25 November 2023: Clinical Research
Risk Factors for Postoperative Knee Stiffness in Patients with Anteromedial Knee Osteoarthritis Undergoing Unicompartmental Knee Arthroplasty with Cemented Prostheses: A Short-Term, Retrospective, Case-Control Study
Congcong Wei1ABCDEF, Xihan Zhang1B, Mingming Dong2B, Boyi Lei1B, Jiangbo Zhao1B, Xiangdong Xi1B, Shuai Zhao1B, Baigang Zhou1AG*DOI: 10.12659/MSM.942440
Med Sci Monit 2023; 29:e942440
Abstract
BACKGROUND: The present study was performed to determine the potential risk factors for postoperative knee stiffness in patients with anteromedial knee osteoarthritis undergoing unicompartmental knee arthroplasty with cemented prostheses.
MATERIAL AND METHODS: This retrospective cohort study evaluated patients with anteromedial knee osteoarthritis who underwent medial unicompartmental knee arthroplasty at our hospital between May 2017 and May 2020. The patients were divided into 2 groups according to their prognosis: those who experienced knee stiffness after undergoing unicompartmental knee arthroplasty and those who did not. The factors associated with stiffness after UKA were identified using univariate analysis. Frequencies are used to express categorical variables, while mean±SD is used to express continuous variables. The t test and chi-square test were used. A multivariate logistic regression model was built to identify the risk factors for postoperative stiffness.
RESULTS: We included 590 knees in the study after unicompartmental knee arthroplasty. The overall incidence of postoperative stiffness in unicompartmental knee arthroplasty surgery was 10.17%. In terms of the radiological measurements, varus deformity (70.34% vs 29.66%) and tibial component posterior slope angle (4.8±2.0 vs 4.6±2.0, P<0.001) were significantly differences between the 2 groups. Four independent risk factors for stiffness after unicompartmental knee arthroplasty were identified: age (95% CI, 1.022-1.048), varus deformity (95% CI, 1.186-1.192), tibial component posterior slope angle (95% CI, 0.550-0.870), and preoperative maximum flexion (95% CI, 0.896-0.923).
CONCLUSIONS: The overall incidence of postoperative knee stiffness in patients with anteromedial knee osteoarthritis undergoing unicompartmental knee arthroplasty with cemented prostheses was 10.17%, which was at a moderate level compared to patients with other diseases undergoing unicompartmental knee arthroplasty. Four independent risk factors were identified: age, varus deformity, preoperative maximum flexion, and tibial component posterior slope angle. Awareness these risk factors might help surgeons prevent the occurrence of postoperative knee stiffness in patients with UKA.
Keywords: Arthroplasty, Replacement, Knee, Osteoarthritis, Knee, Postoperative Period, Risk Factors
Background
Unicompartmental knee arthroplasty (UKA) has a limited but proven indication for this procedure for the treatment of osteoarthritis of the knee involving isolated unicompartmental knee disease with normal anterior cruciate ligament (ACL) function [1]. For patients with end-stage degenerative and inflammatory arthritis who have failed conservative and nonoperative treatment, total knee arthroplasty is recommended [2]. According to Riddle et al [3], the proportion of unicompartmental knee arthroplasty was 6570 implants in 1998 and 44 990 implants in 2005. UKA grew at an average rate of 32.5% over the study period, with unicompartmental implants currently accounting for less than 8% of all knee replacement procedures. Mikkelsen et al reported that compared to total knee arthroplasty (TKA), medial UKAs has lower mortality rates, shorter hospital stays, is less invasive, has shorter operative times, higher satisfaction rates, lower infection rates, and fewer complications, and are more cost-effective for the treatment of medial anterior osteoarthritis [4]. Consequently, UKA is a surgical alternative that offers distinct advantages over other procedures [5].
UKA may not always provide satisfactory prognosis for patients who do not have a total knee arthroplasty with artificial joint implant [6]. Different cohorts have different incidences of stiffness in these types of knee joints. According to Fournier et al, the prevalence of stiffness treated with UKA was 9% at the 1-year follow-up [7]. Hurst et al revealed that 12% of patients experienced stiffness in their knee joints, which subsequently led to treatment failures [8]. Stiff knees can cause pain and limited function during daily activities, particularly when ascending or descending stairs, sitting or standing up, and tying shoelaces [9]. Meanwhile, more complex surgical procedures, such as surgical dissolution of scar tissue (arthroscopic or open surgery) or revision arthroplasty, are required in some recalcitrant cases to relieve pain and restore knee function [7]. We reviewed many studies. Knee stiffness can be disabling and is among the most common causes of patient dissatisfaction following UKA. The treatment of stiffness can range from aggressive physical therapy to revision arthroplasty [7,10–14]. Therefore, knowing how to reduce the incidence of knee stiffness after UKA has become crucial.
Researchers in the field of knee surgery are continuously investigating various factors that may contribute to postoperative knee stiffness following UKA [15,16]. Fournier et al retrospectively analyzed data from 240 patients undergoing UKA surgery. Robotic-assisted surgery was performed in 164 patients and mechanical instrumentation in 76 patients. They demonstrated that stiffness after UKA is correlated with mechanical instrumentation as a risk factor [7]. Researchers such as Saito et al have argued that inserting a component that is too thick into a narrow space can result in joint stiffness. Therefore, it is important to determine the different levels of tightness in the surrounding soft tissues after implantation [6]. The results above show that the knee stiffness after UKA is influenced by multiple factors, not just one. In this regard, it is worth noting that UKA typically exhibits a low incidence of stiffness [17,18]. Although the knee stiffness after UKA is a known complication [19], there is a lack of comprehensive literature on the potential multifactorial risks associated with this condition. This study aimed to fill this research gap by analyzing the potential factors that contribute to knee stiffness after UKA. Identifying independent risk factors for postoperative knee stiffness following UKA is crucial for developing effective treatment strategies that can improve patient outcomes. This will significantly improve patients’ quality of life after UKA and reduce healthcare costs due to postoperative stiffness, and will elucidate the mechanisms of the onset and development of postoperative stiffness in UKA.
Material and Methods
STUDY DESIGN:
This retrospective case-control study evaluated patients with anteromedial knee osteoarthritis who underwent medial UKA at our hospital between May 2017 and May 2020. Our evaluation of patients lasted 1 year. The patients were divided into 2 groups according to their prognosis: those who experienced knee stiffness after undergoing UKA and those who did not. Independent risk factors for knee stiffness after receiving UKA therapy were identified. These factors can help healthcare professionals make better-informed clinical decisions.
PARTICIPANTS:
The inclusion criteria were as follows: (1) patients who were diagnosed with anteromedial osteoarthritis and had radiological findings consistent with anteromedial osteoarthritis; (2) patients who underwent 1 UKA operations on a unilateral knee; (3) medical records and radiological examinations were available for identifying the demographic information, anatomical characteristics, and surgical procedure characteristics.
To calculate the sample size required in our study, we used the N ≥A+Bm rule. Green et al [20,21] reported that slightly more complex rules-of-thumb of the form that N ≥A+Bm show slightly better agreement with power analysis results.
The exclusion criteria were as follows: (1) patients who had been followed up for less than 1 year; (2) periprosthetic fractures occurring during patient follow-up; (3) patients who had previous knee surgery before and after UKA surgery. Based on the inclusion and exclusion criteria, 590 eligible patients were retrospectively screened and included in this study.
The study was approved by the Institutional Review Board of the No. 215 Hospital of Shaanxi Nuclear Industry and was conducted in accordance with the Declaration of Helsinki and the regulations of the Health Insurance Portability and Accountability Act (HIPAA).
The need for informed consent was waived because this was a retrospective study and all patient information was deidentified before the analysis.
It is important to note that the surgical indications for UKA include anteromedial osteoarthritis and osteonecrosis, which are often characterized by severe pain in the inner side of the knee [22].
DEMOGRAPHIC INFORMATION:
The medical records were used to extract demographic data about the patients, including age, sex, hypertension, BMI, smoking, osteoporosis, and diabetes.
CLINICAL EVALUATIONS: The preoperative Knee Society knee score (KSKS) and preoperative Knee Society functional score (KSFS) were documented and preoperative knee extension and flexion angles were measured by using a 2-arm goniometer with the patients in the supine position. In our study, pre- and postoperative knee range of motion measurements were performed and compared by a single observer. Severity of knee osteoarthritis were classified based on the Ahlback grade system [23]. The visual analog scale (VAS) was used to assess the patient’s pain symptoms before UKA. Preoperative activity level, preoperative maximum flexion, preoperative maximum extension, varus deformity, and preoperative hip-knee-ankle axis (HKA) angle were evaluated.
RADIOLOGICAL MEASUREMENTS: Before and after surgery, all patients had anterior–posterior view X-ray examinations of the knee and both lower extremities performed. To measure the coronal hip-knee-ankle (HKA) angles before and after the surgery, we performed full-length standing radiography. The Oxford partial knee surgical technique operating manual was used to assess the alignment of femoral and tibial components [24]. We also recorded femoral component position relative to the femur with varus/valgus, flexion/extension, tibial component position relative to the tibia with varus/valgus, and anterior–posterior slope. Flexion and varus in the femoral component as well as varus and posterior slope of the tibial component were considered positive values.
SURGICAL TECHNIQUES: All patients underwent surgery performed by the same surgical team, and the surgeries were all conducted by a highly skilled and experienced surgeon. All operations were done with a minimally invasive approach. With the knee in moderate flexion, an incision was made medial to midline, extending from the proximal pole of the patella to just medial to the tibial tubercle. The tibial alignment was set to 90 degrees to the mechanical axis in the frontal plane and 7 degrees to the posterior slope in the sagittal plane during osteotomy. Achieving a 90-degree angle with the mechanical axis in the frontal plane was the goal for femoral alignment, with flexion ranging from 5 to 15 degrees in the sagittal plane. This can be achieved using either the Phase 3 or Microplasty system. After the osteotomy procedures, we conducted gap balancing and employed the implantation technique (Figure 1).
POSTOPERATIVE REHABILITATION:
All patients were treated with the same rehabilitation protocols. All patients were instructed by healthcare professionals to perform quadriceps exercises 3 times daily, with approximately 20 repetitions each time. Specifically, each patient would sit in long sitting posture with the back against the wall. For a period of 10 seconds, the patient would perform a maximal active isometric contraction of the quadriceps with the ankle in a dorsiflexed position. Twenty repetitions per set, 3 repetitions per day, and 5 repetitions per week were performed for the isometric contraction. Each exercise activity was completed under the supervision of healthcare professionals during the hospitalization of all patients. The patients received both oral and written instructions for home exercises upon discharge from the hospital. As part of their instructions, they were also advised to perform ankle pump exercises promptly. This advice aimed to reduce the risks associated with deep vein thrombosis (DVT) and pulmonary embolism (PE), as well as enhance the tracking of the patella. On the first day after surgery, patients were encouraged to start partial weight bearing and engage in knee exercises that involve both assisted range of motion (ROM) and active participation.
OUTCOME OF INTEREST:
Stiffness after UKA is defined as flexion <90° or a flexion contracture >10° (lack of extension).
STATISTICAL ANALYSIS:
The statistical analysis was carried out using Excel 2016 for Windows (Microsoft Corporation, Seattle, WA, USA) and SPSS 19.0 statistical software for Windows (IBM, Armonk, NY, USA). The factors associated with stiffness after UKA were identified using univariate analysis. Frequency is used to express categorical variables, while mean±SD is used to express continuous variables. The
Results
DEMOGRAPHIC AND GENERAL INFORMATION:
We finally included 590 knees in the study after UKA, comprising 296 male and 294 female patients with knee osteoarthritis. At the 1-year follow-up, the incidence of postoperative stiffness in UKA surgery was 10.17%. There were no differences in the demographic and baseline characteristics between the 2 groups, including the body mass index (25.18±3.22 vs 25.03±3.10, P=0.356), sex (50.17% vs 49.83%, P=0.752), smoking (81.36% vs 18.64%, P=0.485), hypertension (89.66% vs 10.34%, P=0.793), OA degree (32.2% vs 67.8%, P=0.370), diabetes(90.68% vs 9.32%, P=0.613), preoperative KSFS (55.4±13.2 vs 50.4±19.7, P=0.081), osteoporosis (0.18±1.37 vs 0.19±1.39, P=0.957), preoperative activity level (39.83% vs 60.17%, P=0.122), preoperative KSKS (45.4±10.0 vs 43.4±10.0, P=0.052), preoperative maximum extension (4.9±4.4 vs 4.7±3.5, P=0.106), and VAS score (3.92±2.45 vs 4.08±2.50, P=0.759). There were significant differences in age (39.83% vs 60.17%, P<0.001) and preoperative maximum flexion (132.0±6.4 vs 126.8±7.2, P<0.001) between the 2 groups. The patients’ baseline characteristics are summarized in Tables 1 and 2.
In terms of the radiological measurements, none of the following radiological characteristics differed between the 2 groups: preoperative HKA angle (169.9±4.3 vs 169.6±4.1, P=0.112), postoperative HKA angle (175.3±3.0 vs 175.6±3.2, P=0.763), femoral component varus/valgus angle (1.3±3.3 vs 0.8±4.0, P=0.530), femoral component flexion/extension angle (12.6±3.5 vs 12.8±7.2, P=0.875) and tibial component varus/valgus angle (2.0±1.3 vs 2.4±1.3, P=0.536). Varus deformity (70.34% vs 29.66%, P<0.001) and tibial component posterior slope angle (4.8±2.0 vs 4.6±2.0, P<0.001) were observed to have significant differences between 2 groups. Tables 2 and 3 give a summary of the radiological characteristics of the patients.
INDEPENDENT RISK FACTORS:
Multivariate logistic regression was used to identify 4 independent risk factors for stiffness after UKA. Age was risk factor for stiffness after UKA. The likelihood of becoming stiff after a UKA increased by 3.5% with each year of increasing age (95% CI, 1.022–1.048). The risk factors for stiffness after UKA were varus deformity (95% CI, 1.186–1.192) and tibial component posterior slope angle (95% CI, 0.550–0.870) in the radiological measurements. Stiffness after UKA was associated with preoperative maximum flexion as another risk factor. The likelihood of stiffness after UKA increased by 9.1% for every 1 degree decrease in preoperative maximum flexion (95% CI, 0.896–0.923). The independent risk factors for stiffness after UKA are summarized in Table 4.
Discussion
LIMITATIONS:
There are some limitations of the study. Firstly, it was a single-center study where all surgeries were performed by the same group of surgeons. However, the influence of surgeons’ surgical skills could not be evaluated. Similarly, the effect of the degree of postoperative rehabilitation could not be assessed. Second, some anatomical and geometric characteristics of the knee were measured on standard X-ray images. Therefore, the projection position might affect the measurement accuracy. Finally, we assessed final outcomes at 1 year postoperatively, which is a relatively short period for evaluating postoperative outcomes. However, as we mainly focused on postoperative knee stiffness, not on the service life of the prosthesis, we believe that 1 year is sufficient to assess patient knee function. Further prospective studies and basic experiments are needed to clarify the mechanisms involved in developing and progressing postoperative stiffness in UKA.
Conclusions
Four independent risk factors were identified in this study: age, varus deformity, preoperative maximum flexion, and tibial component posterior slope angle. Comprehending these risk factors might help surgeons prevent the occurrence of these postoperative knee stiffness in patients with unicompartmental knee arthroplasty. Based on our research, we recommend the following steps to avoid postoperative knee stiffness in patients with anteromedial knee osteoarthritis undergoing unicompartmental knee arthroplasty. First, it is vital to emphasize the significance of perioperative rehabilitation exercises, which can aid in improving knee joint flexibility and overall function. Second, for patients with maximum flexion reduction before the operation and significant preoperative varus deformities, we recommend early intervention whenever possible. Finally, a higher posterior tibial slope could also be advantageous in preventing postoperative knee stiffness.
Tables
Table 1. General information on patients with knee osteoarthritis undergoing unicompartmental knee arthroplasty.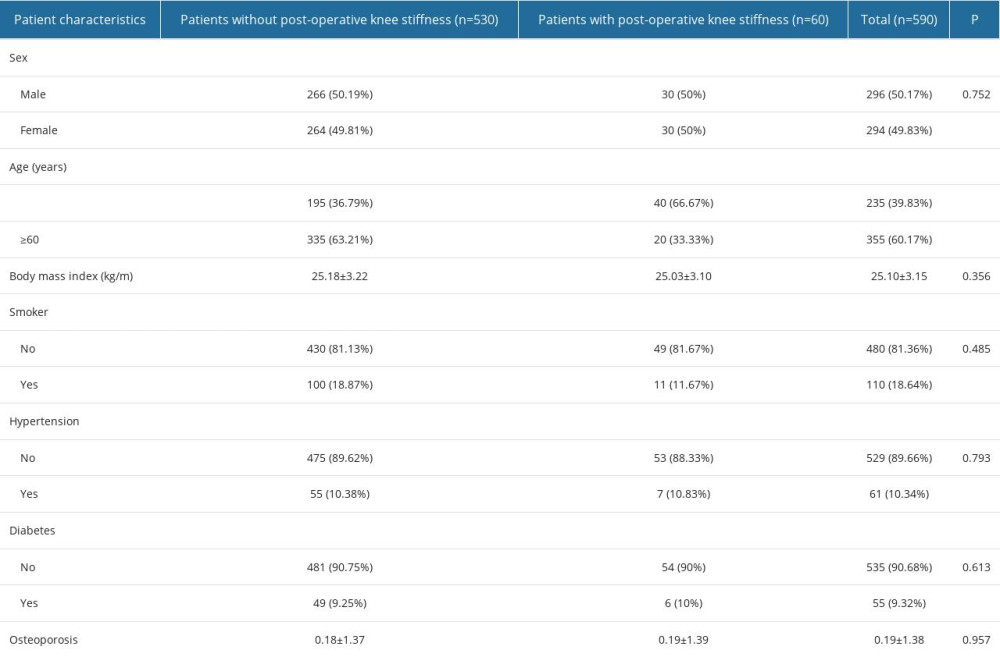 Table 2. Preoperative clinical results in patients with center knee osteoarthritis undergoing unicompartmental knee arthroplasty.
Table 2. Preoperative clinical results in patients with center knee osteoarthritis undergoing unicompartmental knee arthroplasty. Table 3. Results of radiological measurements in patients with center knee osteoarthritis undergoing unicompartmental knee arthroplasty.
Table 3. Results of radiological measurements in patients with center knee osteoarthritis undergoing unicompartmental knee arthroplasty.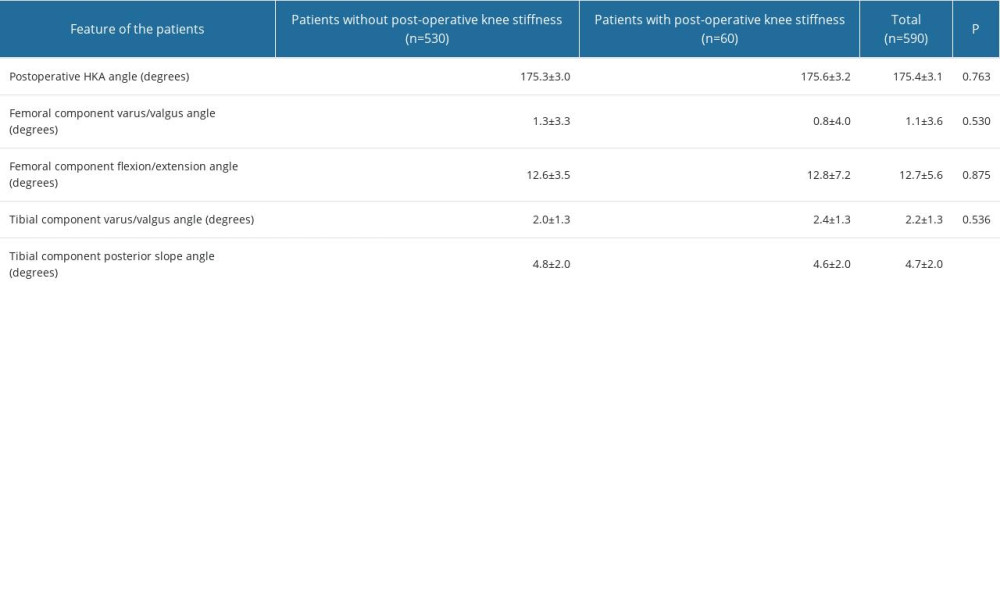 Table 4. Independent risk factors for postoperative knee stiffness in patients with knee osteoarthritis undergoing unicompartmental knee arthroplasty.
Table 4. Independent risk factors for postoperative knee stiffness in patients with knee osteoarthritis undergoing unicompartmental knee arthroplasty.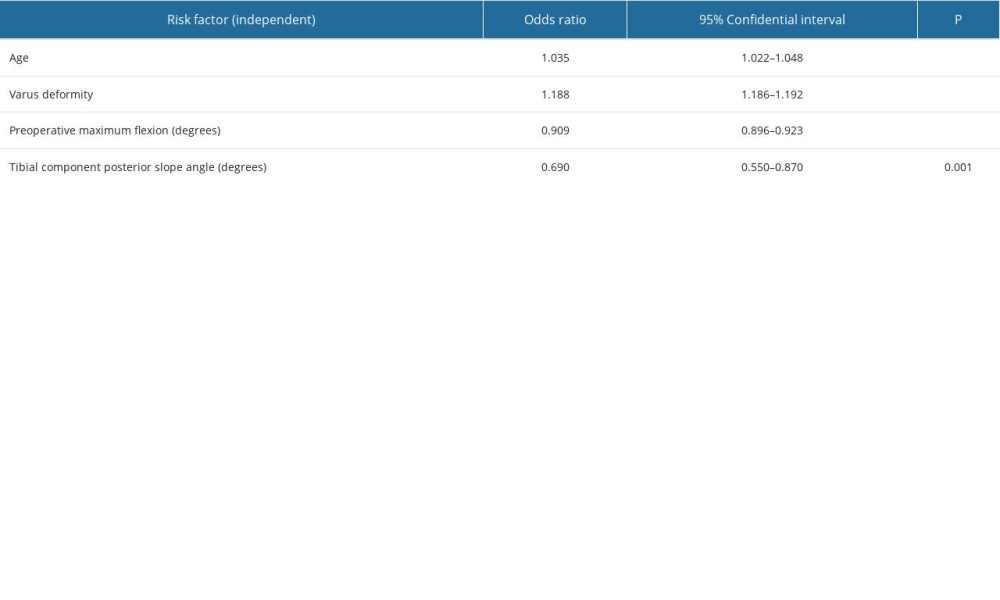
References
1. Tille E, Beyer F, Auerbach K, Tinius M, Lützner JJBMD, Better short-term function after unicompartmental compared to total knee arthroplasty: BMC Musculoskeletal Disorders, 2021; 22(1); 1-9
2. Tateishi H, Indications for total knee arthroplasty and choice of prosthesis: Japan Medical Association Journal, 2001; 44(4); 153-58
3. Riddle DL, Jiranek WA, McGlynn F, Yearly incidence of unicompartmental knee arthroplasty in the United States: J Arthroplasty, 2008; 23(3); 408-12
4. Mikkelsen M, Wilson HA, Gromov K, Comparing surgical strategies for end-stage anteromedial osteoarthritis: Total versus unicompartmental knee arthroplasty: Bone Jt Open, 2022; 3(5); 441-47
5. Karaca S, Erdem MN, Oztermeli A, Clinical and radiological results of oxford phase-3 medial unicompartmental knee arthroplasty: Cureus, 2019; 11(11); e6070
6. Saito T, Takeuchi R, Yamamoto K, Unicompartmental knee arthroplasty for osteoarthritis of the knee: remaining postoperative flexion contracture affecting overall results: J Arthroplasty, 2003; 18(5); 612-18
7. Fournier G, Gaillard R, Swan J, Stiffness after unicompartmental knee arthroplasty: Risk factors and arthroscopic treatment: SICOT J, 2021; 7; 35
8. Hurst JM, Ranieri R, Berend KR, Outcomes after arthroscopic evaluation of patients with painful medial unicompartmental knee arthroplasty: J Arthroplasty, 2018; 33(10); 3268-72
9. Hao K, Wei M, Ji G, Comparison of the imaging and clinical outcomes among the measured resection, gap balancing, and hybrid techniques in primary total knee arthroplasty: Orthop Surg, 2023; 15(1); 93-102
10. Sun X, Zheng S, A meta-analysis of unicompartmental knee arthroplasty revised to total knee arthroplasty versus primary total knee arthroplasty: J Orthop Surg Res, 2018; 13(1); 1-9
11. Wilson HA, Middleton R, Abram SG, Patient relevant outcomes of unicompartmental versus total knee replacement: Systematic review and meta-analysis: BMJ, 2019; 364; l352
12. Dyrhovden GS, Lygre SHL, Badawy M, Have the causes of revision for total and unicompartmental knee arthroplasties changed during the past two decades?: Clin Orthop Relat Res, 2017; 475; 1874-86
13. Hartman CW, Ting NT, Moric M, Revision total knee arthroplasty for stiffness: J Arthroplasty, 2010; 25(6); 62-66
14. Tay ML, McGlashan SR, Monk AP, Revision indications for medial unicompartmental knee arthroplasty: A systematic review: Arch Orthop Trauma Surg, 2022; 142(2); 301-14
15. Friesenbichler B, Item-Glatthorn JF, Wellauer V, Short-term functional advantages after medial unicompartmental versus total knee arthroplasty: Knee, 2018; 25(4); 638-43
16. Morris MJ, Molli RG, Berend KR, Lombardi AV, Mortality and perioperative complications after unicompartmental knee arthroplasty: Knee, 2013; 20(3); 218-20
17. Drager J, Hart A, Abou Khalil J, Shorter hospital stay and lower 30-day readmission after unicondylar knee arthroplasty compared to total knee arthroplasty: J Arthroplasty, 2016; 31(2); 356-61
18. Giordano L, Maffulli N, Morenghi E, A BMI above 30 results in satisfying outcomes in patients undergoing fixed-bearing lateral unicompartmental knee arthroplasty: Knee Surg Sports Traumatol Arthrosc, 2023; 31(3); 1106-12
19. Kim KT, Lee S, Lee JI, Kim JW, Analysis and treatment of complications after unicompartmental knee arthroplasty: Knee Surg Relat Res, 2016; 28(1); 46-54
20. Clarius M, Hauck C, Seeger JB, Correlation of positioning and clinical results in Oxford UKA: Int Orthop, 2010; 34; 1145-51
21. Johnstone SF, Tranovich MJ, Vyas D, Unicompartmental arthritis in the aging athlete: osteotomy and beyond: Curr Rev Musculoskelet Med, 2013; 6; 264-72
22. Zhang Q, Zhang Q, Guo W, The learning curve for minimally invasive Oxford phase 3 unicompartmental knee arthroplasty: Cumulative summation test for learning curve (LC-CUSUM): J Orthop Surg Res, 2014; 9; 81
23. Ahlback SJARD, Osteoarthrosis of the knee. A radiographic investigation: Acta Radiol Diagn (Suppl), 1968; 277; 7-72
24. Clarius M, Hauck C, Seeger JB, Correlation of positioning and clinical results in Oxford UKA: Int Orthop, 2010; 34; 1145-51
25. Johnstone SF, Tranovich MJ, Vyas D, Wright VJ, Unicompartmental arthritis in the aging athlete: Osteotomy and beyond: Curr Rev Musculoskelet Med, 2013; 6; 264-72
26. Jordan L, Kligman M, Sculco TP, Total knee arthroplasty in patients with poliomyelitis: J Arthroplasty, 2007; 22(4); 543-48
27. Tirveilliot F, Migaud H, Gougeon FManagement of stiffness after total knee arthroplasty: Indication for different mobility management in 62 cases: Rev Chir Orthop Reparatrice Appar Mot, 2003; 89(1); 27-34 [in French]
28. Kim J, Nelson CL, Lotke PAJJ, Stiffness after total knee arthroplasty: Prevalence of the complication and outcomes of revision: JBJS, 2004; 86(7); 1479-84
29. Ahmed T, Haboubi N, Ciia J, Assessment and management of nutrition in older people and its importance to health: Clin Interv Aging, 2010; 5; 207-16
30. Özüdoğru A, Gelecek N, Effects of closed and open kinetic chain exercises on pain, muscle strength, function, and quality of life in patients with knee osteoarthritis: Rev Assoc Med Bras (1992), 2023; 69; e20230164
31. Zhu S, Zhang X, Chen X, Degree of coronal alignment correction can’t predict knee function in total knee replacement: BMC Surg, 2021; 21; 383
32. Magnussen RA, Weppe F, Demey G, Residual varus alignment does not compromise results of TKAs in patients with preoperative varus: Clin Orthop Relat Res, 2011; 469; 3443-50
33. Kahlenberg CA, Trivellas M, Lee Y-Y, Padgett DE, Preoperative valgus alignment does not predict inferior outcome of total knee arthroplasty: HSS J, 2018; 14(1); 50-54
34. Su EP, Su SL, Valle AGDJO, Stiffness after TKR: How to avoid repeat surgery: Orthopedics, 2010; 33(9); 658
35. Schiavone Panni A, Cerciello S, Traumatology. Stiffness in total knee arthroplasty: J Orthop Traumatol, 2009; 10(3); 111-18
36. Gandhi R, de Beer J, Leone J, Predictive risk factors for stiff knees in total knee arthroplasty: J Arthroplasty, 2006; 21(1); 46-52
37. Rauzi MR, Foran JR, Bade MJJP, Multimodal conservative management of arthrofibrosis after total knee arthroplasty compared to manipulation under anesthesia: A feasibility study with retrospective cohort comparison: Pilot Feasibility Stud, 2022; 8(1); 71
38. Goldberg SR, Ounpuu S, Arnold AS, Kinematic and kinetic factors that correlate with improved knee flexion following treatment for stiff-knee gait: J Biomech, 2006; 39(4); 689-98
39. Hada M, Mizu-Uchi H, Okazaki K, Posterior tibial slope and anterior post-cam contact can change knee kinematics in extension in bi-cruciate stabilized total knee arthroplasty: Bone Joint Res, 2020; 9(11); 761-67
40. Shi X, Shen B, Kang P, The effect of posterior tibial slope on knee flexion in posterior-stabilized total knee arthroplasty: Knee Surg Sports Traumatol Arthrosc, 2013; 21; 2696-703
41. Okamoto S, Mizu-uchi H, Okazaki K, Effect of tibial posterior slope on knee kinematics, quadriceps force, and patellofemoral contact force after posterior-stabilized total knee arthroplasty: J Arthroplasty, 2015; 30(8); 1439-43
42. Elyasi E, Cavalié G, Perrier A, A systematic review on selected complications of open-wedge high tibial osteotomy from clinical and biomechanical perspectives: Appl Bionics Biomech, 2021; 2021; 9974666
43. Anchustegui N, Grimm NL, Milbrandt TA, Medial and lateral posterior tibial slope in the skeletally immature: A cadaveric study: Orthop J Sports Med, 2022; 10(4); 23259671221088331
44. Marra MA, Strzelczak M, Heesterbeek PJ, Anterior referencing of tibial slope in total knee arthroplasty considerably influences knee kinematics: A musculoskeletal simulation study: Knee Surg Sports Traumatol Arthrosc, 2018; 26; 1540-48
45. Bakaa N, Chen LH, Carlesso L, Reporting of post-operative rehabilitation interventions for Total knee arthroplasty: A scoping review: BMC Musculoskelet Disord, 2021; 22(1); 602
46. Ekhtiari S, Bozzo A, Madden K, Unicompartmental knee arthroplasty: survivorship and risk factors for revision: A population-based cohort study with minimum 10-year follow-up: J Bone Joint Surg Am, 2021 [Online ahead of print]
47. Mistry JB, Elmallah RD, Bhave A, Rehabilitative guidelines after total knee arthroplasty: A review: J Knee Surg, 2016; 29(3); 201-17
48. Blasco J-M, Hernández-Guillen D, Domínguez-Navarro F, Sensorimotor training prior total knee arthroplasty and effects on functional outcome: A systematic review and meta-analysis: Gait Posture, 2021; 86; 83-93
49. Held MB, Boddapati V, Sarpong NO, Operative duration and short-term postoperative complications after unicompartmental knee arthroplasty: J Arthroplasty, 2021; 36(3); 905-9
50. Winkler T, Bell L, Bender A, Periarticular muscle status affects in vivo tibio-femoral joint loads after total knee arthroplasty: Front Bioeng Biotechnol, 2023; 11; 1075357
51. Ishii Y, Noguchi H, Sato J, Preoperative characteristics and intraoperative factors do not correlate with accomplishments of active straight-leg raising, standing up, and walking after primary total knee arthroplasty: J Orthop Surg Res, 2021; 16(1); 487
52. Szilágyiné Lakatos T, Lukács B, Veres-Balajti I, Cost-effective healthcare in rehabilitation: Physiotherapy for total endoprosthesis surgeries from prehabilitation to function restoration: Int J Environ Res Public Health, 2022; 19(22); 15067
53. Husted RS, Troelsen A, Thorborg K, Efficacy of pre-operative quadriceps strength training on knee-extensor strength before and shortly following total knee arthroplasty: Protocol for a randomized, dose-response trial (The QUADX-1 trial): Trials, 2018; 19; 47
Tables
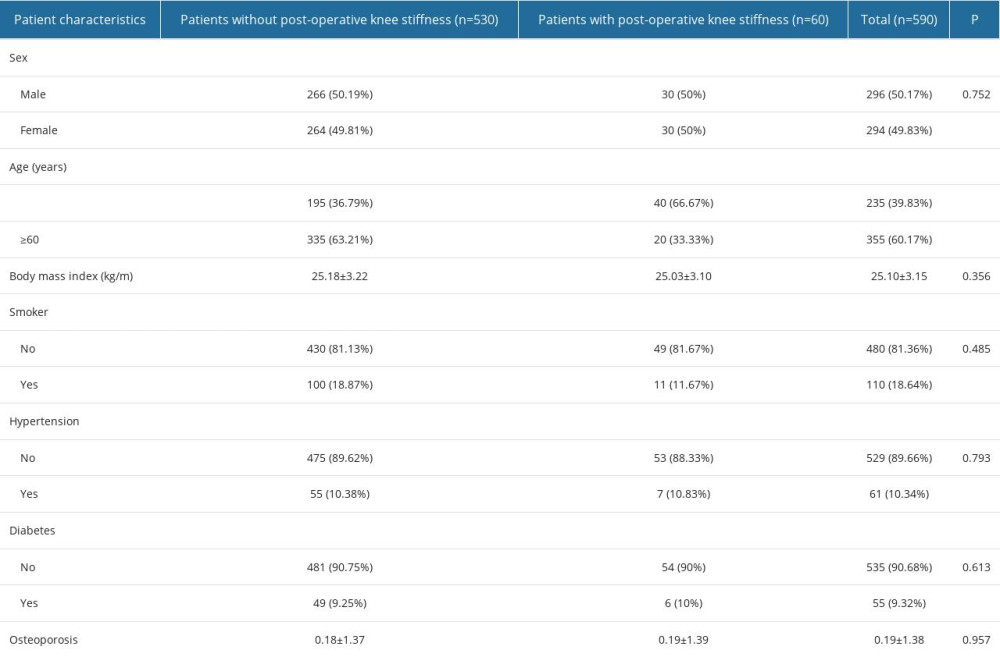 Table 1. General information on patients with knee osteoarthritis undergoing unicompartmental knee arthroplasty.
Table 1. General information on patients with knee osteoarthritis undergoing unicompartmental knee arthroplasty. Table 2. Preoperative clinical results in patients with center knee osteoarthritis undergoing unicompartmental knee arthroplasty.
Table 2. Preoperative clinical results in patients with center knee osteoarthritis undergoing unicompartmental knee arthroplasty.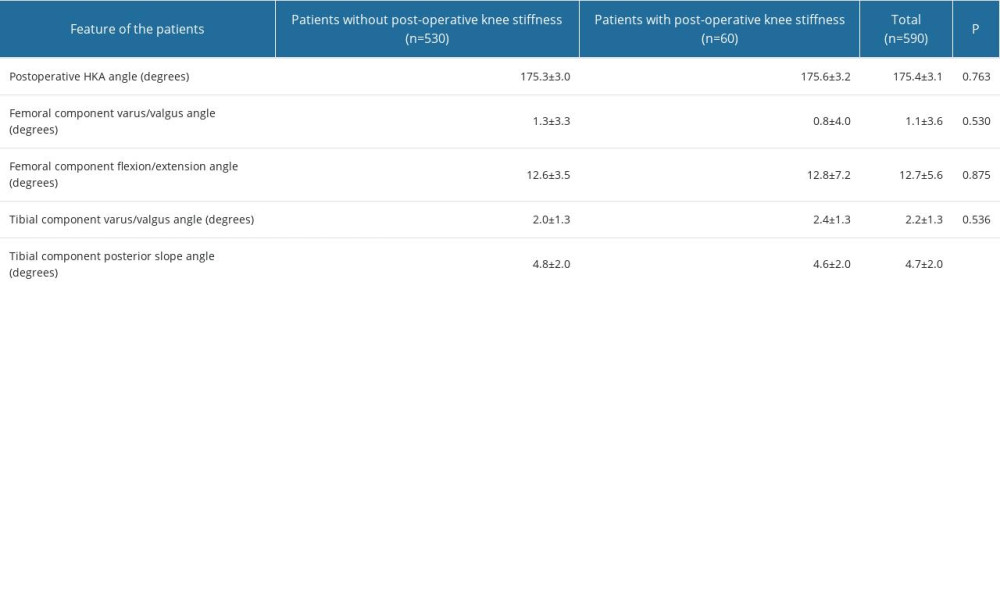 Table 3. Results of radiological measurements in patients with center knee osteoarthritis undergoing unicompartmental knee arthroplasty.
Table 3. Results of radiological measurements in patients with center knee osteoarthritis undergoing unicompartmental knee arthroplasty.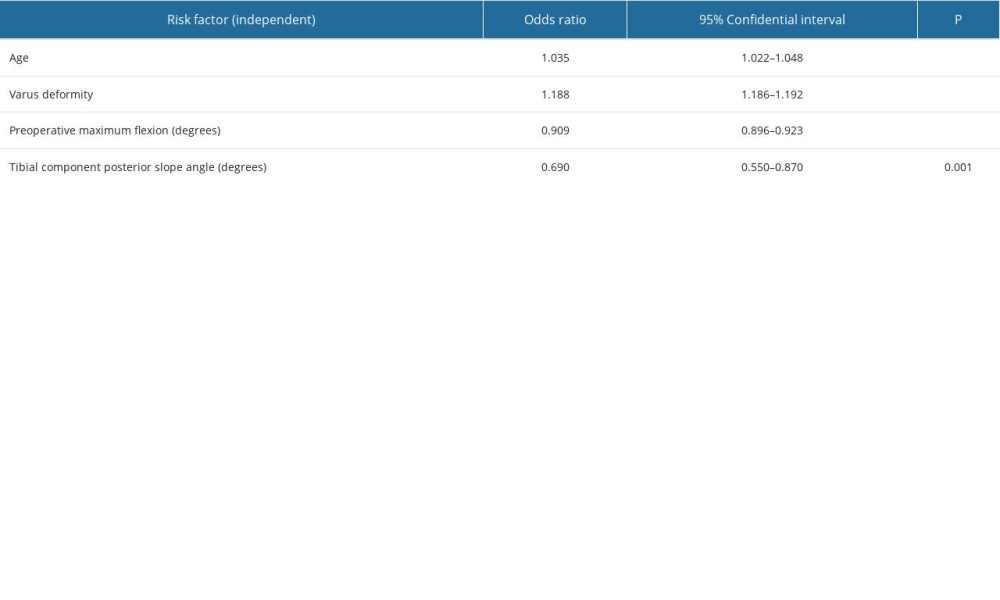 Table 4. Independent risk factors for postoperative knee stiffness in patients with knee osteoarthritis undergoing unicompartmental knee arthroplasty.
Table 4. Independent risk factors for postoperative knee stiffness in patients with knee osteoarthritis undergoing unicompartmental knee arthroplasty.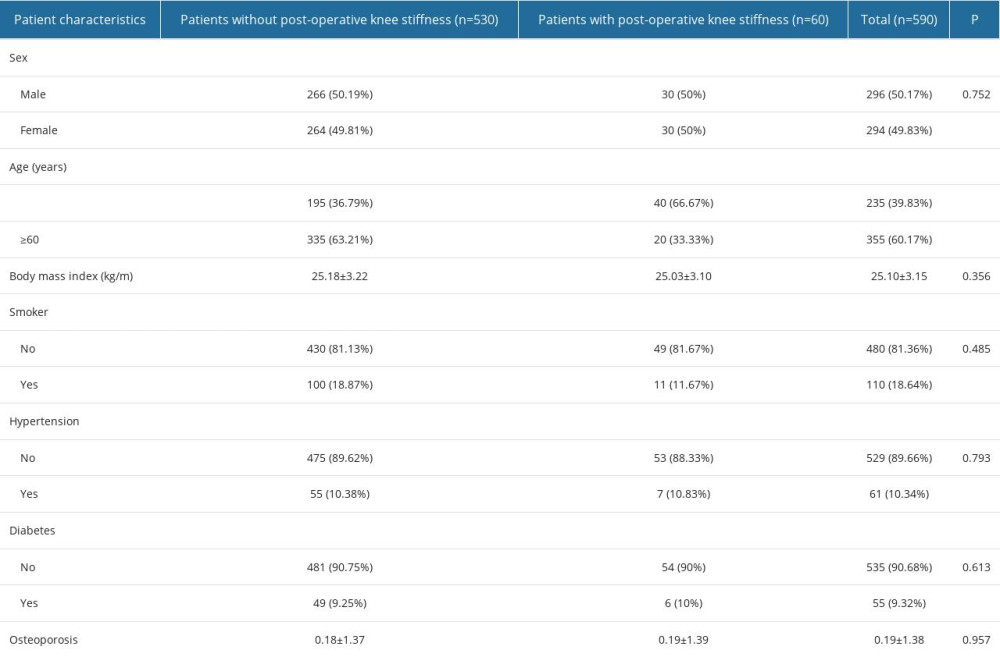 Table 1. General information on patients with knee osteoarthritis undergoing unicompartmental knee arthroplasty.
Table 1. General information on patients with knee osteoarthritis undergoing unicompartmental knee arthroplasty. Table 2. Preoperative clinical results in patients with center knee osteoarthritis undergoing unicompartmental knee arthroplasty.
Table 2. Preoperative clinical results in patients with center knee osteoarthritis undergoing unicompartmental knee arthroplasty.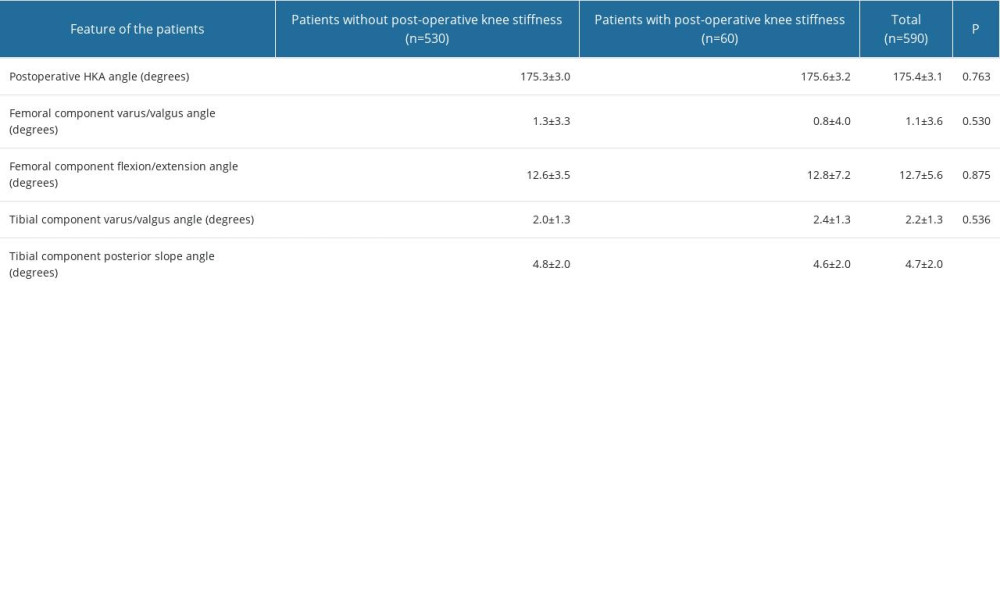 Table 3. Results of radiological measurements in patients with center knee osteoarthritis undergoing unicompartmental knee arthroplasty.
Table 3. Results of radiological measurements in patients with center knee osteoarthritis undergoing unicompartmental knee arthroplasty.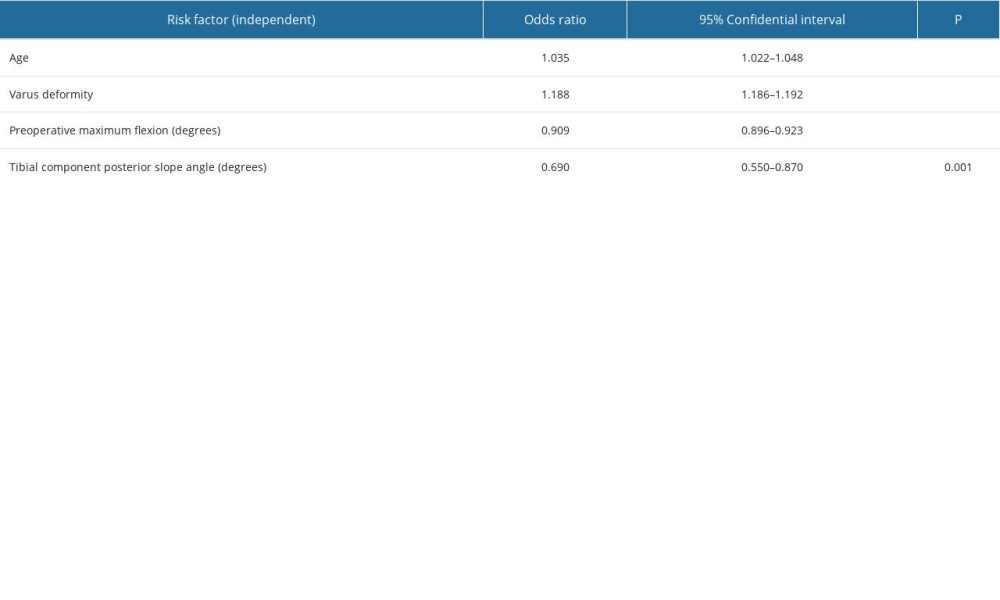 Table 4. Independent risk factors for postoperative knee stiffness in patients with knee osteoarthritis undergoing unicompartmental knee arthroplasty.
Table 4. Independent risk factors for postoperative knee stiffness in patients with knee osteoarthritis undergoing unicompartmental knee arthroplasty. In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952









