21 March 2024: Clinical Research
Factors Influencing the Occurrence of Intraoperative Hypothermia in Patients Undergoing General Anesthesia Intervention: A Study in a Tertiary Care Hospital
Huiqiong Yang1ABE*, Sang Gu1ACD, Juan Fan1AEF, Wei Li1ADGDOI: 10.12659/MSM.943463
Med Sci Monit 2024; 30:e943463
Abstract
BACKGROUND: Intraoperative and postoperative hypothermia of patients can be caused by the use of anesthetic drugs and the complicated and time-consuming procedures of interventional surgery. This retrospective study included 184 patients to investigate the incidence and factors associated with hypothermia during intraoperative anesthesia in a single center in China between January and October 2023.
MATERIAL AND METHODS: A convenient sampling method was used to select 184 patients who underwent general anesthesia intervention in a tertiary hospital in Sichuan Province from January to October 2023 as the study population. The independent factors influencing the occurrence of intraoperative hypothermia were analyzed. A survey was conducted to collect 5 demographic factors, 4 preoperative-related factors, and 10 surgically related factors. According to the occurrence of intraoperative hypothermia, the independent influencing factors of unplanned hypothermia during perioperative period were further analyzed.
RESULTS: Among 184 patients, 64 (34.78%) experienced perioperative unplanned hypothermia, of which 5 (7.81%) cases occurred before the start of surgery, 7 (10.94%) occurred before the start of surgery after anesthesia, and 52 (81.25%) occurred during surgery. Logistic regression analysis showed that body temperature at the beginning of surgery (P<0.001), set operating room temperature (P<0.001), duration of anesthesia (P=0.006), and age (P=0.001) were independent influencing factors for unplanned hypothermia during perioperative period.
CONCLUSIONS: The incidence of intraoperative hypothermia is high in patients undergoing general anesthesia interventions. Age, duration of anesthesia, set operating room temperature, and body temperature at the beginning of the operation were independent influencing factors for the occurrence of unplanned hypothermia during the perioperative period.
Keywords: Radiology, Interventional, Hypothermia, Risk Factors, Anesthesia
Introduction
Inadvertent perioperative hypothermia (IPH) is an inadvertent perioperative core body temperature lower than 36 °C due to various reasons [1]. It is a recognized and common complication in the perioperative period. Prevention is the best management method [2]. The incidence of perioperative hypothermia is high (7–90%), with 39.9% reported in Beijing in 2015 and 44.5% reported in a cross-sectional investigation in 2017 [3–5]. Hypothermia can enhance the discomfort of patients during anesthesia and recovery, such as reducing metabolism of anesthetic drugs and delaying recovery. Increased incidence of adverse events, such as infection and wound complications, cardiovascular complications, decreased coagulation, and increased need for blood transfusions, can occur [6,7]. With the development of medical technology, interventional surgery has been widely used in clinical practice because of its lower trauma and faster recovery [8]. However, due to the use of anesthetic drugs and the complicated and time-consuming procedures of interventional surgery, intraoperative and postoperative hypothermia of patients can be caused, and the problem of intraoperative hypothermia of patients undergoing interventional surgery under general anesthesia requires urgent attention [9,10]. The current research on intraoperative hypothermia mostly focuses on open surgery, such as gastrointestinal surgery, orthopedics, thoracic obstetrics, and gynecology, and focuses on the application of thermal insulation equipment and nursing intervention, and there are no relevant studies on the current occurrence of hypothermia during interventional surgery and its influencing factors [11–13]. Therefore, this retrospective study included 184 patients to investigate the incidence and related factors of hypothermia during anesthesia in a single center in China from January to October 2023.
Material and Methods
STUDY DESIGN:
The investigators wrote the study protocol and submitted the informed consent form and other materials to the Biomedical Ethics Review Committee of West China Hospital of Sichuan University, which approved the study after strict review and modification (approval number: 2021541). The investigators informed all patients of the purpose and methods of the study before surgery, clarified the patients’ informed consent, and instructed them to sign the informed consent form.
Patients undergoing general anesthesia interventional surgery in a grade III hospital in Sichuan Province from January 2023 to October 2023 were selected by a convenience sampling method as the study participants. The inclusion criteria were as follows: (1) patients who planned to undergo interventional surgery under general anesthesia; (2) age ≥18 years old; and (3) clear consciousness and ability to communicate normally. The exclusion criteria were as follows: (1) preoperative core body temperature >37.5°C due to infectious diseases and other reasons; (2) serious complications occurred during perioperative period, such as intraperitoneal hemorrhage and ruptured intracranial aneurysm; (3) patients undergoing re-operation within 24 h; and (4) cognitive impairment or communication disorder.
The sample size was calculated as follows. The number of positive samples was taken from 5 to 10 times the number of variables. Through systematic literature review and expert consultation, we identified 20 factors that can affect IPH. Therefore, the number of positive samples was 100 to 200, and the incidence of hypothermia was 44.3% to 72.7%, while 58.5% was taken in this study. The final sample size should be 170 to 341 cases. In this study, a total of 190 patients met the inclusion criteria, including 2 patients who refused to participate and 4 patients who were missing important data items; a total of 184 patients were included in this study.
DETA COLLECTION:
The collected data included 5 demographic factors (age, sex, height, weight, body mass index), 4 preoperative related factors (preoperative fasting time, preoperative basal body temperature, preoperative heart rate, preoperative blood pressure), and 10 operation-related factors (American Society of Anesthesiologists classification, operation name, operation time, anesthesia time, intraoperative fluid replacement, intraoperative fluid loss, set operating room temperature, warming duration, post-anesthesia body temperature, temperature at beginning of surgery).
To ensure the consistency of the study, the investigators involved in this study were trained in the use of the electronic medical record system and the general questionnaire filling method. The investigators obtained the general information of the patients through the hospital electronic medical record system before the operation, and obtained the temperature information of the operating room through the temperature and humidity control system of the operating room. Surgery-related information was reviewed by the investigator after surgery and filled in according to the anesthesia record sheet. Each questionnaire was completed on the day of the end of the operation and was handed over to a designated person for custody, with 10% of the patient data taken for review.
HYPOTHERMIA COMPLICATIONS AND MANAGEMENT:
A perioperative core body temperature below 36°C due to various reasons is known as perioperative hypothermia, also known as perioperative accidental hypothermia [14]. Hypothermia is caused when the body gives off more heat than it absorbs or produces, resulting in the body’s inability to produce enough heat to maintain a sufficient temperature for normal functioning. Although the underlying causes of accidental hypothermia are excessive cold stress and insufficient heat production by the body (thermogenesis), there are other factors that increase the risk of hypothermia [15]. Perioperative hypothermia can have a variety of deleterious effects, such as cardiac arrhythmias and ischemia, increased peripheral vascular resistance, leftward shift of the hemoglobin-oximetry curve, reversible coagulation dysfunction (platelet dysfunction), postoperative proteolytic metabolism, altered stress response, altered mental status, impaired renal function, decreased medication metabolism, decreased incidence of wound healing, and increased incidence of infection [16]. Once hypothermia has occurred, it is important that the patient be rewarmed promptly to minimize potential complications. There are several interventions that can be used to rewarm the patient. Active heating, particularly forced air heating, appears to reduce the clinically important time it takes for patients with postoperative hypothermic to reach normothermia (between 36°C and 37.5°C) [17].
STATISTICAL METHODS:
All information obtained was organized on an Excel spreadsheet (Microsoft, Redmond, WA, USA) and analyzed using SPSS version 26.0 (IBM Corp, Armonk, NY, USA). Measurements were expressed as mean±standard deviation, and
Results
GENERAL INFORMATION OF PATIENTS:
A total of 184 patients undergoing interventional surgery under general anesthesia were included in this study, including 77 men (41.85%) and 107 women (58.15%), aged 24 to 85 (56.72±12.09) years old. A total of 139 patients (75.54%) underwent cerebrovascular surgery and 45 patients (24.46%) underwent digestive system surgery.
OCCURRENCE OF HYPOTHERMIA DURING SURGERY:
IPH occurred in 64 of the 184 patients (34.78%), with 5 (7.81%) cases occurring before the operation, 7 (10.94%) before the operation after anesthesia, and 52 (81.25%) during the operation.
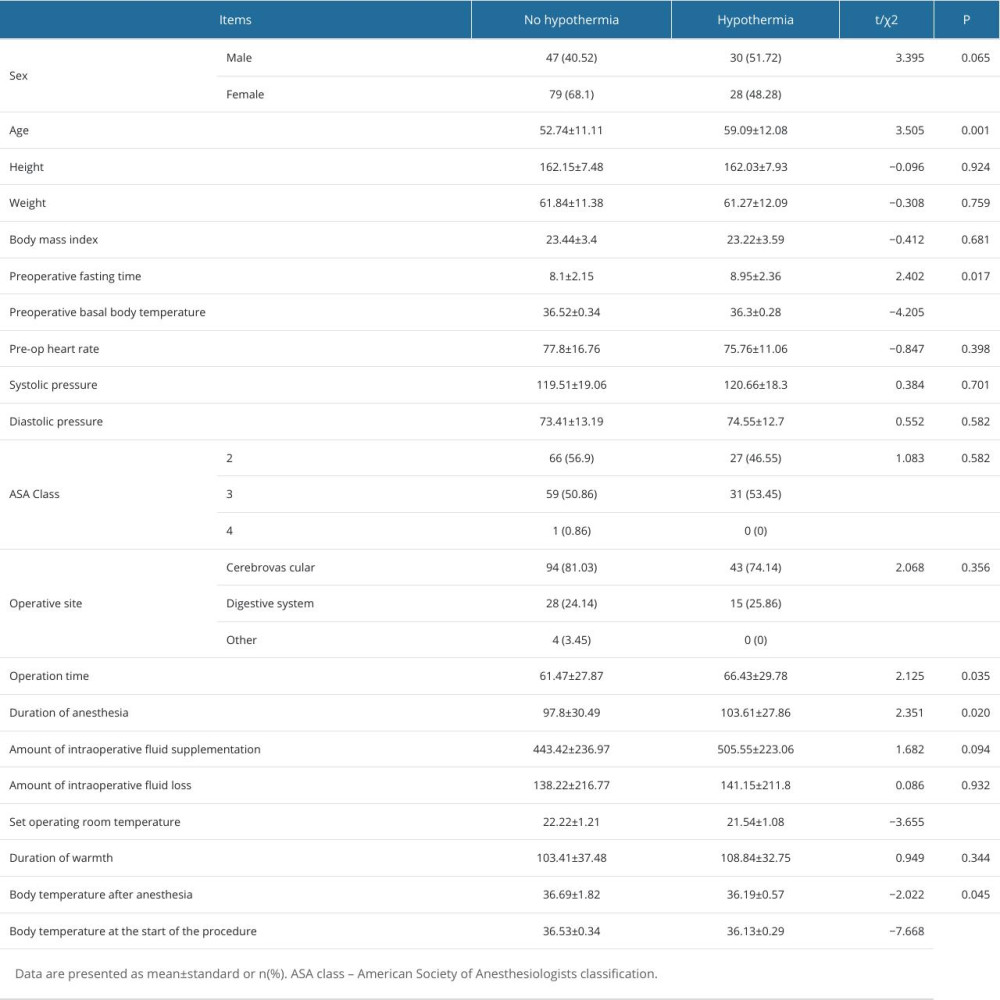
UNIVARIATE ANALYSIS OF INTRAOPERATIVE HYPOTHERMIA IN PATIENTS:
The occurrence of intraoperative hypothermia in patients undergoing interventional surgery under general anesthesia was taken as the dependent variable, and socio-demographic characteristics, preoperative relevant characteristics, operative relevant characteristics, and anesthesia characteristics were taken as independent variables. The results showed that set operating room temperature, preoperative fasting time, age, operation time, anesthesia time, preoperative core body temperature, post-anesthesia body temperature, and body temperature at the beginning of surgery were the influencing factors for the occurrence of intraoperative hypothermia in patients with general anesthesia intervention (P<0.05), as shown in Table 1.
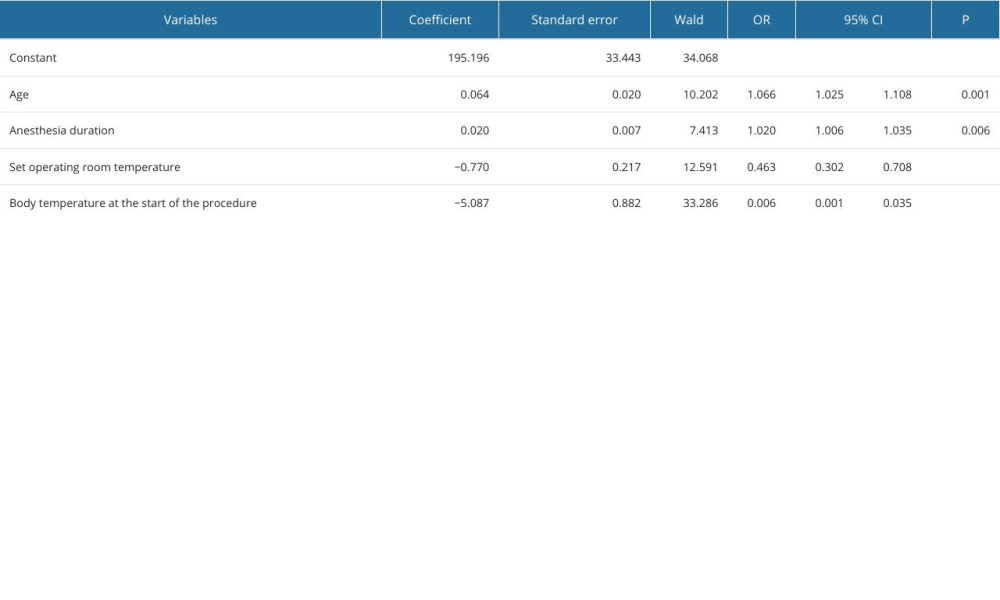
The variables with P<0.05 in the univariate analysis were taken as independent variables and the occurrence of IPH was taken as the dependent variable for logistic regression analysis. The results showed that age, duration of anesthesia, set operating room temperature, and body temperature at the beginning of the operation were independent influencing factors of IPH, as shown in Table 2.
Discussion
We conducted a retrospective single-center study to determine the risk factors of hypothermia in patients undergoing interventional surgery under general anesthesia. Our results showed that age, duration of anesthesia, set operating room temperature, and body temperature at the beginning of the operation were closely related to the occurrence of hypothermia during the operation. Our research showed that IPH occurred in 64 of 184 patients (34.78%), with 5 (7.81%) cases before the operation, 7 (10.94%) before the operation after anesthesia, and 52 (81.25%) during the operation. Our findings were similar to those of Frisch et al, who found the incidence of intraoperative hypothermia in patients was 32.6% to 43.9% [18].
Our study included patients aged 24 to 85 years, with a mean age of 56±12.09 years. The mean age of the intraoperative hypothermia group was 59.09±12.08 years, and the mean age of the group without hypothermia was 52.74±11.11 years, with a significant difference between the 2 groups (
In this study, the hypothermia group had a longer anesthesia time than did the group without hypothermia, and results showed that prolonged anesthesia time was an important factor in the development of intraoperative hypothermia in patients, which is consistent with the results of Emmert et al [21]. The longer the duration of anesthesia, the more likely the occurrence of intraoperative hypothermia. When the duration of anesthesia ≥3 h, the risk of hypothermia increased by 4.02 times [22]. This may be related to peripheral vascular dilation after anesthesia, which can easily lead to hypotension. At the same time, with prolonged anesthesia, the body temperature regulation center is inhibited, and the reflex is dull, which can easily lead to hypothermia. It is recommended to enhance intraoperative monitor and record the patient’s body temperature before and during anesthesia induction. If the operation is difficult and the duration of anesthesia is expected to be long, family members and relevant medical staff should be informed in advance and insulation measures should be taken.
The set operating room temperature was an influential factor for hypothermia during general anesthesia intervention, which is consistent with the results of Li et al [23]. In clinical work, the temperature of an interventional operating room is usually set at 20°C to 23°C. However, relevant studies have shown that when the ambient temperature is less than 23°C, the risk of patients with hypothermia increases [24,25]. During surgery, we should dynamically adjust the operating room temperature according to the actual situation, such as the season and the thermal comfort of patients, to reduce the heat dissipation of the patient’s body. Meanwhile, body temperature at the beginning of surgery was also an influential factor in the present study, which is consistent with the results of Moola et al [26]. Previous studies have shown that when the preoperative body temperature is higher, the temperature difference between the peripheral skin and core is smaller. The decrease of redistribution of core heat can reduce the occurrence of hypothermia [27]. Moola et al reported that taking warming measures before surgery to prevent hypothermia before surgery could prevent intraoperative hypothermia, which was consistent with the conclusion in the present study, that body temperature at the beginning of surgery affected the occurrence of intraoperative hypothermia. Therefore, we should take effective thermal insulation measures during the whole process of preoperative preparation, transportation, waiting, and entering the operating room [28].
As an observational study, this study had a few limitations. This was a single-center study, there may have been information bias and patient selection bias in the process of data collection, and the sample size was limited. Patient temperature values were derived from electronically captured intraoperative clinical data. Although the use of electronic data capture can reduce human error, it can occasionally introduce spurious values due to increased oral secretions or sensor translocation. The extrapolation of the results still needs to be further verified by multi-center data. In addition, risk prediction tools for intraoperative hypothermia suitable for different surgeries should be further constructed in the future to lay a foundation for accurate intervention of intraoperative hypothermia.
Conclusions
The incidence of intraoperative hypothermia in patients undergoing general anesthesia is high. Age, duration of anesthesia, set operating room temperature, and body temperature at the beginning of the operation are independent risk factors for intraoperative hypothermia in patients undergoing general anesthesia. Clinical medical staff should identify the high-risk groups of intraoperative hypothermia in patients undergoing general anesthesia intervention, and implement efficient intraoperative hypothermia management for patients undergoing general anesthesia intervention in a timely manner to reduce the incidence of intraoperative hypothermia.
References
1. Warttig S, Alderson P, Campbell G, Interventions for treating inadvertent postoperative hypothermia: Cochrane Database Syst Rev, 2014; 2014(11); CD009892
2. Akers JL, Dupnick AC, Hillman EL, Inadvertent perioperative hypothermia risks and postoperative complications: A retrospective study: AORN J, 2019; 109(6); 741-47
3. Schmied H, Kurz A, Sessler DI, Mild hypothermia increases blood loss and transfusion requirements during total hip arthroplasty: Lancet, 1996; 347; 289-92
4. Campbell G, Alderson P, Smith AF, Warming of intravenous and irrigation fluids for preventing inadvertent perioperative hypothermia: Cochrane Database Syst Rev, 2015; 2015(4); CD009891
5. Li Y, Liang HS, Feng Y, Prevalence and multivariable factors associated with inadvertent intraoperative hypothermia in video-assisted thoracoscopic surgery: A single-center retrospective study: BMC Anesthesiology, 2020; 20(1); 25
6. Simegn GD, Bayable SD, Fetene MB, Prevention and management of perioperative hypothermia in adult elective surgical patients: A systematic review: Ann Med Surg (Lond), 2021; 72; 103059
7. Jeican II, The pathophysiological mechanisms of the onset of death through accidental hypothermia and the presentation of “The little match girl” case: Clujul Med, 2014; 87(1); 54-60
8. De Filippo M, Brunese L, Reginelli A, Advances in diagnostic and interventional radiology: Acta Biomed 24, 2019; 90(5-S); 5-8
9. Hong JM, Lee JS, Song HJ, Therapeutic hypothermia after recanalization in patients with acute ischemic stroke: Stroke, 2014; 45(1); 134-40
10. Xu R, Nair SK, Kilgore CB, Hypothermia is associated with improved neurological outcomes after mechanical thrombectomy: World Neurosurg, 2024; 181; e126-e32
11. Li L, Lu Y, Yang LL, Construction and validation of postoperative hypothermia prediction model for patients undergoing joint replacement surgery: J Clin Nurs, 2023; 32(13–14); 3831-39
12. Wu YT, Influencing factors and nursing intervention strategies of intraoperative hypothermia in elderly orthopedic patients: Gen Pract Nurs, 2019; 19(26); 3663-66
13. Han SJ, Tan ZH, He HF, Effect of composite thermal insulation nursing mode on incidence of hypothermia and surgical outcome in high-risk patients undergoing thoracic surgery: J Clin Nurs, 2019; 20(04); 53-55
14. National Quality Control Center of Anesthesia Specialties, Chinese Medical Association Anesthesiology Branch, Expert consensus on prevention and treatment of hypothermia in perioperative patients (2017): Concord Med J, 2017; 8(6); 352-58
15. Warttig S, Alderson P, Campbell G, Interventions for treating inadvertent postoperative hypothermia: Cochrane Database Syst Rev, 2014(11); CD009892
16. Duong H, Patel G, Hypothermia. [Updated 2022 Jan 24]: StatPearls [Internet], 2023, Treasure Island (FL), StatPearls Publishing Available from: https://www.ncbi.nlm.nih.gov/books/NBK545239/
17. Madrid E, Urrútia G, Roqué i Figuls M, Active body surface warming systems for preventing complications caused by inadvertent perioperative hypothermia in adults: Cochrane Database Syst Rev, 2016; 4(4); CD009016
18. Frisch NB, Pepper AM, Rooney E, Intraoperative hypothermia in total hip and knee arthroplasty: Orthopedics, 2017; 40(1); 56-63
19. Güven B, İbrahimoğlu Ö, Kuş İ, Inadvertent perioperative hypothermia in ambulatory surgery patients: Incidence, risk factors, and prevention initiatives: J Perianesth Nurs, 2023; 38(5); 792-98
20. Wang YY, Gao X, The application of comprehensive intervention in the prevention of intraoperative hypothermia in elderly patients: Chinese Journal of Gerontology, 2019; 41(3); 558-61
21. Emmert A, Gries G, Wand S, Association between perioperative hypothermia and patient outcomes after thoracic surgery: A single center retrospective analysis: Medicine (Baltimore), 2018; 97(17); e0528
22. Xiong C, Gao XL, Xiang YT, Meta-analysis of influencing factors of intraoperative hypothermia in adult surgical patients: J Nurs, 2018; 25(2); 48-53
23. Li L, Yan Y, Fang X, Construction and verification of intraoperative hypothermia risk prediction model for patients undergoing laparoscopic surgery: Chinese Journal of Nursing, 2019; 57(4); 463-68
24. Lai LL, See MH, Rampal S, Significant factors influencing inadvertent hypothermia in pediatric anesthesia: J Clin Monit Comput, 2019; 33(6); 1105-12
25. Tong M, Zhou XY, Effect of warm air heater on prevention of hypothermia on recovery of cesarean section patient: Maternal and Child Health Care in China, 2021; 36(15); 3632-36
26. Moola S, Lockwood C, Effectiveness of strategies for the management and/or prevention of hypothermia within the adult perioperative environment: Int J Evid Based Healthc, 2011; 9(4); 337-45
27. Lee SY, Kim SJ, Jung JY, Effects of 10-min prewarming on core body temperature during gynecologic laparoscopic surgery under general anesthesia: A randomized controlled trial: Anesth Pain Med (Seoul), 2020; 15(3); 349-55
28. Ma ZL, Yi J, Expert consensus on prevention and treatment of hypothermia in perioperative patients (2017): Concord Med J, 2017; 8(06); 352-58
In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952