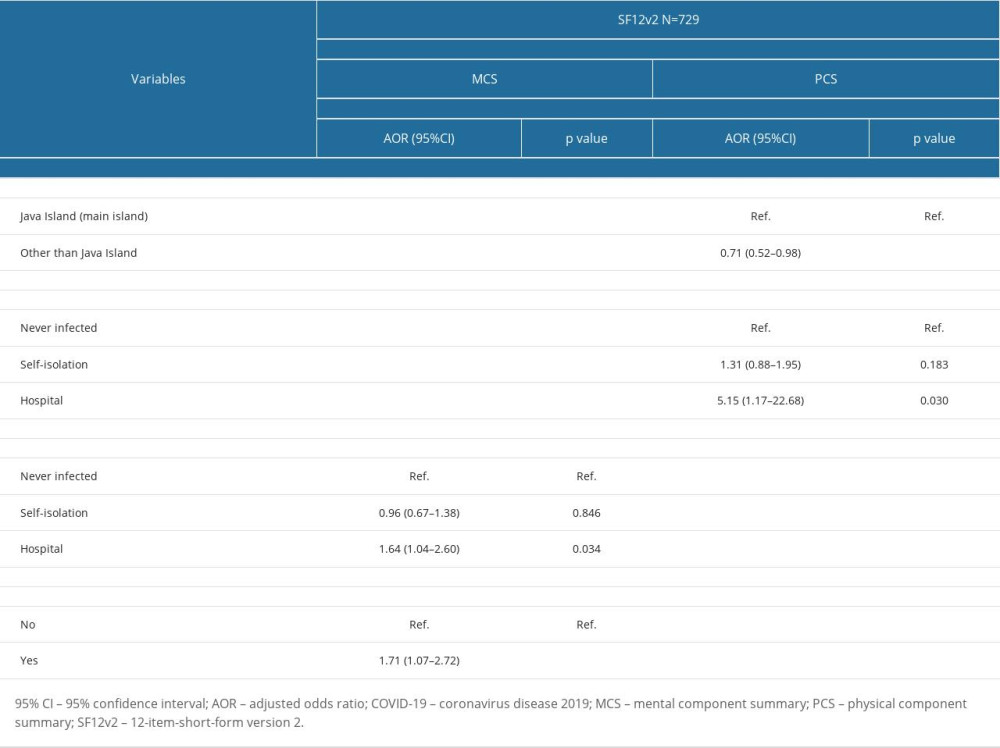 Table 3. Multivariate logistic regression analysis for impaired health-related quality of life.
Table 3. Multivariate logistic regression analysis for impaired health-related quality of life.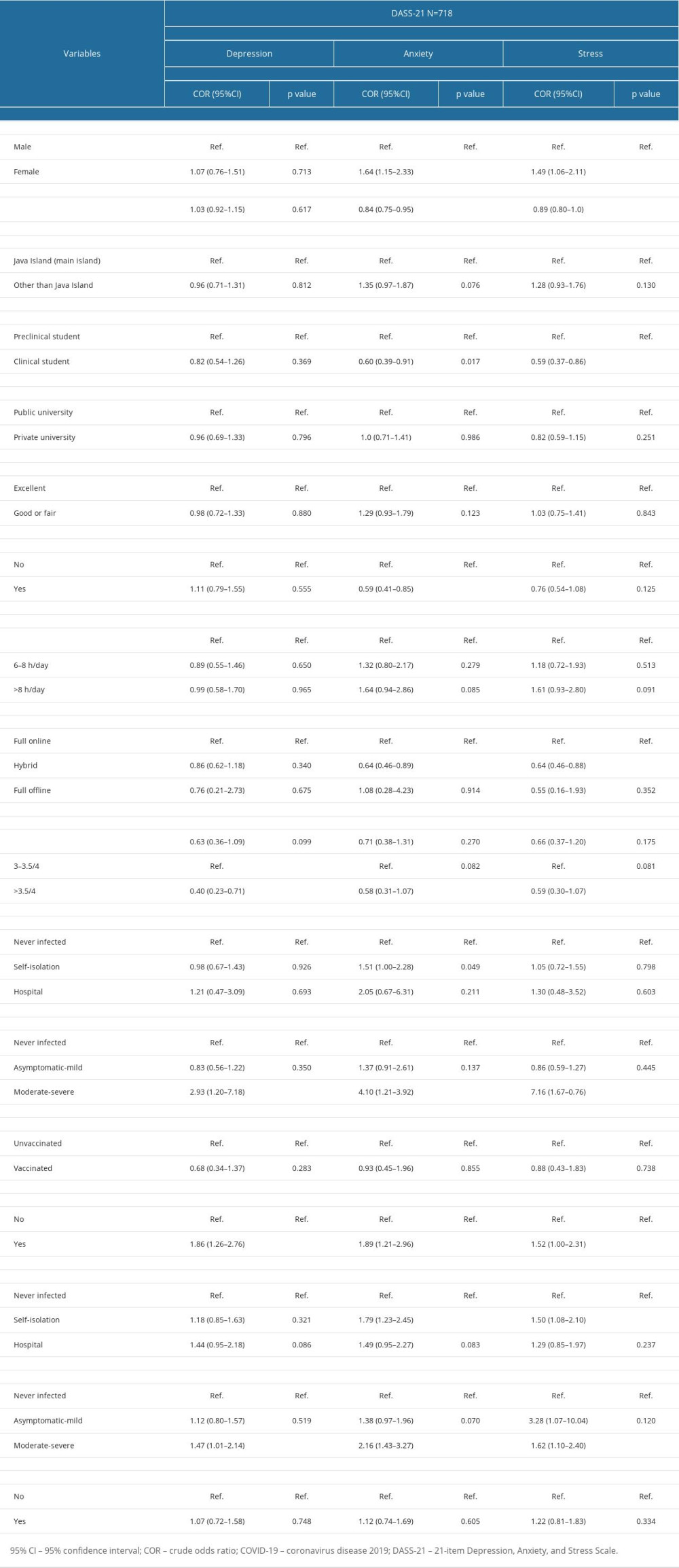 Table 4. Univariate logistic regression analysis for mental health problems.
Table 4. Univariate logistic regression analysis for mental health problems.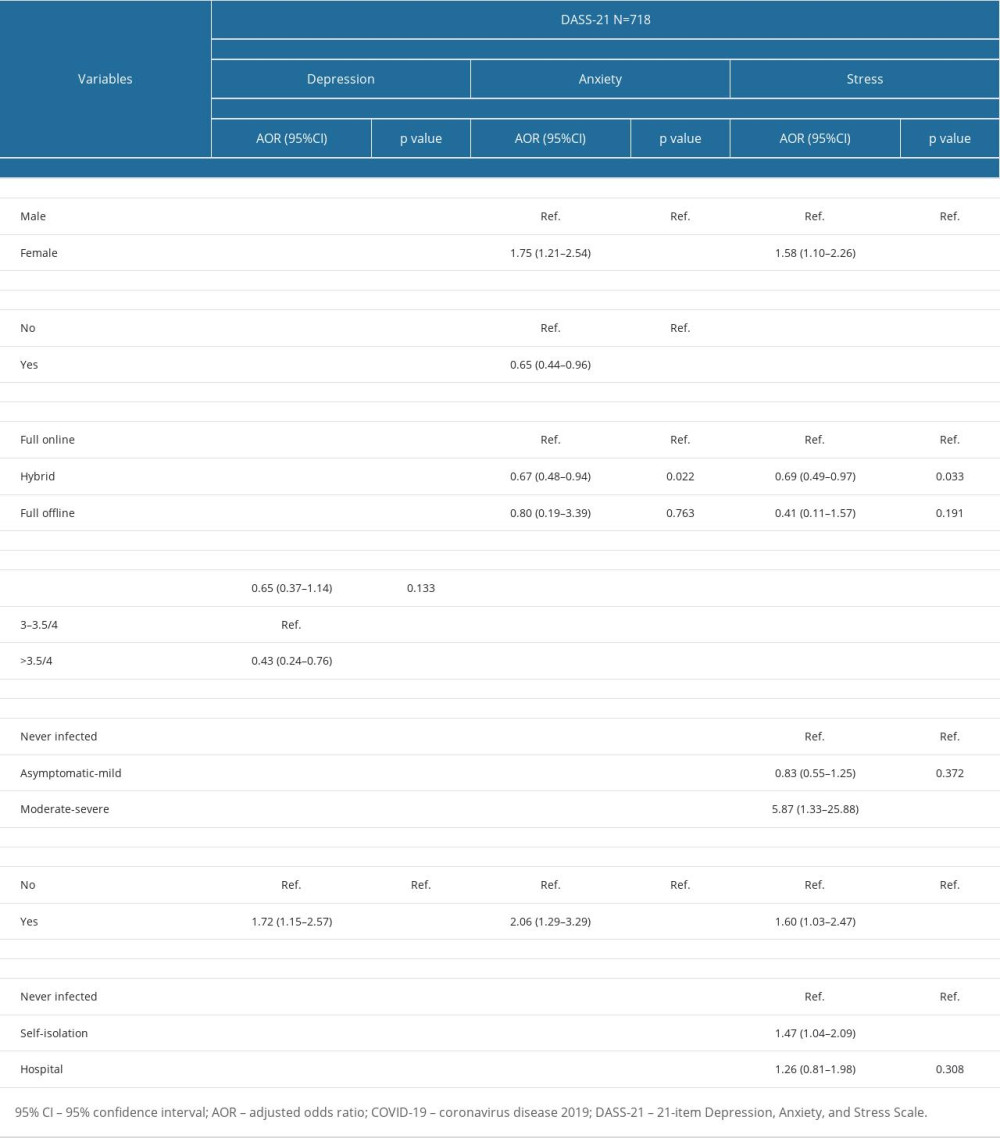 Table 5. Multivariate logistic regression analysis for mental health problems.
Table 5. Multivariate logistic regression analysis for mental health problems.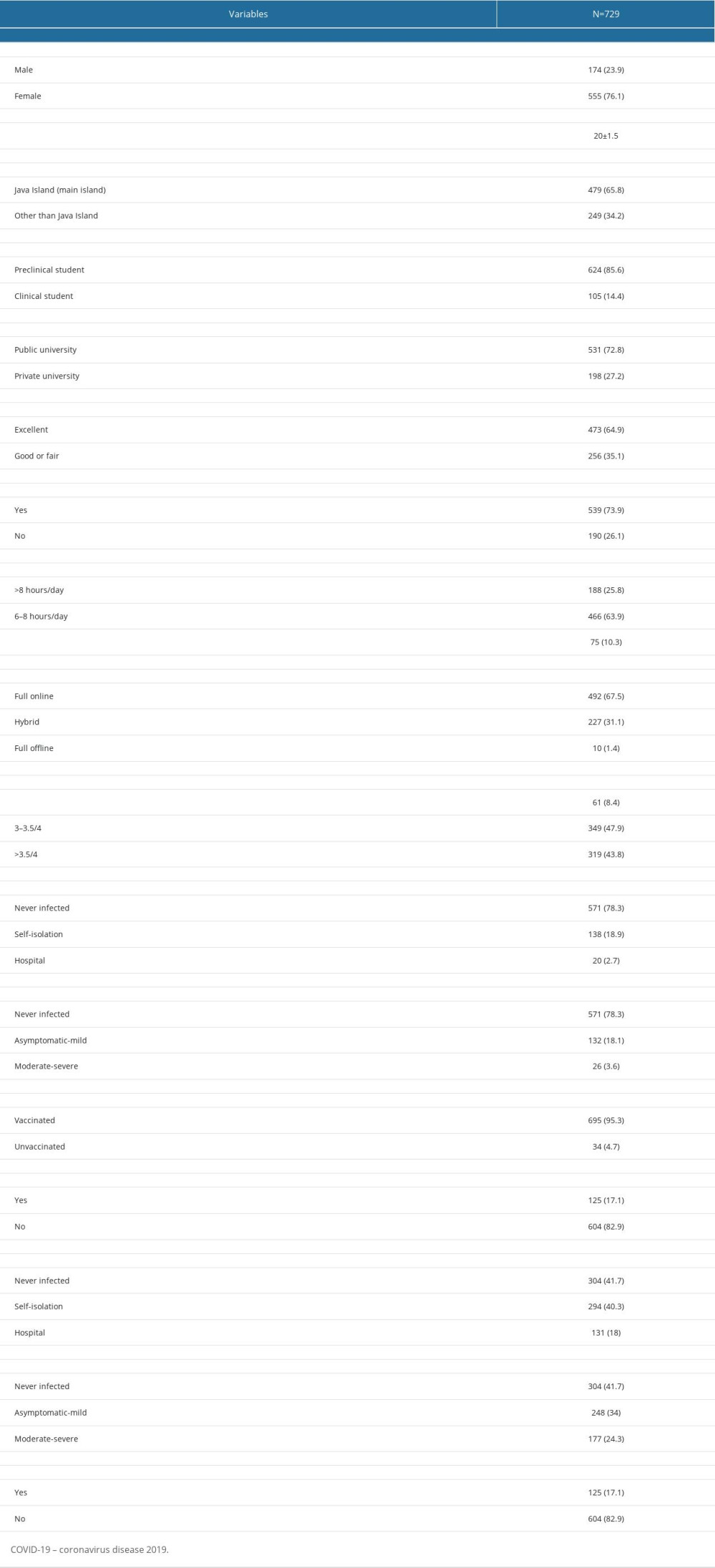 Table 1. Characteristics of the study participants.
Table 1. Characteristics of the study participants.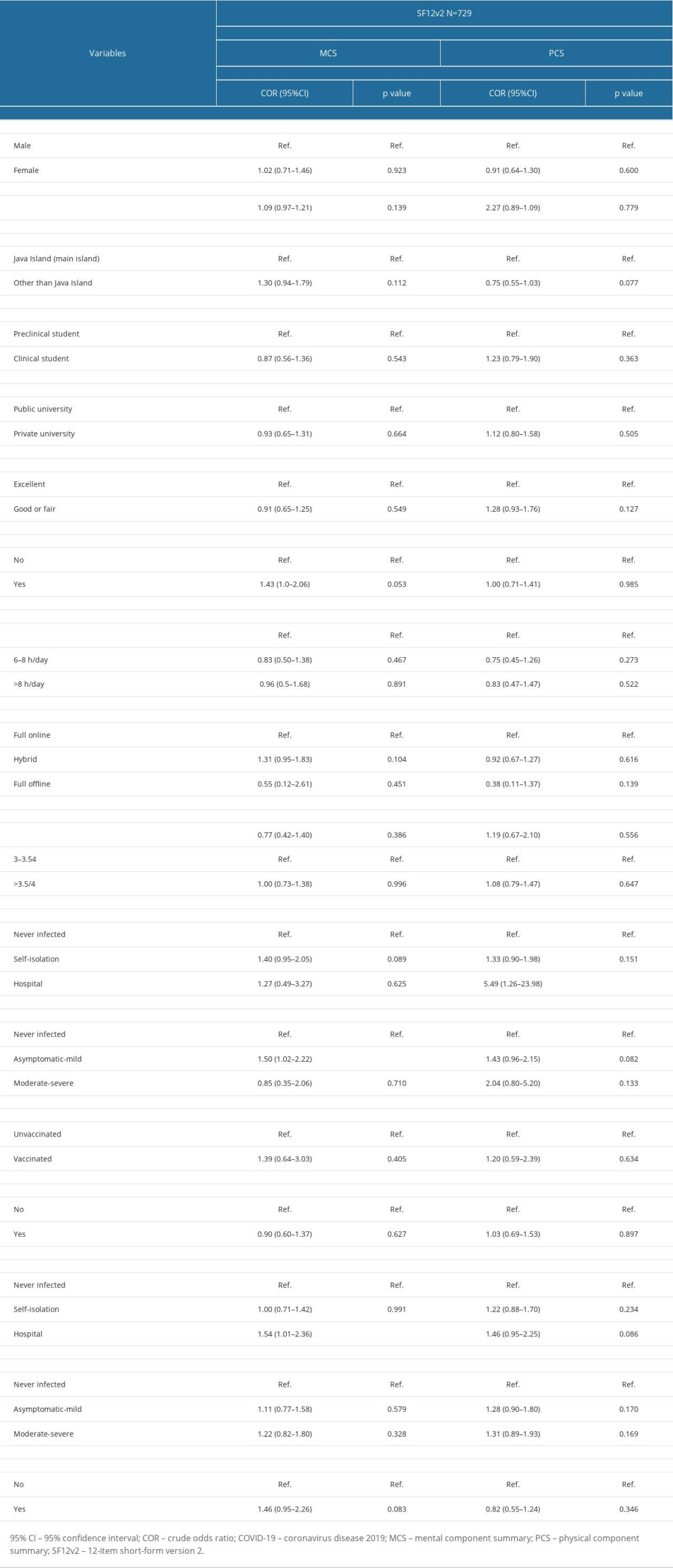 Table 2. Univariate logistic regression analysis for impaired health-related quality of life.
Table 2. Univariate logistic regression analysis for impaired health-related quality of life.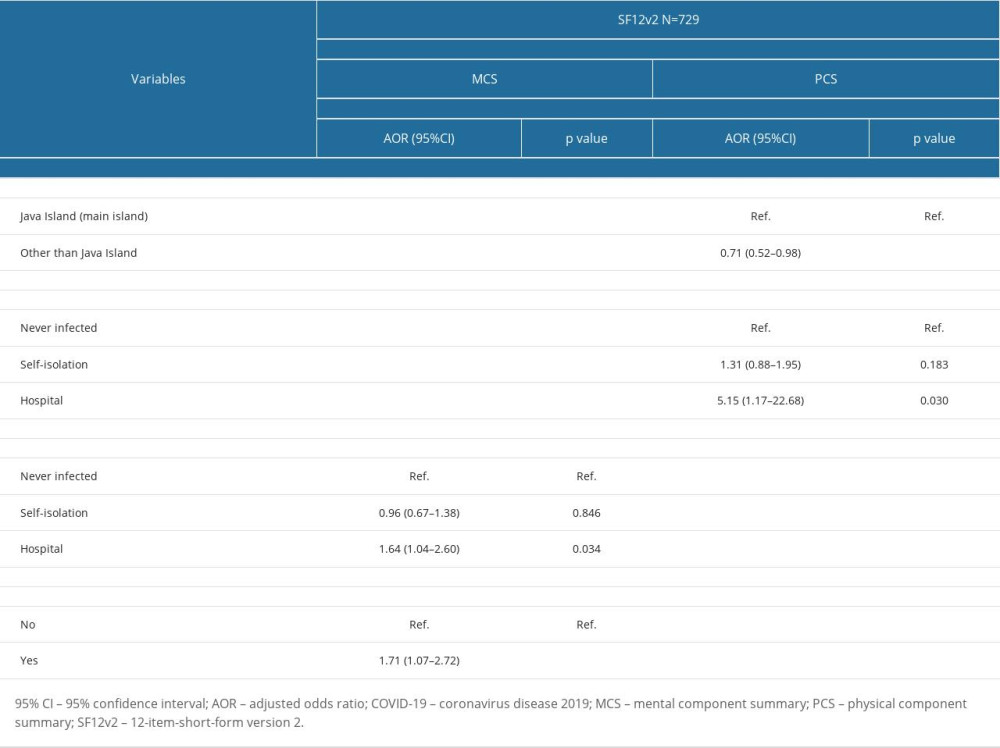 Table 3. Multivariate logistic regression analysis for impaired health-related quality of life.
Table 3. Multivariate logistic regression analysis for impaired health-related quality of life.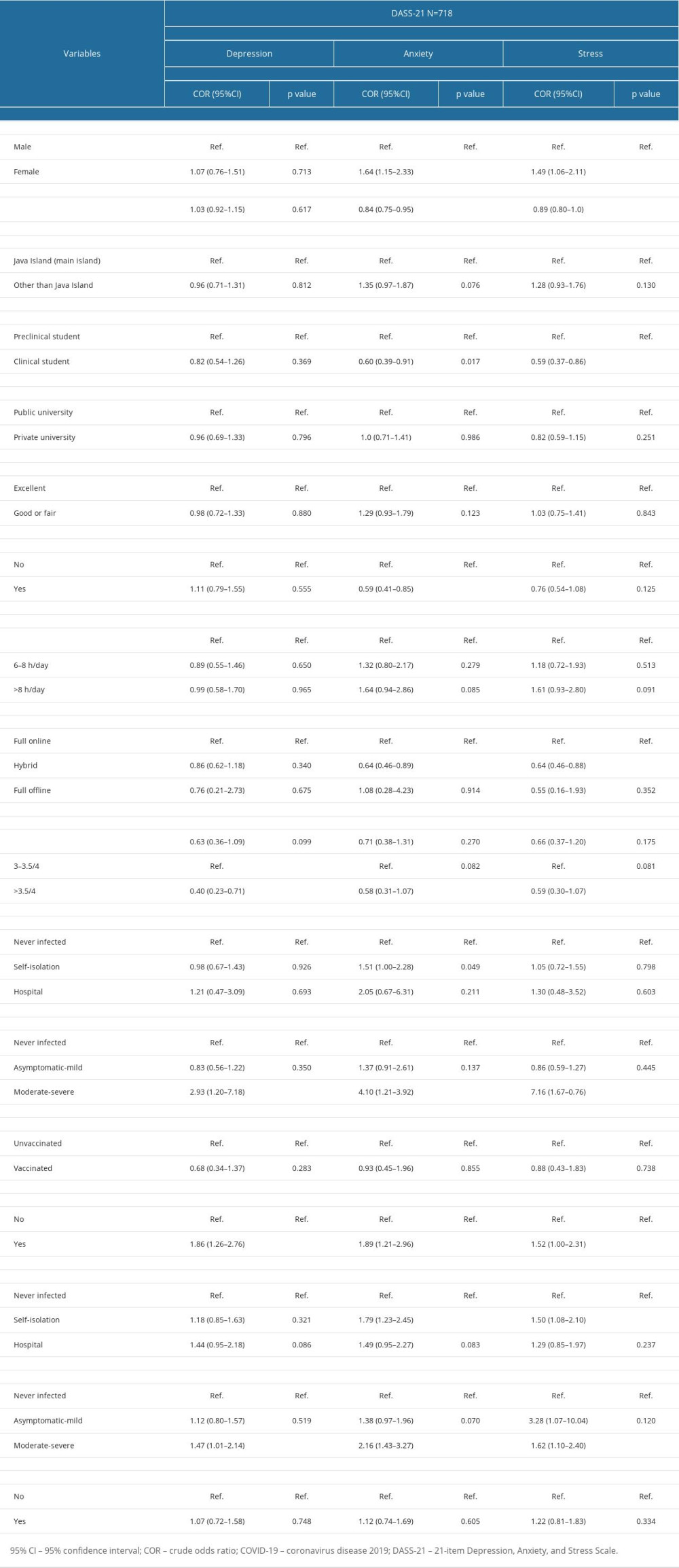 Table 4. Univariate logistic regression analysis for mental health problems.
Table 4. Univariate logistic regression analysis for mental health problems.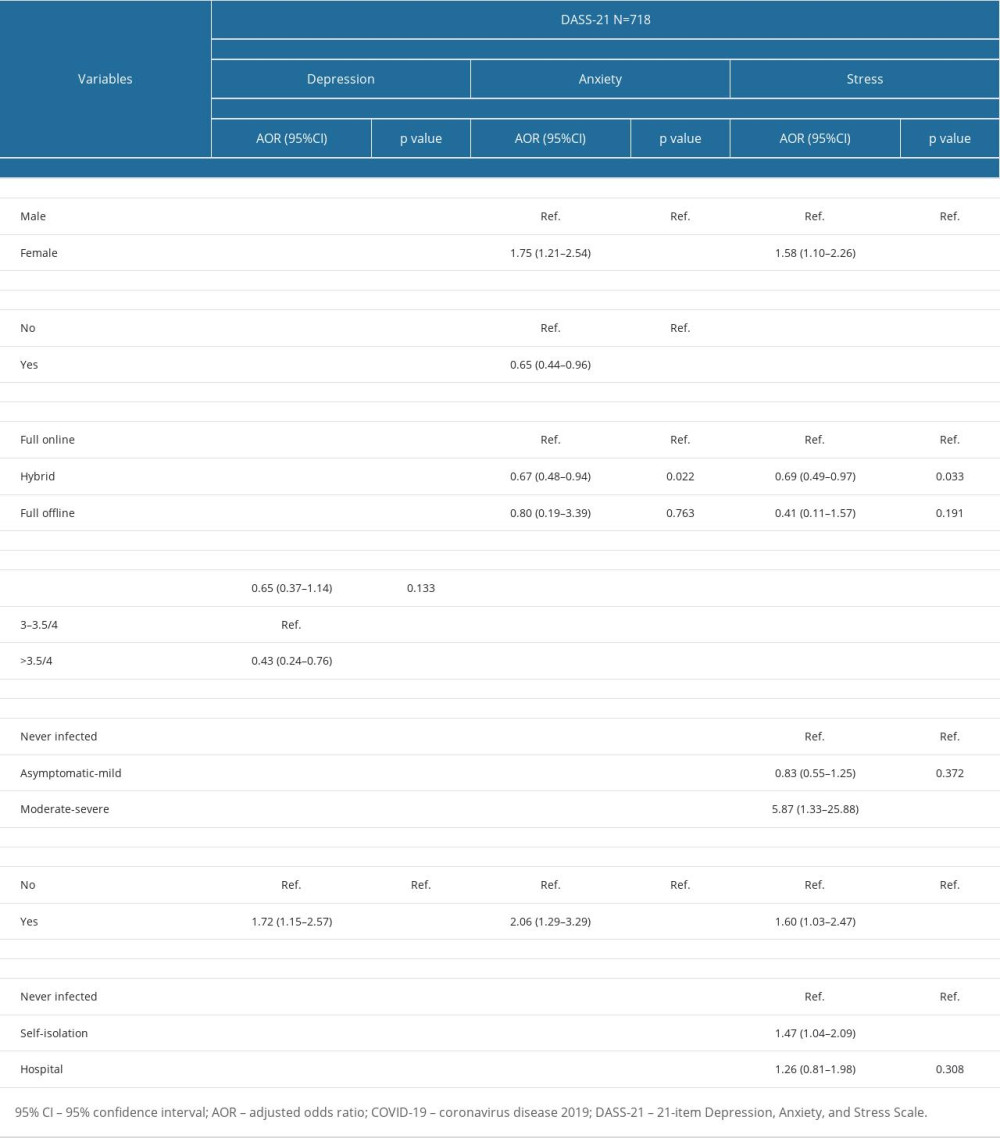 Table 5. Multivariate logistic regression analysis for mental health problems.
Table 5. Multivariate logistic regression analysis for mental health problems. In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952


