18 December 2023: Clinical Research
Enhanced Pain Relief and Function Improvement in Children with Osgood-Schlatter Disease: Leukocyte-Rich Platelet-Rich Plasma (LR-PRP) as a Complementary Treatment to Standard Conservative Therapy
Tomasz GuszczynDOI: 10.12659/MSM.941523
Med Sci Monit 2023; 29:e941523
Abstract
BACKGROUND: Osgood-Schlatter disease (OSD) causes pain and loss of function of the knee in growing children. This study aimed to evaluate pain and function of the knee joint in 152 growing children with chronic OSD before and after treatment with LR-PRP when used with standard conservative treatment.
MATERIAL AND METHODS: Treatment efficacy was evaluated using the VAS, Tegner, Lyshom, and KOOS scales. Patient satisfaction, post-surgery athletic performance, and X-ray assessment were also used to determine the success of the procedure.
RESULTS: We found that 75% of the subjects were satisfied with the results of the treatment, and 72% of the subjects returned to full physical activity. The analysis showed a significant decrease in the median VAS score after treatment compared to the pre-treatment score (P<0.05), and an increase in the median scores of the Tegner, Lysholm, and KOOS scales compared to the pre-treatment score (P<0.05; P<0.05; P<0.05, respectively). The results showed that the shorter the duration of the disease, the better the treatment results were received. Return to activity and patient satisfaction were highest in the study group previously rehabilitated.
CONCLUSIONS: LR-PRP injection of the tibial tuberosity in patients with chronic OSD with open growth cartilage is an effective and uncomplicated method. We did not observe any adverse effects, which suggests the relatively high safety of the procedure. The use of PRP in the earlier phase of the disease and additional rehabilitation before treatment significantly increases the effectiveness of treatment.
Keywords: osteochondrosis, platelet-rich plasma, Treatment Outcome
Background
Osgood-Schlatter disease (OSD) belongs to the group of sterile bone necrosis and is a common cause of knee pain during growth and musculoskeletal development [1]. The disease mainly affects boys between the ages of 10 and 15 and girls between the ages of 8 and 14 [1,2]. Risk factors for the development of OSD include being overweight, increased tension and significant strength of the quadriceps muscle of the thigh, and decreased flexibility of the muscles of the posterior group of the thigh [3].
Clinical manifestation of the disease consists of pain in the tibial tuberosity projection that worsens after physical activity, tenderness at the distal attachment of the patellar ligament, and pain while kneeling. These symptoms persist for 6 to 18 months [2,4,5]. The disease is self-limiting in most cases; however, the duration of persistence can be up to 2 years [6]. For this reason, OSD modifies or even completely excludes young athletes from physical activities.
Conservative treatment has been successful in acute cases of OSD and includes: physiotherapy, modification of physical activity, or the use of ice packs to reduce pain [6,7]. Surgical treatment has a high success rate but is reserved for patients who are found to have symptoms of the disease despite growth cartilage fusion [8,9].
Considering the above information, it seems important to look for alternative treatments to the existing therapies to enable a shorter recovery time and full physical activity. These will be addressed in particular to patients engaged in competitive sports as well as patients with a chronic form of the disease who are not eligible for surgical treatment.
OSD refers to pathological changes around the distal attachment of the patellar tendon, and this area is known as the enthesis. Increased incidence of injury in this area can lead to inflammation of the enthesis, known as enthesopathy. The enthesis is divided into 4 zones: tendon, non-calcified fibrocartilage, calcified fibrocartilage, and bone. According to a previous study on rats and mice, overexertion activities with eccentric contractions, similar to those responsible for inducing the OSD, increase the proportion of fibrocartilage in the enthesis [10,11].
Methods involving injecting the enthesis with substances containing potential therapeutic properties have become increasingly popular. The only B level of evidence literature for regenerative injection at the tibial tuberosity in OSD is of dextrose prolotherapy, first described by Topol et al in 2011 [12]. Subsequent studies using dextrose for OSD treatment were published by Nakase in 2020 [13] and Wu in 2022 [14]. These cited papers report good treatment outcomes with dextrose injections and a high rate of return to athletic activity without symptoms. Another treatment option based on stimulating regenerative processes, among others, is platelet-rich plasma (PRP) [15], which is a preparation with many platelets in a small volume of plasma [16]. The beneficial effects of PRP in tissue healing and regeneration are related to growth factors released in large quantities by platelets [17]. There are also reports of a strong stimulating effect of PRP on collagen synthesis [18]. Preliminary reports indicate the positive effect of PRP in the treatment of tendon pathology, patellar ligament tendinopathy, and shoulder epicondylar enthesopathy [19–21].
This study evaluated pain and function of the knee joint in 152 children with open growth cartilage with chronic OSD both before and after treatment with LR-PRP, when used along with standard conservative treatment. A particular group of patients with OSD, for which there is currently no effective and safe treatment, is the group of growing children with the chronic form of the disease. The chronic form of OSD leads to significant difficulties in children’s sports participation. In future studies, we will also perform similar experiments with the use of PRP in a group of patients with the acute form of OSD.
Material and Methods
PATIENTS AND STUDY DESIGN:
The study group consisted of 152 patients (45 girls, 107 boys) who arrived with pain symptoms in the knee area at the Department of Orthopedics and Traumatology of the Children’s Clinical Hospital in Białystok. Osgood-Schlatter disease was diagnosed in all patients. The inclusion criteria for our study required the patient to be diagnosed with OSD for a minimum of 12 months. The diagnosis was made by noting a history of reduced sports activity due to pain in the tibial tuberosity region. Clinical examination revealed pain, swelling, and/or hypertrophy in the tibial tuberosity area. Radiographic imaging showed enlargement of the tibial tuberosity outline and/or loose bone fragments at the patellar ligament attachment site. Exclusion criteria included prior knee injuries and other knee joint conditions, concurrent medical conditions, especially rheumatologic and endocrinologic disorders, and use of non-steroidal anti-inflammatory drugs within the last 14 days.
PRP PREPARATION:
A total of 40 ml of venous blood was collected from the patient to obtain the PRP preparation. The blood was collected from the elbow vein and was centrifuged in a syringe containing 1 ml of anticoagulant - sodium citrate (S-Monovette; 10ml 9NC: 0.106 mol/l). Blood samples were centrifuged once at 3000 rpm for 10 min at room temperature. In this way, a supernatant is obtained, where the upper layer is platelet-poor plasma and the lower layer is platelet-rich plasma (PRP). In this way, we obtained about 2.5–3 ml of PRP final preparation. The PRP preparation meets the criteria for LR-PRP. The median PLT count per cubic millimeter was 850.4±348 and 215.8±84 for PRP and venous blood (VB). The median WBC concentration per cubic millimeter was 10.7±5.5 and 5.8±1.5 for PRP and VB. All procedures were performed under sterile conditions.
TREATMENT:
The knee was injected in the supine position. The PRP preparation was injected into the tibial tuberosity area in a volume of about 1–1.5 ml. The injection site was prepared in advance and the surface anesthetized with ethyl chloride so as not to dilute the PRP preparation. The needle was inserted into the area of the tibial tuberosity indicated by the patient as the point of maximum tenderness. The needle was advanced until it encountered resistance from the bone, and the PRP was deposited. According to the assumption that fibrocartilage tissue is responsible for the symptoms of OSD, the PRP preparation was administered in its vicinity. Before and during treatment, the patients did not use NSAID medications. The knee was immobilized in a brace with approximately 15 degrees of flexion for 2 weeks with a ban on sports activities for a total of 6 weeks after the injection. After removal of the orthosis, patients were able to walk without restriction and gradually increase their exertion, from swimming in the pool to cycling. After 6 weeks, the patient was allowed to return to athletic activities. Usually this was a one-time procedure; unless the result obtained was unsatisfactory, the patient’s knee was re-injected at the earliest 3 months after the previous procedure.
DATA COLLECTION:
The general characteristics of the patients, such as gender, age, knee, and duration of symptoms are shown in the table (Table 1). Evaluation of knee joint function in patients before PRP injection and after the observation period was performed using the following scales: Lysholm Knee Scoring scale (LKSS), Tegner Activity scale, and Knee Osteoarthritis Outcome Score (KOOS). The LKSS is used to assess knee function and is based on the patient’s subjective assessment of their limitations in daily activities [22]. LKSS consists of 8 items, with each question response being assigned an arbitrary score on an increasing scale – The Tegner Activity scale, which is a self-administered patient-reported measure that describes the level of work- and sports-based activity. Tegner’s scale is classified as a numerical scale; the range of obtained values is from 0 (sick leave/pension due to knee problems) to 10 (playing competitive sports) [22,23]. The KOOS scale is based on 5 subscales: 1) Pain; 2) Other Symptoms; 3) Activities of Daily Living (ADL); 4) Sport and Recreational Functioning (Sport/Rec); and 5) Knee-related Quality of Life (QoL). Each of the 5 scales is rated from 0 (extreme knee problems) to 100 (no knee problems). The KOOS scale evaluates both short-term and long-term symptoms and function of the knee [24,25]. In addition, the degree of knee pain was assessed using the VAS Pain scale before PRP injection of the tibial tuberosity and after the follow-up period. The VAS scale is used to assess pain, with a range of 0 to 10, where 0 means no pain and 10 means the worst imaginable pain. The scale is based on the patient’s subjective assessment of that pain [26]. Data from all the tests used (Lysholm, Tegner, KOOS, and VAS) were obtained through the completion of the paper version in the presence of a physician. The observation period was an average of 40 months (min 24 months, max 81 months, S.D. 13.72). Patients filled out forms according to their feelings. Moreover, X-rays were taken before PRP injection and after the follow-up period. Before the PRP treatment, 22% of patients were treated with immobilization for 2 weeks, 62.5% of patients received drug treatment (NSAID) for 2 weeks, 60.5% of patients underwent physiotherapy for at least 6 weeks, and in 88% of patients conservative methods were used for at least 6 weeks. Our study was in accordance with the protocol. A total of 152 patients who adhered to the recommendations were included in the study, none of whom had prematurely terminated treatment, and each patient’s course was completed according to the protocol.
STATISTICAL ANALYSIS:
After evaluating the normality of the distribution for the parameters studied with the Shapiro-Wilk test, which revealed significant deviations from normal distribution, we performed statistical analysis using non-parametric tests. We used the chi-square test to evaluate statistical differences between groups. We assessed correlations between the scales studied using the Spearman rank-sum test. The comparison of the results of the knee pain and function scales (VAS, Lysholm, Tegner, and KOOS) before and after treatment was conducted using the Wilcoxon test for paired data. The evaluation of the influence of individual parameters on the final results of the analyzed scales after the completed treatment was assessed by multivariate linear regression models.
Results
SATISFACTION WITH TREATMENT AND RETURN TO ACTIVITY:
We found that 75% of respondents were satisfied with the results obtained from the treatment procedure, and 72% of them returned to full physical activity. Of the 38 unsatisfied patients, 16 (10.5% of the total study group) opted for surgical treatment and underwent surgery after achieving growth cartilage fusion of the tibial tuberosity by arthroscopic bursoscopy.
RADIOLOGICAL EVALUATION:
We did not note any complications resulting from the treatment. Radiological images before and after treatment showed no changes (Figure 1). The injection did not cause any changes in the bone structure of the tibial tuberosity of the OSD.
EVALUATION OF KNEE PAIN AND FUNCTION USING SELECTED SCALES:
Analysis of VAS scale scores showed a significant reduction in the median score received after the procedure (1pct) compared to the score before PRP treatment (7 pct, P<0.05). Patients were evaluated for knee function using the Lysholm scale. The analysis showed a significant increase in the median score after treatment (95 points) compared to the score before treatment (84 points; P<0.05). In addition, scores using the Tegner scale were compared, showing a significant increase in the median score after PRP injection (6 points) compared to the pre-treatment score (5 points; P<0.05). Scores based on the KOOS scale before PRP injection also showed a statistically significant increase in value (97 points), compared to pre-treatment scores (83 points; P<0.05). The results obtained by comparing the scales are shown in Table 2.
The minimally clinically important difference (MCID) of VAS, based on data from adult rheumatology populations, has been suggested to be a reduction by 1.37 [27]. In our study, the minimal clinically important difference (MCID) for the VAS scale above 2 points was achieved by 95% of patients. The MCID values for the Lysholm, KOOS, and Tegner scales in knee pathology were assessed by Qiao and are as follows: for the Lysholm scale, MCID=11.1; for the KOOS scale, MCID=10.0; and for the Tegner scale, MCID=0.9 [28]. Referring to the above data, in our study, MCID for the Lysholm scale >11.1 points was achieved by 44.1% of patients, MCID for the KOOS scale >10 points was achieved by 49.3%, and MCID >0.9 points for the Tegner scale was achieved by 59.9% of patients.
LINEAR REGRESSION ANALYSIS:
We subjected the VAS, Tegner, Lysholm, and KOOS scores obtained after PRP injection to a linear regression model. The data obtained clearly show that the score of each scale after PRP injection is affected by the duration of symptoms. A longer duration of symptoms means that the scale score is worse by 0.02 points on the Tegner scale, 0.2 points on the Lysholm scale, 0.3 points on the KOOS scale, and 0.05 points on the VAS scale. The results of the linear regression model after stepwise elimination are shown in Table 3.
The results of the scales we evaluated, subjected to linear regression, showed that immobilization as a form of conservative treatment prior to injection treatment also has a significant impact on the final outcome. Immobilization of the limb before PRP injection decreased the Tegner scale score by 0.350 points, decreased the Lysholm scale score by 1.5 points, decreased the KOOS scale score by 3.3 points, and decreased the VAS scale score by about 1 point. The results we obtained are shown in Table 4.
CONSERVATIVE TREATMENT EFFECTS ON PRP INJECTION OUTCOMES:
In our study, we attempted to assess whether the final effect of PRP injection is influenced by the conservative treatment used previously. We considered the following as conservative treatment: immobilization, rehabilitation, cessation of physical activity, use of NSAIDs, and comparison of the results of the scales to the results of the scales obtained from patients with no prior treatment.
Our study showed that patients who received prior conservative treatment had relatively more better scale values than those who received no treatment. Patients who had been rehabilitated before PRP injection showed significantly better Tegner scale (P=0.004*), Lysholm scale (P<0.05*), KOOS scale (P<0.05*) and VAS scale (P<0.05*) values after PRP injection compared to non-rehabilitated patients. There was a similar favorable effect of activity cessation on the outcome of scales after PRP injection; however, these changes were not statistically significant. Interestingly, we found that immobilization of the limb before PRP injection has an adverse effect on the treatment effect. The values of the Tegner (P=0.028*), Lysholm (P=0.011*), and KOOS (P<0.05*) scales were significantly lower in patients with an immobilized limb before PRP injection compared to patients who did not receive this type of conservative treatment. In addition, VAS scale values were significantly better (P=0.003*) after PRP injection in patients who were not immobilized compared to those who received limb immobilization. All the results obtained are shown in Figure 2.
The above results suggest that an important issue that significantly affects the outcome of treatment with PRP injection is the conservative treatment used previously. In Table 5, we have included the data we obtained on the satisfaction and percentage of return to full physical activity of patients we treated with PRP injection, depending on the type of treatment before the procedure.
More than 89% of those previously rehabilitated patients returned to full physical activity, and these individuals also showed significantly higher treatment satisfaction (95.7%). Similar but lower values for return to activity (77.9%) and satisfaction with treatment (81.1%) were found in patients who were advised to stop activity before PRP injection. Interestingly, the lack of any treatment prior to PRP injection and the use of immobilization significantly lowered the percentage of patients who returned to full physical activity and their degree of satisfaction.
Discussion
Osgood-Schlatter disease mainly affects highly physically active children 8–15 years, especially those doing intensive sports training [1,29]. As a result of chronic overload, numerous micro-injuries to the tibial tuberosity area occur, contributing to inflammation and pain in the tibial tuberosity area [1,30].
OSD is a serious problem due to the children’s long cessation of physical activity. It affects young people who associate their future with sports. For this reason, it seems important to find an effective therapy to allow children with open growth cartilage to return to training.
The purpose of our study was to evaluate the efficacy of PRP injections in skeletally immature children with a chronic form of Osgood-Schlatter disease that prevents sports activities.
The most important finding of the present study is that 75% of respondents were satisfied with the results obtained from the treatment procedure. In addition, 72% of them returned to full physical activity. Furthermore, the procedure can be safely performed in children with open growth cartilage without causing growth disturbances or changes in the X-ray images.
Rathleff et al [31] proposed a therapy including modification of physical activity, observation of pain intensity, gradual strengthening, and a return to sports paradigm, achieving successful results with this among OSD patients (80% of patients returned to full activity after 12 weeks and 90% after 12 months), with 16% of subjects returning to sports after 12 weeks and 67% after 6 months. Krause et al [32] reported that 90% of patients with OSD treated with conservative methods had full recovery of symptoms within about 1 year, although decreased strength levels and functional deficits can persist over time. Considering that OSD is an 80–90% self-limiting condition, resolving spontaneously after cessation of physical activity within 12 months of diagnosis, achieving good therapeutic results in 80–90% of cases does not indicate successful treatment.
In contrast to the data listed above, our study included patients with disease symptoms lasting for at least 12 months, averaging 2.5 years, in whom previous treatment had not had the desired effect. Conservative methods were used in 88% of patients, physiotherapy in 60.5% of patients, drug treatment in 62.5% of patients, and immobilization (minimum 2 weeks) in 22% of patients. Each patient included in the study underwent an X-ray examination, which showed defragmentation of the tuberosity or formation of a free fragment, further confirming the chronic course of the condition. At the time of qualifying for the study, the disease had required patients to completely stop engaging in their previous sports. Six weeks after the PRP injection, 72% of the study patients returned to full activity, and the effect was long-lasting, with follow-up averaging 40 months.
The treatment method for patients with chronic OSD, when conservative methods are ineffective, is surgical treatment [9,30]. The effectiveness of surgical treatment in adults was a 75% return to preoperative levels of sports activity in the 2009 Pihlajamaki et al [8] study and the 2007 Weiss et al [33] study, and 91% complete resolution of problems in the 2010 El-Husseini et al [34] study.
Unfortunately, all of these methods carry the risk of growth disorders of the tibial tuberosity and are therefore not recommended for the treatment of OSD in children with open growth cartilage [32], who were the patients included in our study. The effectiveness of PRP injection can be compared to that of surgery in adults.
In our study group, PRP injections did not cause any change in X-ray images taken 1 year after injection. In addition, we found no significant complications in patients, only discomfort and pain reported during the injection and in the first hour after the procedure. The above data suggest that injecting PRP preparations into patients with chronic OSD may be an alternative treatment option. Most importantly, PRP preparations can be used during the intensive growth period, a time when surgical treatment is not recommended, and can protect patients from the need for surgical treatment in the future. This result confirms the safety of using PRP in patients with open growth cartilages, as it does not affect their premature overgrowth. Surgical treatment, on the other hand, carries the risk of complications such as sensory disturbances in the scar area, postoperative wound infections, wound gaping, and knee stiffness [35].
In 2011, the use of hyperosmolar dextrose solution in young athletes with recurrent OSD was first described [12]. Topol et al [12] described the effects of administering a double-blind injection of 1% lidocaine solution with or without 12.5% dextrose to 65 knees. The authors suggested that the time to return to activity as well as the duration of symptoms may be shorter for patients injected with dextrose solution compared to those treated with lidocaine injection, or usual care in those with OSD. An important conclusion drawn from the study by Topol et al [12] is that the return to sports within a 1-year observation period for patients treated with dextrose was 84%. This result is better than what we achieved in our study (72%). However, this difference could be attributed to the fact that PRP was administered only once, while dextrose was administered 3 times. Notable distinctions between these studies include a significantly larger study group (152 for PRP compared to 54 for dextrose). Additionally, the observation period in our study was over 3 times longer. Another advantage of the Topol study, as well as subsequent studies using dextrose, is the presence of a control group [12]. In contrast, a subsequent study on the efficacy of dextrose in OSD by Nakase et al [13] did not confirm its superiority over lignocaine. However, it is worth noting that the study by Nakase et al [13] is marred by an error arising from comparative analysis between groups based on raw scores rather than score changes. If the analysis had been conducted correctly, the changes in VISA-P scores would have been 27 points for dextrose and 19.8 for saline. Further support for the effectiveness of dextrose treatment is also provided by a study published by Wu et al [14]. This double-blind randomized controlled trial from 2022 indicates significantly better outcomes after dextrose administration compared to saline administration [14]. The mechanism of action, safety, and efficacy of dextrose prolotherapy is well established in the current literature [36]. It is hypothesized that this method of intentional small-scale “therapeutic trauma” at the injection site initiates the body’s wound healing cascade of inflammation, extracellular matrix (ECM) formation, and remodeling [37,38].
Analyzing the pathophysiology of OSD, it seems reasonable to look for preparations that will not only modulate the inflammatory process, but also stimulate the processes of remodeling, collagen biosynthesis, and remodeling of the extracellular matrix. Such preparations include leukocyte-rich platelet-rich plasma (LR-PRP), which has anabolic effects due to platelet-derived cytokines, primarily peptide patterning factors, but also exhibits pro-inflammatory effects due to catabolic cytokines such as IL-1beta, TNF-alpha, and metalloproteinases. In addition, Zhi-Hao et al [39] and Ke Xie et al [40] in their studies suggest that PRP improves angiogenesis and revascularization, which may promote healing of the chronic inflammation that takes place in OSD.
In vitro studies suggest that PRP activates a complex of growth factors and adhesion receptors that stimulate cell proliferation, migration, and collagen biosynthesis [18,41]. In addition, a recent systematic review and meta-analysis found that PRP injections were effective in treating symptomatic tendinopathy [42]. It also seems to be very important in treatment of the chronic form of OSD that LR-PRP preparations show an anti-inflammatory effect through COX-2 inhibition [43]. For these reasons, it seems reasonable to use PRP and especially LR-PRP in the treatment of chronic OSD.
Our study is the first to analyze the efficacy of LR-PRP in a homogeneous group of patients with a chronic form of the disease and with open growth cartilage with OSD. There are only 2 case reports in the literature on the use of PRP in patients with OSD [44].
In our study group, we found a statistically significant increase in physical activity, as measured by the Tegner scale, from 5 points to 6 points. The activity level of the patients was assessed twice: before the onset of disease symptoms and on the day of the end of the study. The study by Eun et al [45] also assessed physical activity using the Tegner scale, noting an increase in activity from 2.7 to 6.2. However, this study assessed the level of physical activity before surgery was performed, that is, during the course of the disease and 24 months after the treatment. The final result is identical to that obtained in our study.
Analyzing the results of the Lysholm and KOOS functional scales also showed a significant increase in values, from 84 to 95 and from 83 to 97 points, respectively. The leading symptom of OSD is pain in the tibial tuberosity cast, which modifies the patient’s activity level. Therefore, the greatest differences in studying the effectiveness of OSD treatment are obtained by comparing the pain reported before and after treatment. In our study, we evaluated the pain experienced during activity, considering it the most authoritative symptom of OSD. The decrease in pain on the VAS scale from 7 to 1, according to our results, is the most measurable indicator of the effectiveness of treatment with PRP preparations. Similar results of pain reduction on the VAS scale, from 6.5 to 0.9, were reported by Eun et al [45] as a result of bursoscopic ossicle excision.
Our statistical analyses showed that shorter duration of disease and earlier PRP injection were associated with better treatment results. A greater reduction in pain on the VAS scale and better efficiency in terms of return to sports activities were obtained. This suggests the possibility that patients with acute OSD can be treated very effectively with injection PRP, but this hypothesis requires further research.
Our study has some limitations, but they do not affect its merits. One limitation was the administration of a single injection, which suggests the need for studies that allow for repeated treatments as needed, preferably with the inclusion of a group treated with dextrose and a control group receiving saline injections. Secondly, only a group of patients with the chronic form of OSD was studied; in the future, we plan to expand our research to include a group of patients with the acute form of the disease.
Conclusions
LR-PRP injection of the tibial tuberosity in patients with chronic OSD with open growth cartilage is a well-tolerated, effective, and uncomplicated method. The elimination of pain in OSD in most patients allows a full return to athletic activities, making this treatment highly regarded by patients. The earlier this method is applied, the higher its effectiveness.
Figures
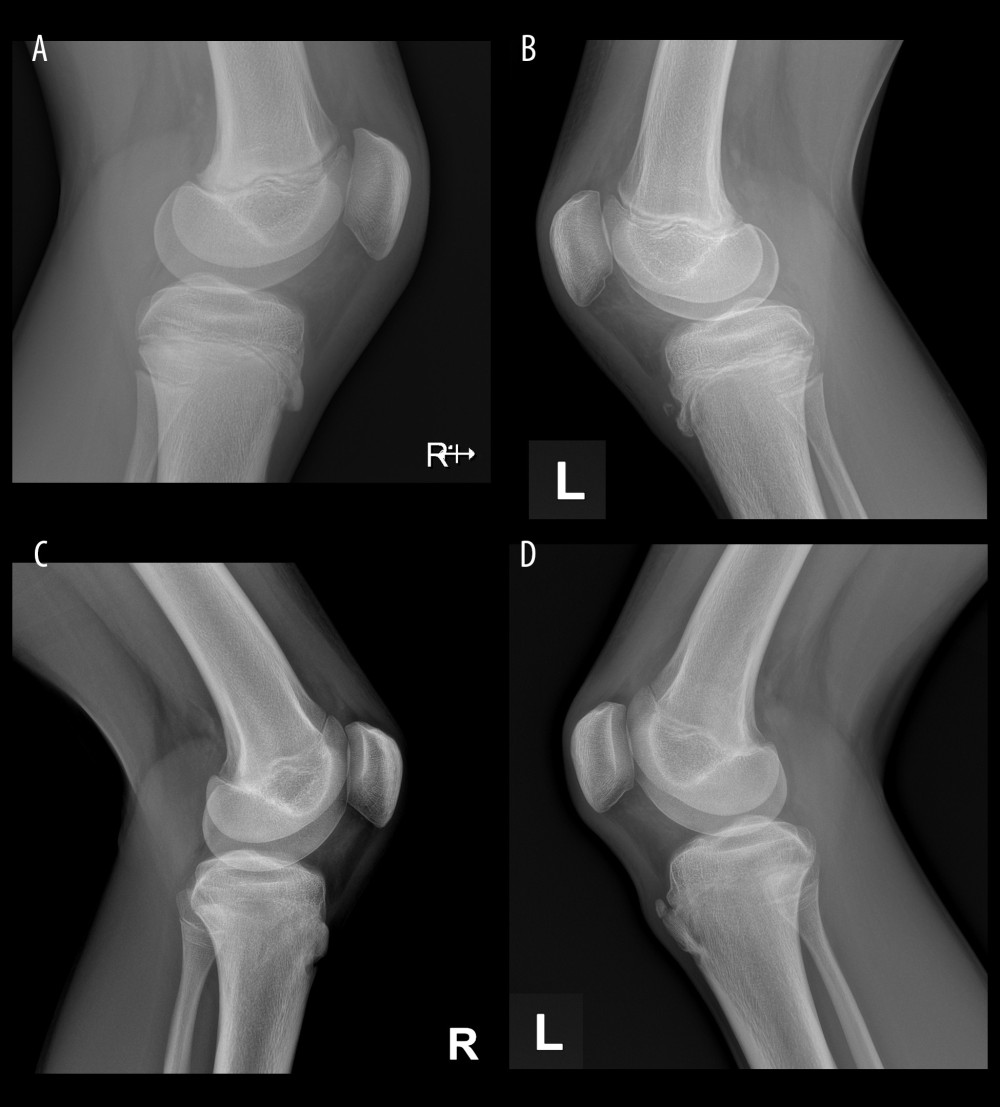 Figure 1. X-ray images belonging to the same patient: (A) healthy right knee; (B) left knee with separated bone fragment before PRP injection; (C) right knee after an observation period of 2 years; (D) left knee with separated bone fragment after PRP (Platelet-Rich Plasma) injection after observation period of 2 years.
Figure 1. X-ray images belonging to the same patient: (A) healthy right knee; (B) left knee with separated bone fragment before PRP injection; (C) right knee after an observation period of 2 years; (D) left knee with separated bone fragment after PRP (Platelet-Rich Plasma) injection after observation period of 2 years. 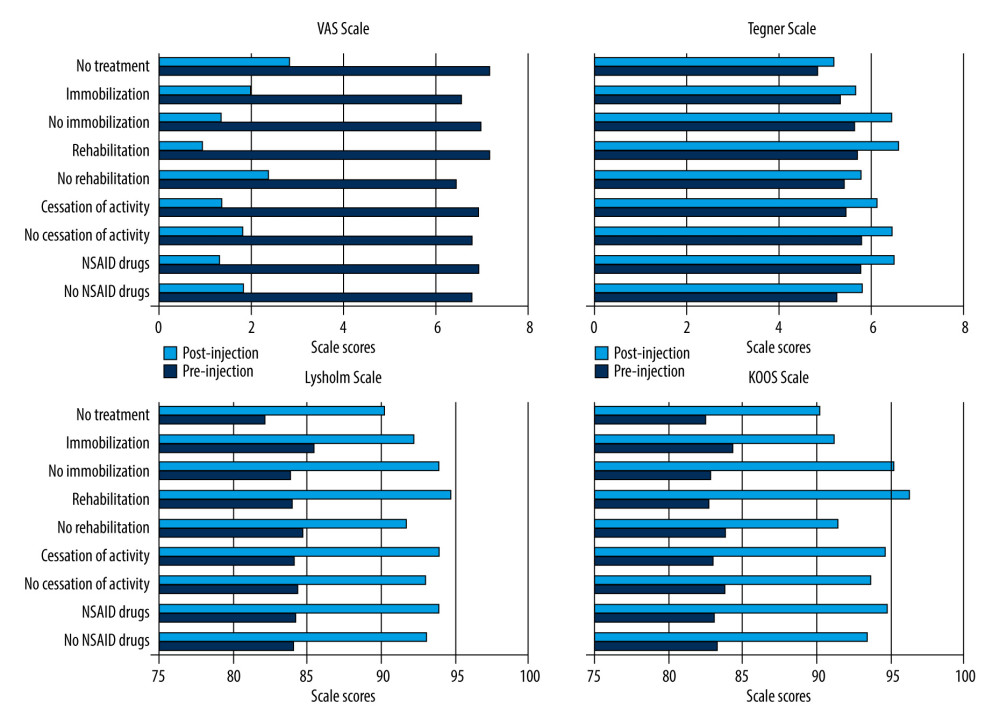 Figure 2. Comparison of the knee pain VAS (The Visual Analogue Scale) and function scales (Lysholm, Tegner, KOOS) scores according to the conservative treatment used.
Figure 2. Comparison of the knee pain VAS (The Visual Analogue Scale) and function scales (Lysholm, Tegner, KOOS) scores according to the conservative treatment used. Tables
Table 1. Patient characteristics.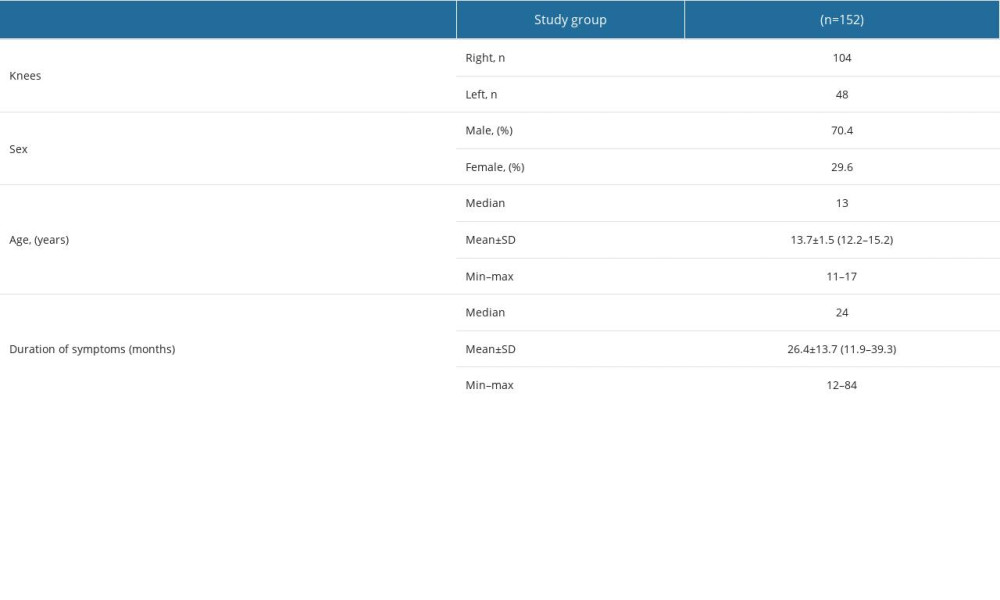 Table 2. The comparison of the results of the knee pain and function scales (VAS, Lysholm, Tegner, and KOOS) before and after PRP (Platelet-Rich Plasma) injection.
Table 2. The comparison of the results of the knee pain and function scales (VAS, Lysholm, Tegner, and KOOS) before and after PRP (Platelet-Rich Plasma) injection.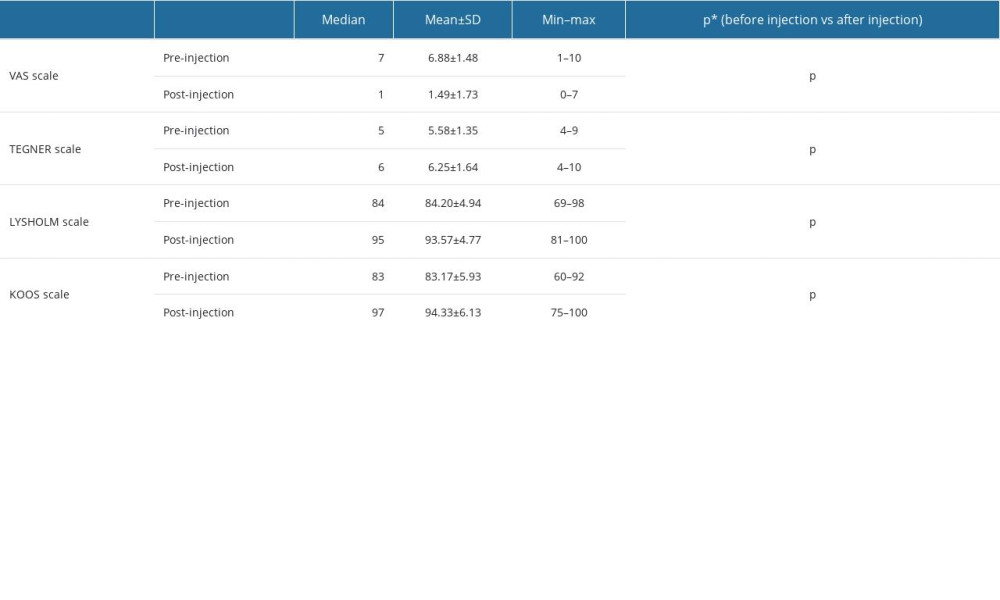 Table 3. The influence of the duration of symptoms on treatment outcomes: the results after PRP injection assessed on the pain scale (VAS) and knee joint function scales (Tegner, Lysholm, and KOOS) was evaluated using the linear regression model after stepwise elimination.
Table 3. The influence of the duration of symptoms on treatment outcomes: the results after PRP injection assessed on the pain scale (VAS) and knee joint function scales (Tegner, Lysholm, and KOOS) was evaluated using the linear regression model after stepwise elimination.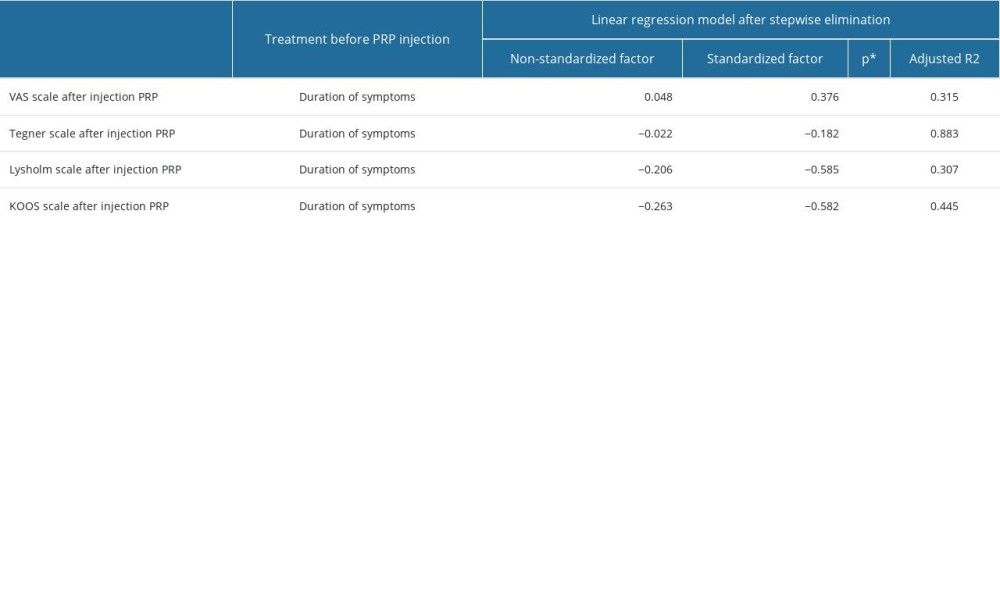 Table 4. The impact of limb immobilization prior to PRP injection on treatment outcomes: the results after PRP injection assessed on the pain scale (VAS) and knee joint function scales (Tegner, Lysholm, and KOOS), was evaluated using the linear regression model after stepwise elimination.
Table 4. The impact of limb immobilization prior to PRP injection on treatment outcomes: the results after PRP injection assessed on the pain scale (VAS) and knee joint function scales (Tegner, Lysholm, and KOOS), was evaluated using the linear regression model after stepwise elimination.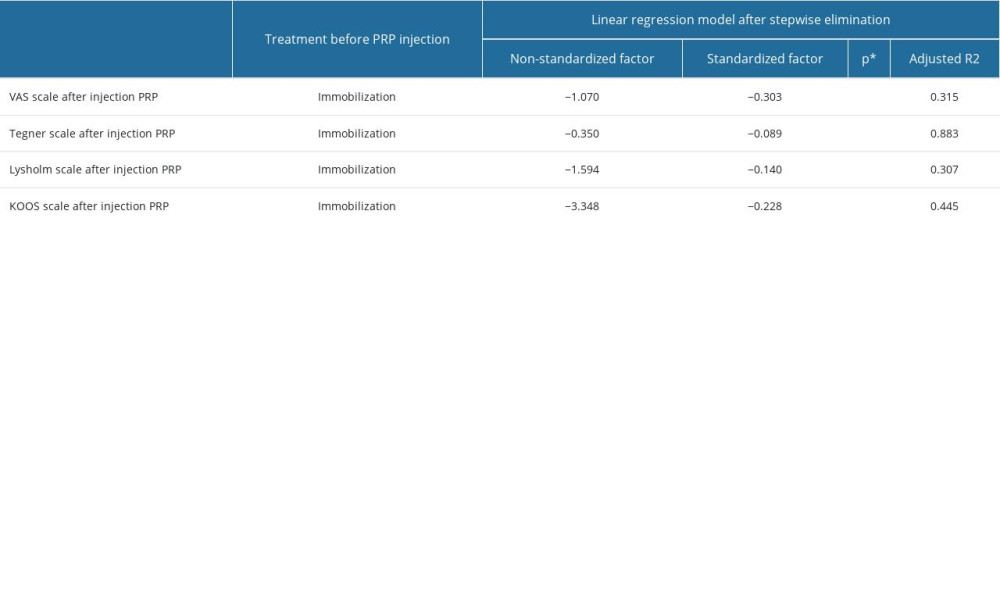 Table 5. Summary of patient satisfaction and return to activity according to treatment before PRP (Platelet-Rich Plasma) injection.
Table 5. Summary of patient satisfaction and return to activity according to treatment before PRP (Platelet-Rich Plasma) injection.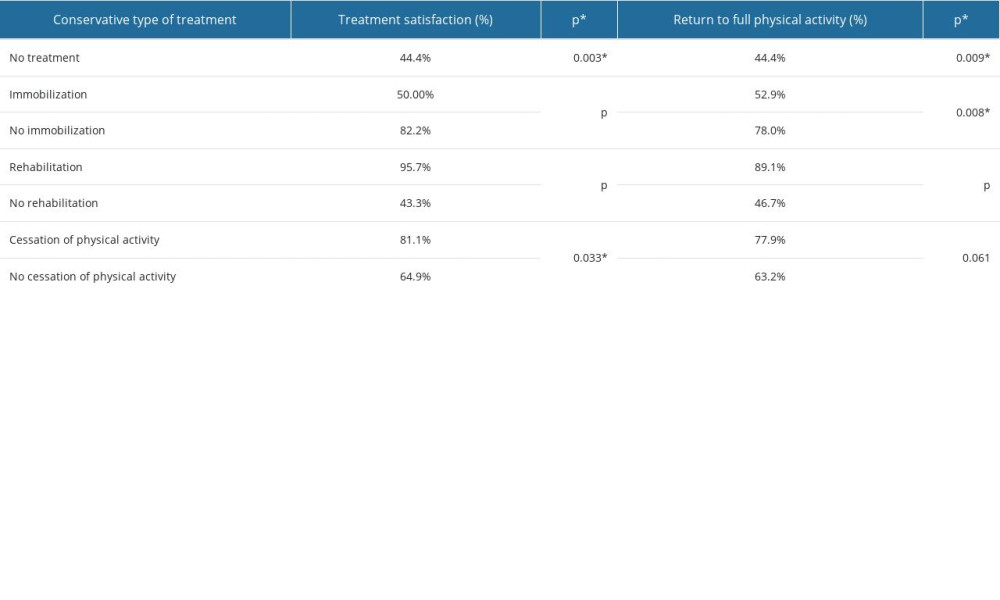
References
1. Gholve PA, Scher DM, Khakharia S, Osgood-Schlatter syndrome: Curr Opin Pediatr, 2007; 19; 44-50
2. Kamiya T, Teramoto A, Mori Y, Nano-arthroscopic ultrasound-guided excision of unresolved Osgood-Schlatter disease: Arthrosc Tech, 2021; 10; e1581-e87
3. Ladenhauf HN, Seitlinger G, Green DW, Osgood-Schlatter disease: A 2020 update of a common knee condition in children: Curr Opin Pediatr, 2020; 32; 107-12
4. Kaya DO, Toprak U, Baltaci G, Long-term functional and sonographic outcomes in Osgood-Schlatter disease: Knee Surg Sports Traumatol Arthrosc, 2013; 21; 1131-39
5. Bezuglov EN, Tikhonova AA, Chubarovskiy PV, Conservative treatment of Osgood-Schlatter disease among young professional soccer players: Int Orthop, 2020; 44; 1737-43
6. Bloom OJ, Mackler L, Barbee J, Clinical inquiries. What is the best treatment for Osgood-Schlatter disease?: J Fam Pract, 2004; 53; 153-56
7. Weiler R, Ingram M, Wolman ROsgood-Schlatter disease: Praxis (Bern 1994), 2011; 100(22); 1369-70 [in German]
8. Pihlajamäki HK, Mattila VM, Parviainen M, Long-term outcome after surgical treatment of unresolved Osgood-Schlatter disease in young men: J Bone Joint Surg Am, 2009; 91; 2350-58
9. Circi E, Atalay Y, Beyzadeoglu T, Treatment of Osgood-Schlatter disease: Review of the literature: Musculoskelet Surg, 2017; 101; 195-200
10. Ozone K, Kokubun T, Takahata K, Structural and pathological changes in the enthesis are influenced by the muscle contraction type during exercise: J Orthop Res, 2022; 40; 2076-88
11. Suito H, Fujikawa K, Ohsako M, Eccentric contractions during downhill running induce Osgood-Schlatter disease in the tibial tuberosity in rats: A focus on histological structures: Sci Rep, 2023; 13; 9863
12. Topol GA, Podesta LA, Reeves KD, Hyperosmolar dextrose injection for recalcitrant Osgood-Schlatter disease: Pediatrics, 2011; 128; e1121-e28
13. Nakase J, Oshima T, Takata Y, No superiority of dextrose injections over placebo injections for Osgood-Schlatter disease: A prospective randomized double-blind study: Arch Orthop Trauma Surg, 2020; 140; 197-202
14. Wu Z, Tu X, Tu Z, Hyperosmolar dextrose injection for Osgood-Schlatter disease: A double-blind, randomized controlled trial: Arch Orthop Trauma Surg, 2022; 142; 2279-85
15. Shahid M, Kundra R, Platelet-rich plasma (PRP) for knee disorders: EFORT Open Rev, 2017; 2; 28-34
16. Wu PI, Diaz R, Borg-Stein J, Platelet-rich plasma: Phys Med Rehabil Clin N Am, 2016; 27(4); 825-53
17. Jain NK, Gulati M, Platelet-rich plasma: A healing virtuoso: Blood Res, 2016; 51; 3-5
18. Guszczyn T, Surażyński A, Zaręba I, Differential effect of platelet-rich plasma fractions on β1-integrin signaling, collagen biosynthesis, and prolidase activity in human skin fibroblasts: Drug Des Devel Ther, 2017; 11; 1849-57
19. Taylor DW, Petrera M, Hendry M, Theodoropoulos JS, A systematic review of the use of platelet-rich plasma in sports medicine as a new treatment for tendon and ligament injuries: Clin J Sport Med, 2011; 21; 344-52
20. Filardo G, Di Matteo B, Kon E, Platelet-rich plasma in tendon-related disorders: Results and indications: Knee Surg Sports Traumatol Arthrosc, 2018; 26; 1984-99
21. Fitzpatrick J, Bulsara M, Zheng MH, Effectiveness of platelet-rich plasma in the treatment of tendinopathy: Response: Am J Sports Med, 2016; 44; NP55-NP56
22. Briggs KK, Steadman JR, Hay CJ, Hines SL, Lysholm score and Tegner activity level in individuals with normal knees: Am J Sports Med, 2009; 37; 898-901
23. Huang H, Zhang S, Wang Y, Reliability and validity of a Chinese Version of the Lysholm Score and Tegner Activity Scale for knee arthroplasty: J Rehabil Med, 2022; 54; jrm00317
24. Collins NJ, Prinsen CA, Christensen R, Knee Injury and Osteoarthritis Outcome Score (KOOS): Systematic review and meta-analysis of measurement properties: Osteoarthritis Cartilage, 2016; 24; 1317-29
25. Kiadaliri A, Alava MH, Roos EM, Englund M, Mapping EQ-5D-3L from the Knee Injury and Osteoarthritis Outcome Score (KOOS): Qual Life Res, 2020; 29; 265-74
26. Akesen S, Akesen B, Atıcı T, Comparison of efficacy between the genicular nerve block and the popliteal artery and the capsule of the posterior knee (IPACK) block for total knee replacement surgery: A prospective randomized controlled study: Acta Orthop Traumatol Turc, 2021; 55; 134-40
27. Diep D, Chen KJQ, Kumbhare D, Ultrasound-guided interventional procedures for myofascial trigger points: A systematic review: Reg Anesth Pain Med, 2021; 46; 73-80
28. Qiao Y, Wu C, Wu X, The value of minimal clinically important difference, substantial clinical benefit, and patient-acceptable symptomatic state for commonly used patient-reported outcomes in recurrent patellar instability patients after MPFLR and TTT: Arthroscopy, 2023 [Online ahead of print]
29. Corbi F, Matas S, Álvarez-Herms J, Osgood-Schlatter disease: Appearance, diagnosis and treatment: A narrative review: Healthcare (Basel), 2022; 10; 1011
30. Lucenti L, Sapienza M, Caldaci A, The etiology and risk factors of Osgood-Schlatter disease: A systematic review: Children (Basel), 2022; 9; 826
31. Rathleff MS, Winiarski L, Krommes K, Activity Modification and knee strengthening for Osgood-Schlatter disease: A prospective cohort study: Orthop J Sports Med, 2020; 8; 2325967120911106
32. Krause BL, Williams JP, Catterall A, Natural history of Osgood-Schlatter disease: J Pediatr Orthop, 1990; 10; 65-68
33. Weiss JM, Jordan SS, Andersen JS, Surgical treatment of unresolved Osgood-Schlatter disease: Ossicle resection with tibial tubercleplasty: J Pediatr Orthop, 2007; 27; 844-47
34. El-Husseini TF, Abdelgawad AA, Results of surgical treatment of unresolved Osgood-Schlatter disease in adults: J Knee Surg, 2010; 23; 103-7
35. Trail IA, Tibial sequestrectomy in the management of Osgood-Schlatter disease: J Pediatr Orthop, 1988; 8; 554-57
36. Sanderson LM, Bryant A, Effectiveness and safety of prolotherapy injections for management of lower limb tendinopathy and fasciopathy: A systematic review: J Foot Ankle Res, 2015; 8; 57
37. Freeman JW, Empson YM, Ekwueme EC, Effect of prolotherapy on cellular proliferation and collagen deposition in MC3T3-E1 and patellar tendon fibroblast populations: Transl Res, 2011; 158; 132-39
38. Martins CA, Bertuzzi RT, Tisot RA, Dextrose prolotherapy and corticosteroid injection into rat Achilles tendon: Knee Surg Sports Traumatol Arthrosc, 2012; 20; 1895-900
39. Li Z-H, Wu G-F, Song H-Q, Artificial dermal scaffold loaded with platelet-rich plasma promotes wound healing in pigs by favoring angiogenesis: Med Sci Monit, 2022; 28; e936186
40. Xie K, Huang M, Zheng Y, Effect of antilogous platelet-rich plasma on the revascularization of rabbit prefabricated flap: Med Sci Monit, 2022; 28; e937718
41. Misiura M, Guszczyn T, Oscilowska I, Platelet-rich plasma promotes the proliferation of human keratinocytes via a progression of the cell cycle. A role of prolidase: Int J Mol Sci, 2021; 22; 936
42. Miller LE, Parrish WR, Roides B, Bhattacharyya S, Efficacy of platelet-rich plasma injections for symptomatic tendinopathy: Systematic review and meta-analysis of randomised injection-controlled trials: BMJ Open Sport Exerc Med, 2017; 3; e000237
43. Guszczyn T, Chalecka M, Kazberuk A, Platelet-rich plasma counteracts interleukin-1 induced inhibition of collagen biosynthesis through recovery of impaired β1-integrin signaling and prolidase activity in human skin fibroblasts: Acta Pol Pharm, 2022; 79; 497-508
44. Danneberg DJ, Successful treatment of Osgood-Schlatter disease with autologous-conditioned plasma in two patients: Joints, 2017; 5; 191-94
45. Eun SS, Lee SA, Kumar R, Direct bursoscopic ossicle resection in young and active patients with unresolved Osgood-Schlatter disease: Arthroscopy, 2015; 31; 416-21
Figures
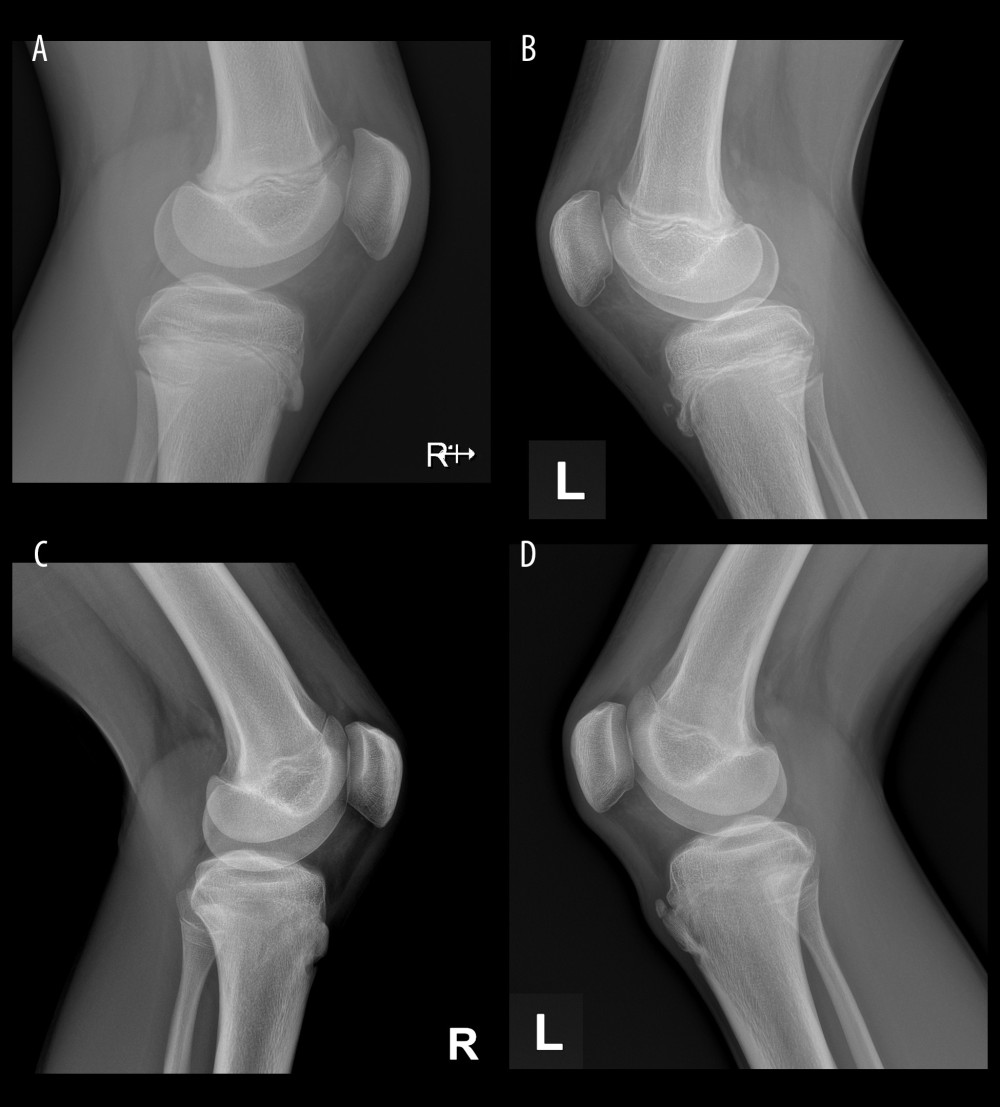 Figure 1. X-ray images belonging to the same patient: (A) healthy right knee; (B) left knee with separated bone fragment before PRP injection; (C) right knee after an observation period of 2 years; (D) left knee with separated bone fragment after PRP (Platelet-Rich Plasma) injection after observation period of 2 years.
Figure 1. X-ray images belonging to the same patient: (A) healthy right knee; (B) left knee with separated bone fragment before PRP injection; (C) right knee after an observation period of 2 years; (D) left knee with separated bone fragment after PRP (Platelet-Rich Plasma) injection after observation period of 2 years.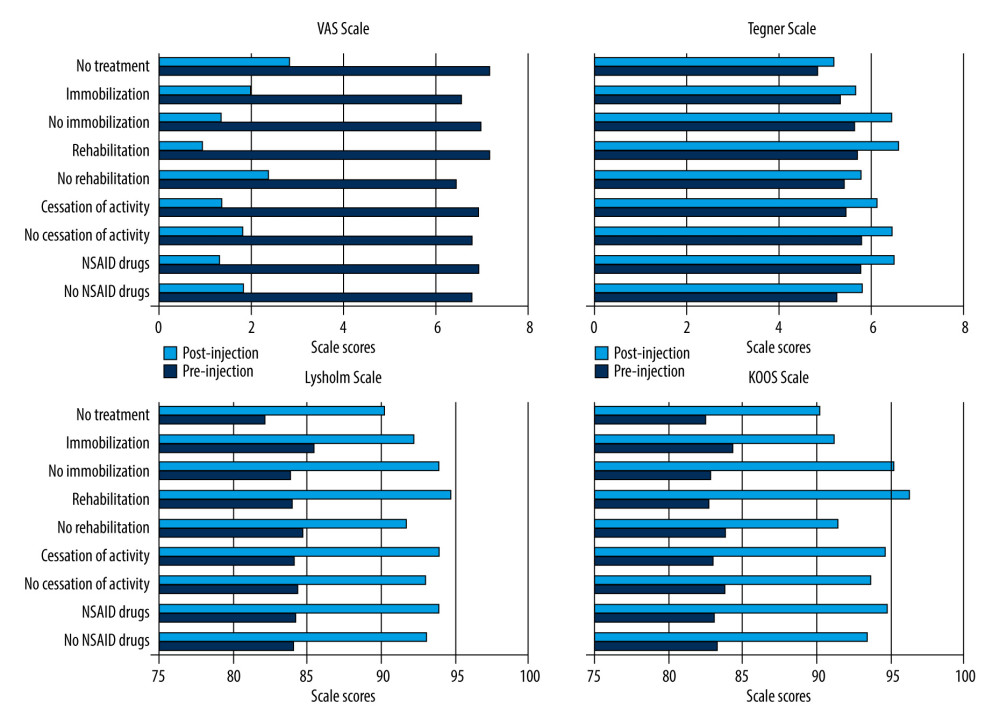 Figure 2. Comparison of the knee pain VAS (The Visual Analogue Scale) and function scales (Lysholm, Tegner, KOOS) scores according to the conservative treatment used.
Figure 2. Comparison of the knee pain VAS (The Visual Analogue Scale) and function scales (Lysholm, Tegner, KOOS) scores according to the conservative treatment used. Tables
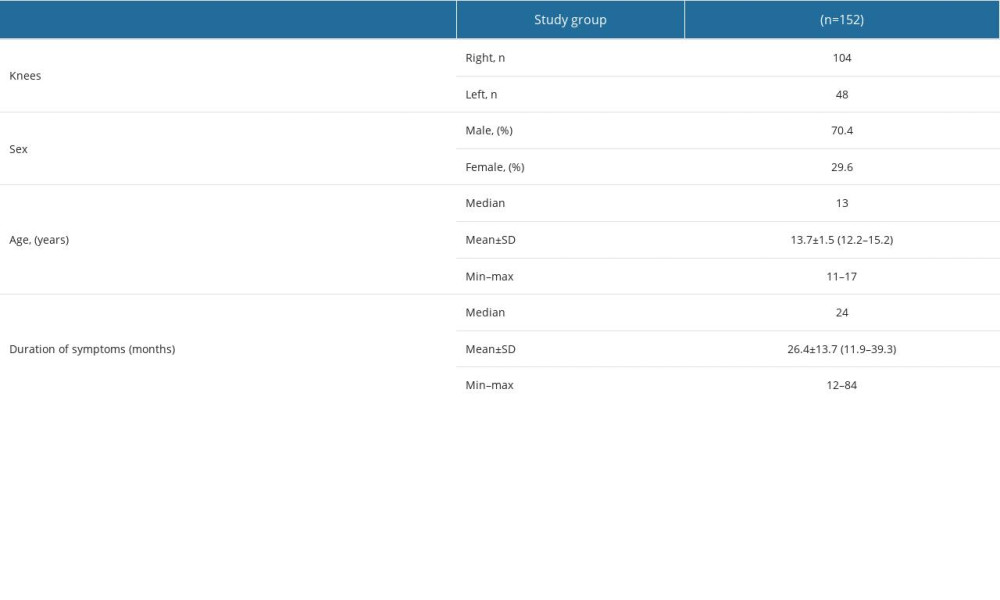 Table 1. Patient characteristics.
Table 1. Patient characteristics.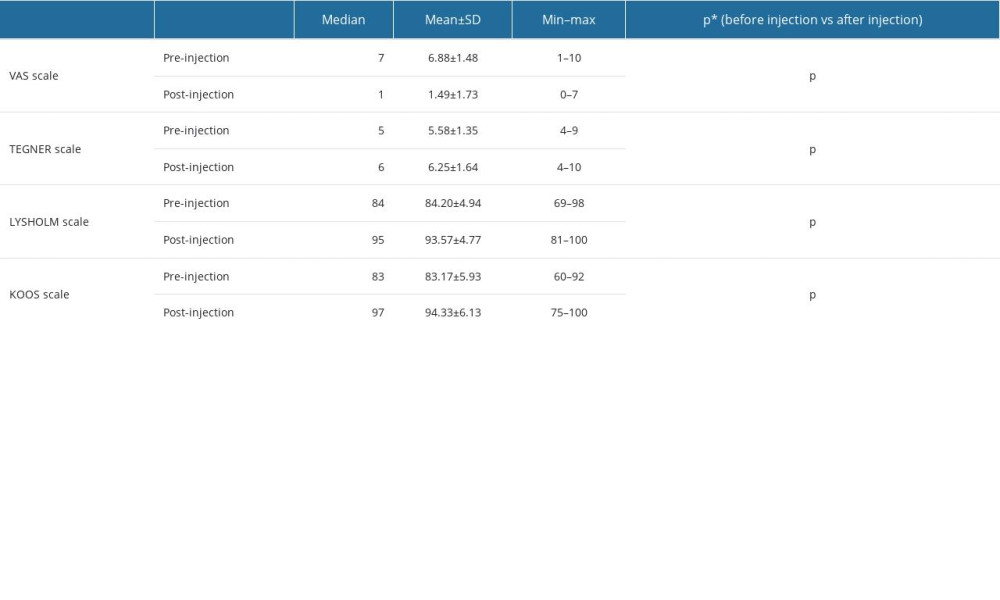 Table 2. The comparison of the results of the knee pain and function scales (VAS, Lysholm, Tegner, and KOOS) before and after PRP (Platelet-Rich Plasma) injection.
Table 2. The comparison of the results of the knee pain and function scales (VAS, Lysholm, Tegner, and KOOS) before and after PRP (Platelet-Rich Plasma) injection.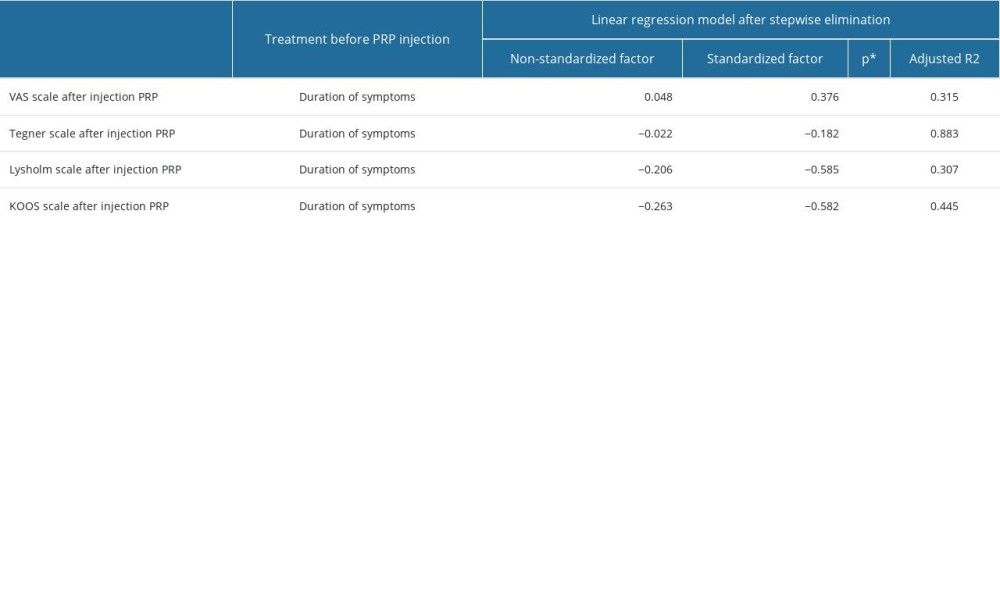 Table 3. The influence of the duration of symptoms on treatment outcomes: the results after PRP injection assessed on the pain scale (VAS) and knee joint function scales (Tegner, Lysholm, and KOOS) was evaluated using the linear regression model after stepwise elimination.
Table 3. The influence of the duration of symptoms on treatment outcomes: the results after PRP injection assessed on the pain scale (VAS) and knee joint function scales (Tegner, Lysholm, and KOOS) was evaluated using the linear regression model after stepwise elimination.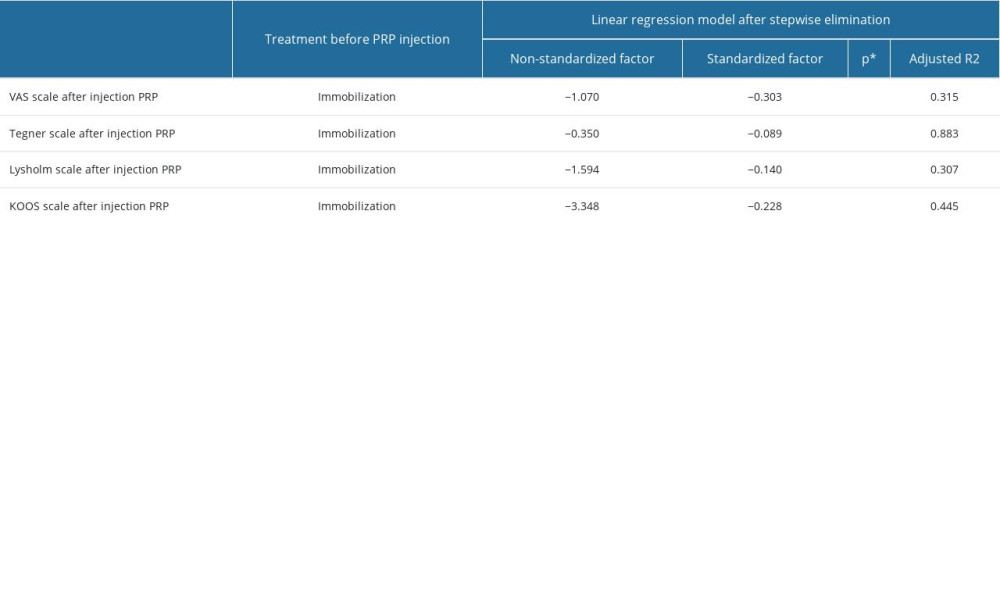 Table 4. The impact of limb immobilization prior to PRP injection on treatment outcomes: the results after PRP injection assessed on the pain scale (VAS) and knee joint function scales (Tegner, Lysholm, and KOOS), was evaluated using the linear regression model after stepwise elimination.
Table 4. The impact of limb immobilization prior to PRP injection on treatment outcomes: the results after PRP injection assessed on the pain scale (VAS) and knee joint function scales (Tegner, Lysholm, and KOOS), was evaluated using the linear regression model after stepwise elimination.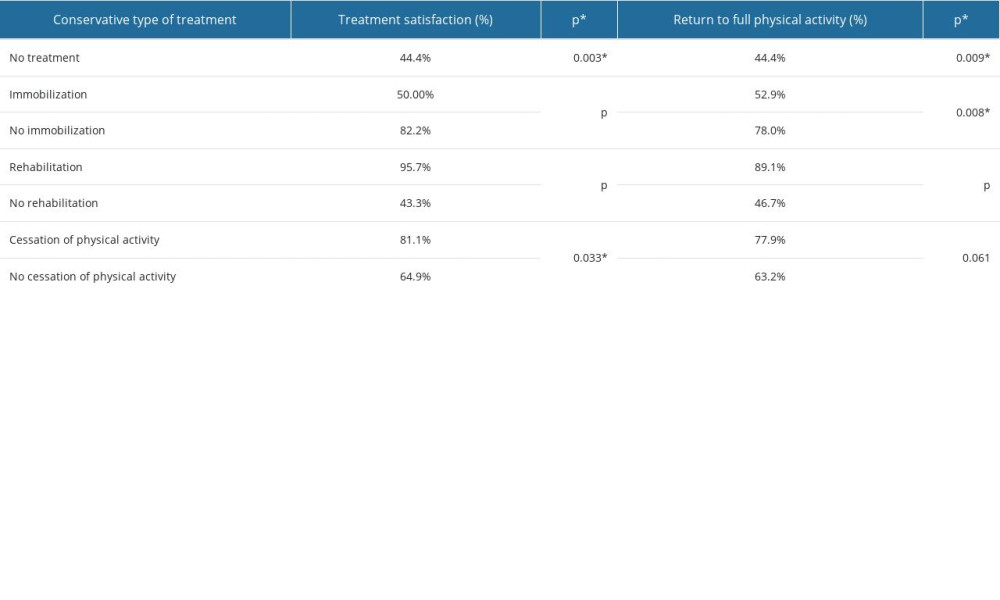 Table 5. Summary of patient satisfaction and return to activity according to treatment before PRP (Platelet-Rich Plasma) injection.
Table 5. Summary of patient satisfaction and return to activity according to treatment before PRP (Platelet-Rich Plasma) injection.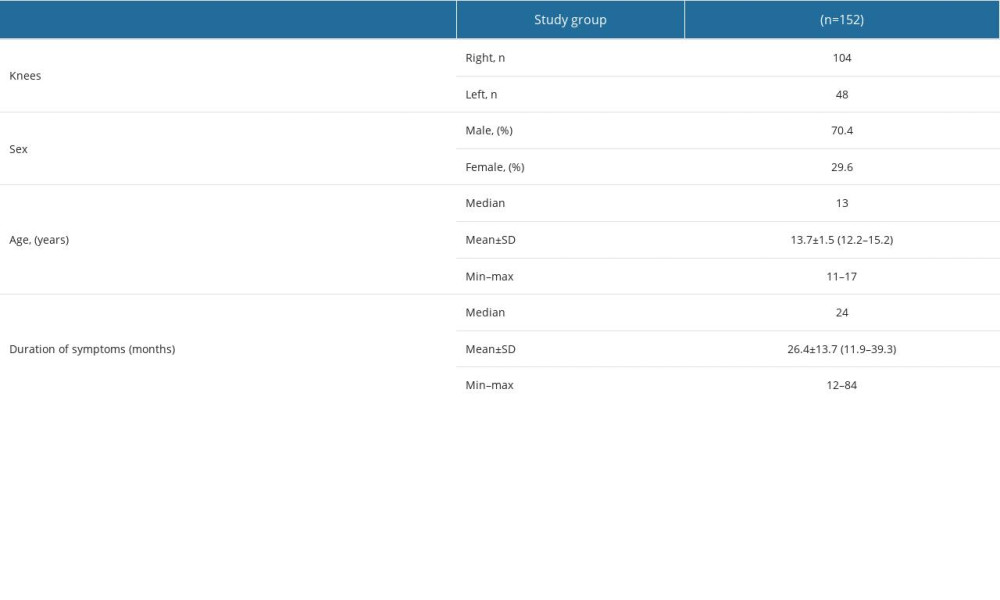 Table 1. Patient characteristics.
Table 1. Patient characteristics.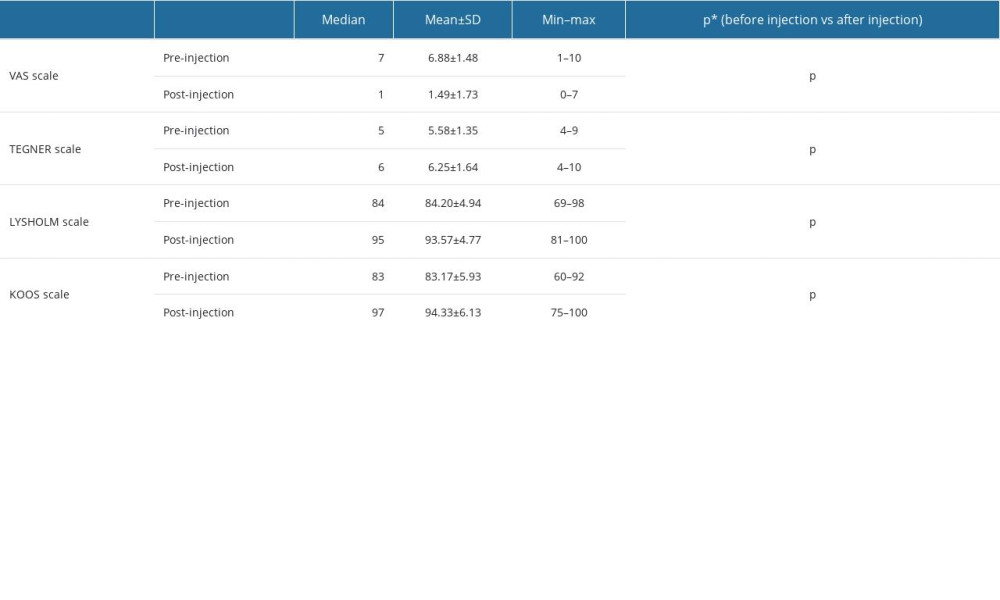 Table 2. The comparison of the results of the knee pain and function scales (VAS, Lysholm, Tegner, and KOOS) before and after PRP (Platelet-Rich Plasma) injection.
Table 2. The comparison of the results of the knee pain and function scales (VAS, Lysholm, Tegner, and KOOS) before and after PRP (Platelet-Rich Plasma) injection.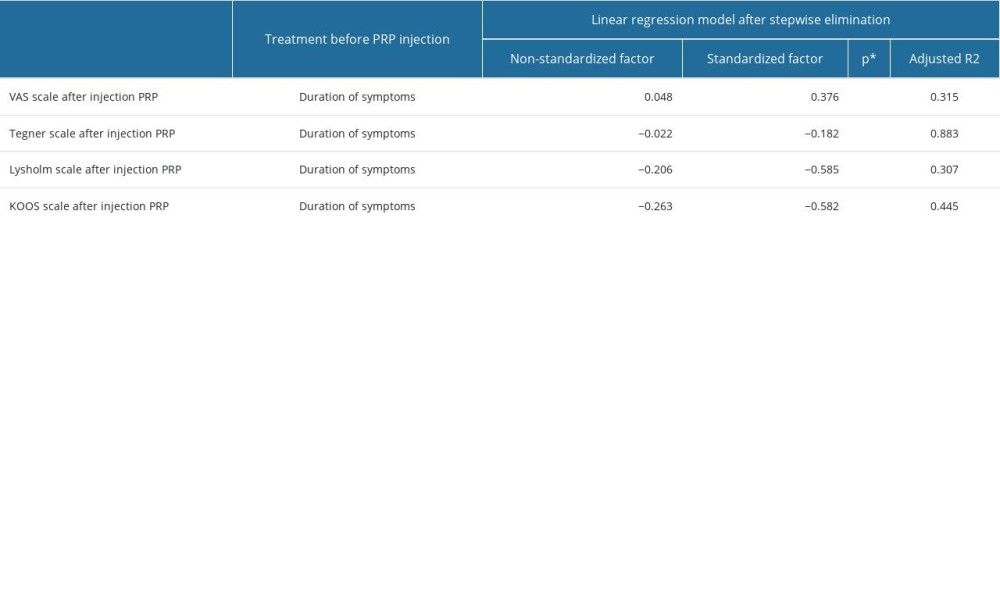 Table 3. The influence of the duration of symptoms on treatment outcomes: the results after PRP injection assessed on the pain scale (VAS) and knee joint function scales (Tegner, Lysholm, and KOOS) was evaluated using the linear regression model after stepwise elimination.
Table 3. The influence of the duration of symptoms on treatment outcomes: the results after PRP injection assessed on the pain scale (VAS) and knee joint function scales (Tegner, Lysholm, and KOOS) was evaluated using the linear regression model after stepwise elimination.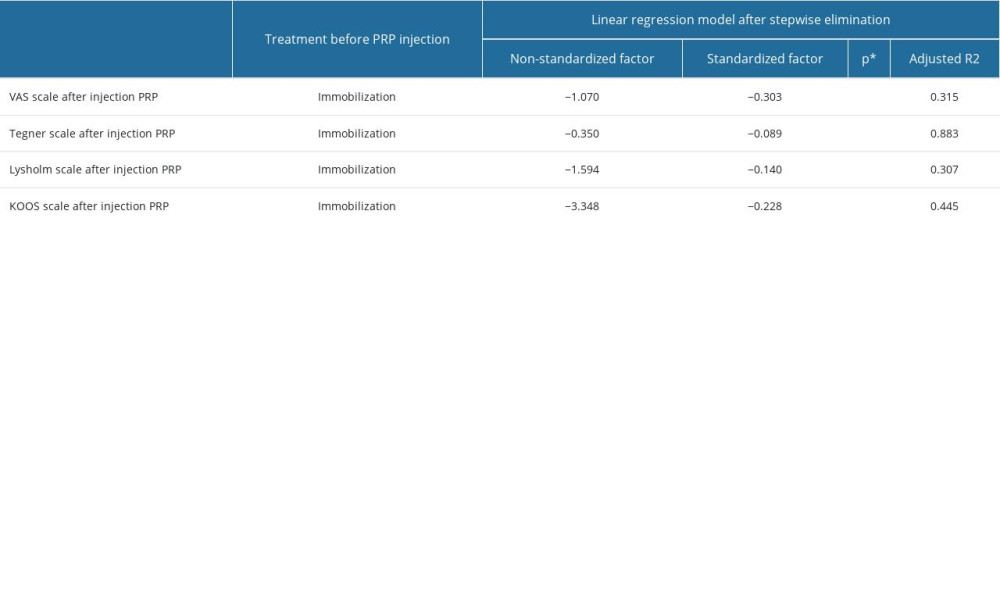 Table 4. The impact of limb immobilization prior to PRP injection on treatment outcomes: the results after PRP injection assessed on the pain scale (VAS) and knee joint function scales (Tegner, Lysholm, and KOOS), was evaluated using the linear regression model after stepwise elimination.
Table 4. The impact of limb immobilization prior to PRP injection on treatment outcomes: the results after PRP injection assessed on the pain scale (VAS) and knee joint function scales (Tegner, Lysholm, and KOOS), was evaluated using the linear regression model after stepwise elimination.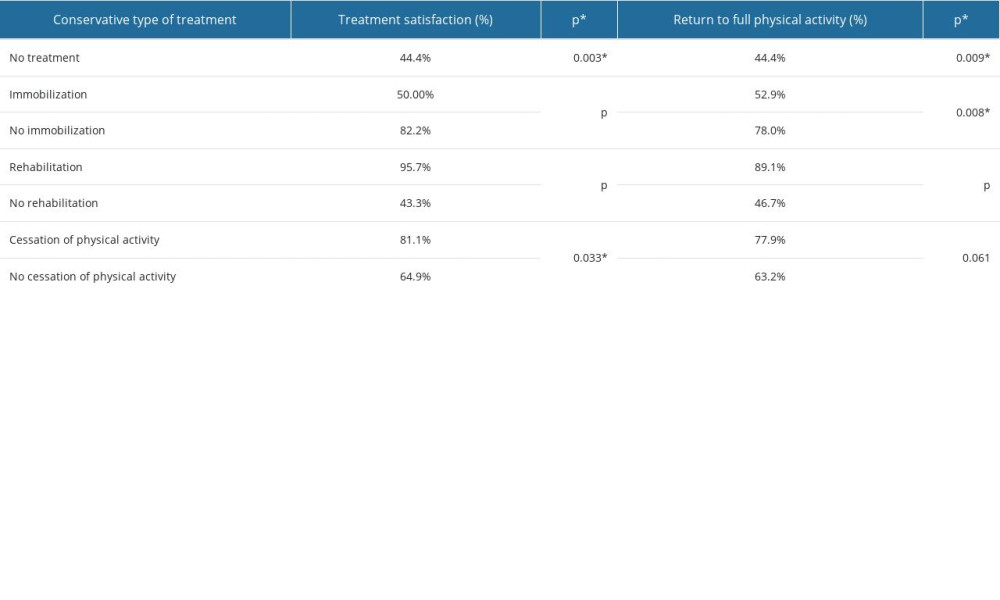 Table 5. Summary of patient satisfaction and return to activity according to treatment before PRP (Platelet-Rich Plasma) injection.
Table 5. Summary of patient satisfaction and return to activity according to treatment before PRP (Platelet-Rich Plasma) injection. In Press
14 Mar 2024 : Clinical Research
Renal Dysfunction Increases Risk of Adverse Cardiovascular Events in 5-Year Follow-Up Study of Intermediate...Med Sci Monit In Press; DOI: 10.12659/MSM.943956
15 Mar 2024 : Clinical Research
Impact of One-Lung Ventilation on Oxygenation and Ventilation Time in Thoracoscopic Heart Surgery: A Compar...Med Sci Monit In Press; DOI: 10.12659/MSM.943089
14 Mar 2024 : Clinical Research
Differential DHA and EPA Levels in Women with Preterm and Term Births: A Tertiary Hospital Study in IndonesiaMed Sci Monit In Press; DOI: 10.12659/MSM.943895
15 Mar 2024 : Clinical Research
Evaluation of an Optimized Workflow for the Radiofrequency Catheter Ablation of Paroxysmal Atrial FibrillationMed Sci Monit In Press; DOI: 10.12659/MSM.943526
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








