14 September 2023: Clinical Research
Predicting Survival Outcomes in Post-Cardiac Arrest Syndrome: The Impact of Combined Sequential Organ Failure Assessment Score and Serum Lactate Measurement
SooHyun Kim1BCE, HeeWon Yang1BE, BangShill Rhee1CE, Hakyoon Song2DF, HyukHoon KimDOI: 10.12659/MSM.942119
Med Sci Monit 2023; 29:e942119
Abstract
BACKGROUND: Post-cardiac arrest syndrome (PCAS) is a major concern and shares pathophysiology with sepsis. Sequential organ failure assessment (SOFA) scores and serum lactate levels, as suggested in the Survival Sepsis Guidelines, have shown significant predictive value for prognosis in patients with sepsis. This retrospective study aimed to evaluate combined use of the SOFA score and serum lactate measurement on survival prognosis in PCAS.
MATERIAL AND METHODS: Our study included patients with return of spontaneous circulation after cardiac arrest who were age >18 years and underwent targeted temperature management. The 438 patients were allocated to a surviving group and a deceased group at discharge. Multivariable regression models were used to evaluate any association with SOFA scores, serum lactate levels, and survival. To evaluate the predictive value of regression models, the area under the receiver operating characteristic curve (AUROC) was assessed.
RESULTS: Lower SOFA score and serum lactate level were associated with better survival rates in the post-cardiac arrest patients (SOFA score: odds ratio (OR), 0.77; 95% confidence interval (CI), 0.67-0.88; P<0.001; lactate level: OR, 0.85; 95% CI, 0.81-0.94; P<0.001). The combined model of the SOFA score and serum lactate level was superior to models including either SOFA score or serum lactate level alone in predicting survival (AUROC, 0.86 vs 0.83, P=0.028, 0.86 vs 0.81, P=0.004).
CONCLUSIONS: Because of the superiority of the combined model of SOFA score and serum lactate level, combining these 2 factors could improve prediction of prognosis and survival outcomes in PCAS.
Keywords: Lactic Acid, Organ Dysfunction Scores, Post-Cardiac Arrest Syndrome, Prognosis, Humans, Adolescent, Retrospective Studies, Heart Arrest, Sepsis, Lactates
Background
Cardiac arrest and management of survivors are major public health issues [1]. The estimated incidence of out-of-hospital cardiac arrest (OHCA) was 50–60 per 100 000 person-years in North America [2]. In South Korea, the number of patients with sudden cardiac arrests in 2020 was 61.6 per 100 000 individuals [3]. However, even when first resuscitated, the overall survival rate to hospital discharge after OHCA was 8.8% globally and 8.2% in South Korea [3,4]. In this context, research on the prognosis of cardiac arrest is important for determining the direction and scope of future treatment for critical patients who survive cardiac arrest and informing caregivers of their prognosis; therefore, there have been many studies on factors predicting survival in patients with cardiac arrest [5–7].
Post-cardiac arrest syndrome (PCAS), which is defined as the clinical status that involves global ischemic-reperfusion injury, aggressive inflammation, myocardial dysfunction, coagulopathy, and adrenal dysfunction after cardiac arrest event, and sepsis are 2 distinct medical conditions that share some similarities, even though cardiac arrest may not be caused by a serious infection [8]. During cardiac arrest, blood flow to organs is reduced or stopped, leading to ischemia and tissue damage [9]. When blood flow is restored after resuscitation, a burst of reactive oxygen species is produced, which can cause further tissue damage and inflammation, known as reperfusion injury [10]. As a result of ischemic/reperfusion injury, a systemic inflammatory response occurs throughout the body, and this aggressive and dysregulated inflammatory response has a deleterious effect on patients [11]. Similar to PCAS, sepsis is characterized by a dysregulated host response to infection, resulting in tissue hypoxia and shock, followed by multi-organ damage [12].
The sequential organ failure assessment (SOFA) score is a scoring system commonly used to evaluate the severity of multi-organ failure in intensive care unit (ICU) patients and is useful for assessing the clinical outcomes of critically ill patients with various conditions, including sepsis [13]. Likewise, the serum level of lactate, which is a normal byproduct of glucose metabolism and can be elevated by increased anaerobic glycolysis in the hypoperfusion state, may also have prognostic value in patients with septic shock [14]. The Surviving Sepsis Campaign recommends the SOFA score and lactate measurement as risk stratification methods and important components in the management of patients with sepsis [12]. Elevation of the SOFA score and serum lactate levels after ICU admission predicted higher mortality in critically ill patients [15–17].
Because patients with PCAS have similar characteristics to patients with sepsis, both SOFA score and serum lactate level could be predictive factors in patients with PCAS, as they are in patients with sepsis. Nevertheless, these factors have not been studied together; therefore, this retrospective study of 438 patients who had cardiac arrest and post-cardiac arrest syndrome (PCAS) after return of spontaneous circulation (ROSC) evaluated the effect of combined use of the sequential organ failure assessment (SOFA) score and serum lactate measurements on patient prognosis and survival.
Material and Methods
ETHICS CONSIDERATIONS:
Our study was conducted in accordance with the principles of the Declaration of Helsinki and was approved by the Institutional Review Board of Ajou University Medical Center (AJOUIRB-DB-2023-0113). Owing to the retrospective nature of this study, the requirement for informed consent was waived.
STUDY SETTING AND ENROLLED PATIENTS:
At our institute, where this study was conducted, almost 90 000 patients visit the Emergency Department (ED) each year, and approximately 500 patients with return of spontaneous circulation (ROSC) after cardiac arrest were admitted and cared for in the ICU from January 2016 to December 2020. From our hospital’s database of cardiopulmonary resuscitation (CPR) events, we collected data on all cardiac arrest cases with ROSC who were >18 years old and who were admitted and underwent targeted temperature management (TTM) in the ICU, regardless of the site of the cardiac arrest. The target temperature for our TTM protocol is 32–37°C [18]. TTM is performed with temperature-adjustable devices with a feedback loop system (Arctic Sun® Energy Transfer Pads™; Medivance Corp., Louisville, KY, USA, or Cool Guard Alsius Icy Heat Exchange Catheter; Alsius Corporation, Irvine, CA, USA) or water-circulating blankets as temperature management methods. Patients undergoing TTM receive sufficient sedative and analgesic treatments with immediate control of shivering and seizures. We excluded patients who could obey commands or had a traumatic cause of arrest, brain hemorrhage, or hemodynamic instability. We also excluded patients with end-stage cancer with a life expectancy of <6 months and those with a do-not-resuscitate order with consent from their families because they had not undergone TTM. Finally, the enrolled patients were grouped based on survival status at discharge, and their data were analyzed to compare the predictive values of SOFA score and lactate level in the survival status at discharge of patients with PCAS.
STUDY VARIABLES AND DATA COLLECTION:
We retrospectively and comprehensively collected data from the electronic medical records and a data registry of patients with PCAS who underwent TTM after ROSC. We collected demographic data, including age, sex, underlying disease (diabetes mellitus and hypertension), and variables related to cardiac arrests, such as witnessed arrest, bystander CPR, automatic external defibrillator (AED) application, prehospital/in-hospital initial rhythm, cause of arrest, no-flow time (time from collapse to the application of life support), total CPR time (time from the application of life support until ROSC), initial SOFA score, initial serum lactate level, serum C-reactive protein level, and TTM method. The SOFA score is used to assess organ dysfunction or failure for critical illness severity evaluation based on the degree of dysfunction of 6 organ systems and plays a crucial role as the main tool for sepsis diagnosis [17]. The SOFA score ranges from 0 to 24, with higher scores indicating a higher mortality risk. Laboratory findings, such as lactate levels, were retrieved from electronic medical records. Variables related to outcomes, including survival status at hospital discharge, were collected from the data registry of patients with PCAS.
STATISTICAL ANALYSIS:
Continuous variables are presented as means (±standard deviations) or medians (interquartile ranges), depending on the data distribution, and categorical data are presented as numbers with percentages (%). We used a
Results
BASELINE CHARACTERISTICS OF ENROLLED PATIENTS:
Of the 2191 adult patients presenting with cardiac arrest to the ED, 1408 were declared dead on arrival or dead before admission, or were transferred to another hospital and excluded. Of the 783 patients admitted alive, 345 were excluded from the TTM, including those who obeyed a command, had hemorrhagic events, or had unstable vital signs. Finally, 438 patients who underwent TTM were included in the study and divided into 2 groups: those who were discharged alive (n=236) and those who died in the hospital before discharge (n=202) (Figure 1). The baseline characteristics of the enrolled patients are presented in Table 1. Age differed significantly between the 2 groups (P<0.001). Other general demographics, including sex and underlying disease, did not differ significantly between the 2 outcome groups. AED application, first monitored rhythm, no-flow time, total CPR time, and presumed cause of arrest significantly differed between the 2 groups. The total SOFA score and lactic acid levels were also significantly different between the 2 groups (P<0.001) (Table 1).
ANALYSIS OF FACTORS ASSOCIATED WITH SURVIVAL OUTCOMES:
In the univariate analysis, lower SOFA score and lactic acid level were associated with survival discharged outcomes: SOFA score (odds ratio (OR), 0.79; 95% confidence interval (CI), 0.73–0.85; P<0.001) and lactic acid (OR, 0.86; 95% CI, 0.82–0.90; P<0.001). Furthermore, in the univariate analysis, other factors, such as younger age, shockable state of initial rhythm, use of AED, cardiogenic etiology, shorter no-flow time, and total CPR time, were associated with survival-to-discharge outcomes (P<0.001). However, even after adjusting for multiple confounding factors, including age, initial shockable rhythm, use of AED, cardiogenic etiology, no-flow time, and total CPR time, SOFA score and serum lactic acid level were still associated with good survival outcomes: SOFA score (OR, 0.77; 95% CI, 0.67–0.88; P<0.001) and serum lactate level (OR, 0.85; 95% CI, 0.81–0.94; P=0.002) (Table 2).
PREDICTION OF SURVIVAL DISCHARGED OUTCOME:
The model that combines the SOFA score and lactate level is more effective in predicting survival outcomes. DeLong’s test was performed for 2 areas under the ROC curve (AUROC) of the multivariable models, which included the SOFA score, the serum lactate level, or both. All 3 multivariable models included variables with statistically significant ORs in the univariate analysis, such as age, initial shockable rhythm state, use of an AED, presumed cardiogenic etiology, no-flow time, and total CPR time. The model that included both the SOFA score and serum lactate level was superior in predicting survival compared to the models including either the SOFA score or the serum lactate level alone (0.86 vs 0.83, P value=0.028, 0.86 vs 0.81, P value=0.004, respectively). Additionally, there was no significant difference between the SOFA score-only and serum lactate level-only models (0.83 vs 0.81, P value=0.050) (Figure 2).
EFFECT OF SERUM LACTIC ACID AND SOFA SCORE ACCORDING TO CAUSE OF ARREST:
In patients with presumed non-cardiogenic cause of arrest, lower serum lactic acid level and SOFA score were still associated with good survival outcomes in multivariable logistic regression models including age, initial shockable rhythm, use of AED, no-flow time, and total CPR time: serum lactate level (OR, 0.85; 95% CI, 0.79–0.92; P<0.001), SOFA score (OR, 0.84; 95% CI, 0.75–0.92; P<0.001). In patients with presumed cardiogenic cause of arrest, lower SOFA score was associated with better survival prognosis (OR, 0.75; 95% CI, 0.62–0.89; P=0.001), but serum lactic acid level was not associated with survival prognosis (OR, 0.91; 95% CI, 0.82–1.00; P=0.07), (Table 3).
Discussion
We evaluated the effect of combined use of the SOFA score and serum lactate measurements on patient prognosis in PCAS, comparing the multivariable regression model AUROC of the combined SOFA score and serum lactate level with models including either the SOFA score alone or the serum lactate level alone. The combination of SOFA score and serum lactate level was significantly better in predicting survival-to-discharge outcomes in patients with PCAS. This finding adds to the results of previous studies that have examined the individual association of SOFA score and serum lactate level with the survival of patients with PCAS, and both the SOFA score and the serum lactate level have significant value in predicting prognosis in patients with PCAS [19,20]. The highest SOFA score over 72 h had an independent association with in-hospital mortality in patients with PCAS [19]. Patients with lower lactate level at specific times and greater percent decrease in lactate level over the first 12 h after cardiac arrest had better survival rates [20]. However, the 2 factors used in each study have not previously been combined to predict the survival of patients with PCAS. Our study demonstrates that the combination of these 2 factors is useful for predicting survival in patients with PCAS and is superior to models that use either factor alone.
Similar to sepsis, the SOFA score reflects the current state of organ failure in patients with PCAS and may be useful in predicting patient survival [21]. The SOFA score is used to assess the severity of organ dysfunction in critically ill patients. It evaluates the functions of 6 organ systems: respiratory, cardiovascular, hepatic, coagulation, renal, and neurological [22]. The SOFA score is commonly used in ICUs to estimate the clinical severity of disease in patients and to monitor the progression of organ failure during patient care [21]. After prolonged hypoxic/ischemic insults during cardiac arrest, patients usually experience a cascade of events, including systemic ischemia/reperfusion injury, dysregulated inflammation, and subsequent multi-organ dysfunction, known as PCAS, during the post-cardiac arrest period [19,24]. The extent of organ dysfunction and failure in patients with PCAS and the severity of the condition are reflected in the SOFA score at the time of measurement. Therefore, as in our study, a higher SOFA score in patients with PCAS indicates more severe organ damage or dysfunction at the time of scoring, which can predict a poor prognosis in terms of survival and discharge from the hospital.
Serum lactate levels, which show the state of energy metabolism and shock in patients with PCAS, indicate organ dysfunction or hypoperfusion and reflect dysregulated immune status in patients with PCAS. Lactate is a metabolic byproduct that accumulates in the body when there is an imbalance between oxygen supply and demand [25]. During cardiac arrest, blood flow to vital organs, including the brain and heart, is disrupted, leading to oxygen deprivation and initiation of anaerobic metabolism [26]. In addition, despite the return of blood flow and adjustment of the hypotensive status after ROSC, tissue perfusion may still be compromised because of impaired microcirculatory dysfunction caused by endothelial dysfunction, nitric oxide dysregulation, or hematologic abnormalities owing to an excessive inflammatory response, which can hinder the delivery of oxygen to tissues and cause persistent anaerobic glycolysis [27]. Elevated lactate levels can indicate aggravation of tissue hypoperfusion and anaerobic metabolism related to cardiac arrest and persistent PCAS [19]. Moreover, serum lactate levels correspond to several clinical variables that reflect the status of systemic inflammation and could serve as early biomarkers of the systemic inflammatory response in sepsis as a prelude to apparent organ dysfunction [28]. Therefore, hyperlactatemia after ROSC may be a predictor of myocardial dysfunction, pressor-dependent hemodynamic instability, microcirculatory failure, hematologic dysfunction, and subsequent multiple organ damage caused by aggressive systemic inflammation. Consequently, the systemic accumulation of lactic acid may be an indicator of hypoperfusion and aggressive inflammation in PCAS and is, therefore, related to poor survival in PCAS.
In addition, SOFA score and serum lactic acid level each have different effects on survival prognosis in patients with PCAS, as shown in the Table 3. This may mean that these 2 factors have different implications for clinical aspects in PCAS patients, and the combination of the 2 factors would have more significant impact on predicting survival in presumed non-cardiac arrest patients than in cardiac arrest patients.
This study had some limitations. First, it had a retrospective design and was conducted at a single institution in South Korea. Prospective studies involving diverse patient populations are warranted. Second, when comparing the basic characteristics of the patients enrolled in our study, there were significant differences in age, CPR time, and AED use. Although these factors were adjusted for during analysis, they may have acted as confounding factors. Third, we excluded patients who were not indicated for TTM or who did not apply for various reasons, which may have introduced a selection bias. After adjusting for these confounding factors, we found that SOFA scores and lactate levels were associated with survival. Fourth, the SOFA score uses the Glasgow Coma Scale (GCS), which has limitations in neurological assessment. The neurological component of the SOFA Score relies on the GCS, which has limitations, such as interobserver variability and reliance on subjective assessment [29].
Conclusions
Our study demonstrated that the combination of SOFA score and lactate level could be valuable in predicting survival in patients with PCAS who have undergone TTM in the ICU setting. SOFA score and lactate level each reflect and involve different clinical aspects in patients. Therefore, by combining these 2 factors, healthcare providers can better predict the survival prognosis in patients with PCAS and this may help clinicians provide appropriate explanations to caregivers. Prospective studies with larger sample sizes and a wider variety of patients are warranted.
Figures
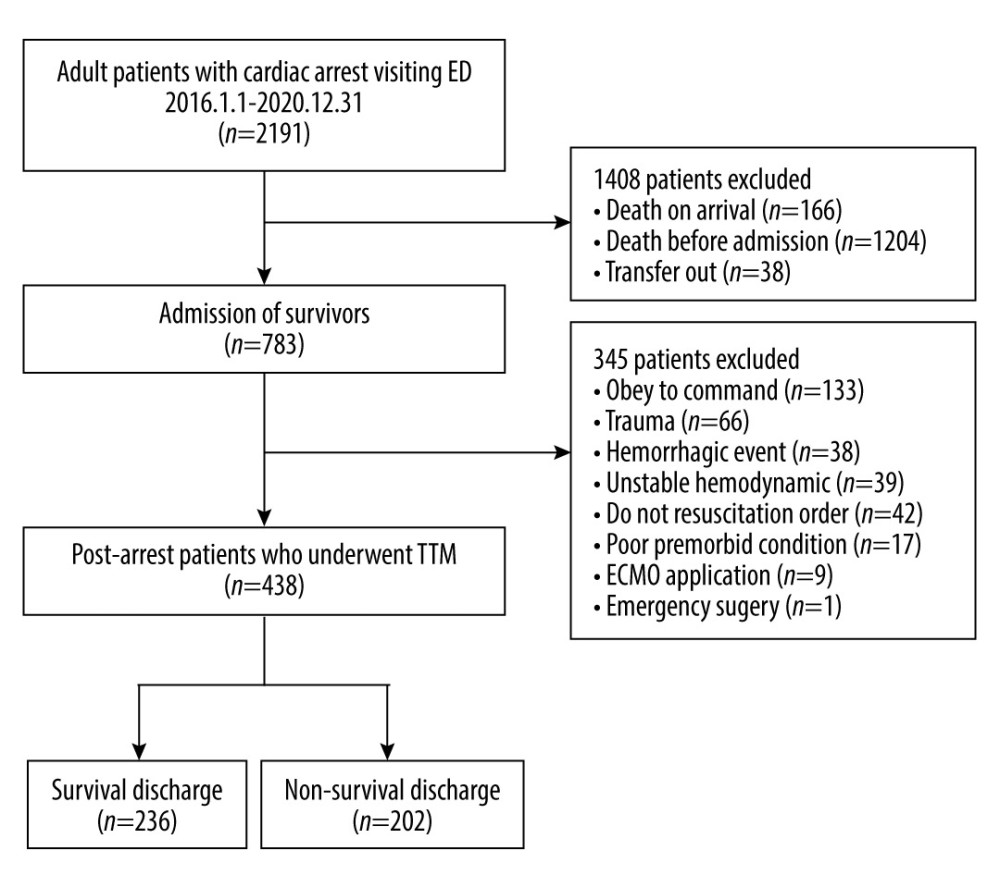 Figure 1. Study enrollment flowchart.
Figure 1. Study enrollment flowchart. 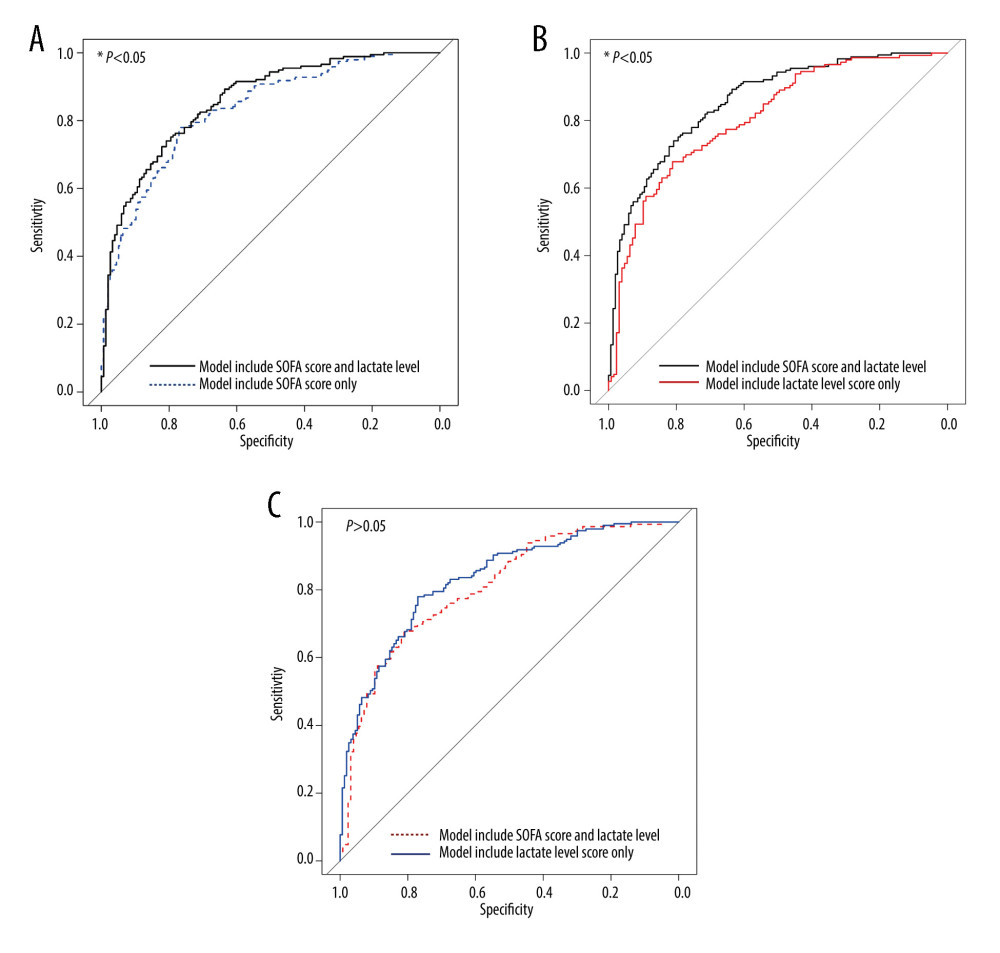 Figure 2. Comparison of receiver operating characteristics (ROC) curves for predicting survival outcome in patients with post-cardiac arrest syndrome. (A) Comparison of the area under the ROC curve (AUROC) of the 2 models, the model including SOFA score and serum lactate level versus the model including SOFA score only (AUROC=0.86 versus 0.83, P value=0.028). (B) Comparison of AUROC of the 2 models, the model including SOFA score and serum lactate level versus the model including serum lactate level only (AUROC=0.86 vs 0.81, P value=0.004) (C) Comparison of the AUROC of the 2 models, the model including the SOFA score versus the model including the serum lactate level (AUROC=0.83 vs 0.81, P value=0.050).
Figure 2. Comparison of receiver operating characteristics (ROC) curves for predicting survival outcome in patients with post-cardiac arrest syndrome. (A) Comparison of the area under the ROC curve (AUROC) of the 2 models, the model including SOFA score and serum lactate level versus the model including SOFA score only (AUROC=0.86 versus 0.83, P value=0.028). (B) Comparison of AUROC of the 2 models, the model including SOFA score and serum lactate level versus the model including serum lactate level only (AUROC=0.86 vs 0.81, P value=0.004) (C) Comparison of the AUROC of the 2 models, the model including the SOFA score versus the model including the serum lactate level (AUROC=0.83 vs 0.81, P value=0.050). References
1. Stecker EC, Reinier K, Marijon E, Public health burden of sudden cardiac death in the United States: Circ Arrhythm Electrophysiol, 2014; 7(2); 212-17
2. Doctor NE, Ahmad NS, Pek PP, The Pan-Asian Resuscitation Outcomes Study (PAROS) clinical research network: What, where, why and how: Singapore Med J, 2017; 58(7); 456-58
3. Roh S-Y, Choi J-I, Park SH, The 10-year trend of out-of-hospital cardiac arrests: A Korean nationwide population-based study: Korean Circ J, 2021; 51(10); 866-74
4. Yan S, Gan Y, Jiang N, The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: A systematic review and meta-analysis: Crit Care, 2020; 24(1); 61
5. Schluep M, Gravesteijn BY, Stolker RJ, One-year survival after in-hospital cardiac arrest: A systematic review and meta-analysis: Resuscitation, 2018; 132; 90-100
6. Martinell L, Nielsen N, Herlitz J, Early predictors of poor outcome after out-of-hospital cardiac arrest: Crit Care, 2017; 21(1); 96
7. Wihersaari L, Ashton NJ, Reinikainen M, Neurofilament light as an outcome predictor after cardiac arrest: A post hoc analysis of the COMACARE trial: Intensive Care Med, 2021; 47(1); 39-48
8. Adrie C, Laurent I, Monchi M, Postresuscitation disease after cardiac arrest: A sepsis-like syndrome?: Curr Opin Crit Care, 2004; 10(3); 208-12
9. Kleinman ME, Brennan EE, Goldberger ZD, Part 5: Adult basic life support and cardiopulmonary resuscitation quality: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care: Circulation, 2015; 132(18 Suppl 2); S414-35
10. Hausenloy DJ, Yellon DM, Myocardial ischemia-reperfusion injury: A neglected therapeutic target: J Clin Invest, 2013; 123(1); 92-100
11. Langeland H, Damås JK, Mollnes TE, The inflammatory response is related to circulatory failure after out-of-hospital cardiac arrest: A prospective cohort study: Resuscitation, 2022; 170; 115-25
12. Evans L, Rhodes A, Alhazzani W, Surviving sepsis campaign: International guidelines for management of sepsis and septic shock 2021: Intensive Care Med, 2021; 47(11); 1181-247
13. Vincent JL, de Mendonça A, Cantraine F, Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine: Crit Care Med, 1998; 26(11); 1793-800
14. Loomba RS, Farias JS, Villarreal EG, Serum lactate and mortality during pediatric admissions: Is 2 really the magic number?: J Pediatr Intensive Care, 2022; 11(2); 83-90
15. Liu V, Morehouse JW, Soule J, Fluid volume, lactate values, and mortality in sepsis patients with intermediate lactate values: Ann Am Thorac Soc, 2013; 10(5); 466-73
16. Ferreira FL, Bota DP, Bross A, Serial evaluation of the SOFA score to predict outcome in critically ill patients: JAMA, 2001; 286(14); 1754-58
17. Karakike E, Kyriazopoulou E, Tsangaris I, The early change of SOFA score as a prognostic marker of 28-day sepsis mortality: Analysis through a derivation and a validation cohort: Crit Care, 2019; 23(1); 387
18. Panchal AR, Bartos JA, Cabañas JG, Part 3: Adult basic and advanced life support: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care: Circulation, 2020; 142(16 Suppl 2); S366-468
19. Roberts BW, Kilgannon JH, Chansky ME, Multiple organ dysfunction after return of spontaneous circulation in postcardiac arrest syndrome: Crit Care Med, 2013; 41(6); 1492-501
20. Donnino MW, Andersen LW, Giberson T, Initial lactate and lactate change in post-cardiac arrest: A multicenter validation study: Crit Care Med, 2014; 42(8); 1804-11
21. Matsuda J, Kato S, Yano H, The Sequential Organ Failure Assessment (SOFA) score predicts mortality and neurological outcome in patients with post-cardiac arrest syndrome: J Cardiol, 2020; 76(3); 295-302
22. Kashyap R, Sherani KM, Dutt T, Current utility of sequential organ failure assessment score: A literature review and future directions: Open Respir Med J, 2021; 15; 1-6
23. Lambden S, Laterre PF, Levy MM, The SOFA score-development, utility and challenges of accurate assessment in clinical trials: Crit Care, 2019; 23(1); 374
24. Dalessio L, Post-cardiac arrest syndrome: AACN Adv Crit Care, 2020; 31(4); 383-93
25. Rabinowitz JD, Enerbäck S, Lactate: The ugly duckling of energy metabolism: Nat Metab, 2020; 2(7); 566-71
26. Zhang M, Zhang Q, Yu Y, Effects of early hemodynamics, oxygen metabolism, and lactate dynamics on prognosis of post-cardiac arrest syndrome: Chin Med J (Engl), 2021; 135(3); 344-46
27. Miranda M, Balarini M, Caixeta D, Microcirculatory dysfunction in sepsis: Pathophysiology, clinical monitoring, and potential therapies: Am J Physiol Heart Circ Physiol, 2016; 311(1); H24-35
28. Mikkelsen ME, Miltiades AN, Gaieski DF, Serum lactate is associated with mortality in severe sepsis independent of organ failure and shock: Crit Care Med, 2009; 37(5); 1670-77
29. Rowley G, Fielding K, Reliability and accuracy of the Glasgow Coma Scale with experienced and inexperienced users: Lancet, 1991; 337(8740); 535-38
Figures
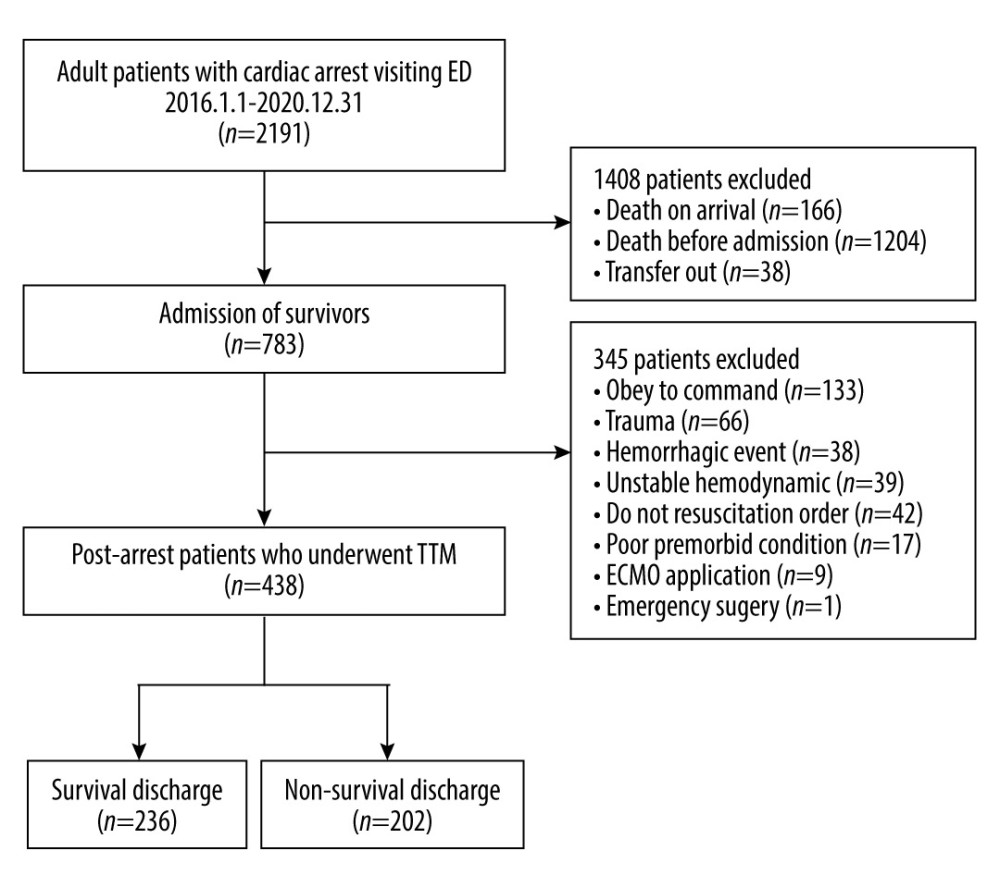 Figure 1. Study enrollment flowchart.
Figure 1. Study enrollment flowchart.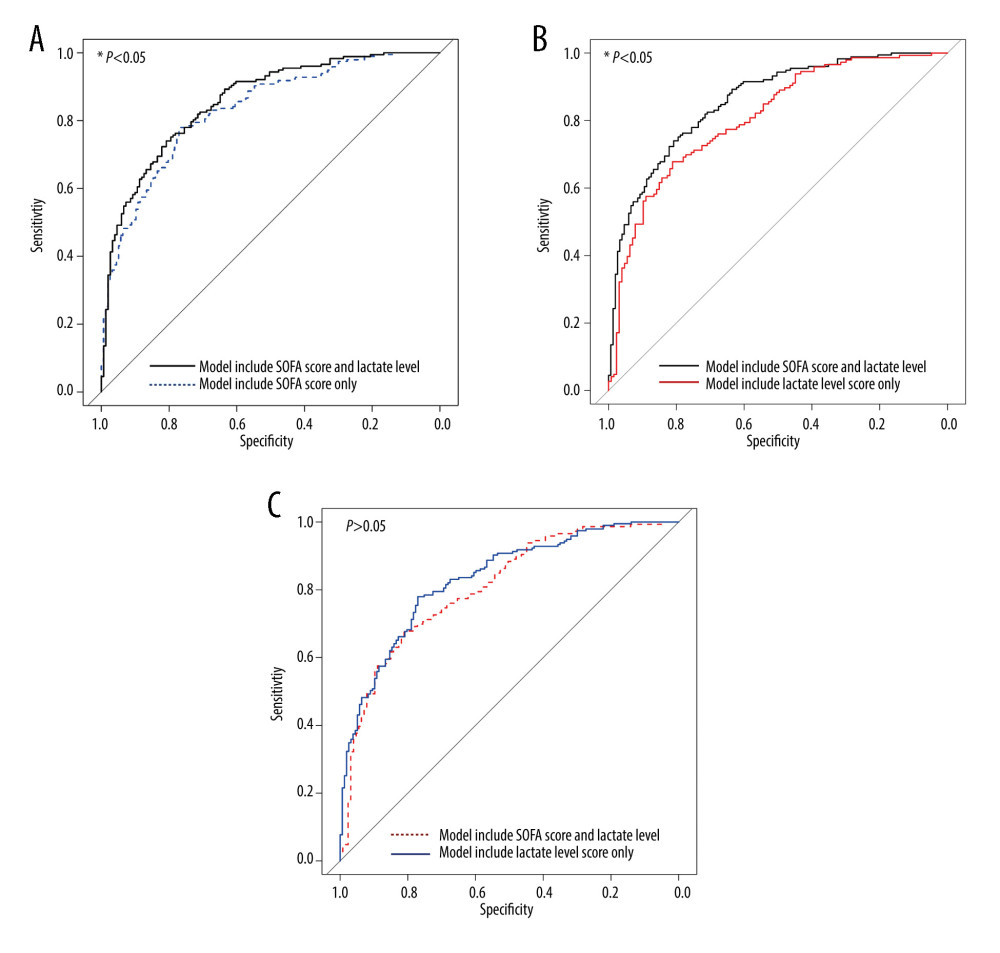 Figure 2. Comparison of receiver operating characteristics (ROC) curves for predicting survival outcome in patients with post-cardiac arrest syndrome. (A) Comparison of the area under the ROC curve (AUROC) of the 2 models, the model including SOFA score and serum lactate level versus the model including SOFA score only (AUROC=0.86 versus 0.83, P value=0.028). (B) Comparison of AUROC of the 2 models, the model including SOFA score and serum lactate level versus the model including serum lactate level only (AUROC=0.86 vs 0.81, P value=0.004) (C) Comparison of the AUROC of the 2 models, the model including the SOFA score versus the model including the serum lactate level (AUROC=0.83 vs 0.81, P value=0.050).
Figure 2. Comparison of receiver operating characteristics (ROC) curves for predicting survival outcome in patients with post-cardiac arrest syndrome. (A) Comparison of the area under the ROC curve (AUROC) of the 2 models, the model including SOFA score and serum lactate level versus the model including SOFA score only (AUROC=0.86 versus 0.83, P value=0.028). (B) Comparison of AUROC of the 2 models, the model including SOFA score and serum lactate level versus the model including serum lactate level only (AUROC=0.86 vs 0.81, P value=0.004) (C) Comparison of the AUROC of the 2 models, the model including the SOFA score versus the model including the serum lactate level (AUROC=0.83 vs 0.81, P value=0.050). Tables
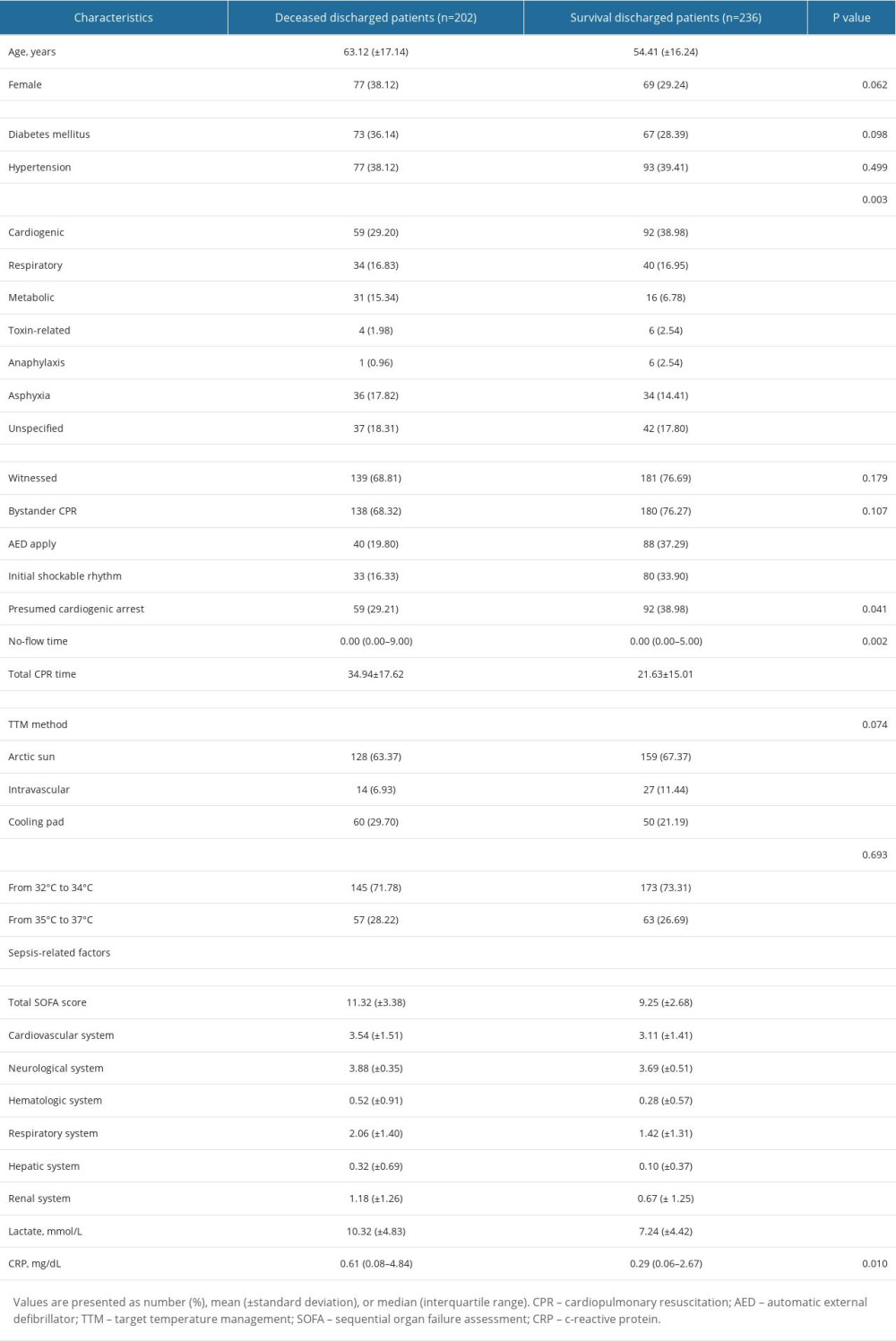 Table 1. Baseline characteristics of the study population.
Table 1. Baseline characteristics of the study population.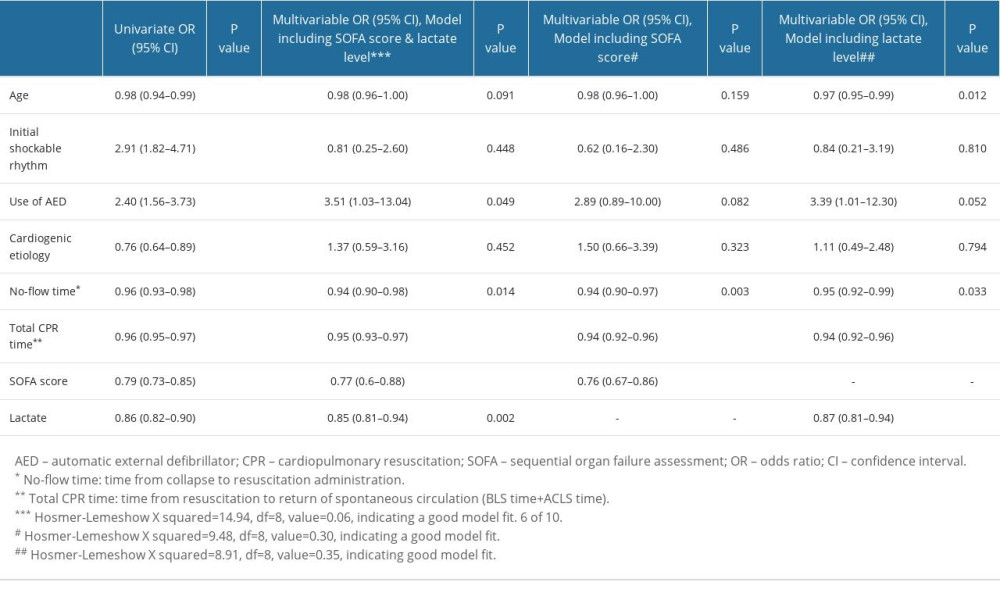 Table 2. Logistic regression models for survival outcomes.
Table 2. Logistic regression models for survival outcomes.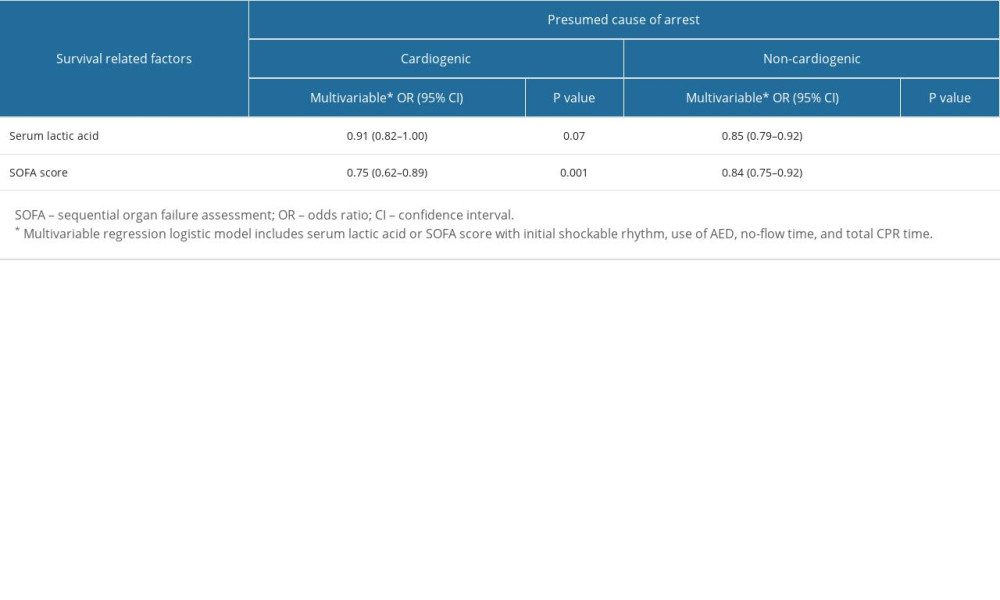 Table 3. Different effects of serum lactic acid and sequential organ dysfunction assessment (SOFA) score on survival prognosis according to presumed cause of arrest.
Table 3. Different effects of serum lactic acid and sequential organ dysfunction assessment (SOFA) score on survival prognosis according to presumed cause of arrest.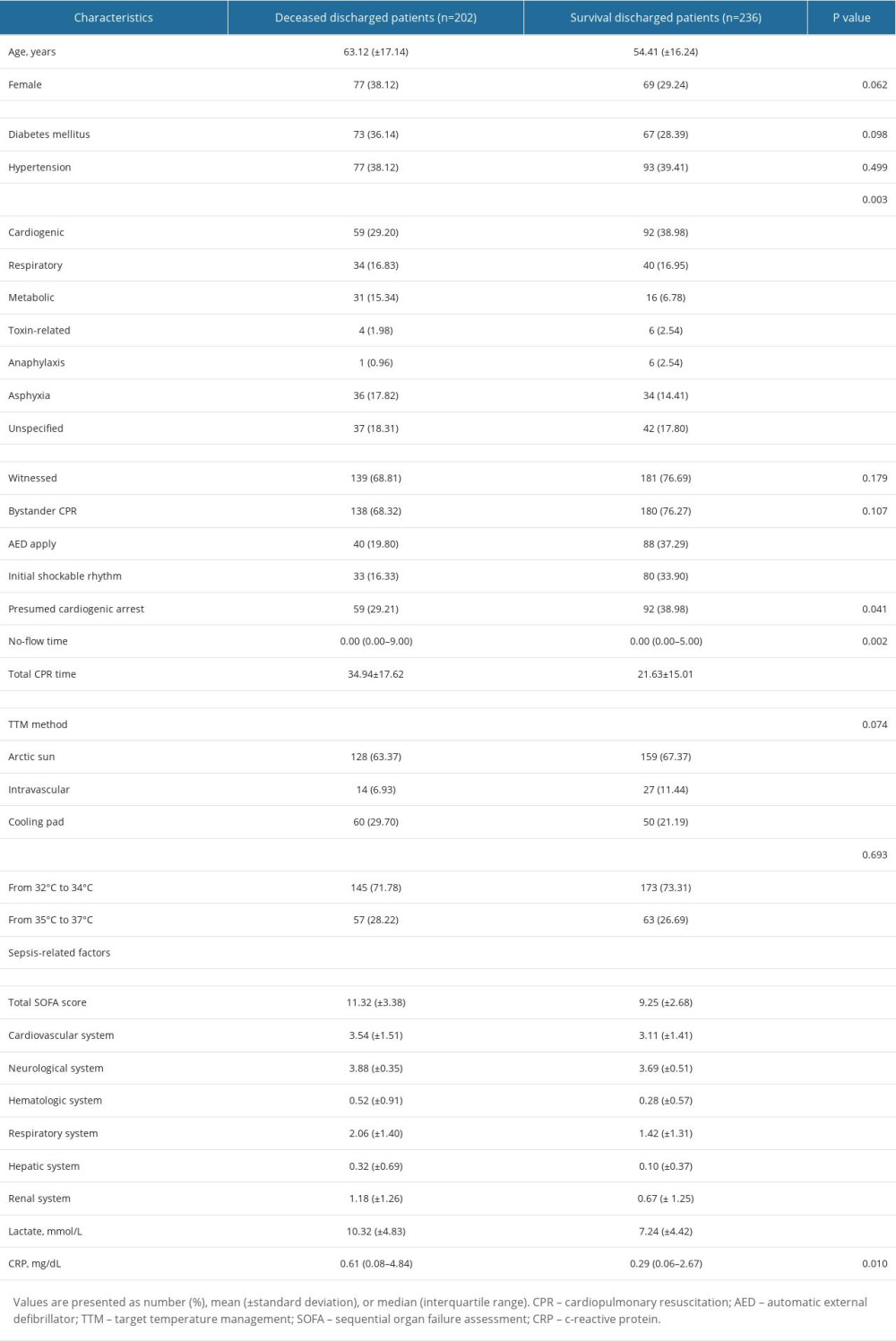 Table 1. Baseline characteristics of the study population.
Table 1. Baseline characteristics of the study population.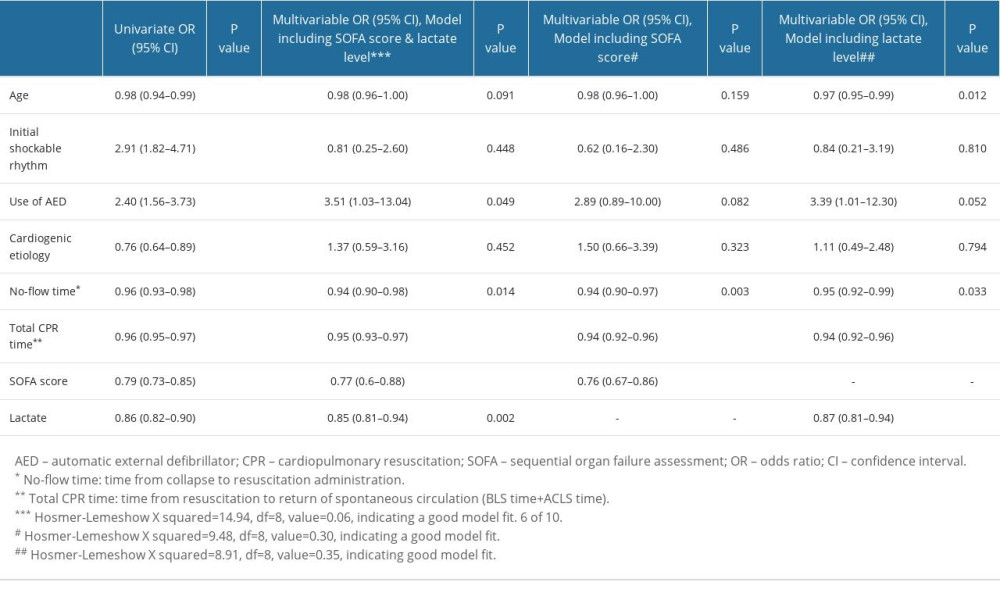 Table 2. Logistic regression models for survival outcomes.
Table 2. Logistic regression models for survival outcomes.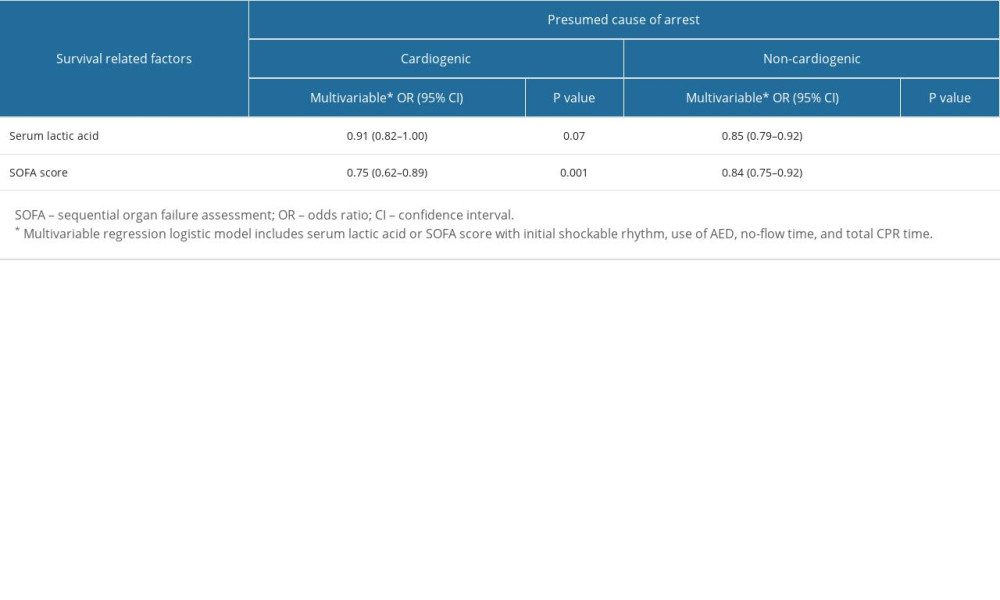 Table 3. Different effects of serum lactic acid and sequential organ dysfunction assessment (SOFA) score on survival prognosis according to presumed cause of arrest.
Table 3. Different effects of serum lactic acid and sequential organ dysfunction assessment (SOFA) score on survival prognosis according to presumed cause of arrest. In Press
12 Mar 2024 : Clinical Research
Metabolomic Alterations in Methotrexate Treatment of Moderate-to-Severe PsoriasisMed Sci Monit In Press; DOI: 10.12659/MSM.943360
14 Mar 2024 : Clinical Research
Renal Dysfunction Increases Risk of Adverse Cardiovascular Events in 5-Year Follow-Up Study of Intermediate...Med Sci Monit In Press; DOI: 10.12659/MSM.943956
15 Mar 2024 : Clinical Research
Impact of One-Lung Ventilation on Oxygenation and Ventilation Time in Thoracoscopic Heart Surgery: A Compar...Med Sci Monit In Press; DOI: 10.12659/MSM.943089
14 Mar 2024 : Clinical Research
Differential DHA and EPA Levels in Women with Preterm and Term Births: A Tertiary Hospital Study in IndonesiaMed Sci Monit In Press; DOI: 10.12659/MSM.943895
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952








